Nicotine Addiction From Vaping Is a Bigger Problem Than Teens Realize
March 19, 2019

Data show clearly that young people are vaping in record numbers. And despite the onslaught of reports and articles highlighting not only its dangers but the marketing tactics seemingly aimed to hook teens and young adults, the number of vaping users continues to climb.
These teens may be overlooking (or underestimating) a key ingredient in the vapors they inhale: nicotine. Though it’s possible to buy liquid or pod refills without nicotine, the truth is you have to look much harder to find them. Teens may not realize that nicotine is deeply addictive. What’s more, studies show that young people who vape are far likelier to move on to cigarettes, which cause cancer and other diseases.

So, why is nicotine so addictive for teens?
Nicotine can spell trouble at any life stage, but it is particularly dangerous before the brain is fully developed, which happens around age 25.
“Adolescents don’t think they will get addicted to nicotine, but when they do want to stop, they find it’s very difficult,” says Yale neuroscientist Marina Picciotto, PhD, who has studied the basic science behind nicotine addiction for decades. A key reason for this is that “the adolescent brain is more sensitive to rewards,” she explains.
The reward system, called the mesolimbic dopamine system, is one of the more primitive parts of the brain. It developed as a positive reinforcement for behavior we need to survive, like eating. Because the mechanism is so engrained in the brain, it is especially hard to resist.
When a teen inhales vapor laced with nicotine, the drug is quickly absorbed through the blood vessels lining the lungs. It reaches the brain in about 10 seconds. There, nicotine particles fit lock-and-key into a type of acetylcholine receptor located on neurons (nerve cells) throughout the brain.
The unique attributes that make nicotine cravings persist
“Nicotine, alcohol, heroin, or any drug of abuse works by hijacking the brain’s reward system,” says Yale researcher Nii Addy, PhD, who specializes in the neurobiology of addiction. The reward system wasn’t meant for drugs—it evolved to interact with natural neurotransmitters already present in the body, like acetylcholine. This neurotransmitter is used to activate muscles in our body. The reason nicotine fits into a receptor meant for acetylcholine is because the two have very similar shapes, biochemically speaking, Addy explains.
Once nicotine binds to that receptor, it sends a signal to the brain to release a well-known neurotransmitter—dopamine—which helps create a ‘feel-good’ feeling. Dopamine is part of the brain’s feedback system that says “whatever just happened felt good” and trains the brain to repeat the action. But nicotine, unlike other drugs such as alcohol, quickly leaves the body once it is broken down by the liver. Once it’s gone, the brain craves nicotine again.
When an addicted teen tries to quit nicotine, the problem of cravings is of course tied to the drug that causes the dopamine rush, Addy says. What’s more, recent animal study research and human brain imaging studies have shown that “environmental cues, especially those associated with drug use, can change dopamine concentrations in the brain,” he says. This means that simply seeing a person you vape with, or visiting a school restroom—where teens say they vape during the school day—can unleash intense cravings. “In the presence of these cues, it’s difficult not to relapse,” Addy says.
Physical changes caused by nicotine
Nicotine can also cause physical changes in the brain, some temporary, and others that some researchers, like Picciotto, worry could be long-lasting.
Decades of cigarette smoking research have shown that, in the short term, the number of acetylcholine receptors in the brain increases as the brain is continuously exposed to nicotine. The fact that there are more of these receptors may make nicotine cravings all the more intense. However, those same studies found that the number of receptors decreases after the brain is no longer exposed to nicotine, meaning that these changes can be reversed.
But animal studies show nicotine also can cause issues with brain function, leading to problems with focus, memory, and learning—and these may be long-lasting. In animals, nicotine can cause a developing brain to have an increased number of connections between cells in the cerebral cortex region, says Picciotto. “If this is also true for humans, the increased connections would interfere with a person’s cognitive abilities,” Picciotto says.
To illustrate how this might work, Picciotto gives an example. A student sitting in a noisy classroom, with traffic passing by the window, needs to be able to focus her attention away from the distracting sounds so she can understand what the teacher says. “Brains not exposed to nicotine learn to decrease connections, and refinement within the brain can happen efficiently,” Picciotto says. “But when you flood the system with nicotine, this refinement doesn’t happen as efficiently.”
“There’s hope that the current vaping epidemic won’t lead to major health problems like lung cancer or pulmonary disease,” Picciotto says. “But we may still see an epidemic of cognitive function problems and attention problems. The changes made in the brain could persist.”
Vaping vs. regular cigarettes
Weighing the pros and cons of vaping versus smoking is difficult to do. On the one hand, e-cigarettes likely do not produce 7,000 chemicals—some of which cause cancer—when they are activated, like regular combustible cigarettes do. However, the aerosol from a vape device has not been proven safe. Studies have found that it contains lead and volatile organic compounds, some of which are linked to cancer. Researchers are still gathering data on the possible long-term health effects from vaping. It’s notable that e-cigarettes have not been approved by the Food and Drug Administration (FDA) as smoking cessation devices. However, e-cigarettes may be a better choice for adult smokers if they completely replace smoking, according to the Centers for Disease Control and Prevention (CDC).
But where nicotine levels are concerned, a newer and popular type of vape device, called a “pod mod,” outcompetes many other e-cigarette devices. The form of nicotine in these pods is estimated to be 2 to 10 times more concentrated than most free-base nicotine found in other vape liquids. A single pod from one vape manufacturer contains 0.7 mL of nicotine, which is about the same as 20 regular cigarettes.
Despite its extremely addictive nature, people can successfully quit using nicotine with personalized approaches, especially under the guidance of physicians who understand addiction.
For young people, intervening early in a vaping habit could make an important difference in the quality of life they have throughout their adult years. It could also mean they won’t become part of next year’s statistics.
More news from Yale Medicine

Nicotine Addiction Essays
Nicotine-containing products, exploring the safety of e-cigarette vaping among youth: a critical examination, popular essay topics.
- American Dream
- Artificial Intelligence
- Black Lives Matter
- Bullying Essay
- Career Goals Essay
- Causes of the Civil War
- Child Abusing
- Civil Rights Movement
- Community Service
- Cultural Identity
- Cyber Bullying
- Death Penalty
- Depression Essay
- Domestic Violence
- Freedom of Speech
- Global Warming
- Gun Control
- Human Trafficking
- I Believe Essay
- Immigration
- Importance of Education
- Israel and Palestine Conflict
- Leadership Essay
- Legalizing Marijuanas
- Mental Health
- National Honor Society
- Police Brutality
- Pollution Essay
- Racism Essay
- Romeo and Juliet
- Same Sex Marriages
- Social Media
- The Great Gatsby
- The Yellow Wallpaper
- Time Management
- To Kill a Mockingbird
- Violent Video Games
- What Makes You Unique
- Why I Want to Be a Nurse
- Send us an e-mail
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Published: 24 March 2022
Tobacco and nicotine use
- Bernard Le Foll 1 , 2 ,
- Megan E. Piper 3 , 4 ,
- Christie D. Fowler 5 ,
- Serena Tonstad 6 ,
- Laura Bierut 7 ,
- Lin Lu ORCID: orcid.org/0000-0003-0742-9072 8 , 9 ,
- Prabhat Jha 10 &
- Wayne D. Hall 11 , 12
Nature Reviews Disease Primers volume 8 , Article number: 19 ( 2022 ) Cite this article
38k Accesses
86 Citations
106 Altmetric
Metrics details
- Disease genetics
- Experimental models of disease
- Preventive medicine
Tobacco smoking is a major determinant of preventable morbidity and mortality worldwide. More than a billion people smoke, and without major increases in cessation, at least half will die prematurely from tobacco-related complications. In addition, people who smoke have a significant reduction in their quality of life. Neurobiological findings have identified the mechanisms by which nicotine in tobacco affects the brain reward system and causes addiction. These brain changes contribute to the maintenance of nicotine or tobacco use despite knowledge of its negative consequences, a hallmark of addiction. Effective approaches to screen, prevent and treat tobacco use can be widely implemented to limit tobacco’s effect on individuals and society. The effectiveness of psychosocial and pharmacological interventions in helping people quit smoking has been demonstrated. As the majority of people who smoke ultimately relapse, it is important to enhance the reach of available interventions and to continue to develop novel interventions. These efforts associated with innovative policy regulations (aimed at reducing nicotine content or eliminating tobacco products) have the potential to reduce the prevalence of tobacco and nicotine use and their enormous adverse impact on population health.
Similar content being viewed by others

Associations between classic psychedelics and nicotine dependence in a nationally representative sample
Use of electronic cigarettes and heated tobacco products during the covid-19 pandemic.
Smoking cessation behaviors and reasons for use of electronic cigarettes and heated tobacco products among Romanian adults
Introduction.
Tobacco is the second most commonly used psychoactive substance worldwide, with more than one billion smokers globally 1 . Although smoking prevalence has reduced in many high-income countries (HICs), tobacco use is still very prevalent in low-income and middle-income countries (LMICs). The majority of smokers are addicted to nicotine delivered by cigarettes (defined as tobacco dependence in the International Classification of Diseases, Tenth Revision (ICD-10) or tobacco use disorder in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5)). As a result of the neuro-adaptations and psychological mechanisms caused by repeated exposure to nicotine delivered rapidly by cigarettes, cessation can also lead to a well-characterized withdrawal syndrome, typically manifesting as irritability, anxiety, low mood, difficulty concentrating, increased appetite, insomnia and restlessness, that contributes to the difficulty in quitting tobacco use 2 , 3 , 4 .
Historically, tobacco was used in some cultures as part of traditional ceremonies, but its use was infrequent and not widely disseminated in the population. However, since the early twentieth century, the use of commercial cigarettes has increased dramatically 5 because of automated manufacturing practices that enable large-scale production of inexpensive products that are heavily promoted by media and advertising. Tobacco use became highly prevalent in the past century and was followed by substantial increases in the prevalence of tobacco-induced diseases decades later 5 . It took decades to establish the relationship between tobacco use and associated health effects 6 , 7 and to discover the addictive role of nicotine in maintaining tobacco smoking 8 , 9 , and also to educate people about these effects. It should be noted that the tobacco industry disputed this evidence to allow continuing tobacco sales 10 . The expansion of public health campaigns to reduce smoking has gradually decreased the use of tobacco in HICs, with marked increases in adult cessation, but less progress has been achieved in LMICs 1 .
Nicotine is the addictive compound in tobacco and is responsible for continued use of tobacco despite harms and a desire to quit, but nicotine is not directly responsible for the harmful effects of using tobacco products (Box 1 ). Other components in tobacco may modulate the addictive potential of tobacco (for example, flavours and non-nicotine compounds) 11 . The major harms related to tobacco use, which are well covered elsewhere 5 , are linked to a multitude of compounds present in tobacco smoke (such as carcinogens, toxicants, particulate matter and carbon monoxide). In adults, adverse health outcomes of tobacco use include cancer in virtually all peripheral organs exposed to tobacco smoke and chronic diseases such as eye disease, periodontal disease, cardiovascular diseases, chronic obstructive pulmonary disease, stroke, diabetes mellitus, rheumatoid arthritis and disorders affecting immune function 5 . Moreover, smoking during pregnancy can increase the risk of adverse reproductive effects, such as ectopic pregnancy, low birthweight and preterm birth 5 . Exposure to secondhand cigarette smoke in children has been linked to sudden infant death syndrome, impaired lung function and respiratory illnesses, in addition to cognitive and behavioural impairments 5 . The long-term developmental effects of nicotine are probably due to structural and functional changes in the brain during this early developmental period 12 , 13 .
Nicotine administered alone in various nicotine replacement formulations (such as patches, gum and lozenges) is safe and effective as an evidence-based smoking cessation aid. Novel forms of nicotine delivery systems have also emerged (called electronic nicotine delivery systems (ENDS) or e-cigarettes), which can potentially reduce the harmful effects of tobacco smoking for those who switch completely from combustible to e-cigarettes 14 , 15 .
This Primer focuses on the determinants of nicotine and tobacco use, and reviews the neurobiology of nicotine effects on the brain reward circuitry and the functioning of brain networks in ways that contribute to the difficulty in stopping smoking. This Primer also discusses how to prevent tobacco use, screen for smoking, and offer people who smoke tobacco psychosocial and pharmacological interventions to assist in quitting. Moreover, this Primer presents emerging pharmacological and novel brain interventions that could improve rates of successful smoking cessation, in addition to public health approaches that could be beneficial.
Box 1 Tobacco products
Conventional tobacco products include combustible products that produce inhaled smoke (most commonly cigarettes, bidis (small domestically manufactured cigarettes used in South Asia) or cigars) and those that deliver nicotine without using combustion (chewing or dipping tobacco and snuff). Newer alternative products that do not involve combustion include nicotine-containing e-cigarettes and heat-not-burn tobacco devices. Although non-combustion and alternative products may constitute a lesser risk than burned ones 14 , 15 , 194 , no form of tobacco is entirely risk-free.
Epidemiology
Prevalence and burden of disease.
The Global Burden of Disease Project (GBDP) estimated that around 1.14 billion people smoked in 2019, worldwide, increasing from just under a billion in 1990 (ref. 1 ). Of note, the prevalence of smoking decreased significantly between 1990 and 2019, but increases in the adult population meant that the total number of global smokers increased. One smoking-associated death occurs for approximately every 0.8–1.1 million cigarettes smoked 16 , suggesting that the estimated worldwide consumption of about 7.4 trillion cigarettes in 2019 has led to around 7 million deaths 1 .
In most populations, smoking prevalence is much higher among groups with lower levels of education or income 17 and among those with mental health disorders and other co-addictions 18 , 19 . Smoking is also more frequent among men than women (Figs 1 – 3 ). Sexual and/or gender minority individuals have disproportionately high rates of smoking and other addictions 17 , 20 . In addition, the prevalence of smoking varies substantially between regions and ethnicities; smoking rates are high in some regions of Asia, such as China and India, but are lower in North America and Australia. Of note, the prevalence of mental health disorders and other co-addictions is higher in individuals who smoke compared with non-smokers 18 , 19 , 21 . For example, the odds of smoking in people with any substance use disorder is more than five times higher than the odds in people without a substance use disorder 19 . Similarly, the odds of smoking in people with any psychiatric disorder is more than three times higher than the odds of smoking in those without a psychiatric diagnosis 22 . In a study in the USA, compared with a population of smokers with no psychiatric diagnosis, subjects with anxiety, depression and phobia showed an approximately twofold higher prevalence of smoking, and subjects with agoraphobia, mania or hypomania, psychosis and antisocial personality or conduct disorders showed at least a threefold higher prevalence of smoking 22 . Comorbid disorders are also associated with higher rates of smoking 22 , 23 .
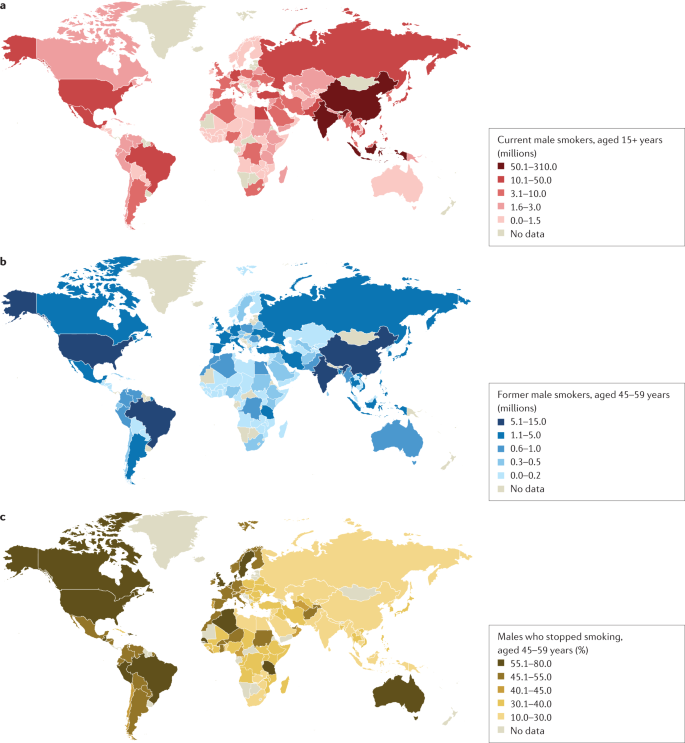
a | Number of current male smokers aged 15 years or older per country expressed in millions. b | Former male smokers aged 45–59 years per country expressed in millions. c | Former male smokers aged 45–59 years per country expressed as the percentage of smokers who stopped. The data shown are for male smokers for the period 2015–2019 from countries with direct smoking surveys. The prevalence of smoking among males is less variable than among females. Data from ref. 1 .
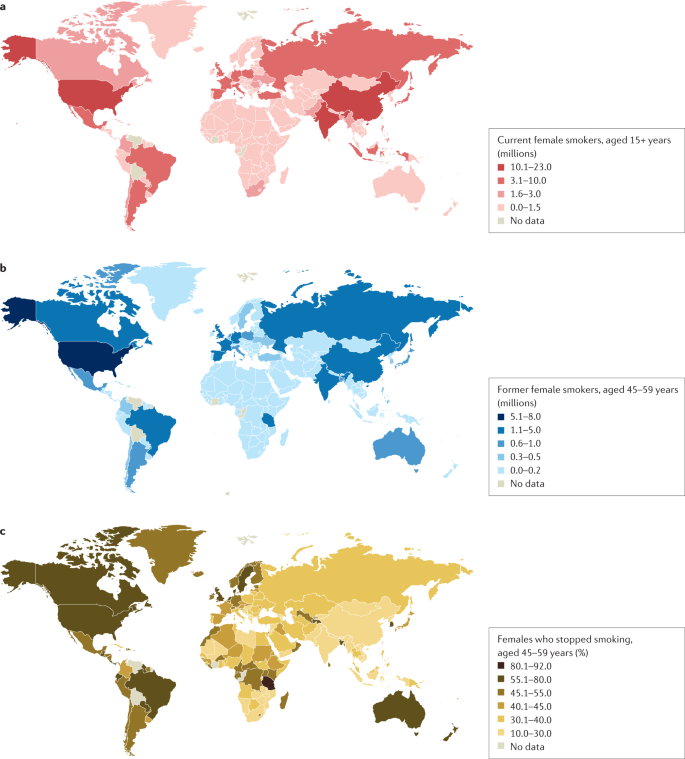
a | Number of current female smokers aged 15 years or older per country expressed in millions. b | Former female smokers aged 45–59 years per country expressed in millions. c | Former female smokers aged 45–59 years per country expressed as the percentage of smokers who stopped. The data shown are for female smokers for the period 2015–2019 from countries with direct smoking surveys. The prevalence of smoking among females is much lower in East and South Asia than in Latin America or Eastern Europe. Data from ref. 1 .
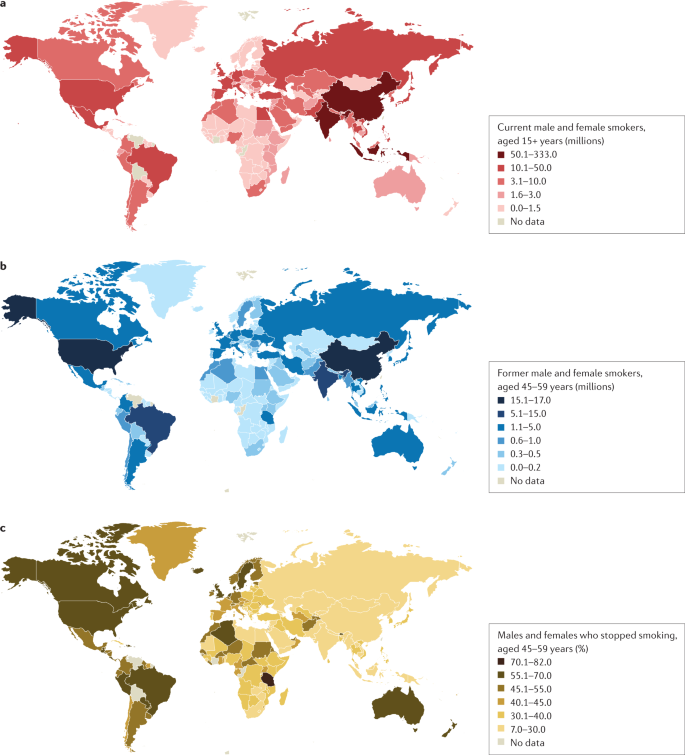
a | Number of current male and female smokers aged 15 years or older per country expressed in millions. b | Former male and female smokers aged 45–59 years per country expressed in millions. c | Former male and female smokers aged 45–59 years per country expressed as the percentage of smokers who stopped. The data shown are for the period 2015–2019 from countries with direct smoking surveys. Cessation rates are higher in high-income countries, but also notably high in Brazil. Cessation is far less common in South and East Asia and Russia and other Eastern European countries, and also low in South Africa. Data from ref. 1 .
Age at onset
Most smokers start smoking during adolescence, with almost 90% of smokers beginning between 15 and 25 years of age 24 . The prevalence of tobacco smoking among youths substantially declined in multiple HICs between 1990 and 2019 (ref. 25 ). More recently, the widespread uptake of ENDS in some regions such as Canada and the USA has raised concerns about the long-term effects of prolonged nicotine use among adolescents, including the possible notion that ENDS will increase the use of combustible smoking products 25 , 26 (although some studies have not found much aggregate effect at the population level) 27 .
Smoking that commences in early adolescence or young adulthood and persists throughout life has a more severe effect on health than smoking that starts later in life and/or that is not persistent 16 , 28 , 29 . Over 640 million adults under 30 years of age smoke in 22 jurisdictions alone (including 27 countries in the European Union where central efforts to reduce tobacco dependence might be possible) 30 . In those younger than 30 years of age, at least 320 million smoking-related deaths will occur unless they quit smoking 31 . The actual number of smoking-related deaths might be greater than one in two, and perhaps as high as two in three, long-term smokers 5 , 16 , 29 , 32 , 33 . At least half of these deaths are likely to occur in middle age (30–69 years) 16 , 29 , leading to a loss of two or more decades of life. People who smoke can expect to lose an average of at least a decade of life versus otherwise similar non-smokers 16 , 28 , 29 .
Direct epidemiological studies in several countries paired with model-based estimates have estimated that smoking tobacco accounted for 7.7 million deaths globally in 2020, of which 80% were in men and 87% were current smokers 1 . In HICs, the major causes of tobacco deaths are lung cancer, emphysema, heart attack, stroke, cancer of the upper aerodigestive areas and bladder cancer 28 , 29 . In some lower income countries, tuberculosis is an additional important cause of tobacco-related death 29 , 34 , which could be related to, for example, increased prevalence of infection, more severe tuberculosis/mortality and higher prevalence of treatment-resistant tuberculosis in smokers than in non-smokers in low-income countries 35 , 36 .
Despite substantial reductions in the prevalence of smoking, there were 34 million smokers in the USA, 7 million in the UK and 5 million in Canada in 2017 (ref. 16 ), and cigarette smoking remains the largest cause of premature death before 70 years of age in much of Europe and North America 1 , 16 , 28 , 29 . Smoking-associated diseases accounted for around 41 million deaths in the USA, UK and Canada from 1960 to 2020 (ref. 16 ). Moreover, as smoking-associated diseases are more prevalent among groups with lower levels of education and income, smoking accounts for at least half of the difference in overall mortality between these social groups 37 . Any reduction in smoking prevalence reduces the absolute mortality gap between these groups 38 .
Smoking cessation has become common in HICs with good tobacco control interventions. For example, in France, the number of ex-smokers is four times the number of current smokers among those aged 50 years or more 30 . By contrast, smoking cessation in LMICs remains uncommon before smokers develop tobacco-related diseases 39 . Smoking cessation greatly reduces the risks of smoking-related diseases. Indeed, smokers who quit smoking before 40 years of age avoid nearly all the increased mortality risks 31 , 33 . Moreover, individuals who quit smoking by 50 years of age reduce the risk of death from lung cancer by about two-thirds 40 . More modest hazards persist for deaths from lung cancer and emphysema 16 , 28 ; however, the risks among former smokers are an order of magnitude lower than among those who continue to smoke 33 .
Mechanisms/pathophysiology
Nicotine is the main psychoactive agent in tobacco and e-cigarettes. Nicotine acts as an agonist at nicotinic acetylcholine receptors (nAChRs), which are localized throughout the brain and peripheral nervous system 41 . nAChRs are pentameric ion channels that consist of varying combinations of α 2 –α 7 and β 2 –β 4 subunits, and for which acetylcholine (ACh) is the endogenous ligand 42 , 43 , 44 . When activated by nicotine binding, nAChR undergoes a conformational change that opens the internal pore, allowing an influx of sodium and calcium ions 45 . At postsynaptic membranes, nAChR activation can lead to action potential firing and downstream modulation of gene expression through calcium-mediated second messenger systems 46 . nAChRs are also localized to presynaptic membranes, where they modulate neurotransmitter release 47 . nAChRs become desensitized after activation, during which ligand binding will not open the channel 45 .
nAChRs with varying combinations of α-subunits and β-subunits have differences in nicotine binding affinity, efficacy and desensitization rate, and have differential expression depending on the brain region and cell type 48 , 49 , 50 . For instance, at nicotine concentrations found in human smokers, β 2 -containing nAChRs desensitize relatively quickly after activation, whereas α 7 -containing nAChRs have a slower desensitization profile 48 . Chronic nicotine exposure in experimental animal models or in humans induces an increase in cortical expression of α 4 β 2 -containing nAChRs 51 , 52 , 53 , 54 , 55 , but also increases the expression of β 3 and β 4 nAChR subunits in the medial habenula (MHb)–interpeduncular nucleus (IPN) pathway 56 , 57 . It is clear that both the brain localization and the type of nAChR are critical elements in mediating the various effects of nicotine, but other factors such as rate of nicotine delivery may also modulate addictive effects of nicotine 58 .
Neurocircuitry of nicotine addiction
Nicotine has both rewarding effects (such as a ‘buzz’ or ‘high’) and aversive effects (such as nausea and dizziness), with the net outcome dependent on dose and others factors such as interindividual sensitivity and presence of tolerance 59 . Thus, the addictive properties of nicotine involve integration of contrasting signals from multiple brain regions that process reward and aversion (Fig. 4 ).
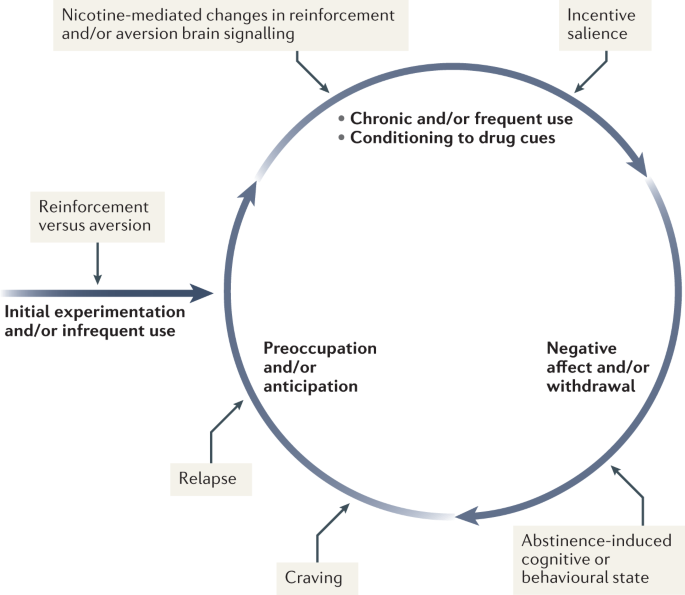
During initial use, nicotine exerts both reinforcing and aversive effects, which together determine the likelihood of continued use. As the individual transitions to more frequent patterns of chronic use, nicotine induces pharmacodynamic changes in brain circuits, which is thought to lead to a reduction in sensitivity to the aversive properties of the drug. Nicotine is also a powerful reinforcer that leads to the conditioning of secondary cues associated with the drug-taking experience (such as cigarette pack, sensory properties of cigarette smoke and feel of the cigarette in the hand or mouth), which serves to enhance the incentive salience of these environmental factors and drive further drug intake. When the individual enters into states of abstinence (such as daily during sleep at night or during quit attempts), withdrawal symptomology is experienced, which may include irritability, restlessness, learning or memory deficits, difficulty concentrating, anxiety and hunger. These negative affective and cognitive symptoms lead to an intensification of the individual’s preoccupation to obtain and use the tobacco/nicotine product, and subsequently such intense craving can lead to relapse.
The rewarding actions of nicotine have largely been attributed to the mesolimbic pathway, which consists of dopaminergic neurons in the ventral tegmental area (VTA) that project to the nucleus accumbens and prefrontal cortex 60 , 61 , 62 (Fig. 5 ). VTA integrating circuits and projection regions express several nAChR subtypes on dopaminergic, GABAergic, and glutamatergic neurons 63 , 64 . Ultimately, administration of nicotine increases dopamine levels through increased dopaminergic neuron firing in striatal and extrastriatal areas (such as the ventral pallidum) 65 (Fig. 6 ). This effect is involved in reward and is believed to be primarily mediated by the action of nicotine on α 4 -containing and β 2 -containing nAChRs in the VTA 66 , 67 .
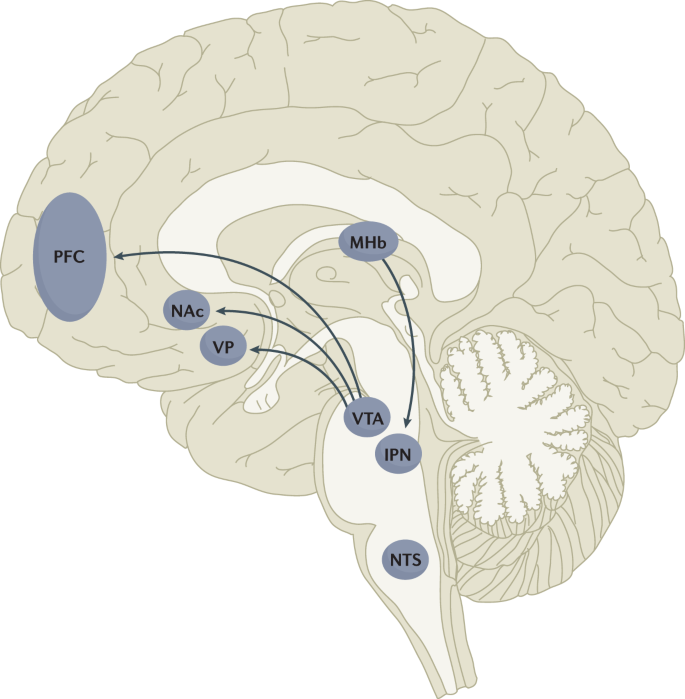
Multiple lines of research have demonstrated that nicotine reinforcement is mainly controlled by two brain pathways, which relay predominantly reward-related or aversion-related signals. The rewarding properties of nicotine that promote drug intake involve the mesolimbic dopamine projection from the ventral tegmental area (VTA) to the nucleus accumbens (NAc). By contrast, the aversive properties of nicotine that limit drug intake and mitigate withdrawal symptoms involve the fasciculus retroflexus projection from the medial habenula (MHb) to the interpeduncular nucleus (IPN). Additional brain regions have also been implicated in various aspects of nicotine dependence, such as the prefrontal cortex (PFC), ventral pallidum (VP), nucleus tractus solitarius (NTS) and insula (not shown here for clarity). All of these brain regions are directly or indirectly interconnected as integrative circuits to drive drug-seeking and drug-taking behaviours.
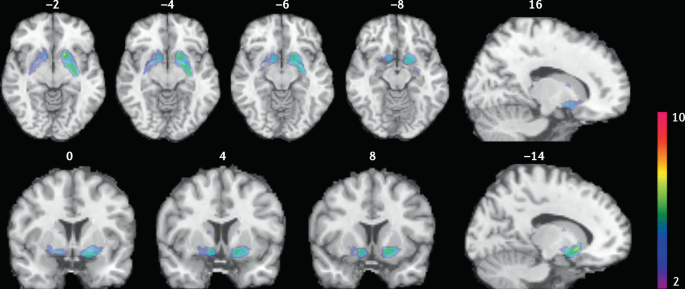
Smokers received brain PET scans with [ 11 C]PHNO, a dopamine D 2/3 PET tracer that has high sensitivity in detecting fluctuations of dopamine. PET scans were performed during abstinence or after smoking a cigarette. Reduced binding potential (BP ND ) was observed after smoking, indicating increased dopamine levels in the ventral striatum and in the area that corresponds to the ventral pallidum. The images show clusters with statistically significant decreases of [ 11 C]PHNO BP ND after smoking a cigarette versus abstinence condition. Those clusters have been superimposed on structural T1 MRI images of the brain. Reprinted from ref. 65 , Springer Nature Limited.
The aversive properties of nicotine are mediated by neurons in the MHb, which project to the IPN. Studies in rodents using genetic knockdown and knockout strategies demonstrated that the α 5 -containing, α 3 -containing and β 4 -containing nAChRs in the MHb–IPN pathway mediate the aversive properties of nicotine that limit drug intake, especially when animals are given the opportunity to consume higher nicotine doses 68 , 69 , 70 , 71 , 72 . In addition to nAChRs, other signalling factors acting on the MHb terminals in the IPN also regulate the actions of nicotine. For instance, under conditions of chronic nicotine exposure or with optogenetic activation of IPN neurons, a subtype of IPN neurons co-expressing Chrna5 (encoding the α 5 nAChR subunit) and Amigo1 (encoding adhesion molecule with immunoglobulin-like domain 1) release nitric oxide from the cell body that retrogradely inhibits MHb axon terminals 70 . In addition, nicotine activates α 5 -containing nAChR-expressing neurons that project from the nucleus tractus solitarius to the IPN, leading to release of glucagon-like peptide-1 that binds to GLP receptors on habenular axon terminals, which subsequently increases IPN neuron activation and decreases nicotine self-administration 73 . Taken together, these findings suggest a dynamic signalling process at MHb axonal terminals in the IPN, which regulates the addictive properties of nicotine and determines the amount of nicotine that is self-administered.
Nicotine withdrawal in animal models can be assessed by examining somatic signs (such as shaking, scratching, head nods and chewing) and affective signs (such as increased anxiety-related behaviours and conditioned place aversion). Interestingly, few nicotine withdrawal somatic signs are found in mice with genetic knockout of the α 2 , α 5 or β 4 nAChR subunits 74 , 75 . By contrast, β 2 nAChR-knockout mice have fewer anxiety-related behaviours during nicotine withdrawal, with no differences in somatic symptoms compared with wild-type mice 74 , 76 .
In addition to the VTA (mediating reward) and the MHb–IPN pathway (mediating aversion), other brain areas are involved in nicotine addiction (Fig. 5 ). In animals, the insular cortex controls nicotine taking and nicotine seeking 77 . Moreover, humans with lesions of the insular cortex can quit smoking easily without relapse 78 . This finding led to the development of a novel therapeutic intervention modulating insula function (see Management, below) 79 , 80 . Various brain areas (shell of nucleus accumbens, basolateral amygdala and prelimbic cortex) expressing cannabinoid CB 1 receptors are also critical in controlling rewarding effects and relapse 81 , 82 . The α 1 -adrenergic receptor expressed in the cortex also control these effects, probably through glutamatergic afferents to the nucleus accumbens 83 .
Individual differences in nicotine addiction risk
Vulnerability to nicotine dependence varies between individuals, and the reasons for these differences are multidimensional. Many social factors (such as education level and income) play a role 84 . Broad psychological and social factors also modulate this risk. For example, peer smoking status, knowledge on effect of tobacco, expectation on social acceptance, exposure to passive smoking modulate the risk of initiating tobacco use 85 , 86 .
Genetic factors have a role in smoking initiation, the development of nicotine addiction and the likelihood of smoking cessation. Indeed, heritability has been estimated to contribute to approximatively half of the variability in nicotine dependence 87 , 88 , 89 , 90 . Important advances in our understanding of such genetic contributions have evolved with large-scale genome-wide association studies of smokers and non-smokers. One of the most striking findings has been that allelic variation in the CHRNA5 – CHRNA3 – CHRNB4 gene cluster, which encodes α 5 , α 3 and β 4 nAChR subunits, correlates with an increased vulnerability for nicotine addiction, indicated by a higher likelihood of becoming dependent on nicotine and smoking a greater number of cigarettes per day 91 , 92 , 93 , 94 , 95 . The most significant effect has been found for a single-nucleotide polymorphism in CHRNA5 (rs16969968), which results in an amino acid change and reduced function of α 5 -containing nAChRs 92 .
Allelic variation in CYP2A6 (encoding the CYP2A6 enzyme, which metabolizes nicotine) has also been associated with differential vulnerability to nicotine dependence 96 , 97 , 98 . CYP2A6 is highly polymorphic, resulting in variable enzymatic activity 96 , 99 , 100 . Individuals with allelic variation that results in slow nicotine metabolism consume less nicotine per day, experience less-severe withdrawal symptoms and are more successful at quitting smoking than individuals with normal or fast metabolism 101 , 102 , 103 , 104 . Moreover, individuals with slow nicotine metabolism have lower dopaminergic receptor expression in the dopamine D2 regions of the associative striatum and sensorimotor striatum in PET studies 105 and take fewer puffs of nicotine-containing cigarettes (compared with de-nicotinized cigarettes) in a forced choice task 106 . Slower nicotine metabolism is thought to increase the duration of action of nicotine, allowing nicotine levels to accumulate over time, therefore enabling lower levels of intake to sustain activation of nAChRs 107 .
Large-scale genetic studies have identified hundreds of other genetic loci that influence smoking initiation, age of smoking initiation, cigarettes smoked per day and successful smoking cessation 108 . The strongest genetic contributions to smoking through the nicotinic receptors and nicotine metabolism are among the strongest genetic contributors to lung cancer 109 . Other genetic variations (such as those related to cannabinoid, dopamine receptors or other neurotransmitters) may affect certain phenotypes related to smoking (such as nicotine preference and cue-reactivity) 110 , 111 , 112 , 113 , 114 , 115 .
Diagnosis, screening and prevention
Screening for cigarette smoking.
Screening for cigarette smoking should happen at every doctor’s visit 116 . In this regard, a simple and direct question about a person’s tobacco use can provide an opportunity to offer information about its potential risks and treatments to assist in quitting. All smokers should be offered assistance in quitting because even low levels of smoking present a significant health risk 33 , 117 , 118 . Smoking status can be assessed by self-categorization or self-reported assessment of smoking behaviour (Table 1 ). In people who smoke, smoking frequency can be assessed 119 and a combined quantity frequency measure such as pack-year history (that is, average number of cigarettes smoked per day multiplied by the number of years, divided by 20), can be used to estimate cumulative risk of adverse health outcomes. The Association for the Treatment of Tobacco Use and Dependence recommends that all electronic health records should document smoking status using the self-report categories listed in Table 1 .
Owing to the advent of e-cigarettes and heat-not-burn products, and the popularity of little cigars in the US that mimic combustible cigarettes, people who use tobacco may use multiple products concurrently 120 , 121 . Thus, screening for other nicotine and tobacco product use is important in clinical practice. The self-categorization approach can also be used to describe the use of these other products.
Traditionally tobacco use has been classified according to whether the smoker meets criteria for nicotine dependence in one of the two main diagnostic classifications: the DSM 122 (tobacco use disorder) and the ICD (tobacco dependence) 123 . The diagnosis of tobacco use disorder according to DSM-5 criteria requires the presence of at least 2 of 11 symptoms that have produced marked clinical impairment or distress within a 12-month period (Box 2 ). Of note, these symptoms are similar for all substance use disorder diagnoses and may not all be relevant to tobacco use disorder (such as failure to complete life roles). In the ICD-10, codes allow the identification of specific tobacco products used (cigarettes, chewing tobacco and other tobacco products).
Dependence can also be assessed as a continuous construct associated with higher levels of use, greater withdrawal and reduced likelihood of quitting. The level of dependence can be assessed with the Fagerström Test for Nicotine Dependence, a short questionnaire comprising six questions 124 (Box 2 ). A score of ≥4 indicates moderate to high dependence. As very limited time may be available in clinical consultations, the Heaviness of Smoking Index (HSI) was developed, which comprises two questions on the number of cigarettes smoked per day and how soon after waking the first cigarette is smoked 125 . The HSI can guide dosing for nicotine replacement therapy (NRT).
Other measures of cigarette dependence have been developed but are not used in the clinical setting, such as the Cigarette Dependence Scale 126 , Hooked on Nicotine Checklist 127 , Nicotine Dependence Syndrome Scale 128 , the Wisconsin Inventory of Smoking Dependence Motives (Brief) 129 and the Penn State Cigarette Dependence Index 130 . However, in practice, these are not often used, as the most important aspect is to screen for smoking and encourage all smokers to quit smoking regardless of their dependence status.
Box 2 DSM-5 criteria for tobacco use disorder and items of the Fagerström Test for nicotine dependence
DSM-5 (ref. 122 )
Taxonomic and diagnostic tool for tobacco use disorder published by the American Psychiatric Association.
A problematic pattern of tobacco use leading to clinically significant impairment or distress as manifested by at least two of the following, occurring within a 12-month period.
Tobacco often used in larger amounts or over a longer period of time than intended
A persistent desire or unsuccessful efforts to reduce or control tobacco use
A great deal of time spent in activities necessary to obtain or use tobacco
Craving, or a strong desire or urge to use tobacco
Recurrent tobacco use resulting in a failure to fulfil major role obligations at work, school or home
Continued tobacco use despite having persistent or recurrent social or interpersonal problems caused or exacerbated by the effects of tobacco (for example, arguments with others about tobacco use)
Important social, occupational or recreational activities given up or reduced because of tobacco use
Recurrent tobacco use in hazardous situations (such as smoking in bed)
Tobacco use continued despite knowledge of having a persistent or recurrent physical or psychological problem that is likely to have been caused or exacerbated by tobacco use
Tolerance, defined by either of the following.
A need for markedly increased amounts of tobacco to achieve the desired effect
A markedly diminished effect with continued use of the same amount of tobacco
Withdrawal, manifesting as either of the following.
Withdrawal syndrome for tobacco
Tobacco (or a closely related substance, such as nicotine) taken to relieve or avoid withdrawal symptoms
Fagerström Test for Nicotine Dependence 124
A standard instrument for assessing the intensity of physical addiction to nicotine.
How soon after you wake up do you smoke your first cigarette?
Within 5 min (scores 3 points)
5 to 30 min (scores 2 points)
31 to 60 min (scores 1 point)
After 60 min (scores 0 points)
Do you find it difficult not to smoke in places where you should not, such as in church or school, in a movie, at the library, on a bus, in court or in a hospital?
Yes (scores 1 point)
No (scores 0 points)
Which cigarette would you most hate to give up; which cigarette do you treasure the most?
The first one in the morning (scores 1 point)
Any other one (scores 0 points)
How many cigarettes do you smoke each day?
10 or fewer (scores 0 points)
11 to 20 (scores 1 point)
21 to 30 (scores 2 points)
31 or more (scores 3 points)
Do you smoke more during the first few hours after waking up than during the rest of the day?
Do you still smoke if you are so sick that you are in bed most of the day or if you have a cold or the flu and have trouble breathing?
A score of 7–10 points is classified as highly dependent; 4–6 points is classified as moderately dependent; <4 points is classified as minimally dependent.
DSM-5, Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition.
Young people who do not start smoking cigarettes between 15 and 25 years of age have a very low risk of ever smoking 24 , 131 , 132 . This age group provides a critical opportunity to prevent cigarette smoking using effective, evidence-based strategies to prevent smoking initiation and reduce escalation from experimentation to regular use 131 , 132 , 133 , 134 , 135 .
Effective prevention of cigarette uptake requires a comprehensive package of cost-effective policies 134 , 136 , 137 to synergistically reduce the population prevalence of cigarette smoking 131 , 135 . These policies include high rates of tobacco taxation 30 , 134 , 137 , 138 , widespread and rigorously enforced smoke-free policies 139 , bans on tobacco advertising and promotions 140 , use of plain packaging and graphic warnings about the health risks of smoking 135 , 141 , mass media and peer-based education programmes to discourage smoking, and enforcement of laws against the sale of cigarettes to young people below the minimum legal purchase age 131 , 135 . These policies make cigarettes less available and affordable to young people. Moreover, these policies make it more difficult for young people to purchase cigarettes and make smoking a much less socially acceptable practice. Of note, these policies are typically mostly enacted in HICs, which may be related to the declining prevalence of smoking in these countries, compared with the prevalence in LMICs.
Pharmacotherapy
Three evidence-based classes of pharmacotherapy are available for smoking cessation: NRT (using nicotine-based patches, gum, lozenges, mini-lozenges, nasal sprays and inhalers), varenicline (a nAChR partial agonist), and bupropion (a noradrenaline/dopamine reuptake inhibitor that also inhibits nAChR function and is also used as an antidepressant). These FDA-approved and EMA-approved pharmacotherapies are cost-effective smoking cessation treatments that double or triple successful abstinence rates compared with no treatment or placebo controls 116 , 142 .
Combinations of pharmacotherapies are also effective for smoking cessation 116 , 142 . For example, combining NRTs (such as the steady-state nicotine patch and as-needed NRT such as gum or mini-lozenge) is more effective than a single form of NRT 116 , 142 , 143 . Combining NRT and varenicline is the most effective smoking cessation pharmacotherapy 116 , 142 , 143 . Combining FDA-approved pharmacotherapy with behavioural counselling further increases the likelihood of successful cessation 142 . Second-line pharmacotherapies (for example, nortriptyline) have some potential for smoking cessation, but their use is limited due to their tolerability profile.
All smokers should receive pharmacotherapy to help them quit smoking, except those in whom pharmacotherapy has insufficient evidence of effectiveness (among adolescents, smokeless tobacco users, pregnant women or light smokers) or those in whom pharmacotherapy is medically contraindicated 144 . Table 2 provides specific information regarding dosing and duration for each FDA-approved pharmacotherapy. Extended use of pharmacotherapy beyond the standard 12-week regimen after cessation is effective and should be considered 116 . Moreover, preloading pharmacotherapy (that is, initiating cessation medication in advance of a quit attempt), especially with the nicotine patch, is a promising treatment, although further studies are required to confirm efficacy.
Cytisine has been used for smoking cessation in Eastern Europe for a long time and is available in some countries (such as Canada) without prescription 145 . Cytisine is a partial agonist of nAChRs and its structure was the precursor for the development of varenicline 145 . Cytisine is at least as effective as some approved pharmacotherapies for smoking cessation, such as NRT 146 , 147 , 148 , and the role of cytisine in smoking cessation is likely to expand in the future, notably owing to its much lower cost than traditional pharmacotherapies. E-cigarettes also have the potential to be useful as smoking cessation devices 149 , 150 . The 2020 US Surgeon General’s Report concluded that there was insufficient evidence to promote cytisine or e-cigarettes as effective smoking cessation treatments, but in the UK its use is recommended for smoking cessation (see ref. 15 for regularly updated review).
Counselling and behavioural treatments
Psychosocial counselling significantly increases the likelihood of successful cessation, especially when combined with pharmacotherapy. Even a counselling session lasting only 3 minutes can help smokers quit 116 , although the 2008 US Public Health Service guidelines and the Preventive Services Task Force 151 each concluded that more intensive counselling (≥20 min per session) is more effective than less intensive counselling (<20 min per session). Higher smoking cessation rates are obtained by using behavioural change techniques that target associative and self-regulatory processes 152 . In addition, behavioural change techniques that will favour commitment, social reward and identity associated with changed behaviour seems associated with higher success rates 152 . Evidence-based counselling focuses on providing social support during treatment, building skills to cope with withdrawal and cessation, and problem-solving in challenging situations 116 , 153 . Effective counselling can be delivered by diverse providers (such as physicians, nurses, pharmacists, social workers, psychologists and certified tobacco treatment specialists) 116 .
Counselling can be delivered in a variety of modalities. In-person individual and group counselling are effective, as is telephone counselling (quit lines) 142 . Internet and text-based intervention seem to be effective in smoking cessation, especially when they are interactive and tailored to a smoker’s specific circumstances 142 . Over the past several years, the number of smoking cessation smartphone apps has increased, but there the evidence that the use of these apps significantly increases smoking cessation rates is not sufficient.
Contingency management (providing financial incentives for abstinence or engagement in treatment) has shown promising results 154 , 155 but its effects are not sustained once the contingencies are removed 155 , 156 . Other treatments such as hypnosis, acupuncture and laser treatment have not been shown to improve smoking cessation rates compared with placebo treatments 116 . Moreover, no solid evidence supports the use of conventional transcranial magnetic stimulation (TMS) for long-term smoking cessation 157 , 158 .
Although a variety of empirically supported smoking cessation interventions are available, more than two-thirds of adult smokers who made quit attempts in the USA during the past year did not use an evidence-based treatment and the rate is likely to be lower in many other countries 142 . This speaks to the need to increase awareness of, and access to, effective cessation aids among all smokers.
Brain stimulation
The insula (part of the frontal cortex) is a critical brain structure involved in cigarette craving and relapse 78 , 79 . The activity of the insula can be modulated using an innovative approach called deep insula/prefrontal cortex TMS (deep TMS), which is effective in helping people quit smoking 80 , 159 . This approach has now been approved by the FDA as an effective smoking cessation intervention 80 . However, although this intervention was developed and is effective for smoking cessation, the number of people with access to it is limited owing to the limited number of sites equipped and with trained personnel, and the cost of this intervention.
Quality of life
Generic instruments (such as the Short-Form (SF-36) Health Survey) can be used to evaluate quality of life (QOL) in smokers. People who smoke rate their QOL lower than people who do not smoke both before and after they become smokers 160 , 161 . QOL improves when smokers quit 162 . Mental health may also improve on quitting smoking 163 . Moreover, QOL is much poorer in smokers with tobacco-related diseases, such as chronic respiratory diseases and cancers, than in individuals without tobacco-related diseases 161 , 164 . The dimensions of QOL that show the largest decrements in people who smoke are those related to physical health, day-to-day activities and mental health such as depression 160 . Smoking also increases the risk of diabetes mellitus 165 , 166 , which is a major determinant of poor QOL for a wide range of conditions.
The high toll of premature death from cigarette smoking can obscure the fact that many of the diseases that cause these deaths also produce substantial disability in the years before death 1 . Indeed, death in smokers is typically preceded by several years of living with the serious disability and impairment of everyday activities caused by chronic respiratory disease, heart disease and cancer 2 . Smokers’ QOL in these years may also be adversely affected by the adverse effects of the medical treatments that they receive for these smoking-related diseases (such as major surgery and radiotherapy).
Expanding cessation worldwide
The major global challenge is to consider individual and population-based strategies that could increase the substantially low rates of adult cessation in most LMICs and indeed strategies to ensure that even in HICs, cessation continues to increase. In general, the most effective tools recommended by WHO to expand cessation are the same tools that can prevent smoking initiation, notably higher tobacco taxes, bans on advertising and promotion, prominent warning labels or plain packaging, bans on public smoking, and mass media and educational efforts 29 , 167 . The effective use of these policies, particularly taxation, lags behind in most LMICs compared with most HICs, with important exceptions such as Brazil 167 . Access to effective pharmacotherapies and counselling as well as support for co-existing mental health conditions would also be required to accelerate cessation in LMICs. This is particularly important as smokers living in LMICs often have no access to the full range of effective treatment options.
Regulating access to e-cigarettes
How e-cigarettes should be used is debated within the tobacco control field. In some countries (for example, the UK), the use of e-cigarettes as a cigarette smoking cessation aid and as a harm reduction strategy is supported, based on the idea that e-cigarette use will lead to much less exposure to toxic compounds than tobacco use, therefore reducing global harm. In other countries (for example, the USA), there is more concern with preventing the increased use of e-cigarettes by youths that may subsequently lead to smoking 25 , 26 . Regulating e-cigarettes in nuanced ways that enable smokers to access those products whilst preventing their uptake among youths is critical.
Regulating nicotine content in tobacco products
Reducing the nicotine content of cigarettes could potentially produce less addictive products that would allow a gradual reduction in the population prevalence of smoking. Some clinical studies have found no compensatory increase in smoking whilst providing access to low nicotine tobacco 168 . Future regulation may be implemented to gradually decrease the nicotine content of combustible tobacco and other nicotine products 169 , 170 , 171 .
Tobacco end games
Some individuals have proposed getting rid of commercial tobacco products this century or using the major economic disruption arising from the COVID-19 pandemic to accelerate the demise of the tobacco industry 172 , 173 . Some tobacco producers have even proposed this strategy as an internal goal, with the idea of switching to nicotine delivery systems that are less harmful ( Philip Morris International ). Some countries are moving towards such an objective; for example, in New Zealand, the goal that fewer than 5% of New Zealanders will be smokers in 2025 has been set (ref. 174 ). The tobacco end-game approach would overall be the best approach to reduce the burden of tobacco use on society, but it would require coordination of multiple countries and strong public and private consensus on the strategy to avoid a major expansion of the existing illicit market in tobacco products in some countries.
Innovative interventions
The COVID-19 pandemic has shown that large-scale investment in research can lead to rapid development of successful therapeutic interventions. By contrast, smoking cessation has been underfunded compared with the contribution that it makes to the global burden of disease. In addition, there is limited coordination between research teams and most studies are small-scale and often underpowered 79 . It is time to fund an ambitious, coordinated programme of research to test the most promising therapies based on an increased understanding of the neurobiological basis of smoking and nicotine addiction (Table 3 ). Many of those ideas have not yet been tested properly and this could be carried out by a coordinated programme of research at the international level.
GBD 2019 Tobacco Collaborators. Spatial, temporal, and demographic patterns in prevalence of smoking tobacco use and attributable disease burden in 204 countries and territories, 1990-2019: a systematic analysis from the Global Burden of Disease Study 2019. Lancet 397 , 2337–2360 (2021). This study summarizes the burden of disease induced by tobacco worldwide .
Google Scholar
West, R. Tobacco smoking: health impact, prevalence, correlates and interventions. Psychol. Health 32 , 1018–1036 (2017).
PubMed PubMed Central Google Scholar
West, R. The multiple facets of cigarette addiction and what they mean for encouraging and helping smokers to stop. COPD 6 , 277–283 (2009).
PubMed Google Scholar
Fagerström, K. Determinants of tobacco use and renaming the FTND to the Fagerström test for cigarette dependence. Nicotine Tob. Res. 14 , 75–78 (2012).
National Center for Chronic Disease Prevention and Health Promotion (US) Office on Smoking and Health. The Health Consequences of Smoking: 50 Years of Progress. A Report of the Surgeon General (Centers for Disease Control and Prevention, 2014).
Doll, R. & Hill, A. B. Smoking and carcinoma of the lung; preliminary report. Br. Med. J. 2 , 739–748 (1950).
CAS PubMed PubMed Central Google Scholar
Royal College of Physicians. Smoking and health. Summary of a report of the Royal College of Physicians of London on smoking in relation to cancer of the lung and other diseases (Pitman Medical Publishing, 1962).
Henningfield, J. E., Smith, T. T., Kleykamp, B. A., Fant, R. V. & Donny, E. C. Nicotine self-administration research: the legacy of Steven R. Goldberg and implications for regulation, health policy, and research. Psychopharmacology 233 , 3829–3848 (2016).
Le Foll, B. & Goldberg, S. R. Effects of nicotine in experimental animals and humans: an update on addictive properties. Hand. Exp. Pharmacol. https://doi.org/10.1007/978-3-540-69248-5_12 (2009).
Article Google Scholar
Proctor, R. N. The history of the discovery of the cigarette–lung cancer link: evidentiary traditions, corporate denial, global toll. Tob. Control. 21 , 87–91 (2012).
Hall, B. J. et al. Differential effects of non-nicotine tobacco constituent compounds on nicotine self-administration in rats. Pharmacol. Biochem. Behav. 120 , 103–108 (2014).
Musso, F. et al. Smoking impacts on prefrontal attentional network function in young adult brains. Psychopharmacology 191 , 159–169 (2007).
CAS PubMed Google Scholar
Goriounova, N. A. & Mansvelder, H. D. Short- and long-term consequences of nicotine exposure during adolescence for prefrontal cortex neuronal network function. Cold Spring Harb. Perspect. Med. 2 , a012120 (2012).
Fagerström, K. O. & Bridgman, K. Tobacco harm reduction: the need for new products that can compete with cigarettes. Addictive Behav. 39 , 507–511 (2014).
Hartmann-Boyce, J. et al. Electronic cigarettes for smoking cessation. Cochrane Database Syst. Rev. 9 , CD010216 (2021).
Jha, P. The hazards of smoking and the benefits of cessation: a critical summation of the epidemiological evidence in high-income countries. eLife https://doi.org/10.7554/eLife.49979 (2020).
Article PubMed PubMed Central Google Scholar
Palipudi, K. M. et al. Social determinants of health and tobacco use in thirteen low and middle income countries: evidence from Global Adult Tobacco Survey. PLoS ONE 7 , e33466 (2012).
Goodwin, R. D., Pagura, J., Spiwak, R., Lemeshow, A. R. & Sareen, J. Predictors of persistent nicotine dependence among adults in the United States. Drug Alcohol. Depend. 118 , 127–133 (2011).
Weinberger, A. H. et al. Cigarette use is increasing among people with illicit substance use disorders in the United States, 2002-14: emerging disparities in vulnerable populations. Addiction 113 , 719–728 (2018).
Evans-Polce, R. J., Kcomt, L., Veliz, P. T., Boyd, C. J. & McCabe, S. E. Alcohol, tobacco, and comorbid psychiatric disorders and associations with sexual identity and stress-related correlates. Am. J. Psychiatry 177 , 1073–1081 (2020).
Hassan, A. N. & Le Foll, B. Survival probabilities and predictors of major depressive episode incidence among individuals with various types of substance use disorders. J. Clin. Psychiatry https://doi.org/10.4088/JCP.20m13637 (2021).
Article PubMed Google Scholar
Smith, P. H., Mazure, C. M. & McKee, S. A. Smoking and mental illness in the U.S. population. Tob. Control. 23 , e147–e153 (2014).
Bourgault, Z., Rubin-Kahana, D. S., Hassan, A. N., Sanches, M. & Le Foll, B. Multiple substance use disorders and self-reported cognitive function in U.S. adults: associations and sex-differences in a nationally representative sample. Front. Psychiatry https://doi.org/10.3389/fpsyt.2021.797578 (2022).
Reitsma, M. B. et al. Spatial, temporal, and demographic patterns in prevalence of smoking tobacco use and initiation among young people in 204 countries and territories, 1990-2019. Lancet Public Health 6 , e472–e481 (2021).
Warner, K. E. How to think–not feel–about tobacco harm reduction. Nicotine Tob. Res. 21 , 1299–1309 (2019).
Soneji, S. et al. Association between initial use of e-cigarettes and subsequent cigarette smoking among adolescents and young adults: a systematic review and meta-analysis. JAMA Pediatr. 171 , 788–797 (2017).
Levy, D. T. et al. Examining the relationship of vaping to smoking initiation among US youth and young adults: a reality check. Tob. Control. 28 , 629–635 (2019).
National Center for Chronic Disease Prevention and Health Promotion (US) Office on Smoking and Health. The health consequences of smoking — 50 years of progress: a report of the Surgeon General (Centers for Disease Control and Prevention, 2014).
Jha, P. & Peto, R. Global effects of smoking, of quitting, and of taxing tobacco. N. Engl. J. Med. 370 , 60–68 (2014). This review covers the impact of tobacco, of quitting smoking and the importance of taxation to impact prevalence of smoking .
Jha, P. & Peto., R. in Tobacco Tax Reform: At the Crossroads of Health and Development . (eds Marquez, P. V. & Moreno-Dodson, B.) 55–72 (World Bank Group, 2017).
Jha, P. et al. 21st-century hazards of smoking and benefits of cessation in the United States. N. Engl. J. Med. 368 , 341–350 (2013).
Banks, E. et al. Tobacco smoking and all-cause mortality in a large Australian cohort study: findings from a mature epidemic with current low smoking prevalence. BMC Med. 13 , 38 (2015).
Pirie, K. et al. The 21st century hazards of smoking and benefits of stopping: a prospective study of one million women in the UK. Lancet 381 , 133–141 (2013).
Jha, P. et al. A nationally representative case-control study of smoking and death in India. N. Engl. J. Med. 358 , 1137–1147 (2008).
Chan, E. D. et al. Tobacco exposure and susceptibility to tuberculosis: is there a smoking gun? Tuberculosis 94 , 544–550 (2014).
Wang, M. G. et al. Association between tobacco smoking and drug-resistant tuberculosis. Infect. Drug Resist. 11 , 873–887 (2018).
Jha, P. et al. Social inequalities in male mortality, and in male mortality from smoking: indirect estimation from national death rates in England and Wales, Poland, and North America. Lancet 368 , 367–370 (2006).
Jha, P., Gelband, H, Irving, H. & Mishra, S. in Reducing Social Inequalities in Cancer: Evidence and Priorities for Research (eds Vaccarella, S et al.) 161–166 (IARC, 2018).
Jha, P. Expanding smoking cessation world-wide. Addiction 113 , 1392–1393 (2018).
Jha, P. Avoidable global cancer deaths and total deaths from smoking. Nat. Rev. Cancer 9 , 655–664 (2009).
Wittenberg, R. E., Wolfman, S. L., De Biasi, M. & Dani, J. A. Nicotinic acetylcholine receptors and nicotine addiction: a brief introduction. Neuropharmacology 177 , 108256 (2020).
Boulter, J. et al. Functional expression of two neuronal nicotinic acetylcholine receptors from cDNA clones identifies a gene family. Proc. Natl Acad. Sci. USA 84 , 7763–7767 (1987).
Couturier, S. et al. A neuronal nicotinic acetylcholine receptor subunit (α7) is developmentally regulated and forms a homo-oligomeric channel blocked by α-BTX. Neuron 5 , 847–856 (1990).
Picciotto, M. R., Addy, N. A., Mineur, Y. S. & Brunzell, D. H. It is not “either/or”: activation and desensitization of nicotinic acetylcholine receptors both contribute to behaviors related to nicotine addiction and mood. Prog. Neurobiol. 84 , 329–342 (2008).
Changeux, J. P. Structural identification of the nicotinic receptor ion channel. Trends Neurosci. 41 , 67–70 (2018).
McKay, B. E., Placzek, A. N. & Dani, J. A. Regulation of synaptic transmission and plasticity by neuronal nicotinic acetylcholine receptors. Biochem. Pharmacol. 74 , 1120–1133 (2007).
Wonnacott, S. Presynaptic nicotinic ACh receptors. Trends Neurosci. 20 , 92–98 (1997).
Wooltorton, J. R., Pidoplichko, V. I., Broide, R. S. & Dani, J. A. Differential desensitization and distribution of nicotinic acetylcholine receptor subtypes in midbrain dopamine areas. J. Neurosci. 23 , 3176–3185 (2003).
Gipson, C. D. & Fowler, C. D. Nicotinic receptors underlying nicotine dependence: evidence from transgenic mouse models. Curr. Top. Behav. Neurosci. 45 , 101–121 (2020).
Hamouda, A. K. et al. Potentiation of (α4)2(β2)3, but not (α4)3(β2)2, nicotinic acetylcholine receptors reduces nicotine self-administration and withdrawal symptoms. Neuropharmacology 190 , 108568 (2021).
Lallai, V. et al. Nicotine acts on cholinergic signaling mechanisms to directly modulate choroid plexus function. eNeuro https://doi.org/10.1523/ENEURO.0051-19.2019 (2019).
Benwell, M. E., Balfour, D. J. & Anderson, J. M. Evidence that tobacco smoking increases the density of (-)-[3H]nicotine binding sites in human brain. J. Neurochem. 50 , 1243–1247 (1988).
Perry, D. C., Davila-Garcia, M. I., Stockmeier, C. A. & Kellar, K. J. Increased nicotinic receptors in brains from smokers: membrane binding and autoradiography studies. J. Pharmacol. Exp. Ther. 289 , 1545–1552 (1999).
Marks, M. J. et al. Nicotine binding and nicotinic receptor subunit RNA after chronic nicotine treatment. J. Neurosci. 12 , 2765–2784 (1992).
Le Foll, B. et al. Impact of short access nicotine self-administration on expression of α4β2* nicotinic acetylcholine receptors in non-human primates. Psychopharmacology 233 , 1829–1835 (2016).
Meyers, E. E., Loetz, E. C. & Marks, M. J. Differential expression of the beta4 neuronal nicotinic receptor subunit affects tolerance development and nicotinic binding sites following chronic nicotine treatment. Pharmacol. Biochem. Behav. 130 , 1–8 (2015).
Zhao-Shea, R., Liu, L., Pang, X., Gardner, P. D. & Tapper, A. R. Activation of GABAergic neurons in the interpeduncular nucleus triggers physical nicotine withdrawal symptoms. Curr. Biol. 23 , 2327–2335 (2013).
Jensen, K. P., Valentine, G., Gueorguieva, R. & Sofuoglu, M. Differential effects of nicotine delivery rate on subjective drug effects, urges to smoke, heart rate and blood pressure in tobacco smokers. Psychopharmacology 237 , 1359–1369 (2020).
Villanueva, H. F., James, J. R. & Rosecrans, J. A. Evidence of pharmacological tolerance to nicotine. NIDA Res. Monogr. 95 , 349–350 (1989).
Corrigall, W. A., Coen, K. M. & Adamson, K. L. Self-administered nicotine activates the mesolimbic dopamine system through the ventral tegmental area. Brain Res. 653 , 278–284 (1994).
Nisell, M., Nomikos, G. G., Hertel, P., Panagis, G. & Svensson, T. H. Condition-independent sensitization of locomotor stimulation and mesocortical dopamine release following chronic nicotine treatment in the rat. Synapse 22 , 369–381 (1996).
Rice, M. E. & Cragg, S. J. Nicotine amplifies reward-related dopamine signals in striatum. Nat. Neurosci. 7 , 583–584 (2004).
Mameli-Engvall, M. et al. Hierarchical control of dopamine neuron-firing patterns by nicotinic receptors. Neuron 50 , 911–921 (2006).
Picciotto, M. R., Higley, M. J. & Mineur, Y. S. Acetylcholine as a neuromodulator: cholinergic signaling shapes nervous system function and behavior. Neuron 76 , 116–129 (2012).
Le Foll, B. et al. Elevation of dopamine induced by cigarette smoking: novel insights from a [11C]-+-PHNO PET study in humans. Neuropsychopharmacology 39 , 415–424 (2014). This brain imaging study identified the brain areas in which smoking elevates dopamine levels .
Maskos, U. et al. Nicotine reinforcement and cognition restored by targeted expression of nicotinic receptors. Nature 436 , 103–107 (2005). This article discusses the implication of the β 2 - containing nAChRs in the VTA in mammalian cognitive function .
Picciotto, M. R. et al. Acetylcholine receptors containing the beta2 subunit are involved in the reinforcing properties of nicotine. Nature 391 , 173–177 (1998). This article discusses the implication of the β 2 - containing nAChRs in addictive effects of nicotine .
Fowler, C. D., Lu, Q., Johnson, P. M., Marks, M. J. & Kenny, P. J. Habenular alpha5 nicotinic receptor subunit signalling controls nicotine intake. Nature 471 , 597–601 (2011). This article discusses the implication of the α5 nicotinic receptor located in the MHb in a mechanism mediating the aversive effects of nicotine .
Elayouby, K. S. et al. α3* Nicotinic acetylcholine receptors in the habenula-interpeduncular nucleus circuit regulate nicotine intake. J. Neurosci. https://doi.org/10.1523/JNEUROSCI.0127-19.2020 (2020).
Ables, J. L. et al. Retrograde inhibition by a specific subset of interpeduncular α5 nicotinic neurons regulates nicotine preference. Proc. Natl Acad. Sci. USA 114 , 13012–13017 (2017).
Frahm, S. et al. Aversion to nicotine is regulated by the balanced activity of β4 and α5 nicotinic receptor subunits in the medial habenula. Neuron 70 , 522–535 (2011).
Jackson, K. J. et al. Role of α5 nicotinic acetylcholine receptors in pharmacological and behavioral effects of nicotine in mice. J. Pharmacol. Exp. Ther. 334 , 137–146 (2010).
Tuesta, L. M. et al. GLP-1 acts on habenular avoidance circuits to control nicotine intake. Nat. Neurosci. 20 , 708–716 (2017).
Salas, R., Pieri, F. & De Biasi, M. Decreased signs of nicotine withdrawal in mice null for the β4 nicotinic acetylcholine receptor subunit. J. Neurosci. 24 , 10035–10039 (2004).
Salas, R., Sturm, R., Boulter, J. & De Biasi, M. Nicotinic receptors in the habenulo-interpeduncular system are necessary for nicotine withdrawal in mice. J. Neurosci. 29 , 3014–3018 (2009).
Jackson, K. J., Martin, B. R., Changeux, J. P. & Damaj, M. I. Differential role of nicotinic acetylcholine receptor subunits in physical and affective nicotine withdrawal signs. J. Pharmacol. Exp. Ther. 325 , 302–312 (2008).
Le Foll, B. et al. Translational strategies for therapeutic development in nicotine addiction: rethinking the conventional bench to bedside approach. Prog. Neuropsychopharmacol. Biol. Psychiatry 52 , 86–93 (2014).
Naqvi, N. H., Rudrauf, D., Damasio, H. & Bechara, A. Damage to the insula disrupts addiction to cigarette smoking. Science 315 , 531–534 (2007). This article discusses the implication of the insular cortex in tobacco addiction .
Ibrahim, C. et al. The insula: a brain stimulation target for the treatment of addiction. Front. Pharmacol. 10 , 720 (2019).
Zangen, A. et al. Repetitive transcranial magnetic stimulation for smoking cessation: a pivotal multicenter double-blind randomized controlled trial. World Psychiatry 20 , 397–404 (2021). This study validated the utility of deep insula/prefrontal cortex rTMS for smoking cessation .
Le Foll, B., Forget, B., Aubin, H. J. & Goldberg, S. R. Blocking cannabinoid CB1 receptors for the treatment of nicotine dependence: insights from pre-clinical and clinical studies. Addict. Biol. 13 , 239–252 (2008).
Kodas, E., Cohen, C., Louis, C. & Griebel, G. Cortico-limbic circuitry for conditioned nicotine-seeking behavior in rats involves endocannabinoid signaling. Psychopharmacology 194 , 161–171 (2007).
Forget, B. et al. Noradrenergic α1 receptors as a novel target for the treatment of nicotine addiction. Neuropsychopharmacology 35 , 1751–1760 (2010).
Garrett, B. E., Dube, S. R., Babb, S. & McAfee, T. Addressing the social determinants of health to reduce tobacco-related disparities. Nicotine Tob. Res. 17 , 892–897 (2015).
Polanska, K., Znyk, M. & Kaleta, D. Susceptibility to tobacco use and associated factors among youth in five central and eastern European countries. BMC Public Health 22 , 72 (2022).
Volkow, N. D. Personalizing the treatment of substance use disorders. Am. J. Psychiatry 177 , 113–116 (2020).
Li, M. D., Cheng, R., Ma, J. Z. & Swan, G. E. A meta-analysis of estimated genetic and environmental effects on smoking behavior in male and female adult twins. Addiction 98 , 23–31 (2003).
Carmelli, D., Swan, G. E., Robinette, D. & Fabsitz, R. Genetic influence on smoking–a study of male twins. N. Engl. J. Med. 327 , 829–833 (1992).
Broms, U., Silventoinen, K., Madden, P. A. F., Heath, A. C. & Kaprio, J. Genetic architecture of smoking behavior: a study of Finnish adult twins. Twin Res. Hum. Genet. 9 , 64–72 (2006).
Kendler, K. S., Thornton, L. M. & Pedersen, N. L. Tobacco consumption in Swedish twins reared apart and reared together. Arch. Gen. Psychiat 57 , 886–892 (2000).
Saccone, N. L. et al. The CHRNA5-CHRNA3-CHRNB4 nicotinic receptor subunit gene cluster affects risk for nicotine dependence in African-Americans and in European-Americans. Cancer Res. 69 , 6848–6856 (2009).
Bierut, L. J. et al. Variants in nicotinic receptors and risk for nicotine dependence. Am. J. Psychiatry 165 , 1163–1171 (2008). This study demonstrates that nAChR gene variants are important in nicotine addiction .
Bierut, L. J. et al. Novel genes identified in a high-density genome wide association study for nicotine dependence. Hum. Mol. Genet. 16 , 24–35 (2007).
Berrettini, W. et al. α-5/α-3 nicotinic receptor subunit alleles increase risk for heavy smoking. Mol. Psychiatry 13 , 368–373 (2008).
Sherva, R. et al. Association of a single nucleotide polymorphism in neuronal acetylcholine receptor subunit alpha 5 (CHRNA5) with smoking status and with ‘pleasurable buzz’ during early experimentation with smoking. Addiction 103 , 1544–1552 (2008).
Thorgeirsson, T. E. et al. Sequence variants at CHRNB3-CHRNA6 and CYP2A6 affect smoking behavior. Nat. Genet. 42 , 448–453 (2010).
Ray, R., Tyndale, R. F. & Lerman, C. Nicotine dependence pharmacogenetics: role of genetic variation in nicotine-metabolizing enzymes. J. Neurogenet. 23 , 252–261 (2009).
Bergen, A. W. et al. Drug metabolizing enzyme and transporter gene variation, nicotine metabolism, prospective abstinence, and cigarette consumption. PLoS ONE 10 , e0126113 (2015).
Mwenifumbo, J. C. et al. Identification of novel CYP2A6*1B variants: the CYP2A6*1B allele is associated with faster in vivo nicotine metabolism. Clin. Pharmacol. Ther. 83 , 115–121 (2008).
Raunio, H. & Rahnasto-Rilla, M. CYP2A6: genetics, structure, regulation, and function. Drug Metab. Drug Interact. 27 , 73–88 (2012).
CAS Google Scholar
Patterson, F. et al. Toward personalized therapy for smoking cessation: a randomized placebo-controlled trial of bupropion. Clin. Pharmacol. Ther. 84 , 320–325 (2008).
Rodriguez, S. et al. Combined analysis of CHRNA5, CHRNA3 and CYP2A6 in relation to adolescent smoking behaviour. J. Psychopharmacol. 25 , 915–923 (2011).
Strasser, A. A., Malaiyandi, V., Hoffmann, E., Tyndale, R. F. & Lerman, C. An association of CYP2A6 genotype and smoking topography. Nicotine Tob. Res. 9 , 511–518 (2007).
Liakoni, E. et al. Effects of nicotine metabolic rate on withdrawal symptoms and response to cigarette smoking after abstinence. Clin. Pharmacol. Ther. 105 , 641–651 (2019).
Di Ciano, P. et al. Influence of nicotine metabolism ratio on [11C]-(+)-PHNO PET binding in tobacco smokers. Int. J. Neuropsychopharmacol. 21 , 503–512 (2018).
Butler, K. et al. Impact of Cyp2a6 activity on nicotine reinforcement and cue-reactivity in daily smokers. Nicotine Tob. Res. https://doi.org/10.1093/ntr/ntab064 (2021).
Benowitz, N. L., Swan, G. E., Jacob, P. 3rd, Lessov-Schlaggar, C. N. & Tyndale, R. F. CYP2A6 genotype and the metabolism and disposition kinetics of nicotine. Clin. Pharmacol. Ther. 80 , 457–467 (2006).
Liu, M. et al. Association studies of up to 1.2 million individuals yield new insights into the genetic etiology of tobacco and alcohol use. Nat. Genet. 51 , 237–244 (2019).
McKay, J. D. et al. Large-scale association analysis identifies new lung cancer susceptibility loci and heterogeneity in genetic susceptibility across histological subtypes. Nat. Genet. 49 , 1126–1132 (2017).
Chukwueke, C. C. et al. The CB1R rs2023239 receptor gene variant significantly affects the reinforcing effects of nicotine, but not cue reactivity, in human smokers. Brain Behav. 11 , e01982 (2021).
Ahrens, S. et al. Modulation of nicotine effects on selective attention by DRD2 and CHRNA4 gene polymorphisms. Psychopharmacology 232 , 2323–2331 (2015).
Harrell, P. T. et al. Dopaminergic genetic variation moderates the effect of nicotine on cigarette reward. Psychopharmacology 233 , 351–360 (2016).
Lerman, C. et al. Role of functional genetic variation in the dopamine D2 receptor (DRD2) in response to bupropion and nicotine replacement therapy for tobacco dependence: results of two randomized clinical trials. Neuropsychopharmacology 31 , 231–242 (2006).
Le Foll, B., Gallo, A., Le Strat, Y., Lu, L. & Gorwood, P. Genetics of dopamine receptors and drug addiction: a comprehensive review. Behav. Pharmacol. 20 , 1–17 (2009).
Chukwueke, C. C. et al. Exploring the role of the Ser9Gly (rs6280) dopamine D3 receptor polymorphism in nicotine reinforcement and cue-elicited craving. Sci. Rep. 10 , 4085 (2020).
The Clinical Practice Guideline Treating Tobacco Use and Dependence 2008 Update Panel, Liaisons, and Staff A clinical practice guideline for treating tobacco use and dependence: 2008 update: a U.S. Public Health Service report. Am. J. Prev. Med. 35 , 158–176 (2008).
Hackshaw, A., Morris, J. K., Boniface, S., Tang, J. L. & Milenković, D. Low cigarette consumption and risk of coronary heart disease and stroke: meta-analysis of 141 cohort studies in 55 study reports. BMJ 360 , j5855 (2018).
Qin, W. et al. Light cigarette smoking increases risk of all-cause and cause-specific mortality: findings from the NHIS cohort study. Int. J. Env. Res. Public Health https://doi.org/10.3390/ijerph17145122 (2020).
Rodu, B. & Plurphanswat, N. Mortality among male smokers and smokeless tobacco users in the USA. Harm Reduct. J. 16 , 50 (2019).
Kasza, K. A. et al. Tobacco-product use by adults and youths in the United States in 2013 and 2014. N. Engl. J. Med. 376 , 342–353 (2017).
Richardson, A., Xiao, H. & Vallone, D. M. Primary and dual users of cigars and cigarettes: profiles, tobacco use patterns and relevance to policy. Nicotine Tob. Res. 14 , 927–932 (2012).
American Psychiatric Association. Diagnostic and Statistical Manual of Mental disorders 5th edn (American Psychiatric Association, 2013).
World Health Organization. Tobacco fact sheet. WHO https://www.who.int/news-room/fact-sheets/detail/tobacco (2021).
Heatherton, T. F., Kozlowski, L. T., Frecker, R. C. & Fagerström, K. O. The Fagerström test for nicotine dependence: a revision of the Fagerström tolerance questionnaire. Br. J. Addict. 86 , 1119–1127 (1991).
Heatherton, T. F., Kozlowski, L. T., Frecker, R. C., Rickert, W. & Robinson, J. Measuring the heaviness of smoking: using self-reported time to the first cigarette of the day and number of cigarettes smoked per day. Br. J. Addict. 84 , 791–799 (1989).
Etter, J. F., Le Houezec, J. & Perneger, T. V. A self-administered questionnaire to measure dependence on cigarettes: the cigarette dependence scale. Neuropsychopharmacology 28 , 359–370 (2003).
DiFranza, J. R. et al. Measuring the loss of autonomy over nicotine use in adolescents: the DANDY (Development and Assessment of Nicotine Dependence in Youths) study. Arch. Pediatr. Adolesc. Med. 156 , 397–403 (2002).
Shiffman, S., Waters, A. & Hickcox, M. The Nicotine Dependence Syndrome Scale: a multidimensional measure of nicotine dependence. Nicotine Tob. Res. 6 , 327–348 (2004).
Smith, S. S. et al. Development of the Brief Wisconsin Inventory of Smoking Dependence Motives. Nicotine Tob. Res. 12 , 489–499 (2010).
Foulds, J. et al. Development of a questionnaire for assessing dependence on electronic cigarettes among a large sample of ex-smoking E-cigarette users. Nicotine Tob. Res. 17 , 186–192 (2015).
National Center for Chronic Disease Prevention and Health Promotion (US) Office on Smoking and Health. Preventing tobacco use among youth and young adults: a report of the Surgeon General (Centers for Disease Control and Prevention, 2012).
World Health Organization. Tobacco control to improve child health and development. Thematic brief (WHO, 2021).
Lantz, P. M. et al. Investing in youth tobacco control: a review of smoking prevention and control strategies. Tob. Control. 9 , 47–63 (2000).
Leão, T., Kunst, A. E. & Perelman, J. Cost-effectiveness of tobacco control policies and programmes targeting adolescents: a systematic review. Eur. J. Public Health 28 , 39–43 (2018).
Royal College of Physicians. Smoking and health 2021: a coming of age for tobacco control? (RCP, 2021).
Higashi, H. et al. Cost effectiveness of tobacco control policies in Vietnam: the case of population-level interventions. Appl. Health Econ. Health Policy 9 , 183–196 (2011).
Ranson, M. K., Jha, P., Chaloupka, F. J. & Nguyen, S. N. Global and regional estimates of the effectiveness and cost-effectiveness of price increases and other tobacco control policies. Nicotine Tob. Res. 4 , 311–319 (2002).
International Agency for Research on Cancer. I ARC Handbooks of Cancer Prevention: Tobacco control Vol. 14 (IARC, 2011).
Frazer, K. et al. Legislative smoking bans for reducing harms from secondhand smoke exposure, smoking prevalence and tobacco consumption. Cochrane Database Syst. Rev. 2 , CD005992 (2016).
Hoffman, S. J. & Tan, C. Overview of systematic reviews on the health-related effects of government tobacco control policies. BMC Public Health 15 , 744 (2015).
McNeill, A. et al. Tobacco packaging design for reducing tobacco use. Cochrane Database Syst. Rev. 4 , CD011244 (2017).
National Center for Chronic Disease Prevention and Health Promotion (US) Office on Smoking and Health. Smoking cessation: a report of the Surgeon General (Department of Health and Human Services, 2020).
Lindson, N. et al. Different doses, durations and modes of delivery of nicotine replacement therapy for smoking cessation. Cochrane Database Syst. Rev. 4 , CD013308 (2019).
Krist, A. H. et al. Interventions for tobacco smoking cessation in adults, including pregnant persons: US Preventive Services Task Force recommendation statement. JAMA 325 , 265–279 (2021).
Tutka, P. & Zatonski, W. Cytisine for the treatment of nicotine addiction: from a molecule to therapeutic efficacy. Pharmacol. Rep. 58 , 777–798 (2006).
Courtney, R. J. et al. Effect of cytisine vs varenicline on smoking cessation: a randomized clinical trial. JAMA 326 , 56–64 (2021).
Walker, N. et al. Cytisine versus nicotine for smoking cessation. N. Engl. J. Med. 371 , 2353–2362 (2014). This study validated the utility of cytisine for smoking cessation .
West, R. et al. Placebo-controlled trial of cytisine for smoking cessation. N. Engl. J. Med. 365 , 1193–1200 (2011).
Hajek, P. et al. E-cigarettes compared with nicotine replacement therapy within the UK Stop Smoking Services: the TEC RCT. Health Technol. Assess. 23 , 1–82 (2019).
Walker, N. et al. Nicotine patches used in combination with e-cigarettes (with and without nicotine) for smoking cessation: a pragmatic, randomised trial. Lancet Respir. Med. 8 , 54–64 (2020).
Siu, A. L., U.S. Preventive Services Task Force. Behavioral and pharmacotherapy interventions for tobacco smoking cessation in adults, including pregnant women: U.S. Preventive Services Task Force recommendation statement. Ann. Intern. Med. 163 , 622–634 (2015).
Black, N. et al. Behaviour change techniques associated with smoking cessation in intervention and comparator groups of randomized controlled trials: a systematic review and meta-regression. Addiction 115 , 2008–2020 (2020).
Center for Substance Abuse and Treatment. Detoxification and Substance Abuse Treatment (Center for Substance Abuse and Treatment, 2006).
Cahill, K., Hartmann-Boyce, J. & Perera, R. Incentives for smoking cessation. Cochrane Database Syst. Rev. https://doi.org/10.1002/14651858.CD004307.pub5 (2015).
Secades-Villa, R., Aonso-Diego, G., García-Pérez, Á. & González-Roz, A. Effectiveness of contingency management for smoking cessation in substance users: a systematic review and meta-analysis. J. Consult. Clin. Psychol. 88 , 951–964 (2020).
Cahill, K. & Perera, R. Competitions and incentives for smoking cessation. Cochrane Database Syst. Rev. https://doi.org/10.1002/14651858.CD004307.pub4 (2011).
Trojak, B. et al. Transcranial magnetic stimulation combined with nicotine replacement therapy for smoking cessation: a randomized controlled trial. Brain Stimul. 8 , 1168–1174 (2015).
Wing, V. C. et al. Brain stimulation methods to treat tobacco addiction. Brain Stimul. 6 , 221–230 (2013).
Dinur-Klein, L. et al. Smoking cessation induced by deep repetitive transcranial magnetic stimulation of the prefrontal and insular cortices: a prospective, randomized controlled trial. Biol. Psychiatry 76 , 742–749 (2014).
Goldenberg, M., Danovitch, I. & IsHak, W. W. Quality of life and smoking. Am. J. Addict. 23 , 540–562 (2014).
Heikkinen, H., Jallinoja, P., Saarni, S. I. & Patja, K. The impact of smoking on health-related and overall quality of life: a general population survey in Finland. Nicotine Tob. Res. 10 , 1199–1207 (2008).
Moayeri, F., Hsueh, Y. A., Dunt, D. & Clarke, P. Smoking cessation and quality of life: insights from analysis of longitudinal Australian data, an application for economic evaluations. Value Health 24 , 724–732 (2021).
Taylor, G. M. et al. Smoking cessation for improving mental health. Cochrane Database Syst. Rev. 3 , CD013522 (2021).
López-Nicolás, Á., Trapero-Bertran, M. & Muñoz, C. Smoking, health-related quality of life and economic evaluation. Eur. J. Health Econ. 19 , 747–756 (2018).
Morris, A. Linking nicotine addiction and T2DM. Nat. Rev. Endocrinol. 16 , 6 (2020).
Willi, C., Bodenmann, P., Ghali, W. A., Faris, P. D. & Cornuz, J. Active smoking and the risk of type 2 diabetes: a systematic review and meta-analysis. Jama 298 , 2654–2664 (2007).
World Health Organization. WHO report on the global tobacco epidemic (WHO, 2019).
Donny, E. C. et al. Randomized trial of reduced-nicotine standards for cigarettes. N. Engl. J. Med. 373 , 1340–1349 (2015). This study tested the impact of reducing the quantity of nicotine present in cigarettes on smoking .
Benowitz, N. L. & Henningfield, J. E. Establishing a nicotine threshold for addiction. The implications for tobacco regulation. N. Engl. J. Med. 331 , 123–125 (1994).
Benowitz, N. L. & Henningfield, J. E. Reducing the nicotine content to make cigarettes less addictive. Tob. Control. 22 , i14–i17 (2013).
Gottlieb, S. & Zeller, M. A nicotine-focused framework for public health. N. Engl. J. Med. 377 , 1111–1114 (2017).
Hall, W. & West, R. Thinking about the unthinkable: a de facto prohibition on smoked tobacco products. Addiction 103 , 873–874 (2008).
Ioannidis, J. P. A. & Jha, P. Does the COVID-19 pandemic provide an opportunity to eliminate the tobacco industry? Lancet Glob. Health 9 , e12–e13 (2021).
Smokefree. Smokefree 2025. Smokefree https://www.smokefree.org.nz/smokefree-in-action/smokefree-aotearoa-2025 (2021).
Morgan, C. J., Das, R. K., Joye, A., Curran, H. V. & Kamboj, S. K. Cannabidiol reduces cigarette consumption in tobacco smokers: preliminary findings. Addict. Behav. 38 , 2433–2436 (2013).
Elsaid, S., Kloiber, S. & Le Foll, B. Effects of cannabidiol (CBD) in neuropsychiatric disorders: a review of pre-clinical and clinical findings. Prog. Mol. Biol. Transl. Sci. 167 , 25–75 (2019).
Butler, K. & Le Foll, B. Novel therapeutic and drug development strategies for tobacco use disorder: endocannabinoid modulation. Expert Opin. Drug Discov. 15 , 1065–1080 (2020).
D’Souza, D. C. et al. Efficacy and safety of a fatty acid amide hydrolase inhibitor (PF-04457845) in the treatment of cannabis withdrawal and dependence in men: a double-blind, placebo-controlled, parallel group, phase 2a single-site randomised controlled trial. Lancet Psychiatry 6 , 35–45 (2019).
Robinson, J. D. et al. Pooled analysis of three randomized, double-blind, placebo controlled trials with rimonabant for smoking cessation. Addict. Biol. 23 , 291–303 (2018).
Gueye, A. B. et al. The CB1 neutral antagonist AM4113 retains the therapeutic efficacy of the inverse agonist rimonabant for nicotine dependence and weight loss with better psychiatric tolerability. Int. J. Neuropsychopharmacol. https://doi.org/10.1093/ijnp/pyw068 (2016).
Yammine, L. et al. Exenatide adjunct to nicotine patch facilitates smoking cessation and may reduce post-cessation weight gain: a pilot randomized controlled trial. Nicotine Tob. Res. 23 , 1682–1690 (2021).
Eren-Yazicioglu, C. Y., Yigit, A., Dogruoz, R. E. & Yapici-Eser, H. Can GLP-1 be a target for reward system related disorders? A qualitative synthesis and systematic review analysis of studies on palatable food, drugs of abuse, and alcohol. Front. Behav. Neurosci. 14 , 614884 (2020).
Vanderkam, P. et al. Effectiveness of drugs acting on adrenergic receptors in the treatment for tobacco or alcohol use disorders: systematic review and meta-analysis. Addiction 116 , 1011–1020 (2021).
Sokoloff, P. & Le Foll, B. The dopamine D3 receptor, a quarter century later. Eur. J. Neurosci. 45 , 2–19 (2017).
David, S. P., Lancaster, T., Stead, L. F., Evins, A. E. & Prochaska, J. J. Opioid antagonists for smoking cessation. Cochrane Database Syst. Rev. https://doi.org/10.1002/14651858.CD003086.pub3 (2013).
Ray, L. A. et al. Efficacy of combining varenicline and naltrexone for smoking cessation and drinking reduction: a randomized clinical trial. Am. J. Psychiatry 178 , 818–828 (2021).
Mooney, M. E. et al. Bupropion and naltrexone for smoking cessation: a double-blind randomized placebo-controlled clinical trial. Clin. Pharmacol. Ther. 100 , 344–352 (2016).
Justinova, Z., Le Foll, B., Redhi, G. H., Markou, A. & Goldberg, S. R. Differential effects of the metabotropic glutamate 2/3 receptor agonist LY379268 on nicotine versus cocaine self-administration and relapse in squirrel monkeys. Psychopharmacology 233 , 1791–1800 (2016).
Le Foll, B., Wertheim, C. E. & Goldberg, S. R. Effects of baclofen on conditioned rewarding and discriminative stimulus effects of nicotine in rats. Neurosci. Lett. 443 , 236–240 (2008).
Franklin, T. R. et al. The GABA B agonist baclofen reduces cigarette consumption in a preliminary double-blind placebo-controlled smoking reduction study. Drug Alcohol. Depend. 103 , 30–36 (2009).
Lotfy, N., Elsawah, H. & Hassan, M. Topiramate for smoking cessation: systematic review and meta-analysis. Tob. Prev. Cessat. 6 , 14 (2020).
Shanahan, W. R., Rose, J. E., Glicklich, A., Stubbe, S. & Sanchez-Kam, M. Lorcaserin for smoking cessation and associated weight gain: a randomized 12-week clinical trial. Nicotine Tob. Res. 19 , 944–951 (2017).
Higgins, G. A., Fletcher, P. J. & Shanahan, W. R. Lorcaserin: a review of its preclinical and clinical pharmacology and therapeutic potential. Pharmacol. Ther. 205 , 107417 (2020).
Stead, L. F. & Lancaster, T. Interventions to reduce harm from continued tobacco use. Cochrane Database Syst. Rev. https://doi.org/10.1002/14651858.CD005231.pub2 (2007).
Download references
Acknowledgements
B.Le F. is supported by a clinician-scientist award from the Department of Family and Community Medicine at the University of Toronto and the Addiction Psychiatry Chair from the University of Toronto. The funding bodies had no role in the study design, collection, analysis or interpretation of the data, writing the manuscript, or the decision to submit the paper for publication. The authors thank H. Fu (University of Toronto) for assistance with Figs 1–3.
Author information
Authors and affiliations.
Translational Addiction Research Laboratory, Campbell Family Mental Health Research Institute, Centre for Addiction and Mental Health, University of Toronto, Toronto, Ontario, Canada
Bernard Le Foll
Departments of Family and Community Medicine, Psychiatry, Pharmacology and Toxicology, University of Toronto, Toronto, Ontario, Canada
Department of Medicine, University of Wisconsin, Madison, WI, USA
Megan E. Piper
University of Wisconsin Center for Tobacco Research and Intervention, Madison, WI, USA
Department of Neurobiology and Behaviour, University of California Irvine, Irvine, CA, USA
Christie D. Fowler
Section for Preventive Cardiology, Department of Endocrinology, Morbid Obesity and Preventive Medicine, Oslo University Hospital, Oslo, Norway
Serena Tonstad
Department of Psychiatry, Washington University School of Medicine, St. Louis, MO, USA
Laura Bierut
Institute of Mental Health, Peking University Sixth Hospital, Peking University, Beijing, China
National Institute on Drug Dependence, Peking University Health Science Center, Beijing, China
Centre for Global Health Research, Unity Health Toronto, University of Toronto, Toronto, Ontario, Canada
- Prabhat Jha
National Centre for Youth Substance Use Research, The University of Queensland, St Lucia, Queensland, Australia
Wayne D. Hall
Queensland Alliance for Environmental Health Sciences, The University of Queensland, Woolloongabba, Queensland, Australia
You can also search for this author in PubMed Google Scholar
Contributions
Introduction (B.Le F.); Epidemiology (P.J. and W.D.H.); Mechanisms/pathophysiology (C.D.F., L.B., L.L. and B.Le F.); Diagnosis, screening and prevention (P.J., M.E.P., S.T. and B.Le F.); Management (M.E.P., S.T., W.D.H., L.L. and B.Le F.); Quality of life (P.J. and W.D.H.); Outlook (all); Conclusions (all). All authors contributed substantially to the review and editing of the manuscript.
Corresponding author
Correspondence to Bernard Le Foll .
Ethics declarations
Competing interests.
B.Le F. has obtained funding from Pfizer (GRAND Awards, including salary support) for investigator-initiated projects. B.Le F. has received some in-kind donations of cannabis product from Aurora and medication donation from Pfizer and Bioprojet and was provided a coil for TMS study from Brainsway. B.Le F. has obtained industry funding from Canopy (through research grants handled by CAMH or the University of Toronto), Bioprojet, ACS, Indivior and Alkermes. B.Le F. has received in-kind donations of nabiximols from GW Pharma for past studies funded by CIHR and NIH. B.Le F. has been an advisor to Shinoghi. S.T. has received honoraria from Pfizer the manufacturer of varenicline for lectures and advice. All other authors declare no competing interests.
Peer review
Peer reviewer information.
Nature Reviews Disease Primers thanks Jamie Brown, Elisardo Iglesias and Ming Li for their contribution to the peer review of this work.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Related links
CTRI website: https://d3futrf33lk36a.cloudfront.net/wp-content/uploads/sites/240/2019/04/Meds-Chart.pdf
Philip Morris International: https://www.pmi.com/
Rights and permissions
Reprints and permissions
About this article
Cite this article.
Le Foll, B., Piper, M.E., Fowler, C.D. et al. Tobacco and nicotine use. Nat Rev Dis Primers 8 , 19 (2022). https://doi.org/10.1038/s41572-022-00346-w
Download citation
Accepted : 07 February 2022
Published : 24 March 2022
DOI : https://doi.org/10.1038/s41572-022-00346-w
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Integrated mrna- and mirna-sequencing analyses unveil the underlying mechanism of tobacco pollutant-induced developmental toxicity in zebrafish embryos.
- Jiasheng Chen
- Xiaoping Zhong
Journal of Translational Medicine (2024)
Influence of substance use on male reproductive health and offspring outcomes
- Jamie O. Lo
- Jason C. Hedges
- Charles A. Easley
Nature Reviews Urology (2024)
Reductions in smoking due to ratification of the Framework Convention for Tobacco Control in 171 countries
- Guillermo Paraje
- Mauricio Flores Muñoz
Nature Medicine (2024)
Impact of benzoic acid and 2,2’-methylenebis (6-tert-butyl-4-methylphenol) on the metabolome of flue-cured tobacco and rhizosphere microbial communities: implications for continuous cropping obstacles
- Qiulian Peng
- Jiayan Zhang
Plant and Soil (2024)
Nicotinic regulation of microglia: potential contributions to addiction
- Alexa R. Soares
- Marina R. Picciotto
Journal of Neural Transmission (2024)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
How a free, anonymous texting program may help teens quit vaping

Stephanie Sy Stephanie Sy
Satvi Sunkara Satvi Sunkara
Leave your feedback
- Copy URL https://www.pbs.org/newshour/show/how-a-free-anonymous-texting-program-may-help-teens-quit-vaping
More than 2 million American middle and high school students now use e-cigarettes, also known as “vaping." A clinical trial found that teens enrolled in the “This is Quitting” anonymous text message program were 35 percent more likely to report quitting after seven months. To learn more about youth nicotine addiction, Stephanie Sy spoke with Amanda Graham, the principal investigator of the study.
Read the Full Transcript
Notice: Transcripts are machine and human generated and lightly edited for accuracy. They may contain errors.
Stephanie Sy:
There is new evidence that a free texting program may help teens quit e-cigarettes, also known as vaping, more than 2 million American middle and high school students now use e-cigarettes. A clinical trial has found teens enrolled in the This is Quitting anonymous text message program where 35 percent more likely to report giving up vaping after seven months.
Doctor Amanda Graham is the principal investigator of the study and the Chief Health Officer at Truth Initiative, a nonprofit aimed at preventing youth nicotine addiction. Dr. Graham, thank you so much for joining us. So this program has been up and running for several years. How many teens have enrolled, and how did you reach them?
Dr. Amanda Graham, Chief Health Officer, Truth Initiative:
We launched the program in January of 2019 and since that time over 780,000 young people have enrolled. This is a program that serves 13 to 24 year olds, and we consistently see tens of thousands of young people enrolling every month of the program is promoted through the Truth campaign the national public education — public education campaign that we've run here at Truth Initiative since 1999 and that reaches young people where we know they're spending the majority of their day, which is on social media.
Briefly describe for us how this texting program works, and how did you design it specifically for the target audience here, which is young people.
Dr. Amanda Graham:
So this is a quit vaping program that we specifically designed to meet the needs of young people. It delivers proven behavior change techniques, things that we know are effective for helping people to break a nicotine addiction, and delivered through text messaging, which we know is the way that young people prefer to communicate.
The program is tailored by age, by the device type that they're using, and by their quit date, which ensures that we're delivering relevant support all throughout their quitting journey. It's a very interactive program. We deliver open ended questions, true, false questions, yes, no, things that are designed to engage young people throughout the process of using the program, and it's highly tailored.
One of the things I'll say that's unique to this program is that we've received tens of thousands of submissions from other program users wanting to support young people, and we folded their tips and advice and encouragement back into the program to convey that lots of other young people are quitting and that quitting successfully is possible.
You know, teen smoking, as you know, Dr, Graham, has been a problem for decades. How do e cigarettes present a different challenge than traditional cigarettes in trying to get teens to stop?
You know, one of the challenges has been the very rapid evolution of these devices over the past five or six years. We know that disposable devices in particular, have evolved to deliver much larger doses of nicotine, much stronger doses of nicotine, and they're relatively inexpensive. And we know that disposable e-cigarettes are the products that young people are using most.
You know, with cigarettes, there was always a clear signal to the end of a smoking episode when you got to the end of a cigarette. And with these big, chunky devices, some of them contain the average amount of nicotine that you would find in seven to 14 packs of cigarettes, that massive amount of nicotine is really what has changed the game for young people today.
And these were originally marketed as somehow safer than cigarettes, right? And now you have governments and bans on the flavorings, and yet they still seem to be so prevalent.
They're very popular among young people. Flavors are something that we know attract adolescents to using e-cigarettes, and they often don't know that most e-cigarettes do contain nicotine and that nicotine is highly addictive.
We also know that nicotine and these products are things that young people turn to, thinking that it will help alleviate stress, it will help alleviate anxiety and boredom. And so there's really important to get information out specifically to young people that there is no safe level of nicotine use.
You know, there's a different story when it comes to adult smokers, and where there may be evidence emerging that e-cigarettes may help some smokers to quit, and so there's a very fine line to tread in public health about how to craft the right message that warns young people about the dangers, but that leaves open the opportunity for smokers.
How effective is something like this texting program compared to something like nicotine replacement therapy, which you would see a full on nicotine addict that was an adult turning to?
So this is the first study of its kind. It's the first evidence that we have about what works for adolescents to help them quit vaping. What we saw was about a 10 percent percentage point difference between participants randomized to this text message intervention, about 38 percent of them quit, compared to about 28 percent in the control arm.
What I'll say is that many clinicians are prescribing nicotine replacement therapy for adolescents off label their support from some of the national bodies for doing this, because we know that a combination of medication and behavioral support can be most effective.
That is Dr. Amanda Graham with the nonprofit Truth Initiative. Doctor Graham, thanks so much for joining us.
Listen to this Segment

Watch the Full Episode
Stephanie Sy is a PBS News Hour correspondent and serves as anchor of PBS News Hour West. Throughout her career, she served in anchor and correspondent capacities for ABC News, Al Jazeera America, CBSN, CNN International, and PBS News Hour Weekend. Prior to joining NewsHour, she was with Yahoo News where she anchored coverage of the 2018 Midterm Elections and reported from Donald Trump’s victory party on Election Day 2016.
Satvi Sunkara is an associate producer for PBS News Weekend.
Support Provided By: Learn more
More Ways to Watch
Educate your inbox.
Subscribe to Here’s the Deal, our politics newsletter for analysis you won’t find anywhere else.
Thank you. Please check your inbox to confirm.
Study reveals how salt-based nicotine and menthol flavors influence e-cigarette use in young adults
- Download PDF Copy

A recent study published in JAMA Network Open examines how salt-based nicotine formulations and menthol flavorings impact nicotine levels and the subjective experience of using e-cigarettes in young adults.

E-cigarette use in young adults
Initially, e-cigarettes were marketed as a safer alternative to conventional cigarettes. However, young adults have become the primary consumers of e-cigarette products as compared to those of any other age group, which has led e-cigarettes to be the most commonly used tobacco product among young American adults.
In 2021, 20% of young adults were current vapers, whereas 10% of middle and high schoolers reported using e-cigarettes in 2023. The early use of e-cigarettes increases the risk of addiction, as daily vaping is currently reported by nearly 50% of young adults and 25% of teenagers in the United States.
Although the concentration of freebase nicotine in e-cigarettes is up to 90% lower than that in traditional cigarettes, the incorporation of various additives leads to the formation of nicotine salts and non-tobacco flavors that facilitate nicotine dependence. As a result, nicotine inhalation through e-cigarettes is smoother and easier, which increases their palatability for continuous use.
This innovation enabled the marketing of e-cigarettes with a nicotine concentration approximately three times higher than that of traditional freebase nicotine e-cigarettes, maximizing nicotine delivery .”
In conventional cigarettes, the presence of menthol reduces the harsh taste of nicotine while also increasing dependence. However, the effects of menthol in e-cigarettes remain unclear.
About the study
The current crossover randomized control trial (RCT) included 72 individuals between 21 and 25 years of age, all of whom reported e-cigarette usage. Study participants were provided with different salt-based or freebase nicotine products with 1% or 5% nicotine concentrations that were either menthol or tobacco-flavored.
In the first session, all study participants used their usual e-cigarette brand. In the following eight sessions, study participants were provided with any of the laboratory-formulated e-cigarette formulations. A five-minute 10-puff inhalation period was followed by 30 minutes of unrestricted vaping.
Related Stories
- Study: E-cigarette use linked to earlier onset of asthma
- Heightened risk of adverse neonatal outcomes from prenatal exposure to both cannabis and nicotine
- Prevalence of nicotine pouch use found to be low among U.S. adults
Blood samples were collected at baseline, five, 10, and 35 minutes during each vaping session for plasma analysis. A visual analog scale (VAS) was also used to assess the intensity of positive effects like desire, enjoyment, pleasure, and satisfaction during the vaping session.
Study participants were provided the Questionnaire of Smoking (QSU) to measure their urges and cravings for nicotine, as well as any withdrawal symptoms, during each vaping session. The duration, intensity, and frequency of puffs were recorded during each session.
What did the study show?
The mean participant age was 22, and nearly 60% of them were female. All study participants smoked at least one of the eight laboratory formulations.
Nicotine uptake
Salt-based nicotine e-cigarettes were associated with the highest nicotine uptake, especially with the 5% concentration. This led to mean plasma levels of 11.2 ng/mL and 17.2 ng/mL at five and 35 minutes, respectively.
Salt-based nicotine led to a 94% increase in plasma nicotine levels at five minutes, which subsequently decreased to 53% after 30 minutes of unrestricted vaping, as compared to freebase products. The 5% nicotine e-liquid increased plasma nicotine levels by about 50% and 65% at five and 35 minutes, respectively, compared to 1% nicotine.
Menthol flavoring increased plasma nicotine levels by 18% at 35 minutes, while no change was observed at five minutes.
Positive experience
Positive feelings were more likely with salt-based nicotine than with freebase e-cigarettes, with scores of 42.8 and 32, respectively. Similar findings were recorded with 1% and 5% nicotine products, with mean scores of 43.4 and 31.2, respectively. Menthol-flavored e-liquid was experienced more positively than tobacco-flavored products, at 43.2 and 31.5, respectively.
Tobacco-flavored 5% freebase nicotine had the least positive subjective outcomes, whereas menthol-flavored 5% nicotine salts had the highest subjective experiences for almost all positive measures.
Puff patterns
Puff intensity increased with nicotine salts and 1% concentration as compared to the freebase or 5% nicotine products.
The 1% e-liquid increased the total puff count by 47%, accompanied by a 20% increase in mean puff duration. Similar increases were observed in mean and total puff volumes and puff frequency.
Nicotine salt use led to 25% more puffs, whereas puff duration increased by 5% with approximately 10% higher mean and total puff volume. These effects were not attributed to menthol flavoring.
All laboratory e-liquids reduced nicotine urges and cravings, especially with the 5% concentration. The mean QSU-Desire score declined from 16.7 with the 1% formulation to 15.4 with 5% nicotine products.
Conclusions
The findings imply that salt-based nicotine formulations prevalent in the market may increase nicotine dependence among young adults already using e-cigarettes and warrant regulation .”
Current American vapes contain 5% nicotine as nicotine salts. Under standardized and unlimited vaping, nicotine levels in blood matched or exceeded those achieved by 10-12 puffs using an ordinary cigarette.
The positive experience and more intense puffing may increase the risk of addiction and abuse among young people using these products. Thus, regulators are advised to consider limiting the level of acidic additives and menthol flavoring present in e-cigarettes. This intervention could maintain the efficacy of e-cigarettes for traditional cigarette users looking to quit while also limiting their appeal to young adults.
- Cho, Y. J., Mehta, T., Hinton, A., et al. (2024). E-Cigarette nicotine delivery among young adults by nicotine form, concentration, and flavor: a crossover randomized clinical trial. JAMA Network Open . doi:10.1001/jamanetworkopen.2024.26702.
Posted in: Child Health News | Medical Science News | Medical Research News
Tags: Addiction , Blood , Cigarette , Clinical Trial , Efficacy , Frequency , Laboratory , Nicotine , Smoking , Tobacco , Vaping

Dr. Liji Thomas
Dr. Liji Thomas is an OB-GYN, who graduated from the Government Medical College, University of Calicut, Kerala, in 2001. Liji practiced as a full-time consultant in obstetrics/gynecology in a private hospital for a few years following her graduation. She has counseled hundreds of patients facing issues from pregnancy-related problems and infertility, and has been in charge of over 2,000 deliveries, striving always to achieve a normal delivery rather than operative.
Please use one of the following formats to cite this article in your essay, paper or report:
Thomas, Liji. (2024, August 14). Study reveals how salt-based nicotine and menthol flavors influence e-cigarette use in young adults. News-Medical. Retrieved on August 14, 2024 from https://www.news-medical.net/news/20240814/Study-reveals-how-salt-based-nicotine-and-menthol-flavors-influence-e-cigarette-use-in-young-adults.aspx.
Thomas, Liji. "Study reveals how salt-based nicotine and menthol flavors influence e-cigarette use in young adults". News-Medical . 14 August 2024. <https://www.news-medical.net/news/20240814/Study-reveals-how-salt-based-nicotine-and-menthol-flavors-influence-e-cigarette-use-in-young-adults.aspx>.
Thomas, Liji. "Study reveals how salt-based nicotine and menthol flavors influence e-cigarette use in young adults". News-Medical. https://www.news-medical.net/news/20240814/Study-reveals-how-salt-based-nicotine-and-menthol-flavors-influence-e-cigarette-use-in-young-adults.aspx. (accessed August 14, 2024).
Thomas, Liji. 2024. Study reveals how salt-based nicotine and menthol flavors influence e-cigarette use in young adults . News-Medical, viewed 14 August 2024, https://www.news-medical.net/news/20240814/Study-reveals-how-salt-based-nicotine-and-menthol-flavors-influence-e-cigarette-use-in-young-adults.aspx.
Suggested Reading

Cancel reply to comment
- Trending Stories
- Latest Interviews
- Top Health Articles

Addressing Important Cardiac Biology Questions with Shotgun Top-Down Proteomics
In this interview conducted at Pittcon 2024, we spoke to Professor John Yates about capturing cardiomyocyte cell-to-cell heterogeneity via shotgun top-down proteomics.

A Discussion with Hologic’s Tim Simpson on the Future of Cervical Cancer Screening
Tim Simpson
Hologic’s Tim Simpson Discusses the Future of Cervical Cancer Screening.

From Waste to Taste: The Transformative Power of Fermented Foods
Maria Marco
In this interview conducted at Pittcon 2024 in San Diego, Maria Marco discusses her research on the health benefits, safety, and waste reduction potential of fermented foods, and the microbial processes involved in their production.

Latest News

Newsletters you may be interested in
Your AI Powered Scientific Assistant
Hi, I'm Azthena, you can trust me to find commercial scientific answers from News-Medical.net.
A few things you need to know before we start. Please read and accept to continue.
- Use of “Azthena” is subject to the terms and conditions of use as set out by OpenAI .
- Content provided on any AZoNetwork sites are subject to the site Terms & Conditions and Privacy Policy .
- Large Language Models can make mistakes. Consider checking important information.
Great. Ask your question.
Azthena may occasionally provide inaccurate responses. Read the full terms .
While we only use edited and approved content for Azthena answers, it may on occasions provide incorrect responses. Please confirm any data provided with the related suppliers or authors. We do not provide medical advice, if you search for medical information you must always consult a medical professional before acting on any information provided.
Your questions, but not your email details will be shared with OpenAI and retained for 30 days in accordance with their privacy principles.
Please do not ask questions that use sensitive or confidential information.
Read the full Terms & Conditions .
Provide Feedback

Duke Health
News & media.
- News Releases
- In The News
- Organization News
- Social Media
- Duke Health Blog
Some E-Cigarette Chemicals Mimic Nicotine, Possibly Bypassing Regulation
DURHAM, N.C. – In what appears to be an effort to bypass public health regulations covering vaping products, some tobacco companies have begun replacing nicotine in e-cigarettes with related chemicals that have similar properties but unknown health effects, Duke Health researchers report.
In a research letter appearing Aug. 7 in JAMA , study authors at Duke and Yale University also found that the quantity of these chemicals, known as nicotine analogs, are not accurately disclosed on the packaging.
“Vaping products containing nicotine are subject to federal laws that prohibit sales to people under the age of 21,” said study co-author Sairam V. Jabba, D.V.M., Ph.D., a senior research scientist at Duke University School of Medicine.
“Nicotine analogs are currently not subject to the FDA process and have not been studied for their health effects,” Jabba said. "Our analysis of some of these analog-containing vaping products sold in the U.S. found significant and concerning inaccuracies in the ingredients these products claim to contain and what they actually contain. Further, it’s possible manufacturers are attempting to avoid FDA tobacco regulation.”
One chemical, known as 6-methyl nicotine, has been shown in rodent experiments to be far more potent than nicotine in targeting the brain’s nicotine receptors and more toxic than nicotine. Another, called nicotinamide, is marketed as targeting the same brain receptors as nicotine, despite evidence it does not bind to these receptors.
The nicotine analogs were included in flavored e-cigarettes, which prior research has indicated are preferred by youths and those who vape for the first time.
Jabba and colleagues, including co-senior author Sven Eric Jordt, Ph.D., analyzed an e-cigarette product sold under the brand name Spree Bar, which comes in at least nine flavors and is listed as containing 5 percent 6-methyl nicotine. Study results showed the actual amount of the chemical was about 88% less than labeled. The e-cigarettes also included an artificial sweetener that is up to 13,000 times sweeter than table sugar, and an artificial coolant that mimics menthol’s effects.
A second brand of e-cigarettes -- marketed as Nixotine, Nixodine, Nixamide and Nic-Safe – contained a nicotine analog called nicotinamide, also at levels lower than the labels indicated, and combined with undisclosed amounts of 6-methyl nicotine. This brand did not include sweeteners or coolants.
“These products appear to be designed to circumvent the laws and regulations in place to protect people -- especially children -- from the harmful effects of smoking and tobacco use,” Jordt said. “We do not know what these chemicals do when they are heated and inhaled. These are questions that should be answered before we allow products on the market.”
In addition to Jordt and Jabba, study authors include Hanno C. Erythropel, Peter Silinski, Paul T. Anastas, Suchitra Krishnan-Sarin and Julie B. Zimmerman.
Yale’s Tobacco Center of Regulatory Science received funding support for the study from the National Institute on Drug Abuse, which is part of the National Institutes of Health (U54DA036151), and the Center for Tobacco Products of the FDA. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH or the FDA.
- Children's Health
Teenage Smoking and Solution to This Problem Essay
- To find inspiration for your paper and overcome writer’s block
- As a source of information (ensure proper referencing)
- As a template for you assignment
Introduction
The underlying causes of teenage smoking and possible solutions, conclusions.
Nicotine addiction among teenagers has recently become one of the most pressing problems in the modern American society. Overall, the attempts made by anti-smoking campaigners hardly yield any results, because they mostly focus on harmfulness of tobacco smoking and the publics’ awareness of the problem, itself, but they do not eradicate the underlying causes of teenage smoking. It is possible to single out three factors that contribute to teenage addiction to nicotine. The considerable shift in social and political thought should be made in order to eliminate these factors. Furthermore, it is worth mentioning that it cannot be done it by compulsion. Perhaps it would more prudent to illustrate this statement.
Accessibility of tobacco products. Children can easily purchase cigarettes in vending machines, and in this case, no one can prevent them from doing it. Additionally, every shop places tobacco products in the forefront, which certainly attracts the attention of the would-be buyer (such technique can be applied not only to children or teenagers, but also to adults). Tobacco manufactures produce such commercials that make smoking look fashionable or even attractive.
Anti-smoking campaigners state that tobacco products should be made more expensive. Such method can be effective; however, it may arouse a wave of protest from manufactures, because the government cannot prohibit them to display their products. As regards price increase, it should be mentioned that such policy can have adverse effects on the economy of the country. Many amendments to the existing legislation should be made, in order to implement such policy. The measures that have already been taken can only reduce the effects of the advertising campaign, though they cannot eliminate the root cause, accessibility of tobacco products.
The impact of parents. It is estimated that approximately seventy three percent of teenagers, addicted to nicotine, have smoking parents. Psychologists believe, that we are inclined to emulate the behavior of our parents (at least subconsciously). The major problem is that very often parents do not realize that they incite their children to smoke. As the Department of Health states, various programs should be launched in order to increase parents awareness of this fact. It is believed that educators can make a considerable contribution, because they can influence not only the students but also their parents.
The influence of popular culture. As it has already been mentioned earlier, we tend to emulate the behavior of other people. Recent researches have proved that there is direct relation between nicotine addiction among teenagers and the tendencies in modern pop culture. Unwillingly some of Hollywood stars make smoking habits almost fashionable. For instance, when John Travolta smokes on television, smoking, itself inevitable becomes an inseparable part of the so-called “cool” behavior. The power that popular icons exercise over the unmolded minds of the young generation is immense. However, the government can hardly affect film industry, because such intervention verges on censorship and it can be viewed as the violation of the Fourth Amendment. It is considered that some of these films, featuring movie stars smoking should rated as R. However, such measures can make Hollywood production literally unavailable, to teenagers.
Now, that the major causes of cause of teenage smoking are identified, it is quite possible to conclude that the government is not able to eradicate all of them by force, the only possible solution is to increase public awareness of the problem, especially parents. Moreover, popular icons should understand that their behavior often drives children or teenagers to smoking. Nevertheless, it should be borne in mind that the existing legislation cannot change current situation.
- Substance Abuse. Drinking by Caroline Knapp
- Smoking Causes and Plausible Arguments
- Anti-Smoking Communication Campaign's Analysis
- Social Marketing: The Truth Anti-Smoking Campaign
- Rhetorical Analysis of Articles on Sweatshops
- Sex and Drugs in Southeast Asia
- Antismoking Campaigns in Dubai: Effectiveness and Impact
- Ranking the Health Hazards of Drugs
- Juvenile Drinking as a Social Problem
- The Debate About Lowering the Drinking Age
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2021, October 20). Teenage Smoking and Solution to This Problem. https://ivypanda.com/essays/teenage-smoking-and-solution-to-this-problem/
"Teenage Smoking and Solution to This Problem." IvyPanda , 20 Oct. 2021, ivypanda.com/essays/teenage-smoking-and-solution-to-this-problem/.
IvyPanda . (2021) 'Teenage Smoking and Solution to This Problem'. 20 October.
IvyPanda . 2021. "Teenage Smoking and Solution to This Problem." October 20, 2021. https://ivypanda.com/essays/teenage-smoking-and-solution-to-this-problem/.
1. IvyPanda . "Teenage Smoking and Solution to This Problem." October 20, 2021. https://ivypanda.com/essays/teenage-smoking-and-solution-to-this-problem/.
Bibliography
IvyPanda . "Teenage Smoking and Solution to This Problem." October 20, 2021. https://ivypanda.com/essays/teenage-smoking-and-solution-to-this-problem/.
- Alzheimer's disease & dementia
- Arthritis & Rheumatism
- Attention deficit disorders
- Autism spectrum disorders
- Biomedical technology
- Diseases, Conditions, Syndromes
- Endocrinology & Metabolism
- Gastroenterology
- Gerontology & Geriatrics
- Health informatics
- Inflammatory disorders
- Medical economics
- Medical research
- Medications
- Neuroscience
- Obstetrics & gynaecology
- Oncology & Cancer
- Ophthalmology
- Overweight & Obesity
- Parkinson's & Movement disorders
- Psychology & Psychiatry
- Radiology & Imaging
- Sleep disorders
- Sports medicine & Kinesiology
- Vaccination
- Breast cancer
- Cardiovascular disease
- Chronic obstructive pulmonary disease
- Colon cancer
- Coronary artery disease
- Heart attack
- Heart disease
- High blood pressure
- Kidney disease
- Lung cancer
- Multiple sclerosis
- Myocardial infarction
- Ovarian cancer
- Post traumatic stress disorder
- Rheumatoid arthritis
- Schizophrenia
- Skin cancer
- Type 2 diabetes
- Full List »
share this!
August 7, 2024
This article has been reviewed according to Science X's editorial process and policies . Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
Some e-cigarette chemicals mimic nicotine, possibly bypassing regulation
by Duke University Medical Center

In what appears to be an effort to bypass public health regulations covering vaping products, some tobacco companies have begun replacing nicotine in e-cigarettes with related chemicals that have similar properties but unknown health effects, Duke Health researchers report.
In a research letter appearing Aug. 7 in JAMA , study authors at Duke and Yale University also found that the quantity of these chemicals, known as nicotine analogs, are not accurately disclosed on the packaging.
"Vaping products containing nicotine are subject to federal laws that prohibit sales to people under the age of 21," said study co-author Sairam V. Jabba, D.V.M., Ph.D., a senior research scientist at Duke University School of Medicine.
"Nicotine analogs are currently not subject to the FDA process and have not been studied for their health effects ," Jabba said.
"Our analysis of some of these analog-containing vaping products sold in the U.S. found significant and concerning inaccuracies in the ingredients these products claim to contain and what they actually contain. Further, it's possible manufacturers are attempting to avoid FDA tobacco regulation."
One chemical , known as 6-methyl nicotine, has been shown in rodent experiments to be far more potent than nicotine in targeting the brain's nicotine receptors and more toxic than nicotine. Another, called nicotinamide, is marketed as targeting the same brain receptors as nicotine, despite evidence it does not bind to these receptors.
The nicotine analogs were included in flavored e-cigarettes, which prior research has indicated are preferred by youths and those who vape for the first time.
Jabba and colleagues, including co-senior author Sven Eric Jordt, Ph.D., analyzed an e-cigarette product sold under the brand name Spree Bar, which comes in at least nine flavors and is listed as containing 5% 6-methyl nicotine. Study results showed the actual amount of the chemical was about 88% less than labeled.
The e-cigarettes also included an artificial sweetener that is up to 13,000 times sweeter than table sugar, and an artificial coolant that mimics menthol's effects.
A second brand of e-cigarettes—marketed as Nixotine, Nixodine, Nixamide and Nic-Safe—contained a nicotine analog called nicotinamide, also at levels lower than the labels indicated, and combined with undisclosed amounts of 6-methyl nicotine . This brand did not include sweeteners or coolants.
"These products appear to be designed to circumvent the laws and regulations in place to protect people—especially children—from the harmful effects of smoking and tobacco use," Jordt said.
"We do not know what these chemicals do when they are heated and inhaled. These are questions that should be answered before we allow products on the market."
Explore further
Feedback to editors

Study reveals diet as main risk factor for colon cancer in younger adults
4 hours ago

New brain-computer interface allows man with ALS to 'speak' again

International study detects consciousness in unresponsive patients with severe brain injury

New clue into the curious case of our aging immune system


New research poised to transform approach to diagnosing and treating acute leukemia in children

Researchers find a way to target the inflammation of endometriosis
5 hours ago

Multiple sclerosis study finds COVID-19 vaccine not tied to relapse

New insights into brain's reward circuitry could aid addiction treatment

Child-parent therapy has biological benefits for traumatized kids
6 hours ago

Unexplainable chronic itch shows unique blood biomarkers that could eventually lead to new targeted treatments
Related stories.

'Tobacco-free nicotine' claims could lead non-smokers to try E-cigarettes
Nov 1, 2021

Increasing use and awareness of oral nicotine pouches detailed
Jun 16, 2024

Study finds youth have misperceptions about synthetic nicotine in e-cigarettes
May 16, 2023

Nicotine pouches are being marketed to young people on social media. But are they safe, or even legal?
Feb 26, 2024

As menthol ban nears, big tobacco is adding synthetic version to cigarettes instead
Oct 11, 2023

AMA calls for greater electronic cigarette regulation
Aug 7, 2018
Recommended for you

An implantable sensor could reverse opioid overdoses
10 hours ago

Hooked on a feeling: Opioids evoke positive feelings through a newly identified brain region
Aug 12, 2024

Key factor found in drug-context links, relapse
Aug 9, 2024

New study defines relationships among heparan and chondroitin sulfate and associated proteins involved in drug abuse
Aug 8, 2024

Text messaging can help teens kick the vaping habit
Let us know if there is a problem with our content.
Use this form if you have come across a typo, inaccuracy or would like to send an edit request for the content on this page. For general inquiries, please use our contact form . For general feedback, use the public comments section below (please adhere to guidelines ).
Please select the most appropriate category to facilitate processing of your request
Thank you for taking time to provide your feedback to the editors.
Your feedback is important to us. However, we do not guarantee individual replies due to the high volume of messages.
E-mail the story
Your email address is used only to let the recipient know who sent the email. Neither your address nor the recipient's address will be used for any other purpose. The information you enter will appear in your e-mail message and is not retained by Medical Xpress in any form.
Newsletter sign up
Get weekly and/or daily updates delivered to your inbox. You can unsubscribe at any time and we'll never share your details to third parties.
More information Privacy policy
Donate and enjoy an ad-free experience
We keep our content available to everyone. Consider supporting Science X's mission by getting a premium account.
E-mail newsletter

- Health A to Z
- Alternative Medicine
- Blood Disorders
- Bone and Joint
- Cardiovascular Diseases
- Child Health
- Coronavirus
- Dental Care
- Digestive System
- Disabilities
- Drug Center
- Ear, Nose, and Throat
- Environmental Health
- Exercise And Fitness
- First Aid and Emergencies
- General Health
- Health Technology
- Hearing Loss
- Hypertension
- Infectious Disease
- LGBTQ Health
- Liver Health
- Men's Health
- Mental Health
- Pain Management
- Public Health
- Pulmonology
- Senior Health
- Sexual Health
- Skin Health
- Women's Health
- News For Medical Professionals
- Our Products
- Consumer News
- Physician's Briefing
- HealthDay TV
- Wellness Library
- HealthDay Living
- Conference Coverage
- Custom Products
- Health Writing
- Health Editing
- Video Production
- Medical Review
Are Vape Makers Using Dubious Nicotine 'Mimics' to Bypass Regulations?
Key takeaways.
Nicotine analogs are starting to show up in vaping products as tobacco companies try to dodge FDA regulation
The analogs act differently than nicotine, sometimes more powerfully and other times activating different brain receptors
The analysis showed that the products’ contents often don’t match the labeling
THURSDAY, Aug. 8, 2024 (HealthDay News) -- That vape pen might contain something even worse than nicotine, new research warns.
Tobacco companies may be trying to duck federal restrictions on vaping products by replacing nicotine with “nicotine analogs” -- related chemicals that have similar properties but unknown health effects, researchers report.
“Vaping products containing nicotine are subject to federal laws that prohibit sales to people under the age of 21,” explained researcher Dr. Sairam Jabba , a toxicologist at Duke University School of Medicine, in Durham, N.C. “Nicotine analogs are currently not subject to the FDA process and have not been studied for their health effects.”
“It’s possible manufacturers are attempting to avoid FDA tobacco regulation,” Jabba added in a Duke news release.
A lab analysis of nicotine analog vapes sold in the United States also “found significant and concerning inaccuracies in the ingredients these products claim to contain and what they actually contain,” Jabba said.
For example, a vaping brand called Spree Bar, which comes in at least nine flavors, is listed as containing 5% 6-methyl nicotine, researchers said.
A nicotine analog, 6-methyl nicotine has been shown in rodent experiments to be far more potent in targeting the brain’s nicotine receptors, researchers noted. It’s also more toxic than nicotine.
Analysis of the Spree Bar products found they contained 88% less 6-methyl nicotine than labeled. They also contained an artificial sweetener up to 13,000 times sweeter than table sugar and an artificial coolant that mimics menthol.
Another analog called nicotinamide is being marketed as targeting the same brain receptors as nicotine, even though evidence has shown it doesn’t bind to those receptors, researchers said.
E-cigarettes labeled as containing nicotinamide -- Nixotine, Nixodine, Nixamide and Nic-Safe -- had levels lower than their labels indicated, and were combined with undisclosed amounts of 6-methyl nicotine, researchers found.
“These products appear to be designed to circumvent the laws and regulations in place to protect people -- especially children -- from the harmful effects of smoking and tobacco use,” said co-senior researcher Sven Eric Jordt , research project director with the Yale Tobacco Center of Regulatory Science.
“We do not know what these chemicals do when they are heated and inhaled,” Jordt stressed. “These are questions that should be answered before we allow products on the market.”
In late May, a coalition of anti-tobacco groups warned the U.S. Food and Drug Administration of at least three nicotine analog products being sold in the United States.
Two of the products, Spree Bar and a snuff made by Outlaw Dip Co., argue on web sites and in promotional videos that their products are not subject to FDA regulation, their letter to FDA Commissioner Dr. Robert Califf noted.
However, the promotional materials also promise the same sort of effects from nicotine analogs that people get from actual nicotine, the letter added.
The letter quotes Spree Bar promotional materials as promising that the product “provides the same satisfaction, pleasure and enjoyment as traditional tobacco products and nicotine e-cigarettes.”
The FDA letter was co-signed by the American Cancer Society Cancer Action Network, American Heart Association, American Lung Association, Campaign for Tobacco-Free Kids, Parents Against Vaping E-cigarettes and Truth Initiative.
The research was published Aug. 7 in the Journal of the American Medical Association .
More information
The American Lung Association has more on nicotine .
SOURCE: Duke University, news release, Aug. 7, 2024
What This Means For You
Parents should dissuade their children from any form of tobacco use, even if the products tout nicotine analogs rather than actual nicotine.
Related Stories

- Foundation for a Smoke-Free World
This page was last edited on 07 August 2024, at 14:21.

In May 2024 the Foundation for a Smoke-Free World (FSFW) rebranded to Global Action to End Smoking (GAES). 1 2 See Global Action to End Smoking
The Foundation for a Smoke-Free World (FSFW) describes itself as “an independent, non-profit organization” 3 that was established and is “operated free from the control or influence of any third party”, which “makes grants and supports medical, agricultural, and scientific research to end smoking and its health effects and to address the impact of reduced worldwide demand for tobacco”. 4 5
It was established in September 2017 and formally launched at the Global Tobacco and Nicotine Forum 2017 , a tobacco-industry funded event. 6 7
FSFW’s tax returns, up until 2023, showed that it remained solely funded by Philip Morris International (PMI), 8 9 10 11 12 despite the fact that in September 2023 the Foundation announced that the pledge agreement between PMI and FSFW was being terminated, with PMI paying a final grant of US$122.5 million to the Foundation, on top of an annual payment of US$17.5 million paid in July 2023 (see below for more details). 13 This pledge termination coincided with the appointment of Clifford E. Douglas as FSFW President and CEO (see below ). 2 12
FSFW’s tax return covering the calendar year 2022, filed on 15 May 2023, showed that PMI contributed US$17.5 million for that year. 11 According to the 2022 pledge agreement, the Foundation was permitted to draw upon up to $US35 million from PMI in 2022, but only received the minimum annual amount, as required by PMI, of $US17.5 million. 14 This represented the fourth significant reduction in annual contribution by PMI in four years. PMI initially pledged US$80 million per year (in 2019), but in 2020 only contributed US$45 million. 8 9 This was further reduced to US$40 million in 2021, 10 and then to US$35 million in 2022. 11
The FSFW tax returns, for the period covering 2020 to 2022, showed that despite publicly claiming to focus funding on low and middle-income countries (LMICs), in reality, each year an average of 8% of available funding was granted to organisations in LMICs, while 85% of funding went to organisations based in the US, UK and EU. 9 15 16 11 17
For further analysis of FSFW’s tax returns 2018-2022 see the STOP Industry Brief 5 Questions to Ask: FSFW’s Tax Returns Suggest It Is Not a Credible Voice
Furthermore, analysis reveals that grants and contributions are not primarily focused on funding scientific research but rather appear to be in line with the Foundation’s public relations and advocacy strategies. Only one in six of the grantees listed in the 2019 tax return appeared to be based within academic institutions. 8 18 For more information on the new grantees and issues around the lack of transparency of FSFW on its award granting, go to Foundation for a Smoke-Free World Grantees . For a briefing on the top 10 takeaways from the Foundation’s 2019 tax return see exposetobacco.org.
Its 2018 tax return showed US$7.6 million of spending on “communications.” 19
There is detailed background information on the Foundation’s staff, grants, how it frames itself and counter arguments in the Tobacco Tactics Resources section .
Visit the Foundation for a Smoke-Free World: Research Database to find out more about its research outputs
Main Staff at the Foundation
In October 2021 FSFW announced that President and Board Director Derek Yach would be leaving the organisation. He was replaced by Heidi Goldstein and David Janazzo as Interim Co-Presidents. 20 21
In October 2023, FSFW announced the appointment of Clifford E. Douglas as President and Chief Executive Officer, replacing Heidi Goldstein and David Janazzo as Interim Co-Presidents. 2 Douglas was formerly director of the University of Michigan’s Tobacco Research Network and the American Cancer Society’s National Vice President for Tobacco Control. 2
David Janazzo appeared to leave the executive team, whilst Heidi Goldstein retained the concurrent roles of Executive Vice President, Chief Operating Officer and Chief Legal Officer. 22
An up-to-date listing of FSFW staff can be found on its website .
- See Foundation for a Smoke-Free World People for more details on staff and board members.
Relationship with the Tobacco Industry
Funded by philip morris international but claims independence.
The Foundation was established with funding from PMI. The tobacco company agreed to contribute US$80 million annually for the next 12 years starting from 2018, with specific contributions depending on the Foundation’s “requirements and operations”. 23
Although a large sum of money, US$80 million represents only 0.1% of PMI’s revenues and 1% of the company’s profits. 24 It is an insignificant sum compared to PMI’s annual spending on its longstanding sponsorship deal with Formula One racing giant Ferrari, which was quietly renewed in September 2017, and has previously been estimated to cost PMI in the region of US$160 million annually. 25 26
However, an updated version of the Pledge Agreement between PMI and FSFW dated September 2020 showed that PMI had decreased the Foundation’s funding. In 2020, it paid out only US$45 million, with plans to contribute the same amount again in 2021. From 2022-2029, PMI pledged to contribute US$35 million per year, a more than 50% reduction from its initial contributions in 2018 and 2019. 27 This pledge agreement ended in 2023. 13
The Foundation’s Launch
The day after the Foundation’s launch, film director Aaron Biebert (whose production company, Attention Era, was commissioned to launch the Foundation 28 29 ) claimed that “PMI will not be the only donor the Foundation. [Yach] will have other big donations coming from traditional sources like the Gates Foundation or Bloomberg Charities, but decided to get going now despite the potential reputational risk he faces”. 30 This claim was swiftly rebutted by both the Gates Foundation and Bloomberg Philanthropies. 31 32 Prior to June 2020, the Foundation asserted that it was “seeking and expects to receive funding from other sources as well”. 33 In June 2020, the language on the Foundation website’s “Funding” page changed to “The Foundation may seek funding from other sources as well”. 34 The 2019 tax return confirms that FSFW remains wholly funded by PMI. 8
The Foundation says that ‘independence’ and ‘transparency’ are its core values, and that the Foundation’s bylaws prevent PMI and other tobacco companies “from having any influence over how the Foundation spends its funds or focuses its activities”. 35 In a BMJ blog post 36 Yach reasserted that the Foundation operates independently from PMI, citing The Foundation’s ‘Certificate of Incorporation’, 37 ‘Bylaws’ 38 and ‘Pledge Agreement’ between the tobacco company and the Foundation 39 as evidence of this independence. The Foundation itself said it would operate “in a manner that ensures the Corporation’s freedom and independence from the influence of any commercial entity”. However, two independent analyses of the constitutive documents suggest that this is not the case. 40 41
One, for example, noted that the governing documents have “multiple loopholes” adding that the Foundation “cannot be regarded as independent”.
The McCabe Centre critique of these constitutive documents argued that there were several ways in which PMI would be able to influence the Foundation’s research agenda and practice. You can see an extensive analysis using this critique by visiting Foundation for a Smoke-Free World: How it Frames Itself .
Further evidence casting the Foundation’s independence came to light in September 2020 when FSFW uploaded an amended version of its Pledge Agreement to its website (see above). The amended agreement changed wording from “free from influence” to “free from improper influence” with regards to the input of PMI, other donors and third parties. A sentence immediately following this change makes it clear that communication with PMI is not prohibited:
“Nothing in this section or elsewhere in this pledge agreement or Foundation’s bylaws shall be interpreted to prohibit the Foundation from exchanging information or interacting with any third party, including but not limited to the pledgor, or other donors, in order to advance the Foundation’s purpose.” 27
On 13 January 2021, the former Director of Digital and Social Media at FSFW, Lourdes Liz, filed a civil complaint against the organisation, in a federal court in New York. 42 43 An amended version of the complaint was filed on 5 May 2021. 44 On June 25 the case was settled out of court and discontinued. 45
Termination of funding announced
In October 2023 the Foundation announced that the pledge agreement with PMI was being terminated, with PMI paying a final lump sum of US$122.5 million, effectively funding the Foundation at a rate of $US17.5 million per year until 2030. 13 46 US$17.5 million is the same value as that of the 2022 and 2023 grants awarded to FSFW by PMI. 11 13
Attempts to Engage with Global Public Health
In January 2019, a letter 47 signed by a total of 279 global health organisations and public health leaders was sent to the Director General and the Executive Board of the World Health Organization (WHO). The letter urged the WHO to reject any affiliation with the Foundation.
This was in response to a letter from FSFW 48 to the WHO’s Executive Board, published on 24th January 2019 within which Derek Yach argued for the “aligning…of…our goals to complement and support the WHO and the FCTC”. The Foundation’s letter to the WHO Executive Board talks of an “unprecedented opportunity to give global tobacco control new energy and a new path” which requires “the ability to seize opportunities as we strive to end smoking together”. 48
Visit Foundation for a Smoke-Free World: How it Frames Itself for an analysis of FSFW’s previous claims of support for the WHO FCTC.
At the same time, the Foundation’s sole funder, PMI, published a statement 49 of their own in January 2019 to coincide with the World Economic Forum in Davos, Switzerland. This statement, entitled ‘Davos 2019 – Time to Take Action’ argued that “anti-tobacco lobbies” and the tobacco industry needed to work collaboratively, calling this “a once in a lifetime opportunity” and writing that “we must seize it – and seize it together”. 49
On 23rd January 2019, the day before FSFW’s open letter to the WHO was published, PMI posted statement 50 announcing the publication of a PMI report 51 entitled ‘Public health – much harder than rocket science’. The report concludes that a “collaborative approach” to global health issues, one which includes corporations, is “possible and needed”.
Calls to reject funding from, and indeed any kind of involvement with, the Foundation have also previously come from many sources, including the WHO themselves:
World Health Organization (WHO) , The WHO Framework Convention on Tobacco Control Secretariat , The International Union against Tuberculosis and Lung Disease (The Union), The World Heart Federation , Deans from the School of Public Health at Johns Hopkins University , Environmental Rights Action and Friends of the Earth Nigeria (who have asked the University of Nigeria Nsukku not to work with FSFW), Polish Ministry of Health (sent a letter to all Polish university medical schools urging them not to accept any funds from FSFW), Campaign for Tobacco Free Kids and other experts in public health. 52 53
Critics have specifically pointed out that PMI continues to actively oppose tobacco control policies aimed at reducing tobacco use and promotes cigarettes to children in Africa and Asia. 52
Funding Scientists with Tobacco Industry Links
The Foundation has funded researchers with tobacco industry links, such as Riccardo Polosa , who has been previously funded by PMI, Jed Rose , who has previously been funded by Philip Morris and Neil McKeganey, who is a grant recipient of the Centre for Substance Use Research (CSUR) which is in turn funded by PMI, BAT , Fontem Ventures (a subsidiary of Imperial Tobacco ), and JUUL Labs (which is majority owned by Altria ). 54
Organisations Cut Ties with the Foundation
Several organisations who have received funds from the Foundation have decided to cut short or discontinue these links due to its ties to PMI. In 2019, BRAC Bangladesh (an NGO) announced that it would be returning the funding it had received from the Foundation in 2018. 55 The University of Cape Town also announced that it would not accept additional funding from the Foundation due to pressure from the university’s faculty of health sciences staff. 56 Oglivy, the public relations consultancy which was contracted by the Foundation in 2017/2018 announced in it no longer worked with the Foundation, in part “to avoid any conflict with its health clients”. 57
Difficulty in Publishing its Science
The Foundation has encountered difficulty in getting its own science published, despite Derek Yach, being on the review committees of several notable global public health journals. 21 The Foundation sought to publish a special issue of a journal titled “15 years after the Framework Convention on Tobacco control’s Adoption: Time for Greater Urgency and Focus” in the International Journal of Environmental Research and Public Health. 58 However, once the journal’s managing editors were made aware of the Foundation’s tobacco industry ties in October 2019, the special issue was withdrawn. 54
Beginning in May 2020, FSFW published a “special issue” of articles in the journal Drugs and Alcohol Today . The articles in this issue are all authored or co-authored by FSFW grantees or employees and are critical of the efficacy of WHO FCTC. Most articles recommend tobacco harm reduction . 59 In February 2021 an “Expression of Concern” statement was added by the publisher, emerald insight, to all articles in the FCTC special edition “to inform readers that credible concerns have been raised regarding the editorial process for this article”. 60
The journal is edited by Axel Klein. 61 Klein is a grantee of FSFW, through his consultancy A.C.K. Consulting. 62 A.C.K. received US$100,000 from FSFW in 2018. 63 Sudhanshu Patwardhan was described as a “guest editor” of the issue. 64 Patwardhan is also a FSFW grantee through his company, the Centre for Health Research and Education (CHRE). See our page on CHRE for more details.
Alignment with PMI
Although the Foundation wants to be seen as a body that is entirely separate from its funder, its actions and affiliations indicate otherwise. A study carried out in 2023 revealed similarities between the Foundation’s practices and previous industry attempts to influence science, including: producing tobacco industry-friendly research and opinion; obscuring industry involvement in science; funding third parties which criticise science that may threaten industry profitability; and promoting tobacco industry credibility. 65
Strategy Alignment
On multiple occasions, both the Foundation and its funder PMI have appeared to synchronise their global and in-country public relations and lobbying activities. 54
Global Synchronization
- Announcement of funding for Euromonitor : The Foundation and PMI Impact , an anti-illicit tobacco initiative also solely funded by PMI, announced funding for market research company Euromonitor within one day of each other. 66
- Use of “Unsmoke” branding: The same branding associated with PMI’s “Unsmoke” campaign was used by the Foundation in a promotional video on World No Tobacco Day 2019. 67
- Statements on the need for collaboration: In January 2019, both PMI and the Foundation published statements to international organisations advocating the need for collaboration between tobacco control and the tobacco industry. These statements used strikingly similar wording 48 49
- Funding of the same media outlet: Both PMI and the Foundation are listed as funders of the Influence Foundation , owner of the online harm reduction magazine, Filter . 68 69
- Responses to the Eighth Session of the Conference of Parties to the WHO FCTC (COP8) in Geneva: Both PMI and the Foundation, through its grantee Knowledge-Action-Change, released publications to coincide with COP8. PMI published a position statement advocating tobacco harm reduction policy interventions and consultation between governments and commercial producers of “emerging” tobacco and nicotine products. 70 The Foundation used the event to launch its “No Fire, No Smoke” report at a side event to the main COP summit. 71
In-Country Synchronization
- New Zealand: In 2019, the head of the Foundation-funded Centre for Research Excellence: Indigenous Sovereignty & Smoking (COREISS) , Marewa Glover, said that higher tobacco taxes in New Zealand would punish Māori and argued that “the compassionate thing to do would be to free up access to risk-reduced alternatives such as vaping, snus and heat-not-burn products”. 72 Following this statement, Philip Morris New Zealand has offered discounted e-cigarettes to the Māori population. 73
- Lobbying for weaker regulation of newer nicotine and tobacco products in Hong Kong: In April 2019, as the Hong Kong government was considering initiating a ban on these products, both PMI 74 and Foundation-funded Knowledge-Action-Change submitted evidence arguing against a potential ban. 75
- In December 2023 The Times newspaper published an article that described the various ways in which FSFW and some of its grantees, including KAC , Riccardo Polosa and CHRE , helped promote e-cigarettes in the UK. 76 The investigation described how “[d]octors, scientists and ‘independent’ activist groups funded by or linked to multinational tobacco companies who sell e-cigarettes have been at the forefront of efforts to ensure Britain retains its liberal approach to vaping”. 76
“Less as a Conflict of Interest than a Confluence of Interest”
In September 2017, Yach told UK newspaper The Guardian that “I have been working with PMI to establish a foundation to accelerate the end of smoking and tackle the consequences for tobacco farmers”. 77 Yach continued: “From the start, the intent has been to create an independent foundation that meets the very highest standards of legal and ethical norms”. 77
In January 2018, Yach gave an interview with the South African Broadcasting Corporation about the Foundation. When asked if PMI funding of FSFW represented a conflict of interest, Yach replied: “I see it less as a conflict of interest than a confluence of interest in terms of trying to lower the public health impact (of tobacco products), which is really devastating at the moment”. 78
However, claims of a confluence of interest between PMI and public health goals are undermined by the tobacco company’s behaviour in other arenas. In July 2017, only one month before the establishment of the Foundation, news agency Reuters published internal PMI documents demonstrating the tobacco company’s attempts to subvert provisions in the Framework Convention on Tobacco Control (FCTC). 79 80 Among other things, it showed the company had lobbied national governments to send non-health delegates to weaken FCTC provisions which usually require consensus to be adopted. The documents also showed that PMI was violating India’s anti-smoking regulations by promoting cigarettes in colourful adverts and handing out free cigarettes at nightclubs and bars frequented by young people. 80
An open letter to PMI dated 14 September 2017 and signed by 123 health groups urged the company, if it were serious about ‘designing a smoke-free future’, to “immediately cease the production, marketing and sale of cigarettes”. 81 PMI responded by an open letter claiming that if it were to stop selling cigarettes, smokers would not quit smoking but switch to its competitors’ brands. 82 “Indeed, our paramount business strategy is to replace cigarettes with less-harmful, smoke-free alternatives. That’s what we call a smoke-free future…”. A smoke-free future that is not based on smoking cessation, but on smokers switching from cigarettes to another tobacco product.
The WHO stated in 2017 that “research and advocacy funded by tobacco companies and their front groups cannot be accepted at face value. When it comes to the Foundation for a Smoke-Free World, there are a number of clear conflicts of interest involved with a tobacco company funding a purported health foundation, particularly if it promotes sale of tobacco and other products found in that company’s brand portfolio. WHO will not partner with the Foundation. Governments should not partner with the Foundation and the public health community should follow this lead.” 83
Working with Organisations with Long-Standing Links to Tobacco Industry
Many of the organisations the Foundation has worked with so far have long-standing links to the tobacco industry. For instance:
- APCO : Foundation board meeting minutes from May 2019 reveal that APCO Worldwide, a PR firm, was engaged by the Foundation to establish its presence in China. 84
- Ogilvy Group : From 2017 Ogilvy Public Relations Worldwide, has provided PR services to the Foundation. 85 86 Initially worth US$ 542,747, 85 the contract quickly grew to more than $5 million in 2018. 86 However this contract appears to have ended by 2020. 9
- Mercury : FSFW 2018 tax return shows that the Foundation paid Mercury US$664,616 for PR services rendered in 2018. 87 Maria Alvarado, Vice President of Mercury’s office in Austin, was listed as the main contact on FSFW press release for World No Smoking Day 2018. 88
- Feinstein Kean Healthcare : Tom Langford of PR consultancy Feinstein Kean Healthcare (FHK) was the spokesperson for the Foundation in September 2017. 89 FKH is part of the Ogilvy Group 90 , a large PR firm which has had long-standing links with the tobacco industry, including running advertising and PR campaigns for the tobacco industry from the 1950s. 91 In the Foundation’s inaugural meeting of the board of directors in November 2017, it was stated that Ogilvy FHK would be responsible for the Foundation’s “website launch, media outreach, stakeholder engagement and the global poll development and execution”. 92
- Kantar Public : Is part of Kantar , the consultancy and research group that conducted the Foundation’s 2018 ‘State of Smoking Survey’. The group has regularly worked for the tobacco industry, and is also linked to the tobacco industry through its parent company WPP group.
- McKinsey : The Foundation employed management consultants McKinsey in organising an October 2017 stakeholder event in London, despite the management consultancy being implicated in a 2017 corruption scandal in South Africa. 93 94 McKinsey has also helped tobacco companies with business planning going as far back as the 1950s, when McKinsey was advising Philip Morris on its research program. 95 In the 1980s, the firm advised Philip Morris USA how to optimise its cigarette sales and marketing processes. 96 97 In the 1990s, McKinsey worked with British American Tobacco . 98
- Baker and Hostetler LLP : In 2015, law firm Baker and Hostetler LLP represented tobacco companies Philip Morris, RJ Reynolds , Liggett and Lorillard in arbitration over proposed adjustments to the payments from the Tobacco Master Settlement Agreement 99 100 101 In 2018, the Foundation for a Smoke-Free World stated that this same law firm had offered them ‘guidance and input’ but in the 2020 tax return they were not listed. 9
- Ernst & Young : Auditors Ernst & Young have tobacco links stretching back years, mainly with British American Tobacco, and have advised on lobbying as well as providing reports which support industry policies in key areas. 8 9 10 11 Ernst & Young not only audits the Foundation, a subsidiary of the audit firm is also a grantee .
- Ruder Finn : In September 2020, Ruder Finn Asia conducted outreach to institutions including the Centres for Disease Control to promote FSFW’s Tobacco Transformation Index. 102 It was paid just over US$2m for public relations services in 2020. 9
Other Contractors
In addition to using companies with established tobacco-industry links, the Foundation has, according to its tax returns, 103 contracted other firms:
- MarketKonnect , a subsidiary of APCO , was paid US$1,137,992 in 2019 for consulting services but little has been revealed about the exact nature of this work which did not appear to continue in 2020. 8 9
- Signals Analytics was paid US$2.1m in 2019 and a further US$2m in 2020 9 to develop ways of monitoring information around harm reduction. It was also asked to look at three specific language groups: English, Japanese and Mandarin. In 2021 Signals Analytics received US$1,527,278 for “data platform development”, and a further US$1,214,201 in 2022. 10 11
- A-Connect provided unspecified management consultancy work in 2018 worth US$610,508 while Cross My Heart Productions, a California media company, was employed the same year for US$770,073 to produce videos. 104
- New York-based Transperfect Translations was paid US$324,000 for website translations in 2020 while Ferguson Cardo, based in Scotland, founded by former FSFW advisor Richard Ferguson, was paid US$326,000 in 2020 and helped produce a report on tobacco trends. 105 9
- CSDConsulting in Switzerland was paid US$240,376 in 2020 for unspecified consulting services. 9 CSD consulting was founded by Chitra Subramaniam, a journalist and FSFW consultant who has co-authored articles critical of the WHO FCTC alongside Derek Yach. 106 107
- Feng Insight consulting company run by Jeanne-Marie Gescher, a lawyer, 108 received US$720,393 in 2021 and $366,016 in 2022. 10 11 In 2019 Feng Insight produced research on “Industry Transformation” in China for FSFW. Gescher is an honorary advisor to British Ambassadors in China and two-time chair of the British Chamber of Commerce. 109 This consultancy continued in 2023. 12
- Glassman Enterprises received £210,000 in 2021 for a report for the International Commission to Reignite the Fight Against Smoking, which is funded by the FSFW. 10 Glassman Enterprises is run by James Glassman, a journalist, author and former Under Secretary for Public Diplomacy and Public Affairs. 110 111 Glassman is chair of the International Commission.. The organisation’s report in September 2021 says that: “Despite bad actions in the past, the tobacco industry is well positioned to contribute to tobacco control through innovation in THR [tobacco harm reduction] products, just as the pharmaceutical industry innovated with vaccines and therapeutics to fight COVID.” 112 In 2003 a profile in Washington Monthly described Glassman as the inventor of “journo-lobbying”, a lobbying method that attempts to “dominate the entire intellectual environment in which officials make policy decisions, which means funding everything from think tanks to issue ads to phony grassroots pressure groups.” 113
- Actum, a global consultancy firm established in 2021 by 12 ex-partners of the PR firm Mercury , received $428,585 in 2022 for “communications”. 11 114 Actum’s team includes members of the British House of Lords and former US Senators. 115 This consultancy continued in 2023. 12
- Ramp Up Technology, a New York based IT support company, received $139,720 in 2022 for IT and website support. 11
Commissioning Evidence
The Foundation funds work through three main streams, or “core pillars” : Health, Science and Technology (HST); Agriculture and Livelihoods; and Industry Transformation. 116 Recipients have included International Network of Nicotine Consumers (INNCO), Knowledge Action Change and several “Centres of Excellence” , located globally. For a full list of third-party grant recipients, visit our page on the Foundation’s grantees .
The Foundation has also produced its own reports and working papers , which can be found on its website.
A full list of the Foundation’s published reports can be found on its website here .
- In June 2021, the private social media network SERMO was granted an unspecified amount to recruit doctors for an eight-month international study “related to cessation and tobacco harm reduction around the world”. 117 SERMO describes itself as the “World’s leading social platform for physicians”. 118 It purportedly makes money by selling user data and advertising pharmaceuticals to doctors. 119
- “Smoky Horizons: Tobacco and Empire in Asia, 1850-2000” by FSFW grantee Asia Public History Foundation examines the history of colonialism and tobacco growing in Asia in the 19 th and 20 th centuries. 120
- “Phasing Out Combustible Cigarettes” advocates for tobacco harm reduction to be a primary goal of tobacco control and warns against “misinformation” on newer nicotine and tobacco products . It was authored by Derek Yach. 120
- “Contradictions and Conflicts” by FSFW grantee Daniel Malan was launched as part of the lead up to the Tobacco Transformation Index . It outlines how state ownership of tobacco companies creates a “conflict of interest” with public health policymaking, and advocates for tobacco harm reduction. 120
- “Dubrovnik Consultation Summary” summarised the findings of the “2020 Dubrovnik Consultation”, which was due to take place in Dubrovnik, Croatia in mid-2020, but was postponed by the COVID-19 pandemic . This report draws on “expert contributions” submitted on the taxation of newer products, called “tobacco harm reduction products” in the report. Its foreword is authored by Derek Yach, Ayda Yurelki and Patricia Kovacevic, a former employee of PMI , Lorillard and Nicopure. 121 122
- “India Country Report” was released in July 2020 and concerns the healthcare implications, economy, regulation and use of tobacco products in India. Its foreword includes endorsements from Drs Pooja and Sudhanshu Patwardhan, directors of the UK-based grantee Centre for Health Research and Education . 123
- “Watching Briefs: Hungary” by FSFW employee Ayda Yurelki documents the “past, present and future of smoking in Hungary”. 120
- “COVID-19 State of Smoking Poll”: FSFW conducted an online poll in April 2020 Italy, India, South Africa, UK and the US (New York and California) to assess the impact of COVID on product use and smoking behaviours. Although it found “virtually no change in reported product consumption” and increased quit attentions and attempts, FSFW focussed on stockpiling behaviours of cigarette smokers. 124
- “Global Perceptions of Tobacco and Nicotine Products” was commissioned as a follow-up to the 2017 report. Nielsen, a FSFW grantee, conducted a survey in seven countries on demographic data, habits and perceptions of tobacco, and users of newer products. 120
- “Insurer Perspectives on Smoking Risks” was conducted by Marsh & McLennan Advantage Insights and Oliver Wyman (both consultancies). This report argued that insurers needed to “rethink how they quantify and reduce smoking risks”. It recommended “potential solutions leveraging emerging technologies, products, and processes to address these barriers”. 120 The Foundation’s focus on insurers here tallies with PMI’s efforts, through its subsidiary insurance group, Reviti , to connect with smokers and promote its newer nicotine and tobacco products through price and policy discounts.
- “Global Trends in Tobacco Production and Trade” was authored by Romita Shah, a Research Manager at the Foundation 21 ; Dianna Bartone, a former Research Analyst at the Foundation 125 and Richard Ferguson, Investment Advisor for the Foundation. 126 It concerned the tobacco manufacture supply chain and emphasised the shift in tobacco production away from high-income and towards low- and middle-income countries. The report was intended to be the first in a series analysing trends in tobacco production and trade. 120
- The 2019 update to the “Global Trends in Nicotine” (2018) report highlighted the growth of the e-cigarette and heated tobacco sectors. It was authored by David Janazzo, the Foundation’s Chief Financial Officer. 120
- “Business Transformation: An analysis of case studies relevant to achieving a smoke-free world” was prepared by Framework LLC for the Foundation. This report presented six cases of companies that have undertaken “significant business transformations” to demonstrate how corporate transformation can be successfully achieved. This aligned well with the stated goal of the Foundation to “foster discussion on the transformational possibilities of achieving a smoke-free world” – which itself echoes the stated goals of its funder. 120 127
- “Global Trends in Nicotine” marked the first report solely authored by the Foundation. It was one of a series intended to lay the groundwork for the Foundation’s “Industry Transformation” stream, and thus the Tobacco Transformation Index. It mainly analysed companies involved in nicotine delivery device manufacture, their geographic focuses and quantifying their output. 120
- Knowledge-Action-Change, founded by Gerry Stimson , published “No Fire, No Smoke: The Global State of Tobacco Harm Reduction 2018”. The “No Fire, No Smoke” report, which was launched in Geneva to coincide with the eighth WHO FCTC Conference of the Parties (COP8), warned against “over-prescriptive regulation and control” in tobacco control. 71
- In August 2018, the Foundation published a report prepared by EY-Parthenon called “Smoking Cessation Products and Services: Global Landscape Analysis”. The report was widely criticised by the public health and tobacco control community as biased, for not adding anything new to science and for “providing market research for PMI.” 128
- In March 2018 the Foundation published its first research output, a survey called “The State of Smoking” 129 by industry-linked Kantar . The survey focused on smoking prevalence rates across 13 different countries. Although ostensibly about understanding smoking in different countries, as the first step towards reducing smoking prevalence rates, it was criticised by experts in public health, who claimed that it worked as a tool with which to gauge the market for harm reduction products and provide “market research for PMI”. 130
Working Papers
Intended to “provide preliminary and timely access to ongoing research being generated by, or closely relevant to, the Foundation’s work”, the Foundation’s “Working Paper Series” are a series of articles posted on the Foundation’s website. Papers published here are not subject to an academic journal level of peer review. Rather, they undergo “at least one double blind peer review by an external expert.” 131 As of February 2020, the only working paper posted to the FSFW website is one funded through its own Agriculture and Livelihoods workstream:
- FSFW Working Paper No. 1: “Rural Perspectives on Alternatives to Tobacco Farming and Environmental Degradation in Malawi” 131
Initiatives
Below is a list of other Foundation initiatives and work projects. Although it does not attempt to be comprehensive, it does highlight the ways in which the Foundation has sought to orient itself as a legitimate funder and creator of independent research, and an expert on issues including tobacco control, agriculture and industry transformation. For more information on organisations that have received grants from the Foundation, visit our page on the grantees .
- In September 2020, the Foundation released its Tobacco Transformation Index (TTI). Read more on our dedicated page on the TTI.
- In 2019, the Foundation began publishing quarterly newsletters, first through its Agricultural Transformation Initiative (ATI) and later adding a Health, Science and Technology version. 132
- In September 2018, the Foundation issued a request for proposals for an annual ‘Index of Industry Actions to End Smoking in this Generation’. 133 The Foundation stated that the index would “critically evaluate industry progress toward achieving a smoke-free world and assess actions taken to undermine that progress.” This announcement was made at the Global Tobacco and Nicotine Forum 2018 . In March 2019, the Foundation announced that it had contracted Euromonitor , a market research organisation, and SustainAbility, a think tank and consultancy, to develop “the first ever Smoke-Free index” to monitor and assess the actions made by tobacco companies to change from traditional combustibles to alternative “smoke-free” products. This work was also the first commissioned in the Foundation’s “Industry Transformation” initiative, one of its core pillars through which it funds grants. 134 However, the Southeast Asia Tobacco Control Alliance (SEATCA) has published a Smoke-Free Index since 2016. SEATCA’s Smoke-Free Index was developed to assess the alliance of smoke-free policies in the Association of Southeast Asian Nations (ASEAN) with the WHO FCTC. In July 2019, SEATCA posted an official complaint on its website with a statement from its Executive Director, Dr Ulysses Dorotheo to say that “[the Foundation’s] use and trademarking of the term “Smoke-Free Index” is misleading, potentially confusing, and tantamount to wrongful appropriation of SEATCA’s intellectual property”. 135 Since November 2019, the Foundation has instead referred to its index as the “Tobacco Transformation Index” and released its first report in September 2020. 136 137
- In August 2018, the Foundation announced the publication of its preliminary Health, Science and Technology (HST) Agenda. 138 The Agenda outlined the Foundation’s research priorities including its focus on product development research in order to bring more ‘reduced risk’ products to market.
- Also in August 2018, the Foundation announced the launch of a Centre of Research Excellence on Indigenous Sovereignty and Smoking (COREISS) in New Zealand, 139 headed by public health researcher, Dr. Marewa Glover. This centre is one of a number proposed by the Foundation in different countries. 19 The Foundation has stated that by funding these research centres it “aims to develop the next generation of leaders and institutions that will accelerate the end of smoking”. 140 Two of the grantees receiving funds to set up ‘Centres of Excellence’, Riccardo Polosa and Neil McKeganey, have previous, direct financial links to PMI. Full details on the research centres, their purposes and the people involved can be found at Foundation for a Smoke-Free World Centres of Excellence .
- Alongside the HST Agenda, the Foundation launched a request in August 2018 for proposals on research concerning ‘Biomarkers of Nicotine Product Use.’ 141 Here, the Foundation outlined a 3-year, nearly US$10 million plan to fund research on biomarkers of exposure to different types of tobacco products.
- The Global Forum on Nicotine (GFN) and Knowledge Action Change (KAC) launched the Tobacco Harm Reduction Scholarship programme in 2018, to fund research into tobacco harm reduction . This programme is sponsored by FSFW. The programme awarded 15 projects up to a value of $7,500 each. 142 For more information on KAC and its scholarship programme see its dedicated page: Knowledge-Action-Change .
- In May 2018, it was reported that the Foundation was “in talks” to work in collaboration with the International Centre for Biotechnology (a UNESCO Category II Centre) at the University of Nigeria Nsukka. 143
- In March 2018, the Foundation launched its Agricultural Transformation Initiative (ATI) in Malawi, headed by Jim Lutzweiler. 144 In July 2018, it was announced that ATI would fund a US$10 million, 5-year project to set up a Center for Agricultural Transformation in Malawi to “contribute to the transformation of the agricultural sector and development of a knowledge economy in one of the world’s least developed countries.” 145
- In November 2017, the Foundation’s Board gave staff approval to make grants up to US$2 million up to March 2018 without Board approval. 92 The Foundation received 60 proposals in response to their first Call of Interest for Projects, and the Foundation was “to convene with grant-making experts and the strongest grant candidates in February 2018”. 146
- Since 2017, the Foundation has funded The Conrad Spirit of Innovation Challenge (in collaboration with the Conrad Foundation), a program which invites high-school students (aged 13-18 years old) to “design 21st century solutions to re-purpose global farmland that is currently used for tobacco production, especially in African countries”. 147 148 The 2019 focus of the program was on India, Malawi and China. 149 The Tobacco Control Research Group at the University of Bath contacted the Conrad Foundation to seek clarification of the nature of its sponsorship agreement with FSFW, but did not receive a reply. 150 For the 2019-2020 round, the Conrad Foundation added a special category, called “Re-purpose Farmlands & Tobacco Crops”, another challenge especially funded by the Foundation. 151 Registration for the 2020-21 Conrad Challenge opened 21 August 2020. 152
Speaking at Conferences & Events
Examples of events at which the Foundation presented, or was scheduled to present:
- In September 2020, a new event website called “15 Years Conference” was launched. It streamed a two day conference sponsored by FSFW on the FCTC and “the challenges and opportunities in tobacco control from the lenses of diversity, development and tobacco harm reduction”. 64 Almost all speakers were FSFW grantees . 153 The event sought to highlight the FSFW-authored special issue in the journal Drugs and Alcohol Today (DAT). The conference organising team included Axel Klein (ACK Consultants) 62 and Sudhanshu Patwardhan ( CHRE ), both FSFW grantees. 64 Klein, is also the Editor of DAT. 61 The University of Kent’s logo appears at the bottom of the “15 Years” website, alongside Emerald Publishing (who publish DAT). 64 Klein is listed as a member of the University of Kent Centre for Biocultural Diversity. 154 The nature of affiliation of this event with the University of Kent is, however, unclear. Klein’s public LinkedIn profile does not refer to the University of Kent. 155
- Also in September 2020, FSFW hosted a booth at the virtual Global Forum on Tobacco and Nicotine (GTNF). This is the same event at which the Foundation was launched three years previously. During the event, FSFW launched its Tobacco Transformation Index , as well as a new website called “Understanding Nicotine” (https://www.understandingnicotine.org/). 156 The website lacks any explicit reference to or branding for FSFW.
- In November 2019, the Agricultural Transformation Initiative (ATI) hosted the second Agricultural Transformation Summit in Malawi. 157
- In November 2018, the Agricultural Transformation Initiative hosted the Agricultural Transformation Summit (ATS) in Malawi. The ATS was attended by Prince Kapondamgaga, CEO of Farmers Union of Malawi, a Foundation grantee, and Dr Alexander Bulirani, Controller of Agriculture Services, Ministry of Agriculture, Irrigation and Water Development, among others. The Foundation announced the launch of a Malawi-based Center of Excellence , the Center for Agricultural Transformation , at the event, as well as the opening of new funding and a scholarship fund endowed by the Foundation at Lilongwe University of Agriculture & Natural Events. 158
- In February 2018, the African Institute of Corporate Citizenship (AICC) (whose self-stated aim is to ‘promote the role of business in development’) collaborated with FSFW, holding ‘consultative meetings’ in Malawi where stakeholders including government officials were due to meet with the Vice President of FSFW, Dyborn Chibonga, who also holds a role on the Board of Directors of AICC. 159 160 161
- The Brocher Foundation’s ‘Ethics of Global Population Health’ event: Yach was scheduled to speak at this five-day event hosted by the Brocher Foundation, from 28 May to 1 June 2018. 162 The Brocher Foundation states the event accepted “no funds from the tobacco industry or from any organizations supported by it”. On 29 May 2018, Yach was no longer listed as speaker on the Brocher Foundation’s website. 163
- Food Prize October 2017: FSFW hosted a session at the World Food Prize (an event that Yach has spoken at previously 164 ) called ‘An Exploration Into Food/Cash Crop Alternatives to Tobacco in Africa’. A website description of the event states that: “Foundation for a Smoke-Free World was founded in part to identify and promote alternate market-driven agricultural supply and value chains, as well as fundamental livelihood alternatives for current smallholder tobacco farmers in Africa. To be successful, this will require a new vision grounded in emerging science-based research, collaboration among corporate and civil society stakeholders based on the formation of new business relationships, change of market and political incentives, alignment of interest with the tobacco industry, and support of governments.” 165
- Food and Drug Law Institute Annual Conference October 2017: Yach gave a keynote address on ‘designing the future of tobacco control’. 166 167
- E-Cigarette Summit November 2017: Yach participated in a discussion about FSFW during a session by Prof. Jean Francois Etter titled ‘The good, the bad and the ugly about the foundation for a smoke-free world’. 168 (Professor Etter noted he consulted Yach in preparation for his presentation) 169
TobaccoTactics Resources
- Foundation for a Smoke-Free World People
- Foundation for a Smoke-Free World Centres of Excellence
- ‘ Foundation for a Smoke-Free World Grantees
- Foundation for a Smoke-Free World: How it Frames Itself
- Foundation for a Smoke-Free World: Research Database
- Philip Morris International
- Front Groups
- MarketKonnect
- Signals Analytics
- Influencing Science
- Influencing Science: Funding Scientists
TCRG Research
- The Foundation for a Smoke-Free World’s rebrand is imminent, but this industry-funded scientific lobby group remains a danger to tobacco control, T. Legg, Tobacco Control Research Group blog , 14 December 2023
- Document analysis of the Foundation for a Smoke-Free World’s scientific outputs and activities: a case study in contemporary tobacco industry agnogenesis , T. Legg, B. Clift, A. B. Gilmore, Tobacco Control, Published Online First: 03 May 2023. doi: 10.1136/tc-2022-057667
- Paying lip service to publication ethics: scientific publishing practices and the Foundation for a Smoke-Free World , T. Legg, M. Legendre, A.B. Gilmore, Tobacco Control , 2021 Nov;30(e1):e65-e72. doi: 10.1136/tobaccocontrol-2020-056003
- The Philip Morris-funded Foundation for a Smoke-Free World: tax return sheds light on funding activities , T.Legg, S.Peeters, P.Chamberlain, A.Gilmore, The Lancet , 6 June 2019
- Big Tobacco is funding the anti-smoking lobby but leaked documents reveal the real reason why , A. Rowell, The Conversation , 13 March 2018
Relevant Links
- Read the STOP report on the Foundation and PMI: Addiction At Any Cost: Philip Morris International Uncovered
- Look at the Top 10 Takeaways from the Foundation’s 2019 tax return.
- Stopping Tobacco Organizations and Products (STOP) Analyses of the Foundation for a Smoke-Free World’s Tax Returns
- Read the January 2020 open “cease and desist” letter from SEATCA and TCRG to the Foundation here .
- Tobacco Free Kids’ Industry Watch on the Foundation
- Foundation for a Smoke-Free World website homepage [archived]
- Global Action to End Smoking website homepage
- ↑ Global Action to End Smoking , website, undated, accessed May 2024
- ↑ a b c d FSFW, Foundation For A Smoke-Free World Names Clifford Douglas CEO As Global Voice In Smoking Cessation Work , FSFW website, 12 October 2023, accessed October 2023
- ↑ Foundation for a Smoke-Free World, About Us , FSFW website, undated, accessed May 2018
- ↑ Foundation for a Smoke-Free World, About Us , accessed May 2018
- ↑ D. Yach, The State of Smoking 2018 Global survey findings and insights , Foundation for a Smoke-Free World, Press Conference Presentation, 19 March 2018, accessed May 2018
- ↑ Foundation for a Smoke-Free World, Media Advisory: Foundation Forming to Eliminate Smoking Worldwide , 12 September 2017, accessed September 2017
- ↑ Global Tobacco & Nicotine Forum 2017 New York City, USA, September 12-14, 2017 , accessed September 2017
- ↑ a b c d e f Foundation for a Smoke-Free World, Form 990-PF , 2019 Tax Return, 15 May 2020, accessed May 2020
- ↑ a b c d e f g h i j k Foundation for a Smoke-Free World, Form 990-PF, 2020 Tax Return , 17 May 2021, accessed May 2021
- ↑ a b c d e f Foundation for a Smoke-Free World, Form 990-PF, 2021 Tax Return , 16 May 2022, accessed May 2022
- ↑ a b c d e f g h i j Foundation for a Smoke-Free World, Form 990-PF, 2022 Tax Return , 15 May 2023, accessed May 2023
- ↑ a b c d Foundation for a Smoke-Free World, Form 990-PF, 2023 Tax Return , 17 May 2024, accessed June 2024
- ↑ a b c d FSFW, Final grant agreement and termination of second amended and restated pledge agreement , FSFW website, 29 September 2023, accessed October 2023
- ↑ Amended and Restated Pledge Agreement , Foundation for a Smoke-Free World website, 12 December 2022, accessed May 2023
- ↑ STOP, FSFW’s 2020 Tax Return Reveals Deep Links to the Tobacco Industry + Other Findings , Industry Brief, 27 May 2021
- ↑ STOP, 10 Key Insights from the Foundation for a Smoke-Free World’s 2021 Tax Returns , Industry Brief, 1 June 2022, accessed June 2022.
- ↑ STOP, 5 Years In, 5 Questions to Ask: FSFW’s Tax Returns Suggest It Is Not a Credible Voice, Industry Brief , June 2023
- ↑ STOP, Big Tobacco front group still spending millions on spin, not science , press release, 18 May 2020, accessed May 2020
- ↑ a b Foundation for a Smoke-Free World, Form 990-PF , 2018 Tax Return, 13 May 2019, accessed May 2019
- ↑ Foundation for a Smoke-Free World, FOUNDATION FOR A SMOKE-FREE WORLD ANNOUNCES LEADERSHIP TRANSITION , Press Release, 25 October 2021, accessed May 2022
- ↑ a b c Foundation for a Smoke-Free World, Our Team , undated, accessed May 2022
- ↑ Foundation for a Smoke-Free World, Our Team , undated, accessed October 2023
- ↑ D. Meyer, Philip Morris Pledges $1 Billion to Anti-Smoking Foundation , Fortune , 13 September 2017, accessed September 2017
- ↑ S. Glantz, Derek Yach’s journey to the Dark Side is now complete , UCSF Center for Tobacco Control Research and Education, 13 September 2017, accessed September 2017
- ↑ L. Edmondson, Ferrari renews Philip Morris partnership , ESPN, 4 September 2017, accessed September 2017
- ↑ Philip Morris renews Ferrari sponsorship on the quiet , ESPN, 14 May 2015, accessed September 2017
- ↑ a b Amended and Restated Pledge Agreement , Foundation for a Smoke-Free World website, 28 September 2020, accessed November 2020
- ↑ Attention Era, A Billion Dollar Foundation , undated, accessed May 2018
- ↑ Vape Craft Incorporated, Interview with Aaron Biebert – A billion lives documentary , 23 April 2018, accessed May 2018
- ↑ A. Biebert, Email sent to undisclosed recipients on 14 September 2017 11:05pm titled “Dr. Derek Yach’s Billion Dollar Foundation Launches”
- ↑ K. Henning, Email to subscribers of FCA mailing list dated 15 September 2017 15:57:09, subject: Re: Fw: [fca_all] Derek Yach’s new foundation to support harm reduction research
- ↑ C. Lewis, Email to subscribers of FCA mailing list dated 15 September 2017 02:24, subject Re: [fca_all] Fw: Derek Yach’s new foundation to support harm reduction research
- ↑ Foundation for Smoke-Free World, Funding , FSFW website, undated, accessed May 2020
- ↑ Foundation for a Smoke-Free World, Funding , FSFW website, accessed June 2020
- ↑ Foundation for a Smoke-Free World, About Us , undated, accessed September 2017
- ↑ D. Yach, Building a Foundation to accelerate an end to smoking , 23 January 2018, BMJ opinion blog, accessed February 2018
- ↑ State of Delaware, Secretary of State, Division of Corporations, Certificate of incorporation of Foundation for a Smoke-Free World, Inc , 8 September 2017, accessed February 2018
- ↑ First amended and restated bylaws of Foundation for a Smoke-Free World, Inc , 19 September 2017, accessed February 2018
- ↑ Foundation for a Smoke-Free World, Pledge Agreement between PMI Global Services Inc., a Delaware corporation, and Foundation for a Smoke-Free World, Inc., a non-profit, non-stock Delaware corporation , 9 January 2018, accessed February 2018
- ↑ J. Liberman, The new Philip Morris-funded Foundation for a Smoke-Free World: independent or not? , McCabe Centre for Law & Cancer, 30 January 2018, accessed February 2018
- ↑ Y. Van der Eijk, L.Bero et al, Philip Morris International-funded ‘Foundation for a Smoke-Free World’: analysing its claims of independence , Tobacco Control , published Online First: 21 September 2018. doi: 10.1136/tobaccocontrol-2018-054278, accessed January 2019
- ↑ Case 1:21-cv-00281: Document 1, Filed 13 January 2021 at the United States District Court, Southern District of New York
- ↑ Campaign for Tobacco-Free Kids & STOP, Lawsuit Alleges Collaboration Between Philip Morris International and the Supposedly Independent Foundation for a Smoke-Free World , joint statement, 15 January 2020, available from exposetobacco.org
- ↑ Amended Complaint , Filed 5 May 2021 at the United States District Court, Southern District of New York
- ↑ Order Case is Discontinued and Settled , Filed 25 June 2021 at the United States District Court, Southern District of New York
- ↑ T. Legg, The Foundation for a Smoke-Free World’s rebrand is imminent, but this industry-funded scientific lobby group remains a danger to tobacco control , Tobacco Control Research Group blog, 14 December 2023
- ↑ Global Public Health Community, An open letter to the Director General and the Executive Board of the World Health Organization , Centre for Good Governance on Tobacco Control, 28 January 2019, accessed January 2019
- ↑ a b c Foundation for a Smoke-Free World, open letter to the WHO Executive Board , Foundation for a Smoke-Free World Website, 24 January 2019, accessed January 2019
- ↑ a b c Philip Morris International, Davos 2019 – Time to Take Action , Philip Morris International Website, January 2019, accessed January 2019
- ↑ Philip Morris International, Davos 2019 – Rethinking how to address global health issues , Philip Morris International Website, 23 January 2019, accessed January 2019
- ↑ Philip Morris International, Public health – much harder than rocket science , Philip Morris International Website, January 2019, accessed January 2019
- ↑ a b R. Malone, S. Chapman, P. Gupta, et al, A ‘Frank Statement’ for the 21st Century? , Tobacco Control , blog piece, 19 September 2017, accessed September 2017
- ↑ S. Chapman. Tobacco giant wants to eliminate smoking…and pigs might fly. BMJ 2017;358:j4443 doi: 10.1136/bmj.j4443
- ↑ a b c Stopping Tobacco Organizations and Products, Addiction At Any Cost: Philip Morris International Uncovered , STOP report, 20 February 2020,accessed February 2020
- ↑ Global Center for Good Governance in Tobacco Control, Tobacco Grants returned by Bangladesh NGO BRAC , GGTC website, 15 August 2019, accessed February 2020
- ↑ J. van Dyk, Dancing with the devil: UCT stubs out tobacco-funded unit , Bhekisisa Centre for Health Journalism website, 16 October 2019, accessed February 2020
- ↑ J. Owen, Health experts criticise tobacco-industry-funded foundation over PR spend , ‘’PRWeek’’ online, 12 June 2019, accessed February 2020
- ↑ International Journal of Environmental Research and Public Health, Special Issue “15 Years After the Framework Convention on Tobacco Control’s Adoption: Time for Greater Urgency and Focus” , MDPI website, undated, accessed February 2020
- ↑ Foundation for a Smoke-Free World, Drugs and Alcohol Today Journal Special Issue , undated, accessed August 2020
- ↑ emerald publishing, Special Issue: Framework Convention on Tobacco Control: lessons learned on harm reduction and public health , Drugs and Alcohol Today, Volume 20 Issue 3, accessed March 2021
- ↑ a b Editorial Team , Drugs and Alcohol Today, undated, accessed 28 September 2020
- ↑ a b Companies House, A.C.K. Consultants LLP , undated, accessed October 2020
- ↑ Foundation for a Smoke-Free World, Agriculture & Livelihoods Approved Grants , FSFW website, undated, accessed July 2020
- ↑ a b c d 15 Years Framework Convention on Tobacco Control , website, undated, accessed October 2020
- ↑ T. Legg, B. Clift, AB. Gilmore, Document analysis of the Foundation for a Smoke-Free World’s scientific outputs and activities: a case study in contemporary tobacco industry agnogenesis, Tobacco Control, Published Online First: 03 May 2023. doi: 10.1136/tc-2022-057667
- ↑ A.W.A. Gallagher and A.B. Gilmore, Euromonitor International now accepts tobacco industry funding: a win for PMI at the expense of research on the tobacco industry , Tobacco Control Blog, 8 April 2019, accessed February 2020
- ↑ Foundation for a Smoke-Free World, World No Tobacco Day 2019 , Youtube, 29 May 2019, accessed February 2020
- ↑ Filter, About the Influence Foundation , ‘’Filter’’ online, undated, accessed February 2020
- ↑ The Influence Foundation, About the Influence Foundation , Filter website, undated, accessed October 2022
- ↑ Philip Morris International, PMI Cop8 Position Statement , PMI website, 2 October 2018, accessed February 2020
- ↑ a b H. Shapiro, No Fire, No Smoke: Global State of Tobacco Harm Reduction , Knowledge-Action-Change, 2018, accessed February 2020
- ↑ The Centre of Research Excellence: Indigenous Sovereignty & Smoking, New Zealand’s Leading Tobacco Control Expert Questions Budget Tobacco Tax Increase , ‘’PR Newswire’’ online, 31 May 2019, accessed February 2020
- ↑ G. Espiner, Big Tobacco targeting Māori with e-cigarettes , ‘’RNZ’’ online, 11 July 2019, accessed February 2020
- ↑ Philip Morris Asia Limited, Submission for Public Hearing on 13th April, 2019 relating to the Smoking (Public Health) (Amendment) Bill 2019 , LC Paper No. CB(2)1175/18-19(32), Legislative Council of the Hong Kong Special Administrative Region of the People’s Republic of China, 8 April 2019, accessed February 2020
- ↑ Harry Shapiro, Submission by Knowledge Action Change (KAC) to the Hong Kong Legislature on the proposal to ban all safer nicotine products (SNP) , undated, accessed February 2020
- ↑ a b B. Kenber, Revealed: how tobacco giants are bankrolling secret pro-vaping campaign , The Times , 14 December 2023, accessed December 2023
- ↑ a b S. Boseley, Tobacco company launches foundation to stub out smoking , The Guardian , 13 September 2017, accessed September 2017
- ↑ SABC Digital News, Foundation for a Smoke-Free World , 2 January 2018, accessed February 2018
- ↑ A. Kalra, P. Bansal, et al, Part 1: Inside Philip Morris’ campaign to subvert the global anti-smoking treaty , Reuters , 15 July 2017, accessed October 2017
- ↑ a b A. Kalra, P. Bansal, et al, Part 2: Philip Morris takes aim at young people in India, and health officials are fuming , Reuters , 18 July 2017, accessed October 2017
- ↑ Open letter from 123 health groups to PMI , 14 September 2017, accessed October 2017
- ↑ Philip Morris International, Open Response to Letter of 14 September 2017 calling on PMI to stop selling cigarettes , 29 September 2017, accessed October 2017
- ↑ World Health Organization, WHO statement on Philip Morris funded Foundation for a Smoke-Free World , 28 September 2017, accessed May 2018
- ↑ Foundation for a Smoke-Free World, Inc., Minutes of a Special Meeting of the Board of Directors, 24 May 2019
- ↑ a b Foundation for a Smoke-Free World, 2017 Tax Return, 26 March 2018, accessed from Charity Navigator website, May 2019
- ↑ Foundation for a Smoke-Free World, Form 990-PF , 2018 Tax Return, 13 May 2019, accessed May 2019
- ↑ Foundation for a Smoke-Free World, New data show 75% of smokers in the UK have tried to quit but have been unsuccessful , 31 May 2018, accessed April 2019
- ↑ Foundation for a Smoke-Free World, Contact Us , undated accessed September 2017
- ↑ Ogilvy FKH, Ogilvy Relationship , undated, accessed September 2017
- ↑ Ogilvy & Mather, Corporate Culture , accessed April 2013
- ↑ a b Foundation for a Smoke-Free World, Minutes of the Inaugural Meeting of the Board of Directors , 3 November 2017, accessed May 2018
- ↑ J. Cotterill, M. Marriage, South African opposition sets sights on McKinsey. Financial Times , 13 September 2017
- ↑ J. Cotterill, M. Marriage, McKinsey drawn further into South Africa’s influence scandal. Financial Times , 28 September 2017
- ↑ A.C. Britton, Five Year Research Program- McKinsey Report , Truth Tobacco Industry Documents, 21 March 1957, Bates No: 1000304953-1000304956, accessed October 2017
- ↑ T. Beane, Final McKinsey Task Force Meeting , Truth Tobacco Industry Documents, 26 October 1988, Bates no: 2041161013-2041161014, accessed October 2017
- ↑ B. O’Brien, McKinsey Report , Truth Tobacco Industry Documents, 26 June 1987, Bates no: 2024667395-2024667396, accessed October 2017
- ↑ N. Davis, Letter from N Davis to KL Chugh regarding interim report from McKinsey , Truth Tobacco Industry Documents, 15 November 1994, Bates no: 500030225-500030226, accessed October 2017
- ↑ P. C. Maloney, Tobacco MSA panel wrongfully deducted over $127M from Pennsylvania’s settlement funds , 10 April 2015, Products Liability Law Daily, accessed May 2018
- ↑ Baker Hostetler, Professionals: Evan M. Mannering, Associate , accessed May 2018
- ↑ Baker Hostetler, Professionals: Elizabeth. B. McCallum, Partner , accessed May 2018
- ↑ Email from Ruder Finn Asia, Subject: Media Invite: Virtual Conference on Diversity and Harm Reduction in Global Tobacco Control Policy, 28 September 2020
- ↑ Foundation for a Smoke-Free World, Form 990-PF , 2019 Tax Return, 15 May 2020, accessed July 2020
- ↑ Foundation for a Smoke-Free World, Form 990-PF , 2018 Tax Return, 13 May 2019, accessed July 2020
- ↑ Ferguson Cardo, Research , website, undated, accessed May 20201
- ↑ D. Yach, E. Latif, C. Subramaniam, Deeper thought, wider discussion needed to improve global governance of pandemics , BMJ Rapid Responses, March 2021, accessed June 2021
- ↑ D. Yach, C. Subramaniam, WHO Doesn’t Help You Quit Smoking , BUSINESSWORLD, January 2021, accessed June 2021
- ↑ Companies House, FENG INSIGHT LTD , undated, accessed May 2022
- ↑ Battle of Ideas Festival, Jeanne-Marie Gescher , Battle of Ideas Festival website, 2015, accessed May 2022
- ↑ Open Corporates, Glassman Enterprises LLC , register entry, undated, accessed May 2022
- ↑ U.S. Chamber of Commerce Foundation, Ambassador James K. Glassman , website, undated, accessed May 2022
- ↑ The International Commission to Reignite the Fight Against Smoking, Commission Report: Reignite the Fight Against Smoking , fightagainstsmoking.org, September 2021, accessed May 2022
- ↑ N. Confessore, Meet the Press , Washington Monthly, 2 December 2003, accessed May 2022
- ↑ Actum, Actum LLC Launches Global Consultancy with Offices in Los Angeles, London, New York, Washington D.C., San Francisco and Sacramento , Global News Wire , 27 January 2022, accessed May 2023
- ↑ Actum, Our Team , Actum website, accessed April 2023
- ↑ Foundation for a Smoke-Free World, Core Pillars , undated, accessed February 2020
- ↑ A. Winkiewicz, email from SERMO to the University of Bath, Subject: Exclusive invitation to join the Doctors and Health Professionals Global Poll 2021 National Advisory Board, dated June 2021
- ↑ SERMO, For Physicians , SERMO.com, undated, accessed June 2021
- ↑ A. Kane, What is SERMO… and can we trust it? , The Medical Republic, April 2016, accessed June 2021
- ↑ a b c d e f g h i j Foundation for a Smoke-Free World, Reports Archive , FSFW website, undated, accessed February 2020
- ↑ Foundation for a Smoke-Free World, Tobacco Harm Reduction: Regulatory, Economic and Taxation Perspectives , July 2020, accessed August 2020
- ↑ Regulation Strategy, About us , undated, accessed October 2020
- ↑ Foundation for a Smoke-Free World, India Country Report , July 2020, accessed August 2020
- ↑ Foundation for a Smoke-Free World, COVID-19 State of Smoking Poll , May 2020, accessed August 2020
- ↑ D. Bartone, LinkedIn profile , undated, accessed February 2020
- ↑ R. Ferguson, LinkedIn profile , undated, accessed February 2020
- ↑ Philip Morris International, Delivering a smoke-free future: How long will PMI be in the cigarette business? , PMI website, undated, accessed February 2020
- ↑ T. Khan, Global smokers’ study criticised as biased , “Businesslive.co.za”, 20 March 2018, accessed February 2020
- ↑ Foundation for a Smoke-Free World, State of Smoking , accessed May 2018
- ↑ T. Kahn, Global smokers’ study criticised as biased , 20 March 2018, Business Day, accessed May 2018
- ↑ a b Foundation for a Smoke-Free World, Working Papers , FSFW website, undated, accessed February 2020
- ↑ Foundation for a Smoke-Free World, Newsletters , FSFW archive, undated, accessed February 2020
- ↑ Foundation for a Smoke-Free World, Foundation for a Smoke-Free World to impact tobacco industry and nicotine ecosystem and drive change through the smoke-free index , September 2018, accessed September 2018
- ↑ Foundation for a Smoke-Free World, Leading global research firms selected to create the first-ever Smoke-Free Index® , FSFW website, 18 March 2018, accessed February 2020
- ↑ Southeast Asia Tobacco Control Alliance, Foundation funded by Philip Morris hijacks SEATCA’s Smoke-Free Index , SEATCA website, 15 July 2019, accessed February 2020
- ↑ U. Dorotheo and A. Gilmore, SEATCA & University of Bath’s Open Letter to the PMI-funded Foundation for a Smoke-free World (FSFW) , SEATCA website, 24 January 2020, accessed February 2020
- ↑ Foundation for a Smoke-Free World, Tobacco Transformation Index website , undated, accessed September 2020
- ↑ Foundation for a Smoke-Free World, Foundation for a smoke-free world health, science, & technology (HST) preliminary agenda for public comment , August 2018, accessed September 2018
- ↑ Foundation for a Smoke-Free World, New centre of research excellence launched in New Zealand , August 2018, accessed September 2018
- ↑ Foundation for a Smoke-Free World, Centers of Excellence , 2019, accessed May 2019
- ↑ Foundation for a Smoke-Free World, Request for proposal: biomarkers of nicotine product use , August 2018, accessed September 2018
- ↑ Knowledge Action Change & Global Forum on Nicotine, Tobacco harm reduction scholarship programme , accessed February 2018
- ↑ Enviro News Nigeria, ERA wants varsity to refuse foundation tobacco research funds , 28 May 2018, accessed May 2018
- ↑ J. Lutzweiler, Back to the fundamentals , Foundation for a Smoke-Free World, News & Views, 19 March 2018, accessed May 2018
- ↑ Foundation for a Smoke-Free World, Foundation for a smoke-free world invites organizations to submit expressions of interest to operate a center for agricultural transformation in Malawi-$10 million for a five-year contract , 23 July 2018, accessed September 2018
- ↑ Foundation for a Smoke-Free World, Inc., Minutes of a Special Meeting of the Board of Directors , 28 December 2017, accessed February 2018
- ↑ Conrad Spirit of Innovation Challenge, Special 2017-2018 Category…Change the world today. Foundation for a smoke-free world , 2017, accessed February 2018
- ↑ Conrad Spirit of Innovation Challenge, Conrad Challenge Sponsors , 2017, accessed February 2018
- ↑ Foundation for a Smoke-Free World, Minutes of a Special Meeting of the Board of Directors June 21, 2018 , FSFW website, accessed September 2018
- ↑ Tobacco Control Research group, Email to the Conrad Foundation dated 21 February 2018, 12:32
- ↑ Conrad Foundation, 2019-2020 Special Category: Re-purposed Farmlands & Tobacco Crops , Conrad Challenge website, undated, accessed February 2020
- ↑ MindRocket Media Group, Registration Opens for 2020-21 Conrad Challenge , EINPresswire, 21 August 2020, accessed August 2020
- ↑ Event Programme , 15yearsconference.net, undated accessed September 2020
- ↑ University of Kent Centre for Biocultural Diversity, Dr Axel Klein , undated, accessed October 2020
- ↑ Axel Klein, LinkedIn profile, accessed 28 September 2020
- ↑ FSFW’s Virtual Booth for 2020 Global Tobacco and Nicotine Forum (GTNF) , undated, accessed September 2020
- ↑ M. Benn, Inspiring Agricultural Innovation and Transformation , FSFW blog, 25 November 2019, accessed February 2020
- ↑ M. Benn, Transformation Through Collaboration, Consortium, And Commitment , FSFW blog, 21 December 2018, accessed February 2020
- ↑ African Institute of Corporate Citizenship, Board Members. Board Director: Dyborn Chibonga , 2016, accessed May 2018
- ↑ African Institute of Corporate Citizenship, About AICC , accessed May 2018
- ↑ Foundation for a Smoke-Free World & African Institute for Corporate Citizenship, Smoke-Free World Consultative Meetings, Sunbird Capital Hotel, Malawi Facebook Event, 28 February 2018, accessed May 2018
- ↑ Bioethics.net, 2018 Brocher Academy in Global Public Health Event May 28th 2018 – 1st June , accessed May 2018
- ↑ Brocher Foundation, Events: 2018 Brocher Summer Academy in Population-level Bioethics, May 28 – June 1, 2018 , accessed May 2018
- ↑ The World Food Prize, 2010 Speaker Biographies 2013, accessed February 2018
- ↑ The World Food Prize, An Exploration Into Food/Cash Crop Alternatives to Tobacco in Africa , 2018, accessed February 2018
- ↑ Foundation for a Smoke-Free World, Designing the Future of Tobacco Control , 27 October 2017, accessed February 2018
- ↑ Food and Drug Law institute, Tobacco Products Regulation and policy Conference: Last Year’s Agenda , Last updated 4 January 2018, accessed February 2018
- ↑ I. Gray, Reflections on The 5th Annual E-Cigarette Summit 2017, The Royal Society, 17th November 2017 , undated, accessed February 2018
- ↑ J. Etter, The good, the bad and the ugly about the Foundation for a Smoke-Free World , 17 November 2017, accessed February 2018
- Countering Critics
- Harm Reduction
- Third Party Techniques
Warning: The NCBI web site requires JavaScript to function. more...
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Institute of Medicine (US) Committee on Preventing Nicotine Addiction in Children and Youths; Lynch BS, Bonnie RJ, editors. Growing up Tobacco Free: Preventing Nicotine Addiction in Children and Youths. Washington (DC): National Academies Press (US); 1994.
Growing up Tobacco Free: Preventing Nicotine Addiction in Children and Youths.
- Hardcopy Version at National Academies Press
2 THE NATURE OF NICOTINE ADDICTION *
Lily Lin, Jr. High School 158, Queens
Cigarettes and other forms of tobacco are addicting. Most smokers use tobacco regularly because they are addicted to nicotine. Furthermore, most smokers find it difficult to quit using tobacco because they are addicted to nicotine. Nicotine addiction develops in the first few years of cigarette smoking. that is, for most people during adolescence or early adulthood. Most smokers begin smoking during childhood or adolescence: 89% of daily smokers tried their first cigarette by or at age 18, and 71% of persons who have ever smoked daily began smoking daily by age 18 ( table 2-1 ). The earlier in life a child tries a cigarette the more likely he or she is to become a regular smoker (that is, to smoke monthly or more frequently) or a daily smoker. For example, 67% of children who initiate smoking in the sixth grade become regular adult smokers, and 46% of teenagers who initiate smoking in the eleventh grade become regular adult smokers. 1 Furthermore, the earlier a youth begins smoking, the more cigarettes he or she will smoke as an adult. 2 Prevention of tobacco addiction and the related health consequences, therefore, requires early intervention for children and adolescents. To understand why youths use tobacco and why prevention measures are necessary and preferable to cessation measures to deter tobacco use by youths, it is useful to understand nicotine dependency. This chapter reviews (1) the general aspects of nicotine dependency, derived from research primarily in adults, and (2) the evidence of nicotine dependency and the factors that promote initiation and progression of tobacco use by youths.
Cumulative percentages of recalled age at which persons aged 30 39 first tried a cigarette or began smoking daily.
- GENERAL ASPECTS OF NICOTINE ADDICTION
The Daily Nicotine Addiction Cycle
Given the pharmacologic properties of nicotine, a daily cycle of addiction can be described as follows. The first cigarette of the day produces substantial pharmacologic effects (pleasure, arousal, enhanced performance), but simultaneously the brain's chemistry changes and tolerance begins to develop. With subsequent cigarettes, nicotine accumulates in the body and is associated with the development of a greater level of tolerance. Withdrawal symptoms become more pronounced between successive cigarettes. The tolerance that develops over the day may be partially overcome by the transiently high brain levels of nicotine that occur immediately after the smoking of individual cigarettes, but the primary pleasurable effects of individual cigarettes tend to lessen throughout the day. As the day progresses, people tend to smoke more to relieve the symptoms of abstinence. Overnight abstinence allows considerable resensitization to the actions of nicotine, and the cycle begins again the next day.
What Is Addiction?
The World Health Organization (WHO) describes drug dependence as "a behavioral pattern in which the use of a given psychoactive drug is given a sharply higher priority over other behaviors that once had a significantly higher value." 3 In other words, the drug comes to control behavior to an extent considered detrimental to the individual or to society.
Historically, drug addiction meant that tolerance developed to the effects of a drug during repetitive use, and that after cessation of such use withdrawal symptoms emerged (termed physical dependence). The prototypical addictive drug was heroin, and drug addiction has had a connotation of social deviance or criminal behavior in the United States. This historical view of addiction was revised by the 1964 Expert Committee of the World Health Organization. As discussed in detail in the 1988 surgeon general's report, such a definition is narrow and does not address addictions such as cocaine or binge alcoholism. A definition based on concepts of drug dependence developed by expert committees of WHO and in publications of the National Institute on Drug Abuse (NIDA) and the American Psychiatric Association includes compulsive drug-seeking behavior, effect of the drug on the brain, and usually a need for the drug to maintain homeostasis. Specific criteria for a drug that produces dependence or addiction have been presented by the U.S. surgeon general ( table 2-2 ), and specific criteria for diagnosing drug dependence or addiction in individuals have been presented by the American Psychiatric Association ( table 2-3 ).
Criteria for drug dependence.
Criteria for substance dependence.
Pharmacologic Aspects of Nicotine
The pharmacologic effects of nicotine are essential to sustaining cigarette smoking. 4 Viewed another way, tobacco is used by people to deliver nicotine to the body. The primary physiologic effects of nicotine (reviewed in detail in the 1988 surgeon general's report) are listed below.
- Electroencephalographic desynchronization
- Increased circulating levels of catecholamines, vasopressin, growth hormone, adrenocorticotropic hormone, cortisol, prolactin, and beta-endorphin
- Increased metabolic rate
- Lipolysis, increased free fatty acids
- Heart rate acceleration
- Cutaneous and coronary vasoconstriction
- Increased cardiac output
- Increased blood pressure
- Skeletal muscle relaxation
Smokers give various explanations for their smoking. Many report that smoking produces arousal, particularly with the first few cigarettes of the day, and relaxation, particularly in stressful situations. Many smokers report that smoking helps them concentrate and lifts their mood. Nicotine has been shown to increase vigilance in the performance of repetitive tasks and to enhance selective attention. Smokers commonly report pleasure and reduced anger, tension, depression, and stress after smoking a cigarette. The extent to which the enhanced performance and mood after smoking are due to the relief of symptoms of abstinence or to an intrinsic enhancement effect on the brain is unclear. A few studies do show improvement in the performance of nonsmoking subjects after dosing with nicotine, suggesting at least some direct enhancement.
Some of the gratifying effects of nicotine are due to the relief of the symptoms of nicotine withdrawal. When nicotine use is abruptly stopped, withdrawal symptoms emerge. The typical symptoms are listed below.
- Restlessness
- Eating more than usual
- Anxiety/tension
- Irritability/anger
- Difficulty concentrating
- Excessive hunger
- Disorientation
- Loss of energy/fatigue
- Stomach or bowel problems
- Heart palpitations
- Craving cigarettes 5
Most withdrawal symptoms reach maximal intensity 24 to 48 hours after cessation of tobacco use and gradually diminish in intensity over several weeks. Some symptoms, such as eating more than usual, weight gain, and craving cigarettes (particularly in stressful situations) may persist for months or even years after cessation.
Actions of Nicotine on the Brain
The nicotine molecule is shaped like acetylcholine. Acetylcholine is a neurotransmitter, that is, a chemical naturally found in the body that is involved in transmitting information from one neuron to another. Receptors (specialized proteins that selectively bind drugs and initiate drug effects in the body) for acetylcholine are called cholinergic receptors. Nicotine acts on certain cholinergic receptors in the brain and other organs of the body. The receptors would normally be acted on by the body's own acetylcholine. By activating cholinergic receptors, nicotine enhances the release of other neurotransmitters and hormones including acetylcholine, norepinephrine, dopamine, vasopressin, serotonin, and beta-endorphin. The physiologic effects of nicotine include behavioral arousal and sympathetic neural activation. Release of specific neurotransmitters has been speculatively linked to particular reinforcing effects of nicotine ( figure 2-1 ). 6 For example, enhanced release of dopamine, norepinephrine, and serotonin may be associated with pleasure as well as appetite suppression, the latter of which may contribute to lower body weight. Release of acetylcholine may be associated with improved performance on behavioral tasks and improvement of memory. Release of beta-endorphin may be associated with reduction of anxiety and tension.
Source: Adapted from Pomerleau, O.F., and C. S. Pomerleau. "Neuro-regulators and the Reinforcement of Smoking: Towards a Biobehavioral Explanation." Neuroscience Behavioral Review 8 (1984): 503-513.
Tolerance and Withdrawal
With prolonged or repetitive exposure to nicotine, the brain cells adapt in such a way as to compensate for the actions of nicotine, that is, to return brain functioning to normal. This process is called neuroadaptation. Neuroadaptation is associated with an increasing number of nicotinic receptors in the brain. Neuroadaptation results in the development of tolerance, that is, a given level of nicotine comes to have less of an effect on the body, and higher levels of nicotine are needed to produce the effects that lower doses formerly produced. Substantial tolerance develops to the behavioral arousal and cardiovascular effects of nicotine when a person smokes multiple cigarettes or uses multiple doses of smokeless tobacco, even within the course of a single day. Regular tobacco users regain sensitivity to the effects of nicotine, at least in part, after overnight abstinence from tobacco.
When the brain has adapted so as to function normally in the presence of nicotine, it also becomes dependent on the presence of nicotine for normal functioning. When nicotine is not available (such as when a smoker stops smoking), the brain function becomes disturbed, resulting in a number of withdrawal symptoms, as mentioned above.
Absorption of Nicotine from Tobacco
Nicotine from tobacco smoke is rapidly absorbed into the systemic circulation after inhalation, then is quickly carried to various body organs including the brain. Nicotine levels in the blood rise quickly after smoking, with arterial blood levels exceeding venous levels in the first few minutes ( figure 2-2 ). Because nicotine is a weak base and is ionized at acid pH, there is little absorption of nicotine through the membranes of the mouth from the acidic smoke of blond (light-colored) tobacco. However, the smoke of pipes, cigars, and dark tobacco is more alkaline, so nicotine is absorbed through the mouth from these products. When oral snuff or chewing tobacco is used, nicotine is also absorbed through the mouth. Nicotine from oral snuff or chewing tobacco is absorbed more slowly than from cigarette smoke; peak plasma concentrations of nicotine in venous blood are similar.
* Average values for 10 subjects. Shaded bars show the period of tobacco (or nicotine) use. Vertical bars indicate ranges. Source: Adapted from Benowitz, Neal L., H. Porchet, L. Sheiner, and P. Jacob III. "Nicotine Absorption and Cardiovascular Effects (more...)
Distribution and Elimination of Nicotine from the Body
A cigarette delivers nicotine to the brain within 10 to 19 seconds from the start of a puff. The rapid passage of nicotine from the lungs to the arterial circulation to the brain provides for rapid behavioral reinforcement for smoking and for the possibility for the smoker to control levels of nicotine in the brain and to modulate pharmacologic effects. Nicotine is also distributed extensively to other body tissues. Slow release from tissues explains in part the elimination half-life of 2 to 3 hours.
Nicotine is eliminated primarily by liver metabolism. The rate of metabolism is quite variable from person to person, so the same level of nicotine intake may be associated with different concentrations of nicotine in the blood of different people. The main metabolite of nicotine, cotinine, has a long half-life (on average 17 hours) and has been widely used by researchers as a biochemical marker of nicotine exposure.
Intake and Accumulation of Nicotine During Cigarette Smoking
On the average, smoking a cigarette results in the absorption into the blood stream of about I mg of nicotine, but the range is from 0.5 to 3.0 mg. The elimination half-life of nicotine is 2 to 3 hours. This means that the level of nicotine in the blood decreases by one-half every 2 or 3 hours. It also means that after a single use of tobacco nicotine remains in the body for 8 to 12 hours. With repeated smoking, nicotine levels accumulate over 6 to 8 hours, plateauing through the remainder of the day, then gradually falling overnight. Thus, regular cigarette smoking results in continued exposure of the brain and body to nicotine.
Addiction and the Light or Occasional Smoker
Among adults the light or occasional smoker, that is, one who regularly smokes 5 or fewer cigarettes per day or who does not smoke every day, is in general less addicted than are daily smokers of more than 5 cigarettes per day. 7 Smoking appears to be reinforced for light smokers by the direct pharmacologic effects of nicotine, as described above, as well as by behavioral aspects of tobacco use, as described below. The use of tobacco in response to withdrawal symptoms is less of a factor in such tobacco users. Among adults, light or occasional smokers are relatively uncommon (less than 10% of adult smokers); 8 they have higher success in smoking cessation than do heavier smokers, although not all light smokers are able to quit. In contrast, many more children than adults are light or occasional smokers; however, light smoking by children is often not a stable pattern but, rather, represents a stage in escalation to becoming daily smokers.
Nicotine Compensation
The "low-yield" cigarette.
Some tobacco advertisements indicate that particular brands of cigarettes deliver less nicotine and tar than their competitors' brands, implying a health benefit to low-yield cigarettes. Some people switch to low-yield cigarettes in an attempt to reduce the health consequences of smoking, but that is an unlikely result. A daily smoker tends to regulate his or her nicotine intake to a specific level in order to achieve desired effects and to minimize withdrawal symptoms.
This nicotine regulation influences how smokers smoke cigarettes with various nicotine yields and how they respond to cutting down on the number of cigarettes they smoke per day. When smoking lower-yield cigarettes, smokers puff more frequently or more intensely than when smoking higher-yield cigarettes, presumably to obtain their usual specific level of nicotine from each cigarette. In switching from high-yield to low-yield cigarettes, smokers consume more nicotine from the low-yield cigarette than predicted by smoking machine tests. Conversely, smokers consume less nicotine than predicted from high-yield cigarettes.
The intake of nicotine, with blood cotinine or nicotine concentrations used as markers of nicotine intake, has been studied in large groups of people smoking their chosen brands of cigarettes. 9 In such studies, nicotine intake correlates only weakly with the advertised yield. The slope of the regression line between advertised nicotine yields and blood nicotine or cotinine levels is shallow, suggesting only small differences of intake from cigarettes of widely different nicotine yields. Because of this compensatory smoking, having smokers switch to low-yield cigarettes reduces the risk of smoking to a much lesser degree, if at all, than suggested by the decreases in yield.
Smoking Fewer Cigarettes
The regulation of nicotine intake by daily smokers is also apparent when the number of cigarettes available to a smoker is restricted. In one study of heavy smokers, when the number of cigarettes was reduced from unlimited (average 37 per day) to 5 cigarettes per day, the average intake of nicotine per cigarette tripled. 10 As a result, reducing the number of cigarettes to 15 per day had very little effect, and reducing to 5 cigarettes per day reduced the daily exposure to tobacco toxins only by 50%. This observation explains why many smokers who are instructed to quit report cutting down to about 10 cigarettes per day, but cannot reduce their consumption to fewer than 10. At 10 cigarettes per day smokers still can absorb adequate nicotine to maintain nicotine addiction.
Behavioral Aspects of Addiction
The behavior of smoking is maintained both by the direct pharmacologic effects of nicotine (including relief of withdrawal) and by learned responses. Anticipatory responses develop as a consequence of repetitive use of tobacco during which various kinds of gratifications from smoking occur in the presence of specific cues from the environment. For example, when a smoker encounters stressors or situational reminders of smoking, these stimuli revivify the pleasurable or other reinforcing aspects of smoking, which then generate the urge to smoke. Such recurrent anticipatory responses may persist 6 months or longer after physical dependence has been overcome, accounting for the relapses that occur beyond the first week or two after cessation of tobacco use. Such anticipatory responses probably also develop to some degree in occasional smokers.
There are various conceptualizations of the nature of the anticipatory response system. One is the conditioning model, in which learned associations between the effects of cigarette smoking and specific cues in the environment motivate smoking. Another model is self-regulation, in which high-risk situations activate cognitive processes in a form of pleasurable expectations and a reduced sense of personal control, which then increases the likelihood of smoking. 11 Examples of common anticipatory reactions include smoking after a meal, with a cup of coffee or an alcoholic beverage, during a break from work, while talking on the phone, or while with friends who smoke.
Of note, aspects of the drug-taking behavior itself often become pleasurable in addition to the pleasure afforded by the pharmacologic effects of nicotine. For example, manipulation of smoking materials or the taste, smell, or feel of tobacco smoke in the throat can become associated with the reinforcing effects of smoking and can become pleasurable in themselves. When a smoker becomes abstinent, he or she must learn not only to forego the pharmacologic pleasures afforded by the drug, but also the pleasure of engaging in those aspects of drug-taking behavior that have become pleasurable through anticipatory mechanisms.
Behavioral factors other than anticipatory mechanisms may also influence personal susceptibility to drug addiction. For example, some smokers, particularly Caucasian women, smoke as a means of maintaining lower body weight. 12 Certain characteristics of individuals appear to promote initiation of smoking and the development of nicotine addiction, as reviewed in more detail in a later section.
Addiction to Smokeless Tobacco
''Smokeless tobacco" (SLT) refers to oral and nasal snuff and chewing tobacco. Smokeless tobacco, commonly used by youths, particularly in rural areas, may be highly addicting. 13 Considerable nicotine is absorbed from smokeless tobacco. A classification scheme for levels of SLT use or addiction is problematic. The nicotine content of smokeless products is not known to the public and the nicotine content of the tobacco provides only a rough estimate of actual nicotine intake. Recent laboratory analysis of popular brands of moist snuff revealed large differences in nicotine content, from 5.7 to 30.7 mg/g. 14 Two studies found evidence for higher addiction levels and greater oral pathology among Copenhagen® users. 15 The systemic dose of nicotine derived from smokeless tobacco can be estimated by measuring blood nicotine levels after SLT use. The systemic dose of nicotine from snuff is 3.6 mg, and for chewing tobacco it is 4.5 mg; an average dose from smoking a cigarette is I mg. 16 No standard self-report measures exist for smokeless tobacco consumption, such as those for smoking. One way to estimate addiction level is to use the number of tins or pouches of SLT product consumed per week, the product used (high, medium, or low nicotine content), and the amount of time (minutes) the tobacco is in the mouth. In surveys, though not standardized, questions typically ask if the individual used one or more dips or chews in the past 7 days, used one or more dips or chews in the past 24 hours (or day), and uses dip or chew daily. In intervention studies, typical measures of the pattern and amount of SLT use have included the number of dips per day, the number of minutes the dip or chew is kept in the mouth, the number of days a tin or pouch lasts, and the number of tins or pouches used per week. All four measures of SLT intercorrelate significantly with saliva cotinine assays. 17 Most users report using a tin or pouch every day or two, but adolescent boys report that a tin of snuff lasts 5 days and that they use an average of five dips a day. 18
Most cessation studies define a "regular user" as someone who has used SLT daily for the past year. Schroeder and colleagues suggest categorizing the SLT user as a light, moderate, or heavy user according to the amount of nicotine consumed per week from chewing tobacco or snuff products. 19 Other measures of the pattern of SLT use and addiction have been adapted from the smoking cessation literature. The Fagerström Tolerance Questionnaire 20 has been adapted and used with a scale applicable to SLT users by simply converting cigarette-based items to SLT-use items, for example, "I chew or dip first thing in the morning or within 30 minutes of waking up in the morning." 21 The scale has been validated by its correlation with saliva cotinine. Some items of this scale have been positively correlated with self-reported severity of nicotine withdrawal. 22
Blood nicotine concentrations throughout the day are similar in regular smokers and people who also use smokeless tobacco. 23 Plasma cotinine levels among regular users of smokeless tobacco are in many cases similar to those of cigarette smokers. 24 Abstinence from smokeless tobacco use results in signs and symptoms of nicotine deprivation that are similar to those seen in smokers after they stop smoking. 25 These symptoms are reversed by administration of tobacco or nicotine gum. Swedish oral snuff users report difficulty in quitting and many consider themselves to be addicted, reporting as much difficulty in giving up smokeless tobacco use as is reported by cigarette smokers trying to quit smoking. 26 Finally, there is evidence that when deprived of snuff, regular snuff users will smoke cigarettes to satisfy their need for nicotine. 27 The regular use of snuff or chewing tobacco by a child therefore increases the likelihood that subsequently the person will take up regular cigarette smoking. 28
Comparison of Nicotine Addiction with Other Drug Addictions
It is obvious that all drugs of dependence share psychoactivity, produce pleasure, and are shown to reinforce drug-taking behavior. (For a detailed review of the comparison of nicotine and other drug addictions, see the 1988 surgeon general's report.) The nature of nicotine's psychoactivity, which is generally subtle and is consistent with high levels of cognitive performance, is considerably different from that of heroin or cocaine, which produce intense euphoria and may be disruptive to performance. The subtle psychoactive effect of nicotine is experienced hundreds of times (puffs) per day, and exerts a powerful effect on behavior over time. Although the psychoactive effect of nicotine is less dramatic than that of other drugs, the strength of the addiction is as powerful or more powerful. The consequences of its addictiveness are clearly more dramatic, making tobacco use the number one health problem in the United States.
Compulsive use can be observed with all addictive drugs, but the compulsiveness is manifested in different patterns. Some drugs, such as cocaine and heroin, are used by some addicted persons only intermittently, that is, every few days or even at longer intervals, but the compulsion to use the drug does repeat. Cigarette smokers, on the other hand, rarely go more than a day without nicotine. At work or in other public places where smoking is proscribed, smokers may need to take numerous breaks throughout the day to smoke. No single physical dependence model describes the way in which drug use is continually compelled, but these compulsive behaviors are strongly controlled by the addictive actions of the drugs.
"Addiction is needing to smoke first thing in the morning, not just when you are bored or hanging out with your friends. " -adolescent in focus group
Use despite harmful effects confirms the difficulty that many persons have in quitting drug use. This is clearly evident to clinicians who treat alcoholics with chronic liver disease, heroin addicts with infective endocarditis, and cigarette smokers. For example, only 50% of smokers who suffer acute myocardial infarction quit smoking, despite a physician's admonition to do so. 29 It has been argued that for many activities that entail risk, such as sex, sunbathing, and skiing, the individual assumes a risk and makes a free choice, and that the same is true of cigarette smoking. However, life-long smoking results in the premature death of one in three smokers and the disability of a great number of smokers from chronic lung disease, indicating a substantially different level of risk.
Relapse rates after abstinence appear to be similar for tobacco, heroin, and alcohol; about 60% of quitters relapse within 3 months and 75% within 6 months. 30 These relapse rates have been observed in clients discharged from treatment programs. It has been argued that the relapse rate for tobacco among spontaneous quitters might be lower than these rates. Recent data indicate that relapse rates for smokers who have undergone minimal intervention treatment in a physician's office and who have successfully abstained for 24 hours are 25% at 2 days, 50% at 1 week, and 75% at 2 months, 31 whereas two-thirds of smokers who quit on their own relapse within 2 days. 32
Recurrent drug cravings have been described for each of the addicting drugs, although there has been considerable debate about the use of the term "craving." A better term might be "strong desire" to use a drug. When desires for different drugs were compared among polydrug abusers, most of whom smoked cigarettes, the reported intensity of desire for cigarettes when they are not available was as high as or higher than for heroin, alcohol, or cocaine when the latter were not available. 33
Tolerance to the various drugs of abuse has been well documented, although the time course varies. Different time courses of tolerance might influence the pattern of drug use. For example, tolerance to many effects of nicotine develops quickly, within the day, and there is resensitization of many responses overnight. Intermittent high levels of nicotine in the brain from individual puffs might also overcome tolerance to some extent so that effects can be experienced from individual cigarettes. Presumably because of the daily cycle of tolerance and resensitization, daily doses of nicotine tend to stabilize, and, after a period of dose escalation in the first few years, many smokers smoke the same number of cigarettes each day. In contrast, tolerance lasts longer in an alcoholic who drinks all day and whose brain is more or less continually exposed to alcohol throughout the day. Tolerance likewise occurs during cocaine binges when progressively larger doses are used in an attempt to maintain a cocaine high; however, between binges, sensitivity to cocaine may be regained. One implication of the development of tolerance is that regular smokers are able to consume far greater amounts of tobacco smoke and associated toxins than if they had not become tolerant.
Physical dependence has been well characterized for smokers as well as for other drug abusers. It has been argued that a marked stereotypic syndrome occurs in a person after stopping use of heroin or alcohol, whereas the withdrawal symptoms after stopping smoking vary widely in nature and magnitude and, in one study, were not sufficiently present in 22% of quitters to constitute a diagnosis of withdrawal. 34 Although it is true that smoking does not result in seizures or delirium tremens, withdrawal from smoking can be extremely disruptive to personal life. Nicotine withdrawal may be viewed as closer to that of withdrawal from other stimulants such as cocaine: the withdrawal syndrome is not life-threatening but it profoundly affects behavior and remains a strong impetus to recurrent drug use. Conversely, some persons dependent on heroin or alcohol stop their drug use abruptly without marked withdrawal symptoms.
Agonist drug "replacement" to modify withdrawal symptoms or to facilitate cessation has been used with narcotic abuse (methadone and L-acetylmethadol) and alcoholism (benzodiazepines) as well as with tobacco addiction (nicotine gum, transdermal nicotine, and nicotine nasal spray). In all cases the agonist relieves withdrawal symptoms. Methadone and nicotine can be used over several months, with gradual tapering, to facilitate cessation. Methadone is also used in the long-term to maintain abstinence. While such use is not recommended for nicotine replacement, 6% to 38% of nicotine gum users do continue to use the gum for a year or more after stopping smoking, apparently as a sort of maintenance treatment. 35
- NICOTINE DEPENDENCY IN YOUTHS
Tobacco use begins with experimentation, often in early adolescence or in the preteen years. The immediate impetus to experiment is social, prompted by friends, or family members, or role models who smoke. Other factors involved in initiation and progression of smoking are discussed in detail in a later section. Estimates of the percentage of youths who experiment with smoking vary from 47% to 90%. Most who experiment smoke only a few cigarettes. Those who smoke three or more cigarettes have a high likelihood of becoming regular smokers. 36 Once a smoker becomes a regular smoker, the number of cigarettes smoked per day tends to escalate over several years. 37 Even when youths are smoking only a few cigarettes per day, they inhale tobacco smoke effectively and take in as much nicotine per cigarette as do adults, as shown in studies measuring salivary cotinine per cigarette smoked per day.
Epidemiology and Natural History of Cigarette Smoking
Data from the Youth Risk Behavior Survey for smoking initiation by high school youths in the United States are presented in table 2-4 (1990) and in table 2-5 (1991) for smoking within the past 30 days. Figure 2-3 shows that in 1990, by age 13, 56% of youths had tried smoking and 9% were regular smokers (that is, they smoked on 5-15 days or more in the past 30 days). The percentage of youths trying cigarettes increases with each year of age, so that by age 17, 77% of youths had tried smoking and 25% were regular smokers. This trend has been reported for current smokers (that is, who smoked within the last 30 days) in other recent surveys ( table 2-5 ).
Percentage of boys and girls who initiate smoking at specific ages.
Percentage of youths who currently smoke cigarettes (who smoked within the last 30 days).
Source: Data from 1990 Youth Risk Behavior Survey, presented in Escobedo, Luis G., Stephen E. Marcus, Deborah Holtzman, and Gary Giovino. "Sports Participation, Age at Smoking Initiation, and the Risk of Smoking Among U.S. High School Students." Journal (more...)
Data on the amount of cigarettes consumed by youths of various ages are provided in table 2-6 . Younger children are less likely to be daily smokers; if they are, they smoke fewer cigarettes per day. Thus, at ages 12-13, 16.5 % of adolescent smokers are daily smokers, compared to 47.5% of teen smokers between 16-18 years old. At ages 12-13, 11% of smokers smoke 10 or more cigarettes per day, compared to 27.2% of smokers 16-18 years old.
Percentage of current smokers by the number of days smoked in the past month and the average number of cigarettes smoked daily.
The development of nicotine addiction has been characterized as a series of five stages:
Preparatory
Initial trying
Experimentation
Regular use
Nicotine addiction 38
The "preparatory" stage includes formation of knowledge, beliefs, and expectations about smoking. "Initial trying" refers to trials with the first 2 or 3 cigarettes (events that are discussed in more detail later in this section). "Experimentation" refers to repeated, irregular use over an extended period of time; such smoking may be situation-specific (for example, smoking at parties). "Regular smoking" by youths may mean smoking every weekend or in certain parts of each day (such as after school with friends). "Nicotine addiction'' refers to regular smoking, usually every day, with an internally regulated need for nicotine. Thus, for individual youths, there is a progression of smoking over time from initiation to experimentation with light smoking to regular and heavy smoking. Unlike adults, in whom intermittent or light smoking may be a stable and relatively nonaddictive pattern of smoking, children who are light smokers are often in a phase of escalation, with a typical interval from initiation to addiction of 2-3 years. The interval between initiation and addiction is based on a comparison of the cumulative prevalence curves for trying a first cigarette and smoking daily ( table 2-1 ) and the interval between initiation of smoking and the rise of salivary cotinine concentrations to adult levels ( figure 2-4 ).
Source: McNeill, A. D., M. J. Jarvis, J. A. Stapleton, R. J. West, and A. Bryant. "Nicotine Intake in Young Smokers: Longitudinal Study of Saliva Cotinine Concentrations." American Journal of Public Health 79 (1989): 172-1.'5.
The natural history of the smoking experience for an individual provides insight into the pharmacology of the addiction process. The first cigarette smoked is often perceived as aversive, producing coughing, dizziness, and/or nausea. With repeated smoking, tolerance develops to the noxious effects of cigarette smoking, and smokers tend to report positive effects of smoking. As the daily intake of nicotine increases, the development of physical dependence, that is, experiencing withdrawal symptoms between cigarettes or when cigarettes are not available, becomes established. Thus, there appears to be a progression over time from smoking initially for social reasons to smoking for pharmacologic reasons. The latter includes both smoking for positive effects of nicotine and smoking to avoid withdrawal symptoms, as discussed above in the section on general aspects of nicotine dependence.
Evidence for Nicotine Dependence in Youths
Many youths describe themselves as being dependent on tobacco, and there is evidence that nicotine dependence does become established in youthful smokers. The evidence reveals that (1) youths consume substantial levels of nicotine, (2) youths report subjective effects and subjective reasons for smoking, (3) youths experience withdrawal symptoms when they are not able to smoke, and (4) youths have difficulty in quitting tobacco use.
That youths consume substantial amounts of nicotine was shown in a 3-year study of 197 London schoolgirls who entered the study between the ages of 11 and 14. Saliva cotinine concentrations in girls who were smokers throughout the 3 years were higher at each year's evaluation. Average salivary cotinine levels were 103, 158, and 208 g/ml. 39 The level of 208 ng/ml is similar to that of many adult daily smokers. The ratio of salivary cotinine per cigarette per day, an index of the amount of nicotine taken in per cigarette, was similar for girls with various levels of cigarette consumption, and similar to that for adults. Thus, there seems to be the same intake of nicotine per cigarette among adolescent girls as among adults. Also of note in the study was that smokers who smoked at the time of all three surveys, as well as smokers who were occasional smokers or nonsmokers at the time of the first survey but who subsequently became daily smokers, showed escalation of cigarette consumption ( figure 2-4 ) and saliva cotinine levels each year.
That youths experience pharmacologic effects of nicotine from tobacco smoke was reported in an earlier study by the same researchers. 40 A smoking questionnaire asked a group of 170 British schoolgirls ages 11-17 about the five subjective effects of smoking specified in figure 2-5 . Feeling high or feeling more alert, which are stimulant-like effects, were described by only a few respondents. Feeling calmer was the most common effect described, and was more likely to be reported by daily smokers than by occasional smokers. There was also a significant correlation between salivary cotinine concentrations and the response of feeling calmer. Feeling calmer may be a beneficial effect that is particularly desirable to youths with high levels of anxiety or depression (as will be discussed later). Alternatively, feeling calmer could represent the reversal of nicotine withdrawal symptoms. In any case, there is clear evidence that youthful smokers do smoke for the pharmacologic effects of tobacco, presumably the effects of nicotine.
* Difference is statistically significant. Source: McNeill, Ann D., Martin Jarvis, and Robert West. "Subjective Effects of Cigarette Smoking in Adolescents." Psychopharmacology 92 (1987): 115-117.
That youths experience withdrawal symptoms when they try to give up smoking has been demonstrated as well. McNeill and colleagues queried 191 schoolgirls 11-17 years old who were current cigarette smokers about how they felt when they tried to stop smoking. 41 Of the group of smokers, 71% of the daily smokers and 72% of the occasional smokers had made at least one attempt to quit and had failed. Of these subjects, the average cigarette consumption by the daily smokers (69 girls) was 6.8 cigarettes per day, with an average salivary cotinine of 182 ng/ml. The average salivary cotinine concentration in the occasional smokers (47 girls) was 22 ng/ml; 74% of the daily smokers and 47% of the occasional smokers experienced one or more of the six symptoms of nicotine withdrawal graphed in figure 2-6 . The withdrawal score correlated significantly with salivary cotinine concentration and with weekly cigarette consumption. This study demonstrates that adolescent smokers experience withdrawal symptoms when they try to quit and that many youths have difficulty quitting. It should be noted that the data on nicotine consumption, pharmacologic effects, and withdrawal symptoms are based on studies of schoolgirls; no data are as yet available on boys. However, based on the difficulty of quitting smoking that is experienced by both boys and girls (described below), it is likely that dependence develops to a similar degree in boys as it does in girls. This issue of the natural history of the development of addiction to nicotine in youths requires further research.
* Difference is statistically significant. Source: McNeill, Ann D., Robert J. West, Martin Jarvis, et al. "Cigarette Withdrawal Symptoms in Adolescent Smokers." Psychopharmacology 90 (1986): 533-536.
Other studies further reveal that many youths want to quit but have difficulty doing so. Townsend and colleagues reported that 60% of adolescent smokers evaluated in a general medical practice made an agreement with the practice doctor or nurse to give up smoking. 42 Stone and Kristeller surveyed tenth grade students in suburban Massachusetts; 14% of the students were daily smokers and, of these, 28% reported that they continued to smoke because they were addicted. 43 The Monitoring the Future Project, which looked at high school seniors in the United States, asked about interest in quitting smoking and prior attempts at quitting ( table 2-7 ). Of smokers (1985-1989) who had smoked at all in the past 30 days, 42.5% reported a desire to stop smoking. Of this group, and of the subgroup who smoked daily, 28% and 39%, respectively, stated that they had tried to stop in the past and could not. 44
High school seniors' attempts to quit smoking.
Another perspective on the difficulty of quitting is youths' expectations regarding their future smoking behavior. Seniors in high school were asked, "Do you think you will be smoking cigarettes 5 years from now?" Among the respondents who were occasional smokers (less than one cigarette per day) 85% stated that they probably or definitely would not be smoking in 5 years, as did 32% of those who smoked one pack per day or more ( table 2-8 ). However, at follow-up 5-6 years later, of those who smoked occasionally only 58% had quit and 28% had actually increased their cigarette consumption. Of those who had smoked one pack or more per day, only 13% had quit and 70% still smoked one pack or more per day. Smokers of 1-5 or about 10 cigarettes per day at the time of the initial questionnaire also were less likely to quit than they had predicted, and on average escalated their smoking over the subsequent 5 years ( table 2-9 ). 45
High school seniors predict whether or not they will be smoking in 5 years (percentage).
Direction of change in smoking between senior year of high school and 5-6 years later.
Thus, consistent with the concept of addiction, smokers' expectations of future smoking behavior shows little relationship to their actual behavior; that is, youths think that they will be able to quit but underestimate the power of their addiction. Even those who smoke only a few cigarettes per day during high school have a high risk of becoming heavy smokers as adults.
These data are evidence that nicotine addiction develops during adolescence, and that most adolescents who are daily cigarette smokers (as well as some who are occasional smokers) are addicted to nicotine. Once adolescents are addicted, cessation is difficult, as it is for adults; thus, interventions are needed at early stages to prevent an established pattern of addiction. The likelihood of successful quitting among adolescents is greater the sooner the adolescent tries to quit after initiating tobacco use, and the fewer cigarettes he or she has smoked. 46
Risk Factors for Smoking Initiation
Understanding why children begin to smoke is important in planning and developing effective prevention strategies. The numerous major factors that influence or predict initiation and escalation of tobacco use were recently reviewed extensively in the 1994 surgeon general's report, and are listed in table 2-10 . In general, the psychosocial risk factors can be described as a continuum of proximal to distal factors. Proximal factors directly affect an individual's choice to use tobacco, whereas distal factors do so indirectly. For example. being offered a cigarette at a party is a proximal factor, but prior exposure to advertising showing young adults smoking at a party would be a distal factor influencing the decision to use tobacco. Although proximal factors may seem more influential because of their immediacy, distal factors:
Psychosocial risk factors in the initiation of tobacco use among adolescents.
. . . acquire potency if they are pervasive and provide consistent, repetitive messages across multiple channels. Distal factors are also powerful because, over time, they affect proximal factors as these influences become interpreted and internalized, particularly among adolescents as they try to shape a mature self-identity. 47
The degree to which any of these risk factors influences smoking behavior varies for each risk factor and among research studies. The reader who wishes a detailed discussion of the risk factors should refer to the surgeon general's report. This section provides only an overview of those issues most pertinent to the policy questions addressed in this report.
Initiation of cigarette smoking is influenced by several kinds of factors: environmental, behavioral, personal, and sociodemographic. 48 Among the environmental factors that influence initiation of smoking is having friends who smoke, having a best friend who smokes, and/or having many friends who smoke strongly influences initiation. Parental smoking is more important in establishing smoking as a normative behavior, and is associated with more positive and fewer negative perceptions of the health consequences of smoking. Advertising and exposure to smoking in other mass media (for example, television, movies, and sports events) reinforces the idea that smoking is an adult, sophisticated, attractive, and sexy behavior, and downplays the adverse health consequences of smoking (see chapter 4 on advertising).
Behavioral analysis indicates that cigarette smoking is often an early manifestation of problem behavior. School children manifest such problem behaviors as poor school performance, low aspiration for future success, school absences, and the intention to drop out of school or actually dropping out. Other problem behaviors linked to cigarette smoking include alcohol and other drug use and other risk-taking or rebellious behaviors.
A number of personal characteristics of adolescents have been linked to cigarette smoking: (1) low self-esteem, poor self-image, low perception of self-efficacy, and susceptibility to peer pressure; (2) sensation-seeking, rebelliousness, sense of invulnerability; (3) low knowledge level of the adverse effects of cigarette smoking; (4) depression and/or anxiety; and (5) pharmacologic response. Considerable recent research has shown a high prevalence of depression among current smokers. Smokers are more likely than nonsmokers to have a history of major depression, even preceding initiation of smoking, 49 and smokers with a history of depression have been found to have lower smoking cessation rates than smokers without depression.
Various pharmacologic responses to smoking (presumably to nicotine) from the first cigarette may also predict the likelihood of progression to regular smoking. Hirschman and colleagues found that a report of dizziness after smoking the first cigarette predicted a high rate of progression to the next cigarette, whereas reports of adverse effects, such as coughing, were not associated with progression. 50 While the mechanism of such a link between dizziness and smoking progression is not apparent, a pharmacologic link between cigarette smoking and depression is reasonable. Nicotine is known to release dopamine, norepinephrine, and serotonin in the brain in animals. Antidepressant drugs have similar effects. Thus, it is possible that pharmacologic responses to nicotine promote tobacco use in people who are depressed.
Evidence from studies of twins suggests a moderate genetic influence both on initiation and on maintenance of cigarette smoking. 51 Possible mechanisms include genetically determined differences in the pharmacologic response to nicotine, differences in personality, and the presence or absence of an affective or other psychiatric disorder, particularly depression. There is a high concordance of cigarette smoking and alcoholism, and studies in twins suggest that these addictions share, to some extent, a common genetic determinant. 52 Some proportion of the genetic predisposition to tobacco addiction thus appears to be specific, but some appears to be linked to alcoholism or to other drug addictions.
The factors that influence initiation may be predominantly of one type, and those that influence the progression of cigarette smoking of another type. Hirschman and colleagues studied 386 urban public school children, grades 210, to determine how many had ever tried smoking, and then how many had progressed to a second and third cigarette. The main risk factors for the 47% of children who had tried at least one cigarette were grade level in school (that is, the higher the grade level and the older the child, the higher the likelihood of trying a cigarette), having a best friend who was a smoker, and risk-taking behavior (reported on a questionnaire). Progression to a second cigarette (32% of those who smoked one cigarette) was predicted by life stress (predicted rapid progression), friends who smoked (predicted slow progression), lack of negative attitudes toward smoking, and an experience of dizziness when smoking the first cigarette. Progression to a third cigarette (in 77% of those who had smoked two cigarettes) was predicted by best friend being a smoker, feelings of helplessness, and rapid progression to the second cigarette. 53 These analyses support the idea that initiation of cigarette smoking is primarily a consequence of environmental factors, whereas progression appears to be more influenced by personal and pharmacologic factors.
Sociodemographic factors that predispose youths to cigarette smoking include low socioeconomic status, low level of parental education, and the individual's developmental state of adolescence. With respect to the latter, the transition years from elementary to high school, grades 7-10, (ages 11-16) appear to be a particularly high-risk time for initiation ( table 2-4 ).
Ethnic Differences in Nicotine Dependency
Differences in tobacco use by youths are specific to and consistent within ethnic groups. The rates for daily smoking for twelfth graders in 1991 were highest among non-Hispanic whites (21%), next among Hispanics (12%), and lowest among African Americans (5%); the rates in 1991 for smoking one or more cigarettes in the preceding 30 days were 32% for non-Hispanic whites, 25% for Hispanics, and 9% for African Americans. 54 A striking trend of decline in smoking has occurred among African-American high school seniors: from 26.8% in 1976 to 4.4% in 1993 for smoking daily during the preceding 30 days 55 ( figure 2-7 ). Differences in the smoking habits of various ethnic groups are notable and may influence the addictive process. Compared to whites, African Americans show a consistent preference for menthol brands, higher tar levels, and higher nicotine levels; and they smoke fewer cigarettes per day. These factors influence inhalation patterns and health risks. For instance, because menthol cigarettes ''provide a sensation of cooling when smoked," they may "promote deeper and more prolonged inhalation." 56 Although current initiation rates are lowest for African Americans, there is evidence that adult African Americans are more highly addicted to tobacco than are whites. The cotinine levels of adult African Americans are higher than those of whites, even though they smoke fewer cigarettes; 57 this suggests that African Americans consume higher levels of nicotine from each cigarette than do whites. A greater dose of nicotine per cigarette may be explained in part by the smoking of menthol cigarettes, as discussed previously. In addition, this observation is consistent with the generally lower income level of African Americans compared to whites, and an economic pressure to extract more nicotine per cigarette. Cessation rates for African-American adults are lower than for whites, which seems to indicate a higher level of addiction for African Americans. 58 The explanation for the apparent inconsistency between lower current initiation rates but higher levels of addiction in adult African Americans is not clear. Possibly this difference reflects a cohort effect, and in the future fewer adult African Americans will be addicted. Alternatively, it may reflect initiation of cigarette smoking later in life among African Americans compared to whites. Further research is needed to clarify these issues. The use of smokeless tobacco is highest among whites and Native Americans, with relatively low levels among African Americans and Hispanics. 59 The reasons for ethnic differences in tobacco use among youths are unclear.
Source: Monitoring the Future Project, University of Michigan, 19761993.
Use of Smokeless Tobacco by Children and Youths
Initiation of smokeless tobacco use begins in the preteen and early teen years. In 1991 smokeless tobacco was used by about 11% of high school seniors ( table 2-11 ). The prevalence of smokeless tobacco use varies considerably in different regions of the country, with lowest rates generally in the Northeast, and lower rates in cities than in rural areas. Of note, the prevalence of smokeless tobacco use is greater than that of cigarette smoking by youths in several states, including Alabama, Idaho, South Dakota, Colorado, Wyoming, and Montana. The prevalence of moist snuff tobacco use by youths has risen dramatically, with a 10-fold increase for 16 to 19-year-olds between 1970 and 1985. 60 There was a brief reduction in 1986-87, but sales of smokeless tobacco products are now increasing, with a 70% overall increase in moist snuff sales from 1982 to 1992. 61 Smokeless tobacco is used primarily by males in all ethnic groups except American Indians and Alaskan natives, where the prevalence of use is similar for males and females.
Percentage of youths who currently (within the past 30 days) use smokeless tobacco.
As discussed earlier, nicotine and cotinine concentrations in the blood of adults who use smokeless tobacco are comparable to those measured in smokers. No such data are available for children. Addiction of youths to smokeless tobacco is documented by reports that many users of smokeless tobacco have tried to quit but have been unsuccessful. According to the 1986-1989 Teenage Attitudes and Practices Survey, 21% of current smokeless tobacco users (12- to 18-year-olds) had tried to quit four or more times unsuccessfully, which is consistent with a high level of addiction. 62
Factors influencing the initiation of smokeless tobacco are in general similar to those that are associated with initiation of cigarette smoking. 63 One difference of note, however, is that smokeless tobacco use has been associated with participation on sponsored athletic teams (for example, baseball, wrestling, football, rodeo), whereas smokers are less likely to participate in such teams. As noted earlier, smokeless tobacco use is a risk factor for cigarette smoking, and vice versa. The exchangeability of tobacco use supports the idea that nicotine addiction can be maintained by tobacco from any source.
- NATURE OF TOBACCO PRODUCTS
Nicotine addiction is maintained by use of tobacco, the only significant source of nicotine. Certain teas and vegetables contain low levels of nicotine, but the amounts available are so low that it is impossible to consume pharmacologically active doses of nicotine from sources other than tobacco. Tobacco is smoked as cigarettes, cigars, and in pipes, but can also be used without smoking by applying smokeless tobacco directly to mucous membranes. Several types of smokeless tobacco are available—oral snuff, nasal snuff, and chewing tobacco.
Production of Tobacco Products
Tobacco products in the United States are made by blending different types of tobacco leaf, to which sugar and other flavorings are added. Lighter tobaccos, which are found in most American cigarettes, produce acidic smoke when burned. Darker tobaccos, such as are used in cigar and pipe tobacco, produce alkaline smoke. As discussed elsewhere, the pH of the smoke determines the extent to which nicotine will be absorbed through the mouth.
In addition to different types of shredded tobacco leaf, tobacco sheet or reconstituted tobacco is also blended into many cigarettes. Tobacco sheet uses scraps and stems of tobacco as well as various additives, which are combined into a homogeneous mixture that can then be incorporated into tobacco. The manufacturing of tobacco sheet allows for production of a relatively uniform composition of tobacco, since additives can be used to achieve the end product. 64
Reports have been made of evidence that tobacco manufacturers manipulate the nicotine content of cigarettes. 65 One way in which manufacturers control the nicotine content of tobacco is by extracting the nicotine from the tobacco, then adding it back in controlled amounts as tobacco extract. Tobacco companies also hold patents for spraying nicotine solutions onto cigarette tobacco, although it is unclear if this practice is actually used in the manufacturing of cigarettes. Tobacco manufacturers state that the reason nicotine is extracted and then reapplied to tobacco is that nicotine in the natural tobacco leaf exists in very uneven concentrations. By extracting and re-adding nicotine, it is possible to provide a more consistent tobacco product, which delivers a consistent amount of nicotine. It has also been suggested that the amount of nicotine in tobacco is controlled so as to ensure a level adequate to maintain nicotine addiction. In support of this idea was an internal memorandum, discovered in recent ligitation, from a Phillip Morris Tobacco Company scientist: "The cigarette should be conceived not as a product but as a package. The product is nicotine . . . smoke is beyond question the most optimized vehicle of nicotine and the cigarette is the most optimized dispenser of smoke." 66 That the pharmacologic actions of nicotine are important determinants of why people smoke is supported by research both by the tobacco industry and by non-industry researchers. 67
In the United States, four primary types of smokeless tobacco are manufactured: loose leaf, plug, twist or roll, and oral snuff. 68 Loose leaf chewing tobacco consists of tobacco leaf that has been heavily treated with licorice and sugars. Plug tobacco is produced from leaves that are immersed in a mixture of licorice and sugar and then pressed into a plug. Twist tobacco is made from leaves that are flavored and twisted to resemble a rope. Oral snuff is available in dry and moist preparations. Dry snuff is powdered tobacco that contains flavor and aroma additives. Moist snuff consists of fine particles of tobacco that contain considerable moisture; many varieties are prepared with flavorings such as wintergreen or mint. The oral use of snuff, called "snuff dipping," involves placing a pinch of the tobacco between the cheek or lips and the gum, or beneath the tongue.
Starter products and distribution of free samples might introduce users to a graduation process of moving from low-nicotine to higher-nicotine snuff products. For example, products low in nicotine and low in pH (which reduces buccal absorption) and products sold in a teabag-like unit dose, would make it easier for first-time users to adapt to snuff products. The use of such low-nicotine-delivery products could be the beginning of a graduated process toward nicotine addiction.
Modifying Cigarette Yields
Tobacco smoke contains more than 4,000 chemicals, many of which are known toxins. Some of the better-known toxins include carbon monoxide, hydrogen cyanide, nitrogen oxides, ammonia, benzene, formaldehyde, nitrosoamines, vinyl chloride, polycyclic hydrocarbons, polonium-210, arsenic, and lead.
Tobacco smoke is an aerosol of droplets containing water, nicotine, and other alkaloids, and tar. Tar is what is left in the particulates after water and alkaloids are removed. Particulates are suspended in a gaseous mixture, which contains carbon monoxide, nitrogen oxides, and other gases.
To estimate the amount of various constituents that smokers are exposed to, cigarettes are routinely tested with a standardized smoking machine test. This test has been referred to as the Federal Trade Commission (FTC) method. The FTC performed and published test results in commercial cigarettes from 1967 until 1985; since that time the tobacco industry has conducted these tests. The FTC test procedure consists of placing a cigarette into a holder and igniting it; then 35-ml puffs are taken via a syringe over 2 seconds, once every minute until the cigarette is burned to a specific butt length. The smoke that is collected is passed through a filter to collect the particulate material (tar and nicotine). The gases that pass through the filter are collected for determination of carbon monoxide and other constituents. Thus, values for yields of tar, nicotine, and carbon monoxide for each cigarette are reported from this type of testing procedure.
Lowering the yields of tar and other toxic constituents of cigarettes smoke makes intuitive sense as a way to reduce the health risks of cigarette smoking. Tobacco companies widely promote cigarettes that are lower in yield, implying a health benefit compared to smoking higher-yield cigarettes. However, the low-yield cigarette concept is in many ways deceptive. To understand why this is so, it is useful to examine how low-yield cigarettes are engineered.
There are several ways in which cigarettes can be engineered to be low-yield by smoking machine tests. The most obvious way is filtration, in which case a filter is placed at the end of the cigarette. This filter can remove a significant amount of tar. In the United States, 95% of cigarettes are filtered. Another way to reduce yields is to reduce the content of nicotine or other toxic substances in tobacco per se. This appears not to be the case with commercial cigarettes. When the nicotine concentration of tobacco in cigarettes of differing yields was measured, it was found that, on average, cigarette tobacco had a nicotine concentration of about 1.6%. 69 There was a significant inverse correlation between concentration of nicotine in tobacco and yield, suggesting that low-yield cigarettes are made with tobacco that contains more, rather than less, nicotine than higher-yield cigarettes. In any case, it is clear that low-yield cigarettes are not low-yield because the contents of nicotine or tar are lower in the tobacco per se. Low-yield cigarettes are engineered to be low-yield based on the standardized smoking machine protocol. This can be done by shortening the cigarette length, increasing the burn rate of the paper, or increasing the length of the filter overwrap so that the machine is able to take fewer puffs before the cigarette is burned to its specified length. Placing less tobacco in each cigarette by using expanded tobacco and/or smaller diameters of cigarettes can also reduce yield. Diluting the mainstream smoke through the use of porous paper or ventilation holes in the filter tipping paper can substantially reduce yields. In the latter case, when the cigarette is inhaled from the tip, considerable room air is drawn in to dilute the tobacco smoke.
Unfortunately, the addicted smoker does not smoke like an FTC smoking machine. Smokers take deeper and more frequent puffs than the machine on average, and can easily alter their smoking behavior as desired. Smokers learn, without realizing what they are doing, that placing their lips or fingers over the cigarette tip improves the draw characteristics of the cigarette. They are actually blocking the ventilation holes so that they are inhaling more tobacco smoke and less room air. Many studies in which the actual intake of nicotine, carbon monoxide, or other constituents of tobacco smoke have been measured in smokers, have shown a very weak relationship, if any, to nominal nicotine yield. Thus, once a smoker becomes addicted to nicotine, he or she can easily adapt smoking behavior to obtain the desired dose of nicotine from any cigarette. Of note, the ultra-low-yield cigarettes (that is, tar less than 1 mg, nicotine less than 0.1 mg) do seem to make it more difficult for smokers to obtain levels of nicotine that they can from high-yield cigarettes. 70 The observation that sales of these ultra-low-yield cigarettes are relatively low suggests that there may be a threshold for nicotine delivery, below which nicotine addiction is not easily maintained. As typically smoked, low-yield cigarettes are not less harmful than higher-yield cigarettes. Because smokers take in much more tar and other toxins than estimated by machine yields, the risk of smoking-caused disease is not significantly reduced by using low-yield cigarettes.
In summary, people smoke cigarettes largely to obtain the nicotine they desire. They do not smoke in a standardized way as do smoking machines, and therefore machines are poor predictors of actual human exposure. Human exposures can be estimated by direct measures of levels of tobacco smoke constituents in biological fluids of smokers. Such markers include nicotine, its metabolite, cotinine, carbon monoxide, adducts of various reactive chemicals to hemoglobin or DNA, and mutagenic activity of the urine.
- CONCLUSIONS AND RESEARCH RECOMMENDATIONS
Having reviewed the research literature on nicotine addiction and tobacco use, the committee finds the following conclusions to be warranted:
Long-term tobacco use is maintained by addiction to nicotine.
Use of any form of tobacco can result in addiction, and smokeless tobacco is becoming an increasingly prevalent behavior among youths. Smokeless tobacco is not a healthful alternative to cigarettes.
Once addicted, a person finds it difficult to quit using tobacco.
Children and youths begin tobacco use. Youths rapidly become addicted to nicotine; the addiction maintains their tobacco use in adulthood.
When youths begin using tobacco, they overestimate the proportion of tobacco use in society, underestimate the addictive nature of tobacco and the risk that they will become addicted over a long-term, and underestimate the danger that they will incur tobacco-related disease. Thus, children and youths become addicted to nicotine before they are able to appreciate fully the consequences of their behavior.
There is considerable individual variation in susceptibility to nicotine addiction. Environmental, behavioral, personal, socioeconomic, and ethnic factors influence susceptibility to initiation and addiction.
The recognition that youths become addicted to nicotine should be incorporated into the design, evaluation, and dissemination of treatment programs for youths to stop tobacco use; as proven strategies emerge, they should be made easily accessible to youths.
Among adults the prevalence of cigarette smoking has declined from 1966 to the present. The prevalence of smoking by youths declined through 1980, but subsequently has been stable, except for African-American youths, for whom there has been a sharp decline. The prevalence of smokeless tobacco use by boys has increased steadily for the past 15 years and represents a significant growing addiction to tobacco.
Available evidence indicates that cigarette manufacturers control the level of nicotine in cigarettes and the nicotine delivery of their products in deliberate ways. However, "low-yield" cigarettes are not low in nicotine content and do not in general deliver less nicotine or tar to smokers than do higher-yield cigarettes.
Prevention of nicotine addiction among youths is an essential part of any policy for reducing tobacco use in society as a whole. Approaches to prevention can be targeted toward the various factors that initiate and maintain tobacco addiction, as will be discussed in subsequent chapters.
The Committee makes the following recommendations for research on nicotine addiction:
Research should be conducted to determine individual susceptibility to nicotine addiction. Particular areas that need research are genetic factors, affective states, and ethnic influences. Such information could facilitate the identification of high-risk children and could lead to more effective prevention strategies.
For all forms of tobacco products, research should be conducted on the characteristics of nicotine addiction in the early stages, that is, in the first few years during which the transition between experimental and addictive nicotine use occurs. Such information could contribute to more effective intervention before youth become highly addicted adult tobacco users.
Research should be conducted on the relationship between the characteristics of tobacco products and addiction. For example, as a basis in developing regulatory guidelines, it would be useful to know the minimal level of nicotine delivery from a tobacco product at which addiction will develop and/ or be sustained.
The terms "drug addiction" and "drug dependency" are used interchangeably in this report, as was done in the 1988 report of the surgeon general on nicotine addiction. which considered the terms to be "scientifically equivalent.''
- Cite this Page Institute of Medicine (US) Committee on Preventing Nicotine Addiction in Children and Youths; Lynch BS, Bonnie RJ, editors. Growing up Tobacco Free: Preventing Nicotine Addiction in Children and Youths. Washington (DC): National Academies Press (US); 1994. 2, THE NATURE OF NICOTINE ADDICTION.
- PDF version of this title (4.9M)
In this Page
Related information.
- PMC PubMed Central citations
- PubMed Links to PubMed
Recent Activity
- THE NATURE OF NICOTINE ADDICTION - Growing up Tobacco Free THE NATURE OF NICOTINE ADDICTION - Growing up Tobacco Free
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers

IMAGES
COMMENTS
Get a custom essay on Teen Vaping: The New Wave of Nicotine Addiction. It might have a significant effect if state officials asked the region's health authority to ban all flavored vape goods in reaction to this issue to safeguard the youth's well-being (Domenico et al., 2021). A state does have other options in addition to that.
ADDICTIVENESS OF TOBACCO. According to the statement of the tobacco companies, nicotine is distinct from other addictive substances since it does not cause abuse or intoxication [].Regarding abuse, in the Diagnostic and Statistical Manual of Mental Disorders, fifth edition (DSM-5) (the latest version published by the American Psychiatric Association in 2013), the distinction between abuse and ...
Nicotine replacement medications, such as gums, lozenges, or patches, can also help people quit smoking by relieving symptoms of withdrawal, which are often a major obstacle to quitting. Because oral ingestion and skin absorption of nicotine are slower and result in much lower peak levels than smoking, these forms of nicotine are less rewarding ...
INTRODUCTION "To lower nicotine too much might end up destroying the nicotine habit in a large number of consumers and prevent it from ever being acquired by new smokers. - British American Tobacco Company internal document, June 1959 ().Combusted tobacco use remains a major cause of premature disability and death around the world ().Cigarette smoke contains an estimated 7000 different ...
The unique attributes that make nicotine cravings persist. "Nicotine, alcohol, heroin, or any drug of abuse works by hijacking the brain's reward system," says Yale researcher Nii Addy, PhD, who specializes in the neurobiology of addiction. The reward system wasn't meant for drugs—it evolved to interact with natural neurotransmitters ...
Nicotine addiction remains one of the easiest addictions to fall into, can develop rapidly and one of the toughest addictions to get rid of. ... [PMC free article: PMC6200636] [PubMed: 30218864] 2. Selby P, Voci S, Zawertailo L, Baliunas D, Dragonetti R, Hussain S. Public health impact of a novel smoking cessation outreach program in Ontario ...
Nicotine Addiction Essays Exploring the Safety of E-Cigarette Vaping Among Youth: A Critical Examination Concerns over the safety and possible health effects of vaping, also known as e-cigarette use among children, have increased in recent years due to the rise in this practice.
Although proxy measures of addiction vary, more frequent EC use (i.e., on more days per month) suggests increasing dependence on nicotine . Recent US and Canadian data found that over a quarter (28% and 40%, respectively) of middle- and high-school students who currently used ECs (i.e., past month) did so on a daily, or almost daily, basis [ 21 ...
Neurobiological findings have identified the mechanisms by which nicotine in tobacco affects the brain reward system and causes addiction. These brain changes contribute to the maintenance of ...
Summary. Tobacco addiction can cause significant harm to the human body and health. It is necessary to treat the symptoms of smoking to combat it and the psychological force of the habit. Scientists have identified a gene in the standard DNA strand that increases the likelihood of developing nicotine addiction and, as a result, lung cancer.
In this paper, we will research what nicotine is, how it influences on us and discuss whether should smoking be banned in public places. Smoking has a first-rate effect on infertility, so each guy and girls discourage it.
Nicotine Addiction. harmful habit. Addiction Mechanism In 1988, the Ministry of Health in the United States defined the nicotine as an addictive substance. Cigarettes and other derivatives substances generate tobacco dependence. The addictive mechanisms are similar to the addiction mechanisms to drugs such as cocaine and heroin.
In 2017, the US Food and Drug Administration (FDA) proposed to reduce nicotine in cigarettes to minimally or non-addictive levels. This study qualitatively explored perceptions of nicotine and addiction, both independently and in response to messages communicating about nicotine reduction. Design. Qualitative study using focus groups.
Theoretically, nicotine addiction can be defined as a chronic disorder that is characterized by the inability to resist the compulsion to consume tobacco or other substances that contain nicotine. This condition is often characterized by the loss of control over nicotine intake and the emergence of negative emotions when a person loses access ...
Other effects that vaping have on teens is that it can distract you from your schoolwork because you're always think about the nicotine high. The number of teens that vape has gone up from 20.6 percent in 2017 to 25.7 percent in 2019, that's about 5 million teens worldwide.
To learn more about youth nicotine addiction, Stephanie Sy spoke with Amanda Graham, the principal investigator of the study. More than 2 million American middle and high school students now use e ...
THE CENTER ON ADDICTION TEEN SURVEY. The findings presented in this report are based on a nationally representative survey of 1,014 teens aged 12-17 living in the United States. Data were collected using an online platform between December 21, 2017 and January 5, 2018.
The nature of nicotine addiction. In: Lynch BS, Bonnie RJ, eds. Growing up tobacco free — preventing nicotine addiction in children and youths. Washington, DC: National Academy Press, 1994:28-68.
The prevalence of everyday smoking has leveled off at 18.1% of the population after dramatically declining over the last several decades. Thus, it is important to identify individual factors that contribute to nicotine addiction, such as stress, and at-risk populations, such as adolescents, in order to continue reducing smoking prevalence rates.
Study: E-Cigarette nicotine delivery among young adults by nicotine form, concentration, and flavor: a crossover randomized clinical trial. Image Credit: sergey kolesnokov / Shutterstock.com. E ...
Nicotine replacement therapy is the family of medications used to help adults quit using nicotine, including over-the-counter patches, gums or lozenges or prescription inhalers or nasal sprays.
DURHAM, N.C. - In what appears to be an effort to bypass public health regulations covering vaping products, some tobacco companies have begun replacing nicotine in e-cigarettes with related chemicals that have similar properties but unknown health effects, Duke Health researchers report.In a research letter appearing Aug. 7 in JAMA, study authors at Duke and Yale University also found that ...
Introduction. Nicotine addiction among teenagers has recently become one of the most pressing problems in the modern American society. Overall, the attempts made by anti-smoking campaigners hardly yield any results, because they mostly focus on harmfulness of tobacco smoking and the publics' awareness of the problem, itself, but they do not eradicate the underlying causes of teenage smoking.
Addiction; August 7, 2024 ... 'Tobacco-free nicotine' claims could lead non-smokers to try E-cigarettes. Nov 1, 2021. Increasing use and awareness of oral nicotine pouches detailed.
Tobacco companies may be trying to duck federal restrictions on vaping products by replacing nicotine with "nicotine analogs" -- related chemicals that have similar properties but unknown ...
The "Treating Nicotine Addiction in Adults, with a Focus on Conventional Cigarettes" section focuses on treatment of nicotine addiction with attention to counseling and behavioral approaches and cessation medications. The tobacco treatment literature is far more developed for combusted cigarettes and relatively sparse in other product areas.
THURSDAY, Aug. 8, 2024 (HealthDay News) -- That vape pen might contain something even worse than nicotine, new research warns. Tobacco companies may be trying to duck federal restrictions on vaping products by replacing nicotine with "nicotine analogs" -- related chemicals that have similar properties but unknown health effects, researchers report.
In May 2024 the Foundation for a Smoke-Free World (FSFW) rebranded 1 to Global Action to End Smoking (GAES), following the cancellation of PMI's funding agreement with FSFW in 2023. 2 See Global Action to End Smoking. Background. The Foundation for a Smoke-Free World (FSFW) describes itself as "an independent, non-profit organization" 3 that was established and is "operated free from ...
Cigarettes and other forms of tobacco are addicting. Most smokers use tobacco regularly because they are addicted to nicotine. Furthermore, most smokers find it difficult to quit using tobacco because they are addicted to nicotine. Nicotine addiction develops in the first few years of cigarette smoking. that is, for most people during adolescence or early adulthood. Most smokers begin smoking ...
Many public health experts say tobacco companies' harm-reduction initiatives are a way to sustain the profitability of tobacco and nicotine products. Although nicotine pouch products have lower ...