An official website of the United States government
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Publications
- Account settings
- Advanced Search
- Journal List


Prevention, screening, and treatment for heavy drinking and alcohol use disorder
Justin knox , ph.d., deborah s hasin , ph.d., farren r r larson , m.a., henry r kranzler , m.d..
- Author information
- Article notes
- Copyright and License information
Correspondence Deborah S. Hasin, PhD, Department of Psychiatry, Columbia University Medical Center, 1051 Riverside Drive, Box 123, New York, NY 10032, USA, Phone: 646-774-7909; Fax: 646-774-7920, [email protected] ; [email protected]
Contributors
JK did the initial data collection (literature search) and wrote the first draft of the paper. DSH and HRK contributed to the literature search coverage, contributed to interpretation of the findings and revision of the writing, and contributed short sections of the paper. FRRL contributed to the writing and revision of the paper, and to the design and creation of the tables and figure.
Issue date 2019 Dec.
Heavy drinking and alcohol use disorder (AUD) are major public health problems. Practitioners not specializing in alcohol treatment are often unaware of the guidelines for preventing, identifying, and treating heavy drinking and AUD. However, a consensus exists that clinically useful and valuable tools are available to address these issues. Here, we provide a critical review of existing information and recent developments in these areas. We also include information on heavy drinking and AUD among individuals with co-occurring psychiatric disorders, including drug use disorders. Areas covered include prevention; screening, brief intervention, and referral for treatment (SBIRT); evidence-based behavioral interventions; medication-assisted treatment; technology-based interventions (eHealth and mHealth); and population-level interventions. We also discuss the key issues that remain for future research.
Heavy drinking and alcohol use disorder (AUD) are major public health concerns
Alcohol consumption is prevalent worldwide. In 2016, 2·4 billion people (33% of the global population) were current drinkers. 1 In the United States, specifically, the prevalence of alcohol use disorder (AUD) and high-risk drinking in adults has increased substantially over the past ten years. 2 One in eight U.S. adults report past-year high-risk drinking, 2 and the prevalence of lifetime AUD is high. 3 In the United Kingdom, the prevalence of heavy drinking and AUD are also high. 4
In this paper, we primarily discuss heavy drinking and AUD. Many measures of alcohol consumption (e.g., heavy drinking, binge drinking) and alcohol-related disorders (e.g., harmful drinking, alcohol dependence, AUD) are used, and often, these reflect geographical preferences. For example, in the United States, Canada, and many other parts of the world, the diagnostic system of choice is the American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders (DSM), which was updated from the 4 th edition (DSM-IV) to the 5 th edition (DSM-5) in 2013. The United Kingdom and other European countries tend to use the World Health Organization’s (WHO) International Classification of Diseases (ICD) system to diagnose mental health conditions, including alcohol-related disorders. Overall, there has been good agreement between DSM and ICD diagnoses, with DSM-5 AUD capturing a wider and different aspect of problematic use than the diagnosis of alcohol dependence used in the ICD and previously in DSM-IV. 5 - 7 The Alcohol Use Disorders Identification Test (AUDIT), and the first three items from the AUDIT focused on consumption, known as the AUDIT-C, 8 , 9 are additional measures developed and validated by the WHO for international use which are common in the literature.
Alcohol use is a leading global cause of disease burden and substantial health loss. 1 Risk of all-cause mortality is positively associated with the level of alcohol consumption, such that any level of consumption is potentially harmful. 1 These findings are consistent with the well-demonstrated relationship of heavy drinking and AUD to numerous adverse health consequences, 2 , 3 , 10 , 11 and to morbidity and mortality worldwide. 12 - 14 Heavy drinking and AUDs also place psychological and financial burdens on individuals who engage in these behaviors, as well as their families, friends, coworkers, and society as a whole. 15 , 16 Compounding the seriousness of this problem, many individuals with AUD who could benefit from alcohol treatment, including those with severe disorders, do not receive it. 2 , 3 , 17 - 19 For example, in the United States, only about 8% of individuals with past-year AUD are treated annually in an alcohol treatment facility. 20
Despite the known adverse health consequences and prevalence of alcohol use (including harmful alcohol use), many practitioners outside the specific areas of alcohol specialization are not knowledgeable about the guidelines for preventing, identifying, and treating heavy drinking or AUD. In this report, we review existing information and recent developments in the prevention, identification, and treatment of heavy drinking and AUD. Whenever available, we include information about heavy drinking and AUD among individuals with co-occurring psychiatric disorders, including drug use disorders (DUD), as these disorders are highly prevalent among persons who drink heavily. 3 , 17 , 21 - 24 There is also a greater risk of relapse among individuals with co-occurring mental health disorders who receive alcohol treatment. 25 As a result, there is a recognized need to address the interrelationship of co-occurring alcohol use and mental health disorders through innovative approaches or adaptations of traditional treatments.
Search strategy and selection criteria
References for this review were identified through searches of PubMed for articles by use of the terms “alcohol,” “heavy drinking,” or “alcohol use disorder,” in combination with “prevention,” “school-based intervention,” “SBIRT,” “behavioral intervention,” “medication assisted treatment,” “technology,” or “population-level intervention.” Articles resulting from these searches and relevant references cited in those articles were reviewed. Articles deemed to have relevant information on preventing, identifying, and treating heavy drinking or AUD were included, with a focus on new developments, unresolved controversies, previous reviews, widely-cited studies, and literature about heavy drinking and AUD among individuals with co-occurring psychiatric disorders (including DUD), when it was available. Only articles published in English were included.
Preventing heavy drinking and AUD
Adolescence is a critical period for the initiation of alcohol use as the age at first drink occurs, on average, at 14 years in the United States 26 and 17 years globally. 27 Therefore, efforts to prevent heavy drinking and AUD are often targeted at youth before they usually begin drinking, and most of these efforts are implemented through schools. A systematic review of school-based interventions concluded that they can be an effective approach to alcohol prevention, at least in the short term. 28 However, another review noted that while school-based interventions increased knowledge and improved attitudes regarding drinking, evidence does not support their sustained effect on behavior. 29 Further, a review conducted in 2009 and updated in 2017 concluded that although alcohol education programs in schools and higher education settings are popular interventions, the evidence does not support their effectiveness. 30 , 31 An important direction for future research in this area would be to obtain more information on the short- and long-term efficacy of school-based alcohol prevention interventions. 28
Screening, Brief Intervention, and Referral for Treatment (SBIRT) for heavy drinking and AUD in clinical settings
Interactions with healthcare providers across a variety of clinical settings present a valuable, yet underutilized opportunity to engage with patients about their alcohol consumption. 32 - 34 Screening, Brief Intervention, and Referral to Treatment (SBIRT) is a paradigm designed for use by healthcare providers who are not specialists in alcohol treatment to identify and reduce harmful drinking, thereby reducing the risk of alcohol abuse and dependence. Figure 1 illustrates the steps involved in SBIRT, as adapted from the National Institute on Alcohol Abuse and Alcoholism (NIAAA) Clinician’s Guide. 33 , 34 SBIRT has also been expanded to address illicit drug use. 35 - 37
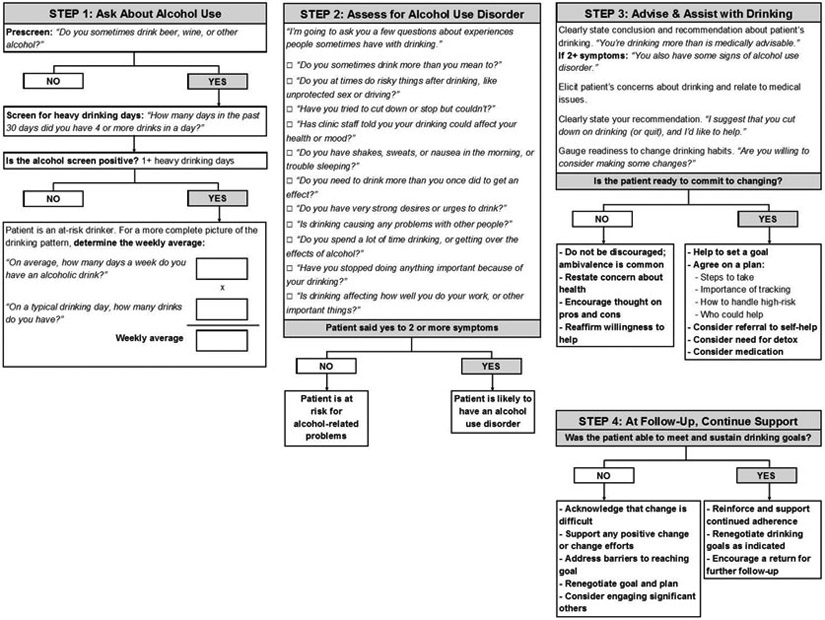
Screening for heavy drinking and AUD, adapted from the NIAAA Clinician’s Guide 34
Harmful alcohol use, including AUD, is the target of alcohol screening. Two screening tools for alcohol use have been recommended by the U.S. Preventive Services Task Force. 38 The AUDIT-C, which comprises the first three items of the 10-item Alcohol Use Disorders Identification Test (AUDIT), focuses on the quantity and frequency of alcohol consumption, including binge drinking. 8 , 9 Alternatively, a single question related to the frequency of binge drinking (defined as five or more drinks in a day for men and four or more drinks in a day for women) can be used. 39 Either tool can readily be incorporated in the clinical encounter.
Brief interventions.
According to SBIRT guidelines, brief interventions are recommended for patients who screen positive for harmful drinking but are not alcohol dependent. In general, brief interventions to reduce heavy drinking in primary care are effective in reducing drinking 36 , 40 - 42 and improving health outcomes. 43 Brief interventions can range in practice from very brief advice to theory-driven intervention, such as trained motivational interviewing. 40 - 42 , 44 , 45 Despite the different evidence-based behavioral treatment frameworks available (see discussion below), 46 current brief intervention efforts in the United States focus mostly on MI approaches aimed at motivating clients to change substance use patterns. 47 The number of sessions of brief treatment offered depend on the program and the patient, including his or her severity of drinking.
Referral for treatment.
Brief intervention has limited effectiveness among individuals with more severe alcohol problems, 42 , 48 - 59 including many who screen positive using the most widely used screening instruments. Referral to treatment may be more useful for this population, which often requires more intensive intervention. 34 , 60 - 65 However, the referral component of SBIRT is limited by the low rate at which individuals with severe alcohol problems follow up on referrals. 40 , 66 - 71 This occurs for a number of reasons, including concerns about stigma, 72 lack of interest in abstinence goals, 73 , 74 preference for self-sufficiency, financial barriers, and doubts about treatment efficacy. 18
SBIRT and patients with comorbid drug problems.
Individuals who drink heavily or have an AUD often use other substances, in many cases to the point of having a DUD. 17 In the U.S. general population, individuals with past-year AUD were three times more likely to have a DUD than those without a past-year AUD. 24 DUDs are prevalent and have been increasing. 75 - 77 They involve clinically significant impairment due to the recurrent use of drugs, 24 , 78 - 83 and create additional societal burden through their association with crime, incarceration, poverty, homelessness, and suicide. 78 , 79 , 81 , 83 SBIRT has been used as a paradigm to guide clinical interactions for individuals with combined illicit drug and alcohol use, with initial evidence of effectiveness. 84 Although calls have been made to implement SBIRT more widely, concerns exist about its efficacy. 85 - 87 This has led some individuals to suggest completely re-thinking the SBIRT model when drugs are involved, 88 while others suggest co-locating care management within primary care settings, including counseling about treatment options. 71 This remains an issue for further research and debate.
SBIRT implementation: Screening.
Despite the availability of validated screening tools, less than 25% of U.S. adult binge drinkers report ever being asked by a health professional about their drinking. 89 Reasons for this low percentage include individuals’ variable engagement with the healthcare system, providers’ lack of time due to competing priorities, and physicians’ concerns that patients will not accurately self-report their drinking. 90 The United Kingdom National Screening Committee does not currently recommend population screening for alcohol misuse due to concerns about the specificity of screening tools, variability in their cut-offs, and lack of evidence linking population screening to reduced alcohol-related harm. 91 However, in integrated healthcare systems where screening is mandated and built into the electronic medical record system, screening can be nearly universal, as it is in the U.S. Veterans Health Administration system. 92
SBIRT implementation: The whole package.
SBIRT has been implemented across a range of clinical care settings around the world, including hospital emergency departments, community health clinics, specialty medical practices (e.g., sexually-transmitted disease clinics), primary care, and other community settings. 93 In the United States, in response to an Institute of Medicine call for increased community-based screening for health risk behaviors (including alcohol use), 94 SBIRT has been scaled up substantially over the past 15 years. 37 For example, the U.S. Preventive Services Task Force issued a clinical guideline for clinicians to screen all adults for alcohol misuse, and provide persons engaged in risky or hazardous drinking with brief behavioral counseling interventions. 39 In addition, the Joint Commission on Accreditation for Health Care Organizations, the major accrediting body for hospitals in the United States, now uses implementation of SBIRT as a quality indicator for general hospital care. 95 Globally, the WHO has focused on studying how to best implement Screening and Brief Intervention (SBI) for alcohol problems in primary care settings, 93 , 96 and how to integrate SBIRT into the health care systems of other countries, with notable success in South Africa, Brazil, and the European Union. 93 , 96
However, despite this investment in resources, well-recognized barriers to implementing these policies include physicians’ time constraints, lack of physicians’ interest and training, alignment with other treatment priorities, perceived lack of effectiveness of brief interventions, challenges with referral to treatment, and concerns about the accuracy of self-reported alcohol use. 96 - 99 A study of the use of SBIRT in primary care settings for adolescents additionally identified challenges related to parental involvement as a barrier to SBIRT implementation, although providers thought that increased reimbursement and dedicated resources would help improve screening rates. 98 In this vein, studies have also identified practices to help overcome challenges associated with implementing SBIRT, which include: having a start-up phase focused on comprehensive education and training, developing intra- and inter-organizational communication and collaboration, opinion leader support, practitioner and host site buy-in, and developing relationships with referral partners. 99 - 101
Evidence is lacking on the efficacy of SBIRT implementation in psychiatric emergency settings or in psychiatric outpatient settings that are not oriented to addressing substance abuse problems. One exception was an effort to implement computerized screening for alcohol and drug use among adults seeking outpatient psychiatric services within a large managed care system, which identified heavy drinking among 33% of patients who participated. 102 Given the high levels of heavy drinking and AUD among individuals with psychiatric disorders, 3 , 17 , 21 - 23 this area warrants further research.
Evidence-based behavioral interventions for heavy drinking and AUD
Because AUD arises from a complex interaction of neurobiological, genetic, and environmental factors, no single treatment works for everyone. Consensus exists that there are several evidence-based behavioral interventions that can be used to treat heavy drinking and AUD ( Table 1 ). Initially, we focus on treatments that have the greatest research support for their efficacy: motivational interviewing (MI), cognitive behavioral therapy (CBT), and contingency management (CM).
Effectiveness of behavioral interventions for treating heavy drinking and alcohol use disorder
MI is a directive, client-centered counseling style used to elicit behavior change by helping clients explore and resolve ambivalence. 103 MI targets theorized mechanisms of effectiveness, 104 - 108 including self-efficacy 109 - 118 and commitment to change. 104 , 106 MI has an extensive evidence base 42 , 48 - 56 , 104 , 119 that consistently supports its use as an effective behavior intervention to help patients reduce risky/heavy drinking. 120 MI has been shown to help patients reduce risky/heavy drinking outside of the United States, including in the United Kingdom, Canada, Australia, Europe and Brazil. 121 While MI has been studied most extensively in alcohol misuse, it is also utilized to treat dependence on other substances. 120 Advantages of MI are that it has been manualized and has a fidelity rating system. 122 Its limitations include requiring training, 123 supervision, 124 , 125 and a certain skill level. 126 Although MI is widely disseminated, 123 , 125 , 127 it is more complicated to administer than commonly assumed, 123 , 128 and its mechanism of effect is not always clear. 129
CBT focuses on challenging and changing unhelpful cognitive distortions and behaviors, improving emotional regulation, and developing personal coping strategies that target current problems. 46 , 130 - 132 CBT is viewed by many as the preferred treatment for psychiatric disorders, 133 and there is also evidence of its effectiveness to treat AUD, including in studies conducted outside of the United States. 131 , 132
CM involves the systematic reinforcement of desired behaviors (using vouchers, privileges, prizes, money, etc.) and the withholding of reinforcement or punishment of undesired behaviors. 134 Evidence supports the effectiveness of CM to improve medication adherence for AUD. 134 There is less evidence available for the effectiveness of CM to treat AUD in its own right. 135 A central challenge in implementing CM is the lack of biomarkers to detect alcohol use beyond the previous 12 hours. 136
In addition to MI, CBT, and CM, other behavioral interventions used to treat heavy drinking and AUD include 12-step facilitation, mindfulness-based interventions, couples-based therapy, and continuing care. In a multisite clinical trial, patients assigned to 12-step facilitation were as likely as those assigned to CBT, and slightly more likely than those assigned to motivational enhancement therapy, to achieve abstinence or moderate drinking without alcohol-related consequences. 137 - 139 In a systematic review of 11 mindfulness-based intervention studies, ten studies showed that mindfulness for AUD was effective compared to no treatment or a non-effective control, with some evidence to suggest it is comparable to other effective treatments. 140 A meta-analysis of couples therapy interventions for married or cohabiting individuals who sought help for AUD showed lower drinking frequency, fewer alcohol-related consequences, and better relationship satisfaction than those in individual treatment. 141 , 142 In a review of studies in which spouses and/or other family members of an alcoholic adult were involved in treatment efforts, marital and family therapy was found to be effective in helping the family cope better, and in motivating alcoholics to enter treatment when they are unwilling to seek help. 143 A systematic review that screened 15,235 studies of continuing care for AUD found only a few (n=6) high quality studies available, and concluded that adding an active intervention to usual continuing care seems to improve AUD treatment outcomes. 144
MI, CBT, and CM are the most commonly evaluated behavioral interventions used to treat individuals with co-occurring alcohol use and mood disorders. 145 While still not widely used, interventions based on these frameworks have shown initial promise in treating alcohol use among individuals with psychiatric comorbidity. 146 - 150 There is also some evidence that mindfulness-based interventions are useful for individuals with AUD and comorbid mental health conditions. 140 In contrast, a recent review found little evidence to support the effectiveness of psychosocial interventions to reduce alcohol consumption among people who use illicit drugs. 151
Medication assisted treatment (MAT) for heavy drinking and AUD
In this section, we discuss medications that are approved by one or more regulatory agencies (e.g., European Medicines Agency, U.S. Food and Drug Administration) for treating AUD. We also discuss medications for which there is empirical evidence of efficacy from placebo-controlled trials despite lack of regulatory approval. The latter group of medications may be used “off-label” to treat heavy drinking or AUD, and some are recommended as second-line medications in clinical guidelines published by healthcare entities (e.g., U.S. Veterans Administration and Department of Defense) or professional groups (e.g., American Psychiatric Association).
Withdrawal.
Alcohol withdrawal occurs on a spectrum of severity ranging from simple withdrawal, with signs and symptoms that include insomnia and tremulousness, to severe manifestations including seizures, hallucinations, and delirium tremens. 152 Most patients undergoing alcohol withdrawal can be treated safely and effectively on an outpatient basis. 153 , 154 Individuals with acute medical or psychiatric illness may require inpatient care to avoid complications of those co-occurring disorders. Benzodiazepines, which target gamma aminobutyric acid receptors to curb excitability in the brain, have the largest and the best evidence base in treating the signs and symptoms of acute alcohol withdrawal. 155 Evidence indicates that anticonvulsants also have good efficacy, either on their own or in combination with sedatives/hypnotics. 156 Treatment of alcohol withdrawal should be followed by treatment for AUD to prevent relapse to heavy drinking. 152
A number of medications are available to treat AUD ( Table 2 ). The U.S. Food and Drug Administration (FDA) has approved three medications for treating AUD: disulfiram, naltrexone, and acamprosate. 157 These medicines are also approved in the United Kingdom and other parts of Europe. Another medication, nalmefene, is approved by the European Medicines Agency (EMA) for treating AUD. 158 U.S. guidelines recommend that MAT, often in combination with a behavioral intervention, be offered to patients with a clinical indication (e.g., a positive screening test or relevant physical symptoms) of AUD. 34 , 62 We describe and review the evidence of efficacy and acceptability for each of these medications, and discuss medications that may be used off-label to treat AUD.
Effectiveness of medications for treating alcohol use disorder 20 , 179
Disulfiram.
When combined with alcohol, disulfiram increases the concentration of acetaldehyde, a toxic intermediary metabolite of alcohol. Excess amounts of acetaldehyde have unpleasant effects such as nausea, headache, and sweating. The anticipation of these unpleasant effects, rather than actually experiencing them, is considered the mechanism through which disulfiram potentially promotes patients’ avoidance of drinking. From 1949 until 1994, disulfiram was the only medication available in the United States for treating patients with alcohol dependence.
Although several clinical studies have assessed the efficacy of disulfiram in treating AUD, 159 , 160 most have not used a rigorous clinical trial methodology, 161 and a systematic review published in 1999 concluded that that the evidence for the efficacy of disulfiram was inconsistent. 162 A more recent meta-analysis of 22 randomized clinical trials using various outcome measures (e.g., continuous abstinence, number of days drinking, time to first relapse) showed a higher success rate for disulfiram than for controls, though the drug was effective only when its ingestion was supervised, and not when providers were blinded to the patients’ treatment condition. 163 Despite the potential clinical utility of disulfiram, it is not considered a primary medication for relapse prevention among patients with alcohol dependence 164 due to its adverse effects, poor adherence rate, and ethical objections to disulfiram among some clinicians. 165
Naltrexone.
Naltrexone blocks opioid receptors, stimulation of which can be involved in the pleasant sensations associated with drinking, and can reduce alcohol craving. Naltrexone was approved by the FDA as an oral medication in 1994 following the results of two randomized placebo-controlled trials (RCTs) which showed that patients treated with naltrexone had better drinking outcomes (i.e., a greater likelihood of abstinence and reduced risk of relapse) than those treated with placebo. 166 , 167 A recent meta-analysis of 53 studies found that naltrexone was associated with a significant reduction in the risk of relapse to any drinking and heavy drinking, although the effect sizes were small (5% and 9% decreased risk, respectively). 62
Despite being one of only three FDA-approved medications for treating heavy drinking and AUD, naltrexone is infrequently prescribed. 168 Various addiction providers (e.g., physicians, managers, pharmacists) have been surveyed and have identified patient non-compliance, affordability, perceived low patient demand, and concerns about efficacy as barriers to prescribing MAT for treating AUD. 169 - 171
In 2006, naltrexone was approved by the FDA for use as a long-acting injectable formulation based on a multisite RCT that compared 190-mg and 380-mg dosages with placebo in 624 actively drinking alcohol dependent adults. 172 Results of this trial indicated a 25% greater reduction in the rate of heavy drinking days (HDD) among individuals who received the 380-mg extended-release naltrexone formulation compared to those on placebo. A multicenter, placebo-controlled RCT of a second naltrexone depot formulation in patients with alcohol dependence showed the active treatment resulted in a longer time to first drinking day, and a higher frequency of abstinent days and complete abstinence during treatment than placebo. 173 Injectable naltrexone has also been found to reduce alcohol consumption in a number of real world settings, including clinical settings among HIV-positive patients with heavy drinking, 174 HIV-positive released prisoners transitioning to the community, 175 and in the criminal justice system among adults with alcohol and opioid problems. 176 Because naltrexone has demonstrated efficacy in reducing the risk of heavy drinking, it is recommended as a first-line treatment for AUD. 20 Although theoretically the long-acting injectable formulation is associated with greater adherence than oral naltrexone, there are no large comparative studies that have evaluated the relative merits of the two formulations.
Acamprosate.
Acamprosate was approved by the FDA in 2004, based on efficacy studies conducted in Europe. Although the medication is assumed to correct an imbalance between GABA and glutamate, thus easing the negative effects of quitting drinking, a more precise understanding of its mechanism of action is lacking. 177 A recent meta-analysis of 27 studies found that although acamprosate had no effect on relapse to heavy drinking, it produced a 9% reduction in the risk of relapse to any drinking. 62
Another opioid receptor antagonist, nalmefene, is approved for treating AUD in Europe but not the United States. 158 A recent meta-analysis of five RCTs among 2,567 participants found that participants taking nalmefene had fewer HDD during treatment and lower total alcohol consumption than those taking placebo. 178 However, there was considerable dropout in the nalmefene groups, often due to adverse effects, which may limit its utility in treating AUD.
Additional medications.
Several other medications are now being evaluated in the United States for treating heavy drinking and AUD, including varenicline, gabapentin, topiramate, zonisamide, baclofen, ondansetron, levetiracetam, quetiapine, aripiprazole, and serotonin reuptake inhibitors. 179 Although none of these are FDA-approved for treating AUD, they are sometimes used off-label for that purpose. Evidence has been mixed on the efficacy of these medications, their side effects, and acceptability. 180 Baclofen and topiramate currently have the most support for efficacy. 181 , 182
Treating co-occurring AUD and psychiatric disorders.
Efforts to treat AUD and co-occurring disorders such as major depression, bipolar disorder, and social anxiety disorder with MAT have evolved over time. Early efforts that used medications such as antidepressants, benzodiazepines, and lithium based on their efficacy in treating the primary psychiatric disorder had mixed success. 183 Such efforts were based on the hypothesis that a reduction in psychiatric symptoms would reduce drinking by reducing the motivation for self-medication with alcohol. In a meta-analysis of RCTs of antidepressants in patients with co-occurring major depression and a substance use disorder (including alcohol dependence), 184 the majority of studies showed a significant or near-significant advantage for the active medication over placebo, with small-to-medium effect sizes. Although studies that showed a medium effect size for treating depression also yielded a medium effect size in reducing substance use, studies that showed smaller effects on depression did not yield beneficial effects on substance use behavior, leading to the conclusion that it is necessary to treat both disorders. A good example of the recommended approach is a study of depressed patients with AUD who were treated with sertraline, naltrexone, sertraline plus naltrexone, or double placebo for 14 weeks; the combined treatment group had a significantly higher abstinence rate and longer time to relapse to heavy drinking than the other three groups, which did not differ from one another. 185 With respect to the effects on depression, at the end of treatment, the percentage of non-depressed patients in the sertraline plus naltrexone group (83·3%) versus the other treatment arms combined (58·3%) approached significance after correction for multiple comparisons. The pharmacotherapy of AUD and co-occurring psychiatric disorders remains an understudied, but clinically important area of research.
Utilization of medications.
Despite the availability of medications with demonstrated efficacy for treating AUD, they are widely underutilized. MAT is prescribed to less than 9% of patients who are likely to benefit from them. 20 A variety of obstacles to greater adoption of substance dependence medications have been identified, 169 , 186 , 187 and include both structural and philosophical barriers among substance abuse specialty providers. 188 Among a national sample of 372 organizations that deliver AUD treatment services in the United States, organizations that offered services related to health problems other than AUD (e.g., primary medical care, medications for smoking cessation, and services to address co-occurring psychiatric conditions) were more likely to offer pharmacotherapy for treating AUD. 189 Regarding the uptake of MAT, a study among a U.S. cohort of 190 publicly-funded treatment organizations that offered no substance use disorder (SUD) medications at baseline showed that 23% offered SUD medications after five years of follow-up. 190 This was more likely to occur in programs that had greater medical resources, Medicaid funding, and contact with pharmaceutical companies. 190
Further research.
Research to identify and develop medications with greater efficacy that can gain widespread clinical acceptance in treating heavy drinking and AUD remains a high priority. 20 However, several methodological barriers impede this effort and the ability to marshal stronger evidence of efficacy for approved medications. For example, MAT efficacy trials for AUD have been small, especially when compared to trials of treatments for other major public health problems such as cardiovascular disease. 89 Other methodological challenges faced by trials to treat AUD involve recruitment and retention, inclusion/exclusion criteria, measurement of medication adherence/intervention fidelity, timing of assessments, statistical analyses, and the outcome measures used. 191 , 192
Outcome measures of treatment efficacy and AUD treatment goals: Non-abstinent drinking reductions
Evaluating the efficacy of treatments for AUD should be placed in the context of evaluating the efficacy of medicines for other chronic conditions (e.g., depression, diabetes) in which a “perfect” outcome is not required for treatment to be considered successful. Historically, the favored outcome for clinical trials of MAT for AUD or alcohol dependence has been abstinence. 193 However, many participants of MAT clinical trials reduce their drinking substantially without achieving complete abstinence. 194 - 196 In this sense, abstinence is a very high-threshold outcome that may be insensitive to clinical benefit. Considering abstinence as the only successful treatment outcome is also problematic because many individuals with AUD are not interested in a goal of total abstinence, 197 - 199 and the assumption that clinicians will expect a goal of abstinence may deter them from seeking treatment at all. Recognizing this, the FDA now accepts an additional outcome for MAT clinical trials: no heavy drinking days (no-HDD; defined as no days in which more than four drinks are consumed by men and more than three drinks are consumed by women), 200 with the proportion of participants having no-HDD compared between treatment arms. However, the no-HDD outcome itself is also narrow and may be insensitive because it classifies patients as treatment failures after any HDD, even though some of these patients substantially reduce their drinking. 194 - 196 Evidence that non-abstinent reductions also provide clinical benefit has been emerging recently, with investigation into the best way to quantify clinically meaningful drinking reductions.
One measure of drinking reduction that has shown promise is the WHO four-level classification of drinking risk (very-high-risk, high-risk, moderate-risk, and low-risk). The EMA currently accepts a two-level reduction in WHO drinking risk levels as a valid clinical trial outcome. 201 , 202 The validity of a reduction in WHO drinking risk levels as a clinical trials outcome has been under investigation since 2012 by the Alcohol Clinical Trials Initiative (ACTIVE) Group, 191 , 203 with greatest interest in drinkers who are initially at the highest levels (very-high-risk and high-risk drinkers), and thus are most relevant to clinical trials for AUD. 204 For the FDA to accept reductions in WHO drinking risk levels as a valid clinical trial outcome, information is needed about the clinical benefit provided by reductions in WHO drinking risk levels, i.e., whether such reductions predict improvements in how individuals feel and function.
Thus far, several clinical studies have demonstrated clinical benefit from reductions in WHO drinking risk levels. As a best example, in a pooled analysis of data from three multisite placebo-controlled RCTs of MAT (naltrexone, varenicline, and topiramate) in adults with DSM-IV alcohol dependence, more respondents met criteria for WHO drinking risk level reductions than total abstinence or no-HDD, yet standardized treatment effects observed for the WHO drinking risk level reductions were comparable to those obtained using either abstinence or no-HDD outcomes. 205 Another study 204 used data from the COMBINE study, 206 a multisite treatment trial for alcohol dependence (n=1,383), to show that reductions in WHO drinking risk levels predicted reduced alcohol consequences on the Drinker Inventory of Consequences (DrinC) 207 and improved mental health functioning on the 12-item Short Form Health Survey (SF-12). 204 , 208 COMBINE study data has also been used to show that reductions in WHO drinking risk levels predict reductions in alcohol-related consequences and systolic blood pressure, and improved mental health functioning, liver enzyme levels, and quality of life. 209 In epidemiologic studies of U.S. drinkers (n=22,005) followed prospectively for three years, reductions from the very-high-risk and high-risk levels predicted decreased rates of overall and chronic alcohol dependence, improved SF-12 mental health functioning, 10 and reduced odds of liver disease, 210 psychiatric comorbidity, 211 and DUDs 212 ( Table 3 ). While more information on the relationship between these reductions and improvements in how individuals feel or function would further strengthen the case for using WHO drinking risk level reduction as a clinical trial outcome, 213 overall, the evidence thus far supports reductions from the highest levels of the four-level WHO drinking risk categories as valid outcomes.
Health outcomes associated with drinking reductions as defined by the WHO drinking risk levels (drinks per day) and change in WHO risk level between Wave 1 (2001-2002) and Wave 2 (2004-2005) of the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) 10 , 210 - 212
▼= decreased risk; ▲ = increased risk; ▼/▲= p≤0·05; ▼ / ▲ = p>0·05; R = reference group; --- = contrast could not be computed because the prevalence of condition at Wave 2 was 0·0%
Note: AUDIT-C results are not included because there were very high proportions of participants at the WHO very-high-risk and high-risk drinking levels with Wave 1 positive AUDIT-C scores; therefore, adjusted odds of positive Wave 2 AUDIT-C scores by change in WHO drinking risk level could not be produced because the regression models used to produce them did not converge.
Adopting valid non-abstinent drinking reduction measures may benefit research (and ultimately, treatment) if such drinking reductions are more sensitive indicators of treatment efficacy (including both behavioral and medication-assisted treatment) than the outcome measures now commonly used. Furthermore, demonstrating that clinical benefit is associated with non-abstinent drinking reductions (including sustained improvements in how individuals feel and function) could serve an additional important purpose by broadening interest in treatment. 157 Offering drinking reduction goals to patients who are not interested in an initial abstinence goal could encourage more of these individuals to enter treatment. 197 Some patients may benefit from reducing their drinking without a need to become abstinent, while other patients, after engaging in treatment, may decide that abstinence is a better goal for them. In summary, non-abstinent drinking reductions could extend the repertoire of tools available to clinicians to treat heavy drinking and AUD by strengthening clinical trial design and broadening interest in treatment.
The use of technology to prevent and treat heavy drinking and AUD
Ehealth and mhealth..
The use of digital technology to prevent and treat heavy drinking and AUD is often called eHealth (electronic-Health) or mHealth (mobile-Health). Even in situations where clinical care is provided onsite, 214 , 215 eHealth and mHealth interventions are emerging as ways to help meet the need for patient self-management and continuing care. 216
Evidence base for eHealth and mHealth interventions.
There is a growing evidence base for the effectiveness of eHealth and mHealth interventions. A recent meta-analysis of 57 studies of digital interventions for alcohol consumption in community-dwelling populations found moderate-quality evidence that digital interventions decrease alcohol consumption. 217 In addition, a meta-analysis of 26 brief web-based or computer-based interventions targeting young adults demonstrated a significant reduction in the mean number of drinks consumed weekly compared to control conditions. 218 eHealth and mHealth interventions have also been developed to address alcohol-related problems. However, a recent systematic review concluded that digital interventions were not consistently effective in people with AUD, and the heterogeneity of interventions, particularly in terms of their complexity, made reaching a consensus about their overall effectiveness challenging. 219 The review also noted that many interventions did not report on outcomes other than changes in drinking levels, such as psychological health or social functioning. 219 The complexity of AUD, which is characterized not only by compulsive alcohol use, but also by loss of control over alcohol intake and a negative emotional state when not using, may increase the challenge of addressing it through a digital platform.
The importance of mHealth is greater in low- and middle-income countries where people lack access to medical care but, oftentimes have a mobile phone. 220 A recent review identified six studies of mHealth interventions that targeted alcohol consumption in low- and middle-income countries (Brazil, Thailand, and Uruguay), all of which demonstrated efficacy in reducing drinking. 220
Examples of eHealth and mHealth interventions.
Several mHealth interventions delivered via smartphone have demonstrated acceptability, feasibility, and efficacy in reducing alcohol consumption among individuals with AUD. 214 The Addiction-Comprehensive Health Enhancement Support System (A-CHESS) promotes AUD recovery through high-risk GPS location tracking, educational resources, social support, a “panic button” (which triggers automated reminders about personal motivations for not drinking, provides alerts to people who could reach out to the user, and offers tools for dealing with urges), regular assessments, and relaxation tools. 221 - 223 A-CHESS users reported significantly fewer risky drinking days than participants in a control condition. 224 Another mHealth intervention, the Location-Based Monitoring and Intervention for Alcohol Use Disorders (LBMI-A), promotes AUD recovery through psychoeducational modules and other features, including high-risk location tracking, regular assessments, social support (users can share their assessment feedback with self-identified supportive others), and motivational tools. 225 , 226 LBMI-A users demonstrated significant decreases in self-reported HDD and drinks per week, and a significant increase in the proportion of days abstinent compared to participants assigned to an online, brief motivational intervention plus bibliotherapy. 226
Other mHealth interventions have been developed to address high-risk drinking in specialized populations. For example, HealthCall 227 , 228 targets drinking reductions among HIV-positive patients with heavy drinking by extending patient engagement beyond an initial brief MI-based intervention with little additional staff time or effort. 229 HealthCall participants had significantly greater reduction in multiple measures of alcohol consumption than a control condition. 227 , 229
Effective eHealth and mHealth interventions have also been developed to address alcohol consumption in patients with co-occurring alcohol and mental health problems. For example, the DEpression-ALcohol (DEAL) Project, a web-based self-help intervention, was associated with statistically significant reductions in quantity and frequency of alcohol use at three months post-intervention in young adults (ages 18–25 years) compared to participants assigned to a web-based attention-control condition. 230 A-CHESS was also translated and adapted for Spanish-speaking individuals with co-occurring alcohol and mental health disorders, and was found to have good acceptability; 231 results of its efficacy have not yet been published.
Future research.
eHealth and mHealth interventions could potentially become more effective if they are adjusted to the individual needs of users, which are often influenced by psychiatric problems such as depression, anxiety, and personality disorders. Little work of this type has been done thus far, but could contribute to reducing the burden of co-occurring AUD and psychiatric disorders, especially if the interventions could be disseminated in real-world clinical settings. 219 Achieving this will likely require a better understanding of how people incorporate technology in their everyday lives, as well as research into effective ways to disseminate interventions that are efficacious in clinical trials. Future research is also needed to examine how mHealth interventions can be better adapted to match the user’s level of alcohol consumption, 232 and to investigate the impact of moderators such as sex, age, race, and comorbid psychiatric disorders on the efficacy of technology-based drinking reduction interventions.
Population-level interventions to prevent and treat heavy drinking and AUD
Beyond the individual-level methods of preventing and treating heavy drinking and AUD discussed thus far, population-level approaches to alcohol prevention are also important. 29 A large base of evidence is available to inform the development and modification of alcohol-related harm prevention policies ( Table 4 ). 30 , 31
Effectiveness of alcohol-related harm prevention policies 30 , 31
Evidence base for effective population-level interventions.
According to multiple reviews, there is clear and consistent evidence that regulating the availability of alcohol is efficacious and cost-effective in reducing overall alcohol consumption and alcohol-related harm. 233 , 234 Limiting alcohol availability is achieved by increasing the price of alcohol, mainly through taxation, which deters consumption because of the increased cost. Other forms of regulation include a minimum purchase age, restricting the days and hours of sale, and regulating the venues where alcohol can be sold. Addressing the marketing of alcohol has the potential to be efficacious and cost-effective in reducing overall alcohol consumption and alcohol-related harm as well. This can be achieved by instating content guidelines and limiting the volume of advertising by alcohol companies, particularly advertising that targets youth. However, evidence suggests that self-regulation of alcohol marketing within the beverage industry is not effective in enforcing these rules. 30 , 31 Other reviews note there is also strong evidence that alcohol-related policies regarding drunk driving implemented through legislation and its enforcement are effective, i.e., lowering the legally allowable blood alcohol concentration level, establishing sobriety checkpoints, and mandating treatment for alcohol-impaired driving offenses. 30 , 31
Many campaigns that provide information and education to the general public increase awareness of alcohol-related harm, but lack evidence for their ability to produce long-lasting changes in behavior. 31 However, these campaigns may help raise awareness and acceptance of efforts to address alcohol consumption through other, more effective policy-level actions. 30 A long-standing, multi-pronged campaign to increase women’s awareness of the risks of drinking during pregnancy 235 may be an important exception to the overall lack of evidence for long-term change from public education, as evidenced by significant increases in the rate of binge drinking between 2002 and 2014 in non-pregnant U.S. women of reproductive age, but not among pregnant women. 236 Reviews note the evidence is weaker for the effectiveness of other population-level interventions to reduce alcohol-related harm, including those that work at the family- and community-level, those based in schools, workplaces, or alcohol serving settings, and those that target illicit alcohol sales. 29
Because most countries do not have adequate policies in place to minimize alcohol-related harm, 237 there is a great need to implement efficacious, cost-effective policies. Efforts to scale up such policies are complicated by the ever-present tension between the beverage industry, whose goal is to increase alcohol consumption, and public health concerns, whose goal is to reduce harmful consumption. Some alcohol industry strategies may seek to undermine effective health policies and programs, increasing the challenges to their implementation and efficacy. 238 , 239 An area meriting exploration is how the alcohol policy environment impacts the efficacy of individual-level methods in preventing and treating heavy drinking and AUD, including among individuals with comorbid psychiatric disorders. More complete knowledge of how individual-level and socio-ecological-level factors interact in the prevention and treatment of AUD would facilitate better targeting of prevention efforts, a particularly important concern given the limited resources available to minimize alcohol-related morbidity and mortality.
Concluding remarks and future directions
This review provides a critical discussion of widely used approaches for the prevention, identification, and treatment of heavy drinking and AUD, including recent interventions that have sought to harness the power of technology. The use of different measures of alcohol consumption (e.g., heavy drinking, binge drinking) and alcohol-related disorders (e.g., harmful drinking, alcohol dependence, AUD) throughout the literature poses challenges to generalizability across studies. Although practitioners not specializing in alcohol treatment are often unaware of the guidelines for preventing, identifying, and treating heavy drinking and AUD, consensus on certain guidelines does exist, and valuable tools are available. 34 Efforts are underway to continue developments in this area, with a focus on preventing, identifying, and treating heavy drinking and AUD among individuals who also suffer from psychiatric and drug use disorders.
One promising area of future research aims to identify individual-level factors that predict treatment response. These include phenotypic predictors such as types of drinker (e.g., reward vs. relief), 240 and genetic predictors such as variation in genes that encode neurotransmitter receptors. 241 , 242 Project MATCH found a number of patient characteristics that predicted response to psychotherapies at follow-up (e.g., psychiatric severity), 137 but not during the treatment period. 138 These approaches, now subsumed under the heading of precision medicine, are an important direction for future research.
Given that alcohol use and binge drinking have increased more in adult women than men over the past several years, 2 , 243 more research is needed on prevention and treatment efforts that address the specific needs of adult women. Also, treatment providers continue to seek more information on heavy drinking and AUD among individuals with co-occurring psychiatric disorders, including drug use disorders. Although researchers can be reluctant to undertake these more complicated studies, and grant review committees may be critical of the study designs due to the increased heterogeneity of samples characterized by comorbidity, this remains an important area that requires further research. Other key issues for future research include: 1) the short- and long-term efficacy of school-based alcohol prevention interventions; 2) targeted prevention efforts focused on identifying youth at increased risk for developing heavy drinking or AUD; 3) improving the efficacy and implementation of SBIRT in clinical settings; 4) assessing the effectiveness of SBIRT in settings where it is currently implemented; 5) implementing SBIRT or similar procedures in mental health settings; 6) improving the uptake of MAT for patients who are eligible and interested in receiving it; 7) developing additional medication options; 8) evaluating the benefits of non-abstinent drinking reductions for clinical trial outcomes; 9) precision medicine; 10) scaling up technology-based interventions beyond the confines of efficacy trials; and 11) examining how the alcohol policy environment impacts individual-level methods of preventing and treating heavy drinking and AUD, including among patients with psychiatric comorbidity. Given the high prevalence of harmful alcohol use and its adverse health consequences, developing a fuller understanding of these issues is a public health priority.
Acknowledgments
Research funding is acknowledged from NIAAA (R01AA025309, PI: Hasin; R01AA023192, PI: Kranzler; R01AA021164, PI: Kranzler); New York State Psychiatric Institute; the Alcohol Clinical Trials Initiative (ACTIVE); the Mental Illness Research, Education and Clinical Center of the Veterans Integrated Service Network 4, U.S. Department of Veterans Affairs; and NIDA (T32DA031099, for Knox; PI: Hasin). The funding sources had no role in study design; in the collection, analysis, and interpretation of data; in the writing of the report; or in the decision to submit the paper for publication.
Conflict of interests
DSH and HRK are members of the American Society of Clinical Psychopharmacology’s Alcohol Clinical Trials Initiative (ACTIVE), which in the past three years was sponsored by AbbVie, Alkermes, Amygdala Neurosciences, Arbor Pharmaceuticals, Ethypharm, Indivior, Lilly, Lundbeck, Otsuka, and Pfizer. HRK is named as an inventor on PCT patent application #15/878,640 entitled "Genotype-guided dosing of opioid agonists," filed January 24, 2018. DSH acknowledges support from Campbell Alliance for an unrelated project on the measurement of opioid addiction. JK and FRRL declare no conflicts of interest.
- 1. GBD 2016 Alcohol Collaborators. Alcohol use and burden for 195 countries and territories, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet 2018; 392(10152): 1015–35. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 2. Grant BF, Chou SP, Saha TD, et al. Prevalence of 12-month alcohol use, high-risk drinking, and DSM-IV alcohol use disorder in the United States, 2001–2002 to 2012–2013: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. JAMA Psychiatry 2017; 74(9): 911–23. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 3. Grant BF, Goldstein RB, Saha TD, et al. Epidemiology of DSM-5 alcohol use disorder: Results from the National Epidemiologic Survey on Alcohol and Related Conditions III. JAMA Psychiatry 2015; 72(8): 757–66. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 4. Parker AJ, Marshall EJ, Ball DM. Diagnosis and management of alcohol use disorders. BMJ 2008; 336(7642): 496–501. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 5. Saunders JB. Substance use and addictive disorders in DSM-5 and ICD 10 and the draft ICD 11. Curr Opin Psychiatry 2017; 30(4): 227–37. [ DOI ] [ PubMed ] [ Google Scholar ]
- 6. Saunders JB, Peacock A, Degenhardt L. Alcohol use disorders in the draft ICD-11, and how they compare with DSM-5. Current Addiction Reports 2018; 5: 257–64. [ Google Scholar ]
- 7. Degenhardt L, Bharat C, Bruno R, et al. Concordance between the diagnostic guidelines for alcohol and cannabis use disorders in the draft ICD-11 and other classification systems: Analysis of data from the WHO’s World Mental Health Surveys. Addiction 2019; 114(3): 534–52. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 8. Saunders JB, Aasland OG, Babor TF, de la Fuente JR, Grant M. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO Collaborative Project on Early Detection of Persons with Harmful Alcohol Consumption-II. Addiction 1993; 88(6): 791–804. [ DOI ] [ PubMed ] [ Google Scholar ]
- 9. Bohn MJ, Babor TF, Kranzler HR. The Alcohol Use Disorders Identification Test (AUDIT): Validation of a screening instrument for use in medical settings. J Stud Alcohol 1995; 56(4): 423–32. [ DOI ] [ PubMed ] [ Google Scholar ]
- 10. Hasin DS, Wall M, Witkiewitz K, et al. Change in non-abstinent WHO drinking risk levels and alcohol dependence: A 3 year follow-up study in the US general population. Lancet Psychiatry 2017; 4(6): 469–76. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 11. Centers for Disease Control and Prevention. Fact sheets: Alcohol use and your health. 2018. https://www.cdc.gov/alcohol/fact-sheets/alcohol-use.htm (accessed Jan 8, 2018).
- 12. Room R, Babor T, Rehm J. Alcohol and public health. Lancet 2005; 365(9458): 519–30. [ DOI ] [ PubMed ] [ Google Scholar ]
- 13. Rehm J, Gmel G, Sempos CT, Trevisan M. Alcohol-related morbidity and mortality. Alcohol Res Health 2003; 27(1): 39–51. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 14. Rehm J Alcohol and all-cause mortality. Int J Epidemiol 1996; 25(1): 215–6; author reply 8–20. [ DOI ] [ PubMed ] [ Google Scholar ]
- 15. Lewis-Laietmark C, Wettlaufer A, Shield KD, et al. The effects of alcohol-related harms to others on self-perceived mental well-being in a Canadian sample. Int J Public Health 2017; 62(6): 669–78. [ DOI ] [ PubMed ] [ Google Scholar ]
- 16. Greenfield TK, Karriker-Jaffe KJ, Kaplan LM, Kerr WC, Wilsnack SC. Trends in alcohol’s harms to others (AHTO) and co-occurrence of family-related AHTO: The four US national alcohol surveys, 2000–2015. Subst Abuse 2015; 9(Suppl 2): 23–31. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 17. Hasin DS, Stinson FS, Ogburn E, Grant BF. Prevalence, correlates, disability, and comorbidity of DSM-IV alcohol abuse and dependence in the United States: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry 2007; 64(7): 830–42. [ DOI ] [ PubMed ] [ Google Scholar ]
- 18. Cohen E, Feinn R, Arias A, Kranzler HR. Alcohol treatment utilization: Findings from the National Epidemiologic Survey on Alcohol and Related Conditions. Drug Alcohol Depend 2007; 86(2–3): 214–21. [ DOI ] [ PubMed ] [ Google Scholar ]
- 19. Shield KD, Rehm J, Rehm MX, Gmel G, Drummond C. The potential impact of increased treatment rates for alcohol dependence in the United Kingdom in 2004. BMC Health Serv Res 2014; 14: 53. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 20. Kranzler HR, Soyka M. Diagnosis and pharmacotherapy of alcohol use disorder: A review. JAMA 2018; 320(8): 815–24. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 21. Grant BF, Stinson FS, Dawson DA, et al. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry 2004; 61(8): 807–16. [ DOI ] [ PubMed ] [ Google Scholar ]
- 22. Hasin DS, Goodwin RD, Stinson FS, Grant BF. Epidemiology of major depressive disorder: Results from the National Epidemiologic Survey on Alcoholism and Related Conditions. Arch Gen Psychiatry 2005; 62(10): 1097–106. [ DOI ] [ PubMed ] [ Google Scholar ]
- 23. Hasin DS, Sarvet AL, Meyers JL, et al. Epidemiology of adult DSM-5 major depressive disorder and its specifiers in the United States. JAMA Psychiatry 2018; 75(4): 336–46. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 24. Grant BF, Saha TD, Ruan WJ, et al. Epidemiology of DSM-5 drug use disorder: Results from the National Epidemiologic Survey on Alcohol and Related Conditions-III. JAMA Psychiatry 2016; 73(1): 39–47. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 25. Witkiewitz K, Villarroel NA. Dynamic association between negative affect and alcohol lapses following alcohol treatment. J Consult Clin Psychol 2009; 77(4): 633–44. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 26. Newes-Adeyi G, Chen CM, Williams GD, Faden VB. Trends in underage drinking in the United States, 1991–2003. Rockville, MD: National Institute on Alcohol Abuse and Alcoholism, 2005. [ Google Scholar ]
- 27. Lim SS, Vos T, Flaxman AD, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012; 380(9859): 2224–60. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 28. Stigler MH, Neusel E, Perry CL. School-based programs to prevent and reduce alcohol use among youth. Alcohol Res Health 2011; 34(2): 157–62. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 29. Martineau F, Tyner E, Lorenc T, Petticrew M, Lock K. Population-level interventions to reduce alcohol-related harm: An overview of systematic reviews. Prev Med 2013; 57(4): 278–96. [ DOI ] [ PubMed ] [ Google Scholar ]
- 30. Anderson P, Chisholm D, Fuhr DC. Effectiveness and cost-effectiveness of policies and programmes to reduce the harm caused by alcohol. Lancet 2009; 373(9682): 2234–46. [ DOI ] [ PubMed ] [ Google Scholar ]
- 31. Burton R, Henn C, Lavoie D, et al. A rapid evidence review of the effectiveness and cost-effectiveness of alcohol control policies: An English perspective. Lancet 2017; 389(10078): 1558–80. [ DOI ] [ PubMed ] [ Google Scholar ]
- 32. Watkins KE, Ober AJ, Lamp K, et al. Collaborative care for opioid and alcohol use disorders in primary care: The SUMMIT randomized clinical trial. JAMA Intern Med 2017; 177(10): 1480–8. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 33. Willenbring ML, Massey SH, Gardner MB. Helping patients who drink too much: An evidence-based guide for primary care clinicians. Am Fam Physician 2009; 80(1): 44–50. [ PubMed ] [ Google Scholar ]
- 34. National Institute on Alcohol Abuse and Alcoholism. Helping patients who drink too much: A clinician’s guide: National Institute on Alcohol Abuse and Alcoholism, 2005. [ Google Scholar ]
- 35. Babor TF, Del Boca F, Bray JW. Screening, brief intervention and referral to treatment: Implications of SAMHSA’s SBIRT initiative for substance abuse policy and practice. Addiction 2017; 112 Suppl 2: 110–7. [ DOI ] [ PubMed ] [ Google Scholar ]
- 36. Babor TF, McRee BG, Kassebaum PA, Grimaldi PL, Ahmed K, Bray J. Screening, brief intervention, and referral to treatment (SBIRT): Toward a public health approach to the management of substance abuse. Subst Abus 2007; 28(3): 7–30. [ DOI ] [ PubMed ] [ Google Scholar ]
- 37. Bray JW, Del Boca FK, McRee BG, Hayashi SW, Babor TF. Screening, brief intervention and referral to treatment (SBIRT): Rationale, program overview and cross-site evaluation. Addiction 2017; 112 Suppl 2: 3–11. [ DOI ] [ PubMed ] [ Google Scholar ]
- 38. US Preventive Services Task Force, Curry SJ, Krist AH, et al. Screening and behavioral counseling interventions to reduce unhealthy alcohol use in adolescents and adults: US Preventive Services Task Force recommendation statement. JAMA 2018; 320(18): 1899–909. [ DOI ] [ PubMed ] [ Google Scholar ]
- 39. Moyer VA, Preventive Services Task Force. Screening and behavioral counseling interventions in primary care to reduce alcohol misuse: U.S. preventive services task force recommendation statement. Ann Intern Med 2013; 159(3): 210–8. [ DOI ] [ PubMed ] [ Google Scholar ]
- 40. Saitz R Alcohol screening and brief intervention in primary care: Absence of evidence for efficacy in people with dependence or very heavy drinking. Drug Alcohol Rev 2010; 29(6): 631–40. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 41. Whitlock EP, Green CA, Polen MR, et al. Behavioral counseling interventions in primary care to reduce risky/harmful alcohol use. Rockville: Agency for Healthcare Research and Quality (US), 2004. [ PubMed ] [ Google Scholar ]
- 42. Whitlock EP, Polen MR, Green CA, Orleans T, Klein J. Behavioral counseling interventions in primary care to reduce risky/harmful alcohol use by adults: A summary of the evidence for the U.S. Preventive Services Task Force. Ann Intern Med 2004; 140(7): 557–68. [ DOI ] [ PubMed ] [ Google Scholar ]
- 43. Chi FW, Weisner CM, Mertens JR, Ross TB, Sterling SA. Alcohol brief intervention in primary care: Blood pressure outcomes in hypertensive patients. J Subst Abuse Treat 2017; 77: 45–51. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 44. Kaner EF, Beyer F, Dickinson HO, et al. Effectiveness of brief alcohol interventions in primary care populations. Cochrane Database Syst Rev 2007; (2). [ DOI ] [ PubMed ] [ Google Scholar ]
- 45. Bertholet N, Daeppen JB, Wietlisbach V, Fleming M, Burnand B. Reduction of alcohol consumption by brief alcohol intervention in primary care: Systematic review and meta-analysis. Arch Intern Med 2005; 165(9): 986–95. [ DOI ] [ PubMed ] [ Google Scholar ]
- 46. Ray LA, Bujarski S, Grodin E, et al. State-of-the-art behavioral and pharmacological treatments for alcohol use disorder. Am J Drug Alcohol Abuse 2019; 45(2): 124–40. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 47. Pringle JL, Kowalchuk A, Meyers JA, Seale JP. Equipping residents to address alcohol and drug abuse: The national SBIRT residency training project. J Grad Med Educ 2012; 4(1): 58–63. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 48. Hettema J, Steele J, Miller WR. Motivational interviewing. Annu Rev Clin Psychol 2005; 1: 91–111. [ DOI ] [ PubMed ] [ Google Scholar ]
- 49. Dunn C, Deroo L, Rivara FP. The use of brief interventions adapted from motivational interviewing across behavioral domains: A systematic review. Addiction 2001; 96(12): 1725–42. [ DOI ] [ PubMed ] [ Google Scholar ]
- 50. Burke BL, Arkowitz H, Menchola M. The efficacy of motivational interviewing: A meta-analysis of controlled clinical trials. J Consult Clin Psychol 2003; 71(5): 843–61. [ DOI ] [ PubMed ] [ Google Scholar ]
- 51. Bien TH, Miller WR, Tonigan JS. Brief interventions for alcohol problems: A review. Addiction 1993; 88(3): 315–35. [ DOI ] [ PubMed ] [ Google Scholar ]
- 52. Burke BL, Vassilev G, Kantchelov A, Zweben A. Motivational interviewing with couples In: Miller WR, Rollnick S, eds. Motivational interviewing: Preparing people for change. 2nd ed. New York: The Guilford Press; 2002: 347–61. [ Google Scholar ]
- 53. Miller WR, Brown J, Simpson TL, et al. What works? A methodological analysis of the alcohol treatment outcome in literature In: Hester RK, Miller WR, eds. Handbook of alcoholism treatment approaches: Effective alternatives. 2nd ed. Boston: Allyn & Bacon; 1995: 12–44. [ Google Scholar ]
- 54. Fleming MF, Balousek SL, Grossberg PM, et al. Brief physician advice for heavy drinking college students: A randomized controlled trial in college health clinics. J Stud Alcohol Drugs 2010; 71(1): 23–31. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 55. Longabaugh R, Woolard RE, Nirenberg TD, et al. Evaluating the effects of a brief motivational intervention for injured drinkers in the emergency department. J Stud Alcohol 2001; 62(6): 806–16. [ DOI ] [ PubMed ] [ Google Scholar ]
- 56. Hungerford DW, Williams JM, Furbee PM, et al. Feasibility of screening and intervention for alcohol problems among young adults in the ED. Am J Emerg Med 2003; 21(1): 14–22. [ DOI ] [ PubMed ] [ Google Scholar ]
- 57. Beich A, Gannik D, Malterud K. Screening and brief intervention for excessive alcohol use: Qualitative interview study of the experiences of general practitioners. BMJ 2002; 325(7369): 870. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 58. Beich A, Gannik D, Saelan H, Thorsen T. Screening and brief intervention targeting risky drinkers in Danish general practice: A pragmatic controlled trial. Alcohol Alcohol 2007; 42(6): 593–603. [ DOI ] [ PubMed ] [ Google Scholar ]
- 59. Beich A, Thorsen T, Rollnick S. Screening in brief intervention trials targeting excessive drinkers in general practice: Systematic review and meta-analysis. BMJ 2003; 327(7414): 536–42. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 60. Vasilaki EI, Hosier SG, Cox WM. The efficacy of motivational interviewing as a brief intervention for excessive drinking: A meta-analytic review. Alcohol Alcohol 2006; 41(3): 328–35. [ DOI ] [ PubMed ] [ Google Scholar ]
- 61. Bogenschutz MP, Donovan DM, Mandler RN, et al. Brief intervention for patients with problematic drug use presenting in emergency departments: A randomized clinical trial. JAMA Intern Med 2014; 174(11): 1736–45. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 62. Jonas DE, Amick HR, Feltner C, et al. Pharmacotherapy for adults with alcohol use disorders in outpatient settings: A systematic review and meta-analysis. JAMA 2014; 311(18): 1889–900. [ DOI ] [ PubMed ] [ Google Scholar ]
- 63. Wilk AI, Jensen NM, Havighurst TC. Meta-analysis of randomized control trials addressing brief interventions in heavy alcohol drinkers. J Gen Intern Med 1997; 12(5): 274–83. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 64. Chambers JE, Brooks AC, Medvin R, et al. Examining multi-session brief intervention for substance use in primary care: Research methods of a randomized controlled trial. Addict Sci Clin Pract 2016; 11(1): 8. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 65. Moyer A, Finney JW, Swearingen CE, Vergun P. Brief interventions for alcohol problems: A meta-analytic review of controlled investigations in treatment-seeking and non-treatment-seeking populations. Addiction 2002; 97(3): 279–92. [ DOI ] [ PubMed ] [ Google Scholar ]
- 66. Miller WR, Baca C, Compton WM, et al. Addressing substance abuse in health care settings. Alcohol Clin Exp Res 2006; 30(2): 292–302. [ DOI ] [ PubMed ] [ Google Scholar ]
- 67. Glass JE, Hamilton AM, Powell BJ, Perron BE, Brown RT, Ilgen MA. Specialty substance use disorder services following brief alcohol intervention: A meta-analysis of randomized controlled trials. Addiction 2015; 110(9): 1404–15. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 68. Glass JE, Hamilton AM, Powell BJ, Perron BE, Brown RT, Ilgen MA. Revisiting our review of screening, brief intervention and referral to treatment (SBIRT): Meta-analytical results still point to no efficacy in increasing the use of substance use disorder services. Addiction 2016; 111(1): 181–3. [ DOI ] [ PubMed ] [ Google Scholar ]
- 69. Castellón PC, Cardenas G, Feaster DJ, et al. Desire for substance use disorder treatment among HIV-infected substance users in two U.S. southern cities. Annual Meeting of the American Public Health Association; 2015 Nov; Chicago, IL; 2015. [ Google Scholar ]
- 70. Kim TW, Bernstein J, Cheng DM, et al. Receipt of addiction treatment as a consequence of a brief intervention for drug use in primary care: A randomized trial. Addiction 2017; 112(5): 818–27. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 71. Saitz R ‘SBIRT’ is the answer? Probably not. Addiction 2015; 110(9): 1416–7. [ DOI ] [ PubMed ] [ Google Scholar ]
- 72. Keyes KM, Hatzenbuehler ML, McLaughlin KA, et al. Stigma and treatment for alcohol disorders in the United States. Am J Epidemiol 2010; 172(12): 1364–72. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 73. Probst C, Moyo D, Purshouse R, Rehm J. Transition probabilities for four states of alcohol use in adolescence and young adulthood: What factors matter when? Addiction 2015; 110(8): 1272–80. [ DOI ] [ PubMed ] [ Google Scholar ]
- 74. van Amsterdam J, van den Brink W. Reduced-risk drinking as a viable treatment goal in problematic alcohol use and alcohol dependence. J Psychopharmacol 2013; 27(11): 987–97. [ DOI ] [ PubMed ] [ Google Scholar ]
- 75. Substance Abuse and Mental Health Services Administration. Key substance use and mental health indicators in the United States: Results from the 2016 National Survey on Drug Use and Health. Rockville: Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration, 2017. [ Google Scholar ]
- 76. Hasin DS, Sarvet AL, Cerda M, et al. US adult illicit cannabis use, cannabis use disorder, and medical marijuana laws: 1991–1992 to 2012–2013. JAMA Psychiatry 2017; 74(6): 579–88. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 77. Martins SS, Sarvet A, Santaella-Tenorio J, Saha T, Grant BF, Hasin DS. Changes in US lifetime heroin use and heroin use disorder: Prevalence from the 2001–2002 to 2012–2013 National Epidemiologic Survey on Alcohol and Related Conditions. JAMA Psychiatry 2017; 74(5): 445–55. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 78. Compton WM, Cottler LB, Jacobs JL, Ben-Abdallah A, Spitznagel EL. The role of psychiatric disorders in predicting drug dependence treatment outcomes. Am J Psychiatry 2003; 160(5): 890–955. [ DOI ] [ PubMed ] [ Google Scholar ]
- 79. Degenhardt L, Hall W. Extent of illicit drug use and dependence, and their contribution to the global burden of disease. Lancet 2012; 379(9810): 55–70. [ DOI ] [ PubMed ] [ Google Scholar ]
- 80. Kessler RC. The epidemiology of dual diagnosis. Biological Psychiatry 2004; 56(10): 730–7. [ DOI ] [ PubMed ] [ Google Scholar ]
- 81. Nock MK, Borges G, Bromet EJ, et al. Cross-national prevalence and risk factors for suicidal ideation, plans and attempts. Br J Psychiatry 2008; 192(2): 98–105. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 82. O’Brien CP, Charney DS, Lewis L, et al. Priority actions to improve the care of persons with co-occurring substance abuse and other mental disorders: A call to action. Biol Psychiatry 2004; 56(10): 703–13. [ DOI ] [ PubMed ] [ Google Scholar ]
- 83. Yuodelis-Flores C, Ries RK. Addiction and suicide: A review. The American Journal on Addictions 2015; 24(2): 98–104. [ DOI ] [ PubMed ] [ Google Scholar ]
- 84. Madras BK, Compton WM, Avula D, Stegbauer T, Stein JB, Clark HW. Screening, brief interventions, referral to treatment (SBIRT) for illicit drug and alcohol use at multiple healthcare sites: Comparison at intake and 6 months later. Drug Alcohol Depend 2009; 99(1–3): 280–95. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 85. Saitz R Candidate performance measures for screening for, assessing, and treating unhealthy substance use in hospitals: Advocacy or evidence-based practice? Ann Intern Med 2010; 153(1): 40–3. [ DOI ] [ PubMed ] [ Google Scholar ]
- 86. Glass JE, Andreasson S, Bradley KA, et al. Rethinking alcohol interventions in health care: A thematic meeting of the International Network on Brief Interventions for Alcohol & Other Drugs (INEBRIA). Addict Sci Clin Pract 2017; 12(1): 14. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 87. Saitz R Lost in translation: The perils of implementing alcohol brief intervention when there are gaps in evidence and its interpretation. Addiction 2014; 109(7): 1060–2. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 88. Hingson R, Compton WM. Screening and brief intervention and referral to treatment for drug use in primary care: Back to the drawing board. JAMA 2014; 312(5): 488–9. [ DOI ] [ PubMed ] [ Google Scholar ]
- 89. McKnight-Eily LR, Liu Y, Brewer RD, et al. Vital signs: Communication between health professionals and their patients about alcohol use, 44 states and the District of Columbia, 2011. MMWR Morb Mortal Wkly Rep 2014; 63(1): 16–22. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 90. Bradley KA, Lapham GT, Hawkins EJ, et al. Quality concerns with routine alcohol screening in VA clinical settings. J Gen Intern Med 2011; 26(3): 299–306. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 91. United Kingdom National Screening Committee. The UK NSC recommendation on alcohol misuse screening in adults. March 2017. https://legacyscreening.phe.org.uk/alcohol .
- 92. Bradley KA, Williams EC, Achtmeyer CE, Volpp B, Collins BJ, Kivlahan DR. Implementation of evidence-based alcohol screening in the Veterans Health Administration. Am J Manag Care 2006; 12(10): 597–606. [ PubMed ] [ Google Scholar ]
- 93. Agerwala SM, McCance-Katz EF. Integrating screening, brief intervention, and referral to treatment (SBIRT) into clinical practice settings: A brief review. J Psychoactive Drugs 2012; 44(4): 307–17. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 94. Institute of Medicine. Crossing the quality chasm: A new health system for the 21st century. Washington: National Academies Press; 2001. [ PubMed ] [ Google Scholar ]
- 95. Makdissi R, Stewart SH. Care for hospitalized patients with unhealthy alcohol use: A narrative review. Addict Sci Clin Pract 2013; 8: 11. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 96. Babor TE, Higgins-Biddle J, Dauser D, Higgins P, Burleson JA. Alcohol screening and brief intervention in primary care settings: Implementation models and predictors. J Stud Alcohol 2005; 66(3): 361–8. [ DOI ] [ PubMed ] [ Google Scholar ]
- 97. Senreich E, Ogden LP, Greenberg JP. A postgraduation follow-up of social work students trained in “SBIRT”: Rates of usage and perceptions of effectiveness. Soc Work Health Care 2017; 56(5): 412–34. [ DOI ] [ PubMed ] [ Google Scholar ]
- 98. Palmer A, Karakus M, Mark T. Barriers faced by physicians in screening for substance use disorders among adolescents. Psychiatr Serv 2019. [ DOI ] [ PubMed ] [ Google Scholar ]
- 99. Rahm AK, Boggs JM, Martin C, et al. Facilitators and barriers to implementing screening, brief intervention, and referral to treatment (SBIRT) in primary care in integrated health care settings. Subst Abus 2015; 36(3): 281–8. [ DOI ] [ PubMed ] [ Google Scholar ]
- 100. Vendetti J, Gmyrek A, Damon D, Singh M, McRee B, Del Boca F. Screening, brief intervention and referral to treatment (SBIRT): Implementation barriers, facilitators and model migration. Addiction 2017; 112 Suppl 2: 23–33. [ DOI ] [ PubMed ] [ Google Scholar ]
- 101. Hargraves D, White C, Frederick R, et al. Implementing SBIRT (Screening, Brief Intervention and Referral to Treatment) in primary care: Lessons learned from a multi-practice evaluation portfolio. Public Health Rev 2017; 38: 31. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 102. Satre D, Wolfe W, Eisendrath S, Weisner C. Computerized screening for alcohol and drug use among adults seeking outpatient psychiatric services. Psychiatr Serv 2008; 59(4): 441–4. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 103. Miller WR. Motivational interviewing with problem drinkers. Behav Cogn Psychother 1983; 11(2): 147–72. [ Google Scholar ]
- 104. Miller WR, Rose GS. Toward a theory of motivational interviewing. Am Psychol 2009; 64(6): 527–37. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 105. Aharonovich E, Amrhein PC, Bisaga A, Nunes EV, Hasin DS. Cognition, commitment language, and behavioral change among cocaine-dependent patients. Psychol Addict Behav 2008; 22(4): 557–62. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 106. Amrhein PC, Miller WR, Yahne CE, Palmer M, Fulcher L. Client commitment language during motivational interviewing predicts drug use outcomes. J Consult Clin Psychol 2003; 71(5): 862–78. [ DOI ] [ PubMed ] [ Google Scholar ]
- 107. Morgenstern J, Kuerbis A, Amrhein P, Hail L, Lynch K, McKay JR. Motivational interviewing: A pilot test of active ingredients and mechanisms of change. Psychol Addict Behav 2012; 26(4): 859–69. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 108. Moyers TB, Martin T, Houck JM, Christopher PJ, Tonigan JS. From in-session behaviors to drinking outcomes: A causal chain for motivational interviewing. J Consult Clin Psychol 2009; 77(6): 1113–24. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 109. DiIorio C, Resnicow K, Thomas S, et al. Keepin’ it R.E.A.L.!: Program description and results of baseline assessment. Health Educ Behav 2002; 29(1): 104–23. [ DOI ] [ PubMed ] [ Google Scholar ]
- 110. Miller WR, Rollnick S. Motivational interviewing: Preparing people for change. 2nd ed. New York: The Guilford Press; 2002. [ Google Scholar ]
- 111. Bandura A Self efficacy: The excercise of control. New York: W.H. Freeman and Company; 1997. [ Google Scholar ]
- 112. DiIorio C, Maibach E, O’Leary A, Sanderson CA, Celentano D. Measurement of condom use self-efficacy and outcome expectancies in a geographically diverse group of STD patients. AIDS Educ Prev 1997; 9(1): 1–13. [ PubMed ] [ Google Scholar ]
- 113. Fishbein M, Hennessy M, Kamb M, et al. Using intervention theory to model factors influencing behavior change: Project RESPECT. Eval Health Prof 2001; 24(4): 363–84. [ DOI ] [ PubMed ] [ Google Scholar ]
- 114. Celentano DD, Cohn S, Davis RO, Vlahov D. Self-efficacy estimates for drug use practices predict risk reduction among injection drug users. J Urban Health 2002; 79(2): 245–56. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 115. Maisto SA, Clifford PR, Longabaugh R, Beattie M. The relationship between abstinence for one year following pretreatment assessment and alcohol use and other functioning at two years in individuals presenting for alcohol treatment. J Stud Alcohol 2002; 63(4): 397–403. [ DOI ] [ PubMed ] [ Google Scholar ]
- 116. Vielva I, Iraurgi I. Cognitive and behavioural factors as predictors of abstinence following treatment for alcohol dependence. Addiction 2001; 96(2): 297–303. [ DOI ] [ PubMed ] [ Google Scholar ]
- 117. O’Leary A, Jemmott LS, Jemmott JB. Mediation analysis of an effective sexual risk-reduction intervention for women: The importance of self-efficacy. Health Psychol 2008; 27(2 Suppl): S180–4. [ DOI ] [ PubMed ] [ Google Scholar ]
- 118. O’Leary A, Kennedy M, Pappas-DeLuca KA, Nkete M, Beck V, Galavotti C. Association between exposure to an HIV story line in The Bold and the Beautiful and HIV-related stigma in Botswana. AIDS Educ Prev 2007; 19(3): 209–17. [ DOI ] [ PubMed ] [ Google Scholar ]
- 119. Apodaca TR, Longabaugh R. Mechanisms of change in motivational interviewing: A review and preliminary evaluation of the evidence. Addiction 2009; 104(5): 705–15. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 120. DiClemente CC, Corno CM, Graydon MM, Wiprovnick AE, Knoblach DJ. Motivational interviewing, enhancement, and brief interventions over the last decade: A review of reviews of efficacy and effectiveness. Psychol Addict Behav 2017; 31(8): 862–87. [ DOI ] [ PubMed ] [ Google Scholar ]
- 121. Foxcroft DR, Coombes L, Wood S, Allen D, Almeida Santimano NM, Moreira MT. Motivational interviewing for the prevention of alcohol misuse in young adults. Cochrane Database Syst Rev 2016; 7: CD007025. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 122. Moyers TB, Martin T, Manuel JK, Hendrickson SM, Miller WR. Assessing competence in the use of motivational interviewing. J Subst Abuse Treat 2005; 28(1): 19–26. [ DOI ] [ PubMed ] [ Google Scholar ]
- 123. Soderlund LL, Madson MB, Rubak S, Nilsen P. A systematic review of motivational interviewing training for general health care practitioners. Patient Educ Couns 2011; 84(1): 16–26. [ DOI ] [ PubMed ] [ Google Scholar ]
- 124. Forsberg L, Forsberg LG, Lindqvist H, Helgason AR. Clinician acquisition and retention of motivational interviewing skills: A two-and-a-half-year exploratory study. Subst Abuse Treat Prev Policy 2010; 5: 8. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 125. Pirlott AG, Kisbu-Sakarya Y, Defrancesco CA, Elliot DL, Mackinnon DP. Mechanisms of motivational interviewing in health promotion: A Bayesian mediation analysis. Int J Behav Nutr Phys Act 2012; 9(1): 69. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 126. Gaume J, Gmel G, Faouzi M, Daeppen JB. Counselor skill influences outcomes of brief motivational interventions. J Subst Abuse Treat 2009; 37(2): 151–9. [ DOI ] [ PubMed ] [ Google Scholar ]
- 127. Cucciare MA, Ketroser N, Wilbourne P, et al. Teaching motivational interviewing to primary care staff in the Veterans Health Administration. J Gen Intern Med 2012; 27(8): 953–61. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 128. Rollnick S, Miller W, Butler C. Motivational interviewing in health care: Helping people change behavior. New York: The Guildford Press; 2007. [ Google Scholar ]
- 129. Bertholet N, Palfai T, Gaume J, Daeppen JB, Saitz R. Do brief alcohol motivational interventions work like we think they do? Alcohol Clin Exp Res 2014; 38(3): 853–9. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 130. Carroll KM, Kiluk BD. Cognitive behavioral interventions for alcohol and drug use disorders: Through the stage model and back again. Psychol Addict Behav 2017; 31(8): 847–61. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 131. Magill M, Ray LA. Cognitive-behavioral treatment with adult alcohol and illicit drug users: A meta-analysis of randomized controlled trials. J Stud Alcohol Drugs 2009; 70(4): 516–27. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 132. McHugh RK, Hearon BA, Otto MW. Cognitive behavioral therapy for substance use disorders. Psychiatr Clin North Am 2010; 33(3): 511–25. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 133. Wu SS, Schoenfelder E, Hsiao RC. Cognitive behavioral therapy and motivational enhancement therapy. Child Adolesc Psychiatr Clin N Am 2016; 25(4): 629–43. [ DOI ] [ PubMed ] [ Google Scholar ]
- 134. Higgins ST, Petry NM. Contingency management: Incentives for sobriety. Alcohol Res Health 1999; 23(2): 122–7. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 135. Petry NM, Martin B, Cooney JL, Kranzler HR. Give them prizes, and they will come: Contingency management for treatment of alcohol dependence. J Consult Clin Psychol 2000; 68(2): 250–7. [ DOI ] [ PubMed ] [ Google Scholar ]
- 136. Kadden RM. Behavioral and cognitive-behavioral treatments for alcoholism: Research opportunities. Addict Behav 2001; 26(4): 489–507. [ DOI ] [ PubMed ] [ Google Scholar ]
- 137. Project MATCH Research Group. Matching alcoholism treatments to client heterogeneity: Project MATCH posttreatment drinking outcomes. J Stud Alcohol 1997; 58(1): 7–29. [ PubMed ] [ Google Scholar ]
- 138. Project MATCH Research Group. Matching alcoholism treatments to client heterogeneity: Treatment main effects and matching effects on drinking during treatment. J Stud Alcohol 1998; 59(6): 631–9. [ DOI ] [ PubMed ] [ Google Scholar ]
- 139. Project MATCH Research Group. Matching alcoholism treatments to client heterogeneity: Project MATCH three-year drinking outcomes. Alcohol Clin Exp Res 1998; 22(6): 1300–11. [ DOI ] [ PubMed ] [ Google Scholar ]
- 140. Byrne SP, Haber P, Baillie A, Costa DSJ, Fogliati V, Morley K. Systematic reviews of mindfulness and acceptance and commitment therapy for alcohol use disorder: Should we be using third wave therapies? Alcohol Alcohol 2019. [ DOI ] [ PubMed ] [ Google Scholar ]
- 141. McCrady BS, Wilson AD, Munoz RE, Fink BC, Fokas K, Borders A. Alcohol-focused behavioral couple therapy. Fam Process 2016; 55(3): 443–59. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 142. Powers MB, Vedel E, Emmelkamp PM. Behavioral couples therapy (BCT) for alcohol and drug use disorders: A meta-analysis. Clin Psychol Rev 2008; 28(6): 952–62. [ DOI ] [ PubMed ] [ Google Scholar ]
- 143. O’Farrell TJ, Clements K. Review of outcome research on marital and family therapy in treatment for alcoholism. J Marital Fam Ther 2012; 38(1): 122–44. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 144. Lenaerts E, Mathei C, Matthys F, et al. Continuing care for patients with alcohol use disorders: A systematic review. Drug Alcohol Depend 2014; 135: 9–21. [ DOI ] [ PubMed ] [ Google Scholar ]
- 145. Carroll KM. Behavioral therapies for co-occurring substance use and mood disorders. Biol Psychiatry 2004; 56(10): 778–84. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 146. Kelly TM, Daley DC, Douaihy AB. Treatment of substance abusing patients with comorbid psychiatric disorders. Addict Behav 2012; 37(1): 11–24. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 147. Martino S, Carroll KM, O’Malley SS, Rounsaville BJ. Motivational interviewing with psychiatrically ill substance abusing patients. Am J Addict 2000; 9(1): 88–91. [ DOI ] [ PubMed ] [ Google Scholar ]
- 148. Weiss RD, Griffin ML, Greenfield SF, et al. Group therapy for patients with bipolar disorder and substance dependence: Results of a pilot study. J Clin Psychiatry 2000; 61(5): 361–7. [ DOI ] [ PubMed ] [ Google Scholar ]
- 149. Brown RA, Evans DM, Miller IW, Burgess ES, Mueller TI. Cognitive-behavioral treatment for depression in alcoholism. J Consult Clin Psychol 1997; 65(5): 715–26. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 150. Monti PM, Abrams DB, Binkoff JA, et al. Communication skills training, communication skills training with family and cognitive behavioral mood management training for alcoholics. J Stud Alcohol 1990; 51(3): 263–70. [ DOI ] [ PubMed ] [ Google Scholar ]
- 151. Klimas J, Fairgrieve C, Tobin H, et al. Psychosocial interventions to reduce alcohol consumption in concurrent problem alcohol and illicit drug users. Cochrane Database Syst Rev 2018; 12: CD009269. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 152. Bayard M, McIntyre J, Hill KR, Woodside J, Jr. Alcohol withdrawal syndrome. Am Fam Physician 2004; 69(6): 1443–50. [ PubMed ] [ Google Scholar ]
- 153. Mayo-Smith MF. Pharmacological management of alcohol withdrawal. A meta-analysis and evidence-based practice guideline. American Society of Addiction Medicine Working Group on Pharmacological Management of Alcohol Withdrawal. JAMA 1997; 278(2): 144–51. [ DOI ] [ PubMed ] [ Google Scholar ]
- 154. Ozdemir V, Bremner KE, Naranjo CA. Treatment of alcohol withdrawal syndrome. Ann Med 1994; 26(2): 101–5. [ DOI ] [ PubMed ] [ Google Scholar ]
- 155. Sachdeva A, Choudhary M, Chandra M. Alcohol withdrawal syndrome: Benzodiazepines and beyond. J Clin Diagn Res 2015; 9(9): VE01–7. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 156. Chhatlani A, Farheen SA, Manikkara G, Setty MJ, DeOreo E, Tampi RR. Anticonvulsants as monotherapy or adjuncts to treat alcohol withdrawal: A systematic review. Ann Clin Psychiatry 2018; 30(4): 312–25. [ PubMed ] [ Google Scholar ]
- 157. National Institute on Alcohol Abuse and Alcoholism. Medications development program. November 2017. https://www.niaaa.nih.gov/research/major-initiatives/medications-development-program (accessed Dec 12 2017).
- 158. Paille F, Martini H. Nalmefene: A new approach to the treatment of alcohol dependence. Subst Abuse Rehabil 2014; 5: 87–94. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 159. Fuller RK, Branchey L, Brightwell DR, et al. Disulfiram treatment of alcoholism: A Veterans Administration cooperative study. JAMA 1986; 256(11): 1449–55. [ PubMed ] [ Google Scholar ]
- 160. Krampe H, Stawicki S, Wagner T, et al. Follow-up of 180 alcoholic patients for up to 7 years after outpatient treatment: Impact of alcohol deterrents on outcome. Alcohol Clin Exp Res 2006; 30(1): 86–95. [ DOI ] [ PubMed ] [ Google Scholar ]
- 161. Hughes JC, Cook CC. The efficacy of disulfiram: A review of outcome studies. Addiction 1997; 92(4): 381–95. [ PubMed ] [ Google Scholar ]
- 162. Garbutt JC, West SL, Carey TS, Lohr KN, Crews FT. Pharmacological treatment of alcohol dependence: A review of the evidence. JAMA 1999; 281(14): 1318–25. [ DOI ] [ PubMed ] [ Google Scholar ]
- 163. Skinner MD, Lahmek P, Pham H, Aubin HJ. Disulfiram efficacy in the treatment of alcohol dependence: A meta-analysis. PLoS One 2014; 9(2): e87366. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 164. Soyka M, Kranzler HR, Hesselbrock V, et al. Guidelines for biological treatment of substance use and related disorders, part 1: Alcoholism, first revision. World J Biol Psychiatry 2017; 18(2): 86–119. [ DOI ] [ PubMed ] [ Google Scholar ]
- 165. Brewer C, Streel E, Skinner M. Supervised disulfiram’s superior effectiveness in alcoholism treatment: Ethical, methodological, and psychological aspects. Alcohol Alcohol 2017; 52(2): 213–9. [ DOI ] [ PubMed ] [ Google Scholar ]
- 166. Volpicelli JR, Alterman AI, Hayashida M, O’Brien CP. Naltrexone in the treatment of alcohol dependence. Arch Gen Psychiatry 1992; 49(11): 876–80. [ DOI ] [ PubMed ] [ Google Scholar ]
- 167. O’Malley SS, Jaffe AJ, Chang G, Schottenfeld RS, Meyer RE, Rounsaville B. Naltrexone and coping skills therapy for alcohol dependence: A controlled study. Arch Gen Psychiatry 1992; 49(11): 881–7. [ DOI ] [ PubMed ] [ Google Scholar ]
- 168. Mark TL, Kassed CA, Vandivort-Warren R, Levit KR, Kranzler HR. Alcohol and opioid dependence medications: Prescription trends, overall and by physician specialty. Drug Alcohol Depend 2009; 99(1–3): 345–9. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 169. Mark TL, Kranzler HR, Song X. Understanding US addiction physicians’ low rate of naltrexone prescription. Drug Alcohol Depend 2003; 71(3): 219–28. [ DOI ] [ PubMed ] [ Google Scholar ]
- 170. Ponce Martinez C, Vakkalanka P, Ait-Daoud N. Pharmacotherapy for alcohol use disorders: Physicians’ perceptions and practices. Front Psychiatry 2016; 7: 182. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 171. Harris AH, Ellerbe L, Reeder RN, et al. Pharmacotherapy for alcohol dependence: Perceived treatment barriers and action strategies among Veterans Health Administration service providers. Psychol Serv 2013; 10(4): 410–9. [ DOI ] [ PubMed ] [ Google Scholar ]
- 172. Garbutt JC, Kranzler HR, O’Malley SS, et al. Efficacy and tolerability of long-acting injectable naltrexone for alcohol dependence: A randomized controlled trial. JAMA 2005; 293(13): 1617–25. [ DOI ] [ PubMed ] [ Google Scholar ]
- 173. Kranzler HR, Wesson DR, Billot L, DrugAbuse Sciences Naltrexone Depot Study Group. Naltrexone depot for treatment of alcohol dependence: A multicenter, randomized, placebo-controlled clinical trial. Alcohol Clin Exp Res 2004; 28(7): 1051–9. [ DOI ] [ PubMed ] [ Google Scholar ]
- 174. Edelman EJ, Moore BA, Holt SR, et al. Efficacy of extended-release naltrexone on HIV-related and drinking outcomes among HIV-positive patients: A randomized-controlled trial. AIDS Behav 2019; 23(1): 211–21. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 175. Springer SA, Di Paola A, Azar MM, Barbour R, Krishnan A, Altice FL. Extended-release naltrexone reduces alcohol consumption among released prisoners with HIV disease as they transition to the community. Drug Alcohol Depend 2017; 174: 158–70. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 176. Crits-Christoph P, Lundy C, Stringer M, Gallop R, Gastfriend DR. Extended-release naltrexone for alcohol and opioid problems in Missouri parolees and probationers. J Subst Abuse Treat 2015; 56: 54–60. [ DOI ] [ PubMed ] [ Google Scholar ]
- 177. Kalk NJ, Lingford-Hughes AR. The clinical pharmacology of acamprosate. Br J Clin Pharmacol 2014; 77(2): 315–23. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 178. Palpacuer C, Laviolle B, Boussageon R, Reymann JM, Bellissant E, Naudet F. Risks and benefits of nalmefene in the treatment of adult alcohol dependence: A systematic literature review and meta-analysis of published and unpublished double-blind randomized controlled trials. PLoS Med 2015; 12(12): e1001924. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 179. Soyka M, Muller CA. Pharmacotherapy of alcoholism: An update on approved and off-label medications. Expert Opin Pharmacother 2017; 18(12): 1187–99. [ DOI ] [ PubMed ] [ Google Scholar ]
- 180. Litten RZ, Wilford BB, Falk DE, Ryan ML, Fertig JB. Potential medications for the treatment of alcohol use disorder: An evaluation of clinical efficacy and safety. Subst Abus 2016; 37(2): 286–98. [ DOI ] [ PubMed ] [ Google Scholar ]
- 181. Blodgett JC, Del Re AC, Maisel NC, Finney JW. A meta-analysis of topiramate’s effects for individuals with alcohol use disorders. Alcohol Clin Exp Res 2014; 38(6): 1481–8. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 182. Pierce M, Sutterland A, Beraha EM, Morley K, van den Brink W. Efficacy, tolerability, and safety of low-dose and high-dose baclofen in the treatment of alcohol dependence: A systematic review and meta-analysis. Eur Neuropsychopharmacol 2018; 28(7): 795–806. [ DOI ] [ PubMed ] [ Google Scholar ]
- 183. Kranzler HR, Knapp C, Ciraulo D. Pharmacotherapy of alcoholism In: Kranzler HR, Ciraulo D, Zindel L, eds. Clinical Manual of Addiction Psychopharmacology. 2nd ed. Washington, DC: American Psychiatric Press; 2014: 1–69. [ Google Scholar ]
- 184. Nunes EV, Levin FR. Treatment of depression in patients with alcohol or other drug dependence: A meta-analysis. JAMA 2004; 291(15): 1887–96. [ DOI ] [ PubMed ] [ Google Scholar ]
- 185. Pettinati HM, Oslin DW, Kampman KM, et al. A double-blind, placebo-controlled trial combining sertraline and naltrexone for treating co-occurring depression and alcohol dependence. Am J Psychiatry 2010; 167(6): 668–75. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 186. Horgan CM, Reif S, Hodgkin D, Garnick DW, Merrick EL. Availability of addiction medications in private health plans. J Subst Abuse Treat 2008; 34(2): 147–56. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 187. Mark TL, Dirani R, Slade E, Russo PA. Access to new medications to treat schizophrenia. J Behav Health Serv Res 2002; 29(1): 15–29. [ DOI ] [ PubMed ] [ Google Scholar ]
- 188. Ducharme LJ, Knudsen HK, Roman PM. Trends in the adoption of medications for alcohol dependence. J Clin Psychopharmacol 2006; 26 Suppl 1: S13–9. [ DOI ] [ PubMed ] [ Google Scholar ]
- 189. Knudsen HK, Roman PM. Service delivery and pharmacotherapy for alcohol use disorder in the era of health reform: Data from a national sample of treatment organizations. Subst Abus 2016; 37(1): 230–7. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 190. Knudsen HK, Roman PM. The transition to medication adoption in publicly funded substance use disorder treatment programs: Organizational structure, culture, and resources. J Stud Alcohol Drugs 2014; 75(3): 476–85. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 191. Anton RF, Litten RZ, Falk DE, et al. The Alcohol Clinical Trials Initiative (ACTIVE): Purpose and goals for assessing important and salient issues for medications development in alcohol use disorders. Neuropsychopharmacology 2012; 37(2): 402–11. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 192. Witkiewitz K, Finney JW, Harris AH, Kivlahan DR, Kranzler HR. Recommendations for the design and analysis of treatment trials for alcohol use disorders. Alcohol Clin Exp Res 2015; 39(9): 1557–70. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 193. DeMartini KS, Devine EG, DiClemente CC, Martin DJ, Ray LA, O’Malley SS. Predictors of pretreatment commitment to abstinence: Results from the COMBINE study. J Stud Alcohol Drugs 2014; 75(3): 438–46. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 194. Witkiewitz K, Wilson AD, Pearson MR, et al. Temporal stability of heavy drinking days and drinking reductions among heavy drinkers in the COMBINE study. Alcohol Clin Exp Res 2017; 41(5): 1054–62. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 195. Maisto SA, Hallgren KA, Roos CR, Witkiewitz K. Course of remission from and relapse to heavy drinking following outpatient treatment of alcohol use disorder. Drug Alcohol Depend 2018; 187: 319–26. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 196. Wilson AD, Bravo AJ, Pearson MR, Witkiewitz K. Finding success in failure: Using latent profile analysis to examine heterogeneity in psychosocial functioning among heavy drinkers following treatment. Addiction 2016; 111(12): 2145–54. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 197. Mann K, Aubin HJ, Charlet K, Witkiewitz K. Can reduced drinking be a viable goal for alcohol dependent patients? World Psychiatry 2017; 16(3): 325–6. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 198. Mann K, Aubin HJ, Witkiewitz K. Reduced drinking in alcohol dependence treatment, what is the evidence? Eur Addict Res 2017; 23(5): 219–30. [ DOI ] [ PubMed ] [ Google Scholar ]
- 199. Probst C, Manthey J, Martinez A, Rehm J. Alcohol use disorder severity and reported reasons not to seek treatment: A cross-sectional study in European primary care practices. Subst Abuse Treat Prev Policy 2015; 10: 32. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 200. US Food and Drug Administration. Alcoholism: Developing drugs for treatment Guidance for industry. Silver Spring, MD: US Department of Health and Human Services, Food and Drug Administration, Center for Drug Evaluation and Research, 2015. [ Google Scholar ]
- 201. World Health Organization. International guide for monitoring alcohol consumption and related harm. Geneva: Department of Mental Health and Substance Dependence, Noncommunicable Diseases and Mental Health Cluster, World Health Organization, 2000. [ Google Scholar ]
- 202. European Medicines Agency. Guideline on the development of medicinal products for the treatment of alcohol dependence. London: European Medicines Agency, 2010. [ Google Scholar ]
- 203. Litten RZ, Falk DE, O’Malley SS, Witkiewitz KA, Mann KF, Anton RF. Letter to editor in response to Johnson’s commentary (2017) on the Witkiewitz and colleagues (2017) article. Alcohol Clin Exp Res 2017; 41(7): 1381–2. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 204. Witkiewitz K, Hallgren KA, Kranzler HR, et al. Clinical validation of reduced alcohol consumption after treatment for alcohol dependence using the World Health Organization risk drinking levels. Alcohol Clin Exp Res 2017; 41(1): 179–86. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 205. Falk DE, O’Malley SS, Witkiewitz K, et al. Evaluation of drinking risk levels as outcomes in alcohol pharmacotherapy trials: A secondary analysis of 3 randomized clinical trials. JAMA Psychiatry 2019. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 206. Anton RF, O’Malley SS, Ciraulo DA, et al. Combined pharmacotherapies and behavioral interventions for alcohol dependence: The COMBINE study: A randomized controlled trial. JAMA 2006; 295(17): 2003–17. [ DOI ] [ PubMed ] [ Google Scholar ]
- 207. Miller WR, Tonigan JS, Longabaugh R. The drinker inventory of consequences (DrInC): An instrument for assessing adverse consequences of alcohol abuse. Rockville: National Institute on Alcohol Abuse and Alcoholism, 1995. [ Google Scholar ]
- 208. Ware J, Kosinski M, Keller SD. A 12-item short-form health survey: Construction of scales and preliminary tests of reliability and validity. Med Care 1996; 34(3): 220–33. [ DOI ] [ PubMed ] [ Google Scholar ]
- 209. Witkiewitz K, Pearson MR, Hallgren KA, et al. Who achieves low risk drinking during alcohol treatment? An analysis of patients in three alcohol clinical trials. Addiction 2017; 112(12): 2112–21. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 210. Knox J, Wall M, Witkiewitz K, et al. Reduction in nonabstinent WHO drinking risk levels and change in risk for liver disease and positive AUDIT-C scores: Prospective 3-year follow-up results in the U.S. general population. Alcohol Clin Exp Res 2018; 42(11): 2256–65. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 211. Knox J, Wall M, Witkiewitz K, et al. Reduction in non-abstinent WHO drinking risk levels and depression/anxiety disorders: 3-year follow-up results in the US general population. Drug Alcohol Depend 2019; 197: 228–35. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 212. Knox J, Wall M, Witkiewitz K, et al. Reduction in non-abstinent WHO drinking risk levels and drug use disorders: 3-year follow-up results in the US general population. Drug Alcohol Depend (In press). [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 213. Stockings E, Farrell M. Drinking-reduction goals offer potential to widen the options for measuring and treating alcohol dependence. Lancet Psychiatry 2017; 4(6): 430–1. [ DOI ] [ PubMed ] [ Google Scholar ]
- 214. Meredith SE, Alessi SM, Petry NM. Smartphone applications to reduce alcohol consumption and help patients with alcohol use disorder: A state-of-the-art review. Adv Health Care Technol 2015; 1: 47–54. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 215. Sugarman DE, Campbell ANC, Iles BR, Greenfield SF. Technology-based interventions for substance use and comorbid disorders: An examination of the emerging literature. Harv Rev Psychiatry 2017; 25(3): 123–34. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 216. Tofighi B, Abrantes A, Stein MD. The role of technology-based interventions for substance use disorders in primary care: A review of the literature. Med Clin North Am 2018; 102(4): 715–31. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 217. Kaner EF, Beyer FR, Garnett C, et al. Personalised digital interventions for reducing hazardous and harmful alcohol consumption in community-dwelling populations. Cochrane Database Syst Rev 2017; 9: CD011479. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 218. Oosterveen E, Tzelepis F, Ashton L, Hutchesson MJ. A systematic review of eHealth behavioral interventions targeting smoking, nutrition, alcohol, physical activity and/or obesity for young adults. Prev Med 2017; 99: 197–206. [ DOI ] [ PubMed ] [ Google Scholar ]
- 219. Nesvag S, McKay JR. Feasibility and effects of digital interventions to support people in recovery from substance use disorders: Systematic review. J Med Internet Res 2018; 20(8): e255. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 220. Naslund JA, Aschbrenner KA, Araya R, et al. Digital technology for treating and preventing mental disorders in low-income and middle-income countries: A narrative review of the literature. Lancet Psychiatry 2017; 4(6): 486–500. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 221. Chih MY, Patton T, McTavish FM, et al. Predictive modeling of addiction lapses in a mobile health application. J Subst Abuse Treat 2014; 46(1): 29–35. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 222. Dennis ML, Scott CK, Funk RR, Nicholson L. A pilot study to examine the feasibility and potential effectiveness of using smartphones to provide recovery support for adolescents. Subst Abus 2015; 36(4): 486–92. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 223. McTavish FM, Chih MY, Shah D, Gustafson DH. How patients recovering from alcoholism use a smartphone intervention. J Dual Diagn 2012; 8(4): 294–304. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 224. Gustafson DH, McTavish FM, Chih MY, et al. A smartphone application to support recovery from alcoholism: A randomized clinical trial. JAMA Psychiatry 2014; 71(5): 566–72. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 225. Dulin PL, Gonzalez VM, King DK, Giroux D, Bacon S. Smartphone-based, self-administered intervention system for alcohol use disorders: Theory and empirical evidence basis. Alcohol Treat Q 2013; 31(3). [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 226. Gonzalez VM, Dulin PL. Comparison of a smartphone app for alcohol use disorders with an Internet-based intervention plus bibliotherapy: A pilot study. J Consult Clin Psychol 2015; 83(2): 335–45. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 227. Aharonovich E, Stohl M, Cannizzaro D, Hasin D. HealthCall delivered via smartphone to reduce co-occurring drug and alcohol use in HIV-infected adults: A randomized pilot trial. J Subst Abuse Treat 2017; 83: 15–26. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 228. Hasin DS, Aharonovich E, Greenstein E. HealthCall for the smartphone: Technology enhancement of brief intervention in HIV alcohol dependent patients. Addict Sci Clin Pract 2014; 9: 5. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 229. Hasin DS, Aharonovich E, O’Leary A, et al. Reducing heavy drinking in HIV primary care: A randomized trial of brief intervention, with and without technological enhancement. Addiction 2013; 108(7): 1230–40. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 230. Deady M, Mills KL, Teesson M, Kay-Lambkin F. An online intervention for co-occurring depression and problematic alcohol use in young people: Primary outcomes from a randomized controlled trial. J Med Internet Res 2016; 18(3): e71. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 231. Muroff J, Robinson W, Chassler D, et al. Use of a smartphone recovery tool for Latinos with co-occurring alcohol and other drug disorders and mental disorders. J Dual Diagn 2017; 13(4): 280–90. [ DOI ] [ PubMed ] [ Google Scholar ]
- 232. Kazemi DM, Borsari B, Levine MJ, Li S, Lamberson KA, Matta LA. A systematic review of the mHealth interventions to prevent alcohol and substance abuse. J Health Commun 2017; 22(5): 413–32. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 233. Elder RW, Lawrence B, Ferguson A, et al. The effectiveness of tax policy interventions for reducing excessive alcohol consumption and related harms. Am J Prev Med 2010; 38(2): 217–29. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 234. Wagenaar AC, Tobler AL, Komro KA. Effects of alcohol tax and price policies on morbidity and mortality: A systematic review. Am J Public Health 2010; 100(11): 2270–8. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 235. Warren KR. A review of the history of attitudes toward drinking in pregnancy. Alcohol Clin Exp Res 2015; 39(7): 1110–7. [ DOI ] [ PubMed ] [ Google Scholar ]
- 236. Hasin D, Shmulewitz D. Time trends in U.S. drinking patterns and problems. Annual Meeting of the Research Society on Alcoholism; 2018 June; San Diego, CA; 2018. [ Google Scholar ]
- 237. Casswell S, Thamarangsi T. Reducing harm from alcohol: Call to action. Lancet 2009; 373(9682): 2247–57. [ DOI ] [ PubMed ] [ Google Scholar ]
- 238. Moodie R, Stuckler D, Monteiro C, et al. Profits and pandemics: Prevention of harmful effects of tobacco, alcohol, and ultra-processed food and drink industries. Lancet 2013; 381(9867): 670–9. [ DOI ] [ PubMed ] [ Google Scholar ]
- 239. Pettigrew S, Hafekost C, Jongenelis M, Pierce H, Chikritzhs T, Stafford J. Behind closed doors: The priorities of the alcohol industry as communicated in a trade magazine. Front Public Health 2018; 6: 217. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 240. Mann K, Roos CR, Hoffmann S, et al. Precision medicine in alcohol dependence: A controlled trial testing pharmacotherapy response among reward and relief drinking phenotypes. Neuropsychopharmacology 2018; 43(4): 891–9. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 241. Johnson BA, Ait-Daoud N, Seneviratne C, et al. Pharmacogenetic approach at the serotonin transporter gene as a method of reducing the severity of alcohol drinking. Am J Psychiatry 2011; 168(3): 265–75. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 242. Kranzler HR, Covault J, Feinn R, et al. Topiramate treatment for heavy drinkers: Moderation by a GRIK1 polymorphism. Am J Psychiatry 2014; 171(4): 445–52. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 243. Grucza RA, Sher KJ, Kerr WC, et al. Trends in adult alcohol use and binge drinking in the early 21st-century United States: A meta-analysis of 6 national survey series. Alcohol Clin Exp Res 2018; 42(10): 1939–50. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 244. Rosner S, Hackl-Herrwerth A, Leucht S, Lehert P, Vecchi S, Soyka M. Acamprosate for alcohol dependence. Cochrane Database Syst Rev 2010; (9): CD004332. [ DOI ] [ PubMed ] [ Google Scholar ]
- 245. Kranzler HR, Feinn R, Morris P, Hartwell EE. A meta-analysis of the efficacy of gabapentin for treating alcohol use disorder. Addiction (Under review). [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 246. Knapp CM, Ciraulo DA, Sarid-Segal O, et al. Zonisamide, topiramate, and levetiracetam: Efficacy and neuropsychological effects in alcohol use disorders. J Clin Psychopharmacol 2015; 35(1): 34–42. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 247. Froehlich JC, Fischer SM, Dilley JE, et al. Combining varenicline (Chantix) with naltrexone decreases alcohol drinking more effectively than does either drug alone in a rodent model of alcoholism. Alcohol Clin Exp Res 2016; 40(9): 1961–70. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 248. Erwin BL, Slaton RM. Varenicline in the treatment of alcohol use disorders. Ann Pharmacother 2014; 48(11): 1445–55. [ DOI ] [ PubMed ] [ Google Scholar ]
- 249. Lynch WJ, Bond C, Breslin FJ, Johnson BA. Severity of drinking as a predictor of efficacy of the combination of ondansetron and topiramate in rat models of ethanol consumption and relapse. Psychopharmacology (Berl) 2011; 217(1): 3–12. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 250. Moore CF, Lycas MD, Bond CW, Johnson BA, Lynch WJ. Acute and chronic administration of a low-dose combination of topiramate and ondansetron reduces ethanol’s reinforcing effects in male alcohol preferring (P) rats. Exp Clin Psychopharmacol 2014; 22(1): 35–42. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 251. Johnson BA, Roache JD, Javors MA, et al. Ondansetron for reduction of drinking among biologically predisposed alcoholic patients: A randomized controlled trial. JAMA 2000; 284(8): 963–71. [ DOI ] [ PubMed ] [ Google Scholar ]
- 252. Kranzler HR, Pierucci-Lagha A, Feinn R, Hernandez-Avila C. Effects of ondansetron in early- versus late-onset alcoholics: A prospective, open-label study. Alcohol Clin Exp Res 2003; 27(7): 1150–5. [ DOI ] [ PubMed ] [ Google Scholar ]
- 253. Kishi T, Sevy S, Chekuri R, Correll CU. Antipsychotics for primary alcohol dependence: A systematic review and meta-analysis of placebo-controlled trials. J Clin Psychiatry 2013; 74(7): e642–54. [ DOI ] [ PubMed ] [ Google Scholar ]
- 254. Guardia J, Roncero C, Galan J, Gonzalvo B, Burguete T, Casas M. A double-blind, placebo-controlled, randomized pilot study comparing quetiapine with placebo, associated to naltrexone, in the treatment of alcohol-dependent patients. Addict Behav 2011; 36(3): 265–9. [ DOI ] [ PubMed ] [ Google Scholar ]
- 255. Fell JC, Voas RB. The effectiveness of a 0.05 blood alcohol concentration (BAC) limit for driving in the United States. Addiction 2014; 109(6): 869–74. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- View on publisher site
- PDF (736.5 KB)
- Collections
Similar articles
Cited by other articles, links to ncbi databases.
- Download .nbib .nbib
- Format: AMA APA MLA NLM
Add to Collections
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 02 November 2024
The impact of alcohol consumption on the quality of life of college students: a study from three Slovak universities
- Dávid Líška ORCID: orcid.org/0000-0002-5700-1341 1 ,
- Erika Liptáková 2 ,
- Miroslava Barcalová 3 &
- Ľubomír Skladaný 4
Humanities and Social Sciences Communications volume 11 , Article number: 1456 ( 2024 ) Cite this article
346 Accesses
Metrics details
- Social policy
Alcohol consumption can influence an individual's quality of life, with the impact varying based on several factors such as the amount of alcohol consumed, frequency of consumption, individual tolerance, and overall health. Slovakia is among the countries with the highest incidence of liver cirrhosis in the world, with alcohol representing a significant risk factor. Therefore, it is important to identify at-risk groups and the potential impact of various factors. The primary objective of this study is to examine the relationship between alcohol consumption and quality of life among college students in the Slovak Universities. A cross-sectional study was conducted in December 2021 and January 2022. The study included college students with an average age of 22.3 years. Participants were surveyed about their alcohol consumption and quality of life using the standardized Alcohol Use Disorders Identification Test (AUDIT) and EuroQol-5D (EQ-5D) questionnaires. These questionnaires were distributed through online school systems. In the study, 88.7% of the students reported drinking alcohol. A low AUDIT score was recorded for 67.1% of the total participants (2573 students). A medium score was found in 23.3% of the participants (893 students). High scores were identified in 2.4% of the participants (92 students), and very high scores were found in 2.2% of the total participants (86 students). Mild pain was reported in 33.8% of cases, while moderate pain was reported in 5.2% of cases. Mild depression and anxiety were reported in 31.1% of the cases, and moderate depression and anxiety were reported in 13.5% of the cases. There is a statistically significant relationship between AUDIT and EuroQOL variables ( p < 0.001). This suggests that the association between alcohol use (measured by AUDIT) and health-related quality of life (measured by EuroQOL) is unlikely to be due to chance. Higher alcohol consumption was associated with a poorer quality of life in Slovak college students. Our results suggest a meaningful connection between alcohol consumption behaviors and overall quality of life, highlighting the potential impact of alcohol use on health outcomes. Further research is warranted to explore the nature and causality of this relationship, which could inform interventions aimed at improving health-related quality of life through alcohol use reduction strategies. The association between higher alcohol consumption and poorer quality of life in Slovak college students raises important questions about causality and the complex interplay between alcohol consumption and one’s overall well-being. The significant relationship between higher alcohol consumption and poorer quality of life suggests the need for targeted public health interventions aimed at reducing alcohol consumption among college students. Programs focusing on awareness and education about the negative impacts of excessive drinking could be implemented to promote healthier lifestyles.
Similar content being viewed by others

Burden of alcohol and other substance use and correlates among undergraduate students at Busitema University in rural Eastern Uganda after COVID-19 lockdown

Alcohol consumption and its associated factors among adolescents in a rural community in central Thailand: a mixed-methods study

Self-management with alcohol over lifespan: psychological mechanisms, neurobiological underpinnings, and risk assessment
Introduction.
Alcohol consumption, including high-risk drinking, is associated with stressful life events, as it often exacerbates emotional distress and can lead to a vicious cycle of increased stress and greater alcohol use (Dich and Doan 2019 ; Hoyland and Latendresse 2018 ; Keyes et al. 2012 ; Rehm et al. 2009 ; Stautz et al. 2016 ). This pattern can negatively impact various aspects of an individual's life, including mental health, relationships, and academic or work performance. Stressful life events may trigger increased alcohol consumption as a coping mechanism, but this, in turn, can heighten stress and anxiety levels, creating a detrimental feedback loop (Becker 2017 ; Dawson et al. 2005 ; Keyes et al. 2012 ). Alcohol consumption is an important public health problem that transcends geographical boundaries, affecting individuals and communities throughout the world, with far-reaching consequences on physical health, mental well-being, social dynamics, and economic stability (GBD 2016 Alcohol Collaborators 2018 ). Alcohol consumption is one of the major risk factors for disability and premature mortality, contributing significantly to a wide range of health problems, including, but not limited to, cardiovascular diseases, liver cirrhosis, certain cancers, mental health disorders, and accidents, which pose a substantial burden on health systems and society as a whole (Rehm and Shield 2014 ; Sohi et al. 2021 ; Xi et al. 2017 ). Alcohol consumption is an important risk factor for several chronic diseases. It plays a pivotal role in exacerbating these health issues, highlighting the need for comprehensive public health strategies to address the detrimental impact of alcohol on long-term well-being. (Barbería-Latasa et al. 2022, 2022 ; McKay and Hiller-Sturmhöfel 2011 ; Shield et al. 2013 ; Zhou et al. 2016 ). Alcohol is the most widespread drug addiction in all geographical regions and in all sections of the population, spanning age, sex, socioeconomic status, and cultural background. Its ubiquity highlights the need for a multifaceted approach to addiction prevention and treatment that addresses the complex factors that contribute to alcohol dependence and abuse in diverse communities and settings (Matošić et al. 2016 ; Volpicelli 2001 ; Wackernah et al. 2014 ; Wang et al. 2020 ).
Slovakia is one of the countries with the highest incidence of liver cirrhosis in the world (Sepanlou et al. 2020 ). High prevalence not only poses a major public health concern but also places a significant burden on the healthcare system. Understanding the underlying reasons for this trend is crucial, as liver cirrhosis can lead to severe health complications and increased mortality rates. This is a troubling health statistic that underscores the urgent need for public health initiatives aimed at preventing alcohol abuse, improving access to healthcare, and raising awareness of the risks associated with excessive alcohol consumption within the population. Among young people, college students have higher alcohol consumption than nonstudents (Quinn and Fromme 2011 ; Slutske, 2005 ). Alcohol consumption is a significant issue among college students, with excessive drinking prevalent in many educational institutions (Casper et al. 2006 ; Chow et al. 2021 ; Freire et al. 2020 ). This practice has significant implications for the quality of life of students. The prevalence of alcohol consumption in educational settings has been widely documented, with various studies indicating high levels of binge drinking and alcohol-related problems among students. The transition to college often coincides with a period of increased autonomy and exposure to social environments where alcohol consumption is prevalent (Hayatbakhsh et al. 2011 ; Lee et al. 2008 ; Ranker and Lipson 2022 ). This phase of life, marked by significant psychological and social changes, can make students particularly vulnerable to developing unhealthy drinking patterns. The interplay between stress, peer pressure, and the desire for social acceptance frequently contributes to the initiation and escalation of alcohol use among students. Alcohol use disorder (AUD) among students is characterized by the inability to control drinking despite adverse consequences (Benjet et al. 2022 ).
These consequences can be academic, such as declining grades and increased dropout rates; social, including impaired relationships and antisocial behavior; and health-related, encompassing both acute and chronic medical issues. The interplay between alcohol consumption and quality of life encompasses various dimensions, including physical health, mental well-being, academic performance, and social relationships. This issue poses immediate risks to student health and safety but can also have long-term consequences, affecting academic performance, mental well-being, and future career prospects.
Therefore, the objective of this study is to determine the level of alcohol consumption and its association with the quality of life among college students.
Materials and methodology
During the third wave of the COVID-19 pandemic and the concurrent lockdown, a cross-sectional study was conducted from December 2021 to January 2022. Three universities participated in the study. The main outcomes were the AUDIT score and quality of life according to EQ-5D. After obtaining informed consent, students completed the structured questionnaires AUDIT and EQ-5D. The questionnaires were distributed through online school systems, leveraging the convenience and accessibility of digital platforms to reach a wider and more diverse range of respondents, ensuring a representative sample for our research. This approach allowed efficient data collection and minimized the need for physical contact during the ongoing pandemic. The study included participants who were college students at a three Slovak university and were 18 years of age or older. The exclusion criteria were as follows: students with visual impairments, students who were not enrolled in a Slovak university, students under the age of 18, students with cognitive impairments that would interfere with their ability to complete the study tasks, and students who were not proficient in the Slovak language.
The Alcohol Use Disorders Identification Test (AUDIT) questionnaire was employed as a robust and validated tool to assess alcohol consumption patterns among the study participants. This questionnaire consists of a series of questions designed to evaluate various aspects of alcohol use, including frequency and quantity of consumption, as well as potential alcohol-related problems or dependence symptoms (Kuitunen-Paul and Roerecke 2018 ; Lundin et al. 2015 ; Verhoog et al. 2020 ). AUDIT can also be used in the younger population (Liskola et al. 2018 ). The Slovak standardized version was used. AUDIT is used as one of the tools to detect alcohol consumption and related risk behaviors in primary care settings (Ballester et al. 2021 ). The AUDIT score is divided into low (scores between 0 and 7), medium (scores between 8 and 15), high (scores between 16 and 19), and very high (scores between 20 and above). The questionnaire contained information on the risk level of drinking (items: frequency of drinking, amount and frequency of excessive drinking), symptoms of addiction (items: impaired control of drinking, increased importance of drinking and early drinking), and harmful alcohol use (items: guilt after drinking, alcohol-related injuries and other drinking related items). A pilot test was conducted before the start of the study to determine the feasibility of submitting a questionnaire.
EuroQol-5D (EQ-5D)
The EuroQol-5D questionnaire is used to measure quality of life. EQ-5D is a valid form of quality of life measurement (Ragusa et al. 2018 ). It includes five aspects: mobility, self-care, daily activities, pain, discomfort, anxiety, and depression, and a visual analog scale that assesses perceived subjective health on a scale from 0 to 100. In other questions, it is possible to choose the answer on a scale from 1 - no problems to 5 - maximum problems. Each health condition defines one “utility” score which can be transformed using a score. A pilot test was conducted before the start of the study to determine the feasibility of submitting a questionnaire.
Statistical analysis
The results were collected in an Excel spread sheet and subsequently subjected to statistical analysis using software IBM SPSS Statistics 19. Unpaired t-test was used to assess the difference between group of men and group of women. Analysis of contingency tables were used to calculate the percentage of students to compare outputs from AUDIT and EuroQol questionnaires. In order to test the potential dependence between AUDIT scores and EuroQol scores, new ordinal variables were first created. Using data from this table, chi-squared test was calculated. The significance level was established at α = 0.05.
Participants
The study involved 4044 students from three Slovak universities. Matej Bel University, Banská Bystrica (n-1066, 26.4%), Technical University of Košice (n-2769, 68.5%) and the Slovak Medical Universities, Faculty of HealthCare in Banská Bystrica (n-209, 5.2%). The characteristics of the sample can be seen in Table 1 . All participants willingly agreed to participate in the study and prior to their involvement.
A total of 4044 students participated in the study, consisting of 1.850 women (45.7%) and 2194 men (54.3%). Of these, 3647 students completed the AUDIT questionnaire.
AUDIT score
A low AUDIT score was recorded for 2573 students (1318 men and 1255 women), accounting for 67.1% of the total participants. A medium score was found for 893 students (583 men and 310 women), representing 23.3% of the total. High scores were identified in 92 students (68 men and 24 women), which is 2.4% of the participants, and very high scores were noted in 86 students (61 men and 25 women), making up 2.2% of the total participants.
Quality of life
In the next part, the quality of life of students during a pandemic is focused on. Quality of life was evaluated according to the EuroQol questionnaire. Mobility and self-care were not problematic for most of the students who stayed. Difficulty performing daily activities was reported by 21.3% of the students. Mild pain was reported in 33.8% of cases, while moderate pain was reported in 5.2% of cases. Mild depression and anxiety were reported in 31.1% of the cases, and moderate depression and anxiety were reported in 13.5% of the cases. Greater mobility problems were reported by women compared to men ( p = 0.017). A statistically significant difference was observed in the incidence of pain ( p < 0.001) and anxiety ( p < 0.001) in women compared to men (Table 2 ).
Relationship between quality of life and alcohol consumption
In the question: “Q1 How often do you drink alcoholic beverages?” 4038 students answered. The answer "4x or more per week” was chosen by 321 (7.9%) students. There are 3717 students who drink less often or do not drink at all. In the most at-risk group of students in terms of drinking frequency, the incidence is twice as high in those who have the worst perception of pain, anxiety, and subjective feeling of health, compared to those who drink less often or do not drink at all (Table 3 A). In the question “Q2 How often do you drink six or more standard drinks on one occasion?” 4021 students answered. 46 (1.14%) students chose the answer “daily or almost daily”. There are 3975 students who drink less or do not drink at all. In the highest-risk group of students, based on the amount of alcohol consumed on a single occasion, severe pain perception is, on average, 10 times more common, along with higher levels of anxiety and poorer subjective health, compared to those who drink less frequently or not at all (Table 3 B). In the question “Q3 How many standard drinks will you drink during a typical day when you drink?” 3717 students answered. The answer “10 and more” was chosen by 287 (7.7%) students. In the most at-risk group of students in terms of the amount of alcohol consumed during a typical day when they drink, those who have the worst perception of pain, anxiety, and subjective health are on average 2 times more likely than those who drink less often or do not drink at all.
Based on the results of the chi-square test between AUDIT and EuroQOL variables (Table 4 ), it can be concluded that there is a statistically significant relationship between AUDIT score and EuroQOL score ( p <0.001).
In our study, we observed a significant correlation between lower quality of life and higher frequency of heavy alcohol consumption among Slovak college students. This connection indicates that students who engage in excessive alcohol consumption are more likely to experience diminished quality of life. These findings highlight the critical need to address alcohol-related issues within the college student population in Slovakia. To improve the well-being of these students, it is essential to recognize the adverse effects of high alcohol consumption on various aspects of their lives. This understanding enables us to refine existing strategies and interventions to specifically target students at risk due to their alcohol consumption patterns. Additionally, further research is necessary to elucidate the underlying mechanisms and contributing factors to the relationship between heavy alcohol consumption and reduced quality of life. A deeper understanding of these dynamics can inform the development of more effective interventions and policies aimed at both preventing excessive alcohol use and enhancing the overall quality of life for college students in Slovakia. Excessive or problematic alcohol consumption is associated with numerous health issues, including liver damage, cardiovascular diseases, and mental health disorders, all of which can significantly impair an individual's quality of life (Roerecke et al. 2019 ). These health problems can cause discomfort, pain, and a reduced ability to participate in daily activities, negatively affecting quality of life. Alcohol abuse is closely related to mental health problems such as depression and anxiety (Barr et al. 2016 ; Kushner et al. 2000 ; Roerecke et al. 2019 ; Smith and Randall 2012 ; Torvik et al. 2019 ). The mood-altering effects of alcohol can provide temporary relief, but in the long run, it can exacerbate these conditions, leading to a poorer quality of life. Excess alcohol consumption can strain relationships, lead to social isolation, and result in legal issues (Gossop et al. 2002 ; Wechsler et al. 2001 ). These social consequences can cause emotional distress and negatively impact one's overall well-being. Funding a heavy drinking habit can lead to financial strain and instability, affecting one's ability to access necessities and engage in enjoyable activities. On the other hand, it is also possible that individuals experiencing a lower quality of life may turn to alcohol as a coping mechanism or means of escape from their challenges. People facing stress, academic pressure, loneliness, or other life difficulties can use alcohol as a way to cope or self-medicate. This can create a cycle in which alcohol is relied on to numb emotional pain or stress. Alcohol consumption can serve as a way to facilitate social interactions or feel more connected. Understanding the directionality of the relationship between alcohol consumption and quality of life is challenging because it often involves a complex interplay of individual factors, including genetics, mental health, social support, and personal experiences. Offering mental health services and resources to help people cope with stress, anxiety, and depression in healthier ways. Addressing both aspects, reducing harmful drinking patterns and improving overall well-being, is crucial to promoting a healthier and happier life among college students and beyond (Alcoholism et al. 1981 ; Boumans et al. 2022 ; Michie et al. 2012 ).
Alcohol consumption is a way of relaxation for many people; however, alcohol can increase an individual’s vulnerability, both physical and mental, and lead to higher risk behaviors such as violent reactions, depression, or anxiety (Calina et al. 2021 ). In our study, alcohol consumption was higher in the group which also reported a higher prevalence of pain, anxiety, and depression. Alcohol consumption is associated with many illnesses and mental disorders (Sharifi-Rad et al. 2020 ). Alcohol has several long-term and short-term effects on every organ of the body, so there is no “safe” limit to alcohol consumption (Aloizou et al. 2021 ; Kokkinakis et al. 2020 ). Due to the social acceptance of high levels of alcohol consumption as part of student culture, risky drinking is often downplayed. This may be partly because many students show easy recovery from hazardous drinking, often without special treatment. However, such behavior may have negative consequences in the future, and in particular, young age is associated with the highest risk of alcohol dependence.
The level of alcohol consumption has also been tested in other countries. Grossman et al. ( 2020 ) investigated consumption during a pandemic in 832 students in the United States. Participants who experienced COVID-19-related stress reported consuming more alcoholic beverages (β = 4.7; CI (0.2, 9.1); p = 0.040) and spending more days drinking alcohol (β = 2.4; CI (0.6, 4.1) p = 0.007). Furthermore, 60% reported increased alcohol consumption, but 13% of participants reported reduced drinking compared to the previous era of COVID-19. The reasons for increased drinking, such as in our study, were increased stress (45.7%). Other reasons given are the increase in alcohol availability (34.4%) and boredom (30.1%). The effect of a pandemic on alcohol consumption in adults was also examined in a study by Nordeck et al. ( 2022 ). Men, white participants and older adults reported a steady increase in drinking days, while women and individuals living below the poverty line showed a reduction in drinking days. Rossow et al. ( 2021 ) measured the level of alcohol consumption in the Norwegian population (n-1.195). A mean slight decrease in consumption was found for most participants. However, the small part with the highest initial consumption significantly increased its consumption and the share of heavy drinkers increased significantly ( p < 0.001). In a study by Chodkiewicz et al. ( 2020 ), alcohol is the most commonly used psychoactive substance (73% during the 2020 lockdown in Poland. More than 30% of Poland have changed their drinking habits as a result of the pandemic, with 16% drinking less while 14% are drinking more. The COVID-19 pandemic had a complex and multifaceted impact on alcohol consumption, with different effects depending on individual circumstances, social factors, and coping mechanisms. Our study was conducted during the COVID-19 pandemic and could have influenced the amount of alcohol that students consumed.
Several factors have been identified as risky for alcohol-related illnesses during a pandemic, such as social isolation, depression, lonely housing, loss of income, unemployment, home office, etc. One of the factors that people start to drink more is loss of work. A study by Weerakoon et al. ( 2021 ) focused on this issue. One-third (33%) of the participants ( n = 2441; 67% of women) reported consuming more alcohol than before the pandemic and 11% said that COVID-19 had a negative impact on their employment. Participants reported drinking more alcohol because they had more time (28%) or boredom (22%). Another important factor in alcohol consumption is social isolation. Social isolation is a major stress factor that can encourage increased alcohol consumption. In a cross-sectional study by Moura et al. ( 2021 ), 992 individuals were tested in self-isolation. A total of 68.5% of participants reported drinking during a pandemic and 22.7% reported increasing alcohol consumption. Alcohol consumption was associated with anxiety, similar to our study ( p <0.01).
Our study was associated with several limitations that can affect the interpretation of the data. The questionnaire was distributed to students and their completion was voluntary. This may have prevented students with high or low alcohol consumption from filling in, thus affecting the overall outcome of the study. Alcohol consumption among students could also be affected by the financial situation and the availability of alcohol in families. The students reported the alcohol consumption data themselves, and it is not possible to prove the truth of the statements, and therefore some answers may be underestimated or overestimated. The cross-sectional nature of the study limits the ability to establish causality between alcohol consumption and quality of life. Longitudinal studies are needed to determine the direction of the relationship. The reliance on self-reported data for alcohol consumption and quality of life may introduce response bias. Participants might underreport or overreport their alcohol use and health status. The findings our are study specific to college students in Slovak and may not be generalizable to college students in other countries or to non-student populations. The study was conducted during the third wave of the COVID-19 pandemic, a period that might have influenced both alcohol consumption patterns and quality of life due to heightened stress and changes in social behavior (Martínez-Cao et al. 2021 ). The pandemic has resulted in many stressors, including social isolation (Banerjee and Rai 2020 ).
Higher alcohol consumption was associated with a poorer quality of life in Slovak college students. Our results underscore the importance of addressing alcohol consumption in this population to potentially enhance their quality of life. The association between higher alcohol consumption and poorer quality of life in Slovak college students raises important questions about causality and the complex interplay between alcohol consumption and one’s overall well-being. This relationship may be influenced by various factors such as mental health, social support, academic stress, and lifestyle choices, all of which warrant further investigation.
These findings could inform interventions aimed at improving health-related quality of life through alcohol use reduction strategies. University health services and policymakers should consider implementing comprehensive alcohol education and prevention programs that address the specific needs and challenges faced by college students. By reducing alcohol consumption, it may be possible to improve not only the immediate health outcomes but also the long-term quality of life for students.
The relationship between alcohol use and quality of life highlights a critical area for public health intervention. Addressing alcohol consumption among university students could lead to substantial improvements in their overall well-being and health-related quality of life.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Aloizou A-M, Siokas V, Pateraki G, Liampas I, Bakirtzis C, Tsouris Z, Lazopoulos G, Calina D, Docea AO, Tsatsakis A, Bogdanos DP, Dardiotis E (2021) Thinking outside the Ischemia Box: Advancements in the Use of Multiple Sclerosis Drugs in Ischemic Stroke. J Clin Med 10(4):630. https://doi.org/10.3390/jcm10040630
Article PubMed PubMed Central CAS Google Scholar
Ballester L, Alayo I, Vilagut G, Almenara J, Cebrià AI, Echeburúa E, Gabilondo A, Gili M, Lagares C, Piqueras JA, Roca M, Soto-Sanz V, Blasco MJ, Castellví P, G. Forero C, Mortier P, Alonso J (2021) Validation of an Online Version of the Alcohol Use Disorders Identification Test (AUDIT) for Alcohol Screening in Spanish University Students. Int J Environ Res Public Health 18(10):5213. https://doi.org/10.3390/ijerph18105213
Article PubMed PubMed Central Google Scholar
Banerjee D, Rai M (2020) Social isolation in Covid-19: The impact of loneliness. Int J Soc Psychiatry 66(6):525–527. https://doi.org/10.1177/0020764020922269
Barbería-Latasa M, Gea A, Martínez-González MA (2022) Alcohol, Drinking Pattern, and Chronic Disease. Nutrients 14(9):1954. https://doi.org/10.3390/nu14091954
Barr T, Helms C, Grant K, Messaoudi I (2016) Opposing effects of alcohol on the immune system. Prog Neuro Psychopharmacol Biol Psychiatry 65:242–251. https://doi.org/10.1016/j.pnpbp.2015.09.001
Article CAS Google Scholar
Becker HC (2017) Influence of stress associated with chronic alcohol exposure on drinking. Neuropharmacology 122:115–126. https://doi.org/10.1016/j.neuropharm.2017.04.028
Benjet C, Mortier P, Kiekens G, Ebert DD, Auerbach RP, Kessler RC, Cuijpers P, Green JG, Nock MK, Demyttenaere K, Albor Y, Bruffaerts R (2022) A risk algorithm that predicts alcohol use disorders among college students. Eur Child Adolesc Psychiatry 31(7):1–11. https://doi.org/10.1007/s00787-020-01712-3
Article PubMed CAS Google Scholar
Boumans J, van de Mheen D, Crutzen R, Dupont H, Bovens R, Rozema A (2022) Understanding How and Why Alcohol Interventions Prevent and Reduce Problematic Alcohol Consumption among Older Adults: A Systematic Review. Int J Environ Res Public Health 19(6):3188. https://doi.org/10.3390/ijerph19063188
Calina D, Hartung T, Mardare I, Mitroi M, Poulas K, Tsatsakis A, Rogoveanu I, Docea AO (2021) COVID-19 pandemic and alcohol consumption: Impacts and interconnections. Toxicol Rep. 8:529–535. https://doi.org/10.1016/j.toxrep.2021.03.005
Casper MF, Child JT, Gilmour D, McIntyre KA, Pearson JC (2006) Healthy research perspectives: Incorporating college student experiences with alcohol. Health Commun 20(3):289–298. https://doi.org/10.1207/s15327027hc2003_8
Chodkiewicz J, Talarowska M, Miniszewska J, Nawrocka N, Bilinski P (2020) Alcohol Consumption Reported during the COVID-19 Pandemic: The Initial Stage. Int J Environ Res Public Health 17(13):E4677. https://doi.org/10.3390/ijerph17134677
Chow MSC, Poon SHL, Lui KL, Chan CCY, Lam WWT (2021) Alcohol Consumption and Depression Among University Students and Their Perception of Alcohol Use. East Asian Arch Psychiatr 31(4):87–96. https://doi.org/10.12809/eaap20108
Dawson DA, Grant BF, Ruan WJ (2005) The association between stress and drinking: Modifying effects of gender and vulnerability. Alcohol Alcohol 40(5):453–460. https://doi.org/10.1093/alcalc/agh176
Article PubMed Google Scholar
Dich N, Doan SN (2019) Moderate emotional reactions to stressful life events are associated with lowest risk of increased alcohol consumption: Evidence from the Whitehall II study. Eur J Public Health 29(4):754–758. https://doi.org/10.1093/eurpub/ckz066
Freire BR, de Castro PASV, Petroianu A (2020) Alcohol consumption by medical students. Rev Da Associacao Med Brasileira (1992) 66(7):943–947. https://doi.org/10.1590/1806-9282.66.7.943
Article Google Scholar
GBD 2016 Alcohol Collaborators (2018) Alcohol use and burden for 195 countries and territories, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet 392(10152):1015–1035. https://doi.org/10.1016/S0140-6736(18)31310-2
Article PubMed Central Google Scholar
Gossop M, Marsden J, Stewart D (2002) Dual dependence: Assessment of dependence upon alcohol and illicit drugs, and the relationship of alcohol dependence among drug misusers to patterns of drinking, illicit drug use and health problems. Addiction 97(2):169–178. https://doi.org/10.1046/j.1360-0443.2002.00028.x
Grossman ER, Benjamin-Neelon SE, Sonnenschein S (2020) Alcohol Consumption during the COVID-19 Pandemic: A Cross-Sectional Survey of US Adults. Int J Environ Res Public Health 17(24):E9189. https://doi.org/10.3390/ijerph17249189
Hayatbakhsh MR, Najman JM, Bor W, Clavarino A, Alati R (2011) School performance and alcohol use problems in early adulthood: A longitudinal study. Alcohol 45(7):701–709. https://doi.org/10.1016/j.alcohol.2010.10.009
Hoyland MA, Latendresse SJ (2018) Stressful Life Events Influence Transitions Among Latent Classes of Alcohol Use. Psychol Addictive Behav 32(7):727–737. https://doi.org/10.1037/adb0000412
Keyes KM, Hatzenbuehler ML, Grant BF, Hasin DS (2012) Stress and alcohol: Epidemiologic evidence. Alcohol Res Curr Rev 34(4):391–400
CAS Google Scholar
Kokkinakis M, Tsakiris I, Tzatzarakis M, Vakonaki E, Alegakis A, Papachristou S, Karzi V, Kokkinaki A, Goumenou M, Kallionakis M, Kalogeraki A (2020) Carcinogenic, ethanol, acetaldehyde and noncarcinogenic higher alcohols, esters, and methanol compounds found in traditional alcoholic beverages. A risk assessment approach. Toxicol Rep 7:1057–1065. https://doi.org/10.1016/j.toxrep.2020.08.017
Kuitunen-Paul S, Roerecke M (2018) Alcohol Use Disorders Identification Test (AUDIT) and mortality risk: A systematic review and meta-analysis. J Epidemiol Community Health 72(9):856–863. https://doi.org/10.1136/jech-2017-210078
Kushner MG, Abrams K, Borchardt C (2000) The relationship between anxiety disorders and alcohol use disorders: A review of major perspectives and findings. Clin Psychol Rev 20(2):149–171. https://doi.org/10.1016/s0272-7358(99)00027-6
Lee CS, Abrantes AM, Colby SM, López SR, Jordan TJ (2008) Medical student judgments of adolescents with alcohol use disorders (AUD). Subst Use Misuse 43(5):709–721. https://doi.org/10.1080/10826080701202791
Liskola J, Haravuori H, Lindberg N, Niemelä S, Karlsson L, Kiviruusu O, Marttunen M (2018) AUDIT and AUDIT-C as screening instruments for alcohol problem use in adolescents. Drug Alcohol Depend 188:266–273. https://doi.org/10.1016/j.drugalcdep.2018.04.015
Lundin A, Hallgren M, Balliu N, Forsell Y (2015) The use of alcohol use disorders identification test (AUDIT) in detecting alcohol use disorder and risk drinking in the general population: Validation of AUDIT using schedules for clinical assessment in neuropsychiatry. Alcohol Clin Exp Res 39(1):158–165. https://doi.org/10.1111/acer.12593
Martínez-Cao C, de la Fuente-Tomás L, Menéndez-Miranda I, Velasco Á, Zurrón-Madera P, García-Álvarez L, Sáiz PA, Garcia-Portilla MP, Bobes J (2021) Factors associated with alcohol and tobacco consumption as a coping strategy to deal with the coronavirus disease (COVID-19) pandemic and lockdown in Spain. Addictive Behav 121:107003. https://doi.org/10.1016/j.addbeh.2021.107003
Matošić A, Marušić S, Vidrih B, Kovak-Mufić A, Cicin-Šain L (2016) Neurobiological bases of alcohol addiction. Acta Clin Croatica 55(1):134–150. https://doi.org/10.20471/acc.2016.55.01.19
McKay JR, Hiller-Sturmhöfel S (2011) Treating Alcoholism As a Chronic Disease. Alcohol Res Health 33(4):356–370
PubMed PubMed Central Google Scholar
Michie S, Whittington C, Hamoudi Z, Zarnani F, Tober G, West R (2012) Identification of behaviour change techniques to reduce excessive alcohol consumption. Addiction 107(8):1431–1440. https://doi.org/10.1111/j.1360-0443.2012.03845.x
Moura HF, von Diemen L, Bulzing RA, Meyer J, Grabovac I, López-Sánchez GF, Sadarangani KP, Tully MA, Smith L, Schuch FB (2021) Alcohol use in self-isolation during the COVID-19 pandemic: A cross-sectional survey in Brazil. Trends in Psychiatry and Psychotherapy. https://doi.org/10.47626/2237-6089-2021-0337
Nordeck CD, Riehm KE, Smail EJ, Holingue C, Kane JC, Johnson RM, Veldhuis CB, Kalb LG, Stuart EA, Kreuter F, Thrul J (2022) Changes in drinking days among United States adults during the COVID-19 pandemic. Addiction 117(2):331–340. https://doi.org/10.1111/add.15622
Panel on alternative policies affecting the prevention of alcohol abuse and alcoholism, Moore MH, Gerstein DR (1981) Reducing Alcohol Abuse: A Critical Review of Educational Strategies. In Alcohol and Public Policy: Beyond the Shadow of Prohibition. National Academies Press (US). https://www.ncbi.nlm.nih.gov/books/NBK216409/
Quinn PD, Fromme K (2011) Alcohol Use and Related Problems Among College Students and Their Noncollege Peers: The Competing Roles of Personality and Peer Influence. J Stud Alcohol Drugs 72(4):622–632
Ragusa R, Bertino G, Bruno A, Frazzetto E, Cicciu F, Giorgianni G, Lupo L (2018) Evaluation of health status in patients with hepatitis c treated with and without interferon. Health Qual Life Outcomes 16:17. https://doi.org/10.1186/s12955-018-0842-x
Ranker LR, Lipson SK (2022) Prevalence of heavy episodic drinking and alcohol use disorder diagnosis among US college students: Results from the national Healthy Minds Study. Addictive Behav 135:107452. https://doi.org/10.1016/j.addbeh.2022.107452
Rehm J, Shield KD (2014) Alcohol and Mortality. Alcohol Res Curr Rev 35(2):174–183
Google Scholar
Rehm J, Samokhvalov AV, Neuman MG, Room R, Parry C, Lönnroth K, Patra J, Poznyak V, Popova S (2009) The association between alcohol use, alcohol use disorders and tuberculosis (TB). A systematic review. BMC Public Health 9(1):450. https://doi.org/10.1186/1471-2458-9-450
Roerecke M, Vafaei A, Hasan OSM, Chrystoja BR, Cruz M, Lee R, Neuman MG, Rehm J (2019) Alcohol Consumption and Risk of Liver Cirrhosis: A Systematic Review and Meta-Analysis. Am J Gastroenterol 114(10):1574–1586. https://doi.org/10.14309/ajg.0000000000000340
Rossow I, Bye EK, Moan IS, Kilian C, Bramness JG (2021) Changes in Alcohol Consumption during the COVID-19 Pandemic-Small Change in Total Consumption, but Increase in Proportion of Heavy Drinkers. Int J Environ Res Public Health 18(8):4231. https://doi.org/10.3390/ijerph18084231
Sepanlou SG, Safiri S, Bisignano C, Ikuta KS, Merat S, Saberifiroozi M, Poustchi H, Tsoi D, Colombara DV, Abdoli A, Adedoyin RA, Afarideh M, Agrawal S, Ahmad S, Ahmadian E, Ahmadpour E, Akinyemiju T, Akunna CJ, Alipour V, Malekzadeh R (2020) The global, regional, and national burden of cirrhosis by cause in 195 countries and territories, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet Gastroenterol Hepatol 5(3):245–266. https://doi.org/10.1016/S2468-1253(19)30349-8
Sharifi-Rad M, Lankatillake C, Dias DA, Docea AO, Mahomoodally MF, Lobine D, Chazot PL, Kurt B, Tumer TB, Moreira AC, Sharopov F, Martorell M, Martins N, Cho WC, Calina D, Sharifi-Rad J (2020) Impact of Natural Compounds on Neurodegenerative Disorders: From Preclinical to Pharmacotherapeutics. J Clin Med 9(4):E1061. https://doi.org/10.3390/jcm9041061
Shield KD, Parry C, Rehm J (2013) Chronic diseases and conditions related to alcohol use. Alcohol Res Curr Rev 35(2):155–173
Slutske WS (2005) Alcohol use disorders among US college students and their non-college-attending peers. Arch Gen Psychiatry 62(3):321–327. https://doi.org/10.1001/archpsyc.62.3.321
Smith JP, Randall CL (2012) Anxiety and alcohol use disorders: Comorbidity and treatment considerations. Alcohol Res Curr Rev 34(4):414–431
Sohi I, Franklin A, Chrystoja B, Wettlaufer A, Rehm J, Shield K (2021) The Global Impact of Alcohol Consumption on Premature Mortality and Health in 2016. Nutrients 13(9):3145. https://doi.org/10.3390/nu13093145
Stautz K, Brown KG, King SE, Shemilt I, Marteau TM (2016) Immediate effects of alcohol marketing communications and media portrayals on consumption and cognition: A systematic review and meta-analysis of experimental studies. BMC Public Health 16(1):465. https://doi.org/10.1186/s12889-016-3116-8
Torvik FA, Rosenström TH, Gustavson K, Ystrom E, Kendler KS, Bramness JG, Czajkowski N, Reichborn-Kjennerud T (2019) Explaining the association between anxiety disorders and alcohol use disorder: A twin study. Depression Anxiety 36(6):522–532. https://doi.org/10.1002/da.22886
Verhoog S, Dopmeijer JM, de Jonge JM, van der Heijde CM, Vonk P, Bovens RHLM, de Boer MR, Hoekstra T, Kunst AE, Wiers RW, Kuipers MAG (2020) The Use of the Alcohol Use Disorders Identification Test – Consumption as an Indicator of Hazardous Alcohol Use among University Students. Eur Addiction Res 26(1):1–9. https://doi.org/10.1159/000503342
Volpicelli JR (2001) Alcohol abuse and alcoholism: An overview. J Clin Psychiatry 62(Suppl 20):4–10
PubMed Google Scholar
Wackernah RC, Minnick MJ, Clapp P (2014) Alcohol use disorder: Pathophysiology, effects, and pharmacologic options for treatment. Subst Abus Rehabilit 5:1–12. https://doi.org/10.2147/SAR.S37907
Wang S-C, Chen Y-C, Chen S-J, Lee C-H, Cheng C-M (2020) Alcohol Addiction, Gut Microbiota, and Alcoholism Treatment: A Review. Int J Mol Sci 21(17):6413. https://doi.org/10.3390/ijms21176413
Wechsler H, Lee JE, Gledhill-Hoyt J, Nelson TF (2001) Alcohol use and problems at colleges banning alcohol: Results of a national survey. J Stud Alcohol 62(2):133–141. https://doi.org/10.15288/jsa.2001.62.133
Weerakoon SM, Jetelina KK, Knell G, Messiah SE (2021) COVID-19 related employment change is associated with increased alcohol consumption during the pandemic. Am J Drug Alcohol Abus 47(6):730–736. https://doi.org/10.1080/00952990.2021.1912063
Xi B, Veeranki SP, Zhao M, Ma C, Yan Y, Mi J (2017) Relationship of Alcohol Consumption to All-Cause, Cardiovascular, and Cancer-Related Mortality in U.S. Adults. J Am Coll Cardiol 70(8):913–922. https://doi.org/10.1016/j.jacc.2017.06.054
Zhou Y, Zheng J, Li S, Zhou T, Zhang P, Li H-B (2016) Alcoholic Beverage Consumption and Chronic Diseases. Int J Environ Res Public Health 13(6):E522. https://doi.org/10.3390/ijerph13060522
Download references
Author information
Authors and affiliations.
Matej Bel University, Faculty of Sport Science and Health, Banská Bystrica, Slovakia
Dávid Líška
Faculty of Economics, Technical University of Košice, Department of Applied Mathematics and Businnes Informatics, Košice, Slovakia
Erika Liptáková
Institute of Languages, Social Sciences and Academic Sports, Technical University of Košice, Department of Academic Sports, 04200, Košice, Slovakia
Miroslava Barcalová
2nd Department of Internal Medicine of the Slovak Medical University Faculty of Medicine, HEGITO (Div Hepatology, Gastroenterology and Liver Transplant), F. D. Roosevelt Teaching Hospital, Banska Bystrica, Slovakia
Ľubomír Skladaný
You can also search for this author in PubMed Google Scholar
Contributions
ĽS and DL: conceptualization. ĽS and DL: methodology. ĽS: validation and supervision. EL: formal analysis. DL, MB, EL: investigation. DL, MB, ĽS, EL: writing. DL, MB, ĽS, EL: original draft preparation. DL, MB, ĽS, EL: writing—review and editing. EL and MB: project administration. All authors contributed to the article and approved the submitted version.
Corresponding author
Correspondence to Dávid Líška .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The study was approved by the ethics committee of Matej Bel University under number no. 2200/21.
Informed consent
All participants agreed to participate in the study and consented to data processing before filling out the questionnaire.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Líška, D., Liptáková, E., Barcalová, M. et al. The impact of alcohol consumption on the quality of life of college students: a study from three Slovak universities. Humanit Soc Sci Commun 11 , 1456 (2024). https://doi.org/10.1057/s41599-024-03931-4
Download citation
Received : 18 February 2024
Accepted : 14 October 2024
Published : 02 November 2024
DOI : https://doi.org/10.1057/s41599-024-03931-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
- Introduction
- Conclusions
- Article Information
eTable 1. Health Deficits of the Frailty Index in the UK Biobank Cohort
eTable 2. Association of Wine Preference and Drinking During Meals With Mortality in Older Drinkers From the UK Biobank Cohort
eTable 3. Association of Average Alcohol Intake Status With Mortality in Older Drinkers From the UK Biobank Cohort, Excluding Participants With Prevalent Cancer at Baseline for Cancer Mortality, or Those With Prevalent CVD at Baseline for CVD Mortality
eTable 4. Association of Wine Preference or Drinking During Meals With Mortality in Older Drinkers From the UK Biobank Cohort, Excluding Participants With Prevalent Cancer at Baseline for Cancer Mortality, or Those With Prevalent CVD at Baseline for CVD Mortality
eTable 5. Association of Wine Preference and Drinking During Meals With Mortality in Older Drinkers From the UK Biobank Cohort, Excluding Participants With Prevalent Cancer at Baseline for Cancer Mortality, or Those With Prevalent CVD at Baseline for CVD Mortality
eTable 6. Association of Average Alcohol Intake Status With Mortality in Older Drinkers From the UK Biobank Cohort, by Drinking Patterns, Excluding Participants With Prevalent Cancer at Baseline for Cancer Mortality, or Those With Prevalent CVD at Baseline for CVD Mortality
Data Sharing Statement
See More About
Sign up for emails based on your interests, select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Digital Health
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Sexual Health
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
Get the latest research based on your areas of interest.
Others also liked.
- Download PDF
- X Facebook More LinkedIn
Ortolá R , Sotos-Prieto M , García-Esquinas E , Galán I , Rodríguez-Artalejo F. Alcohol Consumption Patterns and Mortality Among Older Adults With Health-Related or Socioeconomic Risk Factors. JAMA Netw Open. 2024;7(8):e2424495. doi:10.1001/jamanetworkopen.2024.24495
Manage citations:
© 2024
- Permissions
Alcohol Consumption Patterns and Mortality Among Older Adults With Health-Related or Socioeconomic Risk Factors
- 1 Department of Preventive Medicine and Public Health, Universidad Autónoma de Madrid, Madrid, Spain
- 2 Center for Biomedical Research in Epidemiology and Public Health, Madrid, Spain
- 3 Department of Environmental Health and Nutrition, Harvard T.H. Chan School of Public Health. Boston, Massachusetts
- 4 Madrid Institute for Advanced Studies Food Institute, Campus of International Excellence Universidad Autónoma de Madrid + Spanish National Research Council, Madrid, Spain
- 5 Department of Chronic Diseases, National Center for Epidemiology, Carlos III Health Institute, Madrid, Spain
Question Do health-related or socioeconomic risk factors modify the associations of alcohol consumption patterns with mortality among older drinkers?
Findings This cohort study in 135 103 older drinkers found that even low-risk drinking was associated with higher mortality among older adults with health-related or socioeconomic risk factors. Wine preference and drinking only with meals were associated with attenuating the excess mortality associated with alcohol consumption.
Meaning This cohort study identified inequalities in the detrimental health outcomes associated with alcohol that should be addressed to reduce the high disease burden of alcohol use.
Importance Alcohol consumption is a leading cause of morbidity and mortality that may be more important in older adults with socioeconomic or health-related risk factors.
Objective To examine the association of alcohol consumption patterns with 12-year mortality and its modification by health-related or socioeconomic risk factors.
Design, Setting, and Participants This prospective cohort study used data from the UK Biobank, a population-based cohort. Participants were current drinkers aged 60 years or older. Data were analyzed from September 2023 to May 2024.
Exposure According to their mean alcohol intake in grams per day, participants’ drinking patterns were classified as occasional: ≤2.86 g/d), low risk (men: >2.86-20.00 g/d; women: >2.86-10.00 g/d), moderate risk (men: >20.00-40.00 g/d; women: >10.00-20.00 g/d) and high risk (men: >40.00 g/d; women: >20.00 g/d).
Main Outcomes and Measures Health-related risk factors were assessed with the frailty index, and socioeconomic risk factors were assessed with the Townsend deprivation index. All-cause and cause-specific mortality were obtained from death certificates held by the national registries. Analyses excluded deaths in the first 2 years of follow-up and adjusted for potential confounders, including drinking patterns and preferences.
Results A total of 135 103 participants (median [IQR] age, 64.0 [62.0-67.0] years; 67 693 [50.1%] women) were included. In the total analytical sample, compared with occasional drinking, high-risk drinking was associated with higher all-cause (hazard ratio [HR], 1.33; 95% CI, 1.24-1.42), cancer (HR, 1.39; 95% CI, 1.26-1.53), and cardiovascular (HR, 1.21; 95% CI, 1.04-1.41) mortality; moderate-risk drinking was associated with higher all-cause (HR, 1.10; 95% CI, 1.03-1.18) and cancer (HR, 1.15; 95% CI, 1.05-1.27) mortality, and low-risk drinking was associated with higher cancer mortality (HR, 1.11; 95% CI, 1.01-1.22). While no associations were found for low- or moderate-risk drinking patterns vs occasional drinking among individuals without socioeconomic or health-related risk factors, low-risk drinking was associated with higher cancer mortality (HR, 1.15; 95% CI, 1.01-1.30) and moderate-risk drinking with higher all-cause (HR, 1.10; 95% CI, 1.01-1.19) and cancer (HR, 1.19; 95% CI, 1.05-1.35) mortality among those with health-related risk factors; low-risk and moderate-risk drinking patterns were associated with higher mortality from all causes (low risk: HR, 1.14; 95% CI, 1.01-1.28; moderate risk: HR, 1.17; 95% CI, 1.03-1.32) and cancer (low risk: HR, 1.25; 95% CI, 1.04-1.50; moderate risk: HR, 1.36; 95% CI, 1.13-1.63) among those with socioeconomic risk factors. Wine preference (>80% of alcohol from wine) and drinking with meals showed small protective associations with mortality, especially from cancer, but only in drinkers with socioeconomic or health-related risk factors and was associated with attenuating the excess mortality associated with high-, moderate- and even low-risk drinking.
Conclusions and Relevance In this cohort study of older drinkers from the UK, even low-risk drinking was associated with higher mortality among older adults with health-related or socioeconomic risk factors. The attenuation of mortality observed for wine preference and drinking only during meals requires further investigation, as it may mostly reflect the effect of healthier lifestyles, slower alcohol absorption, or nonalcoholic components of beverages.
Alcohol consumption is a leading cause of morbidity and mortality, accounting for approximately 5.1% of the global burden of disease and 5.3% of all deaths and being responsible for significant social and economic losses, thus representing a major public health problem. 1 Additionally, the assumed benefits of drinking low amounts of alcohol, especially on cardiovascular disease (CVD) mortality, 2 - 4 are being questioned due to selection biases, reverse causation, and residual confounding, 5 supporting health messaging that the safest level of drinking is no drinking at all or less is better. 6 , 7 Selection biases are often overlooked, but they can lead to a systematic underestimation of alcohol-related burden. That is the case of the abstainer bias, whereby the apparently lower mortality of light drinkers compared with abstainers could be explained by the higher death risk of the abstainers because they include former drinkers who quit alcohol due to poor health, as well as lifetime abstainers, 5 who often have worse lifestyle and health characteristics than regular drinkers. 8 Also, the healthy drinker/survivor bias, caused by overrepresentation of healthier drinkers who have survived the deleterious effects of alcohol, can distort comparisons, especially in older age. 5 In addition, drinking habits may influence the association between the amount of alcohol consumed and health. In this context, wine preference has been associated with lower risk of death, 9 CVD morbimortality, 10 and diabetes, 11 attributing the beneficial associations of wine to its high content in polyphenols. 12 Furthermore, drinking with meals has been associated with lower risk of all-cause, non-CVD, and cancer deaths 13 and frailty, 14 so this might be a safer option for alcohol drinkers along with moderate consumption. 15
The health impact of alcohol consumption may be greater in individuals with socioeconomic or health-related risk factors. On one hand, older adults with health-related risk factors are more susceptible to the harmful outcomes associated with alcohol due to their greater morbidity, higher use of alcohol-interacting drugs, and reduced tolerance. 16 , 17 However, some studies have observed benefits of alcohol on unhealthy aging or frailty, especially of light alcohol intake 18 , 19 and of a Mediterranean alcohol drinking pattern, defined as moderate alcohol consumption, preferably wine and accompanying meals, 14 , 20 suggesting that the protective associations of these potentially beneficial drinking patterns might be greater in individuals with ill health, although they might be due to the aforementioned methodological issues. 5 Therefore, it would be of interest to examine whether health-related risk factors modify the associations between alcohol consumption patterns and mortality.
On the other hand, there is evidence that socioeconomically disadvantaged populations have higher rates of alcohol-related harms for equivalent and even lower amounts of alcohol, probably due to the coexistence of other health challenges, including less healthy lifestyles, and lower social support or access to health care. 21 , 22 Also, the potentially beneficial associations of wine preference and drinking during meals might be more important in individuals with socioeconomic risk factors. However, to our knowledge, no previous research has examined whether socioeconomic status modifies the associations between these potentially beneficial drinking patterns and health.
Therefore, the aim of our study is to examine the associations of several potentially beneficial alcohol consumption patterns, that is, consumption of low amounts of alcohol, wine preference, and drinking only during meals, with all-cause, cancer, and CVD mortality in older adults and their modification by health-related or socioeconomic risk factors, while addressing the main methodological issues deemed to bias such associations. Thus, we restrict analyses to current drinkers and use occasional drinkers instead of abstainers as the reference group to prevent selection biases, exclude deaths in the first 2 years of follow-up to reduce reverse causation, and adjust analyses for many sociodemographic, lifestyle, and clinical variables to palliate residual confounding. We also restrict analyses to older adults because most deaths occur in this population group, which also has a high prevalence of health-related risk factors and because the protective associations of alcohol consumption have been specifically observed in older adults, 6 which is consistent with our aim to study potentially beneficial drinking patterns.
This cohort study was approved by the North West Multi-Centre Research Ethics Committee, and all participants provided written informed consent before enrollment. This study is reported following the Strengthening the Reporting of Observational Studies in Epidemiology ( STROBE ) reporting guideline.
We used data from the UK Biobank cohort, a multicenter, prospective, population-based study with more than 500 000 participants aged 40 to 69 years identified from National Health Service primary care registers and enrolled at 22 assessment sites across England, Scotland, and Wales between 2006 and 2010. At the baseline assessment visit, they completed a computer-assisted interview and a touch-screen questionnaire on sociodemographic, lifestyle, and clinical characteristics, provided biological samples, and underwent physical and medical examinations. They were followed-up for mortality through linkage to national death registries. Additional information on the UK Biobank study has been reported elsewhere. 23 , 24
At the baseline assessment visit, study participants were asked about the frequency and mean amount of the main types of alcoholic beverages that they consumed, and alcohol content was estimated by multiplying the volume ingested (in milliliters) by the volume percentage of alcohol (4.5% for beer and cider, 11.5% for white and sparkling wine, 13% for red wine, 20% for fortified wine, and 40% for spirits) and by the specific gravity of ethanol (0.789 g/mL). According to their mean alcohol intake, drinking patterns were classified into occasional (≤2.86 g/d), low risk (men: >2.86-20.00 g/d; women: >2.86-10.00 g/d), moderate risk (men: >20.00-40.00 g/d; women: >10-20.00 g/d), and high risk (men: >40.00 g/d; women: >20.00 g/d), a categorization based on the recommendations from health authorities that we have used in previous studies. 25 - 27 When more than 80% of alcohol came from a certain type of beverage, drinkers were classified as with preference for wine, with preference for other drinks, or with no preference. 27 Participants were also classified as drinkers only during meals and as drinkers either only outside of meals or at any time. Finally, participants were classified as drinkers with no wine preference nor drinking only during meals, drinkers with wine preference or drinking only during meals, and drinkers with wine preference and drinking only during meals.
Health-related risk was assessed at baseline using the frailty index (FI) developed specifically for the UK Biobank 28 based on the procedure used by Rockwood et al. 29 A total of 49 health deficits were considered, most dichotomously (1 point if present and 0 points otherwise), and a few according to severity (0 points for no deficit, 0.25-0.75 points for mild to moderate deficits, and 1 point for severe deficit). The FI score was calculated as the total sum of points assigned to each health deficit divided by the number of deficits considered and ranged from 0.00 to 0.57. The complete list of health deficits and associated scores can be found in eTable 1 in Supplement 1 . Participants were considered to have health-related risk factors if they were prefrail or frail (FI > 0.12). 28
Socioeconomic risk was assessed at baseline using the Townsend deprivation index (TDI), 30 which measures the level of an area’s socioeconomic deprivation. TDI ranges from −6.26 to 10.16, with higher score indicating greater deprivation. Participants were considered to have socioeconomic risk factors if they lived in more deprived areas (TDI > 0) and not if they lived in more affluent areas (TDI ≤ 0).
Information on mortality was obtained from death certificates held by the National Health Service (NHS) Information Centre (NHS England) up to September 30, 2021, for participants in England and Wales, and by the NHS Central Register Scotland (National Records of Scotland) up to October 31, 2021, for participants in Scotland. 31 , 32 Length of follow-up was estimated as the time from the baseline assessment visit to the date of death or administrative censoring, whichever came first. Cause-specific mortality was ascertained with the International Statistical Classification of Diseases and Related Health Problems, Tenth Revision ( ICD-10 ) classification 33 : codes C00 to C97 as primary cause of death for cancer and codes I00 to I99 for CVD.
We also used baseline information on sociodemographic, lifestyle, and clinical characteristics, including sex, age, self-reported race and ethnicity, education (college or university degree; A levels, AS levels, or equivalent; O levels, General Certificate of Secondary Education, or equivalent; Certificate of Secondary Education or equivalent; National Vocational Qualification, Higher National Diploma, Higher National Certificate, or equivalent; other professional qualifications; and no qualifications), tobacco smoking (never, former, or current), leisure-time physical activity (metabolic equivalents of task-hours per week), time spent watching television (hours per day), and prevalent morbidities (diabetes, CVD, and cancer) that could have a potential effect on the amount of alcohol consumed. In the UK Biobank, race and ethnicity are classified as Asian (Indian, Pakistani, Bangladeshi, any other Asian background), Black (Caribbean, African, any other Black background), Chinese, multiple (White and Black Caribbean, White and Black African, White and Asian, any other mixed background), White (British, Irish, any other White background), and other (any group not specified, eg, Arab).
From 217 462 participants aged at least 60 years in the UK Biobank cohort, we excluded 36 284 with incomplete information on alcohol consumption, 10 456 never drinkers, 8295 former drinkers, and 20 167 known binge drinkers (those who consumed ≥6 units of alcohol in 1 session) to avoid classifying binge drinkers with low mean alcohol intake as low-risk drinkers. We additionally excluded 1140 participants who died in the first 2 years of follow-up and 6017 participants with missing information on the FI (194 participants), the TDI (116 participants), and potential confounders (5707 participants). Thus, the analytical sample included 135 103 individuals.
The associations of alcohol consumption patterns (mean alcohol intake status, wine preference, and drinking during meals) at baseline with all-cause and cause-specific mortality were summarized with hazard ratios (HRs) and their 95% CIs obtained from Cox regression; the models included interactions between alcohol consumption patterns and health-related or socioeconomic risk factors and adjusted for baseline sociodemographic (sex, age, race and ethnicity, education, and TDI [except when stratifying by socioeconomic risk factors]), lifestyle (tobacco smoking, leisure-time physical activity, and time spent watching television), and clinical characteristics (diabetes, CVD, cancer, and FI score [except when stratifying by health-related risk factors]) of study participants. Analyses of alcohol intake were further adjusted for wine preference and drinking during meals, whereas analyses of wine preference and drinking during meals were further adjusted for mean alcohol intake and the other drinking pattern.
To characterize whether wine preference and drinking during meals modified the association of mean alcohol intake with mortality, we tested interaction terms defined as the product of the categories of mean alcohol intake by 3 categories of drinking patterns (no wine preference nor drinking only during meals, wine preference or drinking only during meals, and wine preference and drinking only during meals).
Additionally, we assessed whether sociodemographic and lifestyle variables modified the study associations by testing interaction terms defined as the product of alcohol consumption patterns by categories of such variables (except mean alcohol intake status by sex, as sex was included in the definition of alcohol intake status). Since no interactions were found, the results are presented for the total sample. Finally, we performed additional sensitivity analyses excluding participants with prevalent cancer at baseline for cancer mortality or those with prevalent CVD at baseline for CVD mortality.
Statistical significance was set at 2-sided P < .05. Analyses were performed with Stata software version 17 (StataCorp). Data were analyzed from September 2023 to May 2024.
A total of 135 103 participants (median [IQR] age, 64.0 [62.0-67.0] years; 67 693 [50.1%] women) were included. Occasional drinkers less often identified as White; were more frequently residents in England, women, and never smokers; were less physically active; had a lower educational level, a lower prevalence of CVD; and had a higher prevalence of diabetes, cancer, and health-related risk factors. Having socioeconomic risk factors was less frequent in low- and moderate-risk drinkers ( Table 1 ).
Over a median (range) follow-up of 12.4 (2.0 to 14.8) years, 15 833 deaths were recorded, including 7871 cancer deaths and 3215 CVD deaths. Compared with occasional drinking, low-risk drinking was associated with higher cancer mortality (HR, 1.11; 95% CI, 1.01-1.22); moderate-risk drinking was associated with higher all-cause (HR, 1.10; 95% CI, 1.03-1.18) and cancer (HR, 1.15; 95% CI, 1.05-1.27) mortality; and high-risk drinking was associated with higher all-cause (HR, 1.33; 95% CI, 1.24-1.42), cancer (HR, 1.39; 95% CI, 1.26-1.53), and CVD (HR, 1.21; 95% CI, 1.04-1.41) mortality ( Table 2 ). Hazards were greater in individuals with health-related or socioeconomic risk factors vs those without across categories of alcohol intake. Interestingly, while no associations with mortality were found in participants without health-related or socioeconomic risk factors among low- or moderate-risk drinkers, low-risk drinkers with health-related risk factors had higher cancer mortality (HR, 1.15; 95% CI, 1.01-1.30) and moderate-risk drinkers with health-related risk factors had higher all-cause (HR, 1.10; 95% CI, 1.01-1.19) and cancer (HR, 1.19; 95% CI, 1.05-1.35) mortality ( Table 2 ). Likewise, both low-risk and moderate-risk drinkers with socioeconomic risk factors showed higher mortality from all causes (low risk: HR, 1.14; 1.01-1.28; moderate risk: 1.17; 95% CI, 1.03-1.32) and cancer (low-risk: HR, 1.25; 95% CI, 1.04-1.50; moderate risk: HR, 1.36; 95% CI, 1.13-1.63) ( Table 2 ).
Wine preference and drinking only during meals were associated with lower all-cause mortality only in participants with health-related risk factors (wine preference: HR, 0.92; 95% CI, 0.87-0.97; drinking only during meals: HR, 0.93; 95% CI, 0.89-0.97), as well as in participants with socioeconomic risk factors (wine preference: HR, 0.84; 95% CI, 0.78-0.90; drinking only during meals: HR, 0.83; 95% CI, 0.78-0.89) ( Table 3 ). Drinking only during meals was also associated with lower cancer mortality in participants with health-related risk factors (HR, 0.92; 95% CI, 0.86-0.99) or socioeconomic risk factors (HR, 0.85; 95% CI, 0.78-0.94) ( Table 3 ). Furthermore, in individuals with socioeconomic risk factors, wine preference was associated with lower cancer mortality (HR, 0.89; 95% CI, 0.80-0.99) and drinking only during meals with lower CVD mortality (HR, 0.86; 95% CI, 0.75-1.00) ( Table 3 ). Adhering to both drinking patterns was associated with lower all-cause, cancer, and CVD mortality in drinkers with health-related or socioeconomic risk factors, and to a lesser extent, with lower all-cause death in drinkers without health-related risk factors (eTable 2 in Supplement 1 ). Importantly, wine preference and drinking during meals modified the association of mean alcohol intake with mortality: the excess risk of all-cause, cancer, and CVD death for high-risk drinkers, of all-cause and cancer death for moderate-risk drinkers, and of cancer death for low-risk drinkers vs occasional drinkers was attenuated and even lost among individuals with these drinking patterns ( Table 4 ). Analyses excluding participants with prevalent cancer at baseline for cancer mortality, or those with prevalent CVD at baseline for CVD mortality showed consistent results (eTables 3-6 in Supplement 1 ).
This cohort study in older alcohol drinkers from the UK found that compared with occasional drinkers, low-risk drinkers had higher cancer mortality, moderate-risk drinkers had higher all-cause and cancer mortality, and high-risk drinkers had higher all-cause, cancer, and CVD mortality. The excess mortality associated with alcohol consumption was higher in individuals with health-related and socioeconomic risk factors, among whom even low-risk drinkers had higher mortality, especially from cancer. Wine preference and drinking only with meals showed small protective associations with mortality, especially from cancer, among drinkers with health-related and socioeconomic risk factors, and these 2 drinking patterns attenuated the excess mortality associated with high-, moderate-, and even low-risk drinking.
In line with recent research on the associations between alcohol use and health, 6 , 34 , 35 our results corroborate the detrimental outcomes associated with heavy drinking in older adults. However, we also found higher risk for all-cause and cancer deaths in moderate-risk drinkers, unlike most previous research, which has reported protective associations of low to moderate alcohol consumption, mainly for all-cause 2 - 4 , 36 and CVD 3 , 36 , 37 mortality, ischemic heart disease, 3 , 6 , 34 and diabetes, 6 or null associations with all-cause mortality, 38 CVD, 39 and unhealthy aging. 20 This discrepancy may be due to the implementation of an important methodological improvement in our analyses, that is, using occasional drinkers as the reference group instead of lifetime abstainers, to prevent selection bias caused by misclassification of former drinkers as abstainers, and to palliate residual confounding because they are more like light drinkers than are never drinkers. 40 , 41 In fact, another analysis of the UK Biobank cohort that also avoided selection biases found an increased CVD risk in the general population for drinking up to 14 units per week. 42
To our knowledge, there are no studies examining the potential modification of health-related risk factors on the association between alcohol use and health. The stronger associations between mean alcohol intake and mortality observed in older adults with health-related risk factors make sense, since they have more morbid conditions potentially aggravated by alcohol and greater use of alcohol-interacting medications than their counterparts without health-related risk factors. 16 , 17 The fact that even low-risk drinkers with these risk factors had higher risk of cancer death is an important finding, which is consistent with the reported increased risk of several types of cancer and cancer mortality even with very low amounts of alcohol. 6 , 36 , 37 , 43
Our results also suggest that socioeconomic status acts as a modifier of the association between the amount of alcohol consumed and mortality, as mortality hazard was much greater in individuals with socioeconomic risk factors than in individuals without, in line with previous research. 21 , 22 , 44 , 45 We even found a detrimental association of low amounts of alcohol with all-cause and cancer mortality in this group, unlike the MORGAM study by DiCasetnuovo et al 44 reporting a lower mortality associated with consuming no more than 10 g/d of alcohol, which was clearer in individuals with higher vs lower education. 44 These discrepant results could again be explained by the different reference groups used: occasional drinkers in our study and never drinkers in the MORGAM study. Importantly, although older adults with socioeconomic risk factors have a higher risk of ill health and death, probably due to the coexistence of other health challenges, especially poorer lifestyles, 21 , 22 the observed associations in our study were independent of lifestyles, suggesting that other factors should account for them.
Regarding the potentially beneficial drinking patterns, that is, wine preference and drinking during meals, the literature is inconsistent. A 2018 pool of studies 34 reported a nondifferential association of specific types of alcoholic drinks with all-cause mortality and several CVD outcomes, whereas other studies have found protective health associations for wine but not other beverages. 15 , 46 Drinking with meals has also shown protective associations with several health outcomes. 15 In our analysis, these drinking patterns modified the association between alcohol intake and death risk. On one hand, the protective association for mortality of these patterns was only observed in individuals with socioeconomic or health-related risk factors, independently of the amount of alcohol consumed. On the other hand, the detrimental association of alcohol intake was more evident in individuals without these patterns. These findings suggest that the less detrimental associations of alcohol intake from wine or during meals are not due to alcohol itself, but to other factors, including nonalcoholic components of wine, such as antioxidants, slower absorption of alcohol ingested with meals and its consequent reduced alcoholaemia, as well as spacing drinks when drinking only with meals, or more moderate attitudes in individuals who choose to adhere to these drinking patterns.
Our study has several strengths, such as the large sample size, the long follow-up, and the methodological improvements implemented to prevent selection biases and reduce reverse causation. However, it also has some limitations. First, alcohol intake was self-reported, and therefore prone to some degree of misclassification. Also, alcohol intake was measured only at baseline and not at multiple time points over the life span, not allowing us to take into account changes in alcohol intake before the baseline assessment or to redistribute former drinkers among categories of current drinkers to reduce selection bias; this may have led to an underestimation of the true effects of alcohol consumption. 5 Second, as in any observational study, we cannot entirely rule out residual confounding, despite adjusting for many potential confounders. And third, this study was conducted in older adults in the UK with a high proportion of White participants, so our results may not be generalizable to other racial ethnic groups or populations with different lifestyles, drinking patterns, or socioeconomic development.
This cohort study among older drinkers from the UK did not find evidence of a beneficial association between low-risk alcohol consumption and mortality; however, we observed a detrimental association of even low-risk drinking in individuals with socioeconomic or health-related risk factors, especially for cancer deaths. The attenuation of the excess mortality associated with alcohol among individuals who preferred to drink wine or drink only during meals requires further investigation to elucidate the factors that may explain it. Finally, these results have important public health implications because they identify inequalities in the detrimental health outcomes associated with alcohol that should be addressed to reduce the high burden of disease of alcohol use.
Accepted for Publication: May 30, 2024.
Published: August 12, 2024. doi:10.1001/jamanetworkopen.2024.24495
Open Access: This is an open access article distributed under the terms of the CC-BY License . © 2024 Ortolá R et al. JAMA Network Open .
Corresponding Author: Rosario Ortolá, MD, PhD, Department of Preventive Medicine and Public Health, School of Medicine, Universidad Autónoma de Madrid, Calle del Arzobispo Morcillo 4, 28029 Madrid, Spain ( [email protected] ).
Author Contributions: Dr Ortolá had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Concept and design: Ortolá.
Acquisition, analysis, or interpretation of data: All authors.
Drafting of the manuscript: Ortolá.
Critical review of the manuscript for important intellectual content: Sotos-Prieto, García-Esquinas, Galán, Rodríguez-Artalejo.
Statistical analysis: Ortolá.
Obtained funding: Sotos-Prieto, Rodríguez-Artalejo.
Administrative, technical, or material support: Rodríguez-Artalejo.
Supervision: García-Esquinas, Galán.
Conflict of Interest Disclosures: None reported.
Funding/Support: This work was supported by the Plan Nacional sobre Drogas, Ministry of Health of Spain (grant No. 2020/17), Instituto de Salud Carlos III, State Secretary of R+D+I and Fondo Europeo de Desarrollo Regional/Fondo Social Europeo (Fondo de Investigación en Salud grants No. 19/319, 20/896, and 22/1111), Agencia Estatal de Investigación (grant No. CNS2022-135623), Carlos III Health Institute and the European Union “NextGenerationEU (grant No. PMP21/00093), and the Fundación Francisco Soria Melguizo (Papel de la Disfunción Mitocondrial en la Relación Entre Multimorbilidad Crónica y Deterioro Funcional en Ancianos project grant). Mercedes Sotos-Prieto holds a Ramón y Cajal contract (contract No. RYC-2018-025069-I) from the Ministry of Science, Innovation and Universities.
Role of the Funder/Sponsor: The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Data Sharing Statement: See Supplement 2 .
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution


Search form
- Advanced search
- Search responses
- Search blogs
- News & Views
- Alcohol consumption...
Alcohol consumption and brain health
- Related content
- Peer review
- Killian A Welch , consultant neuropsychiatrist and honorary senior lecturer
- Robert Fergusson Unit, Royal Edinburgh Hospital, EH10 5HF, UK
- Killian.Welch{at}nhslothian.scot.nhs.uk
Even moderate drinking is linked to pathological changes in the brain
Epidemiological studies often report better heath in moderate drinkers compared with abstainers. Observed first in studies of incidence of myocardial infarction, 1 the “J shaped curve” (describing the graphical appearance of health measures plotted against consumption) reappears in studies of diabetes, stroke, and even chronic widespread pain. 2 As methods of investigating the association between alcohol and health are refined, however, the size of the apparent benefits reduces substantially. 3 Studies using “Mendelian randomisation,” purportedly impervious to confounding or reverse causality, do not support the original claim that moderate drinking improves cardiovascular health. 4
Regarded as a further example of the J shaped curve, a protective effect of moderate alcohol consumption against “all cause” dementia has been reported. 5 This has not been underpinned by a convincing neural correlate, however, and it is here that the linked study by Topiwala and colleagues (doi: 10.1136/bmj.j2353 ) is particularly ambitious. 6 In their prospective cohort of 550 civil servants, none of whom were alcohol dependent, the authors repeatedly assessed alcohol consumption and cognition over 30 years. Participants underwent brain imaging at the most recent review, enabling examination of relations between average alcohol use, cognition, and brain structure.
After adjustment for numerous potential confounders, alcohol use was associated with reduced right hippocampal volume in a dose dependent manner; even moderate drinkers (classified as up to 21 units a week for men at the time of the study) were three times more likely to have hippocampal atrophy than abstainers, and very light drinking (1-6 units a week) conferred no protection relative to abstinence. Higher alcohol consumption was also associated with reduced white matter integrity and faster decline in lexical fluency, a test of “executive function.”
With increasing longevity, maintenance of brain health into older age is the key priority of our time. Leaving aside the human cost of dementia, care of cognitively impaired older people is a looming financial crisis, prompting politicians to consider controversial and deeply unpopular policy decisions. 7 Alcohol dependence is already established as a major cause of dementia, alcohol related brain damage (ARBD) accounts for possibly 10% of early onset dementia 8 and potentially 10-24% of dementia cases in nursing homes. 9
Existing on a spectrum of severity, alcohol related brain damage typically involves relatively young people, often in their 40s or 50s, meaning the more severely affected require decades of institutional care. While alcohol related brain damage generally afflicts malnourished drinkers consuming very high levels of alcohol, some degree of potentially reversible cognitive impairment is detectable in most people starting treatment for alcohol dependence. 10 Alcohol can be the primary cause of cognitive impairment in some individuals, but it is a likely contributor to cognitive decline in many more.
The chief medical officer recently changed guidance for low risk drinking in men, reducing the recommended maximum intake from 21 to 14 units a week. 11 This was because of accumulating evidence that even light drinking increases the risk of various malignancies. 12 The relation between alcohol and brain health is more complex than the relation between alcohol and cancer. While there is almost universal agreement that heavy drinking is associated with cognitive impairment, numerous observational studies do report that light to moderate consumption is associated with a reduced risk of all cause dementia.
While concerns about confounding and inconsistencies between studies make it difficult to define what level of intake is “optimal” for cognition, it seems to be low; in these studies around a unit a day is associated with the lowest risk of dementia, with risk for drinkers clearly exceeding abstainers by 4 units a day. 13 Topiwala and colleagues’ report of adverse effects at even lower levels of intake, coupled with the finding that drinking more than 14 units a week was associated with both brain pathology and cognitive decline, provides further support for the chief medical officer’s recent decision.
How should this paper inform discussions with patients? It certainly strengthens the view that if alcohol does confer beneficial effects on health, the link is probably confined to low intakes of no more than a unit a day. Even this level of consumption carries risk relative to abstinence for conditions such as breast cancer, and the evidence of benefit is certainly not strong enough to justify advising abstainers to drink.
As intake increases, so does the risk to health, probably in a dose dependent manner. Heavy consumption is associated with potentially severe impairments in memory and executive function, even when other obvious risk factors are absent. Topiwala and colleagues’ findings strengthen the argument that drinking habits many regard as normal have adverse consequences for health. This is important. We all use rationalisations to justify persistence with behaviours not in our long term interest. With publication of this paper, justification of “moderate” drinking on the grounds of brain health becomes a little harder.
- Research, doi: 10.1136/bmj.j2353
Competing interests: I have read and understood the BMJ policy on declaration of interests and have no interests to declare.
Provenance and peer review: Commissioned; not externally reviewed.
This is an Open Access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/ .
- ↵ Klatsky AL, Friedman GD, Siegelaub AB. Alcohol consumption before myocardial infarction. Results from the Kaiser-Permanente epidemiologic study of myocardial infarction. Ann Intern Med 1974 ; 357 : 294 - 301 . doi:10.7326/0003-4819-81-3-294 pmid:4850474 . OpenUrl
- ↵ Beasley MJ, Macfarlane TV, Macfarlane GJ. Is alcohol consumption related to likelihood of reporting chronic widespread pain in people with stable consumption? Results from UK biobank. Pain 2016 ; 357 : 2552 - 60 . doi:10.1097/j.pain.0000000000000675 pmid:27437785 . OpenUrl
- ↵ Knott CS, Coombs N, Stamatakis E, Biddulph JP. All cause mortality and the case for age specific alcohol consumption guidelines: pooled analyses of up to 10 population based cohorts. BMJ 2015 ; 357 : h384 . doi:10.1136/bmj.h384 pmid:25670624 . OpenUrl
- ↵ Holmes MV, Dale CE, Zuccolo L, et al. InterAct Consortium. Association between alcohol and cardiovascular disease: Mendelian randomisation analysis based on individual participant data. BMJ 2014 ; 357 : g4164 . doi:10.1136/bmj.g4164 pmid:25011450 . OpenUrl
- ↵ Neafsey EJ, Collins MA. Moderate alcohol consumption and cognitive risk. Neuropsychiatr Dis Treat 2011 ; 357 : 465 - 84 . doi:10.2147/NDT.S23159 pmid:21857787 . OpenUrl
- ↵ Topiwala A, Allan C, Valkanova V, et al. Moderate alcohol consumption as risk factor for adverse brain outcomes and cognitive decline: longitudinal cohort study. BMJ 2017 ; 357 : j2353 . OpenUrl Abstract / FREE Full Text
- ↵ Asthana A, Elgot J, Asthana A, Elgot J. Theresa may ditches manifesto plan with ‘dementia tax’ U-turn. Guardian. 22nd May 2017. https://www.theguardian.com/society/2017/may/22/theresa-may-u-turn-on-dementia-tax-cap-social-care-conservative-manifesto .
- ↵ Harvey RJ, Skelton-Robinson M, Rossor MN. The prevalence and causes of dementia in people under the age of 65 years. J Neurol Neurosurg Psychiatry 2003 ; 357 : 1206 - 9 . doi:10.1136/jnnp.74.9.1206 pmid:12933919 . OpenUrl
- ↵ Ridley NJ, Draper B, Withall A. Alcohol-related dementia: an update of the evidence. Alzheimers Res Ther 2013 ; 357 : 3 . doi:10.1186/alzrt157 pmid:23347747 . OpenUrl
- ↵ Iverson GL, Lange RT, Franzen MD. Effects of mild traumatic brain injury cannot be differentiated from substance abuse. Brain Inj 2005 ; 357 : 11 - 8 . doi:10.1080/02699050410001720068 pmid:15762097 . OpenUrl
- ↵ UK chief medical officers’ alcohol guidelines review: Summary of the proposed new guidelines. Department of Health, 2016.
- ↵ Bagnardi V, Rota M, Botteri E, et al. Light alcohol drinking and cancer: a meta-analysis. Ann Oncol 2013 ; 357 : 301 - 8 . doi:10.1093/annonc/mds337 pmid:22910838 . OpenUrl
- ↵ Xu W, Wang H, Wan Y, et al. Alcohol consumption and dementia risk: a dose-response meta-analysis of prospective studies. Eur J Epidemiol 2017 ; 357 : 31 - 42 . doi:10.1007/s10654-017-0225-3 pmid:28097521 . OpenUrl

An official website of the United States government
Here's how you know
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.

Published Date: December 1, 2013
The Burden of Alcohol Use: Excessive Alcohol Consumption and Related Consequences Among College Students
Aaron White, Ph.D., and Ralph Hingson, Sc.D.
Aaron White, Ph.D., is program director, College and Underage Drinking Prevention Research; and
Ralph Hingson, Sc.D., is director, Division of Epidemiology and Prevention Research, both at the National Institute on Alcohol Abuse and Alcoholism, Bethesda, Maryland.
Volume 35, Issue 2 ⦁ Pages: 201-218
Research shows that multiple factors influence college drinking, from an individual’s genetic susceptibility to the positive and negative effects of alcohol, alcohol use during high school, campus norms related to drinking, expectations regarding the benefits and detrimental effects of drinking, penalties for underage drinking, parental attitudes about drinking while at college, whether one is member of a Greek organization or involved in athletics, and conditions within the larger community that determine how accessible and affordable alcohol is. Consequences of college drinking include missed classes and lower grades, injuries, sexual assaults, overdoses, memory blackouts, changes in brain function, lingering cognitive deficits, and death. This article examines recent findings about the causes and consequences of excessive drinking among college students relative to their non-college peers and many of the strategies used to collect and analyze relevant data, as well as the inherent hurdles and limitations of such strategies.
Since 1976, when the National Institute on Alcohol Abuse and Alcoholism (NIAAA) issued its first report on alcohol misuse by college students, research advances have transformed our understanding of excessive drinking on college campuses and the negative outcomes that follow from it. For instance, we now know that a broad array of factors influence whether a particular college student will choose to drink, the types of consequences they suffer from drinking, and how they respond to those consequences. We have learned that predisposing factors include an individual’s genetic susceptibility to the positive and negative effects of alcohol, alcohol use during high school, campus norms related to drinking, expectations regarding the benefits and detrimental effects of drinking, penalties for underage drinking, parental attitudes about drinking while at college, whether one is member of a Greek organization or involved in athletics, and conditions within the larger community that determine how accessible and affordable alcohol is. Consequences include missed classes and lower grades, injuries, sexual assaults, overdoses, memory blackouts, changes in brain function, lingering cognitive deficits, and death.
This article reviews recent research findings about alcohol consumption by today’s college students and the outcomes that follow. It examines what we know about the causes and consequences of excessive drinking among college students relative to their non-college peers and many of the strategies used to collect and analyze relevant data, as well as the inherent hurdles and limitations of such strategies.
Excessive Drinking At College
Currently, only two active national survey studies are able to characterize the drinking habits of college students in the United States. The National Survey on Drug Use and Health (NSDUH), an annual survey sponsored by the Substance Abuse and Mental Health Services Administration (SAMHSA), involves face-to-face interviews with approximately 67,500 persons ages 12 and older each year regarding use of alcohol and other drugs. Monitoring the Future (MTF) is an annual, paper-and-pencil national survey of alcohol and other drug use with a sample comprising nearly 50,000 students in 8th, l0th, and 12th grades drawn from roughly 420 public and private schools. Approximately 2,400 graduating seniors are resurveyed in subsequent years, allowing for the monitoring of trends in college drinking.
In addition, two prior surveys yielded data on college drinking that remain valuable and relevant. The National Epidemiologic Survey on Alcohol and Related Conditions (NESARC), sponsored by NIAAA, collected data on alcohol and other drug use from a sample of roughly 46,500 citizens 18 and older using face-to-face computer-assisted interviews. Two waves of data (2001 and 2004) were collected from the same sample, and data from an independent sample are scheduled to be collected in 2013. The Harvard College Alcohol Study (CAS), although no longer active, was a landmark paper-and-pencil survey that provided national data (years 1993, 1997, 1999, and 2001) from roughly 15,000 students on more than 100 college campuses each year (Wechsler and Nelson 2008). Data from both NESARC and Harvard CAS remain useful for examining associations between patterns of drinking at college and the frequency and prevalence of alcohol-related consequences for both drinkers and nondrinkers.
Data from NSDUH and MTF suggest that roughly 65 percent of college students drink alcohol in a given month (see figure 1 for data from MTF), and Harvard CAS all suggest that a large percentage of college students who drink do so to excess. Excessive, or “binge,” drinking is defined in NSDUH, MTF, and NESARC as consuming five or more drinks in an evening, although the instruments vary in the specified time frames given (i.e., once or more in the past month for NSDUH, past 2 weeks for MTF, and multiple time periods for NESARC) (Johnston et al. 2001 a ; SAMHSA 2011). The Harvard CAS was the first national study of college students to utilize a gender-specific definition of binge drinking (i.e., four or more drinks in an evening for females or five or more for males in the past 2 weeks) to equate the risk of alcohol-related harms (Wechsler et al. 1995). The Centers for Disease Control and Prevention (CDC) utilizes the same four or more/five or more gender-specific measures but specifies a 30-day time period (Chen et al. 2011). NIAAA uses the four or more/five or more gender-specific measure but specifies a time frame of 2 hours for consumption, as this would generate blood alcohol levels of roughly 0.08 percent, the legal limit for driving, for drinkers of average weight (NIAAA 2004).
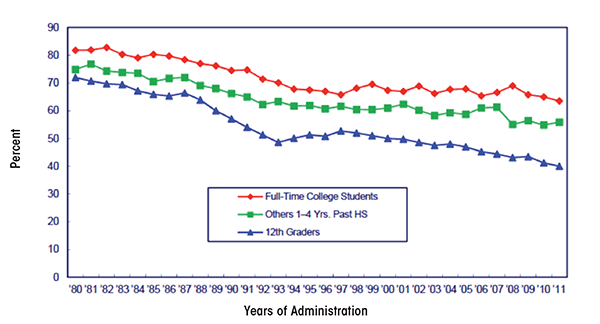
According to NSDUH, the percentage of 18- to 22-year- old college students who reported drinking five or more drinks on an occasion in the previous 30 days remained relatively stable from 2002 (44 percent) to 2010 (44 percent) (SAMHSA 2011). Among 18- to 22-year-olds not enrolled in college, the percentage who engaged in binge drinking decreased significantly from 2002 (39 percent) to 2010 (36 percent) (see figure 2).
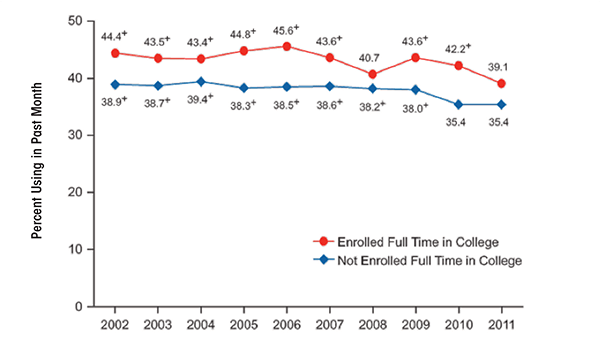
Looking at a longer time period, data from MTF suggest that there have been significant declines in the percentage of college students consuming five or more drinks in the previous 2 weeks, from 44 percent in 1980 to 36 percent in 2011 (Johnston et al. 2012) (see figure 3). This time frame includes the passage of the National Minimum Drinking Age Act of 1984, which effectively increased the drinking age from 18 to 21 in the United States.
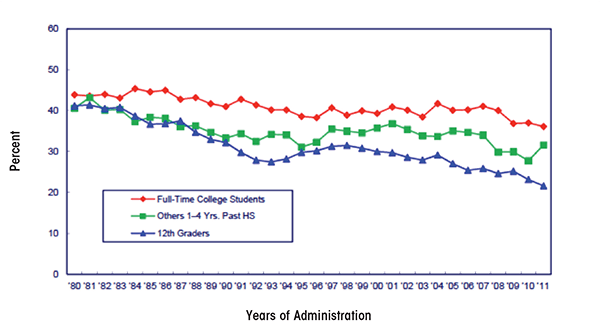
Across the four waves of data collection in the Harvard CAS (1993, 1997, 1999, and 2001), rates of binge drinking remained relatively stable (44, 43, 45, and 44 percent, respectively) (Wechsler et al. 2002) (see figure 4). However, the number of non–binge drinkers decreased, whereas the number of frequent binge drinkers (three or more binge-drinking episodes in a 2-week period) increased. Wechsler and colleagues (2002) reported that binge drinkers consumed 91 percent of all the alcohol consumed by college students during the study period. Frequent binge drinkers, a group comprising only 1 in 5 college students, accounted for 68 percent of all alcohol consumed (Wechsler and Nelson 2008).
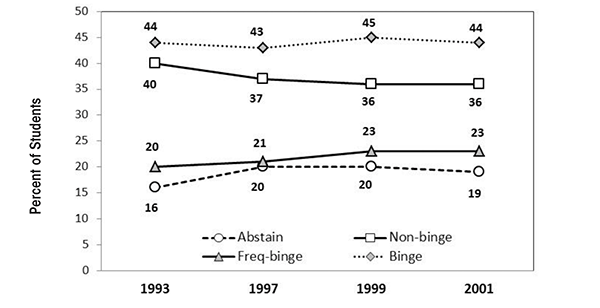
Individual and Environmental Contributors to Excessive Drinking
Survey data indicate that males outpace females with regard to binge drinking. According to MTF, in 2011, 43 percent of male and 32 percent of female college students crossed the binge threshold in a given 2-week period. Further, 40 percent of students—more males (44 percent) than females (37 percent)—reported getting drunk in a given month. Research suggests that gender differences in alcohol use by college students have narrowed considerably over the years. In their landmark 1953 report on college drinking, Yale researchers Straus and Bacon indicated that, based on survey data from more than 15,000 students on 27 college campuses, 80 percent of males and 49 percent of females reported having been drunk at some point. Nearly 60 years later, in 2011, data from MTF indicated that 68 percent of males and 68 percent females reported having been drunk. These new, higher levels of drinking among females seem to be ingrained in the youth drinking culture. Whereas binge-drinking rates declined significantly among high-school seniors over the last decade, the effect was driven by a decline among males only. Binge-drinking rates among females remained relatively stable (Johnston et al. 2012) (see figure 5).
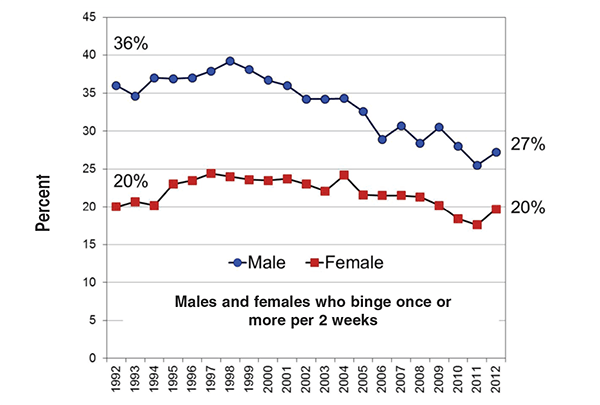
Beyond gender, survey studies of college drinking reveal a range of characteristics of both individual students and campus environments that influence the likelihood of binge drinking. Data from the Harvard CAS and other studies reveal that males, Caucasians, members of Greek organizations, students on campuses with lower percentages of minority and older students, athletes, students coping with psychological distress, those on campuses near a high density of alcohol outlets, students with access to cheap drink specials, a willingness to endure the consequences of alcohol misuse, and drinking at off-campus parties and bars all contribute to excessive drinking (Mallett et al. 2013; Wechsler and Kuo 2003; Yusko et al. 2008). Further, students living off campus and/or in Greek housing, those who drink to try to fit it, students with inflated beliefs about the proportion of other students who binge drink, and those with positive expectations about the results of drinking are more likely to drink excessively (Scott-Sheldon et al. 2012; Wechsler and Nelson 2008). Importantly, excessive drinking prior to college relative to other college-bound students is predictive of both excessive drinking at college and experiencing alcohol-related consequences (Varvil-Weld et al. 2013; White et al. 2002).
Strengths and Weaknesses of Binge-Drinking Measures
Several studies indicate that crossing commonly used binge-drinking thresholds increases a college student’s risk of experiencing negative alcohol-related consequences. For instance, data from the Harvard CAS indicate that students who binge one or two times during a 2-week period are roughly three times as likely as non–binge drinkers to get behind in school work, do something regretful while drinking, experience a memory blackout, have unplanned sex, fail to use birth control during sex, damage property, get in trouble with police, drive after drinking, or get injured (Wechsler et al. 2000). The more often a student binges, the greater the risk of negative outcomes. Further, the more binge drinking that occurs on a campus, the more likely non–binge drinkers and abstainers are to experience secondhand consequences of alcohol use, such as having studying or sleep disrupted, being a victim of sexual assault, and having property damaged (Wechsler and Nelson 2008).
Because of the increased risk of consequences to self and others that occurs when a person drinks at or beyond the binge threshold, a great deal of emphasis is placed on tracking the percentage of college students that cross binge thresholds. Although this has proven extremely valuable, as Wechsler and Nelson (2001, p. 289) state, “Alcohol use is a complex behavior. No single measure will capture all the relevant aspects of alcohol use.” One limitation of using a single threshold is that it removes data regarding just how heavily students actually drink (Alexander and Bowen 2004; Read et al. 2008) and assigns the same level of risk to all students who cross the thresholds regardless of how far beyond the threshold they go. This is an important consideration as recent studies suggest that plenty of college students who cross the binge threshold when they drink go far beyond it.
In a study of 10,424 first-semester college freshmen, more than one-half of all males and one-third of all females categorized as binge drinkers drank at levels two or more times the binge threshold (8 or more drinks for women and 10 or more drinks for men) at least once in the 2 weeks before the survey. Indeed, one in four binge-drinking males consumed 15 or more drinks at a time during that period (White et al. 2006). Naimi and colleagues (2010) reported that 18- 24-year-olds in the United States drink an average of 9.5 drinks per binge episode, nearly twice the standard binge threshold. Data from MTF also reveal that both college students and their non-college peers often drink at levels that exceed the binge threshold. On average, between 2005 and 2011, 7 percent of college females surveyed and 24 percent of college males consumed 10 or more drinks at least once in a 2-week period, compared with 7 percent of females and 18 percent of males not in college. Further, 2 percent of all college females surveyed and 10 percent of college males consumed 15 or more drinks in a 2-week period. Rates among non-college peers were similar, at 2 percent among females and 9 percent among males (Johnston et al. 2012). For a 140-pound female, consuming 15 drinks over a 6-hour period would produce an estimated blood alcohol level above 0.4 percent, a level known to have claimed, directly, several lives on college campuses in recent years. For a 160-pound male, drinking in this way would lead to a blood alcohol level above 0.3 percent, a potentially lethal level associated with memory blackouts and injury deaths.
Data from the Harvard CAS suggested that students who binge drink frequently (three or more times in a 2-week period) are at particularly high risk of negative alcohol-related outcomes. Compared with students who binge drink one or two times in a 2-week period, those who binge three or more times are twice as likely to experience alcohol-induced memory losses (27 percent vs. 54 percent, respectively), not use protection during sex (10 percent vs. 20 percent, respectively), engage in unplanned sex (22 percent vs. 42 percent, respectively), and get hurt or injured (11 percent vs. 27 percent, respectively), and are equally likely to need medical treatment for an overdose (1 percent vs. 1 percent). Whereas binge frequency is associated with an increased risk of negative outcomes, additional research indicates that there is a relationship between how often a student binges and the peak number of drinks he or she consumes. White and colleagues (2006) reported that 19 percent of frequent binge drinkers consume three or more times the binge threshold (12 or more drinks for females and 15 or more for males) at least once in a 2-week period compared with only 5 percent of infrequent binge drinkers. As a result of the association between frequency of binge drinking and peak levels of consumption, it is difficult to determine if the increase in risk that comes with frequent bingeing is a result of the number of binge episodes, per se, or the number of drinks consumed in an episode.
Importantly, although evidence suggests that many students drink at levels far beyond the binge threshold, additional research suggests that the majority of alcohol-related harms on college campuses result from drinking at levels near the standard four/five-drink measure. This is related to the well-known prevention paradox in which the majority of health problems, such as alcohol-related consequences, tend to occur among those considered to be at lower risk (Rose 1985).
For a particular individual, the odds of experiencing alcohol-related harms increase as the level of consumption increases (Wechsler and Nelson 2001). However, at the population level, far fewer people drink in this manner. As a result, more total consequences occur among those who drink at relatively lower risk levels. For instance, based on data from roughly 9,000 college-student drinkers across 14 college campuses in California, Gruenewald and colleagues (2010) estimated that more than one-half of all alcohol-related consequences resulted from drinking occasions in which four or fewer drinks were consumed. Similarly, using national data from nearly 50,000 students surveyed across the four waves of the Harvard CAS, Weitzman and Nelson (2004) observed that roughly one-quarter to one-third of alcohol-related consequences, including getting injured, vandalizing property, having unprotected sex, and falling behind in school, occurred among students who usually consume three or four drinks per occasion. Such findings raise the possibility that a reduction in high peak levels of consumption might not necessarily result in large overall reductions in alcohol-related consequences on a campus. However, a reduction in high peak levels of drinking would certainly help save the lives of students who drink at these high levels.
In summary, while binge-drinking thresholds are useful for sorting students into categories based on levels of risk, a single threshold cannot adequately characterize the drinking habits of college students or the risks associated with alcohol use on college campuses (Read et al. 2008). It is not uncommon for college students to far exceed standard binge thresholds. Presently, only MTF tracks and reports the incidence of drinking beyond the binge threshold on college campuses. Such data are important as they allow for better tracking of changes in the drinking habits of students. For instance, it is possible that the number of students who drink at extreme levels could increase, whereas the overall percentage of students who binge drink declines or remains stable. Such a phenomenon might help explain why some consequences of excessive alcohol use, like overdoses requiring hospitalization, seem to be on the rise despite relatively stable levels of binge drinking on college campuses across several decades. Finally, although sorting students into binge drinking categories fails to capture high peak levels of consumption among students, a large proportion of harms actually occurs at or near the standard four or more/five or more threshold.
Do Students Know How to Define Standard Servings?
Despite concerns about the accuracy of self-report data for assessing levels of alcohol use among college students and the general population, such surveys remain the most common tool for assessing alcohol use. One major concern is whether students and other young adults are aware of what constitutes a single serving of alcohol. Research shows that college students and the general public tend to define and pour single servings of alcohol that are significantly larger than standard drinks, suggesting they might underestimate their true levels of consumption on surveys (Devos-Comby and Lange 2008; Kerr and Stockwell 2012). For instance, White and colleagues (2003, 2005) asked students to pour single servings of different types of alcohol beverages into cups of various sizes. Overall, students poured drinks that were too large. When asked to simply define standard drinks in terms of fluid ounces, students tended to overstate the number of ounces in a standard drink. The average number of ounces of liquor in student-defined mixed drinks was 4.5 ounces rather than the 1.5 ounces in actual standard drinks (White et al. 2005). When students were provided with feedback regarding discrepancies between their definitions of single servings and the actual sizes of standard drinks, they tended to revise their self-reported levels of consumption upward, leading to a significant increase in the number of students categorized as binge drinkers (White et al. 2005). Such findings suggest that students underreport their levels of consumption on surveys, raising the possibility that more students drink excessively than survey data indicate.
Although a lack of knowledge regarding standard serving sizes could lead students to underestimate, and thus underreport, how much they drink, field research suggests that the discrepancy between self-reported and actual levels of consumption might be smaller than expected from lab studies. For instance, Northcote and Livingston (2011) conducted a study in which they monitored the number of drinks consumed by research participants in bars and then asked them to report their consumption a few days later. Reports by study participants were consistent with the observations made by researchers for participants who had consumed less than eight total drinks. Only those who consumed eight drinks or more tended to underestimate their consumption. When comparing estimated blood alcohol concentrations (BAC) based on self-report to actual BAC readings in college students returning to campus from bars, actual BAC levels tended to be lower, rather than higher, than levels calculated using self-reported consumption (Kraus et al. 2005). Similarly, when actual BAC levels are compared with estimated BAC levels in bar patrons, estimates are spread evenly between accurate, underestimates, and overestimates (Clapp et al. 2009).
In short, although self-reported drinking data might not be perfect, and college students lack awareness of how standard drink sizes are defined, research does not suggest that the discrepancies between self-reported and actual drinking levels are large enough to question the general findings of college drinking surveys.
Paper-and-Pencil, Face-To-Face, and Electronic Surveys: Does It Make a Difference?
National surveys of college drinking often utilize paper-and-pencil questionnaires (e.g., MTF and Harvard CAS) or face-to-face computer-assisted personal interviews (e.g., NSDUH and NESARC). It now is possible to collect survey data electronically via the Internet and also using handheld devices, such as smartphones and personal digital assistants. This raises questions about the comparability between traditional survey methods and electronic data collection.
Several studies comparing traditional (e.g., paper and pencil) and electronic means of data collection suggest that the approaches yield generally similar results from survey participants (Boyer et al. 2002; Jones and Pitt 1999; LaBrie et al. 2006; Lygidakis et al. 2010). For instance, in a comparison of Web-based and paper-and-pencil survey approaches, Knapp and Kirk (2003) found no differences in outcomes, suggesting that Web-based surveys do not diminish the accuracy or honesty of responses. Similarly, LaBrie and colleagues (2006) observed similar outcomes of self-reported alcohol consumption in a paper-and-pencil survey and an electronic survey. However, other studies suggest that students actually feel more comfortable answering personal questions truthfully when completing questionnaires electronically (Turner et al. 1998), which can lead to higher levels of self-reported substance use and other risky behaviors. Both Lygidakis and colleagues (2010) and Wang and colleagues (2005) indicate that adolescents completing electronic surveys reported higher levels of alcohol and other drug use compared with those completing paper-and-pencil versions.
Response rate is an important consideration, with higher response rates increasing the representativeness of the sample and limiting the likelihood that response biases will influence the outcomes. Two national paper-and-pencil surveys mentioned above, MTF and Harvard CAS, report response rates for college students of approximately 59 percent. For MTF, this response rate represents a retention rate, as the participants were followed up after high school. Response rates for the in-person computer-assisted personal interviews, NSDUH and NESARC, which assess college student drinking but are not limited to college students, are roughly 77 percent and 81 percent, respectively. Currently, there is no basis for assessing response rates for national Web-based assessments of college drinking. However, smaller studies suggest that response rates might be comparable, if not higher, than other approaches. McCabe and colleagues (2002) reported that, among 7,000 undergraduate students, one-half of whom were surveyed about alcohol and other drug use via the Internet and half surveyed via paper-and-pencil surveys delivered through the mail, the response rates were 63 percent for the Web survey and 40 percent for the paper-and-pencil survey. Further, response rates for Web-based surveys can be improved by sending reminders via e-mail (van Gelder et al. 2010).
In summary, in recent years an increasing number of researchers have utilized electronic survey methods to collect college-drinking data. At present, evidence suggests that these methods can yield results quite similar to those obtained from traditional survey methods and that response rates might actually be higher.
Alcohol-Related Consequences Among College Students
Drinking to intoxication leads to widespread impairments in cognitive abilities, including decisionmaking and impulse control, and impairments in motor skills, such as balance and hand-eye coordination, thereby increasing the risk of injuries and various other harms. Indeed, research suggests that students who report “getting drunk” even just once in a typical week have a higher likelihood of being injured, experiencing falls that require medical treatment, causing injury in traffic crashes, being taken advantage of sexually, and injuring others in various ways (O’Brien et al. 2006). Students who drink with the objective of getting drunk are far more likely to experience a range of consequences, from hangovers to blackouts, than other students who drink (Boekeloo et al. 2011).
National estimates suggest that thousands of college students are injured, killed, or suffer other significant consequences each year as a result of drinking. However, researchers have questioned the manner in which such national estimates are calculated. In many cases, the lack of college identifiers in datasets means that the actual amount of annual alcohol-attributable harm that occurs among college students is unknown. Although the Harvard CAS collected data regarding the consequences of drinking, its final year of administration was 2001. Currently, assessing the damage done, on a national level, by college drinking requires estimating rates of consequences using a variety of data sources. Such assessments are complicated by the fact that outcomes considered to be negative consequences by researchers (e.g., blackouts and hangovers) are not always perceived as negative by students (Mallett et al. 2013). Further, college students often drink off campus, such as during spring breaks and summer vacations, meaning that many alcohol-related consequences experienced by college students are not necessarily associated with college itself. As such, our understanding of alcohol-related consequences among college students remains somewhat cloudy.
In one set of estimates, Hingson and colleagues (2002, 2005, 2009) utilized census data and national datasets regarding traffic crashes and other injury deaths to estimate the prevalence of various alcohol-related harms among all young people aged 18–24. Next, they attributed an amount of harm to college students equal to the proportion of all 18- to 24-year-olds who were enrolled full time in 4-year colleges (33 percent in 2005, the most recent year analyzed) (Hingson et al. 2009). Because college students drink more heavily than their non-college peers, it is possible this approach underestimated the magnitude of alcohol-related consequences on college campuses. Hingson and colleagues (2002, 2005, 2009) also used the percentage of college students who reported various alcohol-related behaviors (e.g., being assaulted by another drinking college student) in national surveys to derive national estimates of the total numbers of college students who experienced these consequences.
Based on the above strategies along with other sources of data, researchers have estimated the following rates and prevalence of alcohol-related harms involving college students:
- Death: It is possible that more than 1,800 college students between the ages of 18 and 24 die each year from alcohol- related unintentional injuries, including motor-vehicle crashes (Hingson et al. 2009).
- Injury: An estimated 599,000 students between the ages of 18 and 24 are unintentionally injured each year under the influence of alcohol (Hingson et al. 2009).
- Physical Assault: Approximately 646,000 students between the ages of 18 and 24 are assaulted each year by another student who has been drinking (Hingson et al. 2009).
- Sexual Assault: Perhaps greater than 97,000 students between the ages of 18 and 24 are victims of alcohol-related sexual assault or date rape each year (Hingson et al. 2009).
- Unsafe Sex: An estimated 400,000 students between the ages of 18 and 24 had unprotected sex and nearly 110,000 students between the ages of 18 and 24 report having been too intoxicated to know if they consented to having sex (Hingson et al. 2002).
- Health Problems: More than 150,000 students develop an alcohol-related health problem each year (Hingson et al. 2002).
- Suicide Attempts: Between 1.2 and 1.5 percent of college students indicate that they tried to commit suicide within the past year as a result of drinking or drug use (Presley et al. 1998).
- Drunk Driving: Roughly 2.7 million college students between the ages of 18 and 24 drive under the influence of alcohol each year (Hingson et al. 2009).
- Memory Loss: National estimates suggest that 10 percent of non–binge drinkers, 27 percent of occasional binge drinkers, and 54 percent of frequent binge drinkers reported at least one incident in the past year of blacking out, defined as having forgotten where they were or what they did while drinking (Wechsler et al. 2000; White 2003).
- Property Damage: More than 25 percent of administrators from schools with relatively low drinking levels and more than 50 percent from schools with high drinking levels say their campuses have a “moderate” or “major” problem with alcohol-related property damage (Wechsler et al. 1995).
- Police Involvement: Approximately 5 percent of 4-year college students are involved with the police or campus security as a result of their drinking (Wechsler et al. 2002) and an estimated 110,000 students between the ages of 18 and 24 are arrested for an alcohol-related violation such as public drunkenness or driving under the influence (Hingson et al. 2002). A more recent national study reported that 8.5 percent of students were arrested or had other trouble with the police because of drinking (Presley and Pimentel 2006).
- Alcohol Abuse and Dependence: Roughly 20 percent of college students meet the criteria for an alcohol use disorder in a given year (8 percent alcohol abuse, 13 percent alcohol dependence). Rates among age mates not in college are comparable (17 percent any alcohol use disorder, 7 percent alcohol abuse, 10 percent alcohol dependence) (Blanco et al. 2008).
With regard to assessing the number of college students who die from alcohol each year, in addition to the lack of college identifiers in datasets, another barrier is the fact that levels of alcohol often are not measured in nontraffic fatalities. As such, attributable fractions, based on analyses of existing reports in which alcohol levels were measured postmortem, are used to estimate the number of deaths by various means that likely involved alcohol. The CDC often uses attributable fractions calculated by Smith and colleagues (1999) based upon a review of 331 medical-examiner studies. An updated approach is needed. The combination of including college identifiers in medical records and measuring alcohol levels in all deaths would allow for accurate assessments of the role of alcohol in the deaths of college students and their non-college peers.
Academic Performance
About 25 percent of college students report academic consequences of their drinking, including missing class, falling behind in class, doing poorly on exams or papers, and receiving lower grades overall (Engs et al. 1996; Presley et al. 1996 a , b; Wechsler et al. 2002). Although some published research studies have not found a statistically significant association between binge drinking and academic performance (Gill 2002; Howland et al. 2010; Paschall and Freisthler 2003; Williams 2003; Wood et al. 1997), studies linking binge drinking to poorer academic performance outnumber the former studies two to one. Presley and Pimentel (2006) reported that in a national survey of college students, those who engaged in binge drinking and drank at least three times per week were 5.9 times more likely than those who drank but never binged to perform poorly on a test or project as a result of drinking (40.2 vs. 6.8 percent), 5.4 times more likely to have missed a class (64.4 vs. 11.9 percent), and 4.2 times more likely to have had memory loss (64.2 vs. 15.3 percent) (Thombs et al. 2009). Singleton and colleagues (2007, 2009), in separate prospective studies, found negative associations between heavy alcohol use and grade point average. Jennison (2004), based on a national prospective study, reported binge drinkers in college were more likely to drop out of college, work in less prestigious jobs, and experience alcohol dependence 10 years later. Wechsler and colleagues (2000) and Powell and colleagues (2004), based on the Harvard CAS, found frequent binge drinkers were six times more likely than non–binge drinkers to miss class and five times more likely to fall behind in school. White and colleagues (2002) observed that the number of blackouts, a consequence of heavy drinking, was negatively associated with grade point average (GPA). It is important to note that although data regarding GPA often are collected via self-report, the negative association between alcohol consumption and GPA holds even when official records are obtained (Singleton 2007). Collectively, the existing research suggests that heavy drinking is associated with poorer academic success in college.
Alcohol Blackouts
Excessive drinking can lead to a form of memory impairment known as a blackout. Blackouts are periods of amnesia during which a person actively engages in behaviors (e.g., walking, talking) but the brain is unable to create memories for the events. Blackouts are different from passing out, which means either falling asleep or becoming unconscious from excessive drinking. During blackouts, people are capable of participating in events ranging from the mundane, such as eating food, to the emotionally charged, such as fights and even sexual intercourse, with little or no recall (Goodwin 1995). Like milder alcohol–induced short-term memory impairments caused by one or two drinks, blackouts primarily are anterograde, meaning they involve problems with the formation and storage of new memories rather than problems recalling memories formed prior to intoxication. Further, short-term memory often is left partially intact. As such, during a blackout, an intoxicated person is able to discuss events that happened prior to the onset of the blackout and to hold new information in short-term storage long enough to have detailed conversations. They will not, however, be able to transfer new information into long-term storage, leaving holes in their memory. Because of the nature of blackouts, it can be difficult or impossible to know when a drinker in the midst of one (Goodwin 1995).
There are two general types of blackouts based on the severity of the memory impairments. Fragmentary blackouts, sometimes referred to as gray outs or brown outs, are a form of amnesia in which memory for events is spotty but not completely absent. This form is the most common. En bloc blackouts, on the other hand, represent complete amnesia for events (Goodwin 1995).
Blackouts surprisingly are common among college students who drink alcohol. White and colleagues (2002) reported that one-half (51 percent) of roughly 800 college students who had ever consumed alcohol at any point in their lives reported experiencing at least one alcohol-induced blackout, defined as awakening in the morning not able to recall things one did or places one went while under the influence. The average number of total blackouts in those who experienced them was six. Of those who had consumed alcohol during the 2 weeks before the survey was administered, 9 percent reported blacking out. Based on data from 4,539 inbound college students during the summer between high-school graduation and the start of the freshmen year, 12 percent of males and females who drank in the previous 2 weeks experienced a blackout during that time (White and Swartzwelder 2009). Data from the Harvard CAS indicate that blackouts were experienced in a 30-day period by 25 percent of students in 1993 and 27 percent of students in 1997, 1999, and 2001 (Wechsler et al. 2002). A small study by White and colleagues (2004), in which 50 students with histories of blackouts were interviewed, suggests that fragmentary blackouts are far more common than en bloc blackouts. Roughly 80 percent of students described their last blackout as fragmentary.
Blackouts tend to occur following consumption of relatively large doses of alcohol and are more likely if one drinks quickly and on an empty stomach, both of which cause a rapid rise and high peak in BAC (Goodwin 1995; Perry et al. 2006). For this reason, pregaming, or prepartying, which typically involves fast-paced drinking prior to going out to an event, increases the risk of blacking out. Labrie and colleagues (2011) reported that 25 percent of 2,546 students who engaged in prepartying experienced at least one blackout in the previous month. Playing drinking games and drinking shots were risk factors. Further, skipping meals to restrict calories on drinking days is associated with an increased risk of blackouts and other consequences (Giles et al. 2009).
Because blackouts typically follow high peak levels of drinking, it is not surprising that they are predictive of other alcohol-related consequences. Mundt and colleagues (2012) examined past-year blackouts in a sample of more than 900 students in a randomized trial of a screening and brief intervention for problem alcohol use and found that blackouts predicted alcohol-related injuries over a subsequent 2-year period. Compared with students who had no history of blackouts, those who reported one to two blackouts at baseline were 1.5 times more likely to experience an alcohol-related injury, whereas those with six or more blackouts were 2.5 times more likely. In a follow-up report based on the same sample, Mundt and Zakletskaia (2012) estimated that among study participants, one in eight emergency-department (ED) visits for alcohol-related injuries involved a blackout. On a campus of 40,000 students, this would translate into roughly $500,000 in annual costs related to blackout-associated ED visits.
In the study of 50 students with blackout histories by White and colleagues (2004), estimated peak BACs during the night of the last blackout generally were similar for males (0.30 percent) and females (0.35 percent), although it is unlikely that self-reported alcohol consumption during nights in which blackouts occur is highly accurate. A study of amnesia in people arrested for either public intoxication, driving under the influence, or underage drinking found that the probability of a fragmentary or en bloc blackout was 50/50 at a BAC of 0.22 percent and the probability of an en bloc blackout, specifically, was 50/50 at a BAC of 0.31 percent, based on breath alcohol readings (Perry et al. 2006). In their study of blackouts in college students, Hartzler and Fromme (2003 a ) noted a steep increase in the likelihood of blackouts above a BAC of 0.25 percent, calculated from self-reported consumption. Thus, from existing research, it seems that the odds of blacking out increase as BAC levels climb and that blackouts become quite common at BAC levels approaching or exceeding 0.30 percent. As such, the high prevalence of blackouts in college students points to the magnitude of excessive consumption that occurs in the college environment. It should be noted, however, that BAC levels calculated based on self-reported consumption are unlikely to be accurate given the presence of partial or complete amnesia during the drinking occasion.
It seems that some people are more sensitive to the effects of alcohol on memory than others and are therefore at increased risk of experiencing blackouts. Wetherill and Fromme (2011) examined the effects of alcohol on contextual memory in college students with and without a history of blackouts. Performance on a task was similar while the groups were sober, but students with a history of blackouts performed more poorly when intoxicated than those without a history of blackouts. Similarly, Hartzler and Fromme (2003 b ) reported that when mildly intoxicated, study participants with a history of blackouts performed more poorly on a narrative recall task than those without a history of blackouts. When performing a memory task while sober, brain activity measured with functional magnetic resonance imaging is similar in people with a history of blackouts and those without such a history (Wetherill et al. 2012). However, when intoxicated, those with a history of blackouts exhibit lower levels of activity in several regions of the frontal lobes compared with subjects without a history of blackouts.
Thus, studies suggest that there are differences in the effects of alcohol on memory and brain function between those who experience blackouts and those who do not. Research by Nelson and colleagues (2004), using data from monozygotic twins, suggests that there could be a significant genetic component to these differences. Controlling for frequency of intoxication, the researchers found that if one twin experienced blackouts, the other was more likely than chance to experience them as well. Further, Asian-American students with the aldehyde dehydrogenase ALDH2*2 allele 1 are less likely to experience blackouts than those without it, even after adjusting for maximum number of drinks consumed in a day (Lucsak et al. 2006).
1 The ALDH2*2 allele results in decreased action by the enzyme acetaldehyde dehydrogenase, which is responsible for the breakdown of acetaldehyde. The accumulation of acetaldehyde after drinking alcohol leads to symptoms of acetaldehyde poisoning, such as facial flushing and increased heart and respiration rates.
Several challenges hinder the assessment of blackouts and the events that transpire during them. Blackouts represent periods of amnesia. As such, it is difficult to imagine that self-reported drinking levels are highly accurate for nights when blackouts occur. Further, in order for a person to know what transpired during a blackout, and sometimes to be aware that a blackout occurred at all, they need to be told by other individuals. Often, the information provided by these other individuals is unreliable as they were intoxicated themselves (Nash and Takarangi 2011). Thus, it is quite likely that self-reported rates and frequencies of blackouts, drinking levels during nights in which blackouts occur, and the rates of various types of consequences that occur during them, are underestimated.
Alcohol Overdoses
When consumed in large quantities during a single occasion, such as a binge episode, alcohol can cause death directly by suppressing brain stem nuclei that control vital reflexes, like breathing and gagging to clear the airway (Miller and Gold 1991). Even a single session of binge drinking causes inflammation and transient damage to the heart (Zagrosek et al. 2010). The acute toxic effects of alcohol in the body can manifest in symptoms of alcohol poisoning, which include vomiting, slow and irregular breathing, hypothermia, mental confusion, stupor, and death (NIAAA 2007 b ; Oster-Aaland et al. 2009). Using data from the Global Burden of Disease Study, the World Health Organization (WHO) estimated that, in 2002, alcohol poisoning caused 65,700 deaths worldwide, with 2,700 poisoning deaths occurring in the United States (WHO 2009). New stories about alcohol overdoses among college students and their non-college peers have become increasingly common, a fact that is perhaps not surprising given the tendency toward excessive drinking in this age-group.
To investigate the prevalence of hospitalizations for alcohol overdoses—which stem from excessive intoxication or poisoning—among college-aged young people in the United States, White and colleagues (2011) examined rates of inpatient hospitalizations for 18- to 24-year-olds between 1999 and 2008 using data from the Nationwide Inpatient Sample, which contains hospital discharge records from roughly 20 percent of all hospitals in the country. Hospitalizations for alcohol overdoses without any other drugs involved increased 25 percent among 18- to 24-year-olds from 1999 to 2008, highlighting the risks involved in heavy drinking. In total, nearly 30,000 young people in this age-group, more males (19,847) than females (9,525) were hospitalized for alcohol overdoses with no other drugs involved in 2008. Hospitalizations for overdoses involving other drugs but not alcohol increased 55 percent over the same time period, while those involving alcohol and drugs in combination rose 76 percent. In total, there were 59,000 hospitalizations in 2008 among 18- to 24-year-olds for alcohol overdoses only or in combination with other drugs. Given that 33 percent of people in this age-group were full-time college students at 4-year colleges in 2008, a conservative estimate would suggest approximately 20,000 hospitalizations for alcohol overdoses alone or in combination with other drugs involved college students, although the exact number is not known.
Data from the Drug Abuse Warning Network (DAWN) indicate that ED visits for alcohol-related events increased in a similar fashion as those observed for inpatient hospitalizations. Among those ages 18 to 20, ED visits for alcohol-related events with no other drugs increased 19 percent, from 67,382 cases in 2005 to 82,786 cases in 2009. Visits related to combined use of alcohol and other drugs increased 27 percent, from 27,784 cases in 2005 to 38,067 cases in 2009. In 2009, 12 percent of ED visits related to alcohol involved use of alcohol in combination with other drugs (SAMHSA 2011).
Alcohol interacts with a wide variety of illicit and prescription drugs, including opioids and related narcotic analgesics, sedatives, and tranquilizers (NIAAA 2007 a ; Tanaka 2002). Importantly, BAC required for fatal overdoses are lower when alcohol is combined with prescription drugs. An analysis of 1,006 fatal poisonings attributed to alcohol alone or in combination with other drugs revealed that the median postmortem BACs in those who overdosed on alcohol alone was 0.33 percent, compared with 0.13 percent to 0.17 percent among those who overdosed on a combination of alcohol and prescription drugs (Koski et al. 2003, 2005). The combined use of alcohol and other drugs peaks in the 18- to 24-year-old age range (McCabe et al. 2006), suggesting that college-aged young adults are at particularly high risk of suffering consequences from alcohol-and-other-drug combinations.
The above findings reflect the fact that heavy consumption of alcohol quickly can become a medical emergency. One does not need to get behind the wheel of a car after drinking or jump off a balcony into a swimming pool on a dare to risk serious harm. Simply drinking too much alcohol is enough to require hospitalization and potentially cause death. Further, combining alcohol with other drugs can increase the risk of requiring medical intervention substantially. Thus, efforts to minimize the consequences of alcohol-related harms on college campuses should not lose sight of the fact that alcohol often is combined with other drugs and, when this is the case, the risks can be greater than when alcohol or drugs are used alone.
Measuring the true scope of medical treatment for alcohol overdoses among college students is difficult for several reasons. First, in datasets such as the Nationwide Emergency Department Sample (NEDS) and the Nationwide Inpatient Sample (NIS), no college identifiers are included to indicate whether a young person treated for an alcohol overdose is enrolled in college. Many schools do not track or report the number of students treated for an alcohol overdose, and many students drink excessively when away from campus. Further, schools that implement Good Samaritan or Amnesty policies, which allow students to get help for overly intoxicated peers without fear of sanctions, could create the false impression that overdoses are on the rise. For instance, after Cornell University implemented an amnesty policy, they witnessed an increase in calls to residence assistants and 911 for help dealing with an intoxicated friend (Lewis and Marchell 2006). Given the dangerous nature of alcohol overdoses, with or without other drugs involved, it is important to improve the tracking of these events at colleges and in the larger community.
Sexual Assault
Sexual assault is a pervasive problem on college campuses, and alcohol plays a central role in it. A study of roughly 5,500 college females on two campuses revealed that nearly 20 percent experienced some form of sexual assault while at college (Krebs et al. 2009). Data from the Harvard CAS suggested that 5 percent of women surveyed were raped while at college (Mohler-Kuo et al. 2004). In a national sample of students who completed the Core Alcohol and Drug Survey in 2005, 82 percent of students who experienced unwanted sexual intercourse were intoxicated at the time. Similarly, nearly three-quarters (72 percent) of respondents to the Harvard CAS study who reported being raped were intoxicated at the time. In many cases, rape victims are incapacitated by alcohol. In one study, 3.4 percent of rape victims reported being so intoxicated they were unable to consent (Mohler-Kuo et al. 2004). In a study of 1,238 college students on three campuses over a 3-year period, 6 percent of students reported being raped while incapacitated by alcohol (Kaysen et al. 2006).
Research suggests that the involvement of alcohol increases the risk of being victimized in several ways, such as by impairing perceptions that one is in danger and by reducing the ability to respond effectively to sexual aggression (Abbey 2002; McCauley et al. 2010; Testa and Livingston 2009). Further, alcohol might increase the chances that a male will commit a sexual assault by leading them to misinterpret a female’s friendly gestures or flirtation as interest in sex and by increasing sexual aggression (Abbey 2002). When asked to read a story about a potential date rape involving intoxicated college students, both male and female subjects who are intoxicated were more likely to view the female as sexually aroused and the male as acting appropriately (Abbey et al. 2003).
It is widely held that sexual assaults, with and without alcohol involvement, are underreported on college campuses. Title IX of the Education Amendments Act of 1972, a Federal civil rights law, requires universities to address sexual harassment and sexual violence. However, universities vary with regard to how they handle such cases, and a student’s perception of safety and protection can influence the likelihood of reporting a sexual assault. Indeed, many universities have indicated changes in rates of reports of assaults consistent with changes in campus policies regarding how such cases are handled. As such, although it is clear that alcohol often is involved in sexual assaults on college campuses, questions about the frequency and nature of such assaults remain.
Spring Break and 21st Birthday Celebrations— Event-Specific Drinking Occasions
More college students drink, and drink more heavily, during specific celebratory events, such as spring break and 21st birthday celebrations, than during a typical week. Spring break is a roughly weeklong recess from school that takes place in the spring at colleges throughout the United States. While some students continue to work, travel home, or simply relax, others use the opportunity to travel to beaches and other party destinations. During spring break, approximately 42 percent of students get drunk on at least 1 day, 11 percent drink to the point of blacking out or passing out, 32 percent report hangovers, and 2 percent get into trouble with the police (Litt et al. 2013). Students with a history of binge drinking and those intending to get drunk tend to drink the heaviest (Patrick et al. 2013), suggesting that prevention efforts aimed at altering students’ intentions to get drunk while on spring break might lead to a reduction in peak drinking and the consequences that follow (Mallett et al. 2013). Interestingly, students who typically are light drinkers are more likely than those who typically are binge drinkers to experience consequences from excessive drinking during spring break (Lee et al. 2009).
In addition to spring break, 21st birthday celebrations are another event-specific opportunity for students to drink excessively. An estimated 4 out of 5 college students drink alcohol to celebrate their 21st birthdays (Rutledge et al., 2008) and many students drink more than they plan. Of 150 male and female college students surveyed about their intentions to drink during their upcoming 21st birthday celebrations, 68 percent consumed more than they anticipated while only 21 percent drank less and 11 percent were accurate. On average, males intended to consume 8.5 drinks but consumed 12.5, while females expected to drink 7 but had 9 (Brister et al., 2010). As with spring-break drinking, students with a history of binge drinking and those who intended to drink heavily on their 21st birthday consumed the most (Brister et al., 2011). In one study, roughly 12 percent of students reported consuming 21 or more drinks while celebrating, and one-third of females (35 percent) and nearly half of males (49 percent) reached estimated BACs above 0.25 percent (Rutledge et al., 2008). Such high levels of consumption substantially increase the odds of sexual assaults, fights, injuries, and death (Mallett et al., 2013). Research indicates that brief interventions conducted in the week leading up to the 21st birthday celebration can reduce levels of consumption and associated consequences, suggesting that the risks of experiencing alcohol related consequences stemming from 21st birthday celebrations could be partially mitigated through specifically timed prevention efforts (Neighbors et al. 2009, 2012).
We have learned a considerable amount about the drinking habits of college students and the consequences that follow since NIAAA first reported on the matter in 1976. Surprisingly, drinking levels have remained relatively stable on and around college campuses over the last 30 years, with roughly two out of five male and female students engaging in excessive, or binge, drinking. Excessive drinking results in a wide range of consequences, including injuries, assaults, car crashes, memory blackouts, lower grades, sexual assaults, overdoses and death. Further, secondhand effects from excessive drinking place non–binge-drinking students at higher risk of injury, sexual assaults, and having their studying disrupted.
Estimates of the rates of alcohol use and related consequences are imperfect. Lack of knowledge of standard drink sizes and the effects of alcohol on memory formation all complicate the collection of accurate data from traditional self-report surveys. Underreporting of sexual assaults leads to difficulty in estimating the true extent of the problem. Lack of college identifiers in mortality records and the fact that alcohol levels are tested too infrequently in non–traffic-related deaths leaves uncertainty regarding the actual number of college students who die each year from alcohol-related causes. Similarly, college identifiers are not present in most crime reports and hospital reports.
Although it is beyond the scope of this review to examine efforts to prevent excessive drinking on college campuses, it should be noted that important strides have been made in this area (Carey et al. 2012). In addition, data from MTF suggest that levels of binge drinking are decreasing among 12th graders, particularly males. Hopefully, as our understanding of the nature of the problem continues to improve with better measurement strategies, improvements in prevention approaches combined with declines in precollege drinking will lead to reductions in both the levels of alcohol consumption by college students and the negative consequences that result.
Disclosures
The authors declare that they have no competing financial interests.
Abbey, A. Alcohol-related sexual assault: A common problem among college students. Journal of Studies on Alcohol (Suppl 14):118–128, 2002. PMID: 12022717
Abbey, A.; Buck, P.O.; Zawacki, T.; and Saenz, C. Alcohol’s effects on perceptions of a potential date rape. Journal of Studies on Alcohol 64(5):669–677, 2003. PMID: 14572189
Alexander, E.N., and Bowen, A.M. Excessive drinking in college: Behavioral outcome, not binge, as a basis for prevention. Addictive Behaviors 29(6):1199–1205, 2004. PMID: 15236823
Blanco, C.; Okuda, M.; Wright, C. et al. Mental health of college students and their non-college-attending peers: Results from the National Epidemiologic Study on Alcohol and Related Conditions. Archives of General Psychiatry 65(12):1429–1437, 2008. PMID: 19047530
Boekeloo, B.O.; Novik, M.G.; and Bush, E. Drinking to get drunk among incoming freshmen college students. American Journal of Health Education 42(2):88–95, 2011. PMID: 23440674
Boyer, K.K.; Olson, J.R.; Calatone, R.J.; and Jackson, E.C. Print versus electronic surveys: A comparison of two data collection methodologies. Journal of Operations Management 20(4):357–373, 2002.
Brister, H.A.; Wetherill, R.R.; and Fromme, K. Anticipated versus actual alcohol consumption during 21st birthday celebrations. Journal of Studies on Alcohol and Drugs 71(2):180–183, 2010. PMID: 20230714
Brown, S.A.; Tapert, S.F.; Granholm, E.; and Delis, D.C. Neurocognitive functioning of adolescents: Effects of protracted alcohol use. Alcoholism: Clinical and Experimental Research 24(2):164–171, 2000. PMID: 10698367
Butler, L.H., and Correia, C.J. Brief alcohol intervention with college student drinkers: Face-to face versus computerized feedback. Psychology of Addictive Behaviors 23(1):163–167, 2009. PMID: 19290702 .
Campbell, C.A.; Hahn, R.A.; Elder, R.; et al. The effectiveness of limiting alcohol outlet density as a means of reducing excessive alcohol consumption and alcohol-related harms. American Journal of Preventive Medicine 37(6):556–569, 2009. PMID: 19944925
Carey, K.B.; Scott-Sheldon, L.A.; Carey, M.P.; and DeMartini, K.S. Individual-level interventions to reduce college student drinking: A meta-analytic review. Addictive Behaviors 32(11):2469–2494, 2007. PMID: 17590277
Carey, K.B.; Scott-Sheldon, L.A.; Elliott, J.C.; et al. Face-to-face versus computer-delivered alcohol interventions for college drinkers: A meta-analytic review, 1998 to 2010. Clinical Psychology Review 32(8):690–703, 2012. PMID: 23022767
Carpenter, C., and Dobkin, C. The minimum legal drinking age and public health. Journal of Economic Perspectives 25(2):133–156, 2011. PMID: 21595328
Chavez, P.R.; Nelson, D.E.; Naimi, T.S.; and Brewer, R.D. Impact of a new gender-specific definition for binge drinking on prevalence estimates for women. American Journal of Preventive Medicine 40(4):468–471, 2011. PMID: 21406282
Clapp, J.D.; Johnson, M.; Voas, R.B.; et al. Reducing DUI among US college students: Results of an environmental prevention trial. Addiction 100(3):327–334, 2005. PMID: 15733246
Clapp, J.D.; Min, J.W.; Trim, R.S.; et al. Predictors of error in estimates of blood alcohol concentration: A replication. Journal of Studies on Alcohol and Drugs 70(5):683–688, 2009. PMID: 19737492
Crego, A.; Rodriguez-Holguin, S.; Parada, M., et al. Reduced anterior prefrontal cortex activation in young binge drinkers during a visual working memory task. Drug and Alcohol Dependence 109(1–3):45–56, 2010. PMID: 20079980
DeJong, W.; Schneider, S.K.; Towvim, L.G.; et al. A multisite randomized trial of social norms marketing campaigns to reduce college student drinking. Journal of Studies on Alcohol 67(6):868–879, 2006. PMID: 17061004
DeJong, W.; Schneider, S.K.; Towvim, L.G.; et al. A multisite randomized trial of social norms marketing campaigns to reduce college student drinking: A replication failure. Substance Abuse 30(2):127–140, 2009. PMID: 19347752
Devos-Comby, L., and Lange, JjE. “My drink is larger than yours”? A literature review of self-defined drink sizes and standard drinks. Current Drug Abuse Reviews 1(2):162–176, 2008. PMID: 19630715
Elder, R.W.; Lawrence, B.; Ferguson, A.; et al. The effectiveness of tax policy interventions for reducing excessive alcohol consumption and related harms. American Journal of Preventive Medicine 38(2):217–229, 2010. PMID: 20117579
Elliott, J.C.; Carey, K.B.; and Bolles, J.R. Computer-based interventions for college drinking: A qualitative review. Addictive Behaviors 33(8):994–1005, 2008. PMID: 18538484
Engs, R.C.; Diebold, B.A.; and Hanson, D.J. The drinking patterns and problems of a national sample of college students, 1994. Journal of Alcohol and Drug Education 41:13–33, 1996.
Fell, J.C.; Fisher, D.A.; Voas, R.B.; et al. The impact of underage drinking laws on alcohol- related fatal crashes of young drivers. Alcoholism: Clinical and Experimental Research 33(7):1208–1219, 2009. PMID: 19389192
Fleming, M.F.; Balousek, S.L.; Grossberg, P.M.; et al. Brief physician advice for heavy drinking college students: A randomized controlled trial in college health clinics. Journal of Studies on Alcohol and Drugs 71(1):23–31, 2010. PMID: 20105410
Giles, S.M.; Champion, H.; Sutfin, E.L.; et al. Calorie restriction on drinking days: An examination of drinking consequences among college students. Journal of American College Health 57(6):603–609, 2009. PMID: 19433398
Gill, J.S. Reported levels of alcohol consumption and binge drinking within the UK undergraduate student population over the last 25 years. Alcohol and Alcoholism 37(2):109–120, 2002. PMID: 11912065
Goodwin, D.W. Alcohol amnesia. Addiction 90(3):315–317, 1995. PMID: 7735016
Hanson, K.L.; Medina, K.L.; Padula, C.B.; et al. Impact of adolescent alcohol and drug use on neuropsychological functioning in young adulthood: 10-year outcomes. Journal of Child & Adolescent Substance Abuse 20(2):135–154, 2011. PMID: 21532924
Hartzler, B., and Fromme, K. Fragmentary and en bloc blackouts: Similarity and distinction among episodes of alcohol-induced memory loss. Journal of Studies on Alcohol 64(4):547–550, 2003 a . PMID: 12921196
Hartzler, B., and Fromme, K. Fragmentary blackouts: Their etiology and effect on alcohol expectancies. Alcoholism: Clinical and Experimental Research 27(4):628–637, 2003 b . PMID: 12711925
Hingson, R.W.; Heeren, T.; Edwards, E.M.; and Saitz, R. Young adults at risk for excess alcohol consumption are often not asked or counseled about drinking alcohol. Journal of General Internal Medicine 27(2):179–184, 2012. PMID: 21935753
Hingson, R.; Heeren, T.; and Winter, M. Lower legal blood-alcohol limits for young drivers. Public Health Reports 109(6):738–744, 1994. PMID: 7800781
Hingson, R.; Heeren, T.; Winter, M.R.; and Wechsler, H. Early age of first drunkenness as a factor in college students’ unplanned and unprotected sex attributable to drinking. Pediatrics 111(1):34–41, 2003 a . PMID: 12509551
Hingson, R.; Heeren, T.; Winter, M.; and Wechsler, H. Magnitude of alcohol-related mortality and morbidity among U.S. college students ages 18-24: Changes from 1998 to 2001. Annual Review of Public Health 26: 259–279, 2005 a . PMID: 15760289
Hingson, R.; Heeren, T.; Zakocs, R., et al. Age of first intoxication, heavy drinking, driving after drinking and risk of unintentional injury among U.S. college students. Journal of Studies on Alcohol 64(1):23–31, 2003 b . PMID: 12608480
Hingson, R.; Heeren, T.; Zakocs, R.; et al. Magnitude of alcohol-related mortality and morbidity among U.S. college students ages 18-24. Journal of Studies on Alcohol 63(2): 136–144, 2002. PMID: 12033690
Hingson, R.; McGovern, T.; Howland, J.; et al. Reducing alcohol-impaired driving in Massachusetts: The Saving Lives Program. American Journal of Public Health 86(6):791–797, 1996. PMID: 8659651
Hingson, R., and White, A. Magnitude and prevention of college alcohol and drug misuse: U.S. college students ages 18-24. In: Kay, J., and Schwartz, V., Eds. Mental Health Care in the College Community. London: John Wiley & Sons, 2010, pp. 289–324.
Hingson, R.W.; Zakocs, R.C.; Heeren, T.; et al. Effects on alcohol related fatal crashes of a community based initiative to increase substance abuse treatment and reduce alcohol availability. Injury Prevention 11(2):84–90, 2005 b . PMID: 15805436
Hingson, R.; Zha, W.; and Weitzman, E.R. Magnitude of and trends in alcohol-related mortality and morbidity among U.S. college students ages 18-24, 1998-2005. Journal of Studies on Alcohol and Drugs (Suppl. 16):12–20, 2009. PMID: 19538908
Holder, H.D.; Gruenewald, P.J.; Ponicki, W.R.; et al. Effect of community-based interventions on high-risk drinking and alcohol-related injuries. JAMA: Journal of the American Medical Association 284(18):2341–2347, 2000. PMID: 11066184
Howland, J.; Rohsenow, D.J.; Greece, J.A.; et al. The effects of binge drinking on college students’ next-day academic test-taking performance and mood state. Addiction 105(4):655–665, 2010. PMID: 20403018
Ichiyama, M.A.; Fairlie, A.M.; Wood, M.D.; et al. A randomized trial of a parent-based intervention on drinking behavior among incoming college freshmen. Journal of Studies on Alcohol and Drugs (Suppl. 16):67–76, 2009. PMID: 19538914
Jennison, K.M. The short-term effects and unintended long-term consequences of binge drinking in college: A 10-year follow-up study. American Journal of Drug and Alcohol Abuse 30(3):659–684, 2004. PMID: 15540499
Johnston, L.D.; O’Malley, P.M.; and Bachman, J.G. Monitoring the Future National Survey Results on Drug Use, 1975–2000. Volume I: Secondary School Students. NIH Publication No. 01–4924. Bethesda, MD: National Institute on Drug Abuse, 2001 a .
Johnston L.D.; O’Malley, P.M.; and Bachman, J.G. Monitoring the Future National Survey Results on Drug Use,1975–2000. Volume II: College Students and Adults Ages 19–40. NIH Publication No. 01–4925. Bethesda, MD: National Institute on Drug Abuse, 2001 b .
Johnston, L.D.; O’Malley, P.M.; Bachman, J.G.; and Schulenberg, J.E. Monitoring the Future National Survey Results on Drug Use, 1975–2006. Volume II: College Students and Adults Ages 19–45. NIH Publication No. 07–6206. Bethesda, MD: National Institute on Drug Abuse, 2007.
Johnston, L.D.; O’Malley, P.M.; Bachman, J.G.; and Schulenberg, J.E. Monitoring the Future National Survey Results on Drug Use, 1975–2011. Volume II: College Students and Adults Ages 19–50. Ann Arbor: Institute for Social Research, the University of Michigan, 2012.
Jones, R., and Lacey, J. Alcohol and Highway Safety 2001: A Review of the State of Knowledge . Report No. DOT HS–809–383. Washington, D.C.: National Highway Traffic Safety Administration, 2001.
Jones, R., and Pitt, N. Health surveys in the workplace: Comparison of postal, email and World Wide Web methods. Occupational Medicine (London) 49(8):556–558, 1999. PMID: 10658310
Kaysen, D.; Neighbors, C.; Martell, J.; et al. Incapacitated rape and alcohol use: A prospective analysis. Addictive Behaviors 31(10):1820–1832, 2006. PMID: 16446044
Kerr, W.C.; and Stockwell, T. Understanding standard drinks and drinking guidelines. Drug and Alcohol Review 31(2):200–205, 2012. PMID: 22050262
Knight, J.R.; Wechsler, H.; Kuo, M.; et al. Alcohol abuse and dependence among U.S. college students. Journal of Studies on Alcohol 63(3):263–270, 2002. PMID: 12086126
Koski, A.; Ojanperä, I.; and Vuori, E. Interaction of alcohol and drugs in fatal poisonings. Human & Experimental Toxicology 22(5):281–287, 2003. PMID: 12774892
Koski, A,; Vuroi, E.; and Ojanperä, I. Relation of postmortem blood alcohol and drug concentrations in fatal poisonings involving amitriptyline, propoxyphene and promazine. Human & Experimental Toxicology 24(8):389–396, 2005. PMID: 16138729
Kraus, C.L.; Salazar, N.C.; Mitchell, J.R.; et al. Inconsistencies between actual and estimated blood alcohol concentrations in a field study of college students: Do students really know how much they drink? Alcoholism: Clinical and Experimental Research 29(9):1672–1676, 2005. PMID: 16205367
Krebs, C.P.; Lindquist, C.H.; Warner, T.D.; et al. College women’s experiences with physically forced, alcohol- or drug-enabled, and drug-facilitated sexual assault before and since entering college. Journal of American College Health 57(6):639–647, 2009. PMID: 19433402
LaBrie, J.; Earleywine, M.; Lamb, T.; and Shelesky, K. Comparing electronic-keypad responses to paper-and-pencil questionnaires in group assessments of alcohol consumption and related attitudes. Addictive Behaviors 31(12):2334-2338, 2006. PMID: 16626878
LaBrie, J.W.; Huchting, K.; Tawalbeh, S.; et al. A randomized motivational enhancement prevention group reduces drinking and alcohol consequences in first-year college women. Psychology of Addictive Behaviors 22(1):149–155, 2008. PMID: 18298242
LaBrie, J.W.; Hummer, J.; Kenney, S.; et al. Identifying factors that increase the likelihood for alcohol-induced blackouts in the prepartying context. Substance Use & Misuse 46(8):992–1002, 2011. PMID: 21222521
Larimer, M.E., and Cronce, J.M. Identification, prevention and treatment: A review of individual-focused strategies to reduce problematic alcohol consumption by college students. Journal of Studies on Alcohol (Suppl. 14):148–163, 2002. PMID: 12022721
Larimer, M.E., and Cronce, J.M. Identification, prevention, and treatment revisited: Individual-focused college drinking prevention strategies 1999-2006. Addictive Behaviors 32(11):2439–2468, 2007. PMID: 17604915
Lee, C.M.; Lewis, M.A.; and Neighbors, C. Preliminary examination of spring break alcohol use and related consequences. Psychology of Addictive Behaviors 23(4):689–694, 2009. PMID: 20025375
Liang, L., and Huang, J. Go out or stay in? The effects of zero tolerance laws on alcohol use and drinking and driving patterns among college students. Health Economics 17(11):1261–1275, 2008. PMID: 18219708
Litt, D.M.; Lewis, M.A.; Patrick, M.E.; et al. Spring break versus spring broken: Predictive utility of spring break alcohol intentions and willingness at varying levels of extremity. Prevention Science , 2013 Feb 13. [Epub ahead of print]. PMID: 23404667
Luczak, S.E.; Shea, S.H.; Hsueh, A.C.; et al. ALDH2*2 is associated with a decreased likelihood of alcohol-induced blackouts in Asian American college students. Journal of Studies on Alcohol 67(3):349–353, 2006. PMID: 16608143
Lygidakis, C.; Rigon, S.; Cambiaso, S.; et al. A web-based versus paper questionnaire on alcohol and tobacco in adolescents. Telemedicine Journal and E-Health 16(9):925– 930, 2010. PMID: 20958200
Mallett, K.A.; Varvil-Weld, L.; Borsari, B.; et al. An update of research examining college student alcohol-related consequences: New perspectives and implications for interventions. Alcoholism: Clinical and Experimental Research 37(5):709–716, 2013. PMID: 23241024
McCabe, S.E.; Cranford, J.A; and Boyd, C.J. The relationship between past-year drinking behaviors and nonmedical use of prescription drugs: Prevalence of co-occurrence in a national sample. Drug and Alcohol Dependence 84(3):281–288, 2006. PMID: 16621337
McCartt, A.T.; Hellinga, L.A.; and Wells, J.K. Effects of a college community campaign on drinking and driving with a strong enforcement component. Traffic Injury Prevention 10(2):141–147, 2009. PMID: 19333826
McCauley, J.L.; Calhoun, K.S.; and Gidycz, C.A. Binge drinking and rape: A prospective examination of college women with a history of previous sexual victimization. Journal of Interpersonal Violence 25(9):1655–1668, 2010. PMID: 20068115
Medina, K.L.; McQueeny, T.; Nagel, B.J.; et al. Prefrontal cortex volumes in adolescents with alcohol use disorders: Unique gender effects. Alcoholism: Clinical and Experimental Research 32(3):386–394, 2008. PMID: 18302722
Meilman, P.W.; Leichliter, J.S.; and Presley, C.A. Greeks and athletes: Who drinks more? Journal of American College Health 47(4):187–190, 1999. PMID: 9919850
Meilman, P.W.; Presley, C.A.; and Cashin, J.R. The sober life at the historically black colleges. Journal of Blacks in Higher Education 9:98–100, 1995.
Meilman, P.W.; Presley, C.A.; and Lyerla, R. Black college students and binge drinking. Journal of Blacks in Higher Education 8:70–71, 1994.
Miller, N.S.; and Gold, M.S. Alcohol. New York: Plenum Publishing Company, 1991.
Miron, J.A., AND Tetelbaum, E. Does the minimum legal drinking age save lives? Economic Inquiry 47(2):317–336, 2009.
Mohler-Kuo, M.; Dowdall, G.B.; Koss, M.P.; and Wechsler, H. Correlates of rape while intoxicated in a national sample of college women. Journal of Studies on Alcohol 65(1):37–45, 2004. PMID: 15000502
Moreira, M.T.; Smith, L.A.; and Foxcroft, D. Social norms interventions to reduce alcohol misuse in university or college students. Cochrane Database of Systematic Reviews (Online) (3):CD006748, 2009. PMID: 19588402
Mundt, M.P.; and Zakletskaia, L.I. Prevention for college students who suffer alcohol-induced blackouts could deter high-cost emergency department visits. Health Affairs (Millwood) 31(4):863–870, 2012.
Mundt, M.P.; Zakletskaia, L.I.; Brown, D.D.; and Fleming, .MF. Alcohol-induced memory blackouts as an indicator of injury risk among college drinkers. Injury Prevention 18(1):44–49, 2012. PMID: 21708813
Naimi, T.S.; Nelson, D.E.; and Brewer, R.D. The intensity of binge alcohol consumption among U.S. adults. American Journal of Preventive Medicine 38(2):201–207, 2010. PMID: 20117577
Nash, R.A., and Takarangi, M.K. Reconstructing alcohol-induced memory blackouts. Memory 19(6):566–573, 2011. PMID: 21919584
National Institute on Alcohol Abuse and Alcoholism (NIAAA). Alcohol Policy Information System, 2010. Available at http://www.alcoholpolicy.niaaa.nih.gov/ . Accessed February 16, 2010.
NIAAA. NIAAA Newsletter, Winter 2004, Number 3. Bethesda, MD: National Institutes of Health, U.S. Department of Health and Human Services (DHHS), 2004. Available at: http://pubs.niaaa.nih.gov/publications/Newsletter/winter2004/Newsletter_Number3.pdf
NIAAA. Harmful Interactions: Mixing Alcohol with Medicines. Bethesda, MD: National Institutes of Health, U.S. Department of Health and Human Services (DHHS), revised 2007 a (NIH Publication No. 07-5329). Available at: http://pubs.niaaa.nih.gov/publications/Medicine/medicine.htm
NIAAA. Parents – Spring Break Is Another Important Time to Discuss College Drinking. Bethesda, MD: National Institutes of Health, DHHS, 2007 b (NIH Publication No. 05-5642).
NIAAA. Task Force of the National Advisory Council on Alcohol Abuse and Alcoholism. A Call to Action: Changing the Culture of Drinking at U.S. Colleges. Bethesda, MD: National Institutes of Health, U.S. Department of Health and Human Services (DHHS), 2002 (NIH Publication No. 02–5010).
NIAAA. What Colleges Need to Know Now: An Update on College Drinking Research. Bethesda, MD: National Institutes of Health, U.S. Department of Health and Human Services (DHHS), 2007 c (NIH Publication No. 07–5010).
National Research Council Institute of Medicine of the National Academies. Reducing Underage Drinking: A Collective Responsibility. Washington, DC: The National Academies Press, 2004.
Neighbors, C.; Lee, C.M.; Lewis, M.A.; et al. Internet-based personalized feedback to reduce 21st-birthday drinking: A randomized controlled trial of an event-specific prevention intervention. Journal of Consulting and Clinical Psychology 77(1):51–63, 2009. PMID: 19170453
Neighbors, C.; Lee, C.M.; Atkins, D.C.; et al. A randomized controlled trial of event-specific prevention strategies for reducing problematic drinking associated with 21st birthday celebrations. Journal of Consulting and Clinical Psychology 80(5):850–862, 2012. PMID: 22823855
Nelson, E.C.; Heath, A.C.; Bucholz, K.K.; et al. Genetic epidemiology of alcohol-induced blackouts. Archives of General Psychiatry 61(3):257–263, 2004. PMID: 14993113
Norberg, K.E.; Bierut, L.J.; and Grucza, R.A. Long-term effects of minimum drinking age laws on past-year alcohol and drug use disorders. Alcoholism: Clinical and Experimental Research 33(12):2180–2190, 2009. PMID: 19775322
Northcote, J., and Livingston, M. Accuracy of self-reported drinking: Observational verification of ‘last occasion’ drink estimates of young adults. Alcohol and Alcoholism 46(6):709–713, 2011. PMID: 21949190
O’Brien, M.C.; McCoy, T.P.; Champion, H.; et al. Single question about drunkenness to detect college students at risk for injury. Academic Emergency Medicine 13(6):629– 636, 2006. PMID: 16614453
O’Hare, T.M. Drinking in college: Consumption patterns, problems, sex differences and legal drinking age. Journal of Studies on Alcohol 51(6):536–541, 1990. PMID: 2270062
Oster-Aaland, L.; Lewis, M.A.; Neighbors, C.; et al. Alcohol poisoning among college students turning 21: Do they recognize the symptoms and how do they help? Journal of Studies on Alcohol and Drugs (Suppl 16):122–130, 2009. PMID: 19538920
Parada, M.; Corral, M.; Caamaño-Isorna, F.; et al. Binge drinking and declarative memory in university students. Alcoholism: Clinical and Experimental Research 35(8):1475– 1484, 2011. PMID: 21575014
Parada, M.; Corral, M.; Mota, N. et al. Executive functioning and alcohol binge drinking in university students. Addictive Behaviors 37(2):167–172, 2012. PMID: 21996093
Paschall, M.J.; Antin, T.; Ringwalt, C.L.; and Saltz, R.F. Effects of AlcoholEdu for College on alcohol-related problems among freshmen: A randomized multicampus trial. Journal of Studies on Alcohol and Drugs 72(4):642–650, 2011 a . PMID: 21683046
Paschall, M.J.; Antin, T.; Ringwalt, C.L.; and Saltz, R.F. Evaluation of an internet-based alcohol misuse prevention course for college freshmen: Findings of a randomized multi-campus trial. American Journal of Preventive Medicine 41(3):300–308, 2011 b . PMID: 21855745
Paschall, M.J., and Freisthler, B. Does heavy drinking affect academic performance in college? Findings from a prospective study of high achievers. Journal of Studies on Alcohol 64(4):515–519, 2003. PMID: 12921193
Patrick, M.E.; Lewis, M.A.; Lee, C.M.; and Maggs, J.L. Semester and event-specific motives for alcohol use during Spring Break: Associated protective strategies and negative consequences. Addictive Behaviors 38(4):1980–1987, 2013. PMID: 23384451
Perry, P.J.; Argo, T.R.; Barnett, M.J.; et al. The association of alcohol-induced blackouts and grayouts to blood alcohol concentrations. Journal of Forensic Sciences 51(4):896– 899, 2006. PMID: 16882236
Powell, L.A.; Williams, J.; and Wechsler, H. Study habits and the level of alcohol use among college students. Education Economics 12(2):135–149, 2004.
Presley, C.A.; Leichliter, J.S.; and Meilman, P.W. Alcohol and Drugs on American College Campuses: A Report to College Presidents. Third in a Series: 1995, 1996, and 1997 , Carbondale, IL: Core Institute, Southern Illinois University, 1998.
Presley, C.A.; Meilman, P.W.; and Cashin, J.R. Alcohol and Drugs on American College Campuses: Use, Consequences, and Perceptions of the Campus Environment. Volume IV: 1992-94. Carbondale, IL: The Core Institute, 1996 a .
Presley, C.A.; Meilman, P.W.; Cashin, J.R.; and Lyera, R. Alcohol and Drugs on American College Campuses: Use, Consequences, and Perceptions of the Campus Environment. Volume III: 1991-93. Carbondale, IL: The Core Institute, 1996 b .
Presley, C.A.; Meilman, P.W., and Leichliter, J.S. College factors that influence drinking. Journal of Studies on Alcohol (Suppl 14):82–90, 2002. PMID: 12022732
Presley, C.A., and Pimentel, E.R. The introduction of the heavy and frequent drinker: A proposed classification to increase accuracy of alcohol assessments in postsecondary educational settings. Journal of Studies on Alcohol 67(2):324–331, 2006. PMID: 16562416
Preusser, D.; Ulmer, R.; and Preisser, C. Obstacles to Enforcement of Youthful (Under 21) Impaired Driving. Washington, DC: National Highway Traffic Safety Administration, 1992 (DOT HS 807–878).
Read, J.P.; Beattie, M.; Chamberlain, R.; and Merrill, J.E. Beyond the “Binge” threshold: Heavy drinking patterns and their association with alcohol involvement indices in college students. Addictive Behaviors 33(2):225–234, 2008. PMID: 17997047
Reboussin, B.A.; Song, E.Y.; and Wolfson, M. The impact of alcohol outlet density on the geographic clustering of underage drinking behaviors within census tracts. Alcoholism: Clinical and Experimental Research 35(8):1541–1549, 2011. PMID: 21463343
Rutledge, P.C.; Park, A.; and Sher, K.J. 21st birthday drinking: Extremely extreme. Journal of Consulting and Clinical Psychology 76(3):511–516, 2008. PMID: 18540744
Saltz, R.F.; Welker, L.R.; Paschall, M.J.; et al. Evaluating a comprehensive campus-community prevention intervention to reduce alcohol-related problems in a college population. Journal of Studies on Alcohol and Drugs (Suppl. 16):21–27, 2009. PMID: 19538909
Schaus, J.F.; Sole, M.L.; McCoy, T.P.; et al. Alcohol screening and brief intervention in a college student health center: A randomized controlled trial. Journal of Studies on Alcohol and Drugs (Suppl. 16):131–141, 2009. PMID: 19538921
Schulenberg, J.; Maggs, J.L.; Long, S.W.; et al. The problem of college drinking: Insights from a developmental perspective. Alcoholism: Clinical and Experimental Research 25(3):473–477, 2001. PMID: 11290861
Schweinsburg, A.D.; McQueeny, T.; Nagel, B. J.; et al. A preliminary study of functional magnetic resonance imaging response during verbal encoding among adolescent binge drinkers. Alcohol 44(1):111–117, 2010. PMID: 20113879
Scribner, R.A.; Mason, K.E.; Simonsen, N.R.; et al. An ecological analysis of alcohol outlet density and campus-reported violence at 32 U.S. colleges. Journal of Studies on Alcohol and Drugs 71(2):184–191, 2010. PMID: 20230715
Scribner, R.; Mason, K.; Theall, K.; et al. The contextual role of alcohol outlet density in college drinking. Journal of Studies on Alcohol and Drugs 69(1):112–120, 2008. PMID: 18080071
Scribner, R.A.; Theall, K.P.; Mason, K.; et al. Alcohol prevention on college campuses: The moderating effect of the alcohol environment on the effectiveness of social norms marketing campaigns. Journal of Studies on Alcohol and Drugs 72(2):232-239, 2011. PMID: 21388596
Shults, R.A.; Elder, R.W.; Sleet, D.A.; et al. Reviews of evidence regarding interventions to reduce alcohol-impaired driving. American Journal of Preventive Medicine 21(Suppl. 4):66-88, 2001. PMID: 11691562
Singleton, R.A. Collegiate alcohol consumption and academic performance. Journal of Studies on Alcohol and Drugs 68(4):548–555, 2007. PMID: 17568960
Singleton, R.A. Jr., and Wolfson, A.R. Alcohol consumption, sleep, and academic performance among college students. Journal of Studies on Alcohol and Drugs 70(3):355– 363, 2009. PMID: 19371486
Smith, G.S.; Branas, C.C.; and Miller, T.R. Fatal nontraffic injuries involving alcohol: A metaanalysis. Annals of Emergency Medicine 33(6):659–668, 1999. PMID: 10339681
Squeglia, L.M.; Spadoni, A.D.; Infante, M.A.; et al. Initiating moderate to heavy alcohol use predicts changes in neuropsychological functioning for adolescent girls and boys. Psychology of Addictive Behaviors 23(4):715–722, 2009. PMID: 20025379
Squeglia, L.M.; Sorg, S.F.; Schweinsburg, A.D.; et al. Binge drinking differentially affects adolescent male and female brain morphometry. Psychopharmacology (Berlin) 220(3):529–539, 2012. PMID: 21952669
Straus, R., and Bacon, S. D. (1953). Drinking in college. New Haven, CT: Yale University Press.
Substance Abuse and Mental Health Services Administration (SAMHSA). The DAWN Report: Trends in Emergency Department Visits Involving Underage Alcohol Use: 2005 to 2009. Rockville, MD, Substance Abuse and Mental Health Services Administration, 2011.
Substance Abuse and Mental Health Services Administration (SAMHSA). Results from the 2001 National Household Survey on Drug Abuse: Volume 1: Summary of National Findings. Rockville, MD: Substance Abuse and Mental Health Services Administration, 2002 (DHHS Publication No. SMA 02–3758, 2002).
Substance Abuse and Mental Health Services Administration (SAMHSA). Results from the 2005 National Survey on Drug Use and Health: National Findings. Rockville, MD: Substance Abuse and Mental Health Services Administration, 2006 (DHHS Publication No. SMA 06–4194).
Substance Abuse and Mental Health Services Administration (SAMHSA). Results from the 2007 National Survey on Drug Use and Health: National Findings. Rockville, MD: Substance Abuse and Mental Health Services Administration, 2008 (NSDUH Series H-34, DHHS Publication No. SMA 08–4343).
Substance Abuse and Mental Health Services Administration (SAMHSA). Summary of Findings of the 1999 National Household Survey on Drug Abuse. Rockville, MD: Substance Abuse and Mental Health Services Administration, 2000 (DHHS Publication No. SMA 00–3466).
Tanaka, E. Toxicological interactions between alcohol and benzodiazepines. Journal of Toxicology. Clinical Toxicology 40(1):69–75, 2002. PMID: 11990206
Testa, M., and Livingston, J.A. Alcohol consumption and women’s vulnerability to sexual victimization: Can reducing women’s drinking prevent rape? Substance Use & Misuse 44(9-10):1349–1376, 2009. PMID: 19938922
Thombs, D.L.; Olds, R.S.; Bondy, S.J.; et al. Undergraduate drinking and academic performance: A prospective investigation with objective measures. Journal of Studies on Alcohol and Drugs 70(5):776–785, 2009. PMID: 19737503
Timberlake, D.S.; Hopfer,C.J.; Rhee, S.H.; et al. College attendance and its effect on drinking behaviors in a longitudinal study of adolescents. Alcoholism: Clinical and Experimental Research 31(6):1020–1030, 2007. PMID: 17403064
Treno, A.J.; Gruenewald P.J.; Lee, J.P.; and Remer, L.G. The Sacramento Neighborhood Alcohol Prevention Project: Outcomes from a community prevention trial. Journal of Studies on Alcohol and Drugs 68(2):197–207, 2007. PMID: 17286338
Turner, C.F.; Ku, L.; Rogers, S.M.; et al. Adolescent sexual behavior, drug use, and violence: Increased reporting with computer survey technology. Science 280(5365):867– 873, 1998. PMID: 9572724
Turrisi, R.; Larimer, M.E.; Mallett, K.A.; et al. A randomized clinical trial evaluating a combined alcohol intervention for high-risk college students. Journal of Studies on Alcohol and Drugs 70(4):555–567, 2009. PMID: 19515296
Upcraft, M.L. Today’s First-Year Students and Alcohol. Paper prepared for the Task Force on College Drinking, National Advisory Council on Alcohol Abuse and Alcoholism, Bethesda, MD, 2000.
Varvil-Weld, L.; Mallett, K.A.; Turrisi, R.; et al. Are certain college students prone to experiencing excessive alcohol-related consequences? Predicting membership in a high-risk subgroup using pre-college profiles. Journal of Studies on Alcohol and Drugs 74(4):542–551, 2013. PMID: 23739017
Voas, R.B., and Williams, A.F. Age differences of arrested and crash-involved drinking drivers. Journal of Studies on Alcohol 47(3):244–248, 1986. PMID: 3724162
Voas, R.B.; Tippetts, A.S.; and Fell, J. The relationship of alcohol safety laws to drinking drivers in fatal crashes. Accident Analysis and Prevention 32(4):483–492, 2000. PMID: 10868751
Wagenaar, A.C., and Toomey, T.L. Effects of minimum drinking age laws: Review and analyses of the literature from 1960 to 2000. Journal of Studies on Alcohol (Suppl. 14):206–225, 2002. PMID: 12022726
Wagenaar, A.C.; Murray, D.M.; and Toomey T.L. Communities Mobilizing for Change on Alcohol (CMCA): Effects of a randomized trial on arrests and traffic crashes. Addiction 95(2):209–217, 2000. PMID: 10723849
Wagenaar, A.C.; O’Malley, P.M.; and LaFond, C. Lowered legal blood alcohol limits for young drivers: Effects on drinking, driving, and driving-after-drinking behaviors in 30 states. American Journal of Public Health 91(5):801–804, 2001. PMID: 11344892
Wagenaar, A.C.; Salois, M.J.; and Komro, K.A. Effects of beverage alcohol price and tax levels on drinking: A meta-analysis of 1003 estimates from 112 studies. Addiction 104(2):179–190, 2009. PMID: 19149811
Wagenaar, A.C.; Erickson, D.J.; Harwood, E.M.; and O’Malley, P.M. Effects of state coalitions to reduce underage drinking: A national evaluation. American Journal of Preventive Medicine 31(4):307–315, 2006. PMID: 16979455
Wang, Y.C.; Lee, C.M; Lew-Ting, C.Y.; et al. Survey of substance use among high school students in Taipei: Web-based questionnaire versus paper-and-pencil questionnaire. Journal of Adolescent Health 37(4):289–295, 2005. PMID: 16182139
Wechsler, H.; Davenport, A.; Dowdall, G.; et al. Health and behavioral consequences of binge drinking in college: A national survey of students at 140 campuses. JAMA: Journal of the American Medical Association 272(21):1672–1677, 1994. PMID: 7966895
Wechsler, H.; Davenport, A.E.; Dowdall, G.W.; et al. Binge drinking, tobacco, and illicit drug use and involvement in college athletics. A survey of students at 140 American colleges. Journal of American College Health 45(5):195–200, 1997. PMID: 9069676
Wechsler, H.; Dowdall, G.W.; Davenport, A.; and Castillo, S. Correlates of college student binge drinking. American Journal of Public Health 85(7):921–926, 1995. PMID: 7604914
Wechsler, H.; Dowdall, G.W.; Davenport, A.; and Rimm, E.B. A gender-specific measure of binge drinking among college students. American Journal of Public Health 85(7):982– 985, 1995. PMID: 7604925
Wechsler, H.; Dowdall, G.W.; Maenner, G.; et al. Changes in binge drinking and related problems among American college students between 1993 and 1997. Results of the Harvard School of Public Health College Alcohol Study. Journal of American College Health 47(2):57–68, 1998. PMID: 9782661
Wechsler, H., and Kuo, M. Watering down the drinks: The moderating effect of college demographics on alcohol use of high-risk groups. American Journal of Public Health, 93(11):1929–1933, 2003. PMID: 14600068
Wechsler, H.; Kuh, G.; and Davenport, A.E. Fraternities, sororities and binge drinking: Results from a national study of American colleges. NASPA Journal 46(3):395–416, 2009.
Wechsler, H.; Lee, J.E.; Kuo, M., et al. Trends in college binge drinking during a period of increased prevention efforts. Findings from 4 Harvard School of Public Health College Alcohol Study surveys: 1993-2001. Journal of American College Health 50(5):203– 217, 2002. PMID: 11990979
Wechsler, H.; Lee, J.E.; Kuo, M.; and Lee, H. College binge drinking in the 1990s: A continuing problem. Results of the Harvard School of Public Health 1999 College Alcohol Survey. Journal of American College Health 48(5):199–210, 2000. PMID: 10778020
Wechsler, H., and Nelson, T.F. What we have learned from the Harvard School of Public Health College Alcohol Study: Focusing attention on college student alcohol consumption and the environmental conditions that promote it. Journal of Studies on Alcohol and Drugs 69(4): 481–490, 2008. PMID: 18612562
Wechsler, H., and Nelson, T. F. Binge drinking and the American college students: What’s five drinks? Psychology of Addictive Behaviors, 15(4), 287–291, 2001. PMID: 11767258
Weitzman, E.R.; Folkman, A; Folkman, M.P.; and Wechsler, H. The relationship of alcohol outlet density to heavy and frequent drinking and drinking-related problems among college students at eight universities. Health & Place 9(1):1–6, 2003. PMID: 12609468
Wetherill, R.R., and Fromme, K. Acute alcohol effects on narrative recall and contextual memory: An examination of fragmentary blackouts. Addictive Behaviors 36(8):886– 889, 2011. PMID: 21497445
Wetherill, R.R.; Schnyer, D.M.; and Fromme, K. Acute alcohol effects on contextual memory BOLD response: Differences based on fragmentary blackout history. Alcoholism: Clinical and Experimental Research 36(6):1108–1115, 2012. PMID: 22420742
White, A.M. What happened? Alcohol, memory blackouts, and the brain. Alcohol Research & Health 27(2):186-196, 2003. PMID: 15303630
White, A.M.; Hingson, R.W.; Pan, I.J.; and Yi, H.Y. Hospitalizations for alcohol and drug overdoses in young adults ages 18-24 in the United States, 1999-2008: Results from the Nationwide Inpatient Sample. Journal of Studies on Alcohol and Drugs 72(5):774– 786, 2011. PMID: 21906505
White, A.M.; Jamieson-Drake, D.W.; and Swartzwelder, H.S. Prevalence and correlates of alcohol–induced blackouts among college students: Results of an e–mail survey. Journal of American College Health 51(3):117–119; 122-131, 2002. PMID: 12638993
White, A.M.; Kraus, C.L.; Flom, J.D.; et al. College students lack knowledge of standard drink volumes: Implications for definitions of risky drinking based on survey data. Alcoholism: Clinical and Experimental Research 29(4):631–638, 2005. PMID: 15834229
White, A.M.; Kraus, C.L.; McCracken, L.A.; and Swartzwelder, H.S. Do college students drink more than they think? Use of a free-pour paradigm to determine how college students define standard drinks. Alcoholism: Clinical and Experimental Research 27(11):1750–1756, 2003. PMID: 14634490
White, A.M.; Kraus, C.L.; and Swartzwelder, H. Many college freshmen drink at levels far beyond the binge threshold. Alcoholism: Clinical and Experimental Research 30(6):1006-1010, 2006. PMID: 16737459
White, A.M.; Signer, M.L.; Kraus, C.L.; and Swartzwelder, H.S. Experiential aspects of alcohol–induced blackouts among college students. American Journal of Drug and Alcohol Abuse 30(1):205–224, 2004. PMID: 15083562
White, A.M., and Swartzwelder, H.S. Inbound college students drink heavily during the summer before their freshman year: Implications for education and prevention efforts. American Journal of Health Education 40:909–96, 2009.
Williams, J.; Powell, L.M.; and Weschler, H. Does alcohol consumption reduce human capital accumulation? Evidence from the College Alcohol Study. Applied Economics 35(10):1227–1245, 2003.
Wolfson, M.; Champion, H.; McCoy, T.P.; et al. Impact of a randomized campus/community trial to prevent high-risk drinking among college students. Alcoholism: Clinical and Experimental Research 36(10):1767–1778, 2012. PMID: 22823091
Wood, P.K.; Sher, K.J.; Erickson, D.J.; and DeBord, K.A. Predicting academic problems in college from freshman alcohol involvement. Journal of Studies on Alcohol 58(2):200– 210, 1997. PMID: 9065898
Wood, M.D.; Sher, K.J.; and McGowan, A.K. Collegiate alcohol involvement and role attainment in early adulthood: Findings from a prospective high-risk study. Journal of Studies on Alcohol 61(2):278–289, 2000. PMID: 10757139
World Health Organization (WHO). Alcohol and Injuries: Emergency Department Studies in an International Perspective. Geneva: World Health Organization, 2009.
Zagrosek, A.; Messroghli, D.; Schulz, O.; et al. Effect of binge drinking on the heart as assessed by cardiac magnetic resonance imaging. JAMA: Journal of the American Medical Association 304(12):1328–1330, 2010. PMID: 20858877
- Research article
- Open access
- Published: 07 July 2020
Peer pressure and alcohol consumption in adults living in the UK: a systematic qualitative review
- Hannah Morris 1 ,
- John Larsen 2 ,
- Emma Catterall 2 ,
- Antony C. Moss 3 &
- Stephan U. Dombrowski ORCID: orcid.org/0000-0001-9832-2777 4
BMC Public Health volume 20 , Article number: 1014 ( 2020 ) Cite this article
57k Accesses
35 Citations
46 Altmetric
Metrics details
Peer pressure to drink alcohol may influence excessive alcohol consumption, which can have adverse impacts on health and wellbeing. While peer pressure to drink alcohol is extensively studied among youth, less examination exists among adults. This systematic review examined qualitative research studies which explored the role and concept of peer pressure within the context of alcohol consumption in adults living in the UK.
Qualitative studies which explored peer pressure within the context of alcohol consumption or alcohol related behaviours and views in adults (age range approximately 18–52 years) living in the UK were included. Systematic searches conducted in Medline, PsycINFO and Web of Science identified 1462 references, of which 13 studies met inclusion criteria. Thematic analysis was conducted.
Five overarching themes were identified. Four of these themes directly address aspects of peer pressure, including: experiences of peer pressure; consequences of peer pressure; strategies to deal with peer pressure; and conditions perceived to affect peer pressure. The fifth overarching theme explains the wider social context influencing peer pressure. Pressure to drink alcohol affects individuals across the life span and can be experienced as overt and aggressive, or subtle and friendly. Those consuming little or no alcohol are more likely to feel overt forms of peer pressure. Some developed strategies to cope with pressure from drinkers. Peer pressure can result in feelings of social isolation, or giving in by consuming alcohol against ones wishes.
Peer pressure to drink alcohol is a complex and multifaceted phenomenon experienced across adulthood requiring better understanding to support initiatives to decrease the impact of pressure-inducing environments and develop strategies to deal with perceived pressure conditions.
Trial Registration
The protocol for this review is registered with PROSPERO ( CRD42019122201 ). Registered 11 February 2019
Peer Review reports
Excessive alcohol consumption has adverse impacts on health and wellbeing [ 1 ]. The harmful use of alcohol is a component cause of over 200 disease and injury conditions [ 2 ] and causes 5.3% of deaths worldwide [ 3 ]. Both the volume of alcohol consumption and pattern of drinking affect the level of alcohol-related harm. In the UK, up to one-quarter of adults (18 years or older) reported exceeding the Chief Medical Officers’ low risk drinking guidelines in 2017 [ 4 , 5 , 6 , 7 , 8 ], and among those who drink 27% reported ‘binge’ drinking (i.e. 8 units for men/6 units for women) on their heaviest drinking day in the previous week [ 9 ]. The Global Drug Survey found that drinkers in Britain “get drunk” 51 times per year on average – more often than any other of the 30 nations surveyed [ 10 ]. While the proportion of drinkers in the UK has declined over the last decade [ 9 ], this reduction has not coincided with a reduction in alcohol harm. In 2017, UK alcohol-specific deaths reached the highest level since 2008, with death rates among men twice that of women [ 11 ]. In England, alcohol misuse is cited as the biggest risk factor attributable to early mortality, ill-health and disability for those aged 15–49 years [ 12 ]. A better understanding of the complex driving forces behind drinking behaviour in the UK is urgently needed to inform successful intervention strategies aimed at reducing alcohol-related harm.
Normative perceptions are a key predictor of alcohol consumption. Several social-cognitive models, such as the theory of planned behaviour [ 13 ], include norm and social influence related constructs as explanation for behaviour [ 14 ]. Systematic review evidence consistently suggests that norms play a key role in explaining alcohol consumption [ 15 , 16 ]. For example, in a systematic review of theory of planned behaviour-based studies predicting alcohol consumption, Cooke et al. (2016) report a sample weighted average correlation of r + =.47 between subjective norms and intentions to consume alcohol, a medium to large effect. Intentions in turn had a large-sized relationship with alcohol consumption (r + = .54). The authors note that the strength of relationship between subjective norms and intentions to consume alcohol is larger than norm-intention relationships typically observed for other health behaviours. The consistency found in relationships between norms and intentions underline the social component driving alcohol consumption.
The social context around alcohol shapes and influences alcohol consumption behaviours, and peer pressure can form a part of this social context. Peer pressure can be defined as ‘ any attempt by one or more peers to compel an individual to follow in the decisions or behaviours favoured by the pressuring individual or group ’ [ 17 ]. Perceived peer pressure has been shown to increase engagement in risky drinking practices, such as drinking games [ 18 , 19 ]. Alcohol consumption frequently occurs in contexts where social influence through others may operate and is embedded within many social rituals. Although a shift towards home drinking has occurred recently in the UK [ 20 , 21 ], this change in drinking context is still amenable to peer influence, as peers might still be present during alcohol consumption. Other social drinking occasions, such as mixed location heavy drinking and going out with friends, represent a fifth of drinking occasions in the UK identified by Ally et al. [ 22 ].
The role of peer pressure in influencing alcohol consumption in adults is poorly understood. Previous systematic reviews on the relationship between peer pressure and alcohol consumption have focussed exclusively on adolescents and college or university students; groups often below the legal age to drink, particularly as the majority of studies have been conducted in a US setting [ 23 , 24 ]. However, perceptions of peer pressure are likely to continue to exist into adulthood. Peer pressure may be especially relevant when individuals are trying to change their past alcohol consumption behaviour, going against established norms and behavioural patterns which have become socially engrained. Ethnographic studies of adults, for example, have shown the importance of peer pressure specifically regarding the tradition of buying ‘rounds’ in the pub [ 25 ]. This highlights an important structural aspect to peer pressure, whereby cultural practices around the way alcohol is purchased and provided to individuals may perpetuate certain patterns of drinking within social groups, potentially even if perceived or actual peer pressure disappeared. A more nuanced understanding of peer pressure might inform the development of successful alcohol reduction strategies.
The aim of this systematic review is to examine qualitative research studies which have explored the role and concept of peer pressure within the context of alcohol consumption in adults living in the UK.
We systematically reviewed qualitative studies reporting on peer pressure within the context of alcohol consumption or alcohol related behaviours and attitudes in UK adults. The protocol for this review is registered with PROSPERO (CRD42019122201). Our reporting follows the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidance.
Inclusion criteria
This review included qualitative studies which explored peer pressure within the context of alcohol consumption or alcohol related behaviours and views in adults living in the UK. Table 1 details all inclusion criteria.
Studies were excluded when examining adults with alcohol dependence, or adults undergoing treatment for alcohol dependence, or if they were not published in English.
Search strategy
The basic search strategy was (alcohol* OR drink) AND (peers OR friend*) AND (United Kingdom OR Great Britain) ( see Additional file 1 for full search strategy ). Searches were conducted in January 2019 and limited to a 25-year time frame (January 1994 to January 2019). Searches were conducted in Medline, PsycINFO and Web of Science core collection.
Five key journals were hand searched in January 2019: Addiction; Alcohol and Alcoholism; Addictive Behaviours; Substance Use and Misuse; and Psychology of Addictive Behaviors. All issues published between January 2018 and January 2019 were checked for possibly relevant papers not yet loaded on electronic databases [ 26 ].
Google scholar was searched using the search strategy (alcohol OR drink) AND (peers OR friend). Searches were limited to those published on or after January 1994. For each search the first 100 results were reviewed to identify any potentially relevant studies.
The reference lists of all included papers were examined for additional relevant papers, and forward citation searches were also conducted on all included papers.
Screening and data extraction
All titles and abstracts were screened independently by two reviewers (EC and HM) with 98% agreement. Full text screening was carried out independently by two reviewers (EC and HM), with 73% agreement. All disagreements were resolved through discussion or arbitration with a third reviewer (JL).
Data extraction was conducted by one reviewer (HM) and checked by a second reviewer (JL). Data for analysis was considered to be text under the heading ‘findings’ or ‘results’ which pertained to peer pressure and alcohol.
Quality appraisal
There is currently no consensus on how to best carry out quality appraisal for qualitative systematic reviews [ 27 ]. This review used the Critical Appraisal Skills Programme [ 28 ] qualitative checklist. The checklist was operationalised so that for each of the ten quality criteria a study could score two points if the criterion was fully met, one point if it was partially met, and zero points if it was not met at all. This provides a possible maximum score of 20. All studies were appraised by one author (HM) and a sample of four studies was checked by a second (EC). Any disagreements between the two study authors were resolved through discussion.
Analysis and synthesis
We carried out a thematic synthesis as described by Thomas and Harden [ 29 ]. Two reviewers (HM and JL) familiarised themselves with the data through close reading of all the studies. Line by line coding of all data was then carried out by one reviewer (HM) with a sample of three studies also coded by a second reviewer (JL). Codes were discussed and descriptive themes were tentatively developed and discussed with all review authors. Through this process new themes emerged, and other themes merged together, resulting in overarching themes and sub-themes. An organising framework was constructed to visualise the identified themes and their possible relationships.
Search results and study selection
The search and study selection process is detailed in the PRISMA flow chart (Fig. 1 ). The review identified 1462 references through database searching. After screening and full article assessment, 13 studies met inclusion criteria for the review.
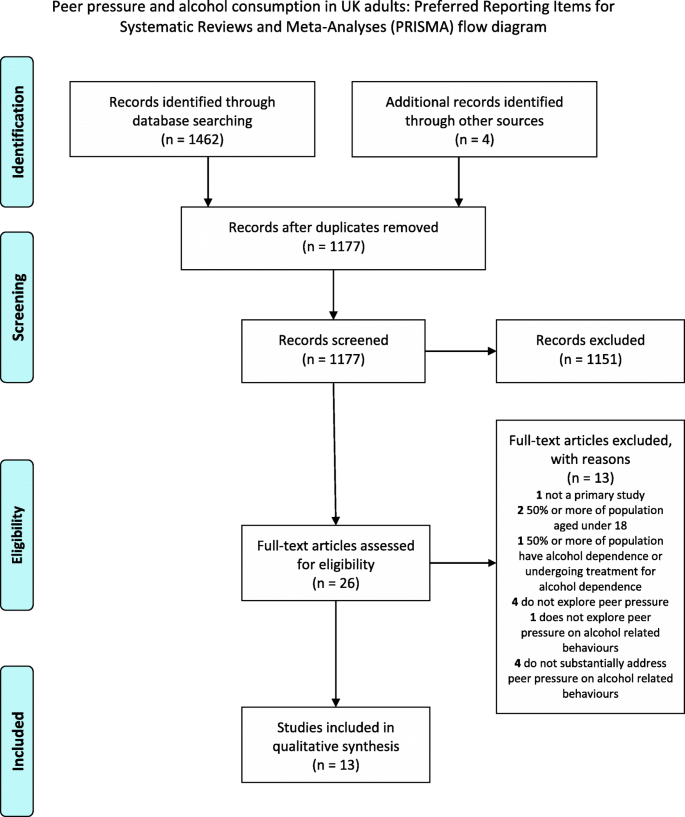
PRISMA flow diagram
Study characteristics
The 13 included studies were published between 2004 and 2018. Seven of the studies exclusively focused on university students [ 30 , 31 , 32 , 33 , 34 , 35 , 36 ]. Not all of these studies provided details of the age of participants, but in those studies where age demographics were provided it ranged from 18 to 33 years. Of the remaining studies, all but one focussed on a specific age demographic. Three focused on young people including students [ 37 , 38 , 39 ], and two focused on individuals in midlife [ 40 , 41 ]. Lastly, one study focused on a specific occupation, looking at nightlife entertainers, and these participants were aged 20 to 49 years [ 42 ].
Of the seven studies examining university students, the universities were in the following locations: the south of England [ 32 ]; East Midlands [ 34 ]; West Midlands [ 35 ]; North West England [ 36 ]; and North England [ 31 ]. In addition, one study reported the university was in England [ 33 ], and one study recruited from three universities in England and Wales [ 30 ]. Of the six non-student studies, three recruited participants from the west of Scotland [ 40 , 41 , 42 ], and one each in South East England [ 37 ] and South West England [ 39 ]. The remaining study reported that the ‘vast majority’ of participants resided in London [ 38 ].
The majority of studies (ten out of 13) included both male and female participants. Two studies examined females only [ 31 , 34 ], and one males only [ 41 ]. Four studies examined light or non-drinkers [ 33 , 34 , 37 , 38 ], the remaining nine studies included participants with a range of drinking profiles.
Eight studies employed interviews for data collection [ 32 , 33 , 34 , 35 , 37 , 38 , 39 , 42 ], three used focus groups [ 31 , 40 , 41 ], one used a narrative question as part of a questionnaire [ 30 ], and one used both interviews and a narrative question as part of a questionnaire [ 36 ].
The assessed quality of studies ranged from a score of ten to 17 out of a maximum of 20 using the operationalised Critical Appraisal Skills Programme (CASP) checklist. We judged a study as being of higher quality if it scored 15 or more, and lower quality if scoring less than 15. Using this classification, six studies were of higher quality [ 32 , 33 , 34 , 37 , 40 , 41 ] and seven were of lower quality [ 30 , 31 , 35 , 36 , 38 , 39 , 42 ]. A weight of evidence was then applied using these quality assessments, with greater weight given to studies of higher quality. Table 2 provides further details on study characteristics.
Five overarching themes were identified and developed into an organising framework, see Fig. 2 . Four of these themes were identified as directly addressing aspects of peer pressure. These were: experiences of peer pressure; consequences of peer pressure; strategies to deal with peer pressure; and conditions perceived to affect peer pressure. The fifth overarching theme provides detail on the wider social context influencing peer pressure. Each of these overarching themes consists of sub-themes derived from the data.
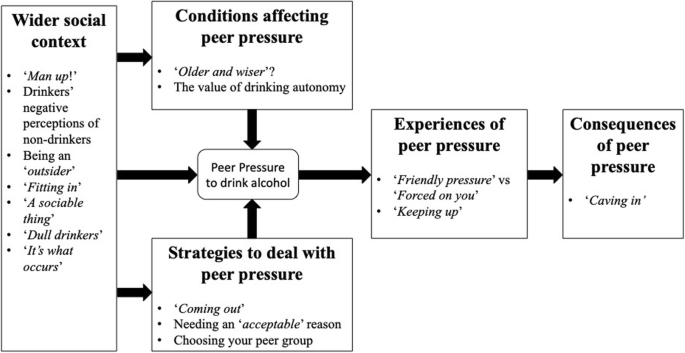
Peer pressure organising framework including overall themes and corresponding sub-themes
All data from primary study participants is presented in italics and double inverted commas, data from primary study authors is presented in single inverted commas and is not in italics.
Experiences of peer pressure
Two sub-themes were identified which described elements of the experience of peer pressure.
‘Friendly pressure’ vs. “Forced on you”
Peer pressure to drink alcohol was described differently by participants across studies. A ‘friendly pressure’ to drink was more often expressed by people who themselves were drinkers–this was not typically perceived as peer pressure, but instead a more friendly style of drinking encouragement. However, non-drinkers and some university students experienced a more aggressive form of pressure which was characterised as at times unpleasant and intimidating.
Those describing friendly pressure to drink did not perceive this as peer pressure. As one participant in Graber et al.’s [ 37 ] study describes “When people talk about peer pressure to drink I’m just like ‘doesn’t exist’. I’ve never felt any pressure to, I do it because I’ve chosen to, not because someone’s forced me to [ … ] [‘peer pressure’] sounds like people are just like ‘Drink drink drink’[ … ] I’ve never had someone be like that to me, or[ … ] it was only jokingly.” The study authors note how she describes being ‘jokingly’ egged on, rejecting any notion of peer pressure. A similar type of friendly pressure is also described by a participant in Orford et al.’s study [ 35 ], “If one of us sort of is a bit reluctant then the rest of us will go, ‘Oh go on’, but it doesn’t take much arm-twisting so it’s not really persuasion.”
In contrast, some participants across studies described experiencing a more ‘forced on you’ and aggressive form of peer pressure. In particular, university students reported to be subject to this kind of pressure. One participant from Black & Monrouxe’s [ 30 ] study of university students describes a threatening form of peer pressure to drink. “ Initiation ceremony [ …] 2nd years, house. Gang of boys dressed in black bin liners, surrounding freshers and shouting at them to down their drinks. I left, and comforted another fresher who didn’t wish to take part.” Similar experiences were reported in Jacobs et al. [ 34 ] study of non-drinking students, ‘All eight participants interviewed expressed that interactions with drinking students were often unpleasant [ …] Seven out of eight students subject to hurtful comments either to their face, or behind their backs.’ However, this aggressive form of peer pressure was not exclusive to university students, and was also reported in Emslie et al.’s [ 40 ] study of individuals in mid-life. ‘(Non-drinkers) described how difficult it was for people to understand and accept that they did not drink alcohol [ …] described receiving a more aggressive reaction [ …] (“ what do you MEAN you don’t drink? ” and “ well, you’ll have one with me! ”)’.
“Keeping up”
One form of peer pressure described in several studies was the pressure of ‘keeping up’ with the pace of faster drinkers. The pressure to keep up could be explicit (‘ you get the piss taken out of you if you’re not keeping up with the guys’ [ 31 ]) but could also be a part of drinking etiquette – an implicit ‘rule’ of drinking that everyone within the group keeps pace together.
Emslie et al. [ 41 ] describes the drinking practice of buying rounds: ‘Buying “ rounds ”—where each man, in turn, bought drinks (usually pints of beer) for the group—was constructed as an essential part of pub etiquette (“ the male equivalent of a friendship bracelet ”), which sometimes led to excessive drinking, due to the pressure to keep up with the fastest drinker.’
A participant in the study by MacArthur et al. [ 39 ] describes a less formalised but almost habitual form of “ keeping up” . “Sometimes you go out with the wrong frame of mind I suppose and my friend’s bought a pint and then I’ll buy a pint, I’ll sort of drink it and they say they’ve finished theirs and I’m like, oh I’ve got to finish mine. Go and get another pint and I’d try and keep up with them cos they get out more often and I get more drunk than they do.”
Consequences of peer pressure
One key sub-theme was identified which explored the consequences of peer pressure.
“Caving in”
Some non-drinkers and moderate drinkers reported instances of ‘caving in’ to the peer pressure to drink alcohol. Caving in was reported as a regrettable experience in most cases and was often due to experiencing more aggressive or persistent forms of peer pressure. For non-drinkers, caving in could mean drinking when they did not intend to consume any alcohol, and for moderate drinkers it could mean drinking more than intended.
Jacobs et al. [ 34 ] describe how one participant was unable to resist peer pressure, leading her to drink alcohol even though she was against doing so. “ They’d be like, you really do want to though don’t you, they’d pour a drink out for me, sort of say oh just have a drink, [ …] well the second time I went out I sort of caved into that.” In this instance, the authors note ‘The process of pouring out drinks, an active offer of alcohol, is evidence of direct encouragement, the most direct form of peer pressure.’
Participants in Black & Monrouxe’s study [ 30 ] also describe caving in to more persistent and aggressive peer pressure, as illustrated by one student “ I gave up alcohol for lent in my first year at uni. My flatmates forced me to break it. We were pre-drinking in our flat before going clubbing. I was with 6 or 7 friends. I was verbally bullied until I started drinking.”
However, stronger forms of peer pressure were not always necessary, with some individuals describing difficulties turning down drinks in response to more subtle forms of pressure. An evening entertainer from Forsyth et al.’s study [ 42 ] describes “People keep offering you drinks, particularly if you are playing, and I think if your band-mates are also drinking it’s quite difficult you know to say ‘oh no”’.
Strategies to deal with peer pressure
Three sub-themes were identified which address strategies to deal with peer pressure.
“Coming out”
Gaining acceptance from peers regarding one’s choices to moderate or abstain from drinking alcohol was rarely reported. Particularly amongst university non-drinkers, the norm appeared to be employing avoidance strategies or excuses rather than “coming out” about ones drinking choices.
Herring et al. [ 38 ] observe ‘the extent to which young people were “ open ” about their drinking behaviour, which varied considerably, with some striving to “ blend in ” and not reveal their “ secret ” and others being “ up front ” about their drinking preferences’.
Black & Monrouxe (2014) describe one individual’s strategy to initially join in with the drinking behaviours of their peer group, but once they had been accepted into the group they were able to assert themselves and refute further peer pressure. “ I was encouraged by a group of sports team-mates to down my drink due to losing a drinking game in a sports social with teammates. [ …] It wasn’t particularly pleasant, especially because drinking until drunk is against my religious beliefs so there was a conflict there. However, since then I have managed to draw the line with my team-mates so if I say I’m not drinking any more, then they are OK with that.”
A similar approach was described by a participant in Conroy & de Visser’s study [ 33 ]. “ When first getting to know people it’s important to look like you’ve got a drink. But once you’ve got to know people and they accept it, the best strategy is just to say ‘No thanks’. [ …] So it’s accepted as part of who I am. It’s not a secret, it’s just not something that you broadcast when people who are around you are heavy drinkers.”
Conroy & de Visser [ 33 ] observe a more direct approach was favoured by female participants within their study. “ I say, ‘no, I don’t drink, I never have drunk, I don’t see the reason in drinking, I am not going to drink now.’ They say, ‘just smell it, you’ll like it.’ It’s like, ‘it doesn’t matter if I like it or not, I don’t want to drink.’ I repeat that for a bit and they tend to give up and go away.” The study authors observe that this participant ‘ preferred to comprehensively refute peer pressure to drink alcohol, choosing to express her behavioural mind-set (“ I don’t” ), its history (“ I haven’t” ) and her stance (“ I don’t see the reason in drinking” ).’
Needing an ‘acceptable’ reason
Non-drinkers or moderate drinkers often reported needing an “ acceptable ” reason to give to their peers to explain their non-drinking. This was required to alleviate pressure from peers to drink, to gain acceptance from peers, to avoid losing social status within the group and sometimes also to avoid appearing rude or antisocial.
“ Acceptable ” reasons identified by participants across studies included: detoxing or dieting (females only); being pregnant; driving; unspecified medical reasons; and being on antibiotics. Other strategies described by participants to avoid being detected as a non-drinker included choosing non-alcoholic drinks which looked like alcoholic drinks, for example ‘pretending the bottle of water he needed to avoid dehydration was “ straight vodka” ’ [ 42 ], or “ having a half full glass of Coke, that everyone assumes is Coke and Jack Daniels” [ 33 ]. This practice was described as ‘mirroring’ drinks by Herring et al. [ 38 ].
Some individuals reported “ nursing ” drinks so that they lasted a long time, buying their own drinks, avoiding being in rounds, and disposing of unwanted drinks.
For other individuals it was easier to avoid situations where the focus was on drinking altogether, as illustrated by a participant in Jacob et al.’s [ 34 ] study. “ That’s how people are social. My flatmates would ask me [ …] are you coming out tonight [ …] when I say ‘no, I’ll give this one a miss’, [ …] it makes me feel really antisocial. Every time I say no, it gives off the message that I don’t wanna be social and they’ll stop asking me. If they ask me in the morning [ …] it’ll be ‘I’ll think about it’, then in the evening I’ll be like ‘I’ll have an early night’. I find it quite difficult ‘cause it’s me saying I don’t want to do this with you is being personal.”
Choosing your peer group
For some non-drinkers and moderate drinkers, strategically selecting peers with similar drinking habits, or mixing with peers with a diverse range of consumption levels, was seen as a helpful strategy in avoiding unwanted peer pressure. The importance of supportive peers who understood and respected their decision not to drink were highlighted.
Graber et al. [ 37 ] describe how careful selection of a peer group can reduce drinking-related peer pressure. ‘(One participant) related finding an accepting friendship group who ranged from moderate drinkers to abstainers. Knowing other non-drinkers and having peers who know other non-drinkers made her teetotal status less salient.’ This finding is also echoed by Piacentini & Banister [ 36 ] ‘Light non-drinkers had a tendency to draw on the ‘seeking social support’ strategy, deliberately seeking the company of other light or nondrinking friends. (One participant) explained how initially she had considered socialising with her university flat mates, but decided against this when she realised the extent of their alcohol consumption. “ I didn’t go out with them. I thought about it at first but when I realised how much they drink [ …] went out with people who don’t drink or drink a little.”’
Conditions perceived to affect peer pressure
Two sub-themes discussed conditions which may affect peer pressure.
“Older and wiser”
In midlife, Emslie et al. [ 40 ] suggest that midlife drinkers’ descriptions initially gave the impression that they experience less peer pressure to drink and are more able to resist peer pressure than their younger selves, by having become “older and wiser”. However, these initial assertions were ‘undermined by drinking stories re-told within friendship groups, jokes which questioned stories of responsible drinking, and accounts of continuing peer pressure to drink’, and it became evident that peer pressure often continues to exist in midlife.
Emslie et al. [ 40 ] illustrate the initial presentation by participants that they would no longer be susceptible to peer pressure. ‘He contrasted his wilder younger self with becoming a “ wise old owl ” now: “[ …] I think we’ve all done that once, hide the drink – get rid of it some way or another, not leave it [because of peer pressure]. But nowadays, you can be honest and say, ‘I’ve had too much – I’ve had enough, and don’t even say to me have another one, because I’m not interested’. I can do that now.”’
However, as the focus groups progressed, these initial assertions were brought into question. ‘They described how their intention not to drink alcohol – or to stop drinking – was sometimes just not accepted and illustrated this through the repeated chants of the group (e.g. “go on, go on, go, on, just the one”, “take one, take one”, “just leave the car, just leave the car” or “another one for the road” ).’
An “ older and wiser ” theme was also identified in younger drinkers, with evidence that peer pressure diminishes as individuals move through adolescence into young adulthood. However, the drinking behaviour of university students is then described in contrast to this, as evidence that peer pressure may not diminish in young adulthood.
MacArthur et al. [ 39 ] observe ‘The influence of peer behaviour diminished somewhat as young people moved through adolescence. Young people still described an influence of their friends, or a more subtle form of influence characterised by “ going along with” the behaviour of their friends, but young people learnt from their experiences, and felt freer to exert their own choices around drinking behaviour ’. However, this study also found university students to be particularly vulnerable to peer pressure: ‘Among those who attended university, peer behaviour and local norms again influenced the habitus, but to a greater extent, with young people reporting a clear awareness that drinking was “ the scene” and integral to university culture. Habitus for these individuals structured more regular and extreme practice reflecting the reported culture of heavy and frequent drinking in these fields and the influence of collective peer behaviour on practice.’
The value of drinking autonomy
For some individuals, being a non-drinker or moderate drinker created a strong sense of autonomy and pride at being able to refute peer pressure. “ Making a free choice” meant feeling like the decisions made about drinking, and while drinking, were truly one’s own. Making a free choice was also experienced as feeling proud about making drinking choices which reflect one’s personality, values and priorities’ [ 37 ].
This theme is further illustrated by Herring et al. [ 38 ]: ‘Some participants placed great value on being different and not following the “ crowd ” this respondent was proud of being “ different” : “ I’d say it’s an important part of who I am because it’s always something that I would say I feel slightly, it may be an arrogant thing to say, but I feel slightly proud of not drinking in the face of the fact that I’ve always been pressured to drink by other people.”’
Wider social context
Seven sub-themes were identified which describe the wider social context in which peer pressure to drink takes place.
For some male participants, drinking was firmly aligned with masculinity. Challenges to masculine identity provide a basis through which men are able to intimidate each other to drink more. Men wishing to avoid gender-based peer pressure to drink tried to find a way of successfully challenging or circumventing it. Additionally, the need to maintain a masculine, heterosexual identity played an important part in how much an individual drank, how often, and what kinds of drink were consumed.
The quantity, and type, of alcohol consumed, was widely viewed as a strong social marker of gender identity and sexual orientation. This is illustrated in a focus group discussion between two male participants in Emslie et al.’s [ 40 ] study. ‘“You walk over with a glass of coke and it’s just [ …]” “Oh! Abuse!” “‘Oh, here comes the gay boy’, do you know what I mean? (laughs)”’. This observation is further explored in Emslie et al.’s [ 41 ] study which included only male participants. ‘Failing to be seen to be drinking like a man was represented as evidence of something being “ wrong ”, which was then associated with being gay or having no money; both appear as reflections of compromised masculinity.’ This was a view held by participants across the reviewed studies, with Conroy & de Visser [ 32 ] observing that negative opinions of male non-drinking was ‘a view commonly expressed by participants concerning the risks to men’s perceived masculinity associated with the decision to not drink.’
Drinkers’ negative perceptions of non-drinkers
Across a number of studies, non-drinkers reported being subject to negative opinion from drinkers. Non-drinkers discussed how they were stereotyped as “ boring ” by drinkers [ 30 , 34 ], or perceived as being judgemental [ 40 ].
Being an “outsider”
Both non-drinkers and drinkers who chose not to drink on certain occasions described feeling like an “ outsider ”. Problems faced by non-drinkers or moderate drinkers included: ‘finding it difficult to get into conversations’ [ 40 ]; ‘feeling as though their peers do not want to socialise with them’ [ 34 ]; feeling uncomfortable witnessing drunken behaviour [ 33 ].
The extent to which drinking alcohol is normalised and expected within UK society was widely commented on across studies. As one young male former drinker explained “People said these things are normal and everybody is doing it and you’ll be like out of society now” [ 38 ].
“Fitting in”
For some participants, drinking and/or getting drunk was an accepted requirement for “fitting in” to a specific social group. In some cases, once individuals had successfully integrated into the group, they could then assert their right not to drink.
Carpenter et al. [ 31 ] reported that ‘The first year students in this study stated that they believed that getting drunk would help them to ‘fit in’: “ You are out of your comfort zone. Your friends and family are back home. You will go out more because you have to in order to meet people and then because of that, you end up drinking.”’.
“A sociable thing”
Participants across studies described how drinking was an integral part of socialising, going out and meeting with friends. As one participant in Emslie et al.’s [ 40 ] study succinctly put it ‘ “If you don’t go to the pub, you’d never see anyone”’.
The integral nature of alcohol for socialising was especially pronounced amongst university students. Piacentini & Banister [ 36 ] noted, ‘Most participants acknowledged that their social life at university revolved around alcohol consumption. The importance of alcohol in the students’ wider social worlds was clear. “ We all like a drink, it cannot be underestimated for its value in social activities.”‘ .
“Dull drinkers”
Moderate and non-drinkers challenged the dominant discourse that drinking is a sociable act. They instead portrayed drinkers as dull, with shallow relationships who limit their social activities to the repetitive act of drinking.
Herring et al. [ 38 ] note how the non-drinking participants in their study had to work hard to encourage drinking friends to consider social activities where alcohol was not a central component. ‘In terms of their social lives, young people often encouraged their drinking friends to participate in activities that did not involve alcohol or where alcohol was incidental rather than integral to the event, e.g. to see a film, visit an exhibition. They felt it was too easy for drinkers to ‘default’ to simply going out drinking and not to consider alternatives.’
Emslie et al. [ 40 ] describe how non-drinking participants challenged the idea that drinkers were fun and sociable. ‘(Respondents who were non-drinkers) commented on how much interaction in their age group consisted of people talking about going to the pub. They inverted the common cultural portrayal of drinkers as ‘fun’ and non-drinkers as ‘boring’, so that people who did not drink were characterised as entertaining, creative, witty, making real connections with other people and taking responsibility for themselves, while drinkers were portrayed as dull, having repetitive conversations, having shallow relationships with others propped up by alcohol and being irresponsible and unimaginative.’
“It’s what occurs”
Across studies, drinking was described as something very normal, which everyone does, and is culturally expected. For many participants it was done without thinking.
Emslie et al. [ 40 ] observe that ‘Going out drinking together was widely constructed as the “ natural ” way for men to socialize’. Students in MacArthur et al.’s [ 39 ] study also construct alcohol consumption as a normal and almost unthinking act “ I can’t think of a thing that you go out to in the evening except bowling and things like that, where you don’t drink, and even bowling you probably do as well, umm yeah, you just kind of do in the evenings, it’s what occurs.” .
This study systematically reviewed qualitative evidence on the role and concept of peer pressure within the context of alcohol consumption or alcohol related behaviours in adults living in the UK. This has led to the development of a preliminary framework for understanding peer pressure, across a broader range of people than have been included in previous studies. Findings based on 13 studies highlight the complex nature of peer pressure and the way it operates within the context of alcohol consumption. Peer pressure was perceived across a range of ages and was not solely restricted to adolescents and young adults. Four key aspects of peer pressure were identified: conditions perceived to affect peer pressure; strategies to deal with peer pressure; experiences of peer pressure; and consequences of peer pressure. These four key aspects of peer pressure are further situated within and influenced by the wider societal context.
The findings offer insight into how peer pressure is expressed in adults living in the UK through social norms which influence people’s drinking intentions and drinking behaviours [ 15 ]. For example, requirements to ‘keep up’ with a certain level of alcohol consumption expected within a social group and linked e.g. to perceptions of gender identity mean that people in order to ‘fit in’ can drink more than they would have liked to. As suggested by Cooper et al. [ 43 ], certain social situations can make it particularly difficult for people to resist social pressure, with student initiation ceremonies among young adults at the extreme end of the scale of social pressure being exercised (e.g., 30), while the pressure is less aggressively expressed, but still present, for example among midlife adults when ‘buying rounds’ in the pub [ 41 ]. Being part of a ‘round’ is also an expression of an overt offer, as suggested by Borsari and Carey [ 23 ].
This review underlines that peer pressure to drink alcohol forms a social ritual in various UK contexts, which is experienced across a range of ages, and not exclusively in adolescents and young adults. Although some individuals perceived a lessening of peer pressure to drink alcohol over time as they age, accounts suggested a persistent, often subtle perceptions of continuing pressure to drink alcohol.
Individuals across studies report using a variety of strategies to cope with and manage perceptions of peer pressure – whether these involve coming up with an ‘acceptable excuse’, seeking to conceal low/no alcohol consumption or ‘coming out’ to openly state the wish not to drink (at all, or to excess). Interestingly, the review identified how such opposition to peer pressure could be a source of positive identity for the individual, and that friendships could be determined and negotiated based on the non- or low-drinking identity. This is in line with a growing trend of non-drinking among young people [ 44 ] and recent societal trends such as (temporal) sobriety [ 45 ].
Suggestions for further research
The current review suggests that further qualitative research is required to understand peer pressure more fully. Despite relatively broad inclusion criteria, only 13 studies could be included. Further qualitative studies focused on peer pressure could build and elaborate on the themes identified in this review (Fig. 1 ).
Although peer pressure to drink alcohol is experienced across the life span, the majority of reviewed research focussed on adolescents and young adults, typically university students. Further primary research focussing explicitly on adults across a range of ages and socioeconomic backgrounds is urgently required. The experience of peer pressure to drink in non-drinkers and light, moderate and heavy drinkers should be further examined. None of the included studies have focused on peer pressure to drink alcohol across the socioeconomic spectrum. Given the relationship between level of disadvantage and increased alcohol-attributable harm [ 46 ], additional research focusing on less privileged populations would be beneficial. It would be particularly interesting, in future work examining these broader demographic groups, to determine whether the framework for different themes which emerged through this review might be a valid framework within which to understand different aspects of peer pressure.
The findings suggest that moderate to heavy drinkers are less likely to perceive peer pressure as something which affects them. Observational and diary-based methods, or other longitudinal methods which allow participants more time to reflect on peer pressure, may be useful methodological approaches to adopt in this population. Unpicking how, and when, adult drinkers acknowledge the influence of peer pressure in their drinking habits maybe a valuable ‘turning point’ which could be harnessed for health promotion strategies. Integrating this qualitative research with the existing quantitative evidence would help target interventions and support for the population segments most vulnerable to this.
The current review has the potential to influence future intervention research in two ways. First, the detailed understanding of the peer pressure process and context provides detail that can inform the selection of appropriate behaviour change techniques [ 47 ] and forms of delivery [ 48 ] to support change in alcohol consumption as a result of peer pressure. Second, the specific strategies reported by several studies demonstrate that individuals frequently attempt to avoid or manage peer pressure to drink alcohol, and could form the basis for intervention.
Strengths and limitations
This review systematically examined the qualitative evidence on peer pressure across a range of ages, and provides a comprehensive overview of the best evidence of peer pressure within the context of alcohol consumption or alcohol related behaviours in adults living in the UK. The thematic analysis developed has the potential to inform future research and intervention studies. Some limitations need to be kept in mind when interpreting the findings of this study. The included studies were variable in terms of methodological quality. Although the review focused on adults living in the UK across all ages, the majority of studies included young adults and university students, somewhat limiting the representation from other age groups. Studies that were included did not necessarily focus on peer pressure, but often explore peer pressure as part of a range of factors. Additional and deeper insights into peer pressure might be obtained by research that exclusively focuses on peer pressure.
Conclusions
Peer pressure to drink alcohol is most commonly associated with adolescents and young adults, but this review found peer pressure affects individuals across the life span. Peer pressure to drink alcohol can take many forms, and may be experienced as overt and aggressive, or subtle and friendly. Non-drinkers are more likely to feel overt forms of peer pressure, whilst heavier drinkers may not identify with peer pressure to drink alcohol, preferring to describe pressure to drink as banter, jokes, and friendly pressure. As a result of the overt pressure to drink, some non-drinkers have developed strategies to cope with pressure from drinkers. Strategies to manage peer pressure worked for some non- or moderate drinkers, for others peer pressure resulted either in feelings of social isolation, or giving into the pressure and consuming alcohol against their wishes.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
Critical appraisal skills programme
Preferred reporting items for systematic reviews and meta-analyses
International prospective register of systematic reviews
United Kingdom
Rehm J, Mathers C, Popova S, Thavorncharoensap M, Teerawattananon Y, Patra J. Global burden of disease and injury and economic cost attributable to alcohol use and alcohol-use disorders. Lancet (London, England). 2009;373(9682):2223–33.
Google Scholar
Rehm J, Baliunas D, Borges GL, Graham K, Irving H, Kehoe T, et al. The relation between different dimensions of alcohol consumption and burden of disease: an overview. Addiction. 2010;105(5):817–43.
PubMed PubMed Central Google Scholar
World Health Organization Management of Substance Abuse Unit. Global status report on alcohol and health. Geneva: World Health Organization; 2018.
Department of Health UK. UK Chief Medical Officers’ low risk drinking guidelines. 2016.
NHS Digital. Health Survey for England 2017: adult health related behaviours- tables. [Dataset]. 2018.
Scottish Government. Scottish health survey 2017: volume one – main report. [Online]. 2018.
Welsh Government. National Survey for Wales: results viewer. [Dataset]. 2019.
Department of Health Northern Ireland. Health survey Northern Ireland: first results 2017/18. [Online]. 2018.
Office for National Statistics. Adult drinking habits in Great Britain. [Dataset]. ONS; 2018.
Winstock AR. Global drug survey 2019. [Online]. London: GDS; 2019.
Office for National Statistics. Alcohol-specific deaths in the UK. ONS; 2018.
Public Health England. The Public Health Burden of Alcohol and the Effectiveness and Cost-Effectiveness of Alcohol Control Policies. London: An evidence review; 2016.
Ajzen I. The theory of planned behavior. Organ Behav Hum Decis Process. 1991;50(2):179–211.
Michie S, Johnston M, Abraham C, Lawton R, Parker D, Walker A. Making psychological theory useful for implementing evidence based practice: a consensus approach. Qual Saf Health Care. 2005;14(1):26.
CAS PubMed PubMed Central Google Scholar
Cooke R, Dahdah M, Norman P, French DP. How well does the theory of planned behaviour predict alcohol consumption? A systematic review and meta-analysis. Health Psychol Rev. 2016;10(2):148–67.
PubMed Google Scholar
McEachan R, Taylor N, Harrison R, Lawton R, Gardner P, Conner M. Meta-analysis of the reasoned action approach (RAA) to understanding health behaviors. Ann Behav Med. 2016;50(4):592–612.
Ngee Sim T, Fen KS. A domain conceptualization of adolescent susceptibility to peer pressure. J Res Adolesc. 2003;13(1):57–80.
Polizzotto MN, Saw MM, Tjhung I, Chua EH, Stockwell TR. Fluid skills: drinking games and alcohol consumption among Australian university students. Drug Alcohol Rev. 2007;26(5):469–75.
Moss AC, Spada MM, Harkin J, Albery IP, Rycroft N, Nikčević AV. ‘Neknomination’: predictors in a sample of UK university students. Addict Behav Rep. 2015;1:73–5.
Foster JH, Ferguson CS. Home drinking in the UK: trends and causes. Alcohol Alcohol. 2012;47(3):355–8.
Office for National Statistics. Family spending in the UK: April 2017 to March 2018. [Online]. ONS; 2019.
Ally AK, Lovatt M, Meier PS, Brennan A, Holmes J. Developing a social practice-based typology of British drinking culture in 2009-2011: implications for alcohol policy analysis. Addiction. 2016;111(9):1568–79.
Borsari B, Carey KB. Peer influences on college drinking: a review of the research. J Subst Abus. 2001;13(4):391–424.
CAS Google Scholar
Leung RK, Toumbourou JW, Hemphill SA. The effect of peer influence and selection processes on adolescent alcohol use: a systematic review of longitudinal studies. Health Psychol Rev. 2014;8(4):426–57.
Heley J. Rounds, range rovers and rurality: the drinking geographies of a new Squirearchy. Drugs: Educ Prev Policy. 2008;15(3):315–21.
York CRD. Systematic reviews. CRD’s guidance for undertaking reviews in healthcare 2009.
Greaves C, Poltawski L, Garside R, Briscoe S. Understanding the challenge of weight loss maintenance: a systematic review and synthesis of qualitative research on weight loss maintenance. Health Psychol Rev. 2017;11(2):145–63.
CASP. Critical Appraisal Skills Programme Qualitative Checklist [Online]. 2018 [Available from: https://casp-uk.net/casp-tools-checklists/ .
Thomas J, Harden A. Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Med Res Methodol. 2008;8(1):45.
Black LF, Monrouxe LV. Being sick a lot, often on each other': students' alcohol-related provocation. Med Educ. 2014;48(3):268–79.
Carpenter R, Fishlock A, Mulroy A, Oxley B, Russell K, Salter C, et al. After 'Unit 1421′: an exploratory study into female students' attitudes and behaviours towards binge drinking at Leeds University. J Public Health. 2008;30(1):8–13.
Conroy D, de Visser R. ‘Man up!’: Discursive constructions of non-drinkers among UK undergraduates. J Health Psychol. 2012;18(11):1432–44.
Conroy D, de Visser R. Being a non-drinking student: an interpretative phenomenological analysis. Psychol Health. 2014;29(5):536–51.
Jacobs L, Conroy D, Parke A. Negative experiences of non-drinking college students in Great Britain: an interpretative phenomenological analysis. Int J Ment Heal Addict. 2018;16(3):737–50.
Orford J, Krishnan M, Balaam M, Everitt M, Van Der Graaf K. University student drinking: the role of motivational and social factors. Drugs: Educ Prev Policy. 2004;11(5):407–21.
Piacentini MG, Banister EN. Getting hammered? ‥‥ students coping with alcohol. J Consumr Behav: Int Res Rev. 2006;5(2):145–56.
Graber R, de Visser R, Abraham C, Memon A, Hart A, Hunt K. Staying in the 'sweet spot': a resilience-based analysis of the lived experience of low-risk drinking and abstention among British youth. Psychol Health. 2016;31(1):79–99.
Herring R, Bayley M, Hurcombe R. “But no one told me it’s okay to not drink”: a qualitative study of young people who drink little or no alcohol. J Subst Abus. 2014;19(1–2):95–102.
MacArthur GJ, Jacob N, Pound P, Hickman M, Campbell R. Among friends: a qualitative exploration of the role of peers in young people's alcohol use using Bourdieu's concepts of habitus, field and capital. Sociol Health Illn. 2017;39(1):30–46.
Emslie C, Hunt K, Lyons A. Older and wiser? Men’s and women’s accounts of drinking in early mid-life. Sociol Health Illn. 2012;34(4):481–96.
Emslie C, Hunt K, Lyons A. The role of alcohol in forging and maintaining friendships amongst Scottish men in midlife. Health Psychol. 2013;32(1):33–41.
Forsyth AJM, Lennox JC, Emslie C. "That's cool, you're a musician and you drink": exploring entertainers' accounts of their unique workplace relationship with alcohol. Int J Drug Policy. 2016;36:85–94.
Cooper ML. Motivations for alcohol use among adolescents: development and validation of a four-factor model. Psychol Assess. 1994;6(2):117–28.
Fat LN, Shelton N, Cable N. Investigating the growing trend of non-drinking among young people; analysis of repeated cross-sectional surveys in England 2005–2015. BMC Public Health. 2018;18(1):1090.
Ramage A, Fairbairns R. The 28 day alcohol-free challenge. London: Pan Macmillan; 2018.
Katikireddi SV, Whitley E, Lewsey J, Gray L, Leyland AH. Socioeconomic status as an effect modifier of alcohol consumption and harm: analysis of linked cohort data. Lancet Public Health. 2017;2(6):e267–e76.
Michie S, Richardson M, Johnston M, Abraham C, Francis J, Hardeman W, et al. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions. Ann Behav Med. 2013;46(1):81–95.
Dombrowski SU, O’Carroll RE, Williams B. Form of delivery as a key ‘active ingredient’in behaviour change interventions. Br J Health Psychol. 2016;21(4):733–40.
Download references
Acknowledgements
Not applicable.
The UK alcohol education charity Drinkaware provided payments to Mrs. Morris for her work on the review and members of the Drinkaware Research team Dr. Larsen and Dr. Catterall were undertaking work related to the review as part of their work hours. The funders of Drinkaware did not play any role in the in the design of the study and collection, analysis, and interpretation of data and in writing the manuscript. Professor Moss and Dr. Dombrowski undertook the work as part of their academic research roles, and with no payments provided.
Author information
Authors and affiliations.
Freelance researcher, Devon, UK
Hannah Morris
Drinkaware, Devon, UK
John Larsen & Emma Catterall
Centre for Addictive Behaviours Research, London South Bank University, Devon, UK
Antony C. Moss
Faculty of Kinesiology, University of New Brunswick, 90 Mackay Drive, Fredericton, New Brunswick, E3B 5A3, Canada
Stephan U. Dombrowski
You can also search for this author in PubMed Google Scholar
Contributions
JL initiated the idea for the study. All study authors were involved in deciding the scope and specific focus of the study. Database searching, screening and quality appraisal was undertaken by HM, JL and EC. AM and SD offered support and advice during this phase of the work. Analysis was undertaken primarily by HM and JL, with input from all study authors. The paper was drafted and written with contributions from all study authors. All authors read and approved the final manuscript
Corresponding author
Correspondence to Stephan U. Dombrowski .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
Mrs. Morris, Dr. Larsen and Dr. Catterall: Drinkaware is funded primarily by voluntary and unrestricted donations from UK alcohol producers, retailers and supermarkets, through an agreement between the UK government and the alcohol industry. The charity is governed independently by a Board of Trustees. The funders of Drinkaware had no involvement in or influence over the review.
Dr. Dombrowski: No conflicts of interest.
Professor Moss: No conflicts of interest.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1..
Full database search strategy.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Morris, H., Larsen, J., Catterall, E. et al. Peer pressure and alcohol consumption in adults living in the UK: a systematic qualitative review. BMC Public Health 20 , 1014 (2020). https://doi.org/10.1186/s12889-020-09060-2
Download citation
Received : 13 November 2019
Accepted : 04 June 2020
Published : 07 July 2020
DOI : https://doi.org/10.1186/s12889-020-09060-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Peer pressure
- Qualitative
- Evidence synthesis
BMC Public Health
ISSN: 1471-2458
- General enquiries: [email protected]

IMAGES
COMMENTS
This article synthesizes the evidence from cohort studies on the association between daily alcohol intake and risk of all-cause mortality. It finds that moderate alcohol consumption is not associated with lower mortality risk, and that the evidence is limited by selection biases and confounding factors.
Abstract. Background: Excessive alcohol consumption has negative effects not only on the drinkers' health but also on others around them. Previous studies suggest that excessive alcohol consumption can be related to a combination of factors such as age, family background, religiosity, etc. Investigating and clarifying these roots of alcohol consumption is crucial so that the right type of ...
Abstract. Alcohol consumption is known to be an addiction that provides negative outcomes mainly on health, excessive drinking of alcohol brings adverse effects on human health, also on activities ...
In this paper, we primarily discuss heavy drinking and AUD. Many measures of alcohol consumption (e.g., heavy drinking, binge drinking) and alcohol-related disorders (e.g., harmful drinking, alcohol dependence, AUD) are used, and often, these reflect geographical preferences. ... are an important direction for future research. Given that ...
Alcohol consumption, particularly heavier drinking, is an important risk factor for many health problems and, thus, is a major contributor to the global burden of disease. ... Alcohol Research ...
Alcohol consumption can influence an individual's quality of life, with the impact varying based on several factors such as the amount of alcohol consumed, frequency of consumption, individual ...
The stronger associations between mean alcohol intake and mortality observed in older adults with health-related risk factors make sense, since they have more morbid conditions potentially aggravated by alcohol and greater use of alcohol-interacting medications than their counterparts without health-related risk factors. 16,17 The fact that ...
In current drinkers of alcohol in high-income countries, the threshold for lowest risk of all-cause mortality was about 100 g/week. For cardiovascular disease subtypes other than myocardial infarction, there were no clear risk thresholds below which lower alcohol consumption stopped being associated with lower disease risk. These data support limits for alcohol consumption that are lower than ...
By use of methodological enhancements of previous iterations,1 the systematic analysis from the Global Burden of Diseases, Injuries, and Risk Factors Study (GBD) 2016 for 195 countries and territories, 1990-2016,2 is the most comprehensive estimate of the global burden of alcohol use to date. The GBD 2016 Alcohol Collaborators clearly demonstrate the substantial, and larger than previously ...
Even moderate drinking is linked to pathological changes in the brain Epidemiological studies often report better heath in moderate drinkers compared with abstainers. Observed first in studies of incidence of myocardial infarction,1 the "J shaped curve" (describing the graphical appearance of health measures plotted against consumption) reappears in studies of diabetes, stroke, and even ...
No direct relationships were found between need to belong or social connectedness and alcohol use, suggesting previous research exploring these relationships may have excluded control variables (e.g., biological sex, race/ethnicity) that better explain the impact of need to belong and social connectedness on alcohol use.
This paper shows how adding alcohol to a social situation transforms the outcome, both internally because of the physical effects due to the inscription of alcohol, and externally because alcohol becomes a factor that modifies the social meanings of situations (Latour, Citation 1994). Identifying mediators involve awareness of the factors that ...
Since 1976, when the National Institute on Alcohol Abuse and Alcoholism (NIAAA) issued its first report on alcohol misuse by college students, research advances have transformed our understanding of excessive drinking on college campuses and the negative outcomes that follow from it. For instance, we now know that a broad array of factors influence whether a particular college student will ...
Abstract. Prior research suggests that college drinking adversely affects education. While several studies have examined the effect of alcohol on the quantity of education using measures such as years of schooling completed, high-school graduation, or dropping out of college, this paper investigates the effect of alcohol use on the quality of education among college students.
The burden-weighted relative risk curves for alcohol use varied by region and age. Among individuals aged 15-39 years in 2020, the TMREL varied between 0 (95% uncertainty interval 0-0) and 0·603 (0·400-1·00) standard drinks per day, and the NDE varied between 0·002 (0-0) and 1·75 (0·698-4·30) standard drinks per day.
Only a small percent of individuals with alcohol use disorder contribute to the greatest societal and economic costs ().For example, in the 2015 National Survey on Drug Use and Health survey (total n = 43,561), a household survey conducted across the United States, 11.8% met criteria for an alcohol use disorder (n = 5124) ().Of these 5124 individuals, 67.4% (n = 3455) met criteria for a mild ...
Background Peer pressure to drink alcohol may influence excessive alcohol consumption, which can have adverse impacts on health and wellbeing. While peer pressure to drink alcohol is extensively studied among youth, less examination exists among adults. This systematic review examined qualitative research studies which explored the role and concept of peer pressure within the context of ...
Abstract. Alcohol abuse is reflected as a major public health concern in worldwide. It impaired many areas of life, including familial, vocational, psychological, legal, social, or physical ...
Alcohol use continues to be a major concern from preadolescence through young adulthood in the United States. Results of recent neuroscience research have helped to elucidate neurobiological models of addiction, substantiated the deleterious effects of alcohol on adolescent brain development, and added additional evidence to support the call to prevent and reduce underage drinking. This ...
Marcella Broccia and colleagues analyse 22 years of linked administrative and health data for all singleton babies born between 1996 and 2018 in Denmark to assess and quantify the association between maternal heavy alcohol use in the preconception period and during pregnancy, with prenatal, birth, and child health outcomes. 8,9 The first of their two papers focuses on obstetric and birth ...
ABSTRACT: Alcohol consumption is known to be an addiction that provides negative outcomes mainly on health, excessive drinking of alcohol brings adverse effects on human health, also on activities that focus on school performance. This research aims to examine the link between alcohol use and the academic success of high school students.
The result revealed that there is a significant relationship between alcohol consumption and academic performance (R 2 =0.74,P<.O5), there is a significant difference in academic performance of ...