- Open access
- Published: 27 June 2011

The case study approach
- Sarah Crowe 1 ,
- Kathrin Cresswell 2 ,
- Ann Robertson 2 ,
- Guro Huby 3 ,
- Anthony Avery 1 &
- Aziz Sheikh 2
BMC Medical Research Methodology volume 11 , Article number: 100 ( 2011 ) Cite this article
796k Accesses
1111 Citations
42 Altmetric
Metrics details
The case study approach allows in-depth, multi-faceted explorations of complex issues in their real-life settings. The value of the case study approach is well recognised in the fields of business, law and policy, but somewhat less so in health services research. Based on our experiences of conducting several health-related case studies, we reflect on the different types of case study design, the specific research questions this approach can help answer, the data sources that tend to be used, and the particular advantages and disadvantages of employing this methodological approach. The paper concludes with key pointers to aid those designing and appraising proposals for conducting case study research, and a checklist to help readers assess the quality of case study reports.
Peer Review reports
Introduction
The case study approach is particularly useful to employ when there is a need to obtain an in-depth appreciation of an issue, event or phenomenon of interest, in its natural real-life context. Our aim in writing this piece is to provide insights into when to consider employing this approach and an overview of key methodological considerations in relation to the design, planning, analysis, interpretation and reporting of case studies.
The illustrative 'grand round', 'case report' and 'case series' have a long tradition in clinical practice and research. Presenting detailed critiques, typically of one or more patients, aims to provide insights into aspects of the clinical case and, in doing so, illustrate broader lessons that may be learnt. In research, the conceptually-related case study approach can be used, for example, to describe in detail a patient's episode of care, explore professional attitudes to and experiences of a new policy initiative or service development or more generally to 'investigate contemporary phenomena within its real-life context' [ 1 ]. Based on our experiences of conducting a range of case studies, we reflect on when to consider using this approach, discuss the key steps involved and illustrate, with examples, some of the practical challenges of attaining an in-depth understanding of a 'case' as an integrated whole. In keeping with previously published work, we acknowledge the importance of theory to underpin the design, selection, conduct and interpretation of case studies[ 2 ]. In so doing, we make passing reference to the different epistemological approaches used in case study research by key theoreticians and methodologists in this field of enquiry.
This paper is structured around the following main questions: What is a case study? What are case studies used for? How are case studies conducted? What are the potential pitfalls and how can these be avoided? We draw in particular on four of our own recently published examples of case studies (see Tables 1 , 2 , 3 and 4 ) and those of others to illustrate our discussion[ 3 – 7 ].
What is a case study?
A case study is a research approach that is used to generate an in-depth, multi-faceted understanding of a complex issue in its real-life context. It is an established research design that is used extensively in a wide variety of disciplines, particularly in the social sciences. A case study can be defined in a variety of ways (Table 5 ), the central tenet being the need to explore an event or phenomenon in depth and in its natural context. It is for this reason sometimes referred to as a "naturalistic" design; this is in contrast to an "experimental" design (such as a randomised controlled trial) in which the investigator seeks to exert control over and manipulate the variable(s) of interest.
Stake's work has been particularly influential in defining the case study approach to scientific enquiry. He has helpfully characterised three main types of case study: intrinsic , instrumental and collective [ 8 ]. An intrinsic case study is typically undertaken to learn about a unique phenomenon. The researcher should define the uniqueness of the phenomenon, which distinguishes it from all others. In contrast, the instrumental case study uses a particular case (some of which may be better than others) to gain a broader appreciation of an issue or phenomenon. The collective case study involves studying multiple cases simultaneously or sequentially in an attempt to generate a still broader appreciation of a particular issue.
These are however not necessarily mutually exclusive categories. In the first of our examples (Table 1 ), we undertook an intrinsic case study to investigate the issue of recruitment of minority ethnic people into the specific context of asthma research studies, but it developed into a instrumental case study through seeking to understand the issue of recruitment of these marginalised populations more generally, generating a number of the findings that are potentially transferable to other disease contexts[ 3 ]. In contrast, the other three examples (see Tables 2 , 3 and 4 ) employed collective case study designs to study the introduction of workforce reconfiguration in primary care, the implementation of electronic health records into hospitals, and to understand the ways in which healthcare students learn about patient safety considerations[ 4 – 6 ]. Although our study focusing on the introduction of General Practitioners with Specialist Interests (Table 2 ) was explicitly collective in design (four contrasting primary care organisations were studied), is was also instrumental in that this particular professional group was studied as an exemplar of the more general phenomenon of workforce redesign[ 4 ].
What are case studies used for?
According to Yin, case studies can be used to explain, describe or explore events or phenomena in the everyday contexts in which they occur[ 1 ]. These can, for example, help to understand and explain causal links and pathways resulting from a new policy initiative or service development (see Tables 2 and 3 , for example)[ 1 ]. In contrast to experimental designs, which seek to test a specific hypothesis through deliberately manipulating the environment (like, for example, in a randomised controlled trial giving a new drug to randomly selected individuals and then comparing outcomes with controls),[ 9 ] the case study approach lends itself well to capturing information on more explanatory ' how ', 'what' and ' why ' questions, such as ' how is the intervention being implemented and received on the ground?'. The case study approach can offer additional insights into what gaps exist in its delivery or why one implementation strategy might be chosen over another. This in turn can help develop or refine theory, as shown in our study of the teaching of patient safety in undergraduate curricula (Table 4 )[ 6 , 10 ]. Key questions to consider when selecting the most appropriate study design are whether it is desirable or indeed possible to undertake a formal experimental investigation in which individuals and/or organisations are allocated to an intervention or control arm? Or whether the wish is to obtain a more naturalistic understanding of an issue? The former is ideally studied using a controlled experimental design, whereas the latter is more appropriately studied using a case study design.
Case studies may be approached in different ways depending on the epistemological standpoint of the researcher, that is, whether they take a critical (questioning one's own and others' assumptions), interpretivist (trying to understand individual and shared social meanings) or positivist approach (orientating towards the criteria of natural sciences, such as focusing on generalisability considerations) (Table 6 ). Whilst such a schema can be conceptually helpful, it may be appropriate to draw on more than one approach in any case study, particularly in the context of conducting health services research. Doolin has, for example, noted that in the context of undertaking interpretative case studies, researchers can usefully draw on a critical, reflective perspective which seeks to take into account the wider social and political environment that has shaped the case[ 11 ].
How are case studies conducted?
Here, we focus on the main stages of research activity when planning and undertaking a case study; the crucial stages are: defining the case; selecting the case(s); collecting and analysing the data; interpreting data; and reporting the findings.
Defining the case
Carefully formulated research question(s), informed by the existing literature and a prior appreciation of the theoretical issues and setting(s), are all important in appropriately and succinctly defining the case[ 8 , 12 ]. Crucially, each case should have a pre-defined boundary which clarifies the nature and time period covered by the case study (i.e. its scope, beginning and end), the relevant social group, organisation or geographical area of interest to the investigator, the types of evidence to be collected, and the priorities for data collection and analysis (see Table 7 )[ 1 ]. A theory driven approach to defining the case may help generate knowledge that is potentially transferable to a range of clinical contexts and behaviours; using theory is also likely to result in a more informed appreciation of, for example, how and why interventions have succeeded or failed[ 13 ].
For example, in our evaluation of the introduction of electronic health records in English hospitals (Table 3 ), we defined our cases as the NHS Trusts that were receiving the new technology[ 5 ]. Our focus was on how the technology was being implemented. However, if the primary research interest had been on the social and organisational dimensions of implementation, we might have defined our case differently as a grouping of healthcare professionals (e.g. doctors and/or nurses). The precise beginning and end of the case may however prove difficult to define. Pursuing this same example, when does the process of implementation and adoption of an electronic health record system really begin or end? Such judgements will inevitably be influenced by a range of factors, including the research question, theory of interest, the scope and richness of the gathered data and the resources available to the research team.
Selecting the case(s)
The decision on how to select the case(s) to study is a very important one that merits some reflection. In an intrinsic case study, the case is selected on its own merits[ 8 ]. The case is selected not because it is representative of other cases, but because of its uniqueness, which is of genuine interest to the researchers. This was, for example, the case in our study of the recruitment of minority ethnic participants into asthma research (Table 1 ) as our earlier work had demonstrated the marginalisation of minority ethnic people with asthma, despite evidence of disproportionate asthma morbidity[ 14 , 15 ]. In another example of an intrinsic case study, Hellstrom et al.[ 16 ] studied an elderly married couple living with dementia to explore how dementia had impacted on their understanding of home, their everyday life and their relationships.
For an instrumental case study, selecting a "typical" case can work well[ 8 ]. In contrast to the intrinsic case study, the particular case which is chosen is of less importance than selecting a case that allows the researcher to investigate an issue or phenomenon. For example, in order to gain an understanding of doctors' responses to health policy initiatives, Som undertook an instrumental case study interviewing clinicians who had a range of responsibilities for clinical governance in one NHS acute hospital trust[ 17 ]. Sampling a "deviant" or "atypical" case may however prove even more informative, potentially enabling the researcher to identify causal processes, generate hypotheses and develop theory.
In collective or multiple case studies, a number of cases are carefully selected. This offers the advantage of allowing comparisons to be made across several cases and/or replication. Choosing a "typical" case may enable the findings to be generalised to theory (i.e. analytical generalisation) or to test theory by replicating the findings in a second or even a third case (i.e. replication logic)[ 1 ]. Yin suggests two or three literal replications (i.e. predicting similar results) if the theory is straightforward and five or more if the theory is more subtle. However, critics might argue that selecting 'cases' in this way is insufficiently reflexive and ill-suited to the complexities of contemporary healthcare organisations.
The selected case study site(s) should allow the research team access to the group of individuals, the organisation, the processes or whatever else constitutes the chosen unit of analysis for the study. Access is therefore a central consideration; the researcher needs to come to know the case study site(s) well and to work cooperatively with them. Selected cases need to be not only interesting but also hospitable to the inquiry [ 8 ] if they are to be informative and answer the research question(s). Case study sites may also be pre-selected for the researcher, with decisions being influenced by key stakeholders. For example, our selection of case study sites in the evaluation of the implementation and adoption of electronic health record systems (see Table 3 ) was heavily influenced by NHS Connecting for Health, the government agency that was responsible for overseeing the National Programme for Information Technology (NPfIT)[ 5 ]. This prominent stakeholder had already selected the NHS sites (through a competitive bidding process) to be early adopters of the electronic health record systems and had negotiated contracts that detailed the deployment timelines.
It is also important to consider in advance the likely burden and risks associated with participation for those who (or the site(s) which) comprise the case study. Of particular importance is the obligation for the researcher to think through the ethical implications of the study (e.g. the risk of inadvertently breaching anonymity or confidentiality) and to ensure that potential participants/participating sites are provided with sufficient information to make an informed choice about joining the study. The outcome of providing this information might be that the emotive burden associated with participation, or the organisational disruption associated with supporting the fieldwork, is considered so high that the individuals or sites decide against participation.
In our example of evaluating implementations of electronic health record systems, given the restricted number of early adopter sites available to us, we sought purposively to select a diverse range of implementation cases among those that were available[ 5 ]. We chose a mixture of teaching, non-teaching and Foundation Trust hospitals, and examples of each of the three electronic health record systems procured centrally by the NPfIT. At one recruited site, it quickly became apparent that access was problematic because of competing demands on that organisation. Recognising the importance of full access and co-operative working for generating rich data, the research team decided not to pursue work at that site and instead to focus on other recruited sites.
Collecting the data
In order to develop a thorough understanding of the case, the case study approach usually involves the collection of multiple sources of evidence, using a range of quantitative (e.g. questionnaires, audits and analysis of routinely collected healthcare data) and more commonly qualitative techniques (e.g. interviews, focus groups and observations). The use of multiple sources of data (data triangulation) has been advocated as a way of increasing the internal validity of a study (i.e. the extent to which the method is appropriate to answer the research question)[ 8 , 18 – 21 ]. An underlying assumption is that data collected in different ways should lead to similar conclusions, and approaching the same issue from different angles can help develop a holistic picture of the phenomenon (Table 2 )[ 4 ].
Brazier and colleagues used a mixed-methods case study approach to investigate the impact of a cancer care programme[ 22 ]. Here, quantitative measures were collected with questionnaires before, and five months after, the start of the intervention which did not yield any statistically significant results. Qualitative interviews with patients however helped provide an insight into potentially beneficial process-related aspects of the programme, such as greater, perceived patient involvement in care. The authors reported how this case study approach provided a number of contextual factors likely to influence the effectiveness of the intervention and which were not likely to have been obtained from quantitative methods alone.
In collective or multiple case studies, data collection needs to be flexible enough to allow a detailed description of each individual case to be developed (e.g. the nature of different cancer care programmes), before considering the emerging similarities and differences in cross-case comparisons (e.g. to explore why one programme is more effective than another). It is important that data sources from different cases are, where possible, broadly comparable for this purpose even though they may vary in nature and depth.
Analysing, interpreting and reporting case studies
Making sense and offering a coherent interpretation of the typically disparate sources of data (whether qualitative alone or together with quantitative) is far from straightforward. Repeated reviewing and sorting of the voluminous and detail-rich data are integral to the process of analysis. In collective case studies, it is helpful to analyse data relating to the individual component cases first, before making comparisons across cases. Attention needs to be paid to variations within each case and, where relevant, the relationship between different causes, effects and outcomes[ 23 ]. Data will need to be organised and coded to allow the key issues, both derived from the literature and emerging from the dataset, to be easily retrieved at a later stage. An initial coding frame can help capture these issues and can be applied systematically to the whole dataset with the aid of a qualitative data analysis software package.
The Framework approach is a practical approach, comprising of five stages (familiarisation; identifying a thematic framework; indexing; charting; mapping and interpretation) , to managing and analysing large datasets particularly if time is limited, as was the case in our study of recruitment of South Asians into asthma research (Table 1 )[ 3 , 24 ]. Theoretical frameworks may also play an important role in integrating different sources of data and examining emerging themes. For example, we drew on a socio-technical framework to help explain the connections between different elements - technology; people; and the organisational settings within which they worked - in our study of the introduction of electronic health record systems (Table 3 )[ 5 ]. Our study of patient safety in undergraduate curricula drew on an evaluation-based approach to design and analysis, which emphasised the importance of the academic, organisational and practice contexts through which students learn (Table 4 )[ 6 ].
Case study findings can have implications both for theory development and theory testing. They may establish, strengthen or weaken historical explanations of a case and, in certain circumstances, allow theoretical (as opposed to statistical) generalisation beyond the particular cases studied[ 12 ]. These theoretical lenses should not, however, constitute a strait-jacket and the cases should not be "forced to fit" the particular theoretical framework that is being employed.
When reporting findings, it is important to provide the reader with enough contextual information to understand the processes that were followed and how the conclusions were reached. In a collective case study, researchers may choose to present the findings from individual cases separately before amalgamating across cases. Care must be taken to ensure the anonymity of both case sites and individual participants (if agreed in advance) by allocating appropriate codes or withholding descriptors. In the example given in Table 3 , we decided against providing detailed information on the NHS sites and individual participants in order to avoid the risk of inadvertent disclosure of identities[ 5 , 25 ].
What are the potential pitfalls and how can these be avoided?
The case study approach is, as with all research, not without its limitations. When investigating the formal and informal ways undergraduate students learn about patient safety (Table 4 ), for example, we rapidly accumulated a large quantity of data. The volume of data, together with the time restrictions in place, impacted on the depth of analysis that was possible within the available resources. This highlights a more general point of the importance of avoiding the temptation to collect as much data as possible; adequate time also needs to be set aside for data analysis and interpretation of what are often highly complex datasets.
Case study research has sometimes been criticised for lacking scientific rigour and providing little basis for generalisation (i.e. producing findings that may be transferable to other settings)[ 1 ]. There are several ways to address these concerns, including: the use of theoretical sampling (i.e. drawing on a particular conceptual framework); respondent validation (i.e. participants checking emerging findings and the researcher's interpretation, and providing an opinion as to whether they feel these are accurate); and transparency throughout the research process (see Table 8 )[ 8 , 18 – 21 , 23 , 26 ]. Transparency can be achieved by describing in detail the steps involved in case selection, data collection, the reasons for the particular methods chosen, and the researcher's background and level of involvement (i.e. being explicit about how the researcher has influenced data collection and interpretation). Seeking potential, alternative explanations, and being explicit about how interpretations and conclusions were reached, help readers to judge the trustworthiness of the case study report. Stake provides a critique checklist for a case study report (Table 9 )[ 8 ].
Conclusions
The case study approach allows, amongst other things, critical events, interventions, policy developments and programme-based service reforms to be studied in detail in a real-life context. It should therefore be considered when an experimental design is either inappropriate to answer the research questions posed or impossible to undertake. Considering the frequency with which implementations of innovations are now taking place in healthcare settings and how well the case study approach lends itself to in-depth, complex health service research, we believe this approach should be more widely considered by researchers. Though inherently challenging, the research case study can, if carefully conceptualised and thoughtfully undertaken and reported, yield powerful insights into many important aspects of health and healthcare delivery.
Yin RK: Case study research, design and method. 2009, London: Sage Publications Ltd., 4
Google Scholar
Keen J, Packwood T: Qualitative research; case study evaluation. BMJ. 1995, 311: 444-446.
Article CAS PubMed PubMed Central Google Scholar
Sheikh A, Halani L, Bhopal R, Netuveli G, Partridge M, Car J, et al: Facilitating the Recruitment of Minority Ethnic People into Research: Qualitative Case Study of South Asians and Asthma. PLoS Med. 2009, 6 (10): 1-11.
Article Google Scholar
Pinnock H, Huby G, Powell A, Kielmann T, Price D, Williams S, et al: The process of planning, development and implementation of a General Practitioner with a Special Interest service in Primary Care Organisations in England and Wales: a comparative prospective case study. Report for the National Co-ordinating Centre for NHS Service Delivery and Organisation R&D (NCCSDO). 2008, [ http://www.sdo.nihr.ac.uk/files/project/99-final-report.pdf ]
Robertson A, Cresswell K, Takian A, Petrakaki D, Crowe S, Cornford T, et al: Prospective evaluation of the implementation and adoption of NHS Connecting for Health's national electronic health record in secondary care in England: interim findings. BMJ. 2010, 41: c4564-
Pearson P, Steven A, Howe A, Sheikh A, Ashcroft D, Smith P, the Patient Safety Education Study Group: Learning about patient safety: organisational context and culture in the education of healthcare professionals. J Health Serv Res Policy. 2010, 15: 4-10. 10.1258/jhsrp.2009.009052.
Article PubMed Google Scholar
van Harten WH, Casparie TF, Fisscher OA: The evaluation of the introduction of a quality management system: a process-oriented case study in a large rehabilitation hospital. Health Policy. 2002, 60 (1): 17-37. 10.1016/S0168-8510(01)00187-7.
Stake RE: The art of case study research. 1995, London: Sage Publications Ltd.
Sheikh A, Smeeth L, Ashcroft R: Randomised controlled trials in primary care: scope and application. Br J Gen Pract. 2002, 52 (482): 746-51.
PubMed PubMed Central Google Scholar
King G, Keohane R, Verba S: Designing Social Inquiry. 1996, Princeton: Princeton University Press
Doolin B: Information technology as disciplinary technology: being critical in interpretative research on information systems. Journal of Information Technology. 1998, 13: 301-311. 10.1057/jit.1998.8.
George AL, Bennett A: Case studies and theory development in the social sciences. 2005, Cambridge, MA: MIT Press
Eccles M, the Improved Clinical Effectiveness through Behavioural Research Group (ICEBeRG): Designing theoretically-informed implementation interventions. Implementation Science. 2006, 1: 1-8. 10.1186/1748-5908-1-1.
Article PubMed Central Google Scholar
Netuveli G, Hurwitz B, Levy M, Fletcher M, Barnes G, Durham SR, Sheikh A: Ethnic variations in UK asthma frequency, morbidity, and health-service use: a systematic review and meta-analysis. Lancet. 2005, 365 (9456): 312-7.
Sheikh A, Panesar SS, Lasserson T, Netuveli G: Recruitment of ethnic minorities to asthma studies. Thorax. 2004, 59 (7): 634-
CAS PubMed PubMed Central Google Scholar
Hellström I, Nolan M, Lundh U: 'We do things together': A case study of 'couplehood' in dementia. Dementia. 2005, 4: 7-22. 10.1177/1471301205049188.
Som CV: Nothing seems to have changed, nothing seems to be changing and perhaps nothing will change in the NHS: doctors' response to clinical governance. International Journal of Public Sector Management. 2005, 18: 463-477. 10.1108/09513550510608903.
Lincoln Y, Guba E: Naturalistic inquiry. 1985, Newbury Park: Sage Publications
Barbour RS: Checklists for improving rigour in qualitative research: a case of the tail wagging the dog?. BMJ. 2001, 322: 1115-1117. 10.1136/bmj.322.7294.1115.
Mays N, Pope C: Qualitative research in health care: Assessing quality in qualitative research. BMJ. 2000, 320: 50-52. 10.1136/bmj.320.7226.50.
Mason J: Qualitative researching. 2002, London: Sage
Brazier A, Cooke K, Moravan V: Using Mixed Methods for Evaluating an Integrative Approach to Cancer Care: A Case Study. Integr Cancer Ther. 2008, 7: 5-17. 10.1177/1534735407313395.
Miles MB, Huberman M: Qualitative data analysis: an expanded sourcebook. 1994, CA: Sage Publications Inc., 2
Pope C, Ziebland S, Mays N: Analysing qualitative data. Qualitative research in health care. BMJ. 2000, 320: 114-116. 10.1136/bmj.320.7227.114.
Cresswell KM, Worth A, Sheikh A: Actor-Network Theory and its role in understanding the implementation of information technology developments in healthcare. BMC Med Inform Decis Mak. 2010, 10 (1): 67-10.1186/1472-6947-10-67.
Article PubMed PubMed Central Google Scholar
Malterud K: Qualitative research: standards, challenges, and guidelines. Lancet. 2001, 358: 483-488. 10.1016/S0140-6736(01)05627-6.
Article CAS PubMed Google Scholar
Yin R: Case study research: design and methods. 1994, Thousand Oaks, CA: Sage Publishing, 2
Yin R: Enhancing the quality of case studies in health services research. Health Serv Res. 1999, 34: 1209-1224.
Green J, Thorogood N: Qualitative methods for health research. 2009, Los Angeles: Sage, 2
Howcroft D, Trauth E: Handbook of Critical Information Systems Research, Theory and Application. 2005, Cheltenham, UK: Northampton, MA, USA: Edward Elgar
Book Google Scholar
Blakie N: Approaches to Social Enquiry. 1993, Cambridge: Polity Press
Doolin B: Power and resistance in the implementation of a medical management information system. Info Systems J. 2004, 14: 343-362. 10.1111/j.1365-2575.2004.00176.x.
Bloomfield BP, Best A: Management consultants: systems development, power and the translation of problems. Sociological Review. 1992, 40: 533-560.
Shanks G, Parr A: Positivist, single case study research in information systems: A critical analysis. Proceedings of the European Conference on Information Systems. 2003, Naples
Pre-publication history
The pre-publication history for this paper can be accessed here: http://www.biomedcentral.com/1471-2288/11/100/prepub
Download references
Acknowledgements
We are grateful to the participants and colleagues who contributed to the individual case studies that we have drawn on. This work received no direct funding, but it has been informed by projects funded by Asthma UK, the NHS Service Delivery Organisation, NHS Connecting for Health Evaluation Programme, and Patient Safety Research Portfolio. We would also like to thank the expert reviewers for their insightful and constructive feedback. Our thanks are also due to Dr. Allison Worth who commented on an earlier draft of this manuscript.
Author information
Authors and affiliations.
Division of Primary Care, The University of Nottingham, Nottingham, UK
Sarah Crowe & Anthony Avery
Centre for Population Health Sciences, The University of Edinburgh, Edinburgh, UK
Kathrin Cresswell, Ann Robertson & Aziz Sheikh
School of Health in Social Science, The University of Edinburgh, Edinburgh, UK
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Sarah Crowe .
Additional information
Competing interests.
The authors declare that they have no competing interests.
Authors' contributions
AS conceived this article. SC, KC and AR wrote this paper with GH, AA and AS all commenting on various drafts. SC and AS are guarantors.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License ( http://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Reprints and permissions
About this article
Cite this article.
Crowe, S., Cresswell, K., Robertson, A. et al. The case study approach. BMC Med Res Methodol 11 , 100 (2011). https://doi.org/10.1186/1471-2288-11-100
Download citation
Received : 29 November 2010
Accepted : 27 June 2011
Published : 27 June 2011
DOI : https://doi.org/10.1186/1471-2288-11-100
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Case Study Approach
- Electronic Health Record System
- Case Study Design
- Case Study Site
- Case Study Report
BMC Medical Research Methodology
ISSN: 1471-2288
- General enquiries: [email protected]
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Published: November 2006
Case Studies: why are they important?
- Julie Solomon 1
Nature Clinical Practice Cardiovascular Medicine volume 3 , page 579 ( 2006 ) Cite this article
19k Accesses
9 Citations
Metrics details
Nature Clinical Practice Cardiovascular Medicine is a journal designed to lighten the reading load for busy doctors; why, then, does it include Case Studies? Isn't the case study just a bit of light reading? It depends on what it is designed to do. So, what is the role of the Case Study?
Case Studies should act as instructive examples to people who might encounter similar problems. Ideally, in medicine, Case Studies should detail a particular medical case, describing the background of the patient and any clues the physician picked up (or should have, with hindsight). They should discuss investigations undertaken in order to determine a diagnosis or differentiate between possible diagnoses, and should indicate the course of treatment the patient underwent as a result. As a whole, then, Case Studies should be an informative and useful part of every physician's medical education, both during training and on a continuing basis.
It's debatable whether they always achieve this aim. Many journals publish what are often close to anecdotal reports (if they publish articles on individual cases at all), rather than detailed descriptions of a case; furthermore, the cases described are often esoteric or the conditions present on such an infrequent basis that a physician working outside a teaching-hospital environment would be hard-pressed to apply their new knowledge. It would be difficult, therefore, to say whether any conclusions could confidently be drawn by readers as a result of these reports. Most physicians would probably want to do some extra research—either in the literature or by canvassing opinions of colleagues.
By proposing, peer-reviewing and reading the Case Studies, you and your fellow physicians could gain a broader understanding of clinical diagnoses, treatments and outcomes.
In this light, then, Nature Clinical Practice Cardiovascular Medicine Case Studies have a specific aim: to help established physicians as well as trainees to improve patient care, without adding to their workload. Rather than being merely anecdotal, they include the etiology, diagnosis and management of a case. Importantly, they give an indication of the decision-making process, so that other physicians can apply lateral thinking to their own cases. Decisions on which of a range of treatment options to follow might involve input from the patient, or might be purely objective, but ideally a Case Study should outline why a particular course was followed. Readers should not have to resort to the Internet or to out-of-date textbooks to find basic background information explaining the reasons for approaching the case in that way; the reasons should be fully explained in the article itself.
Nature Clinical Practice Cardiovascular Medicine Case Studies represent an opportunity to spread the benefit of knowledge across the physical boundaries imposed by looking at one case, in one place, at one time. It's not so that fingers can be pointed at 'incorrect' treatment but instead so that geographical differences in practice can be highlighted, for example, or clearer descriptions be reached to explain a case more completely and accurately.
By proposing, peer-reviewing and reading the Case Studies, you and your fellow physicians could gain a broader understanding of clinical diagnoses, treatments and outcomes. So, we're inviting you to contribute to the further education of your colleagues. Will you meet the challenge?
Author information
Authors and affiliations.
Assistant Publisher of the Nature Clinical Practice journals,
Julie Solomon
You can also search for this author in PubMed Google Scholar
Ethics declarations
Competing interests.
The author declares no competing financial interests.
Rights and permissions
Reprints and permissions
About this article
Cite this article.
Solomon, J. Case Studies: why are they important?. Nat Rev Cardiol 3 , 579 (2006). https://doi.org/10.1038/ncpcardio0704
Download citation
Issue Date : November 2006
DOI : https://doi.org/10.1038/ncpcardio0704
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Have a language expert improve your writing
Run a free plagiarism check in 10 minutes, generate accurate citations for free.
- Knowledge Base
Methodology
- What Is a Case Study? | Definition, Examples & Methods
What Is a Case Study? | Definition, Examples & Methods
Published on May 8, 2019 by Shona McCombes . Revised on November 20, 2023.
A case study is a detailed study of a specific subject, such as a person, group, place, event, organization, or phenomenon. Case studies are commonly used in social, educational, clinical, and business research.
A case study research design usually involves qualitative methods , but quantitative methods are sometimes also used. Case studies are good for describing , comparing, evaluating and understanding different aspects of a research problem .
Table of contents
When to do a case study, step 1: select a case, step 2: build a theoretical framework, step 3: collect your data, step 4: describe and analyze the case, other interesting articles.
A case study is an appropriate research design when you want to gain concrete, contextual, in-depth knowledge about a specific real-world subject. It allows you to explore the key characteristics, meanings, and implications of the case.
Case studies are often a good choice in a thesis or dissertation . They keep your project focused and manageable when you don’t have the time or resources to do large-scale research.
You might use just one complex case study where you explore a single subject in depth, or conduct multiple case studies to compare and illuminate different aspects of your research problem.
| Research question | Case study |
|---|---|
| What are the ecological effects of wolf reintroduction? | Case study of wolf reintroduction in Yellowstone National Park |
| How do populist politicians use narratives about history to gain support? | Case studies of Hungarian prime minister Viktor Orbán and US president Donald Trump |
| How can teachers implement active learning strategies in mixed-level classrooms? | Case study of a local school that promotes active learning |
| What are the main advantages and disadvantages of wind farms for rural communities? | Case studies of three rural wind farm development projects in different parts of the country |
| How are viral marketing strategies changing the relationship between companies and consumers? | Case study of the iPhone X marketing campaign |
| How do experiences of work in the gig economy differ by gender, race and age? | Case studies of Deliveroo and Uber drivers in London |
Prevent plagiarism. Run a free check.
Once you have developed your problem statement and research questions , you should be ready to choose the specific case that you want to focus on. A good case study should have the potential to:
- Provide new or unexpected insights into the subject
- Challenge or complicate existing assumptions and theories
- Propose practical courses of action to resolve a problem
- Open up new directions for future research
TipIf your research is more practical in nature and aims to simultaneously investigate an issue as you solve it, consider conducting action research instead.
Unlike quantitative or experimental research , a strong case study does not require a random or representative sample. In fact, case studies often deliberately focus on unusual, neglected, or outlying cases which may shed new light on the research problem.
Example of an outlying case studyIn the 1960s the town of Roseto, Pennsylvania was discovered to have extremely low rates of heart disease compared to the US average. It became an important case study for understanding previously neglected causes of heart disease.
However, you can also choose a more common or representative case to exemplify a particular category, experience or phenomenon.
Example of a representative case studyIn the 1920s, two sociologists used Muncie, Indiana as a case study of a typical American city that supposedly exemplified the changing culture of the US at the time.
While case studies focus more on concrete details than general theories, they should usually have some connection with theory in the field. This way the case study is not just an isolated description, but is integrated into existing knowledge about the topic. It might aim to:
- Exemplify a theory by showing how it explains the case under investigation
- Expand on a theory by uncovering new concepts and ideas that need to be incorporated
- Challenge a theory by exploring an outlier case that doesn’t fit with established assumptions
To ensure that your analysis of the case has a solid academic grounding, you should conduct a literature review of sources related to the topic and develop a theoretical framework . This means identifying key concepts and theories to guide your analysis and interpretation.
There are many different research methods you can use to collect data on your subject. Case studies tend to focus on qualitative data using methods such as interviews , observations , and analysis of primary and secondary sources (e.g., newspaper articles, photographs, official records). Sometimes a case study will also collect quantitative data.
Example of a mixed methods case studyFor a case study of a wind farm development in a rural area, you could collect quantitative data on employment rates and business revenue, collect qualitative data on local people’s perceptions and experiences, and analyze local and national media coverage of the development.
The aim is to gain as thorough an understanding as possible of the case and its context.
In writing up the case study, you need to bring together all the relevant aspects to give as complete a picture as possible of the subject.
How you report your findings depends on the type of research you are doing. Some case studies are structured like a standard scientific paper or thesis , with separate sections or chapters for the methods , results and discussion .
Others are written in a more narrative style, aiming to explore the case from various angles and analyze its meanings and implications (for example, by using textual analysis or discourse analysis ).
In all cases, though, make sure to give contextual details about the case, connect it back to the literature and theory, and discuss how it fits into wider patterns or debates.
If you want to know more about statistics , methodology , or research bias , make sure to check out some of our other articles with explanations and examples.
- Normal distribution
- Degrees of freedom
- Null hypothesis
- Discourse analysis
- Control groups
- Mixed methods research
- Non-probability sampling
- Quantitative research
- Ecological validity
Research bias
- Rosenthal effect
- Implicit bias
- Cognitive bias
- Selection bias
- Negativity bias
- Status quo bias
Cite this Scribbr article
If you want to cite this source, you can copy and paste the citation or click the “Cite this Scribbr article” button to automatically add the citation to our free Citation Generator.
McCombes, S. (2023, November 20). What Is a Case Study? | Definition, Examples & Methods. Scribbr. Retrieved September 4, 2024, from https://www.scribbr.com/methodology/case-study/
Is this article helpful?
Shona McCombes
Other students also liked, primary vs. secondary sources | difference & examples, what is a theoretical framework | guide to organizing, what is action research | definition & examples, get unlimited documents corrected.
✔ Free APA citation check included ✔ Unlimited document corrections ✔ Specialized in correcting academic texts
- Open access
- Published: 15 May 2024
Learning together for better health using an evidence-based Learning Health System framework: a case study in stroke
- Helena Teede 1 , 2 na1 ,
- Dominique A. Cadilhac 3 , 4 na1 ,
- Tara Purvis 3 ,
- Monique F. Kilkenny 3 , 4 ,
- Bruce C.V. Campbell 4 , 5 , 6 ,
- Coralie English 7 ,
- Alison Johnson 2 ,
- Emily Callander 1 ,
- Rohan S. Grimley 8 , 9 ,
- Christopher Levi 10 ,
- Sandy Middleton 11 , 12 ,
- Kelvin Hill 13 &
- Joanne Enticott ORCID: orcid.org/0000-0002-4480-5690 1
BMC Medicine volume 22 , Article number: 198 ( 2024 ) Cite this article
1281 Accesses
2 Altmetric
Metrics details
In the context of expanding digital health tools, the health system is ready for Learning Health System (LHS) models. These models, with proper governance and stakeholder engagement, enable the integration of digital infrastructure to provide feedback to all relevant parties including clinicians and consumers on performance against best practice standards, as well as fostering innovation and aligning healthcare with patient needs. The LHS literature primarily includes opinion or consensus-based frameworks and lacks validation or evidence of benefit. Our aim was to outline a rigorously codesigned, evidence-based LHS framework and present a national case study of an LHS-aligned national stroke program that has delivered clinical benefit.
Current core components of a LHS involve capturing evidence from communities and stakeholders (quadrant 1), integrating evidence from research findings (quadrant 2), leveraging evidence from data and practice (quadrant 3), and generating evidence from implementation (quadrant 4) for iterative system-level improvement. The Australian Stroke program was selected as the case study as it provides an exemplar of how an iterative LHS works in practice at a national level encompassing and integrating evidence from all four LHS quadrants. Using this case study, we demonstrate how to apply evidence-based processes to healthcare improvement and embed real-world research for optimising healthcare improvement. We emphasize the transition from research as an endpoint, to research as an enabler and a solution for impact in healthcare improvement.
Conclusions
The Australian Stroke program has nationally improved stroke care since 2007, showcasing the value of integrated LHS-aligned approaches for tangible impact on outcomes. This LHS case study is a practical example for other health conditions and settings to follow suit.
Peer Review reports
Internationally, health systems are facing a crisis, driven by an ageing population, increasing complexity, multi-morbidity, rapidly advancing health technology and rising costs that threaten sustainability and mandate transformation and improvement [ 1 , 2 ]. Although research has generated solutions to healthcare challenges, and the advent of big data and digital health holds great promise, entrenched siloes and poor integration of knowledge generation, knowledge implementation and healthcare delivery between stakeholders, curtails momentum towards, and consistent attainment of, evidence-and value-based care [ 3 ]. This is compounded by the short supply of research and innovation leadership within the healthcare sector, and poorly integrated and often inaccessible health data systems, which have crippled the potential to deliver on digital-driven innovation [ 4 ]. Current approaches to healthcare improvement are also often isolated with limited sustainability, scale-up and impact [ 5 ].
Evidence suggests that integration and partnership across academic and healthcare delivery stakeholders are key to progress, including those with lived experience and their families (referred to here as consumers and community), diverse disciplines (both research and clinical), policy makers and funders. Utilization of evidence from research and evidence from practice including data from routine care, supported by implementation research, are key to sustainably embedding improvement and optimising health care and outcomes. A strategy to achieve this integration is through the Learning Health System (LHS) (Fig. 1 ) [ 2 , 6 , 7 , 8 ]. Although there are numerous publications on LHS approaches [ 9 , 10 , 11 , 12 ], many focus on research perspectives and data, most do not demonstrate tangible healthcare improvement or better health outcomes. [ 6 ]
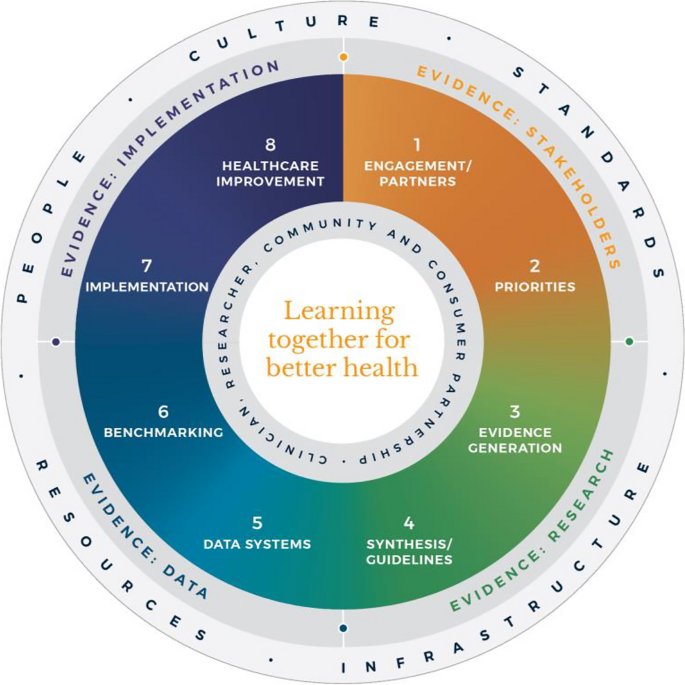
Monash Learning Health System: The Learn Together for Better Health Framework developed by Monash Partners and Monash University (from Enticott et al. 2021 [ 7 ]). Four evidence quadrants: Q1 (orange) is evidence from stakeholders; Q2 (green) is evidence from research; Q3 (light blue) is evidence from data; and, Q4 (dark blue) is evidence from implementation and healthcare improvement
In developed nations, it has been estimated that 60% of care provided aligns with the evidence base, 30% is low value and 10% is potentially harmful [ 13 ]. In some areas, clinical advances have been rapid and research and evidence have paved the way for dramatic improvement in outcomes, mandating rapid implementation of evidence into healthcare (e.g. polio and COVID-19 vaccines). However, healthcare improvement is challenging and slow [ 5 ]. Health systems are highly complex in their design, networks and interacting components, and change is difficult to enact, sustain and scale up. [ 3 ] New effective strategies are needed to meet community needs and deliver evidence-based and value-based care, which reorients care from serving the provider, services and system, towards serving community needs, based on evidence and quality. It goes beyond cost to encompass patient and provider experience, quality care and outcomes, efficiency and sustainability [ 2 , 6 ].
The costs of stroke care are expected to rise rapidly in the next decades, unless improvements in stroke care to reduce the disabling effects of strokes can be successfully developed and implemented [ 14 ]. Here, we briefly describe the Monash LHS framework (Fig. 1 ) [ 2 , 6 , 7 ] and outline an exemplar case in order to demonstrate how to apply evidence-based processes to healthcare improvement and embed real-world research for optimising healthcare. The Australian LHS exemplar in stroke care has driven nationwide improvement in stroke care since 2007.
An evidence-based Learning Health System framework
In Australia, members of this author group (HT, AJ, JE) have rigorously co-developed an evidence-based LHS framework, known simply as the Monash LHS [ 7 ]. The Monash LHS was designed to support sustainable, iterative and continuous robust benefit of improved clinical outcomes. It was created with national engagement in order to be applicable to Australian settings. Through this rigorous approach, core LHS principles and components have been established (Fig. 1 ). Evidence shows that people/workforce, culture, standards, governance and resources were all key to an effective LHS [ 2 , 6 ]. Culture is vital including trust, transparency, partnership and co-design. Key processes include legally compliant data sharing, linkage and governance, resources, and infrastructure [ 4 ]. The Monash LHS integrates disparate and often siloed stakeholders, infrastructure and expertise to ‘Learn Together for Better Health’ [ 7 ] (Fig. 1 ). This integrates (i) evidence from community and stakeholders including priority areas and outcomes; (ii) evidence from research and guidelines; (iii) evidence from practice (from data) with advanced analytics and benchmarking; and (iv) evidence from implementation science and health economics. Importantly, it starts with the problem and priorities of key stakeholders including the community, health professionals and services and creates an iterative learning system to address these. The following case study was chosen as it is an exemplar of how a Monash LHS-aligned national stroke program has delivered clinical benefit.
Australian Stroke Learning Health System
Internationally, the application of LHS approaches in stroke has resulted in improved stroke care and outcomes [ 12 ]. For example, in Canada a sustained decrease in 30-day in-hospital mortality has been found commensurate with an increase in resources to establish the multifactorial stroke system intervention for stroke treatment and prevention [ 15 ]. Arguably, with rapid advances in evidence and in the context of an ageing population with high cost and care burden and substantive impacts on quality of life, stroke is an area with a need for rapid research translation into evidence-based and value-based healthcare improvement. However, a recent systematic review found that the existing literature had few comprehensive examples of LHS adoption [ 12 ]. Although healthcare improvement systems and approaches were described, less is known about patient-clinician and stakeholder engagement, governance and culture, or embedding of data informatics into everyday practice to inform and drive improvement [ 12 ]. For example, in a recent review of quality improvement collaborations, it was found that although clinical processes in stroke care are improved, their short-term nature means there is uncertainty about sustainability and impacts on patient outcomes [ 16 ]. Table 1 provides the main features of the Australian Stroke LHS based on the four core domains and eight elements of the Learning Together for Better Health Framework described in Fig. 1 . The features are further expanded on in the following sections.
Evidence from stakeholders (LHS quadrant 1, Fig. 1 )
Engagement, partners and priorities.
Within the stroke field, there have been various support mechanisms to facilitate an LHS approach including partnership and broad stakeholder engagement that includes clinical networks and policy makers from different jurisdictions. Since 2008, the Australian Stroke Coalition has been co-led by the Stroke Foundation, a charitable consumer advocacy organisation, and Stroke Society of Australasia a professional society with membership covering academics and multidisciplinary clinician networks, that are collectively working to improve stroke care ( https://australianstrokecoalition.org.au/ ). Surveys, focus groups and workshops have been used for identifying priorities from stakeholders. Recent agreed priorities have been to improve stroke care and strengthen the voice for stroke care at a national ( https://strokefoundation.org.au/ ) and international level ( https://www.world-stroke.org/news-and-blog/news/world-stroke-organization-tackle-gaps-in-access-to-quality-stroke-care ), as well as reduce duplication amongst stakeholders. This activity is built on a foundation and culture of research and innovation embedded within the stroke ‘community of practice’. Consumers, as people with lived experience of stroke are important members of the Australian Stroke Coalition, as well as representatives from different clinical colleges. Consumers also provide critical input to a range of LHS activities via the Stroke Foundation Consumer Council, Stroke Living Guidelines committees, and the Australian Stroke Clinical Registry (AuSCR) Steering Committee (described below).
Evidence from research (LHS quadrant 2, Fig. 1 )
Advancement of the evidence for stroke interventions and synthesis into clinical guidelines.
To implement best practice, it is crucial to distil the large volume of scientific and trial literature into actionable recommendations for clinicians to use in practice [ 24 ]. The first Australian clinical guidelines for acute stroke were produced in 2003 following the increasing evidence emerging for prevention interventions (e.g. carotid endarterectomy, blood pressure lowering), acute medical treatments (intravenous thrombolysis, aspirin within 48 h of ischemic stroke), and optimised hospital management (care in dedicated stroke units by a specialised and coordinated multidisciplinary team) [ 25 ]. Importantly, a number of the innovations were developed, researched and proven effective by key opinion leaders embedded in the Australian stroke care community. In 2005, the clinical guidelines for Stroke Rehabilitation and Recovery [ 26 ] were produced, with subsequent merged guidelines periodically updated. However, the traditional process of periodic guideline updates is challenging for end users when new research can render recommendations redundant and this lack of currency erodes stakeholder trust [ 27 ]. In response to this challenge the Stroke Foundation and Cochrane Australia entered a pioneering project to produce the first electronic ‘living’ guidelines globally [ 20 ]. Major shifts in the evidence for reperfusion therapies (e.g. extended time-window intravenous thrombolysis and endovascular clot retrieval), among other advances, were able to be converted into new recommendations, approved by the Australian National Health and Medical Research Council within a few months of publication. Feedback on this process confirmed the increased use and trust in the guidelines by clinicians. The process informed other living guidelines programs, including the successful COVID-19 clinical guidelines [ 28 ].
However, best practice clinical guideline recommendations are necessary but insufficient for healthcare improvement and nesting these within an LHS with stakeholder partnership, enables implementation via a range of proven methods, including audit and feedback strategies [ 29 ].
Evidence from data and practice (LHS quadrant 3, Fig. 1 )
Data systems and benchmarking : revealing the disparities in care between health services. A national system for standardized stroke data collection was established as the National Stroke Audit program in 2007 by the Stroke Foundation [ 30 ] following various state-level programs (e.g. New South Wales Audit) [ 31 ] to identify evidence-practice gaps and prioritise improvement efforts to increase access to stroke units and other acute treatments [ 32 ]. The Audit program alternates each year between acute (commencing in 2007) and rehabilitation in-patient services (commencing in 2008). The Audit program provides a ‘deep dive’ on the majority of recommendations in the clinical guidelines whereby participating hospitals provide audits of up to 40 consecutive patient medical records and respond to a survey about organizational resources to manage stroke. In 2009, the AuSCR was established to provide information on patients managed in acute hospitals based on a small subset of quality processes of care linked to benchmarked reports of performance (Fig. 2 ) [ 33 ]. In this way, the continuous collection of high-priority processes of stroke care could be regularly collected and reviewed to guide improvement to care [ 34 ]. Plus clinical quality registry programs within Australia have shown a meaningful return on investment attributed to enhanced survival, improvements in quality of life and avoided costs of treatment or hospital stay [ 35 ].
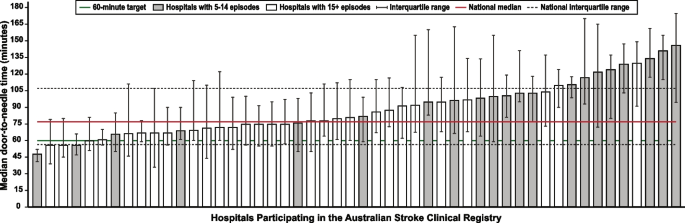
Example performance report from the Australian Stroke Clinical Registry: average door-to-needle time in providing intravenous thrombolysis by different hospitals in 2021 [ 36 ]. Each bar in the figure represents a single hospital
The Australian Stroke Coalition endorsed the creation of an integrated technological solution for collecting data through a single portal for multiple programs in 2013. In 2015, the Stroke Foundation, AuSCR consortium, and other relevant groups cooperated to design an integrated data management platform (the Australian Stroke Data Tool) to reduce duplication of effort for hospital staff in the collection of overlapping variables in the same patients [ 19 ]. Importantly, a national data dictionary then provided the common data definitions to facilitate standardized data capture. Another important feature of AuSCR is the collection of patient-reported outcome surveys between 90 and 180 days after stroke, and annual linkage with national death records to ascertain survival status [ 33 ]. To support a LHS approach, hospitals that participate in AuSCR have access to a range of real-time performance reports. In efforts to minimize the burden of data collection in the AuSCR, interoperability approaches to import data directly from hospital or state-level managed stroke databases have been established (Fig. 3 ); however, the application has been variable and 41% of hospitals still manually enter all their data.
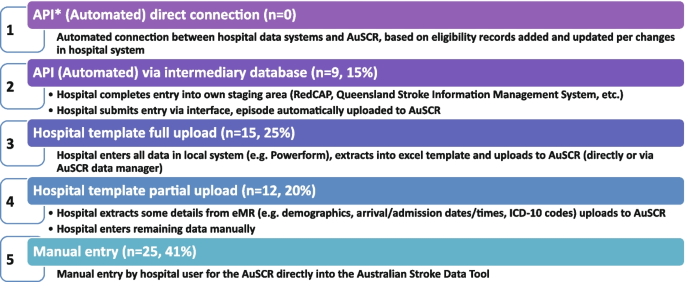
Current status of automated data importing solutions in the Australian Stroke Clinical Registry, 2022, with ‘ n ’ representing the number of hospitals. AuSCR, Australian Stroke Clinical Registry; AuSDaT, Australian Stroke Data Tool; API, Application Programming Interface; ICD, International Classification of Diseases; RedCAP, Research Electronic Data Capture; eMR, electronic medical records
For acute stroke care, the Australian Commission on Quality and Safety in Health Care facilitated the co-design (clinicians, academics, consumers) and publication of the national Acute Stroke Clinical Care Standard in 2015 [ 17 ], and subsequent review [ 18 ]. The indicator set for the Acute Stroke Standard then informed the expansion of the minimum dataset for AuSCR so that hospitals could routinely track their performance. The national Audit program enabled hospitals not involved in the AuSCR to assess their performance every two years against the Acute Stroke Standard. Complementing these efforts, the Stroke Foundation, working with the sector, developed the Acute and Rehabilitation Stroke Services Frameworks to outline the principles, essential elements, models of care and staffing recommendations for stroke services ( https://informme.org.au/guidelines/national-stroke-services-frameworks ). The Frameworks are intended to guide where stroke services should be developed, and monitor their uptake with the organizational survey component of the Audit program.
Evidence from implementation and healthcare improvement (LHS quadrant 4, Fig. 1 )
Research to better utilize and augment data from registries through linkage [ 37 , 38 , 39 , 40 ] and to ensure presentation of hospital or service level data are understood by clinicians has ensured advancement in the field for the Australian Stroke LHS [ 41 ]. Importantly, greater insights into whole patient journeys, before and after a stroke, can now enable exploration of value-based care. The LHS and stroke data platform have enabled focused and time-limited projects to create a better understanding of the quality of care in acute or rehabilitation settings [ 22 , 42 , 43 ]. Within stroke, all the elements of an LHS culminate into the ready availability of benchmarked performance data and support for implementation of strategies to address gaps in care.
Implementation research to grow the evidence base for effective improvement interventions has also been a key pillar in the Australian context. These include multi-component implementation interventions to achieve behaviour change for particular aspects of stroke care, [ 22 , 23 , 44 , 45 ] and real-world approaches to augmenting access to hyperacute interventions in stroke through the use of technology and telehealth [ 46 , 47 , 48 , 49 ]. The evidence from these studies feeds into the living guidelines program and the data collection systems, such as the Audit program or AuSCR, which are then amended to ensure data aligns to recommended care. For example, the use of ‘hyperacute aspirin within the first 48 h of ischemic stroke’ was modified to be ‘hyperacute antiplatelet…’ to incorporate new evidence that other medications or combinations are appropriate to use. Additionally, new datasets have been developed to align with evidence such as the Fever, Sugar, and Swallow variables [ 42 ]. Evidence on improvements in access to best practice care from the acute Audit program [ 50 ] and AuSCR is emerging [ 36 ]. For example, between 2007 and 2017, the odds of receiving intravenous thrombolysis after ischemic stroke increased by 16% 9OR 1.06 95% CI 1.13–1.18) and being managed in a stroke unit by 18% (OR 1.18 95% CI 1.17–1.20). Over this period, the median length of hospital stay for all patients decreased from 6.3 days in 2007 to 5.0 days in 2017 [ 51 ]. When considering the number of additional patients who would receive treatment in 2017 in comparison to 2007 it was estimated that without this additional treatment, over 17,000 healthy years of life would be lost in 2017 (17,786 disability-adjusted life years) [ 51 ]. There is evidence on the cost-effectiveness of different system-focussed strategies to augment treatment access for acute ischemic stroke (e.g. Victorian Stroke Telemedicine program [ 52 ] and Melbourne Mobile Stroke Unit ambulance [ 53 ]). Reciprocally, evidence from the national Rehabilitation Audit, where the LHS approach has been less complete or embedded, has shown fewer areas of healthcare improvement over time [ 51 , 54 ].
Within the field of stroke in Australia, there is indirect evidence that the collective efforts that align to establishing the components of a LHS have had an impact. Overall, the age-standardised rate of stroke events has reduced by 27% between 2001 and 2020, from 169 to 124 events per 100,000 population. Substantial declines in mortality rates have been reported since 1980. Commensurate with national clinical guidelines being updated in 2007 and the first National Stroke Audit being undertaken in 2007, the mortality rates for men (37.4 deaths per 100,000) and women (36.1 deaths per 100,0000 has declined to 23.8 and 23.9 per 100,000, respectively in 2021 [ 55 ].
Underpinning the LHS with the integration of the four quadrants of evidence from stakeholders, research and guidelines, practice and implementation, and core LHS principles have been addressed. Leadership and governance have been important, and programs have been established to augment workforce training and capacity building in best practice professional development. Medical practitioners are able to undertake courses and mentoring through the Australasian Stroke Academy ( http://www.strokeacademy.com.au/ ) while nurses (and other health professionals) can access teaching modules in stroke care from the Acute Stroke Nurses Education Network ( https://asnen.org/ ). The Association of Neurovascular Clinicians offers distance-accessible education and certification to develop stroke expertise for interdisciplinary professionals, including advanced stroke co-ordinator certification ( www.anvc.org ). Consumer initiative interventions are also used in the design of the AuSCR Public Summary Annual reports (available at https://auscr.com.au/about/annual-reports/ ) and consumer-related resources related to the Living Guidelines ( https://enableme.org.au/resources ).
The important success factors and lessons from stroke as a national exemplar LHS in Australia include leadership, culture, workforce and resources integrated with (1) established and broad partnerships across the academic-clinical sector divide and stakeholder engagement; (2) the living guidelines program; (3) national data infrastructure, including a national data dictionary that provides the common data framework to support standardized data capture; (4) various implementation strategies including benchmarking and feedback as well as engagement strategies targeting different levels of the health system; and (5) implementation and improvement research to advance stroke systems of care and reduce unwarranted variation in practice (Fig. 1 ). Priority opportunities now include the advancement of interoperability with electronic medical records as an area all clinical quality registry’s programs needs to be addressed, as well as providing more dynamic and interactive data dashboards tailored to the need of clinicians and health service executives.
There is a clear mandate to optimise healthcare improvement with big data offering major opportunities for change. However, we have lacked the approaches to capture evidence from the community and stakeholders, to integrate evidence from research, to capture and leverage data or evidence from practice and to generate and build on evidence from implementation using iterative system-level improvement. The LHS provides this opportunity and is shown to deliver impact. Here, we have outlined the process applied to generate an evidence-based LHS and provide a leading exemplar in stroke care. This highlights the value of moving from single-focus isolated approaches/initiatives to healthcare improvement and the benefit of integration to deliver demonstrable outcomes for our funders and key stakeholders — our community. This work provides insight into strategies that can both apply evidence-based processes to healthcare improvement as well as implementing evidence-based practices into care, moving beyond research as an endpoint, to research as an enabler, underpinning delivery of better healthcare.
Availability of data and materials
Not applicable
Abbreviations
Australian Stroke Clinical Registry
Confidence interval
- Learning Health System
World Health Organization. Delivering quality health services . OECD Publishing; 2018.
Enticott J, Braaf S, Johnson A, Jones A, Teede HJ. Leaders’ perspectives on learning health systems: A qualitative study. BMC Health Serv Res. 2020;20:1087.
Article PubMed PubMed Central Google Scholar
Melder A, Robinson T, McLoughlin I, Iedema R, Teede H. An overview of healthcare improvement: Unpacking the complexity for clinicians and managers in a learning health system. Intern Med J. 2020;50:1174–84.
Article PubMed Google Scholar
Alberto IRI, Alberto NRI, Ghosh AK, Jain B, Jayakumar S, Martinez-Martin N, et al. The impact of commercial health datasets on medical research and health-care algorithms. Lancet Digit Health. 2023;5:e288–94.
Article CAS PubMed PubMed Central Google Scholar
Dixon-Woods M. How to improve healthcare improvement—an essay by Mary Dixon-Woods. BMJ. 2019;367: l5514.
Enticott J, Johnson A, Teede H. Learning health systems using data to drive healthcare improvement and impact: A systematic review. BMC Health Serv Res. 2021;21:200.
Enticott JC, Melder A, Johnson A, Jones A, Shaw T, Keech W, et al. A learning health system framework to operationalize health data to improve quality care: An Australian perspective. Front Med (Lausanne). 2021;8:730021.
Dammery G, Ellis LA, Churruca K, Mahadeva J, Lopez F, Carrigan A, et al. The journey to a learning health system in primary care: A qualitative case study utilising an embedded research approach. BMC Prim Care. 2023;24:22.
Foley T, Horwitz L, Zahran R. The learning healthcare project: Realising the potential of learning health systems. 2021. Available from https://learninghealthcareproject.org/wp-content/uploads/2021/05/LHS2021report.pdf . Accessed Jan 2024.
Institute of Medicine. Best care at lower cost: The path to continuously learning health care in America. Washington: The National Academies Press; 2013.
Google Scholar
Zurynski Y, Smith CL, Vedovi A, Ellis LA, Knaggs G, Meulenbroeks I, et al. Mapping the learning health system: A scoping review of current evidence - a white paper. 2020:63
Cadilhac DA, Bravata DM, Bettger J, Mikulik R, Norrving B, Uvere E, et al. Stroke learning health systems: A topical narrative review with case examples. Stroke. 2023;54:1148–59.
Braithwaite J, Glasziou P, Westbrook J. The three numbers you need to know about healthcare: The 60–30-10 challenge. BMC Med. 2020;18:1–8.
Article Google Scholar
King D, Wittenberg R, Patel A, Quayyum Z, Berdunov V, Knapp M. The future incidence, prevalence and costs of stroke in the UK. Age Ageing. 2020;49:277–82.
Ganesh A, Lindsay P, Fang J, Kapral MK, Cote R, Joiner I, et al. Integrated systems of stroke care and reduction in 30-day mortality: A retrospective analysis. Neurology. 2016;86:898–904.
Lowther HJ, Harrison J, Hill JE, Gaskins NJ, Lazo KC, Clegg AJ, et al. The effectiveness of quality improvement collaboratives in improving stroke care and the facilitators and barriers to their implementation: A systematic review. Implement Sci. 2021;16:16.
Australian Commission on Safety and Quality in Health Care. Acute stroke clinical care standard. 2015. Available from https://www.safetyandquality.gov.au/our-work/clinical-care-standards/acute-stroke-clinical-care-standard . Accessed Jan 2024.
Australian Commission on Safety and Quality in Health Care. Acute stroke clinical care standard. Sydney: ACSQHC; 2019. Available from https://www.safetyandquality.gov.au/publications-and-resources/resource-library/acute-stroke-clinical-care-standard-evidence-sources . Accessed Jan 2024.
Ryan O, Ghuliani J, Grabsch B, Hill K, G CC, Breen S, et al. Development, implementation, and evaluation of the Australian Stroke Data Tool (AuSDaT): Comprehensive data capturing for multiple uses. Health Inf Manag. 2022:18333583221117184.
English C, Bayley M, Hill K, Langhorne P, Molag M, Ranta A, et al. Bringing stroke clinical guidelines to life. Int J Stroke. 2019;14:337–9.
English C, Hill K, Cadilhac DA, Hackett ML, Lannin NA, Middleton S, et al. Living clinical guidelines for stroke: Updates, challenges and opportunities. Med J Aust. 2022;216:510–4.
Cadilhac DA, Grimley R, Kilkenny MF, Andrew NE, Lannin NA, Hill K, et al. Multicenter, prospective, controlled, before-and-after, quality improvement study (Stroke123) of acute stroke care. Stroke. 2019;50:1525–30.
Cadilhac DA, Marion V, Andrew NE, Breen SJ, Grabsch B, Purvis T, et al. A stepped-wedge cluster-randomized trial to improve adherence to evidence-based practices for acute stroke management. Jt Comm J Qual Patient Saf. 2022.
Elliott J, Lawrence R, Minx JC, Oladapo OT, Ravaud P, Jeppesen BT, et al. Decision makers need constantly updated evidence synthesis. Nature. 2021;600:383–5.
Article CAS PubMed Google Scholar
National Stroke Foundation. National guidelines for acute stroke management. Melbourne: National Stroke Foundation; 2003.
National Stroke Foundation. Clinical guidelines for stroke rehabilitation and recovery. Melbourne: National Stroke Foundation; 2005.
Phan TG, Thrift A, Cadilhac D, Srikanth V. A plea for the use of systematic review methodology when writing guidelines and timely publication of guidelines. Intern Med J . 2012;42:1369–1371; author reply 1371–1362
Tendal B, Vogel JP, McDonald S, Norris S, Cumpston M, White H, et al. Weekly updates of national living evidence-based guidelines: Methods for the Australian living guidelines for care of people with COVID-19. J Clin Epidemiol. 2021;131:11–21.
Grimshaw JM, Eccles MP, Lavis JN, Hill SJ, Squires JE. Knowledge translation of research findings. Implement Sci. 2012;7:50.
Harris D, Cadilhac D, Hankey GJ, Hillier S, Kilkenny M, Lalor E. National stroke audit: The Australian experience. Clin Audit. 2010;2:25–31.
Cadilhac DA, Purvis T, Kilkenny MF, Longworth M, Mohr K, Pollack M, et al. Evaluation of rural stroke services: Does implementation of coordinators and pathways improve care in rural hospitals? Stroke. 2013;44:2848–53.
Cadilhac DA, Moss KM, Price CJ, Lannin NA, Lim JY, Anderson CS. Pathways to enhancing the quality of stroke care through national data monitoring systems for hospitals. Med J Aust. 2013;199:650–1.
Cadilhac DA, Lannin NA, Anderson CS, Levi CR, Faux S, Price C, et al. Protocol and pilot data for establishing the Australian Stroke Clinical Registry. Int J Stroke. 2010;5:217–26.
Ivers N, Jamtvedt G, Flottorp S, Young J, Odgaard-Jensen J, French S, et al. Audit and feedback: Effects on professional practice and healthcare outcomes. Cochrane Database Syst Rev . 2012
Australian Commission on Safety and Quality in Health Care. Economic evaluation of clinical quality registries. Final report. . 2016:79
Cadilhac DA, Dalli LL, Morrison J, Lester M, Paice K, Moss K, et al. The Australian Stroke Clinical Registry annual report 2021. Melbourne; 2022. Available from https://auscr.com.au/about/annual-reports/ . Accessed 6 May 2024.
Kilkenny MF, Kim J, Andrew NE, Sundararajan V, Thrift AG, Katzenellenbogen JM, et al. Maximising data value and avoiding data waste: A validation study in stroke research. Med J Aust. 2019;210:27–31.
Eliakundu AL, Smith K, Kilkenny MF, Kim J, Bagot KL, Andrew E, et al. Linking data from the Australian Stroke Clinical Registry with ambulance and emergency administrative data in Victoria. Inquiry. 2022;59:469580221102200.
PubMed Google Scholar
Andrew NE, Kim J, Cadilhac DA, Sundararajan V, Thrift AG, Churilov L, et al. Protocol for evaluation of enhanced models of primary care in the management of stroke and other chronic disease (PRECISE): A data linkage healthcare evaluation study. Int J Popul Data Sci. 2019;4:1097.
CAS PubMed PubMed Central Google Scholar
Mosalski S, Shiner CT, Lannin NA, Cadilhac DA, Faux SG, Kim J, et al. Increased relative functional gain and improved stroke outcomes: A linked registry study of the impact of rehabilitation. J Stroke Cerebrovasc Dis. 2021;30: 106015.
Ryan OF, Hancock SL, Marion V, Kelly P, Kilkenny MF, Clissold B, et al. Feedback of aggregate patient-reported outcomes (PROs) data to clinicians and hospital end users: Findings from an Australian codesign workshop process. BMJ Open. 2022;12:e055999.
Grimley RS, Rosbergen IC, Gustafsson L, Horton E, Green T, Cadigan G, et al. Dose and setting of rehabilitation received after stroke in Queensland, Australia: A prospective cohort study. Clin Rehabil. 2020;34:812–23.
Purvis T, Middleton S, Craig LE, Kilkenny MF, Dale S, Hill K, et al. Inclusion of a care bundle for fever, hyperglycaemia and swallow management in a national audit for acute stroke: Evidence of upscale and spread. Implement Sci. 2019;14:87.
Middleton S, McElduff P, Ward J, Grimshaw JM, Dale S, D’Este C, et al. Implementation of evidence-based treatment protocols to manage fever, hyperglycaemia, and swallowing dysfunction in acute stroke (QASC): A cluster randomised controlled trial. Lancet. 2011;378:1699–706.
Middleton S, Dale S, Cheung NW, Cadilhac DA, Grimshaw JM, Levi C, et al. Nurse-initiated acute stroke care in emergency departments. Stroke. 2019:STROKEAHA118020701.
Hood RJ, Maltby S, Keynes A, Kluge MG, Nalivaiko E, Ryan A, et al. Development and pilot implementation of TACTICS VR: A virtual reality-based stroke management workflow training application and training framework. Front Neurol. 2021;12:665808.
Bladin CF, Kim J, Bagot KL, Vu M, Moloczij N, Denisenko S, et al. Improving acute stroke care in regional hospitals: Clinical evaluation of the Victorian Stroke Telemedicine program. Med J Aust. 2020;212:371–7.
Bladin CF, Bagot KL, Vu M, Kim J, Bernard S, Smith K, et al. Real-world, feasibility study to investigate the use of a multidisciplinary app (Pulsara) to improve prehospital communication and timelines for acute stroke/STEMI care. BMJ Open. 2022;12:e052332.
Zhao H, Coote S, Easton D, Langenberg F, Stephenson M, Smith K, et al. Melbourne mobile stroke unit and reperfusion therapy: Greater clinical impact of thrombectomy than thrombolysis. Stroke. 2020;51:922–30.
Purvis T, Cadilhac DA, Hill K, Reyneke M, Olaiya MT, Dalli LL, et al. Twenty years of monitoring acute stroke care in Australia from the national stroke audit program (1999–2019): Achievements and areas of future focus. J Health Serv Res Policy. 2023.
Cadilhac DA, Purvis T, Reyneke M, Dalli LL, Kim J, Kilkenny MF. Evaluation of the national stroke audit program: 20-year report. Melbourne; 2019.
Kim J, Tan E, Gao L, Moodie M, Dewey HM, Bagot KL, et al. Cost-effectiveness of the Victorian Stroke Telemedicine program. Aust Health Rev. 2022;46:294–301.
Kim J, Easton D, Zhao H, Coote S, Sookram G, Smith K, et al. Economic evaluation of the Melbourne mobile stroke unit. Int J Stroke. 2021;16:466–75.
Stroke Foundation. National stroke audit – rehabilitation services report 2020. Melbourne; 2020.
Australian Institute of Health and Welfare. Heart, stroke and vascular disease: Australian facts. 2023. Webpage https://www.aihw.gov.au/reports/heart-stroke-vascular-diseases/hsvd-facts/contents/about (accessed Jan 2024).
Download references
Acknowledgements
The following authors hold National Health and Medical Research Council Research Fellowships: HT (#2009326), DAC (#1154273), SM (#1196352), MFK Future Leader Research Fellowship (National Heart Foundation #105737). The Funders of this work did not have any direct role in the design of the study, its execution, analyses, interpretation of the data, or decision to submit results for publication.
Author information
Helena Teede and Dominique A. Cadilhac contributed equally.
Authors and Affiliations
Monash Centre for Health Research and Implementation, 43-51 Kanooka Grove, Clayton, VIC, Australia
Helena Teede, Emily Callander & Joanne Enticott
Monash Partners Academic Health Science Centre, 43-51 Kanooka Grove, Clayton, VIC, Australia
Helena Teede & Alison Johnson
Stroke and Ageing Research, Department of Medicine, School of Clinical Sciences at Monash Health, Monash University, Level 2 Monash University Research, Victorian Heart Hospital, 631 Blackburn Rd, Clayton, VIC, Australia
Dominique A. Cadilhac, Tara Purvis & Monique F. Kilkenny
Stroke Theme, The Florey Institute of Neuroscience and Mental Health, University of Melbourne, Heidelberg, VIC, Australia
Dominique A. Cadilhac, Monique F. Kilkenny & Bruce C.V. Campbell
Department of Neurology, Melbourne Brain Centre, Royal Melbourne Hospital, Parkville, VIC, Australia
Bruce C.V. Campbell
Department of Medicine, Faculty of Medicine, Dentistry and Health Sciences, University of Melbourne, Victoria, Australia
School of Health Sciences, Heart and Stroke Program, University of Newcastle, Hunter Medical Research Institute, University Drive, Callaghan, NSW, Australia
Coralie English
School of Medicine and Dentistry, Griffith University, Birtinya, QLD, Australia
Rohan S. Grimley
Clinical Excellence Division, Queensland Health, Brisbane, Australia
John Hunter Hospital, Hunter New England Local Health District and University of Newcastle, Sydney, NSW, Australia
Christopher Levi
School of Nursing, Midwifery and Paramedicine, Australian Catholic University, Sydney, NSW, Australia
Sandy Middleton
Nursing Research Institute, St Vincent’s Health Network Sydney and and Australian Catholic University, Sydney, NSW, Australia
Stroke Foundation, Level 7, 461 Bourke St, Melbourne, VIC, Australia
Kelvin Hill
You can also search for this author in PubMed Google Scholar
Contributions
HT: conception, design and initial draft, developed the theoretical formalism for learning health system framework, approved the submitted version. DAC: conception, design and initial draft, provided essential literature and case study examples, approved the submitted version. TP: revised the manuscript critically for important intellectual content, approved the submitted version. MFK: revised the manuscript critically for important intellectual content, provided essential literature and case study examples, approved the submitted version. BC: revised the manuscript critically for important intellectual content, provided essential literature and case study examples, approved the submitted version. CE: revised the manuscript critically for important intellectual content, provided essential literature and case study examples, approved the submitted version. AJ: conception, design and initial draft, developed the theoretical formalism for learning health system framework, approved the submitted version. EC: revised the manuscript critically for important intellectual content, approved the submitted version. RSG: revised the manuscript critically for important intellectual content, provided essential literature and case study examples, approved the submitted version. CL: revised the manuscript critically for important intellectual content, provided essential literature and case study examples, approved the submitted version. SM: revised the manuscript critically for important intellectual content, provided essential literature and case study examples, approved the submitted version. KH: revised the manuscript critically for important intellectual content, provided essential literature and case study examples, approved the submitted version. JE: conception, design and initial draft, developed the theoretical formalism for learning health system framework, approved the submitted version. All authors read and approved the final manuscript.
Authors’ Twitter handles
@HelenaTeede
@DominiqueCad
@Coralie_English
@EmilyCallander
@EnticottJo
Corresponding authors
Correspondence to Helena Teede or Dominique A. Cadilhac .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests, additional information, publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Teede, H., Cadilhac, D.A., Purvis, T. et al. Learning together for better health using an evidence-based Learning Health System framework: a case study in stroke. BMC Med 22 , 198 (2024). https://doi.org/10.1186/s12916-024-03416-w
Download citation
Received : 23 July 2023
Accepted : 30 April 2024
Published : 15 May 2024
DOI : https://doi.org/10.1186/s12916-024-03416-w
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Evidence-based medicine
- Person-centred care
- Models of care
- Healthcare improvement
BMC Medicine
ISSN: 1741-7015
- General enquiries: [email protected]
- Utility Menu
harvardchan_logo.png

Harvard T.H. Chan School of Public Health Case-Based Teaching & Learning Initiative
Teaching cases & active learning resources for public health education, writing a case.
An overview of the case planning and writing process, by experienced case-writer and CBTL workshop leader Kirsten Lundberg.
2019. The Case Centre . Visit website A non-profit clearing house for materials on the case method, the Case Centre holds a large and diverse collection of cases, articles, book chapters and teaching materials, including the collections of leading business schools across the globe.
Abell, D. , 1997. What makes a good case? . ECCHO–The Newsletter of the European Case Clearing House , 17 (1) , pp. 4-7. Read online "Case writing is both art and science. There are few, if any, specific prescriptions or recipes, but there are key ingredients that appear to distinguish excellent cases from the run-of-the-mill. This technical note lists ten ingredients to look for if you are teaching somebody else''s case - and to look out for if you are writing it yourself."
Roberts, M.J. , 2001. Developing a teaching case (abridged) , Harvard Business School Publishing. Publisher's Version A straightforward and comprehensive overview of how to write a teaching case, including sections on what makes a good case; sources for and types of cases; and steps in writing a case.
- Writing a case (8)
- Writing a teaching note (4)
- Active learning (12)
- Active listening (1)
- Asking effective questions (5)
- Assessing learning (1)
- Engaging students (5)
- Leading discussion (10)
- Managing the classroom (4)
- Planning a course (1)
- Problem-based learning (1)
- Teaching & learning with the case method (14)
- Teaching inclusively (3)
- Skip to primary navigation
- Skip to main content
- Skip to footer

Elite Editing
You write it. We right it.™

Why Are Case Studies Important in Health Care?
Case studies can be powerful tools for a range of professionals across all industries, but they are especially important in health care. Not only do they give us valuable insights into patient care, but they also help us understand the bigger questions like how to reduce medical errors and improve health outcomes overall. As content marketers and writers , it’s essential that we become familiar with this type of research so we can better convey crucial information to our audiences when creating compelling stories about health care. In this blog post, we’ll explore why case studies matter in health care and how you can use them to your advantage as a writer or marketer.
What are case studies and how do they help health-care professionals make decisions?
Case studies are a valuable tool in our arsenal . They allow us to analyze real-world scenarios and understand how different treatments or interventions have been applied in the past. By understanding the nuances of each case and how various factors influenced the outcome, we can approach our own patients’ situations with a more informed perspective.
Examining the benefits of using case studies in health care
The use of case studies has become increasingly popular in the health-care industry, and for good reason. Not only do they offer an opportunity to analyze real-life scenarios and explore potential solutions, but they also provide valuable insights into the decision-making processes of health-care providers. Case studies allow for a more comprehensive understanding of the complexities of health-care delivery and patient outcomes, enabling practitioners to make more informed decisions and ultimately improve patient care. By examining the benefits and drawbacks of various approaches, case studies play a vital role in shaping the direction of health care. As the industry continues to evolve, the use of case studies will undoubtedly remain crucial to advancing the field and ensuring the best possible outcomes for patients.
Analyzing how case studies can improve patient outcomes
In the field of health care, patient outcomes are a top priority. Many health-care professionals are turning to case studies as a method to improve these outcomes. Case studies allow for an in-depth look at specific patient situations and provide valuable insights into the effectiveness of certain treatments and interventions. This innovative approach to health care not only improves patient outcomes but also enhances the overall quality of care. With case studies, health-care professionals can continue to evolve and adapt to the ever-changing needs of their patients.
Exploring the role of technology in gathering and utilizing data from case studies
Technology has revolutionized the way we approach case studies, offering a wealth of data and insight that can be utilized to drive progress and innovation. With the advent of sophisticated tools and algorithms, we can now gather and analyze vast amounts of data quickly and efficiently, enabling us to hone in on key trends and patterns. But the role of technology doesn’t stop there. It also allows us to visualize and communicate our findings in powerful and compelling ways, ensuring that our insights are not just informative but also impactful. As we continue to explore the potential of technology in case studies, we can look forward to an exciting future of discovery and transformation.
Understanding how to use evidence-based practice to implement best practices in health care
One way to achieve the best outcomes is through evidence-based practice, a method that’s rooted in the latest research and reliable data. By combining clinical expertise, patient values, and the best available evidence, we can implement best practices that have been proven to work. Let’s continue to learn, grow, and implement the best practices in health care.
Looking ahead—challenges and opportunities for applying case studies in health care
As the health-care industry continues to evolve, it’s essential that we keep looking ahead to address the challenges and opportunities that will arise. Utilizing case studies is one way to advance our understanding of the ever-changing landscape of health care. Through case studies, we can explore various situations and apply critical thinking skills to find solutions to complex problems. Hospitals and health-care providers can benefit greatly from this approach as they seek to improve patient care and outcomes. Each case must be evaluated on an individual basis, taking into account the unique circumstances and variables at play. By embracing the power of case studies while also exercising caution and attention to detail, we can continue to push the boundaries of health-care innovation.
In conclusion, case studies are a powerful tool for improving patient outcomes and making evidence-based improvements in health care. Moving forward, implementing case studies in health care will bring a variety of challenges. With that said, if health-care organizations are willing to commit resources and effort toward developing a robust case-study platform, they can benefit enormously from the critical insights gained from studying individual cases. If you’re a health-care professional looking to develop more effective practices in your workplace through the use of case studies, contact Elite Editing —we offer a suite of editing services designed specifically for the health-care industry! We’ll help you craft top-notch copy that will tell your story and meet your goals for reaching current patients, potential patients, donors, or other stakeholders.
Other Resources You Might Like

Content Marketing
How to Establish a Content Marketing Strategy, for E-Commerce

Tips for Maximizing Your Content Marketing Budget
Balancing Quantity and Quality: Tips for Consistency in Content Creation
Get elite updates straight to your inbox..
- Content Writing
- Marketing and Sales Enablement
- Program Management
- AI Implementation
Who We Help
- Thought Leaders
- Cybersecurity
- Health Care
- Full-Time Careers
- Freelance Opportunities
- Press and Awards
- Success Stories
- About Elite
In the News
- Elite Creative Makes the Inc. 5000 for the Third Year in a Row

- Research article
- Open access
- Published: 31 August 2020
Exploring psychological safety in healthcare teams to inform the development of interventions: combining observational, survey and interview data
- Róisín O’Donovan ORCID: orcid.org/0000-0003-1993-5319 1 &
- Eilish McAuliffe 1
BMC Health Services Research volume 20 , Article number: 810 ( 2020 ) Cite this article
29k Accesses
67 Citations
41 Altmetric
Metrics details
Psychological safety allows healthcare professionals to take the interpersonal risks needed to engage in effective teamwork and to maintain patient safety. In order to improve psychological safety in healthcare teams, an in-depth understanding of the complex and nuanced nature of psychological safety is needed. Psychological safety concepts, including voice, silence, learning behaviour, support and familiarity, informed the current study’s investigation of psychological safety. This study aims to use a mixed-methods approach to develop an in-depth understanding of psychological safety within healthcare teams and to build on this understanding to inform the development of future interventions to improve it.
Survey, observational and interview data are triangulated in order to develop an in- depth understanding of psychological safety within four healthcare teams, working within one case study hospital. The teams taking part included one multidisciplinary and three unidisciplinary teams. Observational and survey data were collected during and immediately following team meetings. Individual interviews were conducted with 31 individuals across the four teams. Thematic analysis was used to analyse these interviews.
Survey results indicated a high level of psychological safety. However, observations and interviews captured examples of silence and situations where participants felt less psychologically safe. Findings from across all three data sources are discussed in relation to voice and silence, learning, familiarity and support.
The results of this study provide a detailed description and in-depth understanding of psychological safety within four healthcare teams. Based on this, recommendations are made for future research and the development of interventions to improve psychological safety.
Peer Review reports
Psychological safety is a multi-dimensional, dynamic phenomenon that concerns team members’ perception of whether it is safe to take interpersonal risks at work [ 1 ]. It is particularly important within healthcare teams who need to work interdependently to co-ordinate safe patient care within a highly complex, dynamic and high stakes work environment [ 2 ]. However, a culture of fear and low psychological safety still exists within healthcare organisations [ 3 , 4 , 5 , 6 , 7 ]. There is a need to develop and implement interventions to improve psychological safety within these teams [ 8 ]. The ongoing Covid-19 pandemic has highlighted the importance of psychological safety within healthcare teams. Cultivating psychological safety is necessary in order to enable healthcare teams to collectively redesign processes and services to cope with new challenges, learn from mistakes and implement changes accordingly [ 9 ]. In order to improve psychological safety, we must first understand the complexity and nuance of psychological safety within healthcare teams [ 8 , 10 ].
To date, there has been a paucity of cross-level and multilevel research on psychological safety [ 10 ]. This has limited our understanding of psychological safety, the concepts related to it and whether it varies across teams within the same organisation [ 10 ]. Within organisational research, collecting different kinds of data on the same phenomenon and triangulating this data can help researchers assess complex phenomena, such as psychological safety, more accurately [ 8 , 11 , 12 , 13 ]. In the current study we use survey, observational and interview data to develop an in-depth understanding of psychological safety within healthcare teams. Building on this understanding, we aim to inform the development of an intervention to improve psychological safety.
The constructs which informed our study design our outlined below. These include constructs which have been linked to either low or high psychological safety (voice and learning behaviour) and which have been found to support psychological safety (positive interpersonal relationships). These constructs play a particularly important role within the context of healthcare teams.
Psychological safety promotes voice and learning behaviour. Speaking up and voice behaviour are interpersonally risky behaviours which play an important role in healthcare teams [ 8 ]. Feeling psychologically safe can enable team members to engage in speaking up behaviour, such as asking questions, pointing out a mistake or near miss and making suggestions for improvement [ 2 , 13 , 14 , 15 , 16 ]. Psychological safety also enables learning behaviours, such as seeking help or feedback [ 1 , 17 , 18 ]. Learning behaviours are integral to healthcare teams’ ability to manage demanding conditions, with rapidly evolving knowledge and practice as well as their ability to learn from failure [ 17 , 18 ]. When healthcare professionals prioritise patient safety by engaging in speaking up and learning behaviours, it is indicative of their levels of psychological safety [ 19 ].
On the other hand, lack of psychological safety inhibits team members from speaking up and causes them to opt for avoidance behaviours, such as silence [ 20 ]. It is important to acknowledge that although employees may frequently engage in voice behaviour, they could also be withholding other ideas, suggestions or concerns [ 20 ]. This highlights the need to go beyond observable behaviours to explore the nuance and complexities of individuals’ experience of psychological safety. In order to do so, this study uses a combination of survey, observation and interview data to gain a full understanding of psychological safety.
Positive interpersonal relationships drive psychological safety [ 21 , 22 ]. Within healthcare teams, having positive relationships, effective role models and better teamwork climates encourages healthcare professionals to speak up for safety [ 19 ]. Team members relationship with the team leader has been found to influence their sense of psychological safety. For example, when leaders engage in supportive behaviour, such as inclusiveness and openness, they foster psychological safety for other team members [ 23 , 24 , 25 ]. Peer support and trust among team members also improves psychological safety within teams [ 10 ]. Psychological safety can build across time, increasing as team members become more familiar with one another and have positive experiences of engaging in interpersonally risky behaviour [ 10 , 13 , 26 , 27 ]. While positive, supportive and trusting interpersonal relationships can foster psychological safety, it is important to note that psychological safety does not imply a team without any conflict or problems [ 5 ]. Psychological safety is needed in order for productive conflict, such as task conflict, to occur [ 28 ]. Task conflict concerns disagreements related to differences in viewpoints, ideas and opinions about the task being performed and can result in learning and improved performance [ 13 , 28 , 29 ].
In this study, focusing on a single hospital as a case study, we use a mixed methods approach to further our understanding of psychological safety within four healthcare teams. We combine data collected through surveys, observations and individual interviews to gain a holistic understanding of psychological safety in these teams. Building on this understanding, we aim to inform the development of future interventions to improve psychological safety in healthcare teams.
Research setting and participants
This study was undertaken by the authors as part of a wider body of research aiming to develop an intervention to improve psychological safety in healthcare teams. This research was conducted with healthcare professionals working on one of four healthcare teams from within the same acute, suburban hospital. Three of the teams were unidisciplinary – physiotherapists, nurses and speech and language therapists – and one was multidisciplinary. The authors collaborated closely with hospital management in order to recruit healthcare teams from within the hospital. These teams were selected in collaboration with hospital management using purposive sampling in order to identify different team types as well as teams that held meetings amenable to observation. The lead researcher contacted the leader of each team to ask if their team would be interested in taking part in the team observation and survey. Before beginning observations, team members from within each team were asked to consent to the meeting being observed and to completing the survey following the meeting. For interviews, a combination of purposive sampling and snowball sampling were employed to recruit team members from within each team. After the observation and surveys were complete, the researcher informed the team that anyone who was willing to take part in an interview could contact them (the researcher) or their team leader who would then refer them to the lead researcher. Team members were recruited from across all staff grades and included team leaders as well as senior and junior team members [ 30 ]. The total number of participants who took part in each phase of data collection can be found in Table 1 .
The team as a whole were observed during regularly scheduled team meetings. Of those who attended the meeting, there was 100% participation rate in the survey within teams A and B. There was one team members in team C and another in team D who was part of the observations but did not complete a survey. Since surveys were kept completely anonymous, it was not possible to assess whether the same participants who completed the survey also took part in an interview. In teams A ( n = 2), B ( n = 1) and D ( n = 1), participants who were not present during observations and who did not complete a survey were recruited by the team leader to take part in an interview.
Data collection
Within case study designs, the use of multiple sources of evidence in recommended in order to capture a holistic understanding of the phenomena being studied [ 31 ]. The current study triangulates multiple sources of data in order to gain an in-depth understanding of psychological safety in healthcare teams. Rather than adopting the commonly used approach to triangulation to gain more credible or valid results, we draw on a post-modern paradigm which views reality as having multiple, fractured dimensions and being socially constructed. This approach requires acknowledgment that all research findings are shaped by the approach used to collect them and that different methods of data collection will offer different results [ 32 ]. Therefore, we use multiple methods to deepen our understanding of psychological safety by encouraging re-interpretation of findings as data sources reveal new insights and, thus, facilitating a more complex and in-depth exploration of healthcare professionals experiences of psychological safety. This approach to triangulation of data has been termed crystallization [ 33 ].
Composite measure of psychological safety
Survey and observational data were collected using the composite measure developed and presented in a recent paper focused on measuring psychological safety in healthcare teams [ 34 ]. For each team, one weekly meeting was observed using the observation measure, which captured voice, silence, supportive or unsupportive and familiarity behaviours. The observational data were collected as part of a pilot test of the measure and, as a result, behaviours were amended following each observation, however the overall categories remained the same. Observations were completed by one researcher who sat at the table or in the room where each meeting was conducted. The observer tracked the behaviours displayed by the team leader and team members by making a mark in the “behaviour count” box for the relevant behaviour. Observations were made by only one researcher in order to reduce the inhibiting effect the presence of two researchers might have on the team’s behaviour. The observed team meetings varied in length. The meeting held by Team A lasted 30 min, Team B’s meeting lasted 90 min, Team C’s meeting lasted 70 min and Team D had a meeting which lasted 120 min. All meeting were the teams regularly scheduled team meetings. Each discussed clinical and/or management issues that were relevant to their team.
Following the meeting, team members were asked to complete the survey component of the composite measure. There were three sections in the survey which assessed participants’ psychological safety in relation to: the team leader, other team members and the team as a whole. As part of a pilot test of the survey, a 7 point Likert scale was used for teams A-C. For team D, a 10 point Likert scale was tested. This was done in order to check if using a 10 point Likert scale would give participants an even wider spectrum of response options and, thus, allow the survey to capture more variability in participants’ responses [ 35 ]. Surveys did not ask for any identifiable information and were kept completely anonymous. Participants completed their survey in the same room as one another. There was plenty of space for them to move freely in order to complete their survey in private and surveys were handed directly to the researcher once completed.
Semi-structured interviews were conducted with 31 participants from across the four teams. The full interview schedule is presented as a supplementary file . This interview data was collected in order to gain an in-depth understanding of individuals’ experience of psychological safety and explore whether there were any emerging differences compared to the team level observations or survey responses. Interviews were conducted in a private room located within the case study hospital and lasted an average of 28 min. A full description of the process used to collect and analyse the interview data can be found in O'Donovan, De Brún & McAuliffe (in preparation). Hybrid inductive-deductive thematic analysis was used to identify themes which correspond to the concepts covered in the observations and survey data. Descriptive, open codes were assigned to each interview. These codes were then reviewed and refined, with reference to the psychological safety literature, in order to identify overarching themes. Analysis also compared findings from individuals in the same team to explore the consistencies and inconsistencies across cases. Thematic analysis was chosen because it is a theoretically flexible approach to qualitative analysis which allows the combination of inductive and deductive methods [ 36 , 37 ]. As highlighted by Braun and Clarke [ 36 ], thematic analysis is a useful method for working within a participatory research paradigm, with participants as collaborators, and for producing qualitative analysis which can inform policy development. Since the overarching aim of this study was to inform the development of an intervention to improve psychological safety which is grounded in the experiences of healthcare professionals, thematic analysis was particularly suitable. Our analysis focused on themes which captured participants’ experiences of speaking up or remaining silent, engaging in learning behaviour and their experience of support, or lack of support and familiarity within the team.
Ethical approval was obtained for this study from the Human Research Ethics Committee in University College Dublin (Reference number: LS-17-67). Written informed consent was obtained from all participants prior to each stage of data collection. In order to maintain anonymity, no identifiable information was collected during observations or surveys. Interviews were assigned a code made up of P (participant), interview number (e.g. the first interview conducted within each team was given the number 1) and team letter (A, B, C or D) and any identifiable characteristics were removed from the interview transcripts.
Survey results
All survey responses are displayed in Table 2 . They indicated that team members felt psychologically safe. In team A, a mean response of 6.700 was given for section 1, 6.597 for section 2 and 6.212 for section 3.
Observations
A positive, constructive atmosphere was observed during the team meeting. While the team leader spoke the most, team members were given opportunities to speak up. However, five to six team members dominated the discussion and not all team members spoke. These observations indicated that both team members and team leaders engaged in voice, learning, supportive and familiarity behaviours. There were no counts of defensive voice, silence or unsupportive behaviour. The specific behaviours displayed can be seen in Table 3 and observer ratings can be seen in Table 4 .
Voice and silence
Team members described an open team atmosphere where they felt listened to, respected and psychologically safe. They felt comfortable speaking up about work issues or things “they felt very strongly” about and would go to their team leader if they were “frustrated” or “struggling” . Interviews highlighted that there were opportunities to speak up during meetings. However, team members remained silent about certain issues. Some team members believed that discussing conflict, personal or confidential issues within a team setting may not be “appropriate” . They would discuss these issues outside the team setting instead.
“but I would say maybe it’s when the group disassembles that some of those opinions come out, you know, it mightn’t always be that effective.”
Conflict was “pushed under the carpet” because team members wanted to avoid insulting or questioning others or didn’t want to “rock the boat or cause issues” . Conflict avoidance was linked to small team size which meant that “everybody knows each other” and it would “make it harder for yourself” to speak up about conflict. One junior team member felt uncomfortable speaking up about confrontational issues with more experienced team members due to a fear that they would be dismissive and think “sure what does {team member} know” . However, junior team members all felt comfortable or “confident” asking for help.
A senior member of team A suggested that explicitly asking for input from junior team members could improve psychological safety and speaking up.
“looking for people’s opinions rather than waiting for somebody to offer, like asking, maybe some of the younger members, because I actually do think their opinion is really valuable.”
A relaxed atmosphere was deliberately cultivated to encourage learning behaviour.
“we’re very aware of trying to create an environment, em, like relaxed environment because you know when they’re relaxed, they’re going to learn more, they’ll ask more questions”
Team members considered patient care to be their “focus” and felt they could speak up about patient safety issues. They recognised that speaking up about errors was important for learning and improvement within the team.
“there’s lots of different failures in the system that probably will lead to that happening again but it is important that we try, I suppose, to remedy them.”
Members of team A talked about their team having a solution-focused approach to problem solving and highlighted that the team’s supervision model created a psychologically safe space for learning. The team leader advocated for the importance of trying new things and learning from them. However, three team members said there was not enough time for learning and there was a need to schedule time for supervision, where concerns and ideas could be voiced.
“it’s just something that kind of does get put on the longer finger a little bit, so that, it probably would be good to actually have time like an actual scheduled time to do that.”
Members of team A talked about feeling supported by their team leader and their peers. This encouraged them to speak up.
“you can go to the group and they’ll have your back, in terms of, yeah, your kind of professional role.”
The team leader provided support in relation to career development as well as personal and work needs. Team members were confident they would be supported by their leader if/when they asked for it.
“whatever small little rubbish is going on in your life, she will take that, you know, really into consideration and she is really so much about the staff member.”
Familiarity
Familiarity between team members facilitated psychological safety. Team members found it easier to speak openly as they got to know one another better and worked together for longer.
“Yeah she’s very easy to talk to… because I’ve worked with her for about X years.”.
Lack of familiarity had a negative impact on team members’ feelings of psychological safety. One team member identified themselves as being new to the team. In addition, team members whose roles were more separate from the rest of the team felt less comfortable.
“I probably wouldn’t feel as comfortable getting involved in some of their discussions.”
Team members highlighted the need to build relationships with those who work in these separate roles.
Survey results indicated that team members felt psychologically safe. Participants gave a mean response of 6.750 for section 1, 6.405 for section 2 and 5.667 for section 3.
At first, the team leader gave feedback, then each team member had an opportunity to contribute. At the end of the meeting, team members were given an opportunity to raise any concerns. There were some tense moments where there may have been an undertone of confrontation. Jokes were used to defuse these moments. During these instances the observer felt that people could be holding back. All participants engaged in voice, supportive, learning and familiarity behaviours but also displayed unsupportive behaviours. Team members displayed defensive voice and silence behaviours.
According to interviews, the leader of team B created an open, inclusive team atmosphere which made team members feel psychologically safe.
“it’s an open forum and I’ve never really felt that I couldn’t say anything.”
Team members prioritised patients and would speak up about patient safety issues.
“because I would kind of be out for the patient, you know, so I would have enough {confidence}, to say that’s not acceptable, or it’s not acceptable behaviour.”
However, according to the team leader, meetings could be “more participative” without certain team members. This suggests that the presence of these team members reduces psychological safety for others. Participants described negative reactions to people speaking up during meetings, such as “tut tutting” , “rolling eyes” or “sighing” . The team leader highlighted the need for improving people’s behaviour during team meetings.
“I suppose people are less likely to contribute if they feel like that’s a risky response or there is the risk of that being a response.”
According to the team leader, improving psychological safety would involve making it clear to all team members that they play a valuable role in the team.
“it’s to convince, like everybody at that table has a critical role to play.”
Similar to Team A, conflict, personal or confidential issues were not deemed “appropriate” for the group setting and were discussed outside of team meetings. While conflict existed within the team it was not “open” and was “sometimes ignored” . Team members would withhold their “true feelings” to try to “keep the peace” , “incubate the mess in front of everybody” and to avoid making other team members feel attacked. When asked why conflict isn’t addressed, the team leader said, “we’re not there yet” .
Team members felt comfortable admitting mistakes and considered it to be the “whole point of the forum {team meeting}” and necessary for learning.
“you can’t fix them if you don’t highlight them.”
However, they also referred to individuals who have not admitted when they haven’t done something and have covered it up because “they don’t like to show up they’re not doing {something}.”
Interviews indicated that the team was going through an “evolution” and trying to become more focused on learning. This involved having dedicated time within and outside regular team meeting to discuss errors and concerns. According to the team leader, this improved speaking up and psychological safety in the team.
“We have had people say ‘I completely messed up’.”
Team members said that their leader is “100% behind you” and that leadership support played an important role in creating a psychologically safe environment.
“I think too it’s down to having the confidence in our leaders, in our leader as well. That you know that it’s kind of a safe space to talk.”
There was one reference to lack of peer support on the team. According to one participant, another team member has complained about a lack of support within the team, but this individual has not given support to others. This presented peer support as a reciprocal relationship between members.
“he wants support, he’s not giving support on the other side of it, he’s not giving support to us.”
One team member said they have received support in the form of other team members’ expertise.
“I’m not the expert in that field, I would be kind of guided by our {lists specific roles}.”
Most team members have worked in the hospital for long enough to be familiar with their colleagues. This made it easier for them to speak up.
“maybe because I’m here so long that maybe it’s a thing with age (laughs). You know, I don’t have a problem really in that kind of a setting speaking.”
There were three team members who identified themselves as being new to the team. A new team member didn’t feel the same level of comfort as others because she felt the team didn’t know her well enough. This team member highlighted the need for time with the team in order for her to become more comfortable.
“I’m still not 100% comfortable, I don’t think they know me yet.”
Survey results indicated that team members felt psychologically safe. Participants gave a mean response of 6.611 for section 1, 6.064 for section 2 and 5.308 for section 3.
There was a collaborative, inclusive and constructive atmosphere during the team meeting. While there were opportunities for participants to speak up, certain individuals dominated the discussions. All participants displayed voice, supportive, learning and familiarity behaviours. Team members displayed one count of unsupportive behaviour. There were no defensive voice or silence behaviours recorded.
Interviews referenced a historical culture of fear which lead to a lack of honesty and low psychological safety. One team member said that it has been difficult to change this culture completely, since the same people are still working there. As a result, some of this culture remained and team members reported silence and a lack of encouragement to speaking up.
“I think overall, the consensus was not to speak, there was never encouragement to speak so I can’t think of any occasion where I actually felt comfortable, there may have been occasions where I became so frustrated, that then I would have, you know, given my opinions, but that would not have been done in a comfortable environment.”
Position in the hierarchy influenced speaking up behaviour. The team leader was aware that team members may remain silent because of her role as leader. According to one team member, there was a reluctance to speak up when the team leader was present. This team member thought that there would be more open discussions and more things would “come out” if they could run their own meetings and meet their leader less regularly.
“they don’t want to say with the management there, because it will show them to be not coping as well.”
However, Team C was going through a “transition” and was changing from the historically “negative” culture. The team leader aimed to make the team more inclusive and let ideas “come from them {team members} up” . Team members felt psychologically safe with the leader because she is “reasonable” and they felt valued by her.
“I actually would be 100% confident, that if I did have to challenge any of her, em, any concerns that there wouldn’t be a problem that she’s extremely reasonable and yeah.”
Team members discussed patient safety and actively raised issues in order to have an open discussion and avoid creating tension or misunderstandings.
“I can voice it and everyone knows what my opinion is and I know what other people’s opinion is rather than them go to a one to one, and say, I don’t agree with x, y and z, because I think that’s kind of going behind people’s backs, in a certain way.”
However, like the other teams, they would discuss personal or confidential issues outside of the team setting.
Learning behaviour
The team leader said that by speaking up about mistakes, she could foster trust and encourage other team members to do the same.
“so I think the more they see me owning up to mistakes, the more they’re going to trust me {…} and the more they’ll own up to mistakes.”
One team member referred to the team as being very “pro-learning” and that team members were encouraged to speak up so they could learn from every “meeting or conflict” .
“they’re very much encouraging you to say it, it’s a safe space we’re not going to go back and, and talk about it, and we can learn, because I might be struggling with something, that someone else mentions, and I go, ‘oh god, I’m actually struggling with that area too, how are you going about it?’”
Team members referred to the leader being supportive, inclusive and “open” . One team member has learned from experience that she was more likely to get support if she approached team members one to one, rather than in a group setting
“I realised you’re better off actually going from one to one to one before than bringing it up {in a group setting}, and then you might get some support behind you.”
Familiarity between team members and the fact that they were all part of the same discipline, encouraged psychological safety.
“most of us have worked together for a while so we know what’s going on.”
One team member identified themselves as being new to the team. There was a lack of familiarity between the team leader and the other team members and there was still a need for trust to build between them.
“going to take a while though, {…} for me to be able to say to you, you know, tell you what, they do trust me and we’re open.”
One team member said that if the team had been given more opportunities to become familiar with one another when they first joined the team, they would feel more comfortable within team meetings.
“to get more familiar with each other and not to be as worried about somebody else being in the room.”
Survey results indicated that team members felt psychologically safe. Based on pilot testing, survey responses were altered to provide participants with a wider spectrum of response options (O’Donovan et al., in press). Responses could be between 1 and 10, 1 being “strongly disagree” and 10 being “strongly agree”. Participants gave a mean response of 7.704 for section 1, 8.071 for section 2 and 7.333 for section 3.
There was a positive, friendly and constructive atmosphere during the team meeting. While some tension was noted between the senior team members, there were opportunities for speaking up and most team members communicated openly. Decisions were made together, and team members seemed not be holding anything back. All participants displayed voice, silence, supportive, learning and familiarity behaviours. There was one count of unsupportive behaviour for the team leader.
All team members felt there were opportunities to speak up within team meetings and gave examples of speaking up about work related issues, including patient safety issues.
“the staff meeting, the biggest decisions are made at those and I think everyone gets an opportunity to weigh in.”
However, team members also noted that meetings mostly focused on operational issues. As a result, the issues that the team members wanted to raise were not given time.
“the bits that maybe us minions (laughs) want to talk about is back loaded.”
Participants suggested building time into meetings to discuss team members’ concerns and for them to connect in “a meaningful way” and understand where one another’s “emotions are at on a daily basis” in order to provide support and reassurance.
There was more pressure when raising issues in the group and so team members would speak to the leader about personal issues or would discuss conflict with one other team member.
“I would be more likely to bring things to my {team leader}, or to talk to people at an individual level em, if it was something sort of, I don’t know, beyond those boundaries.”
The majority of team members’ silence occurred when they gathered together as a group. Conflict or disagreements happened “under the covers” or got “brushed away” and were not discussed openly. Team members said they remained silent in team meetings to be polite and respectful to one another. They position this as a functional way to maintain good working relationships.
“so yeah, I think politeness really underpins a lot of our interactions.”
The influence of hierarchy and experience was also noted. Senior members were aware that junior team members were less likely “to rock the boat or make suggestions” . While junior team members were more nervous about speaking up, they became more psychologically safe as they gained experience.
“knowing what’s too much for one person really helped me figure out when to kind of just get on with it or when to kind of ask around.”
There were team members who remained silent about their ideas for change rather than risk sharing them with the team.
“don’t know if I’d feel comfortable suggesting too much change, just because I’d feel like that’s not really my remit or you know, everything, there’s a lot of well-established routines and I wouldn’t really be one to rock the boat too much.”
However, participants commented that the team has improved and become more open to learning and change. One member said it was easier for them to speak up and share their opinions during the meeting which was observed as part of this study.
“people were speaking up and we were able to push what was going to work best for us across.”
Examples were given of peer support. One participant referred to being supported during a difficult experience, explained that the team is very supportive, and that providing support is part of their jobs.
“I think this is one of the most supportive teams that I have ever experienced, em like I said there is nobody on the team that I haven’t spoken to about one thing or another.”
The leader was described as approachable, inclusive and supportive. Receiving support from the team leader made participants “confident in their choice” to speak up and share their opinion.
Familiarity between team members influenced psychological safety. They were more comfortable speaking to the team members who they worked closely with or considered good friends. There was one team member who identified themselves as being new to the team. One participant said that she would feel more “conscious” of what she was saying to team members who she didn’t work closely with, suggesting lower psychological safety. Others said their psychological safety improved as they got to know their colleagues better.
“I’ve become much more comfortable as I’ve gotten to know people to ask for help.”
This study provides an in-depth understanding of psychological safety within four healthcare teams working in the same case study hospital. It addresses recent calls for the use of multiple methods to capture a more accurate and nuanced understanding of psychological safety in healthcare teams [ 8 , 10 ]. While survey results from each team reflected high psychological safety, observations and interviews captured exceptional cases and more subtle dynamics within teams. Observations captured behaviours displayed during team meetings while interviews offered an insight into psychological safety both within and outside meetings, as well as within a historical context. An overview of the results can be seen in Fig. 1 . In this figure, we aim to highlight the indicators of psychological safety identified at both team and individual levels. Figure 1 also illustrates the added degree of variance in psychological safety captured by observations and interviews, in comparison to survey results. While survey results indicated medium to high levels of psychological safety within all teams, both observations and interviews captured examples of silence and an absence of learning behaviour. In addition, interviews highlighted examples of low levels of support from other team members and a lack of familiarity between certain team members. Survey and observation results captured team level dynamics which gave context to our understanding of individual level perceptions of psychological safety. This was particularly important, given that the overarching aim of this research is to inform the development of a team-level intervention to improve psychological safety.
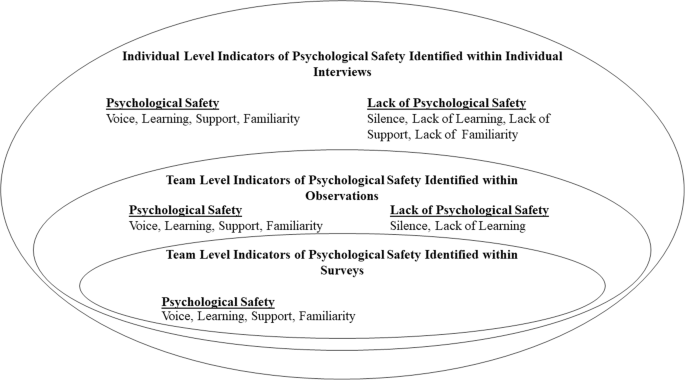
Indicators of Psychological Safety Identified at the Team and Individual Levels. This figure illustrated the key findings coming from each data collection source. Positive and negative indicators of psychological safety are indicated in relation to voice, learning, support and familiarity
According to interviews, team members felt more psychologically safe speaking up about certain topics. All teams prioritised patient safety and felt comfortable speaking up about concerns related to patient safety, indicating a sense of psychological safety [ 19 ]. However, silence was observed in teams A, B and C, there were lower survey scores for questions referring to speaking up about personal issues or disagreements, and interviews indicated that team members found speaking up about conflict or personal issues difficult. While junior team members could ask senior members for help and advice, they found it difficult to raise issues that could be deemed as challenging or confrontational. The influence of hierarchy was seen in all teams. This corresponds with research illustrating that those with higher status reported higher levels of psychological safety [ 26 , 27 , 38 ]. While team members found it difficult to engage with conflict or disagreements during team meetings, some found it easier during one-to-one discussions with either the team leader or another team member involved in the issue. Learning behaviours were displayed throughout team observations, and team members’ survey responses indicated that they could ask questions and share ideas. Interviews highlight that teams B, C and D are going through transitions, engaging in more learning initiatives, and becoming more psychologically safe. The leaders of teams B and C are both actively creating an open and inclusive team environment. According to interviews, the leader of team C engages in inclusive leadership by explicitly asking team members for their input and sharing her mistakes with the team in order to role model speaking up behaviour. Research has shown that doing this encourages psychological safety [ 18 , 39 , 40 , 41 ]. In team B, the leader introduced protected time for developing teamwork and discussing concerns or mistakes made. While interviews indicated that team D has become more open, team members highlighted the need for protected time during team meetings for people to raise issues that were important to them, to connect to one another and to discuss their experiences that week.
All leaders displayed supportive behaviour during observations. The leader of team B showed the most supportive behaviour, using inclusive language throughout the meeting. Survey and interview data indicated that team members felt supported by their team leaders. However, interviews highlighted that there were still examples of team members not feeling comfortable taking interpersonal risks. While past research has highlighted the role of supportive leaders play in promoting psychological safety [ 23 , 24 , 25 ], supportive leadership alone is not enough. As discussed above, there were still issues that team members didn’t feel comfortable discussing and the impact of hierarchy and historical cultures of fear could still be seen.
Interpersonal dynamics also influenced psychological safety. As outlined in previous literature, peer support improves psychological safety within teams [ 10 ]. During observations of team B, team members showed lower supportive behaviours than their team leader and, during interviews, only one team member mentioned receiving peer support. Lower levels of peer support were found in the multidisciplinary team, where team members worked in different departments. When team members worked within the same discipline, it was easier for them to support one another in their roles and this facilitated psychological safety.
Since members of team B had been working in the hospital for a long time, they were familiar with one another. However, on teams A and D, some team members worked separately from the rest of the team. As a result, they were less familiar with and comfortable around other team members. A member of team C suggested that if team members were given time to get to know one another without the presence of their leader, they would become more comfortable and issues could be discussed more openly. Having close and connected working roles facilitates familiarity and, as a result, psychological safety. This highlights the need for teams whose roles are more separate from one another to make deliberate efforts to cultivate familiarity. This corresponds with the need to develop interventions which are suited for use across and between multiple disciplines [ 8 ]. This is particularly important in a healthcare context, where psychological safety is needed for “teaming”, an active process which allows multidisciplinary healthcare teams to work together to deliver increasingly complex patient care [ 10 , 42 ].
Implications for practice and future research
In addition to gaining an understanding of psychological safety within healthcare teams, this study aimed to inform the development of interventions to improve it. A recent systematic review of such interventions has highlighted that in order to improve their effectiveness, interventions targeting psychological safety need to be grounded in the experiences of the target audience [ 8 ]. This study contributes to a more in-depth understanding of psychological safety within healthcare teams which is needed to develop future interventions. Compared to observation and survey data, the data collected through interviews with team members provided the most valuable insights into the specific areas which interventions can target. This is because participants were given the opportunity to discuss areas in which they thought psychological safety in their team could be improved. Firstly, the issue of time was raised in each team. This mainly involved giving time during meetings for discussing more personal issues or experiences rather than only focusing on operational issues. This had already been done within team B and the team leader had noticed some improvements in trust and openness as a result. Time was also needed for prioritising learning and becoming more familiar with one another. Secondly, since team members felt more psychologically safe talking about difficult subjects during one-to-one interactions, these opportunities for interactions outside of a team setting should be encouraged. Interviews also highlighted the need to build relationships and foster familiarity with new team members and team members who work separately from the rest of the team. Lastly, interventions should encourage an awareness that all team members play a valuable role and explicitly ask for input from team members who are more vulnerable to low psychological safety, such as junior team members.
For future research, it is important to note the impact different data collection methods has on our understanding of psychological safety. As can be seen from Fig. 1 , surveys provided an overview of the levels of psychological safety within the teams, however, observations and interviews provide more detailed and nuanced understanding. Observations provided a more objective view of behaviours relating to psychological safety [ 34 ] and interviews offered insight into team members’ past and present experiences both within and outside team meetings. Researchers should be aware of the different levels of understanding gained from the use of these different methods of data collection and use this to ensure the type of data they collect is suited to their research question.
Strengths and limitations
This study combined survey, observation and interview data to gain an in-depth understanding of psychological safety within four healthcare teams. The deliberate inclusion of common components across the survey, observations, and interview analysis facilitated the triangulation of data. This provided a more detailed and holistic understanding of psychological safety.
However, some limitations must also be noted. Data was collected within one case study hospital, restricting the generalisability of findings. To address this, we have presented detailed analysis and given as much contextual information as possible for each team, without compromising the anonymity of participants. This should allow readers to determine whether they are applicable in other settings [ 32 , 43 ].
Through examining the different outputs using multiple methods of data collection, this study provides a more in-depth understanding of psychological safety in healthcare teams. Within observations, it was difficult to accurately observe silence, count individual episodes of silence and determine the motivation behind silence. However, interviews were a valuable source for exploring team members’ reasons for remaining silent. While both interviews and surveys are vulnerable to self-report bias [ 44 ], the observation measure offers a more objective measure of psychological safety. The observation measure also provides information on team-level dynamics related to psychological safety. This team-level understanding aided our analysis of interviews in order to capture individual team members’ perceptions of psychological safety. This understanding is important since the overarching aim of the programme of research (of which this study is one component) is to inform the design of an intervention to improve psychological safety at the team level. In order to calculate inter-rater reliability for the observation measure without inhibiting teams by having multiple coders present, future research could use a video camera to record meetings [ 45 , 46 ].
This study examines psychological safety within four healthcare teams. Results from surveys, observations and interviews are considered together in order to gain an in-depth understanding of psychological safety within these teams. Based on our findings, recommendations are made for future research and the development of interventions to improve psychological safety.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Edmondson A. Psychological safety and learning behavior in work teams. Adm Sci Q. 1999;44(2):350–83.
Google Scholar
Nembhard IM, Edmondson AC. Making it safe: the effects of leader inclusiveness and professional status on psychological safety and improvement efforts in health care teams. J Organ Behav. 2006;27(7):941–66.
Moore L, McAuliffe E. To report or not to report? Why some nurses are reluctant to whistleblow. Clin Gov Int J. 2012;17(4):332–42.
Moore L, McAuliffe E. Is inadequate response to whistleblowing perpetuating a culture of silence in hospitals? Clin Gov Int J. 2010;15(3):166–78.
Edmondson AC. Speaking up in the operating room: how team leaders promote learning in interdisciplinary action teams. J Manag Stud. 2003;40(6):1419–52.
Unal A, Seren S. Medical error reporting attitudes of healthcare personnel, barriers and solutions: a literature review. J Nurs Care. 2016;5(6):377.
Swendiman RA, Edmondson AC, Mahmoud NN. Burnout in surgery viewed through the lens of psychological safety. Ann Surg. 2019;269(2):234–5.
PubMed Google Scholar
O’Donovan R, McAuliffe E. A systematic review exploring the content and outcomes of interventions to improve psychological safety, speaking up and voice behaviour. BMC Health Serv Res. 2020;20(1):1–11.
Stoller JK. Reflections on leadership in the time of COVID-19. BMJ Lead. 2020;4(2):77–9.
Newman A, Donohue R, Eva N. Psychological safety: a systematic review of the literature. Hum Resour Manag Rev. 2017;27(3):521–35.
Molina-Azorin JF, Bergh DD, Corley KG, Ketchen DJ Jr. Mixed methods in the organizational sciences: taking stock and moving forward. Organ Res Methods. 2017;20(2):179–92.
Edmondson AC, McManus SE. Methodological fit in management field research. Acad Manag Rev. 2007;32(4):1246–64.
Edmondson AC, Lei Z. Psychological safety: the history, renaissance, and future of an interpersonal construct. Annu Rev Organ Psychol Organ Behav. 2014;1(1):23–43.
Pearsall MJ, Ellis AP. Thick as thieves: the effects of ethical orientation and psychological safety on unethical team behavior. J Appl Psychol. 2011;96(2):401.
Bienefeld N, Grote G. Speaking up in ad hoc multiteam systems: individual-level effects of psychological safety, status, and leadership within and across teams. Eur J Work Organ Psychol. 2014;23(6):930–45.
Leroy H, Dierynck B, Anseel F, Simons T, Halbesleben JR, McCaughey D, et al. Behavioral integrity for safety, priority of safety, psychological safety, and patient safety: a team-level study. J Appl Psychol. 2012;97(6):1273–81.
Carmeli A, Sheaffer Z. How learning leadership and organizational learning from failures enhance perceived organizational capacity to adapt to the task environment. J Appl Behav Sci. 2008;44(4):468–89.
Hirak R, Peng AC, Carmeli A, Schaubroeck JM. Linking leader inclusiveness to work unit performance: the importance of psychological safety and learning from failures. Leadersh Q. 2012;23(1):107–17.
O’Donovan R, Mcauliffe E. A systematic review of factors that enable psychological safety in healthcare teams. Int J Qual Health Care. 2020;32(4):240–50.
Sherf EN, Parke MR, Isaakyan S. Distinguishing voice and silence at work: unique relationships with perceived impact, psychological safety, and burnout. Acad Manag J. 2020. https://doi.org/10.5465/amj.2018.1428 .
Carmeli A, Gittell JH. High-quality relationships, psychological safety, and learning from failures in work organizations. J Organ Behav Int J Ind Occup Organ Psychol Behav. 2009;30(6):709–29.
May DR, Gilson RL, Harter LM. The psychological conditions of meaningfulness, safety and availability and the engagement of the human spirit at work. J Occup Organ Psychol. 2004;77(1):11–37.
Appelbaum NP, Dow A, Mazmanian PE, Jundt DK, Appelbaum EN. The effects of power, leadership and psychological safety on resident event reporting. Med Educ. 2016;50(3):343–50.
Aranzamendez G, James D, Toms R. Finding antecedents of psychological safety: a step toward quality improvement. Nurs Forum. 2015;50(3):171–8.
Edmondson AC. Managing the risk of learning: Psychological safety in work teams. In: International Handbook of Organizational Teamwork. Chichester: Wiley; 2008. p. 255.
Jain AK, Fennell ML, Chagpar AB, Connolly HK, Nembhard IM. Moving toward improved teamwork in cancer care: the role of psychological safety in team communication. J Oncol Pract. 2016;12(11):1000–11.
Reese J, Simmons R, Barnard J. Assertion practices and beliefs among nurses and physicians on an inpatient pediatric medical unit. Hosp Pediatr. 2016;6(5):275–81.
Hoenderdos JW. Towards an observational measure for team psychological safety [dissertation]. The Netherlands: University of Twente; 2013.
Bradley BH, Postlethwaite BE, Klotz AC, Hamdani MR, Brown KG. Reaping the benefits of task conflict in teams: the critical role of team psychological safety climate. J Appl Psychol. 2012;97(1):151.
Devers K, Frankel R. Study design in qualitative research—2: sampling and data collection strategies. Educ Health. 2000;13(2):263–71.
CAS Google Scholar
Yin RK. Case study research and applications: design and methods. Thousand Oaks: Sage publications; 2017.
Tracy SJ. Qualitative quality: eight “big-tent” criteria for excellent qualitative research. Qual Inq. 2010;16(10):837–51.
Ellingson LL. Engaging crystallization in qualitative research: an introduction. Thousand Oaks: Sage; 2009.
O’Donovan R, Van Dun D, McAuliffe E. Measuring psychological safety in healthcare teams: developing a more accurate and nuanced mixed-methods approach. BMC Med Res Methodol. 2020;20(1):1–17.
Darbyshire P, McDonald H. Choosing response scale labels and length: Guidance for researchers and clients. Australas J Market Res. 2004;12(2):17–26.
Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101.
Boyatzis RE. Transforming qualitative information: Thematic analysis and code development. Thousand Oaks: Sage; 1998.
Schwappach DL, Gehring K. Trade-offs between voice and silence: a qualitative exploration of oncology staff’s decisions to speak up about safety concerns. BMC Health Serv Res. 2014;14(1):303.
PubMed PubMed Central Google Scholar
Halbesleben JR, Rathert C. The role of continuous quality improvement and psychological safety in predicting work-arounds. Health Care Manag Rev. 2008;33(2):134–44.
Raes E, Decuyper S, Lismont B, Van den Bossche P, Kyndt E, Demeyere S, et al. Facilitating team learning through transformational leadership. Instr Sci. 2013;41(2):287–305.
Alingh CW, van Wijngaarden JD, van de Voorde K, Paauwe J, Huijsman R. Speaking up about patient safety concerns: the influence of safety management approaches and climate on nurses’ willingness to speak up. BMJ Qual Saf. 2019;28(1):39–48.
Edmondson AC. Teaming: how organizations learn, innovate, and compete in the knowledge economy. San Francisco: Wiley; 2012.
Gomm R, Hammersley M, Foster P. Case study method: key issues, key texts. Thousand Oaks: Sage; 2000.
Donaldson SI, Grant-Vallone EJ. Understanding self-report bias in organizational behavior research. J Bus Psychol. 2002;17(2):245–60.
Hoogeboom MAMG, Wilderom CPM. A complex adaptive systems approach to real-life team interaction patterns, task context, information sharing, and effectiveness. Group Organ Manag. 2020;45(1):3–42.
Waller MJ, Kaplan SA. Systematic Behavioral observation for emergent team phenomena: key considerations for quantitative video-based approaches. Organ Res Methods. 2018;21(2):500–15.
Download references
Acknowledgements
Not applicable.
This research is funded by the Irish Research Council and the Ireland East Hospital Group under the Employment Based Partnership Scholarship. The funders did not play a role in the design of the study, data collection, analysis and interpretation or in writing the manuscript.
Author information
Authors and affiliations.
Centre for Interdisciplinary Research, Education, and Innovation in Health Systems (IRIS), School of Nursing, Midwifery & Health Systems, Health Sciences Centre, University College Dublin, Dublin 4, Ireland
Róisín O’Donovan & Eilish McAuliffe
You can also search for this author in PubMed Google Scholar
Contributions
Both authors were involved in the design and planning of this study. ROD completed data collection and analysis. EMcA analysed 10% of interviews completed. ROD drafted the manuscript and EMcA contributed to writing and revising the paper. Both authors read and approved the final manuscript.
Corresponding author
Correspondence to Róisín O’Donovan .
Ethics declarations
Ethics approval and consent to participate.
Ethical approval was obtained for this study from the Human Research Ethics Committee in University College Dublin (Reference number: LS-17-67). Written informed consent was obtained from all participants prior to each stage of data collection.
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
O’Donovan, R., McAuliffe, E. Exploring psychological safety in healthcare teams to inform the development of interventions: combining observational, survey and interview data. BMC Health Serv Res 20 , 810 (2020). https://doi.org/10.1186/s12913-020-05646-z
Download citation
Received : 14 April 2020
Accepted : 12 August 2020
Published : 31 August 2020
DOI : https://doi.org/10.1186/s12913-020-05646-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Psychological safety
- Mixed methods
- Healthcare teams
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]

The importance of patient case studies in delivery of evidence-based care
Posted On 3 Jun, 2024 Read Time 3 min Tags case study , clinical education , collaboration , evidence-based care , NALHN , ophthalmology , podcast , rare conditions
Ongoing education is a core aspect of healthcare delivery at Central Adelaide Local Health Network (CALHN).
But with busy schedules and only so many hours in the day, it can be challenging for clinicians to keep up-to-date with all the specialist areas of health. That’s why published patient case studies are so valuable.
“Doctors share case studies to spread knowledge about unique or rare clinical scenarios they encounter,” said CALHN Basic Physician Trainee Dr Brandon Stretton. “By publishing these cases, they help other healthcare professionals learn from their experiences, which can be incredibly useful in diagnosing and treating future patients.” “Case studies are a way to contribute to the collective knowledge and improve patient care across the board.”
A case study is a write-up of the presentation and clinical management of a specific patient, with all personal details removed and consent provided.

Sudden vision loss – but what’s causing it?
Dr Stretton and CALHN opthalmologist Dr Sumu Simon recently published a case study about a man who presented to the emergency department reporting sudden onset vision loss in his right eye lasting several hours. The case is also presented in a recent episode of the Royal Australasian College of Physicians podcast, Pomegranate Health, which was prepared in collaboration with clinicians from Northern Adelaide Local Health Network (NALHN).
“This case is particularly significant because it highlights a sight-threatening manifestation of a systemic disease, which is crucial for clinicians to recognise and engage the appropriate multi-disciplinary teams,” Dr Stretton said. “Awareness of such cases can lead to prompt diagnosis and treatment, potentially preventing serious complications.” “Publishing and discussing this case helps to inform and educate a wide range of healthcare providers about the condition, its diagnosis, and the latest treatment approaches.”
In this case, the patient was effectively managed through accurate identification and timely management of the cause of his vision loss.

Keeping up-to-date
Dr Stretton said case studies play an important role in medical education.
“Many doctors, including myself, do regularly read case studies,” he says. “Case studies are particularly engaging and educational, offering practical insights that can be directly applied to patient care.” “Case studies are often used in training and ongoing professional development because they provide real-life contexts that enhance understanding and retention of medical knowledge.”
When included in reputable medical journals, case studies undergo a rigorous peer-review process – that is, they are scrutinised by experts in the field before publication.
Read the research
With co-authors Dr Yiran Tan and Dr Mark Hassall, Dr Stretton and Dr Simon published the paper The Role of Tocilizumab in Glucocorticoid Resistant Giant Cell Arteritis: A Case Series and Literature Review in the Journal of Neuro-Ophthalmology.
The podcast episode is hosted by Neurology Registrar Dr Stephen Bacchi from NALHN.
If you have published a case report that may benefit others through discussion in a podcast format, please reach out to Dr Stretton ([email protected]) and Dr Bacchi ([email protected]).
Related Posts:

Recent Posts
- Kidney transplant, or not? Research to guide difficult decisions
- It’s all about the details: how well-designed research improves clinical care
- New research targets the vicious cycle of infection in chronic lung disease
- Case study: the small South Australian fish that packs a dangerous toxin
- CALHN invested in a bespoke program to support patients after surgery. Now the world is taking notice
- Ask the Expert
- Central Adelaide LHN Staff
- Hampstead Rehabilitation Centre
- prison health
- Refugee Health Service
- Repat Health Precinct
- Research Pulse
- Translating Research
- Business Essentials
- Leadership & Management
- Credential of Leadership, Impact, and Management in Business (CLIMB)
- Entrepreneurship & Innovation
- Digital Transformation
- Finance & Accounting
- Business in Society
- For Organizations
- Support Portal
- Media Coverage
- Founding Donors
- Leadership Team

- Harvard Business School →
- HBS Online →
- Business Insights →
Business Insights
Harvard Business School Online's Business Insights Blog provides the career insights you need to achieve your goals and gain confidence in your business skills.
- Career Development
- Communication
- Decision-Making
- Earning Your MBA
- Negotiation
- News & Events
- Productivity
- Staff Spotlight
- Student Profiles
- Work-Life Balance
- AI Essentials for Business
- Alternative Investments
- Business Analytics
- Business Strategy
- Business and Climate Change
- Creating Brand Value
- Design Thinking and Innovation
- Digital Marketing Strategy
- Disruptive Strategy
- Economics for Managers
- Entrepreneurship Essentials
- Financial Accounting
- Global Business
- Launching Tech Ventures
- Leadership Principles
- Leadership, Ethics, and Corporate Accountability
- Leading Change and Organizational Renewal
- Leading with Finance
- Management Essentials
- Negotiation Mastery
- Organizational Leadership
- Power and Influence for Positive Impact
- Strategy Execution
- Sustainable Business Strategy
- Sustainable Investing
- Winning with Digital Platforms
5 Benefits of Learning Through the Case Study Method

- 28 Nov 2023
While several factors make HBS Online unique —including a global Community and real-world outcomes —active learning through the case study method rises to the top.
In a 2023 City Square Associates survey, 74 percent of HBS Online learners who also took a course from another provider said HBS Online’s case method and real-world examples were better by comparison.
Here’s a primer on the case method, five benefits you could gain, and how to experience it for yourself.
Access your free e-book today.
What Is the Harvard Business School Case Study Method?
The case study method , or case method , is a learning technique in which you’re presented with a real-world business challenge and asked how you’d solve it. After working through it yourself and with peers, you’re told how the scenario played out.
HBS pioneered the case method in 1922. Shortly before, in 1921, the first case was written.
“How do you go into an ambiguous situation and get to the bottom of it?” says HBS Professor Jan Rivkin, former senior associate dean and chair of HBS's master of business administration (MBA) program, in a video about the case method . “That skill—the skill of figuring out a course of inquiry to choose a course of action—that skill is as relevant today as it was in 1921.”
Originally developed for the in-person MBA classroom, HBS Online adapted the case method into an engaging, interactive online learning experience in 2014.
In HBS Online courses , you learn about each case from the business professional who experienced it. After reviewing their videos, you’re prompted to take their perspective and explain how you’d handle their situation.
You then get to read peers’ responses, “star” them, and comment to further the discussion. Afterward, you learn how the professional handled it and their key takeaways.
Learn more about HBS Online's approach to the case method in the video below, and subscribe to our YouTube channel for more.
HBS Online’s adaptation of the case method incorporates the famed HBS “cold call,” in which you’re called on at random to make a decision without time to prepare.
“Learning came to life!” said Sheneka Balogun , chief administration officer and chief of staff at LeMoyne-Owen College, of her experience taking the Credential of Readiness (CORe) program . “The videos from the professors, the interactive cold calls where you were randomly selected to participate, and the case studies that enhanced and often captured the essence of objectives and learning goals were all embedded in each module. This made learning fun, engaging, and student-friendly.”
If you’re considering taking a course that leverages the case study method, here are five benefits you could experience.
5 Benefits of Learning Through Case Studies
1. take new perspectives.
The case method prompts you to consider a scenario from another person’s perspective. To work through the situation and come up with a solution, you must consider their circumstances, limitations, risk tolerance, stakeholders, resources, and potential consequences to assess how to respond.
Taking on new perspectives not only can help you navigate your own challenges but also others’. Putting yourself in someone else’s situation to understand their motivations and needs can go a long way when collaborating with stakeholders.
2. Hone Your Decision-Making Skills
Another skill you can build is the ability to make decisions effectively . The case study method forces you to use limited information to decide how to handle a problem—just like in the real world.
Throughout your career, you’ll need to make difficult decisions with incomplete or imperfect information—and sometimes, you won’t feel qualified to do so. Learning through the case method allows you to practice this skill in a low-stakes environment. When facing a real challenge, you’ll be better prepared to think quickly, collaborate with others, and present and defend your solution.
3. Become More Open-Minded
As you collaborate with peers on responses, it becomes clear that not everyone solves problems the same way. Exposing yourself to various approaches and perspectives can help you become a more open-minded professional.
When you’re part of a diverse group of learners from around the world, your experiences, cultures, and backgrounds contribute to a range of opinions on each case.
On the HBS Online course platform, you’re prompted to view and comment on others’ responses, and discussion is encouraged. This practice of considering others’ perspectives can make you more receptive in your career.
“You’d be surprised at how much you can learn from your peers,” said Ratnaditya Jonnalagadda , a software engineer who took CORe.
In addition to interacting with peers in the course platform, Jonnalagadda was part of the HBS Online Community , where he networked with other professionals and continued discussions sparked by course content.
“You get to understand your peers better, and students share examples of businesses implementing a concept from a module you just learned,” Jonnalagadda said. “It’s a very good way to cement the concepts in one's mind.”
4. Enhance Your Curiosity
One byproduct of taking on different perspectives is that it enables you to picture yourself in various roles, industries, and business functions.
“Each case offers an opportunity for students to see what resonates with them, what excites them, what bores them, which role they could imagine inhabiting in their careers,” says former HBS Dean Nitin Nohria in the Harvard Business Review . “Cases stimulate curiosity about the range of opportunities in the world and the many ways that students can make a difference as leaders.”
Through the case method, you can “try on” roles you may not have considered and feel more prepared to change or advance your career .
5. Build Your Self-Confidence
Finally, learning through the case study method can build your confidence. Each time you assume a business leader’s perspective, aim to solve a new challenge, and express and defend your opinions and decisions to peers, you prepare to do the same in your career.
According to a 2022 City Square Associates survey , 84 percent of HBS Online learners report feeling more confident making business decisions after taking a course.
“Self-confidence is difficult to teach or coach, but the case study method seems to instill it in people,” Nohria says in the Harvard Business Review . “There may well be other ways of learning these meta-skills, such as the repeated experience gained through practice or guidance from a gifted coach. However, under the direction of a masterful teacher, the case method can engage students and help them develop powerful meta-skills like no other form of teaching.”

How to Experience the Case Study Method
If the case method seems like a good fit for your learning style, experience it for yourself by taking an HBS Online course. Offerings span eight subject areas, including:
- Business essentials
- Leadership and management
- Entrepreneurship and innovation
- Digital transformation
- Finance and accounting
- Business in society
No matter which course or credential program you choose, you’ll examine case studies from real business professionals, work through their challenges alongside peers, and gain valuable insights to apply to your career.
Are you interested in discovering how HBS Online can help advance your career? Explore our course catalog and download our free guide —complete with interactive workbook sections—to determine if online learning is right for you and which course to take.

About the Author

“Case Studies in Healthcare: Success Stories and Lessons Learned”

Table of Contents
The healthcare industry is an ever-evolving field with innovations and improvements happening daily. As healthcare providers strive to deliver the best care possible, case studies have become a valuable resource for learning and growth. In this article, we will explore various case studies in healthcare, highlighting both success stories and the lessons learned along the way. By analyzing what works and why, we can gain insight into the practices that lead to triumphs in healthcare and potentially replicate these successes in our own organizations.
Case Studies in Healthcare: A Closer Look at Triumphs and Takeaways
Healthcare case studies provide a unique opportunity to dissect real-world scenarios, understand the decisions made, and measure the outcomes of those choices. One notable success story is the implementation of telemedicine in rural areas. By leveraging technology, healthcare providers have successfully expanded access to care for patients who would otherwise have to travel long distances for treatment. Lessons learned include the importance of investing in reliable technology and training staff to effectively use telemedicine platforms.
Another critical case study involves the management of electronic health records (EHRs). When a large hospital system transitioned to a new EHR system, they faced significant resistance from physicians who were accustomed to the old way of doing things. However, by involving physicians in the planning and implementation process, the hospital successfully integrated the new system, leading to improved efficiency and patient care. This case study highlights the value of stakeholder engagement and effective change management.
In the fight against infectious diseases, case studies have shown the significance of swift and coordinated responses. An example of this is the containment of Ebola in West Africa. Through international collaboration and the rapid deployment of healthcare resources, the spread of the virus was effectively limited. This case study underscores the importance of preparedness, communication, and teamwork in tackling healthcare crises.
Success Stories in Healthcare: Analyzing What Works and Why
Understanding why certain strategies succeed is crucial for replicating positive results in the healthcare industry. For instance, one hospital’s initiative to reduce patient readmissions focused on comprehensive discharge planning and follow-up care. By ensuring patients had clear instructions and support after leaving the hospital, readmission rates dropped significantly. This case study emphasizes the role of thorough patient education and post-discharge care in improving outcomes.
In the realm of preventive care, a primary care clinic introduced a program to increase vaccination rates among its patient population. By actively reaching out to patients due for immunizations and offering flexible scheduling options, the clinic saw a dramatic increase in vaccination rates. The takeaway from this case study is the impact of proactive patient engagement and removing barriers to care.
Lastly, a healthcare organization’s embrace of continuous quality improvement (CQI) led to enhanced patient safety and satisfaction. By fostering a culture of open communication and ongoing learning, the organization identified areas for improvement and systematically implemented changes. This case study demonstrates the power of a commitment to CQI as a driver for excellence in healthcare.
The healthcare industry is rich with case studies that provide valuable insights and lessons learned. By analyzing and understanding these success stories, healthcare providers can apply similar strategies to achieve positive outcomes in their own organizations. Whether it’s through technology, stakeholder engagement, or quality improvement initiatives, these case studies offer a blueprint for triumph and provide a roadmap for future success in the ever-changing landscape of healthcare.
Why are case studies valuable in the healthcare industry, and how do they provide insights into successful decision-making and problem-solving within healthcare organizations?
Case studies are valuable as they offer real-world examples of challenges and solutions in healthcare. They provide insights into successful decision-making, problem-solving, and strategies that can be applied by healthcare professionals and organizations facing similar scenarios.
How does the article select and present case studies, and what criteria are considered to ensure the relevance and applicability of the showcased success stories to a diverse audience?
The article discusses the criteria for selecting case studies, such as their impact on healthcare outcomes, innovation, or overcoming significant challenges. It highlights the diversity of cases to ensure relevance to a broad audience, considering different healthcare settings, specialties, and contexts.
Can you provide examples of healthcare case studies featured in the article, and how do these stories illustrate successful decision-making or lessons learned that can benefit readers in the healthcare field?
Certainly! Examples may include cases where innovative technologies improved patient outcomes, or instances where strategic decisions enhanced operational efficiency. The article presents these stories to illustrate valuable lessons learned and best practices that readers can apply in their own healthcare settings.
In what ways do case studies contribute to professional development and learning opportunities for healthcare professionals, and how can organizations leverage these stories for continuous improvement and staff training?
The article explores how case studies offer learning opportunities, allowing healthcare professionals to gain insights from others’ experiences. Organizations can leverage these stories for staff training, fostering a culture of continuous improvement and encouraging employees to apply lessons learned to their daily practices.
For healthcare leaders seeking to implement successful strategies within their organizations, what recommendations and actionable insights does the article provide based on the analysis of the showcased case studies?
The article offers recommendations based on the case studies, such as the importance of collaboration, data-driven decision-making, and embracing innovation. It provides actionable insights that healthcare leaders can use to inform their decision-making processes and drive positive outcomes within their organizations.
Leave a comment Cancel reply
You must be logged in to post a comment.
+1 (800) 782 1768
Pardon Our Interruption
As you were browsing something about your browser made us think you were a bot. There are a few reasons this might happen:
- You've disabled JavaScript in your web browser.
- You're a power user moving through this website with super-human speed.
- You've disabled cookies in your web browser.
- A third-party browser plugin, such as Ghostery or NoScript, is preventing JavaScript from running. Additional information is available in this support article .
To regain access, please make sure that cookies and JavaScript are enabled before reloading the page.
Former UTV Broadcaster shares blood cancer story to highlight importance of medical research in Northern Ireland
Giving hope for 60 years: Leukaemia & Lymphoma NI's legacy in the fight against blood cancer - As we celebrate 60 years of Leukaemia & Lymphoma NI's tireless work in the fight against blood cancer, we are honoured to share the powerful stories of those who have been directly touched by this disease. Through a series of compelling case studies, patients, family members and researchers open up about their personal journeys, offering a poignant look at the challenges they’ve faced, the resilience they’ve shown and the hope that continues to drive them forward.
- 18:13, 1 SEP 2024
- Updated 13:06, 2 SEP 2024

A former UTV broadcaster has been sharing the story of his battle with Chronic Lymphocytic Leukemia, a type of blood cancer, to highlight the importance of supporting local medical research funded by Leukaemia & Lymphoma NI.
Ken Reid joined UTV in 1994 and climbed the ranks to become Political Editor, a position he held until his retirement in 2021. After developing pain in his foot in 2016, Ken visited his doctor and was referred to Antrim Area Hospital.
"I thought it was perhaps an infection," Ken said.
READ MORE: MLA opens up about husband's battle with rare blood cancer
READ MORE: NI man's tribute to father who died from rare blood cancer
"But everything changed in an instant, when the very professional and caring young doctor there broke the news to me that I did, in fact, have Leukaemia."
After receiving his diagnosis, Ken agreed to take part in a clinical trial, testing the efficacy of a new drug treatment.
He added: "The trial opened my eyes to a world of medical science which I was not previously aware of. I was regularly monitored through appointments at Belfast City Hospital, but the trial was being conducted through partnerships with other cancer centres, the lead facility being in Leeds.
"It wasn’t always easy. Whilst the drugs I was taking did improve the prognosis on my Leukaemia, I experienced some strong side effects which took a toll. Last year I was in hospital for a two-month period, developed an infection and at one stage, caught coronavirus .
"But I’m glad to say that eight years on from my original diagnosis, I am feeling better than I have in a long time. That’s thanks to the cutting-edge treatment I’ve received."
Ken established strong links with Leukaemia & Lymphoma NI through the team of medical professionals with whom he was meeting regularly.
"What you begin to realise is that the Patrick G Johnston Centre at Queen’s University is part of a global network of research institutes, all devoted to establishing better outcomes for patients like me," he continued.

"We have a world-class facility in Belfast punching well above its weight in terms of the levels of research being conducted. I felt very strongly I needed to lend my support to the charity."
Throughout his treatment, and now acting as patron of the blood cancer charity, Ken has seen first hand how research funded by LLNI impacts the lives of people in Northern Ireland.
"When you regularly visit the Bridgewater Suite for cancer patients at City Hospital like I have, you get to know the doctors, nurses and your fellow patients. I’ve seen people have their conditions turned around thanks to treatments that were not available as recently as five or ten years ago.
"Leukaemia & Lymphoma NI are funding research and trials which are quite literally life changing. It’s work that deserves our support because the statistics around blood cancer in Northern Ireland are alarming, but the track record of research shows that our brilliant medical scientists, clinicians, doctors and nurses are finding solutions."
Leukaemia and Lymphoma NI recently announced a special programme of activities to mark the 60th year of the charity and raise funds for the fight against blood cancer. Alongside this, the charity is calling for those who have experienced Leukaemia, Lymphoma or Myeloma and their loved ones to share their experiences online via the LLNI website.
The photos and extended captions gathered will form part of a special online canvas presented online where members of the public can read the stories of people affected by blood cancer across the region.
On September 1, LLNI will kick off a series of fundraising activities with a Reflections evening walk around Hillsborough Forest Park lake for anyone affected directly or indirectly by blood cancer. The programme will culminate in the charity hosting a Black Tie & Diamonds Gala Ball at Titanic Belfast, where the winner of an ongoing raffle for a diamond pendant necklace will be selected at random.
Members of the public can share their story, make a donation or buy tickets for the diamond necklace raffle on the Leukaemia & Lymphoma NI website here.
Join our Belfast Live breaking news service on WhatsApp

Click this link or scan the QR code to receive breaking news and top stories from Belfast Live. We also treat our community members to special offers, promotions, and adverts from us and our partners. If you don’t like our community, you can check out any time you like. If you’re curious, you can read our Privacy Notice .
For all the latest news, visit the Belfast Live homepage here and sign up to our daily newsletter here.
- Most Recent

- Open access
- Published: 31 August 2024
Spatial analysis of the impact of urban built environment on cardiovascular diseases: a case study in Xixiangtang, China
- Shuguang Deng 1 ,
- Jinlong Liang 1 ,
- Ying Peng 2 ,
- Wei Liu 3 ,
- Jinhong Su 1 &
- Shuyan Zhu 1
BMC Public Health volume 24 , Article number: 2368 ( 2024 ) Cite this article
Metrics details
The built environment, as a critical factor influencing residents' cardiovascular health, has a significant potential impact on the incidence of cardiovascular diseases (CVDs).
Taking Xixiangtang District in Nanning City, Guangxi Zhuang Autonomous Region of China as a case study, we utilized the geographic location information of CVD patients, detailed road network data, and urban points of interest (POI) data. Kernel density estimation (KDE) and spatial autocorrelation analysis were specifically employed to identify the spatial distribution patterns, spatial clustering, and spatial correlations of built environment elements and diseases. The GeoDetector method (GDM) was used to assess the impact of environmental factors on diseases, and geographically weighted regression (GWR) analysis was adopted to reveal the spatial heterogeneity effect of environmental factors on CVD risk.
The results indicate that the built environment elements and CVDs samples exhibit significant clustering characteristics in their spatial distribution, with a positive correlation between the distribution density of environmental elements and the incidence of CVDs (Moran’s I > 0, p < 0.01). Further factor detection revealed that the distribution of healthcare facilities had the most significant impact on CVDs ( q = 0.532, p < 0.01), followed by shopping and consumption ( q = 0.493, p < 0.01), dining ( q = 0.433, p < 0.01), and transportation facilities ( q = 0.423, p < 0.01), while the impact of parks and squares ( q = 0.174, p < 0.01) and road networks ( q = 0.159, p < 0.01) was relatively smaller. Additionally, the interaction between different built environment elements exhibited a bi-factor enhancement effect on CVDs. In the local analysis, the spatial heterogeneity of different built environment elements on CVDs further revealed the regional differences and complexities.
Conclusions
The spatial distribution of built environment elements is significantly correlated with CVDs to varying degrees and impacts differently across regions, underscoring the importance of the built environment on cardiovascular health. When planning and improving urban environments, elements and areas that have a more significant impact on CVDs should be given priority consideration.
Peer Review reports
Cardiovascular diseases (CVDs) have become one of the most common lethal diseases worldwide, with both the number of affected individuals and the mortality rate continuously rising over the past two decades. Statistical data reveal that from 1990 to 2019, the number of individuals with CVDs globally increased from 271 to 523 million, while deaths climbed from 12.1 million to 18.6 million, accounting for approximately one-third of the total annual global deaths [ 1 ]. The severity of CVDs poses not only a global health challenge but also exerts immense pressure on the healthcare system and the economy [ 2 ]. According to the World Heart Federation, global medical costs for CVDs are projected to rise from approximately 863 billion US dollars in 2010 to 1044 billion US dollars by 2030 [ 3 ]. Thus, it is particularly important to deeply explore the mechanisms that influence CVDs and to develop effective and sustainable strategies to reduce risk and prevent these diseases.
The urban built environment refers to the comprehensive physical structure and man-made surroundings of an urban area, including buildings, transportation systems, infrastructure, land use planning, and elements of natural and artificial spaces [ 4 ]. Numerous studies have focused on the close connection between the built environment and human health, particularly with respect to cardiovascular health. Research indicates that the impact of the built environment on cardiovascular health is a process network structure with various influencing factors, including but not limited to factors contributing to CVDs such as obesity, diabetes, high blood pressure [ 5 , 6 , 7 , 8 , 9 , 10 ], environmental issues like traffic noise and air pollution [ 11 , 12 ], as well as aspects of physical exercise, psychological stress, and lifestyle [ 13 , 14 , 15 , 16 , 17 ], all of which collectively affect the pathogenesis of CVDs [ 18 , 19 , 20 ]. Studies show that optimizing urban design, such as rational land allocation and planning street layouts, can guide people to access more life services, cultivate proactive attitudes and healthy bodies, thereby reducing the risk of CVDs [ 21 , 22 ]. Urban spatially compact development models can encourage physical activity, reducing the risk of cardiovascular and metabolic issues [ 23 ]. In contrast, long commutes and high traffic density may lead to chronic stress and lack of exercise, increasing the risk of obesity and hypertension. Conversely, appropriate intersection density, land-use diversity, destination convenience, and accessibility might encourage walking, improve health, and reduce the risk of obesity, diabetes, hypertension, and dyslipidemia, which are cardiovascular-related problems [ 24 , 25 , 26 ]. The density and accessibility of supermarkets have a direct impact on the dietary habits of community residents, wherein excessive density may increase the risk of obesity and diabetes and correlate with blood pressure levels [ 27 ]. Urban green spaces and outdoor recreational areas have a positive effect on cardiovascular health; green spaces not only offer places for exercise and relaxation but also help alleviate stress, improve mental states, and enhance air quality, thus mitigating the harm caused by air pollution and protecting cardiac and vascular health [ 28 ]. Research also indicates that individuals residing in areas with high greenery rates are more likely to enjoy opportunities that promote physical activity, mental health, and healthy lifestyles, thereby minimizing CVD risks [ 29 , 30 ]. In summary, scientific and rational urban planning, such as diversified land use, appropriate building density, good street connectivity, convenient destinations, short-distance commuting, and beautiful environments, are key factors in promoting overall health and preventing CVDs.
Although numerous studies have focused on exploring the relationship between the built environment and CVDs, the specific mechanisms underlying this relationship remain unclear. This knowledge gap is mainly due to the complexity of the built environment itself and the multifactorial pathogenesis of CVDs. Current research mostly concentrates on individual aspects of the built environment, such as noise, air pollution, green spaces, and transportation [ 31 ], lacking consideration for the overall complexity of the built environment. Many elements of the built environment are interactive; for instance, pedestrian-friendly urban design may enhance physical activity and social interaction, yet it could also be counteracted by air and noise pollution caused by urban traffic [ 32 ]. Therefore, the same element of the built environment might have different effects in different contexts, adding complexity to the study of the built environment. Furthermore, while existing research has exhibited considerable depth and breadth in exploring the complex and dynamic relationship between the built environment and CVDs, many areas still require further improvement and deepening. Traditional linear correlation analyses, such as OLS and logistic regression models, have been widely used to assess the significance level between built environment characteristics and CVDs mortality rates, and to investigate factors such as intersection density, slope, greening, and commercial density [ 33 , 34 ]. However, these methods fall short in addressing the complexity and non-linear characteristics of spatial data.
Therefore, from a geographical perspective, it is particularly important to adopt more appropriate methods to capture the non-stationarity and heterogeneity of spatial data and to explore the spatial correlation characteristics between the built environment and CVDs. However, current research utilizing spatial models has mainly focused on macro-level perspectives, such as national or provincial levels. For example, ŞENER et al. employed spatial autocorrelation models and hot spot analysis models to assess the spatiotemporal variation characteristics of CVD mortality across multiple provincial administrative regions [ 35 ]. Baptista et al. analyzed the impact of factors such as per capita GDP, urbanization rate, education, and cigarette consumption on the growth trends of CVD incidence using spatial lag and spatial error models across different countries or regions [ 36 ]. Eun et al. used Bayesian spatial multilevel models to measure built environment variables in 546 administrative districts of Gyeonggi Province, South Korea, and evaluated the impact of the built environment on CVDs [ 37 ]. While these studies have, to some extent, revealed the spatial distribution characteristics of CVDs and their spatial relationships with environmental features, the scope of these studies is often large, and they tend to overlook the heterogeneity at the micro-level within cities and its specific impact on residents' health. As a result, it is challenging to accurately capture the differential effects of the built environment on CVD incidence across different areas within a city, and many critical environmental factors at the micro-geographical scale, which are directly related to the daily lives and health of residents, may be obscured.
Given this, we focus on Xixiangtang District in Nanning City, China, and construct a research framework centered on multi-source data, including the distribution of CVDs, road networks, and urban POI data. By employing KDE to reveal hotspot areas, spatial autocorrelation analysis to explore spatial dependence, the GDM to dissect key factors, and GWR to capture the spatial heterogeneity effects, we deeply analyze the complex mechanisms by which the urban built environment influences the incidence of CVDs. Our study aims to answer: Is there a significant spatial association between urban built environment elements and the incidence rate of CVDs? To what extent do different built environment elements impact CVDs? And, what are the regional differences in the impact of built environment elements on CVDs in different areas?
This study focuses on Xixiangtang District in Nanning City (Fig. 1 ), an important administrative district located in the northwest of Nanning City, covering an area of approximately 1,276 square kilometers with a permanent population of over one million. As an exemplary early-developed area of Nanning City, the built environment of Xixiangtang not only carries a rich historical and cultural heritage but also witnesses the transformation from a traditional old town to a modern emerging area, forming a unique urban–rural transitional zone. However, with the acceleration of urbanization, Xixiangtang District also faces numerous environmental challenges, such as declining air quality, congested traffic networks, increasing noise pollution, and continuously rising population density, all of which may pose potential threats to residents' cardiovascular health. Therefore, choosing the built environment of Xixiangtang as the core area of this study is not only due to its representativeness but also because the issues faced by this area are of profound practical significance for exploring the health impacts of urbanization and formulating effective environmental improvement strategies.

Location of study area
The CVD case data is sourced from the cardiovascular department's medical records at Guangxi National Hospital. Located in the southeastern core area of Xixiangtang District, near metro stations and densely populated areas, the hospital's superior geographical location and convenient transportation conditions greatly facilitate patient visits, especially for those seeking high-level cardiovascular medical services. Although spatial distance is an important consideration for patients when choosing a medical facility, our study on the spatial distribution patterns of CVDs also takes into account various influencing factors, including socioeconomic status, environmental factors, patient health conditions, and healthcare-seeking behaviors, ensuring the depth and accuracy of the results. Additionally, Guangxi National Hospital is one of the few top-tier (tertiary A) comprehensive hospitals in Xixiangtang District, with its cardiovascular department being a key specialty. The department's outstanding reputation and wide influence, combined with its advantages in equipment, technology, and healthcare costs compared to other non-specialized cardiovascular departments in the region, make it particularly attractive to patients in Xixiangtang, thus rendering the data relatively representative. To ensure the fairness of our study results, we have implemented multiple verification measures, including comprehensive data collection, independent evaluation of medical standards, rigorous statistical analysis, and consideration of healthcare costs.
With authorization from Guangxi National Hospital, we obtained and analyzed the cardiovascular department's data records. Our study adheres to ethical principles and does not involve any operations that have a substantial impact on patients. The cardiovascular data records include basic patient information (such as age, gender, address, etc.), diagnostic information (disease type, diagnosis date, etc.), and treatment records. We focused on CVD patients diagnosed between January 1, 2020, and December 31, 2022. Through systematic screening and organization, we constructed a database of CVD patients during this period. During the data processing procedure, we implemented a rigorous data cleaning process, identifying and excluding incomplete, duplicate, or abnormal data records. This included checking for missing data, logical errors (such as extremely large or small ages), and consistency in diagnostic codes, ensuring the quality and reliability of the data. After data cleaning, we selected 3,472 valid samples, which are representative in terms of disease types, patient characteristics, and geographic distribution. Considering the study involves geographic location analysis, we used a text-to-coordinate tool developed based on the Amap (Gaode) API to convert patient address information into precise geographic coordinates. Finally, using ArcGIS 10.8 software, we visualized the processed case data on a map.
As a multidimensional and comprehensive conceptual framework, the built environment encompasses a vast and intricate system of elements. Given the accessibility, completeness of data, and the robust foundation in current research domains, we have centered our in-depth analysis on two core components: the urban road system and urban POIs. Road data is primarily sourced from OpenStreetMap (OSM) and processed using ArcGIS 10.8 to filter and handle incomplete records. We ultimately selected five types of roads for analysis: highways, expressways, arterial roads, secondary roads, and local roads [ 38 ]. Urban POI data was selected based on existing research and obtained through Amap. Amap is a leading map service provider in China, known for its vast user data, precise geocoding system, and advanced intelligent analysis technology, which accurately captures and presents the spatial distribution and attribute characteristics of various urban facilities. We used Amap's API interface and offline map data package to obtain the coordinates and basic attributes of POIs in the study area, including six key environment elements: dining [ 39 ], parks [ 40 ], transportation [ 20 ], shopping [ 41 ], sports [ 42 ], and healthcare [ 43 ] (Table 1 ). These elements significantly reflect the distribution status of the urban built environment. This comprehensive and detailed data provides a solid foundation for further exploring the relationship between the built environment and cardiovascular health.
- Spatial analysis
Based on existing research findings, we have identified key built environment factors that influence the occurrence of cardiovascular diseases (CVDs) and meticulously processed the data sourced from [ 34 , 35 , 44 ]. The preprocessed data was then subjected to spatial analysis utilizing software tools such as ArcGIS 10.8, Geoda, and the Geographic Detector. Through various methods including KDE, spatial autocorrelation analysis (encompassing both univariate and bivariate analyses), factor detection and interaction detection using the Geographic Detector, as well as GWR, we aimed to explore the potential links between the urban built environment and CVDs (Fig. 2 ).

Research framework
Kernel Density Estimation (KDE)
Before delving into the complex relationship between the built environment and CVDs, it is crucial to accurately depict the spatial distribution of these key elements within the study area. Given this need, KDE, an advanced non-parametric statistical technique, was introduced as our core analytical tool. KDE is a non-parametric method used to estimate the probability density function of a random variable, and we implemented it using ArcGIS 10.8 software. Compared to other density estimation methods, such as simple counting or histograms, KDE more accurately reflects the true distribution of spatial elements, helping us identify hotspots and cold spots in the city with greater precision. The core of this method lies in assigning a smooth kernel function to each observation point, which describes the influence range of the observation point on its surrounding space, known as bandwidth. The density distribution map of the entire area is then obtained by overlaying the kernel functions of all observation point [ 45 , 46 , 47 ]. In parameter settings, we set the cell size to 100 m, based on a comprehensive consideration of the study area's scope, the distribution characteristics of geographic phenomena, and computational resource limitations. This aimed to maintain sufficient precision while avoiding excessive computational burden and amplification of data noise. To further refine the analysis and visually present the continuous spatial distribution of CVDs, we used the natural breaks method to classify the KDE results into five levels. KDE visually displays the continuous spatial distribution of CVDs, identifying high-risk and low-risk areas, and provides foundational data support for subsequent spatial analyses.
Spatial autocorrelation analysis
Spatial autocorrelation analysis is a statistical method used to assess the similarity or correlation between observed values in geographic space. We derived the point attribute values from the kernel density transformation and conducted univariate global spatial autocorrelation analysis, as well as bivariate global spatial autocorrelation analysis between built environment factors and CVDs using Geoda software. Univariate global spatial autocorrelation analysis was used to study the spatial distribution characteristics of the overall dataset, using Moran's I to evaluate whether the dataset exhibits spatial autocorrelation, indicating clustering or dispersion trends [ 48 , 49 ]. Bivariate global spatial autocorrelation further analyzed the spatial correlation between different indicators [ 50 , 51 ]. Spatial autocorrelation analysis helps verify whether the spatial clustering in KDE results is significant and preliminarily explores whether there is spatial interdependence between environmental factors and CVDs.
The results of spatial autocorrelation analysis include the Moran's I index, which directly reflects the strength and direction of spatial autocorrelation, as well as key indicators such as p values and Z values, together constructing a comprehensive quantitative system for evaluating spatial autocorrelation. In the results of spatial autocorrelation analysis, when the p -value is less than 0.01, the confidence level reaches 99%, and the Z value is greater than 2.58, the null hypothesis can be rejected, indicating that the research results are highly reliable. The degree of spatial clustering of variables is measured by Moran's I. The range of Moran's I is [-1, 1]; if Moran's I > 0, it indicates positive correlation, with higher values indicating stronger clustering; if Moran's I < 0, it indicates negative correlation, with lower values indicating stronger clustering; and if Moran's I = 0, the variables are not clustered and show a dispersed distribution, with the correlation weakening as the value approaches 0 [ 52 ].
The GeoDetector method (GDM)
We analyzed the processed kernel density attribute data using the GDM to parse the influence of the built environment on CVDs and uncover the underlying driving factors. The geographic detector tool was developed by a team led by Researcher Jinfeng Wang at the Institute of Geographic Sciences and Natural Resources Research, Chinese Academy of Sciences [ 53 ]. The GDM mainly includes factor detection, interaction detection, risk area detection, and ecological detection, and it has been widely applied in multiple fields. We used the factor detection function to evaluate the impact of environmental factors on the distribution of CVDs and utilized the interaction detection function to analyze the interaction between different environmental factors [ 54 , 55 ]. The purpose of the factor detector is to detect the extent to which independent variables explain the spatial differentiation of the dependent variable. It quantifies the influence of independent variables on the spatial distribution of the dependent variable to reveal which factors are the main contributors to the spatial distribution differences of the dependent variable. However, the impact of built environment elements on CVDs may not be determined by a single factor but rather by the synergistic effect of multiple built environment factors. Therefore, through the means of interaction detection, we further analyzed the synergistic impact of pairs of built environment elements on the spatial distribution of CVDs.
In this analysis, the q value was used as a quantitative indicator of the influence of environmental factors on CVDs, with values ranging between [0,1]. A higher q value indicates a more significant influence of the environmental factor, whereas a lower q value indicates a smaller influence. Additionally, a significance level of p < 0.01 further emphasizes the reliability of these factors' significant impact on the distribution of CVD samples.
Geographically Weighted Regression (GWR)
However, while the GDM can reveal the overall impact of built environment elements on CVDs, its limitation lies in its difficulty to finely characterize the specific differences and dynamic changes of these impacts within different geographic spatial units. To address this shortcoming, we introduced the GWR model through the spatial analysis tools of ArcGIS 10.8 software for local analysis. This model dynamically maps the distribution and variation trajectory of regression coefficients in geographic space, incorporating the key variable of spatial location into the regression analysis. In this way, the GWR model can reveal the spatial heterogeneity of parameters at different geographic locations, accurately capturing the relationships between local variables, thus overcoming the limitations of traditional global regression models in handling spatial non-stationarity [ 56 , 57 ]. Compared to traditional global regression models, the GWR model excels in reducing model residuals and improving fitting accuracy.
When interpreting the results of the GWR model, it is necessary to consider the regression coefficients, R 2 (coefficient of determination), and adjusted R 2 comprehensively. The dynamic changes in regression coefficients in space reveal the complex relationships between independent and dependent variables at different geographic locations, with their sign and magnitude directly reflecting the nature and intensity of the impact. Although the R 2 value, as an indicator of the model's goodness of fit, focuses more on local effects in the GWR, its variation still helps to assess the explanatory power of the model in each area. These comprehensive indicators together form a thorough evaluation of the GWR model's performance. Through a comprehensive evaluation of the GWR model results, we can more precisely capture the relationships between local variables, revealing the specific impact of environmental factors on CVD risk within different regions.
Kernel density distribution characteristics
By applying kernel density analysis, the spatial distribution pattern of CVD samples and various built environment elements was detailed, effectively capturing their spatial density characteristics. The obtained kernel density levels were divided into five tiers using the natural breaks method and arranged in descending order, as shown in Fig. 3 . Analysis results indicate that high-density areas of elements such as shopping, dining, transportation facilities, and medical care are mainly focused in the southeastern part of the city, i.e., the city center. The high-density areas of the road network extend along the southern Yonjiang belt and appear patchy in the city center. Dense areas of parks are mostly near the southern riverside areas, while high-density distributions of sports facilities extend in the southeastern and central regions. Overall, the distribution pattern of these environmental factors reveals that Xixiangtang District's development trend mainly extends from southeast to northwest, indicating that the northeastern part of the region is relatively underdeveloped, with a sparse population and a lack of various infrastructure layouts. Additionally, kernel density distribution characteristics show that high-incidence areas of CVDs are concentrated in the southeast, highly coinciding with the high-density areas of most built environment elements.
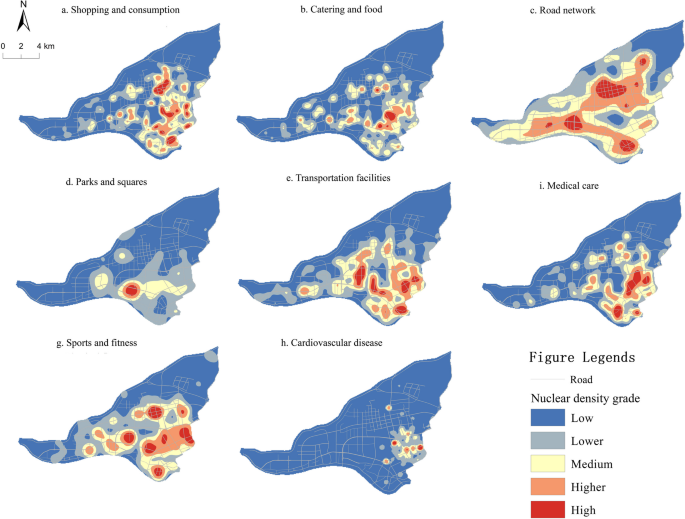
Distribution of nuclear density of each element in the study area
Spatial Autocorrelation Characteristics
To explore the spatial relationship between urban built environment elements and the distribution of CVDs, spatial autocorrelation analysis was performed using Geoda software [ 58 ]. The study involved univariate and bivariate global spatial autocorrelation analyses (Table 2 ). The results of the analysis passed the significance level test at 0.01, with p values below 0.01 and Z values exceeding 2.58, achieving a 99% confidence level. This reinforces the reliability of the spatial autocorrelation results.
Univariate analysis is used to evaluate the clustering or dispersion status of feature points in space. In univariate analysis, the Moran's I value of the road network was 0.957, which significantly indicates a clustering trend in its spatial distribution. Moran's I values for other built environment elements, such as parks, transportation facilities, sports and fitness, and medical care, all exceeded 0.9, while the Moran's I values for shopping and dining also surpassed 0.8. By comparison, the Moran's I value for CVD samples was 0.697, approaching 0.7, revealing significant aggregation. Overall, the clustering nature of the built environment elements and CVD samples in Xixiangtang District implies that these elements are not randomly deployed but follow some patterns of hierarchical assembly.
Bivariate analysis, on the other hand, is used to evaluate the spatial correlation between different environmental factors and CVDs. Bivariate analysis further revealed the spatial interaction between environmental factors and CVDs. The results show that all considered environmental elements exhibited significant positive correlation with CVDs. The spatial association between medical care elements and CVDs was the strongest, with a Moran's I value of 0.431, surpassing the significant threshold of 0.4. Additionally, the Moran's I values for dining, transportation facilities, shopping, and sports and fitness were all over 0.3. Road networks and parks, on the other hand, showed relatively weaker correlations with CVDs, with Moran's I values around 0.1, indicating that in that region, the spatial connection between these built environment elements and CVDs is comparably weak.
Geodetector results analysis
A detailed analysis of the impact of various environmental factors on CVDs was achieved through the factor detection model of the GDM. According to the factor detection results shown in Table 3 , significant differences in the impact of environmental factors on the distribution of CVD samples were observed. The analysis results indicate that the environmental factors influencing the distribution of CVDs, in descending order of impact, are: healthcare services > shopping > dining > transportation facilities > sports and fitness > parks and squares > road networks. Specifically, healthcare services lead with a q value of 0.532, indicating that the spatial distribution of healthcare services has the most significant impact on the spatial distribution of CVDs. This highlights the importance of a high-density layout of healthcare facilities in the prevention and treatment of CVDs and suggests that individuals at risk for CVDs tend to prefer living in areas with convenient access to medical services [ 59 ].
Subsequently, shopping, dining, and transportation facilities all have q values exceeding 0.4, reflecting their significant effects on the urban built environment's clustering characteristics and regional commercial vitality. The concentration of human traffic brought about by these factors may, while increasing residents' lifestyle choices, also lead to certain psychological burdens and declining air quality, thereby indirectly placing a burden on the cardiovascular system. In contrast, parks and squares and road networks have relatively low q values (both less than 0.2), suggesting that the incidence of CVDs is lower in areas concentrated with these environmental elements, likely related to their ecological and transportation benefits.
Subsequently, interaction detection was used to analyze the synergistic impact of pairs of built environment elements on the spatial distribution of CVDs. From the results shown in Table 4 , it is evident that any two built environment elements exhibit a bi-factor enhancement effect on CVDs, suggesting that the combined influence of two built environment elements exceeds the effect of a single element. Among these, the interaction between healthcare services and shopping has the greatest impact on CVDs, with a value of 0.571. This indicates that CVDs patients or high-risk individuals tend to prefer living in areas rich in healthcare resources and convenient for shopping, as they can more easily access health services and daily necessities. Conversely, the interaction between road networks and parks and squares has the weakest impact on CVDs, with a value of 0.313. This suggests that their combined effect in reducing CVD risk is relatively limited, possibly due to the negative impacts of road networks, such as traffic congestion and air pollution, which may offset some of the health benefits provided by parks and squares. This result further validates an important point: the impact of the built environment on CVDs is not driven by a single element but by the synergistic effects of multiple environmental factors working together.
Geographically weighted regression analysis
The GDM revealed the influence of built environment factors on CVDs. To further uncover the spatial heterogeneity effects of built environment elements on CVDs in different regions, we employed the GWR model. To ensure the rigor of the analysis, we conducted multicollinearity detection for all built environment elements before establishing the model. We confirmed that the Variance Inflation Factor (VIF) values for all elements did not exceed the conventional threshold of 5, effectively avoiding multicollinearity issues and ensuring the robustness of the model results. The GWR model results showed that the model's coefficient of determination R 2 was 0.596, and the adjusted R 2 was 0.575, indicating that the model could adequately explain the relationships between variables in the study. The analysis results also highlighted the spatial non-stationarity of the effects of built environment elements, manifested by different degrees of variation and fluctuation characteristics, as shown by the coefficient magnitudes and their dynamic changes in spatial distribution in Table 5 .
Looking more closely at the details, as demonstrated in Fig. 4 , the regression coefficients of the dining elements fluctuated relatively little, ranging from -0.372 to 0.471, reflecting a relatively balanced spatial effect. Moreover, although this factor's impact in the Xixiangtang District showed both positive and negative aspects in different areas, more than half of the analysis units indicated positive values, especially in the southern and northeastern parts of the Xixiangtang District. In contrast, the high-incidence areas of CVDs in the eastern part and areas in the north showed negative correlations.

Spatial distribution of regression coefficient of built-up environmental factors
The GWR coefficients and their fluctuations for parks were significant, ranging from -69.757 to 35.43, indicating significant spatial differences in their impact on the distribution of CVDs. Specifically, the spatial distribution of positive and negative impacts was nearly 1:1, revealing the complexity of its effects. In high-incidence areas of CVDs, the distribution of parks showed a significantly negative correlation with disease distribution, while a significant increase in positive correlation was observed north of the significantly negative regions. This implies the presence of other moderating factors influencing the direction of the impact of parks on CVDs.
The regression coefficients and fluctuations for shopping were the smallest among the seven environmental factors, confined to a range of -0.093 to 0.219, suggesting a high consistency in its spatial effects. In the Xixiangtang built-up area, nearly two-thirds of the spatial units yielded positive impacts. Particularly in the northern, northeastern, southern, and southeastern regions, the positive impacts of shopping were especially pronounced.
The regression coefficients and fluctuations for transportation facilities were relatively large, ranging from -0.487 to 7.363. For the Xixiangtang District, nearly three-quarters of the analysis units displayed positive spatial impacts, with the largest positive value areas concentrated in the southeastern part. However, areas with negative impacts from transportation facilities were relatively fewer, suggesting a clear positive correlation with the distribution of CVDs.
The fluctuation range for sports and fitness regression coefficients was also broad, from -10.578 to 33.256. The analysis indicated that only a quarter of the analysis units in the Xixiangtang District had a positive correlation. The most significant positive values were located near the high-density areas for CVDs, suggesting that sports and fitness facilities might have a positive correlation with the disease distribution in these areas. Meanwhile, the intensity of the negative correlation increased north of the areas with significant positive values, potentially pointing to other factors' potential moderating effects on the relationship between sports and CVDs.
The regression coefficients and their fluctuations for healthcare were relatively small, ranging from -1.235 to 3.352. In the Xixiangtang District, the vast majority of analysis units showed a positive correlation, especially in the northern regions. The southern areas exhibited negative correlations, highlighting potential differences in medical resources in that region.
Of all the built environment elements, road networks had the largest range of regression coefficients and fluctuations, swinging from -7905.743 to 411.617, demonstrating extremely strong spatial variability. Only a small portion of the spatial units in the Xixiangtang District showed positive correlations, while the significantly negative regions were mostly concentrated in high-incidence areas for CVDs. This phenomenon was similar to the negative correlation distribution trend of parks, pointing to a significantly negative correlation between park distribution and the distribution of CVDs. Notably, the effect of road networks was opposite to transportation facilities, which could be related to the connectivity of the road network and traffic congestion conditions, factors that could influence the incidence of CVDs.
This study reveals a high-density aggregation of CVDs and various built environment elements in the southeastern part of the study area, i.e., the urban central area. Through spatial statistical analysis, all examined environmental elements and CVDs showed high Moran's I values, indicating significant clustering in their spatial distribution. Furthermore, the positive spatial correlation between these environmental elements and CVDs corroborates the deep connection between the urban built environment and the incidence of CVDs.
Geodetector analysis reveals significant differences in the impact of different built environment elements on CVDs. Healthcare facilities had the most influence, followed by shopping, dining, and transportation facilities, while parks and road networks had relatively weaker impacts. Notably, the occurrence of CVDs is not only related to individual built environment elements but likely results from the combined effects of multiple elements. Further interaction detection analysis confirmed this hypothesis, finding that the joint impact of any two environmental elements was stronger than any individual element, showing a clear dual-factor enhancement effect. Specifically, the interaction between healthcare and shopping had the most significant impact on the distribution of CVDs, while the combined effect of road networks and parks was the least. By delving into individual factors and their interaction effects, this study reveals a comprehensive view of the impact of the built environment on CVDs, highlighting the complex relationships and differences between environmental elements and the occurrence of diseases.
The GWR model was used to analyze in detail how built environment elements affect CVDs in different regions, aiming to gain a deep understanding of the local effects of the built environment. The research results showed the regression coefficients of built environment elements and their range of variation. Specifically, the regression coefficients for dining exhibited relatively stable trends in spatial distribution. Although the overall impact was moderate, slight fluctuations revealed a slightly enhanced positive correlation in specific areas such as densely commercial or culturally vibrant dining regions. Particularly in the southern and northeastern parts, the combination of diverse dining options and frequent dining consumption patterns showed a slight positive correlation with CVD risk. This reflects the complex impact of dietary habits, food composition, and intake levels on cardiovascular health [ 60 , 61 ].
The regression coefficients for parks and squares showed relatively large fluctuations in spatial distribution, indicating significant regional heterogeneity. This is mainly due to factors such as differences in regional population density and per capita park and square area. In our study, the southeastern region, which is a high-incidence area for CVDs, exhibited negative regression coefficients for parks and squares. This is because this region is the central urban area with a high population density, leading to a significant shortage of per capita green space, thus showing a negative correlation. Conversely, in the northern region, where population distribution is more balanced and parks and squares are more abundant, the per capita green space is relatively sufficient. Therefore, CVD patients have more access to green spaces and exercise areas, showing a positive correlation [ 29 ].
The regression coefficients for shopping consumption showed the smallest fluctuations in spatial distribution. The positive and negative effects were not significantly different, with the positive effects being notably concentrated in the northern, northeastern, and southern commercial thriving areas. Compared to other regions, these areas might have relatively well-developed commercial facilities or superior shopping environments. This could indirectly affect CVD risk through various dimensions, such as physical exertion from walking or cycling during shopping and the regulation of psychological states like satisfaction and pleasure after shopping [ 44 ].
The regression coefficients for transportation facilities showed a significant positive correlation in high-incidence areas of CVDs, with notable fluctuations. This deeply reveals the direct and important impact of traffic conditions, especially congestion and pollution, on cardiovascular health across different regions. In traffic-dense areas such as city centers and transportation hubs, high traffic volume, severe congestion, and increased noise and air pollution collectively pose major threats to residents' cardiovascular health. This not only directly harms the cardiovascular system through accumulated psychological stress and exposure to air pollution but also further exacerbates the risk due to a lack of exercise opportunities [ 62 ].
The regression coefficients for sports and fitness facilities exhibited a high degree of heterogeneity in spatial distribution, showing a significant positive correlation in the southeastern high-incidence area for CVDs, which gradually shifts to a negative correlation towards the outer regions. This deeply reflects the regional differences in the allocation of sports and fitness facilities, residents' exercise habits, and participation rates. In areas with well-developed urban facilities and strong resident awareness of physical activity, the positive effects of sports and fitness activities on cardiovascular health are particularly significant. These activities effectively reduce CVD risk by enhancing physical activity, optimizing cardiopulmonary function, and lowering body fat percentage. However, in areas with relatively scarce sports facilities and poor exercise habits among residents, negative impacts may be observed, highlighting the potential threats to public health due to uneven distribution of sports resources and a lack of exercise culture [ 63 ].
The regression coefficients for healthcare services showed regional differences in spatial distribution. In the northern region, due to the lower population density, the abundance and superior quality of per capita healthcare resources have a significant positive effect on residents' cardiovascular health. In contrast, the southern region, with relatively scarce resources or limited service quality, fails to fully realize the potential benefits of healthcare services. This disparity not only reveals the current uneven distribution of healthcare resources but also emphasizes the importance of enhancing the equalization of healthcare services [ 64 ]. The positive impact of healthcare on CVDs is primarily achieved through efficient prevention, precise diagnosis, and timely treatment. Its effectiveness is influenced by multiple factors, including the sufficiency of medical resources, service quality, residents' healthcare-seeking behavior, medical policies, and technological advancements.
The road network and transportation facilities together constitute the urban transportation system. In the process of transportation planning, we advocate for the continuous optimization of the road network layout, reserving space for future traffic growth, and utilizing intelligent technology to optimize traffic signal management to alleviate congestion. Meanwhile, in the densely populated eastern and southeastern areas, we emphasize enhancing the convenience of public transportation by adding routes and optimizing station locations, making it the preferred mode of travel for residents. Additionally, measures such as the construction of sound barriers and green belts are implemented to effectively reduce noise and air pollution caused by public transportation. Furthermore, we actively promote green travel methods such as cycling and walking by building a comprehensive network of bike lanes and pedestrian paths, thereby promoting public health and environmental protection [ 20 ].
These findings provide a more comprehensive understanding of the complex interactions between built environment elements and CVDs. Therefore, it is essential to balance the integrated impact of these factors in urban planning and public health interventions. Based on a comprehensive analysis of existing research and our study's results, we propose the following viewpoints.
Firstly, healthcare is the primary factor influencing the distribution of CVDs. Living near medical institutions offers substantial benefits to cardiovascular patients, not only enhancing the accessibility of medical services but also helping to quickly respond to emergency medical situations, providing a sense of security for patients. We suggest establishing additional medical centers in the densely populated southeastern region to ensure that community members can easily access high-quality medical services [ 65 ].
Secondly, shopping and dining are the next most important factors affecting the spatial distribution of CVDs. Although the spatial variation of these factors is not significant, their long-term cumulative impact should not be overlooked. We recommend that future urban renewal or renovation efforts reasonably control and plan the density of commercial areas, especially in the eastern region. This requires ensuring that residents can enjoy convenient shopping services to meet their daily needs while avoiding the increased living costs and stress caused by excessive commercial concentration. Additionally, it is necessary to strengthen the management of dining environments, including encouraging dining establishments to offer more healthy food options, such as low-sugar, low-fat, and high-fiber dishes. It is also important to increase the availability of healthy dining options by establishing healthy restaurants and vegetarian eateries, while reasonably controlling and optimizing the layout and number of high-sugar and high-fat food outlets within communities to reduce health risks induced by frequent exposure to such foods [ 66 ].
Road networks and transportation facilities together form the city's transportation system. In transportation planning, we advocate for the continuous optimization of road network layouts, reserving space for future traffic growth, and leveraging intelligent technology to optimize traffic signal management to alleviate congestion. Additionally, enhancing the convenience of public transportation by adding routes and optimizing stops can make it the preferred mode of travel for residents. Complementing this with the construction of sound barriers and green belts can effectively reduce noise and air pollution caused by public transportation. Furthermore, promoting green travel methods such as cycling and walking by building a comprehensive network of cycling lanes and walking paths can foster both health and environmental benefits [ 20 ].
Sports and fitness facilities, along with parks and squares, are essential for improving residents' quality of life and promoting healthy lifestyles. During planning, sports and fitness facilities should be reasonably distributed, especially in the northern part of the study area, to ensure that all communities have convenient access to exercise amenities. Diverse fitness facilities catering to different age groups and exercise needs, such as basketball courts, soccer fields, and fitness equipment zones, should be provided to meet the varied exercise requirements of different groups. Additionally, parks and squares, as crucial spaces for residents' leisure and entertainment, should be planned with a harmonious balance of ecology and landscape. In densely populated and space-constrained southeastern areas, small green spaces, leisure seating, and children's play facilities can be added to provide residents with a pleasant environment for relaxation and nature interaction [ 67 ].
We have explored the mechanisms by which environmental elements impact CVDs and proposed suggestions for optimizing the urban built environment, but this paper still has certain limitations. The impact of the environment on health and disease is complex, and due to time and resource constraints, it was not possible to consider and analyze all potential variables comprehensively, which may have some impact on the research results. To further deepen the study of the relationship between the built environment and cardiovascular health, future research could consider the following aspects: first, expand the scope of research, collecting and analyzing data from different cities and regions to better understand geographical differences in the impact of the built environment on cardiovascular health; second, enhance the scientific nature of the research methods, using more objective and precise methods for data collection and analysis to improve the reliability and accuracy of the research; and finally, deepen the study of the mechanisms between the built environment and cardiovascular health, exploring biological and psychological mechanisms to better understand their relationship.
Focusing on the built-up area of Xixiangtang in Nanning City as the research area, this study delves into the intrinsic connection between the urban built environment and CVDs, uncovering several findings. Utilizing hospital cardiovascular data and urban POI data, and employing spatial analysis techniques such as KDE, spatial autocorrelation analysis, geodetectors, and GWR, we systematically assessed the extent and mechanisms through which various built environment elements impact CVDs. The results show a significant positive correlation between the urban built environment and CVDs. Particularly, healthcare facilities, shopping venues, restaurants, and transportation facilities have significant effects on the incidence and distribution of CVDs. The spatial aggregation of these elements and the dense distribution of CVDs demonstrate significant consistency, further confirming the close link between the built environment and CVDs. Simultaneously, we discovered spatial heterogeneity in the impact of different built environment elements on CVDs. This indicates that in planning and improving the urban environment, elements and areas with a greater impact on CVDs should be considered specifically.
Availability of data and materials
The datasets used or analyzed during the current study are available from the corresponding author upon reasonable request.
Abbreviations
Cardiovascular Disease
Geographically weighted regression
Multiscale geographically weighted regression
The GeoDetector method
OpenStreetMap
Kernel Density Estimation
Points of Interest
Variance Inflation Factor
Application Programming Interface
Roth GA, Mensah GA, Fuster V. The global burden of cardiovascular diseases and risks: a compass for global action. American College of Cardiology Foundation Washington DC; 2020. p. 2980–1.
Masaebi F, Salehi M, Kazemi M, Vahabi N, Azizmohammad Looha M, Zayeri F. Trend analysis of disability adjusted life years due to cardiovascular diseases: results from the global burden of disease study 2019. BMC Public Health. 2021;21:1–13.
Article Google Scholar
Murray CJ, Aravkin AY, Zheng P, Abbafati C, Abbas KM, Abbasi-Kangevari M, et al. Global burden of 87 risk factors in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. The lancet. 2020;396(10258):1223–49.
Bloom DE, Cafiero E, Jané-Llopis E, Abrahams-Gessel S, Bloom LR, Fathima S, et al. The global economic burden of noncommunicable diseases. Program on the Global Demography of Aging; 2012.
Xu J, Jing Y, Xu X, Zhang X, Liu Y, He H, et al. Spatial scale analysis for the relationships between the built environment and cardiovascular disease based on multi-source data. Health Place. 2023;83:103048.
Article PubMed Google Scholar
Sarkar C, Webster C, Gallacher J. Are exposures to ready-to-eat food environments associated with type 2 diabetes? A cross-sectional study of 347 551 UK Biobank adult participants. Lancet Planetary Health. 2018;2(10):e438–50.
Grazuleviciene R, Andrusaityte S, Gražulevičius T, Dėdelė A. Neighborhood social and built environment and disparities in the risk of hypertension: A cross-sectional study. Int J Environ Res Public Health. 2020;17(20):7696.
Article PubMed PubMed Central Google Scholar
Ghosh-Dastidar B, Cohen D, Hunter G, Zenk SN, Huang C, Beckman R, et al. Distance to store, food prices, and obesity in urban food deserts. Am J Prev Med. 2014;47(5):587–95.
Braun LM, Rodríguez DA, Evenson KR, Hirsch JA, Moore KA, Roux AVD. Walkability and cardiometabolic risk factors: cross-sectional and longitudinal associations from the multi-ethnic study of atherosclerosis. Health Place. 2016;39:9–17.
Anza-Ramirez C, Lazo M, Zafra-Tanaka JH, Avila-Palencia I, Bilal U, Hernández-Vásquez A, et al. The urban built environment and adult BMI, obesity, and diabetes in Latin American cities. Nat Commun. 2022;13(1):7977.
Article PubMed PubMed Central CAS Google Scholar
Hartig T, Evans GW, Jamner LD, Davis DS, Gärling T. Tracking restoration in natural and urban field settings. J Environ Psychol. 2003;23(2):109–23.
Levy L. Dietary strategies, policy and cardiovascular disease risk reduction in England. Proceedings of the Nutrition Society. 2013;72(4):386–9.
Article PubMed CAS Google Scholar
Dalal HM, Zawada A, Jolly K, Moxham T, Taylor RS. Home based versus centre based cardiac rehabilitation: Cochrane systematic review and meta-analysis. BMJ. 2010;340.
Humpel N, Owen N, Leslie E. Environmental factors associated with adults’ participation in physical activity: a review. Am J Prev Med. 2002;22(3):188–99.
Jia X, Yu Y, Xia W, Masri S, Sami M, Hu Z, et al. Cardiovascular diseases in middle aged and older adults in China: the joint effects and mediation of different types of physical exercise and neighborhood greenness and walkability. Environ Res. 2018;167:175–83.
Murtagh EM, Nichols L, Mohammed MA, Holder R, Nevill AM, Murphy MH. The effect of walking on risk factors for cardiovascular disease: an updated systematic review and meta-analysis of randomised control trials. Prev Med. 2015;72:34–43.
Newby DE, Mannucci PM, Tell GS, Baccarelli AA, Brook RD, Donaldson K, et al. Expert position paper on air pollution and cardiovascular disease. Eur Heart J. 2015;36(2):83–93.
Chum A, O’Campo P. Cross-sectional associations between residential environmental exposures and cardiovascular diseases. BMC Public Health. 2015;15:1–12.
Diener A, Mudu P. How can vegetation protect us from air pollution? A critical review on green spaces’ mitigation abilities for air-borne particles from a public health perspective-with implications for urban planning. Sci Total Environ. 2021;796:148605.
Nieuwenhuijsen MJ. Influence of urban and transport planning and the city environment on cardiovascular disease. Nat Rev Cardiol. 2018;15(7):432–8.
Chandrabose M, den Braver NR, Owen N, Sugiyama T, Hadgraft N. Built environments and cardiovascular health: review and implications. J Cardiopulm Rehabil Prev. 2022;42(6):416–22.
Lee E, Choi J, Lee S, Choi B. P70 Association between built environment and cardiovascular diseases. BMJ Publishing Group Ltd; 2019.
Sallis JF, Floyd MF, Rodríguez DA, Saelens BE. Role of built environments in physical activity, obesity, and cardiovascular disease. Circulation. 2012;125(5):729–37.
Chandrabose M, Rachele JN, Gunn L, Kavanagh A, Owen N, Turrell G, et al. Built environment and cardio-metabolic health: systematic review and meta-analysis of longitudinal studies. Obes Rev. 2019;20(1):41–54.
Ewing R, Cervero R. “Does compact development make people drive less?” The answer is yes. J Am Plann Assoc. 2017;83(1):19–25.
Loo CJ, Greiver M, Aliarzadeh B, Lewis D. Association between neighbourhood walkability and metabolic risk factors influenced by physical activity: a cross-sectional study of adults in Toronto, Canada. BMJ Open. 2017;7(4):e013889.
Dendup T, Feng X, Clingan S, Astell-Burt T. Environmental risk factors for developing type 2 diabetes mellitus: a systematic review. Int J Environ Res Public Health. 2018;15(1):78.
Malambo P, Kengne AP, De Villiers A, Lambert EV, Puoane T. Built environment, selected risk factors and major cardiovascular disease outcomes: a systematic review. PLoS ONE. 2016;11(11):e0166846.
Seo S, Choi S, Kim K, Kim SM, Park SM. Association between urban green space and the risk of cardiovascular disease: A longitudinal study in seven Korean metropolitan areas. Environ Int. 2019;125:51–7.
Yeager RA, Smith TR, Bhatnagar A. Green environments and cardiovascular health. Trends Cardiovasc Med. 2020;30(4):241–6.
Liu M, Meijer P, Lam TM, Timmermans EJ, Grobbee DE, Beulens JW, et al. The built environment and cardiovascular disease: an umbrella review and meta-meta-analysis. Eur J Prev Cardiol. 2023;30(16):1801–27.
Koohsari MJ, McCormack GR, Nakaya T, Oka K. Neighbourhood built environment and cardiovascular disease: knowledge and future directions. Nat Rev Cardiol. 2020;17(5):261–3.
Howell NA, Tu JV, Moineddin R, Chen H, Chu A, Hystad P, et al. Interaction between neighborhood walkability and traffic-related air pollution on hypertension and diabetes: the CANHEART cohort. Environ Int. 2019;132:104799.
Patino JE, Hong A, Duque JC, Rahimi K, Zapata S, Lopera VM. Built environment and mortality risk from cardiovascular disease and diabetes in Medellín, Colombia: An ecological study. Landsc Urban Plan. 2021;213:104126.
Şener R, Türk T. Spatiotemporal analysis of cardiovascular disease mortality with geographical information systems. Appl Spat Anal Policy. 2021;14(4):929–45.
Baptista EA, Queiroz BL. Spatial analysis of cardiovascular mortality and associated factors around the world. BMC Public Health. 2022;22(1):1556.
Lee EY, Choi J, Lee S, Choi BY. Objectively measured built environments and cardiovascular diseases in middle-aged and older Korean adults. Int J Environ Res Public Health. 2021;18(4):1861.
Pourabdollah A, Morley J, Feldman S, Jackson M. Towards an authoritative OpenStreetMap: conflating OSM and OS OpenData national maps’ road network. ISPRS Int J Geo Inf. 2013;2(3):704–28.
Mazidi M, Speakman JR. Association of Fast-Food and Full-Service Restaurant Densities With Mortality From Cardiovascular Disease and Stroke, and the Prevalence of Diabetes Mellitus. J Am Heart Assoc. 2018;7(11):e007651.
Grazuleviciene R, Vencloviene J, Kubilius R, Grizas V, Dedele A, Grazulevicius T, et al. The effect of park and urban environments on coronary artery disease patients: a randomized trial. BioMed Res Int. 2015;2015.
Haralson MK, Sargent RG, Schluchter M. The relationship between knowledge of cardiovascular dietary risk and food shopping behaviors. Am J Prev Med. 1990;6(6):318–22.
Hoevenaar-Blom MP, Wendel-Vos GW, Spijkerman AM, Kromhout D, Verschuren WM. Cycling and sports, but not walking, are associated with 10-year cardiovascular disease incidence: the MORGEN Study. Eur J Prev Cardiol. 2011;18(1):41–7.
Sepehrvand N, Alemayehu W, Kaul P, Pelletier R, Bello AK, Welsh RC, et al. Ambulance use, distance and outcomes in patients with suspected cardiovascular disease: a registry-based geographic information system study. Eur Heart J. 2020;9(1_suppl):45–58.
Google Scholar
Malambo P, De Villiers A, Lambert EV, Puoane T, Kengne AP. The relationship between objectively-measured attributes of the built environment and selected cardiovascular risk factors in a South African urban setting. BMC Public Health. 2018;18:1–9.
Chen W, Liu L, Liang Y. Retail center recognition and spatial aggregating feature analysis of retail formats in Guangzhou based on POI data. Geogr Res. 2016;35(4):703–16.
Feng L, Lei G, Nie Y. Exploring the eco-efficiency of cultivated land utilization and its influencing factors in black soil region of Northeast China under the goal of reducing non-point pollution and net carbon emission. Environmental Earth Sciences. 2023;82(4):94.
Article CAS Google Scholar
Guan Z, Wang T, Zhi X. Temporal-spatial pattern differentiation of traditional villages in central plains economic region. Econ Geogr. 2017;37(9):225–32.
Chen Y. Development and method improvement of spatial autocorrelation theory based on Moran statistics. Geogr Res. 2009;28(6):1449–63.
Pang R, Teng F, Wei Y. A gwr-based study on dynamic mechanism of population urbanization in JIlin province. Sci Geogr Sin. 2014;34:1210–7.
Anselin L, Rey SJ. Modern spatial econometrics in practice: A guide to GeoDa, GeoDaSpace and PySAL. (No Title). 2014.
Zhang Z, Shan B, Lin Q, Chen Y, Yu X. Influence of the spatial distribution pattern of buildings on the distribution of PM2. 5 concentration. Stochastic Environmental Research and Risk Assessment. 2022:1–13.
Dehnad K. Density estimation for statistics and data analysis. Taylor & Francis; 1987.
Wang JF, Li XH, Christakos G, Liao YL, Zhang T, Gu X, et al. Geographical detectors-based health risk assessment and its application in the neural tube defects study of the Heshun Region, China. Int J Geogr Inf Sci. 2010;24(1):107–27.
Shu T, Ren Y, Shen L, Qian Y. Study on spatial heterogeneity of consumption vibrancy and its driving factors in large city: a case of Chengdu City. Urban Development Studies. 2020;27(1):16–21.
Jinfeng W, Chengdong X. Geodetector: Principle and prospective. Acta Geogr Sin. 2017;72(1):116–34.
Feuillet T, Commenges H, Menai M, Salze P, Perchoux C, Reuillon R, et al. A massive geographically weighted regression model of walking-environment relationships. J Transp Geogr. 2018;68:118–29.
Yu H, Gong H, Chen B, Liu K, Gao M. Analysis of the influence of groundwater on land subsidence in Beijing based on the geographical weighted regression (GWR) model. Sci Total Environ. 2020;738:139405.
Anselin L. An introduction to spatial autocorrelation analysis with GeoDa. Spatial Analysis Laboratory: University of Illinois, Champagne-Urbana, Illinois; 2003.
Nicholl J, West J, Goodacre S, Turner J. The relationship between distance to hospital and patient mortality in emergencies: an observational study. Emerg Med J. 2007;24(9):665–8.
Osman AA, Abumanga ZM. The relationship between physical activity status and dietary habits with the risk of cardiovascular diseases. E Journal of Cardiovascular Medicine. 2019;7(2):72.
Shan Z, Li Y, Baden MY, Bhupathiraju SN, Wang DD, Sun Q, et al. Association between healthy eating patterns and risk of cardiovascular disease. JAMA Intern Med. 2020;180(8):1090–100.
Münzel T, Treede H, Hahad O, Daiber A. Too loud to handle? Transportation noise and cardiovascular disease. Can J Cardiol. 2023;39(9):1204–18.
Halonen JI, Stenholm S, Kivimäki M, Pentti J, Subramanian S, Kawachi I, et al. Is change in availability of sports facilities associated with change in physical activity? A prospective cohort study Prev Med. 2015;73:10–4.
PubMed Google Scholar
Wekesah FM, Kyobutungi C, Grobbee DE, Klipstein-Grobusch K. Understanding of and perceptions towards cardiovascular diseases and their risk factors: a qualitative study among residents of urban informal settings in Nairobi. BMJ Open. 2019;9(6):e026852.
Berlin C, Panczak R, Hasler R, Zwahlen M. Do acute myocardial infarction and stroke mortality vary by distance to hospitals in Switzerland? Results from the Swiss National Cohort Study. BMJ Open. 2016;6(11):e013090.
Lim K, Kwan Y, Tan C, Low L, Chua A, Lee W, et al. The association between distance to public amenities and cardiovascular risk factors among lower income Singaporeans. Preventive medicine reports. 2017;8:116–21.
Pereira G, Foster S, Martin K, Christian H, Boruff BJ, Knuiman M, et al. The association between neighborhood greenness and cardiovascular disease: an observational study. BMC Public Health. 2012;12:1–9.
Download references
Acknowledgements
Not appliable.
The General Project of Humanities and Social Sciences Research of the Ministry of Education in 2020: A Study on the Assessment and Planning of Healthy Cities Based on Spatial Data Mining (No. 20YJA630011) and the Natural Resources Digital Industry Academy Construction Project.
Author information
Authors and affiliations.
School of Geographical and Planning, Nanning Normal University, Nanning, 530100, Guangxi, China
Shuguang Deng, Jinlong Liang, Jinhong Su & Shuyan Zhu
School of Architecture, Guangxi Arts University, Nanning, 530009, Guangxi, China
Fatulty of Innovation and Design, City University of Macau, Macau, 999078, China
You can also search for this author in PubMed Google Scholar
Contributions
D.S. Provides research topics, conceptual guidance, translation, paper revision and financial support; L.J. Conceived the framework and wrote the original draft; P.Y. Manuscript checking, chart optimization; L.W. Provided suggestions for revision, and reviewed and edited them; S.J. Is responsible for data acquisition and editing; Z.S. Edits the visual map.
Corresponding author
Correspondence to Jinlong Liang .
Ethics declarations
Ethics approval and consent to participate.
Our study was conducted in accordance with the ethical principles outlined in the Declaration of Helsinki, as well as relevant national and institutional guidelines for human research. The study received approval from the Medical Ethics Committee of Guangxi Zhuang Autonomous Region Nationality Hospital (Approval No.: 2024–65). The de-identified data records from the cardiovascular department that we accessed and analyzed were authorized by Guangxi Nationality Hospital. These data were collected and maintained in compliance with the hospital's patient data management policies and procedures. Given that our study involved only a retrospective analysis of existing medical records, with no direct interaction with patients and no potential for causing any substantial harm, the Medical Ethics Committee of Guangxi Zhuang Autonomous Region Nationality Hospital determined that individual patient informed consent was not required. Nonetheless, we have ensured that all data used in the study were fully anonymized and protected, adhering to the highest standards of confidentiality and privacy.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/ .
Reprints and permissions
About this article
Cite this article.
Deng, S., Liang, J., Peng, Y. et al. Spatial analysis of the impact of urban built environment on cardiovascular diseases: a case study in Xixiangtang, China. BMC Public Health 24 , 2368 (2024). https://doi.org/10.1186/s12889-024-19884-x
Download citation
Received : 27 April 2024
Accepted : 26 August 2024
Published : 31 August 2024
DOI : https://doi.org/10.1186/s12889-024-19884-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Built environment
- Impact mechanism
BMC Public Health
ISSN: 1471-2458
- General enquiries: [email protected]
Network analysis of depression, anxiety, and quality of life among widowed older adults in China
- Published: 02 September 2024
Cite this article

- Yuanyuan Wu ORCID: orcid.org/0009-0008-0833-8889 1 &
- Meng Cai 1
Mental health is an important aspect of healthy aging, especially for widowed older adults. This study aims to examine the interrelationships between depression and anxiety symptoms and their associations with quality of life among widowed older adults. Using data from the 2017–2018 Chinese Longitudinal Healthy Longevity Survey (CLHLS), we selected a sample of 6,061 widowed older adults ( M age = 88.97, SD = 10.01). Depression, anxiety, and quality of life were assessed using the Center for Epidemiological Studies Depression (CESD-10) Scale, the Generalized Anxiety Disorder (GAD-7) Scale, and a self-reported question of quality of life (QoL), respectively. The network analysis was performed to identify central and bridge symptoms of depression and anxiety. Network stability was tested using a case-dropping bootstrap procedure. The “flow” package was used to identify symptoms directly or indirectly associated with QoL. The R package NetworkComparisonTest (NCT) was conducted to examine whether network characteristics differed by gender. Network analysis revealed that GAD2 “Uncontrollable worry” emerged as the most central symptom in the network of depression and anxiety. Bridge symptoms such as GAD1 “Nervousness”, CESD6 “Felt fearful”, and CESD1 “Felt bothered” were identified as triggers for depression and anxiety. CESD5 “Hopelessness” exhibited the most negative association with the quality of life among widowed older adults. Gender did not significantly influence the network structure and global strength. These findings deepen our understanding of the inter-relationships between depression and anxiety among Chinese widowed older adults. Targeting central and bridge symptoms for treatments or interventions, and promoting hope among widowed older adults may enhance their quality of life.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Subscribe and save.
- Get 10 units per month
- Download Article/Chapter or eBook
- 1 Unit = 1 Article or 1 Chapter
- Cancel anytime
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions
Similar content being viewed by others

Network analysis of anxiety and depressive symptoms during the COVID-19 pandemic in older adults in the United Kingdom

Associations between anxiety, depression, and personal mastery in community-dwelling older adults: a network-based analysis

Physical symptoms and anxiety and depression in older patients with advanced cancer in China: a network analysis
Bai, W., Zhao, Y. J., Cai, H., Sha, S., Zhang, Q., Lei, S. M.,... & Xiang, Y. T. (2022). Network analysis of depression, anxiety, insomnia and quality of life among Macau residents during the COVID-19 pandemic. Journal of Affective Disorders , 311 , 181–188. https://doi.org/10.1016/j.jad.2022.05.061
Article PubMed PubMed Central Google Scholar
Bakkane Bendixen, A., Engedal, K., Selbæk, G., & Hartberg, C. B. (2018). Anxiety symptoms in older adults with depression are associated with suicidality. Dementia Geriatric Cognitive Disorders , 45 , 180–189. https://doi.org/10.1159/000488480
Article PubMed Google Scholar
Beard, C., Millner, A. J., Forgeard, M. J., Fried, E. I., Hsu, K. J., Treadway, M. T., & Björgvinsson, T. (2016). Network analysis of depression and anxiety symptom relationships in a psychiatric sample. Psychological Medicine , 46 (16), 3359–3369. https://doi.org/10.1017/S0033291716002300
Beck, A. T. (2005). The current state of cognitive therapy: A 40-year retrospective. Archives of General Psychiatry , 62 (9), 953–959. https://doi.org/10.1001/archpsyc.62.9.953
Bornstein, P. E., Clayton, P. J., Halikas, J. A., Maurice, W. L., & Robins, E. (1973). The depression of widowhood after thirteen months. British Journal of Psychiatry , 122 (570), 561–566. https://doi.org/10.1192/bjp.122.5.561
Article Google Scholar
Borsboom, D. (2017). A network theory of mental disorders. World Psychiatry , 16 (1), 5–13. https://doi.org/10.1002/wps.20375
Borsboom, D., & Cramer, A. O. (2013). Network analysis: An integrative approach to the structure of psychopathology. Annual Review of Clinical Psychology , 9 (1), 91–121. https://doi.org/10.1146/annurev-clinpsy-050212-185608
Bozo, Ö., Toksabay, N. E., & Kürüm, O. (2009). Activities of daily living, depression, and social support among elderly Turkish people. The Journal of Psychology , 143 (2), 193–206. https://doi.org/10.3200/JRLP.143.2.193-206
Carr, D., & Utz, R. (2001). Late-life widowhood in the United States: New directions in research and theory. Ageing International , 27 , 65–88. https://doi.org/10.1007/s12126-001-1016-3
Chappell, N. L. (1991). Living arrangements and sources of caregiving. Journal of Gerontology , 46 (1), S1–S8. https://doi.org/10.1093/geronj/46.1.S1
Chen, J., Wang, Q., Liang, Y., Chen, B., & Ren, P. (2023). Comorbidity of loneliness and social anxiety in adolescents: Bridge symptoms and peer relationships. Social Science & Medicine , 334 , 116195. https://doi.org/10.1016/j.socscimed.2023.116195
Cheng, S. T., & Chan, A. C. (2005). The center for epidemiologic studies depression scale in older Chinese: Thresholds for long and short forms. International Journal of Geriatric Psychiatry: A Journal of the Psychiatry of late life and Allied Sciences , 20 (5), 465–470. https://doi.org/10.1002/gps.1314
Contreras, A., Nieto, I., Valiente, C., Espinosa, R., & Vazquez, C. (2019). The study of psychopathology from the network analysis perspective: A systematic review. Psychotherapy and Psychosomatics , 88 (2), 71–83. https://doi.org/10.1159/000497425
Cramer, A. O., Waldorp, L. J., Van Der Maas, H. L., & Borsboom, D. (2010). Comorbidity: A network perspective. Behavioral and Brain Sciences , 33 , 137–150. https://doi.org/10.1017/S0140525X09991567
Das, P., Saha, S., Das, T., Das, P., & Roy, T. B. (2024). Association of depression with widowhood, loneliness, and social non-participation among older women in India. Journal of Medicine Surgery and Public Health , 3 , 100111. https://doi.org/10.1016/j.glmedi.2024.100111
Deng, Y., Zhao, H., Liu, Y., Liu, H., Shi, J., Zhao, C., & He, M. (2022). Association of using biomass fuel for cooking with depression and anxiety symptoms in older Chinese adults. Science of the Total Environment , 811 , 152256. https://doi.org/10.1016/j.scitotenv.2021.152256
Dixit, D., Spreadbury, J., Orlando, R., Hayward, E., & Kipps, C. (2021). Quality of life assessments in individuals with young-onset dementia and their caregivers. Journal of Geriatric Psychiatry and Neurology , 34 (5), 426–433. https://doi.org/10.1177/0891988720933348
Epskamp, S., & Fried, E. I. (2018). A tutorial on regularized partial correlation networks. Psychological Methods , 23 (4), 617. https://doi.org/10.1037/met0000167
Epskamp, S., Cramer, A. O. J., Waldorp, L. J., Schmittmann, V. D., Borsboom, D., Waldrop, L. J., Schmittmann, V. D., & Borsboom, D. (2012). Qgraph: Network visualizations of relationships in psychometric data. Journal of Statistical Software , 48 (4), 1–18. https://doi.org/10.18637/jss.v048.i04
Epskamp, S., Borsboom, D., & Fried, E. I. (2018). Estimating psychological networks and their accuracy: A tutorial paper. Behavior Research Methods , 50 , 195–212. https://doi.org/10.3758/s13428-017-0862-1
Foygel, R., & Drton, M. (2010). Extended bayesian information criteria for gaussian graphical models. NIPS , 23.
GBD 2019 Mental Disorders Collaborators. (2022). Global, regional, and national burden of 12 mental disorders in 204 countries and territories, 1990–2019: A systematic analysis for the global burden of Disease Study 2019. The Lancet Psychiatry , 9 (2), 137–150. https://doi.org/10.1016/S2215-0366(21)00395-3
Article PubMed Central Google Scholar
Gorman, J. M. (1996). Comorbid depression and anxiety spectrum disorders. Depression And Anxiety , 4(4), 160–168. https://doi.org/10.1002/(SICI)1520-6394(1996)4%3C;160::AID-DA2%3E;3.0.CO;2-J
Hegelund, E. R., Wimmelmann, C. L., Strizzi, J. M., Folker, A. P., Mortensen, E. L., & Flensborg-Madsen, T. (2020). Birth weight and quality of life in midlife: A 50-year follow-up study of 2079 individuals in Denmark. Quality of Life Research , 29 , 1047–1054. https://doi.org/10.1007/s11136-019-02348-w
Holmes, T. H., & Rahe, R. H. (1967). The social readjustment rating scale. Journal of Psychosomatic Research . https://doi.org/10.1016/0022-3999(67)90010-4
Hossain, B., & James, K. S. (2024). Widowhood status, morbidity, and mortality in India: Evidence from a follow-up survey. Journal of Biosocial Science , 56 (3), 574–589. https://doi.org/10.1017/S0021932023000226
Hou, B., & Zhang, H. (2023). Latent profile analysis of depression among older adults living alone in China. Journal of Affective Disorders , 325 , 378–385. https://doi.org/10.1016/j.jad.2022.12.154
Houston, K. T., Shrestha, A., Kafle, H. M., Singh, S., Mullany, L., Thapa, L., & Surkan, P. J. (2016). Social isolation and health in widowhood: A qualitative study of Nepali widows’ experiences. Health Care for Women International , 37 (12), 1277–1288. https://doi.org/10.1080/07399332.2016.1142546
Huang, X., Zhang, M., Fang, J., Zeng, Q., Wang, J., & Li, J. (2022). Classifying and characterizing the development of self-reported overall quality of life among the Chinese elderly: A twelve-year longitudinal study. BMC Public Health , 22 (1), 1139. https://doi.org/10.1186/s12889-022-13314-6
Jacobson, N. C., & Newman, M. G. (2017). Anxiety and depression as bidirectional risk factors for one another: A meta-analysis of longitudinal studies. Psychological Bulletin , 143 (11), 1155. https://doi.org/10.1037/bul0000111
Jilili, M., & Liu, L. (2022). Examining the impact of functional disability and cognitive impairment on mental health of Chinese elderly. Social Work in Health Care , 61 , 338–352. https://doi.org/10.1080/00981389.2022.2091080
Jones, P. J., Ma, R., & McNally, R. J. (2021). Bridge centrality: A network approach to understanding comorbidity. Multivariate Behavioral Research , 56 (2), 353–367. https://doi.org/10.1080/00273171.2019.1614898
Kaiser, T., Herzog, P., Voderholzer, U., & Brakemeier, E. L. (2021). Unraveling the comorbidity of depression and anxiety in a large inpatient sample: Network analysis to examine bridge symptoms. Depression and Anxiety , 38 (3), 307–317. https://doi.org/10.1002/da.23136
Kim, Y., & Kim, C. S. (2016). Will the pain of losing a husband last forever? The effect of transition to widowhood on mental health. Development and Society , 45 (1), 165–187. https://www.jstor.org/stable/deveandsoci.45.1.165
Kinsella, K. G., & Taeuber, C. M. (1993). An aging world II (Vol. 3). US Government Printing Office.
Google Scholar
Li, A., Wang, D., Lin, S., Chu, M., Huang, S., Lee, C. Y., & Chiang, Y. C. (2021). Depression and life satisfaction among middle-aged and older adults: Mediation effect of functional disability. Frontiers in Psychology , 12 , 755220. https://doi.org/10.3389/fpsyg.2021.755220
Li, Q., Smith, J. P., & Zhao, Y. (2023). Understanding the effects of widowhood on health in China: Mechanisms and heterogeneity. The Journal of the Economics of Ageing , 25 , 100458. https://doi.org/10.1016/j.jeoa.2023.100458
Liu, Y., Chen, X., & Yan, Z. (2020). Depression in the house: The effects of household air pollution from solid fuel use among the middle-aged and older population in China. Science of the Total Environment , 703 , 134706. https://doi.org/10.1016/j.scitotenv.2019.134706
Locke, D. E., Decker, P. A., Sloan, J. A., Brown, P. D., Malec, J. F., Clark, M. M., & Buckner, J. C. (2007). Validation of single-item linear analog scale assessment of quality of life in neuro-oncology patients. Journal of pain and Symptom Management , 34 (6), 628–638. https://doi.org/10.1016/j.jpainsymman.2007.01.016
Maccallum, F., & Bryant, R. A. (2020). A network approach to understanding quality of life impairments in prolonged grief disorder. Journal of Traumatic Stress , 33 (1), 106–115. https://doi.org/10.1002/jts.22383
Maj, M. (2005). Psychiatric comorbidity’: An artefact of current diagnostic systems? The British Journal of Psychiatry , 186 (3), 182–184. https://doi.org/10.1192/bjp.186.3.182
Marchetti, I. (2019). Hopelessness: A network analysis. Cognitive Therapy and Research , 43 (3), 611–619. https://doi.org/10.1007/s10608-018-9981-y
Montorio, I., Nuevo, R., Márquez, M., Izal, M., & Losada, A. (2003). Characterization of worry according to severity of anxiety in elderly living in the community. Aging & Mental Health , 7 (5), 334–341. https://doi.org/10.1080/1360786031000150694
Naef, R., Ward, R., Mahrer-Imhof, R., & Grande, G. (2013). Characteristics of the bereavement experience of older persons after spousal loss: An integrative review. International Journal of Nursing Studies , 50 (8), 1108–1121. https://doi.org/10.1016/j.ijnurstu.2012.11.026
Niu, L., Qiu, Y., Luo, D., Chen, X., Wang, M., Pakenham, K. I., & Xiao, S. (2016). Cross-culture validation of the HIV/AIDS stress scale: The development of a revised Chinese version. PLoS One , 11 (4), e0152990. https://doi.org/10.1371/journal.pone.0152990
Ohrnberger, J., Fichera, E., & Sutton, M. (2017). The dynamics of physical and mental health in the older population. The Journal of the Economics of Ageing , 9 , 52–62. https://doi.org/10.1016/j.jeoa.2016.07.002
Onrust, S. A., & Cuijpers, P. (2006). Mood and anxiety disorders in widowhood: A systematic review. Aging & Mental Health , 10 (4), 327–334. https://doi.org/10.1080/13607860600638529
Pan, H., & Liu, Q. (2021). Difference of depression between widowed and non-widowed older people in China: A network analysis approach. Journal of Affective Disorders , 280 , 68–76. https://doi.org/10.1017/S2045796021000275
Prigerson, H. G., Shear, M. K., Newsom, J. T., Frank, E., Reynolds, C. F. III, MaciejewskiP. K.,... & Kupfer, D. J. (1996). Anxiety among widowed elders: Is it distinct from depression and grief? Anxiety , 2 (1), 1–12. https://doi.org/10.1002/(SICI)1522-7154(1996)2:1%3C;1::AID-ANXI1%3E;3.0.CO;2-V
Radloff, L. S. (1977). The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement , 1 (3), 385–401. https://doi.org/10.1177/014662167700100306
Ren, L., Wang, Y., Wu, L., Wei, Z., Cui, L. B., Wei, X., & Liu, X. (2021). Network structure of depression and anxiety symptoms in Chinese female nursing students. BMC Psychiatry , 21 , 1–12. https://doi.org/10.1186/s12888-021-03276-1
Sajeev, A., Kakunje, A., & Karkal, R. (2022). Hopelessness and quality of life in elderly: A community-based cross-sectional study. Journal of Geriatric Mental Health , 9 (1), 21–25. https://doi.org/10.4103/jgmh.jgmh_12_22
Sasson, I., & Umberson, D. J. (2014). Widowhood and depression: New light on gender differences, selection, and psychological adjustment. Journals of Gerontology Series B: Psychological Sciences and Social Sciences , 69 (1), 135–145. https://doi.org/10.1093/geronb/gbt058
Silva, P., Gonçalves, R., Magalhães, R., & Delerue Matos, A. (2023). Can the internet mitigate the negative effect of widowhood on quality of life? A gender analysis. Journal of Population Ageing , 16 (3), 679–697. https://doi.org/10.1007/s12062-022-09373-7
Spitzer, R. L., Kroenke, K., Williams, J. B., & Löwe, B. (2006). A brief measure for assessing generalized anxiety disorder: The GAD-7. Archives of Internal Medicine , 166 (10), 1092–1097. https://doi.org/10.1001/archinte.166.10.1092
Stroebe, M. S., Stroebe, W., & Hansson, R. O. (Eds.). (1993). Handbook of bereavement: Theory, research, and intervention. Cambridge University Press , 175–195. https://doi.org/10.1017/CBO9780511664076.013
Umberson, D., Wortman, C. B., & Kessler, R. C. (1992). Widowhood and depression: Explaining long-term gender differences in vulnerability. Journal of health and social behavior , 10–24. https://doi.org/10.2307/2136854
UNDESA (2017). World Population Prospects: The 2017 Revision. United Nations, Department of Economic and Social Affairs, Population Division, New York. https://population.un.org/wpp
Van Boekel, L. C., Cloin, J. C. M., & Luijkx, K. G. (2021). Community-dwelling and recently widowed older adults: Effects of spousal loss on psychological well-being, perceived quality of life, and health-care costs. The International Journal of Aging and Human Development , 92 (1), 65–82. https://doi.org/10.1177/0091415019871204
Van Borkulo, C. D., Van Bork, R., Boschloo, L., Kossakowski, J. J., Tio, P., Schoevers, R. A., Borsboom, D., & Waldorp, L. J. (2022). Comparing network structures on three aspects: A permutation test. Psychological Methods . https://doi.org/10.1037/met0000476
Wang, G. Z., & Ge, Y. X. (2013). Status of widowed elderly population in China and its development trend. Scientific Research on Aging , 1 (1), 44–55. (in Chinese).
Wang, S., Hou, W., Tao, Y., Ma, Z., Li, K., Wang, Y.,... & Zhang, L. (2022). Mapping network connection among symptoms of anxiety, depression, and sleep disturbance in Chinese high school students. Frontiers in Public Health , 10 , 1015166. https://doi.org/10.3389/fpubh.2022.1015166
Xu, J., Wu, Z., Schimmele, C. M., & Li, S. (2020). Widowhood and depression: A longitudinal study of older persons in rural China. Aging & Mental Health , 24 (6), 914–922. https://doi.org/10.1080/13607863.2019.1571016
Yang, F. (2021). Widowhood and loneliness among Chinese older adults: The role of education and gender. Aging & Mental Health , 25 (7), 1214–1223. https://doi.org/10.1080/13607863.2020.1732293
Yang, F., & Gu, D. (2021). Widowhood, widowhood duration, and loneliness among older adults in China. Social Science & Medicine , 283 , 114179. https://doi.org/10.1016/j.socscimed.2021.114179
Yang, X., Fang, Y., Chen, H., Zhang, T., Yin, X., Man, J.,... & Lu, M. (2021). Global, regional and national burden of anxiety disorders from 1990 to 2019: Results from the global burden of Disease Study 2019. Epidemiology and Psychiatric Sciences , 30 , e36. https://doi.org/10.1017/S2045796021000275
Yohannes, A. M., Dodd, M., Morris, J., & Webb, K. (2011). Reliability and validity of a single item measure of quality of life scale for adult patients with cystic fibrosis. Health and Quality of life Outcomes , 9 , 1–8. https://doi.org/10.1186/1477-7525-9-105
Yu, L., & Chen, C. (2024). Symptom patterns of comorbid depression and anxiety among older adults in China and their predictors. PsyCh Journal , 13 (3), 494–511. https://doi.org/10.1002/pchj.729
Zeng, Y. (2017). Chinese Longitudinal Healthy Longevity Survey (CLHLS), 1998–2014.
Zhang, W. J., Li, S. Z., & Feldman, M. W. (2005). Gender differences in activity of daily living of the elderly in rural China: Evidence from Chaohu. Journal of Women & Aging , 17 , 73–89. https://doi.org/10.1300/J074v17n03_06
Zhang, P., Wang, L., Zhou, Q., Dong, X., Guo, Y., Wang, P., & Sun, C. (2023a). A network analysis of anxiety and depression symptoms in Chinese disabled elderly. Journal of Affective Disorders , 333 , 535–542. https://doi.org/10.1016/j.jad.2023.04.065
Zhang, Y., Cui, Y., Li, Y., Lu, H., Huang, H., Sui, J., & Miao, D. (2023b). Network analysis of depressive and anxiety symptoms in older Chinese adults with diabetes mellitus. Research Square . https://doi.org/10.21203/rs.3.rs-2712115/v2
Download references
Acknowledgements
The data are publicly available. We thank the Center for China Survey and Data Center at Renmin University of China for opening access to this dataset.
This study was supported by the National Social Science Fund of China (No. 22BSH109).
Author information
Authors and affiliations.
School of Humanities and Social Science, Xi’an Jiaotong University, 28 Xianning West Rd., Beilin District, Xi’an, 710049, Shaanxi, P.R. China
Yuanyuan Wu & Meng Cai
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Yuanyuan Wu .
Ethics declarations
Ethical approval.
This study was reviewed and approved by the Ethics Committee of Renmin University of China. All participants provided writted informed consent, and the study was conducted in accordance with the Declaration of Helsinki.
Conflicts of interest
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Rights and permissions.
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Wu, Y., Cai, M. Network analysis of depression, anxiety, and quality of life among widowed older adults in China. Curr Psychol (2024). https://doi.org/10.1007/s12144-024-06634-w
Download citation
Accepted : 29 August 2024
Published : 02 September 2024
DOI : https://doi.org/10.1007/s12144-024-06634-w
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Quality of life
- Widowed older adults
- Network analysis
- Find a journal
- Publish with us
- Track your research
- Our Litigation Approach
- Diversity, Equity & Inclusion
- Public Interest & Pro Bono
- Recent Victories
- SG Careers Overview
- Associate Life
- Associate Compensation & Benefits
- Meet Our Associates
- Summer Program
- Selendy Gay Fellowship
- Publications

September 4, 2024
Selendy Gay Secures $1 Billion Trial Victory Against Johnson & Johnson
Selendy Gay and Delaware co-counsel Ross Aronstam & Moritz secured a very significant trial victory on behalf of the former stockholders of Auris Health, Inc (represented by Fortis Advisors) in their long-running earnout dispute with Johnson & Johnson. Following a January trial, Vice Chancellor Lori W. Will of the Delaware Court of Chancery issued a decision awarding more than $1 billion in damages for J&J’s breach of contract, breach of implied covenant, and fraud. The 145-page decision constitutes the most important precedent and largest award in Delaware history in an earnout case.
The dispute stemmed from J&J’s acquisition of Auris Health in 2019 and its subsequent actions ensuring that the milestones set forth in the merger agreement would not be achieved, and thus that $2.35 billion of the merger consideration would never be paid.
Under the terms of the deal, Auris stockholders were to receive these earnout payments upon the achievement of certain regulatory and net sales milestones related to Auris’s cutting edge robotically assisted surgical devices. As VC Will found, Auris was “on a path to bring life-changing technologies to market” and that “[l]ed by Dr. Frederic Moll, the visionary architect of robotic surgery, Auris had developed two novel surgical robots in record time: Monarch and iPlatform.” VC Will found that “Monarch had unmatched capability to diagnose and treat lung cancer”, while “iPlatform took Moll’s original market-leading surgical robot to new heights with innovative features for laparoscopic and endoscopic procedures.”
VC Will found that immediately after the acquisition, J&J began breaching its contractual obligation to make “commercially reasonable efforts” to meet the iPlatform milestones. She found that “[i]nstead of providing efforts and resources to achieve the regulatory milestones, J&J thrust iPlatform into a head-to-head faceoff” against its own competing laparoscopic robot, Verb, which substantially delayed progress toward iPlatform’s regulatory milestones. Moreover, even after J&J decided iPlatform was “the better bet,” “[t]o salvage its years of investment in Verb, J&J directed that Verb’s hardware and team be added to iPlatform,” effectively turning iPlatform into “a parts shop for Verb.” VC Will found that J&J knew all this would hinder achievement of the regulatory milestones, but “viewed the resulting delays as beneficial since it could avoid making the earnout payment,” and that it then wrote off the iPlatform regulatory milestones “under the pretext of an unforeseen [regulatory] policy change.”
VC Will found that J&J breached its contractual obligations to treat iPlatform as a priority device, to provide efforts in support of the regulatory milestones, and to avoid making decisions based on the contingent payment – “most blatantly when iPlatform was made to compete against and combine with Verb.” She further found that J&J breached the implied covenant of good faith and fair dealing when it failed to devote efforts to achieve the revised regulatory pathway.
In addition, VC Will found that J&J committed fraud to induce Auris to agree to a Monarch milestone involving regulatory clearance using a J&J-developed catheter. “J&J told Auris that this milestone was so certain to be met that J&J viewed the associated payment as up front consideration. J&J neglected to mention that it was under a regulatory investigation because a patient in a clinical study using the catheter had recently died, which put the milestone in doubt.”
VC Will found J&J liable to pay more than $1 billion in damages and interest to “compensate[] Auris’s former stockholders for the earnout payment they would have received absent J&J’s failed efforts and fraud.” She further noted that “[w]hat remains irretrievably lost is the transformative potential of Auris’s robots.”
The Fortis team was led by Selendy Gay partners Philippe Z. Selendy, Jennifer Selendy, Sean Baldwin, and Oscar Shine and associates Meredith Nelson, Julie Singer, and Jeff Zalesin, as well as Bradley R. Aronstam and Roger S. Stronach of Ross Aronstam & Moritz LLP.
In a joint statement, Philippe Z. Selendy, Jennifer Selendy, and Sean Baldwin said, "The firm appreciates the exhaustive analysis of the Delaware Court of Chancery in this important matter."

Philippe Z. Selendy Partner

Jennifer Selendy Partner

Sean Baldwin Partner

Oscar Shine Partner

Meredith Nelson Associate

Julie Singer Associate

Jeff Zalesin Associate
Mainstreaming of Gender Equality, Disability, and Social Inclusion (GEDSI) in Water, Sanitation, and Hygiene (WASH) in health-care facilities, Kandy District, Sri Lanka
I ntroduction
Water, Sanitation, and Hygiene (WASH) are essential pillars of healthcare that profoundly influence the quality of care, patient safety, and overall public health. In Kandy District, Sri Lanka, the critical role of WASH in healthcare settings has gained increasing attention, particularly considering the challenges experienced by both healthcare workers and patients.
Recognizing the pressing need for improvement, the World Health Organization (WHO) Sri Lanka, in collaboration with the Office of the Kandy Regional Director of Health Service (RDHS), conducted a comprehensive two-fold brainstorming session on 31 July 2024. This session brought together both health and non-health staff selected by the RDHS’s Office to evaluate the current WASH needs across the district's healthcare facilities.
The Kandy District was chosen as the pilot for this brainstorming discussion and training due to its notable climate vulnerability. As part of the Central Province, Sri Lanka’s second-largest province located in the highland interior of the island, Kandy District is particularly susceptible to environmental risks. The Central Province comprises three administrative districts: Kandy, Matale, and Nuwara Eliya. Within Kandy District, numerous Grama Niladhari [1] Divisions are identified with varying levels of landslide risk, including both high and low potential for rainfall-induced landslides [2] and flooding during the Monsoon Seasons.
Brainstorming Discussion
A case study was developed following the brainstorming discussion, and it explores the key insights collected from this discussion, delving into the specific needs, challenges, and priorities identified, and providing actionable recommendations for enhancing WASH services in the region. The findings highlight gaps in infrastructure, training, and community engagement, all of which contribute to the need to improve the overall state of WASH services in the district. Addressing these challenges requires a coordinated effort involving legal reforms, community education, and a thorough mapping and planning process. By prioritizing WASH, Kandy District can make significant strides towards improving health outcomes and ensuring that all community members have access to safe and sanitary healthcare facilities.
Implementing the recommendations outlined in the developed case study will therefore undoubtedly require the commitment and collaboration of all stakeholders, including healthcare workers, government officials, community members, and development partners. However, with the right strategies and resources in place, it is possible to transform the WASH services in Kandy District's healthcare facilities, ensuring that they meet the needs of all users and contribute to the overall well-being of the community
/countries/sri-lanka/gedsi-training-1.jpeg?sfvrsn=7785cb51_5)
Images captured during the Brainstorm Discussions being led by the WHO Sri Lanka, National Consultant on Gender, Equity and Rights (GER) Naushalya Rajapaksha on the 31 July, in Kandy.
Training Sessions
On 2 and 3 August 2024, a groundbreaking training session was held in Kandy District, focusing on the integration of Gender Equality, Disability, and Social Inclusion (GEDSI) into Water, Sanitation, and Hygiene (WASH) practices within healthcare facilities. Organized by the WHO Sri Lanka and the Office of the Kandy RDHS, this workshop brought together over 80 regional health and non-health workers for an intensive two-day program.
The workshop aimed to embed GEDSI principles into the planning, implementation, and management of WASH programs, policies, and practices within Kandy's healthcare institutions. This event was particularly significant as it marked the first time such a comprehensive training on GEDSI integration into WASH in healthcare facilities had been conducted in Sri Lanka The workshop was based on the "Toolkit on Mainstreaming Gender Equality, Disability, and Social Inclusion in WASH in Health-Care Facilities 2023 [3] ," developed by WHO's South-East Asia Regional Office (SEARO). This toolkit serves as a critical resource for policymakers, program managers, and facility administrators, offering guidance on how to design and manage healthcare facilities that are not only hygienic but also inclusive, accessible, and respectful of the rights and dignity of every individual.
The workshop's curriculum was meticulously designed to address the unique challenges faced in Sri Lanka's healthcare settings, particularly in Kandy District. It included sessions on identifying and addressing barriers to access, understanding the specific WASH needs of diverse populations, and developing strategies to ensure that WASH facilities are safe, clean, and accessible to all. The training emphasized the importance of creating environments where gender, disability, and social inclusion are not just mere afterthoughts but integral components of the ongoing and future WASH programs in the Kandy District.
/countries/sri-lanka/gedsi-training-group-picture-1.jpeg?sfvrsn=6971c67_6)
Images captured during the two-day training programme led by the WHO Sri Lanka, National Consultant on Gender, Equity and Rights (GER) Naushalya Rajapaksha on 1 and 2 of August, in Kandy.
Good Practices
A key highlight of the event was its unwavering adherence to WHO's Code of Conduct on Events, underscoring a firm commitment to ethical practices and sustainability. To further reinforce this commitment, stationery stations were centrally located, accompanied by prominently displayed materials on WHO’s Policy on Preventing and Addressing Sexual Misconduct (PRSM). These displays also included WHO’s three-year strategy for Preventing and Responding to Sexual Misconduct (2023-2025) and the WHO Accountability Framework for 2023. Participants were encouraged to engage with the facilitator to discuss these policies and procedures in depth, fostering a deeper understanding of WHO’s approach to addressing and preventing sexual misconduct. This initiative not only highlighted the organization’s dedication to upholding high ethical standards but also provided a platform for meaningful dialogue on critical issues concerning PRSM.
/countries/sri-lanka/gedsi-awareness-session-1.jpeg?sfvrsn=1b929f9d_4)
Images captured during the two-day training programme led by the WHO Sri Lanka, National Consultant on Gender, Equity and Rights (GER) Naushalya Rajapaksha where participants had the opportunity to meaningfully engage with the facilitator about WHO’s PRSM policies and procedures.
The facilitator also took an innovative approach by minimizing the use of printed materials, instead utilizing strategically placed QR codes throughout the training hall. These QR codes allowed participants to access a wide range of information and training materials digitally, enhancing the learning experience while also significantly reducing the event's environmental footprint.
/countries/sri-lanka/gedsi-awareness-with-qr-code.jpeg?sfvrsn=d7156816_4)
Images captured during the two-day training programme led by the WHO Sri Lanka, National Consultant on Gender, Equity and Rights (GER) Naushalya Rajapaksha where participants actively scanning the QR scan code to access the necessary materials related to the workshop.
By the conclusion of the workshop, participants were thoroughly equipped with the knowledge and tools necessary to implement Gender Equality, Disability, and Social Inclusion (GEDSI) principles within their respective healthcare facilities. This event not only marked a significant milestone in advancing Sri Lanka's approach to Water, Sanitation, and Hygiene (WASH) in healthcare settings but also set a new precedent for future initiatives aimed at fostering more equitable and inclusive health systems. The training session represents a critical step forward in ensuring that all individuals, regardless of gender, ability, or social status, have access to safe, clean, and dignified healthcare environments across Sri Lanka.
At the workshop's conclusion, the Kandy Regional Director of Health Service extended an invitation to all participants, encouraging them to submit written recommendations on how to enhance the existing WASH facilities within the healthcare institutions in Kandy District. He emphasized the importance of integrating GEDSI principles into these improvements, thereby ensuring that WASH services are not only functional but also inclusive and accessible to all. This collaborative approach underscores the commitment to continuous improvement and the creation of healthcare environments that truly reflect the needs and rights of every individual.
/countries/sri-lanka/gedsi-field-training.jpeg?sfvrsn=408396bc_4)
Images captured during a three-day capacity development workshop on climate-resilient water safety plan audits was conducted by the National Water Supply and Drainage Board, with the support of the World Health Organization. On the second day, participants engaged in practical field training, auditing water supply schemes, water treatment plants, distribution centers, and interacting with consumers. This hands-on experience as captured was aimed to enhance the participants' ability to assess the resilience of water systems to climate change-related challenges .
[2] Climate Change Risk Profile of the Mountain Region in Sri Lanka, May 2022, Asian Development Bank : https://www.adb.org/sites/default/files/publication/798386/climate-change-risk-profile-mountain-region-sri-lanka.pdf
[3] Toolkit on mainstreaming of gender, equality, disability, and social inclusion (GEDSI) in WASH in health-care facilities, 2023 : https://iris.who.int/handle/10665/373608
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- BMJ Open Qual
- v.11(2); 2022

Defining case management success: a qualitative study of case manager perspectives from a large-scale health and social needs support program
Margae knox.
1 School of Public Health, University of California, Berkeley, Berkeley, California, USA
Emily E Esteban
2 Contra Costa Health Services, Martinez, California, USA
Elizabeth A Hernandez
Mark d fleming, nadia safaeinilli, amanda l brewster, associated data.
No data are available. Data are not publicly available to protect potentially sensitive information. For data inquiries, please contact the corresponding author.
Health systems are expanding efforts to address health and social risks, although the heterogeneity of early evidence indicates need for more nuanced exploration of how such programs work and how to holistically assess program success. This qualitative study aims to identify characteristics of success in a large-scale, health and social needs case management program from the perspective of interdisciplinary case managers.
Case management program for high-risk, complex patients run by an integrated, county-based public health system.
Participants
30 out of 70 case managers, purposively sampled to represent their interdisciplinary health and social work backgrounds. Interviews took place in March–November 2019.
Primary and secondary outcome measures
The analysis intended to identify characteristics of success working with patients.
Case managers described three characteristics of success working with patients: (1) establishing trust; (2) observing change in patients’ mindset or initiative and (3) promoting stability and independence. Cross-cutting these characteristics, case managers emphasised the importance of patients defining their own success, often demonstrated through individualised, incremental progress. Thus, moments of success commonly contrasted with external perceptions and operational or productivity metrics.
Conclusions
Themes emphasise the importance of compassion for complexity in patients’ lives, and success as a step-by-step process that is built over longitudinal relationships.
What is already known on this topic?
- Case management programs to support health and social needs have demonstrated promising yet mixed results. Underlying mechanisms and shared definitions of successful case management are underdeveloped.
What this study adds?
- Case managers emphasised building trust over time and individual, patient-defined objectives as key markers of success, a contrast to commonly used quantitative evaluation metrics.
How this study might affect research, practice or policy?
- Results suggest that lighter touch case management interventions face limitations without an established patient relationship. Results also support a need for alternative definitions of case management success including patient-centered measures such as trust in one’s case manager.
Introduction
Health system efforts to address both health and social needs are expanding. In the USA, some state Medicaid programmes are testing payments for non-medical services to address transportation, housing instability and food insecurity. Medicaid provides healthcare coverage for lower income individuals and families, jointly funded by federal and state governments. Similarly, social prescribing, or the linking of patients with social needs to community resources, is supported by the UK’s National Health Service and has also been piloted by Canada’s Alliance for Healthier Communities. 1
A growing evidence base suggests promising outcomes from healthcare interventions addressing social needs. In some contexts, case managers or navigators providing social needs assistance can improve health 2 and reduce costly hospital use. 3–5 Yet systematic reviews also report mixed results for measures of health and well-being, hospitalisation and emergency department use, and overall healthcare costs. 6–9 Notably, a randomised trial of the Camden Care Coalition programme for patients with frequent hospitalisations due to medically and socially complex needs 10 found no difference in 180-day readmission between patients assigned to a care transitions programme compared with usual hospital postdischarge care. In the care transition programme, patients received follow-up from a multidisciplinary team of nurses, social workers and community health workers. The team conducted home visits, scheduled and accompanied patients to follow-up outpatient visits, helped with managing medications, coached patients on self-care and connected patients with social services and behavioural healthcare. The usual care group received usual postdischarge care with limited follow-up. 11 This heterogeneity of early evidence indicates a need for more nuanced explorations of how social needs assistance programmes work, and how to holistically assess whether programmes are successful. 12 13
Social needs case management may lead to health and well-being improvements through multiple pathways involving both material and social support. 14 15 Improvements are often a long-term, non-linear process. 16 17 At the same time, quality measures specific to social needs assistance programmes currently remain largely undefined. Studies often analyse utilisation and cost outcomes but lack granularity on interim processes and markers of success.
In order to translate a complex and context-dependent intervention like social needs case management from one setting to another, these interim processes and outcomes need greater recognition. 18–20 Early efforts to refine complex care measures are underway and call out a need for person-centred and goal-concordant measures. 21 Further research on how frontline social needs case managers themselves define successes in their work could help leaders improve programme design and management and could also inform broader quality measure development efforts.
Our in-depth, qualitative study sought to understand how case managers defined success in their work with high-risk patients. Case managers were employed by CommunityConnect, a large-scale health and social needs care management programme that serves a mixed-age adult population with varying physical health, mental health and social needs. Each case manager’s workflow includes an individualised, regularly updated dashboard of operational metrics. It is unclear, however, whether or how these operational factors relate to patient success in a complex care programme. Thus, the case managers’ perspectives on defining success are critical for capturing how programmes work and identifying essential principles.
Study design and setting
In 2017, the Contra Costa County Health Services Department in California launched CommunityConnect, a case management programme to coordinate health, behavioural health and social services for County Medicaid patients with complex health and social conditions. The County Health Services Department serves approximately 15% (180 000) of Contra Costa’s nearly 1.2 million residents. CommunityConnect enrollees were selected based on a predictive model, which leveraged data from multiple county systems to identify individuals most likely to use hospital or emergency room services for preventable reasons. Enrollees are predominantly women (59%) and under age 40 (49%). Seventy-seven per cent of enrollees have more than one chronic condition, particularly hypertension (42%), mood disorders (40%) and chronic pain (35%). 22 Programme goals include improving beneficiary health and well-being through more efficient and effective use of resources.
Each case manager interviewed in this study worked full time with approximately 90 patients at a time. Case managers met patients in-person, ideally at least once a month for 1 year, although patients sometimes continue to receive ongoing support at the case manager’s discretion in cases of continued need. Overall, up to 6000 individuals at a time receive in-person case management services through CommunityConnect, with approximately 200–300 added and 200–300 graduated per month. At the time of the study, CommunityConnect employed approximately 70 case managers trained in various public health and social work disciplines (see table 1 , Interview Sample). Case managers and patients are matched based on an algorithm that prioritises mental health history, primary language and county region.
Interview sample
| # Case managers | # Interviewed | |
| Public health nurse | 28 | 9 |
| Substance use counsellor | 12 | 5 |
| Community health worker specialist | 9 | 2 |
| Social worker | 8 | 6 |
| Mental health clinical specialist | 7 | 4 |
| Homeless services specialist | 6 | 4 |
| Total | 70 | 30 |
Although case managers bring unique experience from their respective discipline, all are expected to conduct similar case management services. Services included discussing any unmet social needs with patients, coordinating applicable resources and partnering with the patient and patient’s care team to improve physical and emotional health. The programme tracks hospital and emergency department utilisation as well as patient benefits such as food stamps, housing or transportation vouchers and continuous Medicaid coverage on an overall basis. Each case manager has access to an individualised dashboard that includes operational metrics such as new patients to contact, and frequency of patient contacts, timeliness for calling patients recently discharged from the hospital, whether patients have continuous Medicaid coverage, and completion of social risk screenings.
Study recruitment
Semistructured interviews were conducted with 30 field-based case managers as part of the programme’s evaluation and quality improvement process. Participants included four mental health clinical specialists, five substance abuse counsellors, six social workers, nine public health nurses, four housing support specialists and two community health worker specialists. Case managers were recruited by email and selected based on purposive sampling to reflect membership across disciplines and experience working with CommunityConnect for at least 1 year. Three case managers declined to participate. Interviews ended when data saturation was achieved. 23
Interview procedures
Interviews were conducted by five CommunityConnect evaluation staff members (including EEE), who received training and supervision from the evaluation director (EH), who also conducted interviews. The evaluation staff were bachelor and masters-level trained. The evaluation director was masters-level trained and held prior experience in healthcare quality and programme planning.
The evaluation team drafted the interview guide to ask about a variety of work processes and experiences with the goal of improving programme operations including staff and patient experiences. Specific questions analysed for this study were (1) how case managers define success with a patient and (2) examples where case managers considered work with patients a success.
Interviews took place in-person in private meeting rooms at case managers’ workplace from March 2019 – November 2019. Interviews lasted 60–90 min and only the interviewer and case manager were present. All interviewers were familiar with CommunityConnect yet did not have a prior relationship with case managers. Case managers did not receive compensation beyond their regular salary for participating in the study and were allowed to opt out of recruitment or end the interview early for any reason. All interviews were audio recorded, transcribed and entered into Nvivo V.12 for analysis.
Patient and public involvement
This project focused on case manager’s perspectives and thus did not directly involve patients. Rather, patients were involved through case manager recollections of experiences working with patients.
Data analysis
We used an integrated approach to develop an initial set of qualitative codes including deductive coding of programme processes and concepts, followed by inductive coding of how case managers defined success. All interviews were coded by two researchers experienced in qualitative research (EEE and MK). Themes were determined based on recurrence across interviews and illustrative examples and being described by more than one case manager type. The two researchers identified preliminary themes independently, then consulted with one another to achieve consensus on final themes. Themes and supporting quotes were then presented to the full author team to ensure collective agreement that key perspectives had been included. Preliminary results were also shared at a staff meeting attended by case managers and other staff as an opportunity for feedback on study findings. This manuscript addresses the Standards for Reporting Qualitative Research, 24 and the Consolidated Criteria for Reporting Qualitative Research checklist is provided as an appendix. 25
All case manager participants provided informed consent. Research procedures were approved by the Contra Costa Regional Medical Center and Health Centers Institutional Review Committee (Protocol 12-17-2018).
Case managers frequently and across multiple roles mentioned three characteristics of success when working with patients: (1) establishing trust; (2) fostering change in patients’ mindset or initiative and (3) promoting stability and independence. Across these characteristics, case managers expressed that success is patient-defined, with individualised and often incremental progress—a contrast with external perceptions of success and common operational or productivity metrics (see figure 1 ).

Illustration of key themes.
Success is establishing trust
Trusting relationships were the most widely noted characteristic of success. Trust was described as both a product of case managers’ consistent follow-up and helpfulness over time and a foundational step to enable progress on patient-centred goals. To build trust, case managers explained, patients must feel seen and heard, and understand the case managers’ desire to help: ‘Success is to know that she knows me very well…I look for her on the streets, and I’m waiting for her to call me back. Hopefully she knows that when she’s ready I will be there at least to provide that resource for her and so it’s that personal relationship that you build’ (Case manager 11, social worker). Case managers also highlighted the longitudinal relationship required to establish trust, distinguishing success as more than one-time information delivery or navigating bureaucratic processes to procure services.
Case managers also identified trust as foundational to provide better support for patients: ‘So they’re as honest with me as they can be. That way I have a clear understanding about realistically what I can do to help them coordinate their care or link them to services.’ (Case manager 2, mental health clinician specialist). Establishing trust was essential to improve communication with patients and produced an amplifying effect. That is, a case manager’s initial help and follow-up builds trust so that patients can be more open, and open communication helps the case manager know what specific services can be most useful. This positive feedback loop further cements trust and builds momentum for a longitudinal relationship.
Permission to have a home visit was mentioned as a valuable indicator of early success in building trust: ‘(Your home is) your sanctuary’, expressed one case manager (Case manager 29, public health nurse), acknowledging the vulnerability of opening one’s home to an outsider. For another case manager, regular home visits in the context of a trusting relationship made the case manager aware of and able to address a difficult situation: ‘Every time I was going to her home, I was noticing more and more gnats flying around… She said it’s because of the garbage…’ After establishing trust, the patient allowed the case manager access to the bedroom where the case manager uncovered numerous soiled diapers. The case manager arranged professional cleaning and sanitation through CommunityConnect, after which, ‘there was room for a dance floor in her bedroom. There was so much room, and the look on her face, it was almost as if her chest got proud, just in that day. She didn’t seem so burdened…So that’s a success’ (Case manager 4, substance abuse counsellor). Across multiple examples, case managers expressed trust as a critical element for effective patient partnerships.
However, the pathways to building trust are less clear cut. Quick wins through tangible support such as a transportation voucher to a medical appointment could help engage a patient initially. Yet case managers more frequently emphasised strategies based on relationships over time. Strategies included expressing empathy (putting yourself in the patient’s shoes), demonstrating respect (especially when the patient has experienced disrespect in other health system encounters), keeping appointments, following through on what you say you will do, calling to check in and ‘being there’. Overall, case managers expressed that trust lets patients know they are not alone and sets the stage for future success.
Success is fostering a change in patients’ mindset or initiative
Case managers described a change in patients’ mindset or initiative as evidence of further success. One case manager explained, ‘Really (success) could be a switch in mind state… If I can get someone to consider addressing an issue. Or just acknowledging an issue. That’s progress’ (Case manager 24, substance abuse counsellor). Another case manager spoke to the importance of mindset by stating, ‘what I try to do is not just change the surface of life’. This case manager elaborated, ‘You help (a patient) get their housing and they’re gonna lose it again, unless they change; something changes in their mindset, and then they see things differently.’ (Case manager 6, mental health clinician specialist). Some case managers suggested that the supportive resources they provide are only band-aid solutions if unaccompanied by a changed mindset to address root causes.
Case managers reported that shared goals and plans are essential, in contrast to solutions identified by case managers without patient involvement. ‘I can’t do everything for them’, expressed one case manager (Case manager 21, public health nurse), while others similarly acknowledged that imposing self-improvement goals or providing resources for which a patient may not be ready may be counterproductive. Rather, one case manager emphasised, ‘I think it’s really important to celebrate people’s ideas, their beliefs, their own goals and values’. (Case manager 4, substance abuse counsellor). As an example, the case manager applauded a patient’s ideas of getting a driver’s license and completing an education certificate. In summary, case managers viewed success as a two-way street where patient’s own ideas and motivation were essential for long-term impact.
Success is promoting stability and independence
Case managers also identified patients’ stability and independence as a characteristic of success. One case manager stated, ‘I define success as having them be more independent in their just manoeuvring the system…how they problem solve’ (Case manager 30, public health nurse). Relative to the other characteristics of success, stability and independence more closely built on resources and services coordinated or procured by the case manager. For example, CommunityConnect provides cell phones free-of-charge to patients who do not currently have a phone or continuous service, which has helped patients build a network beyond the case manager: ‘Once we get them that cell phone then they’re able to make a lot of connections … linking to services on their own. They actually become a lot more confident in themselves is what I’ve seen’. (Case manager 23, substance abuse counsellor). In another example, a case manager helped a patient experiencing complex health issues to reconcile and understand various medications. For this patient stability means, ‘when he does go into the emergency room, it’s needed. … even though he’s taking his medication like he’s supposed to… it’s just his health gets bad. So, yea I would say that one (is a success)’ (Case manager 8, social worker). Thus, stability represents maintained, improved well-being, supported by care coordination and resources, even while challenges may still be present.
As a step further, ‘Absolute success’, according to one case manager, ‘(is when a patient) drops off my caseload and I don’t hear from them, not because they’re not doing well but because they are doing well, because they are independent’ (Case manager 12, social worker). Patients may still need periodic help knowing who to contact but can follow through on their own. This independence may arise because patients have found personal support networks and other resources that allow them to rely less and less on the case manager. While not all patients reach this step of sustained independence and stability, it is an accomplishment programmatically and for case managers personally.
Success is patient-defined, built on individualised and incremental progress
Case managers widely recognised that success comes in different shapes and sizes, dependent on their patient’s situation. Irrespective of the primary concern, many identified the patient’s own judgement as the benchmark for success. One case manager explained, ‘I define success with my patients by they are telling me it was a success. It’s by their expression, it’s just not a success until they say it’s a success for them’ (Case manager 7, social worker). In a more specific example, a case manager highlighted checking in with a patient instead of assuming a change is successful: ‘It’s not just getting someone housed or getting someone income. Like the male who we’re working towards reconciliation with his parents… that’s a huge step but if he doesn’t feel good about it… then that’s not a success.’ The same case manager elaborated, ‘it’s really engaging with the knowing where the patient him or herself is at mentally, for me. Yeah. That’s a success’ (Case manager 18, homeless services specialist). This comment challenges the current paradigm where, for example, if a patient has a housing need and is matched to housing, then the case is a success. Rather, case managers viewed success as more than meeting a need but also reciprocal satisfaction from the patient.
Often, case managers valued individualised, even if seemingly small, achievements as successes: ‘Every person’s different you know. A success could be just getting up and brushing their teeth. Sometimes success is actually getting them out of the house or getting the care they need’ (Case manager 28, social worker). Another case manager echoed, ‘(Success) depends on where they’re at … it runs the gamut, you know, but they’re all successes’ (Case manager 10, public health nurse). CommunityConnect’s interdisciplinary focus was identified as an important facilitator for tailoring support to individualised client needs. In contrast with condition-specific case management settings, for example, a case manager with substance abuse training noted, ‘whether someone wants to address their substance use or not, they still have these other needs, and (with CommunityConnect) I can still provide assistance’ (Case manager 24).
However, the individualised and incremental successes are not well captured by common case management metrics. One case manager highlighted a tension between operational productivity metrics and patient success, noting, ‘I get it, that there has to be accountability. We’re out in the field, I mean people could really be doing just a whole lot of nothing… (Yet), for me I don’t find the success in the numbers. I don’t think people are a number. Oh, look I got a pamphlet for you, I’m dropping it off… I don’t think that that is what’s really going to make this programme successful’ (Case manager 8, social worker). One case manager mentioned change in healthcare utilisation as a marker of success, but more often, case managers offered stories of patient success that diverge from common programme measures. For example, one case manager observed, ‘The clear (successes) are nice: when you apply for Social Security and they get it that’s like a hurrah. And then there’s other times it’s just getting them to the dentist’ (Case manager 28, social worker). Another case manager elaborated, ‘It’s not always the big number—the how many people did I house this year. It’s the little stuff like the fact that this 58-year-old woman who believes she’s pregnant and has been living outside for years and years, a victim of domestic violence, has considered going inside. Like that is gigantic’ (Case manager 18, homeless services specialist). Overwhelmingly, case managers defined success through the interpersonal relationship with their patients within patients’ complex, daily life circumstances.
Case managers’ definitions of success focused on establishing trust, fostering patients change in mindset or initiative, and, for some patients, achieving independence and stability. Examples of success were commonly incremental and specific to an individual’s circumstances, contrasting with programmatic measures such as reduction in hospital or emergency department utilisation, benefits and other resources secured, or productivity expectations. Study themes heavily emphasise the interpersonal relationship that case managers have with patients and underscore the importance of patient-centred and patient-defined definitions of success over other outcome measures.
Our results complement prior work on clinic-based programmes for complex patients. For example, interdisciplinary staff in a qualitative study of an ambulatory intensive care centre also identified warm relationships between patients and staff as a marker of success. 26 In another study interviewing clinicians and leaders across 12 intensive outpatient programmes, three key facilitators of patient engagement emerged: (1) financial assistance and other resources to help meet basic needs, (2) working as a multi-disciplinary care team and (3) adequate time and resources to develop close relationships focused on patient goals. 27 Our results concur on the importance of a multi-disciplinary approach, establishing trusting relationships, and pursuing patient-centred goals. Our results diverge on the role of resources to meet basic needs. Case managers in our study indicated that while connections to social services benefits and other resources help initiate the case manager-patient relationship, lasting success involved longer-term relationships in which they supported patients in developing patients’ own goal setting skills and motivation.
An important takeaway from case managers’ definitions of success is the ‘how’ they go about their work, in contrast to the ‘what’ of particular care coordination activities. For example, case managers emphasise interpersonal approaches such as empathy and respect over specific processes and resource availability. Primary care clinicians, too, have expressed how standard HEDIS or CAHPS quality metrics fail to capture, and in some cases disincentivise, the intuitions in their work that are important for high quality care. 28 29 Complex care management programmes must also wrestle with this challenge of identifying standards without extinguishing underlying quality constructs.
Strengths and limitations
This study brings several strengths, including bringing to light the unique, unexplored perspective of case managers working on both health and social needs with patients facing diverse circumstances that contribute to high-risk of future hospital or emergency department utilisation. The fact that our study explores perspectives across an array of case manager disciplines is also a strength, however a limitation is that we are unable to distinguish how success differed by discipline based on smaller numbers of each discipline in this study sample. Other study limitations include generalisability to other settings, given that all case managers worked for a single large-scale social needs case management programme. Comments around productivity concerns or interdisciplinary perspectives on ways to support patients may be unique to the infrastructure or management of this organisation. In addition, at the time of the study, all case managers were able to meet with patients in-person; future studies may explore whether definitions of success change when interactions become virtual or telephonic as occurred amidst COVID-19 concerns.
This study is the first to our knowledge to inquire about holistic patient success from the perspective of case managers in the context of a social needs case management programme. The findings offer important implications for researchers as well as policy makers and managers who are designing complex case management programmes.
Our results identify patient-directed goals, stability and satisfaction, as aspects of social needs case management which are difficult to measure but nonetheless critical to fostering health and well-being. Case managers indicated these aspects are most likely to emerge through a longer-term connection with their patients. Thus, while resource-referral solutions may play an important role in addressing basic needs, 30 our findings suggest that weak patient–referrer rapport may be a limitation for such lighter touch interventions. The need for sustained rapport building is also one explanation why longer time horizons may be necessary to show outcome improvements in rigorous studies. 16
Relatedly, results point to trusting relationships as an under-recognised and understudied feature of social needs case management. Existing research finds that patients’ trust in their primary care physician is associated with greater self-reported medication adherence 31 along with health behaviours such as exercise and smoking cessation. 32 Similar quantitative results have not yet been illuminated in social needs case management contexts, yet the prominence of trusting relationships in this study as well as other sources 26 27 33 34 suggests that measures of trust should be used to complement currently emphasised outcomes such as inpatient and outpatient utilisation. Future research and programme evaluation will need to develop new trust measurement or modify existing trust measures for the social needs case management context. 31 35
In summary, study themes provide waypoints of how to conceptualise programme design, new staff training and potential measurement development for complex case management programmes like CommunityConnect. Despite the broad swath of social needs addressed, case managers coalesced on establishing a trusting relationship as a necessary foundation to appropriately identify needs and facilitate connections. Second, fostering patients’ own ideas, including a change their mindset or initiative, was important to fully make use of programme resources. Third, supporting new-found independence or stability was a gratifying, but not universally achieved marker of success. Commonly, case managers highlighted moments of success with mindfulness toward small victories, illuminating that success is non-linear with no certain path nor single end point. Themes emphasise the importance of bringing compassion for the complexity in patients’ lives and developing collaborative relationships one interaction at a time.
Acknowledgments
The authors would like to thank the CommunityConnect evaluation team for their support conducting and transcribing interviews and applying preliminary coding, especially Gabriella Quintana, Alison Stribling, Julia Surges and Camella Taylor.
Contributors: MK coded and analysed qualitative data, identified key themes and related discussion areas, and drafted and critically revised the manuscript. EEE conducted interviews, coded and analysed qualitative data, and drafted and critically revised the manuscript. EH developed the study instrument, conducted interviews, supervised data collection, contributed to the data interpretation and critically revised the manuscript. MDF contributed to the interpretation and critically revised the manuscript. NS contributed to the interpretation and critically revised the manuscript. ALB contributed to the design and interpretation and critically revised the manuscript. All authors approve of the final version to be published.
Funding: MK was supported by the Agency for Healthcare Research and Quality (AHRQ) under the Ruth L. Kirschstein National Research Service Award T32 (T32HS022241). MDF was supported by the Agency for Healthcare Research and Quality, grant # K01HS027648.
Disclaimer: Its contents are solely the responsibility of the authors and do not necessarily represent the official views of AHRQ. Funding had no role in the study’s design, conduct or reporting.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement
Ethics statements, patient consent for publication.
Not applicable.
Ethics approval
This study involves human participants and was approved by Contra Costa Regional Medical Center and Health Centers Institutional Review Committee (Protocol 12-17-2018). Participants gave informed consent to participate in the study before taking part.

COMMENTS
Introduction. The popularity of case study research methodology in Health Services Research (HSR) has grown over the past 40 years. 1 This may be attributed to a shift towards the use of implementation research and a newfound appreciation of contextual factors affecting the uptake of evidence-based interventions within diverse settings. 2 Incorporating context-specific information on the ...
Case study is a research methodology, typically seen in social and life sciences. There is no one definition of case study research.1 However, very simply… 'a case study can be defined as an intensive study about a person, a group of people or a unit, which is aimed to generalize over several units'.1 A case study has also been described as an intensive, systematic investigation of a ...
The case study approach allows in-depth, multi-faceted explorations of complex issues in their real-life settings. The value of the case study approach is well recognised in the fields of business, law and policy, but somewhat less so in health services research. Based on our experiences of conducting several health-related case studies, we reflect on the different types of case study design ...
The Design of Case Study Research in Health Care (DESCARTE) model suggests a series of questions to be asked of a case study researcher (including clarity about the philosophy underpinning their research), study design (with a focus on case definition) and analysis (to improve process). The model resembles toolkits for enhancing the quality and ...
By proposing, peer-reviewing and reading the Case Studies, you and your fellow physicians could gain a broader understanding of clinical diagnoses, treatments and outcomes. In this light, then ...
Felicity Hasson is a Senior Lecturer in the Institute of Nursing Research at the University of Ulster with 20 years' experience in research. A social researcher by background, she has extensive experience and knowledge of qualitative, quantitative and mixed method research and has been involved in numerous research studies in palliative and end-of-life care.
Case studies are good for describing, comparing, evaluating and understanding different aspects of a research problem. Table of contents. When to do a case study. Step 1: Select a case. Step 2: Build a theoretical framework. Step 3: Collect your data. Step 4: Describe and analyze the case.
Using this case study, we demonstrate how to apply evidence-based processes to healthcare improvement and embed real-world research for optimising healthcare improvement. ... The important success factors and lessons from stroke as a national exemplar LHS in ... Teede, H., Cadilhac, D.A., Purvis, T. et al. Learning together for better health ...
A case study method provides a holistic approach to everyday events with several benefits: Allows for flexibility depending on the context of the real-world situation. Aids in connecting research and theory to practice. Provides problem-solving skills applicable to practice. Immerses the learner in complex clinical realities.
Writing a case. Farooqui, S., 2021. A Short Guide to Writing and Teaching Inclusive Cases, Harvard T.H. Chan School of Public Health. Developed by 2020-2021 Harvard Chan Equity, Diversity, and Inclusion Fellow Sana Farooqui (MPH 2021), this guide provides suggestions for case writers and course instructors on writing and selecting cases ...
Case studies allow for a more comprehensive understanding of the complexities of health-care delivery and patient outcomes, enabling practitioners to make more informed decisions and ultimately improve patient care. By examining the benefits and drawbacks of various approaches, case studies play a vital role in shaping the direction of health care.
Organisational change in health systems is common. Success is often tied to the actors involved, including their awareness of the change, personal engagement and ownership of it. In many health systems, one of the most common changes we are witnessing is the redevelopment of long-standing hospitals. However, we know little about how hospital staff understand and experience such potentially far ...
Prior to the case studies, the AIR research team conducted a review of the literature to determine whether an evidence base exists for using Lean in health care. We found that the majority of studies about Lean lack data on key areas and domains important for understanding quality improvement, organizational behavior, and organizational change.
This study provides an in-depth understanding of psychological safety within four healthcare teams working in the same case study hospital. It addresses recent calls for the use of multiple methods to capture a more accurate and nuanced understanding of psychological safety in healthcare teams [8, 10]. While survey results from each team ...
Context: Health work forces globally are needing to reorganise and reconfigure in order to meet the challenges posed by the increased numbers of people living with long-term conditions in an efficient and sustainable manner.Through studying the introduction of General Practitioners with a Special Interest in respiratory disorders, this study aimed to provide insights into this important issue ...
Ongoing education is a core aspect of healthcare delivery at Central Adelaide Local Health Network (CALHN). But with busy schedules and only so many hours in the day, it can be challenging for clinicians to keep up-to-date with all the specialist areas of health. That's why published patient case studies are so valuable.
5. Build Your Self-Confidence. Finally, learning through the case study method can build your confidence. Each time you assume a business leader's perspective, aim to solve a new challenge, and express and defend your opinions and decisions to peers, you prepare to do the same in your career. According to a 2022 City Square Associates survey ...
Case study is a research methodology, typically seen in social and life sciences. There is no one definition of case study research.1However, very simply… 'a case study can be defined as an intensive study about a person, a group of people or a unit, which is aimed to generalize over several units'.1A case study has also been described as ...
Case management in healthcare plays several important roles, such as reducing the length of patients' stay in the health facilities, decreasing the readmission rates, reducing wasteful utilization ...
Introduction. Medical and health care-related education is currently changing. Since the advent of adult education, educators have realized that learners need to see the relevance and be actively engaged in the topic under study. 1 Traditionally, students in health care went to lectures and then transitioned into patient care as a type of on-the-job training.
By leveraging technology, healthcare providers have successfully expanded access to care for patients who would otherwise have to travel long distances for treatment. Lessons learned include the importance of investing in reliable technology and training staff to effectively use telemedicine platforms. Another critical case study involves the ...
A. Root Cause Analysis is a systematic approach used in the healthcare setting to identify the underlying cause of an incident or issue and contributing factors to help prevent future occurrences (Institute for Healthcare Improvement [IHI], n.d.). 1. Identify what happened: 2. Determine what should have happened: 3. Determine causes ("Ask why five times"): 4.
Although the UK case provided the first proof-of-principle study, our findings add novel and unique insights and important updates. This case study reports the first high-resolution cases of meningoencephalitis associated with persistence of Ebola virus in the CNS in two survivors of Ebola virus disease in an African setting (in which all known ...
A former UTV broadcaster has been sharing the story of his battle with Chronic Lymphocytic Leukemia, a type of blood cancer, to highlight the importance of supporting local medical research funded ...
The popularity of case study research methodology in Health Services Research (HSR) has grown over the past 40 years. 1 This may be attributed to a shift towards the use of implementation research and a newfound appreciation of contextual factors affecting the uptake of evidence-based interventions within diverse settings. 2 Incorporating context-specific information on the delivery and ...
The built environment, as a critical factor influencing residents' cardiovascular health, has a significant potential impact on the incidence of cardiovascular diseases (CVDs). Taking Xixiangtang District in Nanning City, Guangxi Zhuang Autonomous Region of China as a case study, we utilized the geographic location information of CVD patients, detailed road network data, and urban points of ...
Mental health is an important aspect of healthy aging, especially for widowed older adults. This study aims to examine the interrelationships between depression and anxiety symptoms and their associations with quality of life among widowed older adults. Using data from the 2017-2018 Chinese Longitudinal Healthy Longevity Survey (CLHLS), we selected a sample of 6,061 widowed older adults (M ...
The 145-page decision constitutes the most important precedent and largest award in Delaware history in an earnout case. The dispute stemmed from J&J's acquisition of Auris Health in 2019 and its subsequent actions ensuring that the milestones set forth in the merger agreement would not be achieved, and thus that $2.35 billion of the merger ...
By prioritizing WASH, Kandy District can make significant strides towards improving health outcomes and ensuring that all community members have access to safe and sanitary healthcare facilities.Implementing the recommendations outlined in the developed case study will therefore undoubtedly require the commitment and collaboration of all ...
In some contexts, case managers or navigators providing social needs assistance can improve health 2 and reduce costly hospital use. 3-5 Yet systematic reviews also report mixed results for measures of health and well-being, hospitalisation and emergency department use, and overall healthcare costs. 6-9 Notably, a randomised trial of the ...