
- Feature Article
- Developmental Biology

Meta-Research: The need for more research into reproductive health and disease
- Natalie D Mercuri
- Department of Physiology, University of Toronto, Canada ;
- Open access
- Copyright information
- Comment Open annotations (there are currently 0 annotations on this page).
- 2,512 views
- 164 downloads
- 5 citations
Share this article
Cite this article.
- Brian J Cox
- Copy to clipboard
- Download BibTeX
- Download .RIS
- Figures and data
Introduction
Conclusions, data availability, decision letter, author response, article and author information.
Reproductive diseases have a significant impact on human health, especially on women’s health: endometriosis affects 10% of all reproductive-aged women but is often undiagnosed for many years, and preeclampsia claims over 70,000 maternal and 500,000 neonatal lives every year. Infertility rates are also rising. However, relatively few new treatments or diagnostics for reproductive diseases have emerged in recent decades. Here, based on analyses of PubMed, we report that the number of research articles published on non-reproductive organs is 4.5 times higher than the number published on reproductive organs. Moreover, for the two most-researched reproductive organs (breast and prostate), the focus is on non-reproductive diseases such as cancer. Further, analyses of grant databases maintained by the Canadian Institutes of Health Research and the National Institutes of Health in the United States show that the number of grants for research on non-reproductive organs is 6–7 times higher than the number for reproductive organs. Our results suggest that there are too few researchers working in the field of reproductive health and disease, and that funders, educators and the research community must take action to combat this longstanding disregard for reproductive science.
It is difficult to overstate the impact of reproductive disease. Adverse pregnancy outcomes – which include preterm delivery, low birth weight, hypertensive disorders, and gestational diabetes –impact the acute and chronic health of the population ( Barker, 1997 ; Williams, 2011 ; Lewis et al., 2012 ). About 20% of all pregnancies require medical intervention ( Murray and Lopez, 1998 ), and in lower resource settings, pregnancy and delivery complications are a leading cause of maternal and neonatal death ( WHO, 2019 ).
In 1992, the Institute of Medicine in the United States published a report called Strengthening Research in Academic OB-GYN Departments that outlined areas of research with obstetrics and gynecology where improvements were needed, such as low-birth-weight infants, fertility complications, and pregnancy-induced hypertension ( Institute of Medicine, 1992 ). Three decades later, despite the essential nature and impact of the reproductive system, these issues are still major challenges in reproductive health.
Gender inequality and bias have been issues since the onset of biological and medical research. For example, including women as subjects in clinical research was not standard practice until after 1986 ( Liu and Mager, 2016 ). There has been progress in developing policies to increase the representation of women (as both subjects and researchers) and in providing education on gender inequality for all researchers, but women are still underrepresented in scientific and medical research ( Huang et al., 2020 ).
There are a variety of stigmas and taboos surrounding any topic relating to reproductive function. Menstruation is one function that has faced stigmatization that persists today ( Litman, 2018 ; Pickering, 2019 ), with women often feeling too embarrassed to talk about this natural process or even complete an essential task, such as purchasing menstrual products at a local store. Political power highly affects reproductive health care and rights over other biological processes. In many countries, ongoing political and legal battles directly affect access to safe reproductive health care, including contraception, safe abortion, and gender identity rights ( Pugh, 2019 ). There are parallels between the low level of research into reproductive diseases and the response to the AIDS epidemic in the 1980s. The long delay in recognizing AIDS as a significant health issue, and then implementing research policies, perpetuated false ideas surrounding the lifestyles of those affected by the disease and created a barrier to expanding sexual education and seeking healthcare, likely costing many lives ( Francis, 2012 ). Despite great advances in AIDS research and treatment, including social awareness, public health stigma still lingers in society ( Turan et al., 2017 ). Similar increases in advocacy and public awareness are needed to overcome these barriers affecting reproductive health.
Reproductive pathologies are often challenging to diagnose and properly treat, which increases the risk of comorbidity development. Moreover, a long-standing lack of research into reproductive health and disease means that the acute and chronic healthcare burden caused by reproductive pathologies is likely to continue increasing. This lack of research likely results from historic and ongoing systemic biases against female-focused research, and from political and legal challenges to female reproductive health ( Coen-Sanchez et al., 2022 ). In this exploratory analysis we seek to understand the “research gap” between reproductive health and disease and other areas of medical research, and to suggest ways of closing this gap.
Comparing numbers of publications
To benchmark research on reproductive health and disease, we used the PubMed database to compare the number of articles published on seven reproductive organs and seven non-reproductive organs between 1966 and 2021 ( Table 1 ). While the reproductive organs are not essential to postnatal life, we posit that the placenta and the uterus are as essential to fetal survival in utero as the lungs and the heart are to postnatal survival after birth. Our analysis revealed that the average number of articles on non-reproductive organs was 4.5 times higher than the number on reproductive organs (and ranged between about 2 and 20 in pairwise comparisons). The reproductive organs with the most publications were the breast and prostate.
Total number of matching articles from PubMed for seven non-reproductive keywords and seven reproductive keywords for the period 1966–2021.
| Keyword | Total matching articles |
|---|---|
| Non-reproductive keywords | |
| 1,058,995 | |
| 851,955 | |
| 834,006 | |
| 652,797 | |
| 451,177 | |
| 120,034 | |
| 99,772 | |
| Reproductive keywords | |
| 464,629 | |
| 197,736 | |
| 83,971 | |
| 57,076 | |
| 55,971 | |
| 32,344 | |
| 15,019 | |
The research landscape can change over time and efforts to reduce gender bias in research might have had an impact on the volume of reproductive research, so we plotted the number of publications on the 14 organs as a function year between 1966 and 2021 ( Figure 1A ). Breast and prostate were the only reproductive organs to increase in publication at a rate similar to the kidney; the second least studied non-reproductive organ in our list. The intestine was the only non-reproductive organ to show similar publication rates to the other five reproductive organs. To investigate further, we compared disease-driven research versus research not related to disease.
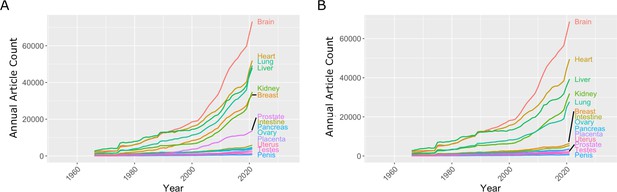
Number of articles published every year on seven reproductive organs and seven non-reproductive organs.
( A ) The number of articles published on most of the non-reproductive organs (including the brain, heart, lung and liver) has increased more rapidly than the number of articles published on the reproductive organs. ( B ) Removing articles that contain the keyword cancer has relatively little effect on the number of articles for non-reproductive organs (with the exception of the lung), but has a significant impact on the number of articles for the two reproductive organs with the most articles: the breast and prostate. Data extracted from PubMed using organ-specific keyword searches for the period 1966–2021.
Figure 1—source data 1
Articles per year for reproductive and non-reproductive organs, with and without the keyword cancer.
Comparing research related to disease and research not related to disease
In the 1970s, the National Institutes of Health (NIH) initiated a war on cancer, and the breast and prostate are both associated with sex-specific cancers. We reassessed publication data with the added search parameter "NOT cancer" to eliminate cancer-based research ( Figure 1B ). We observed a reduction of approximately 20% for most non-reproductive organs; however, the reduction for publication on the breast and prostate was about 80%, suggesting that most research on these organs is driven by an interest in cancer research rather than reproductive health and disease ( Figure 1B ).
Then, for each organ, we plotted the number of publications related to disease on the vertical axis, and the number not related to disease on the horizontal axis, which revealed a high degree of variation among the organs ( Figure 2 ). For three non-reproductive organs (brain, heart, and liver) the number of publications not related to disease was almost three times as high as the number related to disease, and for two non-reproductive organs (kidney and lung) the numbers were similar. For the breast and prostate, on the other hand, the number of publications related to disease was three times as high as the number not related to disease. For the five remaining reproductive organs, and also for the intestine and pancreas, the number of publications not related to disease was about twice as high as the number related to disease (although the total number of publications for these seven organs was about an order of magnitude lower than the number for the other seven organs).
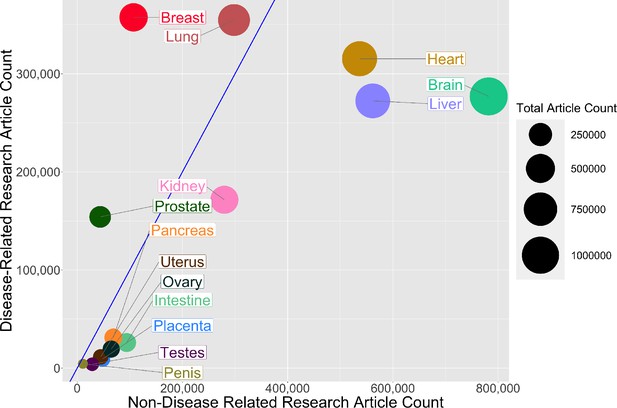
Comparing research related to disease and research not related to disease for reproductive and non-reproductive organs.
For each organ (colored circles) the vertical axis shows the number of publications for the period 1966–2021 related to disease, and the horizontal axis shows the number not related to disease: the area of the circle is proportional to the total number of publications. The straight blue line corresponds to equal numbers of disease-related and non-disease-related publications, so organs to the right of this line (notably non-reproductive organs such as the brain, heart and liver) tend to be the subject of more basic or non-disease-related research, whereas organs to the left of this line (notably reproductive organs such as the breast and prostate) tend to be the subject of disease-related research. The lung is the only non-reproductive organ in our sample to the left of the blue line.
Figure 2—source data 1
Total number of articles on research related to disease and research not related to disease for reproductive and non-reproductive organs.
Research funding
Next we used databases belonging to the Canadian Institutes of Health Research (CIHR) and the NIH to investigate funding trends for the different organs. The 14 keywords (brain, heart, liver, lung, kidney, intestine, pancreas, breast, prostate, ovary, uterus, penis, testes, and placenta) were entered into each database, and we extracted funding data for the period between 2013 and 2018. These organs were chosen as keywords to investigate the funding related to a basic understanding of the biology of these organs. Although grants that relate to pregnancy or fertility may not be captured, these topics are much broader and would introduce subtopics outside of the reproductive scope, similar to using keywords such as metabolism or behaviour. Table 2 gives the number of projects for each keyword and the corresponding average funding amount per grant for the CIHR, and the same for the NIH. Our analysis found that the mean grant amounts for the CIHR and NIH are similar between different keyword research topics (CIHR: $ 370 000 ± $ 50 000; NIH: $ 481 500 ± $ 50 000). The similar funding amounts between different organs are encouraging and may result from standard funding guidelines for biomedical research. However, our analysis found that the average number of funded projects is much higher for non-reproductive organs compared to reproductive organs for both the CIHR (800 vs 115) and the NIH (31 000 vs 5 300).
Total number of projects funded and average grant (in Canadian or US dollars) for the Canadian Institutes of Health Research (columns 2 and 3) and the US National Institutes of Health (columns 4 and 5) for the years 2013–2018 for seven non-reproductive keywords and seven reproductive keywords (column 1).
| Keyword | Number of projects (CIHR) | Average grant funded (CAD) | Number of projects(NIH) | Average grant funded(USD) |
|---|---|---|---|---|
| Non-reproductive keywords | ||||
| 1686 | $391,023 | 81666 | $441,149 | |
| 1214 | $369,665 | 43833 | $491,993 | |
| 1597 | $314,473 | 22072 | $454,276 | |
| 526 | $371,154 | 34492 | $525,631 | |
| 347 | $424,360 | 21176 | $508,853 | |
| 128 | $444,490 | 5800 | $371,727 | |
| 96 | $491,274 | 8649 | $482,901 | |
| Reproductive keywords | ||||
| 459 | $336,734 | 19132 | $525,134 | |
| 143 | $299,034 | 8960 | $514,638 | |
| 42 | $379,349 | 4814 | $520,804 | |
| 105 | $369,825 | 2169 | $526,147 | |
| 45 | $324,690 | 1356 | $509,250 | |
| 10 | $372,110 | 340 | $500,160 | |
| 1 | $304,676 | 323 | $369,434 | |
Table 2—source data 1
Source data for Table 2 .
Our analysis suggests a bias against research into reproductive health and disease, and it is important that efforts are made to eliminate this bias so that research into reproductive medicine does not fall further behind. The higher levels of research observed for some reproductive organs (notably the breast and prostate) were driven by cancer-focused research, but this has not led to an increase in the level of non-disease-related research on these organs ( Figure 1B ). Factors such as Breast Cancer Awareness Month ( Jacobsen and Jacobsen, 2011 ) and screening programmes for prostate cancer ( Dickinson et al., 2016 ) likely led to the increase in publications about these two reproductive organs.
While our analysis is suggestive that many reproductive organs achieve a good balance of non-disease versus disease-related research, the paucity of research is highly problematic to the field. An important consideration is that a lack of non-disease-related research on reproductive organs may hinder progress in diagnosing and treating a wide range of pathologies (including preeclampsia, polycystic ovary syndrome, and endometriosis).
In a competitive funding system, publications are correlated to successful grants and dollar values awarded. Across research areas, we found that the mean grant dollar amounts per project are similar. However, the numbers of funded research projects on non-reproductive organs were higher than the numbers for reproductive organs by a factor of 6–7 (which is slightly larger than the discrepancy seen in publication rates). An important consideration is that the part of the NIH that supports reproductive research in the US, the National Institute of Child Health and Development, is one of the lowest-funded institutes at the NIH and does not have the word reproduction in its title. In Canada, the Human Development, Child and Youth Health Institute of CIHR is a funder of most pregnancy and reproductive biology grants, typically awarded through the Clinical Investigation – A panel, and it may be that the use of a clinical panel to fund this area of research inhibits non-diseased focused research. This panel is well-funded relative to other panels; however, some research areas (e.g., cardiovascular and neurological research) have more than one panel.
A growing political and societal emphasis is placed on disease-related research, such as cancer. This may arise from a view of basic research as ineffective or inefficient compared to applied research ( Lee, 2019 ). Perhaps this is best seen in our analysis by the high percentage of research publications on the prostate and breast that are due to cancer research, whereas most research on the other reproductive organs we studied was not disease-related. While the placenta and uterus are widely viewed as causal organs for reproductive complications that claim large numbers of maternal and neonatal lives, and treatments cost tens of billions of US dollars every year, there is relatively little disease-related research into these organs. The investigation of cancer biology within a reproductive organ can rely on knowledge of cancer in other organ systems. However, the low levels of research into reproductive organs relative to other organs means that there is much less foundational knowledge to rely on when seeking to develop treatments for diseases of these organs. Moreover, there are fewer researchers who are experienced on working with these organs.
There are several limitations to our approach. One important limitation is that the number of unfunded grant applications is not accessible, so we could not determine if the lower numbers of grants for research on reproductive health and disease were due to proportionally lower total application numbers, or to a bias against reproductive research. Funding bodies should conduct internal analyses to determine appropriate action. The use of keywords to distinguish between non-disease and disease-related research is a limitation, and the relatively low numbers of publications on reproductive organs can also present challenges when making comparisons. However, the differences we observe between research into reproductive and non-reproductive organs (as measured by numbers of publications and levels of funding) are large and are unlikely to result from missing search terms.
How can we address the research gap and enable the field of reproductive health and disease to catch up with other areas of research? Based on our analysis, we need to increase the number of researchers working on reproductive organs and related pathologies. Recent efforts by the NIH, such as the Human Placenta Project ( Guttmacher et al., 2014 ), indicate a recognition of the need to increase research capacity in reproductive sciences, and may lead to further increases in both interest and research capacity in the longer term.
New researchers may avoid the reproductive field due to social and political factors and the research gap (ie, the low levels of grant funding and publications), and this in turn may discourage students and trainees, which will make it even more difficult to increase the size of the research base. While continued advocacy, education, and political lobbying may help to overcome many of the social and political factors, closing the research gap will require other approaches.
To increase researchers and research output, we may learn lessons from the examples of breast and prostate cancer. In both cases, research increased dramatically from a historically low level. While public campaigns played a prominent role in these increases, the existence of a large pool of researchers and trainees already working on other types of cancers was probably more important (as it was these researchers, rather than those doing non-disease-related research on these organs, who did most of the work on breast and prostate cancer). However, this is unlikely to work for preeclampsia and other reproductive pathologies as there are no large pools of existing researchers available to switch the focus of their work.
Therefore, to increase research capacity, we should promote collaborations between researchers working on reproductive health and disease and those working in other areas of physiology and medicine, especially other areas with much higher research capacities. There are plenty of examples that show the benefit of such an integrated approach. For instance, female sex hormones protect against many aging diseases, such as cardiovascular and neurological diseases, leading to the prescription of hormone replacement therapies after menopause in some women ( Paciuc, 2020 ).
Links to immunology, cardiology and other systems can be used to increase research capacity. During pregnancy, there are dramatic changes in maternal physiology, including metabolism, the immune system, and cardio-pulmonary systems, and consequently, these are the same systems affected by reproductive pathologies. Preeclampsia predisposes the mother to a long-term cardiovascular risk of developing peripheral artery disease, coronary artery disease, and congestive heart failure ( Rana et al., 2019 ). Additionally, complications of the liver and kidney are associated with preeclampsia. Polycystic ovary syndrome and endometriosis are related to metabolism problems and the risk of cancer development. Children born from pregnancies affected by preeclampsia or fetal growth restriction are at a 2.5 times higher risk of developing hypertension and require anti-hypertensive medications as adults ( Ferreira et al., 2009 ; Fox et al., 2019 ).
The pathological interaction of reproductive with non-reproductive systems and organs should attract investigators from nephrology, hepatology and cardiovascular research, where the total number of researchers is 10–20 times as high as the number in reproductive health and disease. If just 1% of the researchers in the cardiovascular field were to refocus on pregnancy-related cardiovascular adaptation and pathologies, this would increase reproductive research by 10%.
Our neglect of the placenta and reproductive biology impedes other biomedical research areas. In cancer research, the methylation patterns of tumours look most like those found in the placenta, but why placenta methylation patterns are so unlike all other organs is not known ( Smith et al., 2017 ; Rousseaux et al., 2013 ). In regenerative medicine, the immune-modulating genes used by the placenta ( Szekeres-Bartho, 2002 ) are repurposed to generate universally transplantable stem cells and tissues ( Han et al., 2019 ). A poor understanding of reproductive biology is dangerous, considering emerging diseases that affect pregnancy and fetal development, such as the recent Zika virus outbreak ( Schuler-Faccini et al., 2016 ; Calvet et al., 2016 ). There are likely many other broad benefits to better understanding reproductive biology. The time to act is now, as waiting longer will not improve the situation.
Publication rates
Published research manuscripts were searched in NCBI’s PubMed database ( https://pubmed.ncbi.nlm.nih.gov/ ) between and including the years 1966 and 2021. Keywords for each search pertained to a specific organ or disease and were limited to the title/abstract of the manuscripts. The organs used for these analyses were the brain, heart, liver, lung, kidney, intestine, pancreas, breast, prostate, ovary, uterus, penis, testes, and placenta. We restricted the organ publication timelines to the years 1966–2021 and extracted the annual article count. The organ publication timeline was reconducted with the addition of the search parameter "NOT cancer".
Funding rates
Grant funding data was obtained from the CIHR funding database ( https://webapps.cihr-irsc.gc.ca/funding/Search?p_language=E&p_version=CIHR ) and the NIH reporter tool ( https://reporter.nih.gov ) by searching keywords in the title and abstracts/summary. Keywords used for these searches were brain, heart, liver, lung, kidney, intestine, pancreas, breast, prostate, ovary, uterus, penis, testes, and placenta. The years were restricted to 2013–2018. The total number of projects pertaining to each search term during this period was extracted, and the total amount of funding for those projects was averaged.
All graphs were produced using R (version 4.0.2) in R Studio (version 1.3.1073). R packages used were ggplot2, tidyverse, formattable, gridExtra, RColorBrewer, ggrepel.
All data were obtained from public databases (PubMed/NCBI, NIH and CIHR). Source data files for Figure 1, Figure 2 and Table 2 are available (see figure and table captions for details).
- Google Scholar
- de Filippis I
- de Sequeira PC
- de Mendonça MCL
- de Oliveira L
- Tschoeke DA
- Thompson FL
- Dos Santos FB
- Nogueira RMR
- de Filippis AMB
- Coen-Sanchez K
- El-Mowafi IM
- Idriss-Wheeler D
- Dickinson J
- Connor Gorber S
- Stehouwer CDA
- Lewandowski AJ
- Guttmacher AE
- Ferreira LMR
- Strominger JL
- Meissner TB
- Barabási AL
- Institute of Medicine
- Jacobsen GD
- Jacobsen KH
- Pickering K
- Karumanchi SA
- Rousseaux S
- Debernardi A
- Nagy-Mignotte H
- Moro-Sibilot D
- Brichon P-Y
- Lantuejoul S
- de Reyniès A
- Brambilla C
- Brambilla E
- Schuler-Faccini L
- Feitosa IML
- Horovitz DDG
- Cavalcanti DP
- Doriqui MJR
- Wanderley HYC
- El-Husny AS
- Sanseverino MTV
- Brazilian Medical Genetics Society–Zika Embryopathy Task Force
- Cacchiarelli D
- Szekeres-Bartho J
- Browning WR
- Mugavero MJ
- Peter Rodgers Senior and Reviewing Editor; eLife, United Kingdom
- Marleen van Gelder Reviewer
- James Roberts Reviewer
In the interests of transparency, eLife publishes the most substantive revision requests and the accompanying author responses.
Decision letter after peer review:
Thank you for submitting the paper "A Poor Research Landscape Hinders the Progression of Knowledge and Treatment of Reproductive Diseases" for consideration by eLife . Your article has been reviewed by 3 peer reviewers, and the evaluation has been overseen by a Reviewing Editor and a Senior Editor. The following individuals involved in review of your submission have agreed to reveal their identity: Marleen van Gelder (Reviewer #1); James Roberts (Reviewer #3).
This article will need considerable revision to be suitable for publication as a Feature Article. In particular, you will need to address the concerns raised by the referees (see below), and also address a number of editorial points.
Reviewer #1
In this manuscript, Mercuri and Cox aimed to quantify the advancement of research in reproductive sciences relative to other medical disciplines. They compared two indicators of the research landscape: published research manuscripts and funded projects. The results showed lower publication rates for research on reproductive organs compared to selected non-reproductive organs, in particular concerning basic research. In addition, a relatively small number of grants was funded for projects on diseases with a reproductive focus. Based on these data, the authors concluded that the gap in knowledge and treatment of diseases of the reproductive organs is at least partially caused by a poor research landscape.
Although the conclusions of this paper are somewhat supported by the data, some aspects of the methods and reporting need to be clarified.
[Note: The following point is covered by the queries in the Word version I have sent you]
1) The manuscript, and in particular the Introduction and Discussion sections, could benefit from restructuring, in which adhering to a relevant reporting guideline may be helpful. For example, the authors provide relatively extensive background information on a number of important reproductive health disorders, but the level of detail does not contribute to setting the aim for the study. Moreover, the last paragraph of the introduction section (lines 92-100) already seems to include the conclusion of this paper.
[Note: Please address points b, d and f below. The other points are covered by the queries in the Word version I have sent you]
2) Concerns regarding the methods:
a) Citations in PubMed are known to be selective before 1966; consider using a fixed start date/year for the search.
b) The results strongly depend on the organs and diseases selected to be included in the 'reference group'. Provide a rationale for the selection of organs, which in the current analysis only seem to include major organs that are known to be well-studied, and not organs such as skin, eyes, intestine, pancreas, spleen or urinary bladder. The selection is vital for drawing robust conclusions from the data.
c) The approach to distinguish between basic and applied research is not validated.
d) The prevalence of diseases reported in Figure 4 is highly country-specific, in particular for tuberculosis. Therefore, this comparison may not be suitable for an international audience.
e) The most important limitation of the grant funding data was already mentioned: "the number and keywords of failed grant applications were not accessible" (lines 271-272). Therefore, it is hard to draw conclusions on failure of grant applications on reproductive health.
f) The rationale for the keywords used in the funding databases is missing and likely to yield selective results. Many reproductive health related projects may be missed, as keywords such as pregnancy and subfertility were not included. And also in this search, the selection of keywords for the reference group seems biased.
[Note: Please consider adding a table as suggested below; however, this is optional rather than essential.]
3) To emphasize the lack of knowledge in relation to disease burden, a table summarizing the prevalence, number of publications, and grants could summarize the results.
[Note: This point is covered by the queries in the Word version I have sent you]
4) A number of topics and statements in the Discussion section seem to be unrelated to the aim of this study. Examples include the female representation in STEM disciplines and the correlation between research publications and changes in policy (this was not specifically analyzed and would require additional analyses).
Reviewer #2
[Note: Please address the following point]
While the authors have attempted to be broad in their assessment of reproduction research, they seem to neglect two very broad areas of women's health for which there is little research: menstruation and menopause. Both are only mentioned in the discussion, and referenced with respect to promotion of the study of human physiology. Given the focus on lack of basic understanding of reproductive organs, it may be worth mentioning these, particularly in comparison to the depth of research on erectile dysfunction; this may also help to emphasize the fact that the lack of research in reproduction primarily affects women (though there are of course consequences for men's health, including the period in the womb).
Figure 1: the color code is not clear; Not sure how this could be better represented, but maybe listing the organs from high to low for both parts a and b in the legend? Or magnifying one part of each graph? In particular, the 80% loss of publications in breast/prostate when applying the search term "NOT cancer" does not come through; so perhaps a graph focusing on just these two organs showing the original search and the "NOT cancer" search results would be best?
Tables 2 and 3: It is not clear how this search was done; was the project title or abstract of grants searched for these key terms?
Discussion (including lines 259-260): I'm not sure that the conclusion drawn here is consistent with the data? The authors somewhat confusingly alternate between lack of research in reproduction as a whole vs. lack of basic research in this area.
[Note: Addressing the following point is optional, not essential.]
Another point of discussion that merits mention here is how the lack of interest/emphasis on reproduction research by funding agencies in turn affects the perception of "impact" of such research: i.e. both in terms of how low impact factors of reproduction journals are compared to journals in other fields, but also how the high-impact journals (Cell/Science/Nature) view/receive submissions from researchers in this area. Reviewer #3
The authors propose that research in reproductive areas lags behind that of other areas of biology. They support this with information from publications and funding sources.
This is a presentation of importance to investigators in all fields, funders and the general public. For reproductive investigators it provides objective data to support the lagging of reproductive research and to investigators in other areas of biology and the general public should be an eye opening demonstration of the huge gap between research in reproduction and other areas of biology. One would hope it would also provide a motivation to funders to modify the situation.
The authors remind us of the importance of reproduction on the survival of the species and provide extensive data on specific examples of the impact of reproductive diseases. They then use review of publications keyed to reproductive organs and non-reproductive organs both currently and over time. They point out that research on non-reproductive organs is 5 to 20 times more frequent than that on reproductive organs. [Note: Please address the point made in the following sentence] They should make it clearer that this is referring to specific organs and not a comparison sum of research on all organs of reproduction and not reproduction. They show that over time this discrepancy has increased with the exception of prostate, and breast research but even with those it is evident this is research related specifically to cancer and not normal organ function.
They make a slightly less compelling comparison on the portion of research devoted to basic understanding or clinical research which for nonreproductive organs is considerably more for basic science than in reproductive organs. [Note: Please address the point made in the following sentence] However, this is likely compromised by the relative minute number of either type of studies in reproduction.
They then make comparisons between the impact of specific reproductive topics and publications. They state that although preeclampsia and breast cancer have a similar prevalence the number of breast cancer publications are much higher. [Note: Please address the point made in the following sentence] To me the comparison of a disorder with high mortality (breast cancer) and far lower mortality (preeclampsia) does not provide a compelling argument and also is a little off target for comparing reproductive and nonreproductive research.
[Note: Please address the point made in the following paragraph]
They make a similar comparison of PCOS a reproductive disorder with other non-reproductive disorders of similar or lower prevalence, autism, tuberculosis, Crohn's Disease and Lupus with a much lower publication rate for PCOS. Again, this seems a bit of comparing apples and oranges.
They investigate the relative funding of research on these topics in the US and Canada and find that the size of individual grants for reproductive and non-reproductive research in both countries is similar but that the number of funded grants for specific non-reproductive organs is, that like that of publications, is about 2 to 20 times higher for nonreproductive organs.
The authors present their conclusions of the reason for the discrepancy. They point out gender bias which has been a target for improvement for several years and has been reduced but research is still not on an equal basis for men and women. However, the bias goes beyond gender since male reproductive research publications and funding also lags. They conclude that there is a general bias against reproductive research. [Note: Please consider mentioning the following point in your article] Interestingly they do not cite a major support for this conclusion, that the major NIH institute supporting reproductive research, the National Institute of Child Health and Development (NICHD)is one lowest funded institutes and does not have reproduction in its title.
They provide two general suggestions to increase reproductive research. The first is to increase funding and the second to involve other forms of research in studies supporting the role of reproductive disorders and physiology in non-reproductive studies. [Note: Please address the point made in the rest of this paragraph] They point out the relationship of preeclampsia to later life cardiovascular disease as an example of this. Unfortunately, they state this relationship as causal which has not been established. Nonetheless studying preeclampsia will likely provide information useful to cardiovascular health.
It is possible that linking publications and funding amounts to conclusions about bias against reproductive research is not precise. However, the magnitude of the differences strongly supports the authors' premise.
This interesting presentation makes and important point about the fact that reproductive research lags beyond other biological research. They do this through the use of publication and grant funding reviews. The differences are large in a direction that support the point they are making. There are some suggestions that I believe would improve the presentation.
[Note: Please address the following three points]
1. There should be a bit more discussion of the limitations of their approach.
2. In the comparisons of disorders of reproduction and non-reproduction they should indicate the limitations of comparing very different disorders.
3. Preeclampsia as a cause of later life CVD has not been established. They are related.
Reviewer #1 In this manuscript, Mercuri and Cox aimed to quantify the advancement of research in reproductive sciences relative to other medical disciplines. They compared two indicators of the research landscape: published research manuscripts and funded projects. The results showed lower publication rates for research on reproductive organs compared to selected non-reproductive organs, in particular concerning basic research. In addition, a relatively small number of grants was funded for projects on diseases with a reproductive focus. Based on these data, the authors concluded that the gap in knowledge and treatment of diseases of the reproductive organs is at least partially caused by a poor research landscape. Although the conclusions of this paper are somewhat supported by the data, some aspects of the methods and reporting need to be clarified. [Note: The following point is covered by the queries in the Word version I have sent you] 1) The manuscript, and in particular the Introduction and Discussion sections, could benefit from restructuring, in which adhering to a relevant reporting guideline may be helpful. For example, the authors provide relatively extensive background information on a number of important reproductive health disorders, but the level of detail does not contribute to setting the aim for the study. Moreover, the last paragraph of the introduction section (lines 92-100) already seems to include the conclusion of this paper.
This query has been responded to the in Word file
[Note: Please address points b, d and f below. The other points are covered by the queries in the Word version I have sent you] 2) Concerns regarding the methods: a) Citations in PubMed are known to be selective before 1966; consider using a fixed start date/year for the search.
This query has been responded to the in Word file. We have now used a fixed date of 1966 as the early timepoint and as indicated in the Word file.
Organs such as brain, heart and lungs are essential for life. The placenta is similarly essential. Other organs such as kidney and liver are also essential but not as immediate. We now include the intestine as a reference point.
Our preliminary analysis found that Skin has over 800,000 publication mentions, but it is not clear if this is the skin organ or a skin on something more work to eliminate background skin hits would be needed. Epidermis has 60,000 hits that are likely more specific, but we did find may abstracts and titles on the skin organ that do not use epidermis. Eyes are nearly 700,000 publications, intestine also over 700,000, pancreas has over 200,000 spleen is also over 200,000 urinary bladder has 130,000, which is similar to the placenta at just over 100,000
This preliminary search seems to still support our conclusion that placenta and reproductive organs are under-researched and only add a list of other organs that are better studied.
Comparisons of diseases has been removed from the manuscript.
We have removed disease focused terms form the search to ensure we capture organ focus research. The inclusion of pregnancy or subfertility would be misleading as it would include disciplines such as sociology and psychology. This is akin to searching for diabetes or metabolism to understand the research landscape on the pancreas.
We felt the separate tables made the information more digestible.
This query has been responded to the in Word file. We have extensively edited and redrafted the Discussion section.
Reviewer #2 [Note: Please address the following point] While the authors have attempted to be broad in their assessment of reproduction research, they seem to neglect two very broad areas of women's health for which there is little research: menstruation and menopause. Both are only mentioned in the discussion, and referenced with respect to promotion of the study of human physiology. Given the focus on lack of basic understanding of reproductive organs, it may be worth mentioning these, particularly in comparison to the depth of research on erectile dysfunction; this may also help to emphasize the fact that the lack of research in reproduction primarily affects women (though there are of course consequences for men's health, including the period in the womb). Figure 1: the color code is not clear; Not sure how this could be better represented, but maybe listing the organs from high to low for both parts a and b in the legend? Or magnifying one part of each graph? In particular, the 80% loss of publications in breast/prostate when applying the search term "NOT cancer" does not come through; so perhaps a graph focusing on just these two organs showing the original search and the "NOT cancer" search results would be best?
These corrections have been made to the in Word file.
We agree and have focused the discussion on the general low level of publications and low level of researchers in the field.
Another point of discussion that merits mention here is how the lack of interest/emphasis on reproduction research by funding agencies in turn affects the perception of "impact" of such research: i.e. both in terms of how low impact factors of reproduction journals are compared to journals in other fields, but also how the high-impact journals (Cell/Science/Nature) view/receive submissions from researchers in this area.
This is an issue many discipline struggle with. A low number of researchers in a field tends to create low levels of impact as measured through citations. Attempts to normalize impact factors and citation rates to the size of the field may help. While we agree with the reviewers comments we cannot address within our study.
Reviewer #3 The authors propose that research in reproductive areas lags behind that of other areas of biology. They support this with information from publications and funding sources. This is a presentation of importance to investigators in all fields, funders and the general public. For reproductive investigators it provides objective data to support the lagging of reproductive research and to investigators in other areas of biology and the general public should be an eye opening demonstration of the huge gap between research in reproduction and other areas of biology. One would hope it would also provide a motivation to funders to modify the situation. The authors remind us of the importance of reproduction on the survival of the species and provide extensive data on specific examples of the impact of reproductive diseases. They then use review of publications keyed to reproductive organs and non-reproductive organs both currently and over time. They point out that research on non-reproductive organs is 5 to 20 times more frequent than that on reproductive organs. [Note: Please address the point made in the following sentence] They should make it clearer that this is referring to specific organs and not a comparison sum of research on all organs of reproduction and not reproduction. They show that over time this discrepancy has increased with the exception of prostate, and breast research but even with those it is evident this is research related specifically to cancer and not normal organ function.
Thank you for this comment. These clarifications have been made to the in Word file.
We agree that the lower level make estimating the ratio of basic to applied very challenging. But there seems to be a tendency to bias to basic research. We made some changes to the results and discussion to acknowledge this challenge.
We agree and have remove the section discussing a comparison of disease prevalence and mortalities. We realize there was no benefit to comparison disease prevalence and severity.
They investigate the relative funding of research on these topics in the US and Canada and find that the size of individual grants for reproductive and non-reproductive research in both countries is similar but that the number of funded grants for specific non-reproductive organs is, that like that of publications, is about 2 to 20 times higher for nonreproductive organs. The authors present their conclusions of the reason for the discrepancy. They point out gender bias which has been a target for improvement for several years and has been reduced but research is still not on an equal basis for men and women. However, the bias goes beyond gender since male reproductive research publications and funding also lags. They conclude that there is a general bias against reproductive research. [Note: Please consider mentioning the following point in your article] Interestingly they do not cite a major support for this conclusion, that the major NIH institute supporting reproductive research, the National Institute of Child Health and Development (NICHD)is one lowest funded institutes and does not have reproduction in its title.
Thank you for this comment, we have added it!
Thank you for the comment, we modified our statement to an observed increased risk of cardiovascular disease, as the risk may be causal or associated as the reviewer stated.
It is possible that linking publications and funding amounts to conclusions about bias against reproductive research is not precise. However, the magnitude of the differences strongly supports the authors' premise. This interesting presentation makes and important point about the fact that reproductive research lags beyond other biological research. They do this through the use of publication and grant funding reviews. The differences are large in a direction that support the point they are making. There are some suggestions that I believe would improve the presentation. 1. There should be a bit more discussion of the limitations of their approach.
We have added more caveats about our approach and interpretation
The comparisons of diseases has been removed.
This is addressed as per the above comment.
Author details
Natalie D Mercuri is in the Department of Physiology, University of Toronto, Toronto, Canada
Contribution
Competing interests.
Brian J Cox is in the Department of Physiology and the Department of Obstetrics and Gynaecology, University of Toronto, Toronto, Canada
For correspondence
University of toronto, canada research chairs.
The funders had no role in study design, data collection and interpretation, or the decision to submit the work for publication.
Acknowledgements
We thank the University of Toronto and the Department of Physiology for providing the opportunity and supporting the completion of this review. We also thank the librarians who offered expert advice on keyword searches of databases.
Publication history
- Received: October 28, 2021
- Preprint posted : November 19, 2021
- Accepted: December 12, 2022
- Accepted Manuscript published : December 13, 2022
- Accepted Manuscript updated : December 13, 2022
- Version of Record published : December 21, 2022
© 2022, Mercuri and Cox
This article is distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use and redistribution provided that the original author and source are credited.
Views, downloads and citations are aggregated across all versions of this paper published by eLife.
Download links
Downloads (link to download the article as pdf).
- Article PDF
Open citations (links to open the citations from this article in various online reference manager services)
Cite this article (links to download the citations from this article in formats compatible with various reference manager tools), categories and tags.
- reproductive biology
- reproductive health
- meta-research
Research organism
- Of interest
FBXO24 deletion causes abnormal accumulation of membraneless electron-dense granules in sperm flagella and male infertility
Further reading.
Ribonucleoprotein (RNP) granules are membraneless electron-dense structures rich in RNAs and proteins, and involved in various cellular processes. Two RNP granules in male germ cells, intermitochondrial cement and the chromatoid body (CB), are associated with PIWI-interacting RNAs (piRNAs) and are required for transposon silencing and spermatogenesis. Other RNP granules in male germ cells, the reticulated body and CB remnants, are also essential for spermiogenesis. In this study, we disrupted FBXO24, a testis-enriched F-box protein, in mice and found numerous membraneless electron-dense granules accumulated in sperm flagella. Fbxo24 knockout (KO) mice exhibited malformed flagellar structures, impaired sperm motility, and male infertility, likely due to the accumulation of abnormal granules. The amount and localization of known RNP granule-related proteins were not disrupted in Fbxo24 KO mice, suggesting that the accumulated granules were distinct from known RNP granules. Further studies revealed that RNAs and two importins, IPO5 and KPNB1, abnormally accumulated in Fbxo24 KO spermatozoa and that FBXO24 could ubiquitinate IPO5. In addition, IPO5 and KPNB1 were recruited to stress granules, RNP complexes, when cells were treated with oxidative stress or a proteasome inhibitor. These results suggest that FBXO24 is involved in the degradation of IPO5, disruption of which may lead to the accumulation of abnormal RNP granules in sperm flagella.
- Cell Biology
Caenorhabditis elegans SEL-5/AAK1 regulates cell migration and cell outgrowth independently of its kinase activity
During Caenorhabditis elegans development, multiple cells migrate long distances or extend processes to reach their final position and/or attain proper shape. The Wnt signalling pathway stands out as one of the major coordinators of cell migration or cell outgrowth along the anterior-posterior body axis. The outcome of Wnt signalling is fine-tuned by various mechanisms including endocytosis. In this study, we show that SEL-5, the C. elegans orthologue of mammalian AP2-associated kinase AAK1, acts together with the retromer complex as a positive regulator of EGL-20/Wnt signalling during the migration of QL neuroblast daughter cells. At the same time, SEL-5 in cooperation with the retromer complex is also required during excretory canal cell outgrowth. Importantly, SEL-5 kinase activity is not required for its role in neuronal migration or excretory cell outgrowth, and neither of these processes is dependent on DPY-23/AP2M1 phosphorylation. We further establish that the Wnt proteins CWN-1 and CWN-2, together with the Frizzled receptor CFZ-2, positively regulate excretory cell outgrowth, while LIN-44/Wnt and LIN-17/Frizzled together generate a stop signal inhibiting its extension.
- Neuroscience
Multiple guidance mechanisms control axon growth to generate precise T-shaped bifurcation during dorsal funiculus development in the spinal cord
The dorsal funiculus in the spinal cord relays somatosensory information to the brain. It is made of T-shaped bifurcation of dorsal root ganglion (DRG) sensory axons. Our previous study has shown that Slit signaling is required for proper guidance during bifurcation, but loss of Slit does not affect all DRG axons. Here, we examined the role of the extracellular molecule Netrin-1 (Ntn1). Using wholemount staining with tissue clearing, we showed that mice lacking Ntn1 had axons escaping from the dorsal funiculus at the time of bifurcation. Genetic labeling confirmed that these misprojecting axons come from DRG neurons. Single axon analysis showed that loss of Ntn1 did not affect bifurcation but rather altered turning angles. To distinguish their guidance functions, we examined mice with triple deletion of Ntn1, Slit1, and Slit2 and found a completely disorganized dorsal funiculus. Comparing mice with different genotypes using immunolabeling and single axon tracing revealed additive guidance errors, demonstrating the independent roles of Ntn1 and Slit. Moreover, the same defects were observed in embryos lacking their cognate receptors. These in vivo studies thus demonstrate the presence of multi-factorial guidance mechanisms that ensure proper formation of a common branched axonal structure during spinal cord development.
Be the first to read new articles from eLife

An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Sex Reprod Health Matters
- v.29(1); 2021
Language: English | French | French
Integrating human rights into sexual and reproductive health research: moving beyond the rhetoric, what will it take to get us there?
Sofia gruskin.
a Director, USC Institute on Inequalities in Global Health, University of Southern California, Los Angeles, CA, USA. Correspondence :, ude.csu.dem@niksurg
William Jardell
b Program Specialist, USC Institute on Inequalities in Global Health, University of Southern California, Los Angeles, CA, USA
Laura Ferguson
c Director, Program on Global Health and Human Rights, USC Institute on Inequalities in Global Health, University of Southern California, Los Angeles, CA, USA
Kristin Zacharias
d Research Associate, USC Institute on Inequalities in Global Health, University of Southern California, Los Angeles, CA, USA
Rajat Khosla
e Human Rights Advisor, World Health Organization, Geneva, Switzerland
The integration of human rights principles in sexual and reproductive health (SRH) research is often recognised to be of value. Good examples abound but lack of clarity persists as to what defines rights-inclusive SRH research. To help move the field forward, this article seeks to explore how key stakeholders responsible for funding and supporting rights in SRH research understand the strengths and weaknesses of what is being done and where, and begins to catalogue potential tools and actions for the future. Interviews with a range of key stakeholders including international civil servants, donors and researchers committed to and supportive of integrating rights into SRH research were conducted and analysed. Interviews confirmed important differences in what is understood to be SRH rights-oriented research and what it can accomplish. General barriers include lack of understanding about the importance of rights; lack of clarity as to the best approach to integration; fear of adding more work with little added benefit; as well as the lack of methodological guidance or published research methodologies that integrate rights. Suggestions include the development of a comprehensive checklist for each phase of research from developing a research statement through ultimately to publication; development of training modules and workshops; inclusion of rights in curricula; changes in journal requirements; and agreement among key funding sources to mandate the integration of rights principles in research proposals they receive. As a next step, cataloguing issues and concerns at local levels can help move the integration of human rights in SRH research from rhetoric to reality.
Résumé
L’utilité de l’intégration des principes des droits de l’homme dans la recherche sur la santé sexuelle et reproductive (SSR) est reconnue. Les bons exemples abondent, mais un manque de clarté persiste sur la définition de la recherche sur la SSR inclusive des droits. Pour aider à progresser dans ce domaine, l’article se demande comment les principaux acteurs responsables du financement et du soutien des droits dans la recherche sur la SSR comprennent les forces et les faiblesses de ce qui est fait et où, et il commence à répertorier les outils potentiels et les mesures pour l’avenir. Des entretiens ont été réalisés et analysés avec un éventail d’acteurs clés, notamment des fonctionnaires publics, des donateurs et des chercheurs qui approuvent et soutiennent l’intégration des droits dans la recherche sur la SSR. Ils ont confirmé d’importantes différences dans ce qui est compris comme une recherche sur la SSR axée sur les droits et ce qu’elle peut accomplir. Les obstacles généraux comprennent le manque de compréhension de l’importance des droits ; l’insuffisante clarté quant à la meilleure approche de l’intégration ; la crainte de créer davantage de travail pour de faibles avantages ajoutés ; de même que le manque de conseils méthodologiques ou de méthodologies de recherche publiées qui intègrent les droits. Les suggestions comprennent la mise au point d’une liste de contrôle exhaustive pour chaque phase de recherche depuis l’élaboration de l’énoncé de la recherche jusqu’à la publication ; la préparation de modules de formation et d’ateliers ; l’inclusion des droits dans le programme d’études ; les changements dans les conditions des revues spécialisées ; et la volonté des principales sources de financement de rendre obligatoire l’intégration des principes des droits dans les propositions de recherche qu’elles reçoivent. En tant que prochaine étape, l’inventaire des problèmes et des préoccupations aux niveaux locaux peut aider à faire passer l’intégration des droits de l’homme dans la recherche sur la SSR de la théorie à la pratique.
La integración de los principios de derechos humanos en investigaciones sobre salud sexual y reproductiva (SSR) es reconocida como valiosa. Abundan los buenos ejemplos, pero persiste la falta de claridad en cuanto a qué define una investigación sobre SSR inclusiva de derechos. Con el fin de que progrese este campo, este artículo busca explorar cómo las partes interesadas clave responsables de financiar y apoyar los derechos en las investigaciones sobre SSR entienden las fortalezas y debilidades de qué se está haciendo y dónde, y empieza a catalogar posibles herramientas y acciones para el futuro. Se realizaron y analizaron entrevistas con una variedad de partes interesadas clave, tales como funcionarios, donantes e investigadores internacionales comprometidos a integrar los derechos en las investigaciones sobre SSR. Las entrevistas confirmaron importantes diferencias en lo que se entiende como investigación sobre SSR orientada hacia los derechos y qué se puede lograr. Entre las barreras generales figuran: la falta de comprensión sobre la importancia de los derechos; falta de claridad en cuanto al mejor enfoque para la integración; temor de agregar más trabajo con poco beneficio adicional; así como la falta de orientación metodológica o metodologías de investigación publicadas que integran los derechos. Algunas sugerencias son incluir la creación de una lista de verificación integral para cada fase de la investigación, desde la elaboración de la declaración de la investigación hasta la publicación; la creación de módulos y talleres de capacitación; la inclusión de derechos en currículos; cambios a los requisitos de revistas; y el acuerdo entre las principales fuentes de financiamiento de exigir la integración de los principios de derechos en las propuestas de investigaciones que reciben. Como un próximo paso, catalogar los problemas y las preocupaciones a nivel local podría ayudar a llevar la integración de los derechos humanos en las investigaciones sobre SSR de la retórica a la realidad.
It is often stated that integrating human rights in sexual and reproductive health (SRH) policies, programmes and services is essential to achieving the 2030 Agenda for Sustainable Development. Sustainable Development Goal (SDG) 3 “Ensure healthy lives and promote well-being for all at all ages” and SDG 5 “Achieve gender equality and empower all women and girls” both include targets that call for universal access to SRH services and realisation of relevant rights. 1 The complex interplay of rights-related factors generally recognised to impact SRH outcomes includes the availability, accessibility, acceptability and quality of health services; informed decision making, privacy and confidentiality in the provision of health services; and nondiscrimination and equality with particular attention to key and marginalised populations. 2 , 3 SRH-related outcomes are all further helped or hindered by the unique legal and policy environment and the larger economic, social, cultural and political determinants of local contexts, including the presence or absence of accessible and functional accountability mechanisms. Attention to all these components forms part of what is considered a rights-based approach to SRH. 4
What this means for the research needed to put these policies and programmes into place is less clear. Previous writings have discussed how incorporating human rights concepts in SRH research can help
“address power imbalances within and between institutions and programs, ensure transparent, inclusive and ethical research processes, enhance good governance of research institutions and promote research programs of particular relevance to people living in poverty/under oppression, women and marginalised groups while not compromising on quality”. 5
In practical terms, the extent to which the range of rights considerations noted above form part of SRH research is not well documented, even in research that claims to have a focus on sexual and reproductive health and rights. It is also not clear from a methodological perspective what such a commitment means for each phase of research, from the development of a research question, through to implementation, analysis and publication. 6
A number of issues can be raised from the outset. How does one determine what qualifies as rights-based SRH research? Is it integration of rights at one or at every stage of the research process? Which rights are included? Is it the legal definition of rights or simply a concern with justice and equality? To qualify as rights-based SRH research, how relevant is the content or subject matter being addressed through the research? Is a focus, for example, on addressing inequalities among various population groups in their access to certain services necessarily rights-based? 5 Must rights principles, such as participation or accountability, be explicitly adopted as such, forming part of the study question and, in turn, how each phase of the research is designed and implemented? 7 , 8 Must the research team include lawyers or others with substantive expertise in rights? And how relevant is the final outcome under consideration – does it matter if the research is focused directly on, for example, increasing access to contraception versus a focus on improving the overall human rights situation for adolescents and young women, which over time will be assumed to improve access and use of contraception? 6
There is no one size fits all, nor should there be, but a number of issues must be considered. Without setting out to explicitly answer each of the questions noted above, we set out to determine the potential factors that may help or hinder efforts to integrate rights into SRH research in practice, with a focus on understanding what is being done and how, and not only the successes, but the challenges faced in integrating rights into research. A literature review found that the integration of rights has yet to be comprehensively explored in the literature, even as confronting these issues and addressing them head-on seem to be recognised as of critical importance to moving the field forward. Identified barriers to implementing rights in SRH programming included broad structural, policy and health systems barriers as well as perceived financial cost, staffing and time constraints and a lack of understanding of how concretely to include human rights, while facilitators included the existence of human rights champions and leadership, strong civil society participation, training, guidelines and funding made available specifically for implementation. 9 Additional key issues identified included the understanding of what human rights are and what they offer, awareness of appropriate methodologies, political will, the need for an enabling environment and clear accountability mechanisms. 9 Identified barriers and best practices were utilised to set the parameters for this study.
This article explores the current status of rights integration in SRH research through key informant interviews to understand what is being done and where, successes and barriers to wider adoption of rights in SRH research, and to begin to consider tools, approaches and other actions that might be useful. These interviews are used as background for the analysis and discussion that follow.
This section describes the methodology used to select key informants as well as the approach taken to data collection and analysis.
Participant selection
Without aiming for saturation, 10 key informants centrally engaged in and committed to integrating rights into SRH research and/or relevant programming from a variety of disciplinary and organisational perspectives were interviewed between April and August 2019. These included donors, international civil servants (e.g. policymakers, programme implementers) and researchers, with both personal and organisational commitment to integrating rights within their work, including from the United Nations, national governments and international funding agencies.
Data collection
Interviews were conducted by a trained interviewer using an interview guide developed for this purpose by the research team. The objective of these interviews was to determine how key stakeholders generally understand the quality and approach to what is being done and where, barriers they see to wider integration of rights in SRH research and tools and other actions they think would be useful to better incorporate rights into every stage of SRH research from the definition of the research question through to implementation, data analysis and publication. Detailed notes were taken during the interviews to capture content reported by informants.
Data analysis
Capturing key points emergent in the interview data, notes from the 10 interviews were analysed looking for examples of current rights integration as well as challenges and successes in integrating rights at each phase of the research process. An iterative process of analysis was conducted. The literature review noted earlier was used to frame and analyse interview data, including attention to potential tools and approaches to take this work forward. 9
Respondents provided general reflections on all that it takes to incorporate rights into SRH research including substantive and methodological challenges. They also noted overarching questions and approaches that they thought might be helpful to move the field forward. The findings presented below include salient quotes to illustrate the points being made.
In the first instance, several ways in which attention to rights can help to strengthen SRH research were noted by respondents. These included attention to power and power dynamics, understanding the condition and position of research subjects (whatever the topic), substantive attention to inequalities, and the potential to use the legal grounding of rights for subsequent advocacy and potential policy change resulting from research findings.
“(Rights) strengthens (research) because it systematically draws attention to the things that we think matter that aren’t often explicitly called out in research and you can tell why things are or are not happening.” (KII7, Researcher)
“Power dynamics affect every part of a person’s experience including how the research is done and perceived, and I don’t think we’re as thoughtful about that as we need to be from the research perspective.” (KII4, Funder)
Nonetheless, a concern raised by one key informant, and echoed by others, centred on the view of many in the SRH research community that rights are political, legal, and/or are not helpful to SRH research unless the research is expressly concerned with addressing a rights concern such as gender inequality.
“The weaknesses are that human rights are in the first instance assumed to be political and people are scared of them, especially governments. Making clear to people that rights can be helpful to get to their outcomes is key to moving this work forward.” (KII7, Researcher)
Respondents also described a general unwillingness among many SRH researchers who fear that the addition of rights to their research may be too expensive, too fuzzy, or take too long.
“It’s considered a second-level priority unless the study is looking at that [rights] explicitly.” (KII1, Senior International Civil Servant)
According to respondents, limited knowledge of sound methodological approaches for how to incorporate rights into research has also hindered their ability to take hold. For example, even as contraception, abortion and maternal health are areas where rights have been more or less successfully integrated from a programming perspective, this has not translated into research efforts, even within these same areas.
“There was some work done around contraception, abortion, and maternal health but that was in programming and it’s not something that researchers would consider a natural part of their work.” (KII3, Retired Senior International Civil Servant and Funder)
Furthermore, it was noted that some researchers think that, because they have a good heart and a general concern with social justice, they are already incorporating rights into SRH research, adding to further confusion about what is actually needed to integrate rights into SRH research effectively. When rights integration has happened systematically, respondents shared that it tends to be associated with specific donors.
“The weakness is methodology, and awareness of the methodologies that do work. Integrating and unpacking on a granular level tends to be very nascent at this stage … When it does happen, it is largely focused on certain geographic areas funded by certain donors only … ” (KII6, International Civil Servant)
The importance of both funders and ethical review boards was a recurring theme. Respondents discussed how the interests of donors or the strength and focus of ethical review boards play a role in how strongly human rights concerns or protections are dealt with when developing and implementing a research study. It seems that, even with the best of intentions, there are few funders or review boards who fully know how to engage rights in research despite general interest in doing so. Even when funders or review boards insist on attention to rights, there are researchers who lack a commitment to rights and simply pay lip service to rights in their initial conceptualisation because they are focused on getting the research through, and not necessarily because they see the added benefit of doing so. Respondents also noted that even when there is a commitment to rights at the time of the initial conceptualisation of a research project, they would often be forgotten as the work moved forward.
“I have not seen many protocols that explicitly mention human rights and include them from the very start and all the way through the structure of the project. However, rights are very often mentioned in the background … It’s mentioned as something that is helpful and important, but it’s rarely incorporated into the design.” (KII2, Senior International Civil Servant)
“As a researcher, if you’re not asked for ‘the why’, then you’re not going to look for those answers.” (KII9, International Civil Servant)
“ … . sometimes when you don’t talk about something you forget about it and then that really biases how you’re understanding the problem. You forget that it’s a part of the equation … It’s like this with rights.” (KII4, Funder)
Even when researchers have a commitment to bringing rights into the operational phases of their research, substantive barriers remain concerning content and actual implementation. One interviewee discussed the importance of having rights-focused indicators for data collection embedded in each phase of the study design to ensure attention to rights can be carried all the way through.
“One of the challenges or barriers in the incorporation of each right per se is that we totally lack the measurements and don’t collect enough data on the context in which we are working or the people we are working with to make an assessment as to if, for example, we are discriminating or leaving people out.” (KII4, Funder)
Another barrier noted to ensuring that rights-oriented methodologies that do exist become known and can be replicated concerns the limited appetite of many peer-reviewed journals to publish the details of the sorts of methodologies needed to incorporate rights into research, resulting in rights being less apparent in published work.
“The bias is in the epidemiological framing. If we do an analysis that brings in rights considerations, getting this paper into X or Y journal may often be more in the editorial section than in the peer-reviewed, biomedical research section.” (KII9, International Civil Servant)
Respondents generally made the point that, even with the best of intentions, the ability to integrate rights into research requires training and experience. They emphasised that any such training needs to make clear not only the need to draw attention to the reasons for paying attention to rights and the potential value added, but the concrete ways rights can be integrated into the different phases of research.
“With gender and human rights as you go beyond what people have learned and it is less familiar this will require more time.” (KII3, Retired Senior International Civil Servant and Funder)
“It’s been a steep learning curve for me … I’ve learned so much in the past few years and I think people at the major public health places need to do the same. As I’ve come to understand a human rights perspective … I have learned a lot: what it is, what it means to apply it, etc.” (KII1, Senior International Civil Servant)
Respondents provided a number of recommendations they saw as useful next steps to facilitate SRH researchers’ ability to bring rights into the different phases of SRH research, from approaches to developing research objectives to the sorts of tools and actions needed at every stage of the research process.
Interviewees discussed as a first order of business the need to establish a willingness among researchers to learn and develop the necessary skills and suggested messaging in a variety of fora on the added value rights could bring to their work.
“There is a need for good public health research in the first place. And then what difference does it make using a rights-based approach to the study design or research questions? What are the underlying determinants, power structure? These questions need to be embedded in the study design. This starts to highlight the nature of tools that are required; training programs, facilitated online platforms that are specific to guiding people through all phases or research.” (KII6, International Civil Servant)
Informed consent was discussed as a potential entry point for communicating with researchers the importance of rights integration, in that even if they are unfamiliar with how to integrate rights into their work, they are aware of the importance of informed consent processes.
“One of the key things is informed consent. Regardless of if the research is biomedical or qualitative, this is the human rights aspect that most of the researchers try to cover also in terms of confidentiality, giving information, etc. Maybe this is a starting point where you can connect with all of them [the researchers]. Informed consent could be the common ground.” (KII10, International Civil Servant)
One key informant, an international civil servant, suggested a methodology to help researchers conceptualise a three-tiered approach to rights in developing their research statement: including attention to contextual factors, the questions to be asked, and the population to be addressed, as a way to explicitly incorporate rights in ways that can impact all aspects of the research. It was noted that this would help researchers to think more broadly than research ethics by bringing attention to the larger contextual factors or environment where the research will take place.
Key informants suggested a variety of approaches as to how to take the integration of rights in research forward. Respondents discussed important considerations including tools, products and approaches including a checklist, trainings, and changes to university curricula and funding requirements by donors.
The development of a tool, such as a checklist with an accompanying training module, was discussed by several respondents as something that could be helpful and useful throughout each stage of research, even without previous human rights training. Respondents extrapolated what such a checklist might look like, and that it could, for example, include a process for establishing the rights most important to a particular SRH research question. Utilisation of a checklist throughout the phases of the research process was described as an easy step for researchers to follow for rights integration, so long as it was as specific as possible.
“I think a checklist and module would be great. I think the complement to this would be to routinely have a discussion of these issues. If there are things included, perhaps in the checklist, you might suggest that a certain type of person be brought into the conversation. A checklist would flag issues to consider, the module would give expertise, and the discussions would supplement.” (KII2, Senior International Civil Servant)
“The more specific one can be in a checklist the better. How to address a specific human right. How to write it into a protocol and what is important. Take the most important human rights as relevant to a specific area of research and why they are important, and how to address each specifically in the protocol.” (KII3, Retired Senior International Civil Servant and Funder)
Another interviewee, in responding more generally, noted that a checklist can help ensure that rights concerns become part of implementation throughout the research process. Another, in discussing the importance of ensuring rights principles are explicit in all phases of the research, noted that for this to be carried through successfully would require consistent check-ins between senior investigators with the research team on the ground to ensure these principles were not inadvertently ignored, and that there was the attention to the potential need for additional trainings as new issues came up (KII5, Researcher).
“I would value some sort of checklist to know what I should be thinking about at each stage of research so that when I write proposals and implement my research, I have in mind what extra steps might need to be incorporated into the project design. At each stage of research it would be helpful to be reminded of rights and how to implement them.” (KII7, Researcher)
It was noted that a short training may facilitate the incorporation of human rights principles or any tools such as a checklist. Respondents shared that laying the foundation for research questions, implementation, data analysis, findings and publication through a human rights lens could be a key component of a training. A training module was described by interviewees as being necessary to ensure that researchers are familiarised with what rights actually offer when attempting to include rights in each phase of research.
As an entry point, one interviewee pointed out that starting by offering training to those who are least resistant and most interested can be a first step in facilitating the integration of rights into research, as it will be necessary to convince researchers that this time is well spent.
“Well-structured 1-2-hour online training courses can be done well and then are very useful if they are directly linkable and could be directly used in developing a protocol/research question. You can say to people this is how you should analyze your data to make sure that you’re including those principles. A checklist that is linked to an online training that is done because they have to, not just because they are interested – this may have a lasting impact.” (KII1, Senior International Civil Servant)
“People must see that it’s something of value to their research. Perhaps include a certification process and incentives as this will also help people who aren’t initially open get involved.” (KII9, International Civil Servant)
Respondents also discussed the pros and cons of bringing in rights specialists to facilitate the efforts of research teams to engage in rights integration at the stage of proposal development, as well as once a proposal has been funded. While it was generally agreed that bringing in a specialist is not ideal, it was recognised to be an efficient way to help researchers become more aware of how to integrate rights principles into their work.
“You want it to be a part of the broader thinking, but I think you would need a human rights specialist or someone who has been through a crash course [on rights].” (KII1, Senior International Civil Servant)
Requiring a human rights specialist on in-country teams may not be possible, therefore other methods including the checklist and requisite training would ideally be stand-alone and not require a human rights expert as a full member of the research team. While none of those interviewed currently work at the local level, there was general agreement on the need to develop local expertise in human rights among public health researchers, and that such an exercise might expand the pool of people committed and able to bring rights effectively into SRH research efforts.
Another, longer term, aspect that respondents brought up was a need for universities and academic programmes training public health students to include human rights training, in particular as it concerns research and monitoring and evaluation in health, in their curricula. When students graduate, it was noted that their ability to understand the value of human rights principles to their research work would help to shape the work they would do once in a job.
Finally, respondents pointed out that if funding bodies require a rights perspective not only in proposals submitted but in the eventual write-up of research findings, researchers might be more inclined to learn more about how to incorporate rights into their work. As funders were described as having an obligation to ensure things are done per established and funded research protocols, an important first step would be to educate funding bodies on the importance of rights in the implementation of health research, and not simply as part of the background statement. They, in turn, would be able to educate researchers on doing proper rights-based work, as well as provide ongoing support, including review committees to ensure implementation is done as prescribed.
“Working with funding bodies … to structure a capacity-building training online that would help the applicant that would include why it’s important in addition to how to do it. It’s the low hanging fruit, people need that information. Maybe going to the key donors and giving them an orientation, get them up to speed as well. As researchers, that would create a motivation because they have to have a protocol the funder will approve.” (KII1, Senior International Civil Servant)
“It’s hard to check that researchers are actually doing what is in the protocol. Having some committees review the protocol would be helpful.” (KII3, Retired Senior International Civil Servant and Funder)
The interviews confirm that even as the need for the integration of rights in SRH research is fairly well established, there is still a general lack of clarity about what this means in practice. SRH research that takes rights into account spans broad social justice framing, very legalistic approaches to rights, and everything in between. This makes it clear that tools and training are needed to support the integration of rights in SRH research that do not dictate only one way of doing things but offer processes that are sufficiently malleable to support the range of approaches that do exist, and, importantly, with respect to every step of the research process. As it appears many in the larger SRH research community still do not see the value of rights for their work, there is a need also for attention to social media and other communication strategies that can highlight the added value of attention to rights for research and outcomes, as well as outreach to journal editors to support publication of relevant research methodologies. Further, it is clear that to truly support rights in SRH research will require larger structural changes, from what is taught in schools of public health to the approaches taken by funding agencies and other large institutions in what they do concretely to support the integration of rights.
Many of the issues that surfaced in previous literature reviews were found to translate to SRH research, but additional issues surfaced including a lack of understanding of how to operationalise specific human rights principles, and how to use rights not only as part of the conceptual background to research being undertaken but to practically support research questions and implementation of a research study, as well as the approach taken to data analysis and writing up the work for publication. 9 Further points noted in the literature, and reiterated through the interviews, include the short timeframes imposed by many donors for demonstrating research outcomes, that inhibit the ability to truly understand and write-up the longer-term changes that might be possible through the inclusion of rights. 6
The recommendations provided by key informant interviews can provide an important starting point for the content of any tools, guidelines or training materials to be developed. Tangibly, a key need identified through the interviews was a checklist, with appropriate training support, that could provide hints or questions for how to integrate rights at each phase of research without attempting to enforce a one-size-fits-all approach. Substantively it was nonetheless clear that certain issues would be relevant to all SRH research, such as attention to power dynamics, including within the research team, and questions of how and why rights are being integrated at each phase, as well as the potential to use research findings based on a rights framework for advocacy and policy change further down the line.
Each of the recommendations that emerged from these interviews would require the development of a robust and carefully thought through and tested strategy so as not to overwhelm researchers, funders or others seeking to better integrate rights into research. The implementation of any tool, such as a training or checklist, would also require careful monitoring to ensure they positively impacted the research process, did not unnecessarily impact cost, workload or personnel, and contributed beneficially to intended outcomes.
For years, there have been those who juxtapose a public health approach against a human rights approach as though the two are distinct and seek to do different things. While patently false this perception nonetheless has particularly stymied integration of rights into research. Hence there is a need for appropriate documentation and effective communication strategies that can highlight research which demonstrates the added value of rights for achieving public health goals, thereby pushing the conversation past a focus on the theoretical advantages of rights integration to actually demonstrating to those who are sceptical what this means in practice.
To bring rights more concretely into SRH research will require both a top-down and a bottom-up approach working in tandem. Ultimately, funding agencies have a key role in shaping where, how, for how long, and even if, research projects that bring in rights can occur. Engaging with publishers, funders and larger institutions on concrete actions that will facilitate the ability of researchers to integrate rights into SRH research will be key, while simultaneously providing very specific guidance to researchers as to how to think about rights at every stage of the research process. Researchers are not likely to incorporate rights into their work in systematic and replicable ways when funding bodies and other agencies are not providing the requisite support for their ability to do so. An enabling environment, even if support for this sort of research exists among funding bodies and global institutions, is necessary for local level action that integrates rights. As a next step, additional analysis to catalogue issues and concerns at grassroots and local level would help ensure the development of tools for rights integration that would adequately address the range of challenges that exist.
Limitations
The key informant interviews conducted provide a range of perspectives, even as they do not provide a comprehensive understanding of all that is happening in terms of rights-based SRH research. While ensuring the perspectives of high-level funders, civil servants and researchers have been captured, in order to capture a more robust understanding as to what is happening in the field and what is needed, additional interviews, particularly within local settings, could provide additional important insights.
Conclusions
Attention to rights at each stage of SRH research must be deliberate. While this study focused on the perspectives of high-level funders, civil servants and researchers, additional attention to local level perspectives would be a key next step for integration of rights in research to be meaningfully taken forward. Utilising the research cycle as the entry point can move this conversation from more general commitments to specific methodologies, providing a level of granularity and methodological approaches for rights consideration from start to finish. Steps can be taken within each phase of research, from developing a research statement through ultimately, to publication, but this requires training and support of researchers seeking to do this work by global and national institutions, as well as organisational change in the curricula used within institutions of higher learning, the issues considered by institutional review boards, and the seriousness of the approach to rights taken by funding agencies and other donors.
Global guidance exists to help support the integration of human rights into the provision of SRH policies, programmes and care. However, little guidance exists that prioritises and supports the integration of human rights into the SRH research process, and few currently have the mandate or tools to support this work in replicable ways. A cataloguing of issues and concerns at the local level culminating in comprehensive global guidance, mandates, tools and trainings will help move the integration of human rights in SRH research from rhetoric to reality.
Acknowledgements
The authors would like to gratefully acknowledge Krishni Satchi for her research assistance. We are indebted to the amazing key informants who provided their valuable insights and thoroughly enriched this discussion.
Funding Statement
This work was supported by World Health Organization [grant number 202040142].
This paper is in the following e-collection/theme issue:
Published on 20.8.2024 in Vol 10 (2024)
Integrating Sexual and Reproductive Health Equity Into Public Health Goals and Metrics: Comparative Analysis of Healthy People 2030’s Approach and a Person-Centered Approach to Contraceptive Access Using Population-Based Data
Authors of this article:

Original Paper
- Anu Manchikanti Gomez 1 , MSc, PhD ;
- Reiley Diane Reed 1 , MPH, MSW ;
- Ariana H Bennett 1 , MPH, DrPH ;
- Megan Kavanaugh 2 , MPH, DrPH
1 School of Social Welfare, University of California, Berkeley, Berkeley, CA, United States
2 Guttmacher Institute, New York, NY, United States
Corresponding Author:
Anu Manchikanti Gomez, MSc, PhD
School of Social Welfare
University of California, Berkeley
120 Haviland Hall MC 7400
Berkeley, CA, 94720-7400
United States
Phone: 1 510 642 0722
Email: [email protected]
Background: The Healthy People initiative is a national effort to lay out public health goals in the United States every decade. In its latest iteration, Healthy People 2030, key goals related to contraception focus on increasing the use of effective birth control (contraceptive methods classified as most or moderately effective for pregnancy prevention) among women at risk of unintended pregnancy. This narrow focus is misaligned with sexual and reproductive health equity, which recognizes that individuals’ self-defined contraceptive needs are critical for monitoring contraceptive access and designing policy and programmatic strategies to increase access.
Objective: We aimed to compare 2 population-level metrics of contraceptive access: a conventional metric, use of contraceptive methods considered most or moderately effective for pregnancy prevention among those considered at risk of unintended pregnancy (approximating the Healthy People 2030 approach), and a person-centered metric, use of preferred contraceptive method among current and prospective contraceptive users.
Methods: We used nationally representative data collected in 2022 to construct the 2 metrics of contraceptive access; the overall sample included individuals assigned female at birth not using female sterilization or otherwise infecund and who were not pregnant or trying to become pregnant (unweighted N=2760; population estimate: 43.9 million). We conducted a comparative analysis to examine the convergence and divergence of the metrics by examining whether individuals met the inclusion criteria for the denominators of both metrics, neither metric, only the conventional metric, or only the person-centered metric.
Results: Comparing the 2 approaches to measuring contraceptive access, we found that 79% of respondents were either included in or excluded from both metrics (reflecting that the metrics converged when individuals were treated the same by both). The remaining 21% represented divergence in the metrics, with an estimated 5.7 million individuals who did not want to use contraception included only in the conventional metric denominator and an estimated 3.5 million individuals who were using or wanted to use contraception but had never had penile-vaginal sex included only in the person-centered metric denominator. Among those included only in the conventional metric, 100% were content nonusers—individuals who were not using contraception, nor did they want to. Among those included only in the person-centered metric, 68% were currently using contraception. Despite their current or desired contraceptive use, these individuals were excluded from the conventional metric because they had never had penile-vaginal sex.
Conclusions: Our analysis highlights that a frequently used metric of contraceptive access misses the needs of millions of people by simultaneously including content nonusers and excluding those who are using or want to use contraception who have never had sex. Documenting and quantifying the gap between current approaches to assessing contraceptive access and more person-centered ones helps clearly identify where programmatic and policy efforts should focus going forward.
Introduction
Reproductive well-being requires the ability to prevent, continue, and end pregnancy in line with one’s desires, values, and preferences. For many people, use of contraception is crucial to reproductive well-being, as it is a key tool that people can use to help them accomplish their self-defined reproductive goals. Programs and policies in the United States that are designed to facilitate contraceptive access should have people’s reproductive well-being as a north star and be explicitly guided by principles of sexual and reproductive health (SRH) equity. The SRH equity framework lays out a vision for the conditions required for individuals to attain their maximal state of SRH and well-being [ 1 , 2 ]. This vision includes attention to structural inequities—based on historical and current systems of oppression—and the ways in which they differentially affect and marginalize certain communities. Similarly, efforts to track the extent to which programs and policies are making progress toward contraceptive access goals should also be guided by SRH equity.
Person-centered contraceptive access refers to the opportunity to have self-defined contraceptive needs fulfilled [ 3 ]. Therefore, person-centered contraceptive access is not just about contraceptive use or the availability of services but also encompasses the formation and realization of preferences, including use of preferred contraceptive methods as well as the accessibility, affordability, and appropriateness of care to obtain desired contraception. One key national effort that sets public health goals related to contraceptive access is the US Healthy People initiative, which, each decade, lays out broad objectives with related targets and activities across multiple health domains to advance health and well-being. In Healthy People and many other public health efforts that focus on contraceptive access, goals and associated metrics typically emphasize contraceptive use over nonuse, often prioritizing use of certain methods and neglecting people’s contraceptive desires [ 4 , 5 ]. Importantly, there are no national-level public health goals that currently place individuals’ contraceptive needs—as they define them—at the center of their objectives and related tracking efforts. Without capturing this important aspect of contraceptive use and access, efforts to conduct surveillance and design strategies to increase contraceptive access are severely constrained and do not take a person-centered approach. Furthermore, without person-centered objectives and data to track progress against, efforts to expand contraceptive access under current public health objectives and benchmarks may result in inefficiency and wasted resources and perpetuate contraceptive coercion and harm.
In this study, we considered 2 contraception-focused objectives and associated metrics of Healthy People 2030 (HP2030), the most recent national initiative guiding contraceptive access and other public health objectives at the national level in the United States. We highlighted key conceptual and empirical limitations embedded in the HP2030 contraception-related goals. Our analysis highlights shortcomings of conventional public health approaches and offers future directions to track and advance person-centered contraceptive access that align with SRH equity.
A Primer on the Healthy People Initiative
The Healthy People initiative plays a significant role in shaping public health and policy in the United States by establishing a comprehensive list of health-related objectives in 10-year cycles. Surgeon General Julius Richmond launched the initiative in 1979, with the first set of objectives (Healthy People 1990) released in 1980 [ 6 ]. New objectives have been released in each decade since. While each update integrates lessons learned, Healthy People remains focused on its original mission of improving health outcomes in the United States. Released in August 2020, HP2030 reflects an evolution of the initiative to address health equity. HP2030 has a stated mission to “eliminate health disparities, achieve health equity, and attain health literacy to improve the health and well-being of all” [ 7 ]. All objectives are set by federal interdisciplinary expert working groups based on alignment with both federal and public health priorities, existing baseline data, and multi-sector stakeholder input via public comment [ 7 ].
Limitations of HP2030’s Focus on Increasing Use of Effective Contraceptive Methods
HP2030 objectives related to contraception fall in the Family Planning topic area, which includes goals focused on improving pregnancy planning and preventing unintended pregnancy [ 8 ]. Many scholars have highlighted the problematic nature of the prevention of unintended pregnancy as a public health goal, emphasizing both the poor measurement and conceptualization of unintended pregnancy, as well as how continued focus on purportedly appropriate timing of childbearing perpetuates stratified reproduction [ 9 - 15 ]. In this paper, we focus more narrowly on 2 of HP2030’s core contraception-focused objectives, each centered on increasing use of effective birth control among those at risk of unintended pregnancy. The first objective focuses on increasing use among women aged 20 to 44 years [ 5 ], whereas the second focuses on adolescent female individuals aged 15 to 19 years [ 4 ].
As with all HP2030 objectives, these 2 contraception-related goals are connected to associated metrics to track progress. The numerator reflects use of effective contraceptive methods, defined as methods considered most or moderately effective at preventing pregnancy (permanent contraception, implant, intrauterine devices [IUDs], injectable contraception, oral contraceptive pills, the patch, the ring, or the diaphragm) [ 16 ]. Although the objectives refer to effective birth control, it is important to note that effectiveness is restricted to pregnancy prevention, neglecting that some methods are effective at achieving other user-desired outcomes (eg, preventing sexually transmitted infections or menstruation management). The denominator for both is the population of those at risk of unintended pregnancy, defined as women in each of the age ranges who have ever had sex with a man; are not pregnant, seeking pregnancy, or post partum; and are not sterile (for surgical noncontraceptive or nonsurgical reasons) [ 17 ]. Progress toward goals is tracked using the National Survey of Family Growth, a periodic, nationally representative survey used to monitor SRH, family and relationships, and health behaviors. The most recent 2017 to 2019 National Survey of Family Growth data indicate that 62.2% of women aged 20 to 44 years and 53.3% of adolescent female individuals aged 15 to 19 years at risk of unintended pregnancy are using effective contraception [ 4 , 5 ]. HP2030 has set a national goal of increasing use of effective contraception to 65.1% among those aged 20 to 44 years and 70.1% among those aged 15 to 19 years.
In the following sections, we highlight key conceptual and empirical limitations of these 2 HP2030 metrics. Furthermore, as the mission of HP2030 includes advancing health equity and eliminating health disparities, we sought to elucidate the alignment—or lack thereof—of these 2 objectives with the principles of SRH equity.
Issues With the Population of Focus
Both HP2030 metrics focus on individuals at risk of unintended pregnancy, which implicitly links contraceptive use to penile-vaginal sex and excludes use of contraception for reasons beyond pregnancy prevention. Extant research describes the many reasons individuals choose to use or not use contraception, including reasons completely delinked from sex and reproduction [ 18 - 21 ]. For example, in a 2023 national survey, 66% of those aged 15 to 29 years who had ever used hormonal contraception did so to manage menstruation-related symptoms, such as heavy bleeding and cramping [ 22 ]. Previous research elucidates that some people may not report actively seeking pregnancy but they may find it acceptable [ 23 - 26 ], that the notion of pregnancy planning is not always salient [ 27 , 28 ], and that individuals may not express explicit intentions because they lack the structural conditions to claim their underlying desires [ 11 ]. Furthermore, because of the focus on (presumed) risk of unintended pregnancy, the HP2030 metrics include in their denominators content nonusers—individuals not using contraception who do not want to use contraception. This conflicts with SRH equity by placing value on use of methods even when individuals prefer to use no method at all [ 1 , 29 ].
Notably, these 2 objectives explicitly name women and female adolescents as the populations of focus, specifically those who ever had sex (with a man) as a proxy for risk of pregnancy. Not all people who (want to) use contraception identify as women or female, some people who identify as men may not produce sperm, and having had sex (presumably penile-vaginal sex) at some point in one’s lifetime does not speak to current risk of pregnancy. As gender-expansive individuals already face increased stigma and discrimination in health care settings and must additionally navigate contraceptive care being provided under the umbrella of women’s health, this approach reiterates a cisnormative, heteronormative binary [ 30 - 33 ]. Notably, the data measurement details for each objective do not detail how gender identity is measured [ 17 ].
Lack of Person-Centeredness
Contraceptive use is a preference-sensitive decision, meaning that there is often no significant medical benefit to one choice versus another; therefore, there are multiple appropriate options for most individuals, including methods deemed as less effective for pregnancy prevention or other reasons [ 34 ]. However, the focus of these HP2030 objectives on increasing use of effective contraception neglects the preference-sensitive nature of contraceptive decision-making. By positioning use of most or moderately effective methods as successful, use of other methods or no method are thereby situated as a failure. This framing may inadvertently motivate family planning providers to encourage their patients to initiate and continue to use highly effective methods, especially long-acting reversible contraception, even in the absence of a patient’s desire to use these methods [ 35 - 40 ]. Such directive contraceptive counseling undermines reproductive autonomy and reinforces mistrust in health care, particularly among communities subjected to historical and ongoing medical coercion and abuse [ 41 , 42 ]. Furthermore, extensive research has documented that effectiveness for pregnancy prevention is only 1 factor among many that people consider when choosing the best contraceptive method for them [ 19 , 43 - 46 ].
Person-centered care, as defined by the Institute of Medicine, is “compassionate, respectful, and responsive to the needs, values, and expressed desires of each individual person” [ 47 ]. Setting population-level goals for use of specific groups of contraceptive methods without clear evidence that individuals desire them—as both HP2030 objectives do—ignores the needs, values, and desires that undergird the choice to use a specific method or to not use contraception. Furthermore, given that contraceptive use is a dynamic journey and US women use a median of 3 methods during their lifetimes [ 48 ], it is expected that individuals—including users of these effective methods—will start, switch, and discontinue methods throughout their lives [ 18 , 49 , 50 ]. For example, one may be using a method that requires a provider to remove it (eg, an implant) but desire to stop using it immediately. Through the lens of the HP2030 metrics, this individual’s use of a highly effective method is framed as a success and would contribute to meeting these targets even though they desire discontinuation. Designating use of these methods as a universally positive outcome without consideration of people’s own preferences is particularly concerning in light of research findings that Black and Latino individuals are more likely to prefer methods that they can start without seeing a health care provider [ 19 ] and less likely to receive person-centered contraceptive counseling [ 51 ].
Use of Preferred Contraceptive Method as a Person-Centered Metric of Contraceptive Access
The ability to realize one’s contraceptive preferences represents one successful outcome in the cumulative process of navigating contraceptive access, from information seeking to desired contraceptive use [ 3 ]. Therefore, one person-centered metric of contraceptive access should capture the extent to which people are using the contraceptive method they prefer and be mindful that not using contraception may be preferred. As Burke and Potter [ 52 ] note, achieving contraceptive preferences is an indicator of reproductive autonomy and, therefore, can be considered to represent one aspect of success in achieving contraceptive access. In an analysis of population-based data, we found that 59.3% of current and prospective users (aged 15-44 years) in the United States were using a preferred contraceptive method [ 53 ].
Given the limitations of the HP2030 approach, use of person-centered contraceptive access metrics aligned with SRH equity is of paramount importance. Understanding the similarities and differences between the HP2030 approach and a person-centered approach highlights the implications of not centering contraceptive preferences—an important task given that population-level metrics of contraceptive access and quality worldwide generally do not align with SRH equity principles [ 29 , 52 ]. Therefore, in this analysis, we drew on nationally representative survey data to compare a conventional metric of contraceptive access approximating the HP2030 metrics (ie, use of effective contraception) to a person-centered metric (ie, use of preferred contraceptive method). With this analysis, we sought to compare SRH and demographic characteristics among the groups that are included in and excluded from the 2 metrics as well as elucidate the contraceptive use preferences of respondents included in the conventional measurement approach that implicitly frames use of effective contraceptive methods as successful. In so doing, we examined the assumptions built into the HP2030 objectives and considered their implications for public health policy and practice and for advancing SRH equity.
We used data collected through the Person-Centered Contraceptive Access Metrics Project, a multiyear, stakeholder-engaged effort to develop new population-level metrics of contraceptive access grounded in person-centeredness and reproductive justice [ 53 , 54 ]. Through a multidisciplinary working group that formulated the metrics, this project built upon the wisdom and expertise of stakeholders experienced in numerous sectors who produce, use, or would like to use contraceptive access metrics. The group developed the metric of use of preferred method of contraception to capture self-defined contraceptive need, described in the following sections [ 53 ].
Data Source
We used nationally representative survey data collected between January 2022 and March 2022 via the AmeriSpeak panel by NORC at the University of Chicago [ 55 ]. AmeriSpeak is a probability-based standing survey panel that is representative of the US population. Eligible panelists were aged 15 to 44 years, assigned female sex at birth, not known to be sterile, and could complete the survey in English or Spanish. The median survey completion time was 25 minutes. Approximately 97% of screened eligible panelists completed the survey (unweighted N=3059). Further details about the survey methods in accordance with the Checklist for Reporting Results of Internet E-Surveys can be found in Multimedia Appendix 1 [ 56 ].
Ethical Considerations
NORC invited all female panelists aged ≥18 years to provide informed consent and complete a brief eligibility screening survey. For panelists aged 15 to 17 years, NORC first obtained parental consent before inviting panelists to assent and participate. Participants received the equivalent of US $8 in NORC’s AmeriSpeak points. NORC provided deidentified data to the research team. The study protocol was approved by the Committee for the Protection of Human Subjects at the University of California, Berkeley (2021-02-14025) and the institutional review board of NORC (21-09-468).
Key Contraceptive Access Metrics
This paper focuses on 2 key population-level metrics of contraceptive access: a conventional metric reflecting use of effective contraception, which is prioritized in the HP2030 contraception-related objectives, and a person-centered metric, reflecting use of preferred method of contraception [ 53 ]. For this analysis, we created both metrics to be as closely comparable as possible on key data inputs (age range and gender) and sample exclusions (fecundity and pregnancy status) while highlighting where they intentionally differ in other data inputs (contraceptive use and preferences and sexual activity; Multimedia Appendix 2 ). While HP2030 includes 2 metrics that separately focus on those aged 15 to 19 years and 20 to 44 years, our comparative analysis included the full age range included in the data set (ages of 15-44 years) to align with the working group’s priority of advancing metrics that were applicable across the spectrum of age and experiences.
The conventional metric, approximating the HP2030 approach to the extent possible with our data, reflects the use of effective contraception among survey respondents presumed at risk of unintended pregnancy. The numerator is the number of individuals using a method classified by the Centers for Disease Control and Prevention [ 16 ] as most or moderately effective for pregnancy prevention in the last month (vasectomy, implant, IUD, injectable contraception, oral contraceptive pills, the patch, the ring, or the diaphragm). The denominator includes individuals assigned female sex at birth who report ever having had penile-vaginal sex and are not currently pregnant or seeking pregnancy. This construction differs slightly from the HP2030 approach due to data availability. Our survey did not assess postpartum status, an exclusion criterion for the HP2030 metrics [ 5 ], and individuals assigned female sex at birth personally using permanent contraception were not eligible for this survey, although they are included in the HP2030 metrics. In addition, while the HP2030 denominators focuses on “women,” we use assignment of female sex at birth, as the HP2030 measurement details do not describe how gender is assessed [ 17 ].
The person-centered metric, use of preferred contraceptive method, reflects a desire to maintain current contraceptive use among current and prospective contraceptive users. The numerator is the number of current contraceptive users who do not want to switch to another or no method or stop using their method as soon as possible. We asked respondents whether they would rather use a (different) method of birth control ( yes , no , or unsure ); notably, some respondents who said that they would rather use a different method indicated that they would prefer to not be using a method altogether [ 53 ]. We developed and refined this question based on interviews with stakeholders, a literature review, an expert review, and cognitive interviews in English and Spanish. In addition, we also asked current contraceptive method users whether they would like to stop using each of their reported methods in the following year ( yes , no , or maybe ); those who indicated that they would like to stop using a method as soon as possible were not classified as using their preferred method, including multiple-method users who indicated a desire to discontinue use of any of their methods immediately. The denominator includes individuals who are current or prospective contraceptive users who are not pregnant or trying to become pregnant; the working group identified this population as having a self-identified need for contraception and related services as it includes (1) current users whose needs may include maintaining use of their current method, switching to a different method, or discontinuing use of their current method; and (2) prospective contraceptive users, that is, individuals not using contraception who indicated that there was a method they would like to use. Excluded are content nonusers—individuals not using a method simply because they do not want to; while this reflects a successful enactment of contraceptive preferences, these content nonusers are not considered to have a self-identified need for contraception. Notably, this metric allows for contraceptive use for reasons beyond pregnancy prevention. Details on the construction of this metric are described in greater depth elsewhere [ 53 ].
Key Demographic and SRH Characteristics
We focused on key sociodemographic and SRH characteristics to understand who is included and excluded in the 2 metrics’ denominators. Sociodemographic characteristics include age, racial and ethnic identity, health insurance status, sexual orientation, and gender identity. SRH characteristics include experience with penile-vaginal sex ( never had , had in the last year , or had more than a year ago ). We asked respondents who indicated that they may or would like to become pregnant in the future what the ideal timing would be ( in the next year , more than a year from now , or don’t know ). We examined current contraceptive method use based on whether respondents reported using any methods in the previous month. We describe all contraceptive methods that respondents reported using in the previous month, including use of multiple methods. We also created a mutually exclusive variable focused on the most effective method that respondents were using and report preference to stop use of this method in the following year overall, including as soon as possible. We describe whether current contraceptive users (1) were using their preferred method, (2) wanted to use a different or no method or stop using any of their methods as soon as possible, and (3) were uncertain about using a different method. We describe whether individuals not currently using contraception were (1) content nonusers (who do not report wanting to use a method), (2) prospective users (nonusers who indicate that there is a method that they want to use), and (3) uncertain nonusers (unsure whether they want to use a method).
Analytic Approach
NORC constructed survey weights to account for differences between the sample and the US population. All analyses used the svy commands in Stata (version 17.0; StataCorp) to account for weighted data and complex survey design [ 57 ]. All reported proportions are weighted.
Sociodemographic and SRH Characteristics of the Sample Overall and by Metric
Our analytic sample (unweighted N=2760) excluded respondents who were pregnant or trying to become pregnant as they were not included in either metric, as well as respondents who were missing data on current contraceptive use. First, we present descriptive statistics for sociodemographic and SRH characteristics for the survey sample overall and for the subsamples meeting inclusion criteria for the 2 contraceptive access metrics examined in this analysis (heretofore referred to as the “conventional metric denominator” for the effective method use metric and the “person-centered metric denominator” for the preferred method use metric). Estimates slightly differ from those in previously published work due to different sample constructions when accounting for missing data in multivariable analyses [ 53 ].
Contraceptive Use and Preferences Among Individuals Included in the Conventional Metric Denominator
We examined contraceptive preferences among individuals meeting the inclusion criteria for the conventional metric denominator (those considered by HP2030 as being at risk of unintended pregnancy). Because this metric, as used in HP2030 and other public health contraceptive initiatives, implicitly frames use of most or moderately effective methods as successful, we leveraged our data set to examine whether those successful individuals’ preferences actually aligned with that assumption vis-à-vis desire to maintain current contraceptive use or nonuse and discontinue use of the current most effective method. Similarly, we examined individuals’ contraceptive preferences among those using other or no methods (the implied unsuccessful groups in the HP2030 approach).
Convergence and Divergence of the Denominators of the Conventional and Person-Centered Metrics
We conducted a comparative analysis to highlight the differences between the conventional measurement approach (ie, use of effective method) and a person-centered measurement approach (ie, use of preferred method). For this analysis, we first determined whether each survey respondent met the inclusion criteria for the conventional and person-centered metrics (ie, would be included in each metric’s denominator). We classified respondents as being in 1 of 4 subgroups according to the 2 features that distinguish these metrics’ denominators ( Figure 1 ): ever having had penile-vaginal sex (conventional metric inclusion criterion), and whether one is a current or prospective contraceptive user (person-centered metric inclusion criterion). The metrics converged when individuals were included in (subgroup 1) or excluded from (subgroup 2) both denominators. The metrics diverged if individuals were only included in the conventional metric denominator (subgroup 3) or the person-centered metric denominator (subgroup 4). As our comparative analysis sought to elucidate where the 2 metrics converged and diverged, we describe the distribution of age and SRH characteristics across the 4 subgroups. For the 2 divergent subgroups (3 and 4), we examined differences in age and ideal pregnancy timing using Rao-Scott–corrected chi-square tests. We also examined the distribution of race and ethnicity, insurance status, and gender; as there were no statistically significant differences, we do not present these results. Chi-square tests were not used for the other variables (sexual activity, current contraceptive use, and desire to use another contraceptive method) because each of these cross-tabulations had a structural 0 cell size; that is, there were no respondents reflected in the cell due to the inclusion requirements for the subgroups.

Sociodemographic and SRH Characteristics Overall and by Metric
Sociodemographic and SRH characteristics are presented in Tables 1 and 2 . The conventional metric denominator was slightly larger than the person-centered metric denominator (79.3% vs 74.3% of the overall sample, respectively; Table 1 ). The denominators were similar in distribution across demographic characteristics. Given the focus on pregnancy prevention, no respondents included in the conventional metric denominator reported never having penile-vaginal sex compared to 10% of those included in the person-centered metric denominator ( Table 2 ). Contraceptive method mix and desire to use another method varied by metric. Most included in the person-centered metric were using contraception (92% compared to 79.3% of those included in the conventional metric denominator). More respondents included in the person-centered metric were current contraceptive users who wanted to use a different or no method or discontinue using a method immediately (20.8% compared to 18.2% included in the conventional metric). With regard to not using contraception, 12.8% of those included in the conventional metric were content nonusers compared to 0% of those included in the person-centered metric. Nonusers who wanted to use contraception (ie, prospective users) comprised a smaller proportion of the conventional metric denominator (4.3%) compared to the person-centered metric denominator (8%).
| Sociodemographic characteristics | Full analytic sample , unweighted n (weighted %) | Conventional metric denominator (unweighted n=2393) , unweighted n (weighted %) | Person-centered metric denominator (unweighted n=2132) , unweighted n (weighted %) | |
| 15-17 | 201 (12.78) | 64 (5.37) | 91 (8) | |
| 18-24 | 296 (27.51) | 226 (25.15) | 226 (28.15) | |
| 25-29 | 574 (20.22) | 503 (22.37) | 470 (21.71) | |
| 30-34 | 637 (17.24) | 597 (20.54) | 518 (19.04) | |
| 35-39 | 598 (12.41) | 563 (14.52) | 476 (13.08) | |
| 40-44 | 454 (9.83) | 440 (12.05) | 351 (10.01) | |
| Asian or Pacific Islander only | 185 (7.15) | 141 (6.24) | 140 (6.26) | |
| Black only | 386 (14.62) | 317 (14.46) | 258 (12.98) | |
| Latinx or Hispanic only | 489 (21.4) | 417 (20.84) | 391 (22.14) | |
| Multiracial, not including Latinx or Hispanic | 137 (3.3) | 122 (3.59) | 104 (3.35) | |
| White only | 1526 (52.82) | 1364 (54.18) | 1214 (54.68) | |
| Another race or ethnicity only | 37 (0.72) | 32 (0.69) | 25 (0.59) | |
| Commercial (eg, employer based, direct purchase, or health insurance exchange) | 1884 (63.24) | 1663 (63.44) | 1491 (64.59) | |
| State Medicaid or CHIP | 460 (19.44) | 402 (21.26) | 358 (20.39) | |
| Other public insurance (including Medicare, military or VA , or IHS ) | 115 (4.42) | 100 (4.35) | 84 (4.46) | |
| None | 174 (6.45) | 154 (6.6) | 129 (6.06) | |
| Do not know | 102 (5.23) | 56 (3.36) | 56 (3.73) | |
| Missing | 25 (1.22) | 18 (0.99) | 14 (0.77) | |
| Straight or heterosexual | 2287 (78.11) | 2040 (81.27) | 1816 (80.47) | |
| Gay or lesbian | 61 (3) | 35 (1.75) | 18 (1.21) | |
| Bisexual | 285 (13.5) | 241 (13.86) | 224 (14.55) | |
| Queer | 58 (2.16) | 45 (1.75) | 42 (1.93) | |
| Something else | 54 (2.57) | 22 (0.94) | 21 (1.37) | |
| Missing | 15 (0.66) | 10 (0.42) | 11 (0.47) | |
| Woman | 2682 (96.64) | 2338 (97.22) | 2078 (96.8) | |
| Man | 10 (0.37) | 7 (0.26) | 7 (0.34) | |
| Transgender | 2 (0.25) | 1 (0.1) | 0 (0) | |
| Genderqueer or nonbinary | 38 (1.36) | 26 (0.93) | 23 (1.15) | |
| >1 gender | 17 (1.01) | 12 (1.07) | 14 (1.24) | |
| Missing | 11 (0.38) | 9 (0.42) | 10 (0.47) | |
a The analytic sample was limited to those who were not sterile, not pregnant or trying to become pregnant, and not missing data on current contraceptive use. The conventional metric was use of most or moderately effective contraceptive methods; the denominator was restricted to those who had ever had penile-vaginal sex. The person-centered metric was current use of preferred contraceptive method; the denominator was restricted to current contraceptive users and prospective users (individuals not using contraception but who would like to use it). Individuals may be included in both the conventional and person-centered metric denominators; therefore, the denominators for these metrics are not mutually exclusive.
b Population size estimate: 43,942,191.
c 79.32% of full sample; population size estimate: 34,853,000.
d 74.29% of full sample; population size estimate: 32,642,737.
e CHIP: Children’s Health Insurance Program.
f VA: Veterans Affairs.
g IHS: Indian Health Service.
| Sexual and reproductive health characteristics | Full analytic sample, unweighted n (weighted %) | Conventional metric denominator, unweighted n (weighted %) | Person-centered metric denominator, unweighted n (weighted %) | ||||||||
| Never had penile-vaginal sex | 353 (20) | 0 (0) | 144 (10.03) | ||||||||
| Had penile-vaginal sex in the last year | 2097 (69.14) | 2097 (87.17) | 1839 (82.26) | ||||||||
| Had penile-vaginal sex more than a year ago | 280 (9.77) | 280 (12.32) | 128 (6.6) | ||||||||
| Had penile-vaginal sex; missing timing of last sexual encounter | 16 (0.4) | 16 (0.51) | 10 (0.34) | ||||||||
| Missing | 14 (0.69) | 0 (0) | 11 (0.76) | ||||||||
| In the next year | 304 (7.93) | 293 (9.55) | 232 (8.27) | ||||||||
| More than a year from now | 783 (36.93) | 659 (36.5) | 591 (36.86) | ||||||||
| Does not know | 612 (22.8) | 513 (21.66) | 428 (20.76) | ||||||||
| Does not ever want to become pregnant | 1054 (32.07) | 925 (32.07) | 875 (33.79) | ||||||||
| Missing | 7 (0.28) | 3 (0.21) | 6 (0.32) | ||||||||
| 1988 (68.33) | 1878 (79.29) | 1988 (91.99) | |||||||||
| Using preferred contraceptive method | 1294 (43.9) | 1225 (51.01) | 1294 (59.09) | ||||||||
| Wants to use a different or no method or stop using any current method as soon as possible | 423 (15.47) | 403 (18.24) | 423 (20.83) | ||||||||
| Uncertain user (unsure whether they prefer using a different or no method) | 266 (8.81) | 246 (9.89) | 266 (11.8) | ||||||||
| 772 (31.67) | 515 (20.71) | 144 (8.01) | |||||||||
| Content nonuser (does not want to use contraception) | 450 (17.65) | 320 (12.8) | 0 (0) | ||||||||
| Prospective user (nonuser who wants to use contraception) | 144 (5.95) | 99 (4.26) | 144 (8.01) | ||||||||
| Uncertain nonuser (unsure whether they want to use contraception) | 174 (7.79) | 95 (3.64) | 0 (0) | ||||||||
| Currently using multiple contraceptive methods | 601 (24.03) | 582 (29.56) | 601 (32.34) | ||||||||
| Withdrawal or pulling out | 639 (25.58) | 621 (31.58) | 639 (34.44) | ||||||||
| Oral contraceptive pill | 549 (21.92) | 487 (23.4) | 549 (29.51) | ||||||||
| External condoms | 478 (18.14) | 468 (22.27) | 478 (24.42) | ||||||||
| Hormonal IUD | 331 (10.57) | 322 (12.56) | 331 (14.22) | ||||||||
| Fertility awareness | 207 (6.72) | 199 (7.96) | 207 (9.04) | ||||||||
| Implant | 108 (4.51) | 101 (5.34) | 108 (6.07) | ||||||||
| Vasectomy | 220 (4.42) | 216 (5.48) | 220 (5.94) | ||||||||
| Copper IUD | 77 (2.18) | 75 (2.68) | 77 (2.94) | ||||||||
| Shot | 52 (2.03) | 50 (2.46) | 52 (2.73) | ||||||||
| Ring | 39 (1.35) | 37 (1.65) | 39 (1.81) | ||||||||
| Emergency contraception | 35 (1.36) | 33 (1.64) | 35 (1.83) | ||||||||
| Internal condoms | 12 (0.69) | 10 (0.78) | 12 (0.93) | ||||||||
| Patch | 14 (0.55) | 12 (0.61) | 14 (0.74) | ||||||||
| Spermicide | 10 (0.22) | 9 (0.27) | 10 (0.3) | ||||||||
| Using any most or moderately effective method | 1324 (45.38) | 1237 (51.64) | 1324 (61.09) | ||||||||
b 9 respondents (unweighted n) were missing the contraceptive use or nonuse subtype.
c One of the 2 key contraceptive access metrics.
d For multiple method users, this metric reflects whether the individual wants to maintain use of all their methods.
e Participants could report the use of multiple methods in the previous month.
f IUD: intrauterine device.
Table 2 includes the key contraception access metrics, with 51% of respondents included in the conventional metric classified as using their preferred method (compared to 59.1% of respondents included in the person-centered metric). Just over half (51.6%) of respondents included in the conventional metric denominator were using a most or moderately effective contraceptive method, compared to 61.1% of respondents included in the person-centered metric.
Contraceptive Use and Preferences Among Those Included in the Conventional Metric Denominator
In Table 3 , we present data on contraceptive use and preferences among those included in the conventional metric denominator of individuals who had ever had penile-vaginal sex who were not pregnant or seeking pregnancy. Approximately half (51.6%) were using a contraceptive method rated as most or moderately effective for pregnancy prevention. More than a quarter (27.7%) were using other contraceptive methods, whereas 20.7% were not using contraception. We examined the distribution of preferred method use, content nonuse, prospective use, and desired discontinuation in the following year by these 3 categories (most or moderately effective method use, other method use, and no contraceptive use). Among those using most or moderately effective contraceptive methods, 69.2% were using their preferred method, compared to 55.6% of those using another contraceptive method. Among those not using contraception, most (61.8%) were content nonusers, whereas 20.6% were prospective users who were interested in using contraception. Regarding discontinuation, among those using contraception, a majority of both users of most or moderately effective methods and users of other methods did not report a desire to stop use of their most effective method in the following year. However, there were still sizable proportions of individuals in both groups who indicated a clear or possible desire to stop using their current most effective method in the following year—11.8% of most or moderately effective method users and 20.4% of users of other methods had clear desires to discontinue, whereas 19.6% of most or moderately effective method users and 27.1% of other method users indicated that they might want to discontinue.
| Contraceptive use and preferences | Using a most or moderately effective contraceptive method (unweighted n=1237) , unweighted n (weighted %) | Using other contraceptive method (unweighted n=641) , unweighted n (weighted %) | Not using contraception (unweighted n=515) , unweighted n (weighted %) | ||||
| Using preferred contraceptive method | 875 (69.2) | 350 (55.6) | — | ||||
| Content nonuser (does not want to use contraception) | — | — | 320 (61.82) | ||||
| Prospective user (nonuser who wants to use contraception) | — | — | 99 (20.59) | ||||
| Uncertain nonuser (unsure whether they want to use contraception) | — | — | 95 (17.59) | ||||
| Yes | 151 (11.82) | 124 (20.35) | — | ||||
| As soon as possible | 37 (3.14) | 41 (7.72) | — | ||||
| No | 853 (68.61) | 338 (52.52) | — | ||||
| Maybe | 218 (19.57) | 176 (27.12) | — | ||||
a Respondents with missing data were excluded from cross-tabulations. The conventional metric was use of most or moderately effective contraceptive methods; the denominator was restricted to those who had ever had penile-vaginal sex.
b 51.64% of those included in the conventional metric denominator; population size estimate: 17,997,224.
c 27.65% of those included in the conventional metric denominator; population size estimate: 9,637,152.
d 20.71% of those included in the conventional metric denominator; population size estimate: 7,218,624.
e For multiple method users, this metric reflects whether the individual wants to maintain use of all their methods.
f Category not applicable. Those not using contraception are not included in numerator of the preferred method use metric, which focuses on current users who want to maintain use of their methods. Those using a moderately or most effective method or another method are not nonusers.
g This represents a mutually exclusive variable describing whether respondents would like to stop using their most effective current contraceptive method. It is independent of the Centers for Disease Control and Prevention designation of most or moderately effective methods.
In our comparative analysis, we first examined where the denominators of the person-centered metric and conventional metrics converged and diverged by determining whether individuals would be included in the denominators for both metrics (subgroup 1), excluded from both (subgroup 2), included only in the conventional metric (subgroup 3), or included only in the person-centered metric (subgroup 4; Figure 1 ). We found alignment across the 2 metrics for most of the sample—66.3% of respondents were included in both metric denominators (subgroup 1), and 12.7% were excluded from both (subgroup 2; Table 4 ). These 2 subgroups represent an estimated nearly 35 million individuals. About 13% of the analytic sample met inclusion criteria only for the conventional metric denominator (population estimate: 5.7 million individuals; subgroup 3); this subgroup exclusively comprised content nonusers who had ever had penile-vaginal sex. Finally, subgroup 4 included 8% of the analytic sample included only in the person-centered metric denominator. Subgroup 4 included current or prospective contraceptive users who had never had penile-vaginal sex (population estimate: 3.5 million individuals); despite their current or desired contraceptive use, they did not meet inclusion criteria for the conventional metric denominator. Examining these 2 divergent subgroups highlights fundamental differences in assumptions of the metrics regarding who is seen as being in need of contraception.
| Age and sexual and reproductive health characteristics | Convergence between the 2 metrics | Divergence between the 2 metrics | ||||||||||
| Subgroup 1 : included in both metrics (unweighted n=1977), unweighted n (weighted %) | Subgroup 2 : excluded from both metrics (unweighted n=212), unweighted n (weighted %) | Subgroup 3 : included only in the conventional metric (unweighted n=416), unweighted n (weighted %) | Subgroup 4 : included only in the person-centered metric (unweighted n=155), unweighted n (weighted %) | value (comparing subgroups 3 and 4) | ||||||||
| <.001 | ||||||||||||
| 15-17 | 51 (5.34) | 97 (48.27) | 13 (5.55) | 40 (30.03) | ||||||||
| 18-24 | 198 (26.82) | 42 (34.99) | 28 (16.64) | 28 (39.09) | ||||||||
| 25-29 | 431 (22.55) | 32 (10.24) | 72 (21.41) | 39 (14.79) | ||||||||
| 30-34 | 497 (20.54) | 19 (3.3) | 100 (20.53) | 21 (6.62) | ||||||||
| 35-39 | 453 (13.67) | 12 (1.8) | 110 (18.87) | 23 (8.23) | ||||||||
| 40-44 | 347 (11.08) | 10 (1.4) | 93 (16.98) | 4 (1.23) | ||||||||
| — | ||||||||||||
| Never had penile-vaginal sex | 0 (0) | 209 (100) | 0 (0) | 144 (100) | ||||||||
| Had penile-vaginal sex in the last year | 1839 (92.21) | 0 (0) | 258 (61.56) | 0 (0) | ||||||||
| Had penile-vaginal sex more than a year ago | 128 (7.40) | 0 (0) | 152 (37.31) | 0 (0) | ||||||||
| Had penile-vaginal sex; missing timing of last sexual encounter | 10 (0.39) | 0 (0) | 6 (0.11) | 0 (0) | ||||||||
| .02 | ||||||||||||
| In the next year | 225 (8.96) | 4 (1.04) | 68 (12.7) | 7 (2.78) | ||||||||
| More than a year from now | 540 (36.78) | 73 (38.83) | 119 (35.57) | 51 (38.68) | ||||||||
| Does not know | 387 (19.88) | 58 (26.4) | 126 (30.96) | 41 (28.68) | ||||||||
| Does not ever want to become pregnant | 822 (34.38) | 76 (33.73) | 103 (20.78) | 53 (29.87) | ||||||||
| — | ||||||||||||
| 1878 (94.9) | 0 (0) | 0 (0) | 110 (67.93) | |||||||||
| Using preferred contraceptive method | 1225 (61.05) | — | — | 69 (42.91) | ||||||||
| Wants to use different or no method or stop using any current method as soon as possible | 403 (21.84) | — | — | 20 (12.48) | ||||||||
| Uncertain user (unsure whether they prefer using a different or no method) | 246 (11.84) | — | — | 20 (12.06) | ||||||||
| 99 (5.11) | 212 (100) | 416 (100) | 45 (32.07) | |||||||||
| Content nonuser (does not want to use contraception) | 0 (0) | 130 (59.25) | 320 (77.78) | 0 (0) | ||||||||
| Prospective user (nonuser who wants to use contraception) | 99 (5.10) | 0 (0) | 0 (0) | 45 (32.07) | ||||||||
| Uncertain nonuser (unsure whether they want to use contraception) | 0 (0) | 79 (38.73) | 95 (22.13) | 0 (0) | ||||||||
| Using any most or moderately effective method | 1237 (61.81) | 0 (0) | 0 (0) | 87 (55.19) | — | |||||||
a Respondents’ missing data were excluded from cross-tabulations.
b Convergence indicates that individuals were treated the same by both metrics, either included (subgroup 1) or excluded (subgroup 2) from both denominators.
c Divergence indicates that individuals were treated differently by the two metrics, only included in the conventional metric denominator (subgroup 3) or only included in the person-centered metric denominator (subgroup 4). Rao-Scott–corrected chi-square tests are presented to compare differences between the 2 divergent subgroups (3 and 4) for age and ideal time to become pregnant.
d 66.27% of full analytic sample; population size estimate: 29,119,287.
e 12.67% of full analytic sample; population size estimate: 5,565,741.
f 13.05% of full analytic sample; population size estimate: 5,733,713.
g 8.02% of full analytic sample; population size estimate: 3,523,450.
h Chi-square tests were not used for sexual activity, current contraceptive use, and current contraceptive use status because each of these cross-tabulations had a structural 0 cell size; that is, there were no respondents reflected in the cell due to the inclusion requirements for the subgroups.
i 9 respondents (unweighted n) were missing the contraceptive use or nonuse subtype.
j For multiple method users, this metric reflects whether the individual wants to maintain use of all their methods.
There were differences in age and SRH experiences among the divergent subgroups ( Table 4 ). Those included only in the person-centered metric denominator (subgroup 4) were disproportionately younger (eg, 69% were aged <25 years compared to 22.1% of those included only in the conventional metric denominator, subgroup 3). Regarding SRH experiences, the 2 divergent subgroups differed in history of penile-vaginal sex (a requirement for inclusion in the conventional metric). All respondents (100%) included only in the conventional metric denominator had previously had penile-vaginal sex, whereas no one included only in the person-centered metric denominator reported ever having penile-vaginal sex. More respondents included only in the conventional metric denominator expressed a desire to become pregnant in the following year (12.7%) compared to those included only in the person-centered metric denominator (2.8%).
Although excluded from the conventional metric, most individuals (67.9%) included only in the person-centered metric reported current contraceptive use. No individuals included only in the conventional metric denominator were prospective users compared to 32.1% of those included only in the person-centered metric denominator. Most respondents included only in the conventional metric were content nonusers (77.8%). For subgroup 4 (included only in the person-centered metric denominator), 42.9% of the respondents were current contraceptive users using their preferred method, whereas more than half (55.2%) were using a most or moderately effective method (primarily contraceptive pills or hormonal IUDs; data not shown).
Principal Findings
In our comparative analysis, we highlighted differences in who meets the inclusion criteria for the conventional metric focused on effective contraceptive method use and for a person-centered metric focused on use of preferred contraceptive method, demonstrating numerous limitations with and assumptions of the conventional approach. Most importantly, we found that 13% of individuals included in the conventional metric denominator expressly did not want to use contraception (translating to an estimated nearly 4.5 million individuals). Furthermore, given the narrow focus on pregnancy prevention as the key driver for understanding contraceptive access, the conventional metric excludes many who are currently using or want to use contraception but are not considered at risk of unintended pregnancy because they have never had penile-vaginal sex. At the population level, as highlighted by our analysis of divergence between the 2 metrics, this translates into an estimated >9 million individuals who may not be accurately represented by one of the most common contraceptive access metrics in the United States.
This analysis highlights the implications of the assumptions of the HP2030 inclusion criteria. First, the denominator for the conventional metric includes individuals whose behaviors are aligned with their desires—they are not using contraception, nor do they want to use contraception. These content or autonomous nonusers’ [ 29 ] preferences are explicitly ignored when those who develop or set contraceptive programs or policies deem this group to be unsuccessful in the metric of effective contraceptive use, essentially targeting this group’s contraceptive behavior as needing to be changed from nonuse to use. Although person-centered data on autonomous nonuse are lacking, we know that some people may not have a found a method that meets their needs [ 19 ] or may be open to the possibility of pregnancy [ 20 ], and others may feel that abortion is an acceptable and feasible outcome should they unexpectedly become pregnant [ 58 ]. Second, the denominator for the conventional metric excludes individuals who have never had penile-vaginal sex, implying that they have no need for contraception because they are presumed to not be at risk of unintended pregnancy and overlooking broad evidence indicating that people use contraception for a variety of reasons, including but not limited to pregnancy prevention. For example, in 2022, a total of 39% of adult female contraceptive users in the United States used their method for a reason beyond just pregnancy prevention, such as menstruation management, managing a medical condition, or prevention of sexually transmitted infections [ 20 ]. Our findings bolster this evidence base; higher levels of contraceptive use among individuals included in the person-centered metric compared to those included in the conventional metric highlight that the former is more broadly inclusive of the range of individuals using contraception for any reason and that the latter is missing people who are using or want to use contraception. Centering SRH equity in contraceptive access and public health goals ensures that everyone who self-identifies a possible need for contraception can obtain it and any related services (including contraceptive care to fulfill the need to switch and discontinue use of methods).
Individuals’ preferences for switching and discontinuing their methods further reveal the limitations of the conventional approach used in HP2030. We found that, among users of a most or moderately effective method within the conventional metric sample, over a quarter were not classified as using their preferred method, and almost one-third wanted to potentially or definitely stop using their current method within a year. This finding highlights another limitation of the conventional metric approach, which implicitly frames use of effective contraceptive methods as successful—focusing on use of these specific methods without accounting for preferences or recognizing the dynamic nature of contraceptive use masks the contraceptive needs of this purportedly successful group. Moreover, among those using other contraceptive methods, more than half were using their preferred method; among those using no method, 62% did not want to use contraception. Importantly, although there were lower rates of desired switching and discontinuation among those using most or moderately effective methods compared to those using other methods or no methods, these percentages still translated to larger overall population estimates with unfulfilled preferences within the group of individuals using most or moderately effective methods. This highlights another key limitation of the conventional focus on increasing use of effective contraception: those considered unsuccessful because they are not using a most or moderately effective contraceptive method are often enacting their preferences. Therefore, targeting them for increased use undermines reproductive autonomy and does not align with SRH equity.
Our comparative analysis highlights the importance of integrating contraceptive preferences into metrics to monitor contraceptive need and access and inform policy and program strategies, both for ensuring appropriate access to high-quality services and to advance SRH equity. Strengths of this work include the intentional and diverse input and feedback that contributed to shaping the survey design and, especially, the preferred method use metric examined in this analysis. The person-centered focus of the survey allowed us to examine contraceptive preferences within the sample, highlighting a significant number of individuals who are misrepresented using the conventional metric approach. Inclusion of items regarding preferences for contraceptive initiation among nonusers and switching and discontinuation among current users revealed important insights about the assumptions of conventional approaches to public health goals and metrics that frame use of certain methods as a universal good. Finally, leveraging recent, nationally representative data to examine the 2 metrics in the comparative analysis allows us to broadly generalize our findings to today’s landscape of contraceptive access and how progress toward increased access is being measured at the national level.
Comparison With Prior Work
While we are aware of no other studies focused on the United States that compare a conventional measurement approach to a person-centered one, prior work examining the concept of unmet need has similarly found substantial misclassification of individuals’ contraceptive needs when metrics are based on assumptions about who should be using contraception with no consideration of the preferences of these presumed users. Unmet need is a population-level metric, typically focused on women in the Global South, that ostensibly claims to identify the population that needs contraception [ 59 ]. This need is determined based on demographic characteristics (gender and age) and sexual behavior and neglects whether individuals want to use contraception. A study by Senderowicz and Maloney [ 60 ] used data from 7 sub-Saharan African countries and found that most individuals classified as having an unmet need for contraception did not express a desire to use contraception. In this same vein, a 1972 paper by Blake and Das Gupta [ 61 ] found that unmet need estimates misclassified 74% of the 4.6 million US women who were poor or near poor and presumed to have an unmet need for contraception.
In our analyses as well as in other research, people who do not identify as women or heterosexual report contraceptive use and preferences regarding use. Indeed, gender-expansive and queer individuals experience greater barriers to accessing contraception [ 30 - 33 , 62 , 63 ], so their contraceptive needs should be included, understood, and prioritized in any initiative seeking to integrate an SRH equity lens into ensuring contraceptive access. In addition, a broader focus beyond pregnancy prevention highlights the importance of including young people in contraceptive access metrics, including adolescents even aged <15 years, who are not represented in our data set or in the contraception-related Healthy People objectives but who may be using (or want to use) contraception for menstruation or acne management even if they are not sexually active [ 22 ].
Limitations
Importantly, individuals assigned female sex at birth who personally use permanent contraception were not included in the survey sample, and thus, these findings cannot be generalized to this group of contraceptive users. Other research highlights that some permanent contraception users express a desire for their sterilization procedures to be reversed [ 64 ], which is important to give voice to even though permanent contraception is not a modifiable contraceptive method. The lower levels of use of most or moderately effectively methods in the conventional metric sample (52% among those aged 15-44 years) compared to national levels most recently cited in HP2030 (62% among those aged 20-44 years) likely reflect difference between the samples based on exclusion or inclusion of individuals who had undergone sterilization procedures [ 5 ]. As a result, our comparative analysis is not an exact estimation of the 2 different approaches with the full ideal populations for both metrics; still, this comparative analysis provides valuable information about the assumptions of the conventional approach. The person-centered metric is not without limitations [ 53 ]. It represents contraceptive use preferences at one moment in time, whereas it may be useful for policy purposes to capture self-identified need over 12 months. In addition, the primary survey question to assess use of preferred method could be further refined by adding the timing of “right now” to the primary question to ensure that individuals desire to use these methods currently and using follow-up questions to understand uncertain responses.
Conclusions
Uptake of methods highly effective for pregnancy prevention, such as long-acting reversible contraception, is frequently cast as a success for contraceptive programs and clinical practice [ 42 ]. However, this framing—reflected in the HP2030 objectives and associated metrics that emphasize use of most or moderately effective methods for pregnancy prevention—neglects individuals’ contraceptive preferences, resulting in programs and policies that do not reflect the priorities of the individuals they seek to serve. Importantly, the population estimates for the 2 metrics were relatively similar, suggesting that the person-centered approach does not significantly decrease the estimated population potentially in need of contraception but rather more precisely identifies it.
Building programs and policies around public health goals and metrics that are not aligned with priorities and preferences of those reflected in the measures is, at best, ineffective and wasteful and, at worst, in violation of people’s autonomy and misaligned with SRH equity. We do not have to look too far back in history to identify examples of how programs or policies that ostensibly were set up in service of increasing contraceptive access veered from this objective and toward problematic justifications for increasing use of specific, effective methods for certain low-income populations via poverty reduction arguments [ 39 , 65 , 66 ]. These examples demonstrate how even the seemingly benign and objective act of constructing metrics is not without subjectivity and can perpetuate inequities rather than help reduce or eradicate them.
National public health objectives and metrics focused on contraceptive access should be informed by SRH equity and center people’s preferences regarding which methods they choose to use and be value neutral about these choices [ 1 ]; current metrics that set goals around use of effective methods meet neither of these criteria and, instead, embed externally set assumptions about which methods are best. Healthy People reflects the public health goals of the United States and is just one of many initiatives that could benefit from a close examination of its objectives and related metrics for alignment with the principles of SRH equity. Our results suggest possibilities for Healthy People and contraceptive access efforts broadly to align program and policy efforts with SRH equity to support people in achieving reproductive autonomy and guard against efforts that perpetuate reproductive injustices.
Acknowledgments
This research was supported by Arnold Ventures. The funder did not have a role in manuscript writing or the decision to submit for publication. The authors thank the members of the Person-Centered Contraceptive Access Metrics Working Group for contributing their time and expertise to develop the priority metrics. Thank you to Drs Cassondra Marshall (coinvestigator) and Jennet Arcara for their work designing and implementing the Person-Centered Contraceptive Access Metrics study and to Stephanie Arteaga for reviewing an earlier version of this manuscript. The authors also thank Brenda Mathias, Mayra Cazares-Minero, and Alex Schulte for supporting data collection and analysis. MK’s affiliation is included for informational purposes only; this work was not conducted under the auspices of the Guttmacher Institute. The views expressed herein are those of the authors and do not necessarily reflect the views of the Guttmacher Institute.
Data Availability
The data sets analyzed during this study will be available in the Open Science Framework repository [ 67 ].
Conflicts of Interest
None declared.
Checklist for Reporting Results of Internet E-Surveys.
Data inputs and exclusions for 3 metrics to examine contraceptive access drawing on an existing population-level metric used in Healthy People 2030 and 2 metrics used in this analysis.
- Hart J, Crear-Perry J, Stern L. US sexual and reproductive health policy: which frameworks are needed now, and next steps forward. Am J Public Health. Jun 2022;112(S5):S518-S522. [ CrossRef ] [ Medline ]
- Stern L, Sterile H, Nguyen D, Moskosky S, Hart J. What is sexual and reproductive health equity and why does it matter for nurse practitioners? National Association of Nurse Practitioners in Women's Health. Nov 2021. URL: https://www.partners4healthequity.com/resource-library/what-sexual-and-reproductive-health-equity-and-why-does-it-matter-nurse [accessed 2023-07-17]
- Levesque JF, Harris MF, Russell G. Patient-centred access to health care: conceptualising access at the interface of health systems and populations. Int J Equity Health. Mar 11, 2013;12:18. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Increase the proportion of adolescent females at risk for unintended pregnancy who use effective birth control — FP‑11. Office of Disease Prevention and Health Promotion, Office of the Assistant Secretary for Health, Office of the Secretary, U.S. Department of Health and Human Services. URL: https://health.gov/healthypeople/objectives-and-data/browse-objectives/family-planning/increase-proportion-adolescent-females-risk-unintended-pregnancy-who-use-effective-birth-control-fp-11 [accessed 2024-02-16]
- Increase the proportion of women at risk for unintended pregnancy who use effective birth control — FP‑10. Office of Disease Prevention and Health Promotion, Office of the Assistant Secretary for Health, Office of the Secretary, U.S. Department of Health and Human Services. URL: https://health.gov/healthypeople/objectives-and-data/browse-objectives/family-planning/increase-proportion-women-risk-unintended-pregnancy-who-use-effective-birth-control-fp-10 [accessed 2024-02-16]
- History of Healthy People. Office of Disease Prevention and Health Promotion, Office of the Assistant Secretary for Health, Office of the Secretary, U.S. Department of Health and Human Services. URL: https://health.gov/our-work/national-health-initiatives/healthy-people/about-healthy-people/history-healthy-people [accessed 2024-02-24]
- Healthy People 2030 questions and answers. Office of Disease Prevention and Health Promotion, Office of the Assistant Secretary for Health, Office of the Secretary, U.S. Department of Health and Human Services. URL: https://health.gov/our-work/national-health-initiatives/healthy-people/healthy-people-2030/questions-answers#q2 [accessed 2024-02-12]
- Family planning. Office of Disease Prevention and Health Promotion, Office of the Assistant Secretary for Health, Office of the Secretary, U.S. Department of Health and Human Services. URL: https://health.gov/healthypeople/objectives-and-data/browse-objectives/family-planning [accessed 2024-02-16]
- Aiken AR, Borrero S, Callegari LS, Dehlendorf C. Rethinking the pregnancy planning paradigm: unintended conceptions or unrepresentative concepts? Perspect Sex Reprod Health. Sep 2016;48(3):147-151. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Gómez AM, Arteaga S, Villaseñor E, Arcara J, Freihart B. The misclassification of ambivalence in pregnancy intentions: a mixed-methods analysis. Perspect Sex Reprod Health. Mar 2019;51(1):7-15. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Gomez AM, Arteaga S, Freihart B. Structural inequity and pregnancy desires in emerging adulthood. Arch Sex Behav. Aug 2021;50(6):2447-2458. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Harris LH, Wolfe T. Stratified reproduction, family planning care and the double edge of history. Curr Opin Obstet Gynecol. Dec 2014;26(6):539-544. [ CrossRef ] [ Medline ]
- Kost K, Zolna M, Murro R. Pregnancies in the United States by desire for pregnancy: estimates for 2009, 2011, 2013, and 2015. Demography. Jun 01, 2023;60(3):837-863. [ CrossRef ] [ Medline ]
- Auerbach SL, Coleman-Minahan K, Alspaugh A, Aztlan EA, Stern L, Simmonds K. Critiquing the unintended pregnancy framework. J Midwifery Womens Health. Mar 2023;68(2):170-178. [ CrossRef ] [ Medline ]
- Dehlendorf C, Perry JC, Borrero S, Callegari L, Fuentes L, Perritt J. Meeting people's pregnancy prevention needs: let's not force people to state an "intention". Contraception. Jul 2024;135:110400. [ CrossRef ] [ Medline ]
- US Medical Eligibility Criteria for contraceptive use, 2016 (US MEC). Centers for Disease Control and Prevention. 2016. URL: https://www.cdc.gov/reproductivehealth/contraception/mmwr/mec/summary.html [accessed 2024-03-01]
- Increase the proportion of women at risk for unintended pregnancy who use effective birth control — FP‑10: data methodology and measurement. Office of Disease Prevention and Health Promotion, Office of the Assistant Secretary for Health, Office of the Secretary, U.S. Department of Health and Human Services. URL: https://health.gov/healthypeople/objectives-and-data/browse-objectives/family-planning/increase-proportion-women-risk-unintended-pregnancy-who-use-effective-birth-control-fp-10/data-methodology [accessed 2024-01-08]
- Downey MM, Arteaga S, Villaseñor E, Gomez AM. More than a destination: contraceptive decision making as a journey. Womens Health Issues. 2017;27(5):539-545. [ CrossRef ] [ Medline ]
- Jackson AV, Karasek D, Dehlendorf C, Foster DG. Racial and ethnic differences in women's preferences for features of contraceptive methods. Contraception. May 2016;93(5):406-411. [ CrossRef ] [ Medline ]
- Frederiksen B, Ranji U, Long M, Diep K, Salganicoff A. Contraception in the United States: a closer look at experiences, preferences, and coverage. Kaiser Family Foundation. Nov 3, 2022. URL: https://www.kff.org/report-section/contraception-in-the-united-states-a-closer-look-at-experiences-preferences-and-coverage-findings/ [accessed 2022-11-11]
- Kavanaugh ML, Pliskin E, Hussain R. Associations between unfulfilled contraceptive preferences due to cost and low-income patients' access to and experiences of contraceptive care in the United States, 2015-2019. Contracept X. May 6, 2022;4:100076. [ FREE Full text ] [ CrossRef ] [ Medline ]
- 2023 #ThxBirthControl survey data. Power to Decide. URL: https://powertodecide.org/what-we-do/information/resource-library/2023-thxbirthcontrol-survey-data [accessed 2024-02-13]
- Borrero S, Nikolajski C, Steinberg JR, Freedman L, Akers AY, Ibrahim S, et al. "It just happens": a qualitative study exploring low-income women's perspectives on pregnancy intention and planning. Contraception. Feb 2015;91(2):150-156. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Gomez AM, Arteaga S, Ingraham N, Arcara J, Villaseñor E. It's not planned, but is it okay? the acceptability of unplanned pregnancy among young people. Womens Health Issues. 2018;28(5):408-414. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Helfferich C, Gerstner D, Knittel T, Pflügler C, Schmidt F. Unintended conceptions leading to wanted pregnancies - an integral perspective on pregnancy acceptance from a mixed-methods study in Germany. Eur J Contracept Reprod Health Care. Jun 2021;26(3):227-232. [ CrossRef ] [ Medline ]
- Manze MG, Romero DR, De P, Hartnett J, Roberts L. The association of pregnancy control, emotions, and beliefs with pregnancy desires: a new perspective on pregnancy intentions. PLoS One. Mar 23, 2021;16(3):e0249032. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Arteaga S, Caton L, Gomez AM. Planned, unplanned and in-between: the meaning and context of pregnancy planning for young people. Contraception. Jan 2019;99(1):16-21. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Hernandez ND, Chandler R, Nava N, Tamler I, Daley EM, Baldwin JA, et al. Young adult US-born Latina women's thoughts, feelings and beliefs about unintended pregnancy. Cult Health Sex. Aug 2020;22(8):920-936. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Senderowicz L. Contraceptive autonomy: conceptions and measurement of a novel family planning indicator. Stud Fam Plann. Jun 2020;51(2):161-176. [ CrossRef ] [ Medline ]
- Norris M, Borneskog C. The cisnormative blindspot explained: healthcare experiences of trans men and non-binary persons and the accessibility to inclusive sexual and reproductive healthcare, an integrative review. Sex Reprod Healthc. Jun 2022;32:100733. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Agénor M, Cottrill AA, Kay E, Janiak E, Gordon AR, Potter J. Contraceptive beliefs, decision making and care experiences among transmasculine young adults: a qualitative analysis. Perspect Sex Reprod Health. Mar 2020;52(1):7-14. [ CrossRef ] [ Medline ]
- Fix L, Durden M, Obedin-Maliver J, Moseson H, Hastings J, Stoeffler A, et al. Stakeholder perceptions and experiences regarding access to contraception and abortion for transgender, non-binary, and gender-expansive individuals assigned female at birth in the U.S. Arch Sex Behav. Oct 2020;49(7):2683-2702. [ CrossRef ] [ Medline ]
- Gomez AM, Hooker N, Olip-Booth R, Woerner P, Ratliff GA. "It's being compassionate, not making assumptions": transmasculine and nonbinary young adults' experiences of "women's" health care settings. Womens Health Issues. 2021;31(4):324-331. [ CrossRef ] [ Medline ]
- Dehlendorf C, Grumbach K, Schmittdiel JA, Steinauer J. Shared decision making in contraceptive counseling. Contraception. May 2017;95(5):452-455. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Amico JR, Bennett AH, Karasz A, Gold M. "I wish they could hold on a little longer": physicians' experiences with requests for early IUD removal. Contraception. Aug 2017;96(2):106-110. [ CrossRef ] [ Medline ]
- Brandi K, Woodhams E, White KO, Mehta PK. An exploration of perceived contraceptive coercion at the time of abortion. Contraception. Apr 2018;97(4):329-334. [ CrossRef ] [ Medline ]
- Mann ES. The power of persuasion: normative accountability and clinicians’ practices of contraceptive counseling. SSM Qual Res Health. Dec 2022;2:100049. [ CrossRef ]
- Manzer JL, Bell AV. The limitations of patient-centered care: the case of early long-acting reversible contraception (LARC) removal. Soc Sci Med. Jan 2022;292:114632. [ CrossRef ] [ Medline ]
- Eeckhaut M, Hara Y. Reproductive oppression enters the twenty-first century: pressure to use long-acting reversible contraception (LARC) in the context of “LARC first”. Socius. Jun 22, 2023;9. [ CrossRef ]
- Donnelly K. Patient-centered or population-centered? How epistemic discrepancies cause harm and sow mistrust. Soc Sci Med. Jan 2024;341:116552. [ CrossRef ] [ Medline ]
- Gomez AM, Wapman M. Under (implicit) pressure: young Black and Latina women's perceptions of contraceptive care. Contraception. Oct 2017;96(4):221-226. [ CrossRef ] [ Medline ]
- Gomez AM, Fuentes L, Allina A. Women or LARC first? Reproductive autonomy and the promotion of long-acting reversible contraceptive methods. Perspect Sex Reprod Health. Sep 2014;46(3):171-175. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Berglas NF, Kimport K, Mays A, Kaller S, Biggs MA. "It's worked well for me": young women's reasons for choosing lower-efficacy contraceptive methods. J Pediatr Adolesc Gynecol. Jun 2021;34(3):341-347. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Coombe J, Harris ML, Loxton D. Motivators of contraceptive method change and implications for long-acting reversible contraception (non-)use: a qualitative free-text analysis. Sex Reprod Healthc. Mar 2019;19:71-77. [ CrossRef ] [ Medline ]
- Gomez AM, Arteaga S, Aronson N, Goodkind M, Houston L, West E. No perfect method: exploring how past contraceptive methods influence current attitudes toward intrauterine devices. Arch Sex Behav. May 2020;49(4):1367-1378. [ CrossRef ] [ Medline ]
- Higgins JA, Wright KQ, Turok DK, Sanders JN. Beyond safety and efficacy: sexuality-related priorities and their associations with contraceptive method selection. Contracept X. Aug 19, 2020;2:100038. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Institute of Medicine, Committee on Quality of Health Care in America. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC. National Academies Press; 2001.
- Daniels K, Mosher WD. Contraceptive methods women have ever used: United States, 1982-2010. Natl Health Stat Report. Feb 14, 2013;(62):1-15. [ FREE Full text ] [ Medline ]
- Darney BG, Biel FM, Oakley J, Coleman-Minahan K, Cottrell EK. Contraceptive method switching and long-acting reversible contraception removal in U.S. safety net clinics, 2016-2021. Obstet Gynecol. Sep 01, 2023;142(3):669-678. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Simmons RG, Baayd J, Waters M, Diener Z, Turok DK, Sanders JN. Assessing contraceptive use as a continuum: outcomes of a qualitative assessment of the contraceptive journey. Reprod Health. Feb 15, 2023;20(1):33. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Welti K, Manlove J, Finocharo J, Faccio B, Kim L. Women's experiences with person-centered family planning care: differences by sociodemographic characteristics. Contracept X. Jul 25, 2022;4:100081. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Burke KL, Potter JE. Meeting preferences for specific contraceptive methods: an overdue indicator. Stud Fam Plann. Mar 2023;54(1):281-300. [ CrossRef ] [ Medline ]
- Gomez AM, Bennett AH, Arcara J, Stern L, Bardwell J, Cadena D, et al. Estimates of use of preferred contraceptive method in the United States: a population-based study. Lancet Reg Health Am. Feb 2024;30:100662. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Gomez A, Marshall CJ. Person-centered contraceptive access metrics project. Sexual Health and Reproductive Equity Program. URL: https://share.berkeley.edu/person-centered-contraceptive-access/ [accessed 2024-08-06]
- Technical overview of the AmeriSpeak® panel NORC’s probability-based household panel. NORC at the University of Chicago. Feb 6, 2018. URL: https://d3qi0qp55mx5f5.cloudfront.net/amerispeak/i/research/AmeriSpeak_Technical_Overview_2018_02_06.pdf?mtime=1517969394 [accessed 2023-08-31]
- Eysenbach G. Improving the quality of web surveys: the Checklist for Reporting Results of Internet E-Surveys (CHERRIES). J Med Internet Res. Sep 29, 2004;6(3):e34. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Statistical software for data science. StataCorp LLC. 2021. URL: https://www.stata.com/ [accessed 2024-08-08]
- O'Donnell J, Goldberg A, Lieberman E, Betancourt T. "I wouldn't even know where to start": unwanted pregnancy and abortion decision-making in Central Appalachia. Reprod Health Matters. Dec 2018;26(52):1513270. [ CrossRef ] [ Medline ]
- Bradley SE, Casterline JB. Understanding unmet need: history, theory, and measurement. Stud Fam Plann. Jun 2014;45(2):123-150. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Senderowicz L, Maloney N. Supply-side versus demand-side unmet need: implications for family planning programs. Popul Dev Rev. Sep 2022;48(3):689-722. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Blake J, Das Gupta P. The fallacy of the five million women: a re-estimate. Demography. Nov 1972;9(4):569-587. [ Medline ]
- Agénor M, Pérez AE, Wilhoit A, Almeda F, Charlton BM, Evans ML, et al. Contraceptive care disparities among sexual orientation identity and racial/ethnic subgroups of U.S. women: a national probability sample study. J Womens Health (Larchmt). Oct 2021;30(10):1406-1415. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Higgins JA, Carpenter E, Everett BG, Greene MZ, Haider S, Hendrick CE. Sexual minority women and contraceptive use: complex pathways between sexual orientation and health outcomes. Am J Public Health. Dec 2019;109(12):1680-1686. [ CrossRef ] [ Medline ]
- Eeckhaut MC, Sweeney MM. Understanding sterilization regret in the United States: the role of relationship context. J Marriage Fam. Oct 2018;80(5):1259-1270. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Foster DG. The problems with a poverty argument for long-acting reversible contraceptive promotion. Am J Obstet Gynecol. Apr 2020;222(4S):S861-S863. [ CrossRef ] [ Medline ]
- Sawhill IV. Reducing poverty by cutting unplanned births. Brookings Institution. Aug 21, 2015. URL: https://www.brookings.edu/articles/reducing-poverty-by-cutting-unplanned-births/ [accessed 2021-01-16]
- Gomez AM, Bennett AH, Schulte A. Person-Centered Contraceptive Access Metrics Project. Open Science Framework. URL: https://osf.io/wvb5m/ [accessed 2024-08-07]
Abbreviations
| Healthy People 2030 |
| intrauterine device |
| sexual and reproductive health |
Edited by A Mavragani; submitted 14.03.24; peer-reviewed by K Burke, M Manze, J Strasser, R Steiner, C Rocca, A Steward; comments to author 09.04.24; revised version received 29.05.24; accepted 04.07.24; published 20.08.24.
©Anu Manchikanti Gomez, Reiley Diane Reed, Ariana H Bennett, Megan Kavanaugh. Originally published in JMIR Public Health and Surveillance (https://publichealth.jmir.org), 20.08.2024.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work, first published in JMIR Public Health and Surveillance, is properly cited. The complete bibliographic information, a link to the original publication on https://publichealth.jmir.org, as well as this copyright and license information must be included.
- Open access
- Published: 04 May 2023
Barriers to the participation of men in reproductive health care: a systematic review and meta-synthesis
- Robab Latifnejad Roudsari 1 , 2 ,
- Farangis sharifi 3 &
- Fatemeh Goudarzi 4 , 5
BMC Public Health volume 23 , Article number: 818 ( 2023 ) Cite this article
7920 Accesses
8 Citations
12 Altmetric
Metrics details
Despite emphasizing the importance and benefits of men's active engagement in reproductive health programs, their engagement in reproductive health care is low. Researchers have identified different barriers to men's avoidance of participation in various aspects of reproductive health in different parts of the world. This study provided an in-depth review of the hindrances to men’s non-participation in reproductive health.
This meta-synthesis was conducted using keyword searches in databases including PubMed, Scopus, Web of Science, Cochrane, and ProQuest until January 2023. Qualitative English-language studies that investigated barriers to men's participation in reproductive health were included in the study. The critical appraisal skills program (CASP) checklist was used to assess the articles' quality. Data synthesis and thematic analysis were done using the standard method.
This synthesis led to the emergence of four main themes such as failure to access all inclusive and integrated quality services, economic issues, couples' personal preferences and attitudes, and sociocultural considerations to seek reproductive healthcare services.
Healthcare system programs and policies, economic and sociocultural issues, and men’s attitudes, knowledge, and preferences, influence men's participation in reproductive healthcare. Reproductive health initiatives should focus on eliminating challenges to men's supportive activities to increase practical men's involvement in reproductive healthcare.
Peer Review reports
Reproductive health is a well-known family and social health component [ 1 ]. According to the definition of the World Health Organization, reproductive health means complete physical, mental, and social well-being in the functions and processes related to the reproductive system, not just the absence of disease and dysfunction or disability. Also, every person can have a good and safe sex life and freely decide about the time and manner of reproduction according to their desire [ 2 ]. From the mid-1990s until now, the importance and the benefits of men's active participation in reproductive health programs on the health of men, women, and children have been recognized and emphasized [ 3 ]. Despite the emphasis and importance of men's health in the definition of reproductive and sexual health, relatively few results for men's health have been obtained from this extensive reproductive health agenda [ 4 ]. In many studies, the role of men in reproductive health has been discussed based on women's health. Men effectively influence women's access to reproductive health care [ 5 ]. Commonly, Men make decisions about women's access to reproductive health care, money allocation for preventing the sexually transmitted diseases, family planning, and women's presence in antenatal and postpartum care, pregnancy and delivery care, transportation, nutrition, and child care [ 6 ].
The presence of women in reproductive health care, including family planning [ 7 ], antenatal care [ 8 ], safe motherhood [ 9 ], postpartum care [ 10 ], prevention of transition of HIV From mother to child(PMTC) [ 11 ], and sexually transmitted infections (STIs) [ 5 ] is often determined by their husbands. However, most men are not engaged in reproductive health care [ 7 ]. Franklin Ani (2015), reportedthe presence of men in reproductive health clinics was low (39.6%). He found that less than one-third of men (30.9%) participated in reproductive health-care [ 5 ]. Olayinka F.F et al. (2020) reported albeit most men were well aware of parenatal care, about 20% of them attended antenatal care with their partner, and (19.6%) participated in post-natal care [ 7 ]. Austin Wesevich et al. (2017) reported that male involvement in PMTC in Myanmar was 13% [ 12 ]. Also, Atuahene (2017) reported that most men (92.2%) did not accompany their wives to receive family planning services [ 9 ]. These quantitative studies provided numerical data about men's participation in reproductive health. These studies did not explain why men did not participate in reproductive health care [ 13 ]. Health system intervention and social, cultural, and economic factors are essential factors in the access and participation of people in reproductive and sexual health services [ 14 ]. We are witnessing different cultural, social, and economic contexts around the world that can make a difference in the access and participation of people, especially men. Thus, there is a need for a deep and detailed investigation of these factors and their impact on men's engagement in reproductive health services in different societies. Numerous qualitative research has explored men's participation in different aspects of reproductive health in various contexts [ 15 - 20 ]. They cited multiple reasons, such as reproductive health care as a feminine issue [ 15 , 20 ], cultural issues [ 15 , 18 , 20 ], occupational matters [ 15 , 18 , 20 ], and economic issues [ 18 , 20 ], were raised as male participation barriers to reproductive health.
Qualitative research helps to explore sentimental phenomena. Qualitative approaches provide the type of data that can help to understand participants' behaviors, feelings, and perceptions about the studied phenomena [ 21 ]. However, the small sample size has reduced the power of these studies to influence policymaking and planning. Another limitation of qualitative studies is the subjective interpretation of the data and the particular population studied, which challenges the transferability of the findings [ 13 ]. Synthesizing the data obtained from several qualitative studies is a way suggested by researchers to overcome the perceived limitations of qualitative approaches [ 22 ]. Meta-synthesis is a powerful method that examine qualitative studies and interprets and explains the phenomenon under study [ 22 ]. A systematic review of qualitative studies focuses on each unique phenomenon and its feedback. It identifies accurate evidence and summarizes it while appraising quality [ 23 ]. According toour knowledge a few studies have systematically reviewed men's participation in reproductive health through a meta-synthesis approach, including Louisa et al. (2014), who investigated men's views on contraception [ 24 ]. In this regard, the purpose of this study was to provide a comprehensive synthesis of views of women, men, and healthcare providers about barriers to men's engagement in reproductive health care that can help policy and planning to remove obstacles to male participation in reproductive health care. Thus, this study is looking for the answer to Why are men not involved in various aspects of reproductive health care?
This qualitative meta-synthesis was conducted according to the methods described by Noblit and Hare (1988) [ 25 ], and the thematic analysis approach described by Braun and Clarke (2006) [ 26 ]. The Noblit and Hare methods consist of seven steps: determining the research question, selecting the research studies related to the research topic, evaluating the studies, deciding on how the studies relate, translating the studies to each other, synthesizing the translated concepts, and presenting the synthesized findings (Table 1 ). The thematic analysis approach described by Braun and Clarke has six steps, including data familiarity, generating primary code, searching themes by reviewing primary code, reviewing emerging themes, defining emerging themes, and preparing Report. According to Noblit and Hare, the first step to conducting a meta-synthesis is determining the aim and topic of the study, so the research question was developed: Why are men not involved in various aspects of reproductive health care?
Search strategy
The databases, including PubMed, Scopus, Web of Science, Cochrane, and ProQuest, were searched, systematically. The search was performed using the MESH terms including "Male Participation" OR "Men Participation "OR "Male Involvement" OR" Men Involvement" OR "Male Engagement" OR “Men Engagement" AND "Reproductive Health Care" OR "Maternal Health " OR "Sexual Health" OR "Family Planning" OR "Child Health" AND "Qualitative Study". The reference for included studies was searched manually. All the original qualitative studies from January 1994 until January 2023, focusing on the barriers to men's engagement in reproductive health care, which were published in the English language and their full text was available, were included in the study. All Studies with a quantitative design, areview, and meta-analysis articles were excluded.
Study selection
The relevance of the articles with the research question was evaluated in several stages, such as the assessment ofthe title, the abstract, and the full text of the articles. This assessment was performed by two authors simultaneously. A total of 1966 articles were obtained from database searches. No article was found in the manual search. At each step of the screening, several studies were removed. The reasons for excluding the studies were the lack of relevance to the subject or the use of a quantitative approach. Finally, full-text screening was performed on 201 articles. Then, 47 qualitative articles related to the subject under study were selected. Figure 1 shows the process of study selection.
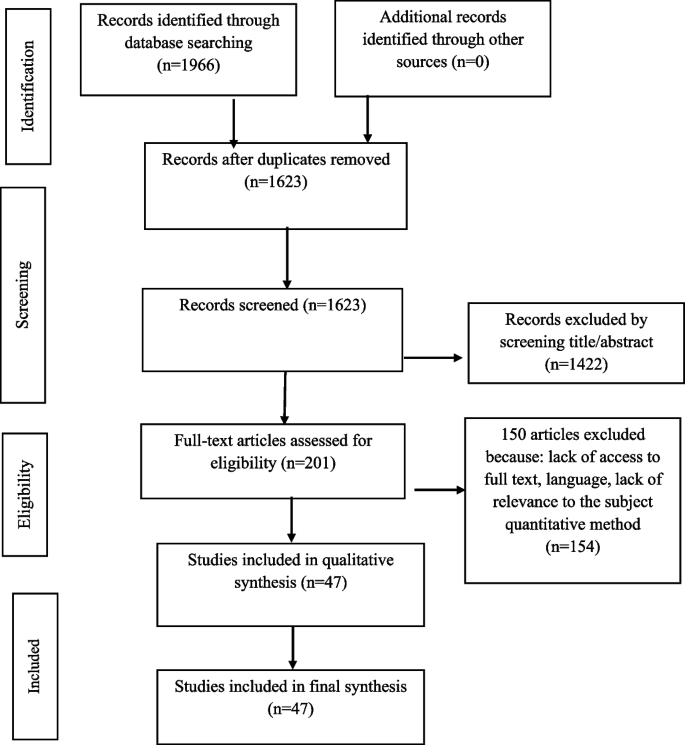
Preferred reporting items for systematic reviews and meta-analyses (PRISMA) flow diagram shows the s study selection process
Quality assessment
We considered the critical appraisal skills program tool (CASP version 2018) for appraising the selected studies [ 27 ]. Although the best way to evaluate the quality of qualitative articles is not agreed upon, in some meta-synthesis studies, the CASP checklist has been used to assess the article's quality [ 28 , 29 ]. The quality of the articles was assessed by two authors separately. In case of disagreements between these authors, the opinion of the third author was discussed to reach a consensus. Table 2 shows the result of the included articles' quality assessment. No study was excluded from the meta-synthesis based on the score obtained from the quality assessment. Overall, the included articles had reasonable quality.
Data extraction
The next step was to read the full text of each article identified for inclusion in the review and to extract the pertinent data using a standardized data extraction form. Data were extracted in collaboration with two authors (F.G and F.S). The extracted data included the author's name, year of publication, the purpose of the study, study population, country of study setting, study design, number of participants, method of analysis, the main focus of the studies, and study's main findings (Table 3 ).
Data synthesis
For the synthesis in this study, a combination of the classical meta-synthesis or meta-ethnography was adopted by Noblit and Hare (1988) [ 25 ], as well as Brown and Clark's (2006) thematic analysis approach [ 26 ], was used. This combination has been successfully used in previous reviews [ 28 , 29 ]. The approach described by Noblit and Hare [1988] focuses on the reciprocal translation, reliable synthesis, and lines of reasoning. Reciprocal translation analysis identifies concepts in each study, compares these concepts with those of other studies, and selects a comprehensive meaning that includes other similar meaning [ 26 ]. Although the Noblit and Hare approach are explained the seven steps of meta-synthesis and translations, the practical process of meta-synthesis of this approach is not clarified clearly Ed [ 67 ]. Studies have criticized this lack of expressiveness [ 67 , 68 ]. It has been discussed that sometimes it is impossible to implement a cross-translational study. For example, an approach such as "first identified translated first "or "oldest paper translated first" can be challenging in meta-synthesis especially, when there is a lot of data and different perspectives. In addition, it is difficult to ensure that the quality of an article that initiates the translation process is better than others. Sometimes it is difficult to agree on a high-quality study [ 69 , 70 ]. Sometimes, the translation process starts with an article, but that article may be conceptually weak, and this issue can affect subsequent translations [ 29 ]. To better manage the data and clarify the analysis process, we used the thematic analysis approach to modify steps 3–6 of the meta-synthesis adopted by Noblit and Hare approach (1988).
Thematic analysis was conducted based on Brown and Clark's approach (2006). It is a six-step process that focuses on examining themes in the text. So after entering the results of the studies in the software MAXQD (version 10), the researchers read the text several times to understand the meanings and patterns of the data. After getting acquainted with the data, the process of coding started. The initial codes were written by describing the label and determining its location (referenced). A list of described codes was prepared. The meaningful sections were identified by a systematic method. Then the data was reduced to mini-meaning units. The extracted codes were frequently compared with each other. The extracted initial codes were reviewed by the third author (R.L.R). The similar extracted codes (concepts) were categorized into subthemes. Then the main theme that covered sub-themes emerged. The main theme was evaluated and condensed in terms of meaningfulness, relevance with sub-themes, and relevance with the concept of the included studies. This step was conducted with the participation of all authors, and a consensus was reached through discussion. Finally, the themes were defined and interpreted. Then the synthesis of the data under each theme was completed that was supported by the evidence from included articles. Finally, the”line of argument” was conducted to clarify the linkages between the extracted concepts from the synthesis. Developing the theoretical insights helps understand the barriers that led to the lack of men's engagement in reproductive health care (Fig. 2 ).
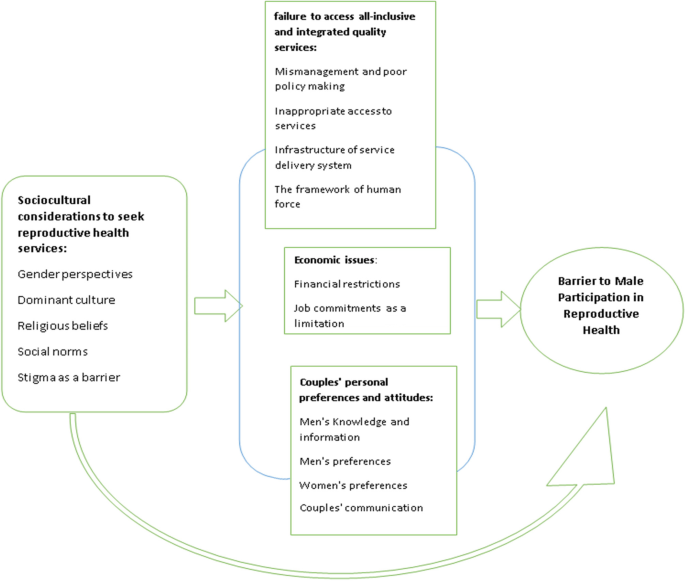
The illustrated conceptual model of the relationship between the identified barriers to men's participation in reproductive health care
Among 1966 articles, 47 studies met the inclusion criteria and were included in the synthesisThe included studies contain of data from 3051 participants. This data were collected using focus groups and in-depth semi-structured interviews. Study participants included men, women, health professionals, and society leaders. These studies examined various aspects of reproductive health care.
Characteristics of included studies
These studies were conducted in 24 countries, such as Tanzania (9 studies), Malawi (6 studies), Ghana (4 studies), Uganda (4 studies), Nigeria (4 studies), South Africa (2 studies), Iran (2 studies), western Kenya (1 study), Guatemala (1study), Ethiopia (1study), Zambia (1 study), Congo (1 study), India (1 study), Burkina Faso (1 study), Gambia (1 study), Bangladesh (1 study), Nepal (1study), Brazil (1 study), Australian (1 study), Pacific (1 study), Togo (1 study), USA (1study), and Eswatini (1 study). These studies focused on various aspects of reproductive health care, including maternal health care, family planning, prevention of transition of HIV from mother to child, sexual and reproductive health education, and maternal and infant health (Table 3 ).
Synthesis of findings
The synthesis of findings led to the emergence of four themes and 14 subthemes. These Themes included: failure to access all-inclusive and integrated quality services, economic issues, couples' personal preferences, and attitudes, as well as sociocultural considerations to seek reproductive health services (Table 4 ), which is elaborated in the following part.
Failure to access all-inclusive and integrated quality services
Based on the literature review, failure to access all-inclusive and integrated quality services was the main hindrance to male engagement in reproductive health care. The availability of health facilities and service environments, including programs, staff, equipment, and professional behaviors, are effective in the presence of men in reproductive health care. This theme emerged from four subthemes: Mismanagement and poor policy-making as hindrances, Inappropriate access to services, The Infrastructure of the service delivery system as a barrier, and the framework of human force.
Mismanagement and poor policy-making as hindrances
Most included studies which explored men's participation in reproductive health have been conducted in developing countries. In developing countries, most policies on various aspects of sexual and reproductive health are focused on women. Multiple studies have reported the neglect of men's participation, contrary to the needs of society, in the planning and macro policy-making in the field of reproductive and sexual health. This sub-theme refers to relevant issues to policy making and planning in reproductive and sexual health programs that prevent men from participating in reproductive health care.
Some articles pointed to the mismanagement during the implementation of reproductive health policies and programs that limit men's participation in reproductive health. Regarding the mismanagement, the following issues were reported in the studies. The men weren't allowed to take part in antenatal care [ 20 , 57 ]. They were not invited to reproductive health services [ 20 ]. Privacy in the design of healthcare facilities was Ignored [ 17 , 31 , 41 ]. Multiple services were offered adjacent to each other [ 31 , 41 ]. Health system factors banned men's participation in reproductive health [ 18 , 33 , 43 ]. The male reproductive needs didn't address[ 52 ]. The presence of a couple together in reproductive health care centers was ignored [ 17 , 33 , 38 , 39 , 43 ]. Healthcare policymakers didn't receive feedback from health workers [ 42 , 48 , 49 ]. In reproductive health services, the support for men's accommodation was ignored [ 42 ]. The men's interaction with the health system was restricted [ 40 ]. The participation of men in reproductive health care services wasn't supported [ 66 ]. Although men were a decisive agent in reproductive health, they were ignored in reproductive health services [ 66 ]. There weren't male-friendly reproductive health services [ 51 ]. There wasn't guidance to provide information for men on various aspects of reproductive health [ 51 ]. The support for performing instructions accurately was limited [ 51 ].
On the other hand, sometimes incomplete and ineffective policymaking has provided the ground for men's non-participation. Ineffective policies on various aspects of reproductive health cause insufficient support for men's participation in reproductive and sexual care. In different studies, this issue has been introduced as one of the obstacles to men's participation in reproductive health care. The Poor policy was described with phrases such as Lack of any target for engaging the men directly [ 20 , 31 , 42 , 49 ], lack of emphasis on the presence of men [ 17 , 20 ], and ignoring of men in the health recommendations [ 40 , 41 , 59 ], ignoring advice and services for men's reproductive health in policy [ 41 ], Lack of guidelines and standards for the presence of men in reproductive health [ 16 , 18 , 41 ], Applying personal preferences in management and policy-making [ 18 ], Governance of gender roles in reproductive health service [ 18 , 41 ], lack of guidelines for the mobilization of men [ 51 ], Limited interaction of key influential decision-makers in the health sector with the community [ 51 ].
We found a gap in translating policies to practice in the literature review, which pointed to poor planning. In the studies, this issue was described with these phrases: lack of education for men about the importance of reproductive health [ 37 , 66 ], design of maternal and child health programs as a limitation [ 47 ], failure to fulfill paternal leave [ 18 ], and lack of planning to achieve a comprehensive view of men's participation in health workers [ 51 ], lack of training, or no Instructions for male integration into health services [ 51 ].
Inappropriate access to services
Most of the studies included in this research were conducted in low resources countries. In these countries, transportation infrastructure is often not suitable. The residence of most people is far away from the main road. Sometimes these areas are difficult to pass. People are not able to pay the financial costs related to transportation. Also, most people live in rural areas. They engage in occupations such as agriculture. These people need to travel long distances to access health care. As a result, they may miss an entire day of work. These issues can lead to inappropriate access to reproductive health care. Improper access to services is one of the reasons described in most articles as a constraint on men's participation in reproductive health services. In included studies, Inappropriate access to reproductive health care was described in the following phrases: Reproductive health services take a long time [ 15 , 17 , 20 , 37 , 38 , 41 - 43 , 49 , 50 , 53 , 58 , 59 ]. Male clients had fewer opportunities for HIV testing [ 40 , 41 ]. In health centers, services were provided only in the morning [ 40 , 52 ]. The distance from home and work to health centers was long [ 16 , 17 , 35 , 44 , 52 , 53 , 65 ]. Access to services is not permanent for male participants [ 31 , 40 , 41 , 53 ]. Access to the centers is difficult due to poor road infrastructure [ 16 , 30 , 34 , 42 , 53 , 58 ]. Access to some services, such as family planning, was low [ 44 ].
The infrastructure of the service delivery system as a barrier (standard logistic equipment)
The customer-friendly environment is a crucial point in increasing the client’s participation in reproductive health clinics. Providing a customer-friendly environment, requires attention to the infrastructure. In the review of included studies in the field of infrastructure, issues such as the physical environment, equipment, costs of consumables, and the emotional aspect of the clinic space have been discussed. In all articles, participants described the physical environment of health centers as inappropriate for the presence of men. Included studies reported that counseling rooms in health centers are small. The small space of these rooms limits the privacy of clients [ 17 ]. There was no private space for men in the health centers [ 17 , 36 , 45 , 51 ]. There wasn't appropriate space for men in the reproductive health clinic [ 18 , 31 , 38 , 42 , 43 , 49 , 51 ]. Health centers have few seats. Often, there aren't seats for males to sit on [ 43 ].
In addition to the physical infrastructure, sometimes the emotional atmosphere of the clinics and the use of the space to implement care programs are unfriendly to the presence of men. Sometimes they are not welcoming to men in the environment of reproductive health clinics. Most articles have reported that another hindrance for men to participate in reproductive health care was the unfriendly atmosphere of centers, which led to the marginalization of male customers. The unfriendly environment of maternity care centers [ 30 , 36 , 45 ], the unwelcome clinic environment for men [ 38 , 49 , 52 , 53 , 57 ], the unfavorable feminine structure of healthcare clinics [ 40 , 46 , 55 , 66 ], Non-private centers [ 44 ], and the unattractive content of services and infrastructure of maternal care centers for men [ 19 ] were described by the male participant in the studies.
One of the factors in the availability of accessible healthcare services is accessibility in terms of health supplies and equipment. Lack of equipment hindered men's participation in reproductive health care. In some studies, participants stated that due to the lack of supplements and equipment in the centers [ 17 , 20 , 31 , 53 ], the restriction on the choice of available male contraceptive methods [ 68 ], the lack of equipment in the health center [ 31 ], the deficiency of diagnostic equipment [ 33 ], the shortage of medicine or equipment [ 53 ], did not participate in reproductive health care.
Plenty of reproductive health services in developing countries are provided free of charge or at a minimal cost. However, several studies have described the costs imposed on participants in reproductive health centers as an obstacle to men's participation in this service. In these studies, participants stated that they rarely referred to reproductive health centers due to fear of soliciting bribes [ 17 ], hidden costs for providing equipment [ 49 ], paying informal out-of-pocket costs [ 53 ], the opportunity costs [ 50 ], especially in areas where services were provided free of charge.
The framework of human force
Healthcare workers are one of the resources for providing reproductive health care. Healthcare workers provide care, education, and counseling services. However, studies have reported that healthcare workers are one of the barriers to men's participation in reproductive healthcare. This issue can be investigated from different aspects, such as Staff deficiency, negative staff attitude, improper staff behavior, and non-professional providing services.
The sufficient number of healthcare providers in reproductive health clinics is associated with the quality of service delivery. Some studies have reported a shortage of health workers as a hindrance to males participating in reproductive health care. The participants reported limited access to professional staff in remote areas [ 34 ]. Shortage of healthcare providers [ 17 , 31 , 43 , 48 ], shortage of male staff at reproductive health centers [ 18 , 36 ], inadequacy of male staff in clinics to train male clients [ 3 , 18 ], absence of healthcare workers [ 52 , 53 ], heavy workload of health staff [ 3 ] are issues that Challenge male participation in reproductive health services.
In addition to the number of staff, interpersonal communication skills and the attitude of staff towards the presence of men in reproductive health clinics affect the participation of men in reproductive health care. In the reviewed studies, unfriendly attitudes of health care providers were one of the factors preventing men from participating in reproductive health care. The unfriendly attitude of the personnel was described in the studies as negative attitudes towards males participating [ 3 , 18 , 30 , 36 , 42 , 43 , 49 , 53 , 60 ]. Unwelcoming attitude [ 31 ], non-acceptance of the presence of men [ 38 ], the presence of a male, that embarrasses female staffs [ 18 ], indifference to work [ 53 ], the potential mistreatment following the health providers negative attitudes [ 52 ] were described in studies. Also, participants explained that the mistreatment of healthcare providers towards women and their husbands reduced men's participation in healthcare. Participants described the misbehavior of healthcare workers as the use of heartless language [ 15 , 17 ], misbehavior [ 17 , 20 , 53 ], unprofessional behavior [ 31 ], mistreatment [ 17 , 41 ], unwelcome behavior [ 38 , 42 ], rude behavior [ 17 , 40 , 44 , 53 ], use of disrespectfullanguage [ 17 , 53 , 59 ], unpleasant behavior [ 48 ], use of harsh and sarcastic expressions [ 49 ].
In addition to the mistreatment of health care providers, care providance in an unprofessional manner makes men reluctant to participate in reproductive health care. The cases mentioned in the studies that confirm the unprofessional behavior of the health care providers are explained with expressions like a passiverole to provide the correct information [ 34 ], failure to state the reason for the importance of men's participation [ 40 ], lack of clear justification of advice for men [ 44 ], ignoring men’s fear and concern [ 44 , 49 ].
Economic issues
According to the literature review, studies have shown that men's economic status is another barrier to engaging theme in reproductive health care. This theme emerged from two sub-themes: financial restriction and job commitments as a limitation.
Financial restriction
The studies reviewed in this study were conducted in developing countries. In these countries, culturally, men are the main factor in decisions related to the health of their family members. Often, decisions about when, where, and how family members access healthcare are made by men. This particular position in decision-making process is related to the role of men as livelihood providers in their families. They are often the main decision-makers regarding the allocation of money for the availability of food, transportation, and costs associated with family members to attend health services. Therefore, as the head of the household, they prefer to being the provider. They prefer to provide necessities for life In these studies, this issue was raised this way. Participants, discussed the challenge of providing necessities for family and participation in reproductive health care [ 16 , 20 , 31 , 36 ]. Some participants cited the funding problem as the reason for inactiveparticipation [ 20 ].
Participants prefer to focus on economic and income-generating activities [ 16 , 36 , 48 , 61 ]. The norms of the community prefer to make money for the family [ 33 ]. Traditional health services for mothers were chosen because of financial issues [ 65 ]. Financial instabilities inhibited male involvement [ 42 ]. Poverty deprived people of the opportunity to choose to participate in PMTCT [ 35 ]. The cost of care prevented men from participating in reproductive health care [ 18 , 48 ]. Concerns about financial support for childcare hinder participation [ 57 ]. Also, the lack of insurance coverage for reproductive health services is one of the obstacles to men's participation [ 40 ].
Job commitments as a limitation
The opportunity cost of men presenting in health service centers instead of attending the workplace plays a significant role in men's decision to participate in reproductive health care. Economic factors affecting men's decision to participate in reproductive health services can be grouped into direct and indirect factors. The direct factors group was explained in the previous sub-theme. The indirect factors have further impact on the decision to attend reproductive health services. In studies, participants discussed the Contrast between job responsibilities with attending reproductive health care for themselves and their spouses. They stated that Job commitments cause a lack of time [ 17 , 31 , 36 - 38 , 40 , 46 , 49 , 53 , 58 , 60 , 63 , 65 ]. Leave requests to participate in antenatal care (ANC) from the employer's point is unusual [ 31 , 50 , 65 ]. It is difficult to adjust the time for accompanying the spouses due to work issues [ 50 , 65 ]. Work takes precedence over accompanying the spouse [ 36 , 46 ]. Men's working hours interfere with the working hours of care centers [ 3 , 38 ]. There is a conflict between financing maternal care and leaving work [ 18 , 61 , 65 ]. The male occupation limited spousal support [ 36 , 42 ].
Couples' personal preferences and attitudes
The preferences of couples, especially the male partner, affect men's participation in reproductive health services. According to the results of the present study, beliefs, attitudes, and interactions between spouses and individual factors such as embarrassment, anxiety, distress, and fear caused by inadequate knowledge were the factors that determine men's participation in reproductive health care. This theme explores the preferences of couples and the factors affecting them. This theme emerged from three sub-themes “Men's Knowledge and information”, “Couples’ Preference”, and “Couples' communications”.
Men's knowledge and information
Two factors that are important in health behavior are as follows:having health knowledge and access to health information. To increase knowledge, access to information plays an important role. Studies found that inadequate knowledge about reproductive health issues and insufficient information about what is done at the reproductive health centers make men give up accepting their responsibilities to participate in reproductive health care [ 15 - 18 , 34 - 36 , 44 , 48 , 52 , 54 , 71 ]. Also, inadequate knowledge about the cause of men's participation in maternity services [ 16 , 59 ] and deficiency of knowledge about the advantages of male participation in health services [ 31 , 55 ] prevented men from participating in these services. Male participation in reproductive health was influenced by misinformation [ 32 , 44 , 55 , 64 ], limited knowledge of the men's role in reproductive services [ 33 , 63 ], and lack of awareness about the importance of males' engagement in maternity care [ 18 , 34 , 36 , 58 ], and misunderstanding of reproductive services [ 62 , 71 ]. They occur due to men's lack of access to reliable sources of information.
Studies also discussed the cause of the deficiency of knowledge about healthcare. Inadequate family education for men's participation [ 18 , 40 ], lack of awareness, Poor family performance to encourage men to participate in reproductive health [ 40 ], and lack of training for men to participate in reproductive health [ 18 ] were the issues raised about lack of awareness. As a result of these issues, it becomes common to follow rumors about reproductive health services. On the other hand, existing knowledge about reproductive health services was not translated into practice [ 34 ].
Couples preferences
Men's preferences are effective intheir engagement in reproductive health care. Many studies have described male preferences as the reason for inactive participation in reproductive health care. In studies regarding the men's preferences, the expressions of unwillingness to participate in reproductive health care, and education [ 17 , 18 , 31 , 40 , 45 ], passive attitude to participation in pregnancy care [ 35 , 54 ], lack of motivation to engage in reproductive health [ 52 ], lack of feeling the need to participate in natural childbirth process [ 16 , 36 , 39 , 58 ], fear of HIV testing [ 17 , 31 , 38 , 43 , 45 , 50 , 53 ], shyness [ 3 , 18 , 31 , 34 , 36 , 40 , 46 , 49 , 55 , 57 , 58 , 66 ], negative attitude towards sexual issues [ 40 ], low Perceived risk [ 40 ], lack of perceived sensitivity to STDs [ 40 ], reluctance to attend a womanly clinic [ 43 ], inexperience about participating in maternal care [ 18 ], attending reproductive health centers as a time-wasting [ 49 ], being concern about privacy [ 31 , 35 , 42 , 43 ], being concern about the intentions of health providers [ 44 ] were used frequently.
In addition to men's preferences for non-participation in reproductive health care, some studies have reported the reluctance of female partners as one of the reasons for men's non-participation. Some female participants preferred to attend health centers alone. In Studies, the reasons for this issue have been described as feminine embarrassment [ 30 ], fear of the husband [ 30 ], ignoring the presence of men [ 45 , 63 ], and trusting their family [ 18 ]. Some female participants prevented males from participating in female-related duties [ 47 ]. They also did not ask their husbands to participate in reproductive health care [ 45 ]. They did not approve of their spouses' decision to have a vasectomy [ 32 ].

Couples' communications
The joint participation of couples can lead to improve use of reproductive health services. This issue requires communication between couples. The communication between couples helps them to be aware of each other's views on reproductive health services, which leads to mutual understanding. The mutual understanding allows them to agree on shared decision-making about reproductive health services. Inappropriate communication between couples makes men refuse to accompany their wives in reproductive health services. In the studies, expressions such as marital problems between couples [ 31 ], predetermined marriage without expressing love [ 31 , 59 ], lack of interest between spouses [ 31 ], lack of consultation between spouses and planning for pregnancy [ 31 ], nagging to the spouse while asking him to accompany [ 31 ], fear of men's extramarital relationship [ 41 ], marital dispute [ 31 , 35 ], poor relationship between couples [ 44 ], mistrust between spouses [ 18 ], inappropriate interaction between spouses [ 18 ] has been described as factors in preventing male engaging in reproductive health services with their spouses.
Sociocultural considerations to seek reproductive health services
The results of the reviewed studies have shown that socio-cultural structures can act as one of the mainbarriers to men's participation in reproductive health services. Also, the results of the studies have shown that people's attitudes toward reproductive health services are influenced by environmental factors such as cultural and social issues. Even more significantly, these attitudes originate from cultural and social issues. As the World Health Organization states, social norms affect families and communities [ 14 ]. Therefore, the participation of people, especially men, in reproductive health care is affected by cultural and social factors. This theme discusses sociocultural factors which affect men's participation in reproductive health services. This theme emerged from five sub- themes “Gender perspectives”, “Dominant culture”, “Religious beliefs”, "Social norms", and "Stigma as a barrier".
Gender perspectives
Most of the articles reviewed in this study were conducted in African, Asian, and Latin American countries, which are traditional societies. In traditional communities, roles are divided by gender. Also, the dominant culture in these countries is the patriarchal culture. In most studies, gender considerations were described as an effective factor for men's engagement in reproductive health programs. The studies showed that gender duties have traditionally been divided between girls and boys [ 31 , 45 , 50 , 52 , 53 ]. Male participants described reproductive health as a women's issue [ 3 , 15 , 17 , 20 , 37 , 39 , 45 , 50 - 52 , 60 , 64 , 66 , 71 ]. Male participants believed that pregnancy, childbirth, and family planning were the responsibility of women [ 16 , 17 , 33 , 45 ]. Therefore, women are responsible for the pregnancy and supporting pregnant women [ 30 ]. Based on gender role division, men described themselves as producers, provider, administrator [ 46 , 47 , 66 ], and decision-makers [ 45 , 66 ]. Gender considerations also included the space of reproductive health centers, and maternal and neonatal service centers were described as women's spaces [ 30 , 33 ]. Studies have shown that gender taboos resulting from gender roles culturally prevent men from participating in reproductive health services [ 40 ].
Dominant culture
The results of the reviewed studies have shown that the dominant culture of societies was the main factor affecting men's participation in reproductive health services. The culture of the communities where these studies were conducted, does not support male participation in most aspects of reproductive health. Participants stated that their presence in maternity care was contrary to the culture of the community [ 15 ]. According to the patriarchal culture in society, men's participation in pregnancy care is unacceptable [ 18 ]. Because of Cultural prejudices, men didn't visit medical centers alongwith women [ 52 ]. Participants described a negative cultural perception of male participation in reproductive health services [ 40 , 49 ]. Expressing interest in one's spouse in the community was also considered culturally inappropriate [ 19 ]. Culturally, women weren't allowed to ask their husbands to participate in reproductive health services [ 37 ]. Men's engagement in maternity care was not culturally accepted [ 45 , 46 , 53 ].
Religious beliefs
Religious beliefs are one of the factors that affect men's participation in reproductive health services. Men's participation in some aspects of reproductive health, including family planning and the investigation of sexually transmitted diseases, is most influenced by religious beliefs. In this study, few articles have described religious beliefs in reducing men's presence in the reproductive health program. The use of modern contraceptives, especially vasectomy, was not accepted in some religious sects [ 32 , 44 , 55 , 64 , 65 ]. Few participants stated that the use of medicine is not according to God's will and contaminates the body of humans which is God's sanctuary. Receiving hospital delivery treatment was described as uncertainty about God's healing power [ 65 ].
Social norms
Men's participation in reproductive health services is a social and behavioral action. The results of these studies have shown that social norm is one of the barriers to men’s participation in reproductive health services. Attention to social norms in men's decisions to attendreproductive health centers was reported in the studies [ 16 , 33 , 36 , 46 , 50 , 51 , 54 , 66 ]. Participants said: in their communities, the presence of men in reproductive health centers was unfamiliar [ 16 , 50 ] and socially unacceptable [ 66 ]. Male participants statethat they refused to attend antenatal care due to fear of being seen by community members [ 36 ]. Social consensus has limited the presence of men in maternity care and reproductive health care [ 52 ]. Some participants described having a crowded family as social credit, so they did not participate in family planning programs [ 33 , 64 , 71 ].Vasectomy was perceived as a factor to therats the role of men as heads of families in society [ 64 ].
Stigma as a barrier
Social stigma can be scandalous, shameful, and even disgusting and can damage people's social identity.The context of the research investigated in this study is patriarchalIn these societies he presence of men in many aspects of reproductive health is socially and culturally stigmatized, so men did not participate in reproductive health services. The results show that one of the main preventive factors for males' participation in reproductive health was fear of stigma [ 30 - 34 , 36 , 37 , 40 , 41 , 43 , 53 , 57 , 58 , 66 ]. Participants reported that men were ridiculed or humiliated for being involved in maternal care [ 47 ]. Fear of other men's reactions, prevented them from participating in various aspects of reproductive health [ 3 , 36 , 37 ]. If men participated in reproductive health programs, they would be described in negative and derogatory terms such as "under the contrl of woman", "waiting like the woman" and "dominated by the woman" [ 19 , 32 , 34 , 40 , 49 , 66 ].
Line of argument synthesis
Despite emphasizing the importance and benefits of men's active participation in reproductive health programs to the health of men, women, and children, most men are not engaged in reproductive health services. The present study originated from the result’s synthesis of 47 studies conducted on multiple aspects of reproductive health in various contexts. In this study, despite the differences in the context of studies, a significant similarity in the experiences about reasons for not men's involving in reproductive health services was shown. The most important reasons for men's non-participation in reproductive health services, which have been mentioned in different parts of the world, included the failure to access all-inclusive and integrated quality services, economic issues, Couples' personal preferences and attitudes, and sociocultural considerations to seek reproductive health services. These factors are interrelated. Meanwhile, other causes are impressed with cultural and social considerations, such as gender roles and patriarchal culture. Therefore, to achieve the active participation of men in reproductive health services, in addition, to paying attention to these reasons, the relationships between them should be considered. The socio-cultural factors can directly and indirectly affect men's participation in sexual and reproductive health services. So it requires special consideration. It is necessary to try to mobilize agents affecting cultural and social issues, including activists of sociocultural, to provide accessibility of men to comprehensive sexual and reproductive health services.
This meta-synthesis focused on barriers to male participation in reproductive healthcare. It provided a deep insight towards creating a comprehensive synthesis of views of women, men, and healthcare providers concerning barriers to men's involvement in reproductive health. The findings of this synthesis can help policy-making and planning to remove barriers to men's engagement in reproductive health care. Qualitative studies conducted in different countries with different socio-cultural contexts pointed to a group of partially common barriers to male participation in reproductive health services. In this meta-synthesis, four main themes emergedsuch as, failure to access all-inclusive and integrated quality services, economic issues, couples' personal preferences and attitudes, and sociocultural considerations to seek reproductive health services.
In the policymaking and managing of reproductive health centers, the concept of male participation in reproductive and sexual health has not been developed yet. In most parts of the world, women are still the primary target of health care services [ 66 ]. In line with the results of this study, political and conceptual barriers related to reproductive and sexual health lead to men deprivation of reproductive and sexual health care services [ 72 ]. The lack of mutual communication between reproductive health policymakers and service recipients (couples) causes reproductive health policy to be designed and implemented hierarchically from top to down [ 73 ]. Mutualinteraction between policymakers, implementers and potential propagandists of reproductive health programs includingreligious leaders and social leaders is the main factor to achieve better results in reproductive and sexual health programs. Lack of clarity of the concept of programs, interaction, and feedback between policymakers, executives, and service recipients leads to disruption of policy implementation [ 51 ].
The availability of health facilities and service environments, including programs, staff, equipment, and professional behaviors, are effective in the presence of men in reproductive health care. Although male participation in reproductive health services is encouraged, the status of healthcare facilities for men and couples has not changed [ 74 ]. It seems that the existence of obstacles such as unfavorable environments, the unfriendly atmosphere of service centers, and the framework of human force have dissuaded men from actively participating in reproductive health care with their wives [ 18 ]. It is recommended that affordable access to reproductive health services should be provided to all, despite gender, race, and socioeconomic status [ 75 ]. According to the study findings, there is no specific target for men in reproductive health programs. These studies found that in addressing gender socialization in male adolescents, reproductive health services have ignored the needs of male adolescents and they are unfriendly to men [ 76 ].
Economic status is one of the main structural determinants of perceived equality in the context of reproductive health [ 76 ]. Clients' financial limitations were reported as an effective factor in the presence of men in reproductive health centers [ 77 ].
Men played the role of the financial supplier of reproductive health care for their families. The high cost of care and the lack of sufficient resources jeopardize the men's role[ 78 ]. According to the findings of this study, in addition to financial constraints, job responsibility also is known as an obstacle to the presence of men in reproductive health care. This factor indirectly affects men's economic status. For men with little daily income, leaving the workplace to attend reproductive healthcare can put their economic situation at risk, and it can affect their decision to participate in reproductive health care [ 79 ].
Men's health-seeking behaviors are influenced by some factors, such as embarrassment, anxiety, distress, and fear caused by inadequate awareness about services and medical culture and the prevalence of patriarchal attitudes in men [ 80 ]. Men's tendency to participate in reproductive health care is related to their knowledge and attitudes toward reproductive health services [ 81 ]. Studies have shown that shamefullness, and reluctance were the main barriers to men's access to reproductive health services such as contraception [ 82 ]. Reproductive health is institutionalized as women's health, so providing services in reproductive health centers is not favored by men [ 72 ]. Males' unawareness and misperceptions regarding reproductive and sexual health are common barriers for male’s participation in reproductive health [ 83 ]. So, promoting the presence of men in reproductive health services requires programs focusing on improving men's knowledge and attitudes using community-based health education programs [ 84 , 85 ]. Consistent with the results of the current study, beliefs, attitudes, and interactions between spouses are main determinants of male participation in reproductive health care. Poor interaction between the couple is associated with poor men's engagement in reproductive health services [ 77 ]. Promoting appropriate couples' interaction about reproductive health services facilitates informed decision-making for spouses [ 24 ]. One of the main factors for the presence of men in reproductive and sexual health is realizing the relationship between spouses and identifying the pattern of spouses'relationships regarding reproductive health. Focusing on the marital context of the couples is essential to promote the quality of reproductive health services [ 86 ].
The findings of a systematic review of the experiences, beliefs, values, and attitudes of adult men about contraception has mentioned that reproductive health-related behaviors affected a person's family, religious, and social contexts which are in confirmity with our findings [ 24 ]. In the health promotion programs, socio-cultural subjects that influence health, should be considered. Although personal preferences and attitudes, such as knowledge about reproductive health and communication between spouses, could predict male involvement in reproductive health, cultural subjects, such as the superior power of men in interaction and decision-making, largely determine the presence of men in reproductive health. One of the factors that discouraged men from participating in reproductive health services is the dominant traditional beliefs and gender roles that are culturally determined [ 87 ].
Generally, in traditional communities, gender roles have been demarcated to feminine and masculine affairs [ 18 ]. There arehuge discrepancies between gender roles. Men's disregard for traditional gender boundaries leads to their ridicule [ 88 ]. Regarding health care services, people refuse to seek health servicesdue to fear of stigma. Various aspects of reproductive health care, such as family planning, voluntary sterilization, and physician-assisted reproductive care, can be associated with stigma for users [ 89 ]. So, it is necessary to adopt culture-based strategies to improve men’s participation [ 18 ]. Therefore, it is necessary to consider the culture of the community in designing reproductive health programs. In designing programs, a couple's attendance should be considered. To educate the community, reproductive health education sessions should be organized in the presence of men and at the community level [ 52 , 53 ].
There are contradictions in the results of studies on the participation of men in some reproductive health services, such as HIV care. Women believed that their male partner's involvement in HIV care during pregnancy and postpartum, could be beneficial and harmful at the same time.. Men's participation could include a range of support for women and control of their behavior. Gender inequality, along with gender norms in society and HIV-induced stigma, made the situation challenging for women [ 90 ]. So, to change the norms of society, action must be taken beyond the health sector to explain policies to protect the rights of men and women on an equal level. Reforms must be aimed at strengthening gender equality so that women can have control over their bodies and lives.Accordingly, every person can decide on his own body without discrimination and compulsion [ 75 ]. It is necessary that specialists and their professional associations, which are committed to preserve human dignity, be active to counteract stigmatization among patients and health care providers [ 89 ]. To change the norms of patriarchy in society, it is necessary to motivate men to challenge the power and privileges traditionally granted to them. Changing men’s gender attitudes requires short-term interventions, including changing school curricula and forming small groups to create critical thinking about unequal power. It also requires broader social action to change the norm of society, which requires a sociological approach that involves parents and schools in addition to men and consequently community mobilization [ 91 ].
Although most of the articles reviewed in the present study were conducted in developing countries, another study also noted the gap and the need for men’s presence while providing health services to women in developed countries. According to the results of this study, Men are almost absent at the time of women's health care and prenatal health education program. Also, programs designed for public health, such as using a social marketing approach, have only targeted women. Men have not been included in the target of "Healthy People 2020 objectives for MCH" [ 92 ]. Although interventions to increase men's engagement in mother and infant care have promoted care, there is still a gap in evidence about the efficacy of men's engagement in mother and infant care on morbidity and mortality. Therefore, care should be taken in designing programs to increase men's participation so that their design and implementation can reduce the potentially harmful effects on marital relationships [ 93 ].
The current study’s strength was that the investigated articles were qualitative studies that extracted deep information about individuals. The study participants included all individuals involved in reproductive health services, including community members, couples, and health professionals. The study examined reproductive health from various aspects, including maternal health care, family planning, prevention transaction HIV from mother to child, reproductive and sexual health education, and maternal and newborn health. The limitation of the study was that all the articles that were available and reviewed in this study belonged to developing countries.
Conclusions
The review of studies and their analysis showed that one of the obstacles to men's participation in reproductive health is the lack of access to inclusive and integrated quality services. One of the causes of this lack of access includes mismanagement and weak policies. In the designing and policymaking of reproductive health programs, the position of men as recipients of health services has not yet been determined, which needs to be considered. Men should be included in the goals of policies and plans in reproductive healthprograms. Consequently,the management of reproductive health services, the design of reproductive health environments, and the center's structure of providing reproductive health services became men-friendly. One of the factors that cause men to be left out of reproductive health care and men themselves not want to participate in reproductive health is the dominant culture and social norms, especially gender norms. So gender norms that influence public attitudes toward men’s participation in reproductive health care need to be addressed. To increase men's participation in reproductive health care programs, men’s points of view must be considered. Paying attention to communication skills, especially among reproductive health care professionals, can be an important step in removing barriers to men's participation in these services. The existing gaps in policy making and planning and implementation of programs in men's participation in reproductive health care should be taken into account in conducting future research. Among the factors that are effective in men's participation in reproductive health care are health system programs, policies, economic, and sociocultural attitudes, knowledge, and men's preferences.Therefore, reproductive health initiatives should focus on eliminating challenges to men's supportive activities to incentive men's participation in reproductive health care.
Availability of data and materials
The datasets analyzed as part of this review are available from the corresponding author on reasonable request.
Abbreviations
Critical Appraisal Skills Program
Preferred Reporting Items for Systematic reviews and Meta-Analyses
Pourkazemi R, Janighorban M, Boroumandfar Z, Mostafavi F. A comprehensive reproductive health program for vulnerable adolescent girls. Reprod Health. 2020;17:1–6.
Article Google Scholar
World Health Organization. Sexual health and its linkages to reproductive health: an operational approach. https://apps.who.int/iris/handle/10665/258738 .
Davis J, Vyankandondera J, Luchters S, Simon D, Holmes W. Male involvement in reproductive, maternal and child health: a qualitative study of policymaker and practitioner perspectives in the Pacific. Reprod Health. 2016;13(1):1–1.
Hawkes S, Hart G. Men’s sexual health matters: promoting reproductive health in an international context. Trop Med Int Health. 2000;A7:37–44.
Ani F, Abiodun O, Sotunsa J, Faturoti O, Imaralu J, Olaleye A. Demographic factors related to male involvement in reproductive health care services in Nigeria. Eur J Contracept Reprod Health Care. 2016;21(1):57–67.
Article PubMed Google Scholar
Langen TT. Gender power imbalance on women\’s capacity to negotiate self-protection against HIV/AIDS in Botswana and South Africa. Afr Health Sci. 2005;5(3):188–97.
PubMed PubMed Central Google Scholar
Falade-Fatila O, Adebayo AM. Male partners’ involvement in pregnancy related care among married men in Ibadan Nigeria. Reprod Health. 2020;17:1–2.
Gibore NS, Ezekiel MJ, Meremo A, Munyogwa MJ, Kibusi SM. Determinants of men’s involvement in maternity care in Dodoma Region Central Tanzania. J Pregnancy. 2019;2019:7637124.
Article PubMed PubMed Central Google Scholar
Atuahene MD, Arde-Acquah S, Atuahene NF, Adjuik M, Ganle JK. Inclusion of men in maternal and safe motherhood services in inner-city communities in Ghana: evidence from a descriptive cross-sectional survey. BMC Pregnancy Childbirth. 2017;17:1.
Adams YJ, Stommel M, Ayoola A, Horodynski M, Malata A, Smith B. Husbands’ knowledge and attendance at wives’ postpartum care among rural farmers. Health Care Women Int. 2018;39(9):1020–37.
Adane HA, Assefa N, Mengistie B, Demis A. Male involvement in prevention of mother to child transmission of human immunodeficiency virus and associated factors in Enebsiesarmider District, north West Ethiopia, 2018: a cross-sectional study. BMC Pregnancy Childbirth. 2020;20:1–8.
Wesevich A, Mtande T, Saidi F, Cromwell E, Tweya H, Hosseinipour MC, Hoffman I, Miller WC, Rosenberg NE. Role of male partner involvement in ART retention and adherence in Malawi’s option B+ program. AIDS Care. 2017;29(11):1417–25.
Speziale HS, Streubert HJ, Carpenter DR. Qualitative research in nursing: Advancing the humanistic imperative. Philadelphia, Baltimor, New York, London: Wolters Kluwer/lippincott William & Wilkams; 2011.
World Health Organization. World Health Organization. Reproductive Health. Medical eligibility criteria for contraceptive use: World Health Organization; 2010.
Google Scholar
Nesane K, Maputle SM, Shilubane H. Male partners’ views of involvement in maternal healthcare services at Makhado Municipality clinics, Limpopo Province, South Africa. Afr J Primary Health Care Fam Med. 2016;8(2):1–5.
Teklesilasie W, Deressa W. Barriers to husbands’ involvement in maternal health care in Sidama zone, Southern Ethiopia: a qualitative study. BMC Pregnancy Childbirth. 2020;20(1):1–8.
Gibore NS, Bali TA. Community perspectives: an exploration of potential barriers to men’s involvement in maternity care in a central Tanzanian community. PLoS ONE. 2020;15(5):e0232939.
Article CAS PubMed PubMed Central Google Scholar
Firouzan V, Noroozi M, Farajzadegan Z, Mirghafourvand M. Barriers to men’s participation in perinatal care: a qualitative study in Iran. BMC Pregnancy Childbirth. 2019;19(1):1–9.
Aborigo RA, Reidpath DD, Oduro AR, Allotey P. Male involvement in maternal health: perspectives of opinion leaders. BMC Pregnancy Childbirth. 2018;18(1):1.
Ongolly FK, Bukachi SA. Barriers to men’s involvement in antenatal and postnatal care in Butula, western Kenya. Afr J Primary Health Care Fam Med. 2019;11(1):1–7.
Holloway I, Galvin K. Qualitative research in nursing and healthcare. Chichester, West Sussex: Wiley; 2016.
Mills E, Jadad AR, Ross C, Wilson K. Systematic review of qualitative studies exploring parental beliefs and attitudes toward childhood vaccination identifies common barriers to vaccination. J Clin Epidemiol. 2005;58(11):1081–8.
McEvoy R, Ballini L, Maltoni S, O’Donnell CA, Mair FS, MacFarlane A. A qualitative systematic review of studies using the normalization process theory to research implementation processes. Implement Sci. 2014;9:1–3.
Hoga LA, Rodolpho JR, Sato PM, Nunes MC, Borges AL. Adult men’s beliefs, values, attitudes and experiences regarding contraceptives: a systematic review of qualitative studies. J Clin Nurs. 2014;23(7–8):927–39.
Noblit GW, Hare RD, Hare RD. Meta-ethnography: Synthesizing qualitative studies. Newbury Park (CA): Sage Publications; 1988.
Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101.
Checklists - Critical Appraisal Skills Programme CASP . 2018. http://www.casp-uk.net/casp-tools-checklists .
Khakbazan Z, Taghipour A, Latifnejad Roudsari R, Mohammadi E. Help seeking behavior of women with self-discovered breast cancer symptoms: a meta-ethnographic synthesis of patient delay. PLoS ONE. 2014;9(12): 110262.
Mohammed MA, Moles RJ, Chen TF. Medication-related burden and patients’ lived experience with medicine: a systematic review and metasynthesis of qualitative studies. BMJ Open. 2016;6(2): e010035.
Kwambai TK, Dellicour S, Desai M, Ameh CA, Person B, Achieng F, Mason L, Laserson KF, Ter Kuile FO. Perspectives of men on antenatal and delivery care service utilisation in rural western Kenya: a qualitative study. BMC Pregnancy Childbirth. 2013;13(1):1.
Nyondo AL, Chimwaza AF, Muula AS. Stakeholders’ perceptions on factors influencing male involvement in prevention of mother to child transmission of HIV services in Blantyre. Malawi BMC Public Health. 2014;14:1–5.
Adongo PB, Tapsoba P, Phillips JF, Tabong PT, Stone A, Kuffour E, Esantsi SF, Akweongo P. “If you do vasectomy and come back here weak, I will divorce you”: a qualitative study of community perceptions about vasectomy in Southern Ghana. BMC Int Health Hum Rights. 2014;14(1):1–8.
Kabagenyi A, Jennings L, Reid A, Nalwadda G, Ntozi J, Atuyambe L. Barriers to male involvement in contraceptive uptake and reproductive health services: a qualitative study of men and women’s perceptions in two rural districts in Uganda. Reprod Health. 2014;11(1):1–9.
Dral AA, Tolani MR, Smet E, van Luijn A. Factors influencing male involvement in family planning in Ntchisi district, Malawi–a qualitative study. Afr J Reprod Health. 2018;22(4):35–43.
PubMed Google Scholar
Auvinen J, Kylmä J, Välimäki M, Bweupe M, Suominen T. Barriers and resources to PMTCT of HIV: Luba-Kasai men’s perspective in Lusaka. Zambia J Assoc Nurs AIDS Care. 2013;24(6):554–68.
Mohlala BK, Gregson S, Boily MC. Barriers to involvement of men in ANC and VCT in Khayelitsha. South Africa AIDS Care. 2012;24(8):972–7.
Falnes EF, Moland KM, Tylleskär T, de Paoli MM, Msuya SE, Engebretsen IM. “It is her responsibility”: partner involvement in prevention of mother to child transmission of HIV programmes, northern Tanzania. J Int AIDS Soc. 2011;14(1):21.
Gill MM, Ditekemena J, Loando A, Ilunga V, Temmerman M, Fwamba F. “The co-authors of pregnancy”: leveraging men’s sense of responsibility and other factors for male involvement in antenatal services in Kinshasa DRC. BMC Pregnancy Childbirth. 2017;17(1):1.
Article CAS Google Scholar
Jungari S, Paswan B. Supported motherhood? An examination of the cultural context of male participation in maternal health care among tribal communities in India. J Biosoc Sci. 2020;52(3):452–71.
MirzaiiNajmabadi K, Karimi L, Ebadi A. Exploring the barriers to sexual and reproductive health education for men in Iran: a qualitative study. Iranian J Nurs Midwife Res. 2019;24(3):179.
Dovel K, Dworkin SL, Cornell M, Coates TJ, Yeatman S. Gendered health institutions: examining the organization of health services and men’s use of HIV testing in Malawi. J Int AIDS Soc. 2020;23:e25517.
Kashaija DK, Mselle LT, Mkoka DA. Husbands’ experience and perception of supporting their wives during childbirth in Tanzania. BMC Pregnancy Childbirth. 2020;20:1–9.
Ladur AN, Colvin CJ, Stinson K. Perceptions of community members and healthcare workers on male involvement in prevention of mother-to-child transmission services in Khayelitsha, Cape Town, South Africa. PLoS ONE. 2015;10(7):e0133239.
Kaida A, Kipp W, Hessel P, Konde-Lule J. Male participation in family planning: results from a qualitative study in Mpigi District. Uganda J Biosoc Sci. 2005;37(3):269–86.
Maluka SO, Peneza AK. Perceptions on male involvement in pregnancy and childbirth in Masasi District, Tanzania: a qualitative study. Reprod Health. 2018;15:1–7.
Lowe M. Social and cultural barriers to husbands’ involvement in maternal health in rural Gambia. Pan Afr Med J. 2017;27:255.
Mkandawire E, Hendriks SL. A qualitative analysis of men’s involvement in maternal and child health as a policy intervention in rural Central Malawi. BMC Pregnancy Childbirth. 2018;18(1):1–2.
Greenspan JA, Chebet JJ, Mpembeni R, Mosha I, Mpunga M, Winch PJ, Killewo J, Baqui AH, McMahon SA. Men’s roles in care seeking for maternal and newborn health: a qualitative study applying the three delays model to male involvement in Morogoro Region Tanzania. BMC Pregnancy Childbirth. 2019;19(1):1–2.
Ganle JK, Dery I. ‘What men don’t know can hurt women’s health’: a qualitative study of the barriers to and opportunities for men’s involvement in maternal healthcare in Ghana. Reprod Health. 2015;12(1):1–3.
Sakala D, Kumwenda MK, Conserve DF, Ebenso B, Choko AT. Socio-cultural and economic barriers, and facilitators influencing men’s involvement in antenatal care including HIV testing: a qualitative study from urban Blantyre Malawi. BMC Public Health. 2021;21(1):1–2.
Gopal P, Fisher D, Seruwagi G, Taddese HB. Male involvement in reproductive, maternal, newborn, and child health: evaluating gaps between policy and practice in Uganda. Reprod Health. 2020;17:1–9.
Shahjahan M, Kabir M. Why males in Bangladesh do not participate in reproductive health: lessons learned from focus group discussions. Int Quart Commun Health Educ. 2006;26(1):45–59.
Sharma G, Penn-Kekana L, Halder K, Filippi V. An investigation into mistreatment of women during labour and childbirth in maternity care facilities in Uttar Pradesh, India: a mixed methods study. Reprod Health. 2019;16(1):1–6.
Vermeulen E, Solnes Miltenburg A, Barras J, Maselle N, Van Elteren M, Van Roosmalen J. Opportunities for male involvement during pregnancy in Magu district, rural Tanzania. BMC Pregnancy Childbirth. 2016;16(1):1–9.
Sharma S, Kc B, Khatri A. Factors influencing male participation in reproductive health: a qualitative study. J Multidisc Healthc. 2018;11:601–8.
Dumbaugh M, Tawiah-Agyemang C, Manu A, ten Asbroek GH, Kirkwood B, Hill Z. Perceptions of, attitudes towards and barriers to male involvement in newborn care in rural Ghana, West Africa: a qualitative analysis. BMC Pregnancy Childbirth. 2014;14:1–9.
Yeganeh N, Simon M, Mindry D, Nielsen-Saines K, Chaves MC, Santos B, Melo M, Mendoza B, Gorbach P. Barriers and facilitators for men to attend prenatal care and obtain HIV voluntary counseling and testing in Brazil. PLoS ONE. 2017;12(4):e0175505.
Willcox ML, Mubangizi V, Natukunda S, Owokuhaisa J, Nahabwe H, Nakaggwa F, Laughton M, Chambers I, Coates S, King E, Fall E. Couples’ decision-making on post-partum family planning and antenatal counselling in Uganda: a qualitative study. PLoS ONE. 2021;16(5):e0251190.
Mapunda B, August F, Mwakawanga D, Mhando I, Mgaya A. Prevalence and barriers to male involvement in antenatal care in Dar es Salaam, Tanzania: a facility-based mixed-methods study. PLoS ONE. 2022;17(8):e0273316.
Okafor IP, Chukwudi CL, Igwilo UU, Ogunnowo BE. “Men are the head of the family, the dominant head”: A mixed method study of male involvement in maternal and child health in a patriarchal setting, Western Nigeria. PLoS ONE. 2022;17(10):e0276059.
Forbes F, Wynter K, Zeleke BM, Fisher J. Fathers’ involvement in perinatal healthcare in Australia: experiences and reflections of Ethiopian-Australian men and women. BMC Health Serv Res. 2021;21:1–3.
Koffi TB, Weidert K, Bitasse EO, Mensah MA, Emina J, Mensah S, Bongiovanni A, Prata N. Engaging men in family planning: perspectives from married men in Lomé Togo. Global Health: Sci Pract. 2018;6(2):317–29.
Dychtwald DK, Kaimal G, Kilby LM, Klobodu C, Milliron BJ. “When a father feels excluded”: a qualitative study exploring the role of fathers in the Women, Infants, and Children (WIC) Supplemental nutrition program. Int J Qual Stud Health Well-Being. 2021;16(1):1932026.
Shongwe P, Ntuli B, Madiba S. Assessing the acceptability of vasectomy as a family planning option: a qualitative study with men in the Kingdom of Eswatini. Int J Environ Res Public Health. 2019;16(24):5158.
Adejoh SO, Olorunlana A, Olaosebikan O. Maternal health: A qualitative study of male partners’ participation in Lagos. Nigeria Int J Behav Med. 2018;25:112–22.
Reuben Mahiti G, Mbekenga CK, Dennis Kiwara A, Hurtig AK, Goicolea I. Perceptions about the cultural practices of male partners during postpartum care in rural Tanzania: a qualitative study. Glob Health Action. 2017;10(1):1361184.
Atkins S, Lewin S, Smith H, Engel M, Fretheim A, Volmink J. Conducting a meta-ethnography of qualitative literature: lessons learnt. BMC Med Res Methodol. 2008;8(1):1.
France EF, Ring N, Thomas R, Noyes J, Maxwell M, Jepson R. A methodological systematic review of what’s wrong with meta-ethnography reporting. BMC Med Res Methodol. 2014;14(1):1–6.
Campbell R, Pound P, Morgan M, Daker-White G, Britten N, Pill R, Yardley L, Pope C, Donovan J. Evaluating meta ethnography: systematic analysis and synthesis of qualitative research. Health Technol Assess. 2011;15:1.
Article CAS PubMed Google Scholar
Dixon-Woods M, Booth A, Sutton AJ. Synthesizing qualitative research: a review of published reports. Qual Res. 2007;7(3):375–422.
Bado AR, Badolo H, Zoma LR. Use of modern contraceptive methods in Burkina Faso: what are the obstacles to male involvement in improving indicators in the centre-east and centre-north regions? Open Access J Contracept. 2020;11:147–56.
Ramirez-Ferrero E, Lusti-Narasimhan M. The role of men as partners and fathers in the prevention of mother-to-child transmission of HIV and in the promotion of sexual and reproductive health. Reprod Health Matters. 2012;20(sup39):103–9.
Grindle MS, Thomas JW. Public choices and policy change: the political economy of reform in developing countries. Baltimore: Johns Hopkins University Press; 1991.
Bhatta DN. Involvement of males in antenatal care, birth preparedness, exclusive breast feeding and immunizations for children in Kathmandu Nepal. BMC Pregnancy Childbirth. 2013;13(1):1–7.
Starrs AM, Ezeh AC, Barker G, Basu A, Bertrand JT, Blum R, Coll-Seck AM, Grover A, Laski L, Roa M, Sathar ZA. Accelerate progress—sexual and reproductive health and rights for all: report of the Guttmacher-Lancet commission. The Lancet. 2018;391(10140):2642–92.
Panjalipour S, Bostani Khalesi Z, Mirhaghjoo SN. Iranian female adolescents’ reproductive health needs: a systematic review. IJWHR. 2018;6:226–32.
Ditekemena J, Koole O, Engmann C, Matendo R, Tshefu A, Ryder R, Colebunders R. Determinants of male involvement in maternal and child health services in sub-Saharan Africa: a review. Reprod Health. 2012;9(1):1–8.
McMahon SA, Chase RP, Winch PJ, Chebet JJ, Besana GV, Mosha I, Sheweji Z, Kennedy CE. Poverty, partner discord, and divergent accounts; a mixed methods account of births before arrival to health facilities in Morogoro Region Tanzania. BMC Pregnancy Childbirth. 2016;16:1–2.
Choko AT, Kumwenda MK, Johnson CC, Sakala DW, Chikalipo MC, Fielding K, Chikovore J, Desmond N, Corbett EL. Acceptability of woman-delivered HIV self-testing to the male partner, and additional interventions: a qualitative study of antenatal care participants in Malawi. J Int AIDS Soc. 2017;20(1):21610.
Yousaf O, Grunfeld EA, Hunter MS. A systematic review of the factors associated with delays in medical and psychological help-seeking among men. Health Psychol Rev. 2015;9(2):264–76.
Nasreen HE, Leppard M, Al Mamun M, Billah M, Mistry SK, Rahman M, Nicholls P. Men’s knowledge and awareness of maternal, neonatal and child health care in rural Bangladesh: a comparative cross sectional study. Reprod Health. 2012;9:1–9.
Galle A, Plaieser G, Van Steenstraeten T, Griffin S, Osman NB, Roelens K, Degomme O. Systematic review of the concept ‘male involvement in maternal health’by natural language processing and descriptive analysis. BMJ Global Health. 2021;6(4):e004909.
Mullany BC. Barriers to and attitudes towards promoting husbands’ involvement in maternal health in Katmandu. Nepal Soc Sci Med. 2006;62(11):2798–809.
Bishwajit G, Tang S, Yaya S, Ide S, Fu H, Wang M, He Z, Da F, Feng Z. Factors associated with male involvement in reproductive care in Bangladesh. BMC Public Health. 2017;17(1):1–8.
Kågesten A, Parekh J, Tunçalp Ö, Turke S, Blum RW. Comprehensive adolescent health programs that include sexual and reproductive health services: a systematic review. Am J Public Health. 2014;104(12):e23-36.
Orne-Gliemann J, Tchendjou PT, Miric M, Gadgil M, Butsashvili M, Eboko F, Perez-Then E, Darak S, Kulkarni S, Kamkamidze G, Balestre E. Couple-oriented prenatal HIV counseling for HIV primary prevention: an acceptability study. BMC Public Health. 2010;10(1):1–1.
Lewis S, Lee A, Simkhada P. The role of husbands in maternal health and safe childbirth in rural Nepal: a qualitative study. BMC Pregnancy Childbirth. 2015;15:1.
Ganle JK, Dery I, Manu AA, Obeng B. ‘If I go with him, I can’t talk with other women’: understanding women’s resistance to, and acceptance of, men’s involvement in maternal and child healthcare in northern Ghana. Soc Sci Med. 2016;166:195–204.
Cook RJ, Dickens BM. Reducing stigma in reproductive health. Int J Gynecol Obstetr. 2014;125(1):89–92.
Hampanda KM, Mweemba O, Ahmed Y, Hatcher A, Turan JM, Darbes L, Abuogi LL. Support or control? Qualitative interviews with Zambian women on male partner involvement in HIV care during and after pregnancy. PLoS ONE. 2020;15(8):e0238097.
Amin A, Kågesten A, Adebayo E, Chandra-Mouli V. Addressing gender socialization and masculinity norms among adolescent boys: policy and programmatic implications. J Adolesc Health. 2018;62(3):S3-5.
Guadagno M, Mackert M, Rochlen A. Improving prenatal health: setting the agenda for increased male involvement. Am J Men’s Health. 2013;7(6):523–6.
Tokhi M, Comrie-Thomson L, Davis J, Portela A, Chersich M, Luchters S. Involving men to improve maternal and newborn health: a systematic review of the effectiveness of interventions. PloS One. 2018;13(1):0191620.
Download references
Acknowledgements
The authors would like to appreciate the researchers whose research results were used in this study.
Not applicable.
Author information
Authors and affiliations.
Nursing and Midwifery Care Research Center, Mashhad University of Medical Sciences, Mashhad, Iran
Robab Latifnejad Roudsari
Department of Midwifery, School of Nursing and Midwifery, Mashhad University of Medical Sciences, Mashhad, Iran
Community-Oriented Nursing Midwifery Research Center, Shahrekord University of Medical Sciences, Shahrekord, Iran
Farangis sharifi
Social Determinants of Health Research Center, Yasuj University of Medical Sciences, Yasuj, Iran
Fatemeh Goudarzi
Department of Midwifery, School of Medicine, Yasuj University of Medical Sciences, Yasuj, Iran
You can also search for this author in PubMed Google Scholar
Contributions
The study was designed by F.G. and R.L.R Data collection, data extraction, and data analysis were done by F. G, F. Sh. Comments on doing these steps were made by R.L.R The manuscript was written by FG. The final version was read and approved by all authors.
Corresponding author
Correspondence to Fatemeh Goudarzi .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Roudsari, R.L., sharifi, F. & Goudarzi, F. Barriers to the participation of men in reproductive health care: a systematic review and meta-synthesis. BMC Public Health 23 , 818 (2023). https://doi.org/10.1186/s12889-023-15692-x
Download citation
Received : 18 July 2022
Accepted : 17 April 2023
Published : 04 May 2023
DOI : https://doi.org/10.1186/s12889-023-15692-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Reproductive health
- Male involvement
- Meta-synthesis
BMC Public Health
ISSN: 1471-2458
- General enquiries: [email protected]
- Open access
- Published: 09 February 2021
A qualitative exploration of contraceptive use and discontinuation among women with an unmet need for modern contraception in Kenya
- Susan Ontiri ORCID: orcid.org/0000-0001-7622-5714 1 , 2 ,
- Lilian Mutea 3 ,
- Violet Naanyu 4 ,
- Mark Kabue 5 ,
- Regien Biesma 2 &
- Jelle Stekelenburg 2 , 6
Reproductive Health volume 18 , Article number: 33 ( 2021 ) Cite this article
12k Accesses
21 Citations
2 Altmetric
Metrics details
Addressing the unmet need for modern contraception underpins the goal of all family planning and contraception programs. Contraceptive discontinuation among those in need of a method hinders the attainment of the fertility desires of women, which may result in unintended pregnancies. This paper presents experiences of contraceptive use, reasons for discontinuation, and future intentions to use modern contraceptives.
Qualitative data were collected in two rural counties in Kenya in 2019 from women with unmet need for contraception who were former modern contraceptive users. Additional data was collected from male partners of some of the women interviewed. In-depth interviews and focus group discussions explored previous experience with contraceptive use, reasons for discontinuation, and future intentionality to use. Following data collection, digitally recorded data were transcribed verbatim, translated, and coded using thematic analysis through an inductive approach.
Use of modern contraception to prevent pregnancy and plan for family size was a strong motivator for uptake of contraceptives. The contraceptive methods used were mainly sourced from public health facilities though adolescents got them from the private sector. Reasons for discontinued use included side effects, method failure, peer influence, gender-based violence due to covert use of contraceptives, and failure within the health system. Five reasons were provided for those not willing to use in the future: fear of side effects, cost of contraceptive services, family conflicts over the use of modern contraceptives, reduced need, and a shift to traditional methods.
This study expands the literature by examining reasons for contraceptive discontinuation and future intentionality to use among women in need of contraception. The results underscore the need for family planning interventions that incorporate quality of care in service provision to address contraceptive discontinuation. Engaging men and other social influencers in family planning programs and services will help garner support for contraception, rather than focusing exclusively on women. The results of this study can inform implementation of family planning programs in Kenya and beyond to ensure they address the concerns of former modern contraception users.
Peer Review reports
Use of contraceptive methods allows spacing of pregnancies or limiting family size, enabling individuals and couples to fulfill their fertility desire by choosing if and when to become pregnant. Contraceptive use not only has positive effects on health-related outcomes, such as improved maternal and child health [ 1 ] but also improves schooling and economic outcomes for girls and women [ 2 ]. Global trends have shown an increase in contraceptive uptake, however, many women, approximately one out of three, discontinue their method within a year [ 3 , 4 ]. Contraceptive discontinuation is an important determinant of contraceptive prevalence, as well as unintended pregnancies, and other demographic impacts as it increases the unmet need for family planning (FP). Several studies have found that contraceptive abandonment and failure contribute substantially to the total fertility rate, unwanted pregnancies, and induced abortions [ 3 , 4 , 5 ]. Analysis of data from 36 developing countries revealed that over one-third of unintended pregnancies resulted from women who had discontinued the use of contraception [ 5 ]. Unintended pregnancies have negative consequences on the health and well-being of women and their families as they can lead to maternal morbidities and even death. Besides, it is documented that children born from unintended pregnancies are: less likely to be breastfed, more likely to be stunted, at risk of a lack of parental love, and at higher risk of child mortality than children from wanted pregnancies [ 6 ].
An analysis of Demographic and Health Surveys conducted by Curtis et al. demonstrated that women’s socio-demographic characteristics—age, education, place of residence, and economic status—are the determinants associated with contraceptive discontinuation [ 7 ]. Even though studies indicate that women with higher levels of education and those residing in urban residences are more likely to discontinue their initial method, additional analyses reveal that these women are more likely to switch than stop after discontinuing a method [ 7 , 8 , 9 ]. This could be because they are enlightened on their contraceptive choices and will discontinue and switch if a particular method does not suit them since they can also easily access the contraceptive services due to shorter distances to health facilities.
Researchers continue to investigate why a woman or a couple would discontinue the use of modern contraception while still in need. Past studies show side effects and health concerns have been the main causes of contraceptive discontinuation [ 3 , 4 , 10 ]. Indeed, side effects account for more than half of the reasons for discontinuing contraceptives while still in need [ 9 , 11 ].
Kenya has implemented a strong national family planning (FP) program since it was launched in 1967 [ 12 ]. Over the past five decades, the country has developed FP/reproductive health policies, strategies, and guidelines and implemented programs aimed at increasing access and utilization of modern contraceptive methods among women of reproductive age and supporting men's involvement. These efforts have borne fruit; the current data estimates a contraceptive prevalence rate of 62.8%, which is mostly driven by the use of modern methods at 60.7% [ 13 ]. However, more than one-third of all pregnancies in Kenya are unintended and one in three women discontinue use of contraceptives by 12 months [ 14 ]. Like other countries, the main reason cited in Kenya for discontinuation is side effects, predominantly side effects associated with hormonal contraception [ 14 ]. Studies have linked poor quality of care, particularly inadequate counseling on side effects with contraceptive discontinuation [ 4 , 15 ]. For instance, data from round 5 to round 7 of Kenya’s Performance Monitoring and Accountability 2020 surveys indicate a glaring gap in the quality of FP services provided in health facilities. Only two-thirds of women were informed about side effects by service providers, with slightly more than half being informed about what to do in case of side effects [ 13 , 16 , 17 ].
Whereas the predictors of contraceptive counseling have been established by several quantitative studies [ 3 , 4 , 18 ], there is a paucity of information to understand the lived-in experiences of women who discontinue the use of contraceptives while still in need. This paper reports qualitative results from in-depth interviews and focus group discussions with discontinuers. The interviews and discussions explored experiences with previous use of modern contraceptives, reasons for discontinuation, and future intention to use contraceptives among discontinuers.
Study design and setting
A cross-sectional qualitative study was conducted as part of a formative assessment in a 24-month longitudinal study on evaluating the dynamics of contraceptive use, discontinuation, and switching in Kenya. The longitudinal study is being conducted in Kitui and Migori, rural counties in Kenya. The two counties have a diverse method mix; Migori’s mCPR is mostly driven by long-acting reversible contraceptives, at 72% while in Kitui, short-term methods are more popular, at 64% [ 14 ]. Details of the longitudinal study, including the study setting, have been published elsewhere [ 19 ]. Ten public health facilities, five in each county were purposively selected based on high FP caseload. The 10 facilities were located in 10 different sub-counties. Routine service statistics revealed that these facilities provided the highest number of contraceptive services in their respective sub-counties. Out of the ten facilities, 2 were county hospitals, 5 sub-county hospitals, 2 health centers, and 1 dispensary. The consolidated criteria for reporting qualitative research (COREQ) was used in this paper [ 20 ]. The completed checklist is available in Additional file 1 .
Study participants
Since the main objective of this study was to explore the experience with contraceptive use and discontinuation among discontinuers, participants who met the following inclusion criteria were selected: women of reproductive age between 15 and 49 years of age, who were sexually active, did not desire pregnancy, and had been but were currently not using modern contraception. The men who were interviewed to explore their perspective on contraceptive discontinuation were purposively selected since they were spouses of the women who met the inclusion criteria. Data collection included FGDs with adolescent mothers aged 15–19 years and women over 20 years and IDIs with couples and adolescent girls. Recruitment of study participants stopped once data saturation was achieved, that is when no new information was derived from the interviews and focus group discussions. In total, 42 data collection sessions (12 FGDs and 30 IDIs) were conducted with 135 study participants-105 in FGDs and 30 in IDIs. (Table 1 ).
Recruitment strategy
The study team selected community health volunteers (CHVs) who were providing health information including family planning to households within the catchment area of the study facilities. The CHVs were trained on the inclusion criteria and thereafter, mobilized and screened community members within their catchment area before referring them to the study staff who contacted, further screened, and recruited those eligible into the study. For couples, the CHV would approach the woman first to establish eligibility, before contacting the spouse. Both partners had to agree to participate before inclusion in the study.
Data collection
Data collection was conducted from May to July 2019. The data collection team was comprised of 10 research assistants, (seven females and three males) who had undergraduate training in Anthropology or Sociology. The team was selected based on their experience conducting qualitative studies. They further received an additional 5-day refresher training before data collection. They worked under the supervision of the lead author. Respondents were not known to the interviewers before the data collection sessions. Written consent was obtained from the participants to conduct and audio-record the data collection sessions. The time and place of the interviews were determined based on the convenience of the participants. The venue for the FGD data collection sessions was community halls while the IDIs were conducted at the participants’ homes. All participants were aware that the study was being conducted to explore their perspective and experience with contraceptive use and discontinuation as part of a formative assessment to improve the quality of family planning services provided.
Semi-structured topic guides covering FP topics for the various audiences were developed and piloted before use. The FGD guide included open-ended prompts related to knowledge and perception of contraceptives, use of FP with their community, and reasons for contraceptive discontinuation, including influencers. The study had IDI guides for the adolescent girls (15–19 years) and for married couples (18–49 years), husbands and wives were interviewed separately. The former group was asked about their knowledge and perceptions around sexual and reproductive health and contraceptive use, experience using contraceptives, and contraceptive discontinuation. The married couples shared their knowledge, perception, and decision-making experiences using contraceptives; FP use and discontinuation; and couple involvement in contraceptive use and discontinuation. The file showing the topic guides used in this study is provided in Additional file 2 .
Two trained interviewers were present at each FGD—one as a session moderator and the other as a note-taker. For the IDIs, only one trained moderator was present for the conversation. No observer was present during data collection. The FGDs and interviews were conducted in local dialect (Kamba and Dholuo) and Swahili. All the interviews were audio-recorded, and field notes were taken for each focus group session. The interview sessions lasted between 30 and 90 min. The data collection team debriefed after the end of each session. Interim findings were discussed weekly by the team and interview guides were modified and revised as needed. At the end of data collection, no new themes were emerging and data saturation had been achieved.
Data analysis
The digital recordings of IDIs and FGDs were transcribed verbatim, translated into English, and analyzed using NVivo 11. Data were analyzed thematically following the approach of Braun and Clarke to identify, analyze, and report patterns within the data [ 21 ]. Coding and theme development were directed by the content of the data (inductively) [ 21 ]. A final agreed thematic framework was applied to all interviews. Transcripts were not returned to participants in advance of coding. Data analyses were performed by two researchers (VN and SO) with in-depth knowledge of qualitative analysis who were supported by two analysts to ensure timely coding and validation of the coding frame. The team identified themes from reading and rereading the transcripts, noting any similarities and differences between and within participants’ accounts. The preliminary findings were shared with some of the study participants for validation.
Ethical considerations
This study was guided by a protocol that was approved by the Kenya Medical Research Institute Institutional Review Board and the Johns Hopkins Bloomberg School of Public Health Institutional Review Board. Participants gave informed written consent/assent to participate in the study. Protection and confidentiality of participants was ensured through conducting data collection sessions in private settings, maintaining confidentiality, and limiting access to study information to only authorized personnel.
The demographic characteristics of the 135 study participants are shown in Table 2 . The majority of the participants were adolescents and youth aged 15–24 years at 51%, had primary education 53%, were farmers 32%, and had one to two children (Table 2 ). The findings from the two study sites were comparable, with no major differences.
Study findings are provided in four themes below: (1) motivation for modern contraceptive use; (2) sources and decision-making for previous contraceptive used; (3) barriers to sustained use of contraceptives; and (4) future intention to use contraceptives.
Motivation for modern contraceptive use
The study explored the participant’s motivation for use of a contraceptive prior to discontinuation. Generally, there was strong consensus among all the study participants that the reasons for using contraceptives were to plan for the number of children they wished to have, and prevent pregnancy. Adolescent participants further noted that the greatest motivation for using contraceptives was to prevent pregnancy so as to pursue studies; they wanted to avoid unplanned pregnancies that might result in having to drop out of school and take on parental responsibilities they had not envisioned.
Economic reasons appeared to be the major impetus for use of contraceptives by adolescent mothers, older women, and married couples, as most participants shared similar sentiments on the need to have children they can manage to raise as illustrated by the following quote:
“We are able to space out the children and able to provide the right foods to the children so that they can be healthy because our incomes are low.” (FGD, Female).
Many participants reported that their motivation for use of contraceptives was to space their pregnancies to allow the healthy growth of children so they could get enough attention, nutrition, and care from their parents. A few married women noted, where couples were experiencing marital conflict, women used contraceptives to avoid getting additional children that they would need to support on their own.
Sources and decision-making for previous contraceptive used
The majority of participants interviewed indicated that they got their contraceptive method from public health facilities. Some, especially adolescents, got their contraceptive methods from private facilities, specifically chemists or pharmacists. Most older respondents indicated that they had opted for injectables and implants, while use of pills was mainly mentioned by adolescents.
“I bought my pills from the pharmacy shop in town” (IDI, Adolescent, Female).
The study findings revealed that before using contraception, most women sought the opinions of partners, peers, or family friends. For adolescent mothers, their mothers were mentioned as helpful in decision-making and accessing contraceptives. Most partners were involved in decision-making about uptake of FP before initiation of a method, while some were engaged after the FP method was started. However, some female participants stated that they had used contraception covertly due to non-supportive spouses or relatives, particularly the in-laws who threatened to report them to their partners.
Barriers to sustained use of contraception
The study further explored the reasons why women did not continue using a contraceptive method yet they still had a need for contraception. Reasons for discontinued use of contraceptives were manifold; five main sub-themes emerged: side effects, method efficacy, peer influence, gender-based violence, and health system factors.
Side effects of contraceptives
Across all the study groups, side effects resulting from use of contraception were repeatedly mentioned among the reasons for discontinuation. The leading side effect was irregular bleeding patterns presenting as menorrhagia (heavy menstrual bleeding) or amenorrhea (absence of menstrual bleeding). This was mainly experienced from the use of hormonal methods, and in particular injectables and implants. For example:
“When I used the three-months injection, I was bleeding excessively. Sometimes I would feel dizzy while walking. The bleeding would even continue for a month without stopping. So, I decided to stop using it.” (IDI, Female).
Heavy bleeding was cited to interfere with the participants’ social and economic lifestyle. The majority of the female participants who reported increased bleeding indicated that they were unable to carry out their economic activities since they were weak as a result of the increased menstrual flow. Another recurrent consequence of the increased bleeding was the interference with their sexual life:
“The reason I chose to stop using depo is for one reason. Sometimes my husband may have the desire to get intimate with you but you cannot, because of the bleeding. Whenever I want us to get intimate he declines because it is so much blood that is why he told me to try quitting it.” (IDI, Female).
On the contrary, some respondents reported that the absence of menstrual bleeding was what triggered discontinuation since they did not know whether they were still fertile or were pregnant.
“When I started using implants, my periods did not come for eight months, then it came back only for two days and disappeared again. I decided to stop using a contraceptive since I was always wondering whether I was pregnant.” (FGD, Adolescent).
Other side effects that led to discontinuation, albeit less frequently mentioned across the various study groups, included weight changes, dizziness, and low sexual libido.
“ My friend who was using the one for three years told me she stopped because she didn’t have an appetite for having sex, so it was raising issues between her and her husband.” (FGD, Adolescent).
Some study participants observed that experiences from other women influenced contraceptive use or discontinuation. Several FGD participants indicated that women discontinued the use of contraceptive methods after learning about side effects experienced by their friends. This prompted even those who were not experiencing the same to discontinue out of fear.
Contraceptive method efficacy
Contraceptive efficacy was a concern mentioned mostly by married couples. Respondents reported method failure whereby women got pregnant unexpectedly while still on a contraceptive method:
“One year after using an implant, I started becoming sick. When I went back to the hospital, I was tested and the results came out that I was four months pregnant, and at the same time I still had the implant in my arm.” (FGD, Female).
“I have a friend; she was using the one for 3 months. After sometime, she was shocked that she was pregnant. So, she decided that she will not use it because even if you use it you still get pregnant.” (FGD, Adolescent).
Several participants revealed that they decided to discontinue use of contraceptives after learning about cases of method failure among women who were using similar methods. On several instances, inconsistent use of contraceptive, especially short-term methods, that resulted in pregnancies were reported as method failure by some participants:
“The one for three months confused her a lot, it came to end without her knowing and she forgot to go back to the clinic for another injection. She became pregnant and then it surprised her. We had tried using it for a long time and I told her that she was using a method of a shorter duration and when it ended she became pregnant without planning.” (IDI, Male).
Covert use of contraception resulting in gender-based violence
Covert use of contraception was common due to lack of spousal support for use of a modern method. Across all the study groups, the participants shared their experiences or cases of other women who discontinued contraceptive use because their partners learned that they were using it covertly. Cases of gender-based violence directed at women by their partner after learning their use of modern contraceptive methods, further solidified their resolve to discontinue as illustrated by this experience:
“Another woman in our village went and got an implant without her husband’s knowledge. When the husband learned of this, he took a knife and removed it from her arm. This made my friends and me afraid, so we decided to just remove it for fear of what our husbands would do if they find out.” (FGD, Female).
Health system factors as a barrier to continuation
Health care system factors were repeatedly mentioned as reasons for discontinuation. Stock-outs of preferred methods during contraceptive initiation or resupply prompted women to either take alternative methods or leave without one. Provider bias that resulted in women taking up methods that they did not approve of came up as a sub-theme particularly by younger women, as shown in the quote below:
“I told him [the provider] I wanted depo and he said that the government does not advise the use of injection, and he refused to put it on me. He convinced me to take up an implant, which I did, but I went to another facility to have it removed.” (FGD, Female).
There were mixed experiences regarding FP counseling, particularly on side effects. Several respondents noted that they got adequate counseling by the health care providers during the initiation of a method; however, some mentioned that they were not informed of any potential side effects that could result from use of contraception.
“When I started using them, the doctor explained to me about the advantages and disadvantages of the various methods of family planning, such that, I know the goodness and effects of the method I am using.” (FGD, Female).
Future intentionality to use contraception
The study explored whether the respondents would consider using modern contraceptives again. Several respondents indicated willingness to use at some time, but some were hesitant. Those who would consider using an FP method again said they would consult widely, select a method with fewer side effects, and one with a longer duration. For those who were doubtful and not considering using FP, five reasons were provided.
First, there were fears about negative side effects. Women indicated that the fear of experiencing another side effect after discontinuation led them to decide not to take up any other modern method despite the counseling that they got from health care workers who were advising them on method switching. One woman shared her experience:
“These medicines bring problems. I stayed with the one injection for a while and every time I would feel sickly, weak, back pains at all times, bleeding from Monday to Monday. I came to the hospital and asked them to remove it. They asked me what the problem was, that they will give me another one, but I did not want one. So that is why I stopped using.” (FGD, Female).
Second, cost was cited as a barrier for continued use. Respondents indicated that the direct and indirect costs associated with uptake of contraceptive services hindered their intention to use. The cost barrier was mainly mentioned for short-term methods that require frequent resupply at facilities, hence, women had to make multiple visits to the facility. Several concerns were also raised regarding the removal of intrauterine contraceptive devices or implants after experiencing side effects. An important issue that participants highlighted was the cost incurred for the removal of a method, which caused women to fear the selection of another method in case they experienced side effects with that method.
“If you go to the facility before the expiry date, you are asked to pay 200 shillings, regardless of the side effects experienced. I wonder why they charge for removal yet they gave it for free. After that one fears to take up another method.” (FGD, Female).
Lastly, FP use caused conflicts in families. Women indicated lack of support from their partners and relatives impeded their intention to use contraception. It was evident that even though the women felt a need to space or limit their family size, that decision was mainly made by their partners. Other women, who had previously used the method covertly and had been discovered by their spouses or relatives, mentioned they could not use the method for fear of gender-based violence. This quote buttresses the point:
“My husband threatened to beat me also if he ever found me using a method. This was after he had observed a disagreement between our neighbors (couple), over the discreet use of contraceptives that ended up with the lady being hit by her husband. I decided to stop using to avoid such an occurrence. ” (IDI, Female).
This qualitative study aimed to explore the dynamics of contraceptive use and discontinuation among women with unmet need for contraceptives in the rural counties of Migori and Kitui, Kenya. A large and diverse group of adolescents, women, and couples who reported contraceptive discontinuation while still in need of a method provided insights on their experiences, perspectives with contraceptive use and reasons for discontinuation. Direct quotes of study participants about their experiences with FP use that culminated in discontinuation have been presented to deepen understanding of participants’ experiences [ 22 ]. From the study findings, it is evident that all the respondents chose to use contraceptives with the conviction that by using a modern method, they would be able to prevent pregnancy or plan when to have children, determine how far apart they want their children to be, and when to stop having children. However, this desire was not fully realized as they discontinued use of the contraceptives while still in need, which added to the pool of women of reproductive age with unmet need for FP.
There were numerous challenges faced by women using contraceptives that prompted them to discontinue their use. As noted in prior studies, side effects play a major role in reported decisions to discontinue [ 4 , 23 , 24 ]. Our study revealed that the most common side effect leading to contraceptive discontinuation were changes in users’ bleeding patterns, findings which are consistent with studies conducted across different parts of the world [ 18 , 25 , 26 ]. Irregularity of bleeding negatively impacts the well-being of women, mainly due to the social consequences, which could explain the low tolerance with contraception when such side effects are encountered. Studies have revealed that women, especially in the sub-Saharan region, believe that menstrual bleeding is a sign of fertility, hence any change that leads to reduced or no bleeding is frowned upon [ 27 , 28 ]. Conversely, increased bleeding impacts women’s socio-economic activities and sexual relationship with their partners [ 28 , 29 ].
Our findings thus provide strong support for addressing side effects experienced by women through management when they occur or being provided options for method switching to ensure the women continue to harness the full benefits of contraception. This can be achieved by conducting client follow-up by service providers to periodically assess the level of satisfaction with the contraceptive method while addressing issues that might prompt clients to discontinue. Proper counseling of clients, and their partners, is crucial to promote continuation with use of modern contraceptive methods as the users are made aware of the contraceptive’s mechanism of action, possible side effects, and what to do when they experience side effects. Helping women understand typical bleeding changes associated with their contraceptive methods could lead to greater acceptance of the changes, increased method uptake, improved satisfaction, and higher continuation rates [ 30 ]. Therefore, capacity building of health care providers on contraceptives should not just focus on the technical skills on insertion and removal (particularly for long-term methods), but also on contraceptives’ mechanisms, how they work, to ensure that providers are well versed on the potential side effects for each method. This is supported by evidence from studies in Madagascar and Ghana that revealed providers were not well informed on the physiological effects of contraception and how to manage side effects [ 4 ]. This resulted in inadequate counseling of women experiencing the side effects; women were counseled to switch to another method instead of being reassured that side effects would settle down over time or being offered medication to control some side effects [ 4 ]. This could be attributed to inadequate training content on side effects. A recent review of FP counseling, training, and reference materials revealed that bleeding changes are insufficiently addressed in capacity building resources and counseling tools for health care providers [ 29 ]. This is alarming, considering that the leading reason for discontinuation has been changes in bleeding pattern. Skilled counseling for side effects, particularly bleeding irregularities, can only be achieved if training materials for health care providers incorporate this information, information that will improve the quality of counseling by health care providers.
Contraceptive method failure was one of the reasons for discontinuation in this study. Method failure is a factor of either failure of a method to work as expected or incorrect/inconsistent use of a method by the user. In low- and middle-income countries, 74 million unintended pregnancies occur annually, of which a sizable share, 30%, are due to contraceptive failure among women using some type of contraceptive method [ 31 ]. Each contraceptive method has a Pearl Index number that reflects pregnancy rates during perfect and typical use, with use of long-term method conferring higher efficacy than short-term methods [ 32 ]. Whereas all contraceptive methods have some degree of failure, even during perfect use, failure rates can be reduced when individuals are sensitized on the proper use of contraception to ensure the method is used correctly and consistently. Provision of clear information about the risks and benefits of all available methods is crucial in facilitating informed contraceptive choice so women can make an educated choice for their preferred methods, which may reduce discontinuation.
Other reasons for contraceptive discontinuation, such as lack of support from partners and other social networks, are also corroborated in researches previously conducted in Kenya [ 28 , 33 ]. In our study, the decision to use or not use contraceptives was still primarily made by men. Although women made solo decisions on FP, they were heavily influenced by their spouses’ preference and would stop using if they thought it would bring marital conflicts. Opposition to contraceptive use by husbands appears to stem from the fear of side effects and the perception that women who use FP are more likely to be promiscuous. Additionally, Kenya being a highly patriarchal society, decision-making around the desired number of children mainly lies with the male partner. FP programs have mainly targeted women with information to promote uptake since they are the ones who face the risk of pregnancy and childbirth. Unfortunately, these programs have left out men, who are in most instances, the decision-makers in male-dominated societies, like most countries in the sub-Saharan region [ 34 ]. The findings from this study reveal the power dynamics when it comes to a couple’s decision to use contraception. This underscores the need to meaningfully involve men in FP programs by informing them of the health, economic, and social benefits realized from proper and consistent use of contraception so they can optimize use of FP services. Demand generation strategies that employ the use of positive deviants, satisfied users, and other key influencers, such as mothers-in-law, may lead to an increase in contraceptive uptake and enhance continuation.
This study indicates that the costs associated with consistent use of FP methods hinder their continued use. Promoting uptake of LARC methods will address the cost associated with the use of short-term method—LARCs have been shown to be more cost-effective and do not require frequent visits to facilities [ 35 ].
Our study also revealed punitive measures women faced, especially those on LARCs, when they wanted to switch to another method before its expiration. Allowing for method switching is indicative of strong FP programs that have an adequate range of methods and a flexible environment to meet women’s needs. Due to the health and social concerns that contraceptive use may confer on individuals, women may try different methods before settling for their preferred option. The health system should have a supportive policy environment that accommodates such needs of women by: instituting guidelines that prohibit penalization for method switching; addressing commodity stock-outs and ensuring sufficient method mix through increased financing of FP programs; and sensitizing providers on the importance of method switching by women who are not satisfied with their methods. Additional studies are needed to document the implications of frequent method switching on commodity security in countries that continue to face widespread stock-outs of contraceptive methods.
The study’s main strength was documenting the experiences of contraceptive use and discontinuation among discontinuers themselves. However, qualitative studies have limitations related to validity, subjectivity, and reliability. To address these issues, efforts were made to increase the rigor and trustworthiness of the findings through the selection of participants with a range of backgrounds and experiences with the guidance and supervision of experts, as well as external review. Information was not collected on the number of eligible participants who refused to participate in the study. Despite this, our study benefits from including a large number of participants, diverse in terms of age, gender, ethnicity, and location, and utilizing different data collection methodologies (FGDs and IDIs) to enrich the findings.
Conclusions
Our study, conducted in two rural counties in Kenya, revealed a number of important findings regarding factors influencing contraceptive use and discontinuation. The participants in this study had a common motivation for using contraception, to avoid pregnancies, however, side effects were a major hindrance in continued use of contraception. Covert use of contraception resulted in discontinuation when it was discovered and, in some instances, led to gender-based violence. Decision-making on contraception, method to use, and the number of children to have, was jointly done by couples or made by the husband. Reasons for discontinuation, specifically on side effects, were influenced by the husbands.
As contraceptive use in a population increases, success in avoiding unintended pregnancies depends less on initial contraceptive uptake and more on effective and persistent use. Enhanced efforts are needed to design and implement programs that focus on contraceptive discontinuation among women with unmet need for FP. Health care providers offering FP services should be well versed with the mechanism of action for the various contraceptive methods, and incorporate quality of care in the provision of contraceptive services. Additionally, contraception technological advancement is urgently needed to expand the method mix and to develop methods that have fewer side effects and side effects that can be more easily tolerated. This will go a long way in promoting continuation of contraceptive use, as indicated by a majority of our study participants who were willing to consider future use of contraception methods with fewer side effects. Findings from this study, as well as other studies, confirm the importance of engaging men and other social influencers in FP programs by educating them on the socio-economic and health benefits of family planning and dispelling any myths and misconceptions to create a social environment that supports use of modern contraception.
Availability of data and materials
The data used and analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
Consolidated criteria for reporting qualitative studies
Community health volunteers
Focus group discussions
Family planning
In-depth interviews
Long-acting and reversible contraceptive
Total fertility rate
Starbird E, Norton M, Marcus R. Investing in family planning: key to achieving the sustainable development goals. Glob Health Sci Pract. 2016;4(2):191–210.
Article Google Scholar
Canning D, Schultz TP. The economic consequences of reproductive health and family planning. Lancet. 2012;380(9837):165–71.
Ali MM, Cleland JG, Shah IH. Causes and consequences of contraceptive discontinuation: evidence from 60 demographic and health surveys. World Health Organization; 2012. https://apps.who.int/iris/bitstream/handle/10665/75429/9789241504058_eng.pdf;jsessionid=33B4B793F06D887458364DE1B36D88BA?sequence=1 .
Castle S, Askew I. Contraceptive discontinuation: reasons, challenges, and solutions. Population Council and FP2020; 2015. http://ec2-54-210-230-186.compute-1.amazonaws.com/wp-content/uploads/2015/12/FP2020_ContraceptiveDiscontinuation_SinglePage_Final_12.08.15.pdf .
Jain AK, Winfrey W. Contribution of contraceptive discontinuation to unintended births in 36 developing countries. Stud Fam Plann. 2017;48(3):269–78.
Hubacher D, Mavranezouli I, McGinn E. Unintended pregnancy in sub-Saharan Africa: magnitude of the problem and potential role of contraceptive implants to alleviate it. Contraception. 2008;78(1):73–8.
Curtis SL, Neitzel K. Contraceptive knowledge, use, and sources. In: DHS Comparative Studies No 19. Calverton, Maryland, USA: Macro International; 1996.
United Nations Department of International Economic and Social Affairs. Levels and trends of contraceptive use as assessed in 1988. United Nations Publications; 1989.
Alvergne A, Stevens R, Gurmu E. Side effects and the need for secrecy: characterising discontinuation of modern contraception and its causes in Ethiopia using mixed methods. Contracept Repro Med. 2017;2(1):24.
Ali MM, Cleland J. Oral contraceptive discontinuation and its aftermath in 19 developing countries. Contraception. 2010;81(1):22–9.
Savabi Esfahany M, Fadaei S, Yousefy A. Use of combined oral contraceptives: retrospective study in Isfahan, Islamic Republic of Iran. East Mediterr Health J. 2006;12(3–4):417–22.
CAS PubMed Google Scholar
Ojakaa D. Trends and determinants of unmet need for family planning in Kenya. In: DHS Working Papers No 56. Calverton, Maryland, USA; 2008.
Performance Monitoring and Accountability 2020 (PMA2020) Project ICRH-K. PMA 2018 Kenya Round 7 Family Planning Brief. Baltimore MD: PMA 2020, Bill and Melinda Gates Institute for Population and Reproductive Health, Johns Hopkins Bloomberg School of Public Health; 2019.
Kenya National Bureau of Statistics. Ministry of Health/Kenya, National AIDS Control Council/Kenya, Kenya Medical Research Institute, Population NCf, Development/Kenya: Kenya Demographic and Health Survey 2014. MD, USA: Rockville; 2015.
Google Scholar
Blanc AK, Curtis SL, Croft TN. Monitoring contraceptive continuation: links to fertility outcomes and quality of care. Stud Fam Plann. 2002;33(2):127–40.
PMA2020 Project ICRH-K. PMA 2018 Kenya Round 5 Family Planning Brief. Baltimore MD: PMA 2020, Bill and Melinda Gates Institute for Population and Reproductive Health, Johns Hopkins Bloomberg School of Public Health; 2017.
PMA2020 Project ICfRH-K: PMA 2018 Kenya round 6 Family Planning Brief. In. Baltimore MD: PMA 2020, Bill and Melinda Gates Institute for Population and Reproductive Health, Johns Hopkins Bloomberg School of Public Health; 2018.
Simmons RG, Sanders JN, Geist C, Gawron L, Myers K, Turok DK. Predictors of contraceptive switching and discontinuation within the first 6 months of use among highly effective reversible contraceptive initiative Salt Lake study participants. Am J Obst Gynecol. 2019;220(4):376.
Ontiri S, Mutea L, Muganda M, Mutanda P, Ajema C, Okoth S, et al. Protocol for a prospective mixed-methods longitudinal study to evaluate the dynamics of contraceptive use, discontinuation, and switching in Kenya. Reprod Health. 2019;16(1):134.
Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19(6):349–57.
Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101.
Corden A, Sainsbury R. Exploring ‘quality’: Research participants’ perspectives on verbatim quotations. Int J Soc Res Methodol. 2006;9(2):97–110.
Wellings K, Brima N, Sadler K, Copas AJ, McDaid L, Mercer CH, et al. Stopping and switching contraceptive methods: findings from Contessa, a prospective longitudinal study of women of reproductive age in England. Contraception. 2015;91(1):57–66.
Barden-O’Fallon J, Speizer IS, Cálix J, Rodriguez F. Contraceptive discontinuation among Honduran women who use reversible methods. Stud Fam Plann. 2011;42(1):11–20.
Azmat SK, Shaikh BT, Hameed W, Bilgrami M, Mustafa G, Ali M, et al. Rates of IUCD discontinuation and its associated factors among the clients of a social franchising network in Pakistan. BMC Women’s Health. 2012;12(1):8.
Ali MM, Sadler RK, Cleland J, Ngo TD, Shah IH. Long-term contraceptive protection discontinuation and switching behaviour. Intrauterine device (IUD) use dynamics in 14 developing countries. London: World Health Organization and Marie Stopes International; 2011.
Chebet JJ, McMahon SA, Greenspan JA, Mosha IH, Callaghan-Koru JA, Killewo J, et al. “Every method seems to have its problems”-Perspectives on side effects of hormonal contraceptives in Morogoro Region, Tanzania. BMC Women’s Health. 2015;15(1):97.
Burke H, Ambasa-Shisanya C. Qualitative study of reasons for discontinuation of injectable contraceptives among users and salient reference groups in Kenya. Af J Reprod Health. 2011;15:2.
Nanvubya A, Wanyenze RK, Kamacooko O, Nakaweesa T, Mpendo J, Kawoozo B, Matovu F, Nabukalu S, Omoding G, Kaweesi J. Barriers and facilitators of family planning use in fishing communities of Lake Victoria in Uganda. J Prim Care Community Health. 2020;11:2150132720943775.
Rademacher KH, Sergison J, Glish L, Maldonado LY, Mackenzie A, Nanda G, Yacobson I. Menstrual bleeding changes are NORMAL: proposed counseling tool to address common reasons for non-use and discontinuation of contraception. Glob Health Sci Pract. 2018;6(3):603–10.
Darroch JE, Singh S, Weissman E. Adding it up: the costs and benefits of investing in sexual and reproductive health 2014—estimation methodology. Appendix B: estimating sexual and reproductive health program and systems costs. New York: Guttmacher Institute 2016.
Trussell J. Contraceptive failure in the United States. Contraception. 2004;70(2):89–96.
Penfold S, Wendot S, Nafula I, Footman K. A qualitative study of safe abortion and post-abortion family planning service experiences of women attending private facilities in Kenya. Reprod Health. 2018;15(1):70.
Green CP, Chohen SI, Belhadj-El Ghouayel H. Male involvement in reproductive health, including family planning and sexual health. United Nations Population Fund New York; 1995.
Blumenthal PD, Voedisch A, Gemzell-Danielsson K. Strategies to prevent unintended pregnancy: increasing use of long-acting reversible contraception. Human Reprod Update. 2010;17(1):121–37.
Download references
Acknowledgements
The authors would like to acknowledge the generous contribution of time and expertise by those who participated in this study. We are grateful to Dr. Solomon Orero and Elizabeth Thompson from Jhpiego for reviewing the manuscript.
The study is funded by USAID Kenya and East Africa under Afya Halisi project, award number AID-615-A-17-00004. The funding institution did not play a role in the study design, implementation, in the writing of the manuscript, or in the decision to submit the article for publication.
Author information
Authors and affiliations.
Jhpiego Corporation, Johns Hopkins University Affiliate, Nairobi, Kenya
Susan Ontiri
Department of Health Sciences, Global Health, University Medical Centre Groningen/University of Groningen, Groningen, The Netherlands
Susan Ontiri, Regien Biesma & Jelle Stekelenburg
USAID Kenya and East Africa, Nairobi, Kenya
Lilian Mutea
School of Arts and Social Sciences, Moi University, Eldoret, Kenya
Violet Naanyu
Jhpiego Corporation, Johns Hopkins University Affiliate, Baltimore, MD, USA
Department of Obstetrics and Gynecology, Leeuwarden Medical Centre, Leeuwarden, The Netherlands
Jelle Stekelenburg
You can also search for this author in PubMed Google Scholar
Contributions
SO, LM, MK, RB and JS contributed to the design of the study. VN and SO performed data analysis. SO drafted the manuscript. All authors critically revised the manuscript and approved the final version. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Susan Ontiri .
Ethics declarations
Ethics approval and consent to participate.
Ethical approval was obtained from the Kenya Medical Research Institute’s Scientific and Ethics Review Unit, Nairobi, Kenya, (Approval number 650) and the Johns Hopkins Bloomberg School of Public Health Institutional Review Board, Baltimore, Maryland, United States of America (Approval number 00009062). Written informed consent was obtained from all study participants.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:.
Consolidated criteria for reporting qualitative research completed checklist.
Additional file 2:
Qualitative interview guides.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Ontiri, S., Mutea, L., Naanyu, V. et al. A qualitative exploration of contraceptive use and discontinuation among women with an unmet need for modern contraception in Kenya. Reprod Health 18 , 33 (2021). https://doi.org/10.1186/s12978-021-01094-y
Download citation
Received : 10 September 2020
Accepted : 31 January 2021
Published : 09 February 2021
DOI : https://doi.org/10.1186/s12978-021-01094-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Contraceptive discontinuation
- Contraceptive side effects
- Quality of care
- Unmet need for family planning
Reproductive Health
ISSN: 1742-4755
- General enquiries: [email protected]
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Reproductive health service utilization and associated factors among adolescents (15-19 years old) in Gondar town, Northwest Ethiopia
- PMID: 23915299
- PMCID: PMC3750465
- DOI: 10.1186/1472-6963-13-294
Background: The utilization of reproductive health services is an important component in preventing adolescents from different sexual and reproductive health problems. It plays a vital role in safeguarding youth in Sub-Saharan African countries including Ethiopia, which accounts for a high proportion of the region's new HIV infections as well as maternal and infant mortality ratios. Due to this, assessing adolescent reproductive health service utilization and associated factors has its own contribution in achieving the national Millennium Development Goals (MDG), especially goals 4 to 6.
Methods: A community based cross-sectional study was conducted from April 5-19, 2012, in 4 randomly selected administrative areas of Gondar town. A total of 1290 adolescents aged 15-19 were interviewed using a pre-tested and structured questionnaire. Data were entered in to the EPI INFO version 3.5.3 statistical software and analyzed using an adapted SPSS version 20 software package. Logistic regression was done to identify possible factors associated with family planning (FP), and voluntary counseling and testing (VCT) service utilization.
Results: Out of the total participants, 79.5% and 72.2% utilized FP and VCT services, respectively. In addition, among sexually experienced adolescents, 68.1% and 88.4% utilized contraceptive methods and VCT service during their first sexual encounter, respectively. Educational status, discussion with family/relatives, peer groups, sexual partners and teachers were significantly associated with FP service utilization. Also, adolescents who had a romantic sexual relationship, and those whose last sexual relationship was long-term, were about 6.5 times (Adjusted Odds Ratio [AOR] = 6.5, 95% CI: 1.23, 34.59), and about 3 times (AOR = 3, 95% CI: 1.02, 8.24) more likely to utilize FP services than adolescents who had no romantic relationship or long-term sexual relationship, respectively. In addition, the variables significantly associated with VCT service utilization were: participants who had secondary education and above, schooling attendance, co- residence with both parents, parental communication, discussion of services with peer groups, health workers, and perception of a risk of HIV/AIDS.
Conclusions: The majority of the adolescents were utilizing FP and VCT service in Northwest Ethiopia. But among the sexually experienced adolescents, utilization of FP at first sexual intercourse and VCT service were found to be low. Educational status, schooling attendance, discussion of services, type of sexual relationship and perception of risk were important factors affecting the utilization of FP and VCT services. Building life skill, facilitating parent to child communication, establishing and strengthening of youth centers and school reproductive health clubs are important steps to improve adolescents' reproductive health (RH) service utilization.
PubMed Disclaimer
Similar articles
- Assessment of access and utilization of adolescent and youth sexual and reproductive health services in western Ethiopia. Tilahun T, Bekuma TT, Getachew M, Seme A. Tilahun T, et al. Reprod Health. 2021 Apr 23;18(1):85. doi: 10.1186/s12978-021-01136-5. Reprod Health. 2021. PMID: 33892759 Free PMC article.
- Reproductive health service utilization and associated factors: the case of north Shewa zone youth, Amhara region, Ethiopia. Negash W, Dessalegn M, Yitayew B, Demsie M, Wagnew M, Nyagero J. Negash W, et al. Pan Afr Med J. 2016 Nov 26;25(Suppl 2):3. doi: 10.11604/pamj.supp.2016.25.2.9712. eCollection 2016. Pan Afr Med J. 2016. PMID: 28439328 Free PMC article.
- Youth friendly sexual and reproductive health service utilization among high and preparatory school students in Debre Tabor town, Northwest Ethiopia: A cross sectional study. Simegn A, Azale T, Addis A, Dile M, Ayalew Y, Minuye B. Simegn A, et al. PLoS One. 2020 Sep 30;15(9):e0240033. doi: 10.1371/journal.pone.0240033. eCollection 2020. PLoS One. 2020. PMID: 32997712 Free PMC article.
- Prevalence and Determinants of Early Initiation of Sexual Intercourse Among Youth Girls in Ethiopia. Abate BB, Kassie AM, Kassaw MW. Abate BB, et al. J Pediatr Nurs. 2020 Nov-Dec;55:e305-e312. doi: 10.1016/j.pedn.2020.06.008. Epub 2020 Jul 29. J Pediatr Nurs. 2020. PMID: 32736839 Review.
- Adolescents' Contraceptive Uptake in Ethiopia: A Meta-Analysis. Mekonnen AG, Odo DB, Nigatu D. Mekonnen AG, et al. Biomed Res Int. 2022 Aug 16;2022:6104467. doi: 10.1155/2022/6104467. eCollection 2022. Biomed Res Int. 2022. PMID: 36017384 Free PMC article. Review.
- Understanding challenges related to menstrual hygiene management: Knowledge and practices among the adolescent girls in urban slums of Jaipur, India. Prasad RR, Dwivedi H, Shetye M. Prasad RR, et al. J Family Med Prim Care. 2024 Mar;13(3):1055-1061. doi: 10.4103/jfmpc.jfmpc_1604_23. Epub 2024 Apr 4. J Family Med Prim Care. 2024. PMID: 38736813 Free PMC article.
- Assessment of the availability, accessibility, and quality of sexual and reproductive health services for young people in conflict affected zones of Cameroon: a mixed method study. Dine RD, Uwamahoro V, Oladapo JO, Eshun G, Effiong FB, Kyei-Arthur F, Tambe AB. Dine RD, et al. BMC Health Serv Res. 2023 Oct 26;23(1):1159. doi: 10.1186/s12913-023-10142-1. BMC Health Serv Res. 2023. PMID: 37884966 Free PMC article.
- Factors Associated with Utilization of Sexual and Reproductive Health Services among the Youth in Lira City West, Northern Uganda: A Cross-Sectional Study. Murungi T, Benyumiza D, Apio J, Nekesa C, Nalubuuka A, Misuk I, Kumakech E. Murungi T, et al. Biomed Res Int. 2023 May 18;2023:9649792. doi: 10.1155/2023/9649792. eCollection 2023. Biomed Res Int. 2023. PMID: 37250751 Free PMC article.
- Determinants of awareness, value perception, and societal support for sexual and reproductive health services among in-school adolescents in South-eastern Nigeria. Eze II, Mbachu CO, Agu IC, Akamike IC, Eigbiremolen G, Onwujekwe O. Eze II, et al. BMC Health Serv Res. 2023 May 17;23(1):505. doi: 10.1186/s12913-023-09470-z. BMC Health Serv Res. 2023. PMID: 37198600 Free PMC article.
- "I Don't Support It for My Children": Perceptions of Parents and Guardians regarding the Use of Modern Contraceptives by Adolescents in Arua City, Uganda. Jalinga Vuamaiku G, Epuitai J, Andru M, Aleni M. Jalinga Vuamaiku G, et al. Int J Reprod Med. 2023 Apr 3;2023:6289886. doi: 10.1155/2023/6289886. eCollection 2023. Int J Reprod Med. 2023. PMID: 37051291 Free PMC article.
- Roudi-Fahimi F, Ashford L. Sexual and Reproductive Health in the Middle East and North Africa: A Guide for reportors. Washington DC: Population Reference Bureau; 2008.
- WHO. Promoting Adolescent sexual and reproductive health through schools in low income countries; an information brief. Geneva: WHO; 2008.
- Kirby D. A proposed adolescent reproductive health intiative:Population Technical Assistance Project. Cairo: USAID, Office of Population; 1994.
- Belachew T, Abebe G, Nigussie S, H/Mariam A, Taye K, Yihdego D, Assefa D. Manual on Reproductive Health. Ethiopia: EPHTI; 2003.
- Ingwersen R. Adolescent reproductive and sexual health in the developing world. Canberra Australia: Development Studies Network; 2001.
Publication types
- Search in MeSH
LinkOut - more resources
Full text sources.
- BioMed Central
- Europe PubMed Central
- PubMed Central
Other Literature Sources
- scite Smart Citations
Miscellaneous
- NCI CPTAC Assay Portal

- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
This paper is in the following e-collection/theme issue:
Published on 20.8.2024 in Vol 26 (2024)
Effective Privacy Protection Strategies for Pregnancy and Gestation Information From Electronic Medical Records: Retrospective Study in a National Health Care Data Network in China
Authors of this article:

Original Paper
- Chao Liu 1 , PhD ;
- Yuanshi Jiao 1 , MPH ;
- Licong Su 2 , MD ;
- Wenna Liu 1 , MD ;
- Haiping Zhang 1 , BS ;
- Sheng Nie 2 * , MD ;
- Mengchun Gong 3 * , MD
1 Digital Health China Technologies Co, Ltd, Beijing, China
2 Department of Nephrology, Nanfang Hospital, Southern Medical University, Guangzhou, China
3 School of Biomedical Engineering, Guangdong Medical University, Zhanjiang, China
*these authors contributed equally
Corresponding Author:
Mengchun Gong, MD
School of Biomedical Engineering, Guangdong Medical University
No 2, Wenming East Road
Xiashan District
Zhanjiang, 524000
Phone: 86 18611768672
Email: [email protected]
Background: Pregnancy and gestation information is routinely recorded in electronic medical record (EMR) systems across China in various data sets. The combination of data on the number of pregnancies and gestations can imply occurrences of abortions and other pregnancy-related issues, which is important for clinical decision-making and personal privacy protection. However, the distribution of this information inside EMR is variable due to inconsistent IT structures across different EMR systems. A large-scale quantitative evaluation of the potential exposure of this sensitive information has not been previously performed, ensuring the protection of personal information is a priority, as emphasized in Chinese laws and regulations.
Objective: This study aims to perform the first nationwide quantitative analysis of the identification sites and exposure frequency of sensitive pregnancy and gestation information. The goal is to propose strategies for effective information extraction and privacy protection related to women’s health.
Methods: This study was conducted in a national health care data network. Rule-based protocols for extracting pregnancy and gestation information were developed by a committee of experts. A total of 6 different sub–data sets of EMRs were used as schemas for data analysis and strategy proposal. The identification sites and frequencies of identification in different sub–data sets were calculated. Manual quality inspections of the extraction process were performed by 2 independent groups of reviewers on 1000 randomly selected records. Based on these statistics, strategies for effective information extraction and privacy protection were proposed.
Results: The data network covered hospitalized patients from 19 hospitals in 10 provinces of China, encompassing 15,245,055 patients over an 11-year period (January 1, 2010-December 12, 2020). Among women aged 14-50 years, 70% were randomly selected from each hospital, resulting in a total of 1,110,053 patients. Of these, 688,268 female patients with sensitive reproductive information were identified. The frequencies of identification were variable, with the marriage history in admission medical records being the most frequent at 63.24%. Notably, more than 50% of female patients were identified with pregnancy and gestation history in nursing records, which is not generally considered a sub–data set rich in reproductive information. During the manual curation and review process, 1000 cases were randomly selected, and the precision and recall rates of the information extraction method both exceeded 99.5%. The privacy-protection strategies were designed with clear technical directions.
Conclusions: Significant amounts of critical information related to women’s health are recorded in Chinese routine EMR systems and are distributed in various parts of the records with different frequencies. This requires a comprehensive protocol for extracting and protecting the information, which has been demonstrated to be technically feasible. Implementing a data-based strategy will enhance the protection of women’s privacy and improve the accessibility of health care services.
Introduction
Medical information is generally considered to be highly sensitive for individuals, and any breach of privacy can cause direct or indirect harm to patients [ 1 ]. For female patients, pregnancy and gestation information is not only highly private but also implies the incidence of abortion, which is extremely controversial in terms of the rights and responsibilities of women in some jurisdictions [ 2 - 4 ]. Evidence suggests that the leakage of such information can negatively impact the attitudes of patients’ social environment and even health care providers [ 4 , 5 ].
The worldwide implementation of electronic medical records (EMRs) has significantly improved patient care by making health information readily accessible to a wide range of data producers. From 2007 to 2018, the average adoption rates of EMR increased from 18.6% to 85.3% [ 6 ]. This rapid growth has led to the processing and storage of various categories of patient information, including demographics, medications, laboratory tests, and diagnostic records, thereby establishing EMR as a valuable resource for large-scale data analysis of real-world data. However, the unprecedented use of EMR posed new challenges for protecting patient information effectively and preventing the unnecessary exposure of sensitive data during real-world evidence (RWE) research. Consequently, there is growing attention to the legal and technical research on extracting pregnancy and gestation information and the relevant privacy protection strategies [ 7 , 8 ].
On March 26, 2021, the Binhai Procuratorate accepted and examined a case of infringement of citizens’ personal information. Staff responsible for preventive health care at a town town-central health center in Binhai County, Jiangsu province, took advantage of their positions to illegally obtain the family contact information and home addresses of pregnant women and newborns, totaling 25,124 items. This information was then resold through digital platforms, resulting in an illegal profit of US $4566 and subjecting pregnant women to telephone harassment. In response to this phenomenon, starting in 2022, local authorities began conducting annual comprehensive inspection of the supervision of fertility information and specifically informed the procuratorial organs of the inspection results [ 9 ]. New laws and regulations have also come out, such as the “Guangdong Province Maternal and Child Health Care Management Regulations” began to implement, which came into effect on June 1, 2023. These regulations emphasize the confidentiality of personal information and privacy in maternal and child health care services and related supervision and management [ 10 ].
According to the “Technical Specifications for Hospital Information Platforms Based on EMR” issued by the National Health Commission of China in 2014, different health institutions in the country share a similar EMR framework comprising several sub–data sets including diagnostic information, medical advice, laboratory test results, examination information, and surgical records [ 11 ]. However, issues of discontinuity and incompleteness in EMR writing pose significant challenges in multicenter data integration [ 12 ]. Traditional information extraction and privacy protection strategies during RWE research and clinical data transfer have primarily focused on fixed sub–data sets, such as marriage and childbearing history, and direct data entities like the number of pregnancies in patients’ EMRs. These approaches, known as fixed site recognition strategies, lead to biased patient inclusion and flawed data masking in RWE research. For pregnancy and gestation information, testing results and procedures can indicate pregnancy status and gestation incidence without explicit descriptions in diagnostic sheets. For instance, a surgical history of pregnancy termination can imply suction aspiration abortion, while pregnancy history can be inferred from clinical test results such as human chorionic gonadotropin (HCG) levels exceeding 10 ng/L or 25 IU/L [ 13 , 14 ].
This study aims to propose protocols for the accurate and automatic extraction of pregnancy and gestation information from Chinese EMRs at the highest possible level of precision. Such information is crucial for patient inclusion and cohort identification in RWE studies to improve pregnancy outcomes [ 15 , 16 ]. Additionally, privacy protection strategies will be developed to maximize the masking of pregnancy data and identify the risk of privacy leakage for different sub–data sets within EMRs. To the best of our knowledge, this study is the first to identify the frequency of privacy information in Chinese EMRs. Then, the related risks can be considered when using patients’ EMRs for RWE research.
Data Source
This retrospective study uses the Chinese Renal Disease Data System (CRDS) database, a comprehensive national EMR database. The CRDS includes data from 19 tertiary referral hospitals across 10 provinces, representing the 5 geographical regions of China (North, Central, East, South, and Southwestern). Each hospital’s database covers the EMRs of all patients who visited from the start of 2010 to the end of 2020. The patient’s EMRs were not specially selected. Complete EMRs from each hospital were transferred to the central database located at Nanfang Hospital of Southern Medical University in Guangzhou. In this study, the total number of patients in the database is 15,245,055. All analyzed hospitalization records were structured based on the CRDS data model [ 17 ].
Sample Patient Inclusion
In this study, female patients aged 14-50 years from January 1, 2010, to December 31, 2020, were selected from the CRDS database. The statistical time here was the patient’s last visit information (including all the previous visit history), and 70% (n=1,110,053) were randomly selected for statistical analysis.
Extraction of Pregnancy and Gestation Information From Chinese EMRs
Following a preliminary investigation of Chinese EMRs, and incorporating expert guidance, teaching materials, guidelines, and literature, the research team developed the Extraction Protocol of Pregnancy and Gestation Information (EPPGI). This protocol was refined through repeated sorting, adjustment, and verification, considering the writing characteristics of various hospital medical records. Traditional methods typically extract patient data using diagnosis codes from the diagnostic sheets of Chinese EMRs. However, we first developed identification rules for test and exam results, covering patients with positive HCG results in different units of measurement and pregnancy tests.
Given the diversity and complexity of the medical coding system in Chinese EMRs, we used regular expressions (regex) to retrieve pregnancy and gestation information across entire EMRs rather than relying solely on diagnosis codes in specific sub–data sets. The adopted regex extended beyond diagnoses to include surgical procedures, chief complaints related to pregnancy status, and gestation histories. Besides, regex for medications related to inducing labor or miscarriage was used to assist in identifying pregnancy information. Other regex, including description of fetus and exclusion rules, was also applied. All regex search patterns were the product of expert meetings and discussions. The detailed rules and regex of EPPGI are listed in Multimedia Appendix 1 .
To implement this approach, we used R software (version 4.2.2; R Core Team) to extract females with reproductive activities (FRA) information from the checklist using regular expressions. In the following example, “final_medtech” represents the checklist, and “TECHNOLOGY_RESULT” is the field containing the check result in the checklist.
The rules of regex allowed us to describe the proportion of patients with a pregnancy history across different sub–data sets of EMRs and the frequency of pregnancy and gestation information. After removing duplicate patients from different sub–data sets, we retrieved data on pregnant women in the selected EMRs using EPPGI.
Privacy Protection Strategies
Based on the statistics of the located information, we proposed privacy protection strategies to avoid unnecessary and unintentional exposure of pregnancy and gestation information in real-world data analytics. Due to the different writing styles in medical records, insufficient desensitization may not fully cover sensitive patient information, while excessive desensitization may obscure other relevant information. First, EPPGI was used to identify keywords of sensitive reproductive information (SRI), such as “助产|难产|平产|早产|死产|死胎” (“midwifery|dystocia| normal birth|preterm birth|stillbirth|stillbirth”). With expert guidance, we finally chose to replace 15 characters before and after these keywords with asterisks (*) to desensitize sensitive information related to pregnancy and childbirth, thereby protecting patient privacy. This approach minimizes the possibility of inferring patients’ SRI from EMRs.
In cases where the use of maternity-related information is unavoidable, the frequency of patient identification and privacy information was used to estimate the risk of unnecessary privacy exposure methodically. We also used diagnosis and marital history as criteria to locate maternity information and compared these results across 6 large sub–data sets of EMRs. A total of 2 independent reviewers (WL and HZ) inspected both methods to ensure accuracy and reliability.
Manual Curation and Verification
Afterward, included cases were randomly selected and manually reviewed by 2 independent groups of reviewers (CL, YJ, LS, WL, HZ, SN, and MG) to test the precision and recall of the data extraction. For the EPPGI, 1000 female cases were randomly assigned to 2 external experts (Aixin Guo and Wenna Liu) to manually extract SRI. The manually extracted results were then compared with the EPPGI results to evaluate the precision and recall rate, as defined below. We also compared the precision and recall rates of the EPPGI with those obtained using only maternal and diagnostic history.
Additionally, the reviewers attempted to identify FRA in privacy-concealed data sets to test the success rate of the privacy protection strategies, as defined in Figure 1 .

Ethical Considerations
This study was approved by the Medical Ethics Committee of Nanfang Hospital, Southern Medical University (approval NFEC-2019-213), which waived the requirement for patient-informed consent due to the retrospective nature of the study. This study was also approved by the China Office of Human Genetic Resources for Data Preservation Application (approval 2021-BC0037). This study complied with the Declaration of Helsinki and the STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) statement.
To the best of our knowledge, this study is the first to identify the frequency of privacy information in Chinese EMRs.
General Information of EMRs
All patient data were extracted from the CRDS database, a real-world database that includes records from 19 hospitals. Based on the inclusion criteria (female patients aged 14-50 years from January 1, 2010, to December 31, 2020) and a 70% entry ratio, a total of 1,110,053 patients were selected as the EMR sample. It is worth noting that removing duplicates reduced the sample size from 2,377,582 to 1,585,801, which is due to multiple diagnostic records for individual patients. The admittance flowchart is shown in Figure 2 , and detailed information is displayed in Table 1 . According to Chinese national specifications for standard EMR structure, EMRs consist of similar sub–data sets with minor differences in nomenclature including doctor’s orders, diagnostic tables, test sheets, examination sheets, surgical sheets, and medical record texts. The medical record texts are further divided into 10 parts: course records, admission records, discharge records, referral records, consultation records, nursing records, death records, surgical notes, informed consent forms, and others. In CRDS, the admission record texts have been preprocessed using natural language processing for allergic history, chief complaint, disease history, tobacco and alcohol history, family history, marriage history, surgical history, and toxic exposure history. The general structure of Chinese EMRs is demonstrated in Figure 3 .

| Hospital number | City and area | Total bed numbers | FRA (n=688,268) | Total patients (n=1,110,053) |
| 1 | Guangzhou, Southern | 2225 | 57,837 | 102,483 |
| 2 | Beijing, Northern | 1650 | 30,410 | 36,757 |
| 3 | Jinan, Northern | 4000 | 79,294 | 94,339 |
| 4 | Hangzhou, Eastern | 3200 | 30,950 | 70,523 |
| 5 | Hangzhou, Eastern | 2400 | 67,086 | 82,977 |
| 6 | Guangzhou, Southern | 3000 | 53,355 | 82,654 |
| 7 | Shenzhen, Southern | 2000 | 41,352 | 48,269 |
| 8 | Nanjing, Eastern | 2499 | 33,709 | 51,919 |
| 9 | Shanghai, Eastern | 800 | 499 | 743 |
| 10 | Chengdu, Southwestern | 1000 | 21,803 | 78,843 |
| 11 | Hefei, Eastern | 3138 | 61,044 | 103,203 |
| 12 | Wuhan, Central | 5613 | 2555 | 4858 |
| 13 | Maoming, Southern | 2500 | 64,299 | 81,673 |
| 14 | Guangzhou, Southern | 2247 | 22,406 | 54,663 |
| 15 | Huizhou, Southern | 2156 | 22,756 | 23,181 |
| 16 | Guiyang, Southwestern | 2000 | 166 | 6138 |
| 17 | Foshan, Southern | 2200 | 63,336 | 125,085 |
| 18 | Guangzhou, Southern | 3000 | 6358 | 20,100 |
| 19 | Guangzhou, Southern | 1000 | 29,053 | 41,645 |
a EMR: electronic medical record.
b FRA: females with reproductive activities.

Number of FRA
After the initial investigation, we applied the EPPGI to a sample of 1,110,053 female patients of childbearing age. This analysis covered 6 different categories of EMRs, with each sub–data set and its components processed separately. Table 2 presents the total number of patients, the identified number of FRA, and their corresponding proportions.
| EMR sub–data sets | Patient number (per person) | Maternal patient number | Percentage (%) | ||
| Order | 955,140 | 146,555 | 15.34 | ||
| Diagnosis from the frontage | 1,073,167 | 312,008 | 29.07 | ||
| Laboratory report | 903,987 | 93,386 | 10.33 | ||
| Examine result | 852,143 | 172,735 | 20.27 | ||
| Prescription of surgical procedures in HIS /CPOE system | 767,693 | 157,027 | 20.45 | ||
| Total | 588,963 | 393,550 | 66.82 | ||
| Course records | 207,575 | 95,012 | 45.77 | ||
| Discharge records | 330,909 | 112,927 | 34.13 | ||
| Referral records | 9699 | 2682 | 27.65 | ||
| Consultation records | 38,728 | 12,639 | 32.64 | ||
| Nursing records | 192,080 | 112,465 | 58.55 | ||
| Death records | 953 | 105 | 11.02 | ||
| Surgical notes | 134,889 | 43,280 | 32.09 | ||
| Informed consent | 238,014 | 102,386 | 43.02 | ||
| Others | 411,637 | 138,892 | 33.74 | ||
| ) | |||||
| Total | 376,176 | 317,962 | 84.52 | ||
| Allergic history | 446,360 | 0 | 0.00 | ||
| Chief complaint | 13,925 | 55 | 0.39 | ||
| Disease history | 446,390 | 11,312 | 2.53 | ||
| Tobacco and alcohol history | 490,028 | 0 | 0.00 | ||
| Family history | 464,516 | 6 | 0.00 | ||
| Marriage history | 467,184 | 295,436 | 63.24 | ||
| Surgical history | 316,282 | 74,118 | 23.43 | ||
| Toxic exposure history | 504,022 | 4 | 0.00 | ||
a EPPGI: Extraction Protocol of Pregnancy and Gestation Information.
c EMR: electronic medical record.
d HIS: hospital information system.
e CPOE: computerized physician order entry.
f NLP: natural language processing.
The number of pregnancies identified solely by diagnosis was 312,008, accounting for 29.07% of the patients in the diagnostic sub–data set. The number of patients who were identified only by their marital and childbearing history was as high as 295,436, accounting for 26.61% of the total study population. The number of pregnancies identified by diagnosis and marital and childbearing history was 521,132, accounting for 46.95% of the total study population. If on the basis of diagnosis and marital history, the identification of diagnosis, examination, and other contents are added, the number of maternity information can be identified as 688,268, accounting for 62% of the total study population.
In the text of medical records, 393,550 patients with SRI were identified, accounting for 66.82% of 588,963 records. Due to the presence of childbearing history, which constitutes the leading source of SRI, over 80% (n=317,962) of female patients in admission records were identified as FRA by EPPGI. Besides, 58.55% (n=112,465) of female patients were identified in nursing history, making it the second highest proportion of FRA.
Based on these results, EPPGI effectively extracts FRA from every sub–data set within Chinese EMRs.
Frequency of Recognition
A single patient can generate multiple encounter records in the EMR system per visit. Therefore, individual EMRs were divided into separate records based on visits, reflecting the actual EMR storage in RWE studies. Table 3 presents the frequency of pregnancy information identification across different sub–data sets of Chinese EMRs. Similar to the results from per-patient records, SRI can be widely identified in each sub–data set of EMRs. SRI is primarily concentrated on diagnosis records, surgical records, and medical records text. In diagnosis records, SRI could be extracted from 15.06% of 15,497,063 records. In surgical records, 11.49% of SRI could be extracted from 1,604,579 records. The text of medical records showed the highest frequency of SRI identification, with an overall recognition rate of 29.92%. Additionally, it is noteworthy that more than 80% of admission records contained SRI.
| EMR sub–data sets | Record number (per visit) | Maternal record number | Percentage (%) | ||||
| Order | 93,182,790 | 384,699 | 0.41 | ||||
| Diagnosis from the frontage | 15,497,063 | 2,334,160 | 15.06 | ||||
| Laboratory report | 102,509,232 | 285,245 | 0.28 | ||||
| Examine result | 6,790,300 | 549,078 | 8.09 | ||||
| Prescription of surgical procedures in HIS /CPOE system | 1,604,579 | 184,335 | 11.49 | ||||
| Total | 8,473,462 | 2,534,940 | 29.92 | ||||
| Course records | 2,132,926 | 527,915 | 24.75 | ||||
| Discharge records | 532,790 | 151,352 | 28.41 | ||||
| Referral records | 25,171 | 6737 | 26.76 | ||||
| Consultation records | 151,564 | 43,695 | 28.83 | ||||
| Nursing records | 965,042 | 268,586 | 27.83 | ||||
| Death records | 2250 | 166 | 7.38 | ||||
| Surgical notes | 482,578 | 106,656 | 22.10 | ||||
| Informed consent | 1,226,875 | 326,284 | 26.59 | ||||
| Others | 2,377,080 | 637,807 | 26.83 | ||||
| Total | 577,186 | 465,742 | 80.69 | ||||
| Allergic history | 1,183,577 | 0 | 0.00 | ||||
| Chief complaint | 45,987 | 59 | 0.13 | ||||
| Disease history | 4,166,715 | 15,057 | 0.36 | ||||
| Tobacco and alcohol history | 858,066 | 0 | 0.00 | ||||
| Family history | 2,076,062 | 6 | 0.00 | ||||
| Marriage history | 708,544 | 444,559 | 62.74 | ||||
| Surgical history | 553,774 | 106,846 | 19.29 | ||||
| Toxic exposure history | 3,954,196 | 4 | 0.00 | ||||
a FRA: females with reproductive activities.
b EMR: electronic medical record.
c HIS: hospital information system.
d CPOE: computerized physician order entry.
e NLP: natural language processing.
Precision and Recall Rate
During the manual curation and certification process, 1000 complete EMRs were randomly selected from the sample patients and reviewed by 2 independent medical experts (Aixin Guo and Wenna Liu) to determine maternal status. The precision and recall rates of the EPPGI were 100% and 99.68%, respectively. When only diagnosis history and marital history were used for identification, the accuracy rate remained 100%, but the recall rate dropped to 73.35%. For details, see Tables 4 and 5 , where “0” represents patients without FRA information and “1” represents patients with FRA information.
| Prediction | Reference | |
| 0 | 1 | |
| 0 | 377 | 2 |
| 1 | 0 | 621 |
| Prediction | Reference | |
| 0 | 1 | |
| 0 | 377 | 166 |
| 1 | 0 | 457 |
We also conducted analyses by time and region, as shown in Tables 6 and 7 . In these tables, “quality inspection” refers to patients assessed by 2 expert manual reviews for quality control to determine the presence of labor process information (from different hospital sources); “EPPGI” refers to patients assessed using EPPGI for maternity information; and “diagnosis history and marital history” refers to patients assessed using diagnosis and marital history for fertility information. In these tables, 0 represents “no maternity information” and 1 represents “there is maternity information.” The results indicated that similar to the overall comparison, the identification of maternal information using the EPPGI method was superior to using diagnosis and marital history alone. By examining the results across different hospitals and time periods, our method proved to be universally applicable across various years and regions.
| Hospital number | Quality inspection | EPPGI | Diagnosis history and marital history | |||
| 0 | 1 | 0 | 1 | 0 | 1 | |
| 1 | 40 | 49 | 40 | 49 | 57 | 32 |
| 10 | 57 | 18 | 57 | 18 | 62 | 13 |
| 11 | 40 | 54 | 40 | 54 | 45 | 49 |
| 12 | 3 | 4 | 3 | 4 | 3 | 4 |
| 13 | 15 | 64 | 16 | 63 | 42 | 37 |
| 14 | 29 | 16 | 29 | 16 | 29 | 16 |
| 15 | 0 | 17 | 0 | 17 | 3 | 14 |
| 16 | 2 | 1 | 2 | 1 | 3 | 0 |
| 17 | 48 | 55 | 48 | 55 | 71 | 32 |
| 18 | 17 | 7 | 17 | 7 | 17 | 7 |
| 19 | 6 | 31 | 6 | 31 | 9 | 28 |
| 2 | 4 | 28 | 4 | 28 | 10 | 22 |
| 3 | 11 | 62 | 11 | 62 | 13 | 60 |
| 4 | 40 | 33 | 41 | 32 | 55 | 18 |
| 5 | 15 | 57 | 15 | 57 | 33 | 39 |
| 6 | 29 | 53 | 29 | 53 | 56 | 26 |
| 7 | 8 | 45 | 8 | 45 | 13 | 40 |
| 8 | 13 | 29 | 13 | 29 | 22 | 20 |
b EPPGI: Extraction Protocol of Pregnancy and Gestation Information.
| Year | Quality inspection | EPPGI | Diagnosis history and marital history | |||
| 0 | 1 | 0 | 1 | 0 | 1 | |
| 2010 | 14 | 9 | 14 | 9 | 19 | 4 |
| 2011 | 18 | 10 | 18 | 10 | 23 | 5 |
| 2012 | 19 | 18 | 19 | 18 | 29 | 8 |
| 2013 | 42 | 40 | 42 | 40 | 55 | 27 |
| 2014 | 46 | 59 | 46 | 59 | 60 | 45 |
| 2015 | 33 | 75 | 34 | 74 | 55 | 53 |
| 2016 | 42 | 93 | 42 | 93 | 69 | 66 |
| 2017 | 63 | 130 | 64 | 129 | 95 | 98 |
| 2018 | 60 | 107 | 60 | 107 | 86 | 81 |
| 2019 | 27 | 58 | 27 | 58 | 36 | 49 |
| 2020 | 13 | 24 | 13 | 24 | 16 | 21 |
The privacy-protection strategies were developed based on the above results. Given that we used regular expressions to identify SRI, additional text surrounding the recognized maternity information needs to be concealed to prevent privacy exposure through context. We randomly selected 1000 EMRs of pregnancy patients for static data desensitization to create a masked sample of EMRs. A total of 2 independent reviewers (Aixin Guo and Wenna Liu) were assigned to manually extract any form of pregnancy and gestation information from the masked samples. Furthermore, the risk of unnecessary privacy exposure was stratified by the frequency of recognition. The text of medical records, having the highest recognition frequency, should be handled with the utmost caution. In contrast, test and examination records are less frequently identified with SRI. It is important to note that the frequency of recognition does not fully represent the risk of privacy leakage, which will be further analyzed in the discussion section.
Principal Findings
This study is one of the first large-scale investigations into privacy leakage and FRA identification of Chinese EMRs, focusing on the frequency of recognition. The originality of this work can be summarized in 3 key aspects.
Originality in Exploring New Observations
The accessibility of EMR inevitably leads to uneven privacy protection awareness among different EMR users. The importance of reliable privacy protection methods has been extensively discussed in the literature, emphasizing their critical role in the successful implementation of EMRs in health care institutions [ 18 , 19 ]. Sensitive information regarding pregnancy, gestation, and abortion is routinely included in EMRs, raising concerns about unnecessary exposure [ 20 , 21 ]. In 2021, the Personal Information Protection Law of the People’s Republic of China came into effect, which clarified the rights and responsibilities related to the use of personal privacy information [ 22 ]. However, prior to this study, there has been little to no effort to address the highest standards of patient privacy protection protocols during RWE studies. To the best of our knowledge, this is the first study in China to use a national-level EMR database to quantitatively evaluate the exposure risk of privacy information related to women’s reproductive health. This study aims to enhance protection strategies in this area.
Originality in Designing New Experiments
The attributes and structure of Chinese EMRs are unique in terms of terminology and data standards. Accurate and comprehensive recognition of maternity information is widely reported to play a critical role in effective privacy protection and the evaluation of RWE [ 23 , 24 ]. While researchers have been working to improve the accuracy of SRI identification in non-Chinese EMRs [ 25 , 26 ], to the best of our knowledge, no prior research has focused on the accurate and complete extraction of FRA from Chinese EMRs. Traditional diagnosis-based patient extraction protocols typically use diagnosis codes, such as the International Classification of Diseases, which have 2 major limitations.
First, the records in the diagnosis sheet are often incomplete. Due to inconsistencies in Chinese EMR documentation, physicians do not always record pregnancy and gestation information as a diagnosis, especially when the patient’s primary complaint is unrelated to maternity. This leads to lower recall rates and potential recall bias. Second, due to the complexity and inconsistency of coding systems in Chinese EMRs, using codes for patient identification is more complicated than using regex, and it is nearly impossible to list all encodings exhaustively. Furthermore, regex can be widely adopted across different sub–data sets of Chinese EMRs. Although the diagnostic sheet contains the major SRI, most Chinese EMRs are still stored in text format without code mapping.
Compared to traditional diagnosis-based patient inclusion methods, the EPPGI method provides more precise results in a practical manner. Whether patient- or visit-based records, EPPGI extracts significantly more FRA with a high precision rate.
Originality in Contributing New Knowledge
Our results demonstrate that traditional fixed-site data masking procedures lead to considerable unnecessary exposure of privacy information. For instance, patients’ HCG test results or delivery procedures are commonly recorded in sub–data sets that cannot simply be concealed during RWE studies and clinical use. The combination of pregnancy and gestation information can even infer the incidence of abortion, which is highly confidential in China. Accurate and complete recognition of maternity information is essential for flawless privacy protection.
EPPGI method first identified pregnancy and gestation information across entire Chinese EMRs. For the identified information, it is practical and convenient to use data desensitization techniques, including data invalidation, data offset, and symmetric encryption, to prevent the misuse of private data. Based on the EMRs in CRDS, we determined the optimal length of additional concealed text to retain most medical information. Additionally, the quantified recognition frequency of pregnancy and gestation information helps researchers use EMRs wisely to avoid unnecessary privacy leakage. Although the frequency of identification cannot fully determine the risk of privacy leakage, which is also associated with the complexities of data desensitization, these results highlight the richness of private information ingrained in EMRs.
From a data asset management perspective, quantifying the risk of privacy leakage is critical under the strict Personal Information Protection Law. Based on statistical results and actual data mining practices, SRI is widely stored in Chinese EMRs, requiring data desensitization when using any EMR sub–data sets. For test results and structured data, the difficulty of data desensitization is relatively lower than that for plain text medical records, given the explicit nature of sensitive data entities and the low probability of reinference from context. Similar to the hazard classification of chemicals, health care data users should be aware of the richness of private information and the risk of unnecessary privacy exposure in EMRs. Maternity information is considered one of the most sensitive types of privacy for women, and our results provide a crucial reference for data users to assess related risks in Chinese EMRs for the first time.
Limitations
Overall, this work provides justification for assessing privacy leakage risk and offers a reference for effective privacy protection in Chinese EMRs. However, the proposed study has several limitations. First, the frequency of sensitive information and the privacy risk estimated in our case study are primarily based on the EMRs of a renal disease database. While there are official directions and guidelines for composing EMRs in China [ 9 ], discrepancies exist between the CRDS and other data networks in terms of data structure and operating environment. Specific protocols and variables should be optimized for generalizations.
Furthermore, the study is limited by its data scale, covering only 688,268 FRA in the CRDS. This limited scope suggests the need for further research involving larger data sets to validate and refine our findings.
Conclusions
Finding an effective and practical way to protect private information in EMRs is both meaningful and useful. We have demonstrated the feasibility of applying the EPPGI method to EMRs from 19 hospitals in different regions. We believe that EPPGI can provide a valuable reference for patient inclusion in any maternity-related studies using Chinese EMRs. Our protocols, designed for Chinese EMR systems, enable the accurate and complete recognition and extraction of pregnancy and gestation data, ensuring its effective protection. Compared to traditional methods of FRA inclusion, the EPPGI method provides more comprehensive results.
Acknowledgments
This work was supported by the National Key Research and Development Program of China (2021YFC2500200 and 2023YFC2706305). This work was supported by the Multi-modality Data Integration and Application Lab of Guangdong Medical University and the National Clinical Research Center for Geriatric Disorders (Huashan). We did not use generative artificial intelligence in any portion of the manuscript writing.
Data Availability
The data sets analyzed during this study are not publicly available due to the sensitivity of hospitals’ data but are available from the corresponding author upon reasonable request. The source code is available in Multimedia Appendix 2 .
Authors' Contributions
MG, CL, and SN conceived and designed the study. LS collected the data. YJ and WL drafted the initial manuscript. HZ and YY integrated and revised the manuscript. MG and SN served as co–corresponding authors. CL, YJ and LS served as co–first authors.
Conflicts of Interest
None declared.
The detailed rules and regex of EPPGI (Extraction Protocol of Pregnancy and Gestation Information).
Source code.
- Patrick H. Towards a privacy access control model for e-Healthcare services. In: DBLP. 2005. Presented at: Conference on Privacy, Security and Trust; October 12, 2005; Canada. URL: https://www.semanticscholar.org/paper/Towards-a-Privacy-Access-Control-Model-for-Services-Hung/e219290f8dc650863831718e97dd0e5e6b2064a2
- Johari V, Jadhav U. Abortion rights judgment: a ray of hope! Indian J Med Ethics. 2017;2(3):180-183. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Uterhark E. International law and the legalization of abortion in Northern Ireland. J Law Health. 2020;34(1):155-189. [ Medline ]
- Påfs J, Rulisa S, Klingberg-Allvin M, Binder-Finnema P, Musafili A, Essén B. Implementing the liberalized abortion law in Kigali, Rwanda: ambiguities of rights and responsibilities among health care providers. Midwifery. 2020;80:102568. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Rigdon SM. Abortion law and practice in China: an overview with comparisons to the United States. Soc Sci Med. 1996;42(4):543-560. [ CrossRef ] [ Medline ]
- Liang J, Li Y, Zhang Z, Shen D, Xu J, Zheng X, et al. Adoption of electronic health records (EHRs) in China during the past 10 years: consecutive survey data analysis and comparison of Sino-American challenges and experiences. J Med Internet Res. 2021;23(2):e24813. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Hager A, Lindblad S, Brommels M, Salomonsson S, Wannheden C. Sharing patient-controlled real-world data through the application of the theory of commons: action research case study. J Med Internet Res. 2021;23(1):e16842. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Festag S, Spreckelsen C. Privacy-preserving deep learning for the detection of protected health information in real-world data: comparative evaluation. JMIR Form Res. 2020;4(5):e14064. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Typical cases of public interest litigation for the protection of women's rights. URL: https://www.spp.gov.cn/xwfbh/dxal/202211/t20221125_593721.shtml [accessed 2024-07-30]
- Regulations of Guangdong Province on the management of maternal and child health care. People's Government of Guangdong Province. URL: https://www.gd.gov.cn/zwgk/wjk/zcfgk/content/post_2524333.html [accessed 2024-07-17]
- Technical specification of hospital information platform based on electronic medical record. National Health Commission of the People's Republic of China. 2014. URL: http://www.nhc.gov.cn/wjw/s9497/201406/a2014514701f4e76b14f3446f6318937.shtml [accessed 2024-07-17]
- Wang Z. Data integration of electronic medical record under administrative decentralization of medical insurance and healthcare in China: a case study. Isr J Health Policy Res. 2019;8(1):24. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Cervinski MA, Lockwood CM, Ferguson AM, Odem RR, Stenman UH, Alfthan H, et al. Qualitative point-of-care and over-the-counter urine hCG devices differentially detect the hCG variants of early pregnancy. Clin Chim Acta. 2009;406(1-2):81-85. [ CrossRef ] [ Medline ]
- Montagnana M, Trenti T, Aloe R, Cervellin G, Lippi G. Human chorionic gonadotropin in pregnancy diagnostics. Clin Chim Acta. 2011;412(17-18):1515-1520. [ CrossRef ] [ Medline ]
- Farland LV, Prescott J, Sasamoto N, Tobias DK, Gaskins AJ, Stuart JJ, et al. Endometriosis and risk of adverse pregnancy outcomes. Obstet Gynecol. 2019;134(3):527-536. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Attali E, Yogev Y. The impact of advanced maternal age on pregnancy outcome. Best Pract Res Clin Obstet Gynaecol. 2021;70:2-9. [ CrossRef ] [ Medline ]
- China Renal Data System. URL: http://www.crds-network.org.cn/#/database [accessed 2024-07-17]
- Kuo KM, Ma CC, Alexander JW. How do patients respond to violation of their information privacy? Health Inf Manag. 2014;43(2):23-33. [ CrossRef ] [ Medline ]
- Moore W, Frye S. Review of HIPAA, part 1: history, protected health information, and privacy and security rules. J Nucl Med Technol. 2019;47(4):269-272. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Hackett KM, Kazemi M, Sellen DW. Keeping secrets in the cloud: mobile phones, data security and privacy within the context of pregnancy and childbirth in Tanzania. Soc Sci Med. 2018;211:190-197. [ CrossRef ] [ Medline ]
- Zhang H, Zhang H, Zhang Z, Wang Y. Patient privacy and autonomy: a comparative analysis of cases of ethical dilemmas in China and the United States. BMC Med Ethics. 2021;22(1):8. [ FREE Full text ] [ CrossRef ] [ Medline ]
- NA. The National People's Congress of the People's Republic of China. 2021. Presented at: Data Security Law of the People's Republic of China; July 2017, 2024; Beijing. URL: http://www.npc.gov.cn/npc/c2/c30834/202108/t20210820_313088.html
- Gokhale M, Stürmer T, Buse JB. Real-world evidence: the devil is in the detail. Diabetologia. 2020;63(9):1694-1705. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Liu M, Qi Y, Wang W, Sun X. Toward a better understanding about real-world evidence. Eur J Hosp Pharm. 2022;29(1):8-11. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Angras K, Boyd VE, Gray C, Young AJ, Paglia MJ, Mackeen AD. Retrospective application of algorithms to improve identification of pregnancy outcomes from the electronic health record. J Perinatol. 2023;43(1):10-14. [ CrossRef ] [ Medline ]
- Moll K, Wong HL, Fingar K, Hobbi S, Sheng M, Burrell TA, et al. Validating claims-based algorithms determining pregnancy outcomes and gestational age using a linked claims-electronic medical record database. Drug Saf. 2021;44(11):1151-1164. [ FREE Full text ] [ CrossRef ] [ Medline ]
Abbreviations
| Chinese Renal Disease Data System |
| electronic medical record |
| Extraction Protocol of Pregnancy and Gestation Information |
| females with reproductive activities |
| human chorionic gonadotropin |
| real-world evidence |
| sensitive reproductive information |
| Strengthening the Reporting of Observational Studies in Epidemiology |
Edited by A Mavragani; submitted 02.05.23; peer-reviewed by S Chaichulee, M Gasmi , W Shuang, F Yu; comments to author 13.09.23; revised version received 02.01.24; accepted 22.06.24; published 20.08.24.
©Chao Liu, Yuanshi Jiao, Licong Su, Wenna Liu, Haiping Zhang, Sheng Nie, Mengchun Gong. Originally published in the Journal of Medical Internet Research (https://www.jmir.org), 20.08.2024.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work, first published in the Journal of Medical Internet Research (ISSN 1438-8871), is properly cited. The complete bibliographic information, a link to the original publication on https://www.jmir.org/, as well as this copyright and license information must be included.

IMAGES
COMMENTS
Sexual/Reproductive Health of Adolescents/Young People in Turkey-1. According to the 2000 census, the population of 10-19 and 20-24 age group is 20.7% and 9.8% of the general population, respectively in Turkey. The 2003 Turkish Demographic and Health Survey (TDHS) results show that women aged 15-24 constitute 15.8% of the female population.
Health Organization (WHO) defines reproductive health as a state of complete physical, mental and. social well-being, not just the absence of a reproductive disease or diseases. Reproductive ...
Sexual and reproductive health interventions to prevent adolescent pregnancy. Studies were included if any form of sexual and reproductive health education, counseling, and access to contraception was delivered to adolescents compared to no intervention or general health education. We identified 1,123 titles from the search conducted in all ...
Reproductive Health and Research (SRH) conducted the global SRMNCAH policy survey in 2018-2019. This survey is the fifth such survey on maternal, newborn, child and adolescent health since 2009-2010, and it is the first to include sexual and reproductive health and to align with the SDGs and the Global Strategy for
Introduction. The World Health Organization (WHO) defines adolescents as young people between the age of 10 and 19 years, and they constitute about a sixth of the world's population. 1 Adolescence has been described as a time when young people engage in increased risk-taking behaviour that exposes them to many health risks. 2,3 Adolescent sexual and reproductive health (ASRH) is a global ...
An Epidemiologic Approach to Reproductive Health Centers for Disease Control Atlanta, Georgia, U.S.A. Family Health International Research Triangle Park, North Carolina, U.S.A. ... Chapter 2 Developing a Research Proposal Learning Objectives Introduction 15 The Proposal Abstract 15 Problem Identification and Definition 17 Justification 21
Introduction. Adolescents make up over half of the world's population and represent the largest generation in history [1,2].Defined by the United Nations (UN), as young people aged 10 to 19 years old, adolescence is a key time influencing the trajectory of individual and community health outcomes [1,2].Of particular interest are adolescent sexual and reproductive health (ASRH) outcomes, as ...
To benchmark research on reproductive health and disease, we used the PubMed database to compare the number of articles published on seven reproductive organs and seven non-reproductive organs between 1966 and 2021 ().While the reproductive organs are not essential to postnatal life, we posit that the placenta and the uterus are as essential to fetal survival in utero as the lungs and the ...
Abstract. Adolescents have a high burden of sexual and repro ductive health problems and it is important to reach. out to youth groups through health promotion initiatives. A literature review was ...
WHO develops guidelines on a broad array of clinical, public health, health system, health promotion and implementation strategies. These interventions are often highly context-specific, with multiple factors that directly and indirectly impact the health and societal outcomes, and as part of these strategies, to identify key research priorities that could accelerate improvement in maternal ...
Research that explores how community-based interventions for strengthening adolescent sexual reproductive health and rights (SRHR) can be integrated and sustained in community health systems, is, to the best of our knowledge, very scarce, if not absent. It is important to document mechanisms that shape integration process in order to improve health systems' responsiveness towards adolescents ...
The sexual and reproductive health needs, and the right to the highest standard of health, for women and girls in humanitarian settings are another important area addressed by the Commission. For some people, the time spent in these difficult settings can last more than two decades. So a baby born in a refugee camp might spend the ...
Areas of work. Human Reproduction Programme. Monitoring and surveillance. Guidelines. Research. About us. We lead WHO's work on sexual and reproductive health across the life course. This work includes HRP, the UN's Special Programme of Research, Development and Research Training in Human Reproduction.
Areas of work. SRH and HRP work collaboratively with partners across the world to shape global thinking on sexual and reproductive health by providing new ideas and insights. We work together to enable high-impact research, inform WHO norms and standards, support research capacity strengthening in low- and middle-income settings, and facilitate ...
Keyword: Adolescent, sex education, reproductive health, School Health Education Programme, Sexual Reproductive Health, Sexually Transmitted Diseases Discover the world's research 25+ million members
of strategies for family planning and reproductive health services, and the health impacts of these strategies have been examined [27-30]. Nevertheless, there is a need for more impact evaluations of family planning interventions using randomized control trials, particularly in Sub-Saharan Africa where rigorous experimental evidence is scarce.
The full title of the project is: 'Promoting sexual and reproductive health among adolescents in southern and eastern Africa - mobilising schools, parents and communities". Acronym: PREPARE. The PREPARE study is funded by the EC Health research programme (under the 7th Framework Programme). Grant Agreement number: 241945.
The integration of human rights principles in sexual and reproductive health (SRH) research is often recognised to be of value. Good examples abound but lack of clarity persists as to what defines rights-inclusive SRH research. ... and agreement among key funding sources to mandate the integration of rights principles in research proposals they ...
1. Conduct a situation analysis that includes analysis of reproductive health issues, an assessment of young people's reproductive health (RH) needs, a stakeholders' analysis and problem analysis. 2. Assess organizational capacity in addressing youth RH needs and integrating youth RH into ongoing programs. 3.
Background: The Healthy People initiative is a national effort to lay out public health goals in the United States every decade. In its latest iteration, Healthy People 2030, key goals related to contraception focus on increasing the use of effective birth control (contraceptive methods classified as most or moderately effective for pregnancy prevention) among women at risk of unintended ...
Despite emphasizing the importance and benefits of men's active engagement in reproductive health programs, their engagement in reproductive health care is low. Researchers have identified different barriers to men's avoidance of participation in various aspects of reproductive health in different parts of the world. This study provided an in-depth review of the hindrances to men's non ...
Background Addressing the unmet need for modern contraception underpins the goal of all family planning and contraception programs. Contraceptive discontinuation among those in need of a method hinders the attainment of the fertility desires of women, which may result in unintended pregnancies. This paper presents experiences of contraceptive use, reasons for discontinuation, and future ...
the landscape of and gaps in existing research on adoles-cent sexual and reproductive health (ASRH) in SSA is needed to help address both barriers. To meet this need, we conducted a comprehensive scoping review of ASRH research in SSA to identify key ASRH topics and countries for which a knowledge base exists, summarise this knowledge and pinpoint
Background: The utilization of reproductive health services is an important component in preventing adolescents from different sexual and reproductive health problems. It plays a vital role in safeguarding youth in Sub-Saharan African countries including Ethiopia, which accounts for a high proportion of the region's new HIV infections as well as maternal and infant mortality ratios.
Project 2025 aims to dramatically reform the National Institutes of Health (NIH) by making it easier to fire employees and to remove DEI programs. The agency would also be stopped from funding research with embryonic stem cells and from promoting equal participation by women. [27] Conservatives consider the NIH corrupt and politically biased. [28]
Background: Pregnancy and gestation information is routinely recorded in electronic medical record (EMR) systems across China in various data sets. The combination of data on the number of pregnancies and gestations can imply occurrences of abortions and other pregnancy-related issues, which is important for clinical decision-making and personal privacy protection.