Technology and Mental Health
This essay about the complex relationship between technology and mental health in modern society. It explores both the positive and negative impacts of technology on mental well-being, highlighting how social media can foster feelings of inadequacy while also discussing the benefits of telemedicine and mental health apps. The essay emphasizes the importance of maintaining a balanced approach to technology use to mitigate adverse effects and maximize its potential for mental health support.
How it works
In this era of digitalization, technology has interwoven itself into the very fabric of daily existence, profoundly shaping our interactions, occupations, and cognitive processes. While heralding a wave of positive metamorphoses, technology’s influence on mental well-being is intricate and multi-faceted. Grasping the nuances of how technology impacts mental health is imperative as we navigate the labyrinth of perpetual connectivity, endeavoring to strike a delicate balance between its advantages and potential psychological pitfalls.
A paramount repercussion of technology on mental well-being is the metamorphosis of social dynamics.
Social media platforms such as Facebook, Instagram, and Twitter have redefined interpersonal connections, rupturing geographical confines and fostering global discourse. Nonetheless, these platforms often curate an idealized façade of existence, engendering unrealistic comparisons and sentiments of inadequacy among users. Research indicates that prolonged exposure to idealized portrayals can precipitate heightened levels of anxiety and despondency, particularly among adolescents and young adults who are susceptible to external affirmation and peer juxtaposition.
Moreover, the perpetual connectivity facilitated by smartphones and the internet can engender information saturation and difficulty in disengagement, potentially exacerbating stress and obstructing mental equilibrium. The expectation of perpetual availability can disrupt the equilibrium between professional and personal life, diminishing the requisite personal respite vital for mental recuperation and intensifying feelings of overwhelm. This phenomenon, colloquially termed “technostress,” epitomizes a contemporary strain associated with the incapacity to adeptly manage novel technologies.
Conversely, technology has also heralded substantial strides in mental health care through telemedicine and mobile applications. Teletherapy services have surged in popularity, rendering therapeutic sessions accessible via video conferencing, thereby obliterating barriers to care such as geographical constraints and social stigma. Applications designed to monitor mood, foster mindfulness, and administer cognitive behavioral therapy exercises have emerged as instrumental aids in daily mental health management. These innovations democratize mental health support, rendering it more accessible to individuals who may have refrained from seeking assistance due to stigma or logistical impediments.
Furthermore, wearable technology equipped to monitor physiological metrics can play a pivotal role in mental health maintenance. Devices adept at tracking heart rate variability, sleep patterns, and physical activity furnish insights into one’s emotional and physical well-being, potentially alerting users to stressors or mental health regressions before they escalate. Such technology empowers individuals to assume control over their health and make well-informed decisions regarding when to seek professional intervention.
Notwithstanding these advantages, the crux lies in sustaining a harmonious equilibrium. The omnipresence of technology can precipitate addictive behaviors, with the dopamine-fueled reinforcement cycles inherent in social media usage posing a significant concern. These platforms are engineered to captivate users for protracted durations, potentially culminating in internet addiction—an unhealthy fixation on digital devices that detrimentally impinges upon life and relationships. Effectively managing technology usage to harness its merits while mitigating adverse repercussions is paramount for preserving mental well-being.
In summation, technology’s impact on mental health is a double-edged sword. While it introduces novel stressors into our milieu, it also furnishes innovative mechanisms for augmenting mental health accessibility and self-care. As we continue to assimilate technology into our quotidian existence, fostering cognizance of how digital habits shape our psychological welfare becomes increasingly imperative. Advocating for salubrious technology usage habits, delineating boundaries for connectivity, and leveraging technological tools to bolster, rather than undermine, mental well-being constitute pivotal strides in navigating this nascent terrain. As technology evolves incessantly, so too must our strategies for safeguarding mental health in an era of perpetual digital interconnectedness.

Cite this page
Technology And Mental Health. (2024, May 01). Retrieved from https://papersowl.com/examples/technology-and-mental-health/
"Technology And Mental Health." PapersOwl.com , 1 May 2024, https://papersowl.com/examples/technology-and-mental-health/
PapersOwl.com. (2024). Technology And Mental Health . [Online]. Available at: https://papersowl.com/examples/technology-and-mental-health/ [Accessed: 3 Sep. 2024]
"Technology And Mental Health." PapersOwl.com, May 01, 2024. Accessed September 3, 2024. https://papersowl.com/examples/technology-and-mental-health/
"Technology And Mental Health," PapersOwl.com , 01-May-2024. [Online]. Available: https://papersowl.com/examples/technology-and-mental-health/. [Accessed: 3-Sep-2024]
PapersOwl.com. (2024). Technology And Mental Health . [Online]. Available at: https://papersowl.com/examples/technology-and-mental-health/ [Accessed: 3-Sep-2024]
Don't let plagiarism ruin your grade
Hire a writer to get a unique paper crafted to your needs.

Our writers will help you fix any mistakes and get an A+!
Please check your inbox.
You can order an original essay written according to your instructions.
Trusted by over 1 million students worldwide
1. Tell Us Your Requirements
2. Pick your perfect writer
3. Get Your Paper and Pay
Hi! I'm Amy, your personal assistant!
Don't know where to start? Give me your paper requirements and I connect you to an academic expert.
short deadlines
100% Plagiarism-Free
Certified writers
- Bipolar Disorder
- Therapy Center
- When To See a Therapist
- Types of Therapy
- Best Online Therapy
- Best Couples Therapy
- Managing Stress
- Sleep and Dreaming
- Understanding Emotions
- Self-Improvement
- Healthy Relationships
- Student Resources
- Personality Types
- Sweepstakes
- Guided Meditations
- Verywell Mind Insights
- 2024 Verywell Mind 25
- Mental Health in the Classroom
- Editorial Process
- Meet Our Review Board
- Crisis Support
For Better or Worse, Technology Is Taking Over the Health World
For many people over the past year and a half, the world has existed primarily through a screen. With social distancing measures in place to protect individuals from becoming infected with the coronavirus, technology has stepped in to fill the void of physical connections. It’s also become a space for navigating existing and new mental health conditions through virtual therapy sessions, meditation apps, mental health influencers, and beyond.
“Over the years, mental health and technology have started touching each other more and more, and the pandemic accelerated that in an unprecedented way,” says Naomi Torres-Mackie, PhD , the head of research at The Mental Health Coalition , a clinical psychologist at Lenox Hill Hospital, and an adjunct professor at Columbia University. “This is especially the case because the pandemic has highlighted the importance of mental health for everyone as we struggle to make sense of an overwhelming new world and can find mental health information and services online.”
This shift is especially critical, with a tremendous spike occurring in mental health conditions. In the period between January and June 2019, 11% of US adults reported experiencing symptoms of an anxiety or depressive disorder. In January 2021, 10 months into the pandemic, in one survey that number increased to 41.1%. Research also points to a potential connection for some between having COVID-19 and developing a mental health condition—whether or not you previously had one.
The pandemic’s bridge between mental health and technology has helped to “meet the needs of many suffering from depression, anxiety, life transition, grief, family conflict, and addiction,” says Miyume McKinley, MSW, LCSW , a psychotherapist and founder of Epiphany Counseling, Consulting & Treatment Services.
Naomi Torres-Mackie, PhD
The risk of greater access is that the floodgates are open for anyone to say anything about mental health, and there’s no vetting process or way to truly check credibility.
This increased reliance on technology to facilitate mental health care and support appears to be a permanent one. Torres-Mackie has witnessed mental health clinicians drop their apprehension around virtual services throughout the pandemic and believes they will continue for good.
“Almost all therapists seem to be at least offering virtual sessions, and a good portion have transitioned their practices to be entirely virtual, giving up their traditional in-person offices,” adds Carrie Torn, MSW, LCSW , a licensed clinical social worker and psychotherapist in private practice in Charlotte, North Carolina.
The general public is also more receptive to technology’s expanded role in mental health care. “The pandemic has created a lasting relationship between technology, and it has helped increase access to mental health services across the world,” says McKinley. “There are lots of people seeking help who would not have done so prior to the pandemic, either due to the discomfort or because they simply didn’t know it was possible to obtain such services via technology.”
Accessibility Is a Tremendous Benefit of Technology
Every expert interviewed agreed: Accessibility is an undeniable and indispensable benefit of mental health’s increasing presence online. Torn points out, “We can access information, including mental health information and treatment like never before, and it’s low cost.”
A 2018 study found that, at the time, 74% of Americans didn’t view mental health as accessible to everyone. Participants cited long wait times, a lack of affordable options, low awareness, and social stigma as barriers to mental health care. The evolution of mental health and technology has alleviated some of these issues—whether it be through influencers creating open discussions around mental health and normalizing it or low-cost therapy apps . In addition, wait times may reduce when people are no longer tied to seeing a therapist in their immediate area.
While some people may still be apprehensive about trying digital therapy, research has shown that it is an effective strategy for managing your mental health. A 2020 review of 17 studies published in EClinicalMedicine found that online cognitive-behavioral therapy sessions were at least as effective at reducing the severity of depression symptoms than in-person sessions. There wasn’t a significant difference in participant satisfaction between the two options.
There Are Limitations to Mental Health and Technology’s Increasing Closeness
One of the most prevalent limitations of technology-fueled mental health care and awareness is the possibility of misleading or inaccurate information.
If you’re attending digital sessions with a therapist, it’s easy to check their qualifications and reviews. However, for most other online mental health resources, it can be more challenging but remains just as critical to verify their expertise and benefits. “The risk of greater access is that the floodgates are open for anyone to say anything about mental health, and there’s no vetting process or way to truly check credibility,” says Torres-Mackle.
To that point, James Giordano, PhD, MPhil , professor of neurology and ethics at Georgetown University Medical Center and author of the book “Neurotechnology: Premises, Potential, and Problems,” cautions that, while there are guiding institutions, the market still contains “unregulated products, resources, and services, many of which are available via the internet. Thus, it’s very important to engage due diligence when considering the use of any mental health technology .”
Verywell / Alison Czinkota
McKinley raises another valuable point: A person’s home is not always a space they can securely explore their mental health. “For many individuals, home is not a safe place due to abuse, addiction, toxic family, or unhealthy living environments,” she says. “Despite technology offering a means of support, if the home is not a safe place, many people won’t seek the help or mental health treatment that they need. For some, the therapy office is the only safe place they have.” Due to the pandemic and a general limit on private places outside of the home to dive into your personal feelings, someone in this situation may struggle to find opportunities for help.
Miyume McKinley, MSW, LCSW
There are lots of people seeking help that would not have done so prior to the pandemic, either due to the discomfort or because they simply didn’t know it was possible to obtain such services via technology.
Torn explains that therapists who work for tech platforms can also suffer due to burnout and low pay. She claims that some of these platforms prioritize seeing new clients instead of providing time for existing clients to grow their relationship. “I’ve heard about clients having to jump from one therapist to the next, or therapists who can’t even leave stops open for their existing clients, and instead their schedule gets filled with new clients,” she says. “Therapists are burning out in general right now, and especially on these platforms, which leads to a lower quality of care for clients.”
Screen Time Can Also Have a Negative Impact
As mental health care continues to spread into online platforms, clinicians and individuals must contend with society’s growing addiction to tech and extended screen time’s negative aspects.
Social media, in particular, has been shown to impact an individual’s mental health negatively. A 2019 study looked at how social media affected feelings of social isolation in 1,178 students aged 18 to 30. While having a positive experience on social media didn’t improve it, each 10% increase in negative experiences elevated social isolation feelings by 13%.
Verywell / Alison Czinkota
While certain aspects like Zoom therapy and mental health influencers require looking at a screen, you can use other digital options such as meditation apps without constantly staring at your device.
What to Be Mindful of as You Explore Mental Health Within Technology
Nothing is all bad or all good and that stands true for mental health’s increased presence within technology. What’s critical is being aware that “technology is a tool, and just like any tool, its impact depends on how it's used,” says Torres-Mackie.
For example, technology can produce positive results if you use the digital space to access treatment that you may have struggled to otherwise, support your mental well-being, or gather helpful—and credible—information about mental health. In contrast, she explains that diving into social media or other avenues only to compare yourself with others and avoid your responsibilities can have negative repercussions on your mental health and relationships.
Giordano expresses the importance of staying vigilant about your relationship with and reliance on tech and your power to control it.
With that in mind, pay attention to how much time you spend online. “We are spending less time outside, and more time glued to our screens. People are constantly comparing their lives to someone else's on social media, making it harder to be present in the moment and actually live our lives,” says Torn.
Between the increase in necessary services moving online and trying to connect with people through a screen, it’s critical to take time away from your devices. According to a 2018 study, changing your social media habits, in particular, can improve your overall well-being . Participants limited Instagram, Facebook, and Snapchat use to 10 minutes a day per platform for three weeks. At the end of the study, they showed significant reductions in depression and loneliness compared to the control group. However, even the increased awareness of their social media use appeared to help the control group lower feelings of anxiety and fear of missing out.
“Remember, it’s okay to turn your phone off. It’s okay to turn notifications off for news, apps, and emails,” says McKinley. Take opportunities to step outside, spend time with loved ones, and explore screen-free self-care activities. She adds, “Most of the things in life that make life worthwhile cannot be found on our devices, apps, or through technology—it’s found within ourselves and each other.”
Kaiser Family Foundation. The implications of COVID-19 for mental health and substance use .
Taquet M, Luciano S, Geddes JR, Harrison PJ. Bidirectional associations between COVID-19 and psychiatric disorder: retrospective cohort studies of 62 354 COVID-19 cases in the USA . Lancet Psychiatry . 2021;8(2):130-140. doi:10.1016/S2215-0366(20)30462-4
Luo C, Sanger N, Singhal N, et al. A comparison of electronically-delivered and face to face cognitive behavioural therapies in depressive disorders: a systematic review and meta-analysis . EClinicalMedicine . 2020;24:100442. doi:10.1016/j.eclinm.2020.100442
Primack BA, Karim SA, Shensa A, Bowman N, Knight J, Sidani JE. Positive and negative experiences on social media and perceived social isolation . Am J Health Promot . 2019;33(6):859-868. doi:10.1177/0890117118824196
Hunt MG, Marx R, Lipson C, Young J. No more FOMO: Limiting social media decreases loneliness and depression . J Soc Clin Psychol . 2018;37(10):751-768. doi:10.1521/jscp.2018.37.10.751

Transforming the understanding and treatment of mental illnesses.
Información en español
Celebrating 75 Years! Learn More >>
- Health Topics
- Brochures and Fact Sheets
- Help for Mental Illnesses
- Clinical Trials
Technology and the Future of Mental Health Treatment
How is technology used for mental health treatment.
Technology has opened a new frontier in mental health care and data collection. Mobile devices like cell phones, smartphones, and tablets are giving the public, health care providers, and researchers new ways to access help, monitor progress, and increase understanding of mental well-being.
Mobile mental health support can be very simple but effective. For example, anyone with a phone or computer can call, text, or chat the 988 Suicide and Crisis Lifeline at any time.
New technology can also be packaged into an extremely sophisticated app for smartphones or tablets. Such apps might use the device’s built-in sensors to collect information on a user’s typical behavior patterns. Then, if the app detects a change in behavior, it can signal that help is needed before a crisis occurs.
Some apps are stand-alone programs designed to improve memory or thinking skills. Other apps help people connect to a peer counselor or a health care professional.
Excitement about the huge range of opportunities technology offers for mental health treatment has led to a burst of development. Thousands of mental health apps are available in iTunes and Android app stores, and the number is growing every year. However, this new technology frontier includes a lot of uncertainty. There is very little industry regulation and very little information on app effectiveness, which can lead people to wonder which apps they should trust.
Before focusing on the state of the science and where it may lead, it’s important to look at the advantages and disadvantages of expanding mental health treatment and research into a mobile world.
What are the pros and cons of mental health apps?
Mental health apps and other technology have a lot of potential, both for people seeking mental health care and mental health professionals providing such services. Some advantages of mobile care technology include the following.
- Convenience : Allows treatment to take place anytime and anywhere, such as at home in the middle of the night or on a bus on the way to work, making it ideal for people who have trouble getting to in-person appointments
- Anonymity : Lets people receive treatment anonymously and privately from the comfort of their homes
- Introduction to care : Acts as a good first step for people who have been reluctant to seek mental health care in the past
- Lower cost : Makes care more affordable through apps that are free or cheaper than traditional in-person care
- Greater outreach : Helps mental health professionals offer treatment to people in remote areas or to large numbers of people in times of sudden need, like after a natural disaster or traumatic event
- Interest : Encourages people to continue therapy by making care more appealing and accessible than traditional in-person treatment
- 24-hour service : Provides around-the-clock monitoring or intervention support
- Consistency : Offers the same treatment program to all people
- Support : Complements traditional therapy by extending in-person sessions, reinforcing new skills, and providing support and monitoring
- Data collection : Collects information, such as location, movement, phone use, and other data
Mental health technology offers great opportunities but also raises concerns. Addressing potential problems will be essential to ensuring that new apps provide benefits without causing harm. Although apps are becoming more appealing and user-friendly, we need more information on their effectiveness.
The following are some limitations of the technology that researchers and developers are trying to answer questions about.
- Effectiveness : Is the app supported by scientific evidence showing that it works and works as well as traditional in-person methods?
- Audience : Does the app work equally well for all people it is meant to help?
- Privacy : How does the app maker guarantee users’ privacy, considering many apps deal with sensitive personal information?
- Guidance : How do people determine if an app is effective when no industry-wide standards exist for evaluating quality?
- Regulation : Who should regulate mental health technology and the data it generates?
- Overselling : Does the app promise more than it delivers and turn people away from using other, more effective therapies?
What are current trends in app development?
Research and engineering teams are combining their skills to address a wide range of mental health concerns. For instance, intervention apps may help people quit smoking; manage symptoms of anxiety, depression, eating disorders, post-traumatic stress, or insomnia; and more. Some popular areas of app development include the following.
Self-management
Self-management apps involve people putting information into the app to receive feedback. For example, they might use the app to set medication reminders or access tools for managing stress, anxiety, or sleep problems. Some software can use additional equipment to track heart rate, breathing patterns, blood pressure, and so forth to help people monitor their progress and receive feedback.
Improve thinking skills
Cognitive remediation apps help people improve their thinking skills. These apps are often designed for people with serious mental illnesses who may have distorted or unhelpful ways of thinking or hold inaccurate beliefs.
Skill training
Skill training apps may feel more like games than other mental health apps as they help people learn new coping or thinking skills. These apps might involve watching an educational video about anxiety management or the importance of social support, for example. People then pick new strategies to try and use the app to track how often they practice those new skills.
Illness management and supported care
Illness management and supported care apps provide additional support by allowing people to interact with another person. The app may connect people with peer support or send information to a trained health care provider who can offer guidance and therapy options. Researchers are working to learn how much human interaction people need for app-based treatments to be effective.
Passive symptom tracking
Symptom tracking apps collect data using the sensors built into smartphones. The sensors might record movement patterns, social interactions (such as the number of texts and phone calls), behavior at different times of day, vocal tone and speed, and more. In the future, apps may be able to analyze these data to determine a person’s real-time state of mind. Such apps may also recognize changes in behavior patterns that signal an episode of mania, depression, or psychosis before it occurs. Although an app may not replace a mental health professional, it can alert caregivers when someone needs additional help. The goal is to create apps that support a range of people, including those with serious mental illnesses.
Data collection
Data collection apps gather data without any help from the person using them. Receiving widescale information from many people at the same time can increase researchers’ understanding of mental health and help them develop better interventions.
Conducting research
Apps can help conduct research. For example, Dr. Patricia Areán’s pioneering BRIGTHEN study showed that research via a smartphone app is a reality. The BRIGHTEN study was remarkable because it used technology to both deliver treatment and conduct research. In other words, the research team used technology to recruit, screen, enroll, treat, and assess participants. BRIGHTEN was especially exciting because the study showed that technology can be an efficient way to test promising new treatments, while also highlighting the need to make those treatments engaging.
If you or someone you know is struggling or having thoughts of suicide, call or text the 988 Suicide and Crisis Lifeline at 988 or chat at 988lifeline.org . In life-threatening situations, call 911 .
Who creates mental health apps?
Developing mental health apps and other technology requires a partnership between mental health professionals and software engineers. Researchers have found that interventions are most effective when people like them, are engaged in them, and want to continue using them. Behavioral health apps work best when they combine engineers’ skills for making an app easy to use and entertaining with providers’ skills for providing effective treatment options. Researchers and engineers are developing and testing apps that do everything from manage medications to teach coping skills to predict when someone may need emotional help.
Who evaluates mental health apps?
There are no review boards, checklists, or widely accepted rules for evaluating or choosing a mental health app or other technology. Most apps do not have peer-reviewed research to support their claims, and it is unlikely that every mental health app will go through a randomized clinical research trial to test its effectiveness. One reason is that testing is a slow process, and technology evolves quickly. By the time an app has been put through rigorous scientific testing, the original technology may be outdated.
Currently, there are no national standards for evaluating the effectiveness of the hundreds of available mental health apps. People should be cautious about trusting an app. However, there are a few suggestions for finding an app that may work for you:
- Ask a trusted health care provider for a recommendation. Some larger providers may offer several apps and collect data on their use.
- Check to see if the app offers recommendations for what to do if symptoms get worse or there is a psychiatric emergency. Know how to get help if needed.
- Decide if you want an app that is completely automated versus an app that offers opportunities for contact with a trained professional.
- Search for information on the app developer, including their credentials and experience.
- Beware of misleading logos. The National Institute of Mental Health (NIMH) has not developed and does not endorse any apps. However, some app developers have unlawfully used the NIMH logo to market their products.
- Search the PubMed database offered by the National Library of Medicine. This resource contains articles on a wide range of research topics, including mental health app development.
- If you cannot find information about a particular app, check to see if the app is based on a treatment that has been tested. For example, research has shown that internet-based cognitive behavior therapy (CBT) is as effective as conventional CBT for disorders that include depression, anxiety, social anxiety disorder, and panic disorder.
- Try it. If you’re interested in an app, test it for a few days and decide if it’s easy to use, holds your attention, and is something you want to continue using. An app is only effective if it keeps you engaged.
What is NIMH’s role in research on mental health intervention technology?
NIMH has awarded over 400 grants for technology-enhanced mental health interventions. NIMH staff continue to actively review and evaluate research grants related to mental health technology.
These grants have focused on many areas, including:
- Feasibility, efficacy, and effectiveness research, such as developing and refining new treatments and interventions
- Technology for addressing a wide range of mental disorders, such as schizophrenia, HIV, depression, anxiety, autism, suicide, eating disorders, and trauma
- Interventions for cognitive issues, illness management, problematic behavior, and health communication
- More accessible and engaging ways to deliver therapies or skill development (for example, interactive formats or game-like approaches) and apps that work on any device
- Incorporating real-time, face-to-face contact or remote counseling (phone or online) with peers and professionals to provide a balance between technology and human touch
- Active and passive mobile assessment and monitoring
- Artificial intelligence (AI) tools and technologies
A significant portion of NIMH funding for these types of technologies is through the NIMH Small Business Innovation Research (SBIR) and Small Business Technology Transfer (STTR) Programs .
In addition, NIMH created the National Advisory Mental Health Council workgroup on Opportunities and Challenges of Developing Information Technologies on Behavioral and Social Science Clinical Research to track and guide this rapidly changing area. In 2017, the workgroup released a report reviewing the opportunities for and challenges of using new information technologies to study human behaviors relevant to the NIMH mission.
NIMH voiced its interest in this research area in a 2022 notice of special interest . The notice called for research on the utility and validity of digital health and AI tools and technologies in epidemiological, clinical, and intervention research.
How can I find a clinical trial on mental health intervention technology?
Clinical trials are research studies that look at new ways to prevent, detect, or treat diseases and conditions. The goal of a clinical trial is to determine if a new test or treatment works and is safe. Although people may benefit from being part of a clinical trial, they should know that the primary purpose of a clinical trial is to gain new scientific knowledge so that others may be better helped in the future.
Researchers at NIMH and around the country conduct many studies with patients and healthy volunteers. We have new and better treatment options today because of what clinical trials have uncovered. Be part of tomorrow’s medical breakthroughs. Talk to a health care provider about clinical trials, their benefits and risks, and whether one is right for you.
To learn more or find a study, visit:
- NIMH’s Clinical Trials webpage : Information about participating in clinical trials
- Clinicaltrials.gov: Current Studies on Mental Health Intervention Technology : List of clinical trials funded by the National Institutes of Health being conducted across the country
Where can I learn more about mental health intervention technology?
Federal resources.
- What Is Telemental Health? (NIMH Fact Sheet)
- How Can You Protect and Secure Health Information When Using a Mobile Device? (Department of Health and Human Services)
- How To Protect Your Privacy on Apps (Federal Trade Commission)
- Device Software Functions Including Mobile Medical Applications (U.S. Food and Drug Administration)
- NIH All of Us Research Program : This big-data initiative aims to recruit one million adult volunteers to share a variety of data, including electronic health records, health and family medical histories, and biological samples, to support research and uncover paths to the delivery of precision medicine.
- The BRAIN ® Initiative : The Brain Research Through Advancing Innovative Neurotechnologies® Initiative, or The BRAIN® Initiative, funds the development of a wide variety of new technologies to help unlock the mysteries of the human brain.
- NIMH SBIR and STTR Funding Opportunities : The NIMH SBIR and STTR Programs are among the largest sources of early stage capital for technology commercialization in the United States.
- Digital Global Mental Health Program : This program supports research on the development, testing, implementation, and cost-effectiveness of digital mental health technologies that are appropriate for low- and middle-income countries.
Science news
- Opportunities and Challenges of Developing Information Technologies on Behavioral and Social Science Clinical Research (NIMH National Advisory Mental Health Council Report)
- Chatbot Encourages People With Eating Disorders to Seek Care (NIMH Research Highlight)
- Driving Innovation in Mental Health Technology Through Small Business Programs (NIMH Director Message)
- Mindful Mood Balance Effective for Treating Residual Depressive Symptoms and Suicidal Ideation (NIMH Research Highlight)
- Smartphone Data May Not Reliably Predict Depression Risk in Diverse Groups (NIMH Research Highlight)
- Understanding the Availability of Mental Telehealth Services (NIMH Research Highlight)
Other resources
The non-federal resources listed below are included for information purposes only. This is not a comprehensive list, and a resource’s inclusion on the list does not constitute an endorsement by NIMH.
- One Mind PsyberGuide : Website run by a nonprofit organization of experts who provide reviews of computer and device-assisted therapies for mental illnesses, focusing on their credibility, user experience, and transparency of privacy practices
- What You Need to Know Before Choosing Online Therapy (American Psychological Association)
Last Reviewed: August 2024
Unless otherwise specified, the information on our website and in our publications is in the public domain and may be reused or copied without permission. However, you may not reuse or copy images. Please cite the National Institute of Mental Health as the source. Read our copyright policy to learn more about our guidelines for reusing NIMH content.
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Topic collections
- BMJ Journals
You are here
- Volume 26, Issue 1
- Digital mental health: challenges and next steps
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- http://orcid.org/0000-0003-2679-1472 Katharine A Smith 1 , 2 , 3 ,
- Charlotte Blease 4 , 5 ,
- http://orcid.org/0000-0002-0462-6444 Maria Faurholt-Jepsen 6 , 7 ,
- Joseph Firth 8 , 9 ,
- http://orcid.org/0000-0001-9237-9297 Tom Van Daele 10 ,
- http://orcid.org/0000-0003-0541-4846 Carmen Moreno 11 ,
- http://orcid.org/0000-0002-2172-8813 Per Carlbring 12 ,
- Ulrich W Ebner-Priemer 13 , 14 ,
- Nikolaos Koutsouleris 15 , 16 , 17 ,
- Heleen Riper 18 , 19 , 20 ,
- Stephane Mouchabac 21 , 22 ,
- http://orcid.org/0000-0002-5362-7937 John Torous 4 ,
- http://orcid.org/0000-0001-5179-8321 Andrea Cipriani 1 , 2 , 3
- 1 Department of Psychiatry , University of Oxford , Oxford , UK
- 2 Oxford Health NHS Foundation Trust , Oxford , UK
- 3 Oxford Precision Psychiatry Lab , NIHR Oxford Health Biomedical Research Centre , Oxford , UK
- 4 Division of Digital Psychiatry, Beth Israel Deaconess Medical Center , Harvard Medical School , Boston , Massachusetts , USA
- 5 Participatory eHealth and Health Data Research Group, Department of Women's and Children's Health , Uppsala University , Uppsala , Sweden
- 6 Copenhagen Affective Disorder Research Center (CADIC) , Psychiatric Center Copenhagen , Frederiksberg , Denmark
- 7 Department of Clinical Medicine , Faculty of Health and Medical Sciences , University of Copenhagen , Denmark
- 8 Division of Psychology and Mental Health, Manchester Academic Health Science Centre , The University of Manchester , Manchester , UK
- 9 Manchester Academic Health Science Centre , Greater Manchester Mental Health NHS Foundation Trust , Manchester , UK
- 10 Expertise Unit Psychology, Technology and Society , Thomas More University of Applied Sciences , Mechelen , Belgium
- 11 Department of Child and Adolescent Psychiatry, Institute of Psychiatry and Mental Health, Hospital General Universitario Gregorio Marañón, IiSGM, CIBERSAM, ISCIII , Universidad Complutense de Madrid Facultad de Medicina , Madrid , Spain
- 12 Department of Psychology , Stockholm University , Stockholm , Sweden
- 13 Mental mHealth Lab, Institute of Sports and Sports Science , Karlsruhe Institute of Technology , Karlsruhe , Germany
- 14 mHealth Methods in Psychiatry, Department of Psychiatry and Psychotherapy, Medical Faculty Mannheim, Central Institute of Mental Health , Heidelberg University , Heidelberg , Germany
- 15 Department of Psychiatry and Psychotherapy , Ludwig Maximilian University of Munich , München , Germany
- 16 Institute of Psychiatry, Psychology and Neuroscience , King's College London , London , UK
- 17 Max-Planck Institute of Psychiatry , Munich , Germany
- 18 Department of Clinical, Neuro and Developmental Psychology , Vrije Universiteit Amsterdam , Amsterdam , Netherlands
- 19 Department of Psychiatry, Amsterdam Public Health Research Institute , Amsterdam University Medical Centre , Duivendrecht , Netherlands
- 20 Department of Psychiatry , University of Turku , Turku , Finland
- 21 Department of Psychiatry, Hôpital Saint-Antoine , Sorbonne Université , Paris , France
- 22 Infrastructure for Clinical Research in Neurosciences (iCRIN), Brain Institute (ICM), INSERM, CNRS, Hôpital de la Pitié Salpêtrière , Sorbonne Université , Paris , France
- Correspondence to Dr Katharine A Smith, Department of Psychiatry, University of Oxford, Oxford OX3 7JX, UK; katharine.smith{at}psych.ox.ac.uk
Digital innovations in mental health offer great potential, but present unique challenges. Using a consensus development panel approach, an expert, international, cross-disciplinary panel met to provide a framework to conceptualise digital mental health innovations, research into mechanisms and effectiveness and approaches for clinical implementation. Key questions and outputs from the group were agreed by consensus, and are presented and discussed in the text and supported by case examples in an accompanying appendix. A number of key themes emerged. (1) Digital approaches may work best across traditional diagnostic systems: we do not have effective ontologies of mental illness and transdiagnostic/symptom-based approaches may be more fruitful. (2) Approaches in clinical implementation of digital tools/interventions need to be creative and require organisational change: not only do clinicians and patients need training and education to be more confident and skilled in using digital technologies to support shared care decision-making, but traditional roles need to be extended, with clinicians working alongside digital navigators and non-clinicians who are delivering protocolised treatments. (3) Designing appropriate studies to measure the effectiveness of implementation is also key: including digital data raises unique ethical issues, and measurement of potential harms is only just beginning. (4) Accessibility and codesign are needed to ensure innovations are long lasting. (5) Standardised guidelines for reporting would ensure effective synthesis of the evidence to inform clinical implementation. COVID-19 and the transition to virtual consultations have shown us the potential for digital innovations to improve access and quality of care in mental health: now is the ideal time to act.
Data availability statement
All data relevant to the study are included in the article or uploaded as supplementary information.
This is an open access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited, appropriate credit is given, any changes made indicated, and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/ .
https://doi.org/10.1136/bmjment-2023-300670
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
Introduction: state of the art and beyond in digital mental health, and current challenges
New innovations, such as digital phenotyping and apps as prevention and treatment interventions, hold tremendous potential in mental health. 1 However, emerging evidence suggests the need for high-quality validation, real-world clinical outcomes, implementation data and a clear vision to ensure such innovations have an ethical and transformative impact on patient outcomes. 2 3
Psychiatry and psychology are constantly evolving fields, with COVID-19 forcing a rapid switch to virtual visits. 4 5 While this transition has had advantages, the projected benefits around increased access and better quality of care have generally not yet been realised for several reasons. 6 Virtual visits are a form of synchronous telehealth and thus access is still limited by the number of clinicians 1 and by digital divides between those who can meaningfully engage with virtual visits and those who cannot. 7 They also require clinician training and patient guidance for optimal benefit and this has been, and often continues to be, lacking. 6 8 In addition, virtual visits do not specifically focus on prevention, which is the only scalable means to reduce demand. 3
By learning from the transition to virtual visits during the COVID-19 pandemic, we can see that now is the ideal time to prepare for the next generation of innovations which will advance the field. Additional and supplementary routes or methods to allow for a more flexible, ‘just-in-time’ and early intervention access to care include digital phenotyping, ecological momentary assessment (EMA), apps, real-time analysis, artificial intelligence (AI) approaches, virtual reality and blended decision-making, but each presents scientific, clinical, ethical and regulatory challenges. In addition, research into the feasibility and utility of integrating these digital techniques into a clinical setting is still just beginning.
The aim of this paper is to offer researchers, clinicians, patients and policy makers a framework to conceptualise the development of digital mental health beyond virtual consultations and its implementation in routine clinical care, to improve access and precision in treatments and outcomes. In providing a framework, we were aware that the scope is very broad and we could not include all advances in digital mental health. While this approach provides advantages in identifying some possible solutions across subspecialties, we acknowledge this has limitations and we do not attempt to cover every innovation in detail, but rather to highlight general principles which may be helpful for all approaches, with examples of case studies to illustrate these. With this broad focus, we aimed to explore and discuss core challenges in gathering and interpreting data and designing implementation strategies, key issues and themes that have emerged across the field in the last few years, and some potential solutions.
We used a consensus development panel approach 9 10 following the methodology described and used by the US National Institutes of Health 11 and WHO. 10 12 This method of consensus formation was chosen as it is most appropriate for identifying general areas of challenge and uncertainty, and formulating broad strategic plans. This is in contrast to the aim of achieving specific decision-making criteria or protocols, which are the focus of alternative approaches such as the Delphi technique or nominal group process. 13 Other advantages are that because the relevant literature and data are collected and circulated in advance of the meeting, the consensus development panel method is more evidence based (rather than on personal experience) and enables a multidisciplinary approach, which is critical in such a fast-moving and novel area.
A core team of panellists (KAS, AC, JT) identified experts with expertise in a variety of specialist areas within digital mental health and invited them to join the process. The 12 panellists were chosen to be representative across different disciplines and professional backgrounds and offered expertise in many specialised and general fields of digital psychiatry, including: digital phenotyping and EMA, blended cognitive–behavioural therapy approaches, virtual consultations, clinical decision-making, AI approaches, ethics, methodology and placebo choice, lifestyle and physical interventions, evidence synthesis, special populations including adolescents, transdiagnostic approaches and codesign. The group composition was gender balanced and professional backgrounds included psychiatry, psychology, methodology, evidence synthesis and ethics. The panel of experts was international (including Belgium, the Netherlands, UK, France, Spain, USA, Denmark, Germany, Sweden).
In advance of the meeting the experts were asked to provide information on their specialised area of digital mental health (or more broadly) in the form of a short abstract supported by up to five references which they considered to be the key references in the last 2–3 years. This was supported by a literature review using PubMed to search for terms relevant to the main themes identified by the experts. This preliminary work identified the areas of recent development, uncertainties or challenges which formed the agenda for the questions to be addressed in the face-to-face meeting. The meeting was held in Rome over 2 days in December 2022. Each expert gave a brief presentation including shared slides, methodology, analysis of data and relevant citations, followed by whole group discussion of their particular topic. The meeting was facilitated by two panel members (JT and AC) and recorded and summarised by KAS. At the end of each day a summary was prepared in discussion with the whole group to agree to the key consensus points, areas of uncertainty and next challenges. The main themes identified were:
Challenges in techniques for gathering and analysing new data (eg, using digital phenotyping, EMA, transdiagnostic or machine learning approaches).
Challenges in designing interventions (including the choice of placebo, and preventative interventions, such as physical health interventions in those with mental illness).
Challenges in combining real-time assessments with intervention.
Challenges in implementation in the real-world clinical setting (including clinical decision-making, education and training and policies in organisations and healthcare systems).
Challenges in developing implementation studies (including reporting guidelines, accessibility and codesign, ethics and potential harms, specialised groups).
Just as important were the agreed decisions about what could not be included in the current consensus. It was also decided by the group that the output of the panel would be a coauthored consensus paper of the overarching challenges, with case studies of specific examples and solutions in the online supplemental appendix . Each panellist was asked to provide a case example illustrating a key challenge in their area.
Supplemental material
The meeting was supported externally (by Angelini Pharma and Excerpta Medica). However, to avoid any potential conflict of interest, neither organisation had any input into the design of the meeting, the identification or selection of the experts, the agenda of the meeting, discussions, consensus or output.
We also performed a series of PubMed searches using keywords relevant to the themes and initial consensus areas identified by the group. Because of the broad scope of the themes addressed and the novelty of the field, consensus was not predefined by percentage. Instead, it was agreed in advance of the meeting that either full consensus would be achieved, or where there was disagreement, this would be reported. 14 An iterative process was then used to reach a consensus on the details of key themes. Question and answers were posed among the group with discussion on key messages. Case examples to illustrate each point were reviewed by the group before they were included in the online supplemental appendix . All experts participated in this process before finalising the consensus summarised here.
Presentation
Theme 1: challenges in techniques for gathering new data, assessments in daily life: digital phenotyping and ema.
Understanding patients’ unique lived experience of their condition is critical to delivering the best care. Momentary real-life assessments such as digital phenotyping and EMA provide a rich source of data to complement information gathered from directly asking people how they feel (see online supplemental appendix table 1 for definitions and case examples). The real-time nature of these assessments promises to avoid several of the recall biases seen in other methods of symptom reporting, 15 and also the issue of ‘back-filling’, commonly seen with paper diaries. 16 When combined with digital phenotyping we can also access new data like environmental factors and mobility patterns (eg, how real-life urban green space exposure and amount of movement may impact mental health symptoms 17 ).
Digital phenotyping (in its broadest definition) is therefore a promising route to supplement clinical decision-making and reduce bias. From these data we have already learnt that momentary real-life patient data (eg, on alcohol use) may not match some of our assumptions about behaviour or traditional views of clinical symptoms over time. 18 Although this discrepancy might be expected, given that recall biases are avoided, systematic evidence that real-time models are more accurate than traditional clinical symptom assessment is still in progress. To date, studies of clinical validation have been scarce, as although digital phenotyping allows for an extensive and broad range of personal data, demonstrating its use and validity in the clinic is challenging especially when many outcomes are personalised. This is particularly so for passive data measures as, unlike standardised diagnostic interview or questionnaire-based measures which are used routinely in clinical trials and outcome management, agreed standards have not been defined for clinical validation of passive digital phenotyping. 19 In addition, standardised approaches have not been uniformly applied to assess how advanced analytical methods, including machine learning algorithms, could be used to reduce the complexity of active and passive phenotyping data to deliver clinically actionable predictive models. 20 For either focus, we need to be careful to avoid ‘black box’ machine learning models that do not explain ‘why’, as this explanation is necessary now for regulatory approval and clinical acceptance and uptake.
Transdiagnostic approaches
One solution to assessing clinical validity is to approach digital phenotyping in a more transdiagnostic manner. For example, in addition to searching for the digital marker of mania in bipolar disorder, markers of clinical transition across states (eg, stable to unstable) are also clinically important and can be followed in large population-based cohorts (see online supplemental appendix table 1 for examples). The digital phenotyping data could add new context and meaning to a core set of high-quality clinical assessments or more gold-standard measurements.
This combination is important as although digital phenotyping data may have high reliability, as noted its clinical validity has been sparingly investigated. The transdiagnostic approach may therefore address the challenge of trying to directly associate a new digital signal with a biological endpoint, as although in some areas the results are promising, there have also been examples of inconsistencies in associating particular metrics (such as sleep measures or screen time) with mental health disorders. 19 One approach would be new prospective studies, but an alternative or complementary strategy could also be to focus more urgently on developing and implementing agreed standards for measuring and reporting digital phenotyping. 2 This would allow data sets to be combined and results replicated and validated across illnesses.
A transdiagnostic approach is also particularly useful in patient populations where diagnostic boundaries are more fluid or in which the impact of development needs to be considered, such as the adolescent population or those with early psychosis (see online supplemental appendix table 2 ).
Machine learning approaches
In parallel with the rapid development of digital phenotyping technology, machine learning methods have emerged as powerful tools to explore high-dimensional, time-series data, such as electroencephalography, resting-state functional MRI or natural language. Machine learning (see online supplemental appendix table 3 ) can be used in this way to ‘make sense’ of digital phenotyping-based big data. However, there are challenges in translating this use to clinical settings, 20 often because the underlying data are not well understood, or the preprocessing steps have made bold assumptions that lack clinical nuance.
Theme 2: challenges in designing interventions
While digital phenotyping and EMA offer a new window into the lived experience of mental illness, using this and new digital modalities to deliver care and new interventions remain an area which needs increased focus. With thousands of health apps and new digital innovations gaining momentum, it is appropriate to consider broader issues around the assessment of their quality and efficacy. As health regulators around the world struggle to assess the ‘true’ effect of new treatments, the importance of placebo-controlled studies for interventions has expanded. Likewise, the focus on innovative digital software to deliver preventative interventions and complex therapies has also raised interest in gaining a better understanding of how interventions actually work.
Choice of placebo
The choice of a placebo is a key element in assessing the effectiveness of an intervention (see online supplemental appendix table 4 for further details), but there is often a lack of placebo literacy in digital health, with considerable variability in how placebos are designed or described. 21 In digital mental health research contexts, investigators should decide in advance what they consider to be the locus of treatment. Rigorous placebos should then be designed that match factors such as the length and number of sessions of the active intervention, the aesthetic features of the interface, contextual features (such as interactivity), training and rationale, and assessing patients’ views of whether they believe they are in the control or treatment group. 22 If necessary, so-called dismantling or additive studies, which incrementally examine the effectiveness of components of the active intervention, 22 could also be devised (see online supplemental appendix table 4 ). While designing placebos is methodologically challenging, this does not abnegate responsibility for due diligence: without adequate controls, researchers, and as a consequence, clinicians, risk overestimating the therapeutic effectiveness of digital mental health treatments.
Preventative interventions: physical health interventions in those with mental illness
The delivery of preventative/behavioural health interventions in the general population is increasingly relying on digital technologies. People with severe mental illness (SMI) are known to be at higher risk of physical health problems, but the use of digital innovations to improve physical health in mental health populations has still not been widely considered. 23 Some examples of interventions are provided in online supplemental appendix table 5 , and these could provide improvements in both the physical and mental health of people with SMI. However, evidence in this area is still nascent, and further research must be directed towards establishing the effectiveness of digital lifestyle intervention in mental illness, along with developing pathways for real-world implementation.
Theme 3: challenges in combining real-time assessments with intervention
Innovations in digital phenotyping and new digital interventions offer synergistic potential. Symptoms are often assessed as relatively slow-moving features, but in fact, they fluctuate frequently over time. Dynamic assessment of mood and behaviour using real-time analysis can be combined with intermittent, but more detailed information which is ‘triggered’ by a significant change. This can be used to assess ‘response’ to the change (eg, a move from one space to another) or to identify a change in behaviour (eg, increased phone calls in the days before a manic episode) which might predict relapse, and prompt a call from a clinician. Just-in-time adaptive interventions (JITAIs) show great potential, but as yet there is a scarcity of clinical examples in mental health. 24 Online supplemental appendix table 6 outlines this in more detail with some examples.
Theme 4: challenges in implementation in the real-world clinical setting
Clinical decision-making.
While JITAIs are not ready for routine clinical use today, there are applications for novel digital technologies. One model is to use these new digital data to inform clinical decision-making and guide shared care decisions, for example, in medication monitoring. While digital data are not a replacement for clinical judgement, they can provide additional information and may help identify or confront bias 25 (see online supplemental appendix table 7 for further discussion and examples). There are several areas to consider for successful implementation; at the clinical level these include the importance of shared decision-making with the patient, speaking the same language and measuring what patients see as important. 26 The decision when to use this, for example, as a population-level screening tool or a tool to confirm clinical suspicion of a condition, needs further data. Clinicians will need to work synergistically with new methods of measurement to inform diagnosis and also perhaps to inform predictions of illness in high-risk individuals. This synergy will also need to assess how the new measurements could effectively work in concert with biological measures such as neuroimaging, genetics or electroencephalography.
Education and training
At the fundamental level, this involves directly and continuously teaching and training clinicians. The lack of digital literacy and formal training among medical students and clinicians remains an ongoing but often overlooked concern. 27 A future challenge is to make better use of available technologies, as well as anticipating future innovations. Given the potential of asynchronous healthcare tools, this also means, for example, creating protocolised treatment manuals that allow non-clinicians to deliver aspects of the treatment in hybrid models of care. It is important to learn from hybrid and online care models that we need to continue to help people to be ‘ready’ for change and ensure there is some ‘alliance’ as active ingredients in any successful therapy. 5 Patients can also benefit from training programmes designed to teach them how to use digital health technologies and increase confidence in general digital skills. 1
How clinicians combine and use digital tools remains a nascent area of exploration. It is unclear how these tools may influence biases or stereotypes held by clinicians, or how effectively digital data are incorporated into routine clinical practice to help mitigate these biases. However, it is generally accepted that clinicians’ attitudes and lack of knowledge towards technology strongly influence its adoption in clinical practice, and so better knowledge and training are needed. 8 28 Knowledge and training can help increase a clinician’s willingness to use technology by influencing known moderators like the expected effort or performance to make use of technology in clinical practice. However, the presence or absence of facilitating conditions such as infrastructure or organisational contexts can also have a significant impact.
Policies in organisations and healthcare systems
In order to fully leverage the benefits of digital mental health, organisations are looking at ways to adapt their workforce and processes. Digital mental health has the potential to provide ongoing support and guidance for both patients and clinicians, and the creation of positions such as digital navigators 1 can help facilitate their use, in the same manner as radiology and pathology technicians play a key role in their respective fields. Hybrid clinics provide an example of a new model of care where a clinician works with a team of digital navigators flexibly combining synchronous and asynchronous digital tools as well as traditional face-to-face assessment. These digital approaches need to be manualised and further research is needed on key parameters such as the duration of treatment, ‘dose’, and exposure as well as effectiveness and cost efficiency. However, with more human involvement, issues around low engagement and missing data may become less acute. While we do not want to ignore chatbots and similar technologies that remove the human, the lack of high-quality data on engagement or outcomes at this time does not make these a viable clinical option yet. 29
Policy makers need also to consider factors outside the clinic in order to integrate these technologies more fully into the mental healthcare system. These include providing proper reimbursement for their use and the costs of staffing and infrastructure, in order to ensure successful implementation and continued use. 1 30
Theme 5: challenges in developing implementation studies
Having identified some of the challenges, the immediate priorities are now to address the potential barriers to the implementation of digital mental health interventions in the real-world clinical setting. First, there are particular questions which need to be considered in the design, reporting and analysis of implementation studies, such as standardisation of outcomes, methods and conceptual frameworks.
Reporting guidelines
Questions such as the design, dose and intensity of an intervention, or the exact type of data collected may be poorly described or lacking in studies of digital observation and intervention, although reporting guidelines have been proposed. 15 31 In addition, information on fidelity to interventions, and updates or technical issues of the digital tools may not be well described. This makes it difficult to compare outcomes across studies: implementation of agreed guidelines for reporting would standardise approaches and allow reliable synthesis of the data to inform clinical practice.
In addition, we lack effective ontologies of mental illnesses, so mapping new data onto current ontologies may not be productive. Ontologies are standard representations of the subject matter of a domain that allow clarity in what is being referred to through provision of unambiguous definitions. They offer a comprehensive computable semantic framework complete with labels and synonyms, definitions and examples, relationships between entities and other meaningful logical axioms. Semantic frameworks broadly interpreted, including ontologies and other kinds of semantic resources such as controlled vocabularies, are not new to the mental health domain and encompass widely used tools such as the Diagnostic and Statistical Manual of Mental Disorders. However, these have so far been developed in isolation to represent distinct perspectives and are not inter-related, thus are not suitable for use in comprehensive and integrative evidence synthesis efforts. Integrative, cross-disciplinary ontologies are therefore essential to enhance the discoverability and interoperability of evidence and reduce fragmentation, as well as driving cost-saving automation. An agreed ontological framework for reporting outcomes in digital mental health would also help focus on the core features to be measured and provide a common language for reporting studies. There is already an established literature on how to develop an ontological framework which could be applicable here. 32
Accessibility and codesign
As a first step for any clinical implementation (and the research studies associated with this), innovations need to be truly accessible for the populations they are aiming to reach. In the context of mental health, it is therefore critical to ensure that innovations are designed to be clear, usable and engaging for those living with mental disorder. 1 This will involve considering aspects of these conditions which may hinder engagement with digital interventions (such as amotivation and cognitive impairments), 33 and working with diverse patient populations during the processes of design and implementation, to ensure patient perspectives and preferences, treatment targets and outcomes are fully integrated. 34 Digital literacy and codesign of tools by stakeholders is also key so that they can direct treatment targets and use cases in an equitable manner (see online supplemental appendix table 8 ).
Ethics and potential harms
A variety of ethical concerns can arise with digital mental health interventions (see online supplemental appendix table 9 ). Issues such as ensuring that digital interventions are based on high-quality evidence from diverse populations, are predictively valid and support accurate diagnoses and prognoses and do not themselves cause harm are key elements to consider and address. In addition, key areas such as patient privacy and confidentiality need to be explained. Patients need to be fully aware and consent to how their data are collected, managed and used, and this is critical to preserving their trust in clinicians. In addition, it is important to address the issue of potential silo formation or fragmentation of data when using specific digital tools. Patients can be disadvantaged if they no longer have access to their data or a digital intervention after a study finishes.
The possibility of harm or potential negative effects from digital mental health interventions, especially for vulnerable populations, is an essential area to consider, but research is scarce. 35 Preliminary data suggest that male gender, lower educational level and comorbid anxiety symptoms increase the risk of dropping out, 36 but further focus and research is needed to identify which aspects are unique to digital health, and which are most amenable to targeted solutions.
Specialised groups
While there are many targeted clinical uses for digital mental health interventions, adolescent populations may be the ideal given the opportunity for early detection, prevention and, if necessary, intervention. With access to youth mental health services limited across the world and now nearly 50% of youth reporting they are online ‘constantly’, innovations like digital phenotyping are a good match (see online supplemental appendix table 10 ). Other groups such as the elderly, people with physical disabilities and those with learning disabilities are also important populations for further study ( online supplemental appendix table 10 ).
In this clinical review, we have summarised some of the key areas of challenge in digital mental health, with illustrative case studies. We are aware of some limitations in our approach, which is a narrative rather than a systematic review of the literature and was reached by expert consensus. We did not address some important approaches that have been tested in digital mental health, such as mobile apps, internet-based interventions (including internet-based cognitive therapy and internet-based self-help interventions) and virtual reality 37 ; however, we aim to cover these in future projects. In addition, while the consensus development panel enabled international and multidisciplinary expert discussion, we are aware that we were not able to include patient and public representation, and rather than using a separate panel—given the novelty and the complexity of the field—we used the whole expert group for consensus. While there have been many calls for consensus guidelines in areas of digital mental health, particularly in the area of mental health apps 38 39 and in the new ethical issues and safety issues raised (eg, in digital monitoring studies in at-risk populations), 40 41 to the best of our knowledge this is the first attempt at consensus recommendations across the broader area of digital mental health. As an expert international and cross-disciplinary consensus panel and on the basis of non-biased discussion, we have attempted to identify the current state of knowledge and bring together the immediate challenges throughout the field of digital psychiatry and mental health. By taking this broad approach we have been able to identify themes and challenges relevant across all subspecialised fields, as well as addressing potential solutions through the case studies in the online supplemental appendix .
In conclusion, the international consensus meeting identified a number of key areas and potential solutions ( box 1 ). Given careful consideration and a clear vision to implement these changes in a challenging landscape, these measures can ensure that we start to harness the huge potential of digital innovations in the real-world clinical setting and ensure improved outcomes for patients and carers, and via preventative measures aimed at at-risk groups, at a wider population level.
Consensus points for future plans in digital mental health
We list here the agreed consensus points for measuring and implementing digital innovations in the real-world clinical setting.
Definitions and reporting of interventions vary. This creates confusion and prevents consistent reporting, which makes the systematic synthesis of data much more difficult. Agreed definitions are needed to ensure replicable and incremental science.
We lack an agreed ontology for mental illness; an agreed framework would also improve reporting, but a transdiagnostic approach focused on symptoms rather than diagnosis may also be a helpful route for validation of digital biomarkers.
Research on perfecting digital measurements is a good start, but will only be helpful if it correlates with real-world clinical symptoms and functional outcomes.
Digital interventions are often best used as an addition to enrich face-to-face or virtual care, they are not necessarily a replacement. Sustained engagement with digital interventions needs human interaction as well. Hybrid approaches in the clinic would combine the advantages of each approach. They could also increase the efficiency of delivery of care, especially if provided by a range of clinicians and support workers (eg, digital navigators) with a combination of standard clinical care and protocolised treatment.
Digital interventions are most useful when implemented in the real-world clinical setting. Clinicians need to be familiar with digital interventions and apply them as stand-alone interventions or combine them flexibly within the standard clinical assessment. Teaching and training for clinicians will be essential to facilitate this.
Ensuring patients are engaged is just as important. Patients and carers will use a technology if they feel it is relevant to their needs, and so codesign is critical. Teaching and training for patients will also be key to ensure equitable access to the technology and care.
Ethics and potential harms are present in all research studies. As well as common challenges (such as the choice of an appropriate placebo, and placebo/nocebo effects) because of the nature of the data collected, digital intervention studies also carry concerns about privacy, confidentiality and information governance. These need to be carefully addressed to ensure that trust is maintained between patients and clinicians.
Ethics statements
Patient consent for publication.
Not applicable.
Acknowledgments
This paper is based on the discussion the authors had during a meeting which was held in Rome on 1–2 December 2022. The meeting was supported by Angelini Pharma. We thank Dr Agnese Cattaneo and Dr Fabrizio Calisti (Angelini Pharma), and Excerpta Medica for taking care of the logistics of the event. The sponsor did not have any influence on the content of the discussion, the outcome and the preparation of this manuscript.
- Bell IH , et al
- Huckvale K ,
- Venkatesh S ,
- Christensen H
- Sheriff R ,
- Smith K , et al
- Sugarman DE ,
- De Witte NAJ ,
- Carlbring P ,
- Etzelmueller A , et al
- Wachter RM ,
- Dufour J-F ,
- Zheng M-H , et al
- Arakawa N ,
- Ferguson JH
- World Health Organization
- Waggoner J ,
- Carline JD ,
- Humphrey-Murto S ,
- Gonsalves C , et al
- Ebner-Priemer UW
- Piasecki TM ,
- Hufford MR ,
- Solhan M , et al
- Reichert M ,
- Braun U , et al
- Freeman LK ,
- Griffin SA , et al
- Harvey PD ,
- Rizzo AA , et al
- Koutsouleris N ,
- Hauser TU ,
- Skvortsova V , et al
- Offidani E ,
- Taraboanta L , et al
- Onyeaka H ,
- Muoghalu C ,
- Malekani M , et al
- Da Fonseca A ,
- Kleim B , et al
- Mouchabac S ,
- Conejero I ,
- Lakhlifi C , et al
- Greenhalgh T ,
- Wherton J ,
- Papoutsi C , et al
- Ferreri F ,
- Ogorzelec L , et al
- Pandya S , et al
- Doukani A ,
- Araya R , et al
- Proudfoot J ,
- Barak A , et al
- Hastings J ,
- Johnston M , et al
- Biagianti B ,
- Hidalgo-Mazzei D ,
- Schouten SE ,
- Dekkers T , et al
- Rozental A ,
- Magnusson K ,
- Boettcher J , et al
- Karyotaki E ,
- Kleiboer A ,
- Smit F , et al
- Jankovic D ,
- Saramago P , et al
- Andersson G ,
- Bertagnoli A , et al
- Huckvale K , et al
- Kleiman EM ,
- Abraham M , et al
- Martinez-Martin N ,
- Greely HT ,
Supplementary materials
Supplementary data.
This web only file has been produced by the BMJ Publishing Group from an electronic file supplied by the author(s) and has not been edited for content.
- Data supplement 1
Twitter @TomVanDaele, @JohnTorousMD, @And_Cipriani
Contributors KAS, AC and JT prepared the manuscript. Other coauthors critically reviewed the typescript. All authors contributed to the consensus meeting and approved the final submitted version of the paper. JT and AC are joint last authors.
Funding KAS and AC are supported by the National Institute for Health Research (NIHR) Oxford Cognitive Health Clinical Research Facility. AC is also supported by an NIHR Research Professorship (Grant RP-2017-08-ST2-006), by the NIHR Oxford and Thames Valley Applied Research Collaboration and by the NIHR Oxford Health Biomedical Research Centre (Grant NIHR203316). JF is supported by a University of Manchester Presidential Fellowship (P123958) and a UK Research and Innovation Future Leaders Fellowship (MR/T021780/1). CM is supported by the Spanish Ministry of Science and Innovation, Instituto de Salud Carlos III (ISCIII, PI21/01929), Consorcio Centro de Investigación Biomédica en Red (CIBER, CB/07/09/0023), cofinanced by the European Union and ERDF Funds from the European Commission, ‘A way of making Europe’, financed by the European Union–Next Generation EU (PMP21/00051), Madrid Regional Government (B2017/BMD-3740 AGES-CM-2), European Union Structural Funds, EU Seventh Framework Program, H2020 Program under the Innovative Medicines Initiative 2 Joint Undertaking: Project c4c (Grant Agreement No 777389), Horizon Europe (HORIZON-HLTH-2021-STAYHLTH-01-02 No 101057529; HORIZON-HLTH-2021-STAYHLTH-01-02 No 101057454; HORIZON-HLTH-2022-STAYHLTH-01-01-two-stage No 101080238), National Institute of Mental Health of the National Institutes of Health, Fundación Familia Alonso and Fundación Alicia Koplowitz.
Disclaimer The views expressed are those of the authors and not necessarily those of the UK National Health Service, the NIHR or the UK Department of Health.
Competing interests MF-J has received support from Angelini Pharma within the past 3 years. JF has received honoraria/consultancy fees from Atheneum, Informa, Gillian Kenny Associates, Big Health, Wood for Trees, Nutritional Medicine Institute, ParachuteBH, Richmond Foundation and Nirakara, independent of this work. UWE-P has received consultant fees from Boehringer Ingelheim and lectures including travel fees from Angelini Pharma. PC has received honoraria/speaker fees from Angelini Pharma, Koa Health and Lundbeck within the past 3 years. CM has received honoraria as a consultant and/or advisor and/or for lectures from Angelini, Esteve, Exeltis, Janssen, Lundbeck, Neuraxpharm, Nuvelution, Otsuka, Pfizer, Servier and Sunovion, outside the submitted work. SM has received fees from Ethypharm, BioSerenity and Angelini Pharma. AC has received research and consultancy fees from Italian Network for Paediatric Clinical Trials (INCiPiT), CARIPLO Foundation, Lundbeck and Angelini Pharma, outside the submitted work. JT is co-founder of a mental health company called Precision Mental Wellness.
Provenance and peer review Not commissioned; externally peer reviewed.
Supplemental material This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Read the full text or download the PDF:
- Skip to main content
- Skip to "About this site"
Language selection
- Français
- Search and menus
Digital Insights Digital well-being: the relationship between technology use, mental health and interpersonal relationships
by Gabrielle Asselin , Howard Bilodeau and Aisha Khalid
Skip to text
Introduction
Younger canadians spend the most time online, taking a break from the internet was not associated with better mental health, but spending less time online was, smartphone use is steadily increasing among canadians, increased smartphone use was linked to lower mental health and satisfaction in relationships with friends and family in 2020, the majority of canadians communicate with others online at least once per week, weekly online communications with friends and family were associated with more frequent in-person interactions in 2022, other articles based on the 2022 cius, digital economy and society statistics portal, methodology, acknowledgements, external references, internal references.
Text begins
Digital technologies have created many new opportunities for individuals to overcome barriers and challenges in their personal lives and at work. As the utility of digital technologies, like smartphones, continues to rise, individuals are spending an increasing amount of time online. The 2022 Canadian Internet Use Survey (CIUS) found that one-quarter of Canadians spent 20 hours or more per week using the Internet for general purposes, up at least 4 percentage points from 2018 (21%) and down only slightly from the beginning of the COVID-19 pandemic in 2020 (27%). Note
In the 2022 CIUS , Canadians reported that their online activities helped them make more informed decisions (51%) and saved them time (47%). However, the use of digital technologies was not always associated with positive outcomes; Canadians also reported that their online activities sometimes made them feel anxious, depressed or envious of the lives of others (22%), interfered with their relationships (8%) and interfered with other aspects of their lives, such as sleep, physical activity, and work- or school-related activities (24%).
This article highlights new data from the 2020 and 2022 CIUS , examining the complex relationship between digital technology use and various measures of well-being. Section 1 explores the relationship between time spent online and self-reported mental health, Section 2 examines how increased smartphone use is related to satisfaction with interpersonal relationships and self-reported mental health, and Section 3 explores the relationship between online communications and in-person interactions.
Section 1: Time spent online and self-reported mental health
About two-fifths of Canadians aged 15 to 24 (42%) reported spending 20 hours or more per week on general Internet use in 2022, the highest among all age groups, followed by those aged 25 to 34 (38%). The percentage of Canadians aged 15 to 24 spending this amount of time online for general purposes was about the same as during the pandemic in 2020 (43%), but at least 10 percentage points higher than before the pandemic in 2018 (32%).
Almost 9 in 10 Canadians watched content online in 2022 (87%) and 17% watched content online for 20 hours or more in a typical week. Watching online content includes activities such as watching television series or movies, watching eSports or other video game streaming services, or watching user-generated content on platforms such as YouTube or TikTok. Again, use was highest for younger Canadians, with 26% of those aged 15 to 24 and 23% of those aged 25 to 34 spending 20 hours or more per week watching online content.
About 37% of Canadians played video games online in 2022, with only 6% doing so for 20 hours or more per week. As with other online activities, those aged 15 to 24 were the most likely to play online video games during a typical week (73%) and spend 20 hours or more per week on this activity (15%).
In 2022, just over 1 in 5 Canadians (22%) reported taking a break from using the Internet or decreasing their time spent on the Internet because they felt they were using it too often or for too long. This was not significantly different from 2020 (24%) or 2018 (21%). In 2022, Canadians aged 15 to 24 (36%) were the age group most likely to report taking a break from or reducing time spent on the Internet.
Of those who took a break from the Internet in 2022, 44% reported having very good or excellent mental health. Conversely, among those who didn’t take a break from the Internet, the percentage reporting very good or excellent mental health was almost 10 percentage points higher (53%). The 2022 CIUS also found that the percentage of Canadians who spent 20 hours or more per week online (regardless of activity) was not significantly different between those who took breaks from the Internet and those who did not. This could be related to a disconnect between the desire to take a break from the Internet and the willingness to actually do so. In the Young Canadians in a Wireless World study conducted by MediaSmarts in 2021, most surveyed school-aged children reported that they were worried about spending too much time online, and also that they would be unhappy if they couldn’t use the Internet for a week. Note
Although taking a break from the Internet wasn’t found to be associated with better mental health in the 2022 CIUS , a correlation between less time spent online and better mental health was identified. The percentage of Canadians reporting very good or excellent mental health was 16 percentage points higher for those who watched content online for less than 10 hours per week, compared with those who watched online content for 20 hours or more per week. Note For general Internet use, the percentage of Canadians reporting very good or excellent mental health was 12 percentage points higher among those who spent less than 10 hours per week online, compared with those who spent 20 hours or more online per week. Note
The percentage of Canadians reporting very good or excellent mental health was significantly lower for all amounts of time spent playing video games online, compared with general Internet use. For example, nearly half (44%) of Canadians who spent 20 hours or more per week on general Internet use reported very good or excellent mental health, compared with 35% of those who spent 20 hours or more per week playing video games online. These findings demonstrate that factors other than time spent online can contribute to the relationship between Internet use and mental health, such as the type of online activity, and the age, sex and gender of the user.
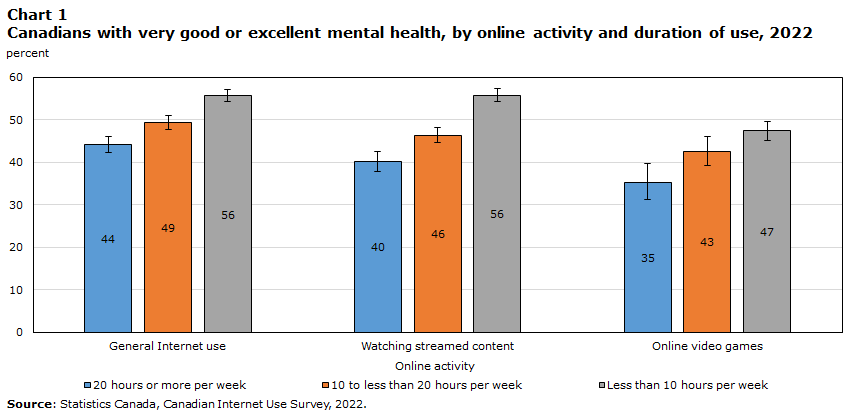
| Online activity | 20 hours or more per week | 10 to less than 20 hours per week | Less than 10 hours per week | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Percent | 95 % confidence interval | Percent | 95% confidence interval | Percent | 95% confidence interval | ||||
| from | to | from | to | from | to | ||||
| General Internet use | 44 | 42 | 46 | 49 | 48 | 51 | 56 | 54 | 57 |
| Watching streamed content | 40 | 38 | 43 | 46 | 45 | 48 | 56 | 54 | 57 |
| Online video games | 35 | 31 | 40 | 43 | 39 | 46 | 47 | 45 | 50 |
| Statistics Canada, Canadian Internet Use Survey, 2022. | |||||||||
In another study recently conducted by Statistics Canada, which examined data on mental health in adolescents aged 12 to 17 from the 2019 Canadian Health Survey on Children and Youth, video game use by girls was found to be associated with lower self-reported mental health, even when controlling for other factors. For boys, no relationship between video game use and mental health could be identified. Similarly, for social media or instant messaging use, no differences in mental health could be identified when controlling for other factors, regardless of sex. Note These findings further demonstrate the importance of considering the type of activity and personal characteristics when examining the relationship between Internet use and mental health.
Section 2: Smartphone use, relationship satisfaction and self-reported mental health
The 2020 CIUS found that most Canadians (84%) had a smartphone for personal use, up 4 percentage points from 2018 (80%). Note The increase was even larger for seniors aged 65 and older (+11 percentage points), despite lower overall use (54%). Meanwhile, smartphone use by teenagers and adults aged 15 to 24 (96%), 25 to 34 (97%) and 35 to 44 (96%) was nearly universal in 2020.
Almost two-thirds of Canadians (64%) used their smartphone at least once per hour in 2020, including to check messages, use social networks and news sites, and check notifications, while one-fifth (20%) used their smartphone a few times per day or less. Younger individuals were more likely to check their smartphone more often—88% of those aged 15 to 24 and those aged 25 to 34 reported using their smartphone at least once per hour, with those aged 35 to 44 not far behind (82%). Many teenagers and young adults aged 15 to 24 (46%) and 25 to 34 (33%) reported using their smartphone as frequently as every 15 minutes.
As smartphone use grows steadily, some Canadians are trying to control their use. The 2022 CIUS found that 20% of Canadians reported modifying smartphone or application settings to manage time spent on their smartphone. This behaviour was most prevalent for those aged 15 to 24 and those aged 25 to 34, with 32% reporting they tried to control their smartphone use.
In 2020, Canadians who checked their smartphone once per hour or more were less likely to report being completely satisfied with their relationships with friends (46%) than those who checked their phone a few times per day or less (54%). Note The same pattern was found when examining relationships with relatives or family members, excluding those the respondent lived with.
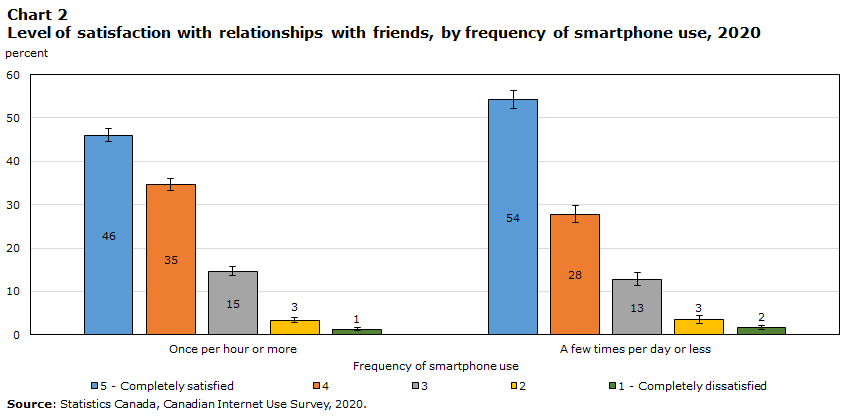
| Frequency of smartphone use | 5 - Completely satisfied | 4 | 3 | 2 | 1 - Completely dissatisfied | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Percent | 95 % confidence interval | Percent | 95% confidence interval | Percent | 95% confidence interval | Percent | 95% confidence interval | Percent | 95% confidence interval | ||||||
| from | to | from | to | from | to | from | to | from | to | ||||||
| Once per hour or more | 46 | 45 | 47 | 35 | 33 | 36 | 15 | 14 | 16 | 3 | 3 | 4 | 1 | 1 | 2 |
| A few times per day or less | 54 | 52 | 56 | 28 | 26 | 30 | 13 | 11 | 14 | 3 | 3 | 4 | 2 | 1 | 2 |
| : Statistics Canada, Canadian Internet Use Survey, 2020. | |||||||||||||||
Checking one’s smartphone more frequently was also associated with lower reported levels of very good or excellent mental health. Among Canadians who checked their phone a few times per day or less, almost 6 in 10 (58%) reported very good or excellent mental health, compared with 5 in 10 of those who checked their phone at least once per hour or more. The most frequent smartphone users also reported the highest level of fair or poor health (19%), compared with 12% of the least frequent users.
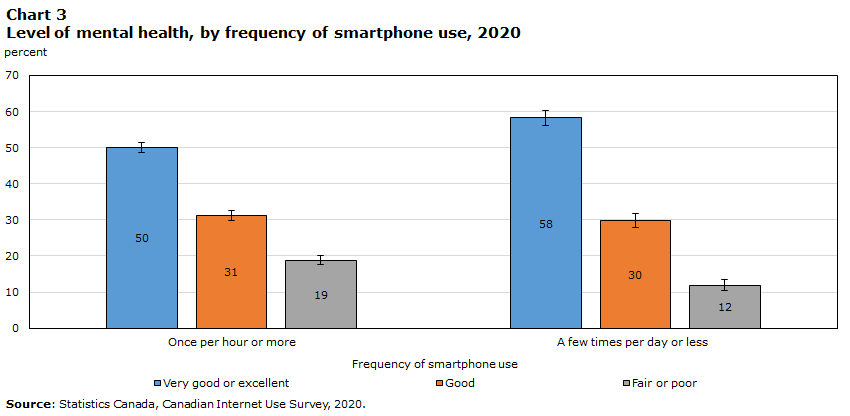
| Frequency of smartphone use | Very good or excellent | Good | Fair or poor | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Percent | 95 % confidence interval | Percent | 95% confidence interval | Percent | 95% confidence interval | ||||
| from | to | from | to | from | to | ||||
| Once per hour or more | 50 | 49 | 52 | 31 | 30 | 33 | 19 | 18 | 20 |
| A few times per day or less | 58 | 56 | 60 | 30 | 28 | 32 | 12 | 10 | 14 |
| Statistics Canada, Canadian Internet Use Survey, 2020. | |||||||||
Section 3: Online communications and in-person interactions
As new digital technologies have become more readily accessible, Canadians have increasingly integrated new communication methods into their lives. The 2022 CIUS found that almost 8 in 10 Canadians (77%) communicated with friends online at least once per week (e.g., iMessage, FaceTime, Facebook Messenger, WhatsApp), and over 6 in 10 (65%) communicated with relatives or family members online at least once per week. Online communications with friends (+4 percentage points) and family (+2 percentage points) increased modestly from 2020 to 2022.
In 2022, teenagers and young adults aged 15 to 24 were most likely to communicate with friends via the Internet at least once per week (93%), with the likelihood decreasing among older age groups. However, for online communications with family, the likelihood of weekly interactions peaked with individuals aged 25 to 34 (79%) and then decreased for older age groups.
| Canadians who use the Internet to communicate with friends | Canadians who use the Internet to communicate with relatives or family members | |||
|---|---|---|---|---|
| At least once per week | A few times per month to once per month | At least once per week | A few times per month to once per month | |
| Percent | Percent | Percent | Percent | |
| All individuals | 77 | 8 | 65 | 16 |
| Age groups | ||||
| 15 to 24 | 93 | 4 E: Use with caution | 64 | 22 |
| 25 to 34 | 91 | 5 | 79 | 14 |
| 35 to 44 | 85 | 8 | 75 | 15 |
| 45 to 54 | 80 | 9 | 70 | 17 |
| 55 to 64 | 70 | 11 | 61 | 17 |
| 65 and older | 54 | 11 | 50 | 15 |
| 65 to 74 | 62 | 11 | 57 | 16 |
| 75 and older | 44 | 10 | 41 | 13 |
| use with caution : Unless otherwise specified, all figures have a quality of “A,” which corresponds to a coefficient of variation of 0 to 16.5%. An "E" indicator corresponds to a coefficient of variation of 16.6% to 33.3%. : Statistics Canada, Canadian Internet Use Survey, 2022 | ||||
The use of video conferencing has also been growing in importance, particularly since the start of the COVID-19 pandemic. Over 6 in 10 (65%) individuals made online voice or video calls in 2022 (excluding business- and school-related use), up 17 percentage points from 2018 (47%) and seemingly stable since 2020 (64%).
Although there may be a connection between rising technology use and decreasing relationship satisfaction and mental health, the relationship between these factors may not be causal. Researchers have proposed that it’s not the amount of time spent with technology that matters most when understanding the impact of technology on well-being, but rather the quality or content of the activities a person engages in. Note Studies on social connectedness through technology have shown that technology use can be associated with positive outcomes; for example, during the COVID-19 pandemic, individuals who communicated more with others online were more likely to engage in positive behaviours, such as maintaining their physical health. Note
Similarly, the 2022 CIUS found a correlation between the frequency of online and in-person interactions. Note Among Canadians who said they interacted with their friends online weekly, over half (52%) reported seeing friends in person outside of work or school at least weekly as well. By comparison, among those who said they interacted with their friends online a few times per month or less, only 22% reported seeing friends in person at least weekly.
For interactions with relatives or family members, the same pattern was observed, but to a lesser extent. For those interacting weekly with family online, just under half (47%) saw family in person (excluding those they live with) at least weekly. Meanwhile, among those who interacted with family online a few times or less per month, only 16% saw their family at least weekly. These findings provide evidence that online interactions aren’t necessarily replacing in-person interactions.
Compared with the overall population (52%), a higher percentage of individuals aged 15 to 24 who interacted weekly with their friends online reported seeing them in person at least weekly (61%). This is likely partly related to younger Canadians using the Internet to communicate with friends more often than older Canadians, and the fact that younger Canadians tend to have more opportunities to see their friends on a weekly basis.
Overall, regardless of the frequency of online interactions, a larger percentage of Canadians reported spending time in person with both friends (+21 percentage points) and family (+15 percentage points) at least weekly in 2022, compared with 2020. A large part of this trend can likely be attributed to the reduction of COVID-19 pandemic restrictions that limited in-person interactions in 2020.
Results from the 2020 and 2022 CIUS demonstrate a complex relationship between technology use and measures of well-being, such as mental health, satisfaction in interpersonal relationships and time spent with others in person. The survey found that increased time spent online and smartphone use were associated with lower self-reported mental health and that increased smartphone use was also associated with lower satisfaction in interpersonal relationships. However, the survey also showed that spending more time with others online was linked to an increased likelihood of seeing others in person, and that the correlation between time spent engaging in online activities and self-reported mental health differed by type of online activity. As other studies have proposed, the quality of time spent online may be a better predictor of digital well-being than time spent online alone.
The CIUS is a rich source of information for understanding the impact of technology on the lives of Canadians. Further research could go beyond the analysis in this article by simultaneously controlling for multiple variables that may impact well-being, such as aggregate time spent online and the personal characteristics of technology users.
Results for the 2022 CIUS were released in The Daily on July 20, 2023.
Visit the Digital economy and society statistics portal to find data, publications, and interactive tools related to the digital economy and society in one convenient location.
This article uses data from the 2018, 2020 and 2022 iterations of the Canadian Internet Use Survey (CIUS) . The CIUS aims to measure the adoption and use of digital technologies by Canadians aged 15 years and older, living in the 10 provinces.
Data for the CIUS were collected through an electronic questionnaire during the following periods:
- 2018: December 15, 2018 to March 21, 2019
- 2020: November 3, 2020 to March 3, 2021
- 2022: December 29, 2022 to April 5, 2023
In the 2018 survey, a sample of approximately 33,000 individuals was used and the response rate was 43.7%. In the 2020 survey, the sample size consisted of approximately 44,800 individuals and the response rate was 41.6%. Finally, in the 2022 survey, the sample size was approximately 55,700 individuals and the response rate was 45.3%.
Error bars on charts represent the 95% confidence interval.
The authors would like to thank Nicole Minnema, Karine Garneau, Mark Uhrbach and Christoph Schimmele for their feedback on an earlier version of this paper.
Boers, E., Afzali M.H., Newton N., & Conrod P. (2019). Association of Screen Time and Depression in Adolescence. JAMA Pediatrics . 173(9):853–859. Retrieved March 16, 2023.
MediaSmarts (2023). Young Canadians in a Wireless World, Phase IV: Trends and Recommendations . Retrieved October 30, 2023.
Royal, C., Wasik, S., Horne, R., Dames, L. S., & Newsome, G. (2017). Digital Wellness: Integrating Wellness in Everyday Life with Digital Content and Learning Technologies. In J. Keengwe & P. Bull (Eds.), Handbook of Research on Transformative Digital Content and Learning Technologies (pp. 103–117). IGI Global. Retrieved March 16, 2023.
Charnock, S., Heisz, A., Kaddatz, J., Spinks, N., & Mann, R. (2021). Canadians' Well-being in Year One of the COVID-19 Pandemic . Income Research Paper Series . Statistics Canada. Retrieved October 30, 2023.
Kerr, S., & Kingsbury, M. (2023). Online digital media use and adolescent mental health . Health Reports . Statistics Canada. Retrieved October 30, 2023.
More information
Note of appreciation.
Canada owes the success of its statistical system to a long-standing partnership between Statistics Canada, the citizens of Canada, its businesses, governments and other institutions. Accurate and timely statistical information could not be produced without their continued co-operation and goodwill.
Standards of service to the public
Statistics Canada is committed to serving its clients in a prompt, reliable and courteous manner. To this end, the Agency has developed standards of service which its employees observe in serving its clients.
Published by authority of the Minister responsible for Statistics Canada.
© His Majesty the King in Right of Canada, as represented by the Minister of Industry, 2024
Use of this publication is governed by the Statistics Canada Open Licence Agreement .
Catalogue no. 22-20-0001
Frequency: Occasional
Technology and Mental Health
- January 2015
- In book: Encyclopedia of Information Science and Technology (pp.6455-6465)
- Edition: Third Edition
- Publisher: Information Science Reference
- Editors: M. Khosrow-Pour
- This person is not on ResearchGate, or hasn't claimed this research yet.

- University of Central Florida
Discover the world's research
- 25+ million members
- 160+ million publication pages
- 2.3+ billion citations
- Kijpokin Kasemsap

- Madeline R. Marks

- Jacob Baumattre
- John Brennan

- Ron Goldman

- AM J COMMUN PSYCHOL

- Joseph H. Albeck
- Jan Cannon-Bowers
- Anya Andrews
- Rachel Joyce
- James Bennett-Levy

- Charles Glisson
- John Landsverk

- Stephen Mayberg

- Debby E. Almonte
- J.S. Anthony

- Recruit researchers
- Join for free
- Login Email Tip: Most researchers use their institutional email address as their ResearchGate login Password Forgot password? Keep me logged in Log in or Continue with Google Welcome back! Please log in. Email · Hint Tip: Most researchers use their institutional email address as their ResearchGate login Password Forgot password? Keep me logged in Log in or Continue with Google No account? Sign up
OPINION article
The need for a mental health technology revolution in the covid-19 pandemic.
Part of this article's content has been mentioned in:
Leveraging Technology for the Wellbeing of Individuals With Autism Spectrum Disorder and Their Families During Covid-19
- Read opinion

- 1 School of Social Welfare, University of California, Berkeley, Berkeley, CA, United States
- 2 Department of Psychiatry, Zuckerberg San Francisco General Hospital, University of California, San Francisco, San Francisco, CA, United States
Introduction
The current coronavirus 2019 (COVID-19) pandemic not only poses a large threat to the physical health of our population, if we fail to act now, it will also have detrimental long-term consequences for mental health.
Though social distancing is a crucial intervention to slow down the destructive effects of the pandemic, it can lead to isolation, decreased physical activity, and increased rumination, which might particularly hurt those with pre-existing mental illness. Further, the stream of disheartening COVID-19 news provides fodder for increased worry and distress, which can be detrimental for people with anxiety disorders. Early cross-sectional surveys in the United States, Canada, and Europe show an increase in symptoms of depression and anxiety for the general population, associated with COVID-19 concerns ( 1 ). Thus, this crisis is exacerbating existing mental health conditions and creating conditions for the development of new ones. Further, if lessons from other outbreaks such as Ebola ( 2 ) and SARS (Severe Acute Respiratory Syndrome) ( 3 ) are any indication, even after an outbreak is controlled, there will likely be a substantial increase in need for psychological support.
Crucially, this public health crisis will magnify and deepen existing shortcomings of mental health care systems. The US was already facing a mental health crisis before the pandemic: less than half of those with mental illness receive the care that they need ( 4 ). Underserved populations, such as low-income or ethnic minority populations, are disproportionately affected; they show the lowest utilization of mental health services ( 5 ). Early data suggest that underserved populations pay a larger health toll from COVID-19: they show higher mortality rates ( 6 , 7 ). They are more likely to work in essential jobs putting them at greater risk of contracting COVID-19, and suffer greater economic consequences. All these factors lead to increased stress and anxiety. We will therefore be faced with an even greater relative shortage of trained professionals and means to mental health care during and after this pandemic.
We argue that what we need during a public health crisis like this is a digital mental health revolution: scaling up the delivery of confidential mental health services to patients across a wide range of platforms, from telemental health to mobile interventions such as apps and text messaging. Here, we provide an overview of technological tools which could help to decrease the mental health burden of COVID-19, provide recommendations on how they could be used and scaled-up, and discuss considerations and limitations of mental health technology applications.
There is a crucial role for the use of teleconferencing software for therapy sessions during the COVID-19 pandemic. Most studies of teleconferencing services showed that effectiveness is comparable to in-person services across disorders including depression, posttraumatic stress disorder, and anxiety disorders ( 8 ). China has had some success with this approach. Researchers recently wrote in a Lancet Commentary that during the worst of the outbreak in January, China successfully provided online psychological counseling and self-help was widely rolled out by mental health professionals in medical institutions, universities, and academic societies ( 9 ).
In the US, the pandemic has also catalyzed a rapid adoption of telehealth ( 10 ). Medicare now allows for billing for telehealth. Further, the Health Insurance Portability and Accountability Act (HIPAA) has been revisited to permit more medical providers to use HIPAA compliant platforms to communicate with patients. This removes a major barrier to wider adoption of telemedicine and could also provide an outstanding opportunity for patients who previously did not feel comfortable seeking mental health care to now approach these services.
However, it is important to attend to disparities in technology access and digital literacy. Before the pandemic, only one in ten patients in the US used telehealth, and 75% said that they were unaware of telehealth options or how to access it ( 11 ). Recent data from primary care clinics showed that, though video care consults went up by 80% in late March and early April, minority groups represented a smaller portions of these visits ( 12 ). This is partly explained because of a lack of Internet availability, which varies due to limited data plans and lack of Wi-Fi, and inability to use smartphone features such as downloading apps ( 13 ). At the moment, some US telecom providers are offering free Internet services ( 14 ). However, longer-term strategies need to be developed to prevent further widening of the digital divide ( 15 ), including providing affordable, high speed Internet access, improving usability of telehealth programs, and providing appropriate guidance/training for patients using these services.
Mental Health Smartphone Applications
Importantly, the use of personal mobile phones presents an opportunity for broad scaling of interventions. Over 90% of Americans have some type of mobile phone and over 80% have smartphones ( 16 ). Even among low-income Americans (71%) and older adults (53%) smartphone ownership is high. Mental health apps have shown effectiveness in decreasing symptoms of depression ( 17 ) and anxiety ( 18 ). Because of COVID-19, multiple meditation and wellness apps designed by the private sector have now temporarily opened up free memberships to aid in easing anxiety, the majority of these being mindfulness apps ( 19 ).
However, there are over 10,000 consumer-available mental health apps in app stores and many of these are not evidence-based ( 20 ). Further, though many people download mental health apps, research shows low rates of continued use over longer periods of time ( 21 ). It is crucial that mental health providers recommend apps that are backed up by evidence. One helpful resource is Psyberguide ( www.psyberguide.org ), a non-profit that rates apps based on the strength of the scientific research that supports it, ease of use, and its privacy policies ( 22 ). Lastly, in order to improve engagement, providers should follow up with patients on their usage of these apps and integrate the app content into their treatment.
Texting Applications
In addition to apps, text-messaging platforms could be leveraged to help people cope with mental health challenges evoked by COVID-19. Because texts are also delivered via individuals' devices, they are easy to provide to many at once using automated text-messaging platforms. Text-messaging interventions have demonstrated effectiveness in behavioral health promotion and disease management ( 23 ). Importantly, text-messaging is an appropriate tool for low digital literacy populations and underserved groups ( 24 ). For instance, our own HIPAA approved texting platform, HealthySMS, was developed with and for low-income populations (mostly Spanish speakers) and shows high acceptability in underserved populations ( 25 ). We recently rolled-out a text-messaging study to provide wide-scale support to interested individuals in the US via daily automated text-messages, containing tips on coping with social distancing and COVID-19 anxiety.
For crisis situations, Crisis Text Line provides free confidential help via text-message. This platform has seen the mention of “coronavirus” in 24% of conversations from March 30th to April 6th ( 26 ). Furthermore, Caremessage, a non-profit organization, has temporarily provided free access to their messaging platform and COVID-19 template text-messaging library with health information ( 27 ). In addition, reliable information can also be delivered by health and government organizations automated via text messages. Scaling of information delivery to patients and the public could also relieve health professionals and public health departments, who are already understaffed, underfunded, and overburdened ( 14 ).
Social Media
Social media plays a complicated role in the management of mental health. On the one hand, it can provide positive and supportive connections during a time of physical isolation. Earlier work shows that many people with mental illness are increasingly turning to social media to share their experiences and seek mental health information and advice ( 28 ). On the other hand, it can also serve to increase depression and anxiety symptoms based on negative social comparisons and the spread of distressing information ( 29 ). For instance, in a recent cross-sectional survey of almost 5,000 participants in China, increased social media exposure on COVID-19 was associated with increases in anxiety and depression symptoms ( 30 ).
Social media has played a large role in the spread of information since the start of the COVID-19 outbreaks, including misinformation and “fake news”. Large social media platforms are now reportedly taking steps to remove false content or conspiracy theories about the pandemic, using artificial intelligence (AI); and distribute reliable information, such as developed by the World Health Organization ( 31 ).
In China, the government provided online mental health education through popular social media platforms, such as WeChat, Weibo, and TikTok during the height of the outbreak in January ( 9 ). In the UK, the National Health Service (NHS) is working with Google, Twitter, Instagram, and Facebook to provide the public with accurate information about COVID-19 ( 32 ).
Social media also provides a unique opportunity for health professionals to distribute accurate information to their patients and the public, or to highlight available mental health resources. In Wuhan China, mental health professionals uploaded videos of mental health education for the general public through WeChat and other Internet platforms at the early stage of the outbreak ( 9 ). In the US and Europe, many physicians have turned to Twitter to share medical information. The social media site has now implemented a mechanism to verify physicians and other scientific experts in an effort to counteract coronavirus misinformation ( 33 ).
However, because of the overload of information on social media, misinformation might still spread too fast to be intercepted by AI algorithms ( 34 , 35 ). A recent report of responses from more than 8,000 people from six countries showed that one third reported seeing a significant amount of false or misleading COVID-19 information on social media or messaging platforms ( 36 ).
Further, posting information on social media raises the question of how health professionals should respond to the information posted by patients, and how that can impact the therapeutic relationship. Currently, there are no clear guidelines for health professionals, to determine how to act on social media. This calls for a push in quickly establishing such a consensus ( 37 ).
The COVID-19 crisis has fast-forwarded the use of technology in mental health care. Technology is crucial in scaling up access to mental health services during and after COVID-19. Given that people interact differently with technology, people of various ages, technical abilities, languages, and levels of literacy will need distinct types of interventions ( 38 ).
Older people are particularly vulnerable during this pandemic and already suffer from high rates of loneliness ( 39 ). This is strongly associated with greater symptoms of depression and anxiety ( 40 ), and physical morbidities and mortality ( 41 ). Previous work shows that older adults are interested in using technology to support their mental health, and that mobile health technology is feasible and reliable for assessing cognitive and mental illness ( 42 ).
However, older adults and those with low digital literacy might lack prior knowledge of digital technology to fully benefit from these tools ( 43 ). Digital health tools suffer from usability issues: they do not always consider digital literacy, health literacy, age, or English proficiency in their design ( 44 ). For instance, previous work showed that even the most basic functions of apps are difficult to use for diverse populations ( 45 ). Top-funded digital health companies test only 30% of their apps in people with clinical conditions ( 46 ). These factors are important because individuals with lower health literacy have worse health outcomes over time due to difficulty making informed health choices ( 47 ).
Therefore, interventions should be specifically targeted toward vulnerable groups, and adapted to their specific needs. This includes design choices such as easy to navigate user interfaces and tailoring vocabulary to older adults or those with low English proficiency ( 48 ). Training for individuals with low-tech skills, through outreach programs by healthcare staff may help patients to understand and use digital tools ( 49 ). Health systems should prioritize implementation of this crucial service ( 12 ).
Further, the right infrastructure needs to be set up to provide digital interventions securely, without personal privacy violations and minimizing the risk of data breaches. Apps and text-messaging must not only be effective, but also safe, secure, and responsible, similar to how therapists are held to standards of responsible practice and confidentiality ( 42 ). Therefore, it is imperative that cybersecurity specialists also become involved in ensuring safe technological services ( 50 ). Finally, just as they have now shown flexibility with telehealth, insurance companies and health systems should begin covering digital and mobile health interventions.
We are now in the midst of an acute health crisis which calls for a grand upscaling of mental health resources. Technology provides a medium for delivering mental health services remotely and on a wide scale, which is particularly important during social distancing measures. Even when the worst of the COVID-19 pandemic has subsided, it is likely that a large need for mental health support and services delivered through technology will remain. Digital mental health tools should be affordable, accessible, and appropriate for a wide group of individuals with varying ages, languages, and digital literacy. The time to massively invest in high quality and accessible online and mobile mental health in the face of the COVID-19 pandemic, and possible future pandemics, is now.
Author Contributions
CF wrote the first draft of the article. AA contributed to the writing and editing of the manuscript. Both authors contributed to the editing of the final manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
1. Nelson B, Pettitt AK, Flannery J, Allen N. Psychological and Epidemiological Predictors of COVID-19 Concern and Health-Related Behaviors. Psyarxiv (preprint) (2012). doi: 10.31234/osf.io/jftze
CrossRef Full Text | Google Scholar
2. Mohammed A, Sheikh TL, Poggensee G, Nguku P, Olayinka A, Ohuabunwo C, et al. Mental health in emergency response: lessons from Ebola. Lancet Psychiatry (2015) 2(11):955–7. doi: 10.1016/S2215-0366(15)00451-4
PubMed Abstract | CrossRef Full Text | Google Scholar
3. Mak IWC, Chu CM, Pan PC, Yiu MGC, Chan VL. Long-term psychiatric morbidities among SARS survivors. Gen Hosp Psychiatry (2009) 31(4):318–26. doi: 10.1016/j.genhosppsych.2009.03.001
4. Mental Health America. The state of mental health in America. Author Alexandria, VA: Mental Health America, Inc. (2019).
Google Scholar
5. Clancy C, Munier W, Brady J, Moy E, Chaves K, Freeman W, et al. 2012 National Healthcare Quality & Disparities Report. Rockville, Washington, DC: AHRQ Publications (2013).
6. Kirby T. Evidence mounts on the disproportionate effect of COVID-19 on ethnic minorities. Lancet Respiratory Med (2020). doi: 10.1016/S2213-2600(20)30228-9
7. Yancy CW. COVID-19 and African Americans. Jama (2020) 323(19):1891–2. doi: 10.1001/jama.2020.6548
8. Ralston AL, Andrews AR III, Hope DA. Fulfilling the promise of mental health technology to reduce public health disparities: Review and research agenda. Clin Psychol: Sci Practice (2019) 26(1):e12277. doi: 10.1111/cpsp.12277
9. Liu S, Yang L, Zhang C, Xiang Y-T, Liu Z, Hu S, et al. Online mental health services in China during the COVID-19 outbreak. Lancet Psychiatry (2020) 7(4):e17–e8. doi: 10.1016/S2215-0366(20)30077-8
10. Wosik J, Fudim M, Cameron B, Gellad ZF, Cho A, Phinney D, et al. Telehealth Transformation: COVID-19 and the rise of Virtual Care. J Am Med Inf Assoc : JAMIA (2020) ocaa067. doi: 10.1093/jamia/ocaa067
11. Power JD. U.S. Telehealth Satisfaction Study. SM, J.D. Power (2019).
12. Nouri S, Khoong EC, Lyles CR, Karliner L. Addressing Equity in Telemedicine for Chronic Disease Management During the Covid-19 Pandemic. Catalyst non-issue content. NEJM Catalyst (2020) 1(3).
13. Anderson M, Perrin A, Jiang J. 13% of Americans don"t use the internet. Who are they. Pew Research Center. (2016). p. 7.
14. New York Times. (2020). [Available from: https://www.usatoday.com/story/money/2020/03/16/utility-cable-internet-phone-coronavirus-covid-19/5060084002/ .
15. Yoon H, Jang Y, Vaughan PW, Garcia M. Older adults' Internet use for health information: Digital divide by race/ethnicity and socioeconomic status. J Appl Gerontol (2020) 39(1):105–10. doi: 10.1177/0733464818770772
16. Pew Research Center. Mobile Fact Sheet: Pew Research Center. Pew Research Center: Internet. Science & Tech. (2018). [Available from: https://www.pewinternet.org/fact-sheet/mobile/ .
17. Firth J, Torous J, Nicholas J, Carney R, Pratap A, Rosenbaum S, et al. The efficacy of smartphone-based mental health interventions for depressive symptoms: a meta-analysis of randomized controlled trials. World Psychiatry : Off J World Psychiatr Assoc (WPA) (2017) 16(3):287–98. doi: 10.1002/wps.20472
18. Firth J, Torous J, Nicholas J, Carney R, Rosenbaum S, Sarris J. Can smartphone mental health interventions reduce symptoms of anxiety? A meta-analysis of randomized controlled trials. J Affect Disord (2017) 218:15–22. doi: 10.1016/j.jad.2017.04.046
19. Techcrunch. (2020). [Available from: https://techcrunch.com/2020/03/18/meditation-apps-offer-free-mindfulness-as-social-distancing-takes-a-toll/ .
20. Larsen ME, Huckvale K, Nicholas J, Torous J, Birrell L, Li E, et al. Using science to sell apps: evaluation of mental health app store quality claims. NPJ Digit Med (2019) 2(1):1–6. doi: 10.1038/s41746-019-0093-1
21. Baumel A, Muench F, Edan S, Kane JM. Objective user engagement with mental health apps: systematic search and panel-based usage analysis. J Med Internet Res (2019) 21(9):e14567. doi: 10.2196/14567
22. Lipczynska S. Psyberguide: a path through the app jungle. J Ment Health (2019) 28(1):104–. doi: 10.1080/09638237.2017.1417574
23. Berrouiguet S, Baca-García E, Brandt S, Walter M, Courtet P. Fundamentals for future mobile-health (mHealth): a systematic review of mobile phone and web-based text messaging in mental health. J Med Internet Res (2016) 18(6):e135. doi: 10.2196/jmir.5066
24. Pew Research Center. Smartphone Ownership Is Growing Rapidly Around the World, but Not Always Equally. Pew Research Center’s Global Attitudes Project (2019).
25. Aguilera A, Berridge C. Qualitative Feedback From a Text Messaging Intervention for Depression: Benefits, Drawbacks, and Cultural Differences. JMIR mHealth uHealth (2014) 2(4):e46. doi: 10.2196/mhealth.3660
26. Crisis Textline. (2020). [Available from: https://www.crisistextline.org/mental-health/notes-on-coronavirus-how-is-america-feeling-part-4/ .
27. CareMessage. (2020). [Available from: https://www.caremessage.org/covid-19-response-messaging-safety-net-providers .
28. Naslund JA, Aschbrenner KA, McHugo GJ, Unützer J, Marsch LA, Bartels SJ. Exploring opportunities to support mental health care using social media: A survey of social media users with mental illness. Early Intervent Psychiatry (2019) 13(3):405–13. doi: 10.1111/eip.12496
29. Primack BA, Shensa A, Escobar-Viera CG, Barrett EL, Sidani JE, Colditz JB, et al. Use of multiple social media platforms and symptoms of depression and anxiety: A nationally-representative study among US young adults. Comput Hum Behav (2017) 69:1–9. doi: 10.1016/j.chb.2016.11.013
30. Gao J, Zheng P, Jia Y, Chen H, Mao Y, Chen S, et al. Mental Health Problems and Social Media Exposure During COVID-19 Outbreak. Plos one (2020) 15(4):e0231924.
31. Lawfare. (2020). [Available from: https://www.lawfareblog.com/covid-19-and-social-media-content-moderation .
32. Healthcare IT News. (2020). [Available from: https://www.healthcareitnews.com/news/europe/nhs-joins-forces-tech-firms-stop-spread-covid-19-misinformation .
33. Medscape. . https://www.medscape.com/viewarticle/930360 . [Available from: https://www.medscape.com/viewarticle/930360 .
34. Politico. (2020). [Available from: https://www.politico.com/news/2020/03/12/social-media-giants-are-fighting-coronavirus-fake-news-its-still-spreading-like-wildfire-127038 .
35. Vosoughi S, Roy D, Aral S. The spread of true and false news online. Science (2018) 359(6380):1146–51. doi: 10.1126/science.aap9559
36. Nielsen RK, Fletcher R, Newman N, Brennen JS, Howard PN. Navigating the ‘Infodemic': How People in Six Countries Access and Rate News and Information about Coronavirus. In: Misinformation, science, and media. The Reuters Institute for the Study of Journalism and University of Oxford (2020). p. 2020–04.
37. American Psychiatric Association Annual Meeting. Social media and psychiatry: challenges and opportunities. San Francisco, CA (2019). [press release]. https://www.psychcongress.com/ .
38. Hall AK, Bernhardt JM, Dodd V, Vollrath MW. The digital health divide: evaluating online health information access and use among older adults. Health Educ Behav (2015) 42(2):202–9. doi: 10.1177/1090198114547815
39. In Time of Social Distancing, Report's Call for Health Care System to Address Isolation and Loneliness Among Seniors Resonates. JAMA Health Forum (2020) 1(3):e200342–e200342. American Medical Association.
40. Santini ZI, Jose PE, Cornwell EY, Koyanagi A, Nielsen L, Hinrichsen C, et al. Social disconnectedness, perceived isolation, and symptoms of depression and anxiety among older Americans (NSHAP): a longitudinal mediation analysis. Lancet Public Health (2020) 5(1):e62–70. doi: 10.1016/S2468-2667(19)30230-0
41. Perissinotto CM, Cenzer IS, Covinsky KE. Loneliness in older persons: a predictor of functional decline and death. Arch Internal Med (2012) 172(14):1078–84. doi: 10.1001/archinternmed.2012.1993
42. Moussa Y, Mahdanian AA, Yu C, Segal M, Looper KJ, Vahia IV, et al. Mobile health technology in late-life mental illness: a focused literature review. Am J Geriatr Psychiatry (2017) 25(8):865–72. doi: 10.1016/j.jagp.2017.04.003
43. Schreurs K, Quan-Haase A, Martin K. Problematizing the digital literacy paradox in the context of older adults' ICT use: Aging, media discourse, and self-determination. Can J Commun (2017) 42(2):1–34. doi: 10.22230/cjc.2017v42n2a3130
44. Schueller SM, Hunter JF, Figueroa C, Aguilera A. Use of Digital Mental Health for Marginalized and Underserved Populations. Curr Treat Options Psychiatry (2019) 6(3):243–55.
45. Sarkar U, Gourley GI, Lyles CR, Tieu L, Clarity C, Newmark L, et al. Usability of commercially available mobile applications for diverse patients. J Gen Internal Med (2016) 31(12):1417–26. doi: 10.1007/s11606-016-3771-6
46. Van Winkle B, Carpenter N, Moscucci M. Why Aren't Our Digital Solutions Working for Everyone? AMA J Ethics (2017) 19(11):1116–24. doi: 10.1001/journalofethics.2017.19.11.stas2-1711
47. Berkman ND, Sheridan SL, Donahue KE, Halpern DJ, Crotty K. Low health literacy and health outcomes: an updated systematic review. Ann Intern Med (2011) 155(2):97–107. doi: 10.7326/0003-4819-155-2-201107190-0005
48. De Barros AC, Leitão R, Ribeiro J. Design and evaluation of a mobile user interface for older adults: navigation, interaction and visual design recommendations. Proc Comput Sci (2014) 27(27):369–78. doi: 10.1016/j.procs.2014.02.041
49. Grossman LV, Masterson Creber RM, Benda NC, Wright D, Vawdrey DK, Ancker JS. Interventions to increase patient portal use in vulnerable populations: a systematic review. J Am Med Inf Assoc (2019) 26(8-9):855–70. doi: 10.1093/jamia/ocz023
50. Alami H, Gagnon M-P, Ahmed MAA, Fortin J-P. Digital health: Cybersecurity is a value creation lever, not only a source of expenditure. Health Policy Technol (2019) 8(4):319–21. doi: 10.1016/j.hlpt.2019.09.002
Keywords: mobile health (mHealth), COVID-19, apps and smartphones, telemental health, public mental health, psychological therapies, depression, anxiety
Citation: Figueroa CA and Aguilera A (2020) The Need for a Mental Health Technology Revolution in the COVID-19 Pandemic. Front. Psychiatry 11:523. doi: 10.3389/fpsyt.2020.00523
Received: 02 April 2020; Accepted: 21 May 2020; Published: 03 June 2020.
Reviewed by:
Copyright © 2020 Figueroa and Aguilera. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Caroline A. Figueroa, [email protected]
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.

How Does Technology Affect Mental Health?
View all blog posts under Articles | View all blog posts under Counseling Resources

Upon completion of a Master of Arts in Counseling degree , individuals can choose to work as mental health counselors — individuals who help clients living with varying mental health and/or interpersonal issues. For example, a mental health counselor may meet with a bereaved woman in the morning who recently has lost her husband, and then a young man in his 20s in the afternoon who is living with an anxiety disorder. The role is challenging and rewarding, and necessitates understanding and expertise for a whole spectrum of mental health concerns.
Given the ubiquity of technology in daily life — particularly the internet and internet-based platforms such as social media sites and smartphone apps — mental health counselors working today likely will encounter clients who are experiencing issues that may be directly or indirectly linked to the use of digital media. According to Dr. Igor Pantic, writing in the literature review “Online Social Networking and Mental Health,” published by the U.S. National Library of Medicine, there is little doubt that the internet and social media platforms such as Facebook have had a notable impact on the way that individuals communicate.
Pantic further explained that a number of recent studies have observed a link between social media use and certain mental health problems, including anxiety and depression. Pantic is quick to assert, however, that the studies are by no means conclusive and that endeavors to understand the relationship between mental health and technology remain in their infancy.
Still, it is useful for mental health counselors to have an understanding of the research and insights into technology’s impact on mental health, which extends to the positive impacts, as well. After all, drawbacks aside, technology continues to improve many aspects of daily life for the better, and the arena of mental health is no exception: there are a number of observable areas in which the development of technology has helped clients take charge of their mental health care in a positive way.
Technology: A force for good?
Despite progress in terms of mental health awareness, journalist Conor Farrington, writing for the Guardian, explained how mental health care still receives a notable lack of funding from international governments. For example, Farrington reported that the per capita expenses on mental health care in industrialized nations such as the U.S. and U.K. amounts to just over $33, which equates to a little under £33. The amount is considerably less in developing countries. Consequently, Farrington argued that technology holds promise as a vehicle for improving access to mental health care, particularly in nations where such services are elementary at best.
Technology is improving mental health care in a number of ways, Lena H. Sun explained, writing for the Los Angeles Times, and it is primarily through platforms such as apps based on smartphones and computers that can help provide services and information to clients in a more cost-effective way. For example, Sun explained how there are now, in addition to smartphone apps that promote mental wellness, certain platforms available that allow patients to complete courses of cognitive behavioral therapy online. In her article, Sun profiled a British-based service known as the Big White Wall, which has been endorsed by the U.K.’s government-funded National Health Service. Big White Wall is an online platform that enables users living with mental health problems such as anxiety and depression to manage their symptoms from home via tools such as educational resources, online conversations and virtual classes on issues of mental health. The efficacy of Big White Wall is conspicuous — Sun reported on a 2009 study that found that a vast majority of the service’s users —some 95 percent —noted an improvement in their symptoms.

How can counselors harness technology?
Mental health counselors can play an important role in facilitating access to services such as Big White Wall and also can help promote smartphone apps and other online services that can be used to help improve general mental health. Technology can be used alongside in-person counseling, as opposed to being employed as a substitution. Counselors even may find that digital platforms allow the development of deeper working relationships with clients, particularly younger clients who are used to utilizing technology on a daily basis. Bethany Bay, writing in an article for Counseling Today, interviewed Sarah Spiegelhoff, a counselor from Syracuse, N.Y., who elaborated on this important point :
“I find technology resources to be great tools to supplement traditional counseling services, as well as a way for counselors to reach larger populations than we typically serve on an individual basis […] I find that college students are quicker to check Facebook and Twitter statuses than their email, so using social media has been one way for us to promote and distribute information on healthy living and outreach events […] I also share information related to new apps that promote wellness both through our social media accounts and directly in counseling sessions. For example, during alcohol awareness programming, we encouraged students to download free blood alcohol calculator apps. We also offer free mindfulness meditation MP3s through iTunes. I find the MP3s to be a great resource because I am able to present them to clients in session, talk about their experiences listening to and practicing the meditations and then develop a treatment plan that includes their use of the meditations outside of the counseling sessions.”
Counselors also can use platforms to connect with clients who may be situated in underserved or rural areas and are unable to travel for in-person meetings. As Farrington explained, some studies, including one from Oxford University, have found that text messaging and phone calls can be effective ways for counselors to connect with clients. Furthermore, telehealth platforms, which include instant messaging or video calling, already are proving useful in primary care settings for helping counselors reach clients. For example, Rob Reinhardt, writing for Counseling Today, interviewed Tasha Holland-Kornegay, a counseling professional who primarily provides counseling services to clients living with HIV via a messaging platform, which incorporates the option for video and audio calls.
Reinhardt, writing in a different piece published by Tame Your Practice, explained how the use of telemedicine platforms in mental health counseling has been shown to be beneficial in a number of ways. Perhaps most importantly, Reinhardt cited a study from researchers based at the University of Zurich, as detailed by Science Daily, which found that counseling conducted online actually can be more effective than face-to-face sessions. Researchers examined two groups of clients — one group received in-person therapy and the other received therapy via a telemedicine platform. Researchers found that the clients who received counseling sessions online actually experienced better outcomes — 53 percent reported that their depression had abated, compared to 50 percent reporting the same in the group that received in-person counseling. Other benefits include the fact that it is cheaper and allows a wider net of clients to be seen and treated, particularly those who are unable to access mental health services in person, whether due to geography, lack of funds or issues such as social anxiety disorder.
A point of clarification needs to be made, however. Whereas counselors may indeed use online technologies to aid the counseling process or to provide counseling services, they always must abide by the ethical guidelines on the use of technologies. These guidelines can be found in the Ethics Code of American Counseling Association and through the National Board for Certified Counselors’ website. Furthermore, counselors are required by law to be licensed in the locations where their clients reside.
Can technology have an adverse impact on mental health?
Although the use of technology can have a positive impact in terms of helping clients manage and get treated for certain mental health conditions, some research has indicated that the use of technology in general — and especially the internet — actually can be connected with the development of mental health conditions, such as anxiety and depression in some individuals. As Pantic noted, while more research is needed in this area, it is useful to take a closer look at what has been published on this topic so far:
Internet addiction
As detailed by Dr. Romeo Vitelli, writing in an article published by Psychology Today, research has indicated that addiction to the internet , particularly among younger demographics such as adolescents, is becoming a notable issue. Vitelli explained that internet addiction disorder shares many similar features when compared with other forms of addiction, such as withdrawal symptoms when online access is precluded. While the internet can be an agent for good in terms of education and the strengthening of interpersonal relationships, internet addiction can be problematic because it can negatively impact academic success and one’s ability to communicate effectively in person. Vitalli noted that research also has observed a link between certain mental illnesses and internet addiction, including depression, low self-esteem and loneliness.
The link between social media use and mental illness
In his literature review, Pantic explained how several studies have shown a link between depression and the use of social media sites, such as Facebook, Twitter and Instagram. Pantic is quick to caution that much more research is needed before the conclusions reached in the aforementioned studies are widely accepted as fact within the counseling community. Still, the findings are worth examining. Pantic reported on one study from 2013, which found that younger adults who frequently used the social networking site Facebook tended to report feeling less happy, with the use of the social platform possibly to blame. Pantic also reported on a study that he personally was involved with that found among high school students, rates of depression tended to be higher among those who regularly utilized social media sites.
Pantic proffered some possible reasons for the findings, explaining that social media sites, for some individuals, can trigger feelings of low self-esteem. For example, a social media site user may see other people on the site and assume those individuals are more successful, beautiful, intelligent and so on. Pantic explained that a study examining students at a Utah university found those who routinely used social media sites tended to feel as though their peers were more successful and happier than they were. Pantic noted that although these feelings are not necessarily linked to depression, there can be a relationship between them, particularly if the individuals in question already experience or are likely to experience mental health problems.
Dr. Saju Mathew was interviewed for an article by Piedmont Health, wherein he elaborated on this important point : “When we get on social media, we are looking for affirmation and consciously or not, we are comparing our life to the lives of others. As a result, we may not enjoy what’s in the moment.”
In conclusion
The impact of technology has extended into the realm of health care, and it is clear that technology also is making positive changes in terms of mental health care. Research has indicated, however, that the very tools that can help alleviate mental health issues, such as smartphone apps, may be linked with the experience of mental health problems in different contexts. As Pantic stressed, more research is needed before definitive conclusions are drawn. Still, for mental health counselors entering the field, a comprehensive understanding of the nuanced relationship between technology and mental health is necessary for effective practice. Counselors are compelled to expand their technological competencies but always in compliance with their respective ethical guidelines and the rule of law.
Consider Bradley University
If you are interested in pursuing a career as a mental health counselor, consider applying to Bradley University’s online Master of Arts in Counseling — Clinical Mental Health Counseling program. Designed with a busy schedule in mind, completion of the degree program will put you on a direct path to becoming licensed to practice.
Recommended Readings
Substance abuse counseling: What you can learn in a MAC program
What are the Clinical Mental Health specialty courses?
Bradley University Online Counseling Programs
- #5 Among Regional Universities (Midwest) – U.S. News & World Report: Best Colleges (2021)
- #5 Best Value Schools, Regional Universities (Midwest) – U.S. News & World Report (2019)
- Bradley Ranked Among Nation’s Best Universities – The Princeton Review: The Best 384 Colleges (2019). Only 15% of all four-year colleges receive this distinction each year, and Bradley has regularly been included on the list.
- Bradley University has been named a Military Friendly School – a designation honoring the top 20% of colleges, universities and trade schools nationwide that are doing the most to embrace U.S. military service members, veterans and spouses to ensure their success as students.
| 1. | What specialization most interests you? |
| 2. | What is your highest level of education? |
| 3. | Who is this brochure for? |
This paper is in the following e-collection/theme issue:
Published on 30.8.2024 in Vol 11 (2024)
Evaluation of Digital Mental Health Technologies in the United States: Systematic Literature Review and Framework Synthesis
Authors of this article:

- Julianna Catania 1 , MPH ;
- Steph Beaver 1 , MChem ;
- Rakshitha S Kamath 1 , MS, MSL ;
- Emma Worthington 2 , MPH ;
- Minyi Lu 3 , PhD ;
- Hema Gandhi 3 , PhD ;
- Heidi C Waters 3 , PhD ;
- Daniel C Malone 4 , PhD
1 Costello Medical, Boston, MA, United States
2 Costello Medical, Cambridge, United Kingdom
3 Otsuka Pharmaceutical Development & Commercialization Inc, Princeton, NJ, United States
4 Department of Pharmacotherapy, Skaggs College of Pharmacy, University of Utah, Salt Lake City, UT, United States
Corresponding Author:
Daniel C Malone, PhD
Department of Pharmacotherapy
Skaggs College of Pharmacy
University of Utah
30 S 2000 East
Salt Lake City, UT, 84112
United States
Phone: 1 801 581 6257
Email: [email protected]
Background: Digital mental health technologies (DMHTs) have the potential to enhance mental health care delivery. However, there is little information on how DMHTs are evaluated and what factors influence their use.
Objective: A systematic literature review was conducted to understand how DMHTs are valued in the United States from user, payer, and employer perspectives.
Methods: Articles published after 2017 were identified from MEDLINE, Embase, PsycINFO, Cochrane Library, the Health Technology Assessment Database, and digital and mental health congresses. Each article was evaluated by 2 independent reviewers to identify US studies reporting on factors considered in the evaluation of DMHTs targeting mental health, Alzheimer disease, epilepsy, autism spectrum disorder, or attention-deficit/hyperactivity disorder. Study quality was assessed using the Critical Appraisal Skills Program Qualitative and Cohort Studies Checklists. Studies were coded and indexed using the American Psychiatric Association’s Mental Health App Evaluation Framework to extract and synthesize relevant information, and novel themes were added iteratively as identified.
Results: Of the 4353 articles screened, data from 26 unique studies from patient, caregiver, and health care provider perspectives were included. Engagement style was the most reported theme (23/26, 88%), with users valuing DMHT usability, particularly alignment with therapeutic goals through features including anxiety management tools. Key barriers to DMHT use included limited internet access, poor technical literacy, and privacy concerns. Novel findings included the discreetness of DMHTs to avoid stigma.
Conclusions: Usability, cost, accessibility, technical considerations, and alignment with therapeutic goals are important to users, although DMHT valuation varies across individuals. DMHT apps should be developed and selected with specific user needs in mind.
Introduction
Digital health comprises a broad range of technologies, including mobile health, health information technology, wearable devices, and personalized medicine, which serve as tools to enhance health care delivery. Recently, several digital mental health (MH) therapeutics, a category of digital MH technologies (DMHTs), have received US Food and Drug Administration (FDA) approval to prevent, manage, or treat a medical disorder or disease based on evidence from superiority trials and compliance with technical guidelines [ 1 , 2 ]. However, most DMHTs, particularly apps, fall outside FDA jurisdiction because they are not intended to diagnose, treat, or prevent disease and because they are “low risk” in that they would not cause harm in the event of malfunction [ 3 ]. Due to this lack of regulatory framework, few DMHTs are supported by published efficacy studies. One study found that only 16% of MH apps recommended by college counseling centers were supported by efficacy studies published in peer-reviewed journals [ 4 ].
Nonetheless, many health care providers (HCPs) use MH apps in clinical practice. Up to 83% of behavioral health providers in a small study covering the Greater Boston area reported using apps as part of their clinical care, particularly mindfulness apps for patient anxiety management [ 5 ]. As many DMHTs are currently widely used in clinical practice without undergoing any formal assessment for quality or relevance, understanding how DMHTs should be assessed based on factors impacting their value from the perspective of key stakeholders, such as patients, caregivers, providers, payers, and employers, could improve the selection of DMHTs for use by patients, thereby increasing care quality and outcomes for those seeking MH support.
To address identified gaps, a systematic literature review (SLR) was conducted using a published framework to synthesize emerging themes from mixed methods evidence in order to understand how digital health solutions, encompassing both digital therapeutics and direct-to-consumer digital health technologies, are valued, with a focus on MH disorders, Alzheimer disease, epilepsy, autism spectrum disorder (ASD), and attention-deficit/hyperactivity disorder (ADHD) in the United States.
The SLR was performed in accordance with a prespecified protocol and reported in line with the Enhancing Transparency in Reporting the Synthesis of Qualitative Research and PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines [ 6 , 7 ]. The protocol was not registered.
Search Strategy
Electronic databases, encompassing MEDLINE (including MEDLINE In-Process, MEDLINE Daily, and MEDLINE Epub Ahead of Print); Embase; the Cochrane Library (including Cochrane Database of Systematic Reviews and Cochrane Central Register of Controlled Trials); PsycINFO; and the Health Technology Assessment Database, were selected in alignment with this SLR’s target indications and were searched on June 17, 2022. The search terms included combinations of free-text and Medical Subject Heading or Emtree terms related to indications of interest, DMHTs, and relevant outcomes or assessment types (eg, technology assessments and cost; Tables S1-S5 in Multimedia Appendix 1 ). Searches were limited to studies performed in the United States and to those published from 2017 onward.
Manual hand searches of gray literature, namely, the bibliographies of relevant SLRs identified from the electronic database searches and key conference proceedings (2019-2022), were performed to identify additional studies of relevance (Table S6 in Multimedia Appendix 1 ). The FDA website was also searched to identify factors involved in the FDA’s appraisal of relevant MH apps, which could supplement the factors identified in this SLR (Table S7 in Multimedia Appendix 1 ).
Study Selection
Studies were included in the SLR if they met prespecified criteria defined using the SPIDER (Sample, Phenomenon of Interest, Design, Evaluation, Research type) framework, which is appropriate for mixed methods research questions. Eligible studies were published in the English language, were set in the United States, and reported quantitative or qualitative outcomes relating to the factors considered in the evaluation of DMHTs. Only studies published in 2017 or later were included because of the rapidly evolving research area. Eligible studies reported on MH, Alzheimer disease, epilepsy, ASD, or ADHD from user, payer, or employer perspectives (Table S8 in Multimedia Appendix 1 ). While the primary focus of the SLR was MH, neurological conditions were also of interest because their pathologies, symptoms, and treatment strategies can overlap with those of mental illnesses. Alzheimer disease, epilepsy, ASD, and ADHD were selected because they are highly researched and represent diverse types of neurological conditions.
The titles and abstracts of records were assessed for inclusion against these eligibility criteria by 2 independent reviewers, and discrepancies were resolved by consensus, with arbitration by a third reviewer if necessary. Full texts of potentially relevant articles were acquired and screened using the same methodology.
Study Prioritization
Due to the large volume of the evidence identified, additional eligibility criteria were applied to prioritize primary research on theoretical DMHT valuation factors. In line with the thematic framework synthesis objective, theoretical valuation factors were defined as user or DMHT attributes that impact interaction with or perception of DMHTs; therefore, studies that reported only efficacy outcomes, such as mental illness symptom improvement, were deprioritized for full-text review. Secondary research was also deprioritized for full-text review. Studies that reviewed a select app against a framework and studies that reported only the outcomes specific to a select app were deprioritized for data extraction. For example, a study reporting the usability of a specific app’s features would have been deprioritized, while a study reporting what types of features increase MH app usability in general would not.
Data Extraction
All relevant data were extracted into a prespecified Microsoft Excel grid, and a quality assessment was performed for each study. Studies that reported only qualitative data were assessed with the Critical Appraisal Skills Program Qualitative Studies Checklist. Studies that reported only quantitative data were evaluated with the Critical Appraisal Skills Program Cohort Study Checklist, and studies reporting both qualitative and quantitative data were evaluated with both checklists [ 8 ]. Data extractions and quality assessments were performed by a single individual for each study, with the information verified by a second independent individual. Discrepancies were resolved by consensus, with arbitration by a third individual if necessary.
Framework Synthesis
A framework synthesis approach was undertaken to synthesize qualitative and quantitative data identified from the SLR. In line with the “best fit” framework synthesis approach, data were indexed deductively against an existing framework where possible, and novel themes were added inductively as needed [ 9 , 10 ]. The American Psychiatric Association (APA) Mental Health App Evaluation framework was considered the most appropriate framework to address the research objectives of this SLR because its key valuation themes were developed using psychiatrist and patient input, are broadly shared by other evaluation frameworks, are widely acknowledged in the literature, and have been described as durable and adaptable [ 11 - 13 ].
The APA model follows a hierarchical and chronological order whereby the evaluator moves through the framework using prompting questions (eg, “Does the app work offline?”). For this SLR, these questions were either thematically grouped into subthemes or left as prompting questions, as appropriate. The framework was therefore ultimately adapted into 3 levels: themes, subthemes, and more granular valuation criteria. It should be emphasized that this SLR did not aim to formally develop an updated framework to be used in practice by HCPs and their patients but rather was used to form a theoretical basis for understanding DMHT valuation factors, for which novel themes were expected to emerge.
A data-based convergent approach was used to synthesize quantitative and qualitative data [ 14 ]. Data were initially indexed deductively against the prespecified themes within the data collection instrument and then further synthesized within Docear [ 15 ], a mind-map software used to organize and connect data and concepts. Indexing was performed by 1 reviewer and checked by a second independent reviewer. New themes and subthemes that emerged from the literature through inductive coding were added post hoc to the thematic framework, with all extracted data then considered against both the prespecified and novel themes. The evidence identified for each theme was synthesized narratively, taking into consideration the context and design of each study.
Included Studies
A total of 4974 records were retrieved from the electronic databases. Of the 3374 (67.83%) unique records identified following deduplication across the databases, 2891 (85.68%) were excluded based on the eligibility criteria, and an additional 456 (13.52%) were deprioritized because they were not directly related to the topic of interest for this SLR. Excluded and deprioritized full texts are listed in Tables S9 and S10 in Multimedia Appendix 1 , respectively. Therefore, 27 (0.54%) articles were included from the electronic database searches. In addition, 1 article reporting on the same study as an already-included conference abstract was identified during supporting targeted searches and included as a supplementary record, resulting in a total of 28 articles reporting on 26 unique studies (Figure S1 in Multimedia Appendix 1 ). No relevant FDA appraisals were identified in the supplementary search.
Of the 26 included studies, 8 (31%) were quantitative, 12 (46%) were qualitative, and 6 (23%) used a mixed methods approach. While 5 (19%) studies assessed prospective cohorts, 22 (85%) used a cross-sectional approach, including 1 (4%) study that contained both a prospective cohort and a cross-sectional cohort ( Table 1 ). All studies (26/26, 100%) investigated a user perspective, with none specifically investigating payer or employer perspectives. Only 1 (4%) study, which examined ingestible sensor pills and smart pill dispensers to track adherence, investigated a DMHT that was not an app [ 16 ].
| Study (author, year) | Design | Perspective and population | Objectives | Data collection methods |
| Afra et al [ ], 2018 | Cross-sectional, quantitative | To develop a drug-device combination product using an app in combination with antiseizure medications as an epilepsy treatment | Custom survey | |
| Beard et al [ ], 2019 | Cross-sectional, quantitative | , BD , anxiety, OCD , stress-related disorders, and psychotic disorders (N=322) | To characterize general smartphone app and social media use in an acute transdiagnostic psychiatric sample with high smartphone ownership, characterize current engagement and interest in the use of smartphone apps to support MH , and test demographic and clinical predictors of smartphone use | Custom survey |
| Borghouts et al [ ], 2022 | Cross-sectional, mixed methods | : members of the Center on Deafness Inland Empire, comprised people with lived experience as members of the deaf or hard-of-hearing community (N=10) | To investigate the MH needs of the deaf or hard-of-hearing community and how MH apps might support these needs | Custom survey; focus group |
| Boster and McCarthy [ ], 2018 | Cross-sectional, qualitative | recruited through social media and professional listserves (N=8) | To gain insight from speech-language pathologists and parents of children with ASD regarding appealing features of augmentative and alternative communication apps | Focus groups; poll questions |
| Buck et al [ ], 2021a | Cross-sectional, quantitative | referrals or ads (N=43) | To assess caregivers’ interest in an array of specific potential mHealth functions to guide the development of mHealth for caregivers of young adults with early psychosis | Custom survey |
| Buck et al [ ], 2021b | Cross-sectional, quantitative | To understand the needs, interests, and preferences of young adults with early psychosis regarding mHealth by surveying interest in mHealth features and delivery modalities and by collecting information about their digital and web-based behaviors | Custom survey | |
| Carpenter-Song et al [ ], 2018 | Prospective cohort, qualitative | To examine current practices and orientations toward technology among consumers in 3 mental health settings in the United States | Semistructured interviews | |
| Casarez et al [ ], 2019 | Cross-sectional, qualitative | To explore how the well-being of spouses and partners of patients with BD can be improved through mHealth technology | Focus groups; minimally structured, open-ended individual interviews | |
| Connolly et al [ ], 2018 | Cross-sectional, qualitative | , alcohol use disorder, or MDD during the previous year at 9 community-based VA outpatient clinics (N=66) | To examine veterans’ attitudes toward smartphone apps and to assess whether openness toward this technology varies by age or rurality | Semistructured interviews informed by the State of the Art Access Model |
| Cummings et al [ ], 2019 | Cross-sectional, qualitative | treatment at 4 safety-net clinics (N=37) | To examine stakeholder perspectives regarding whether mHealth tools can improve MH treatment for low-income youth with ADHD in safety-net settings and what functions would improve treatment | Focus groups (caregivers) and interviews (HCPs and staff), both semistructured and including open-ended questions and targeted probes |
| Dinkel et al [ ], 2021 | Cross-sectional, qualitative | To explore patient and clinic-level perceptions of the use of depression self-management apps within an integrated primary care setting | Semistructured focus groups; semistructured interviews | |
| Forma et al [ ], 2022 | Cross-sectional, quantitative | To assess caregivers’ preferences and willingness to pay for digital (ingestible sensor pill, medication containers with electronic monitoring, mobile apps, and smart pill dispensers) and nondigital (medication diary and simple pill organizer) tools | Custom discrete choice experiment survey | |
| Hoffman et al [ ], 2019 | Prospective interventional, mixed methods | To test the feasibility of using mHealth apps to augment integrated primary care services, solicit feedback from patients and providers to guide implementation, and develop an MH app toolkit for system-wide dissemination | Custom survey | |
| Huberty et al [ ], 2022 | Cross-sectional (current Calm (Calm.com, Inc) users) and prospective interventional (nonusers of Calm, HCPs), qualitative | : patients with cancer and survivors of cancer with smartphones, some of whom were current subscribers of Calm, a meditation app (N=17) | To develop a mobile meditation app prototype specifically designed for patients with cancer and survivors of cancer | Custom surveys; focus groups |
| Kern et al [ ], 2018 | Cross-sectional, quantitative | : students from a midwestern university with smartphones (N=721) | To investigate the potential usefulness of MH apps and attitudes toward using them | Custom survey |
| Knapp et al [ ], 2021 | Prospective cohort, qualitative | To learn about considerations and perspectives of community behavioral HCPs on incorporating digital tools into their clinical care for children and adolescents | Focus groups | |
| Kornfield et al [ ], 2022 | Prospective cohort, qualitative | or GAD-7 questionnaires, but without serious mental illnesses (eg, BD, schizophrenia), who were not receiving formal care and recruited upon completing free web-based MH self-screening surveys hosted by Mental Health America (N=28) | To investigate how digital technologies can engage young adults in self-managing their MH outside the formal care system | Web-based asynchronous discussion; synchronous web-based design workshop |
| Lipschitz et al [ ], 2019 | Cross-sectional, quantitative | To assess patients’ interest in mHealth interventions for MH, to identify whether provider endorsement would impact interest, to determine reasons for nonuse of mHealth interventions for MH, and to identify what mHealth content or features are of most interest to patients | Custom survey | |
| Mata-Greve et al [ ], 2021 | Cross-sectional, mixed methods | : essential workers during the COVID-19 pandemic or workers who were unemployed or furloughed because of the COVID-19 pandemic, recruited from a web-based research platform (N=1987) | To document psychological stress, to explore DMHT use in response to COVID-19–related stress, to explore the usability and user burden of DMHTs, and to explore which aspects and features of DMHTs were seen as necessary for managing stress during a pandemic by having participants design their own ideal DMHTs | Survey combining custom and validated measures (System Usability Scale, Use Burden Scale) |
| Melcher et al [ ], 2022 and Melcher and Torous [ ], 2020 | Cross-sectional, mixed methods | : college students aged 18-25 years, recruited through social media and word of mouth (N=100) | To examine why college students show poor engagement with MH apps and how apps may be adapted to suit this population | Custom survey; interviews |
| Schueller et al [ ], 2018 | Cross-sectional, mixed methods | : smartphone owners recruited from a research registry (N=827) | To understand where users search for MH apps, what aspects of MH apps they find appealing, and what factors influence their decisions to use MH apps | Custom survey; focus group interviews |
| Schueller et al [ ], 2021 | Cross-sectional, qualitative | : participants who had used an app that allowed them to track their mood, feelings, or mental well-being for ≥2 weeks, recruited from a research registry (N=22) | To understand motivations for and experiences in using mood-tracking apps from people who used them in real-world contexts | Semistructured interviews |
| Stiles-Shields et al [ ], 2017 | Cross-sectional, qualitative | : participants recruited from web-based postings; approximately equal numbers of participants were above and below the criteria for a referral for psychotherapy for depression (N=20) | To identify the barriers to the use of a mobile app to deliver treatment for depression and to provide design implications on the basis of identified barriers | Card sorting task |
| Storm et al [ ], 2021 | Cross-sectional, qualitative | To identify stakeholders’ perspectives on partnering to inform the software development life cycle of a smartphone health app intervention for people with serious mental illness | Semistructured interviews | |
| Torous et al [ ], 2018 | Cross-sectional, quantitative | To understand how individuals with mental illness use their mobile phones by exploring their access to mobile phones and their use of MH apps | Custom survey | |
| Zhou and Parmanto [ ], 2020 | Cross-sectional, mixed methods | To determine user preferences among the several privacy protection methods used in current mHealth apps and the reasons behind those preferences | Custom survey; interview |
a Only information relevant to this systematic literature review is reported in this table.
b MDD: major depressive disorder.
c BD: bipolar disorder.
d OCD: obsessive-compulsive disorder.
e MH: mental health.
f General users are participants who were not necessarily diagnosed with indications of interest.
g ASD: autism spectrum disorder.
h HCP: Health care provider.
i mHealth: mobile health.
j PTSD: posttraumatic stress disorder.
k VA: Veterans Affairs.
l ADHD: attention-deficit/hyperactivity disorder.
m PHQ-9: Personal Health Questionnaire-9.
n GAD-7: Generalized Anxiety Disorder-7.
o DMHT: digital mental health technology.
Most frequently, studies focused on indications for mood, anxiety, or psychotic disorders (15/26, 58%), with other indications of focus including ADHD (2/26, 8%), ASD (1/26, 4%), and epilepsy (1/26, 4%). No relevant studies focused on Alzheimer disease were identified.
A total of 8 (31%) studies assessed the perspectives toward DMHTs of general population participants who were not necessarily diagnosed with relevant conditions [ 19 , 28 , 29 , 33 - 37 ]. Of these populations, several were identified as having an increased risk of MH conditions, such as patients with cancer [ 28 ], college students [ 29 , 34 ], deaf or hard-of-hearing individuals [ 19 ], and people who were unemployed or furloughed during the COVID-19 pandemic [ 33 ]. In addition, 1 (4%) study included a mix of patients who were above and below the referral criteria for psychotherapy for depression [ 37 ].
Thematic Analysis
Evidence was identified for all 5 themes included in the APA framework: engagement style (23/26, 88%), background and accessibility (16/26, 62%), privacy and security (13/26, 50%), therapeutic goal (12/26, 46%), and clinical foundation (8/26, 31%; Table 2 ). Five novel criteria were identified and added to the framework post hoc, 1 each under engagement style (forgetting or feeling unmotivated to use DMHTs) and privacy and security (personal image and stigma) and 3 under background and accessibility (willingness to pay, insurance restrictions, and cost savings compared with professional care).
| Subtheme | Criteria (study reference) | ||
| Short-term usability | , , , ] - , , , , , , ] | ||
| Long-term usability | , - , , , - , - ] [ , , , ] | ||
| Customizability | , , , , , , ] | ||
| Technical | , , , , , ] , , , - , , , ] | ||
| Business model | | ||
| Costs | , ] , , , ] [ ] [ ] - , ] | ||
| Medical claims | | ||
| Stability | , ] | ||
| No specific subtheme | , , ] | ||
| Data collection and storage | , , , , ] | ||
| Privacy policy | , , ] ] ] | ||
| Personal health information | ] , , , ] | ||
| Security measures | , , ] | ||
| Impressions of use | , ] | ||
| User feedback | , ] | ||
| Clinical validity | , ] , - ] , , ] | ||
| Clinically actionable | , , - , , , , ] - , ] | ||
| Therapeutic alliance | , , , , , ] , ] | ||
| Data ownership, access, and export | | ||
a Novel findings that emerged from this systematic literature review.
b These subthemes and criteria were included in the American Psychiatric Association’s framework but were not reported on by studies included in this systematic literature review.
c HCP: health care provider.
Theme 1: Engagement Style
Engagement style was the most reported theme, with evidence identified from 23 (88%) of the 26 studies. Engagement style encompasses how and why users do or do not interact with DMHTs. The long-term usability subtheme was reported by 96% (22/23) of studies, short-term usability by 12 (52%) studies, and customizability by 7 (30%) studies. Findings from short- and long-term usability subthemes were highly interconnected.
A total of 4 studies reported that ease of use promoted short-term DMHT engagement. In the study by Schueller et al [ 35 ], 89.6% of a general population of smartphone users reported ease of use for MH apps as “important” or “very important,” and users qualitatively reported dislike of “overwhelming,” difficult-to-navigate apps. In addition, users valued apps that were “simplistic” [ 34 ], fit into their daily schedules, and were available when needed (eg, during acute symptom experiences) [ 5 , 25 ]. Select supporting qualitative data are presented in Table 3 .
| Subtheme and criteria: findings | Key quotes | |||
| Ease of use | ] ] | |||
| Available engagement styles: use of animation and visuals | ] ] [ ] | |||
| Alignment of app with needs and priorities: gamification | ] | |||
| Alignment of app with needs and priorities: anxiety management | center peer support specialist] [ ] ] | |||
| Alignment of app with needs and priorities: tracking mood, symptoms, or sleep | ] ] [ ] | |||
| Alignment of app with needs and priorities: social media–like features | ] | |||
| Alignment of app with needs and priorities: peer support and chat functions | ] ] [ ] | |||
| Forgot or unmotivated to use | ] ] ] | |||
| Accessibility: mobility barriers | ] | |||
| Accessibility: technical literacy | ] | |||
| Offline functionality: internet and mobile data access as a barrier to use | ] ] | |||
| Willingness to pay | ] ] | |||
| Security associated with collection, use, and transmission of sensitive data (including personal health information) | ] ] | |||
| Transparency and accessibility of privacy policy | ] | |||
| Personal image and stigma | that is protected in the same way my EMR is protected.” [Patient in routine behavioral health care] [ ] | |||
| Security systems used | ] | |||
| Positive change or skill acquisition: apps that impart skills and encourage positive change, in an easy way | ] in cancer care] [ ] | |||
| Ease of sharing and interpretation of data: increase of engagement and symptom reporting | ] | |||
| Therapeutic alliance between patient and HCP | ] | |||
| Evidence of specific benefit: HCP recommendations | ] | |||
| Evidence of specific benefit: increased usage if supported by research, academic institution, or reputable professional society | ] ] | |||
a ASD: autism spectrum disorder.
b MH: mental health.
c ADHD: attention-deficit/hyperactivity disorder
d BD: bipolar disorder.
e Novel criteria identified by this systematic literature review.
f CHA: Cambridge Health Alliance.
g EMR: electronic medical record.
h HCP: health care provider.
Users valued DMHT features that aligned with their needs and priorities, as reflected by findings within the long-term usability subtheme. Across 9 studies, quantitative and qualitative findings demonstrated high interest in anxiety management features such as relaxation tools, breathing exercises, and mindfulness or meditation activities, and 10 studies identified interest in mood, symptom, or sleep tracking ( Tables 3 and 4 ). While most studies (24/26, 92%) focused on MH, patients with epilepsy also reported high interest in features to record seizure dates and types [ 17 ]. Importantly, users in 2 studies emphasized the need for developers to tailor DMHTs to the needs and priorities of the target population ( Table 3 ) [ 28 , 31 ]. Relatedly, mixed attitudes were reported toward positive affirmations and words of encouragement, with many users expressing interest but others emphasizing the value of a human component to DMHTs or cautioning against blanket encouragement and automated messages that could feel insincere [ 19 , 25 , 31 ].
| Features, study, perspective, and finding | Patients, n (%) | Likert score, mean (SD) | |||||
| ], 2021b | |||||||
| Interest in skill practices for managing stress and improving mood | 64 (84.2) | 3.30 (0.98) | |||||
| Interest in skill practices for relaxation | 57 (76) | 3.09 (1.12) | |||||
| Interest in information about relaxation exercises | 59 (77.6) | 3.00 (1.16) | |||||
| Interest in information about healthy sleep practices | 56 (73.7) | 2.93 (1.15) | |||||
| Interest in mindfulness or meditation practices | 44 (59.4) | 2.61 (1.34) | |||||
| ], 2018 | |||||||
| Interest in music to help seizure control | — (75) | — | |||||
| Interest in relaxing music that may help alleviate stress | — (68) | — | |||||
| Interest in relaxing imagery that may help alleviate stress | — (40) | — | |||||
| Interest in drawing or writing while listening to music | — (35) | — | |||||
| Interest in practicing mindfulness | — (63) | — | |||||
| ], 2018 | |||||||
| Comfort level for mindfulness and therapy | — | 3.75 | |||||
| Comfort level for mindfulness and therapy | — | 3.17 | |||||
| ], 2019 | |||||||
| Current use of an MH app with the primary purpose being mindfulness or meditation | — (71) | — | |||||
| ], 2021 | |||||||
| Most frequently endorsed mindfulness tools as a feature when provided options to build their own app | 687 (67.8) | — | |||||
| Most frequently endorsed mindfulness tools as a feature when provided options to build their own app | 584 (60) | — | |||||
| Most frequently endorsed mindfulness tools as a feature when provided options to build their own app | 305 (61.4) | — | |||||
| Most frequently endorsed mindfulness tools as a feature when provided options to build their own app | 966 (65.3) | — | |||||
| ], 2019 | |||||||
| The ability to manage mood, anxiety, or substance use through the use of DMHTs was seen as a benefit of incorporating DMHTs into clinical care | 13 (57) | — | |||||
| ], 2018 | |||||||
| Willingness to use an MH app to track mood or anxiety | 41 (10.3) | — | |||||
| ], 2018 | |||||||
| Interest in a diary to record the date of seizures | — (85) | — | |||||
| Interest in a digital diary to record the type of seizure | — (73) | — | |||||
| Interest in digital diary to log the missed dosages of their medications | — (78) | — | |||||
| ], 2019 | |||||||
| , or PTSD | |||||||
| Interested in progress monitoring (track mood, stress, anxiety, or PTSD symptoms) | 95 (63.8) | — | |||||
| Interested in progress monitoring (track mood, stress, anxiety, or PTSD symptoms) | 80 (67.2) | — | |||||
| ], 2021b | |||||||
| Interest in a feature to set and track goals | 60 (78) | 3.10 (1.05) | |||||
| Interest in a feature to track symptoms over time | 70 (90.9) | 3.44 (0.90) | |||||
| Interest in a feature to track changes in progress toward goals | 66 (86.9) | 3.37 (0.86) | |||||
| Interest in a feature to track wellness behaviors (eg, steps or activity) | 48 (64.9) | 2.86 (1.22) | |||||
| ], 2019 | |||||||
| Current use of an MH app with the primary purpose being mood tracking | — (10) | — | |||||
| Willingness to use an MH app daily to monitor condition | 262 (81) | — | |||||
| Willingness to use an MH app daily to monitor condition | — (85) | — | |||||
| Willingness to use an MH app daily to monitor condition | — (77) | — | |||||
| ], 2021 | |||||||
| Most frequently endorsed symptom tracking (tracking sleep or mood) as a feature when provided options to build their app | 605 (59.7) | — | |||||
| Most frequently endorsed symptom tracking (tracking sleep or mood) as a feature when provided options to build their app | 555 (57) | — | |||||
| Most frequently endorsed symptom tracking (tracking sleep or mood) as a feature when provided options to build their app | 270 (54.3) | — | |||||
| Most frequently endorsed symptom tracking (tracking sleep or mood) as a feature when provided options to build their own app | 890 (60.2) | — | |||||
| ], 2018 | |||||||
| Comfort level for in-app symptom surveys | — | 3.50 | |||||
| Comfort level for in-app symptom surveys | — | 3.11 | |||||
| Comfort level for passive call or text monitoring | — | 2.32 | |||||
| Comfort level for passive call or text monitoring | — | 2.39 | |||||
| Comfort level for passive GPS monitoring | — | 2.31 | |||||
| Comfort level for passive GPS monitoring | — | 2.78 | |||||
a A 5-point Likert scale (0-4) was used.
b Not available.
c A 5-point Likert scale (1-5) was used.
d MH: mental health.
e DMHT: digital mental health technology.
f MDD: major depressive disorder.
g PTSD: posttraumatic stress disorder.
Both patients and caregivers expressed interest in psychoeducational content that aligned with their needs and priorities. When surveyed, >60% of veterans with anxiety or major depressive disorder (MDD), patients with epilepsy, young adults with psychosis, and essential and furloughed workers during the COVID-19 pandemic expressed interest in relevant psychoeducational content [ 17 , 22 , 32 , 33 ]. In contrast, only 4% of college students in another study reported using an MH app for information about MH, although an MH diagnosis was not required for study participation [ 29 ].
Caregivers of young adults with psychosis, caregivers of children with ADHD, and spouses and partners of people with bipolar disorder (BD) were all interested in information related to caring for the individual with the given disorder, such as information on psychological and pharmacological treatments, symptoms and symptom changes, and the MH system [ 21 , 24 , 26 ]. Comparatively smaller, but still notable, proportions of caregivers of patients with psychosis were interested in caregiver-focused information; for instance, 62% to 69% were interested in relaxation exercises, stress and mood management, and community events for caregivers, while 85% to 90% were interested in the aforementioned patient-focused information [ 21 ].
Information delivery–style preference was captured under the short-term usability subtheme. One study in young adults with psychosis and another study with their caregivers revealed that delivering information in a variety of formats was important; when presented with nonmutually exclusive options, >50% of both populations were interested in text content, video content, audio content, and discussion boards [ 21 , 22 ].
Social interaction promoted long-term engagement. Qualitatively, 3 studies found that users valued learning about similar experiences from others via social media–like features, which normalized their experiences and could provide new symptom management strategies ( Table 3 ) [ 28 , 31 , 36 ]. Similarly, 67% of both young adults with psychosis and deaf or hard-of-hearing survey participants (N=9) reported interest in peer support via chat features [ 19 , 22 ]. However, a comparatively smaller proportion of veterans with anxiety or MDD (48.3% of the full cohort and 51.3% of the smartphone user subgroup) were interested in peer support [ 32 ].
Overall, users endorsed social features to support their MH. In the study by Casarez et al [ 24 ], spouses and partners of people with BD likewise desired features to communicate with other caregivers and also emphasized that DMHTs could facilitate conversation and understanding with patients, a sentiment echoed by peer support specialists by Storm et al [ 38 ] ( Table 3 ). However, one oncology HCP cautioned that similar to support groups, “very strict guidelines of what is said” should be implemented to manage potential risks from shared social media–like content, although little additional context was provided [ 28 ].
Spouses and partners of people with BD also suggested both in-app information on accessing professional resources and direct counseling for the patient at times when other support might be inaccessible [ 24 ]. More than half of all workers, employed or unemployed during the COVID-19 pandemic, likewise endorsed links to resources, counseling, and crisis support as DMHT features, and 81.6% of young adults with psychosis endorsed a feature to communicate with professional experts [ 22 , 33 ]. Importantly, compared with patients attending public clinics, patients attending private psychiatric clinics expressed a higher comfort level for in-app communication with HCPs, suggesting demographic differences in the valuation of access to professional support through DMHTs [ 39 ].
A total of 9 studies reported an interest in DMHT reminders and notifications. Across 3 studies, >70% of patients or caregivers were interested in appointment reminders [ 17 , 21 , 22 ]. In addition, 73% and 68% of patients with epilepsy reported interest in reminders for medication refills and adherence, respectively [ 17 ]. Beyond apps, caregivers of patients with MDD, BD, and schizophrenia preferred an ingestible pill sensor that tracked medication adherence, physical activity, mood, and rest 9.79 (95% CI 4.81-19.9), 7.47 (95% CI 3.81-14.65), and 6.71 (95% CI 3.29-13.69) times more than a nondigital pill organizer, respectively [ 16 ]. Qualitatively, patients and caregivers also appreciated reminders, especially if reasonably timed or delivered via text messages [ 27 , 31 ].
Short-term DMHT engagement was also supported by games and graphics, which could communicate information in an accessible way [ 24 ], provide tools for stress management [ 17 , 33 ], and be used therapeutically with children [ 20 , 30 ]. However, some HCPs and caregivers expressed concerns that graphics and games may be distracting for certain children ( Table 3 ) [ 20 ].
In a novel finding, 3 studies reported forgetfulness or lack of motivation as an influence on DMHT engagement. In some cases, disuse was related to stress, other MH symptoms, or poor technical literacy ( Table 3 ) [ 5 , 25 , 31 ]. In contrast, “forgetting to use” DMHTs and “lack of motivation” were perceived as relatively small barriers to use in the study by Stiles-Shields et al [ 37 ].
The third subtheme under engagement style was customizability, which was generally valued by users; 70.9% of a general population of smartphone users noted customization was an important factor [ 35 ]. Similarly, 9.4% of all surveyed veterans and 10.9% of those with smartphones reported disliking a prior DMHT due to a lack of personalization [ 32 ]. Users specifically wanted to be able to opt out of irrelevant features, customize audiovisual and design elements, add personal notes to tracked mood data, and provide ongoing feedback to facilitate personalization [ 20 , 24 , 28 , 31 , 34 ].
Theme 2: Background and Accessibility
A total of 16 (62%) studies reported findings related to DMHT background and accessibility, which considers the developer of the DMHT, as well as functionality and accessibility. Of these, 12 (75%) studies reported on the technical considerations subtheme, 9 (56%) on costs, and 2 (13%) on stability.
Under technical considerations, 9 studies assessed diverse accessibility concerns. Broadly, Storm et al [ 38 ] emphasized that DMHTs should be developed in consideration of patients’ social, cognitive, and environmental needs to avoid overwhelming users. Specifically, 2 studies reported language as a barrier. Deaf or hard-of-hearing participants recommended visual content presentation, such as videos and icons, alongside text and American Sign Language translations where possible [ 19 ]. Similarly, when discussing English-only apps, 1 provider stated as follows: “language is a barrier for some [patients]” [ 5 ]. Mobility issues related to MH symptoms or other conditions and technical literacy, such as difficulties remembering passwords and navigating smartphones or apps, created accessibility barriers as well ( Table 3 ) [ 5 , 25 , 27 , 28 ]. Additional concerns included apps that restricted use based on geographic location [ 19 ], user difficulty in finding relevant, useful apps [ 32 ], and limited mobile device memory for downloading apps [ 5 , 19 ].
Offline functionality, reported by 6 studies, was also captured under the technical considerations subtheme. A majority (5/9, 56%) of participants included in the study by Borghouts et al [ 19 ] expressed concern about their mobile data plans when using their devices. Correspondingly, “availability of Wi-Fi” was noted as a top barrier to the use of apps for depression by Stiles-Shields et al [ 37 ], and several veterans in another study reported that home Wi-Fi connectivity facilitated app use by eliminating cellular data fees [ 25 , 37 ]. Quotes from patients and HCPs echoed the concern about apps without offline functionality ( Table 3 ) [ 23 , 30 ].
Data fees were also captured under the costs subtheme, with hidden or additional costs described as a barrier to app use by 2 studies [ 26 , 37 ]. Parents of children with ADHD reported that difficulty paying phone bills could result in their phones being shut off, limiting DMHT use; one MH clinic administrator stated as follows: “We often encounter parents’ phones being shut off because they haven’t paid their bill...If the app were free or low cost, I imagine it could be very helpful” [ 26 ]. In addition to hidden costs, this quote identifies up-front app costs as a barrier. Quantitatively, more than half of a general population of surveyed college students expressed that cost was a top concern for the use of MH apps [ 34 ]. Qualitative findings from 2 additional studies likewise identified cost as a barrier to DMHT use [ 25 , 27 ].
Three novel cost attributes were identified by this SLR: willingness to pay, insurance restrictions, and cost savings compared with professional care. Four studies, 3 of which focused on apps, explored willingness to pay for DMHTs from a user perspective. Willingness to pay varied based on user preference; some surveyed college students and smartphone users among general populations valued free apps due to financial restrictions or uncertainty around app effectiveness, although 1 student commented that the quality of free trials might be inferior [ 34 , 35 ]. Some smartphone users also voiced a limit on how much they would be willing to spend for an app subscription ( Table 3 ) [ 35 ]. Forma et al [ 16 ] found that caregivers were willing to pay US $255.04 (95% CI US $123.21-US $386.86) more per month for a pill with an ingestible sensor that tracked medication adherence, physical activity, and rest and could connect to an app that also collected self-reported mood data. Moreover, the caregivers were willing to pay US $124.50 (95% CI US $48.18-US $200.81) more per month for an app-connected pill organizer alone than for a nondigital pill organizer [ 16 ]. In contrast, some veterans expressed total disinterest in paid apps, with 1 user citing poor technical literacy (“don’t have the knowledge”) in addition to cost as affecting willingness to pay [ 25 ].
In another novel finding, a speech-language pathologist working with children with ASD preferred a single app including multiple features over separate apps for particular features due to insurance restrictions: “I agree that teaching Apps should be an in-App feature versus their own app because sometimes insurance doesn’t allow us to open the iPads purchased through insurance” [ 20 ]. Although no further detail was provided for this finding, it suggests that there may be restrictions on the use of other apps on devices purchased under insurance, which may have implications for DMHT use in formal care settings due to the lack of financial support.
In a third novel cost-related finding, a small number of participants from a general population of students (3.6%) in one study preferred using an MH app to seeing an MH professional due to cost savings [ 29 ].
A total of 13% (2/16) of studies reported on the subtheme of app stability and technical difficulties, with crashes and poor display quality decreasing DMHT value [ 35 , 37 ]. Participants in the study by Schueller et al [ 35 ] reported that technical difficulties were often an issue for apps developed by medical institutions, which might be effective and safe but less usable than apps from other developers.
Theme 3: Privacy and Security
A total of 13 (50%) out of 26 studies reported findings related to the privacy and security theme, which covered the use and protection of user data by DMHTs. Subthemes were reported relatively equally: data collection and storage (5/13, 38%), personal health information (PHI; 5/13, 38%), privacy policies (4/13, 31%), general privacy (3/13, 23%), and security measures (3/13, 23%).
Quantitative and qualitative findings on general privacy (ie, evidence not categorized under any specific subtheme), the data collection and storage subtheme, and the privacy policies subtheme revealed heterogeneous concerns ( Table 3 ). A total of 74% of a general population of college students reported privacy as a top concern for MH apps, although further details on the specific area of concern were unclear [ 34 ]. In the study by Stiles-Shields et al [ 37 ], participants were highly concerned with data access but less so with general privacy. Echoing the concerns about data collection and storage, 59.1% of veterans with anxiety or MDD in 1 study were concerned about in-app PHI protection [ 32 ]; however, a qualitative study in veterans with posttraumatic stress disorder, alcohol use disorder, or MDD reported that a relatively small number of participants expressed privacy concerns. In the latter study, reasons for the concerns included distrust in Veterans Affairs, belief that digital data are inherently not confidential, and fear of phone hacking [ 25 ]. From an HCP perspective, none of the surveyed behavioral health HCPs agreed with the statement “My patients are concerned about data security,” despite multiple patients within the same study reporting privacy concerns [ 5 ].
Still, privacy policies were important overall, with 70.5% of smartphone MH app users rating having a privacy policy as “very important” or “important” [ 35 ]. Melcher et al [ 34 ] found that although users valued data protection, some reported a lack of awareness about data privacy, and others were concerned about obscure privacy policies and PHI use. As noted in the data collection and storage subtheme, veteran concerns about government use of PHI were heterogeneous [ 25 ].
A novel valuation factor not included in the APA framework related to user concern with PHI privacy and security regarding MH diagnoses and MH app use is a desire to upkeep their personal image or avoid stigma ( Table 3 ) [ 5 , 25 , 29 , 40 ]. For instance, 21.1% of a general college student population preferred MH app use to seeing an MH professional due to anonymity or reduced stigma [ 29 ]. One participant in a study of Veterans Affairs health service users described access to professional care via MH apps as convenient because they could avoid disclosing their use of MH services to explain leaving work early for an appointment [ 25 ].
In line with the overarching concern about PHI privacy and security, users valued app security measures. Schueller et al [ 35 ] reported that 74.2% of users rated data encryption as “important” or “very important.” Users in another study perceived the level of privacy protection as the highest for apps using a combination of a generic app name (ie, not reflecting the indicated MH disorder); easily hidden modules; and secure, user-authenticated web portals for making module changes [ 40 ]. Behavioral health clinic staff echoed the importance of discreet MH app names ( Table 3 ) [ 30 ].
Theme 4: Therapeutic Goal
There were 12 (46%) studies that reported on the factors relating to the integration of DMHTs with users’ therapeutic goals. The clinical actionability and therapeutic alliance subthemes were reported by 83% (10/12) and 58% (7/12) of studies, respectively.
A total of 9 studies reported the value of clinically actionable insights from apps where the users could acquire and practice new skills to make positive changes in their lives ( Table 3 ). For instance, patient and caregiver app users reported interests in “daily tips,” “new ideas,” and “solutions or recommendations” for symptom management [ 26 , 27 , 36 ]. Furthermore, an app that could serve as a resource for multiple management strategies was preferable [ 26 , 28 , 31 ]. Quantitatively, 4% of patients receiving acute treatment in a partial hospitalization program for MH conditions, including mood and psychotic disorders, reported that the primary purpose of their DMHT use was therapy skills practice [ 18 ]. HCPs similarly appreciated that DMHTs could facilitate patients practicing skills outside of formal treatment sessions [ 5 ]. In particular, clinicians from a youth behavioral health clinic noted that DMHTs might be especially beneficial for young users because they could be conveniently and discreetly incorporated into their daily lives [ 30 ].
Users valued easy data sharing with clinicians, particularly for mood- or symptom-tracking features, which could improve communication and the accuracy of symptom reporting during clinical visits [ 5 , 25 - 27 , 34 , 36 ]. For instance, 53% of a general college student population believed that the potential to share information with their clinician was “one of the top benefits” of using DMHTs [ 34 ]. In addition, many HCPs reported active use or interest in the use of DMHTs in clinical practice to facilitate asynchronous communication and increase patient engagement with treatments outside of formal appointments; however, some preferred traditional care strategies for their personalization and flexibility ( Table 3 ) [ 5 , 26 , 30 ].
Theme 5: Clinical Foundation
A total of 8 (31%) studies reported findings related to the clinical foundation of DMHTs, that is, their utility and appropriateness for patients. Clinical validity was the most reported subtheme, with evidence identified from 6 (75%) studies; 2 (25%) studies reported on the user feedback subtheme and 2 (25%) on the impressions of use subtheme, which captured users’ perceptions of app content as accurate and relevant.
Across subthemes, users valued evidence of DMHT benefit or efficacy from various sources. A total of 71.8% of surveyed veterans said that they would use a DMHT if they “saw proof that it worked” for their MH conditions [ 32 ]. Similarly, among the 811 general population participants surveyed, 69.5% ranked direct research evidence as “important” or “very important” for DMHT, and 66.8% ranked indirect research evidence the same [ 35 ]. Qualitative data identified recommendations from HCPs or academic institutions, as well as evidence of DMHT benefit from publications or research studies, as specific sources for clinically valid evidence of benefits ( Table 3 ) [ 27 , 34 , 35 ].
In addition to academic and professional support, the user feedback subtheme captured user interest in whether DMHTs were beneficial for peers or recommended by other trusted individuals. Patients with depression reported that other users’ experiences influenced their app use, with one user wanting to know “...if other people had success using it” [ 27 ]. Quantitatively, user ratings and user reviews were ranked as “important” or “very important” factors in DMHT use by 59.4% and 58.7% of the general population participants, respectively [ 35 ].
Quality Assessment
The risk of bias was overall moderate. Of the 14 studies including quantitative components, only 1 (7%) used relevant validated outcome measurement instruments [ 33 ]; all others used custom questionnaires. Of the 18 studies with qualitative components, 4 (22%) were at risk of selection bias due to participants being exclusively recruited using web-based postings and research registries [ 33 - 35 , 37 ], and only 1 (6%) considered the relationship between researcher and participant when interpreting the results [ 36 ]. Full quality assessments for qualitative and quantitative study components can be found in Tables S11 and S12 in Multimedia Appendix 1 , respectively.
Principal Findings
This SLR aimed to identify and synthesize qualitative and quantitative evidence on how DMHTs are valued by users, payers, and employers in the United States. Evidence from users with or without diagnosed relevant disorders, caregivers, and HCPs was captured across a wide range of demographics. No study reported evaluating an app from a payer or employer perspective. Furthermore, all but one included study focused on mobile apps.
No relevant appraisals of DMHTs were identified from the FDA website searches; however, 8 relevant FDA approval labels or notifications for MH apps or guidance documents for industry and FDA staff were identified. The content of these materials overlapped with some valuation factors identified in this SLR, including evidence of clinical efficacy and safety, app maintenance, and privacy and security.
Engagement style, although not covered by the FDA materials, was the most reported theme by the studies included in this SLR and was found to overlap heavily with other themes. Engagement may be a key consideration for app developers, as app user retention can be low: 1 study showed that >90% of users had abandoned free MH apps within 30 days of installation [ 41 ]. Engagement is also a key clinical concern in terms of DMHT efficacy; one meta-analysis of 25 studies showed that increased use of DMHT modules was significantly associated with positive outcomes regardless of the target MH condition [ 42 ]. The findings of this SLR may therefore be informative to both DMHT designers and HCPs who integrate DMHTs into clinical care by providing insight on DMHT valuation and thus how use and benefit can be improved. For instance, users valued DMHTs that were easy to use and aligned with their needs and priorities, particularly through features that supported their therapeutic goals. In addition, content presented through multiple delivery modes, such as both text and visuals, promoted engagement as well as accessibility.
However, engagement and feature preference varied across populations. For instance, DMHT valuation was affected by technical literacy, which may relate to user demographics; in this SLR, veterans repeatedly emphasized technical literacy as a barrier to DMHT use [ 25 ]. Similarly, offline functionality may be more important for some users. Although 85% of the total United States population owns smartphones, only 59% of Medicare beneficiaries have access to a smartphone with a wireless plan. Moreover, beneficiaries who are older, less educated, disabled, or Black or Hispanic have even lower digital access [ 43 , 44 ]. These findings emphasize the importance of customizability and suggest that app development and selection in the clinical setting should consider the demographics of the target population, particularly in relation to ease of use and offline functionality.
Background and accessibility findings also identified up-front and hidden costs as barriers to DMHT use, with the willingness to pay varying among individuals. This has important implications for app development, considering that many MH apps currently on the market are direct-to-consumer sales and require out-of-pocket payment. App developers often take this approach as it does not require the accumulation of formal evidence of clinical benefit for FDA approval [ 45 ], but it may present a financial barrier to use for consumers.
Privacy and security, reported by 13 (50%) out of 26 studies, was a prevalent theme, with users primarily concerned with data and PHI security within apps. This finding reflects wider research; a 2019 review of 116 depression-related apps retrieved from iTunes and Google Play stores in 2017 found that only 4% of the identified apps had acceptable transparency in privacy and security, with many completely lacking a privacy policy [ 46 ]. Similarly, 39% of MH apps recommended by college counseling centers had no privacy policy, and of those with a policy, 88% collected user data, and 49% shared that data with third parties [ 4 ]. Most evidence identified in this SLR under this theme, as well as findings previously published in the wider literature, focuses on these remote privacy risks. However, local privacy concerns are also important to users. In particular, inconspicuous naming and the ability to hide sensitive modules within MH apps were rated as highly important by both patients and HCPs to maintain user privacy. Users emphasized a desire to avoid the stigma associated with mental illness, which was also reflected by the findings in the engagement style theme: more young adults with psychosis were more interested in in-app messaging with other patients in psychosis recovery (67.1%) than a provider and family member together (47.3%) or their personal support network (59.8%) [ 22 ]. Similarly, youths were interested in apps that could be used discreetly in school or other public settings to avoid potential MH stigma. This is a key, novel finding of this SLR, considering that many app or DMHT components on the market are named after their target disorder.
The use of DMHTs to achieve therapeutic goals was discussed from patient, caregiver, and HCP perspectives, all of which valued DMHTs that had evidence of efficacy, presented clinically actionable information, and facilitated patient-clinician relationships. Of the 5 studies that explored how HCPs value DMHTs in clinical practice, 2 (40%) were restricted to the oncology or ASD settings and were not readily generalizable to wider MH settings [ 20 , 28 ]. In other studies, providers reported interest in using DMHTs to facilitate asynchronous communication with patients and their caregivers, promote patient skill practice, and improve care for children through the use of games and visuals [ 26 , 30 ]. However, while HCPs overall believed that DMHTs improved care, some believed that their clinical training allowed for care personalization beyond what DMHTs could provide. Feature customizability and receipt of input from HCPs and users during app development and testing may be a way to mitigate these concerns, as well as concerns about safety and efficacy, as many available apps do not appropriately address user health concerns [ 47 ].
Findings additionally suggested that training and resources on DMHTs would be beneficial to ensure that HCPs were equipped to integrate DMHTs into their practices [ 5 ]. Collaboration between DMHT specialists and HCPs, along with a shift from randomized controlled trials to effectiveness-implementation hybrid trials, may be a way to streamline the integration of DMHTs into clinical care and provide more training and resources for HCPs [ 30 , 48 ].
This review followed a prespecified protocol and used systematic methods in line with the York Centre for Reviews and Dissemination guidelines [ 49 ] to conduct an exhaustive search of the literature, identifying evidence relevant to the review objectives from multiple databases and supplementary sources. The framework synthesis approach allowed for the inclusion and analysis of both qualitative and quantitative data, providing a detailed picture of not only what DMHT features users value but why they value them, especially in areas where valuation varies across patient demographics. In addition, the APA framework is a robust model created with patient and HCP input that incorporates key valuation themes broadly shared by other frameworks and widely acknowledged in the literature [ 11 - 13 ].
Limitations
Methodological limitations should be considered when interpreting the findings of this SLR. Only publications in English and in United States populations were included. As perceptions of value are influenced by factors including cultures, laws, and health care settings, the findings of this SLR should not be generalized to other countries. For instance, trust in HCPs and rates of longstanding relationships between patients and primary care providers are lower in the United States than in many European nations [ 50 , 51 ], which could impact the type of support users want from DMHTs (ie, engagement style) or interest in DMHT integration with therapeutic goals.
In addition to the prespecified eligibility criteria, deprioritization strategies were implemented due to the large volume of the identified evidence, and this may have resulted in missing relevant articles. In particular, the deprioritization of secondary research and opinion pieces likely led to the exclusion of relevant discussion around payer perspectives and reimbursement, for which no evidence was included in this SLR. Furthermore, although unlikely, there may have been reporting biases in the included studies due to missing results, which this SLR was not able to assess.
This SLR identified no evidence for 3 subthemes included in the APA framework: business model (background and accessibility), which covers DMHT funding sources and potential sources of conflict, medical claims (background and accessibility), which examines whether DMHTs claim to be medical and the trustworthiness of their creators, and data ownership, access, and export (therapeutic goal), which includes sharing data with eHealth records or wellness devices (eg, Apple HealthKit [Apple Inc], Fitbit [Google LLC]). The valuation of these subthemes should be evaluated in future research.
Conclusions
In summary, app usability, cost, accessibility and other technical considerations, and alignment with therapeutic goals were the most reported valuation factors identified by this SLR. Many studies also reported user preference for apps that incorporated privacy and security features that provided protection from stigma. However, individual DMHTs and their features are valued differently across individuals based on demographics and personal preferences. MH apps should be developed and selected with these specific user needs in mind. Feature customizability and input from users and HCPs during development may improve app usability and clinical benefit.
Acknowledgments
The authors thank Max Lee, Costello Medical, US, for medical writing and editorial assistance based on the authors’ input and direction.
Conflicts of Interest
DCM is a consultant for Otsuka Pharmaceutical Development & Commercialization (OPDC) Inc for this project and has received consulting funds from Pear Therapeutics, Sanofi, Avidity, Sarepta, Novartis, and BioMarin. ML, HG, and HCW are employees of OPDC. JC, SB, RSK, and EW are employees of Costello Medical. This research was funded by OPDC.
Electronic database and supplementary search terms, systematic literature review eligibility criteria, publications excluded or deprioritized at full-text review, quality assessments of included studies, and the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flow diagram of the identified publications.
PRISMA checklist.
- Content of premarket submissions for device software functions: guidance for industry and Food and Drug Administration staff. U.S. Food and Drug Administration. Jun 14, 2023. URL: https://www.fda.gov/media/153781/download [accessed 2024-07-19]
- Patel NA, Butte AJ. Characteristics and challenges of the clinical pipeline of digital therapeutics. NPJ Digit Med. Dec 11, 2020;3(1):159. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Policy for device software functions and mobile medical applications: guidance for industry and Food and Drug Administration staff. U.S. Food and Drug Administration. URL: https://www.fda.gov/media/80958/download [accessed 2023-01-06]
- Melcher J, Torous J. Smartphone apps for college mental health: a concern for privacy and quality of current offerings. Psychiatr Serv. Nov 01, 2020;71(11):1114-1119. [ CrossRef ] [ Medline ]
- Hoffman L, Benedetto E, Huang H, Grossman E, Kaluma D, Mann Z, et al. Augmenting mental health in primary care: a 1-year study of deploying smartphone apps in a multi-site primary care/behavioral health integration program. Front Psychiatry. 2019;10:94. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Tong A, Flemming K, McInnes E, Oliver S, Craig J. Enhancing transparency in reporting the synthesis of qualitative research: ENTREQ. BMC Med Res Methodol. Nov 27, 2012;12(1):181. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. Jul 21, 2009;339(jul21 1):b2535. [ FREE Full text ] [ CrossRef ] [ Medline ]
- CASP critical appraisal checklists. Critical Appraisal Skills Programme. URL: https://casp-uk.net/casp-tools-checklists/ [accessed 2022-01-06]
- Carroll C, Booth A, Cooper K. A worked example of "best fit" framework synthesis: a systematic review of views concerning the taking of some potential chemopreventive agents. BMC Med Res Methodol. Mar 16, 2011;11(1):29. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Carroll C, Booth A, Leaviss J, Rick J. "Best fit" framework synthesis: refining the method. BMC Med Res Methodol. Mar 13, 2013;13(1):37. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Kolasa K, Kozinski G. How to value digital health interventions? a systematic literature review. Int J Environ Res Public Health. Mar 23, 2020;17(6):2119. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Lagan S, Aquino P, Emerson MR, Fortuna K, Walker R, Torous J. Actionable health app evaluation: translating expert frameworks into objective metrics. NPJ Digit Med. 2020;3:100. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Lagan S, Emerson MR, King D, Matwin S, Chan SR, Proctor S, et al. Mental health app evaluation: updating the American Psychiatric Association's framework through a stakeholder-engaged workshop. Psychiatr Serv. Sep 01, 2021;72(9):1095-1098. [ CrossRef ] [ Medline ]
- Hong QN, Pluye P, Bujold M, Wassef M. Convergent and sequential synthesis designs: implications for conducting and reporting systematic reviews of qualitative and quantitative evidence. Syst Rev. Mar 23, 2017;6(1):61. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Beel J, Gipp B, Langer S, Genzmehr M. Docear: an academic literature suite for searching, organizing and creating academic literature. In: Proceedings of the 11th annual international ACM/IEEE joint conference on Digital libraries. 2011. Presented at: JCDL '11; June 13-17, 2011:565-566; Ottawa, ON. URL: https://dl.acm.org/doi/10.1145/1998076.1998188 [ CrossRef ]
- Forma F, Chiu K, Shafrin J, Boskovic DH, Veeranki SP. Are caregivers ready for digital? caregiver preferences for health technology tools to monitor medication adherence among patients with serious mental illness. Digit Health. 2022;8:20552076221084472. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Afra P, Bruggers CS, Sweney M, Fagatele L, Alavi F, Greenwald M, et al. Mobile software as a medical device (SaMD) for the treatment of epilepsy: development of digital therapeutics comprising behavioral and music-based interventions for neurological disorders. Front Hum Neurosci. 2018;12:171. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Beard C, Silverman AL, Forgeard M, Wilmer MT, Torous J, Björgvinsson T. Smartphone, social media, and mental health app use in an acute transdiagnostic psychiatric sample. JMIR Mhealth Uhealth. Jun 07, 2019;7(6):e13364. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Borghouts J, Neary M, Palomares K, de Leon C, Schueller SM, Schneider M, et al. Understanding the potential of mental health apps to address mental health needs of the deaf and hard of hearing community: mixed methods study. JMIR Hum Factors. Apr 11, 2022;9(2):e35641. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Boster JB, McCarthy JW. Designing augmentative and alternative communication applications: the results of focus groups with speech-language pathologists and parents of children with autism spectrum disorder. Disabil Rehabil Assist Technol. May 10, 2018;13(4):353-365. [ CrossRef ] [ Medline ]
- Buck B, Chander A, Monroe-DeVita M, Cheng SC, Stiles B, Ben-Zeev D. Mobile health for caregivers of young adults with early psychosis: a survey study examining user preferences. Psychiatr Serv. Aug 01, 2021;72(8):955-959. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Buck B, Chander A, Tauscher J, Nguyen T, Monroe-DeVita M, Ben-Zeev D. mHealth for young adults with early psychosis: user preferences and their relationship to attitudes about treatment-seeking. J Technol Behav Sci. 2021;6(4):667-676. [ CrossRef ] [ Medline ]
- Carpenter-Song E, Noel VA, Acquilano SC, Drake RE. Real-world technology use among people with mental illnesses: qualitative study. JMIR Ment Health. Nov 23, 2018;5(4):e10652. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Casarez RL, Barlow E, Iyengar SM, Soares JC, Meyer TD. Understanding the role of m-health to improve well-being in spouses of patients with bipolar disorder. J Affect Disord. May 01, 2019;250:391-396. [ CrossRef ] [ Medline ]
- Connolly SL, Miller CJ, Koenig CJ, Zamora KA, Wright PB, Stanley RL, et al. Veterans' attitudes toward smartphone app use for mental health care: qualitative study of rurality and age differences. JMIR Mhealth Uhealth. Aug 22, 2018;6(8):e10748. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Cummings JR, Gaydos LM, Mensa-Kwao A, Song M, Blake SC. Perspectives on caregiver-focused mHealth technologies to improve mental health treatment for low-income youth with ADHD. J Technol Behav Sci. Mar 9, 2019;4(1):6-16. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Dinkel D, Harsh Caspari J, Fok L, Notice M, Johnson DJ, Watanabe-Galloway S, et al. A qualitative exploration of the feasibility of incorporating depression apps into integrated primary care clinics. Transl Behav Med. Sep 15, 2021;11(9):1708-1716. [ CrossRef ] [ Medline ]
- Huberty J, Bhuiyan N, Neher T, Joeman L, Mesa R, Larkey L. Leveraging a consumer-based product to develop a cancer-specific mobile meditation app: prototype development study. JMIR Form Res. Jan 14, 2022;6(1):e32458. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Kern A, Hong V, Song J, Lipson SK, Eisenberg D. Mental health apps in a college setting: openness, usage, and attitudes. Mhealth. Jun 2018;4:20. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Knapp AA, Cohen K, Nicholas J, Mohr DC, Carlo AD, Skerl JJ, et al. Integration of digital tools into community mental health care settings that serve young people: focus group study. JMIR Ment Health. Aug 19, 2021;8(8):e27379. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Kornfield R, Meyerhoff J, Studd H, Bhattacharjee A, Williams JJ, Reddy MC, et al. Meeting users where they are: user-centered design of an automated text messaging tool to support the mental health of young adults. In: Proceedings of the 2022 CHI Conference on Human Factors in Computing Systems. 2022. Presented at: CHI '22; April 29-May 5 2022:1-6; New Orleans, LA. URL: https://dl.acm.org/doi/abs/10.1145/3491102.3502046
- Lipschitz J, Miller CJ, Hogan TP, Burdick KE, Lippin-Foster R, Simon SR, et al. Adoption of mobile apps for depression and anxiety: cross-sectional survey study on patient interest and barriers to engagement. JMIR Ment Health. Jan 25, 2019;6(1):e11334. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Mata-Greve F, Johnson M, Pullmann MD, Friedman EC, Griffith Fillipo I, Comtois KA, et al. Mental health and the perceived usability of digital mental health tools among essential workers and people unemployed due to COVID-19: cross-sectional survey study. JMIR Ment Health. Aug 05, 2021;8(8):e28360. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Melcher J, Camacho E, Lagan S, Torous J. College student engagement with mental health apps: analysis of barriers to sustained use. J Am Coll Health. Oct 13, 2022;70(6):1819-1825. [ CrossRef ] [ Medline ]
- Schueller SM, Neary M, O'Loughlin K, Adkins EC. Discovery of and interest in health apps among those with mental health needs: survey and focus group study. J Med Internet Res. Jun 11, 2018;20(6):e10141. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Schueller SM, Neary M, Lai J, Epstein DA. Understanding people's use of and perspectives on mood-tracking apps: interview study. JMIR Ment Health. Aug 11, 2021;8(8):e29368. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Stiles-Shields C, Montague E, Lattie EG, Kwasny MJ, Mohr DC. What might get in the way: barriers to the use of apps for depression. Digit Health. Jun 08, 2017;3:2055207617713827. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Storm M, Venegas M, Gocinski A, Myers A, Brooks J, Fortuna KL. Stakeholders' perspectives on partnering to inform the software development lifecycle of smartphone applications for people with serious mental illness: enhancing the software development lifecycle through stakeholder engagement. In: Proceedings of the 2021 IEEE Global Humanitarian Technology Conference. 2021. Presented at: GHTC '21; October 19-23, 2021:195-199; Seattle, WA. URL: https://ieeexplore.ieee.org/document/9612444 [ CrossRef ]
- Torous J, Wisniewski H, Liu G, Keshavan M. Mental health mobile phone app usage, concerns, and benefits among psychiatric outpatients: comparative survey study. JMIR Ment Health. Nov 16, 2018;5(4):e11715. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Zhou L, Parmanto B. User preferences for privacy protection methods in mobile health apps: a mixed-methods study. Int J Telerehabil. Dec 08, 2020;12(2):13-26. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Baumel A, Muench F, Edan S, Kane JM. Objective user engagement with mental health apps: systematic search and panel-based usage analysis. J Med Internet Res. Sep 25, 2019;21(9):e14567. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Gan DZ, McGillivray L, Han J, Christensen H, Torok M. Effect of engagement with digital interventions on mental health outcomes: a systematic review and meta-analysis. Front Digit Health. 2021;3:764079. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Mobile fact sheet. Pew Research Center. 2021. URL: https://www.pewresearch.org/internet/fact-sheet/mobile/ [accessed 2024-04-29]
- Roberts ET, Mehrotra A. Assessment of disparities in digital access among Medicare beneficiaries and implications for telemedicine. JAMA Intern Med. Oct 01, 2020;180(10):1386-1389. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Powell AC, Torous JB, Firth J, Kaufman KR. Generating value with mental health apps. BJPsych Open. Feb 05, 2020;6(2):e16. [ FREE Full text ] [ CrossRef ] [ Medline ]
- O'Loughlin K, Neary M, Adkins EC, Schueller SM. Reviewing the data security and privacy policies of mobile apps for depression. Internet Interv. Mar 2019;15:110-115. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Akbar S, Coiera E, Magrabi F. Safety concerns with consumer-facing mobile health applications and their consequences: a scoping review. J Am Med Inform Assoc. Feb 01, 2020;27(2):330-340. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Curran GM, Bauer M, Mittman B, Pyne JM, Stetler C. Effectiveness-implementation hybrid designs: combining elements of clinical effectiveness and implementation research to enhance public health impact. Med Care. Mar 2012;50(3):217-226. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Systematic reviews: CRD's guidance for undertaking reviews in health care. Centre for Reviews and Dissemination. 2008. URL: https://www.york.ac.uk/media/crd/Systematic_Reviews.pdf [accessed 2024-04-29]
- Gumas ED, Lewis C, Horstman C, Gunja MZ. Finger on the pulse: the state of primary care in the U.S. and nine other countries. The Commonwealth Fund. URL: https://www.commonwealthfund.org/publications/issue-briefs/2024/mar/finger-on-pulse-primary-care-us-nine-countries [accessed 2024-04-29]
- Huang EC, Pu C, Chou YJ, Huang N. Public trust in physicians-health care commodification as a possible deteriorating factor: cross-sectional analysis of 23 countries. Inquiry. Mar 05, 2018;55:46958018759174. [ FREE Full text ] [ CrossRef ] [ Medline ]
Abbreviations
| attention-deficit/hyperactivity disorder |
| American Psychiatric Association |
| autism spectrum disorder |
| bipolar disorder |
| digital mental health technology |
| Food and Drug Administration |
| health care provider |
| major depressive disorder |
| mental health |
| personal health information |
| Preferred Reporting Items for Systematic Reviews and Meta-Analyses |
| systematic literature review |
| Sample, Phenomenon of Interest, Design, Evaluation, Research type |
Edited by J Torous; submitted 15.02.24; peer-reviewed by A Mathieu-Fritz, K Stawarz; comments to author 05.05.24; revised version received 20.06.24; accepted 21.06.24; published 30.08.24.
©Julianna Catania, Steph Beaver, Rakshitha S Kamath, Emma Worthington, Minyi Lu, Hema Gandhi, Heidi C Waters, Daniel C Malone. Originally published in JMIR Mental Health (https://mental.jmir.org), 30.08.2024.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work, first published in JMIR Mental Health, is properly cited. The complete bibliographic information, a link to the original publication on https://mental.jmir.org/, as well as this copyright and license information must be included.
- Adolescents’ Mental Health Under Impact of Technologies Words: 569
- Effect of Social Media on Adolescent Mental Health Words: 3538
- The Influence of Social Media on Mental Health Words: 2391
- The Impact of Social Media on Mental Health Words: 1367
- Social Media and Mental Health Words: 539
- Social Media’s Multifaceted Impact on Mental Health Words: 1270
- Social Media’s Impact on Mental Health Conditions Words: 1396
- Improving Mental Health by Preventing Mental Illness Words: 4130
- Social Media Use and the Impact on Mental Health Words: 2250
- Social Media and Its Effect on Mental Health Words: 1119
- How Social Media Contribute to Mental Health Words: 1744
- Social Media and Mental Health Relationship Words: 1481
- Adverse Effects of Social Media on Mental Health Words: 2769
- Addressing Mental Health in Higher Education Words: 1629
- Social Media Impact on Mental Health Words: 678
- Mental Health and Illness: Sociological Approach Words: 1375
- Effects of Social Media on Mental Health Words: 656
- Impact of Social Media on Mental Health Words: 1193
- Annotated Bibliography: Social Media and Mental Health Words: 1096
The Impact of Technology on Mental Health
In the contemporary world, symptoms of depression, stress, anxiety, and other mental disorders have become more prevalent among university students. Researchers have proven that time spent on social media, videos, and Instant messaging is directly associated with psychological distress. This bibliography examines different literature discussing how technology affects mental wellness.
The scope of this research is to uncover the consequences of technology use on mental health. The research question above will help examine the relationship between technology use and how this action results in mental illnesses such as anxiety and depression. Information used in this study includes both primary and secondary sources focusing on their observational and experimental data analysis.
The article explores how web-based social networking is a significant limitation to mental health. Deepa and Priya (2020) introduce a concept of time whereby they explain that the hours spent on social networking platforms promote depression and anxiety (Deepa & Priya, 2020). Some of the digital technology students use are Instagram, Facebook, Twitter, YouTube, and other web-based sites platforms, which have become a threat to mental health (Deepa & Priya, 2020). The authors explain that researchers discovered that excessive social media use was linked to mental illnesses during schooling. However, it may be alleviated by dialectical thinking, positivity, meditation, and active coping.
The authors used descriptive research using simple sampling questionnaires and ANOVA to study different groups of students and the social media platforms they use. This system provided mixed results based on these groups and examinations (Deepa & Priya, 2020). The research findings revealed a relationship between being active on social media and depression. The authors contradict a study done by Gordon et al. (2007) that mentions that the time spent on the internet has nothing to do with depression (Deepa & Priya, 2020). Instead, it is what students engage in when they are active online. This study is credible because it is not outdated and involved many participants, which helped strengthen the hypothesis created. This source will be integral in answering the types of technology students use and their consequences on mental wellness. Additionally, the journal’s credibility is guaranteed, considering that the article is an international publication. This title indicates that the journal has been peer-reviewed by many other scholars to ensure the information provided is accurate.
The article examines how internet use affects well-being by analyzing the rate of internet use among college students. Gordon et al. (2007) mention that technology use is triggered by self-expression, consumptive motives, and sharing information. In this study, Gordon et al. (2007) posit that frequency of internet use does not affect mental illness. Instead, they mention that what students do on those platforms is the factor that contributes to mental illness.
First, they mention that the internet has provided ways for students to get new acquaintances, find intimate partners, and conduct research for their college assignments, among other things. This factor indicates that these students’ daily life has become increasingly reliant on the internet (Gordon et al., 2007). Therefore, increased internet use has formed a new environment, full of peer pressure. This explanation is an indication of what they do on the internet. The reason is that they see, admire, and adopt new habits which increase stress and depressive symptoms. Additionally, overdependence on technology has affected family cohesion and social connectedness.
The article provides similar ideologies as Junco et al. (2011) that technology causes social isolation by keeping students from the realities in their environment. It explains that students live a fictional life by actively engaging in technology to hide their true selves (Gordon et al., 2007). The research is valid considering it applies rationales from different authors to justify their deduction that technology use has become an avenue for peer pressure among students. This article is essential since it explains the negative impact of technology on mental health, which is explored in this research. It is also a scholarly article considering that these authors have doctors of philosophy in education, indicating vast knowledge and command to undertake this research.
These researchers use unique survey data to investigate the adverse effects of instant messaging on academic achievement. They explain that instant messaging is not destructive since it can provide company when needed. However, excessive use of instant messaging reduces concentration by diverting the mind’s attention away from the facts of the surroundings. Students lose focus when multitasking activities like chatting while studying (Junco & Cotten, 2011). It also impacts the essential, incidental, and representational processing systems, the foundation for learning and memory. When they fail their tests, they become withdrawn with significant effects, such as anxiety and depression.
Additionally, the authors mention that students using IM become socially disengaged since IM becomes their point of contact with others. Considering all these effects, it is evident that IM can cause anxiety, depression, and social isolation if not regulated. Unlike Gordon et al. (2007), who mention only the detrimental effects of using technology, these authors mention that IM, an example of technology, helps students manage stress (Junco & Cotten, 2011). They explain that through a survey of a target group whereby students reported that IM and other online platforms such as video games had provided contact with the outside world, which relieves stress.
This article’s viability is uncertain because most arguments presented are derived from other researchers’ work (Junco & Cotten, 2011). However, the article is helpful for my research because it provides the negative and positive effects of using technology. The position of this research is that IM can help deal with stress. The viability of this research is verified considering the research has been reviewed by Mendeley Company which generates citations for scholarly articles.
Karim et al. (2020) explore how social media impacts mental health. They begin by conducting a qualitative analysis of 16 different studies provided by various researchers on the topic (Karim et al., 2020). First, they listed different types of social media platforms, including Twitter, Linkedin, Facebook, Instagram, and Snapchat, to be the most widely used social media platforms among the youth. They also mention that social media has become an influential technology in the contemporary world (Karim et al., 2020). Although social media has incredible benefits, it is linked to various mental health issues such as depression and anxiety. Some works agreed that social media use is detrimental to mental well-being, and the timing does not matter (Karim et al., 2020). In contrast, other studies suggested that no evidence justifies the maximum time one should be active on social media. None of the research provided the limit of time recommended for anyone to be active on social media.
The credibility of the piece is jeopardized because the researchers did not conduct their study to identify the correlation between mental health and technology (Karim et al., 2020). However, it provides substantial ideas drawn from other credible sources, which are essential in providing information addressing this topic. For example, their position is that long hours of social media use contribute to depression and anxiety (Karim et al., 2020). This focus is integral in my research since it addresses the impact of technology on mental health by explaining the possible avenues for mental health crises.
Lattie et al. (2019) investigate how the rise in mental disorders such as anxiety and depression correlates with computing technologies. According to these authors, personal computing technologies such as smartphones have become the source of mental health crises since they provide access to social media (Lattie et al., 2019). This platform has promoted harmful ideas that make people experience peer comparison. For instance, “fear of missing out (FOMO) is a pressure promoted by media which dictates how people interact, behave and talk within these platforms” (Lattie et al., 2019, para. 8). FOMO is when people feel the need to fit in with a specific trend by emulating verbatim how their internet friends behave, dress or talk. For instance, if all the girls on social media put on branded clothes for attention, every girl on the platform would also want to be like them. This pressure will result in stress to keep up with the standards set, promoting mental health disorders. These authors conclude that the pressure to feel accepted has increased the number of students negatively affected by technology.
However, the authors also mention that this digital platform has played a significant role in promoting mental health wellness. In addition, some of the interventions available such as the Headspace and Pacifica applications, are technology-enabled and provide coping skills when students face a crisis (Lattie et al., 2019). Lattie et al. (2019) provide similar sentiments as Junco et al. (2011), who also stated that technology is not entirely to blame for mental crises considering that activities such as assimilation of culture affect well-being. Additionally, this article is relevant since it has applied different up-to-date scholarly reasoning to create a hypothesis (Lattie et al., 2019). Finally, the article’s position is that social media promotes mental health by providing coping skills while also deteriorating it by contributing to disorders such as depression. However, this information is contrary to what Junco et al. (2011) mention that technology has the power to relieve stress by providing a coping mechanism.
The article provides informative discussions on the risks that digital presence has promoted. Skillbred-Fjeld et al. (2020) mention that many people have experienced harassment online based on their appearance, ethnicity, age, race, and religion. This exposure to bullying has resulted in psychological distress such as depression and suicidal thoughts. The authors indicate that most students spend more hours on digital media than how they spend with families and friends while also being more exposed to harassment. This disconnect is also a challenge to maintaining mental health, considering it breaks the bond between families and friends.
These authors stress that cyberbullying is a prevalent occurrence in online engagement and has detrimental effects on individuals. This article does not share similar rationales with other articles in this search since it focuses on proving how cyberbullying results in mental illness. The article answers the proposed research question, and its position is that cyberbullying affects most students using digital communication systems (Skilbred-Fjeld et al., 2020). The article is credible for this research since the author engaged in intensive searches, which enhanced the viability of the information provided.
In her article “Cyberspace and Identity,” Turkle (1999) posits that the development of cyberspace interactions has extended the range of identities. The author establishes her case with four essential points. Her first observation is that digital presence is based on fiction and not reality. Second, she claims that digital profile results from a digital exhibition that does not last. The third point made by Turkle (1999) is that online identity affects real self-considering the fact that it affects thoughts and behaviors). Finally, she claims that online identity exemplifies a cultural conception of diversity.
This author introduces the aspect of role-playing promoted by digital presence. She mentions that people are given a chance to portray themselves in a different light from reality on digital platforms considering the anonymity established when altering self-image through textual construction (Turkle, 1999). The research by Gordon et al. (2007) reinforced this claim when they mentioned that digital engagement does not cause mental illness. Instead, what students do on those platforms is the primary factor contributing to mental illness (Turkle, 1999). This factor is relatable in the current digital world since people share their adventurous moments, making others who cannot enjoy such things feel unworthy, posing a significant threat to mental wellness. The article’s position is that images portrayed on digital platforms are illusions, and they have promoted peer pressure, anxiety, and depression in people who believe them to be true (Turkle, 1999). The same sentiments are shared by Skilbred-Fjeld et al. (2020) since they mention that social media has become a site to dehumanize others who are less privileged. This occurrence promotes fear, self-hate, and depression, indicating a match in reasoning among these authors.
Deepa, M., & Priya, K. (2020). Impact of social media on mental health of students. International Journal of Scientific & Technology Research , 9 (03). Web.
Gordon, C., Juang, L., & Syed, M. (2007). Internet use and well-being among college students: Beyond frequency of use. Journal of College Student Development , 48( 6), 674-688. Web.
Junco, R., & Cotten, S. R. (2011). Perceived academic effects of instant messaging use.
Computer & Education , 56 (2), 370-378. Web.
Karim, F., Oyewande, A. A., Abdalla, L. F., Ehsanullah, R. C., & Khan, S. (2020). Social media use and its connection to mental health: A systematic review. Cureus , 12 (6). Web.
Lattie, E. G., Lipson, S. K., & Eisenberg, D. (2019). Technology and college student mental health: Challenges and opportunities. Frontiers in psychiatry , (10) , 246. Web.
Skilbred-Fjeld, S., Reme, S. E., & Mossige, S. (2020). Cyberbullying involvement and mental health problems among late adolescents. Cyberpsychology: Journal of Psychosocial Research on Cyberspace , 14 (1). Web.
Turkle, S. (1999). Looking toward cyberspace: Beyond grounded sociology. Cyberspace and identity. Contemporary Sociology , 28 (6), Web.
Cite this paper
- Chicago (N-B)
- Chicago (A-D)
StudyCorgi. (2022, December 10). The Impact of Technology on Mental Health. https://studycorgi.com/the-impact-of-technology-on-mental-health/
"The Impact of Technology on Mental Health." StudyCorgi , 10 Dec. 2022, studycorgi.com/the-impact-of-technology-on-mental-health/.
StudyCorgi . (2022) 'The Impact of Technology on Mental Health'. 10 December.
1. StudyCorgi . "The Impact of Technology on Mental Health." December 10, 2022. https://studycorgi.com/the-impact-of-technology-on-mental-health/.
Bibliography
StudyCorgi . "The Impact of Technology on Mental Health." December 10, 2022. https://studycorgi.com/the-impact-of-technology-on-mental-health/.
StudyCorgi . 2022. "The Impact of Technology on Mental Health." December 10, 2022. https://studycorgi.com/the-impact-of-technology-on-mental-health/.
This paper, “The Impact of Technology on Mental Health”, was written and voluntary submitted to our free essay database by a straight-A student. Please ensure you properly reference the paper if you're using it to write your assignment.
Before publication, the StudyCorgi editorial team proofread and checked the paper to make sure it meets the highest standards in terms of grammar, punctuation, style, fact accuracy, copyright issues, and inclusive language. Last updated: December 10, 2022 .
If you are the author of this paper and no longer wish to have it published on StudyCorgi, request the removal . Please use the “ Donate your paper ” form to submit an essay.
Participant Behavior and Community Response in Online Mental Health Communities: Insights from Reddit
39 Pages Posted: 30 Aug 2024
Virginia Morini
University of Pisa
Maria Sansoni
affiliation not provided to SSRN
Giulio Rossetti
Dino pedreschi, carlos castillo.
Universitat Pompeu Fabra
The growing presence of online mutual-help communities has significantly changed how people access and provide mental health support. While extensive research has explored self-disclosure and social support dynamics within these communities, less is known about users' distinctive behavioral patterns, posting intents, and community response. This study analyzes a large-scale, five-year Reddit dataset of 67 mental health-related subreddits, comprising over 3.4 million posts and 24 million comments from approximately 2.4 million users. We categorize subreddits based on the Diagnostic and Statistical Manual of Mental Disorders and compare behavioral patterns found in these communities with Reddit non-mental health ones. Leveraging Reddit's post flair feature, we define a ground truth for post intents and apply an automated classification method to infer intents across the dataset. We then use causal inference analysis to assess the effect of community responses on subsequent user behavior.Our analysis reveals that mental health-related subreddits feature unique characteristics in content length, throwaway account usage, user actions, persistence, and community response. These online behaviors mirror those in other mutual-help Reddit communities and resonate with offline patterns, while diverging from non-support-oriented subreddits. We also find that seeking support and venting are the predominant posting intents, with users tending to maintain consistent intents over time. Furthermore, we observe that receiving comments and reactions significantly influences user follow-up engagement, fostering increased participation.These findings highlight the supportive role of online mental health communities and emphasize the need for tailored design to optimize user experience and support for individuals facing mental health challenges.
Keywords: Online Mental health communities, Reddit, mental health, Self-disclosure, Posting Intents, Community Response
Suggested Citation: Suggested Citation
Virginia Morini (Contact Author)
University of pisa ( email ).
Lungarno Pacinotti, 43 Pisa PI, 56126 Italy
affiliation not provided to SSRN ( email )
No Address Available
Universitat Pompeu Fabra ( email )
Ramon Trias Fargas, 25-27 Barcelona, E-08005 Spain
Do you have a job opening that you would like to promote on SSRN?
Paper statistics, related ejournals, psychology research methods ejournal.
Subscribe to this fee journal for more curated articles on this topic

45,000+ students realised their study abroad dream with us. Take the first step today
Meet top uk universities from the comfort of your home, here’s your new year gift, one app for all your, study abroad needs, start your journey, track your progress, grow with the community and so much more.

Verification Code
An OTP has been sent to your registered mobile no. Please verify

Thanks for your comment !
Our team will review it before it's shown to our readers.

- Speech Writing /

5 Minutes Speech on Technology and Mental Health

- Updated on
- May 6, 2024

Technology and Mental Health Speech: Can you live without your smartphone for a minute? You know what your answer is. We are all addicted to our gadgets and it almost seems impossible to live without them.
Technology has overpowered us. On one hand, technology has improved and lessened the workload on our shoulders, but on the other hand, it has become one of the ways to get distracted from work. Checking notifications every minute, worrying about the specifications of recently launched gadgets, and many other activities indicate this addiction. All this dependency somewhere leads to mental unrest as well.
Table of Contents
- 1 Speech on Technology and Mental Health
- 2 10 Lines Speech on Technology and Mental Health
- 3 Paragraph on Technology and Mental Health
Also Read: Essay on Advantages And Disadvantages of Social Media
Speech on Technology and Mental Health
‘Greetings to all teachers and students gathered here. Today, I stand before you to deliver my point of view on the trending topic in society, which is technology and mental health.
As students, we are growing in an environment where technology is slowly and steadily becoming the core of our private lives. Whether it is social media, smartphones, or any electronic amenities, everywhere we are surrounded by a digital panorama.
So shall we say that these robotics are bringing positive changes to us as well as to the community?
In the first place, advances in medical technology help in better diagnosis and treatment; conversely, telemedicine, robotic surgery, and telehealth help individuals without any geographical boundaries. Patients can easily get access to medical consultations, receive diagnoses, and even undergo surgeries without the physical availability of health consultants.
However, the same technology that showered these unexpected miracles also has a flip side. The absence of smartphones, and social media, contributes to the feeling of loneliness and social isolation. It is therefore suggested to maintain a balance the virtual and real-world interactions. Engaging with people face-to-face not only helps in quality connection and communication but also contributes positive impacts to healthy mental conditions.
One major concern about the impact of technology through social media is the constant exposure of carefully selected visuals and refined lifestyles on platforms like Facebook, Instagram and likewise. Students need to understand that whatever they are seeing online is not the full picture.
Another noteworthy issue of the impact of technology is the rise of cyberbullying. Anonymous people by online platforms harm individuals to engage in harmful behaviour. Students should be aware of the potential results of cyberbullying and try to connect with people whom they know well.
Apart from this online mode of communication, the prevalence of gaming and screen time among students is again a crucial area which requires attention. While video games can be entertaining and even educational too, excessive gaming may lead children to sedentary behaviour and lack of physical activity which can negatively impact mental health at last.
Moreover, the constant gaming and screen time among students also matter as gaming excessiveness may lead to sedentary behavior and a lack of physical activity can negatively impact the mental health of the students. The practice of encouraging outdoor activities and a balanced approach to screen time can help for overall well-being of the students.
While covering every aspect of the negative effects, how can we forget about the constant notification and overloaded information that keeps on ringing and can students stress and create hurdles in concentration?
As students, we must learn to utilise the power of digital technology positively. Creating a healthy relationship with technology has a positive impact on mental health. It is important to prioritise self-care, with adequate sleep, physical activity, and maintaining real-world connections. You should remember that taking breaks from the digital world is a strong signal of strength and not weakness.
In helping the students learn about the drawbacks of technology school can also play an important role. Incorporation of digital literacy and mental health into the curriculum can empower the students to understand digital technology positively. Teachers and parents should keep an open conversation about technology, mental health, and the importance of finding a balance between the two.
In conclusion, technology and mental health are complex. While technology offers opportunities and conveniences, it also poses challenges that require thoughtful consideration. As a student, you are the architect of the future, and it depends on how you want to handle this digital age which will not only help to shape your future but also the well-being of generations to come.
Stay connected with technology to enhance knowledge rather than hinder mental health. Do not be afraid to take support whenever need to get out of this addiction after all, everything comes with a boon as well as a bane.
Also Read: Speech on Future of Technology in India
Also Read: How to Prepare for UPSC in 6 Months?
10 Lines Speech on Technology and Mental Health
Here is the short and simple 10-line on technology and mental health.
- The constant connectivity with overloaded information through various technical gadgets can lead to stress and anxiety.
- As a part of technology, social media also contributes to cyberbullying, unrealistic beauty standards,s and the omnipresent fear of missing out.
- The pressure of creating an online persona likes, and comments can also pressure the mental well-being of the individual.
- It is a difficult task for students to recognize the fake images and lifestyles on social media.
- Excessive screen time on smartphones, tablets, or computers is the source of various mental issues.
- Long exposure to gadgets and screens, especially before bedtime, disturbs the sleeping pattern of a person and also affects mood as well as mental health.
- It is seen that students who are addicted to online video games and social media pose a risk to their mental health.
- Digital detox is necessary to detoxify from the constant stimuli of technology.
- Students should be encouraged to take periodic breaks from screens and should be engaging more in outdoor activities.
- Technology can be used to make use of mediate sessions and mental health resources.
Paragraph on Technology and Mental Health
Spending maximum time on social media and other online platforms can make you feel isolated. Also, constant notifications and pressure to keep one connected can lead to burnout.
The five ways to improve mental health are as follows: Try to spend more time in the natural environment. Do not isolate yourself. Instead, attend social activities and connect with others. It is suggested to give time to physical activities such as jogging, long walks, and regular exercise. Take complete sleep. Learn to be creative in every small thing you do.
Excessive screen time affects sleeping disturbance and can create strain in the eye. All these disturbances can affect the mental health of a person.
Yes, technology influences the behaviour of an individual. For example, social media affects self-esteem, and online interaction can impact real-world social skills.
The five negative effects of science and technology are environmental degradation, privacy breaches, social inequalities, and misuse of user rights and creative common licences.
Related Articles
For more information on such interesting speech topics for your school, visit our speech writing page and follow Leverage Edu .
Deepika Joshi
Deepika Joshi is an experienced content writer with educational and informative content expertise. She has hands-on experience in Education, Study Abroad and EdTech SaaS. Her strengths lie in conducting thorough research and analysis to provide accurate and up-to-date information to readers. She enjoys staying updated on new skills and knowledge, particularly in the education domain. In her free time, she loves to read articles, and blogs related to her field to expand her expertise further. In her personal life, she loves creative writing and aspires to connect with innovative people who have fresh ideas to offer.
Leave a Reply Cancel reply
Save my name, email, and website in this browser for the next time I comment.
Contact no. *

Connect With Us
45,000+ students realised their study abroad dream with us. take the first step today..

Resend OTP in

Need help with?
Study abroad.
UK, Canada, US & More
IELTS, GRE, GMAT & More
Scholarship, Loans & Forex
Country Preference
New Zealand
Which English test are you planning to take?
Which academic test are you planning to take.
Not Sure yet
When are you planning to take the exam?
Already booked my exam slot
Within 2 Months
Want to learn about the test
Which Degree do you wish to pursue?
When do you want to start studying abroad.
January 2024
September 2024
What is your budget to study abroad?
How would you describe this article ?
Please rate this article
We would like to hear more.
Have something on your mind?

Make your study abroad dream a reality in January 2022 with
India's Biggest Virtual University Fair

Essex Direct Admission Day
Why attend .

Don't Miss Out
Can smartphone applications and wearable technologies improve workplace well-being and help manage stress? A systematic review
- Published: 24 August 2024
Cite this article

- Margherita Herold ORCID: orcid.org/0000-0001-9062-9846 1 , 2 ,
- Silvia Simbula 1 , 2 &
- Marcello Gallucci 1
In recent years, increasing attention has been paid to identifying new approaches to improve workplace well-being and manage stress with the help of m-health solutions. The primary purpose of this review is to provide an overview of the current use of smartphone applications integrated with wearable technologies in stress management and the promotion of well-being in the workplace. A key terms literature search was performed using multiple electronic databases. The review process followed the international PRISMA statement guidelines. A quality assessment was conducted using the Mixed Methods Appraisal Tool. A total of 25 eligible papers published between 2016 and 2023 were included. Interventions proposed were heterogeneous and primarily based on smartphone applications (72%). 84% of the interventions had background theories, with a high preference for Mindfulness. Interventions were reported as generally significant, and the combined use of smartphone applications and wearable technologies increased awareness at the individual and collective levels. In conclusion, the review demonstrates how the interventions developed through the synergy of technologies can effectively promote well-being and reduce stress in the workplace context, decreasing the stigma still related to mental health and increasing peer support strategies. This work opens the doors to several possibilities for future research. It could be interesting to indagate more in-depth the value of integration between technologies and, eventually, the integration with more traditional type of interventions, e.g., face-to-face activities, evaluating if this synergy can amplify and strengthen the results.
Protocol registration: The review protocol was registered with PROSPERO: CRD42023423126 (May 2nd, 2023).
This is a preview of subscription content, log in via an institution to check access.
Access this article
Subscribe and save.
- Get 10 units per month
- Download Article/Chapter or eBook
- 1 Unit = 1 Article or 1 Chapter
- Cancel anytime
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions

Similar content being viewed by others

mHealth interventions to reduce stress in healthcare workers (fitcor): study protocol for a randomized controlled trial

Monitoring and Reducing Workplace Stress with Smartphone Usage: A Systematic Literature Review

Effectiveness of Mobile-Based Mindfulness Interventions in Improving Mindfulness Skills and Psychological Outcomes for Adults: a Systematic Review and Meta-regression
Explore related subjects.
- Artificial Intelligence
Agyapong, V. I. O., Hrabok, M., Vuong, W., Gusnowski, A., Shalaby, R., Mrklas, K., & Greenshaw, A. J. (2020). Closing the psychological treatment gap during the COVID-19 pandemic with a supportive text messaging program: Protocol for implementation and evaluation. JMIR Research Protocols , 9 (6), e19292.
Article PubMed PubMed Central Google Scholar
Ajzen, I. (1991). The theory of planned behavior. Organizational Behavior and Human Decision Processes , 50 (2), 179–211.
Article Google Scholar
Ajzen, I. (2020). The theory of planned behavior: Frequently asked questions. Human Behavior and Emerging Technologies , 2 (4), 314–324.
Asadzadeh, A., & Kalankesh, L. R. (2021). A scope of mobile health solutions in COVID-19 pandemics. Informatics in Medicine Unlocked , 23 , 100558.
Attaran, M. (2020). July). Digital technology enablers and their implications for supply chain management. Supply Chain Forum: An International Journal (Vol. 21, pp. 158–172). Taylor & Francis. 3.
Google Scholar
Axelsen, J. L., Meline, J. S. J., Staiano, W., & Kirk, U. (2022). Mindfulness and music interventions in the workplace: Assessment of sustained attention and working memory using a crowdsourcing approach. BMC Psychology , 10 (1), 1–16.
Bakker, A. B., & Demerouti, E. (2007). The job demands-resources model: State of the art. Journal of Managerial Psychology , 22 (3), 309–328.
Bannai, A., & Tamakoshi, A. (2014). The association between long working hours and health: A systematic review of epidemiological evidence. Scandinavian Journal of work Environment & Health , 40 , 5–18.
Bartlett, L., Martin, A., Neil, A. L., Memish, K., Otahal, P., Kilpatrick, M., & Sanderson, K. (2019). A systematic review and meta-analysis of workplace mindfulness training randomized controlled trials. Journal of Occupational Health Psychology , 24 (1), 108.
Article PubMed Google Scholar
Bartlett, L., Martin, A. J., Kilpatrick, M., Otahal, P., Sanderson, K., & Neil, A. L. (2022). Effects of a mindfulness app on employee stress in an Australian public sector workforce: Randomized controlled trial. JMIR mHealth and uHealth , 10 (2), e30272.
Bhardwaj, A., & Srivastava, A. (2008). Occupational health and psychological well-being of industrial employees. Industrial Psychiatry Journal , 17 (1), 28–32.
Bootsman, R., Markopoulos, P., Qi, Q., Wang, Q., & Timmermans, A. A. (2019). Wearable technology for posture monitoring at the workplace. International Journal of Human-Computer Studies , 132 , 99–111.
Borjalilu, S., Mazaheri, M. A., & Talebpour, A. (2019). Effectiveness of mindfulness-based stress management in the mental health of Iranian university students: A comparison of blended therapy, face-to-face sessions, and mHealth app (Aramgar). Iranian Journal of Psychiatry and Behavioral Sciences , 13 (2), e84726.
Boutron, I., Page, M. J., Higgins, J. P., Altman, D. G., Lundh, A., Hróbjartsson, A., & Cochrane Bias Methods Group. (2019). Considering bias and conflicts of interest among the included studies. Cochrane handbook for systematic reviews of interventions , 177–204.
Chen, J., Abbod, M., & Shieh, J. S. (2021). Pain and stress detection using wearable sensors and devices—. A Review Sensors , 21 (4), 1030.
Coelhoso, C. C., Tobo, P. R., Lacerda, S. S., Lima, A. H., Barrichello, C. R. C., AmaroJr, E., & Kozasa, E. H. (2019). A new mental health mobile app for well-being and stress reduction in working women: Randomized controlled trial. Journal of Medical Internet Research , 21 (11), e14269.
Cohen, C., Pignata, S., Bezak, E., Tie, M., & Childs, J. (2023). Workplace interventions to improve well-being and reduce burnout for nurses, physicians and allied healthcare professionals: A systematic review. British Medical Journal Open , 13 (6), e071203. https://doi.org/10.1136/bmjopen-2022-071203
Colbert, A., Yee, N., & George, G. (2016). The digital workforce and the workplace of the future. Academy of Management Journal , 59 (3), 731–739.
Cook, R., Billings, D., Hersch, R., Back, A., & Hendrickson, A. (2007). A field test of a web-based workplace health promotion program to improve dietary practices, reduce stress, and increase physical activity: Randomized controlled trial. Journal of Medical Internet Research , 9 (2), e627.
Cooper, C. L., & Cartwright, S. (1997). An intervention strategy for workplace stress. Journal of Psychosomatic Research , 43 (1), 7–16.
Cortes, G. M., & Salvatori, A. (2019). Delving into the demand side: Changes in workplace specialization and job polarization. Labour Economics , 57 , 164–176.
Cox, T., Griffiths, A., & Rial-Gonzalez, E. (2000). Work-related stress . Office for Official Publications of the European Communities.
Crivelli, D., Fronda, G., Venturella, I., & Balconi, M. (2019). Stress and neurocognitive efficiency in managerial contexts: A study on technology-mediated mindfulness practice. International Journal of Workplace Health Management , 12 (2), 42–56.
Danna, K., & Griffin, R. W. (1999). Health and well-being in the workplace: A review and synthesis of the literature. Journal of Management , 25 (3), 357–384.
Das, K. V., Jones-Harrell, C., Fan, Y., Ramaswami, A., Orlove, B., & Botchwey, N. (2020). Understanding subjective well-being: Perspectives from psychology and public health. Public Health Reviews , 41 , 1–32.
De Korte, E. M., Wiezer, N., Janssen, J. H., Vink, P., & Kraaij, W. (2018). Evaluating an mHealth app for health and well-being at work: Mixed-method qualitative study. JMIR mHealth and uHealth , 6 (3), e6335.
Deen, M. J. (2015). Information and communications technologies for elderly ubiquitous healthcare in a smart home. Personal and Ubiquitous Computing , 19 , 573–599.
Delle Fave, A. (Ed.). (2006). Dimensions of well-being: research and intervention . FrancoAngeli.
Dembe, A. E., Erickson, J. B., Delbos, R. G., & Banks, S. M. (2005). The impact of overtime and long work hours on occupational injuries and illnesses: New evidence from the United States. Occupational and Environmental Medicine , 62 (9), 588–597.
Dementyev, A., Hodges, S., Taylor, S., & Smith, J. (2013, April). Power consumption analysis of Bluetooth Low Energy, ZigBee and ANT sensor nodes in a cyclic sleep scenario. In 2013 IEEE International Wireless Symposium (IWS) (pp. 1–4). IEEE.
Di Pasquale, V., De Simone, V., Radano, M., & Miranda, S. (2022). Wearable devices for health and safety in production systems: A literature review. IFAC-PapersOnLine , 55 (10), 341–346.
Diener, E. (2000). Subjective well-being: The science of happiness and a proposal for a national index. American Psychologist , 55 (1), 34.
Diener, E. (Ed.). (2009). Assessing well-being: The collected works of Ed Diener (Vol. 39). Springer Science & Business Media.
Dunne, L., Walsh, P., Smyth, B., & Caulfield, B. (2007). A system for wearable monitoring of seated posture in computer users. In 4th International Workshop on Wearable and Implantable Body Sensor Networks (BSN 2007) March 26–28, 2007 RWTH Aachen University, Germany (pp. 203–207). Springer Berlin Heidelberg.
Ebert, D. D., Kählke, F., Buntrock, C., Berking, M., Smit, F., Heber, E., & Lehr, D. (2018). A health economic outcome evaluation of an internet-based mobile-supported stress management intervention for employees. Scandinavian Journal of work Environment & Health , 171–182.
Economides, M., Bolton, H., Male, R., & Cavanagh, K. (2022). Feasibility and preliminary efficacy of web-based and mobile interventions for common mental health problems in working adults: Multi-arm randomized pilot trial. JMIR Formative Research , 6(3), e34032.
Engbers, L., & Sattelmair, J. (2008). Monitoring and evaluation of worksite health promotion progams: Current state of knowledge and implications for practice . World Health Organization (WHO).
European Agency for Safety and Health at Work. (EU-OSHA) (2022). OSH Pulse - Occupational safety and health in post-pandemic workplaces . https://osha.europa.eu/en/publications/osh-pulse-occupational-safety-and-health-post-pandemic-workplaces Accessed 10 April 2024.
Eysenbach, G. (2001). What is e-health? Journal of Medical Internet Research , 3 (2), e833.
Ferraro, V., & Ugur, S. (2011, June). Designing wearable technologies through a user centered approach. In Proceedings of the 2011 Conference on Designing Pleasurable Products and Interfaces (pp. 1–8).
Fiol-DeRoque, M. A., Serrano-Ripoll, M. J., Jiménez, R., Zamanillo-Campos, R., Yáñez-Juan, A. M., Bennasar-Veny, M., & Ricci-Cabello, I. (2021). A mobile phone–based intervention to reduce mental health problems in health care workers during the COVID-19 pandemic (PsyCovidApp): Randomized controlled trial. JMIR mHealth and uHealth , 9 (5), e27039.
Free, C., Phillips, G., Galli, L., Watson, L., Felix, L., Edwards, P., Patel, V., & Haines, A. (2013). The effectiveness of mobile-health technology-based health behaviour change or disease management interventions for health care consumers: A systematic review. PLoS Medicine , 10 (1), e1001362.
Frone, M. R. (2006). Prevalence and distribution of illicit drug use in the workforce and in the workplace: Findings and implications from a U.S. National survey. Journal of Applied Psychology , 91 (4), 856–869.
Giddens, L., Leidner, D., & Gonzalez, E. (2017). The role of fitbits in corporate wellness programs . Does step count matter?.
Glance, D. G., Ooi, E., Berman, Y. E., Glance, C. F., & Barrett, H. R. (2016, April). Impact of a digital activity tracker-based workplace activity program on health and well-being. In Proceedings of the 6th International Conference on Digital Health Conference (pp. 37–41).
Guest, D. E. (2002). Perspectives on the study of work-life balance. Social Science Information , 41 (2), 255–279.
Haddaway, N. R., Page, M. J., Pritchard, C. C., & McGuinness, L. A. (2022). PRISMA2020: An R package and Shiny app for producing PRISMA 2020-compliant flow diagrams, with interactivity for optimized digital transparency and open synthesis. Campbell Systematic Reviews , 18 (2), e1230.
Hayes, S. C., Pankey, J., & Gregg, J. (2002). Acceptance and commitment therapy. Anxiety disorders: A practitioner’s guide to comparative treatments, 110–136.
Hedman, E., Andersson, G., Ljótsson, B., Andersson, E., Rück, C., Mörtberg, E., & Lindefors, N. (2011). Internet-based cognitive behavior therapy vs. cognitive behavioral group therapy for social anxiety disorder: A randomized controlled non-inferiority trial. PloS ONE , 6 (3), e18001.
Hong, Y. J., Kim, I. J., Ahn, S. C., & Kim, H. G. (2010). Mobile health monitoring system based on activity recognition using accelerometer. Simulation Modelling Practice and Theory , 18 (4), 446–455.
Hong, Q. N., Pluye, P., Fàbregues, S., Bartlett, G., Boardman, F., Cargo, M., & Vedel, I. (2018). Mixed methods appraisal tool (MMAT), version 2018. Registration of Copyright , 1148552(10).
Howarth, A., Quesada, J., Silva, J., Judycki, S., & Mills, P. R. (2018). The impact of digital health interventions on health-related outcomes in the workplace: A systematic review. Digital Health , 4 , 2055207618770861.
Huberty, J. L., Espel-Huynh, H. M., Neher, T. L., & Puzia, M. E. (2022). Testing the pragmatic effectiveness of a consumer-based Mindfulness Mobile App in the Workplace: Randomized Controlled Trial. JMIR mHealth and uHealth , 10(9), e38903.
Hwang, W. J., & Jo, H. H. (2019). Evaluation of the effectiveness of mobile app-based stress-management program: A randomized controlled trial. International Journal of Environmental Research and Public Health , 16 (21), 4270.
Hwang, H., Kim, S. M., Netterstrøm, B., & Han, D. H. (2022). The efficacy of a smartphone-based app on stress reduction: Randomized controlled trial. Journal of Medical Internet Research , 24 (2), e28703.
International Labour Organization (2016). Workplace stress: A collective challenge . Geneva.
Jamal, M. (1990). Relationship of job stress and type-A behavior to employees’ job satisfaction, organizational commitment, psychosomatic health problems, and turnover motivation. Human Relations , 43 , 727–738. https://doi.org/10.1177/001872679004300802
Jukic, T., Ihan, A., Strojnik, V., Stubljar, D., & Starc, A. (2020). The effect of active occupational stress management on psychosocial and physiological well-being: A pilot study. BMC Medical Informatics and Decision Making , 20 (1), 1–8.
Kabat-Zinn, J. (2003). Mindfulness-based interventions in context: past, present, and future. https://doi.org/10.1093/clipsy.bpg016
Kabat-Zinn, J., & Hanh, T. N. (2009). Full catastrophe living: Using the wisdom of your body and mind to face stress, pain, and illness . Delta.
Kampmeijer, R., Pavlova, M., Tambor, M., Golinowska, S., & Groot, W. (2016). The use of e-health and m-health tools in health promotion and primary prevention among older adults: A systematic literature review. BMC Health Services Research , 16 (5), 467–479.
Keng, S. L., Chin, J. W. E., Mammadova, M., & Teo, I. (2022). Effects of mobile app-based mindfulness practice on healthcare workers: A randomized active controlled trial. Mindfulness , 13 (11), 2691–2704.
Khakurel, J., Melkas, H., & Porras, J. (2018). Tapping into the wearable device revolution in the work environment: A systematic review. Information Technology & People , 31 (3), 791–818.
Kritzler, M., Bäckman, M., Tenfält, A., & Michahelles, F. (2015, November). Wearable technology as a solution for workplace safety. In Proceedings of the 14th International Conference on Mobile and Ubiquitous Multimedia (pp. 213–217).
Kroenke, K., Spitzer, R. L., & Williams, J. B. (2001). The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine , 16 (9), 606–613.
Kuziemsky, C. E., & O’Sullivan, T. L. (2015). A model for common ground development to support collaborative health communities. Social Science & Medicine , 128 , 231–238.
Larsen, L. H., Lauritzen, M. H., Sinkjaer, M., & Kjaer, T. W. (2021). A multi-component intervention to affect physical activity, sleep length and stress levels in office workers. Smart Health , 22 , 100219.
Leka, S., & Jain, A. (2010). Health Impact of Psychosocial hazards at Work: An overview . World Health Organization.
Liesa-Orús, M., Latorre-Cosculluela, C., Vázquez-Toledo, S., & Sierra-Sánchez, V. (2020). The technological challenge facing higher education professors: Perceptions of ICT tools for developing 21st century skills. Sustainability , 12 (13), 5339.
Lindeman, D. (2011). mHealth technologies: applications to benefit older adults. Oakland, CA: Center for Technology and Aging; http://www.techandaging.org/mHealth_Position_Paper_Discussion_Draft.pdf Accessed 10 July 2023.
Lipschitz, J. M., Pike, C. K., Hogan, T. P., et al. (2023). The Engagement Problem: A review of Engagement with Digital Mental Health Interventions and recommendations for a path Forward. Current Treatment Options in Psychiatry , 10 , 119–135. https://doi.org/10.1007/s40501-023-00297-3
Liu, X., Vega, K., Maes, P., & Paradiso, J. A. (2016, February). Wearability factors for skin interfaces. In Proceedings of the 7th Augmented Human International Conference 2016 (pp. 1–8).
Loeppke, R. R., Hohn, T., Baase, C., Bunn, W. B., Burton, W. N., Eisenberg, B. S., Ennis, T., Fabius, R., Hawkins, R. J., Hudson, T. W., Hymel, P. A., Konicki, D., Larson, P., McLellan, R. K., Roberts, M. A., Usrey, C., Wallace, J. A., Yarborough, C. M., & Siuba, J. (2015). Integrating health and safety in the workplace: How closely aligning health and safety strategies can yield measurable benefits. Journal of Occupational and Environmental Medicine/American College of Occupational and Environmental Medicine , 57 (5), 585–597.
Lu, Y., Remond, J., Bunting, M., Ilies, R., Tripathi, N., & Narayanan, J. (2021). An app-based workplace mindfulness intervention, and its effects over time. Frontiers in Psychology , 12 , 615137.
Lundberg, U. (2005). Stress hormones in health and illness: The roles of work and gender. Psychoneuroendocrinology , 30 (10), 1017–1021.
Lupton, D. (2013). Digitized health promotion: personal responsibility for health in the web 2.0 era, Working Paper No. 5, Sydney Health & Society Group, Sydney.
Lupton, D. (2014). Self-tracking cultures: towards a sociology of personal informatics, OZCHI 2014: The 26th Australian Computer-Human Interaction Conference: Designing Futures, the Future of Design, pp. 1–10.
Lupton, D. (2015). Health Promotion in the Digital era: A critical commentary . Health Promotion International.
Majumder, S., Mondal, T., & Deen, M. (2017). Wearable Sensors for Remote Health Monitoring. Sensors , 17 (12), 130. MDPI AG.
Marcengo, A., & Rapp, A. (2014). Visualization of human behavior data: The quantified self. Innovative approaches of data visualization and visual analytics (pp. 236–265). IGI Global.
Chapter Google Scholar
Matsumoto, A., Kamita, T., Tawaratsumida, Y., Nakamura, A., Fukuchimoto, H., Mitamura, Y., & Inoue, T. (2021). Combined use of virtual reality and a Chatbot reduces emotional stress more than using them separately. JUCS: Journal of Universal Computer Science , 27 (12), 1371–1389.
McEvoy, P. M., Watson, H., Watkins, E. R., & Nathan, P. (2013). The relationship between worry, rumination, and comorbidity: Evidence for repetitive negative thinking as a transdiagnostic construct. Journal of Affective Disorders , 151 (1), 313–320.
McEwen, B. S. (1998). Stress, adaptation, and disease: Allostasis and allostatic load. Annals of the New York Academy of Sciences , 840 (1), 33–44.
McFarlin, S. K., & Fals-Stewart, W. (2002). Workplace absenteeism and alcohol use: A sequential analysis. Psychology of Addictive Behaviors , 16 (1), 17–21.
Miller, G. (2012). The smartphone psychology manifesto. Perspectives on Psychological Science , 7 (3), 221–237.
Moher, D., Liberati, A., Tetzlaff, J., Altman, D. G., & Group*, P. R. I. S. M. A., T (2009). Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Annals of Internal Medicine , 151 (4), 264–269.
Monfries, N., Sandhu, N., & Millar, K. (2023). A smartphone app to reduce burnout in the Emergency Department: A pilot randomized controlled trial. Workplace Health & Safety , 71 (4), 181–187.
Muaremi, A., Arnrich, B., & Tröster, G. (2013). Towards measuring stress with smartphones and wearable devices during workday and sleep. BioNanoScience , 3 , 172–183.
Munakata, T. (2006). SAT therapy . KANEKOSHOBO.
Mundt, J. C., Marks, I. M., Shear, M. K., & Greist, J. M. (2002). The work and Social Adjustment Scale: A simple measure of impairment in functioning. The British Journal of Psychiatry , 180 (5), 461–464.
National Institute for Occupational Safety and Health (NIOSH) (1999). Stress at Work. Centers for Disease Control and Prevention. https://www.cdc.gov/niosh/docs/99-101/ Accessed 8 July 2024.
Nelis, D., Kotsou, I., Quoidbach, J., Hansenne, M., Weytens, F., Dupuis, P., & Mikolajczak, M. (2011). Increasing emotional competence improves psychological and physical well-being, social relationships, and employability. Emotion , 11 (2), 354.
Nemati, E., Deen, M. J., & Mondal, T. (2012). A wireless wearable ECG sensor for long-term applications. IEEE Communications Magazine , 50 (1), 36–43.
Ong, A. D., Bergeman, C. S., Bisconti, T. L., & Wallace, K. A. (2006). Psychological resilience, positive emotions, and successful adaptation to stress in later life. Journal of Personality and Social Psychology , 91 (4), 730–749.
Ouzzani, M., Hammady, H., Fedorowicz, Z., & Elmagarmid, A. (2016). Rayyan—a web and mobile app for systematic reviews. Systematic Reviews , 5 , 1–10.
Paganin, G., & Simbula, S. (2020). Smartphone-based interventions for employees’ well-being promotion: A systematic review. Electronic Journal of Applied Statistical Analysis , 13 (3), 682–712.
Pantelopoulos, A., & Bourbakis, N. G. (2009). A survey on wearable sensor-based systems for health monitoring and prognosis. IEEE Transactions on Systems Man and Cybernetics Part C (Applications and Reviews) , 40 (1), 1–12.
Pascucci, P. (2021). Il Testo Unico sulla salute e Sicurezza Sul lavoro: Spunti di riflessione (a fronte dei cambiamenti in atto) e proposte di modifica. Bilancio E prospettive di una ricerca. Il Sistema Prevenzionistico E Le tutele assicurative alla prova della IV Rivoluzione industriale (Vol. 1, pp. 499–518). ADAPT University.
Patel, V., Chesmore, A., Legner, C. M., & Pandey, S. (2022). Trends in workplace wearable technologies and connected-worker solutions for next‐generation occupational safety, health, and productivity. Advanced Intelligent Systems , 4 (1), 2100099.
Peltzer, K., Shisana, O., Zuma, K., Van Wyk, B., & Zungu-Dirwayi, N. (2009). Job stress, job satisfaction and stress-related illnesses among South African educators. Stress and Health , 25 , 247–257.
Philippe, T. J., Sikder, N., Jackson, A., Koblanski, M. E., Liow, E., & Pilarinos, A. & Vasarhelyi K. (2022). Digital Health Interventions for Delivery of Mental Health Care: Systematic and comprehensive Meta-review. JMIR Mental Health , 9 (5):e35159. https://doi.org/10.2196/35159
Podsakoff, N. P., LePine, J. A., & LePine, M. A. (2007). Differential challenge stressor-hindrance stressor relationships with job attitudes, turnover intentions, turnover, and withdrawal behavior: A meta-analysis. Journal of Applied Psychology , 92 (2), 438.
Rich, R. M., Ogden, J., & Morison, L. (2021). A randomized controlled trial of an app-delivered mindfulness program among university employees: Effects on stress and work-related outcomes. International Journal of Workplace Health Management , 14 (2), 201–216.
Riper, H., Blankers, M., Hadiwijaya, H., Cunningham, J., Clarke, S., Wiers, R., & Cuijpers, P. (2014). Effectiveness of guided and unguided low-intensity internet interventions for adult alcohol misuse: A meta-analysis. PloS ONE , 9 (6), e99912.
Rowland, S. P., Fitzgerald, J. E., Holme, T., Powell, J., & McGregor, A. (2020). What is the clinical value of mHealth for patients? NPJ Digital Medicine , 3 (1), 4.
Rudics, E., Nagy, Á., Dombi, J., Hompoth, E. A., Szabó, Z., Horváth, R., & Szendi, I. (2023). Photoplethysmograph based biofeedback for stress reduction under real-life conditions in Healthcare Frontline. Applied Sciences , 13 (2), 835.
Sanatkar, S., Counson, I., Mackinnon, A., Bartholomew, A., Glozier, N., & Harvey, S. (2022). Preliminary Investigation of Shift, a Novel Smartphone App to Support Junior Doctors’ Mental Health and Well-being: Examination of Symptom Progression, Usability, and Acceptability After 1 Month of Use. Journal of Medical Internet Research , 24(9), e38497.
Sauter, S. L., Brightwell, W. S., Colligan, M. J., Hurrell, J. J., Katz, T. M., LeGrande, D. E., & Peters, R. H. (2002). The changing organization of work and the safety and health of working people. Cincinnati: National Institute for Occupational Safety and Health .
Schaufeli, W. B. (2017). Applying the job demands-resources model. Organizational Dynamics , 2 (46), 120–132.
Schulte-Frankenfeld, P. M., & Trautwein, F. M. (2022). App‐based mindfulness meditation reduces perceived stress and improves self‐regulation in working university students: A randomized controlled trial. Applied Psychology: Health and Well-Being , 14 (4), 1151–1171.
PubMed Google Scholar
Seligman, M. E. (2002). Authentic happiness: Using the new positive psychology to realize your potential for lasting fulfillment . Simon and Schuster.
Seligman, M. E. (2002a). Positive psychology, positive prevention, and positive therapy. Handbook of positive psychology, 2 (2002), 3–12.
Seligman, M. (2018). PERMA and the building blocks of well-being. The Journal of Positive Psychology , 13 (4), 333–335.
Seneviratne, S., Hu, Y., Nguyen, T., Lan, G., Khalifa, S., Thilakarathna, K., & Seneviratne, A. (2017). A survey of wearable devices and challenges. IEEE Communications Surveys & Tutorials , 19 (4), 2573–2620.
Signore, F., Catalano, A., De Carlo, E., Madaro, A., & Ingusci, E. (2019). The role of employability in students during academic experience: A preliminary study through PLS-PM technique. Electronic Journal of Applied Statistical Analysis , 12 (4), 720–747.
Skoumpopoulou, D., Wong, A., Ng, P., & Lo, M. (2018). Factors that affect the acceptance of new technologies in the workplace: A cross case analysis between two universities. International Journal of Education and Development Using ICT , 14 (3), 209.
Smith, E. N., Santoro, E., Moraveji, N., Susi, M., & Crum, A. J. (2020). Integrating wearables in stress management interventions: Promising evidence from a randomized trial. International Journal of Stress Management , 27 (2), 172.
Sole, M., Musu, C., Boi, F., Giusto, D., & Popescu, V. (2013, July). Control system for workplace safety in a cargo terminal. In 2013 9th International Wireless Communications and Mobile Computing Conference (IWCMC) (pp. 1035–1039). IEEE.
Spagnolli, A., Guardigli, E., Orso, V., Varotto, A., & Gamberini, L. (2014). Measuring user acceptance of wearable symbiotic devices: validation study across application scenarios. In Symbiotic Interaction: Third International Workshop, Symbiotic 2014, Helsinki, Finland, October 30–31, 2014, Proceedings 3 (pp. 87–98). Springer International Publishing.
Spitzer, R. L., Kroenke, K., Williams, J. B., & Löwe, B. (2006). A brief measure for assessing generalized anxiety disorder: The GAD-7. Archives of Internal Medicine , 166 (10), 1092–1097.
Steptoe, A., Deaton, A., & Stone, A. A. (2015). Subjective wellbeing, health, and ageing. The Lancet , 385 (9968), 640–648.
Stratton, E., Lampit, A., Choi, I., Calvo, R. A., Harvey, S. B., & Glozier, N. (2017). Effectiveness of eHealth interventions for reducing mental health conditions in employees: A systematic review and meta-analysis. PloS ONE , 12 (12), e0189904.
Suzuki, T., Tanaka, H., Minami, S., Yamada, H., & Miyata, T. (2013, March). Wearable wireless vital monitoring technology for smart health care. In 2013 7th International Symposium on Medical Information and Communication Technology (ISMICT) (pp. 1–4). IEEE.
Tang, C. S., Au, W., Schwarzer, R., & Schmitz, G. (2001). Mental Health outcomes of Job stress among Chinese teachers: Role of stress resource factors and burnout. Journal of Organizational Behavior , 22 (8), 887–901. http://www.jstor.org/stable/3649577
Taylor, H., Cavanagh, K., Field, A. P., & Strauss, C. (2022). Health Care Workers’ Need for Headspace: Findings From a Multisite Definitive Randomized Controlled Trial of an Unguided Digital Mindfulness-Based Self-help App to Reduce Healthcare Worker Stress. JMIR mHealth and uHealth , 10 (8), e31744.
Tindale, L. C., Chiu, D., Minielly, N., Hrincu, V., Talhouk, A., & Illes, J. (2022). Wearable biosensors in the Workplace: Perceptions and perspectives. Frontiers in Digital Health , 4 , 800367.
Van Aert, R. C., Wicherts, J. M., & Van Assen, M. A. (2019). Publication bias examined in meta-analyses from psychology and medicine: A meta-meta-analysis. PloS ONE , 14 (4), e0215052.
Van Tulder, M., Furlan, A., Bombardier, C., Bouter, L., & Editorial Board of the Cochrane Collaboration Back Review Group. (2003). Updated method guidelines for systematic reviews in the Cochrane Collaboration Back Review Group. Spine , 28 (12), 1290–1299.
Vonderlin, R., Biermann, M., Bohus, M., & Lyssenko, L. (2020). Mindfulness-based programs in the workplace: A meta-analysis of randomized controlled trials. Mindfulness , 11 , 1579–1598.
Wang, B., Liu, Y., Qian, J., & Parker, S. K. (2021). Achieving Effective Remote Working during the COVID-19 pandemic: A Work Design Perspective. Applied Psychology , 70 , 16–59.
Warr, P. (2007). Work, happiness, and unhappiness (1st ed.). Psychology.
Weber, S., Lorenz, C., & Hemmings, N. (2019). Improving stress and positive mental health at work via an app-based intervention: A large-scale multi-center randomized control trial. Frontiers in Psychology , 10 , 2745.
Wilson, C. J., Deane, F. P., Ciarrochi, J. V., & Rickwood, D. (2005). Measuring help seeking intentions: properties of the general help seeking questionnaire.
World Health Organization (WHO) (July 2024). Regional Office for the Eastern Mediterranean. (2002). Occupational health: a manual for primary health care workers. https://iris.who.int/handle/10665/116326 Accessed 10.
Wright, T. A., Cropanzano, R., & Bonett, D. G. (2007). The moderating role of employee positive well being on the relation between job satisfaction and job performance. Journal of Occupational Health Psychology , 12 (2), 93.
Xu, H., Eley, R., Kynoch, K., & Tuckett, A. (2022). Effects of mobile mindfulness on emergency department work stress: A randomized controlled trial. Emergency Medicine Australasia , 34 (2), 176–185.
Xue, Y. (2019). A review on intelligent wearables: Uses and risks. Human Behavior and Emerging Technologies , 1 (4), 287–294.
Xue, M., Liang, R. H., Hu, J., Yu, B., & Feijs, L. (2022, April). Understanding How Group Workers Reflect on Organizational Stress with a Shared, Anonymous Heart Rate Variability Data Visualization. In CHI Conference on Human Factors in Computing Systems Extended Abstracts (pp. 1–7).
Yeh, Y. C., Lin, B. Y. J., Lin, W. H., et al. (2010). Job stress: Its relationship to hospital pharmacists’ insomnia and work outcomes. International Journal of Behavioral Medicine , 17 , 143–153.
Yoon, S. I., Lee, S. I., Suh, H. W., Chung, S. Y., & Kim, J. W. (2022). Effects of mobile mindfulness training on mental health of employees: A CONSORT-compliant pilot randomized controlled trial. Medicine , 101 (35), e30260.
You, C. W., Yuan, C. W., Bi, N., Hung, M. W., Huang, P. C., & Wang, H. C. (2021, May). Go gig or go home: enabling social sensing to share personal data with intimate partner for the health and well-being of long-hour workers. In Proceedings of the 2021 CHI Conference on Human Factors in Computing Systems (pp. 1–16). Zenonos, A., Khan, A., Kalogridis, G., Vatsikas, S., Lewis, T., & Sooriyabandara, M. (2016, March). HealthyOffice: Mood recognition at work using smartphones and wearable sensors. In 2016 IEEE International Conference on Pervasive Computing and Communication Workshops (PerCom Workshops) (pp. 1–6). IEEE.
Download references
This systematic review was realized within the MUSA – Multilayered Urban Sustainability Action – project, funded by the European Union – NextGenerationEU, under the National Recovery and Resilience Plan (NRRP) Mission 4 Component 2 Investment Line 1.5: Strengthening of research structures and creation of R&D “innovation ecosystems”, set up of “territorial leaders in R&D”.
Author information
Authors and affiliations.
Department of Psychology, University of Milano-Bicocca, Piazza dell’Ateneo Nuovo, 1 - 20126, Milan, Italy
Margherita Herold, Silvia Simbula & Marcello Gallucci
Bicocca Center for Applied Psychology, University of Milano-Bicocca, Piazza dell’Ateneo Nuovo, 1 - 20126, Milan, Italy
Margherita Herold & Silvia Simbula
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Margherita Herold .
Ethics declarations
This Systematic Review has been realized within the MUSA – Multilayered Urban Sustainability Action – project, funded by the European Union – NextGenerationEU, under the National Recovery and Resilience Plan (NRRP) Mission 4 Component 2 Investment Line 1.5: Strengthening of research structures and creation of R&D “innovation ecosystems”, set up of“territorial leaders in R&D”.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Herold, M., Simbula, S. & Gallucci, M. Can smartphone applications and wearable technologies improve workplace well-being and help manage stress? A systematic review. Curr Psychol (2024). https://doi.org/10.1007/s12144-024-06534-z
Download citation
Accepted : 06 August 2024
Published : 24 August 2024
DOI : https://doi.org/10.1007/s12144-024-06534-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Work-related stress
- Workers well-being
- Smartphone applications
- Wearable technologies
- Systematic review
- Find a journal
- Publish with us
- Track your research
- DOI: 10.1108/jpmh-04-2024-0055
- Corpus ID: 272230078
Defining mental health literacy: a systematic literature review and educational inspiration
- Shengnan Zeng , Richard Bailey , +1 author Xiaohui Chen
- Published in Journal of Public Mental… 2 September 2024
- Psychology, Education
56 References
A systematic review of the limitations and associated opportunities of chatgpt, deductive qualitative analysis: evaluating, expanding, and refining theory, conceptualising and measuring positive mental health literacy: a systematic literature review, mental health education integration into the school curriculum needs to be implemented, review: school-based mental health literacy interventions to promote help-seeking - a systematic review., public opinion towards mental health (the case of the vologda region), quantifying the global burden of mental disorders and their economic value, mental health literacy: it is now time to put knowledge into practice, clarifying the concept of mental health literacy: protocol for a scoping review, positive mental health literacy: a concept analysis, related papers.
Showing 1 through 3 of 0 Related Papers

Friday essay: Bad therapy or cruel world? How the youth mental health crisis has been sucked into the culture wars
Professor of Psychology, The University of Melbourne
Disclosure statement
Nick Haslam receives funding from the Australian Research Council.
University of Melbourne provides funding as a founding partner of The Conversation AU.
View all partners
Rates of mental ill health among young people are on the rise. Between the years 2020 and 2022, 39% of Australians aged 16 to 24 had a mental disorder in the previous year , compared to 26% in that age range in 2007, and 27% of those aged 18–24 in 1997.
The recent Lancet Psychiatry commission on youth mental health documents equally steep increases in mental illness in the United States, UK and Denmark. Governments, mental health services, educational institutions and parents are struggling to respond. But what is behind these trends?
Two accounts seem to be emerging. According to one, which I’ll call the “cruel world” narrative, young people are distressed because the world is in bad shape and getting worse.
Facing climate emergency, unaffordable housing, precarious employment, rising inequality and other dire mega-trends, they are canaries in a societal coalmine. By this account, the mental health crisis is the direct result of systemic adversity.
The alternative, which I’ll call the “cultural trend” narrative, is a little less bleak. Young people are experiencing more mental illness not primarily because the world is grim and getting grimmer, but because cultural shifts have shaped how they perceive and inhabit it.
This narrative suggests a culture preoccupied with harm creates vulnerability and leads people to view life problems through a psychiatric lens. Adversity and social dislocation undoubtedly contribute to young people’s distress, but the way therapeutic culture frames their suffering makes it worse.
The two narratives offer different prescriptions.
From the “cruel world” perspective, the ultimate causes of the mental health crisis are the basic structures of our society, economy and ecology. Only systemic, macro-level changes can arrest them.
For proponents of the “cultural trend” narrative, the focus of intervention is more micro. We should challenge the social practices and technologies that create vulnerability and undermine mental health.

As a social psychologist, I take it as self-evident that adverse social environments play a leading role in the creation of mental ill health: that we can’t isolate human misery from its broader context. However, I’m equally certain that culture plays a crucial part.
A range of cultural changes that could plausibly undermine mental health are well underway: increased immersion in the digital world, rising political polarisation and preoccupation with risk and harm, among others. Separating them from the tangled skein of factors that contribute to the youth mental health crisis is a matter of urgency.
Abigail Shrier’s new book Bad Therapy , a forceful exposition of the “cultural trend” narrative, provides a golden opportunity to explore some of them.
Youth mental health and the culture wars
Journalist and cultural critic Soraya Chemaly’s recent book The Resilience Myth exemplifies the first narrative. Young people are distressed “because the world is distressing, and adults have failed them”. Their sensitivity and emotional honesty place them at higher risk of distress than their elders, and the ubiquity of trauma, oppression and existential climate threat tip that risk into illness.
Chemaly’s solutions lean towards the revolutionary. Her targets include individualism, rigid gender ideologies, capitalism and white supremacy.
Social psychologist Jonathan Haidt’s The Anxious Generation presents a version of the second narrative. Haidt does not deny the magnitude of the challenges young people face. However, he questions whether their rising rates of mental ill health directly follow increases in adversity.
This inflection point in the trajectory of young people’s mental ill health appears to have occurred in the early 2010s. However, many of the systemic trends now held responsible for the crisis – like climate change and rising income inequality – have been building over a much longer period, when rates of ill health were relatively stable. By implication, the precipitating causes must be more specific, recent developments.
Haidt identifies two such changes: the advent of smartphones and “safetyism”. His focus on smartphones has been widely reported . But his equally important emphasis on the cultural preoccupation with protecting us from harm has received less attention.

Haidt argues that parental and institutional over-protection hampers the development of young people’s resilience and autonomy. Citing the idea of “anti-fragility” he proposes that risk, challenge and failure are required to build strength.
By now, it should be obvious that the youth mental health crisis has become politicised, sucked into the vortex of the culture wars.
The crisis can be attributed either to an uncaring system that oppresses the most vulnerable, or to emerging social trends that do young minds no favours. It can be addressed either by progressive social change, such as economic redistribution and environmental protection, or by winding back some damaging cultural developments, such as promoting unsupervised play for children and restricting access to smartphones in schools .
Blaming ‘bad therapy’
Whereas Haidt spends much of his book on the damage done by young people’s immersion in the digital world, in Bad Therapy, Shrier castigates mental health experts for contributing to the crisis they claim to be addressing.

Shrier is a controversial figure. Her previous book Irreversible Damage drew protests and bans for critiquing youth gender medicine and arguing that social contagion plays a role in the rise of girls seeking gender transition.
The former lawyer and Wall Street Journal columnist, who has not previously written at length on mental health, is just as fierce in prosecuting the case against the growing influence of mental health expertise.
Bad Therapy begins by arguing that the rise in mental ill health among young people is not merely a response to deepening life challenges. Instead, Shrier writes, it is driven by destructive cultural shifts and misguided experts. She suggests many people who are experiencing ordinary problems in living have been led to believe their unhappiness is psychiatric in nature.
Shrier is quick to clarify that distress often is genuinely severe. There are “two distinct groups of young people”, she argues: those experiencing “profound mental illness” and “the worriers; the fearful; the lonely, lost, and sad”.
This second group is Shrier’s battleground. These “worriers” have fallen victim to shifts in education and parenting, and to the expansionism of the mental health field. On this point, she doesn’t mince her words. “No industry refuses the prospect of exponential growth,” she writes, and “the mental health industry is minting patients faster than it can cure them.” As a result, “we rush to remedy a misdiagnosed condition with the wrong sort of cure”.
Shrier challenges the common view that mental health interventions – therapy for short – are invariably beneficial. She reviews evidence suggesting therapy is less helpful than it is touted to be, and that it can sometimes be actively harmful. For instance, “psychological debriefing” immediately after exposure to traumas can interfere with recovery .
Mental health treatment can undermine recovery, she suggests, by “hijack[ing] our normal processes of resilience” and creating dependency on professionals. It can crystallise illness by applying diagnostic labels too liberally.
Diagnoses may bring relief to anxious and desperate parents, but they can also affect how their children perceive themselves and are perceived by others. Much like therapeutic staples such as trauma and chemical imbalance , diagnostic terms can convey the view that young people are fundamentally damaged and have little control over their predicaments.
Many of these critiques of therapy chime with familiar attacks on medicalisation . But Shrier also advances some newer criticisms. Mental health treatment can induce rumination and a passive focus on feelings: common features of anxiety and depression. “Bad therapy encourages hyperfocus on one’s emotional states, which in turn makes symptoms worse.”
Therapy can also affirm young people’s worries and encourage public sharing of distress in ways that can entrench unhelpful patterns. “A dose of repression,” Shrier counters, “appears to be a fairly useful psychological tool for getting on with life.”
Mental health workers overlook the possibility that talk therapy can have these adverse consequences, Shrier argues – although it is no less plausible that some psychological treatments may do harm than that some medications can have adverse side effects. Without questioning therapists’ desire to help, she takes the hardheaded view that they have incentives not to acknowledge the harm they may be causing.
Should teachers be delivering therapy?
The clear implication of Shrier’s argument is that we should challenge, rather than expand, therapeutic approaches to young people’s mental health. Instead, she finds that American schools are riddled with bad therapy, often under the banner of “social-emotional learning”.
Shrier maintains that social-emotional learning licenses psychologically untrained teachers to work in a therapeutic mode. It encourages excessive self-focus, demands emotional disclosure and can expose children to dual relationships, all out of view of their parents.
Social-emotional learning and related elements of therapeutic schooling don’t just encourage unhelpful inwardness, she argues. She contends they also use questionable teaching methods and draw time and energy away from academic learning.

Of one effort to smuggle emotional learning into a maths class, Shrier writes: “I began to wonder whether this wasn’t some sort of ploy by the Chinese Communist Party to obliterate American mathematical competence.” She concludes that
social-emotional learning turns out to be a lot like the Holy Roman Empire. Neither social, nor good for emotional health, nor something that can be learned.
Schools’ therapeutic missions also undermine how they educate disadvantaged students. Shrier contends that some “trauma-informed” practice prejudges students who have experienced hardship as fragile and in need of blanket mental health interventions, while lowering expectations for their behaviour and academic achievement. Meanwhile, classroom chaos is created by excessive accommodation of disruptive students.
Shrier takes aim at the outsized role “trauma” plays in currently popular accounts of mental ill health. She reserves some of her sharpest criticism for psychiatrist Bessel van der Kolk , whose bestselling book, The Body Keeps the Score, places trauma front and centre in mental ill health, and physician Gabriel Maté , who claims trauma contributes to everything from cancer to ADHD.
Seeing childhood trauma as the buried root of most adult mental health problems conflicts with copious evidence that resilience is the normal response to adversity – and that trauma memories tend to be recalled accurately, rather than locked voiceless in the body. Shrier maintains that the concept of trauma has become trivialised through over-use. She chastises experts for characterising problems ranging from anger outbursts to procrastination as trauma responses.
In the school environment, the consequences of elevating trauma are troubling:
under the banner of “whole child” education and “trauma-informed” care, educators greet every child with the emotional analogue of a gurney, all but begging kids to hop in. They never wait to see who might be injured because every child is encouraged to see herself as overtaxed and worn out. They encourage every child, constantly, to think about herself and her struggles.
Against ‘gentle’ parenting and ‘overmanaged’ kids
Shrier condemns schools for usurping parental authority, but argues that contemporary parenting also subverts itself.
“Gentle” styles of child-rearing end up creating anxious, unresilient children whose demands are endlessly accommodated and whose dependency is reinforced. A strange combination of permissiveness and over-involvement makes for exhausted parents who are unwilling to exercise adult authority or to impose consequences on behaviour, she argues.
Liberal American parents may look askance at earlier styles of parenting, but by placing emotional wellness front and centre in their relationships with their children, they are making their task harder and more thankless.
As Shrier observes:
forty-year-old parents – accomplished, brilliant, and blessed with a spouse – treat the raising of kids like a calculus problem that was put to them in the dead of night: Get it right or I pull this trigger .
Ultimately, the failures of therapeutic parenting are another strike against the mental health experts who advocated for it. Shrier urges parents to cut themselves loose from the advice of parenting sages, for the good of their children: “love means occasionally telling an expert to get lost”.

Concretely, parents should step back, stop compulsively monitoring and over-praising their children, reduce scheduled activities, enforce consequences and encourage independent behaviour. She writes: “if you could do something at their age, let them give it a whirl”.
A parent’s goal should be to set their children free from an “overmanaged, veal-calf life” and ensure they experience “all of the pains of adulthood, in smaller doses, so that they build up immunity to the poison of heartache and loss”.
Not all therapy is bad therapy
Bad Therapy is an unashamedly polemical book. Shrier has strong views on what is wrong with the culture of mental health in the US – and takes these supposed failings as examples of broader progressive trends she opposes.
The mental health crisis troubles her not only for its human costs, but because it erodes key conservative values: self-reliance, strength, parental authority and freedom from institutional compulsion.
Shrier’s rhetoric is sharp-elbowed, with a memorable turn of phrase. Some villains are identified and savaged, though the criticised cabal of mental health experts is often a faceless mass. The book is studded with revealing case studies and she interviews many leading scientists, like Paul Bloom, author of Against Empathy , memory expert Elizabeth Loftus , leading trauma psychologist Richard McNally , and generational difference researcher Jean Twenge .
Though she presents herself as defending science against ideology, at times Shrier’s claims run ahead of the data. There is little evidence that mental health interventions are creating ill health on a large scale, for example, or that increases in self-diagnosis among young people account for increases in their levels of distress.

Some schools may implement socio-emotional learning in problematic ways. But studies typically find that they benefit academic achievement . And though there is evidence that today’s young adults are reaching some developmental milestones later than earlier generations, there is little direct evidence that gentle parenting is responsible for the delays.
Shrier tends to present the mental health world as a monolith. But anyone working in it knows it to be criss-crossed with divisions: between researchers and practitioners, consumers and professionals, medical and non-medical workers, and numerous disciplines and therapeutic tribes.
The idea that this Babel of voices is united in a process of crisis creation is hard to credit. Not all therapy is bad therapy. Indeed, many of the positions Shrier espouses – for facing challenges head on and experiencing the consequences of our behaviour, and against safetyism, over-medication and the therapeutic excavation of our childhoods – are gospel for mainstream cognitive behaviour therapists.
Correcting concerning trends
Even so, for all its exaggerations and simplifications, Bad Therapy is a timely corrective to some real and concerning trends. It is increasingly clear that over-diagnosis of mental illness is common, especially among young people, and that diagnostic labelling can have adverse implications .
It now seems likely that campaigns to boost mental health awareness sometimes backfire and pathologise ordinary unhappiness. School-based prevention initiatives are sometimes ineffective and can even reduce wellbeing.
Most of all, it is becoming obvious that although there is a high unmet need for treatment, simply expanding the current mental health system – training more therapists, funding more sessions and services, further boosting awareness of mental health, embedding a therapeutic sensibility in more of our institutions – cannot be relied on to substantially reduce mental ill health.
Research on the so-called “treatment-prevalence paradox” demonstrates that large increases in service provision have failed to reduce rates of mental illness. Current treatment practices have only modest efficacy in real-world settings. Reasons likely include the complexity and recurring nature of many mental health problems, and the low quality implementation and short-lived benefit of many treatments.
Some treatments also clearly do more harm than good, for some patients. A recent evaluation of Australia’s Better Access program, which gives Medicare rebates to help people access mental health care, found that patients who sought help for relatively mild distress were three times more likely to deteriorate than to improve (patients in more severe distress typically improved).
In this context, Shrier has some grounds to be sceptical that doing more of the same will turn around the mental health crisis. There is no question that more needs to be done – but believing that the solution is to scale up current practice seems, as Samuel Johnson said of a second marriage, a triumph of hope over experience.
Shrier addresses her concluding chapters to parents, urging them to reclaim the confidence that they know what’s right for their child. The trouble is, parents rarely know to which of Shrier’s “two distinct groups of young people” their child belongs.
How could they know? No bright line separates the supposed victims of therapy culture from the profoundly ill. Faced with a loved one’s distress, what can parents do but seek the forms of help that are currently available?
Our young people will continue to be funnelled toward mental health treatment in alarming numbers. We can only hope it will become more effective and less necessary.
- Overdiagnosis
- Gentle parenting
- Friday essay
- Youth mental health crisis

Chief Financial Officer

Director of STEM

Community member - Training Delivery and Development Committee (Volunteer part-time)

Chief Executive Officer

Head of Evidence to Action
Technology in Mental Health: Creating New Knowledge and Inventing the Future of Services
Information & authors, metrics & citations, view options, revisiting the parameters of research and practice, inventing the future of mental health care, a call for creativity in research, practice, and policy, information, published in.
Cover: Love of Winter , by George Wesley Bellows, 1914. Oil on canvas. Friends of American Art Collection (1914.1018), the Art Institute of Chicago. Photography ©The Art Institute of Chicago, www.artic.edu .
- Computer technology
- Research/service delivery
- Smartphones
- Digital health
- Telemedicine
Competing Interests
Export citations.
If you have the appropriate software installed, you can download article citation data to the citation manager of your choice. Simply select your manager software from the list below and click Download. For more information or tips please see 'Downloading to a citation manager' in the Help menu .
| Format | |
|---|---|
| Citation style | |
| Style | |
To download the citation to this article, select your reference manager software.
There are no citations for this item
View options
Login options.
Already a subscriber? Access your subscription through your login credentials or your institution for full access to this article.
Not a subscriber?
Subscribe Now / Learn More
PsychiatryOnline subscription options offer access to the DSM-5-TR ® library, books, journals, CME, and patient resources. This all-in-one virtual library provides psychiatrists and mental health professionals with key resources for diagnosis, treatment, research, and professional development.
Need more help? PsychiatryOnline Customer Service may be reached by emailing [email protected] or by calling 800-368-5777 (in the U.S.) or 703-907-7322 (outside the U.S.).
Share article link
Copying failed.
PREVIOUS ARTICLE
Next article, request username.
Can't sign in? Forgot your username? Enter your email address below and we will send you your username
If the address matches an existing account you will receive an email with instructions to retrieve your username
Create a new account
Change password, password changed successfully.
Your password has been changed
Reset password
Can't sign in? Forgot your password?
Enter your email address below and we will send you the reset instructions
If the address matches an existing account you will receive an email with instructions to reset your password.
Your Phone has been verified
As described within the American Psychiatric Association (APA)'s Privacy Policy and Terms of Use , this website utilizes cookies, including for the purpose of offering an optimal online experience and services tailored to your preferences. Please read the entire Privacy Policy and Terms of Use. By closing this message, browsing this website, continuing the navigation, or otherwise continuing to use the APA's websites, you confirm that you understand and accept the terms of the Privacy Policy and Terms of Use, including the utilization of cookies.
Internet explorer is no longer supported
We have detected that you are using Internet Explorer to visit this website. Internet Explorer is now being phased out by Microsoft. As a result, NHS Digital no longer supports any version of Internet Explorer for our web-based products, as it involves considerable extra effort and expense, which cannot be justified from public funds. Some features on this site will not work. You should use a modern browser such as Edge, Chrome, Firefox, or Safari. If you have difficulty installing or accessing a different browser, contact your IT support team.
Publication, Part of Excess under 75 mortality rates in adults with serious mental illness
Excess Under 75 Mortality Rates in Adults With Serious Mental Illness, 2021 to 2023
Experimental statistics, Official statistics in development
(Upcoming, not yet published)
In the wellness industry, your mental health is for sale

Kelly Brogan attends the in goop Health Summit on January 27, 2018 in New York City. Dimitrios Kambouris/Getty Images
Jonathan N. Stea is a practising clinical psychologist, an adjunct assistant professor in the department of psychology at the University of Calgary, and the author of Mind the Science: Saving Your Mental Health from the Wellness Industry , from which this essay has been adapted.
In 2018, millions of subscribers to Goop – Gwyneth Paltrow’s wildly successful natural lifestyle company – were introduced to a new promoted product: the Implant O’Rama , a do-it-yourself coffee-enema device. The product’s website claimed that coffee enemas “can mean relief from depression, confusion, general nervous tension, many allergy related symptoms, and most importantly, relief from severe pain.” The company told its consumers: “Ask not what your colon can do for you, but rather, what you can do for your colon.” Coffee enemas were even endorsed on Goop by seemingly respectable physicians: namely, a cardiologist, Alejandro Junger, identified as an “adrenal fatigue expert,” and “holistic psychiatrist” Kelly Brogan in her New York Times bestseller, A Mind of Your Own: The Truth About Depression and How Women Can Heal Their Bodies to Reclaim Their Lives.
What’s the problem? Well, it turns out that shooting coffee up your bum will not help with depression or any other health concern. Coffee enemas have a long history in the alternative-medicine community despite their lack of credible evidence . They were first introduced as a part of the Gerson Therapy, which was developed by a physician, Max Gerson, in the 1930s for the treatment of degenerative diseases, including cancer. Modern proponents of the therapy still claim that coffee enemas work by helping with liver and intestinal detoxification. The scientific reality is that there is no medical theory or body of research supporting the use of coffee enemas, and in fact they can be quite dangerous and result in burns, inflammation, bacteria in the bloodstream, and even death.
Goop subscribers who purchased Ms. Brogan’s book about depression were introduced to even more products, services and “natural treatments for whole-body wellness” beyond coffee enemas. They were told in Ms. Brogan’s book that a laundry list of supplements was critical to their health and that “unless you are growing your own organic food in a bubble hermetically sealed from the ravages of the modern industrial world, strategic supplementation is almost always going to help you get better and stay better.” They were recommended to doubt whether the scientific construct of depression was even real and were warned about the purported dangers of antidepressant medication, Advil, Lipitor, Prilosec, fluoride, fragrances, genetically modified foods (GMOs), antibiotics, vaccines and birth-control pills. In short, they were sold a cornucopia of misinformation.
There exists little evidence to support the vast majority of Ms. Brogan’s claims. For example, in the American Psychological Association’s official clinical practice guidelines for the treatment of depression – which were developed by health professionals from psychology, psychiatry and primary care, as well as community members who self-identified as having had depression – it’s recommended that depression be treated with evidence-based psychotherapies and antidepressants. After reviewing the science, the guidelines don’t recommend anything resembling Ms. Brogan’s unnecessary and expensive testing and supplementing or dietary plan. And of course, there’s no mention of coffee enemas.
This problem, of course, is much larger and older than coffee enemas, Ms. Brogan and her book. Snake-oil salesmen have been around forever, but it was in the late 19th and early 20th centuries that a guy named Clark Stanley sold actual “snake oil liniment” as a cure-all for various health conditions – incidentally, it didn’t work, and it didn’t even contain actual snake oil.
The problem is that snake-oil salesmen, in the spirit of Clark Stanley, never went away. In the world of mental-health care, scientists have estimated that there are at least 600 “brands” of psychotherapy, an unreasonably and quickly growing number, many of which are ineffective and could be harmful. Beyond that world exist countless unregulated providers of mental-health-related services in the wellness industry and alternative-medicine community who market themselves as “life coaches,” “wellness consultants” and – depending on particular countries and jurisdictions – other various non-legally protected titles, such as “therapists,” “psychotherapists,” “counsellors” and “practitioners.”
As a clinical psychologist, I have encountered many patients who received pseudoscientific assessments and treatments for their mental-health concerns. The tidal wave of pseudoscientific mental-health practices originates both within and outside of the mental-health professions. The global health and wellness industry has an estimated value of more than US $5.6-trillion , which includes legitimate sources of health – such as club memberships and exercise classes – as well as alternative-medicine products and services that purport to improve health, based on baseless or exaggerated claims and questionable evidence of safety and effectiveness.
At the end of the day, your mental health is on the line. And your mental health is precious. You need it to experience joy. You need it to live with purpose, to function in society and to be there for your loved ones. There’s no price tag high enough to measure its value.
Yet, in the wellness industry, your mental health is for sale. You’ve been told you lack it and it’s available for purchase. You just need to buy the latest book with the latest 30-day diet plan, swallow 15 supplements “they” don’t want you to know about, cleanse the toxins from your body by following “10 easy steps,” spiritually awaken on a five-day wellness retreat, or undergo the revolutionary new therapy that most doctors haven’t heard about. That cheapened, commodified version of mental health is a wolf in sheep’s clothing. It’s sexy. It’s alluring. And it’s a sham. It will take you down a yellow brick road paved with pseudoscience, leaving your mental health for dead.
What’s the solution? Pseudoscience and wellness aren’t going anywhere, but it’s rejuvenating to know that we can affect their demand. While it’s the mandate of regulatory bodies of various health professions to protect the public from harm, a vitally important, perhaps counterintuitive lesson is this: We cannot rely merely on care providers and regulatory bodies to protect our mental health. The onus is also on us to empower ourselves with knowledge, such that we can protect ourselves from mental-health scams, charlatanry, and poor or misguided health practices. A person who views their mental health with a scientific lens is advantaged. Grifters hold less power over those who can see through their charades.
Providers that advertise their services to address mental-health concerns but that do not value, respect or understand the role of science in mental-health care risk compromising the safety of patients. And unfortunately for patients, it can very much be a buyer-beware approach to their mental health, both within our health care systems and in the unregulated space where mental-health care is marketed and sold. Improving the science and mental-health literacy skills of both the general public and health care professionals can help mitigate this alarming problem. In part, this involves learning how to spot and avoid false information and pseudoscientific practices.
Unlike rocket science, each of us has experience with the topic of mental health, which makes it easier to believe we can assess claims made without evidence and make claims of our own without expertise. But false information is worse than no information – and without science, it prevails.
Report an editorial error
Report a technical issue
Editorial code of conduct
Interact with The Globe
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 31 August 2024
Knowledge mapping and evolution of research on older adults’ technology acceptance: a bibliometric study from 2013 to 2023
- Xianru Shang ORCID: orcid.org/0009-0000-8906-3216 1 ,
- Zijian Liu 1 ,
- Chen Gong 1 ,
- Zhigang Hu 1 ,
- Yuexuan Wu 1 &
- Chengliang Wang ORCID: orcid.org/0000-0003-2208-3508 2
Humanities and Social Sciences Communications volume 11 , Article number: 1115 ( 2024 ) Cite this article
Metrics details
- Science, technology and society
The rapid expansion of information technology and the intensification of population aging are two prominent features of contemporary societal development. Investigating older adults’ acceptance and use of technology is key to facilitating their integration into an information-driven society. Given this context, the technology acceptance of older adults has emerged as a prioritized research topic, attracting widespread attention in the academic community. However, existing research remains fragmented and lacks a systematic framework. To address this gap, we employed bibliometric methods, utilizing the Web of Science Core Collection to conduct a comprehensive review of literature on older adults’ technology acceptance from 2013 to 2023. Utilizing VOSviewer and CiteSpace for data assessment and visualization, we created knowledge mappings of research on older adults’ technology acceptance. Our study employed multidimensional methods such as co-occurrence analysis, clustering, and burst analysis to: (1) reveal research dynamics, key journals, and domains in this field; (2) identify leading countries, their collaborative networks, and core research institutions and authors; (3) recognize the foundational knowledge system centered on theoretical model deepening, emerging technology applications, and research methods and evaluation, uncovering seminal literature and observing a shift from early theoretical and influential factor analyses to empirical studies focusing on individual factors and emerging technologies; (4) moreover, current research hotspots are primarily in the areas of factors influencing technology adoption, human-robot interaction experiences, mobile health management, and aging-in-place technology, highlighting the evolutionary context and quality distribution of research themes. Finally, we recommend that future research should deeply explore improvements in theoretical models, long-term usage, and user experience evaluation. Overall, this study presents a clear framework of existing research in the field of older adults’ technology acceptance, providing an important reference for future theoretical exploration and innovative applications.
Similar content being viewed by others
Research progress and intellectual structure of design for digital equity (DDE): A bibliometric analysis based on citespace
Exploring the role of interaction in older-adult service innovation: insights from the testing stage

Smart device interest, perceived usefulness, and preferences in rural Alabama seniors
Introduction.
In contemporary society, the rapid development of information technology has been intricately intertwined with the intensifying trend of population aging. According to the latest United Nations forecast, by 2050, the global population aged 65 and above is expected to reach 1.6 billion, representing about 16% of the total global population (UN 2023 ). Given the significant challenges of global aging, there is increasing evidence that emerging technologies have significant potential to maintain health and independence for older adults in their home and healthcare environments (Barnard et al. 2013 ; Soar 2010 ; Vancea and Solé-Casals 2016 ). This includes, but is not limited to, enhancing residential safety with smart home technologies (Touqeer et al. 2021 ; Wang et al. 2022 ), improving living independence through wearable technologies (Perez et al. 2023 ), and increasing medical accessibility via telehealth services (Kruse et al. 2020 ). Technological innovations are redefining the lifestyles of older adults, encouraging a shift from passive to active participation (González et al. 2012 ; Mostaghel 2016 ). Nevertheless, the effective application and dissemination of technology still depends on user acceptance and usage intentions (Naseri et al. 2023 ; Wang et al. 2023a ; Xia et al. 2024 ; Yu et al. 2023 ). Particularly, older adults face numerous challenges in accepting and using new technologies. These challenges include not only physical and cognitive limitations but also a lack of technological experience, along with the influences of social and economic factors (Valk et al. 2018 ; Wilson et al. 2021 ).
User acceptance of technology is a significant focus within information systems (IS) research (Dai et al. 2024 ), with several models developed to explain and predict user behavior towards technology usage, including the Technology Acceptance Model (TAM) (Davis 1989 ), TAM2, TAM3, and the Unified Theory of Acceptance and Use of Technology (UTAUT) (Venkatesh et al. 2003 ). Older adults, as a group with unique needs, exhibit different behavioral patterns during technology acceptance than other user groups, and these uniquenesses include changes in cognitive abilities, as well as motivations, attitudes, and perceptions of the use of new technologies (Chen and Chan 2011 ). The continual expansion of technology introduces considerable challenges for older adults, rendering the understanding of their technology acceptance a research priority. Thus, conducting in-depth research into older adults’ acceptance of technology is critically important for enhancing their integration into the information society and improving their quality of life through technological advancements.
Reviewing relevant literature to identify research gaps helps further solidify the theoretical foundation of the research topic. However, many existing literature reviews primarily focus on the factors influencing older adults’ acceptance or intentions to use technology. For instance, Ma et al. ( 2021 ) conducted a comprehensive analysis of the determinants of older adults’ behavioral intentions to use technology; Liu et al. ( 2022 ) categorized key variables in studies of older adults’ technology acceptance, noting a shift in focus towards social and emotional factors; Yap et al. ( 2022 ) identified seven categories of antecedents affecting older adults’ use of technology from an analysis of 26 articles, including technological, psychological, social, personal, cost, behavioral, and environmental factors; Schroeder et al. ( 2023 ) extracted 119 influencing factors from 59 articles and further categorized these into six themes covering demographics, health status, and emotional awareness. Additionally, some studies focus on the application of specific technologies, such as Ferguson et al. ( 2021 ), who explored barriers and facilitators to older adults using wearable devices for heart monitoring, and He et al. ( 2022 ) and Baer et al. ( 2022 ), who each conducted in-depth investigations into the acceptance of social assistive robots and mobile nutrition and fitness apps, respectively. In summary, current literature reviews on older adults’ technology acceptance exhibit certain limitations. Due to the interdisciplinary nature and complex knowledge structure of this field, traditional literature reviews often rely on qualitative analysis, based on literature analysis and periodic summaries, which lack sufficient objectivity and comprehensiveness. Additionally, systematic research is relatively limited, lacking a macroscopic description of the research trajectory from a holistic perspective. Over the past decade, research on older adults’ technology acceptance has experienced rapid growth, with a significant increase in literature, necessitating the adoption of new methods to review and examine the developmental trends in this field (Chen 2006 ; Van Eck and Waltman 2010 ). Bibliometric analysis, as an effective quantitative research method, analyzes published literature through visualization, offering a viable approach to extracting patterns and insights from a large volume of papers, and has been widely applied in numerous scientific research fields (Achuthan et al. 2023 ; Liu and Duffy 2023 ). Therefore, this study will employ bibliometric methods to systematically analyze research articles related to older adults’ technology acceptance published in the Web of Science Core Collection from 2013 to 2023, aiming to understand the core issues and evolutionary trends in the field, and to provide valuable references for future related research. Specifically, this study aims to explore and answer the following questions:
RQ1: What are the research dynamics in the field of older adults’ technology acceptance over the past decade? What are the main academic journals and fields that publish studies related to older adults’ technology acceptance?
RQ2: How is the productivity in older adults’ technology acceptance research distributed among countries, institutions, and authors?
RQ3: What are the knowledge base and seminal literature in older adults’ technology acceptance research? How has the research theme progressed?
RQ4: What are the current hot topics and their evolutionary trajectories in older adults’ technology acceptance research? How is the quality of research distributed?
Methodology and materials
Research method.
In recent years, bibliometrics has become one of the crucial methods for analyzing literature reviews and is widely used in disciplinary and industrial intelligence analysis (Jing et al. 2023 ; Lin and Yu 2024a ; Wang et al. 2024a ; Xu et al. 2021 ). Bibliometric software facilitates the visualization analysis of extensive literature data, intuitively displaying the network relationships and evolutionary processes between knowledge units, and revealing the underlying knowledge structure and potential information (Chen et al. 2024 ; López-Robles et al. 2018 ; Wang et al. 2024c ). This method provides new insights into the current status and trends of specific research areas, along with quantitative evidence, thereby enhancing the objectivity and scientific validity of the research conclusions (Chen et al. 2023 ; Geng et al. 2024 ). VOSviewer and CiteSpace are two widely used bibliometric software tools in academia (Pan et al. 2018 ), recognized for their robust functionalities based on the JAVA platform. Although each has its unique features, combining these two software tools effectively constructs mapping relationships between literature knowledge units and clearly displays the macrostructure of the knowledge domains. Particularly, VOSviewer, with its excellent graphical representation capabilities, serves as an ideal tool for handling large datasets and precisely identifying the focal points and hotspots of research topics. Therefore, this study utilizes VOSviewer (version 1.6.19) and CiteSpace (version 6.1.R6), combined with in-depth literature analysis, to comprehensively examine and interpret the research theme of older adults’ technology acceptance through an integrated application of quantitative and qualitative methods.
Data source
Web of Science is a comprehensively recognized database in academia, featuring literature that has undergone rigorous peer review and editorial scrutiny (Lin and Yu 2024b ; Mongeon and Paul-Hus 2016 ; Pranckutė 2021 ). This study utilizes the Web of Science Core Collection as its data source, specifically including three major citation indices: Science Citation Index Expanded (SCIE), Social Sciences Citation Index (SSCI), and Arts & Humanities Citation Index (A&HCI). These indices encompass high-quality research literature in the fields of science, social sciences, and arts and humanities, ensuring the comprehensiveness and reliability of the data. We combined “older adults” with “technology acceptance” through thematic search, with the specific search strategy being: TS = (elder OR elderly OR aging OR ageing OR senile OR senior OR old people OR “older adult*”) AND TS = (“technology acceptance” OR “user acceptance” OR “consumer acceptance”). The time span of literature search is from 2013 to 2023, with the types limited to “Article” and “Review” and the language to “English”. Additionally, the search was completed by October 27, 2023, to avoid data discrepancies caused by database updates. The initial search yielded 764 journal articles. Given that searches often retrieve articles that are superficially relevant but actually non-compliant, manual screening post-search was essential to ensure the relevance of the literature (Chen et al. 2024 ). Through manual screening, articles significantly deviating from the research theme were eliminated and rigorously reviewed. Ultimately, this study obtained 500 valid sample articles from the Web of Science Core Collection. The complete PRISMA screening process is illustrated in Fig. 1 .
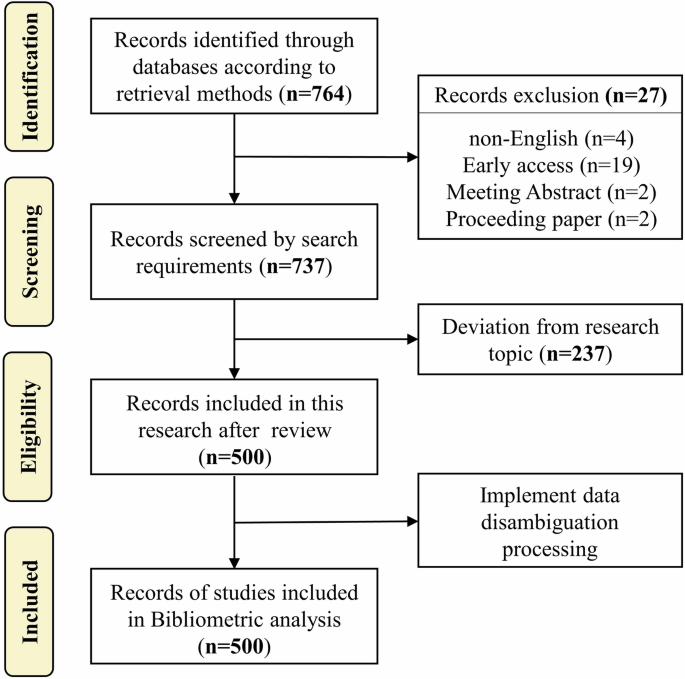
Presentation of the data culling process in detail.
Data standardization
Raw data exported from databases often contain multiple expressions of the same terminology (Nguyen and Hallinger 2020 ). To ensure the accuracy and consistency of data, it is necessary to standardize the raw data (Strotmann and Zhao 2012 ). This study follows the data standardization process proposed by Taskin and Al ( 2019 ), mainly executing the following operations:
(1) Standardization of author and institution names is conducted to address different name expressions for the same author. For instance, “Chan, Alan Hoi Shou” and “Chan, Alan H. S.” are considered the same author, and distinct authors with the same name are differentiated by adding identifiers. Diverse forms of institutional names are unified to address variations caused by name changes or abbreviations, such as standardizing “FRANKFURT UNIV APPL SCI” and “Frankfurt University of Applied Sciences,” as well as “Chinese University of Hong Kong” and “University of Hong Kong” to consistent names.
(2) Different expressions of journal names are unified. For example, “International Journal of Human-Computer Interaction” and “Int J Hum Comput Interact” are standardized to a single name. This ensures consistency in journal names and prevents misclassification of literature due to differing journal names. Additionally, it involves checking if the journals have undergone name changes in the past decade to prevent any impact on the analysis due to such changes.
(3) Keywords data are cleansed by removing words that do not directly pertain to specific research content (e.g., people, review), merging synonyms (e.g., “UX” and “User Experience,” “aging-in-place” and “aging in place”), and standardizing plural forms of keywords (e.g., “assistive technologies” and “assistive technology,” “social robots” and “social robot”). This reduces redundant information in knowledge mapping.
Bibliometric results and analysis
Distribution power (rq1), literature descriptive statistical analysis.
Table 1 presents a detailed descriptive statistical overview of the literature in the field of older adults’ technology acceptance. After deduplication using the CiteSpace software, this study confirmed a valid sample size of 500 articles. Authored by 1839 researchers, the documents encompass 792 research institutions across 54 countries and are published in 217 different academic journals. As of the search cutoff date, these articles have accumulated 13,829 citations, with an annual average of 1156 citations, and an average of 27.66 citations per article. The h-index, a composite metric of quantity and quality of scientific output (Kamrani et al. 2021 ), reached 60 in this study.
Trends in publications and disciplinary distribution
The number of publications and citations are significant indicators of the research field’s development, reflecting its continuity, attention, and impact (Ale Ebrahim et al. 2014 ). The ranking of annual publications and citations in the field of older adults’ technology acceptance studies is presented chronologically in Fig. 2A . The figure shows a clear upward trend in the amount of literature in this field. Between 2013 and 2017, the number of publications increased slowly and decreased in 2018. However, in 2019, the number of publications increased rapidly to 52 and reached a peak of 108 in 2022, which is 6.75 times higher than in 2013. In 2022, the frequency of document citations reached its highest point with 3466 citations, reflecting the widespread recognition and citation of research in this field. Moreover, the curve of the annual number of publications fits a quadratic function, with a goodness-of-fit R 2 of 0.9661, indicating that the number of future publications is expected to increase even more rapidly.
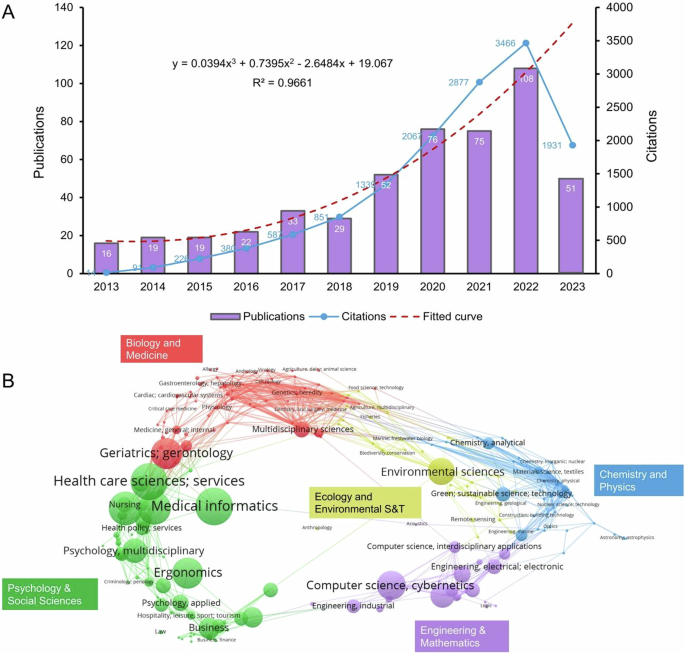
A Trends in trends in annual publications and citations (2013–2023). B Overlay analysis of the distribution of discipline fields.
Figure 2B shows that research on older adults’ technology acceptance involves the integration of multidisciplinary knowledge. According to Web of Science Categories, these 500 articles are distributed across 85 different disciplines. We have tabulated the top ten disciplines by publication volume (Table 2 ), which include Medical Informatics (75 articles, 15.00%), Health Care Sciences & Services (71 articles, 14.20%), Gerontology (61 articles, 12.20%), Public Environmental & Occupational Health (57 articles, 11.40%), and Geriatrics & Gerontology (52 articles, 10.40%), among others. The high output in these disciplines reflects the concentrated global academic interest in this comprehensive research topic. Additionally, interdisciplinary research approaches provide diverse perspectives and a solid theoretical foundation for studies on older adults’ technology acceptance, also paving the way for new research directions.
Knowledge flow analysis
A dual-map overlay is a CiteSpace map superimposed on top of a base map, which shows the interrelationships between journals in different domains, representing the publication and citation activities in each domain (Chen and Leydesdorff 2014 ). The overlay map reveals the link between the citing domain (on the left side) and the cited domain (on the right side), reflecting the knowledge flow of the discipline at the journal level (Leydesdorff and Rafols 2012 ). We utilize the in-built Z-score algorithm of the software to cluster the graph, as shown in Fig. 3 .
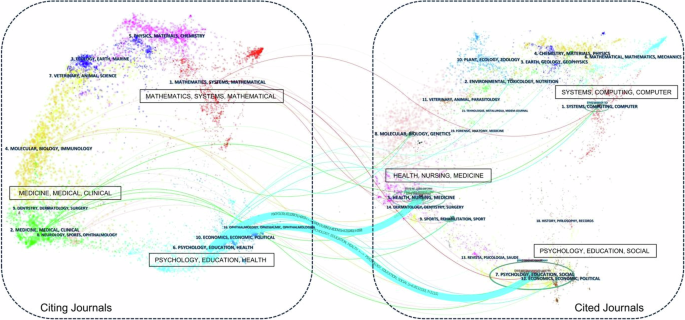
The left side shows the citing journal, and the right side shows the cited journal.
Figure 3 shows the distribution of citing journals clusters for older adults’ technology acceptance on the left side, while the right side refers to the main cited journals clusters. Two knowledge flow citation trajectories were obtained; they are presented by the color of the cited regions, and the thickness of these trajectories is proportional to the Z-score scaled frequency of citations (Chen et al. 2014 ). Within the cited regions, the most popular fields with the most records covered are “HEALTH, NURSING, MEDICINE” and “PSYCHOLOGY, EDUCATION, SOCIAL”, and the elliptical aspect ratio of these two fields stands out. Fields have prominent elliptical aspect ratios, highlighting their significant influence on older adults’ technology acceptance research. Additionally, the major citation trajectories originate in these two areas and progress to the frontier research area of “PSYCHOLOGY, EDUCATION, HEALTH”. It is worth noting that the citation trajectory from “PSYCHOLOGY, EDUCATION, SOCIAL” has a significant Z-value (z = 6.81), emphasizing the significance and impact of this development path. In the future, “MATHEMATICS, SYSTEMS, MATHEMATICAL”, “MOLECULAR, BIOLOGY, IMMUNOLOGY”, and “NEUROLOGY, SPORTS, OPHTHALMOLOGY” may become emerging fields. The fields of “MEDICINE, MEDICAL, CLINICAL” may be emerging areas of cutting-edge research.
Main research journals analysis
Table 3 provides statistics for the top ten journals by publication volume in the field of older adults’ technology acceptance. Together, these journals have published 137 articles, accounting for 27.40% of the total publications, indicating that there is no highly concentrated core group of journals in this field, with publications being relatively dispersed. Notably, Computers in Human Behavior , Journal of Medical Internet Research , and International Journal of Human-Computer Interaction each lead with 15 publications. In terms of citation metrics, International Journal of Medical Informatics and Computers in Human Behavior stand out significantly, with the former accumulating a total of 1,904 citations, averaging 211.56 citations per article, and the latter totaling 1,449 citations, with an average of 96.60 citations per article. These figures emphasize the academic authority and widespread impact of these journals within the research field.
Research power (RQ2)
Countries and collaborations analysis.
The analysis revealed the global research pattern for country distribution and collaboration (Chen et al. 2019 ). Figure 4A shows the network of national collaborations on older adults’ technology acceptance research. The size of the bubbles represents the amount of publications in each country, while the thickness of the connecting lines expresses the closeness of the collaboration among countries. Generally, this research subject has received extensive international attention, with China and the USA publishing far more than any other countries. China has established notable research collaborations with the USA, UK and Malaysia in this field, while other countries have collaborations, but the closeness is relatively low and scattered. Figure 4B shows the annual publication volume dynamics of the top ten countries in terms of total publications. Since 2017, China has consistently increased its annual publications, while the USA has remained relatively stable. In 2019, the volume of publications in each country increased significantly, this was largely due to the global outbreak of the COVID-19 pandemic, which has led to increased reliance on information technology among the elderly for medical consultations, online socialization, and health management (Sinha et al. 2021 ). This phenomenon has led to research advances in technology acceptance among older adults in various countries. Table 4 shows that the top ten countries account for 93.20% of the total cumulative number of publications, with each country having published more than 20 papers. Among these ten countries, all of them except China are developed countries, indicating that the research field of older adults’ technology acceptance has received general attention from developed countries. Currently, China and the USA were the leading countries in terms of publications with 111 and 104 respectively, accounting for 22.20% and 20.80%. The UK, Germany, Italy, and the Netherlands also made significant contributions. The USA and China ranked first and second in terms of the number of citations, while the Netherlands had the highest average citations, indicating the high impact and quality of its research. The UK has shown outstanding performance in international cooperation, while the USA highlights its significant academic influence in this field with the highest h-index value.
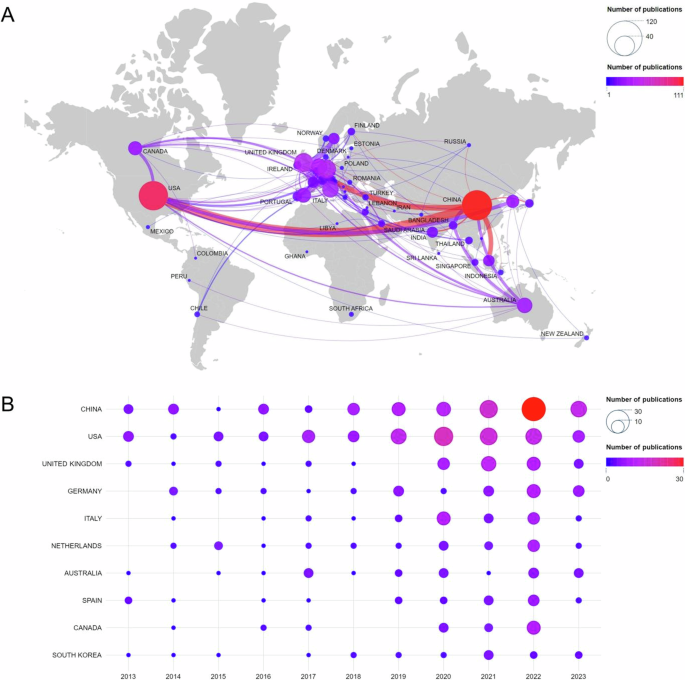
A National collaboration network. B Annual volume of publications in the top 10 countries.
Institutions and authors analysis
Analyzing the number of publications and citations can reveal an institution’s or author’s research strength and influence in a particular research area (Kwiek 2021 ). Tables 5 and 6 show the statistics of the institutions and authors whose publication counts are in the top ten, respectively. As shown in Table 5 , higher education institutions hold the main position in this research field. Among the top ten institutions, City University of Hong Kong and The University of Hong Kong from China lead with 14 and 9 publications, respectively. City University of Hong Kong has the highest h-index, highlighting its significant influence in the field. It is worth noting that Tilburg University in the Netherlands is not among the top five in terms of publications, but the high average citation count (130.14) of its literature demonstrates the high quality of its research.
After analyzing the authors’ output using Price’s Law (Redner 1998 ), the highest number of publications among the authors counted ( n = 10) defines a publication threshold of 3 for core authors in this research area. As a result of quantitative screening, a total of 63 core authors were identified. Table 6 shows that Chen from Zhejiang University, China, Ziefle from RWTH Aachen University, Germany, and Rogers from Macquarie University, Australia, were the top three authors in terms of the number of publications, with 10, 9, and 8 articles, respectively. In terms of average citation rate, Peek and Wouters, both scholars from the Netherlands, have significantly higher rates than other scholars, with 183.2 and 152.67 respectively. This suggests that their research is of high quality and widely recognized. Additionally, Chen and Rogers have high h-indices in this field.
Knowledge base and theme progress (RQ3)
Research knowledge base.
Co-citation relationships occur when two documents are cited together (Zhang and Zhu 2022 ). Co-citation mapping uses references as nodes to represent the knowledge base of a subject area (Min et al. 2021). Figure 5A illustrates co-occurrence mapping in older adults’ technology acceptance research, where larger nodes signify higher co-citation frequencies. Co-citation cluster analysis can be used to explore knowledge structure and research boundaries (Hota et al. 2020 ; Shiau et al. 2023 ). The co-citation clustering mapping of older adults’ technology acceptance research literature (Fig. 5B ) shows that the Q value of the clustering result is 0.8129 (>0.3), and the average value of the weight S is 0.9391 (>0.7), indicating that the clusters are uniformly distributed with a significant and credible structure. This further proves that the boundaries of the research field are clear and there is significant differentiation in the field. The figure features 18 cluster labels, each associated with thematic color blocks corresponding to different time slices. Highlighted emerging research themes include #2 Smart Home Technology, #7 Social Live, and #10 Customer Service. Furthermore, the clustering labels extracted are primarily classified into three categories: theoretical model deepening, emerging technology applications, research methods and evaluation, as detailed in Table 7 .
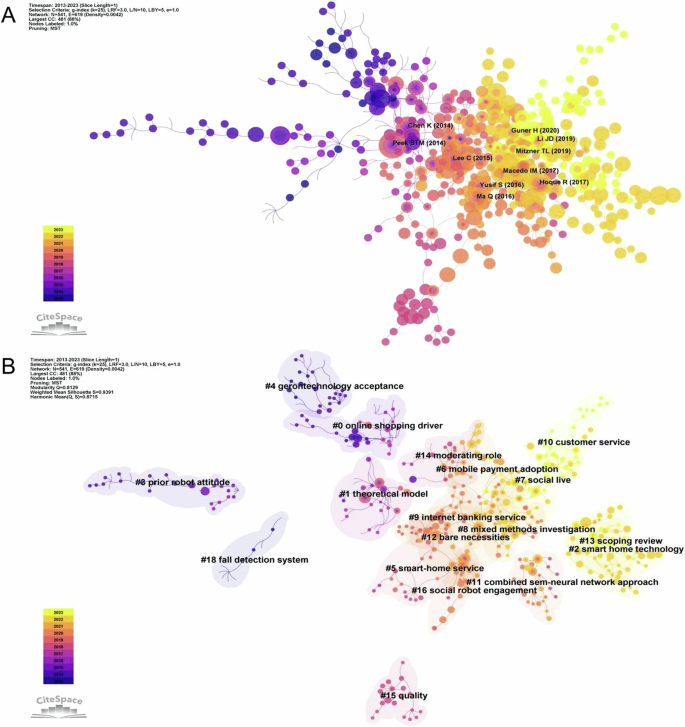
A Co-citation analysis of references. B Clustering network analysis of references.
Seminal literature analysis
The top ten nodes in terms of co-citation frequency were selected for further analysis. Table 8 displays the corresponding node information. Studies were categorized into four main groups based on content analysis. (1) Research focusing on specific technology usage by older adults includes studies by Peek et al. ( 2014 ), Ma et al. ( 2016 ), Hoque and Sorwar ( 2017 ), and Li et al. ( 2019 ), who investigated the factors influencing the use of e-technology, smartphones, mHealth, and smart wearables, respectively. (2) Concerning the development of theoretical models of technology acceptance, Chen and Chan ( 2014 ) introduced the Senior Technology Acceptance Model (STAM), and Macedo ( 2017 ) analyzed the predictive power of UTAUT2 in explaining older adults’ intentional behaviors and information technology usage. (3) In exploring older adults’ information technology adoption and behavior, Lee and Coughlin ( 2015 ) emphasized that the adoption of technology by older adults is a multifactorial process that includes performance, price, value, usability, affordability, accessibility, technical support, social support, emotion, independence, experience, and confidence. Yusif et al. ( 2016 ) conducted a literature review examining the key barriers affecting older adults’ adoption of assistive technology, including factors such as privacy, trust, functionality/added value, cost, and stigma. (4) From the perspective of research into older adults’ technology acceptance, Mitzner et al. ( 2019 ) assessed the long-term usage of computer systems designed for the elderly, whereas Guner and Acarturk ( 2020 ) compared information technology usage and acceptance between older and younger adults. The breadth and prevalence of this literature make it a vital reference for researchers in the field, also providing new perspectives and inspiration for future research directions.
Research thematic progress
Burst citation is a node of literature that guides the sudden change in dosage, which usually represents a prominent development or major change in a particular field, with innovative and forward-looking qualities. By analyzing the emergent literature, it is often easy to understand the dynamics of the subject area, mapping the emerging thematic change (Chen et al. 2022 ). Figure 6 shows the burst citation mapping in the field of older adults’ technology acceptance research, with burst citations represented by red nodes (Fig. 6A ). For the ten papers with the highest burst intensity (Fig. 6B ), this study will conduct further analysis in conjunction with literature review.
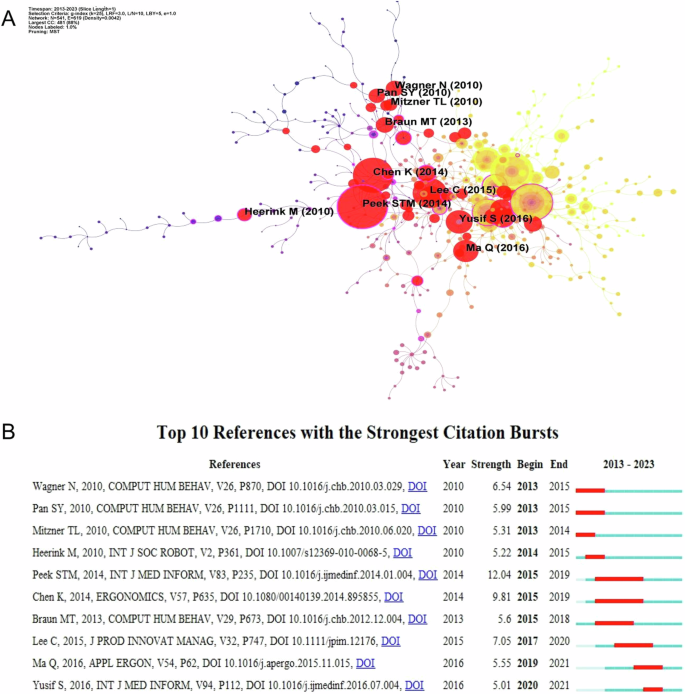
A Burst detection of co-citation. B The top 10 references with the strongest citation bursts.
As shown in Fig. 6 , Mitzner et al. ( 2010 ) broke the stereotype that older adults are fearful of technology, found that they actually have positive attitudes toward technology, and emphasized the centrality of ease of use and usefulness in the process of technology acceptance. This finding provides an important foundation for subsequent research. During the same period, Wagner et al. ( 2010 ) conducted theory-deepening and applied research on technology acceptance among older adults. The research focused on older adults’ interactions with computers from the perspective of Social Cognitive Theory (SCT). This expanded the understanding of technology acceptance, particularly regarding the relationship between behavior, environment, and other SCT elements. In addition, Pan and Jordan-Marsh ( 2010 ) extended the TAM to examine the interactions among predictors of perceived usefulness, perceived ease of use, subjective norm, and convenience conditions when older adults use the Internet, taking into account the moderating roles of gender and age. Heerink et al. ( 2010 ) adapted and extended the UTAUT, constructed a technology acceptance model specifically designed for older users’ acceptance of assistive social agents, and validated it using controlled experiments and longitudinal data, explaining intention to use by combining functional assessment and social interaction variables.
Then the research theme shifted to an in-depth analysis of the factors influencing technology acceptance among older adults. Two papers with high burst strengths emerged during this period: Peek et al. ( 2014 ) (Strength = 12.04), Chen and Chan ( 2014 ) (Strength = 9.81). Through a systematic literature review and empirical study, Peek STM and Chen K, among others, identified multidimensional factors that influence older adults’ technology acceptance. Peek et al. ( 2014 ) analyzed literature on the acceptance of in-home care technology among older adults and identified six factors that influence their acceptance: concerns about technology, expected benefits, technology needs, technology alternatives, social influences, and older adult characteristics, with a focus on differences between pre- and post-implementation factors. Chen and Chan ( 2014 ) constructed the STAM by administering a questionnaire to 1012 older adults and adding eight important factors, including technology anxiety, self-efficacy, cognitive ability, and physical function, based on the TAM. This enriches the theoretical foundation of the field. In addition, Braun ( 2013 ) highlighted the role of perceived usefulness, trust in social networks, and frequency of Internet use in older adults’ use of social networks, while ease of use and social pressure were not significant influences. These findings contribute to the study of older adults’ technology acceptance within specific technology application domains.
Recent research has focused on empirical studies of personal factors and emerging technologies. Ma et al. ( 2016 ) identified key personal factors affecting smartphone acceptance among older adults through structured questionnaires and face-to-face interviews with 120 participants. The study found that cost, self-satisfaction, and convenience were important factors influencing perceived usefulness and ease of use. This study offers empirical evidence to comprehend the main factors that drive smartphone acceptance among Chinese older adults. Additionally, Yusif et al. ( 2016 ) presented an overview of the obstacles that hinder older adults’ acceptance of assistive technologies, focusing on privacy, trust, and functionality.
In summary, research on older adults’ technology acceptance has shifted from early theoretical deepening and analysis of influencing factors to empirical studies in the areas of personal factors and emerging technologies, which have greatly enriched the theoretical basis of older adults’ technology acceptance and provided practical guidance for the design of emerging technology products.
Research hotspots, evolutionary trends, and quality distribution (RQ4)
Core keywords analysis.
Keywords concise the main idea and core of the literature, and are a refined summary of the research content (Huang et al. 2021 ). In CiteSpace, nodes with a centrality value greater than 0.1 are considered to be critical nodes. Analyzing keywords with high frequency and centrality helps to visualize the hot topics in the research field (Park et al. 2018 ). The merged keywords were imported into CiteSpace, and the top 10 keywords were counted and sorted by frequency and centrality respectively, as shown in Table 9 . The results show that the keyword “TAM” has the highest frequency (92), followed by “UTAUT” (24), which reflects that the in-depth study of the existing technology acceptance model and its theoretical expansion occupy a central position in research related to older adults’ technology acceptance. Furthermore, the terms ‘assistive technology’ and ‘virtual reality’ are both high-frequency and high-centrality terms (frequency = 17, centrality = 0.10), indicating that the research on assistive technology and virtual reality for older adults is the focus of current academic attention.
Research hotspots analysis
Using VOSviewer for keyword co-occurrence analysis organizes keywords into groups or clusters based on their intrinsic connections and frequencies, clearly highlighting the research field’s hot topics. The connectivity among keywords reveals correlations between different topics. To ensure accuracy, the analysis only considered the authors’ keywords. Subsequently, the keywords were filtered by setting the keyword frequency to 5 to obtain the keyword clustering map of the research on older adults’ technology acceptance research keyword clustering mapping (Fig. 7 ), combined with the keyword co-occurrence clustering network (Fig. 7A ) and the corresponding density situation (Fig. 7B ) to make a detailed analysis of the following four groups of clustered themes.
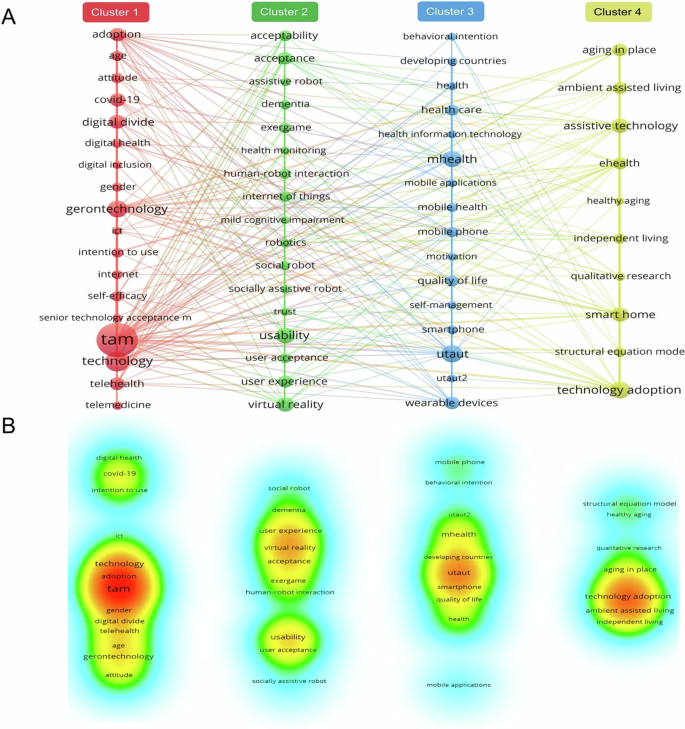
A Co-occurrence clustering network. B Keyword density.
Cluster #1—Research on the factors influencing technology adoption among older adults is a prominent topic, covering age, gender, self-efficacy, attitude, and and intention to use (Berkowsky et al. 2017 ; Wang et al. 2017 ). It also examined older adults’ attitudes towards and acceptance of digital health technologies (Ahmad and Mozelius, 2022 ). Moreover, the COVID-19 pandemic, significantly impacting older adults’ technology attitudes and usage, has underscored the study’s importance and urgency. Therefore, it is crucial to conduct in-depth studies on how older adults accept, adopt, and effectively use new technologies, to address their needs and help them overcome the digital divide within digital inclusion. This will improve their quality of life and healthcare experiences.
Cluster #2—Research focuses on how older adults interact with assistive technologies, especially assistive robots and health monitoring devices, emphasizing trust, usability, and user experience as crucial factors (Halim et al. 2022 ). Moreover, health monitoring technologies effectively track and manage health issues common in older adults, like dementia and mild cognitive impairment (Lussier et al. 2018 ; Piau et al. 2019 ). Interactive exercise games and virtual reality have been deployed to encourage more physical and cognitive engagement among older adults (Campo-Prieto et al. 2021 ). Personalized and innovative technology significantly enhances older adults’ participation, improving their health and well-being.
Cluster #3—Optimizing health management for older adults using mobile technology. With the development of mobile health (mHealth) and health information technology, mobile applications, smartphones, and smart wearable devices have become effective tools to help older users better manage chronic conditions, conduct real-time health monitoring, and even receive telehealth services (Dupuis and Tsotsos 2018 ; Olmedo-Aguirre et al. 2022 ; Kim et al. 2014 ). Additionally, these technologies can mitigate the problem of healthcare resource inequality, especially in developing countries. Older adults’ acceptance and use of these technologies are significantly influenced by their behavioral intentions, motivational factors, and self-management skills. These internal motivational factors, along with external factors, jointly affect older adults’ performance in health management and quality of life.
Cluster #4—Research on technology-assisted home care for older adults is gaining popularity. Environmentally assisted living enhances older adults’ independence and comfort at home, offering essential support and security. This has a crucial impact on promoting healthy aging (Friesen et al. 2016 ; Wahlroos et al. 2023 ). The smart home is a core application in this field, providing a range of solutions that facilitate independent living for the elderly in a highly integrated and user-friendly manner. This fulfills different dimensions of living and health needs (Majumder et al. 2017 ). Moreover, eHealth offers accurate and personalized health management and healthcare services for older adults (Delmastro et al. 2018 ), ensuring their needs are met at home. Research in this field often employs qualitative methods and structural equation modeling to fully understand older adults’ needs and experiences at home and analyze factors influencing technology adoption.
Evolutionary trends analysis
To gain a deeper understanding of the evolutionary trends in research hotspots within the field of older adults’ technology acceptance, we conducted a statistical analysis of the average appearance times of keywords, using CiteSpace to generate the time-zone evolution mapping (Fig. 8 ) and burst keywords. The time-zone mapping visually displays the evolution of keywords over time, intuitively reflecting the frequency and initial appearance of keywords in research, commonly used to identify trends in research topics (Jing et al. 2024a ; Kumar et al. 2021 ). Table 10 lists the top 15 keywords by burst strength, with the red sections indicating high-frequency citations and their burst strength in specific years. These burst keywords reveal the focus and trends of research themes over different periods (Kleinberg 2002 ). Combining insights from the time-zone mapping and burst keywords provides more objective and accurate research insights (Wang et al. 2023b ).
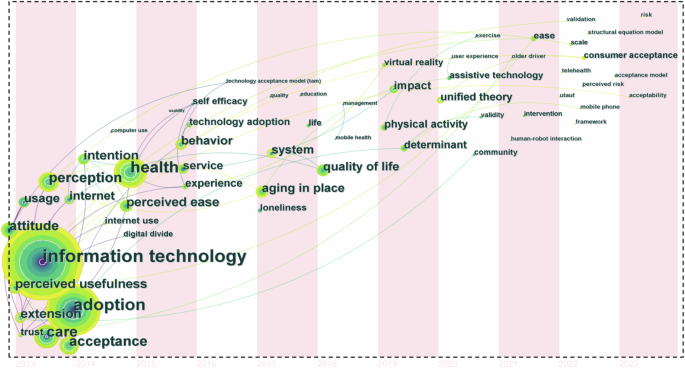
Reflecting the frequency and time of first appearance of keywords in the study.
An integrated analysis of Fig. 8 and Table 10 shows that early research on older adults’ technology acceptance primarily focused on factors such as perceived usefulness, ease of use, and attitudes towards information technology, including their use of computers and the internet (Pan and Jordan-Marsh 2010 ), as well as differences in technology use between older adults and other age groups (Guner and Acarturk 2020 ). Subsequently, the research focus expanded to improving the quality of life for older adults, exploring how technology can optimize health management and enhance the possibility of independent living, emphasizing the significant role of technology in improving the quality of life for the elderly. With ongoing technological advancements, recent research has shifted towards areas such as “virtual reality,” “telehealth,” and “human-robot interaction,” with a focus on the user experience of older adults (Halim et al. 2022 ). The appearance of keywords such as “physical activity” and “exercise” highlights the value of technology in promoting physical activity and health among older adults. This phase of research tends to make cutting-edge technology genuinely serve the practical needs of older adults, achieving its widespread application in daily life. Additionally, research has focused on expanding and quantifying theoretical models of older adults’ technology acceptance, involving keywords such as “perceived risk”, “validation” and “UTAUT”.
In summary, from 2013 to 2023, the field of older adults’ technology acceptance has evolved from initial explorations of influencing factors, to comprehensive enhancements in quality of life and health management, and further to the application and deepening of theoretical models and cutting-edge technologies. This research not only reflects the diversity and complexity of the field but also demonstrates a comprehensive and in-depth understanding of older adults’ interactions with technology across various life scenarios and needs.
Research quality distribution
To reveal the distribution of research quality in the field of older adults’ technology acceptance, a strategic diagram analysis is employed to calculate and illustrate the internal development and interrelationships among various research themes (Xie et al. 2020 ). The strategic diagram uses Centrality as the X-axis and Density as the Y-axis to divide into four quadrants, where the X-axis represents the strength of the connection between thematic clusters and other themes, with higher values indicating a central position in the research field; the Y-axis indicates the level of development within the thematic clusters, with higher values denoting a more mature and widely recognized field (Li and Zhou 2020 ).
Through cluster analysis and manual verification, this study categorized 61 core keywords (Frequency ≥5) into 11 thematic clusters. Subsequently, based on the keywords covered by each thematic cluster, the research themes and their directions for each cluster were summarized (Table 11 ), and the centrality and density coordinates for each cluster were precisely calculated (Table 12 ). Finally, a strategic diagram of the older adults’ technology acceptance research field was constructed (Fig. 9 ). Based on the distribution of thematic clusters across the quadrants in the strategic diagram, the structure and developmental trends of the field were interpreted.
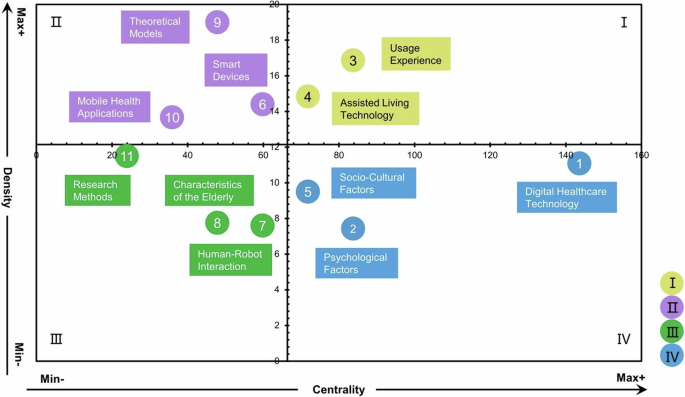
Classification and visualization of theme clusters based on density and centrality.
As illustrated in Fig. 9 , (1) the theme clusters of #3 Usage Experience and #4 Assisted Living Technology are in the first quadrant, characterized by high centrality and density. Their internal cohesion and close links with other themes indicate their mature development, systematic research content or directions have been formed, and they have a significant influence on other themes. These themes play a central role in the field of older adults’ technology acceptance and have promising prospects. (2) The theme clusters of #6 Smart Devices, #9 Theoretical Models, and #10 Mobile Health Applications are in the second quadrant, with higher density but lower centrality. These themes have strong internal connections but weaker external links, indicating that these three themes have received widespread attention from researchers and have been the subject of related research, but more as self-contained systems and exhibit independence. Therefore, future research should further explore in-depth cooperation and cross-application with other themes. (3) The theme clusters of #7 Human-Robot Interaction, #8 Characteristics of the Elderly, and #11 Research Methods are in the third quadrant, with lower centrality and density. These themes are loosely connected internally and have weak links with others, indicating their developmental immaturity. Compared to other topics, they belong to the lower attention edge and niche themes, and there is a need for further investigation. (4) The theme clusters of #1 Digital Healthcare Technology, #2 Psychological Factors, and #5 Socio-Cultural Factors are located in the fourth quadrant, with high centrality but low density. Although closely associated with other research themes, the internal cohesion within these clusters is relatively weak. This suggests that while these themes are closely linked to other research areas, their own development remains underdeveloped, indicating a core immaturity. Nevertheless, these themes are crucial within the research domain of elderly technology acceptance and possess significant potential for future exploration.
Discussion on distribution power (RQ1)
Over the past decade, academic interest and influence in the area of older adults’ technology acceptance have significantly increased. This trend is evidenced by a quantitative analysis of publication and citation volumes, particularly noticeable in 2019 and 2022, where there was a substantial rise in both metrics. The rise is closely linked to the widespread adoption of emerging technologies such as smart homes, wearable devices, and telemedicine among older adults. While these technologies have enhanced their quality of life, they also pose numerous challenges, sparking extensive research into their acceptance, usage behaviors, and influencing factors among the older adults (Pirzada et al. 2022 ; Garcia Reyes et al. 2023 ). Furthermore, the COVID-19 pandemic led to a surge in technology demand among older adults, especially in areas like medical consultation, online socialization, and health management, further highlighting the importance and challenges of technology. Health risks and social isolation have compelled older adults to rely on technology for daily activities, accelerating its adoption and application within this demographic. This phenomenon has made technology acceptance a critical issue, driving societal and academic focus on the study of technology acceptance among older adults.
The flow of knowledge at the level of high-output disciplines and journals, along with the primary publishing outlets, indicates the highly interdisciplinary nature of research into older adults’ technology acceptance. This reflects the complexity and breadth of issues related to older adults’ technology acceptance, necessitating the integration of multidisciplinary knowledge and approaches. Currently, research is primarily focused on medical health and human-computer interaction, demonstrating academic interest in improving health and quality of life for older adults and addressing the urgent needs related to their interactions with technology. In the field of medical health, research aims to provide advanced and innovative healthcare technologies and services to meet the challenges of an aging population while improving the quality of life for older adults (Abdi et al. 2020 ; Wilson et al. 2021 ). In the field of human-computer interaction, research is focused on developing smarter and more user-friendly interaction models to meet the needs of older adults in the digital age, enabling them to actively participate in social activities and enjoy a higher quality of life (Sayago, 2019 ). These studies are crucial for addressing the challenges faced by aging societies, providing increased support and opportunities for the health, welfare, and social participation of older adults.
Discussion on research power (RQ2)
This study analyzes leading countries and collaboration networks, core institutions and authors, revealing the global research landscape and distribution of research strength in the field of older adults’ technology acceptance, and presents quantitative data on global research trends. From the analysis of country distribution and collaborations, China and the USA hold dominant positions in this field, with developed countries like the UK, Germany, Italy, and the Netherlands also excelling in international cooperation and research influence. The significant investment in technological research and the focus on the technological needs of older adults by many developed countries reflect their rapidly aging societies, policy support, and resource allocation.
China is the only developing country that has become a major contributor in this field, indicating its growing research capabilities and high priority given to aging societies and technological innovation. Additionally, China has close collaborations with countries such as USA, the UK, and Malaysia, driven not only by technological research needs but also by shared challenges and complementarities in aging issues among these nations. For instance, the UK has extensive experience in social welfare and aging research, providing valuable theoretical guidance and practical experience. International collaborations, aimed at addressing the challenges of aging, integrate the strengths of various countries, advancing in-depth and widespread development in the research of technology acceptance among older adults.
At the institutional and author level, City University of Hong Kong leads in publication volume, with research teams led by Chan and Chen demonstrating significant academic activity and contributions. Their research primarily focuses on older adults’ acceptance and usage behaviors of various technologies, including smartphones, smart wearables, and social robots (Chen et al. 2015 ; Li et al. 2019 ; Ma et al. 2016 ). These studies, targeting specific needs and product characteristics of older adults, have developed new models of technology acceptance based on existing frameworks, enhancing the integration of these technologies into their daily lives and laying a foundation for further advancements in the field. Although Tilburg University has a smaller publication output, it holds significant influence in the field of older adults’ technology acceptance. Particularly, the high citation rate of Peek’s studies highlights their excellence in research. Peek extensively explored older adults’ acceptance and usage of home care technologies, revealing the complexity and dynamics of their technology use behaviors. His research spans from identifying systemic influencing factors (Peek et al. 2014 ; Peek et al. 2016 ), emphasizing familial impacts (Luijkx et al. 2015 ), to constructing comprehensive models (Peek et al. 2017 ), and examining the dynamics of long-term usage (Peek et al. 2019 ), fully reflecting the evolving technology landscape and the changing needs of older adults. Additionally, the ongoing contributions of researchers like Ziefle, Rogers, and Wouters in the field of older adults’ technology acceptance demonstrate their research influence and leadership. These researchers have significantly enriched the knowledge base in this area with their diverse perspectives. For instance, Ziefle has uncovered the complex attitudes of older adults towards technology usage, especially the trade-offs between privacy and security, and how different types of activities affect their privacy needs (Maidhof et al. 2023 ; Mujirishvili et al. 2023 ; Schomakers and Ziefle 2023 ; Wilkowska et al. 2022 ), reflecting a deep exploration and ongoing innovation in the field of older adults’ technology acceptance.
Discussion on knowledge base and thematic progress (RQ3)
Through co-citation analysis and systematic review of seminal literature, this study reveals the knowledge foundation and thematic progress in the field of older adults’ technology acceptance. Co-citation networks and cluster analyses illustrate the structural themes of the research, delineating the differentiation and boundaries within this field. Additionally, burst detection analysis offers a valuable perspective for understanding the thematic evolution in the field of technology acceptance among older adults. The development and innovation of theoretical models are foundational to this research. Researchers enhance the explanatory power of constructed models by deepening and expanding existing technology acceptance theories to address theoretical limitations. For instance, Heerink et al. ( 2010 ) modified and expanded the UTAUT model by integrating functional assessment and social interaction variables to create the almere model. This model significantly enhances the ability to explain the intentions of older users in utilizing assistive social agents and improves the explanation of actual usage behaviors. Additionally, Chen and Chan ( 2014 ) extended the TAM to include age-related health and capability features of older adults, creating the STAM, which substantially improves predictions of older adults’ technology usage behaviors. Personal attributes, health and capability features, and facilitating conditions have a direct impact on technology acceptance. These factors more effectively predict older adults’ technology usage behaviors than traditional attitudinal factors.
With the advancement of technology and the application of emerging technologies, new research topics have emerged, increasingly focusing on older adults’ acceptance and use of these technologies. Prior to this, the study by Mitzner et al. ( 2010 ) challenged the stereotype of older adults’ conservative attitudes towards technology, highlighting the central roles of usability and usefulness in the technology acceptance process. This discovery laid an important foundation for subsequent research. Research fields such as “smart home technology,” “social life,” and “customer service” are emerging, indicating a shift in focus towards the practical and social applications of technology in older adults’ lives. Research not only focuses on the technology itself but also on how these technologies integrate into older adults’ daily lives and how they can improve the quality of life through technology. For instance, studies such as those by Ma et al. ( 2016 ), Hoque and Sorwar ( 2017 ), and Li et al. ( 2019 ) have explored factors influencing older adults’ use of smartphones, mHealth, and smart wearable devices.
Furthermore, the diversification of research methodologies and innovation in evaluation techniques, such as the use of mixed methods, structural equation modeling (SEM), and neural network (NN) approaches, have enhanced the rigor and reliability of the findings, enabling more precise identification of the factors and mechanisms influencing technology acceptance. Talukder et al. ( 2020 ) employed an effective multimethodological strategy by integrating SEM and NN to leverage the complementary strengths of both approaches, thus overcoming their individual limitations and more accurately analyzing and predicting older adults’ acceptance of wearable health technologies (WHT). SEM is utilized to assess the determinants’ impact on the adoption of WHT, while neural network models validate SEM outcomes and predict the significance of key determinants. This combined approach not only boosts the models’ reliability and explanatory power but also provides a nuanced understanding of the motivations and barriers behind older adults’ acceptance of WHT, offering deep research insights.
Overall, co-citation analysis of the literature in the field of older adults’ technology acceptance has uncovered deeper theoretical modeling and empirical studies on emerging technologies, while emphasizing the importance of research methodological and evaluation innovations in understanding complex social science issues. These findings are crucial for guiding the design and marketing strategies of future technology products, especially in the rapidly growing market of older adults.
Discussion on research hotspots and evolutionary trends (RQ4)
By analyzing core keywords, we can gain deep insights into the hot topics, evolutionary trends, and quality distribution of research in the field of older adults’ technology acceptance. The frequent occurrence of the keywords “TAM” and “UTAUT” indicates that the applicability and theoretical extension of existing technology acceptance models among older adults remain a focal point in academia. This phenomenon underscores the enduring influence of the studies by Davis ( 1989 ) and Venkatesh et al. ( 2003 ), whose models provide a robust theoretical framework for explaining and predicting older adults’ acceptance and usage of emerging technologies. With the widespread application of artificial intelligence (AI) and big data technologies, these theoretical models have incorporated new variables such as perceived risk, trust, and privacy issues (Amin et al. 2024 ; Chen et al. 2024 ; Jing et al. 2024b ; Seibert et al. 2021 ; Wang et al. 2024b ), advancing the theoretical depth and empirical research in this field.
Keyword co-occurrence cluster analysis has revealed multiple research hotspots in the field, including factors influencing technology adoption, interactive experiences between older adults and assistive technologies, the application of mobile health technology in health management, and technology-assisted home care. These studies primarily focus on enhancing the quality of life and health management of older adults through emerging technologies, particularly in the areas of ambient assisted living, smart health monitoring, and intelligent medical care. In these domains, the role of AI technology is increasingly significant (Qian et al. 2021 ; Ho 2020 ). With the evolution of next-generation information technologies, AI is increasingly integrated into elder care systems, offering intelligent, efficient, and personalized service solutions by analyzing the lifestyles and health conditions of older adults. This integration aims to enhance older adults’ quality of life in aspects such as health monitoring and alerts, rehabilitation assistance, daily health management, and emotional support (Lee et al. 2023 ). A survey indicates that 83% of older adults prefer AI-driven solutions when selecting smart products, demonstrating the increasing acceptance of AI in elder care (Zhao and Li 2024 ). Integrating AI into elder care presents both opportunities and challenges, particularly in terms of user acceptance, trust, and long-term usage effects, which warrant further exploration (Mhlanga 2023 ). These studies will help better understand the profound impact of AI technology on the lifestyles of older adults and provide critical references for optimizing AI-driven elder care services.
The Time-zone evolution mapping and burst keyword analysis further reveal the evolutionary trends of research hotspots. Early studies focused on basic technology acceptance models and user perceptions, later expanding to include quality of life and health management. In recent years, research has increasingly focused on cutting-edge technologies such as virtual reality, telehealth, and human-robot interaction, with a concurrent emphasis on the user experience of older adults. This evolutionary process demonstrates a deepening shift from theoretical models to practical applications, underscoring the significant role of technology in enhancing the quality of life for older adults. Furthermore, the strategic coordinate mapping analysis clearly demonstrates the development and mutual influence of different research themes. High centrality and density in the themes of Usage Experience and Assisted Living Technology indicate their mature research status and significant impact on other themes. The themes of Smart Devices, Theoretical Models, and Mobile Health Applications demonstrate self-contained research trends. The themes of Human-Robot Interaction, Characteristics of the Elderly, and Research Methods are not yet mature, but they hold potential for development. Themes of Digital Healthcare Technology, Psychological Factors, and Socio-Cultural Factors are closely related to other themes, displaying core immaturity but significant potential.
In summary, the research hotspots in the field of older adults’ technology acceptance are diverse and dynamic, demonstrating the academic community’s profound understanding of how older adults interact with technology across various life contexts and needs. Under the influence of AI and big data, research should continue to focus on the application of emerging technologies among older adults, exploring in depth how they adapt to and effectively use these technologies. This not only enhances the quality of life and healthcare experiences for older adults but also drives ongoing innovation and development in this field.
Research agenda
Based on the above research findings, to further understand and promote technology acceptance and usage among older adults, we recommend future studies focus on refining theoretical models, exploring long-term usage, and assessing user experience in the following detailed aspects:
Refinement and validation of specific technology acceptance models for older adults: Future research should focus on developing and validating technology acceptance models based on individual characteristics, particularly considering variations in technology acceptance among older adults across different educational levels and cultural backgrounds. This includes factors such as age, gender, educational background, and cultural differences. Additionally, research should examine how well specific technologies, such as wearable devices and mobile health applications, meet the needs of older adults. Building on existing theoretical models, this research should integrate insights from multiple disciplines such as psychology, sociology, design, and engineering through interdisciplinary collaboration to create more accurate and comprehensive models, which should then be validated in relevant contexts.
Deepening the exploration of the relationship between long-term technology use and quality of life among older adults: The acceptance and use of technology by users is a complex and dynamic process (Seuwou et al. 2016 ). Existing research predominantly focuses on older adults’ initial acceptance or short-term use of new technologies; however, the impact of long-term use on their quality of life and health is more significant. Future research should focus on the evolution of older adults’ experiences and needs during long-term technology usage, and the enduring effects of technology on their social interactions, mental health, and life satisfaction. Through longitudinal studies and qualitative analysis, this research reveals the specific needs and challenges of older adults in long-term technology use, providing a basis for developing technologies and strategies that better meet their requirements. This understanding aids in comprehensively assessing the impact of technology on older adults’ quality of life and guiding the optimization and improvement of technological products.
Evaluating the Importance of User Experience in Research on Older Adults’ Technology Acceptance: Understanding the mechanisms of information technology acceptance and use is central to human-computer interaction research. Although technology acceptance models and user experience models differ in objectives, they share many potential intersections. Technology acceptance research focuses on structured prediction and assessment, while user experience research concentrates on interpreting design impacts and new frameworks. Integrating user experience to assess older adults’ acceptance of technology products and systems is crucial (Codfrey et al. 2022 ; Wang et al. 2019 ), particularly for older users, where specific product designs should emphasize practicality and usability (Fisk et al. 2020 ). Researchers need to explore innovative age-appropriate design methods to enhance older adults’ usage experience. This includes studying older users’ actual usage preferences and behaviors, optimizing user interfaces, and interaction designs. Integrating feedback from older adults to tailor products to their needs can further promote their acceptance and continued use of technology products.
Conclusions
This study conducted a systematic review of the literature on older adults’ technology acceptance over the past decade through bibliometric analysis, focusing on the distribution power, research power, knowledge base and theme progress, research hotspots, evolutionary trends, and quality distribution. Using a combination of quantitative and qualitative methods, this study has reached the following conclusions:
Technology acceptance among older adults has become a hot topic in the international academic community, involving the integration of knowledge across multiple disciplines, including Medical Informatics, Health Care Sciences Services, and Ergonomics. In terms of journals, “PSYCHOLOGY, EDUCATION, HEALTH” represents a leading field, with key publications including Computers in Human Behavior , Journal of Medical Internet Research , and International Journal of Human-Computer Interaction . These journals possess significant academic authority and extensive influence in the field.
Research on technology acceptance among older adults is particularly active in developed countries, with China and USA publishing significantly more than other nations. The Netherlands leads in high average citation rates, indicating the depth and impact of its research. Meanwhile, the UK stands out in terms of international collaboration. At the institutional level, City University of Hong Kong and The University of Hong Kong in China are in leading positions. Tilburg University in the Netherlands demonstrates exceptional research quality through its high average citation count. At the author level, Chen from China has the highest number of publications, while Peek from the Netherlands has the highest average citation count.
Co-citation analysis of references indicates that the knowledge base in this field is divided into three main categories: theoretical model deepening, emerging technology applications, and research methods and evaluation. Seminal literature focuses on four areas: specific technology use by older adults, expansion of theoretical models of technology acceptance, information technology adoption behavior, and research perspectives. Research themes have evolved from initial theoretical deepening and analysis of influencing factors to empirical studies on individual factors and emerging technologies.
Keyword analysis indicates that TAM and UTAUT are the most frequently occurring terms, while “assistive technology” and “virtual reality” are focal points with high frequency and centrality. Keyword clustering analysis reveals that research hotspots are concentrated on the influencing factors of technology adoption, human-robot interaction experiences, mobile health management, and technology for aging in place. Time-zone evolution mapping and burst keyword analysis have revealed the research evolution from preliminary exploration of influencing factors, to enhancements in quality of life and health management, and onto advanced technology applications and deepening of theoretical models. Furthermore, analysis of research quality distribution indicates that Usage Experience and Assisted Living Technology have become core topics, while Smart Devices, Theoretical Models, and Mobile Health Applications point towards future research directions.
Through this study, we have systematically reviewed the dynamics, core issues, and evolutionary trends in the field of older adults’ technology acceptance, constructing a comprehensive Knowledge Mapping of the domain and presenting a clear framework of existing research. This not only lays the foundation for subsequent theoretical discussions and innovative applications in the field but also provides an important reference for relevant scholars.
Limitations
To our knowledge, this is the first bibliometric analysis concerning technology acceptance among older adults, and we adhered strictly to bibliometric standards throughout our research. However, this study relies on the Web of Science Core Collection, and while its authority and breadth are widely recognized, this choice may have missed relevant literature published in other significant databases such as PubMed, Scopus, and Google Scholar, potentially overlooking some critical academic contributions. Moreover, given that our analysis was confined to literature in English, it may not reflect studies published in other languages, somewhat limiting the global representativeness of our data sample.
It is noteworthy that with the rapid development of AI technology, its increasingly widespread application in elderly care services is significantly transforming traditional care models. AI is profoundly altering the lifestyles of the elderly, from health monitoring and smart diagnostics to intelligent home systems and personalized care, significantly enhancing their quality of life and health care standards. The potential for AI technology within the elderly population is immense, and research in this area is rapidly expanding. However, due to the restrictive nature of the search terms used in this study, it did not fully cover research in this critical area, particularly in addressing key issues such as trust, privacy, and ethics.
Consequently, future research should not only expand data sources, incorporating multilingual and multidatabase literature, but also particularly focus on exploring older adults’ acceptance of AI technology and its applications, in order to construct a more comprehensive academic landscape of older adults’ technology acceptance, thereby enriching and extending the knowledge system and academic trends in this field.
Data availability
The datasets analyzed during the current study are available in the Dataverse repository: https://doi.org/10.7910/DVN/6K0GJH .
Abdi S, de Witte L, Hawley M (2020) Emerging technologies with potential care and support applications for older people: review of gray literature. JMIR Aging 3(2):e17286. https://doi.org/10.2196/17286
Article PubMed PubMed Central Google Scholar
Achuthan K, Nair VK, Kowalski R, Ramanathan S, Raman R (2023) Cyberbullying research—Alignment to sustainable development and impact of COVID-19: Bibliometrics and science mapping analysis. Comput Human Behav 140:107566. https://doi.org/10.1016/j.chb.2022.107566
Article Google Scholar
Ahmad A, Mozelius P (2022) Human-Computer Interaction for Older Adults: a Literature Review on Technology Acceptance of eHealth Systems. J Eng Res Sci 1(4):119–126. https://doi.org/10.55708/js0104014
Ale Ebrahim N, Salehi H, Embi MA, Habibi F, Gholizadeh H, Motahar SM (2014) Visibility and citation impact. Int Educ Stud 7(4):120–125. https://doi.org/10.5539/ies.v7n4p120
Amin MS, Johnson VL, Prybutok V, Koh CE (2024) An investigation into factors affecting the willingness to disclose personal health information when using AI-enabled caregiver robots. Ind Manag Data Syst 124(4):1677–1699. https://doi.org/10.1108/IMDS-09-2023-0608
Baer NR, Vietzke J, Schenk L (2022) Middle-aged and older adults’ acceptance of mobile nutrition and fitness apps: a systematic mixed studies review. PLoS One 17(12):e0278879. https://doi.org/10.1371/journal.pone.0278879
Barnard Y, Bradley MD, Hodgson F, Lloyd AD (2013) Learning to use new technologies by older adults: Perceived difficulties, experimentation behaviour and usability. Comput Human Behav 29(4):1715–1724. https://doi.org/10.1016/j.chb.2013.02.006
Berkowsky RW, Sharit J, Czaja SJ (2017) Factors predicting decisions about technology adoption among older adults. Innov Aging 3(1):igy002. https://doi.org/10.1093/geroni/igy002
Braun MT (2013) Obstacles to social networking website use among older adults. Comput Human Behav 29(3):673–680. https://doi.org/10.1016/j.chb.2012.12.004
Article MathSciNet Google Scholar
Campo-Prieto P, Rodríguez-Fuentes G, Cancela-Carral JM (2021) Immersive virtual reality exergame promotes the practice of physical activity in older people: An opportunity during COVID-19. Multimodal Technol Interact 5(9):52. https://doi.org/10.3390/mti5090052
Chen C (2006) CiteSpace II: Detecting and visualizing emerging trends and transient patterns in scientific literature. J Am Soc Inf Sci Technol 57(3):359–377. https://doi.org/10.1002/asi.20317
Chen C, Dubin R, Kim MC (2014) Emerging trends and new developments in regenerative medicine: a scientometric update (2000–2014). Expert Opin Biol Ther 14(9):1295–1317. https://doi.org/10.1517/14712598.2014.920813
Article PubMed Google Scholar
Chen C, Leydesdorff L (2014) Patterns of connections and movements in dual‐map overlays: A new method of publication portfolio analysis. J Assoc Inf Sci Technol 65(2):334–351. https://doi.org/10.1002/asi.22968
Chen J, Wang C, Tang Y (2022) Knowledge mapping of volunteer motivation: A bibliometric analysis and cross-cultural comparative study. Front Psychol 13:883150. https://doi.org/10.3389/fpsyg.2022.883150
Chen JY, Liu YD, Dai J, Wang CL (2023) Development and status of moral education research: Visual analysis based on knowledge graph. Front Psychol 13:1079955. https://doi.org/10.3389/fpsyg.2022.1079955
Chen K, Chan AH (2011) A review of technology acceptance by older adults. Gerontechnology 10(1):1–12. https://doi.org/10.4017/gt.2011.10.01.006.00
Chen K, Chan AH (2014) Gerontechnology acceptance by elderly Hong Kong Chinese: a senior technology acceptance model (STAM). Ergonomics 57(5):635–652. https://doi.org/10.1080/00140139.2014.895855
Chen K, Zhang Y, Fu X (2019) International research collaboration: An emerging domain of innovation studies? Res Policy 48(1):149–168. https://doi.org/10.1016/j.respol.2018.08.005
Chen X, Hu Z, Wang C (2024) Empowering education development through AIGC: A systematic literature review. Educ Inf Technol 1–53. https://doi.org/10.1007/s10639-024-12549-7
Chen Y, Chen CM, Liu ZY, Hu ZG, Wang XW (2015) The methodology function of CiteSpace mapping knowledge domains. Stud Sci Sci 33(2):242–253. https://doi.org/10.16192/j.cnki.1003-2053.2015.02.009
Codfrey GS, Baharum A, Zain NHM, Omar M, Deris FD (2022) User Experience in Product Design and Development: Perspectives and Strategies. Math Stat Eng Appl 71(2):257–262. https://doi.org/10.17762/msea.v71i2.83
Dai J, Zhang X, Wang CL (2024) A meta-analysis of learners’ continuance intention toward online education platforms. Educ Inf Technol 1–36. https://doi.org/10.1007/s10639-024-12654-7
Davis FD (1989) Perceived usefulness, perceived ease of use, and user acceptance of information technology. MIS Q 13(3):319–340. https://doi.org/10.2307/249008
Delmastro F, Dolciotti C, Palumbo F, Magrini M, Di Martino F, La Rosa D, Barcaro U (2018) Long-term care: how to improve the quality of life with mobile and e-health services. In 2018 14th International Conference on Wireless and Mobile Computing, Networking and Communications (WiMob), pp. 12–19. IEEE. https://doi.org/10.1109/WiMOB.2018.8589157
Dupuis K, Tsotsos LE (2018) Technology for remote health monitoring in an older population: a role for mobile devices. Multimodal Technol Interact 2(3):43. https://doi.org/10.3390/mti2030043
Ferguson C, Hickman LD, Turkmani S, Breen P, Gargiulo G, Inglis SC (2021) Wearables only work on patients that wear them”: Barriers and facilitators to the adoption of wearable cardiac monitoring technologies. Cardiovasc Digit Health J 2(2):137–147. https://doi.org/10.1016/j.cvdhj.2021.02.001
Fisk AD, Czaja SJ, Rogers WA, Charness N, Sharit J (2020) Designing for older adults: Principles and creative human factors approaches. CRC Press. https://doi.org/10.1201/9781420080681
Friesen S, Brémault-Phillips S, Rudrum L, Rogers LG (2016) Environmental design that supports healthy aging: Evaluating a new supportive living facility. J Hous Elderly 30(1):18–34. https://doi.org/10.1080/02763893.2015.1129380
Garcia Reyes EP, Kelly R, Buchanan G, Waycott J (2023) Understanding Older Adults’ Experiences With Technologies for Health Self-management: Interview Study. JMIR Aging 6:e43197. https://doi.org/10.2196/43197
Geng Z, Wang J, Liu J, Miao J (2024) Bibliometric analysis of the development, current status, and trends in adult degenerative scoliosis research: A systematic review from 1998 to 2023. J Pain Res 17:153–169. https://doi.org/10.2147/JPR.S437575
González A, Ramírez MP, Viadel V (2012) Attitudes of the elderly toward information and communications technologies. Educ Gerontol 38(9):585–594. https://doi.org/10.1080/03601277.2011.595314
Guner H, Acarturk C (2020) The use and acceptance of ICT by senior citizens: a comparison of technology acceptance model (TAM) for elderly and young adults. Univ Access Inf Soc 19(2):311–330. https://doi.org/10.1007/s10209-018-0642-4
Halim I, Saptari A, Perumal PA, Abdullah Z, Abdullah S, Muhammad MN (2022) A Review on Usability and User Experience of Assistive Social Robots for Older Persons. Int J Integr Eng 14(6):102–124. https://penerbit.uthm.edu.my/ojs/index.php/ijie/article/view/8566
He Y, He Q, Liu Q (2022) Technology acceptance in socially assistive robots: Scoping review of models, measurement, and influencing factors. J Healthc Eng 2022(1):6334732. https://doi.org/10.1155/2022/6334732
Heerink M, Kröse B, Evers V, Wielinga B (2010) Assessing acceptance of assistive social agent technology by older adults: the almere model. Int J Soc Robot 2:361–375. https://doi.org/10.1007/s12369-010-0068-5
Ho A (2020) Are we ready for artificial intelligence health monitoring in elder care? BMC Geriatr 20(1):358. https://doi.org/10.1186/s12877-020-01764-9
Hoque R, Sorwar G (2017) Understanding factors influencing the adoption of mHealth by the elderly: An extension of the UTAUT model. Int J Med Inform 101:75–84. https://doi.org/10.1016/j.ijmedinf.2017.02.002
Hota PK, Subramanian B, Narayanamurthy G (2020) Mapping the intellectual structure of social entrepreneurship research: A citation/co-citation analysis. J Bus Ethics 166(1):89–114. https://doi.org/10.1007/s10551-019-04129-4
Huang R, Yan P, Yang X (2021) Knowledge map visualization of technology hotspots and development trends in China’s textile manufacturing industry. IET Collab Intell Manuf 3(3):243–251. https://doi.org/10.1049/cim2.12024
Article ADS Google Scholar
Jing Y, Wang C, Chen Y, Wang H, Yu T, Shadiev R (2023) Bibliometric mapping techniques in educational technology research: A systematic literature review. Educ Inf Technol 1–29. https://doi.org/10.1007/s10639-023-12178-6
Jing YH, Wang CL, Chen ZY, Shen SS, Shadiev R (2024a) A Bibliometric Analysis of Studies on Technology-Supported Learning Environments: Hotopics and Frontier Evolution. J Comput Assist Learn 1–16. https://doi.org/10.1111/jcal.12934
Jing YH, Wang HM, Chen XJ, Wang CL (2024b) What factors will affect the effectiveness of using ChatGPT to solve programming problems? A quasi-experimental study. Humanit Soc Sci Commun 11:319. https://doi.org/10.1057/s41599-024-02751-w
Kamrani P, Dorsch I, Stock WG (2021) Do researchers know what the h-index is? And how do they estimate its importance? Scientometrics 126(7):5489–5508. https://doi.org/10.1007/s11192-021-03968-1
Kim HS, Lee KH, Kim H, Kim JH (2014) Using mobile phones in healthcare management for the elderly. Maturitas 79(4):381–388. https://doi.org/10.1016/j.maturitas.2014.08.013
Article MathSciNet PubMed Google Scholar
Kleinberg J (2002) Bursty and hierarchical structure in streams. In Proceedings of the eighth ACM SIGKDD international conference on Knowledge discovery and data mining, pp. 91–101. https://doi.org/10.1145/775047.775061
Kruse C, Fohn J, Wilson N, Patlan EN, Zipp S, Mileski M (2020) Utilization barriers and medical outcomes commensurate with the use of telehealth among older adults: systematic review. JMIR Med Inform 8(8):e20359. https://doi.org/10.2196/20359
Kumar S, Lim WM, Pandey N, Christopher Westland J (2021) 20 years of electronic commerce research. Electron Commer Res 21:1–40. https://doi.org/10.1007/s10660-021-09464-1
Kwiek M (2021) What large-scale publication and citation data tell us about international research collaboration in Europe: Changing national patterns in global contexts. Stud High Educ 46(12):2629–2649. https://doi.org/10.1080/03075079.2020.1749254
Lee C, Coughlin JF (2015) PERSPECTIVE: Older adults’ adoption of technology: an integrated approach to identifying determinants and barriers. J Prod Innov Manag 32(5):747–759. https://doi.org/10.1111/jpim.12176
Lee CH, Wang C, Fan X, Li F, Chen CH (2023) Artificial intelligence-enabled digital transformation in elderly healthcare field: scoping review. Adv Eng Inform 55:101874. https://doi.org/10.1016/j.aei.2023.101874
Leydesdorff L, Rafols I (2012) Interactive overlays: A new method for generating global journal maps from Web-of-Science data. J Informetr 6(2):318–332. https://doi.org/10.1016/j.joi.2011.11.003
Li J, Ma Q, Chan AH, Man S (2019) Health monitoring through wearable technologies for older adults: Smart wearables acceptance model. Appl Ergon 75:162–169. https://doi.org/10.1016/j.apergo.2018.10.006
Article ADS PubMed Google Scholar
Li X, Zhou D (2020) Product design requirement information visualization approach for intelligent manufacturing services. China Mech Eng 31(07):871, http://www.cmemo.org.cn/EN/Y2020/V31/I07/871
Google Scholar
Lin Y, Yu Z (2024a) An integrated bibliometric analysis and systematic review modelling students’ technostress in higher education. Behav Inf Technol 1–25. https://doi.org/10.1080/0144929X.2024.2332458
Lin Y, Yu Z (2024b) A bibliometric analysis of artificial intelligence chatbots in educational contexts. Interact Technol Smart Educ 21(2):189–213. https://doi.org/10.1108/ITSE-12-2022-0165
Liu L, Duffy VG (2023) Exploring the future development of Artificial Intelligence (AI) applications in chatbots: a bibliometric analysis. Int J Soc Robot 15(5):703–716. https://doi.org/10.1007/s12369-022-00956-0
Liu R, Li X, Chu J (2022) Evolution of applied variables in the research on technology acceptance of the elderly. In: International Conference on Human-Computer Interaction, Cham: Springer International Publishing, pp 500–520. https://doi.org/10.1007/978-3-031-05581-23_5
Luijkx K, Peek S, Wouters E (2015) “Grandma, you should do it—It’s cool” Older Adults and the Role of Family Members in Their Acceptance of Technology. Int J Environ Res Public Health 12(12):15470–15485. https://doi.org/10.3390/ijerph121214999
Lussier M, Lavoie M, Giroux S, Consel C, Guay M, Macoir J, Bier N (2018) Early detection of mild cognitive impairment with in-home monitoring sensor technologies using functional measures: a systematic review. IEEE J Biomed Health Inform 23(2):838–847. https://doi.org/10.1109/JBHI.2018.2834317
López-Robles JR, Otegi-Olaso JR, Porto Gomez I, Gamboa-Rosales NK, Gamboa-Rosales H, Robles-Berumen H (2018) Bibliometric network analysis to identify the intellectual structure and evolution of the big data research field. In: International Conference on Intelligent Data Engineering and Automated Learning, Cham: Springer International Publishing, pp 113–120. https://doi.org/10.1007/978-3-030-03496-2_13
Ma Q, Chan AH, Chen K (2016) Personal and other factors affecting acceptance of smartphone technology by older Chinese adults. Appl Ergon 54:62–71. https://doi.org/10.1016/j.apergo.2015.11.015
Ma Q, Chan AHS, Teh PL (2021) Insights into Older Adults’ Technology Acceptance through Meta-Analysis. Int J Hum-Comput Interact 37(11):1049–1062. https://doi.org/10.1080/10447318.2020.1865005
Macedo IM (2017) Predicting the acceptance and use of information and communication technology by older adults: An empirical examination of the revised UTAUT2. Comput Human Behav 75:935–948. https://doi.org/10.1016/j.chb.2017.06.013
Maidhof C, Offermann J, Ziefle M (2023) Eyes on privacy: acceptance of video-based AAL impacted by activities being filmed. Front Public Health 11:1186944. https://doi.org/10.3389/fpubh.2023.1186944
Majumder S, Aghayi E, Noferesti M, Memarzadeh-Tehran H, Mondal T, Pang Z, Deen MJ (2017) Smart homes for elderly healthcare—Recent advances and research challenges. Sensors 17(11):2496. https://doi.org/10.3390/s17112496
Article ADS PubMed PubMed Central Google Scholar
Mhlanga D (2023) Artificial Intelligence in elderly care: Navigating ethical and responsible AI adoption for seniors. Available at SSRN 4675564. 4675564 min) Identifying citation patterns of scientific breakthroughs: A perspective of dynamic citation process. Inf Process Manag 58(1):102428. https://doi.org/10.1016/j.ipm.2020.102428
Mitzner TL, Boron JB, Fausset CB, Adams AE, Charness N, Czaja SJ, Sharit J (2010) Older adults talk technology: Technology usage and attitudes. Comput Human Behav 26(6):1710–1721. https://doi.org/10.1016/j.chb.2010.06.020
Mitzner TL, Savla J, Boot WR, Sharit J, Charness N, Czaja SJ, Rogers WA (2019) Technology adoption by older adults: Findings from the PRISM trial. Gerontologist 59(1):34–44. https://doi.org/10.1093/geront/gny113
Mongeon P, Paul-Hus A (2016) The journal coverage of Web of Science and Scopus: a comparative analysis. Scientometrics 106:213–228. https://doi.org/10.1007/s11192-015-1765-5
Mostaghel R (2016) Innovation and technology for the elderly: Systematic literature review. J Bus Res 69(11):4896–4900. https://doi.org/10.1016/j.jbusres.2016.04.049
Mujirishvili T, Maidhof C, Florez-Revuelta F, Ziefle M, Richart-Martinez M, Cabrero-García J (2023) Acceptance and privacy perceptions toward video-based active and assisted living technologies: Scoping review. J Med Internet Res 25:e45297. https://doi.org/10.2196/45297
Naseri RNN, Azis SN, Abas N (2023) A Review of Technology Acceptance and Adoption Models in Consumer Study. FIRM J Manage Stud 8(2):188–199. https://doi.org/10.33021/firm.v8i2.4536
Nguyen UP, Hallinger P (2020) Assessing the distinctive contributions of Simulation & Gaming to the literature, 1970–2019: A bibliometric review. Simul Gaming 51(6):744–769. https://doi.org/10.1177/1046878120941569
Olmedo-Aguirre JO, Reyes-Campos J, Alor-Hernández G, Machorro-Cano I, Rodríguez-Mazahua L, Sánchez-Cervantes JL (2022) Remote healthcare for elderly people using wearables: A review. Biosensors 12(2):73. https://doi.org/10.3390/bios12020073
Pan S, Jordan-Marsh M (2010) Internet use intention and adoption among Chinese older adults: From the expanded technology acceptance model perspective. Comput Human Behav 26(5):1111–1119. https://doi.org/10.1016/j.chb.2010.03.015
Pan X, Yan E, Cui M, Hua W (2018) Examining the usage, citation, and diffusion patterns of bibliometric map software: A comparative study of three tools. J Informetr 12(2):481–493. https://doi.org/10.1016/j.joi.2018.03.005
Park JS, Kim NR, Han EJ (2018) Analysis of trends in science and technology using keyword network analysis. J Korea Ind Inf Syst Res 23(2):63–73. https://doi.org/10.9723/jksiis.2018.23.2.063
Peek ST, Luijkx KG, Rijnaard MD, Nieboer ME, Van Der Voort CS, Aarts S, Wouters EJ (2016) Older adults’ reasons for using technology while aging in place. Gerontology 62(2):226–237. https://doi.org/10.1159/000430949
Peek ST, Luijkx KG, Vrijhoef HJ, Nieboer ME, Aarts S, van der Voort CS, Wouters EJ (2017) Origins and consequences of technology acquirement by independent-living seniors: Towards an integrative model. BMC Geriatr 17:1–18. https://doi.org/10.1186/s12877-017-0582-5
Peek ST, Wouters EJ, Van Hoof J, Luijkx KG, Boeije HR, Vrijhoef HJ (2014) Factors influencing acceptance of technology for aging in place: a systematic review. Int J Med Inform 83(4):235–248. https://doi.org/10.1016/j.ijmedinf.2014.01.004
Peek STM, Luijkx KG, Vrijhoef HJM, Nieboer ME, Aarts S, Van Der Voort CS, Wouters EJM (2019) Understanding changes and stability in the long-term use of technologies by seniors who are aging in place: a dynamical framework. BMC Geriatr 19:1–13. https://doi.org/10.1186/s12877-019-1241-9
Perez AJ, Siddiqui F, Zeadally S, Lane D (2023) A review of IoT systems to enable independence for the elderly and disabled individuals. Internet Things 21:100653. https://doi.org/10.1016/j.iot.2022.100653
Piau A, Wild K, Mattek N, Kaye J (2019) Current state of digital biomarker technologies for real-life, home-based monitoring of cognitive function for mild cognitive impairment to mild Alzheimer disease and implications for clinical care: systematic review. J Med Internet Res 21(8):e12785. https://doi.org/10.2196/12785
Pirzada P, Wilde A, Doherty GH, Harris-Birtill D (2022) Ethics and acceptance of smart homes for older adults. Inform Health Soc Care 47(1):10–37. https://doi.org/10.1080/17538157.2021.1923500
Pranckutė R (2021) Web of Science (WoS) and Scopus: The titans of bibliographic information in today’s academic world. Publications 9(1):12. https://doi.org/10.3390/publications9010012
Qian K, Zhang Z, Yamamoto Y, Schuller BW (2021) Artificial intelligence internet of things for the elderly: From assisted living to health-care monitoring. IEEE Signal Process Mag 38(4):78–88. https://doi.org/10.1109/MSP.2021.3057298
Redner S (1998) How popular is your paper? An empirical study of the citation distribution. Eur Phys J B-Condens Matter Complex Syst 4(2):131–134. https://doi.org/10.1007/s100510050359
Sayago S (ed.) (2019) Perspectives on human-computer interaction research with older people. Switzerland: Springer International Publishing. https://doi.org/10.1007/978-3-030-06076-3
Schomakers EM, Ziefle M (2023) Privacy vs. security: trade-offs in the acceptance of smart technologies for aging-in-place. Int J Hum Comput Interact 39(5):1043–1058. https://doi.org/10.1080/10447318.2022.2078463
Schroeder T, Dodds L, Georgiou A, Gewald H, Siette J (2023) Older adults and new technology: Mapping review of the factors associated with older adults’ intention to adopt digital technologies. JMIR Aging 6(1):e44564. https://doi.org/10.2196/44564
Seibert K, Domhoff D, Bruch D, Schulte-Althoff M, Fürstenau D, Biessmann F, Wolf-Ostermann K (2021) Application scenarios for artificial intelligence in nursing care: rapid review. J Med Internet Res 23(11):e26522. https://doi.org/10.2196/26522
Seuwou P, Banissi E, Ubakanma G (2016) User acceptance of information technology: A critical review of technology acceptance models and the decision to invest in Information Security. In: Global Security, Safety and Sustainability-The Security Challenges of the Connected World: 11th International Conference, ICGS3 2017, London, UK, January 18-20, 2017, Proceedings 11:230-251. Springer International Publishing. https://doi.org/10.1007/978-3-319-51064-4_19
Shiau WL, Wang X, Zheng F (2023) What are the trend and core knowledge of information security? A citation and co-citation analysis. Inf Manag 60(3):103774. https://doi.org/10.1016/j.im.2023.103774
Sinha S, Verma A, Tiwari P (2021) Technology: Saving and enriching life during COVID-19. Front Psychol 12:647681. https://doi.org/10.3389/fpsyg.2021.647681
Soar J (2010) The potential of information and communication technologies to support ageing and independent living. Ann Telecommun 65:479–483. https://doi.org/10.1007/s12243-010-0167-1
Strotmann A, Zhao D (2012) Author name disambiguation: What difference does it make in author‐based citation analysis? J Am Soc Inf Sci Technol 63(9):1820–1833. https://doi.org/10.1002/asi.22695
Talukder MS, Sorwar G, Bao Y, Ahmed JU, Palash MAS (2020) Predicting antecedents of wearable healthcare technology acceptance by elderly: A combined SEM-Neural Network approach. Technol Forecast Soc Change 150:119793. https://doi.org/10.1016/j.techfore.2019.119793
Taskin Z, Al U (2019) Natural language processing applications in library and information science. Online Inf Rev 43(4):676–690. https://doi.org/10.1108/oir-07-2018-0217
Touqeer H, Zaman S, Amin R, Hussain M, Al-Turjman F, Bilal M (2021) Smart home security: challenges, issues and solutions at different IoT layers. J Supercomput 77(12):14053–14089. https://doi.org/10.1007/s11227-021-03825-1
United Nations Department of Economic and Social Affairs (2023) World population ageing 2023: Highlights. https://www.un.org/zh/193220
Valk CAL, Lu Y, Randriambelonoro M, Jessen J (2018) Designing for technology acceptance of wearable and mobile technologies for senior citizen users. In: 21st DMI: Academic Design Management Conference (ADMC 2018), Design Management Institute, pp 1361–1373. https://www.dmi.org/page/ADMC2018
Van Eck N, Waltman L (2010) Software survey: VOSviewer, a computer program for bibliometric mapping. Scientometrics 84(2):523–538. https://doi.org/10.1007/s11192-009-0146-3
Vancea M, Solé-Casals J (2016) Population aging in the European Information Societies: towards a comprehensive research agenda in eHealth innovations for elderly. Aging Dis 7(4):526. https://doi.org/10.14336/AD.2015.1214
Venkatesh V, Morris MG, Davis GB, Davis FD (2003) User acceptance of information technology: Toward a unified view. MIS Q 27(3):425–478. https://doi.org/10.2307/30036540
Wagner N, Hassanein K, Head M (2010) Computer use by older adults: A multi-disciplinary review. Comput Human Behav 26(5):870–882. https://doi.org/10.1016/j.chb.2010.03.029
Wahlroos N, Narsakka N, Stolt M, Suhonen R (2023) Physical environment maintaining independence and self-management of older people in long-term care settings—An integrative literature review. J Aging Environ 37(3):295–313. https://doi.org/10.1080/26892618.2022.2092927
Wang CL, Chen XJ, Yu T, Liu YD, Jing YH (2024a) Education reform and change driven by digital technology: a bibliometric study from a global perspective. Humanit Soc Sci Commun 11(1):1–17. https://doi.org/10.1057/s41599-024-02717-y
Wang CL, Dai J, Zhu KK, Yu T, Gu XQ (2023a) Understanding the Continuance Intention of College Students Toward New E-learning Spaces Based on an Integrated Model of the TAM and TTF. Int J Hum-comput Int 1–14. https://doi.org/10.1080/10447318.2023.2291609
Wang CL, Wang HM, Li YY, Dai J, Gu XQ, Yu T (2024b) Factors Influencing University Students’ Behavioral Intention to Use Generative Artificial Intelligence: Integrating the Theory of Planned Behavior and AI Literacy. Int J Hum-comput Int 1–23. https://doi.org/10.1080/10447318.2024.2383033
Wang J, Zhao W, Zhang Z, Liu X, Xie T, Wang L, Zhang Y (2024c) A journey of challenges and victories: a bibliometric worldview of nanomedicine since the 21st century. Adv Mater 36(15):2308915. https://doi.org/10.1002/adma.202308915
Wang J, Chen Y, Huo S, Mai L, Jia F (2023b) Research hotspots and trends of social robot interaction design: A bibliometric analysis. Sensors 23(23):9369. https://doi.org/10.3390/s23239369
Wang KH, Chen G, Chen HG (2017) A model of technology adoption by older adults. Soc Behav Personal 45(4):563–572. https://doi.org/10.2224/sbp.5778
Wang S, Bolling K, Mao W, Reichstadt J, Jeste D, Kim HC, Nebeker C (2019) Technology to Support Aging in Place: Older Adults’ Perspectives. Healthcare 7(2):60. https://doi.org/10.3390/healthcare7020060
Wang Z, Liu D, Sun Y, Pang X, Sun P, Lin F, Ren K (2022) A survey on IoT-enabled home automation systems: Attacks and defenses. IEEE Commun Surv Tutor 24(4):2292–2328. https://doi.org/10.1109/COMST.2022.3201557
Wilkowska W, Offermann J, Spinsante S, Poli A, Ziefle M (2022) Analyzing technology acceptance and perception of privacy in ambient assisted living for using sensor-based technologies. PloS One 17(7):e0269642. https://doi.org/10.1371/journal.pone.0269642
Wilson J, Heinsch M, Betts D, Booth D, Kay-Lambkin F (2021) Barriers and facilitators to the use of e-health by older adults: a scoping review. BMC Public Health 21:1–12. https://doi.org/10.1186/s12889-021-11623-w
Xia YQ, Deng YL, Tao XY, Zhang SN, Wang CL (2024) Digital art exhibitions and psychological well-being in Chinese Generation Z: An analysis based on the S-O-R framework. Humanit Soc Sci Commun 11:266. https://doi.org/10.1057/s41599-024-02718-x
Xie H, Zhang Y, Duan K (2020) Evolutionary overview of urban expansion based on bibliometric analysis in Web of Science from 1990 to 2019. Habitat Int 95:102100. https://doi.org/10.1016/j.habitatint.2019.10210
Xu Z, Ge Z, Wang X, Skare M (2021) Bibliometric analysis of technology adoption literature published from 1997 to 2020. Technol Forecast Soc Change 170:120896. https://doi.org/10.1016/j.techfore.2021.120896
Yap YY, Tan SH, Choon SW (2022) Elderly’s intention to use technologies: a systematic literature review. Heliyon 8(1). https://doi.org/10.1016/j.heliyon.2022.e08765
Yu T, Dai J, Wang CL (2023) Adoption of blended learning: Chinese university students’ perspectives. Humanit Soc Sci Commun 10:390. https://doi.org/10.1057/s41599-023-01904-7
Yusif S, Soar J, Hafeez-Baig A (2016) Older people, assistive technologies, and the barriers to adoption: A systematic review. Int J Med Inform 94:112–116. https://doi.org/10.1016/j.ijmedinf.2016.07.004
Zhang J, Zhu L (2022) Citation recommendation using semantic representation of cited papers’ relations and content. Expert Syst Appl 187:115826. https://doi.org/10.1016/j.eswa.2021.115826
Zhao Y, Li J (2024) Opportunities and challenges of integrating artificial intelligence in China’s elderly care services. Sci Rep 14(1):9254. https://doi.org/10.1038/s41598-024-60067-w
Article ADS MathSciNet PubMed PubMed Central Google Scholar
Download references
Acknowledgements
This research was supported by the Social Science Foundation of Shaanxi Province in China (Grant No. 2023J014).
Author information
Authors and affiliations.
School of Art and Design, Shaanxi University of Science and Technology, Xi’an, China
Xianru Shang, Zijian Liu, Chen Gong, Zhigang Hu & Yuexuan Wu
Department of Education Information Technology, Faculty of Education, East China Normal University, Shanghai, China
Chengliang Wang
You can also search for this author in PubMed Google Scholar
Contributions
Conceptualization, XS, YW, CW; methodology, XS, ZL, CG, CW; software, XS, CG, YW; writing-original draft preparation, XS, CW; writing-review and editing, XS, CG, ZH, CW; supervision, ZL, ZH, CW; project administration, ZL, ZH, CW; funding acquisition, XS, CG. All authors read and approved the final manuscript. All authors have read and approved the re-submission of the manuscript.
Corresponding author
Correspondence to Chengliang Wang .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Ethical approval
Ethical approval was not required as the study did not involve human participants.
Informed consent
Informed consent was not required as the study did not involve human participants.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/ .
Reprints and permissions
About this article
Cite this article.
Shang, X., Liu, Z., Gong, C. et al. Knowledge mapping and evolution of research on older adults’ technology acceptance: a bibliometric study from 2013 to 2023. Humanit Soc Sci Commun 11 , 1115 (2024). https://doi.org/10.1057/s41599-024-03658-2
Download citation
Received : 20 June 2024
Accepted : 21 August 2024
Published : 31 August 2024
DOI : https://doi.org/10.1057/s41599-024-03658-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- HHS Author Manuscripts

Social Media and Mental Health: Benefits, Risks, and Opportunities for Research and Practice
John a. naslund.
a Department of Global Health and Social Medicine, Harvard Medical School, Boston, MA
Ameya Bondre
b CareNX Innovations, Mumbai, India
John Torous
c Department of Psychiatry, Beth Israel Deaconess Medical Center, Boston, MA
Kelly A. Aschbrenner
d Department of Psychiatry, Geisel School of Medicine at Dartmouth, Lebanon, NH
Social media platforms are popular venues for sharing personal experiences, seeking information, and offering peer-to-peer support among individuals living with mental illness. With significant shortfalls in the availability, quality, and reach of evidence-based mental health services across the United States and globally, social media platforms may afford new opportunities to bridge this gap. However, caution is warranted, as numerous studies highlight risks of social media use for mental health. In this commentary, we consider the role of social media as a potentially viable intervention platform for offering support to persons with mental disorders, promoting engagement and retention in care, and enhancing existing mental health services. Specifically, we summarize current research on the use of social media among mental health service users, and early efforts using social media for the delivery of evidence-based programs. We also review the risks, potential harms, and necessary safety precautions with using social media for mental health. To conclude, we explore opportunities using data science and machine learning, for example by leveraging social media for detecting mental disorders and developing predictive models aimed at characterizing the aetiology and progression of mental disorders. These various efforts using social media, as summarized in this commentary, hold promise for improving the lives of individuals living with mental disorders.
Introduction
Social media has become a prominent fixture in the lives of many individuals facing the challenges of mental illness. Social media refers broadly to web and mobile platforms that allow individuals to connect with others within a virtual network (such as Facebook, Twitter, Instagram, Snapchat, or LinkedIn), where they can share, co-create, or exchange various forms of digital content, including information, messages, photos, or videos ( Ahmed, Ahmad, Ahmad, & Zakaria, 2019 ). Studies have reported that individuals living with a range of mental disorders, including depression, psychotic disorders, or other severe mental illnesses, use social media platforms at comparable rates as the general population, with use ranging from about 70% among middle-age and older individuals, to upwards of 97% among younger individuals ( Aschbrenner, Naslund, Grinley, et al., 2018 ; M. L. Birnbaum, Rizvi, Correll, Kane, & Confino, 2017 ; Brunette et al., 2019 ; Naslund, Aschbrenner, & Bartels, 2016 ). Other exploratory studies have found that many of these individuals with mental illness appear to turn to social media to share their personal experiences, seek information about their mental health and treatment options, and give and receive support from others facing similar mental health challenges ( Bucci, Schwannauer, & Berry, 2019 ; Naslund, Aschbrenner, Marsch, & Bartels, 2016b ).
Across the United States and globally, very few people living with mental illness have access to adequate mental health services ( Patel et al., 2018 ). The wide reach and near ubiquitous use of social media platforms may afford novel opportunities to address these shortfalls in existing mental health care, by enhancing the quality, availability, and reach of services. Recent studies have explored patterns of social media use, impact of social media use on mental health and wellbeing, and the potential to leverage the popularity and interactive features of social media to enhance the delivery of interventions. However, there remains uncertainty regarding the risks and potential harms of social media for mental health ( Orben & Przybylski, 2019 ), and how best to weigh these concerns against potential benefits.
In this commentary, we summarized current research on the use of social media among individuals with mental illness, with consideration of the impact of social media on mental wellbeing, as well as early efforts using social media for delivery of evidence-based programs for addressing mental health problems. We searched for recent peer reviewed publications in Medline and Google Scholar using the search terms “mental health” or “mental illness” and “social media”, and searched the reference lists of recent reviews and other relevant studies. We reviewed the risks, potential harms, and necessary safety precautions with using social media for mental health. Overall, our goal was to consider the role of social media as a potentially viable intervention platform for offering support to persons with mental disorders, promoting engagement and retention in care, and enhancing existing mental health services, while balancing the need for safety. Given this broad objective, we did not perform a systematic search of the literature and we did not apply specific inclusion criteria based on study design or type of mental disorder.
Social Media Use and Mental Health
In 2020, there are an estimated 3.8 billion social media users worldwide, representing half the global population ( We Are Social, 2020 ). Recent studies have shown that individuals with mental disorders are increasingly gaining access to and using mobile devices, such as smartphones ( Firth et al., 2015 ; Glick, Druss, Pina, Lally, & Conde, 2016 ; Torous, Chan, et al., 2014 ; Torous, Friedman, & Keshavan, 2014 ). Similarly, there is mounting evidence showing high rates of social media use among individuals with mental disorders, including studies looking at engagement with these popular platforms across diverse settings and disorder types. Initial studies from 2015 found that nearly half of a sample of psychiatric patients were social media users, with greater use among younger individuals ( Trefflich, Kalckreuth, Mergl, & Rummel-Kluge, 2015 ), while 47% of inpatients and outpatients with schizophrenia reported using social media, of which 79% reported at least once-a-week usage of social media websites ( Miller, Stewart, Schrimsher, Peeples, & Buckley, 2015 ). Rates of social media use among psychiatric populations have increased in recent years, as reflected in a study with data from 2017 showing comparable rates of social media use (approximately 70%) among individuals with serious mental illness in treatment as compared to low-income groups from the general population ( Brunette et al., 2019 ).
Similarly, among individuals with serious mental illness receiving community-based mental health services, a recent study found equivalent rates of social media use as the general population, even exceeding 70% of participants ( Naslund, Aschbrenner, & Bartels, 2016 ). Comparable findings were demonstrated among middle-age and older individuals with mental illness accessing services at peer support agencies, where 72% of respondents reported using social media ( Aschbrenner, Naslund, Grinley, et al., 2018 ). Similar results, with 68% of those with first episode psychosis using social media daily were reported in another study ( Abdel-Baki, Lal, D.-Charron, Stip, & Kara, 2017 ).
Individuals who self-identified as having a schizophrenia spectrum disorder responded to a survey shared through the National Alliance of Mental Illness (NAMI), and reported that visiting social media sites was one of their most common activities when using digital devices, taking up roughly 2 hours each day ( Gay, Torous, Joseph, Pandya, & Duckworth, 2016 ). For adolescents and young adults ages 12 to 21 with psychotic disorders and mood disorders, over 97% reported using social media, with average use exceeding 2.5 hours per day ( M. L. Birnbaum et al., 2017 ). Similarly, in a sample of adolescents ages 13-18 recruited from community mental health centers, 98% reported using social media, with YouTube as the most popular platform, followed by Instagram and Snapchat ( Aschbrenner et al., 2019 ).
Research has also explored the motivations for using social media as well as the perceived benefits of interacting on these platforms among individuals with mental illness. In the sections that follow (see Table 1 for a summary), we consider three potentially unique features of interacting and connecting with others on social media that may offer benefits for individuals living with mental illness. These include: 1) Facilitate social interaction; 2) Access to a peer support network; and 3) Promote engagement and retention in services.
Summary of potential benefits and challenges with social media for mental health
| Features of Social Media | Examples | Studies |
|---|---|---|
| 1) Facilitate social interaction | • Online interactions may be easier for individuals with impaired social functioning and facing symptoms • Anonymity can help individuals with stigmatizing conditions connect with others • Young adults with mental illness commonly form online relationships • Social media use in individuals with serious mental illness associated with greater community and civic engagement • Individuals with depressive symptoms prefer communicating on social media than in-person • Online conversations do not require iimnediate responses or non-verbal cues | ( ; ; ; ; ; ; ; ) |
| 2) Access to peer support network | • Online peer support helps seek information, discuss symptoms and medication, share experiences, learn to cope and for self-disclosure. • Individuals with mental disorders establish new relationships, feel less alone or reconnect with people. • Various support patterns are noted in these networks (e.g. ‘informational’, ‘esteem’, ‘network’ and ‘emotional’) | ( ; ; ; ; ; ; ; ; ) |
| 3) Promote engagement and retention in services | • Individuals with mental disorders connect with care providers and access evidence-based services • Online peer support augments existing interventions to improve client engagement and compliance. • Peer networks increase social connectedness and empowerment during recovery. • Interactive peer-to-peer features of social media enhance social functioning • Mobile apps can monitor symptoms, prevent relapses and help users set goals • Digital peer-based interventions target fitness and weight loss in people with mental disorders • Online networks support caregivers of those with mental disorders | ( ; ; ; ; ; ; ; ; ; ; ; ; ) |
| 1) Impact on symptoms | • Studies show increased exposure to harm, social isolation, depressive symptoms and bullying • Social comparison pressure and social isolation after being rejected on social media is coimnon • More frequent visits and more nmnber of social media platforms has been linked with greater depressive symptoms, anxiety and suicide • Social media replaces in-person interactions to contribute to greater loneliness and worsens existing mental symptoms | ( ; ; ; ; ; ; ; ; ; ; ; ) |
| 2) Facing hostile interactions | • Cyberbullying is associated with increased depressive and anxiety symptoms • Greater odds of online harassment in individuals with major depressive symptoms than those with mild or no symptoms. | ( ; ; ; ) |
| 3) Consequences for daily life | • Risks pertain to privacy, confidentiality, and unintended consequences of disclosing personal health information • Misleading information or conflicts of interest, when the platforms promote popular content • Individuals have concerns about privacy, threats to employment, stigma and being judged, adverse impact on relationships and online hostility | ( ; ; ; ) |
Facilitate Social Interaction
Social media platforms offer near continuous opportunities to connect and interact with others, regardless of time of day or geographic location. This on demand ease of communication may be especially important for facilitating social interaction among individuals with mental disorders experiencing difficulties interacting in face-to-face settings. For example, impaired social functioning is a common deficit in schizophrenia spectrum disorders, and social media may facilitate communication and interacting with others for these individuals ( Torous & Keshavan, 2016 ). This was suggested in one study where participants with schizophrenia indicated that social media helped them to interact and socialize more easily ( Miller et al., 2015 ). Like other online communication, the ability to connect with others anonymously may be an important feature of social media, especially for individuals living with highly stigmatizing health conditions ( Berger, Wagner, & Baker, 2005 ), such as serious mental disorders ( Highton-Williamson, Priebe, & Giacco, 2015 ).
Studies have found that individuals with serious mental disorders ( Spinzy, Nitzan, Becker, Bloch, & Fennig, 2012 ) as well as young adults with mental illness ( Gowen, Deschaine, Gruttadara, & Markey, 2012 ) appear to form online relationships and connect with others on social media as often as social media users from the general population. This is an important observation because individuals living with serious mental disorders typically have few social contacts in the offline world, and also experience high rates of loneliness ( Badcock et al., 2015 ; Giacco, Palumbo, Strappelli, Catapano, & Priebe, 2016 ). Among individuals receiving publicly funded mental health services who use social media, nearly half (47%) reported using these platforms at least weekly to feel less alone ( Brusilovskiy, Townley, Snethen, & Salzer, 2016 ). In another study of young adults with serious mental illness, most indicated that they used social media to help feel less isolated ( Gowen et al., 2012 ). Interestingly, more frequent use of social media among a sample of individuals with serious mental illness was associated with greater community participation, measured as participation in shopping, work, religious activities or visiting friends and family, as well as greater civic engagement, reflected as voting in local elections ( Brusilovskiy et al., 2016 ).
Emerging research also shows that young people with moderate to severe depressive symptoms appear to prefer communicating on social media rather than in-person ( Rideout & Fox, 2018 ), while other studies have found that some individuals may prefer to seek help for mental health concerns online rather than through in-person encounters ( Batterham & Calear, 2017 ). In a qualitative study, participants with schizophrenia described greater anonymity, the ability to discover that other people have experienced similar health challenges, and reducing fears through greater access to information as important motivations for using the Internet to seek mental health information ( Schrank, Sibitz, Unger, & Amering, 2010 ). Because social media does not require the immediate responses necessary in face-to-face communication, it may overcome deficits with social interaction due to psychotic symptoms that typically adversely affect face-to-face conversations ( Docherty et al., 1996 ). Online social interactions may not require the use of non-verbal cues, particularly in the initial stages of interaction ( Kiesler, Siegel, & McGuire, 1984 ), with interactions being more fluid, and within the control of users, thereby overcoming possible social anxieties linked to in-person interaction ( Indian & Grieve, 2014 ). Furthermore, many individuals with serious mental disorders can experience symptoms including passive social withdrawal, blunted affect and attentional impairment, as well as active social avoidance due to hallucinations or other concerns ( Hansen, Torgalsbøen, Melle, & Bell, 2009 ); thus, potentially reinforcing the relative advantage, as perceived by users, of using social media over in person conversations.
Access to a Peer Support Network
There is growing recognition about the role that social media channels could play in enabling peer support ( Bucci et al., 2019 ; Naslund, Aschbrenner, et al., 2016b ), referred to as a system of mutual giving and receiving where individuals who have endured the difficulties of mental illness can offer hope, friendship, and support to others facing similar challenges ( Davidson, Chinman, Sells, & Rowe, 2006 ; Mead, Hilton, & Curtis, 2001 ). Initial studies exploring use of online self-help forums among individuals with serious mental illnesses have found that individuals with schizophrenia appeared to use these forums for self-disclosure, and sharing personal experiences, in addition to providing or requesting information, describing symptoms, or discussing medication ( Haker, Lauber, & Rössler, 2005 ), while users with bipolar disorder reported using these forums to ask for help from others about their illness ( Vayreda & Antaki, 2009 ). More recently, in a review of online social networking in people with psychosis, Highton-Williamson et al (2015) highlight that an important purpose of such online connections was to establish new friendships, pursue romantic relationships, maintain existing relationships or reconnect with people, and seek online peer support from others with lived experience ( Highton-Williamson et al., 2015 ).
Online peer support among individuals with mental illness has been further elaborated in various studies. In a content analysis of comments posted to YouTube by individuals who self-identified as having a serious mental illness, there appeared to be opportunities to feel less alone, provide hope, find support and learn through mutual reciprocity, and share coping strategies for day-to-day challenges of living with a mental illness ( Naslund, Grande, Aschbrenner, & Elwyn, 2014 ). In another study, Chang (2009) delineated various communication patterns in an online psychosis peer-support group ( Chang, 2009 ). Specifically, different forms of support emerged, including ‘informational support’ about medication use or contacting mental health providers, ‘esteem support’ involving positive comments for encouragement, ‘network support’ for sharing similar experiences, and ‘emotional support’ to express understanding of a peer’s situation and offer hope or confidence ( Chang, 2009 ). Bauer et al. (2013) reported that the main interest in online self-help forums for patients with bipolar disorder was to share emotions with others, allow exchange of information, and benefit by being part of an online social group ( Bauer, Bauer, Spiessl, & Kagerbauer, 2013 ).
For individuals who openly discuss mental health problems on Twitter, a study by Berry et al. (2017) found that this served as an important opportunity to seek support and to hear about the experiences of others ( Berry et al., 2017 ). In a survey of social media users with mental illness, respondents reported that sharing personal experiences about living with mental illness and opportunities to learn about strategies for coping with mental illness from others were important reasons for using social media ( Naslund et al., 2017 ). A computational study of mental health awareness campaigns on Twitter provides further support with inspirational posts and tips being the most shared ( Saha et al., 2019 ). Taken together, these studies offer insights about the potential for social media to facilitate access to an informal peer support network, though more research is necessary to examine how these online interactions may impact intentions to seek care, illness self-management, and clinically meaningful outcomes in offline contexts.
Promote Engagement and Retention in Services
Many individuals living with mental disorders have expressed interest in using social media platforms for seeking mental health information ( Lal, Nguyen, & Theriault, 2018 ), connecting with mental health providers ( M. L. Birnbaum et al., 2017 ), and accessing evidence-based mental health services delivered over social media specifically for coping with mental health symptoms or for promoting overall health and wellbeing ( Naslund et al., 2017 ). With the widespread use of social media among individuals living with mental illness combined with the potential to facilitate social interaction and connect with supportive peers, as summarized above, it may be possible to leverage the popular features of social media to enhance existing mental health programs and services. A recent review by Biagianti et al (2018) found that peer-to-peer support appeared to offer feasible and acceptable ways to augment digital mental health interventions for individuals with psychotic disorders by specifically improving engagement, compliance, and adherence to the interventions, and may also improve perceived social support ( Biagianti, Quraishi, & Schlosser, 2018 ).
Among digital programs that have incorporated peer-to-peer social networking consistent with popular features on social media platforms, a pilot study of the HORYZONS online psychosocial intervention demonstrated significant reductions in depression among patients with first episode psychosis ( Alvarez-Jimenez et al., 2013 ). Importantly, the majority of participants (95%) in this study engaged with the peer-to-peer networking feature of the program, with many reporting increases in perceived social connectedness and empowerment in their recovery process ( Alvarez-Jimenez et al., 2013 ). This moderated online social therapy program is now being evaluated as part of a large randomized controlled trial for maintaining treatment effects from first episode psychosis services ( Alvarez-Jimenez et al., 2019 ).
Other early efforts have demonstrated that use of digital environments with the interactive peer-to-peer features of social media can enhance social functioning and wellbeing in young people at high risk of psychosis ( Alvarez-Jimenez et al., 2018 ). There has also been a recent emergence of several mobile apps to support symptom monitoring and relapse prevention in psychotic disorders. Among these apps, the development of PRIME (Personalized Real-time Intervention for Motivational Enhancement) has involved working closely with young people with schizophrenia to ensure that the design of the app has the look and feel of mainstream social media platforms, as opposed to existing clinical tools ( Schlosser et al., 2016 ). This unique approach to the design of the app is aimed at promoting engagement, and ensuring that the app can effectively improve motivation and functioning through goal setting and promoting better quality of life of users with schizophrenia ( Schlosser et al., 2018 ).
Social media platforms could also be used to promote engagement and participation in in-person services delivered through community mental health settings. For example, the peer-based lifestyle intervention called PeerFIT targets weight loss and improved fitness among individuals living with serious mental illness through a combination of in-person lifestyle classes, exercise groups, and use of digital technologies ( Aschbrenner, Naslund, Shevenell, Kinney, & Bartels, 2016 ; Aschbrenner, Naslund, Shevenell, Mueser, & Bartels, 2016 ). The intervention holds tremendous promise as lack of support is one of the largest barriers toward exercise in patients with serious mental illness ( Firth et al., 2016 ) and it is now possible to use social media to counter such. Specifically, in PeerFIT, a private Facebook group is closely integrated into the program to offer a closed platform where participants can connect with the lifestyle coaches, access intervention content, and support or encourage each other as they work towards their lifestyle goals ( Aschbrenner, Naslund, & Bartels, 2016 ; Naslund, Aschbrenner, Marsch, & Bartels, 2016a ). To date, this program has demonstrate preliminary effectiveness for meaningfully reducing cardiovascular risk factors that contribute to early mortality in this patient group ( Aschbrenner, Naslund, Shevenell, Kinney, et al., 2016 ), while the Facebook component appears to have increased engagement in the program, while allowing participants who were unable to attend in-person sessions due to other health concerns or competing demands to remain connected with the program ( Naslund, Aschbrenner, Marsch, McHugo, & Bartels, 2018 ). This lifestyle intervention is currently being evaluated in a randomized controlled trial enrolling young adults with serious mental illness from a variety of real world community mental health services settings ( Aschbrenner, Naslund, Gorin, et al., 2018 ).
These examples highlight the promise of incorporating the features of popular social media into existing programs, which may offer opportunities to safely promote engagement and program retention, while achieving improved clinical outcomes. This is an emerging area of research, as evidenced by several important effectiveness trials underway ( Alvarez-Jimenez et al., 2019 ; Aschbrenner, Naslund, Gorin, et al., 2018 ), including efforts to leverage online social networking to support family caregivers of individuals receiving first episode psychosis services ( Gleeson et al., 2017 ).
Challenges with Social Media for Mental Health
The science on the role of social media for engaging persons with mental disorders needs a cautionary note on the effects of social media usage on mental health and well being, particularly in adolescents and young adults. While the risks and harms of social media are frequently covered in the popular press and mainstream news reports, careful consideration of the research in this area is necessary. In a review of 43 studies in young people, many benefits of social media were cited, including increased self-esteem, and opportunities for self-disclosure ( Best, Manktelow, & Taylor, 2014 ). Yet, reported negative effects were an increased exposure to harm, social isolation, depressive symptoms and bullying ( Best et al., 2014 ). In the sections that follow (see Table 1 for a summary), we consider three major categories of risk related to use of social media and mental health. These include: 1) Impact on symptoms; 2) Facing hostile interactions; and 3) Consequences for daily life.
Impact on Symptoms
Studies consistently highlight that use of social media, especially heavy use and prolonged time spent on social media platforms, appears to contribute to increased risk for a variety of mental health symptoms and poor wellbeing, especially among young people ( Andreassen et al., 2016 ; Kross et al., 2013 ; Woods & Scott, 2016 ). This may partly be driven by the detrimental effects of screen time on mental health, including increased severity of anxiety and depressive symptoms, which have been well documented ( Stiglic & Viner, 2019 ). Recent studies have reported negative effects of social media use on mental health of young people, including social comparison pressure with others and greater feeling of social isolation after being rejected by others on social media ( Rideout & Fox, 2018 ). In a study of young adults, it was found that negative comparisons with others on Facebook contributed to risk of rumination and subsequent increases in depression symptoms ( Feinstein et al., 2013 ). Still, the cross sectional nature of many screen time and mental health studies makes it challenging to reach causal inferences ( Orben & Przybylski, 2019 ).
Quantity of social media use is also an important factor, as highlighted in a survey of young adults ages 19 to 32, where more frequent visits to social media platforms each week were correlated with greater depressive symptoms ( Lin et al., 2016 ). More time spent using social media is also associated with greater symptoms of anxiety ( Vannucci, Flannery, & Ohannessian, 2017 ). The actual number of platforms accessed also appears to contribute to risk as reflected in another national survey of young adults where use of a large number of social media platforms was associated with negative impact on mental health ( Primack et al., 2017 ). Among survey respondents using between 7 and 11 different social media platforms compared to respondents using only 2 or fewer platforms, there was a 3 times greater odds of having high levels of depressive symptoms and a 3.2 times greater odds of having high levels of anxiety symptoms ( Primack et al., 2017 ).
Many researchers have postulated that worsening mental health attributed to social media use may be because social media replaces face-to-face interactions for young people ( Twenge & Campbell, 2018 ), and may contribute to greater loneliness ( Bucci et al., 2019 ), and negative effects on other aspects of health and wellbeing ( Woods & Scott, 2016 ). One nationally representative survey of US adolescents found that among respondents who reported more time accessing media such as social media platforms or smartphone devices, there was significantly greater depressive symptoms and increased risk of suicide when compared to adolescents who reported spending more time on non-screen activities, such as in-person social interaction or sports and recreation activities ( Twenge, Joiner, Rogers, & Martin, 2018 ). For individuals living with more severe mental illnesses, the effects of social media on psychiatric symptoms have received less attention. One study found that participation in chat rooms may contribute to worsening symptoms in young people with psychotic disorders ( Mittal, Tessner, & Walker, 2007 ), while another study of patients with psychosis found that social media use appeared to predict low mood ( Berry, Emsley, Lobban, & Bucci, 2018 ). These studies highlight a clear relationship between social media use and mental health that may not be present in general population studies ( Orben & Przybylski, 2019 ), and emphasize the need to explore how social media may contribute to symptom severity and whether protective factors may be identified to mitigate these risks.
Facing Hostile Interactions
Popular social media platforms can create potential situations where individuals may be victimized by negative comments or posts. Cyberbullying represents a form of online aggression directed towards specific individuals, such as peers or acquaintances, which is perceived to be most harmful when compared to random hostile comments posted online ( Hamm et al., 2015 ). Importantly, cyberbullying on social media consistently shows harmful impact on mental health in the form of increased depressive symptoms as well as worsening of anxiety symptoms, as evidenced in a review of 36 studies among children and young people ( Hamm et al., 2015 ). Furthermore, cyberbullying disproportionately impacts females as reflected in a national survey of adolescents in the United States, where females were twice as likely to be victims of cyberbullying compared to males ( Alhajji, Bass, & Dai, 2019 ). Most studies report cross-sectional associations between cyberbullying and symptoms of depression or anxiety ( Hamm et al., 2015 ), though one longitudinal study in Switzerland found that cyberbullying contributed to significantly greater depression over time ( Machmutow, Perren, Sticca, & Alsaker, 2012 ).
For youth ages 10 to 17 who reported major depressive symptomatology, there was over 3 times greater odds of facing online harassment in the last year compared to youth who reported mild or no depressive symptoms ( Ybarra, 2004 ). Similarly, in a 2018 national survey of young people, respondents ages 14 to 22 with moderate to severe depressive symptoms were more likely to have had negative experiences when using social media, and in particular, were more likely to report having faced hostile comments, or being “trolled”, from others when compared to respondents without depressive symptoms (31% vs. 14%) ( Rideout & Fox, 2018 ). As these studies depict risks for victimization on social media and the correlation with poor mental health, it is possible that individuals living with mental illness may also experience greater hostility online compared to individuals without mental illness. This would be consistent with research showing greater risk of hostility, including increased violence and discrimination, directed towards individuals living with mental illness in in-person contexts, especially targeted at those with severe mental illnesses ( Goodman et al., 1999 ).
A computational study of mental health awareness campaigns on Twitter reported that while stigmatizing content was rare, it was actually the most spread (re-tweeted) demonstrating that harmful content can travel quickly on social media ( Saha et al., 2019 ). Another study was able to map the spread of social media posts about the Blue Whale Challenge, an alleged game promoting suicide, over Twitter, YouTube, Reddit, Tumblr and other forums across 127 countries ( Sumner et al., 2019 ). These findings show that it is critical to monitor the actual content of social media posts, such as determining whether content is hostile or promotes harm to self or others. This is pertinent because existing research looking at duration of exposure cannot account for the impact of specific types of content on mental health and is insufficient to fully understand the effects of using these platforms on mental health.
Consequences for Daily Life
The ways in which individuals use social media can also impact their offline relationships and everyday activities. To date, reports have described risks of social media use pertaining to privacy, confidentiality, and unintended consequences of disclosing personal health information online ( Torous & Keshavan, 2016 ). Additionally, concerns have been raised about poor quality or misleading health information shared on social media, and that social media users may not be aware of misleading information or conflicts of interest especially when the platforms promote popular content regardless of whether it is from a trustworthy source ( Moorhead et al., 2013 ; Ventola, 2014 ). For persons living with mental illness there may be additional risks from using social media. A recent study that specifically explored the perspectives of social media users with serious mental illnesses, including participants with schizophrenia spectrum disorders, bipolar disorder, or major depression, found that over one third of participants expressed concerns about privacy when using social media ( Naslund & Aschbrenner, 2019 ). The reported risks of social media use were directly related to many aspects of everyday life, including concerns about threats to employment, fear of stigma and being judged, impact on personal relationships, and facing hostility or being hurt ( Naslund & Aschbrenner, 2019 ). While few studies have specifically explored the dangers of social media use from the perspectives of individuals living with mental illness, it is important to recognize that use of these platforms may contribute to risks that extend beyond worsening symptoms and that can affect different aspects of daily life.
In this commentary we considered ways in which social media may yield benefits for individuals living with mental illness, while contrasting these with the possible harms. Studies reporting on the threats of social media for individuals with mental illness are mostly cross-sectional, making it difficult to draw conclusions about direction of causation. However, the risks are potentially serious. These risks should be carefully considered in discussions pertaining to use of social media and the broader use of digital mental health technologies, as avenues for mental health promotion, or for supporting access to evidence-based programs or mental health services. At this point, it would be premature to view the benefits of social media as outweighing the possible harms, when it is clear from the studies summarized here that social media use can have negative effects on mental health symptoms, can potentially expose individuals to hurtful content and hostile interactions, and can result in serious consequences for daily life, including threats to employment and personal relationships. Despite these risks, it is also necessary to recognize that individuals with mental illness will continue to use social media given the ease of accessing these platforms and the immense popularity of online social networking. With this in mind, it may be ideal to raise awareness about these possible risks so that individuals can implement necessary safeguards, while also highlighting that there could also be benefits. For individuals with mental illness who use social media, being aware of the risks is an essential first step, and then highlighting ways that use of these popular platforms could also contribute to some benefits, ranging from finding meaningful interactions with others, engaging with peer support networks, and accessing information and services.
To capitalize on the widespread use of social media, and to achieve the promise that these platforms may hold for supporting the delivery of targeted mental health interventions, there is need for continued research to better understand how individuals living with mental illness use social media. Such efforts could inform safety measures and also encourage use of social media in ways that maximize potential benefits while minimizing risk of harm. It will be important to recognize how gender and race contribute to differences in use of social media for seeking mental health information or accessing interventions, as well as differences in how social media might impact mental wellbeing. For example, a national survey of 14- to 22-year olds in the United States found that female respondents were more likely to search online for information about depression or anxiety, and to try to connect with other people online who share similar mental health concerns, when compared to male respondents ( Rideout & Fox, 2018 ). In the same survey, there did not appear to be any differences between racial or ethnic groups in social media use for seeking mental health information ( Rideout & Fox, 2018 ). Social media use also appears to have a differential impact on mental health and emotional wellbeing between females and males ( Booker, Kelly, & Sacker, 2018 ), highlighting the need to explore unique experiences between gender groups to inform tailored programs and services. Research shows that lesbian, gay, bisexual or transgender individuals frequently use social media for searching for health information and may be more likely compared to heterosexual individuals to share their own personal health experiences with others online ( Rideout & Fox, 2018 ). Less is known about use of social media for seeking support for mental health concerns among gender minorities, though this is an important area for further investigation as these individuals are more likely to experience mental health problems and more likely to experience online victimization when compared to heterosexual individuals ( Mereish, Sheskier, Hawthorne, & Goldbach, 2019 ).
Similarly, efforts are needed to explore the relationship between social media use and mental health among ethnic and racial minorities. A recent study found that exposure to traumatic online content on social media showing violence or hateful posts directed at racial minorities contributed to increases in psychological distress, PTSD symptoms, and depression among African American and Latinx adolescents in the United States ( Tynes, Willis, Stewart, & Hamilton, 2019 ). These concerns are contrasted by growing interest in the potential for new technologies including social media to expand the reach of services to underrepresented minority groups ( Schueller, Hunter, Figueroa, & Aguilera, 2019 ). Therefore, greater attention is needed to understanding the perspectives of ethnic and racial minorities to inform effective and safe use of social media for mental health promotion efforts.
Research has found that individuals living with mental illness have expressed interest in accessing mental health services through social media platforms. A survey of social media users with mental illness found that most respondents were interested in accessing programs for mental health on social media targeting symptom management, health promotion, and support for communicating with health care providers and interacting with the health system ( Naslund et al., 2017 ). Importantly, individuals with serious mental illness have also emphasized that any mental health intervention on social media would need to be moderated by someone with adequate training and credentials, would need to have ground rules and ways to promote safety and minimize risks, and importantly, would need to be free and easy to access.
An important strength with this commentary is that it combines a range of studies broadly covering the topic of social media and mental health. We have provided a summary of recent evidence in a rapidly advancing field with the goal of presenting unique ways that social media could offer benefits for individuals with mental illness, while also acknowledging the potentially serious risks and the need for further investigation. There are also several limitations with this commentary that warrant consideration. Importantly, as we aimed to address this broad objective, we did not conduct a systematic review of the literature. Therefore, the studies reported here are not exhaustive, and there may be additional relevant studies that were not included. Additionally, we only summarized published studies, and as a result, any reports from the private sector or websites from different organizations using social media or other apps containing social media-like features would have been omitted. Though it is difficult to rigorously summarize work from the private sector, sometimes referred to as “gray literature”, because many of these projects are unpublished and are likely selective in their reporting of findings given the target audience may be shareholders or consumers.
Another notable limitation is that we did not assess risk of bias in the studies summarized in this commentary. We found many studies that highlighted risks associated with social media use for individuals living with mental illness; however, few studies of programs or interventions reported negative findings, suggesting the possibility that negative findings may go unpublished. This concern highlights the need for a future more rigorous review of the literature with careful consideration of bias and an accompanying quality assessment. Most of the studies that we described were from the United States, as well as from other higher income settings such as Australia or the United Kingdom. Despite the global reach of social media platforms, there is a dearth of research on the impact of these platforms on the mental health of individuals in diverse settings, as well as the ways in which social media could support mental health services in lower income countries where there is virtually no access to mental health providers. Future research is necessary to explore the opportunities and risks for social media to support mental health promotion in low-income and middle-income countries, especially as these countries face a disproportionate share of the global burden of mental disorders, yet account for the majority of social media users worldwide ( Naslund et al., 2019 ).
Future Directions for Social Media and Mental Health
As we consider future research directions, the near ubiquitous social media use also yields new opportunities to study the onset and manifestation of mental health symptoms and illness severity earlier than traditional clinical assessments. There is an emerging field of research referred to as ‘digital phenotyping’ aimed at capturing how individuals interact with their digital devices, including social media platforms, in order to study patterns of illness and identify optimal time points for intervention ( Jain, Powers, Hawkins, & Brownstein, 2015 ; Onnela & Rauch, 2016 ). Given that most people access social media via mobile devices, digital phenotyping and social media are closely related ( Torous et al., 2019 ). To date, the emergence of machine learning, a powerful computational method involving statistical and mathematical algorithms ( Shatte, Hutchinson, & Teague, 2019 ), has made it possible to study large quantities of data captured from popular social media platforms such as Twitter or Instagram to illuminate various features of mental health ( Manikonda & De Choudhury, 2017 ; Reece et al., 2017 ). Specifically, conversations on Twitter have been analyzed to characterize the onset of depression ( De Choudhury, Gamon, Counts, & Horvitz, 2013 ) as well as detecting users’ mood and affective states ( De Choudhury, Gamon, & Counts, 2012 ), while photos posted to Instagram can yield insights for predicting depression ( Reece & Danforth, 2017 ). The intersection of social media and digital phenotyping will likely add new levels of context to social media use in the near future.
Several studies have also demonstrated that when compared to a control group, Twitter users with a self-disclosed diagnosis of schizophrenia show unique online communication patterns ( Michael L Birnbaum, Ernala, Rizvi, De Choudhury, & Kane, 2017 ), including more frequent discussion of tobacco use ( Hswen et al., 2017 ), symptoms of depression and anxiety ( Hswen, Naslund, Brownstein, & Hawkins, 2018b ), and suicide ( Hswen, Naslund, Brownstein, & Hawkins, 2018a ). Another study found that online disclosures about mental illness appeared beneficial as reflected by fewer posts about symptoms following self-disclosure (Ernala, Rizvi, Birnbaum, Kane, & De Choudhury, 2017). Each of these examples offers early insights into the potential to leverage widely available online data for better understanding the onset and course of mental illness. It is possible that social media data could be used to supplement additional digital data, such as continuous monitoring using smartphone apps or smart watches, to generate a more comprehensive ‘digital phenotype’ to predict relapse and identify high-risk health behaviors among individuals living with mental illness ( Torous et al., 2019 ).
With research increasingly showing the valuable insights that social media data can yield about mental health states, greater attention to the ethical concerns with using individual data in this way is necessary ( Chancellor, Birnbaum, Caine, Silenzio, & De Choudhury, 2019 ). For instance, data is typically captured from social media platforms without the consent or awareness of users ( Bidargaddi et al., 2017 ), which is especially crucial when the data relates to a socially stigmatizing health condition such as mental illness ( Guntuku, Yaden, Kern, Ungar, & Eichstaedt, 2017 ). Precautions are needed to ensure that data is not made identifiable in ways that were not originally intended by the user who posted the content, as this could place an individual at risk of harm or divulge sensitive health information ( Webb et al., 2017 ; Williams, Burnap, & Sloan, 2017 ). Promising approaches for minimizing these risks include supporting the participation of individuals with expertise in privacy, clinicians, as well as the target individuals with mental illness throughout the collection of data, development of predictive algorithms, and interpretation of findings ( Chancellor et al., 2019 ).
In recognizing that many individuals living with mental illness use social media to search for information about their mental health, it is possible that they may also want to ask their clinicians about what they find online to check if the information is reliable and trustworthy. Alternatively, many individuals may feel embarrassed or reluctant to talk to their clinicians about using social media to find mental health information out of concerns of being judged or dismissed. Therefore, mental health clinicians may be ideally positioned to talk with their patients about using social media, and offer recommendations to promote safe use of these sites, while also respecting their patients’ autonomy and personal motivations for using these popular platforms. Given the gap in clinical knowledge about the impact of social media on mental health, clinicians should be aware of the many potential risks so that they can inform their patients, while remaining open to the possibility that their patients may also experience benefits through use of these platforms. As awareness of these risks grows, it may be possible that new protections will be put in place by industry or through new policies that will make the social media environment safer. It is hard to estimate a number needed to treat or harm today given the nascent state of research, which means the patient and clinician need to weigh the choice on a personal level. Thus offering education and information is an important first step in that process. As patients increasingly show interest in accessing mental health information or services through social media, it will be necessary for health systems to recognize social media as a potential avenue for reaching or offering support to patients. This aligns with growing emphasis on the need for greater integration of digital psychiatry, including apps, smartphones, or wearable devices, into patient care and clinical services through institution-wide initiatives and training clinical providers ( Hilty, Chan, Torous, Luo, & Boland, 2019 ). Within a learning healthcare environment where research and care are tightly intertwined and feedback between both is rapid, the integration of digital technologies into services may create new opportunities for advancing use of social media for mental health.
As highlighted in this commentary, social media has become an important part of the lives of many individuals living with mental disorders. Many of these individuals use social media to share their lived experiences with mental illness, to seek support from others, and to search for information about treatment recommendations, accessing mental health services, and coping with symptoms ( Bucci et al., 2019 ; Highton-Williamson et al., 2015 ; Naslund, Aschbrenner, et al., 2016b ). As the field of digital mental health advances, the wide reach, ease of access, and popularity of social media platforms could be used to allow individuals in need of mental health services or facing challenges of mental illness to access evidence-based treatment and support. To achieve this end and to explore whether social media platforms can advance efforts to close the gap in available mental health services in the United States and globally, it will be essential for researchers to work closely with clinicians and with those affected by mental illness to ensure that possible benefits of using social media are carefully weighed against anticipated risks.
Acknowledgements
Dr. Naslund is supported by a grant from the National Institute of Mental Health (U19MH113211). Dr. Aschbrenner is supported by a grant from the National Institute of Mental Health (1R01MH110965-01).
Publisher's Disclaimer: This Author Accepted Manuscript is a PDF file of a an unedited peer-reviewed manuscript that has been accepted for publication but has not been copyedited or corrected. The official version of record that is published in the journal is kept up to date and so may therefore differ from this version.
Conflict of Interest
The authors have nothing to disclose.
- Abdel-Baki A, Lai S, D.-Charron O, Stip E, & Kara N, (2017). Understanding access and use of technology among youth with first - episode psychosis to inform the development of technology - enabled therapeutic interventions . Early intervention in psychiatry , 77 ( 1 ), 72–76. [ PubMed ] [ Google Scholar ]
- Ahmed YA, Ahmad MN, Ahmad N, & Zakaria NH (2019). Social media for knowledge-sharing: A systematic literature review . Telematics and informatics , 37 , 72–112 . [ Google Scholar ]
- Alhajji M, Bass S, & Dai T (2019). Cyberbullying, mental health, and violence in adolescents and associations with sex and race: data from the 2015 Youth Risk Behavior Survey . Global pediatric health , 6 , 2333794X19868887. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Alvarez-Jimenez M, Bendall S, Koval P, Rice S, Cagliarini D, Valentine L, … Penn DL (2019). HORYZONS trial: protocol for a randomised controlled trial of a moderated online social therapy to maintain treatment effects from first-episode psychosis services . BMJ open , 9 ( 2 ), e024104. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Alvarez-Jimenez M, Bendall S, Lederman R, Wadley G, Chinnery G, Vargas S, … Gleeson JF (2013). On the HORYZON: moderated online social therapy for long-term recovery in first episode psychosis . Schizophrenia research , 143 ( 1 ), 143–149. [ PubMed ] [ Google Scholar ]
- Alvarez-Jimenez M, Gleeson J, Bendall S, Penn D, Yung A, Ryan R, … Miles C (2018). Enhancing social functioning in young people at Ultra High Risk (UHR) for psychosis: A pilot study of a novel strengths and mindfulness-based online social therapy . Schizophrenia research , 202 , 369–377. [ PubMed ] [ Google Scholar ]
- Andreassen CS, Billieux J, Griffiths MD, Kuss DJ, Demetrovics Z, Mazzoni E, & Pallesen S (2016). The relationship between addictive use of social media and video games and symptoms of psychiatric disorders: A large-scale cross-sectional study . Psychology of Addictive Behaviors , 30 ( 2 ), 252. [ PubMed ] [ Google Scholar ]
- Aschbrenner KA, Naslund JA, & Bartels SJ (2016). A mixed methods study of peer-to-peer support in a group-based lifestyle intervention for adults with serious mental illness . Psychiatric rehabilitation journal , 39 ( 4 ), 328. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Aschbrenner KA, Naslund JA, Gorin AA, Mueser KT, Scherer EA, Viron M, … Bartels SJ, (2018). Peer support and mobile health technology targeting obesity-related cardiovascular risk in young adults with serious mental illness: Protocol for a randomized controlled trial . Contemporary clinical trials , 74 , 97–106. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Aschbrenner KA, Naslund JA, Grinley T, Bienvenida JCM, Bartels SJ, & Brunette M (2018). A Survey of Online and Mobile Technology Use at Peer Support Agencies . Psychiatric Quarterly , 1–10. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Aschbrenner KA, Naslund JA, Shevenell M, Kinney E, & Bartels SJ (2016). A pilot study of a peer-group lifestyle intervention enhanced with mHealth technology and social media for adults with serious mental illness . The Journal of nervous and mental disease , 204 ( 6 ), 483–486. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Aschbrenner KA, Naslund JA, Shevenell M, Mueser KT, & Bartels SJ (2016). Feasibility of behavioral weight loss treatment enhanced with peer support and mobile health technology for individuals with serious mental illness . Psychiatric Quarterly , 57 ( 3 ), 401–415. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Aschbrenner KA, Naslund JA, Tomlinson EF, Kinney A, Pratt SI, & Brunette MF (2019). Adolescents’ Use of Digital Technologies and Preferences for Mobile Health Coaching in Mental Health Settings . Frontiers in Public Health . [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Badcock JC, Shah S, Mackinnon A, Stain HJ, Galletly C, Jablensky A, & Morgan VA (2015). Loneliness in psychotic disorders and its association with cognitive function and symptom profile . Schizophrenia research , 169 ( 1-3 ), 268–273. [ PubMed ] [ Google Scholar ]
- Batterham PJ, & Calear AJ (2017). Preferences for internet-based mental health interventions in an adult online sample: Findings from ann online community survey . JMIR mental health , 4 ( 2 ), e26. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Bauer R, Bauer M, Spiessl H, & Kagerbauer T (2013). Cyber-support: an analysis of online self-help forums (online self-help forums in bipolar disorder) . Nordic journal of psychiatry , 67 ( 3 ), 185–190. [ PubMed ] [ Google Scholar ]
- Berger M, Wagner TH, & Baker LC (2005). Internet use and stigmatized illness . Social science & medicine , 67 ( 8 ), 1821–1827. [ PubMed ] [ Google Scholar ]
- Berry N, Emsley R, Lobban F, & Bucci S (2018). Social media and its relationship with mood, self - esteem and paranoia in psychosis . Acta Psychiatrica Scandinavica , 138 , 558–570. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Berry N, Lobban F, Belousov M, Emsley R, Nenadic G, & Bucci S (2017). # Why We Tweet MH: understanding why people use Twitter to discuss mental health problems . Journal of medical Internet research , 19 ( 4 ), e107. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Best P, Manktelow R, & Taylor B (2014). Online communication, social media and adolescent wellbeing: A systematic narrative review . Children and Youth Services Review , 41 , 27–36. [ Google Scholar ]
- Biagianti B, Quraishi SH, & Schlosser DA (2018). Potential benefits of incorporating peer-to-peer interactions into digital interventions for psychotic disorders: a systematic review . Psychiatric Services , 69 ( 4 ), 377–388. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Bidargaddi N, Musiat P, Makinen V-P, Ermes M, Schrader G, & Licinio J (2017). Digital footprints: facilitating large-scale environmental psychiatric research in naturalistic settings through data from everyday technologies . Molecular psychiatry , 22 ( 2 ), 164. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Birnbaum ML, Emala SK, Rizvi AF, De Choudhury M, & Kane JM (2017). A Collaborative Approach to Identifying Social Media Markers of Schizophrenia by Employing Machine Learning and Clinical Appraisals . Journal of medical Internet research , 79 ( 8 ), e289. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Birnbaum ML, Rizvi AF, Correll CU, Kane JM, & Confino J (2017). Role of social media and the Internet in pathways to care for adolescents and young adults with psychotic disorders and non - psychotic mood disorders . Early intervention in psychiatry , 77 ( 4 ), 290–295. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Booker CL, Kelly YJ, & Sacker A (2018). Gender differences in the associations between age trends of social media interaction and well-being among 10-15 year olds in the UK . BMC public health , 18 ( 1 ), 321. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Brunette M, Achtyes E, Pratt S, Stilwell K, Opperman M, Guarino S, & Kay-Lambkin F (2019). Use of smartphones, computers and social media among people with SMI: opportunity for intervention . Community mental health journal , 1–6. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Brusilovskiy E, Townley G, Snethen G, & Salzer MS (2016). Social media use, community participation and psychological well-being among individuals with serious mental illnesses . Computers in Human Behavior , 65 , 232–240. [ Google Scholar ]
- Bucci S, Schwannauer M, & Berry N (2019). The digital revolution and its impact on mental health care . Psychology and Psychotherapy: Theory, Research and Practice , 1–21. [ PubMed ] [ Google Scholar ]
- Chancellor S, Birnbaum ML, Caine ED, Silenzio V, & De Choudhury M (2019). A taxonomy of ethical tensions in inferring mental health states from social media . Paper presented at the Proceedings of the Conference on Fairness, Accountability, and Transparency. [ Google Scholar ]
- Chang HJ (2009). Online supportive interactions: Using a network approach to examine communication patterns within a psychosis social support group in Taiwan . Journal of the American Society for Information Science and Technology , 60 ( 7 ), 1504–1517. [ Google Scholar ]
- Davidson L, Chinman M, Sells D, & Rowe M (2006). Peer support among adults with serious mental illness: a report from the field . Schizophrenia bulletin , 32 ( 3 ), 443–450. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- De Choudhury M, Gamon M, & Counts S (2012). Happy, nervous or surprised? classification of human affective states in social media . Paper presented at the Sixth International AAAI Conference on Weblogs and Social Media. [ Google Scholar ]
- De Choudhury M, Gamon M, Counts S, & Horvitz E (2013). Predicting Depression via Social Media . Paper presented at the Association for the Advancement of Artificial Intelligence. [ Google Scholar ]
- Docherty NM, Hawkins KA, Hoffman RE, Quinlan DM, Rakfeldt J, & Sledge WH (1996). Working memory, attention, and communication disturbances in schizophrenia . Journal of Abnormal Psychology , 105 ( 2 ), 212. [ PubMed ] [ Google Scholar ]
- Emala SK, Rizvi AF, Birnbaum ML, Kane JM, & De Choudhury M (2017). Linguistic Markers Indicating Therapeutic Outcomes of Social Media Disclosures of Schizophrenia . Proc. ACMHum.-Comput. Interact , 1 ( 1 ), 43. [ Google Scholar ]
- Feinstein BA, Hershenberg R, Bhatia V, Latack JA, Meuwly N, & Davila J (2013). Negative social comparison on Facebook and depressive symptoms: Rumination as a mechanism . Psychology of Popular Media Culture , 2 ( 3 ), 161. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Firth J, Cotter J, Torous J, Bucci S, Firth JA, & Yung AR (2015). Mobile phone ownership and endorsement of “mHealth” among people with psychosis: a meta-analysis of cross-sectional studies . Schizophrenia bulletin , 42 ( 2 ), 448–455. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Firth J, Rosenbaum S, Stubbs B, Gorczynski P, Yung AR, & Vancampfort D (2016). Motivating factors and barriers towards exercise in severe mental illness: a systematic review and meta-analysis . Psychological medicine , 46 ( 14 ), 2869–2881. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Gay K, Torous J, Joseph A, Pandya A, & Duckworth K (2016). Digital technology use among individuals with schizophrenia: results of an online survey . JMIR mental health , 3 ( 2 ), el5. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Giacco D, Palumbo C, Strappelli N, Catapano F, & Priebe S (2016). Social contacts and loneliness in people with psychotic and mood disorders . Comprehensive Psychiatry , 66 , 59–66. [ PubMed ] [ Google Scholar ]
- Gleeson J, Lederman R, Herrman H, Koval P, Eleftheriadis D, Bendall S, … Alvarez-Jimenez M (2017). Moderated online social therapy for carers of young people recovering from first-episode psychosis: study protocol for a randomised controlled trial . Trials , 75 ( 1 ), 27. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Glick G, Druss B, Pina J, Lally C, & Conde M (2016). Use of mobile technology in a community mental health setting . Journal of telemedicine and telecare , 22 ( 7 ), 430–435. [ PubMed ] [ Google Scholar ]
- Goodman LA, Thompson KM, Weinfurt K, Corl S, Acker P, Mueser KT, & Rosenberg SD (1999). Reliability of reports of violent victimization and posttraumatic stress disorder among men and women with serious mental illness . Journal of Traumatic Stress: Official Publication of the International Society for Traumatic Stress Studies , 12 ( 4 ), 587–599. [ PubMed ] [ Google Scholar ]
- Gowen K, Deschaine M, Gruttadara D, & Markey D (2012). Young adults with mental health conditions and social networking websites: seeking tools to build community . Psychiatric rehabilitation journal , 35 ( 3 ), 245–250. [ PubMed ] [ Google Scholar ]
- Guntuku SC, Yaden DB, Kern ML, Ungar LH, & Eichstaedt JC (2017). Detecting depression and mental illness on social media: an integrative review . Current Opinion in Behavioral Sciences , 18 , 43–49. [ Google Scholar ]
- Haker EL, Lauber C, & Rossler W (2005). Internet forums: a self - help approach for individuals with schizophrenia? Acta Psychiatrica Scandinavica , 112 ( 6 ), 474–477. [ PubMed ] [ Google Scholar ]
- Hamm MP, Newton AS, Chisholm A, Shulhan J, Milne A, Sundar P, … Hartling L (2015). Prevalence and effect of cyberbullying on children and young people: A scoping review of social media studies . JAMA pediatrics , 769 ( 8 ), 770–777. [ PubMed ] [ Google Scholar ]
- Hansen CF, Torgalsboen A-K, Melle I, & Bell MD (2009). Passive/apathetic social withdrawal and active social avoidance in schizophrenia: difference in underlying psychological processes . The Journal of nervous and mental disease , 197 ( 4 ), 274–277. [ PubMed ] [ Google Scholar ]
- Highton-Williamson E, Priebe S, & Giacco D (2015). Online social networking in people with psychosis: a systematic review . International Journal of Social Psychiatry , 61 ( 1 ), 92–101. [ PubMed ] [ Google Scholar ]
- Hilty DM, Chan S, Torous J, Luo J, & Boland RJ (2019). Mobile health, smartphone/device, and apps for psychiatry and medicine: competencies, training, and faculty development issues . Psychiatric Clinics , 42 ( 2 ), 513–534. [ PubMed ] [ Google Scholar ]
- Hswen Y, Naslund JA, Brownstein JS, & Hawkins JB (2018a). Monitoring online discussions about suicide among Twitter users with schizophrenia: exploratory study . JMIR mental health , 5 ( 4 ), e11483. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Hswen Y, Naslund JA, Brownstein JS, & Hawkins JB (2018b). Online communication about depression and anxiety among twitter users with schizophrenia: preliminary findings to inform a digital phenotype using social media . Psychiatric Quarterly , 89 ( 3 ), 569–580. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Hswen Y, Naslund JA, Chandrashekar P, Siegel R, Brownstein JS, & Hawkins JB (2017). Exploring online communication about cigarette smoking among Twitter users who self-identify as having schizophrenia . Psychiatry research , 257 , 479–484. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Indian M, & Grieve R (2014). When Facebook is easier than face-to-face: social support dervied from Facebook in socially anxious individuals . Personality and Individual Differences , 59 , 102–106. [ Google Scholar ]
- Jain SH, Powers BW, Hawkins JB, & Brownstein JS (2015). The digital phenotype . Nature Biotechnology , 33 ( 5 ), 462. [ PubMed ] [ Google Scholar ]
- Kiesler S, Siegel J, & McGuire TW (1984). Social psychological aspects of computer-mediated communication . American Psychologist , 39 , 1123–1134. [ Google Scholar ]
- Kross E, Verduyn P, Demiralp E, Park J, Lee DS, Lin N, … Ybarra O (2013). Facebook use predicts declines in subjective well-being in young adults . PloS one , 5 ( 8 ), e69841. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Lai S, Nguyen V, & Theriault J (2018). Seeking mental health information and support online: experiences and perspectives of young people receiving treatment for first - episode psychosis . Early intervention in psychiatry , 72 ( 3 ), 324–330. [ PubMed ] [ Google Scholar ]
- Lin LY, Sidani JE, Shensa A, Radovic A, Miller E, Colditz JB, … Primack BA (2016). Association between social media use and depression among US young adults . Depression and anxiety , 22 ( 4 ), 323–331. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Machmutow K, Perren S, Sticca F, & Alsaker FD (2012). Peer victimisation and depressive symptoms: can specific coping strategies buffer the negative impact of cybervictimisation? Emotional and Behavioural Difficulties , 17 ( 3-4 ), 403–420. [ Google Scholar ]
- Manikonda L, & De Choudhury M (2017). Modeling and understanding visual attributes of mental health disclosures in social media . Paper presented at the Proceedings of the 2017 CHI Conference on Human Factors in Computing Systems. [ Google Scholar ]
- Mead S, Hilton D, & Curtis L (2001). Peer support: A theoretical perspective . Psychiatric rehabilitation journal , 25 ( 2 ), 134. [ PubMed ] [ Google Scholar ]
- Mereish EH, Sheskier M, Hawthorne DJ, & Goldbach JT (2019). Sexual orientation disparities in mental health and substance use among Black American young people in the USA: effects of cyber and bias-based victimisation . Culture, health & sexuality , 21 ( 9 ), 985–998. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Miller BJ, Stewart A, Schrimsher J, Peeples D, & Buckley PF (2015). How connected are people with schizophrenia? Cell phone, computer, email, and social media use . Psychiatry research , 225 ( 3 ), 458–463. [ PubMed ] [ Google Scholar ]
- Mittal VA, Tessner KD, & Walker EF (2007). Elevated social Internet use and schizotypal personality disorder in adolescents . Schizophrenia research , 94 ( 1-3 ), 50–57. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Moorhead SA, Hazlett DE, Harrison L, Carroll JK, Irwin A, & Hoving C (2013). A new dimension of health care: systematic review of the uses, benefits, and limitations of social media for health communication . Journal of medical Internet research , 15 ( 4 ), e85. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Naslund JA, & Aschbrenner KA (2019). Risks to privacy with use of social media: understanding the views of social media users with serious mental illness . Psychiatric Services , appi. ps. 201800520. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Naslund JA, Aschbrenner KA, & Bartels SJ (2016). How people living with serious mental illness use smartphones, mobile apps, and social media . Psychiatric rehabilitation journal , 39 ( 4 ), 364–367. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Naslund JA, Aschbrenner KA, Marsch LA, & Bartels SJ (2016a). Feasibility and acceptability of Facebook for health promotion among people with serious mental illness . Digital health , 2 , 2055207616654822. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Naslund JA, Aschbrenner KA, Marsch LA, & Bartels SJ (2016b). The future of mental health care: peer-to-peer support and social media . Epidemiology and Psychiatric Sciences , 25 ( 2 ), 113–122. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Naslund JA, Aschbrenner KA, Marsch LA, McHugo GJ, & Bartels SJ (2018). Facebook for supporting a lifestyle intervention for people with major depressive disorder, bipolar disorder, and schizophrenia: an exploratory study . Psychiatric Quarterly , 59 ( 1 ), 81–94. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Naslund JA, Aschbrenner KA, McHugo GJ, Unutzer J, Marsch LA, & Bartels SJ (2017). Exploring opportunities to support mental health care using social media: A survey of social media users with mental illness . Early intervention in psychiatry . [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Naslund JA, Gonsalves PP, Gruebner O, Pendse SR, Smith SL, Sharma A, & Raviola G (2019). Digital innovations for global mental health: opportunities for data science, task sharing, and early intervention . Current Treatment Options in Psychiatry , 1–15. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Naslund JA, Grande SW, Aschbrenner KA, & Elwyn G (2014). Naturally occurring peer support through social media: the experiences of individuals with severe mental illness using YouTube . PloS one , 9 ( 10 ), e110171. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Onnela J-P, & Rauch SL (2016). Harnessing smartphone-based digital phenotyping to enhance behavioral and mental health . Neuropsychopharmacology , 41 ( 7 ), 1691. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Orben A, & Przybylski AK (2019). The association between adolescent well-being and digital technology use . Nature Human Behaviour , 3 ( 2 ), 173. [ PubMed ] [ Google Scholar ]
- Patel V, Saxena S, Lund C, Thornicroft G, Baingana F, Bolton P, … Eaton J (2018). The Lancet Commission on global mental health and sustainable development . The Lancet . [ PubMed ] [ Google Scholar ]
- Primack BA, Shensa A, Escobar-Viera CG, Barrett EL, Sidani JE, Colditz JB, & James AE (2017). Use of multiple social media platforms and symptoms of depression and anxiety: A nationally-representative study among US young adults . Computers in Human Behavior , 69 , 1–9. [ Google Scholar ]
- Reece AG, & Danforth CM (2017). Instagram photos reveal predictive markers of depression . EPJ Data Science , 6 ( 1 ), 15. [ Google Scholar ]
- Reece AG, Reagan AJ, Lix KL, Dodds PS, Danforth CM, & Langer EJ (2017). Forecasting the onset and course of mental illness with Twitter data . Scientific reports , 7 ( 1 ), 13006. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Rideout V, & Fox S (2018). Digital health practices, social media use, and mental well-being among teens and young adults in the U.S Retrieved from San Francisco, CA: https://www.hopelab.org/reports/pdf/a-national-survey-by-hopelab-and-well-being-trust-2018.pdf [ Google Scholar ]
- Saha K, Torous J, Ernala SK, Rizuto C, Stafford A, & De Choudhury M (2019). A computational study of mental health awareness campaigns on social media . Translational behavioral medicine . [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Schlosser DA, Campellone T, Kim D, Truong B, Vergani S, Ward C, & Vinogradov S (2016). Feasibility of PRIME: a cognitive neuroscience-informed mobile app intervention to enhance motivated behavior and improve quality of life in recent onset schizophrenia . JMIR research protocols , 5 ( 2 ). [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Schlosser DA, Campellone TR, Truong B, Etter K, Vergani S, Komaiko K, & Vinogradov S (2018). Efficacy of PRIME, a mobile app intervention designed to improve motivation in young people with schizophrenia . Schizophrenia bulletin , 44 ( 5 ), 1010–1020. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Schrank B, Sibitz I, Unger A, & Amering M (2010). How patients with schizophrenia use the internet: qualitative study . Journal of medical Internet research , 12 ( 5 ), e70. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Schueller SM, Hunter JF, Figueroa C, & Aguilera A (2019). Use of digital mental health for marginalized and underserved populations . Current Treatment Options in Psychiatry , 6 ( 3 ), 243–255. [ Google Scholar ]
- Shatte AB, Hutchinson DM, & Teague SJ (2019). Machine learning in mental health: a scoping review of methods and applications . Psychological medicine , 49 ( 9 ), 1426–1448. [ PubMed ] [ Google Scholar ]
- Spinzy Y, Nitzan U, Becker G, Bloch Y, & Fennig S (2012). Does the Internet offer social opportunities for individuals with schizophrenia? a cross-sectional pilot study . Psychiatry research , 198 ( 2 ), 319–320. [ PubMed ] [ Google Scholar ]
- Stiglic N, & Viner RM (2019). Effects of screentime on the health and well-being of children and adolescents: a systematic review of reviews . BMJopen , 9 ( 1 ), e023191. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Sumner SA, Galik S, Mathieu J, Ward M, Kiley T, Bartholow B, … Mork P (2019). Temporal and geographic patterns of social media posts about an emerging suicide game . Journal of Adolescent Health . [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Torous J, Chan SR, Tan SY-M, Behrens J, Mathew I, Conrad EJ, … Keshavan M (2014). Patient smartphone ownership and interest in mobile apps to monitor symptoms of mental health conditions: a survey in four geographically distinct psychiatric clinics . JMIR mental health , 1 ( 1 ), e5. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Torous J, Friedman R, & Keshavan M (2014). Smartphone ownership and interest in mobile applications to monitor symptoms of mental health conditions . JMIR mHealth and uHealth , 2 ( 1 ), e2. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Torous J, & Keshavan M (2016). The role of social media in schizophrenia: evaluating risks, benefits, and potential . Current opinion in psychiatry , 29 ( 3 ), 190–195. [ PubMed ] [ Google Scholar ]
- Torous J, Wisniewski H, Bird B, Carpenter E, David G, Elejalde E, … Henson P (2019). Creating a digital health smartphone app and digital phenotyping platform for mental health and diverse healthcare needs: an interdisciplinary and collaborative approach . Journal of Technology in Behavioral Science , 1–13. [ Google Scholar ]
- Trefflich F, Kalckreuth S, Mergl R, & Rummel-Kluge C (2015). Psychiatric patients’ internet use corresponds to the internet use of the general public . Psychiatry research , 226 , 136–141. [ PubMed ] [ Google Scholar ]
- Twenge JM, & Campbell WK (2018). Associations between screen time and lower psychological well-being among children and adolescents: Evidence from a population-based study . Preventive medicine reports , 12 , 271–283. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Twenge JM, Joiner TE, Rogers ML, & Martin GN (2018). Increases in depressive symptoms, suicide-related outcomes, and suicide rates among US adolescents after 2010 and links to increased new media screen time . Clinical Psychological Science , 6 ( 1 ), 3–17. [ Google Scholar ]
- Tynes BM, Willis HA, Stewart AM, & Hamilton MW (2019). Race-related traumatic events online and mental health among adolescents of color . Journal of Adolescent Health , 65 ( 3 ), 371–377. [ PubMed ] [ Google Scholar ]
- Vannucci A, Flannery KM, & Ohannessian CM (2017). Social media use and anxiety in emerging adults . Journal of affective disorders , 207 , 163–166. [ PubMed ] [ Google Scholar ]
- Vayreda A, & Antaki C (2009). Social support and unsolicited advice in a bipolar disorder online forum . Qualitative health research , 19 ( 7 ), 931–942. [ PubMed ] [ Google Scholar ]
- Ventola CL (2014). Social media and health care professionals: benefits, risks, and best practices . Pharmacy and Therapeutics , 39 ( 7 ), 491. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- We Are Social. (2020). Digital in 2020 . Retrieved from https://wearesocial.com/global-digital-report-2019
- Webb H, Jirotka M, Stahl BC, Housley W, Edwards A, Williams M, … Burnap P (2017). The ethical challenges of publishing Twitter data for research dissemination . Paper presented at the Proceedings of the 2017 ACM on Web Science Conference. [ Google Scholar ]
- Williams ML, Burnap P, & Sloan L (2017). Towards an ethical framework for publishing Twitter data in social research: Taking into account users’ views, online context and algorithmic estimation . Sociology , 57 ( 6 ), 1149–1168. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Woods HC, & Scott H (2016). # Sleepyteens: Social media use in adolescence is associated with poor sleep quality, anxiety, depression and low self-esteem . Journal of adolescence , 57 , 41–49. [ PubMed ] [ Google Scholar ]
- Ybarra ML (2004). Linkages between depressive symptomatology and Internet harassment among young regular Internet users . Cyber Psychology & Behavior , 7 ( 2 ), 247–257. [ PubMed ] [ Google Scholar ]

IMAGES
VIDEO
COMMENTS
This essay about the complex relationship between technology and mental health in modern society. It explores both the positive and negative impacts of technology on mental well-being, highlighting how social media can foster feelings of inadequacy while also discussing the benefits of telemedicine and mental health apps.
Background: Research increasingly shows how selective and targeted use of technology within care and welfare can have several advantages including improved quality of care and active user involvement. Purpose: The current overview of reviews aims to summarize the research on the effectiveness of technology for mental health and wellbeing. The goal is to highlight and structure the diverse ...
Debating digital-technology use and teenage mental health. ... but it is not films or video chats with friends that damage mental health. When research papers allow us to zoom in on social media, ...
The general public is also more receptive to technology's expanded role in mental health care. "The pandemic has created a lasting relationship between technology, and it has helped increase access to mental health services across the world," says McKinley. "There are lots of people seeking help who would not have done so prior to the ...
Between 2009 and 2015, the National Institute of Mental Health awarded more than 400 grants totaling $445 million for technology-enhanced mental-health interventions to further investigate roles for technology in preventing and treating mental disorders. 55 Investigators have studied the efficacy of various online mental health interventions.
Technology has opened a new frontier in mental health care and data collection. Mobile devices like cell phones, smartphones, and tablets are giving the public, health care providers, and researchers new ways to access help, monitor progress, and increase understanding of mental well-being. Mobile mental health support can be very simple but ...
Introduction: state of the art and beyond in digital mental health, and current challenges. New innovations, such as digital phenotyping and apps as prevention and treatment interventions, hold tremendous potential in mental health.1 However, emerging evidence suggests the need for high-quality validation, real-world clinical outcomes, implementation data and a clear vision to ensure such ...
1. Introduction. The psychological treatment of mental health problems is beginning to undergo a fundamental change. This change is being driven by the widespread availability of "digital technology" by which we mean computers, the internet, mobile devices such as smartphones, and mobile software applications (apps).
The promise of digital, mobile, and connected technologies to advance mental health, and especially psychiatric rehabilitation, continues to rapidly evolve.In 2017, 77% of Americans owned a smartphone, and by 2020 there will be 6 billion in use across the globe (Poushter, 2017).But unlike the rapid proliferation of digital technology, the worldwide shortage of mental health clinicians is ...
In another study recently conducted by Statistics Canada, which examined data on mental health in adolescents aged 12 to 17 from the 2019 Canadian Health Survey on Children and Youth, video game use by girls was found to be associated with lower self-reported mental health, even when controlling for other factors.
The Impact of Technology on Mental Health. August 2019. DOI: 10.1201/9780429325632-4. In book: Electrical Brain Stimulation for the Treatment of Neurological Disorders (pp.353-402) Authors: Bahman ...
Inventing the Future of Mental Health Care. Technology is not a panacea. Effectively treating mental illness and delivering mental health services are complex and multifaceted challenges. New technology may offer us some novel solutions. We now have the capacity to engage with people digitally, in real time and in real place.
The demand for technological forms of mental health support has grown in recent years. In the UK, the number of people searching for mental health apps increased substantially during the COVID-19 pandemic.9 Investment in mental health technology is also rising. Global funding for mental health tech start-ups reached $5.5 billion in 2021.10 ...
Bowers, Hitt, Hoeft, and Dunn (2003), modified Kirk-. patrick's (1959a, 1959b, 1960a, 1960b, 1976) training. model for application to clinical settings. Training in. the area of mental health is ...
Introduction. The current coronavirus 2019 (COVID-19) pandemic not only poses a large threat to the physical health of our population, if we fail to act now, it will also have detrimental long-term consequences for mental health. Though social distancing is a crucial intervention to slow down the destructive effects of the pandemic, it can lead ...
The impact of technology has extended into the realm of health care, and it is clear that technology also is making positive changes in terms of mental health care. Research has indicated, however, that the very tools that can help alleviate mental health issues, such as smartphone apps, may be linked with the experience of mental health ...
Journal of Technology in Behavioral Science - In 2020, there are an estimated 3.8 billion social media users worldwide, representing half the global population (We Are Social 2020).Recent studies have shown that individuals with mental disorders are increasingly gaining access to and using mobile devices, such as smartphones (Firth et al. 2015; Glick et al. 2016; Torous et al. 2014a, b).
Background: Digital mental health technologies (DMHTs) have the potential to enhance mental health care delivery. However, there is little information on how DMHTs are evaluated and what factors influence their use. Objective: A systematic literature review was conducted to understand how DMHTs are valued in the United States from user, payer, and employer perspectives.
Gordon et al. (2007) mention that technology use is triggered by self-expression, consumptive motives, and sharing information. In this study, Gordon et al. (2007) posit that frequency of internet use does not affect mental illness. Instead, they mention that what students do on those platforms is the factor that contributes to mental illness.
Abstract. The growing presence of online mutual-help communities has significantly changed how people access and provide mental health support. While extensive research has explored self-disclosure and social support dynamics within these communities, less is known about users' distinctive behavioral patterns, posting intents, and community response.
Abstract. Social media are responsible for aggravating mental health problems. This systematic study summarizes the effects of social network usage on mental health. Fifty papers were shortlisted from google scholar databases, and after the application of various inclusion and exclusion criteria, 16 papers were chosen and all papers were ...
Here is the short and simple 10-line on technology and mental health. The constant connectivity with overloaded information through various technical gadgets can lead to stress and anxiety. As a part of technology, social media also contributes to cyberbullying, unrealistic beauty standards,s and the omnipresent fear of missing out.
In recent years, increasing attention has been paid to identifying new approaches to improve workplace well-being and manage stress with the help of m-health solutions. The primary purpose of this review is to provide an overview of the current use of smartphone applications integrated with wearable technologies in stress management and the promotion of well-being in the workplace. A key terms ...
Purpose This paper aims to explore how the term "mental health literacy" (MHL) is defined and understand the implications for public mental health and educational interventions. Design/methodology/approach An extensive search was conducted by searching PubMed, ERIC, PsycINFO, Scopus and Web of Science. Keywords such as "mental health literacy" and "definition" were used. The ...
Rates of mental ill health among young people are on the rise. Between the years 2020 and 2022, 39% of Australians aged 16 to 24 had a mental disorder in the previous year, compared to 26% in that ...
The mental health services now in place are intrinsically linked with the technology that has been at our disposal for decades of research and practice. Advancements in Web, mobile, sensor, and informatics technology can do more than serve as tools to enhance existing models of care. Novel technologies can help us better understand the very nature of mental illness and revise our fundamental ...
We're the national information and technology partner to the health and social care system using digital technology to transform the NHS and social care. ... Excess Under 75 Mortality Rates in Adults With Serious Mental Illness, 2021 to 2023. Experimental statistics, Official statistics in development Publication Date: Dec 2024 ...
Providers that advertise their services to address mental-health concerns but that do not value, respect or understand the role of science in mental-health care risk compromising the safety of ...
The rapid expansion of information technology and the intensification of population aging are two prominent features of contemporary societal development. Investigating older adults' acceptance ...
Social Media Use and Mental Health. In 2020, there are an estimated 3.8 billion social media users worldwide, representing half the global population (We Are Social, 2020).Recent studies have shown that individuals with mental disorders are increasingly gaining access to and using mobile devices, such as smartphones (Firth et al., 2015; Glick, Druss, Pina, Lally, & Conde, 2016; Torous, Chan ...