

Empathy in Healthcare: Putting Care Back into the System
More compassion, less judgmentalism, will help both doctors and patients..
Posted January 31, 2023 | Reviewed by Hara Estroff Marano
- The Importance of Empathy
- Take our Empathy Test
- Find a therapist near me
- Listening to patient concerns can create opportunity for open dialogue in the healthcare setting.
- Putting yourself in your patients' shoes can allow for understanding and empathy.
- Being open-minded, patient, and understanding to patients' concerns can build trust over time.
- Compassion is warranted for patients' healthcare concerns, not judgment.

In today's fast-paced world, healthcare providers are often under immense pressure to diagnose and treat patients quickly and efficiently. However, in their quest for efficiency, it is all too easy for them to lose sight of the fact that their patients are human beings with emotions, fears, and concerns. This is where empathy comes in. Empathy is the ability to understand and share the feelings of another person. It is a vital component of patient-centered care and one that is often overlooked in today's healthcare system.
The lack of empathy in healthcare has become a growing issue, particularly in cases where healthcare concerns are ignored or mothers are threatened in medical settings. A recent study, entitled "Giving Voice to Mothers," reviewed the inequities and mistreatment of mothers in medical decision-making . Out of the 2,700 participants surveyed, one in six women reported experiencing one or more forms of mistreatment, including being ignored, refused, shouted at, scolded, or threatened by their healthcare provider. The rates of mistreatment of women of color were consistently higher, at 27.2%, compared to 18.7% of their white counterparts.
Providers may bully patients into compliance by threatening to call child protective services, as seen in cases of mothers who hesitate or disagree with treatment protocols for their children. They may suggest the parents are neglectful without evidence.
Such actions go against the ethical guidelines set by the American College of Obstetrics and Gynecology, which condemns the use of legal threats to coerce patients into treatment. The study highlights the need for increased empathy in healthcare to ensure that mothers receive respectful, informed, and dignified care.
This type of behavior goes against the very principles of patient-centered care. It is important to remember that patients are not just bodies that need to be treated; they are individuals with their own unique experiences and perspectives. By showing empathy, healthcare providers can create a more positive and supportive environment that not only improves patient outcomes but also reduces the risk of burnout among healthcare professionals.

So, how can healthcare providers put care back into the system by incorporating empathy into their practice? Here are some tips:
Listen to patients' concerns and feelings One of the simplest and most effective ways to show empathy is to listen to what patients are saying. Give them your full attention and try to understand their perspective. This can help to build trust and create a more positive relationship between the patient and the healthcare provider.
Put yourself in the patient's shoes. Another way to show empathy is to try and imagine what it would be like to be in the patient's situation. This can help you to understand their feelings and concerns and respond in a way that is more supportive and understanding.
Be patient and nonjudgmental. Patients who are already worried or anxious about their health will likely be even more so in the face of a healthcare provider who seems impatient or judgmental. By being patient and nonjudgmental, healthcare providers can create a more positive and supportive environment for their patients.
Show compassion. Compassion is an important aspect of empathy, and it is often the missing ingredient in many healthcare interactions. Showing compassion can be as simple as smiling, making eye contact, or offering a comforting touch.
Encourage open communication. Open communication is key to building a positive relationship with patients. Encourage patients to ask questions and express their concerns. This not only shows that you are listening but also helps to build trust and improve patient outcomes.
By incorporating empathy into their practice, healthcare providers can put care back into the system and create a more positive and supportive environment for patients. Not only does this help to improve patient outcomes, but it also reduces the risk of burnout among healthcare professionals.
Remember, patients are individuals with their own unique experiences and perspectives, and it is our job as healthcare providers to show them the empathy and compassion that they deserve. By doing so, we can help to build trust and create a more positive and supportive environment for both our patients and ourselves.
DiBlasio, A., & Barazandeh, M. (2010). The importance of empathy in patient-physician relationships. The Journal of Family Practice, 59(2), 84-89.
Epstein, R. M. (1999). Mindful practice in medicine. The Journal of the American Medical Association, 282(9), 833-839.
Firth-Cozens, J. (1997). Empathy in general practice consultations: A research review. British Journal of General Practice, 47(420), 723-727.
Hojat, M., & Gonnella, J. S. (2015). The impact of empathy in medical care: A systematic review. PloS one, 10(3), e0122171.
Richardson, A. (2018, November 20). The use of Child Protective Services and court orders to enforce medical compliance in the labor and Delivery Room: How Threats of Legal Action Limit Reproductive Choice . Harvard Journal of Law & Gender. Retrieved January 30, 2023, from https://harvardjlg.com/2018/11/the-use-of-child-protective-services-and…
Vedam, S., Stoll, K., Taiwo, T. K., Rubashkin, N., Cheyney, M., Strauss, N., McLemore, M., Cadena, M., Nethery, E., Rushton, E., Schummers, L., & Declercq, E. (2019, June 11). The giving voice to mothers study: Inequity and mistreatment during pregnancy and childbirth in the United States - Reproductive Health . BioMed Central. Retrieved January 30, 2023, from https://reproductive-health-journal.biomedcentral.com/articles/10.1186/…

Erica Steele, DNM, ND, a naturopathic doctor in family practice, is trained in holistic medicine, functional medicine, integrative medicine, and homeopathy, and helps people heal all over the world.
- Find a Therapist
- Find a Treatment Center
- Find a Psychiatrist
- Find a Support Group
- Find Online Therapy
- United States
- Brooklyn, NY
- Chicago, IL
- Houston, TX
- Los Angeles, CA
- New York, NY
- Portland, OR
- San Diego, CA
- San Francisco, CA
- Seattle, WA
- Washington, DC
- Asperger's
- Bipolar Disorder
- Chronic Pain
- Eating Disorders
- Passive Aggression
- Personality
- Goal Setting
- Positive Psychology
- Stopping Smoking
- Low Sexual Desire
- Relationships
- Child Development
- Self Tests NEW
- Therapy Center
- Diagnosis Dictionary
- Types of Therapy

It’s increasingly common for someone to be diagnosed with a condition such as ADHD or autism as an adult. A diagnosis often brings relief, but it can also come with as many questions as answers.
- Emotional Intelligence
- Gaslighting
- Affective Forecasting
- Neuroscience
Empathy in patient care: from ‘Clinical Empathy’ to ‘Empathic Concern’
- Review Article
- Open access
- Published: 01 July 2021
- Volume 24 , pages 573–585, ( 2021 )
Cite this article
You have full access to this open access article

- Clarissa Guidi 1 &
- Chiara Traversa ORCID: orcid.org/0000-0002-4419-2599 1
22k Accesses
40 Citations
18 Altmetric
Explore all metrics
As empathy gains importance within academia, we propose this review as an attempt to bring clarity upon the diverse and widely debated definitions and conceptions of empathy within the medical field. In this paper, we first evaluate the limits of the Western mainstream medical culture and discuss the origins of phenomena such as dehumanization and detached concern as well as their impacts on patient care. We then pass on to a structured overview of the debate surrounding the notion of clinical empathy and its taxonomy in the medical setting. In particular, we present the dichotomous conception of clinical empathy that is articulated in the debate around cognitive empathy and affective empathy . We thus consider the negative impacts that this categorization brings about. Finally, we advocate for a more encompassing, holistic conception of clinical empathy; one that gives value to a genuine interest in welcoming, acknowledging and responding to the emotions of those suffering. Following this line of reasoning, we advance the notion of ‘empathic concern’, a re-conceptualization of clinical empathy that finds its source in Halpern in Med Health Care Philos (2014) 17:301–311 engaged curiosity . We ultimately advance Narrative Medicine as an approach to introduce, teach and promote such an attitude among medical trainees and practitioners.
Similar content being viewed by others

Should physicians be empathetic? Rethinking clinical empathy
Engaging otherness: care ethics radical perspectives on empathy, empathy as care: the model of palliative medicine, explore related subjects.
- Medical Ethics
- Artificial Intelligence
Avoid common mistakes on your manuscript.
Introduction
In the last thirty years, the notion of empathy has gained great attention within academia. Commonly defined as “feeling as others” (Hein and Singer 2008 , p. 157), the value of empathy has been up for debate. If some emphasize the importance of empathy as the essential tool for achieving a better civil society (Nussbaum 1996 ) and dealing with prominent global issues such as climate crisis (Rifkin 2009 ), others believe that empathy can “motivate cruelty and aggression and lead to burnout and exhaustion” (Bloom 2017 , p. 24).
Depending on the field of research, the notion of empathy has acquired different connotations and meanings (Cuff et al. 2016 ). In the medical field the definition of empathy has been widely debated among scholars; whereas some hold that clinical empathy is limited to a mere cognitive understanding of others’ emotional states (Finset 2010 ), others believe that clinical empathy should reflect the human purpose of medicine (Hardy 2017 ; Halpern 2014 ).
The relation between empathy and healthcare is particularly prominent in ‘Narrative Medicine’, an approach which focuses on promoting the importance of storytelling and on facilitating the empathic encounter between health practitioner and patient.
Twelve years since the establishment of the Master of Science in Narrative Medicine at Columbia University, we decided to explore the current state of empathy in the medical field and particularly in the caregiver-patient interaction.
Our aim is to provide a systematic overview of the debate on the topic, and to offer our views on the notion of ‘clinical empathy’ understood as “the ability to observe emotions in others, the ability to feel those emotions, and finally the ability to respond to those emotions” (Finset 2010 , p. 4, our italics). Ultimately, we support the conception of clinical empathy as a result of a “genuine, emotionally engaged interest in learning more about the complexity of the patient’s point of view” (Halpern 2014 , p. 308, our italics); we thus advance the notion of ‘empathic concern’ as a conceptual substitute for clinical empathy.
In accordance with Haque and Waytz ( 2012 ), we believe that the working of the current medical system can be detrimental to the well-being of both health professionals and patients. More specifically, the current medical approach has been repeatedly criticized for becoming a narrow and rigid system that does not honor the subjective experience of human suffering (Charon 2006 ). Rather, the longstanding adherence and reliance on a specific conception and application of the scientific method has, in the long run, translated itself into a cold, detached and dehumanized healthcare. Objectivity, emotional detachment and detached concern appear to be all-encompassing and thereby leave no or insufficient space for the human dimensions of illness. This phenomenon has shown to cause negative consequences for health practitioners and patients alike (Eknam and Krasner 2017 ).
As mentioned above, the mainstream medical culture is characterized by its reliance on objectivity, emotional detachment and detached concern (Coulehan and Williams 2001 cited in Shapiro 2011 ). In this paper, we will further explore how such concepts can be limiting rather than beneficial to the medical practice. Mere scientific rigor within the medical field has led to overlooking the human aspects of disease as well as its multidimensionality (Johna and Rahman 2011 ); the latter encompassing the psychological, social and moral dimensions of suffering. In this context, the distinction between disease and illness, defined as the “innately human experience of symptoms and suffering” (Johna and Rahman 2011 , p. 92), is ignored and disregarded (Reiss 2010 ).
Following this line of reasoning, we speak of detached concern as the most aspired ideal for medical professionalism, as it expresses the capacity of being concerned about something without being emotionally involved (Aring 1958 , Blumgart 1964 cited in Halpern 2014 ).
Detached concern has become an attitude that reflects a commitment to eradicate disease rather than a genuine interest in providing care. This has led to a widespread tendency to overlook ‘clinical empathy’, here defined as “the ability to observe emotions in others, the ability to feel those emotions, and finally the ability to respond to those emotions” (Finset 2010 , p. 4, our italics).
As we will see, multiple studies have shown that clinical empathy brings benefits to patients, medical students and health practitioners. In concrete terms, positive clinical outcomes for patients (AAMC 1998 cited in Ekman and Krasner 2017 ; Gleichgerrcht and Decety 2013 cited in Hooker 2015 ; Hojat et al. 2011 , 2013 ; Rosenthal et al. 2011 ) include therapeutic effectiveness, improvement in physiological responses and shorter hospitalization. Benefits that not only improve patients’ well-being (Stepien and Baernstein 2006 ; Bikker 2005 ; MacPherson et al. 2003 ; Coulehan et al. 2001 ; Vermeire et al. 2001 ; Suchman et al. 1993 cited in Chen et al. 2012 ) but also bring about economic advantages (Ekman and Krasner 2017 ; Rosenthal et al. 2011 ; Shanafelt et al. 2009 cited in Reiss 2010 ; Hojat 2009 ).
Furthermore, as we will touch upon, correlated benefits for health practitioners include an increase in professionals’ personal well-being and job satisfaction (Shanafelt et al. 2012 ; AAMC 1998 cited in Ekman and Krasner 2017 ; Larson and Yao 2005 cited in Hooker 2015 ; Rosenthal et al. 2011 ; Hojat 2009 ) together with a decrease in malpractice claims and patients’ litigations (Rosenthal et al. 2011 ; Hojat 2009 ). Additionally, higher levels of empathy have been correlated with a decrease in stress symptoms for both medical trainees and physicians (Shanafelt et al. 2009 cited in Reiss 2010 ).
The article begins by reviewing the limits of the current medical culture. Here, we first consider the origins of the phenomena of dehumanization and detached concern by looking at the American medical tradition and culture, greatly shaped by the teachings of Abraham Flexner. Secondly, we analyze the educational consequences of Flexner’s model. More specifically, we look at the decline of empathy in medical education and training, which rather reinforces a “tacit commitment to an ethic of detachment, self-interest and objectivity” (Coulehan and Williams 2001 cited in Shapiro 2011 ; p. 275).
We then pass on to explore the different conceptions of empathy within the medical setting and shed light upon the debate regarding the topic and its impact on the medical culture. While some scholars support what has been defined as cognitive empathy, others hold that affective empathy is also essential for the quality of patient care and the healthcare system in general (Hardy 2017 ; Gair 2012 ; Gallagher 2003 cited in Halpern 2014 ; Coplan and Goldie 2011 ; Stueber 2006 cited in Hooker 2015 ; Halpern 2011 ; Shapiro 2011 ; Garden 2009 ).
Within this context we argue that the dichotomous vision that prevails within such debate has led to an excessively rigid taxonomy. We try to overcome this by presenting the views of scholars that support a more inclusive and holistic definition of how empathy in the clinical setting should be understood. Following this discussion, we look at the clinical, social and economic benefits of this latter interpretation of clinical empathy for both patients and healthcare professionals.
This being said, we attempt to overcome potential downfalls of the rigid taxonomy surrounding the term ‘empathy’, whereby empathy is dichotomously divided into ‘cognitive’ and ‘emotional’ empathy. This is why we advance the notion of ‘empathic concern’ , where the focus rather lies on the notion of ‘concern’ that configures itself as a genuine interest towards the other and that results from ‘engaged curiosity; an attitude that gives value to the act of welcoming and acknowledging the complexity in the experience of those suffering (Halpern 2011 ).
Accordingly, empathic concern bears both the more cognitive perspective taking as well as the emotional engagement and responsiveness dimensions of empathy. This is how a mere commitment to heal can translate into a validation of the patient’s suffering and needs. In this sense, clinical empathy should be understood as empathic concern and as a result of ‘engaged curiosity’. We ultimately advance Narrative Medicine as an approach to introduce, teach and promote such an attitude among medical trainees and practitioners.
Limitations of mainstream medical culture
Current Western medical culture is known for its scientific rigor and its emphasis on objectivity and emotional detachment. This culture has led the Western medical system to become highly dehumanized. The origin of dehumanization in the North-American medical tradition can be traced back to the twentieth century, and partly to Abraham Flexner (1886–1959), who went down in history for his reform of medicine and higher education in the United States.
Flexner believed that the proper goal of medicine was to “attempt to fight the battle against disease” (Flexner 1912 , p. 23 cited in Johna and Rahman 2011 ). In fact, he argued that the practice and the development of medicine merely depended on those rigorously trained in natural sciences. Accordingly, Flexner believed that clinicians had to be “impregnated with the fundamental truth of biology” (Flexner 1912 , p. 23 cited in Johna and Rahman 2011 ), thus disregarding all human aspects of disease: the psychological, social and moral dimensions of suffering. Flexner thus ignored the distinction between disease and illness ; the latter being defined as the “innately human experience of symptoms and suffering” (Johna and Rahman 2011 , p. 92).
As medicine progressively relied upon objectivity and scientific rigor, it also sacrificed the subjective human experience of suffering. Illness became a “set of symptoms” (Finset 2010 ) that affected “bodies, organs and tissues” (Lewis 2011 cited in Johna and Rahman 2011 ). Still today, medicine tends to overlook patients’ humanity, and rather regards them as a cluster of organs, which display a series of biological and chemical processes. The latter are legitimately rooted at the base of medical training and of clinical practice. However, in accordance with a long tradition of scholarship, we believe that the afore-mentioned emphasis on a mere scientific approach has brought about a medical culture that pays insufficient attention to the value of understanding and honoring the human body and the person as a whole (Haque & Waytz 2012 ; Reiss 2010 ).
It is in this sense that we see the current medical approach as a narrow and rigid system; the symptoms one manifests tend to be medically suppressed rather than being taken as tools to deepen and investigate the etiology of a particular symptom or illness. The body has been separated from the mind and the self; it is in fact cut out of the picture, thus producing a dichotomy in which the physical body-world is deprived of the mental and spiritual spheres. This separation leads to the dehumanization of the ill, whose disease becomes more important than the person themselves.
The establishment of the above-mentioned medical culture, to some extent initiated by Flexner’s reform, deeply shaped the mainstream clinical practice and patient care. In fact, the latter are characterized by the so-called ‘detached concern’, a notion that originated between the 1950s and 1960s (Aring 1958 ; Blumgart 1964 cited in Halpern 2014 ). Since then, detached concern has been considered as the most coveted ideal for medical professionalism and its enactment has translated into a widespread tendency to overlook the value of a “genuine, emotionally engaged interest in learning more about the complexity of the patient’s point of view” (Halpern 2014 , p. 308).
Accordingly, sociologists identify the loss of the human sphere in medicine and the de-personalization of care as two social phenomena that originated in the 1960s. As objectification, together with commodification and standardization, became the reasoning behind medical achievements, healthcare began to deny the significance of meaning, interest and compassion. In this context, objectification exemplifies and upholds medicine’s commitment to the mechanistic Cartesian mind–body divide, a tendency to transform the subjective/social into the objective/biological (Scheper et al. 1987 ).
In recent decades, some academics have started to point out the fact that medical education is indeed “overvaluing scientific measurements and undervaluing subjective experiences” (Reiss 2010 , p. 1604); something that greatly impacts the quality of healthcare. In fact, illness is not only physical and reducible to biological dysfunctions; it is rather multidimensional (Johna and Rahman 2011 ). As such, the ill person can be disempowered due to bodily impairment, lack of the necessary knowledge and hope to take rational steps towards recovery, loss of some degree of autonomy and the alteration of self-image and identity due to such circumstances (Pellegrino 1981 cited in Johna and Rahman ( 2011 ). Likewise, patients are not just bodies, organs and tissues; as any other human being, they “live meaning-centered lives, and they have complicated emotional and historical relationships with their bodies” (Lewis 2011 , p. 92 cited in Johna & Rahman 2011 ).
Nevertheless, the medical system often does not recognize the complex and unique human capacities and resources of patients. As Michel Foucault suggested, medical institutions and the scientific disciplines of modernity are characterized by an objectification of bodies aimed at turning humans into subjects and objects of knowledge (Foucault 1973–1978 cited in Timmermans 2009 ). In this light, medicine has become a science for science’s sake, leaving behind its original human-centered purpose. This translates to a generalized shortage of empathy in patient care. In fact, medical practitioners are trained to embrace the notion of detached concern and reject engaged human connection.
The above-mentioned principles that characterize the current Western medical culture are also reinforced by and through medical education. Although in recent years, there have been attempts to reintroduce the values of compassion and empathy in the medical training, the medical establishment still relies on a “tacit commitment to an ethic of detachment, self-interest and objectivity” (Coulehan and Williams 2001 cited in Shapiro 2011 , p. 275). The medical culture, together with its fear and rejection of human emotions, thus contributes to shaping a medical training that perpetuates “emotional detachment” and “clinical neutrality” (Hojat et al. 2009 cited in Reiss 2010 ). Correspondingly, physicians learn to feel uncomfortable admitting error. In this regard, studies show that when error occurs, caregivers tend to feel guilty and inadequate (Gallagher et al. 2003 cited in Halpern 2014 ).
Medical training is based on a positivist worldview that promotes the objectification of patients; the latter can lead to a feeling of alienation from rather than empathy towards the patient, on the part of the doctor (Crandall and Marion 2009 cited in Shapiro 2011 ). Accordingly, the cultural norms that shape medical education expect aspiring doctors to conceal emotion (Shapiro 2011 ). Thereby, the most widely accepted conception of medical professionalism is one in which physicians “respond to the suffering of patients with objectivity and detachment” (Coulehan 2009a , b cited in Shapiro 2011 ).
Overall, medical pedagogy promotes detached concern, which in turn devalues the importance of subjectivity, the role of emotions and the healing power of relationship and solidarity (Coulehan 2005 cited in Shapiro 2011 ). According to several studies (Bellini and Shea 2005 ; Hojat et al. 2004 ; Bellini et al. 2002 cited in Chen et al. 2012 ), detached concern becomes prominent during the third year of medical training; when students become interns and first enter the professional world. The third-year decline of empathy, partly due to actual contact with suffering, death and deficiency in training in engaging emotions has also been correlated to students’ inexperience in modulating their emotional states in the context of demanding environments (Hojat et al. 2009 cited in Reiss 2010 ).
Empathy in the medical setting
In the last two decades the notion of empathy has gained remarkable attention within the academic world. Generally speaking, outside the medical setting, empathy is defined as the ability to ‘feel with’ another person or to put oneself into someone else’s shoes (Halpern 2014 ).
In the medical setting, definitions of empathy are still widely debated; scholars commonly agree that empathy is distinguished from sympathy. The latter is usually understood as the action of ‘feeling for’ another person; in other words, caring about the patient.
According to some (Trevithick 2005 ; Boulton 1987 cited in Gair 2012 ), empathy is understood as ‘feeling with’ the patient. Others, instead, define empathy as the cognitive skill that allows the practitioner to understand the patient. Those who follow this latter line of reasoning create a divide between the cognitive ability to understand the other (belonging to their notion of cognitive empathy) and the affective dimension of feeling for (which they relegate to sympathy), and with the other (which they relate to emotional empathy). In any case, there is a tendency among scholars to distinguish between two main categories of empathy: cognitive empathy and affective empathy.
Cognitive empathy
‘Cognitive empathy’ is defined as the ability to perceive emotions in others and as the capacity to attribute mental states to them. In other words, it can be understood as an equivalent of the ‘Theory of Mind’ phenomenon (Schulte-Ruther et al. 2007 cited in Finset 2010 ). This mental process is reached through the so-called ‘Simulation Theory’. According to this theory we understand the mental states of others by simulating them and it is our very ability to see the world from the other’s point of view that allows us to gain an understanding of the other’s experiences of the world (Gladstein 1983 ; Rushton 1980 cited in Pedersen 2008 ). This notion of empathy excludes any emotional engagement.
The emphasis on the cognitive dimension of empathy makes this notion compatible with the predominant medical culture; one that values detachment, objectivity, and standardization. Thereby, this notion of empathy has become predominant in the context of medical care. In fact, it is believed that it allows physicians to maintain a professional distance from patients, to make objective clinical decisions and to regard patients as equally deserving of care (Coulehan 1995 ; Roter et al. 1997 cited in Halpern 2011 ).
Nevertheless, cognitive empathy has been criticized for numerous reasons. In fact, according to Garden ( 2009 ), this type of empathy brings about the risk of obscuring rather than shedding light on patients’ experience of illness. This is due to the mentioned simulation process; in fact, “when the physician simulates the patient, the physician’s understanding is limited to what the physician can imagine about the patient’s experiences” (Hardy 2017 ). This is referred to as “the diversity problem” pointed out by Gallagher (2012), by which the clinician’s understanding of what a patient is going through is limited to what caregivers themselves have experienced. In this sense, it is believed that a shared experience or “common wound” is necessary for empathic understanding (Gair 2012 ).
According to Shapiro ( 2011 ), the strong emotional suppression that characterizes cognitive empathy, and which tends to arise when dealing with death, disability, medical error, and mortality, can lead to exhaustion and burnout; making this vision of empathy less sustainable than what the medical community has upheld. Moreover, according to Hooker ( 2015 ), when physicians employ a parallel understanding, they neglect not only the fundamental differences between themselves and the patient, but also the distinction between each individual patient. Lastly, Hardy ( 2017 ) holds that the use of cognitive empathy reinforces and upholds the objectification of the patient, by which the individual is still being treated as an object for observation and judgment, rather than a subject with whom physicians interact.
Affective empathy
On the other hand, ‘affective empathy’ is described as the emotional engagement that occurs when confronted with the suffering of another person. As such, this form of empathy is disregarded by the medical community and the mentioned medical culture. In fact, it is common belief that emotional empathy relies on “untrustworthy feelings” (Halpern 2014 ). Despite this attitude, there is growing support of the idea that affective empathy facilitates the recognition of the emotional state and/or predicament of the patient. Additionally, emotional engagement is seen as beneficial as it can kindle the desire ‘to heal’ in physicians; thus, moving beyond the sense of duty to simply eradicate disease.
However, due to a longstanding fear of over-identifying with patients, emotional engagement itself has been identified as one of the main risk factors for the loss of objectivity and the manifestation of emotional distress (Halpern 2001 ). As we have seen, objectivity is considered the bedrock in most clinical circumstances and interventions; for instance, in the case of a difficult diagnosis and/or when invasive treatment is necessary (Halpern 2014 ). In fact, it is believed that emotions undermine the ability to achieve successful medical outcomes in delicate circumstances (Coulehan 1995 cited in Halpern 2011 ).
As already noted, affective empathy is furthermore considered to lead to emotional burnout. This apprehension has determined the implementation of detached concern, shaping decades of medical education and training, which, still to this day, overlooks the individual’s experience of illness. Given the established association between emotional engagement and the occurrence of distress and/or burnout on behalf of physicians (Fox et al. 2009 ; Alma & Smaling 2006 ; Astell 2004 ; Figley 2002 cited in Gair 2012 ), it has been suggested that emotional down-regulation may be necessary (Reiss 2010 cited in Halpern 2011 ).
Finally, the attempt to avoid burnout has led to the formulation of an idealized version of empathy on the part of the doctor, “one in which they suppress personal emotions yet are motivated by an altruistic yet ‘detached’ concern for patients” (Halpern 2014 , p. 301).
Debate on the definition of empathy
The heated discussion concerning the above-mentioned divide has led scholars and the medical community to attempt to identify the best type of empathy to call upon in the clinical setting as well as to speculate whether an integration of cognitive and affective empathy may be neurologically possible.
In relation to the first point of debate, for the reasons mentioned above the mainstream medical culture has privileged cognitive empathy over emotional empathy and has established the former as the most suitable type to employ within the clinical setting. However, studies support the idea that both the cognitive and the affective dimensions of empathy are valuable. In fact, as stated by Coplan and Goldie ( 2011 ) as well as Stueber ( 2006 ), empathy is all about understanding the patient. This understanding, however, is not merely cognitive but also involves a genuine emotional response that fully recognizes the patient.
Hence, according to Shapiro ( 2011 ), we should not dismiss the emotional component of empathy based on the misconception that emotional engagement is dangerous in-patient care. In fact, Shapiro suggests that, contrary to the dominant belief, purely cognitive empathy without a balanced amount of emotion brings about the risk of making the medical encounter over-operationalized and excessively codified. In other words, “a richer clinical empathy, involving emotional and cognitive empathy, makes for more effective medical care.” (Halpern 2011 , p. 229, our italics).
Furthermore, in relation to Halpern’s statement ( 2011 ), it has been reported that patients are considerably hungry for and deeply desirous of being understood and recognized (Broyard 1993 cited in Hooker 2015 ). Keeping this in mind, the importance of combining the two facets of empathy is valuable not only to achieve effective medical outcomes, but also to validate and dignify the human needs of patients.
Coming to the second point: given the importance of the co-existence of the discussed cognitive and affective aspects of empathy, scientists have investigated the neurological possibility of the two co-occurring. Research in psychology has tended to assume incompatibility, according to which the two dimensions of empathy are mutually exclusive. The result has been setting one against the other (Zaki et al. 2008 cited in Halpern 2014 ). Similarly, neuroscientific studies have shown that there are distinct brain pathways in the empathic response. In fact, it appears that different parts of the brain are activated depending on cognitive versus affective cues (Decety 2011 cited in Halpern 2014 ).
Nonetheless, according to Halpern, these conclusions do not imply that the mentioned brain pathways do not coordinate in real life settings. On this line of reasoning, Zaki et al. ( 2008 ) suggests that it is likely that in naturalistic settings they interact in complex ways. In fact, real life interactions involve multimodal cues , in contrast to the pathways of separate responses that usually make use of written word narratives versus facial expressions .
Thereby, which pathway (and thus type of empathy) one uses depends and varies according to the context. In the medical setting, this translates into an empathic response that is elicited by both verbal and non-verbal cues is elicited by both verbal and non-verbal cues (Halpern 2014 ).
Impact of the debate on medical culture
Influenced by the medical culture and its view of cognitive and affective empathy as being mutually exclusive, the medical research community has tried to scientifically prove the need to privilege cognitive empathy over its emotional counterpart. To this regard, in a study conducted by Decety ( 2010 ) it was reported that physicians’ brains showed more brain activity than non-physicians in the regions involving executive control and self-regulation; at the same time, they displayed a down-regulation of the brain regions involved in emotional responsiveness. Additionally, another study (Neumann et al. 2011 cited in Halpern 2014 ) showed that medical students who reported more emotional discomfort in response to their patients’ distress had lower scores in cognitive empathy during their training.
These findings have led some to wonder if medical students with more emotional empathy will lack its more accepted counterpart, that is cognitive empathy. Following this line of reasoning, others have suggested that it is vital for physicians to use cognitive empathy when communicating with patients about painful procedures and that it is fundamental to use cognitive empathy to ensure that the patient’s needs are being adequately addressed (Halpern 2014 ).
However, the above-mentioned studies overlook important distinctions between self-related anxiety and the emotional distress that may derive from the affective resonance with others; something that still needs further investigation. In fact, as Halpern ( 2014 ) suggests, while some physicians may respond with emotional distress when interacting with patients, others may react with a genuine prompt to heal. This calls for further investigation.
- Clinical empathy
As we have seen, there is a dichotomous vision that prevails in the medical culture to the point that medical research has tried to prove the mutual exclusivity between cognitive and affective empathy. Overall, the competing aspect of the debate around the two conceptions of empathy results in creating an excessively rigid taxonomy. In order to overcome such difficulties, scholars have advanced a more inclusive and holistic definition of what empathy in the clinical setting should really entail.
Despite being identified with cognitive empathy, the notion of clinical empathy goes beyond the mere cognitive understanding of the other’s emotions. ‘Clinical empathy’ has been defined as “the ability to observe emotions in others, the ability to feel those emotions, and finally the ability to respond to those emotions” (Finset 2010 , p. 4, our italics).
As a multidimensional ability, clinical empathy branches out in three distinct components: a cognitive component, an emotional component and an action component. If the first one is the mental process through which “the physician ‘enters’ the perspective of the patients”, the emotional component allows the practitioner to “[put] himself or herself in the place of the patient”. Finally, the action component, whereby the physician “communicates understanding by checking back with the patient” (Coulehan et al. 2001 ; Hojat et al. 2001 cited in Chen et al. 2012 ; Johna and Rahman 2011 cited in Finset 2010 ).
To this regard, it has been noted by Alma and Smaling ( 2006 ) that the empathic communicative response is not merely expressed through words. It can also be non-verbal, including tone of voice, facial expressions, body posture, and natural gestures (Gair 2012 ). This view is shared by Haslam ( 2007 ), who states that “empathy is not only a compassionate appreciation of the patient’s emotions, but also [includes] an expression of that awareness to the patient” (cited in Gair 2012 , p. 135). This comprehensive vision of empathy translates to the affective capacity to “feel with” the suffering of the patient and the cognitive ability to take the perspective or to “put yourself in the shoes of the patient” (Reiss 2010 cited in Ekman and Krasner 2017 ).
Others support the multidimensional nature of empathy, but indicate slightly different components. Decety and Lamm ( 2006 ), for instance, hold that empathy consists of three dimensions: emotion sharing, perspective-taking and emotional regulation. However, this third component differs from the ones stated above, as it involves the capability to both regulate and modulate the empathic response. With regards to this formulation, Shapiro ( 2011 ) suggests that we should not ignore and suppress the uprise of emotions, but rather regulate and modulate them.
In line with this reasoning, research in neuroscience has shown that the awareness of a distinction between the experiences of the self and the experiences of others constitutes a crucial aspect of an ideal clinical empathy. Thus, the psychological construct of empathy could be defined as the intersubjective induction process by which emotions are shared without forgetting what feelings belong to whom (Decety and Meyer 2008 cited in Ekman and Krasner 2017 ).
In fact, empathy can only be effective if individuals are able to separate their own feelings from those shared with others, thus having self-awareness and other-awareness (Decety and Lamm 2006 ). In other words, “to sense the [careseeker] private world ‘as if’ it were your own but without ever losing the ‘as if’ quality—this is empathy and this seems essential to therapy” (Gair 2012 , p. 832).
This being said, clinical empathy encloses a detailed experiential and a cognitive understanding of what the patient is feeling. As such, it is neither emotional detachment nor a complete immersion in the other’s experience. Accordingly, and as we will later stress, empathy is “an ongoing double movement of emotional resonance and compassionate curiosity about the meaning of the clinical situation to the patient” (Shapiro 2011 , p. 276).
Building upon Geldard and Geldard ( 2005 ), we believe that empathy is about “having a togetherness with the [patient]... going on a journey with [patients], listening with sensitivity, matching their every move... walking beside the [patient]” (p. 18). When experienced with self-awareness, clinical empathy shows to be a mutually healing connection with the patient (Kearney et al. 2009 cited in Shapiro 2011 ); and thus, it is not lived as a detrimental emotional burden.
Benefits of empathy in patient care
As mentioned, patients have reported the longing for a more human-oriented contact with caregivers. According to research, clinical empathy allows patients to feel respected and validated in their experience of illness (Beckman et al. 1994 ). Within this framework, there have been attempts to bring the medical approach towards a relationship-centered care model; where the human dimension is central and patients’ experiences are seen as valuable. Here, clinical empathy is considered as a means of helping patients to experience and express emotions (Beach and Inui 2006 cited in Garden 2009 ).
Research shows that allowing space for a patient’s narrative is neither inefficient nor time-consuming. In fact, giving patients space to express their personal concerns has been shown to take no longer than 90 s and yet to considerably improve patient satisfaction and adherence to treatment (Langewitz et al. 2002 cited in Halpern 2014 ).
This being said, not only does this type of empathy promote patients’ and physicians’ satisfaction and well-being, but it also plays a role in improving medical outcomes (Bikker et al. 2005 ; MacPherson et al. 2003 ; Coulehan et al. 2001 ; Vermeire et al. 2001 ; Suchman et al. 1993 cited in Chen et al. 2012 ). In fact, clinical empathy helps clinicians recognize, understand and accept patients in their suffering. This inclusive understanding is the first step towards alleviating their distress; something that occurs through the process of ‘being moved’ to action (Garden 2009 ).
For patients
Through its capacity to cultivate trust, communication, and mutual understanding, clinical empathy has positive impacts on multiple levels. Generally speaking, it has been reported that empathic caregiving improves patient satisfaction as well as clinical outcomes, to name a few (Mercer et al. 2016 ; Shanafelt et al. 2002 ; Shapiro et al. 1989 cited in Ekman & Krasner 2017 ; Derksen et al. 2013 ; Gleichgerrcht & Decety 2013 cited in Hooker 2015 ; Hojat et al. 2013 ; 2011 ; Rosenthal et al. 2011 ; Zachariae et al. 2003 cited in Finset 2010 ; Bertakis et al. 1991 ; Beckman et al. 1984 ; Francis et al. 1969 cited in Hojat 2009 ).
In a study conducted by Zachariae et al. ( 2003 ) with oncology patients, high scores of physician’s empathy and consideration resulted in improved patient’s experience of care. Additionally, the scores were associated with increased autonomy, and reduced emotional distress after the consultatio (Finset 2010 ). In another study (Graugaard et al. 2004 cited in Finset 2010 ), empathy was shown to increase fibromyalgia patients’ satisfaction; in particular among those with difficulties in expressing their own emotions.
Further, it has been reported that one of the biggest limitations of effective medical treatment is patient non-adherence. To this regard, studies have shown that about fifty percent of treatments are not taken as prescribed (Ekman and Krasner 2017 ); something that can negatively interfere with the patient’s recovery.
According to academic research, empathy may offer a solution to this problem. In fact, empathy in patient care results into positive clinical outcomes, such as patients’ compliance with the medical care plan and engagement in medical recommendations (Ekman and Krasner 2017 ; Rosenthal et al. 2011 ; Roter et al. 1998 cited in Halpern 2014 ; DiMatteo et al. 1986 , 1993 ; Squier 1990 ; Eisenthal et al. 1979 cited in Hojat 2009 ).
Additionally, empathy has been shown to facilitate patients’ understanding of treatment options and participation in making decisions concerning therapy. By feeling empowered in the therapeutic process, patients are more inclined to follow their medical treatment plan (Halpern 2014 , 2001 cited in Hooker 2015 ).
Going back to the central role played by trust in the empathic relationship between health practitioner and patient, a meta-analysis of factors that improve adherence to treatment (Roter et al. 1998 ) illustrates that trust was one of the most important steps towards engagement in medical treatment. In other words, the patient’s feeling of trust was the sense that the physician was genuinely worried about them.
Additionally, other studies (Kim et al. 2004 cited in Halpern 2014 ) have suggested that patients trust empathic physicians more, and that this increases the effectiveness of medical care. Overall, an empathic relationship leads to better physiological responses and shorter hospitalization (Reiss 2010 cited in Halpern 2011 ). Such benefits result in lower costs of medical care (Rosenthal et al. 2011 ; Hojat 2009 ).
Another factor that leads to reducing costs has been studied by Nightingale et al. ( 1991 ). In this study, it was shown that empathic physicians avoided unnecessary costs by ordering fewer laboratory tests and were less inclined to perform invasive and costly interventions, unless strictly necessary.
As mentioned, the current medical culture stigmatizes and does not provide a sufficient framework to prevent medical error. In a study conducted by a group of medical residents training at the Mayo Clinic, error was associated with lower levels of empathy (Ekman and Krasner 2017 ). Thereby, we may assume that through the use of empathy physicians make fewer errors during the diagnostic procedure. This may occur because empathic physicians are more prone to obtain critical information and deeper insights; something that positively affects the overall quality of care and fosters favorable medical outcomes (Shanafelt et al. 2009 cited in Reiss 2010 ).
For caregivers and medical students
Coming to the benefits for physicians and medical students, research has reported a correlation between an empathic approach and health professionals’ personal well-being and job satisfaction (Shanafelt et al. 2012 ; AAMC 1998 cited in Ekman and Krasner 2017 ; Larson and Yao 2005 cited in Hooker 2011 ; Rosenthal et al. 2011 ; Hojat 2009 ).
Additionally, empathic communication has been correlated with fewer malpractice claims and fewer patients’ litigations (Rosenthal et al. 2011 ; Moore et al. 2000 ; Steward et al. 1999 ; Levinson et al. 1997 ; Beckman et al. 1994 ; Hickson et al. 1992 ; 1994 ; Shapiro et al. 1989 ; Avery 1985 cited in Hojat 2009 ).
Furthermore, lower empathy may increase the occurrence of medical errors as well as increase the distress experienced by health professionals (Ekman and Krasner 2017 ). On the same line of reasoning and contrarily to the tendency to regard empathy as unnecessary, when not harmful, higher levels of empathy have been shown to prevent symptoms of burnout (Diorio and Nowaczyk 2019 ), substance abuse and suicide amongst both physicians and trainees (Shanafelt et al. 2009 cited in Reiss 2010 ).
From clinical empathy to empathic concern
We have looked at the benefits that come along with the implementation of what we refer to as clinical empathy. In accordance with academic scholar Halpern ( 2011 ) we hold that we should go beyond the mere focus on the debate regarding the different components of empathy and the manner in which they interrelate in empathic interaction.
In this section we attempt to overcome the potential downfalls of the rigid taxonomy surrounding the term ‘empathy’, whereby empathy is dichotomously divided into ‘cognitive’ and ‘emotional’ empathy. This is why we propose the notion of ‘empathic concern’, whereby clinical empathy is understood as the attitude of genuine interest towards the experience of the other, and that results from ‘engaged curiosity’.
In the attempt to address the patient’s need to be valued and understood, Halpern ( 2011 ) suggests that clinicians embrace the notion of ‘engaged curiosity’ . She defines the latter as a “genuine, emotionally engaged interest in learning more about the complexity of the patient’s (and our responsive) emotional points of view” (p. 308); something that we propose a precondition for ‘empathic concern’. Here, ‘concern’ is very different from the said detached concern and translates a mere commitment to heal to a validation of the patient’s suffering and needs.
Thereby, empathic concern in the clinical setting derives from a genuine interest in the patient and varies according to each unique experience (Halpern, 2011 ). In fact, the latter can never be generalized and strictly associated with a specific ‘type’ of empathy. This empathic engagement is reached through curiosity about what the patient is specifically concerned about, non-verbal attunement and the effort to imagine the other’s experience. The health professional is thus led to welcome a deeper and more comprehensive understanding of the patient’s experience.
In fact, there are situations in which it is simply necessary to acknowledge the patient as a human being “with feelings and worth” (Halpern 2011 ). This means that in many contexts clinicians are not expected to engage in any sort of specific empathy. To this regard, according to Halpern ( 2011 ) patients reportedly appreciate their physician’s curiosity even in moments when the caregiver has trouble fully understanding them and what they are going through.
Moreover, clinicians are aware of the fact that they will not completely understand their patients unless they actively try to find out more about the patient’s situated experience; that is, what the patient is needing, seeking or afraid of. This awareness is what allows clinicians to maintain the distinction between the self and the other; something that ultimately avoids unnecessary distress and/or error deriving from over-identification (ibid).
Multiple studies have shown the validity of such an approach. For instance, an observational study conducted by Shanafelt et al. ( 2005 ) in 2005 illustrated that when physicians show non-verbal attunement (for example through gestures), patients give fuller stories and are more open to talk about the emotional aspects of their narratives; often critical elements for a correct diagnosis, and thus essential for an effective medical treatment. Similarly, Suchman et al. ( 1997 ) reported that, in many cases, patients tell important information to physicians who are not verbally attuned, but who rather show hints of their emotional engagement.
In line with the above-mentioned results, according to Halpern ( 2014 ) engaged curiosity can help caregivers avoid clinical mistakes, such as ‘projection’, ‘overidentification’ and ‘naive sympathy’. Projection is the process by which physicians project themselves onto the patients. When this occurs, physicians think that they know what their patient is worried or concerned about; even when, in actuality, this is not the case. It may also happen that clinicians over-empathize with their patient, and thus think that what the latter is going through is similar to what they have experienced.
By doing so, the physician overlooks the fact that individuals may experience the same thing in a different manner, and thereby fall into the trap of overidentification. Both projection and overidentification may give rise to naive sympathy; a superficial emotional engagement that is usually not appreciated by the patient, as it does not confer an adequate importance to the patient’s situation (Halpern 2014 ).
Fostering empathic concern in patient care: the role of Narrative Medicine
We have seen how the current medical culture, with its worship of objectivity and emotional detachment, has put aside the importance of acknowledging the human experience of illness. This phenomenon is closely linked to medical training. In fact, the latter has the tendency to neglect the individual of the fundamental aspects of patient care; namely, the human relationship in the context of illness.
In this paper, we have made an attempt to problematize the rigid taxonomy and dissection of the notion of empathy that is still prominent in existing scholarship. By questioning the widespread dichotomous distinction between cognitive and affective empathy, we highlighted the potential of what is referred to as clinical empathy as a more holistic human capacity.
According to Halpern ( 2014 ), one of the basic elements of patient care is the caregiver’s ability to make an effort to listen to the patient’s unique experience with illness and sensitively communicate this understanding to them.
Following this line of reasoning, we illustrated Halpern’s notion of engaged curiosity as a precondition for what we propose as a new understanding of clinician empathy; namely, empathic concern. The latter being an approach that gives value to a genuine interest in welcoming, in acknowledging and in responding to the emotions of those suffering. In this sense, empathic concern calls for an interest on behalf of the clinician that allows patients to feel recognized, understood and accepted in their hardship.
This approach presents many analogies with ‘Narrative Medicine’, a medical approach that “fortifies the clinical practice with the narrative competence to recognize, absorb, interpret and to be moved by the stories of illness” (Charon 2007 , p. 1265). In this sense, Narrative Medicine represents a form of medical practice that brings to light and validates the stories of the ill. Illness unfolds in stories and it should be the medical practitioner’s concern to listen and to honor those narratives, so as to recognize and legitimize the basic dignity of the patient.
Narrative Medicine is a person-centered approach, as it focuses on active listening and engaged communication, which elicit the patient’s perspective and experience (Finset 2010 ; Charon 2004 ). In this sense, Narrative Medicine represents one of the attempts to rehumanize medicine and to address the issues that can be found in Flexner’s model, as discussed in the section concerning the current western medical culture.
As a more holistic and comprehensive medical-care model, Narrative Medicine promotes self-awareness and other-awareness. In this sense, it constitutes a ‘middle ground’ between medical practitioners and patients, as it allows the former to take the other’s perspective and explore a subjective experience of illness through the facilitation of the patient’s expression (Johna and Rahman 2011 ). This occurs thanks to the recognition of empathic opportunities; in other words, hints and cues that can elicit empathic concern towards the patient (Eide et al. 2004 cited in Finset 2010 ).
As mentioned, the core values of Narrative Medicine can also be reached by fortifying the current medical training with narrative practices. In fact, something that is central to narrative competence is the capacity for self-reflection, awareness and interpretation of emotional responses of the other, and the development of insight and sensitivity to be moved and act accordingly to the patient’s needs, being these emotional or physiological.
To this regard, in a 2001 study Charon ( 2001 ) has shown that clinicians who learn to write their patient’s narratives display more empathic concern for their patients in subsequent clinical work. Following this line of reasoning, it has been shown that writing exercises and the study of literary texts can help caregivers to keep their focus on, as well as to value their patient’s unique experience of illness (Garden 2009 ).
Additionally, Bonvicini et al. ( 2009 ) have reported the results of a randomized controlled study, according to which by taking part in a communication training practice, physicians significantly improved their empathic expression when interacting with a patient. By welcoming and acknowledging their patient’s suffering, health professionals carry out one of the basic tasks, that is welcoming the human experience of suffering and respecting the individual in their entirety.
As we have seen, the definition of empathy and its application in the medical field are widely debated among scholars. In this critical review, we attempted to present some of the different views on the topic of debate. We then shed light on the dehumanization of the medical system (Haque and Waytz 2012 ), and its negative impacts on the quality of healthcare and on the wellbeing of both patients and health practitioners. Further, we illustrated how such a phenomenon is reinforced in and by medical education and training.
After analyzing the discussion on the very essence of empathy and then, on its application within the clinical setting, we have come to the conclusion that such debate leads to an excessively rigid taxonomy, as it divides the cognitive and the emotional dimensions of empathy.
Following this, we attempted to overcome potential downfalls of the rigid taxonomy surrounding the term ‘empathy’, whereby empathy is dichotomously divided into ‘cognitive’ and ‘emotional’ empathy. In this sense, we believe that clinical empathy should be conceived of as ‘empathic concern’; an attitude that configures itself as a genuine interest towards the other, and that results from Halpern’s notion of ‘engaged curiosity’. The latter being understood as a posture that gives value to a genuine interest in welcoming and acknowledging the complexity in the experience of those suffering (Halpern 2011 ).
In our view, empathic concern would avoid some of the misleading discussions that revolve around the very definition of clinical empathy. Further, it would redirect the focus of research towards a more multidimensional conception of empathy in patient care and beyond the taxonomy of empathy. In fact, empathic concern bears both the more cognitive perspective and the emotional engagement and responsiveness dimensions of empathy. This is how a mere commitment to heal can translate into a validation of the patient’s suffering and needs.
Finally, we stressed the potential link between Halpern’s engaged curiosity and the practice of Narrative Medicine, as defined by Rita Charon in Narrative Medicine: Honoring the Stories of Illness (2006). We see the latter as a practical solution to address the lack of empathic concern in the caregiver-patient interaction. To this regard, we call for further research in the field of Narrative Medicine and, particularly, in its role in teaching and promoting engaged curiosity, which we identified as a precondition for empathic concern.
AAMC, P. 1998. Report II: Contemporary Issues in Medicine: Medical Informatics and Population Health. Washington, DC: Association of American Medical Colleges 25.
Alma, Hans A., and Adri Smaling. 2006. The meaning of empathy and imagination in health care and health studies. International Journal of Qualitative Studies on Health and Wellbeing 1 , 195–211. http://www.ijqhw.net/index.php/qhw/article/view/4934 .
Aring, Charles D. 1958. Sympathy and empathy. Journal of the American Medical Association 167 (4): 448–452.
Article Google Scholar
Astell, Ann W. 2004. Saintly mimesis, contagion, and empathy in the thought of Rene Girard, Edith Stein and Simone Weil. Shofar an International Journal of Jewish Studies 22 (2): 116–131. https://doi.org/10.1353/sho.2004.000 .
Avery, J. K. 1985. Lawyers tell what turns some patients litigious. Med Malpractice Rev , 2, pp. 35–37.
Beach, Mary Catherine, and Thomas Inui. 2006. Relationship-centered care. Journal of General Internal Medicine 21 (1): 3–8.
Beckman, Howard B., Kathryn M. Markakis, Anthony L. Suchman, and Richard M. Frankel. 1994. The doctor-patient relationship and malpractice: lessons from plaintiff depositions. Archives of Internal Medicine 154 (12): 1365–1370.
Bellini, Lisa M., and Judy A. Shea. 2005. Mood change and empathy decline persist during three years of internal medicine training. Academic Medicine 80 (2): 164–167.
Bellini, Lisa M., Michael Baime, and Judy A. Shea. 2002. Variation of mood and empathy during internship. JAMA 287 (23): 3143–3146.
Bertakis, Klea D., Debra Roter, and Sean M. Putnam. 1991. The relationship of physician medical interview style to patient satisfaction. Journal of Family Practice 32 (2): 175–181.
Google Scholar
Bikker, Annemieke P., Stewart W. Mercer, and David Reilly . 2005. A pilot prospective study on the consultation and relational empathy, patient enablement, and health changes over 12 months in patients going to the Glasgow Homoeopathic Hospital. Journal of Alternative & Complementary Medicine 11 (4): 591–600.
Bloom, Paul. 2017. Against empathy: The case for rational compassion . Random House.
Blumgart, Herrman L. 1964. Caring for the patient. New England Journal of Medicine 270 (9): 449–456.
Bonvicini, Kathleen A., Michael J. Perlin, Carma L. Bylund, Gregory Carroll, Ruby A. Rouse, and Michael G. Goldstein. 2009. Impact of communication training on physician expression of empathy in patient encounters. Patient Education and Counseling 75 (1): 3–10.
Boulton, Robert. 1987. People skills . Sydney, New South Wales, Australia: Simon & Schuster.
Broyard, Anatole. 1993. Intoxicated by my illness: and other writings on life and death . Fawcett Books.
Charon, Rita. 2001. Narrative medicine: A model for empathy, reflection, profession, and trust. JAMA 286 (15): 1897–1902.
Charon, Rita. 2004. The ethicality of narrative medicine. Narrative Research in Health and Illness . https://doi.org/10.1002/9780470755167 .
Charon, Rita. 2006. Narrative medicine: Honoring the stories of illness . Oxford University Press.
Charon, Rita. 2007. What to do with stories: The sciences of narrative medicine. Canadian Family Physician 53 (8): 1265–1267.
Chen, Daniel CR., Daniel S. Kirshenbaum, Jun Yan, Elaine Kirshenbaum, and Robert H. Aseltine. 2012. Characterizing changes in student empathy throughout medical school. Medical Teacher 34 (4): 305–311.
Coplan, Amy, and Peter Goldie, eds. 2011. Empathy: Philosophical and psychological perspectives . Oxford: Oxford University Press.
Coulehan, John L. 1995. Tenderness and steadiness: Emotions in medical practice. Literature and Medicine 14 (2): 222–236.
Coulehan, Jack. 2005. Today’s professionalism: engaging the mind but not the heart. Academic Medicine 80 (10): 892–898.
Coulehan, Jack, and Peter C. Williams. 2001. Vanquishing virtue: The impact of medical education. Academic Medicine 76 (6): 598–605.
Coulehan, John L., Frederic W. Platt, Barry Egener, Richard Frankel, Chen-Tan. Lin, Beth Lown, and William H. Salazar. 2001. “Let me see if I have this right…”: Words that help build empathy. Annals of Internal Medicine. 135: 221.
Coulehan, Jack. 2009a. Compassionate solidarity: Suffering, poetry, and medicine. Perspectives in Biology and Medicine 52: 585–603.
Coulehan, Jack. 2009b. Rescuing empathy. Literature, Arts, and Medicine Blog , Nov. 30. Retrieved from http://medhum.med.nyu.edu/blog .
Crandall, Sonia J., and Gail S. Marion. 2009. Commentary: Identifying attitudes towards empathy: An essential feature of professionalism. Academic Medicine 84 (9): 1174–1176.
Cuff, Benjamin MP., Sarah J. Brown, Laura Taylor, and Douglas J. Howat. 2016. Empathy: A review of the concept. Emotion Review 8 (2): 144–153.
Decety, Jean. 2010. The neurodevelopment of empathy in humans. Developmental neuroscience , 32 (4), pp. 257–267.
Decety, Jean. 2011. Dissecting the neural mechanisms mediating empathy. Emotion Review 3 (1): 92–108.
Decety, Jean, and Claus Lamm. 2006. Human empathy through the lens of social neuroscience. The Scientific World Journal 6: 1146.
Decety, Jean, and Meghan Meyer. 2008. From emotion resonance to empathic understanding: A social developmental neuroscience account. Development and Psychopathology 20 (4): 1053–1080.
Derksen, Frans, Jozien Bensing, and Antoine Lagro-Janssen. 2013. Effectiveness of empathy in general practice: A systematic review. British Journal of General Practice 63 (606): e76–e84.
DiMatteo, M. Robin., Ron D. Hays, and Louise M. Prince. 1986. Relationship of physicians’ nonverbal communication skill to patient satisfaction, appointment noncompliance, and physician workload. Health Psychology 5 (6): 581.
DiMatteo, M. Robin., Cathy Donald Sherbourne, Ron D. Hays, Lynn Ordway, Richard L. Kravitz, Elizabeth A. McGlynn, Sherrie Kaplan, and William H. Rogers. 1993. Physicians’ characteristics influence patients’ adherence to medical treatment: Results from the Medical Outcomes Study. Health Psychology 12 (2): 93.
Diorio, Caroline, and Ma.łgorzata Nowaczyk. 2019. Half as sad: A plea for narrative medicine in pediatric residency training. Pediatrics 143 (1): e20183109.
Eide, Hilde, Richard Frankel, Anne Christine Bull. Haaversen, Kerstin Anine Vaupel, Peter K. Graugaard, and Arnstein Finset. 2004. Listening for feelings: Identifying and coding empathic and potential empathic opportunities in medical dialogues. Patient Education and Counseling 54 (3): 291–297.
Eisenthal, Sherman, Robert Emery, Aaron Lazare, and Harriet Udin. 1979. “Adherence” and the negotiated approach to patienthood. Archives of General Psychiatry 36 (4): 393–398.
Ekman, Eve, and Michael Krasner. 2017. Empathy in medicine: Neuroscience, education and challenges. Medical Teacher 39 (2): 164–173.
Figley, Charles R. 2002. Treating compassion fatigue . New York: Brunner-Routledge.
Finset, Arnstein. 2010. Conceptual explorations on person-centered medicine 2010: emotions, narratives and empathy in clinical communication. International Journal of Integrated Care . https://doi.org/10.5334/ijic.490 .
Flexner, Abraham. 1912. Medical education in Europe: A report to the Carnegie Foundation for the Advancement of Teaching 6. Carnegie Foundation for the advancement of teaching.
Fox, Fiona E., Karen J. Rodham, Michael F. Harris, Gordon J. Taylor, Jane Sutton, Jenny Scott, and Brian Robinson. 2009. Experiencing “the other side”: A study of empathy and empowerment in general practitioners who have been patients. Qualitative Health Research 19: 1580–1588. https://doi.org/10.1177/1049732309350732 .
Francis, Vida, Barbara M. Korsch, and Marie J. Morris. 1969. Gaps in doctor-patient communication: Patients’ response to medical advice. New England Journal of Medicine 280 (10): 535–540.
Gair, Susan. 2012. Feeling their stories: Contemplating empathy, insider/outsider positionings, and enriching qualitative research. Qualitative Health Research 22 (1): 134–214.
Gallagher, Thomas H., Amy D. Waterman, Alison G. Ebers, Victoria J. Fraser, and Wendy Levinson. 2003. Patients’ and physicians’ attitudes regarding the disclosure of medical errors. JAMA 289 (8): 1001–1007.
Garden, Rebecca. 2009. Expanding clinical empathy: An activist perspective. Journal of General Internal Medicine 24 (1): 122–125.
Geldard, David, and Kathryn Geldard. 2005. Basic personal counselling . Sydney, Australia: Pearson Education.
Gladstein, Gerald A. 1983. Understanding empathy: Integrating counseling, developmental, and social psychology perspectives. Journal of Counseling Psychology 30 (4): 467.
Gleichgerrcht, Ezequiel, and Jean Decety. 2013. Empathy in clinical practice: how individual dispositions, gender, and experience moderate empathic concern, burnout, and emotional distress in physicians. PLoS ONE 8 (4): e61526.
Graugaard, Peter Kjær, Kjersti Holgersen, and Arnstein Finset. 2004. Communicating with alexithymic and non-alexithymic patients: An experimental study of the effect of psychosocial communication and empathy on patient satisfaction. Psychotherapy and Psychosomatics 73 (2): 92–100.
Halpern, Jodi. 2001. From detached concern to empathy: Humanizing medical practice . Oxford: Oxford University Press.
Book Google Scholar
Halpern, Jodi. 2011. 13 Clinical empathy in medical care. In Empathy: From bench to bedside , 229–244. Cambridge: MIT Press.
Halpern, Jodi. 2014. From idealized clinical empathy to empathic communication in medical care. Medicine, Health Care and Philosophy 17 (2): 301–311.
Haque, Omar Sultan, and Adam Waytz. 2012. Dehumanization in Medicine: Causes, solutions and functions. Perspectives on Psychological Science 7 (2): 176–186.
Hardy, Carter. 2017. A Phenomenological approach to clinical empathy: Rethinking empathy within its intersubjective and affective contexts.
Haslam, Nick. 2007. Humanising medical practice: The role of empathy. Medical Journal of Australia 187 (7): 381–382.
Hein, Grit, and Tania Singer. 2008. I feel how you feel but not always: The empathic brain and its modulation. Current Opinion in Neurobiology 18: 153–158. https://doi.org/10.1016/j.conb.2008.07.012 .
Hickson, Gerald B., et al. 1992. Factors that prompted families to file medical malpractice claims following perinatal injuries. JAMA 267 (10): 1359–1363.
Hickson, Gerald B., et al. 1994. Obstetricians’ prior malpractice experience and patients’ satisfaction with care. JAMA 272 (20): 1583–1587.
Hojat, Mohammadreza. 2009. Ten approaches for enhancing empathy in health and human services cultures. Journal of Health and Human Services Administration 31: 412–450.
Hojat, Mohammadreza, Salvatore Mangione, Thomas J. Nasca, Mitchell JM. Cohen, Joseph S. Gonnella, James B. Erdmann, Jon Veloski, and Mike Magee. 2001. The Jefferson scale of physician empathy: Development and PRELIMINARY psychometric data. Educational and Psychological Measurement 61 (2): 349–365.
Hojat, Mohammadreza, Salvatore Mangione, Thomas J. Nasca, Susan Rattner, James B. Erdmann, Joseph S. Gonnella, and Mike Magee. 2004. An empirical study of decline in empathy in medical school. Medical Education 38 (9): 934–941.
Hojat, Mohammadreza, Daniel Z. Louis, Fred W. Markham, Richard Wender, Carol Rabinowitz, and Joseph S. Gonnella. 2011. Physicians’ empathy and clinical outcomes for diabetic patients. Academic Medicine 86 (3): 359–364.
Hojat, Mohammadreza, Daniel Z. Louis, Vittorio Maio, and Joseph S. Gonnella. 2013. Empathy and health care quality. American Journal of Medical Quality . https://doi.org/10.1177/1062860612464731 .
Hooker, Christine I., Lori Bruce, Sara Hope Lincoln, Melissa Fisher, and Sophia Vinogradov. 2011. Theory of mind skills are related to gray matter volume in the ventromedial prefrontal cortex in schizophrenia. Biological psychiatry , 70 (12), pp. 1169–1178.
Hooker, Claire. 2015. Understanding empathy: Why phenomenology and hermeneutics can help medical education and practice. Medicine, Health Care and Philosophy 18 (4): 541–552.
Johna, Samir, and Simi Rahman. 2011. Humanity before science: Narrative medicine, clinical practice, and medical education. The Permanent Journal 15 (4): 92.
Kearney, Michael K., Radhule B. Weininger, Mary LS. Vachon, Richard L. Harrison, and Balfour M. Mount. 2009. Self-care of physicians caring for patients at the end of life: Being connected a key to my survival. JAMA 301 (11): 1155–1164.
Kim, Sung Soo, Stan Kaplowitz, and Mark V. Johnston. 2004. The effects of physician empathy on patient satisfaction and compliance. Evaluation & the Health Professions 27 (3): 237–251.
Langewitz, Wolf, Martin Denz, Anne Keller, Alexander Kiss, Sigmund Rütimann, and Brigitta Wössmer. 2002. Spontaneous talking time at start of consultation in outpatient clinic: Cohort study. BMJ 325 (7366): 682–683.
Larson, Eric B., and Xin Yao. 2005. Clinical empathy as emotional labor in the patient-physician relationship. JAMA 293 (9): 1100–1106.
Levinson, Wendy, et al. 1997. Physician-patient communication: The relationship with malpractice claims among primary care physicians and surgeons. JAMA 277 (7): 553–559.
Lewis, Bradley E. 2011. Narrative medicine and healthcare reform. Journal of Medical Humanities 32 (1): 9–20.
MacPherson, Hugh, Stewart W. Mercer, Tony Scullion, and Kate J. Thomas. 2003. Empathy, enablement, and outcome: An exploratory study on acupuncture patients’ perceptions. The Journal of Alternative & Complementary Medicine 9 (6): 869–876.
Mercer, Stewart W., Maria Higgins, Annemieke M. Bikker, Bridie Fitzpatrick, Alex McConnachie, Suzanne M. Lloyd, Paul Little, and Graham CM. Watt. 2016. General practitioners’ empathy and health outcomes: A prospective observational study of consultations in areas of high and low deprivation. The Annals of Family Medicine 14 (2): 117–124.
Moore, Philip J., Nancy E. Adler, and Patricia A. Robertson. 2000. Medical malpractice: The effect of doctor-patient relations on medical patient perceptions and malpractice intentions. Western Journal of Medicine 173 (4): 244.
Neumann, Melanie, Friedrich Edelhäuser, Diethard Tauschel, Martin R. Fischer, Markus Wirtz, Christiane Woopen, Aviad Haramati, and Christian Scheffer. 2011. Empathy decline and its reasons: A systematic review of studies with medical students and residents. Academic Medicine 86 (8): 996–1009.
Nightingale, Stephen D., Paul R. Yarnold, and Michael S. Greenberg. 1991. Sympathy, empathy, and physician resource utilization. Journal of General Internal Medicine 6 (5): 420–423.
Nussbaum, Martha. 1996. Compassion: The basic social emotion. Social Philosophy and Policy 13 (1): 27–58.
Pedersen, Reidar. 2008. Empathy: A wolf in sheep’s clothing? Medicine, Health Care and Philosophy 11 (3): 325.
Pellegrino, Edmund D. 1981. Being ill and being healed: Some reflections on the grounding of medical morality. Bulletin of the New York Academy of Medicine 57 (1): 70.
Reiss, Helen. 2010. Empathy in medicine—a neurobiological perspective. JAMA 304 (14): 1604–1605.
Rifkin, Jeremy. 2009. The empathic civilization : The race to global consciousness in a world in crisis . Cambridge: Penguin.
Rosenthal, Susan, Brian Howard, Yvette R. Schlussel, B. Dana Herrigel, Gabriel Smolarz, Brian Gable, Jennifer Vasquez, Heather Grigo, and Margit Kaufman. 2011. Humanism at heart: Preserving empathy in third-year medical students. Academic Medicine 86 (3): 350–358.
Roter, Debra L., Moira Stewart, Samuel M. Putnam, Mack Lipkin, William Stiles, and Thomas S. Inui. 1997. Communication patterns of primary care physicians. JAMA 277 (4): 350–356.
Roter, Debra L., Judith A. Hall, Rolande Merisca, Beth Nordstrom, Deborah Cretin, and Bonnie Svarstad. 1998. Effectiveness of interventions to improve patient compliance: a meta-analysis. Medical Care 36: 1138–1161.
Rushton, J. Philippe. 1980. Altruism, socialization, and society . Prentice-Hall.
Scheper-Hughes, Nancy, and Margaret M. Lock. 1987. The mindful body: A prolegomenon to future work in medical anthropology. Medical Anthropology Quarterly 1 (1): 6–41.
Schulte-Rüther, Martin, Hans J. Markowitsch, Gereon R. Fink, and Martina Piefke. 2007. Mirror neuron and theory of mind mechanisms involved in face-to-face interactions: A functional magnetic resonance imaging approach to empathy. Journal of Cognitive Neuroscience 19 (8): 1354–1372.
Shanafelt, Tait D., Katharine A. Bradley, Joyce E. Wipf, and Anthony L. Back. 2002. Burnout and self-reported patient care in an internal medicine residency program. Annals of Internal Medicine 136 (5): 358–367.
Shanafelt, Tait D., Colin West, Xinghua Zhao, Paul Novotny, Joseph Kolars, Thomas Habermann, and Jeff Sloan. 2005. Relationship between increased personal well-being and enhanced empathy among. Journal of General Internal Medicine 20 (7): 559–564.
Shanafelt, Tait D., Charles M. Balch, Gerald J. Bechamps, Thomas Russell, Lotte Dyrbye, Daniel Satele, Paul Collicott, Paul J. Novotny, Jeff Sloan, and Julie A. Freischlag. 2009. Burnout and career satisfaction among American surgeons. Annals of Surgery 250 (3): 463–471.
Shanafelt, Tait D., Sonja Boone, Litjen Tan, Lotte N. Dyrbye, Wayne Sotile, Daniel Satele, Colin P. West, Jeff Sloan, and Michael R. Oreskovich. 2012. Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Archives of Internal Medicine 172 (18): 1377–1385.
Shapiro, Johanna. 2011. 16 The paradox of teaching empathy in medical education. In Empathy: From bench to bedside , ed. Jean Decety, 275–290. Cambridge: MIT Press.
Shapiro, Robyn S., Deborah E. Simpson, Steven L. Lawrence, Anne Marie Talsky, Kathleen A. Sobocinski, and David L. Schiedermayer. 1989. A survey of sued and non sued physicians and suing patients. Archives of Internal Medicine 149 (10): 2190–2196.
Squier, Roger W. 1990. A model of empathic understanding and adherence to treatment regimens in practitioner-patient relationships. Social Science & Medicine 30 (3): 325–339.
Stepien, Kathy A., and Amy Baernstein. 2006. Educating for empathy. Journal of General Internal Medicine 21 (5): 524–530.
Stewart, Moira, et al. 1999. Evidence on patient-doctor communication. Cancer 25 (1999): 30.
Stueber, Karsten. 2006. Rediscovering empathy . Cambridge: Massachusetts Institute of Technology.
Suchman, Anthony L., Debra Roter, Michele Green, Mack Lipkin Jr., and The Collaborative Study Group of the American Academy on Physician and Patient. 1993. Physician satisfaction with primary care office visits. Medical Care 31: 1083–1092.
Suchman, Anthony L., Kathryn Markakis, Howard B. Beckman, and Richard Frankel. 1997. A model of empathic communication in the medical interview. JAMA 277 (8): 678–682.
Timmermans, Stefan, and Rene Almeling. 2009. Objectification, standardization, and commodification in health care: A conceptual readjustment. Social Science & Medicine 69 (1): 21–27.
Trevithick, Pamela. 2005. Social work skills . Berkshire, UK: Open University Press.
Vermeire, Etienne, Hilary Hearnshaw, Paul Van Royen, and Joke Denekens. 2001. Patient adherence to treatment: three decades of research. A comprehensive review. Journal of Clinical Pharmacy and Therapeutics 26 (5): 331–342.
Zachariae, Robert, Christina Gundgaard Pedersen, Anders Bonde Jensen, Eva Ehrnrooth, Philip B. Rossen, and Hans von der Maase. 2003. Association of perceived physician communication style with patient satisfaction, distress, cancer-related self-efficacy, and perceived control over the disease. British Journal of Cancer 88 (5): 658–665.
Zaki, Jamil, Niall Bolger, and Kevin Ochsner. 2008. It takes two: The interpersonal nature of empathic accuracy. Psychological Science 19 (4): 399–404.
Download references
Author information
Authors and affiliations.
University of Groningen, Groningen, The Netherlands
Clarissa Guidi & Chiara Traversa
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Chiara Traversa .
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Guidi, C., Traversa, C. Empathy in patient care: from ‘Clinical Empathy’ to ‘Empathic Concern’. Med Health Care and Philos 24 , 573–585 (2021). https://doi.org/10.1007/s11019-021-10033-4
Download citation
Accepted : 20 June 2021
Published : 01 July 2021
Issue Date : December 2021
DOI : https://doi.org/10.1007/s11019-021-10033-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Patient care
- Empathic concern
- Engaged curiosity
- Narrative medicine
- Find a journal
- Publish with us
- Track your research

Oxford University Press's Academic Insights for the Thinking World

Becoming “properly empathic”: the importance of empathy in healthcare

The Art of Conversation in Cancer Care
- By Richard P. McQuellon
- August 13 th 2022
Nina Ann, a colleague and cancer patient once said to me, “I never was properly empathic until I had peripheral neuropathy (PN).” She had undergone many treatments for breast cancer for nine years. She said it was now difficult to button her shirt and she experienced shooting pains in her hands and feet, hallmark symptoms of PN. This was the first I heard her self-criticism. I knew her to be a very empathic person. She had been active organizing support groups and volunteered to speak to patients who wanted a veteran cancer patient’s point of view. I asked her to tell me what she meant. She had heard patients talk about PN but it was only when she experienced it herself that she really “got it.” I subsequently have had many conversations with patients, colleagues, and oncology health care providers about empathy and the prerequisites for achieving a state of empathic connection with another. The implication of Nina Ann’s observation is that it is necessary to have a problem before we can empathize with it. Is she correct?
What is empathy?
Empathy is the act of understanding another person’s thoughts, feelings, and experience, by imagining oneself into their situation. The empathizer apprehends the other’s experience as if it were their own. It is “ walking a mile in their shoes .” The English word “empathy” emerged over a century ago as the translation for the German psychological term “Einfuhlung,” meaning “feeling into.” Its origin is found in the Greek, “em” in + “pathos” feeling = empatheia.
Empathy differs from sympathy with regard to the emotional component. Simply stated, empathy is feeling with and sympathy is feeling for . Nina Ann criticized herself because she did not feel properly empathic until after experiencing peripheral neuropathy. She concluded she needed to have PN in order to empathize properly. If this conclusion is valid, we have little capacity for going beyond our own experience. However, the essence of empathy is the capacity to imagine ourselves into another’s situation without experiencing it. While it is not necessary to have PN to empathize with it, it may be important to have experience with some unpleasant physical sensation to “get it” about suffering. In fact, sharing a similar experience, e.g., chemotherapy treatment, can mislead a person into thinking “this is how chemotherapy is for everyone,” which is far from accurate. There are many different types of chemotherapy treatment and countless variations on individuals’ responses.
There are three components to empathy and its expression: cognitive—the ability to grasp what the person thinks, to see things from their perspective; affective—the ability to discern another’s feelings; and importantly, the ability to act in such a way as to convey understanding to the other, sometimes referred to as compassionate empathy. It is a complex cognitive and affective process as well as a social behavior, which can be facilitated by direct or indirect experience. Reading literary fiction is an indirect, vicarious experience; it can enhance empathic capacity . Stories inform our capacity to understand other people. However, it is not enough to understand the person’s thinking and feeling, which is largely an internal process; it is necessary to translate that understanding into compassionate action. The behavior of the listener creates the empathic connection, through body language and words well spoken.
Empathy is best thought of as an interpersonal process. In a conversation, being empathic means putting aside our agenda in order to see the others point of view and take account of their emotions. It involves listening with the heart as well as the ears and eyes and communicating that listening/understanding to the person. Empathy expressed effectively results in the other feeling cared for and heard. The empathic healthcare provider may even affect the course of illness .
Are the effects of empathy always positive?
We assume the effects of empathy are positive but there can be a downside . For example, a highly empathic caregiver may feel the suffering of their loved one to the extent that they develop compassion fatigue. In this case, while empathy facilitates caregiving behavior and closeness, it can be at the expense of the self. Professional healthcare providers, during this time of pandemic, have been especially vulnerable to compassion fatigue, a result of the constant experience of empathic connection with suffering patients.
There is also evidence that empathy for our own group is wired in neurologically and can result in unconscious bias . The practical implication of this discovery in neuroscience is that being properly empathic with people who are not in our own group may be more challenging for healthcare providers.
However, t he majority of research on empathy reports positive outcomes . For example, high empathy capacity is associated with more prosocial behaviors and stronger relationships with others. In healthcare, we think of empathy as a skill used to connect with suffering which is largely true. However, being properly empathic can also connect us with people sharing positive experiences and humor, a healing elixir in any setting.
Can empathy be taught and learned?
Empathy is both a skill and a quality of the heart. The skill can be learned and the quality can be nurtured. Some people are natural “empaths” and need little training , just as some people are natural athletes. Clinicians in medical settings have studied the important elements of communication training and identified empathy as key to promoting patient involvement in care . Excellent written and internet/video resources are now available. At Atrium Health Wake Forest Baptist Medical Center, a training program to enhance relationship-centered communication is available to all employees. Finally, teaching empathy was the topic of a study on a medical student lecture and practice session at the 2021 American Psychosocial Oncology Society Virtual Conference (see “ Facilitating Empathy in medical students with art: An exercise in focused attention, T46 ”). Variations on these programs are available at other institutions and websites for professional caregivers. They have one important element in common: recognition of empathy as a key component in helpful communication with patients.
Nurturing the qualities that energize empathy, e.g., deep listening, energy, kindness, compassion etc., may be more challenging. A weary professional caregiver burdened with an overload of very sick patients may find little emotional reserve to be empathic when on the front lines of care. Fortunately, there is the recognition that both institutional and individual factors are important in maintaining healthcare providers who can be both competent and empathic in their work.
The empathy exams
Nina Ann felt she failed her own version of “ The Empathy Exams ,” a phrase used to describe the training some medical schools employ in assessing the effectiveness of Dr-patient relationship skills. I felt her self-rated failure to understand PN was overly critical. Nina Ann was a very empathic person. Her self-reflection was evidence of her sensitivity to others. Developing peripheral neuropathy gave her improved ability to gauge her level of pain relative to others and in so doing, more deeply understanding the other, a form of useful social comparison. It is likely we all have an internal “rating scale” for another’s experience and use it to judge suffering which in turn can activate a certain level of empathic response. Nina Ann established a new threshold for her empathy after her personal encounter with peripheral neuropathy. Her self-observation of deficiency was a testament to her flexibility and openness, both skills useful in developing an empathic connection.
What does it take to be “properly empathic”? An open heart and mind that can imagine the experience of the other and express that connection verbally and nonverbally. Simply stated, becoming properly empathic means listening carefully and responding thoughtfully.
Richard P. McQuellon , PhD, is Professor of Medicine and Director, Psychosocial Oncology, Wake Forest University Baptist Health System, Winston-Salem, North Carolina. He has authored two books with OUP, The Art of Conversation in Cancer Care and The Nell Dialogues.
- Health & Medicine
- Science & Medicine
Our Privacy Policy sets out how Oxford University Press handles your personal information, and your rights to object to your personal information being used for marketing to you or being processed as part of our business activities.
We will only use your personal information to register you for OUPblog articles.
Or subscribe to articles in the subject area by email or RSS
Related posts:

Recent Comments
Harnessing the power of listening and responding with empathy is life changing.
I have read your books and find them inspiring and motivational. The empathy you feel for others overflows on each page.
Thank you, Dr. McQuellon, for sharing your thoughtful research and insights on such a meaningful and universal topic.
Comments are closed.
What is Empathy in Nursing? (With Examples, Importance, & Challenges)

Nursing is a profession known for caring for others. As nurses, we work closely with patients, their families and loved ones, and our professional peers. It is natural to develop bonds and feel emotionally connected to others in our line of work. One important quality nurses develop is the ability to show empathy. If you are new to nursing or wonder what makes it different from other nursing characteristics, you may ask, “What is empathy in nursing?” In this article, I will answer that question and share insight about the importance of empathy in nursing. As you read on, you will learn reasons why it is important to be an empathetic nurse, some most common examples of empathy in nursing, the challenges of demonstrating empathy, and how to overcome them.
What Exactly Is Empathy In Nursing?
Empathy vs. sympathy vs. compassion in nursing: main differences, 7 reasons why empathy is so important in nursing practice, reason #1: empathy in nursing promotes communication and healthy nurse/patient relationships, reason #2: empathy in nursing is associated with better patient outcomes, reason #3: patients report higher satisfaction rates when cared for by empathetic nurses, reason #4: empathy allows you to truly recognize your patient’s needs, reason #5: when nurses demonstrate empathy, it creates a better work environment, reason #6: empathetic nurses are better patient advocates, reason #7: empathetic nurses experience less work-related health issues, what are the most common examples of empathy in nursing, example #1: provide a calm environment, example #2: acknowledge your patient’s feelings, example #3: show genuine interest in what your patient says, example #4: find ways to truly relate with your patient, example #5: make each encounter with your patients personal, example #6: be mindful of your body language, example #7: make eye contact with your patient, example #8: use positive nonverbal cues, example #9: be aware of and challenge your personal prejudices, example #10: keep the focus on your patient, 5 most common challenges nurses face in showing empathy and how to overcome them, challenge #1: being overworked, about the challenge:, how to overcome:, challenge #2: demanding patients, challenge #3: poor work environments, challenge #4: empathy fatigue, challenge #5: poor leadership, bonus 4 key things you can do to improve your ability to practice empathy in nursing, skill #1: show true concern for what your patient says, skill #2: be genuinely kind and considerate, skill #3: remember to treat patients like people, not “cases”, skill #4: learn the value of cultural competence and implement it in your practice, my final thoughts, list of sources used for this article.

Greater Good Science Center • Magazine • In Action • In Education
How to Overcome Barriers to Empathy in Health Care
The field of medicine is facing a dilemma when it comes to empathy. On one hand, research has found that receiving empathy from caregivers—feeling understood and accepted—is critical for patient satisfaction , a key aspect of hospital reimbursement . On the other hand, over 60 percent of health care providers are experiencing burnout across professions, making now a harder time than ever to prioritize additional training.
Attend Our Institute for Health Professionals
When : October 10-12, 2019 Where : Marshall, CA
This two-and-a-half-day intensive institute, led by GGSC director of training Eve Ekman, Ph.D., MSW, will give health professionals concrete, research-informed strategies to enhance their sense of purpose, manage stress in their personal and professional lives, and better support and connect with their patients, clients, and colleagues. Apply today .
Will our health care system be able to embrace empathy as a core value going forward?
I recently spent an evening in front of a live audience in conversation with author, doctor, and empathy researcher Helen Riess to discuss her new book, The Empathy Effect . Riess—who has been a mentor and friend to me over several years—is an assistant professor of medicine and the director of the Empathy and Relational Science Program at Harvard Medical School and founder and chief scientific officer at Empathetics, which offers empathy training across industries. Her research suggests that empathy is a skill that can be taught—not something we just have or we don’t—and further research has found that empathic doctors have patients with greater adherence to medications, improved trust (fewer malpractice suits), and even reduced symptoms.

How can health care providers learn skills to help others with an open heart when they already feel overworked, emotionally depleted, and cynical? In our conversation below, Riess and I address this difficult question, as well as other barriers to empathy, and explore how empathy can promote more meaningful work and greater compassion.
Eve Ekman: I want to start with a simple question: Why did you write this book and why now?
Helen Riess: This topic has been very near and dear to me throughout my psychiatry training, and then it has become more and more critical as I’ve worked in the health care world, where I have seen a dramatic drop in empathy. Through my own clinical practice, I have heard many patients complain bitterly about a lack of empathy. They describe how little contact they actually have with their caregivers and how they’re treated like a number. Medical care has become so focused on getting people in and out of doctor’s offices that they are missing out on the true healing in a relationship that is so vital.
I started this book for the medical profession, but in my empathy training work, I get calls from every industry—from the law, to parenting, to business, and leadership. I’m confident that if everybody were given a choice, they would prefer a more empathic interaction than a less empathic interaction, and yet it’s still such an obstacle. We need training.
EE: I often hear people concerned that if they increase their empathy, they will be overwhelmed: “The world is so painful and stressful; how am I going to manage all of that?” What are your thoughts on the relationship between burnout and empathy?
HR: As you said, some people think that if they open their hearts to too many more people, they’re just going to be flooded with everyone’s burdens, and they’re going to be crushed by the needs and the emotional weight of connecting. Actually, I think that’s absolutely a risk, but I also think that the secret is learning self-regulation skills, such as meditating, learning how to name and identify emotions, how to manage them, and self-care.
Self-care practices are needed to simply “fill the tank.” I think what contributes to burnout is when the tank is empty and we don’t take time to fill it with what truly nourishes and soothes us. We keep trying to be a certain way (like compassionate) when we haven’t filled ourselves up adequately for the task. So I think empathy and self-care are really intricately interdependent.
Empathy can make us burn out if we don’t tend to ourselves, but empathy can also actually enliven and invigorate us. One author in the Journal of the American Medical Association , Michael Kearney, wrote about the concept of “exquisite empathy.” He used that phrase to refer to that magical moment when a person feels thoroughly cared about; it enlivens and quickens the relationship not just for the patient but also for the caregiver.
EE: There is a provocative viral video making the rounds among health care professionals suggesting that burnout is the wrong term and we should call it moral injury—the result of being asked to work in an environment that is toxic and untenable. Beyond not filling our own tanks, are there more systemic causes of burnout, whether it’s in a hospital or a company?
HR: Burnout is an interesting word, because I think it implies to the burned-out person that it’s their fault—that they’re not resilient, not tough, or that they’re weak. Statistics in the last ten years show that up to 60 percent of physicians are showing symptoms of burnout, with equal numbers of nurses. It can’t be that all of a sudden 60 percent of the workforce is unable to cope. Something’s happening within the whole system of health care. The disconnection in these systems is that the people making decisions about how medicine is practiced are not the ones in the frontlines.
Leaders who have never been doctors or nurses view health care as a business. In the last few decades, there’s been this “lean six sigma” approach to health care that has nearly dropped the humanity out of it and brought in the spirit of a Toyota factory, where you try to make the parts as cheaply as possible and get the workers to work as quickly as possible. We have kind of lost the magic of what a health care profession can offer. It really is the system that’s burning people out; it’s not that people have become somehow weak.
I think it’s a real challenge to figure out how health care workers can approach their leadership teams and help them to recognize that the organizations they lead are not going to get the outcomes that they want—which are happy, satisfied, and well-cared-for patients—if the providers working with them are emotionally and physically exhausted and deriving very little pleasure from their work. EE: What other challenges do health care providers face when trying to be empathic?
HR: I developed some training around how we maintain empathy even in the most challenging situations. It’s very easy to have empathy if a patient is nice and grateful. However, one example of a challenge is if patients are not so happy with whatever you prescribe—maybe it’s not working and they’re still having symptoms, and they’re calling you frequently because nothing is quite satisfying—that can become challenging merely because it can make physicians and caregivers feel helpless. And when they feel helpless, they don’t like that feeling. They may decide they don’t really like the patient that much and empathy is challenged.
What we were trying to do is help health caregivers see the vulnerability that the patient is feeling, and not dismiss them because they’re having an emotion, but actually figure out what’s going on so we help them with their specific needs. These skills also help with parenting and other important relationships. I wish I had known some of these empathy skills when I was raising my children. I’ve learned a lot along the way.
EE: One of the emotions that gets in the way of these beautiful reflections is a feeling of fear, like when we want to give money or a meal to a person living on the street who’s clearly in need, but feel fearful to engage because they appear mentally ill. How can we work with fear, when we feel threatened personally but actually want empathy to arise?
HR: Empathy is the antidote to fear. When we live in a state of fear, we close off our heart defensively, whereas empathy opens our hearts. As a society, we are living in a state of massive fear exaggeration right now, and it is really closing a lot of hearts and minds. We are all wired to recognize threats, and we recognize threats much more quickly than we recognize gratitude and opportunity. A large percentage of what we perceive as threatening we’re actually projecting out onto others.
So much of the tone that’s been set in medicine has been about rushing into getting the most out of everybody and acting as if there is such a scarcity in everything, which is a kind of fear. I think one of the biggest myths is to have everyone feel as if there’s just “not enough.” If we just flipped that around and said, “There’s enough for everyone,” I think we could ease up on everything. That abundance has to come from our leaders, but also from within.
I would love to see everyone in a leadership position learn about the value of valuing the people who work with you. To recognize that the more you invest in the people, the more you’re going to get out of your bottom line—and the more you use people and treat them like objects and want them to be a cog in the wheel, the more impoverished your organization is going to be. This applies to health care leaders, business leaders, and deans and presidents of all kinds of institutions of education.
EE: How do we train empathy in a way that leads to showing compassion and actually taking action to relieve suffering?
HR: Opening our perceptions of what’s going on in other people typically leads to empathic concern, but the concern doesn’t always lead to action. That transition to compassion has to come from a more reflective life, where you don’t just pass by a homeless person and think, “Oh, I should help,” but never do. We can reflect on the abundance we live with, about humanity as a brotherhood, and the possibility of joining with other people in the journey to have a more compassionate society. The fact that things aren’t this way can embolden us to do more.
EE: In your book, I was really struck by your sharing of your painful personal experiences and how that made you more open to empathy. If people got in touch with their own struggles, would this help them be more present, open, and caring to others?
HR: We know that when people have struggled, they’re much more able to relate to people who have similar struggles. Let’s work toward the end of our conversation with a quote by Carl Jung, who said that “the sole purpose of life is to kindle the light in the darkness of mere being.” And when you think about empathy, I think of it as a light that we’re able to put forth into the world. That just puts a little light into someone’s experience. It doesn’t have to be a heavy lift; it could be a kind word or a knowing look or a nice smile at somebody. But if we think that the sole purpose of life is to kindle the light in the darkness of mere being, there is a lot of darkness in life. We all can make the life of others lighter.
About the Author

Eve Ekman, Ph.D., MSW , is a GGSC Senior Fellow. An experienced speaker, researcher, and group facilitator, she brings a unique background ideally suited to training individuals and organizations in the science of happiness, resilience, compassion, mindfulness, and emotional awareness.
You May Also Enjoy

Are Empathic Doctors Seen as More Competent?

How to Stay Empathic Without Suffering So Much

Building Empathy in Healthcare

Can Compassion Training Help Physicians Avoid Burnout?

Should We Train Doctors for Empathy?

Sustaining Compassion in Health Care
- Open access
- Published: 04 April 2022
The development of empathy in the healthcare setting: a qualitative approach
- Chou Chuen YU 1 ,
- Laurence TAN 1 , 2 ,
- Mai Khanh LE 1 ,
- Bernard TANG 1 ,
- Sok Ying LIAW 3 ,
- Tanya TIERNEY 4 ,
- Yun Ying HO 5 ,
- Beng Eng Evelyn LIM 6 ,
- Daphne LIM 6 ,
- Reuben NG 7 ,
- Siew Chin CHIA 8 &
- James Alvin LOW 1 , 2
BMC Medical Education volume 22 , Article number: 245 ( 2022 ) Cite this article
18k Accesses
33 Citations
18 Altmetric
Metrics details
Healthcare professionals’ empathetic behaviors have been known to lead to higher satisfaction levels and produce better health outcomes for patients. However, empathy could decrease over time especially during training and clinical practice. This study explored factors that contributed to the development of empathy in the healthcare setting. Findings could be used to improve the effectiveness and sustainability of empathy training.
A qualitative approach, informed by aspects of grounded theory, was utilized to identify factors that enabled the development of empathy from the perspectives of doctors, nurses, allied healthcare workers and students. Twelve sessions of focus group discussions were conducted with 60 participants from two hospitals, a medical school, and a nursing school. Data was analyzed independently by three investigators who later corroborated to refine the codes, subthemes, and themes. Factors which influence the development of empathy were identified and categorized. This formed the basis of the creation of a tentative theory of empathy development for the healthcare setting.
The authors identified various personal (e.g. inherent characteristics, physiological and mental states, professional identity) and external (e.g. work environment, life experience, situational stressors) factors that affected the development of empathy. These could be further categorized into three groups based on the stability of their impact on the individuals’ empathy state, contributed by high, medium, or low stability factors. Findings suggest empathy is more trait-like and stable in nature but is also susceptible to fluctuation depending on the circumstances faced by healthcare professionals. Interventions targeting medium and low stability factors could potentially promote the development of empathy in the clinical setting.
Conclusions
Understanding factors that impact the development of empathy allows us to develop measures that could be implemented during training or at the workplace leading to improve the quality of care and higher clinical work satisfaction.
Peer Review reports
Introduction
Mercer and Reynolds [ 1 ] defined empathy in the medical context as the understanding of patients’ emotions, concerns and situations, communicating that understanding to the patient and acting on that understanding. Empathy improves diagnostic accuracy, patient satisfaction and compliance, and lowers psychological distress and medical complications [ 2 , 3 , 4 , 5 ]. Lack of empathy is correlated with physical, emotional, and work-related issues such as depression, burnout, sleep disturbance, and poor concentration, all of which could negatively impact patient care [ 6 ].
Despite extensive efforts to promote empathy through education, a decline in empathy has been observed among medical students, especially when they have spent more time interacting with patients [ 7 , 8 , 9 , 10 , 11 , 12 ]. This decline persists throughout residency and into their practice. Residents have been found to be less empathic and humanistic, and more cynical over time, while physicians from different specialties are at risk of compassion fatigue [ 7 , 12 , 13 , 14 ]. While a decline in empathy was commonly reported in American medical schools, recent studies observed conflicting empathy trends in medical schools and empathy trends in other parts of the world were inconclusive [ 15 , 16 ]. Consequently, this highlights a need to understand how clinical empathy develops among healthcare students and professionals.
Nezlek et al [ 17 ] believed that empathy should be considered both as a trait (a personal disposition that determines one’s ability to recognize, experience, and react to others’ emotions) and a state (the extent to which one empathizes with others in a specific event at a specific time). The same view was shared by Hojat [ 18 ] who considered empathy as neither a highly stable trait nor an easily fluctuating state, which was a result of a complex interplay of factors such as evolution, genetic dispositions, individual development, education and personal experiences. Hence, targeting these factors is thought to enable modification and development of empathy.
Many factors can affect an individual’s empathy level, such as gender, personality, career choices, common experience with patients, education background, and work environment. Females have been shown to have personality traits that lower stress levels [ 11 , 19 ]. Medical students who prefer specialties with a more human touch [ 10 , 11 ] have higher levels of empathy. Sharing common experiences with patients allowed healthcare professionals to empathize more with patients [ 20 ]. Medical education which focused more on science than humanities, and trainee distress are thought to lower empathy levels [ 7 , 20 , 21 , 22 ]. Work experience and work environment could either positively or negatively influence empathy levels [ 23 ] while stress and burnout have been shown to lower empathy levels [ 5 , 24 ].
Unfortunately, little is known about how these factors influence empathy at the trait and state levels. In social science, childhood experiences have been shown to have a long-lasting impact on individual trait empathy [ 5 , 25 ]. On the other hand, cognitive load impedes empathy experience and reduces empathic responses [ 26 ], which is highly applicable to healthcare professionals as they constantly face massive workloads and responsibilities, thus affecting how they experience and exhibit empathy. While empathy research in healthcare has focused mainly on the experience of healthcare students and research on empathy interventions has focused solely on the success of these interventions, few have evaluated the development of empathy in healthcare workers [ 7 , 8 , 27 , 28 , 29 , 30 , 31 ]. Hence, the aim of this study is to qualitatively understand the underlying construct of empathy both as a trait and state in healthcare professionals and students, and determine what are the factors that may influence the development of empathy in the heatlhcare context.

Research design
The research design was informed by the constructivist approach to grounded theory [ 32 , 33 ] in which the aim was for researchers and participants to co-construct the theory on the development of empathy. A qualitative approach was adopted for this study as it was considered the most appropriate way to uncover and understand the meaning of empathy from the ‘emic’ perspective (i.e. the contexts, lives and meanings of those involved). This approach was also important considering that little is known about the theory of change whereby various factors influence the development of empathy of those experiencing empathy in the clinical setting. In view of practical constraints faced by the study team, approaches in grounded theory were adapted for the purpose of data collection and data analysis. Ethics approval for this study was granted by the National Health Group Domain Specific Review Board (DSRB), reference number 2018/00020.
Data collection
Data was collected from care providers consisting of physicians, nurses, multidisciplinary teams, as well as medical and nursing students. While grounded theory would employ theoretical sampling to focus on and support a constant comparative analysis of data, this study adapted the sampling approach whereby clinicians on the study team made a strategic a priori decision based on their expertise to sample from various groups who would provide the most information-rich source of data. Healthcare professionals from various hospitals, medical students from a medical school and nursing students from a nursing school were invited via email to participate in the study. Participants were informed of the study details and written informed consent was obtained. Data was collected from 60 participants via 12 homogeneous focus group discussions (FGDs). Each FGD lasted approximately two hours. All FGDs were conducted in English and hence translation was not required. The demographic information is presented in Table 1 .
The FGDs were conducted in pairs by a female research officer (MK) with either a male medical doctor (LT), or male research fellow (CC) in rotation. All have practice experience in qualitative research and interviewing. MK and CC also had educational qualifications in psychology. Being a clinician, LT was able to reflexively use his knowledge of clinical practice to facilitate discussions in the clinical context whereas MK and CC approached the interviews from an outsider “naïve” position, thereby reducing the possibility of biasing the responses. For each FGD, one researcher would keep notes of the conversation to aid the interpretation of transcripts. Prior to the start of the FGD, each participant was provided with an information sheet containing details about the study and the research team introduced their roles in the study. Only researchers were present at all data collection settings except at the nursing school where the site investigators (part of the study team) were present to provide logistical support. These procedures in place adhered to common best practices to ensure trustworthiness in qualitative research [ 34 ]. Participants had no contact with the research team prior to study commencement.
The initial guided questions were broad and developed based on existing literature on empathy.
These questions focused on beliefs, thoughts, emotional feelings, behaviors and experiences and served as a guide to encourage participants to share their personal stories about their experiences of empathy especially in the clinical context and emerging themes were explored [ 33 ]. Examples of such questions included:
What are your personal experiences of empathy in the care of patients?
What are some of the things doctors or nurses do when they show empathy?
Do you think empathy levels in someone can be changed? Or is it inborn, meaning it cannot be taught?
Some questions were focused on more, or were included during subsequent interviews, as investigators felt that they were important issues that had surfaced during earlier interviews. This required the investigators to be sensitive and open to the views being shared. Examples of such questions included:
Limited time to see patients is a factor that can influence empathy levels? What are your views on this?
Some people are able to maintain their level of empathy despite personal or work related problems. Why do you think this is the case?
Stressors at work can impact empathy levels. What is your view on this?
Negative case discussions were also encouraged as it allowed for emerging theories to be developed and modified while cases that did not fit led to generating of new knowledge [ 34 ]. Examples of such discussions included asking participants to discuss the negative consequences of having no empathy and possible negative effects that could result from having empathy. To ensure that the groups sampled were adequate, the investigators reviewed their field notes and logic diagram following each FGD to aid the assessment of saturation.
Data analysis
Investigators met after each FGD to compare their memos, identify key themes generated by participants, compare findings with previous FGDs, and revise questions based on new themes that emerged. Upon completion of every two FGDs, the audio recordings were transcribed ad verbatim by one of two investigators and counterchecked against the recordings by LT. The investigators subsequently met regularly over a period of 12 months to compare codes and to form themes. Differences in opinion were mediated till a consensus was reached. This “immediate analysis” approach is an important part inspired by grounded theory [ 35 ] as it allowed the investigators to identify similarities and differences in the data. Additionally, it also informs the manner through which questions were developed and raised in each subsequent round of data collection.
Coding occurred in three stages [ 36 ]. First, open coding was conducted from the onset to generate as many ideas as possible regarding how empathy was described by participants, and whether the components of empathy could be categorized into the four domains postulated by the investigators. Axial coding then determined how the various codes related to each other throughout the dataset (e.g. factors related to childhood, environment, workplace, stress affecting empathy). Finally, selective coding involved the investigators selecting central core categories of ‘between and within person changes’ and ‘development over time’ and relating the codes to these categories. To support this whole process, diagrams of how the factors influenced participants’ empathy were constructed to identify the relationship between factors and categories after each FGD. A coherent theory of ‘empathy development’ was drafted by the 6 th FGD. This theory was further refined throughout the study until data saturation and this was achieved by the 12 th FGD.
Participants on the whole considered empathy as both a trait and state. Although there were innate qualities that determined empathic tendencies and responses, these could also be learned and developed over time. Environmental and personal factors later in life are important determinants and these factors can be categorized according to difference in resistance to change which we termed ‘stability factors’ of which there are three levels: high, medium, and low. High stability factors form the foundation of an individual’s trait empathy (e.g. childhood experience, parental values and religious values). Their impact on one’s empathy, for instance, how one responses and reacts to others’ emotions, is long-lasting and less amenable to change. Low stability factors are those that are highly situation specific (e.g. unexpected stressors faced at work) whereby the impact is to cause momentary fluctuations in empathy levels. Medium stability factors are those that tend to be persistent and enduring in one’s environment (e.g. one’s job scope) and arguably have the potential to influence empathy levels over the long run. These factors often represent the environmental and personal constraints that exist for an extended period of time, and can influence one’s ability to empathize over the long run. The interaction between these factors and how they define empathy are presented in Fig. 1 . All factors which influenced empathy, along with their representative quotes are listed in Table 2 .
High stability factors moulds trait empathy
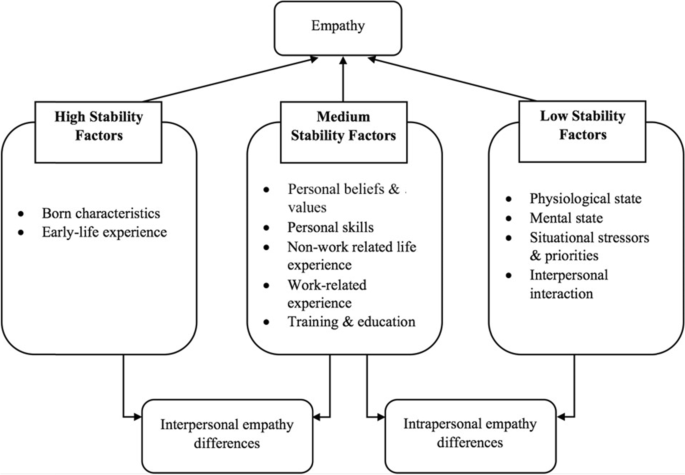
Empathy development model in healthcare setting
High stability factors were often the first thoughts that came to the participants’ mind when asked where they derived their sense of empathy from. Participants believed that individual baseline empathy determined their tendency to empathize with others and was shaped by inborn characteristics and early life experiences. The influence of high stability factors on empathy was persistent and fairly stable. Some participants felt that factors which occurred at the later stages of life, such as empathy training in schools, may not be able to fundamentally change an individual’s trait empathy level and response:
“[…] everybody is born with a certain personality type. And whatever nurture you get beyond that is still working on the baseline that you’re already inborn [born] with, and nurture might not be able to overcome what nature has already given you”. 20-FGD4.
As different individuals have different upbringing and early life experiences, high stability factors also seemed to explain the differences in empathy levels among individuals.
“I think it depends on the person’s upbringing and the environment they grew up in ‘cause [because] throughout my life I’ve seen a lot of people who are able to put themselves in other people’s shoes and some who just aren’t.” 59-FGD12.
Medium stability factors can have enduring effects empathy levels
Medium stability factors can have an important influence on empathy levels, despite less permanent impact than that of high stability factors. These include current belief and value systems, education and training, group influences, work experiences and culture, supervisory influences, and the professional identity that one adopts. In the clinical context, values in medical practice guides how one understands or appreciates another person’s behavior and situation, which in turn influences their empathy level and response. Additionally, factors such as emotion regulation, coping capabilities, perspective-taking, self-reflective ability, as well as verbal and non-verbal communication skills, allowed healthcare professionals to feel, understand, and communicate better in response to patients’ emotions and reactions.
Participants also shared that religious teachings or other forms of educational training could benefit in helping one empathize with others. Tools and frameworks from educational training helped in relating and communicating affectively, for instance, what to say and do in certain scenarios faced by the patients. Interestingly, with more life experiences, healthcare professionals found it easier to relate to the lived experiences of patients. Work experiences could also improve emotional maturity, knowledge acquisition, coping strategies and communication skills:
“… empathy also comes from your experience, as all of them have mentioned earlier, like the kind of experiences you’ve been through which allows you to put yourself in the shoes of these patients which you’ll be seeing, and also having that experience of [for example] like say breaking bad news to this patient multiple times, I would learn how to do it better, and improve myself like maybe the fifth [time] and by- compared to the like one hundredth time I’ve done it, so I think if I had to choose one I think empathy is something that yes, as- there’s a basal level of like inborn like empathy, but it can definitely be developed and honed, so that you are able to like connect with your patients better.” 25-FGD5.
Most participants felt that it was easier to empathize with patients when they had more experience. Participants also shared various examples of how work responsibilities, standards and guidelines, culture, supervisors, surveillance, and reward structure affected empathy levels, as shown in Table 2 . Despite the stress and various challenges that came with the role of providing care, participants highlighted that their professional identities spurred them to maintain empathy even in difficult times, and they did this by contemplating what it meant to be a healthcare professional as well as prioritizing work and responsibilities of patient care.
Although participants felt that the impact of high stability factors was harder to alter, empathy levels could still change over time through interactions with medium stability factors. In some situations, they could override the influence of high stability factors, as mentioned by one participant:
“Parents teach us [to] always be nice to people, do things nicely. But when we step out to the world, we see like the world is not actually friendly. We try to be nice to people but they just shut us out. So it’s a different kind of empathy, and what triggers this empathy in us is experiences. How we see things, how we mature ourselves and for example if we have a situation at hand, how we handle it, how we show our feelings, is different from what our parents would teach us. And depends, either we ourselves would want to follow what our parents have taught, or we want to change and adapt to it.” 47-FGD9.
Similar to high stability factors, there are inter-individual differences in medium stability factors. At the same time, these factors of influence do change over time (e.g. transitioning from medical school to the clinical setting resulted in changes in work responsibilities and expectations). Hence, medium stability factors could account for both interpersonal (between individuals) and intrapersonal (within an individual at different time points) differences in empathy level.
State empathy fluctuates due to low stability factors
While trait empathy is relatively stable, one could still experience transient fluctuations in the experience and expression of empathy due to the presence of low stability factors. These factors often acted as short-term barriers or facilitators that determined how healthcare professionals felt or expressed empathy in a given situation:
“… how much innate empathy you have and then your experiences, and then how that leads to how much empathy you feel, but how much you express depends also a lot on the circumstances of the practice, and how much time you have.” 28-FGD5.
Low stability factors in individuals ranged from physiological states, such as being tired or hungry, to psychological conditions, such as stress and anxiety. Occasionally, situational imperatives and demands such as in the case of a medical emergency, made it challenging to feel or express empathy. Negative interactions and poor rapport between healthcare professionals and patients or family members (e.g. rude demands from family members) that affected mood could also hamper empathic response whereas positive interactions have been reported to have the opposite effect.
With prolonged negative interactions, participants shared that healthcare professionals in certain conditions might become ‘desensitized’ or even experience burnout, leading to avoidance behavior as a coping strategy, with negative consequences on empathy levels. However, high and medium stability factor can have protective effects and buffer against some of the negative interactions. As one participant shared in response to negative experiences faced by healthcare professionals, possessing strong trait empathy and a supportive work environment might protect individuals from the effects of stress or burnout, and help individuals maintain their empathy level:
“It’s tough. I mean if you got it you got it. May [Maybe] you got a very strong empathy, I think you can keep that. […] Maybe situation supports them; maybe the environment supports them to be there.” 38-FGD7.
Understanding empathy in the clinical setting allows trainers and mentors to focus on factors which will positively influence empathy development in clinicians. Our study showed concurring opinions among students and healthcare professionals with regard to empathy development in clinicians. The key findings suggest that the factors affecting empathy development can be categorized into high, medium, and low stability factors, which explains the inter-individual and intra-individual variations in the experiences and expressions of empathy.
In line with past research, high stability factors such as inborn personal characteristics have been shown to influence empathy [ 11 , 37 , 38 ]. This is also the case for other factors identified such as childhood influence from family members and parenting style [ 39 , 40 ]. As highlighted by the participants, social interactions during childhood including school experiences could also determine an individual’s emotional and prosocial tendency development [ 5 , 25 ].
Medium stability factors were also found to be important in the development of empathy. As with prior research, the findings suggest that empathy development could be influenced by whether one’s values prioritizes the welfare of others [ 41 ]. The relationship between religion and empathy was another area of interest among researchers. In line with what other studies have found, while religion seemed to have an influence on prosocial behaviors, the relationship between religion and empathy was affected by how individuals interpreted religious teachings [ 42 , 43 ]. Similarly, culture was also found to have an influence on empathy [ 44 ]. As culture often dictates communication norms, this determines the ability to build trust between patients and healthcare professionals as well as the perception of empathy in healthcare settings [ 45 ].
Factors attributable to the erosion or development of empathy during medical school training and clinical practice which were reported in previous studies were also found in our study. The inability to relate to patients due to lack of life experience or contact with patients, negative encounters with patients, heavy workload, desensitization, burnout, stress, hostile work environment, training, and work culture could lower empathy level. On the other hand, emphasizing the value of empathy during training or in the work culture, interactions with a role model and supervisor, and conducting communication training could improve empathy [ 46 , 47 , 48 , 49 , 50 , 51 , 52 , 53 , 54 , 55 , 56 , 57 ].
Our findings on the effects of low stability factors generally mirrored previous studies where mental state, situational stressors, and interpersonal interactions were found to influence empathy [ 7 , 24 , 48 , 49 ]. Similar to an exploratory study by Pohontsch et al. [ 50 ], we found that negative mood, work stress, lack of time, and negative interactions with patients, inhibited empathy although our study included not only students but also healthcare professionals. Other than one study in the healthcare setting that the authors are aware of, extant evidence is limited regarding the effects of physiological state (e.g. mood, hunger, fatigue) on empathy and findings from this study add to the literature by suggesting they can have detrimental effects. Thomas et al. [ 48 ] showed that well-being correlated positively with empathy whilst poor sleep impacted the capacity of mental health nurses to provide empathic and compassionate care [ 58 ]. Such effects on empathy were also reported in our sample. Supporting the well-being of trainees and clinicians, as well as investing in a healthy work-place culture that includes measures to protect healthcare professionals from verbal abuse, could therefore be important.
Overall, findings from this sample suggest that empathy tended to be more trait-like and stable in nature but is also susceptible to regular fluctuation depending on the circumstances healthcare professionals find themselves in. The stability of their effect has been studied mostly in the field of social and developmental psychology. The work of Knafo and colleagues [ 59 ] demonstrated the influence of genetic and environmental factors on empathy development at an early age. Empathy was found to be a stable disposition determined by genetics but could change due to both genetic and environmental factors. The environmental variables shared by children could explain empathy stability while non-shared environmental variables determined the change in empathy. Taylor et al. [ 60 ] showed that the long-lasting impact of personalities, parental guidance, and experiences on empathy at an early age were able to predict future prosocial behaviors. In addition, Greenberg et al. [ 61 ] showed that people who experienced traumatic events when they were young tended to have higher levels of empathy at adulthood.
Implications for practice
Our tentative theory of empathy development provides a framework to understand potential targets for empathy interventions. While targeting high stability factors may not be possible in an attempt to change trait empathy, developing the manner healthcare professionals/students understand, relate and respond emphatically to patients in medical or nursing schools as well as other clinical settings can be achieved and sustained by targeting both medium and low stability factors. Attempts to improve empathy in medical schools, nursing schools, and clinical practice over the years have largely been focused on social skills and perspective-taking [ 30 , 31 , 62 , 63 ]. A recent longitudinal study of Japanese medical students showed that communication skills education could improve empathy, but the effect was short-lived [ 64 ]. The challenge with focusing on social skills alone was that it often felt forced into a teaching curriculum as individuals were not always able to feel authentic empathy in simulated settings [ 46 ]. Shapiro et al. [ 65 ] was more successful in creating a sustainable positive effect by targeting different factors such as communication skills, coping techniques, well-being enhancing strategies, and exposure to patients; these are some of the factors outlined in our proposed model which adopted a more experiential approach in a real-life setting.
Our theory of empathy development is holistic and highlights that healthcare professionals should be equipped with the necessary skills, experience, and guidance to react empathically in the clinical setting, and that their work environment has to be conducive to minimize the effect of low stability factors. For example, forming healthcare students’ and professionals’ professional identity at an early stage and regularly reinforcing the identity, creating a supportive work culture, training and education, supervisory guidance and peer influence, and even developing a monitoring system that rewards empathic behaviors could help eliminate the effect of low stability factors on empathy.
Strengths and limitations
The strength of this study involves understanding views from a sample of doctors, nurses, multidisciplinary team members, medical students and nursing students and findings is therefore not narrowly confined to only one group, which is quite typical for qualitative research. In addition, this study was conducted in a multi-cultural setting with participants from different ethnic groups, religious beliefs and work setting (acute hospital, community hospital, home care and schools). With findings echoing those found by scholars in the field of empathy, this suggests that the theory of empathy development is applicable in the international community as it provides a framework to understand potential targets for empathy interventions.
One limitation was that as mentioned in the method section, theoretical sampling was not used. This would be expected for any study that adhered strictly to grounded theory. The sampling procedure therefore was guided by strategic a priori decision based on the expertise of the clinicians in the study teams that was in part guided by situational constraints and access especially with regards to the doctors and nurses. As there were more participants coming from ‘high-touch’ clinical setting such as palliative care and geriatrics, future studies may need to consider whether views about empathy from other settings such as the emergency department may differ. As identified in this study, participants felt that empathy levels may be affected in highly demanding clinical situations such as an emergency.
Another limitation of this study is that the use of FGDs may have induced socially desirable responses from participants. For the healthcare professionals, there is a possibility that what was shared may not be truly reflective of their personal views since the sessions were conducted in the presence of fellow colleagues from the same institution. Likewise, the study team also felt that the role of religion was not fully explored in the FGDs as there were instances participants did not feel comfortable or appropriate sharing their personal views on religion in the presence of other fellow medical professionals and associates.
To a large extent, empathy is an inborn trait and fundamental to being human. However, it is dynamic, constantly evolving, and develops under the influence of various personal and situational factors. Our proposed theory of empathy development consolidates the factors influencing empathy and describes their involvement in influencing empathy over time both intra-personally and inter-personally. With a clearer understanding of how empathy develops in the healthcare setting, quality of clinical care in the future may be improved as healthcare providers could implement measures during training or at the workplace, to encourage empathy and compassion in healthcare.
Availability of data and materials
The authors declare that the data supporting the findings of this study are available within the article.
Abbreviations
Focus group discussion
Mercer SW, Reynolds WJ. Empathy and quality of care. Br J Gen Pract. 2002;52(Suppl):S9–12.
Google Scholar
Rakel DP, Hoeft TJ, Barrett BP, Chewning BA, Craig BM, Niu M. Practitioner empathy and the duration of the common cold. Fam Med. 2009;41(7):494–501.
Derksen F, Bensing J, Lagro-Janssen A. Effectiveness of empathy in general practice: a systematic review. Br J Gen Prac. 2013;63(606):76–84. https://doi.org/10.3399/bjgp13X660814 .
Article Google Scholar
Larson EB, Yao X. Clinical empathy as emotional labor in the patient-physician relationship. JAMA. 2005;293(9):1100–6. https://doi.org/10.1001/jama.293.9.1100 .
Neumann M, Bensing J, Mercer S, Ernstmann N, Ommen O, Pfaff H. Analyzing the “nature” and “specific effectiveness” of clinical empathy: a theoretical overview and contribution towards a theory-based research agenda. Patient Educ Couns. 2009;74(3):339–46. https://doi.org/10.1016/j.pec.2008.11.013 .
Sorenson C, Bolick B, Wright K, Hamilton R. Understanding compassion fatigue in healthcare providers: a review of current literature. J Nurs Scholarsh. 2016;48(5):456–65. https://doi.org/10.1111/jnu.12229 .
Neumann M, Edelhäuser F, Tauschel D, et al. Empathy decline and its reasons: a systematic review of studies with medical students and residents. Acad Med. 2011;86(8):996–1009. https://doi.org/10.1097/ACM.0b013e318221e615 .
Pedersen R. Empathy development in medical education–a critical review. Med Teach. 2010;32(7):593–600. https://doi.org/10.3109/01421590903544702 .
Stratton TD, Saunders JA, Elam CL. Changes in medical students’ emotional intelligence: an exploratory study. Teach Learn Med. 2008;20(3):279–84. https://doi.org/10.1080/10401330802199625 .
Hojat M, Vergare MJ, Maxwell K, et al. The devil is in the third year: a longitudinal study of erosion of empathy in medical school. Acad Med. 2009;84(9):1182–91. https://doi.org/10.1097/ACM.0b013e3181b17e55 .
Chen D, Lew R, Hershman W, Orlander J. A cross-sectional measurement of medical student empathy. J Gen Intern Med. 2007;22(10):1434–8. https://doi.org/10.1007/s11606-007-0298-x .
Gribben JL, Kase SM, Waldman ED, Weintraub AS. A cross-sectional analysis of compassion fatigue, burnout, and compassion satisfaction in pediatric critical care physicians in the United States. Pediatr Crit Care Med. 2019;20(3):213–22. https://doi.org/10.1097/PCC.0000000000001803 .
Collier VU, McCue JD, Markus A, Smith L. Stress in medical residency: status quo after a decade of reform? Ann Intern Med. 2002;136(5):384–90. https://doi.org/10.7326/0003-4819-136-5-200203050-00011 .
Hunt P, Denieffe S, Gooney M. Running on empathy: Relationship of empathy to compassion satisfaction and compassion fatigue in cancer healthcare professionals. Eur J Cancer Care (Engl). 2019;28(5): e13124. https://doi.org/10.1111/ecc.13124 .
Andersen FA, Johansen AB, Søndergaard J, Andersen CM, Assing HE. Revisiting the trajectory of medical students’ empathy, and impact of gender, specialty preferences and nationality: a systematic review. BMC Med Educ. 2020;20(1):52. https://doi.org/10.1186/s12909-020-1964-5 .
Ferreira-Valente A, Monteiro JS, Barbosa RM, Salgueira A, Costa P, Costa MJ. Clarifying changes in student empathy throughout medical school: a scoping review. Adv Health Sci Educ Theory Pract. 2017;22(5):1293–313. https://doi.org/10.1007/s10459-016-9704-7 .
Nezlek JB, Schütz A, Lopes P, Smith CV. Naturally occurring variability in state empathy. Empathy in Mental Illness. 2007;187–200. https://doi.org/10.1017/cbo9780511543753.012
Hojat M. Empathy in Patient Care: Antecedents, Development, Measurement, and Outcomes. New York, NY: Springer; 2007.
McManus IC, Keeling A, Paice E. Stress, burnout and doctors’ attitudes to work are determined by personality and learning style: a twelve-year longitudinal study of UK medical graduates. BMC Med. 2004;2:29. https://doi.org/10.1186/1741-7015-2-29 .
Ekman E, Krasner M. Empathy in medicine: Neuroscience, education and challenges. Med Teach. 2017;39(2):164–73. https://doi.org/10.1080/0142159X.2016.1248925 .
Jeffrey D. A meta-ethnography of interview-based qualitative research studies on medical students’ views and experiences of empathy. Med Teach. 2016;38(12):1214–20. https://doi.org/10.1080/0142159X.2016.1210110 .
Eikeland HL, Ørnes K, Finset A, Pedersen R. The physician’s role and empathy - a qualitative study of third year medical students. BMC Med Educ. 2014;14:165. https://doi.org/10.1186/1472-6920-14-165 .
Gleichgerrcht E, Decety J. The relationship between different facets of empathy, pain perception and compassion fatigue among physicians. Front Behav Neurosci. 2014;8:243. https://doi.org/10.3389/fnbeh.2014.00243 .
Wilkinson H, Whittington R, Perry L, Eames C. Examining the relationship between burnout and empathy in healthcare professionals: A systematic review. Burn Res. 2017;6:18–29. https://doi.org/10.1016/j.burn.2017.06.003 .
Volling BL, Kolak AM, Kennedy DE. Empathy and Compassionate Love in Early Childhood: Development and Family Influence. The science of compassionate love: Theory, research, and applications. 2008; 161–200 https://doi.org/10.1002/9781444303070.ch6
Meiring L, Subramoney S, Thomas KG, Decety J, Fourie MM. Empathy and helping: effects of racial group membership and cognitive load. South African Journal of Psychology. 2014;44(4):426–38. https://doi.org/10.1177/0081246314530280 .
Pedersen R. Empirical research on empathy in medicine—a critical review. Patient Educ Couns. 2009;76(3):307–22.
Sulzer SH, Feinstein NW, Wendland CL. Assessing empathy development in medical education: a systematic review. Med Educ. 2016;50(3):300–10.
Yu J, Kirk M. Measurement of empathy in nursing research: systematic review. J Adv Nurs. 2008;64(5):440–54.
Kelm Z, Womer J, Walter JK, Feudtner C. Interventions to cultivate physician empathy: a systematic review. BMC Med Educ. 2014;14:219. https://doi.org/10.1186/1472-6920-14-219 .
Batt-Rawden SA, Chisolm MS, Anton B, Flickinger TE. Teaching empathy to medical students: an updated, systematic review. Acad Med. 2013;88(8):1171–7. https://doi.org/10.1097/ACM.0b013e318299f3e3 .
Charmaz K. Premises, principles, and practices in qualitative research: Revisiting the foundations. Qual Health Res. 2004;14(7):976–93.
Charmaz K. Constructing grounded theory: A practical guide through qualitative analysis. Sage Publicatoins; 2006 Jan 13.
Lincoln YS, Guba EG. Naturalistic inquiry. Sage Publications; 1985.
Engward H. Understanding grounded theory. Nursing Standard (through 2013). 2013 Oct 16;28(7):37.
Strauss A, Corbin J. Basics of qualitative research. Sage Publications; 1990.
Austin EJ, Evans P, Magnus B, O’Hanlon K. A preliminary study of empathy, emotional intelligence and examination performance in MBChB students. Med Educ. 2007;41(7):684–9. https://doi.org/10.1111/j.1365-2923.2007.02795.x .
Newton BW, Barber L, Clardy J, Cleveland E, O’Sullivan P. Is there hardening of the heart during medical school? Acad Med. 2008;83(3):244–9. https://doi.org/10.1097/ACM.0b013e3181637837 .
Strayer J, Roberts W. Children’s empathy and role taking: Child and parental factors, and relations to prosocial behavior. J Appl Dev Psychol. 1989;10(2):227–39. https://doi.org/10.1016/0193-3973(89)90006-3 .
Yoo H, Feng X, Day RD. Adolescents’ empathy and prosocial behavior in the family context: a longitudinal study. J Youth Adolesc. 2013;42(12):1858–72. https://doi.org/10.1007/s10964-012-9900-6 .
Balliet D, Joireman J, Daniels D, George-Falvy J. Empathy and the Schwartz value system: a test of an integrated hypothesis. Individ Differ Res. 2008;6(4):269–79.
Saroglou V, Pichon I, Trompette L, Verschueren M, Dernelle R. Prosocial behavior and religion: new evidence based on projective measures and peer ratings. J Sci Study Relig. 2005;44(3):323–48. https://doi.org/10.1111/j.1468-5906.2005.00289.x .
Duriez B. Are religious people nicer people? Taking a closer look at the religion–empathy relationship. Ment Health Relig Cult. 2004;7(3):249–54.
Chung W, Chan S, Cassels TG. The role of culture in affective empathy: cultural and bicultural differences. J Cogn Cult. 2010;10(3–4):309–26.
Lorié Á, Reinero DA, Phillips M, Zhang L, Riess H. Culture and nonverbal expressions of empathy in clinical settings: A systematic review. Patient Educ Couns. 2017;100(3):411–24. https://doi.org/10.1016/j.pec.2016.09.018 .
Laughey WF, Brown MEL, Finn GM. 'I'm sorry to hear that'-Empathy and Empathic Dissonance: the Perspectives of PA Students. Med Sci Educ. 2020; 1–10. doi: https://doi.org/10.1007/s40670-020-00979-0
West CP, Shanafelt TD. The influence of personal and environmental factors on professionalism in medical education. BMC Med Educ. 2007;7:29. https://doi.org/10.1186/1472-6920-7-29 .
Thomas MR, Dyrbye LN, Huntington JL, et al. How do distress and well-being relate to medical student empathy? a multicenter study. J Gen Intern Med. 2007;22(2):177–83. https://doi.org/10.1007/s11606-006-0039-6 .
Bayne H, Neukrug E, Hays D, Britton B. A comprehensive model for optimizing empathy in person-centered care. Patient Educ Couns. 2013;93(2):209–15. https://doi.org/10.1016/j.pec.2013.05.016 .
Pohontsch NJ, Stark A, Ehrhardt M, Kötter T, Scherer M. Influences on students’ empathy in medical education: an exploratory interview study with medical students in their third and last year. BMC Med Educ. 2018;18(1):1–9.
Winseman J, Malik A, Morison J, Balkoski V. Students’ views on factors affecting empathy in medical education. Acad Psychiatry. 2009;33(6):484–91. https://doi.org/10.1176/appi.ap.33.6.484 .
Bandini J, Mitchell C, Epstein-Peterson ZD, et al. Student and faculty reflections of the hidden curriculum. Am J Hosp Palliat Care. 2017;34(1):57–63. https://doi.org/10.1177/1049909115616359 .
Meadors P, Lamson A. Compassion fatigue and secondary traumatization: provider self care on intensive care units for children. J Pediatr Health Care. 2008;22(1):24–34. https://doi.org/10.1016/j.pedhc.2007.01.006 .
Smith-MacDonald L, Venturato L, Hunter P, et al. Perspectives and experiences of compassion in long-term care facilities within Canada: a qualitative study of patients, family members and health care providers. BMC Geriatr. 2019;19(1):128. https://doi.org/10.1186/s12877-019-1135-x .
Dev V, Fernando AT 3rd, Kirby JN, Consedine NS. Variation in the barriers to compassion across healthcare training and disciplines: A cross-sectional study of doctors, nurses, and medical students. Int J Nurs Stud. 2019;90:1–10. https://doi.org/10.1016/j.ijnurstu.2018.09.015 .
Epstein RM, Hadee T, Carroll J, Meldrum SC, Lardner J, Shields CG. “Could this be something serious?” reassurance, uncertainty, and empathy in response to patients’ expressions of worry. J Gen Intern Med. 2007;22(12):1731–9. https://doi.org/10.1007/s11606-007-0416-9 .
Vogel D, Meyer M, Harendza S. Verbal and non-verbal communication skills including empathy during history taking of undergraduate medical students. BMC Med Educ. 2018;18(1):157.
Gerace A, Rigney G. Considering the relationship between sleep and empathy and compassion in mental health nurses: It’s time. Int J Ment Health Nurs. 2020;29(5):1002–10. https://doi.org/10.1111/inm.12734 .
Knafo A, Zahn-Waxler C, Van Hulle C, Robinson JL, Rhee SH. The developmental origins of a disposition toward empathy: genetic and environmental contributions. Emotion. 2008;8(6):737–52. https://doi.org/10.1037/a0014179 .
Taylor ZE, Eisenberg N, Spinrad TL, Eggum ND, Sulik MJ. The relations of ego-resiliency and emotion socialization to the development of empathy and prosocial behavior across early childhood. Emotion. 2013;13(5):822–31. https://doi.org/10.1037/a0032894 .
Greenberg DM, Baron-Cohen S, Rosenberg N, Fonagy P, Rentfrow PJ. Elevated empathy in adults following childhood trauma. PLoS ONE. 2018;13(10): e0203886. https://doi.org/10.1371/journal.pone.0203886 .
Levett-Jones T, Cant R, Lapkin S. A systematic review of the effectiveness of empathy education for undergraduate nursing students. Nurse Educ Today. 2019;75:80–94. https://doi.org/10.1016/j.nedt.2019.01.006 .
Bas-Sarmiento P, Fernández-Gutiérrez M, Baena-Baños M, Correro-Bermejo A, Soler-Martins PS, de la Torre-Moyano S. Empathy training in health sciences: A systematic review. Nurse Educ Pract. 2020;44: 102739. https://doi.org/10.1016/j.nepr.2020.102739 .
Kataoka H, Iwase T, Ogawa H, et al. Can communication skills training improve empathy? A six-year longitudinal study of medical students in Japan. Med Teach. 2019;41(2):195–200. https://doi.org/10.1080/0142159X.2018.1460657 .
Shapiro J, Youm J, Kheriaty A, Pham T, Chen Y, Clayma R. The human kindness curriculum: An innovative preclinical initiative to highlight kindness and empathy in medicine. Educ Health (Abingdon). 2019;32(2):53–61. https://doi.org/10.4103/efh.EfH_133_18 .
Download references
Acknowledgements
The authors would like to thank Khoo Teck Puat Hospital, Tan Tock Seng Hospital, Yong Loo Lin School of Medicine (National University of Singapore), Lee Kong Chian School of Medicine (Nanyang Technological University), and Nanyang Polytechnic for their assistance in recruitment. Additionally, the authors wish to thank Ms. Isabelle Lim, Geriatric Education and Research Institute, for contributions to research administration support.
This study was funded by Geriatric Education and Research Institute’s Intramural Fund (reference number: GERI/1616).
Author information
Authors and affiliations.
Geriatric Education and Research Institute Ltd, Singapore, Singapore
Chou Chuen YU, Laurence TAN, Mai Khanh LE, Bernard TANG & James Alvin LOW
Department of Geriatric Medicine, Khoo Teck Puat Hospital, Singapore, Singapore
Laurence TAN & James Alvin LOW
Alice Lee Centre for Nursing Studies, Yong Loo Lin School of Medicine, National University of Singapore, Singapore, Singapore
Sok Ying LIAW
Lee Kong Chian School of Medicine, Nanyang Technological University, Singapore, Singapore
Tanya TIERNEY
Ministry of Health Holdings, Singapore, Singapore
Yun Ying HO
School of Health & Social Sciences, Nanyang Polytechnic, Singapore, Singapore
Beng Eng Evelyn LIM & Daphne LIM
Lee Kuan Yew School of Public Policy, National University of Singapore, Singapore, Singapore
Tan Tock Seng Hospital, Singapore, Singapore
Siew Chin CHIA
You can also search for this author in PubMed Google Scholar
Contributions
LT is the principal investigator of the study who made significant contribution to study design, investigation, analysis and reviewing of this manuscript. MKL made significant contribution to study design, investigation, analysis, study administration and writing this manuscript. CCY made significant contribution to study design, investigation, analysis, and reviewing this manuscript. BT made major contribution to reviewing this manuscript. SYL, EL, DL, and YYH made major contribution to study investigation. TT, SCC, and JL made major contribution to study design and investigation. RN made major contribution to study design. All authors have read and approved the manuscript.
Corresponding author
Correspondence to Bernard TANG .
Ethics declarations
Ethics approval and consent to participate.
Ethics approval for this study was granted by the National Health Group Domain Specific Review Board (DSRB), reference number 2018/00020. Written informed consent was obtained from all participants. All methods were carried out in accordance with relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
YU, C.C., TAN, L., LE, M.K. et al. The development of empathy in the healthcare setting: a qualitative approach. BMC Med Educ 22 , 245 (2022). https://doi.org/10.1186/s12909-022-03312-y
Download citation
Received : 25 October 2021
Accepted : 24 March 2022
Published : 04 April 2022
DOI : https://doi.org/10.1186/s12909-022-03312-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Empathy development
- Empathy assessment
- Empathy definition
- Medical education
BMC Medical Education
ISSN: 1472-6920
- General enquiries: [email protected]

Cultivating empathy
Psychologists’ research offers insight into why it’s so important to practice the “right” kind of empathy, and how to grow these skills
Vol. 52 No. 8 Print version: page 44
- Personality

In a society marked by increasing division, we could all be a bit more kind, cooperative, and tolerant toward others. Beneficial as those traits are, psychological research suggests empathy may be the umbrella trait required to develop all these virtues. As empathy researcher and Stanford University psychologist Jamil Zaki, PhD, describes it, empathy is the “psychological ‘superglue’ that connects people and undergirds co-operation and kindness” ( The Economist , June 7, 2019). And even if empathy doesn’t come naturally, research suggests people can cultivate it—and hopefully improve society as a result.
“In general, empathy is a powerful predictor of things we consider to be positive behaviors that benefit society, individuals, and relationships,” said Karina Schumann , PhD, a professor of social psychology at the University of Pittsburgh. “Scholars have shown across domains that empathy motivates many types of prosocial behaviors, such as forgiveness, volunteering, and helping, and that it’s negatively associated with things like aggression and bullying.”
For example, research by C. Daniel Batson , PhD, a professor emeritus of social psychology at the University of Kansas, suggests empathy can motivate people to help someone else in need ( Altruism in Humans , Oxford University Press, 2011), and a 2019 study suggests empathy levels predict charitable donation behavior (Smith, K. E., et al., The Journal of Positive Psychology , Vol. 15, No. 6, 2020).
Ann Rumble , PhD, a psychology lecturer at Northern Arizona University, found empathy can override noncooperation, causing people to be more generous and forgiving and less retaliative ( European Journal of Social Psychology , Vol. 40, No. 5, 2010). “Empathic people ask themselves, ‘Maybe I need to find out more before I jump to a harsh judgment,’” she said.
Empathy can also promote better relationships with strangers. For example, Batson’s past research highlights that empathy can help people adopt more positive attitudes and helping behavior toward stigmatized groups, particularly disabled and homeless individuals and those with AIDS ( Journal of Personality and Social Psychology , Vol. 72, No. 1, 1997).
Empathy may also be a crucial ingredient in mitigating bias and systemic racism. Jason Okonofua , PhD, an assistant professor of psychology at the University of California, Berkeley, has found that teachers are more likely to employ severe discipline with Black students—and that they’re more likely to label Black students as “troublemakers” ( Psychological Science , Vol. 26, No. 5, 2015).
These labels, Okonofua said, can shape how teachers interpret behavior, forging a path toward students’ school failure and incarceration. When Okonofua and his colleagues created an intervention to help teachers build positive relationships with students and value their perspectives, their increased empathy reduced punitive discipline ( PNAS , Vol. 113, No. 19, 2016).
Similarly, Okonofua and colleagues found empathy from parole officers can prevent adults on probation from reoffending ( PNAS , Vol. 118, No. 14, 2021).
In spite of its potential benefits, empathy itself isn’t an automatic path toward social good. To develop empathy that actually helps people requires strategy. “If you’re trying to develop empathy in yourself or in others, you have to make sure you’re developing the right kind,” said Sara Konrath , PhD, an associate professor of social psychology at Indiana University who studies empathy and altruism.
The right kind of empathy
Empathy is often crucial for psychologists working with patients in practice, especially when patients are seeking validation of their feelings. However, empathy can be a draining skill if not practiced correctly. Overidentifying with someone else’s emotions can be stressful, leading to a cardiovascular stress response similar to what you’d experience in the same painful or threatening situation, said Michael J. Poulin , PhD, an associate professor of psychology at the University at Buffalo who studies how people respond to others’ adversity.
Outside of clinical practice, some scholars argue empathy is unhelpful and even damaging. For example, Paul Bloom, PhD , a professor of psychology at Yale University, argues that because empathy directs helping behavior toward specific individuals—most often, those in one’s own group—it may prevent more beneficial help to others ( Against Empathy: The Case for Rational Compassion , Ecco , 2016).
In some cases, empathy may also promote antagonism and aggression (Buffone, A. E. K., & Poulin, M. J., Personality and Social Psychology Bulletin , Vol. 40, No. 11, 2014). For example, Daryl Cameron , PhD, an associate professor of psychology and senior research associate in the Rock Ethics Institute and director of the Empathy and Moral Psychology Lab at Penn State University, has found that apparent biases in empathy like parochialism and the numbness to mass suffering may sometimes be due to motivated choices. He also notes that empathy can still have risks in some cases. “There are times when what looks like empathy promotes favoritism at the expense of the outgroup,” said Cameron.
Many of these negative outcomes are associated with a type of empathy called self-oriented perspective taking—imagining yourself in someone else’s shoes. “How you take the perspective can make a difference,” said John Dovidio , PhD, the Carl I. Hovland Professor Emeritus of Psychology and a professor emeritus in the Institute for Social and Policy Studies and of Epidemiology at Yale University. “When you ask me to imagine myself in another person’s position,” Dovidio said, “I may experience a lot of personal distress, which can interfere with prosocial behaviors.” Taking on that emotional burden, Schumann added, could also increase your own risk for distressing emotions, such as anxiety.
According to Konrath, the form of empathy shown most beneficial for both the giver and the receiver is an other-oriented response. “It’s a cognitive style of perspective taking where someone imagines another person’s perspective, reads their emotions, and can understand them in general,” she said.
Other-oriented perspective taking may result in empathic concern, also known as compassion, which could be seen as an emotional response to a cognitive process. It’s that emotion that may trigger helping behavior. “If I simply understand you’re in trouble, I may not act, but emotion energizes me,” said Dovidio.
While many practitioners may find empathy to come naturally, psychologists’ research can help clinicians guide patients toward other-oriented empathy and can also help practitioners struggling with compassion fatigue to re-up their empathy. According to Poulin, people are more likely to opt out of empathy if it feels cognitively or emotionally taxing, which could impact psychologists’ ability to effectively support their patients.
To avoid compassion fatigue with patients—and maintain the empathy required for helping them—Poulin said it’s important to reflect on the patient’s feeling or experience without necessarily trying to feel it yourself. “It’s about putting yourself in the right role,” he said. “Your goal isn’t to be the sufferer, but to be the caregiver.”
Be willing to grow
Cameron’s research found that the cognitive costs of empathy could cause people to avoid it but that it may be possible to increase empathy by teaching people to do it effectively ( Journal of Experimental Psychology: General , Vol. 148, No. 6, 2019).
Further, research by Schumann and Zaki shows that the desire to grow in empathy can be a driver in cultivating it. They found people can extend empathic effort—asking questions and listening longer to responses—in situations where they feel different than someone, primarily if they believe empathy could be developed with effort ( Journal of Personality and Social Psychology , Vol. 107, No. 3, 2014).
Similarly, Erika Weisz , PhD, a postdoctoral fellow in psychology at Harvard University, said that the first step to increasing your empathy is to adopt a growth mindset—to believe you’re capable of growing in empathy.
“People who believe that empathy can grow try harder to empathize when it doesn’t come naturally to them, for instance, by empathizing with people who are unfamiliar to them or different than they are, compared to people who believe empathy is a stable trait,” she said.
For example, Weisz found addressing college students’ empathy mindsets increases the accuracy with which they perceive others’ emotions; it also tracks with the number of friends college freshmen make during their first year on campus ( Emotion , online first publication, 2020).
Expose yourself to differences
To imagine another’s perspective, the more context, the better. Shereen Naser , PhD, a professor of psychology at Cleveland State University, said consuming diverse media—for example, a White person reading books or watching movies with a non-White protagonist—and even directly participating in someone else’s culture can provide a backdrop against which to adopt someone else’s perspective.
When you’re in these situations, be fully present. “Paying attention to other people allows you to be moved by their experiences,” said Sara Hodges , PhD, a professor of psychology at the University of Oregon. “Whether you are actively perspective-taking or not, if you just pay more attention to other people, you’re likely to feel more concerned for them and become more involved in their experiences.”
For example, in a course focused on diversity, Naser encourages her graduate students to visit a community they’ve never spent time in. “One student came back saying they felt like an outsider when they attended a Hindu celebration and that they realized that’s what marginalized people feel like every day,” she said. Along with decreasing your bias, such realizations could also spark a deeper understanding of another’s culture—and why they might think or feel the way they do.
Read fiction
Raymond Mar , PhD, a professor of psychology at York University in Toronto, studies how reading fiction and other kinds of character-driven stories can help people better understand others and the world. “To understand stories, we have to understand characters, their motivations, interactions, reactions, and goals,” he said. “It’s possible that while understanding stories, we can improve our ability to understand real people in the real world at the same time.”
When you engage with a story, you’re also engaging the same cognitive abilities you’d use during social cognition ( Current Directions in Psychological Science , Vol. 27, No. 4, 2018). You can get the same effect with any medium—live theater, a show on Netflix, or a novel—as long as it has core elements of a narrative, story, and characters.
The more one practices empathy (e.g., by relating to fictional characters), the more perspectives one can absorb while not feeling that one’s own is threatened. “The foundation of empathy has to be a willingness to listen to other peoples’ experiences and to believe they’re valid,” Mar said. “You don’t have to deny your own experience to accept someone else’s.”
Harness the power of oxytocin
The social hormone oxytocin also plays a role in facilitating empathy. Bianca Jones Marlin , PhD, a neuroscientist and assistant professor of psychology at Columbia University, found that mice that had given birth are more likely to pick up crying pups than virgin animals and that the oxytocin released during the birth and parenting process actually changes the hearing centers of the brain to motivate prosocial and survival behaviors ( Nature , Vol. 520, No. 7548, 2015).
Oxytocin can also breed helping responses in those who don’t have a blood relationship; when Marlin added oxytocin to virgin mice’s hearing centers, they took care of pups that weren’t theirs. “It’s as if biology has prepared us to take care of those who can’t take care of themselves,” she said. “But that’s just a baseline; it’s up to us as a society to build this in our relationships.”
Through oxytocin-releasing behaviors like eye contact and soft physical touch, Marlin said humans can harness the power of oxytocin to promote empathy and helping behaviors in certain contexts. Oxytocin is also known to mediate ingroup and outgroup feelings.
The key, Marlin said, is for both parties to feel connected and unthreatened. To overcome that hurdle, she suggests a calm but direct approach: Try saying, “I don’t agree with your views, but I want to learn more about what led you to that perspective.”
Identify common ground
Feeling a sense of social connection is an important part of triggering prosocial behaviors. “You perceive the person as a member of your own group, or because the situation is so compelling that your common humanity is aroused,” Dovidio said. “When you experience this empathy, it motivates you to help the other person, even at a personal cost to you.”
One way to boost this motivation is to manipulate who you see as your ingroup. Jay Van Bavel , PhD, an associate professor of psychology and neural science at New York University, found that in the absence of an existing social connection, finding a shared identity can promote empathy ( Journal of Experimental Social Psychology , Vol. 55, 2014). “We find over and over again when people have a common identity, even if it’s created in the moment, they are more motivated to get inside the mind of another person,” Van Bavel said.
For example, Van Bavel has conducted fMRI research that suggests being placed on the same team for a work activity can increase cooperation and trigger positive feelings for individuals once perceived as outgroup, even among different races ( Psychological Science , Vol. 19, No. 11, 2008).
To motivate empathy in your own interactions, find similarities instead of focusing on differences. For instance, maybe you and a neighbor have polar opposite political ideologies, but your kids are the same age and go to the same school. Build on that similarity to create more empathy. “We contain multiple identities, and part of being socially intelligent is finding the identity you share,” Van Bavel said.
Ask questions
Existing research often measures a person’s empathy by accuracy—how well people can label someone’s face as angry, sad, or happy, for example. Alexandra Main , PhD, an assistant professor of psychology at the University of California, Merced, said curiosity and interest can also be an important component of empathy. “Mind reading isn’t always the way empathy works in everyday life. It’s more about actively trying to appreciate someone’s point of view,” she said. If you’re in a situation and struggling with empathy, it’s not necessarily that you don’t care—your difficulty may be because you don’t understand that person’s perspective. Asking questions and engaging in curiosity is one way to change that.
While Main’s research focuses on parent-child relationships, she says the approach also applies to other relationship dynamics; for example, curiosity about why your spouse doesn’t do the dishes might help you understand influencing factors and, as a result, prevent conflict and promote empathy.
Main suggests asking open-ended questions to the person you want to show empathy to, and providing nonverbal cues like nodding when someone’s talking can encourage that person to share more. Certain questions, like ones you should already know the answer to, can have the opposite effect, as can asking personal questions when your social partner doesn’t wish to share.
The important thing is to express interest. “These kinds of behaviors are really facilitative of disclosure and open discussion,” Main said. “And in the long term, expressing interest in another person can facilitate empathy in the relationship” ( Social Development , Vol. 28, No. 3, 2019).
Understand your blocks
Research suggests everyone has empathy blocks, or areas where it is difficult to exhibit empathy. To combat these barriers to prosocial behavior, Schumann suggests noticing your patterns and focusing on areas where you feel it’s hard to connect to people and relate to their experiences.
If you find it hard to be around negative people, for example, confront this difficulty and spend time with them. Try to reflect on a time when you had a negative outlook on something and observe how they relate. And as you listen, don’t interrupt or formulate rebuttals or responses.
“The person will feel so much more validated and heard when they’ve really had an opportunity to voice their opinion, and most of the time people will reciprocate,” Schumann said. “You might still disagree strongly, but you will have a stronger sense of why they have the perspective they do.”
Second-guess yourself
Much of empathy boils down to willingness to learn—and all learning involves questioning your assumptions and automatic reactions in both big-picture issues, such as racism, and everyday interactions. According to Rumble, it’s important to be mindful of “what-ifs” in frustrating situations before jumping to snap judgments. For example, if a patient is continually late to appointments, don’t assume they don’t take therapy seriously––something else, like stress or unreliable transportation, might be getting in the way of their timeliness.
And if you do find yourself making a negative assumption, slow down and admit you could be wrong. “As scientists, we second-guess our assumptions all the time, looking for alternative explanations,” said Hodges. “We need to do that as people, too.”
Further reading
What’s the matter with empathy? Konrath, S. H., Greater Good Magazine , Jan. 24, 2017
Addressing the empathy deficit: Beliefs about the malleability of empathy predict effortful responses when empathy is challenging Schumann, K., et al., Journal of Personality and Social Psychology , 2014
It is hard to read minds without words: Cues to use to achieve empathic accuracy Hodges, S. D., & Kezer, M., Journal of Intelligence , 2021
Recommended Reading
Contact apa, you may also like.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Br J Gen Pract
- v.63(606); January 2013

Effectiveness of empathy in general practice: a systematic review
Empathy as a characteristic of patient–physician communication in both general practice and clinical care is considered to be the backbone of the patient–physician relationship. Although the value of empathy is seldom debated, its effectiveness is little discussed in general practice. This literature review explores the effectiveness of empathy in general practice. Effects that are discussed are: patient satisfaction and adherence, feelings of anxiety and stress, patient enablement, diagnostics related to information exchange, and clinical outcomes.
To review the existing literature concerning all studies published in the last 15 years on the effectiveness of physician empathy in general practice.
Design and setting
Systematic literature search.
Searches of PubMed, EMBASE, and PsychINFO databases were undertaken, with citation searches of key studies and papers. Original studies published in English between July 1995 and July 2011, containing empirical data about patient experience of GPs’ empathy, were included. Qualitative assessment was applied using Giacomini and Cook’s criteria.
After screening the literature using specified selection criteria, 964 original studies were selected; of these, seven were included in this review after applying quality assessment. There is a good correlation between physician empathy and patient satisfaction and a direct positive relationship with strengthening patient enablement. Empathy lowers patients’ anxiety and distress and delivers significantly better clinical outcomes.
Although only a small number of studies could be used in this search, the general outcome seems to be that empathy in the patient–physician communication in general practice is of unquestionable importance.
INTRODUCTION
Patients consider empathy as a basic component of all therapeutic relationships and a key factor in their definitions of quality of care. 1 , 2 One hundred years ago, Tichener introduced the word ‘empathy’ into the English literature, based on the philosophical aesthetics concept of ‘Einfühlung’ of Theodor Lipps. 3 Another important historical moment is the way Rogers speaks about empathy in 1961 in his book: On Becoming a Person: a Therapist’s View of Psychotherapy. 4 Since then, various authors have written about empathy in the setting of psychotherapy and about its functionality in patient–physician communication. Neuroscientific research of recent decades has achieved significant progress in establishing the neurobiological basis for empathy, after discovering the mirror neuron system (MNS) 5 , 6 as probably being related to people’s capacity to be empathic. 7 Scientists have now added new insights, based on functional magnetic resonance imaging (fMRI) experiments. They have discovered that the MNS consists of mirror neurons in the ventral premotor cortex and the parietal area of the brain and neurons in the somatosensory areas and in limbic and paralimbic structures. 8 The insula plays a fundamental role in connecting these regions. 9 fMRI experiments have shown that individuals who score higher in a questionnaire measuring their tendency to place themselves in the other person’s shoes activate their MNS more strongly while listening to other people’s problems. 10 , 11 These results draw the ‘soft’ concept of empathy into ‘hard’ science, which opens a challenging new field of research with potentially important clinical implications. 12 However, these neurobiological studies do not give information about the impact of empathy in clinical care. Within the current opinion of ‘evidence-based health care’, it is important also to get evidence about the effectiveness of empathy in the daily practice of GPs.
To assess the effectiveness of empathy, it is necessary to define what authors mean when using the term ‘empathy’. Although many authors experience difficulties in giving a clear definition, 1 , 2 , 13 – 20 a number of core elements can be identified. In general, authors consider empathy as the competence of a physician to understand the patient’s situation, perspective, and feelings; to communicate that understanding and check its accuracy; and to act on that understanding in a helpful therapeutic way. It has an affective, a cognitive, and a behavioural dimension. 1 , 21 – 24
Empathy can therefore be defined at three levels: as an attitude (affective), 25 , 26 as a competency (cognitive), 2 , 15 and as a behaviour. 2 , 16
Attitude is based on moral standards in the mind of the physician; such as respectfulness for the authenticity of the other person, interest in the other person, impartiality, and receptivity. These standards are formed by a physician’s own human development, their socialisation process, their medical training, their personal experience with patients; by reading professional literature; and by watching movies and reading books. 13 , 15 , 22 , 27 – 29
How this fits in
Empathy is seen, as well as by patients as by physicians, as the base of good patient-physician communication. Despite these opinions one can see a decrease of interest in good patient-physician communication. There is an increase of technological aspects of care and of a prevalence on productivity in general practice. This systematic review shows that also a “soft” skill like empathy has its effectiveness on patient satisfaction, adherence, decrease of anxiety and stress, better diagnostics and outcomes and patient enablement. Physicians should be more aware of this. In the near future it is a challenge to draw the attention of policy makers and health insures on these aspects of empathy.
Competency can be subdivided into empathic skill, a communication skill, and the skill to build up a relationship with a patient based on mutual trust. Empathic skill is the approach by which the physician can elicit the inner world of the patient and get as much information as possible from the patient, while at the same time recognising the patient’s problem. 2 , 30 , 31 Communication skill is used to check, clarify, support, understand, reconstruct, and reflect on the perception of a patient’s thoughts and feelings. 15 , 23 The skill to build up a trusting and long-standing patient–physician relationship encourages physicians to resonate with the patient emotionally. These long-term relationships are important for telling and listening to the stories of illness. 32 , 33
Behaviour has a cognitive and an affective part. The cognitive part includes verbal and/or non-verbal skills. 14 , 15 , 22 , 25 , 26 The affective part includes recognition of the emotional state or situation of the patient, being moved, and recognising a feeling of identification with someone who suffers with anger, grief, and disappointment. After this recognition, the physician, in their behaviour, reflects on and communicates their understanding to the patient ( Figure 1 ). 20 , 23

Subdivisions of empathy.
Both patients and physicians mention empathy as the basis for a humane patient-centred method in general practice, and as an important component of professionalism. 1 , 17 , 34 A large number of patients, nearly 80%, would recommend an empathic physician to other individuals. 35
Despite these opinions, one can see a decrease of interest in good patient–physician communication. Reynolds et al report a low level of empathy in professional relationships. 34 In their view, this is widespread in modern medicine and many recipients of professional help may not feel that their situation is understood by professionals. 34 A study by Kenny et al suggests that physicians and patients have a different perspective on physicians’ communication skills: the perceptions of the medical encounter have been characterised as being so different that they appear to be from ‘different worlds’. 36
Moreover, different authors report a rising prevalence in the last decade of technological and biomedical aspects of care and of more emphasis on effectiveness and productivity in family care. 17 , 20 , 37 Peabody proved to be prophetic when, in 1927, in his lecture The Care of the Patient, he expressed concern that rapidly growing scientific technology was crowding out human values in the management of patients. 38 Just as Spiro asks attention for the ‘unseen and unheard’ patient in these developments, 20 it is important to pay attention to the effectiveness of empathy in patient–physician communication.
The purpose of this literature review is to get a clear view on the proven effectiveness of empathy in patient–physician communication, in particular in general practice.
A search was undertaken of PubMed, EMBASE, and PsychINFO databases, between July 1995 and July 2011, with the support of a professional librarian, to identify studies of general practice, empathy, and effectiveness or outcome of empathy. The search terms used are shown in Box 1 . The search was performed using major medical subject heading (MeSH) terms in titles and/or abstracts ( Box 1 ). After removal of duplicate studies, titles and abstracts were assessed as to whether the articles were pertinent to this literature review and whether they dealt with general practice. Potentially relevant articles were read in full text. Further papers were sought by checking references and citation searches of included and other leading articles (snowball method). After this selection, articles were assessed as to whether or not they fitted within the inclusion criteria.
Box 1. Database search terms used
((empathy[MeSH] OR empath*[tiab])) AND (Physicians, Family[MeSH] OR Primary Health Care[MeSH] OR Family Practice[MeSH] OR “General Practice”[MeSH] OR “General Practitioners”[MeSH] OR Family Physician*[tiab] OR Primary Health Care[tiab] OR Primary Healthcare[tiab] OR Primary Care[tiab] OR Family Practice*[tiab] OR General Practice*[tiab] OR General Practitioner*[tiab] OR Family Medicine[tiab]) AND outcome*[tw]
To fulfil the inclusion criteria, articles had to detail original and empirical studies, published in English. Studies had to contain patient experience, and outcome measures of empathy and measures of GPs’ empathy. Exclusion criteria were: reviews, guidelines, and theoretical or opinion articles. In the last selection, the studies were evaluated by the criteria of quality developed by Giacomini and Cook ( Box 2 ). 39 From the initial 964 papers, seven meeting the inclusion and qualitative criteria were identified ( Figure 2 ).

Selection process for papers on the effectiveness of empathy in general practice.
Box 2. Giacomini and Cook’s criteria 39
- The participant selection is well reasoned and the inclusion is relevant to the research question; the population is representative.
- The data-collection methods are appropriate for the research objectives and setting; the data collection is valid and reliable.
- The data-collection process, which includes field observation, interviews, and document analysis, must be comprehensive enough to support rich and robust description of the observed events.
- The data must be appropriately analysed and the findings adequately corroborated by using multiple sources of information.
Seven studies were found ( Table 1 ). 40 – 46 The effectiveness of empathy in patient–physician communication in the studies included is described as improvement of patient satisfaction and adherence, decrease of anxiety and distress, better diagnostic and clinical outcomes, and more patient enablement. Patient outcomes were measured by questionnaires and laboratory tests, and by analysing audio- and videotapes.
Summary of included articles
| Author | Country | Quality assessment score | Measure/empathy level | Design | Method | Sample size | Research question | Key findings |
|---|---|---|---|---|---|---|---|---|
| Hojat , 2011 | US | 6 | JSPE/physician rating/cognitive and attitude | Quantitative/RCT with statistical controls | Laboratory results | 891 patients/31 GPs | To test the hypothesis that physician empathy is associated with positive clinical outcomes for patients with diabetes. | Patients of physicians with high empathy scores were significantly more likely to have good control of HbA1c (56%) than were patients of physicians with low empathy scores (40%). Similarly, the proportion of patients with good LDL-C control was significantly higher for physicians with high empathy scores (59%) than for patients of physicians with low scores (44%). |
| Rakel , 2011 | US | 5 | CARE/patient rating/skill and attitude | Quantitative/RCT | Questionnaire and laboratory results | 348 patients/6 GPs | To evaluate the effects of patient–physician interaction on the severity and duration of the common cold. | The ‘physician empathy perfect’ group was associated with the shortest cold duration (5.89 days versus 7.00 days). The amount of change of interleukin-8 and neutrophil level was greater for the ‘physician empathy perfect’ group. |
| van Dulmen et al, 2004 | Netherlands | 4 | RIAS/observer rating/skills | Quantitative | Questionnaire and analysis of video consultations | 698 patients/142 GPs | To examine the physicians’ responses to patients’ concerns in relation to the patient’s empathic preference and perception and the level of anxiety provoked by the medical visit. | 95% of the patients reported that they have perceived their GP to be empathic. The patients who had perceived a more empathic GP reported lower levels of anxiety. |
| Mercer , 2008 | Scotland | 5 | CARE/patient rating/skill and attitude | Qualitative/prospective | Questionnaires | 323 patients/5 GPs | To investigate the relationships between GPs’ empathy, patient enablement and patient-assessed outcomes in primary care consultations in an area of high socioeconomic deprivation in Scotland. | There is a direct relationship between physician empathy and patient enablement. |
| Hojat , 2011 | US | 6 | JSPPPE physician rating cognitive and attitude | Qualitative/RCT | Questionnaires | 535 patients | To develop and examine an instrument to measure patients’ overall satisfaction with their GP. | A large correlation between the perception of physician empathy and patient satisfaction. |
| Buszewicz , 2006 | UK | 6 | TAR/patient rating/long working relationships | Qualitative | Patient interviews | 20 patients/12 GPs | To identify which aspects of GP consultations patients presenting with psychological problems experience as helpful or unhelpful. | Genuine interest and empathy, within a continuing relationship, was highly valued both for psychological and non-psychological problems. |
| Levinson and Roter, 1995 | US | 6 | RIAS/observer rating/skills | Qualitative | Analysis of audiotapes | 412 patients/29 GPs | To assess the relationship between physicians’ beliefs about the psychosocial aspects of patient care and their routine communication with patients. | Physicians who had positive attitudes used more statements of emotions, such as empathy, reassurance, and fewer closed-ended questions than did their colleagues who had less positive attitudes. The patients of these physicians offer more information about psychological and social issues. |
CARE = the Consultation and Relational Empathy measure. HbA1c = gylcosylated haemoglobin. JSPE = Jefferson scale of Physician Empathy. JSPPPE = Jefferson Scale of Patient Perception of Physician Empathy. LDL-C = low-density lipoprotein cholesterol. RCT = randomised controlled trial. RIAS = Roter Interaction Analysis System. TAR = Tape Assistance Recall method.
Improvement of patient satisfaction and adherence
Hojat et al found a good correlation between patients’ satisfaction and their perceptions of physicians’ empathic engagement. 40 Corrected item–total score correlations of the patient satisfaction scale ranged from 0.85 to 0.96; correlation between patient satisfaction scores and patient perception of physician empathy was 0.93. 40
Decrease of anxiety and distress
In the study by van Dulmen et al it was found that the more anxious patients were, the more adequately their GPs tended to respond. Patients who perceived their GP as empathic reported lower levels of anxiety. 41
Better diagnostics and clinical outcomes
Levinson and Roter confirm that communication between physicians and patients is associated with underlying physician attitudes. 42 Specifically, physicians with positive attitudes towards psychosocial issues make more statements expressing concern and empathy. The patients of these physicians offer relatively more information about psychological and social issues. These patterns of communication are associated with improved patient satisfaction and patient outcomes. 42 An underlying attitude of genuine interest and empathy, within a continuing relationship, was highly valued. Patients described how the GP’s attitude helped or hindered them in discussing their problems. Patients also described how the GP helped them make sense of, or resolve, their problems and supported their efforts to change. 43
Hojat et al found a positive relationship between physician empathy and patients’ clinical outcomes. Patients with diabetes had their glycosylated haemoglobin (HbA1c) and low-density lipoprotein (LDL) cholesterol levels checked. Both tests showed significantly better results in patients with a more empathic physician. It is suggested that more empathy in the physician–patient relationship enhances mutual understanding and trust between the physician and patient, which in turn promotes sharing without concealment, leading to a better alignment between patients’ needs and treatment plans, and thus more accurate diagnosis and greater adherence. 44
Even the most common infectious disease on earth, a common cold, is shown to last for significantly less time and to be less severe in cases where there is good physician–patient empathy. A ‘physician empathy perfect group’ was associated with the shortest cold duration (5.89 days versus 7.00 days). The amount of change of interleukin-8 and neutrophil level was greater for the ‘physician empathy perfect’ group. Interleukin-8 and neutrophil counts were obtained from nasal wash at baseline and 48 hours later. 45
More patient enablement
There is a direct positive relationship between GP empathy and patient enablement, as well as between enablement and changes in main complaint and wellbeing. 46 Patient enablement was measured by the Patient Enablement Instrument (PEI), with questions on topics such as: ability to cope with life and illness, and patients’ confidence about their health and their ability to help themselves. 46
This review investigates the relationship between GP empathy and patient outcomes. A GP’s daily practice involves many elements that are not evidence based. The existence and use of empathy in communication is one of these ‘soft’ elements. However, this review shows that there is empirical evidence for effects of human aspects in patient–physician interaction. There is a relationship between empathy in patient–physician communication and patient satisfaction and adherence, patients’ anxiety and distress, better diagnostic and clinical outcomes, and strengthening of patients’ enablement.
As mentioned in the introduction, there are different levels of empathy. Authors used different types of tests to measure these different levels, such as the Jefferson Scale of Patient Perceptions of Physician Empathy (JSPPPE), a self-report measuring scale for cognitive and attitude factors; the Consultation and Relational Empathy Measure (CARE), a patient rating system that measures physicians’ communication skills and attitudes; the Roter Interaction Analysis System (RIAS), an observer rating system that measures empathy skills; and the Tape Assisted Recall method (TAR), which measures the development of a long working relationship. 47
Strengths and limitations
A previous review by Beck et al mentioned that actual empirical data were relatively scarce. 48 With the inclusion criteria used in this review, seven articles were found with a bearing on general practice.
This study has a potential cultural bias in interpreting and judging phenomena by standards inherent to European culture. General practice in Europe is most commonly delivered by GPs. In the US, primary care includes both general internists and paediatricians, as well as GPs.
A possible limitation of this review is the underexposure of ‘the danger of empathy’, such as a physician losing their professional distance, which, in certain situations, might make empathy a less desirable aspect of patient–physician communication. 16 , 49
In focusing on empathy, the effects of contextual factors on specific health outcomes are possibly underexposed, such as intrinsic and/or extrinsic factors, healthcare setting, access to care, GP’s workload or pressure, and sociocultural factors. 50
General limitations of this review are that only articles written in English are included. Furthermore, the existing measures of empathy have been taken as presented in the literature; no critical reflection of the validity of these measures has taken place.
Comparison with existing literature
The results of the studies seem to be supported by other authors. For patient satisfaction and adherence, Neumann et al , 21 Kim et al , 51 and Lelorain et al 52 confirm the data; they found links between physician empathy and patient satisfaction, in various clinical settings. Mercer et al have shown that patients view quality of consultation in general practice as related to both the GP’s competence and the GP’s empathic care. 53 Further, Neumann et al argue that affective-oriented effects of empathy are related to more satisfaction, adherence, and trust. 16 Indirectly, patients who are more satisfied with the care received exercise greater adherence to agreed and recommended treatment regimens and courses of action. 3
In relation to decrease of anxiety and distress, in experimental research in which a GP was trained in special communication styles, Verheul et al found that combining a warm and empathic communication style with raising positive expectations leads to positive effects on the patient’s anxiety. 12
In relation to better diagnostics and clinical outcomes, authors have shown that empathic communication achieves the effect that patients talk more about their symptoms and concerns, enabling the physician to collect more detailed medical and psychosocial information. This leads to more accurate medical and psychosocial perception and ultimately to more accurate diagnosis and treatment regimens. 13 , 22 Neumann et al based their ‘effect model of empathic communication in the clinical encounter’ on this evidence. 16 It has also been mentioned that patients’ overall satisfaction with healthcare services, adherence to medical regimens, comprehension, and perception of a good personal relationship are positively related with interpersonal communication between the patient and care provider and are particularly related to the physician’s empathic behaviour. 24 , 48 , 51 , 54 – 57 However, physician-perceived stress has also been shown to correlate negatively with enablement. 57
Implications for practice and research
Empathy is a familiar term in the helping and caring literature. In 2008, the World Health Organization (WHO) reaffirmed the importance of primary health care with its report Primary Health Care Now More Than Ever. 58 The key challenge was ‘to put people first, since good care is about people’. 58 Rakel said that good medical care will continue to depend on care by concerned and compassionate family physicians who can communicate with patients, understand them, know their families, and see them as more than a case. 59
Qualitative studies show that physicians link empathy to fidelity, prosocial behaviour, moral thinking, good communication, patient and professional satisfaction, good therapeutic relationships, fewer damage claims, good clinical outcomes, and building up a trusting relationship with the patient. 15 , 24 , 25 , 60 , 61 In her study, Shapiro explored how primary care clinician-teachers actually attempt to convey empathy to medical students; they argued that the moral development of the GP, their basic willingness to help, their genuine interest in the other, and an emphasis on the other’s feelings are basic principles for acceptance of the empathic approach to the patient. 25
In GPs’ views, limiting factors during consultation are: time pressure, heavy workload, a cynical view on the effectiveness of empathy, and a lack of skill. 13 , 51 , 62 Neumann et al have shown that patients also see time pressure and busyness on the physician’s part as a limiting factor. 21
Thus empathy can be seen as a part of patient–GP communication, characterised by feelings such as interest and recognition and the physician remaining objective. However, barriers exist for implementation in general practice. 13 , 14 , 24 , 30 , 31 , 47 , 63 , 64
Another finding of this review is that some studies suggest that the degree of empathy shown by medical students declines over the course of their training. 20 , 65 , 66 Empathy appears to increase during the first year of medical school, but decreases after the third year and remains low through the final year of medical school, measured using the Jefferson Scale of Physician Empathy–Student Version (JSPE-S). 17 , 66 , 67 In the study by Hojat et al , 66 there are no sex differences. On the other hand, Quince et al discovered that among males during medical education, in both the bachelor and clinical phases, affective empathy slightly but significantly declined and cognitive empathy was unchanged. Among females, neither affective nor cognitive empathy changed. 68 It is ironic that there are indications that when students can finally begin doing the work they came to medical school to do (that is, taking care of patients) they seem to begin losing empathy. 69 Possible explanations of the decline are: a lack of good role models and changes in general cultural and ethical views on illness, health, and portrayals of mankind. Interviews with physicians show that they think that, in current western society, it has become less a part of human nature to be interested in another person and to be affected by someone else’s misery. 17 In their study of American college students, comparing the temporal changes between 1979 and 2009, Konrath et al showed that this development has social roots. 65 Considering these possible tendencies in education and the above-mentioned technological changes within the healthcare system, which probably influence the patient–physician alliance negatively and could undermine empathy in these relationships, it makes sense to emphasise the results of the present review. The evidence of a correlation between empathy and clinical outcomes should be made widely known, especially among medical students and physicians. Some authors already believe empathy can be improved by targeted educational activities and they indicate opportunities to enhance empathy during education. 16 , 17 , 26 , 38 , 69 – 71
It should be mentioned that, until now, the widely acclaimed benefits of empathy only have a small empirical base. Although a few studies of sufficiently high quality show promising results, much more research is needed to claim the effectiveness of empathy in clinical practice on evidence-based grounds. Neumann et al have already highlighted the need for an examination of the cost-effectiveness of empathy in the light of the recent focus of policy makers and health insurers on the efficiency of health care. 16 It is a challenge to draw the attention of policy makers to empathy as an effective and efficient way of delivering health care. A vast majority of patients want empathic physicians, particularly, but not exclusively, in general practice. 72 Indirectly, authors suppose empathic behaviour improves the physician–patient relationship and causes satisfaction for the patient but also for the physician, 1 , 13 , 22 resulting in fewer cases of compassion fatigue or burn out.
Further research is needed on the practical use of empathy in general practice, with a focus on the effects and side effects of empathy and the expectations of patients and GPs. In this context, it is important to take account of how researchers have measured empathy. Measuring empathy is often based solely on self-reports and is therefore often remote from patients’ and physicians’ concrete feelings, experiences, and interpretations in practice. Only patient-perceived empathy is significantly related to patient outcomes. Therefore, it appears best to use a patient-perceived empathy scale to measure physician empathy in practice. 47 , 48 , 63 , 65 , 73
It is remarkable that empirical studies on physician empathy are still relatively scarce. According to the results of the studies included in this systematic review, empathy is an important factor in patient satisfaction and adherence, in decreasing patients’ anxiety and distress, in better diagnostic and clinical outcomes, and in strengthening patient enablement. Thus, physician empathy seems to improve physical and psychosocial health outcomes.
Acknowledgments
I am most grateful to E Peters, specialist librarian of the medical library, for her help with the database searches.
The study was not funded.
Freely submitted; externally peer reviewed.
Competing interests
The authors have declared no competing interests.
Discuss this article
Contribute and read comments about this article on the Discussion Forum: http://www.rcgp.org.uk/bjgp-discuss

IMAGES
VIDEO
COMMENTS
Empathy is the ability to understand and share other people's feelings [ 10 ]. It is a core concept as, according to the psychodynamic, behavioral and person-centered approaches, it facilitates the development of a therapeutic relationship with the health care user, providing the basis for therapeutic change [ 11 ].
Show compassion. Compassion is an important aspect of empathy, and it is often the missing ingredient in many healthcare interactions. Showing compassion can be as simple as smiling, making eye ...
Introduction. In the last thirty years, the notion of empathy has gained great attention within academia. Commonly defined as "feeling as others" (Hein and Singer 2008, p. 157), the value of empathy has been up for debate.If some emphasize the importance of empathy as the essential tool for achieving a better civil society (Nussbaum 1996) and dealing with prominent global issues such as ...
The applications of empathy are widespread [1,2], and are especially relevant in fields such as medicine, where the successful treatment of patients depends on effective patient-physician interactions. This article explores the concept of empathy and examines its utility in medicine from the perspective of a medical student. What is Empathy?
1. INTRODUCTION. A good patient care experience is a core component of patient‐centered care 1 and thus quality health care. 2 A positive care experience has occurred when patients report that they experienced what they desired during their interactions with care providers and the system, for example, respectful communication, coordinated care, and timeliness. 1, 3 Such care demonstrates the ...
The goal is to operationalize empathy by directly incorporating the patient's voice into how care systems are developed. This approach requires a thorough understanding of the patient journey, including their pain points, challenges, and obstacles. This perspective is usually obtained through surveys and focus groups.
Self-empathy is a much neglected area and is necessary to ensure that health-care workers have the necessary resources to remain empathic toward others. Human beings have intricate, shared neural circuits in motor, sensory, and emotional (limbic) areas of the brain to help them understand the experience of others, leading to helping behaviors.
As empathy gains importance within academia, we propose this review as an attempt to bring clarity upon the diverse and widely debated definitions and conceptions of empathy within the medical field. In this paper, we first evaluate the limits of the Western mainstream medical culture and discuss the origins of phenomena such as dehumanization and detached concern as well as their impacts on ...
Objective. To summarize the predictors and outcomes of empathy by health care personnel, methods used to study their empathy, and the effectiveness of interventions targeting their empathy, in order to advance understanding of the role of empathy in health care and facilitate additional research aimed at increasing positive patient care experiences and outcomes.
The behavior of the listener creates the empathic connection, through body language and words well spoken. Empathy is best thought of as an interpersonal process. In a conversation, being empathic means putting aside our agenda in order to see the others point of view and take account of their emotions. It involves listening with the heart as ...
Empathy, sympathy and compassion are defined and conceptualised in many different ways in the literature and the terms are used interchangeably in research reports and in everyday speech. 1 This conceptual and semantic confusion has practical implications for clinical practice, research and medical education. Empathy, sympathy and compassion also share elements with other forms of pro-social ...
Simply stated, empathy fatigue is the term used to describe the mental, emotional, and physical exhaustion that occurs when providing long-term emotional support to others. It is a common occurrence in people who are overexposed to the emotional needs of others, such as nurses and other healthcare workers.
Much of the recent research in this area has focused on whether empathic and positive communication are beneficial, 6,7 and whether empathic communication can be taught (it seems that it can). 8 A 2001 systematic review found that empathy and positive communication might also improve patient outcomes. 9 However, the evidence has moved on significantly, with numerous randomised trials having ...
Method. A qualitative approach, informed by aspects of grounded theory, was utilized to identify factors that enabled the development of empathy from the perspectives of doctors, nurses, allied healthcare workers and students. Twelve sessions of focus group discussions were conducted with 60 participants from two hospitals, a medical school ...
Dr. Helen Riess. Empathy matters for a couple of reasons. First, empathy is good for patients. It builds trust, which increases patient satisfaction and compliance. When patients perceive that they connect on common ground with the physician, they have better recovery rates. Second, empathy is good for doctors.
The field of medicine is facing a dilemma when it comes to empathy. On one hand, research has found that receiving empathy from caregivers—feeling understood and accepted—is critical for patient satisfaction, a key aspect of hospital reimbursement.On the other hand, over 60 percent of health care providers are experiencing burnout across professions, making now a harder time than ever to ...
Background Healthcare professionals' empathetic behaviors have been known to lead to higher satisfaction levels and produce better health outcomes for patients. However, empathy could decrease over time especially during training and clinical practice. This study explored factors that contributed to the development of empathy in the healthcare setting. Findings could be used to improve the ...
This essay is partly the product of a workshop held at the Nuffield Department of Primary Care, Oxford, on 25 and 26 October 2016 (see Supplemental File). JH, in communication with MG, conceptualised the idea for a reappraisal of the role of empathy in healthcare and developed the plan to hold a workshop to progress this idea.
The first course is Enhancing Empathy in Healthcare, which helps clinicians recognize their own reaction to patients. This introductory course covers the definitions of empathy, why it's important in medicine, and what the consequences are when patients receive unempathetic care. PAs will also learn how to manage themselves with emotional ...
Alexandra Main, PhD, an assistant professor of psychology at the University of California, Merced, said curiosity and interest can also be an important component of empathy. "Mind reading isn't always the way empathy works in everyday life. It's more about actively trying to appreciate someone's point of view," she said.
This essay is partly the product of a workshop held at the Nuffield Department of Primary Care, Oxford, on 25 and 26 October 2016 (see Supplemental File). JH, in communication with MG, conceptualised the idea for a reappraisal of the role of empathy in healthcare and developed the plan to hold a workshop to progress this idea.
INTRODUCTION. Patients consider empathy as a basic component of all therapeutic relationships and a key factor in their definitions of quality of care. 1, 2 One hundred years ago, Tichener introduced the word 'empathy' into the English literature, based on the philosophical aesthetics concept of 'Einfühlung' of Theodor Lipps. 3 Another important historical moment is the way Rogers ...
In the work of the Lancet Commission on the emotional determinants of health, 2 we consider the trajectory of medical school education from a "hidden curriculum" 3 that has historically cultivated detached concern, to an era where empathy is encouraged, 4 yet senior physicians in clinical encounters might model emotional detachment, or worse, harsh or humiliating treatment. 5 Especially in ...
empathy needs action, 'empathy without action is not empathy'.32 Bondi37 emphasises the maintenance of the self-other boundary: Empathy is a process in which one person imaginatively enters the experien-tial world of another without losing an awareness of its difference from one's own. Moral empathy Morse identifies a moral component ...