- About Project
- Testimonials

Business Management Ideas

Essay on Obesity
List of essays on obesity, essay on obesity – short essay (essay 1 – 150 words), essay on obesity (essay 2 – 250 words), essay on obesity – written in english (essay 3 – 300 words), essay on obesity – for school students (class 5, 6, 7, 8, 9, 10, 11 and 12 standard) (essay 4 – 400 words), essay on obesity – for college students (essay 5 – 500 words), essay on obesity – with causes and treatment (essay 6 – 600 words), essay on obesity – for science students (essay 7 – 750 words), essay on obesity – long essay for medical students (essay 8 – 1000 words).
Obesity is a chronic health condition in which the body fat reaches abnormal level. Obesity occurs when we consume much more amount of food than our body really needs on a daily basis. In other words, when the intake of calories is greater than the calories we burn out, it gives rise to obesity.
Audience: The below given essays are exclusively written for school students (Class 5, 6, 7, 8, 9, 10, 11 and 12 Standard), college, science and medical students.
Introduction:
Obesity means being excessively fat. A person would be said to be obese if his or her body mass index is beyond 30. Such a person has a body fat rate that is disproportionate to his body mass.
Obesity and the Body Mass Index:
The body mass index is calculated considering the weight and height of a person. Thus, it is a scientific way of determining the appropriate weight of any person. When the body mass index of a person indicates that he or she is obese, it exposes the person to make health risk.
Stopping Obesity:
There are two major ways to get the body mass index of a person to a moderate rate. The first is to maintain a strict diet. The second is to engage in regular physical exercise. These two approaches are aimed at reducing the amount of fat in the body.
Conclusion:
Obesity can lead to sudden death, heart attack, diabetes and may unwanted illnesses. Stop it by making healthy choices.
Obesity has become a big concern for the youth of today’s generation. Obesity is defined as a medical condition in which an individual gains excessive body fat. When the Body Mass Index (BMI) of a person is over 30, he/ she is termed as obese.
Obesity can be a genetic problem or a disorder that is caused due to unhealthy lifestyle habits of a person. Physical inactivity and the environment in which an individual lives, are also the factors that leads to obesity. It is also seen that when some individuals are in stress or depression, they start cultivating unhealthy eating habits which eventually leads to obesity. Medications like steroids is yet another reason for obesity.
Obesity has several serious health issues associated with it. Some of the impacts of obesity are diabetes, increase of cholesterol level, high blood pressure, etc. Social impacts of obesity includes loss of confidence in an individual, lowering of self-esteem, etc.
The risks of obesity needs to be prevented. This can be done by adopting healthy eating habits, doing some physical exercise regularly, avoiding stress, etc. Individuals should work on weight reduction in order to avoid obesity.
Obesity is indeed a health concern and needs to be prioritized. The management of obesity revolves around healthy eating habits and physical activity. Obesity, if not controlled in its initial stage can cause many severe health issues. So it is wiser to exercise daily and maintain a healthy lifestyle rather than being the victim of obesity.
Obesity can be defined as the clinical condition where accumulation of excessive fat takes place in the adipose tissue leading to worsening of health condition. Usually, the fat is deposited around the trunk and also the waist of the body or even around the periphery.
Obesity is actually a disease that has been spreading far and wide. It is preventable and certain measures are to be taken to curb it to a greater extend. Both in the developing and developed countries, obesity has been growing far and wide affecting the young and the old equally.
The alarming increase in obesity has resulted in stimulated death rate and health issues among the people. There are several methods adopted to lose weight and they include different diet types, physical activity and certain changes in the current lifestyle. Many of the companies are into minting money with the concept of inviting people to fight obesity.
In patients associated with increased risk factor related to obesity, there are certain drug therapies and other procedures adopted to lose weight. There are certain cost effective ways introduced by several companies to enable clinic-based weight loss programs.
Obesity can lead to premature death and even cause Type 2 Diabetes Mellitus. Cardiovascular diseases have also become the part and parcel of obese people. It includes stroke, hypertension, gall bladder disease, coronary heart disease and even cancers like breast cancer, prostate cancer, endometrial cancer and colon cancer. Other less severe arising due to obesity includes osteoarthritis, gastro-esophageal reflux disease and even infertility.
Hence, serious measures are to be taken to fight against this dreadful phenomenon that is spreading its wings far and wide. Giving proper education on benefits of staying fit and mindful eating is as important as curbing this issue. Utmost importance must be given to healthy eating habits right from the small age so that they follow the same until the end of their life.
Obesity is majorly a lifestyle disease attributed to the extra accumulation of fat in the body leading to negative health effects on a person. Ironically, although prevalent at a large scale in many countries, including India, it is one of the most neglect health problems. It is more often ignored even if told by the doctor that the person is obese. Only when people start acquiring other health issues such as heart disease, blood pressure or diabetes, they start taking the problem of obesity seriously.
Obesity Statistics in India:
As per a report, India happens to figure as the third country in the world with the most obese people. This should be a troubling fact for India. However, we are yet to see concrete measures being adopted by the people to remain fit.
Causes of Obesity:
Sedentary lifestyle, alcohol, junk food, medications and some diseases such as hypothyroidism are considered as the factors which lead to obesity. Even children seem to be glued to televisions, laptops and video games which have taken away the urge for physical activities from them. Adding to this, the consumption of junk food has further aggravated the growing problem of obesity in children.
In the case of adults, most of the professions of today make use of computers which again makes people sit for long hours in one place. Also, the hectic lifestyle of today makes it difficult for people to spare time for physical activities and people usually remain stressed most of the times. All this has contributed significantly to the rise of obesity in India.
Obesity and BMI:
Body Mass Index (BMI) is the measure which allows a person to calculate how to fit he or she is. In other words, the BMI tells you if you are obese or not. BMI is calculated by dividing the weight of a person in kg with the square of his / her height in metres. The number thus obtained is called the BMI. A BMI of less than 25 is considered optimal. However, if a person has a BMI over 30 he/she is termed as obese.
What is a matter of concern is that with growing urbanisation there has been a rapid increase of obese people in India? It is of utmost importance to consider this health issue a serious threat to the future of our country as a healthy body is important for a healthy soul. We should all be mindful of what we eat and what effect it has on our body. It is our utmost duty to educate not just ourselves but others as well about this serious health hazard.
Obesity can be defined as a condition (medical) that is the accumulation of body fat to an extent that the excess fat begins to have a lot of negative effects on the health of the individual. Obesity is determined by examining the body mass index (BMI) of the person. The BMI is gotten by dividing the weight of the person in kilogram by the height of the person squared.
When the BMI of a person is more than 30, the person is classified as being obese, when the BMI falls between 25 and 30, the person is said to be overweight. In a few countries in East Asia, lower values for the BMI are used. Obesity has been proven to influence the likelihood and risk of many conditions and disease, most especially diabetes of type 2, cardiovascular diseases, sleeplessness that is obstructive, depression, osteoarthritis and some cancer types.
In most cases, obesity is caused through a combination of genetic susceptibility, a lack of or inadequate physical activity, excessive intake of food. Some cases of obesity are primarily caused by mental disorder, medications, endocrine disorders or genes. There is no medical data to support the fact that people suffering from obesity eat very little but gain a lot of weight because of slower metabolism. It has been discovered that an obese person usually expends much more energy than other people as a result of the required energy that is needed to maintain a body mass that is increased.
It is very possible to prevent obesity with a combination of personal choices and social changes. The major treatments are exercising and a change in diet. We can improve the quality of our diet by reducing our consumption of foods that are energy-dense like those that are high in sugars or fat and by trying to increase our dietary fibre intake.
We can also accompany the appropriate diet with the use of medications to help in reducing appetite and decreasing the absorption of fat. If medication, exercise and diet are not yielding any positive results, surgery or gastric balloon can also be carried out to decrease the volume of the stomach and also reduce the intestines’ length which leads to the feel of the person get full early or a reduction in the ability to get and absorb different nutrients from a food.
Obesity is the leading cause of ill-health and death all over the world that is preventable. The rate of obesity in children and adults has drastically increased. In 2015, a whopping 12 percent of adults which is about 600 million and about 100 million children all around the world were found to be obese.
It has also been discovered that women are more obese than men. A lot of government and private institutions and bodies have stated that obesity is top of the list of the most difficult and serious problems of public health that we have in the world today. In the world we live today, there is a lot of stigmatisation of obese people.
We all know how troubling the problem of obesity truly is. It is mainly a form of a medical condition wherein the body tends to accumulate excessive fat which in turn has negative repercussions on the health of an individual.
Given the current lifestyle and dietary style, it has become more common than ever. More and more people are being diagnosed with obesity. Such is its prevalence that it has been termed as an epidemic in the USA. Those who suffer from obesity are at a much higher risk of diabetes, heart diseases and even cancer.
In order to gain a deeper understanding of obesity, it is important to learn what the key causes of obesity are. In a layman term, if your calorie consumption exceeds what you burn because of daily activities and exercises, it is likely to lead to obesity. It is caused over a prolonged period of time when your calorie intake keeps exceeding the calories burned.
Here are some of the key causes which are known to be the driving factors for obesity.
If your diet tends to be rich in fat and contains massive calorie intake, you are all set to suffer from obesity.
Sedentary Lifestyle:
With most people sticking to their desk jobs and living a sedentary lifestyle, the body tends to get obese easily.
Of course, the genetic framework has a lot to do with obesity. If your parents are obese, the chance of you being obese is quite high.
The weight which women gain during their pregnancy can be very hard to shed and this is often one of the top causes of obesity.
Sleep Cycle:
If you are not getting an adequate amount of sleep, it can have an impact on the hormones which might trigger hunger signals. Overall, these linked events tend to make you obese.
Hormonal Disorder:
There are several hormonal changes which are known to be direct causes of obesity. The imbalance of the thyroid stimulating hormone, for instance, is one of the key factors when it comes to obesity.
Now that we know the key causes, let us look at the possible ways by which you can handle it.
Treatment for Obesity:
As strange as it may sound, the treatment for obesity is really simple. All you need to do is follow the right diet and back it with an adequate amount of exercise. If you can succeed in doing so, it will give you the perfect head-start into your journey of getting in shape and bidding goodbye to obesity.
There are a lot of different kinds and styles of diet plans for obesity which are available. You can choose the one which you deem fit. We recommend not opting for crash dieting as it is known to have several repercussions and can make your body terribly weak.
The key here is to stick to a balanced diet which can help you retain the essential nutrients, minerals, and, vitamins and shed the unwanted fat and carbs.
Just like the diet, there are several workout plans for obesity which are available. It is upon you to find out which of the workout plan seems to be apt for you. Choose cardio exercises and dance routines like Zumba to shed the unwanted body weight. Yoga is yet another method to get rid of obesity.
So, follow a blend of these and you will be able to deal with the trouble of obesity in no time. We believe that following these tips will help you get rid of obesity and stay in shape.
Obesity and overweight is a top health concern in the world due to the impact it has on the lives of individuals. Obesity is defined as a condition in which an individual has excessive body fat and is measured using the body mass index (BMI) such that, when an individual’s BMI is above 30, he or she is termed obese. The BMI is calculated using body weight and height and it is different for all individuals.
Obesity has been determined as a risk factor for many diseases. It results from dietary habits, genetics, and lifestyle habits including physical inactivity. Obesity can be prevented so that individuals do not end up having serious complications and health problems. Chronic illnesses like diabetes, heart diseases and relate to obesity in terms of causes and complications.
Factors Influencing Obesity:
Obesity is not only as a result of lifestyle habits as most people put it. There are other important factors that influence obesity. Genetics is one of those factors. A person could be born with genes that predispose them to obesity and they will also have difficulty in losing weight because it is an inborn factor.
The environment also influences obesity because the diet is similar in certain environs. In certain environments, like school, the food available is fast foods and the chances of getting healthy foods is very low, leading to obesity. Also, physical inactivity is an environmental factor for obesity because some places have no fields or tracks where people can jog or maybe the place is very unsafe and people rarely go out to exercise.
Mental health affects the eating habits of individuals. There is a habit of stress eating when a person is depressed and it could result in overweight or obesity if the person remains unhealthy for long period of time.
The overall health of individuals also matter. If a person is unwell and is prescribed with steroids, they may end up being obese. Steroidal medications enable weight gain as a side effect.
Complications of Obesity:
Obesity is a health concern because its complications are severe. Significant social and health problems are experienced by obese people. Socially, they will be bullied and their self-esteem will be low as they will perceive themselves as unworthy.
Chronic illnesses like diabetes results from obesity. Diabetes type 2 has been directly linked to obesity. This condition involves the increased blood sugars in the body and body cells are not responding to insulin as they should. The insulin in the body could also be inadequate due to decreased production. High blood sugar concentrations result in symptoms like frequent hunger, thirst and urination. The symptoms of complicated stages of diabetes type 2 include loss of vision, renal failure and heart failure and eventually death. The importance of having a normal BMI is the ability of the body to control blood sugars.
Another complication is the heightened blood pressures. Obesity has been defined as excessive body fat. The body fat accumulates in blood vessels making them narrow. Narrow blood vessels cause the blood pressures to rise. Increased blood pressure causes the heart to start failing in its physiological functions. Heart failure is the end result in this condition of increased blood pressures.
There is a significant increase in cholesterol in blood of people who are obese. High blood cholesterol levels causes the deposition of fats in various parts of the body and organs. Deposition of fats in the heart and blood vessels result in heart diseases. There are other conditions that result from hypercholesterolemia.
Other chronic illnesses like cancer can also arise from obesity because inflammation of body cells and tissues occurs in order to store fats in obese people. This could result in abnormal growths and alteration of cell morphology. The abnormal growths could be cancerous.
Management of Obesity:
For the people at risk of developing obesity, prevention methods can be implemented. Prevention included a healthy diet and physical activity. The diet and physical activity patterns should be regular and realizable to avoid strains that could result in complications.
Some risk factors for obesity are non-modifiable for example genetics. When a person in genetically predisposed, the lifestyle modifications may be have help.
For the individuals who are already obese, they can work on weight reduction through healthy diets and physical exercises.
In conclusion, obesity is indeed a major health concern because the health complications are very serious. Factors influencing obesity are both modifiable and non-modifiable. The management of obesity revolves around diet and physical activity and so it is important to remain fit.
In olden days, obesity used to affect only adults. However, in the present time, obesity has become a worldwide problem that hits the kids as well. Let’s find out the most prevalent causes of obesity.
Factors Causing Obesity:
Obesity can be due to genetic factors. If a person’s family has a history of obesity, chances are high that he/ she would also be affected by obesity, sooner or later in life.
The second reason is having a poor lifestyle. Now, there are a variety of factors that fall under the category of poor lifestyle. An excessive diet, i.e., eating more than you need is a definite way to attain the stage of obesity. Needless to say, the extra calories are changed into fat and cause obesity.
Junk foods, fried foods, refined foods with high fats and sugar are also responsible for causing obesity in both adults and kids. Lack of physical activity prevents the burning of extra calories, again, leading us all to the path of obesity.
But sometimes, there may also be some indirect causes of obesity. The secondary reasons could be related to our mental and psychological health. Depression, anxiety, stress, and emotional troubles are well-known factors of obesity.
Physical ailments such as hypothyroidism, ovarian cysts, and diabetes often complicate the physical condition and play a massive role in abnormal weight gain.
Moreover, certain medications, such as steroids, antidepressants, and contraceptive pills, have been seen interfering with the metabolic activities of the body. As a result, the long-term use of such drugs can cause obesity. Adding to that, regular consumption of alcohol and smoking are also connected to the condition of obesity.
Harmful Effects of Obesity:
On the surface, obesity may look like a single problem. But, in reality, it is the mother of several major health issues. Obesity simply means excessive fat depositing into our body including the arteries. The drastic consequence of such high cholesterol levels shows up in the form of heart attacks and other life-threatening cardiac troubles.
The fat deposition also hampers the elasticity of the arteries. That means obesity can cause havoc in our body by altering the blood pressure to an abnormal range. And this is just the tip of the iceberg. Obesity is known to create an endless list of problems.
In extreme cases, this disorder gives birth to acute diseases like diabetes and cancer. The weight gain due to obesity puts a lot of pressure on the bones of the body, especially of the legs. This, in turn, makes our bones weak and disturbs their smooth movement. A person suffering from obesity also has higher chances of developing infertility issues and sleep troubles.
Many obese people are seen to be struggling with breathing problems too. In the chronic form, the condition can grow into asthma. The psychological effects of obesity are another serious topic. You can say that obesity and depression form a loop. The more a person is obese, the worse is his/ her depression stage.
How to Control and Treat Obesity:
The simplest and most effective way, to begin with, is changing our diet. There are two factors to consider in the diet plan. First is what and what not to eat. Second is how much to eat.
If you really want to get rid of obesity, include more and more green vegetables in your diet. Spinach, beans, kale, broccoli, cauliflower, asparagus, etc., have enough vitamins and minerals and quite low calories. Other healthier options are mushrooms, pumpkin, beetroots, and sweet potatoes, etc.
Opt for fresh fruits, especially citrus fruits, and berries. Oranges, grapes, pomegranate, pineapple, cherries, strawberries, lime, and cranberries are good for the body. They have low sugar content and are also helpful in strengthening our immune system. Eating the whole fruits is a more preferable way in comparison to gulping the fruit juices. Fruits, when eaten whole, have more fibers and less sugar.
Consuming a big bowl of salad is also great for dealing with the obesity problem. A salad that includes fibrous foods such as carrots, radish, lettuce, tomatoes, works better at satiating the hunger pangs without the risk of weight gain.
A high protein diet of eggs, fish, lean meats, etc., is an excellent choice to get rid of obesity. Take enough of omega fatty acids. Remember to drink plenty of water. Keeping yourself hydrated is a smart way to avoid overeating. Water also helps in removing the toxins and excess fat from the body.
As much as possible, avoid fats, sugars, refined flours, and oily foods to keep the weight in control. Control your portion size. Replace the three heavy meals with small and frequent meals during the day. Snacking on sugarless smoothies, dry fruits, etc., is much recommended.
Regular exercise plays an indispensable role in tackling the obesity problem. Whenever possible, walk to the market, take stairs instead of a lift. Physical activity can be in any other form. It could be a favorite hobby like swimming, cycling, lawn tennis, or light jogging.
Meditation and yoga are quite powerful practices to drive away the stress, depression and thus, obesity. But in more serious cases, meeting a physician is the most appropriate strategy. Sometimes, the right medicines and surgical procedures are necessary to control the health condition.
Obesity is spreading like an epidemic, haunting both the adults and the kids. Although genetic factors and other physical ailments play a role, the problem is mostly caused by a reckless lifestyle.
By changing our way of living, we can surely take control of our health. In other words, it would be possible to eliminate the condition of obesity from our lives completely by leading a healthy lifestyle.
Health , Obesity
Get FREE Work-at-Home Job Leads Delivered Weekly!

Join more than 50,000 subscribers receiving regular updates! Plus, get a FREE copy of How to Make Money Blogging!
Message from Sophia!
Like this post? Don’t forget to share it!
Here are a few recommended articles for you to read next:
- Essay on Cleanliness
- Essay on Cancer
- Essay on AIDS
- Essay on Health and Fitness
No comments yet.
Leave a reply click here to cancel reply..
You must be logged in to post a comment.
Billionaires
- Donald Trump
- Warren Buffett
- Email Address
- Free Stock Photos
- Keyword Research Tools
- URL Shortener Tools
- WordPress Theme
Book Summaries
- How To Win Friends
- Rich Dad Poor Dad
- The Code of the Extraordinary Mind
- The Luck Factor
- The Millionaire Fastlane
- The ONE Thing
- Think and Grow Rich
- 100 Million Dollar Business
- Business Ideas
Digital Marketing
- Mobile Addiction
- Social Media Addiction
- Computer Addiction
- Drug Addiction
- Internet Addiction
- TV Addiction
- Healthy Habits
- Morning Rituals
- Wake up Early
- Cholesterol
- Reducing Cholesterol
- Fat Loss Diet Plan
- Reducing Hair Fall
- Sleep Apnea
- Weight Loss
Internet Marketing
- Email Marketing
Law of Attraction
- Subconscious Mind
- Vision Board
- Visualization
Law of Vibration
- Professional Life
Motivational Speakers
- Bob Proctor
- Robert Kiyosaki
- Vivek Bindra
- Inner Peace
Productivity
- Not To-do List
- Project Management Software
- Negative Energies
Relationship
- Getting Back Your Ex
Self-help 21 and 14 Days Course
Self-improvement.
- Body Language
- Complainers
- Emotional Intelligence
- Personality
Social Media
- Project Management
- Anik Singal
- Baba Ramdev
- Dwayne Johnson
- Jackie Chan
- Leonardo DiCaprio
- Narendra Modi
- Nikola Tesla
- Sachin Tendulkar
- Sandeep Maheshwari
- Shaqir Hussyin
Website Development
Wisdom post, worlds most.
- Expensive Cars
Our Portals: Gulf Canada USA Italy Gulf UK
Privacy Overview
| Cookie | Duration | Description |
|---|---|---|
| cookielawinfo-checkbox-analytics | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookie is used to store the user consent for the cookies in the category "Analytics". |
| cookielawinfo-checkbox-functional | 11 months | The cookie is set by GDPR cookie consent to record the user consent for the cookies in the category "Functional". |
| cookielawinfo-checkbox-necessary | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookies is used to store the user consent for the cookies in the category "Necessary". |
| cookielawinfo-checkbox-others | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookie is used to store the user consent for the cookies in the category "Other. |
| cookielawinfo-checkbox-performance | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookie is used to store the user consent for the cookies in the category "Performance". |
| viewed_cookie_policy | 11 months | The cookie is set by the GDPR Cookie Consent plugin and is used to store whether or not user has consented to the use of cookies. It does not store any personal data. |
470 Obesity Essay Topic Ideas & Examples
Looking for obesity essay topics? Being a serious problem, obesity is definitely worth writing about.
Obesity Essay: A Complete Guide and Topics
By: Nova A.
11 min read
Reviewed By: Jacklyn H.
Published on: Aug 31, 2021

Are you assigned to write an essay about obesity? The first step is to define obesity.
The obesity epidemic is a major issue facing our country right now. It's complicated- it could be genetic or due to your environment, but either way, there are ways that you can fix it!
Learn all about what causes weight gain and get tips on how you can get healthy again.

On this Page
What is Obesity
What is obesity? Obesity and BMI (body mass index) are both tools of measurement that are used by doctors to assess body fat according to the height, age, and gender of a person. If the BMI is between 25 to 29.9, that means the person has excess weight and body fat.
If the BMI exceeds 30, that means the person is obese. Obesity is a condition that increases the risk of developing cardiovascular diseases, high blood pressure, and other medical conditions like metabolic syndrome, arthritis, and even some types of cancer.
Obesity Definition
Obesity is defined by the World Health Organization as an accumulation of abnormal and excess body fat that comes with several risk factors. It is measured by the body mass index BMI, body weight (in kilograms) divided by the square of a person’s height (in meters).
Obesity in America
Obesity is on the verge of becoming an epidemic as 1 in every 3 Americans can be categorized as overweight and obese. Currently, America is an obese country, and it continues to get worse.

Paper Due? Why Suffer? That's our Job!
Causes of obesity
Do you see any obese or overweight people around you?
You likely do.
This is because fast-food chains are becoming more and more common, people are less active, and fruits and vegetables are more expensive than processed foods, thus making them less available to the majority of society. These are the primary causes of obesity.
Obesity is a disease that affects all age groups, including children and elderly people.
Now that you are familiar with the topic of obesity, writing an essay won’t be that difficult for you.
How to Write an Obesity Essay
The format of an obesity essay is similar to writing any other essay. If you need help regarding how to write an obesity essay, it is the same as writing any other essay.
Obesity Essay Introduction
The trick is to start your essay with an interesting and catchy sentence. This will help attract the reader's attention and motivate them to read further. You don’t want to lose the reader’s interest in the beginning and leave a bad impression, especially if the reader is your teacher.
A hook sentence is usually used to open the introductory paragraph of an essay in order to make it interesting. When writing an essay on obesity, the hook sentence can be in the form of an interesting fact or statistic.
Head on to this detailed article on hook examples to get a better idea.
Once you have hooked the reader, the next step is to provide them with relevant background information about the topic. Don’t give away too much at this stage or bombard them with excess information that the reader ends up getting bored with. Only share information that is necessary for the reader to understand your topic.
Next, write a strong thesis statement at the end of your essay, be sure that your thesis identifies the purpose of your essay in a clear and concise manner. Also, keep in mind that the thesis statement should be easy to justify as the body of your essay will revolve around it.
Body Paragraphs
The details related to your topic are to be included in the body paragraphs of your essay. You can use statistics, facts, and figures related to obesity to reinforce your thesis throughout your essay.
If you are writing a cause-and-effect obesity essay, you can mention different causes of obesity and how it can affect a person’s overall health. The number of body paragraphs can increase depending on the parameters of the assignment as set forth by your instructor.
Start each body paragraph with a topic sentence that is the crux of its content. It is necessary to write an engaging topic sentence as it helps grab the reader’s interest. Check out this detailed blog on writing a topic sentence to further understand it.
End your essay with a conclusion by restating your research and tying it to your thesis statement. You can also propose possible solutions to control obesity in your conclusion. Make sure that your conclusion is short yet powerful.
Obesity Essay Examples
Essay about Obesity (PDF)
Childhood Obesity Essay (PDF)
Obesity in America Essay (PDF)
Essay about Obesity Cause and Effects (PDF)
Satire Essay on Obesity (PDF)
Obesity Argumentative Essay (PDF)
Obesity Essay Topics
Choosing a topic might seem an overwhelming task as you may have many ideas for your assignment. Brainstorm different ideas and narrow them down to one, quality topic.
If you need some examples to help you with your essay topic related to obesity, dive into this article and choose from the list of obesity essay topics.
Childhood Obesity
As mentioned earlier, obesity can affect any age group, including children. Obesity can cause several future health problems as children age.
Here are a few topics you can choose from and discuss for your childhood obesity essay:
- What are the causes of increasing obesity in children?
- Obese parents may be at risk for having children with obesity.
- What is the ratio of obesity between adults and children?
- What are the possible treatments for obese children?
- Are there any social programs that can help children with combating obesity?
- Has technology boosted the rate of obesity in children?
- Are children spending more time on gadgets instead of playing outside?
- Schools should encourage regular exercises and sports for children.
- How can sports and other physical activities protect children from becoming obese?
- Can childhood abuse be a cause of obesity among children?
- What is the relationship between neglect in childhood and obesity in adulthood?
- Does obesity have any effect on the psychological condition and well-being of a child?
- Are electronic medical records effective in diagnosing obesity among children?
- Obesity can affect the academic performance of your child.
- Do you believe that children who are raised by a single parent can be vulnerable to obesity?
- You can promote interesting exercises to encourage children.
- What is the main cause of obesity, and why is it increasing with every passing day?
- Schools and colleges should work harder to develop methodologies to decrease childhood obesity.
- The government should not allow schools and colleges to include sweet or fatty snacks as a part of their lunch.
- If a mother is obese, can it affect the health of the child?
- Children who gain weight frequently can develop chronic diseases.
Obesity Argumentative Essay Topics
Do you want to write an argumentative essay on the topic of obesity?
The following list can help you with that!
Here are some examples you can choose from for your argumentative essay about obesity:
- Can vegetables and fruits decrease the chances of obesity?
- Should you go for surgery to overcome obesity?
- Are there any harmful side effects?
- Can obesity be related to the mental condition of an individual?
- Are parents responsible for controlling obesity in childhood?
- What are the most effective measures to prevent the increase in the obesity rate?
- Why is the obesity rate increasing in the United States?
- Can the lifestyle of a person be a cause of obesity?
- Does the economic situation of a country affect the obesity rate?
- How is obesity considered an international health issue?
- Can technology and gadgets affect obesity rates?
- What can be the possible reasons for obesity in a school?
- How can we address the issue of obesity?
- Is obesity a chronic disease?
- Is obesity a major cause of heart attacks?
- Are the junk food chains causing an increase in obesity?
- Do nutritional programs help in reducing the obesity rate?
- How can the right type of diet help with obesity?
- Why should we encourage sports activities in schools and colleges?
- Can obesity affect a person’s behavior?
Health Related Topics for Research Paper
If you are writing a research paper, you can explain the cause and effect of obesity.
Here are a few topics that link to the cause and effects of obesity.Review the literature of previous articles related to obesity. Describe the ideas presented in the previous papers.
- Can family history cause obesity in future generations?
- Can we predict obesity through genetic testing?
- What is the cause of the increasing obesity rate?
- Do you think the increase in fast-food restaurants is a cause of the rising obesity rate?
- Is the ratio of obese women greater than obese men?
- Why are women more prone to be obese as compared to men?
- Stress can be a cause of obesity. Mention the reasons how mental health can be related to physical health.
- Is urban life a cause of the increasing obesity rate?
- People from cities are prone to be obese as compared to people from the countryside.
- How obesity affects the life expectancy of people? What are possible solutions to decrease the obesity rate?
- Do family eating habits affect or trigger obesity?
- How do eating habits affect the health of an individual?
- How can obesity affect the future of a child?
- Obese children are more prone to get bullied in high school and college.
- Why should schools encourage more sports and exercise for children?
Tough Essay Due? Hire Tough Writers!
Topics for Essay on Obesity as a Problem
Do you think a rise in obesity rate can affect the economy of a country?
Here are some topics for your assistance regarding your economics related obesity essay.
- Does socioeconomic status affect the possibility of obesity in an individual?
- Analyze the film and write a review on “Fed Up” – an obesity epidemic.
- Share your reviews on the movie “The Weight of The Nation.”
- Should we increase the prices of fast food and decrease the prices of fruits and vegetables to decrease obesity?
- Do you think healthy food prices can be a cause of obesity?
- Describe what measures other countries have taken in order to control obesity?
- The government should play an important role in controlling obesity. What precautions should they take?
- Do you think obesity can be one of the reasons children get bullied?
- Do obese people experience any sort of discrimination or inappropriate behavior due to their weight?
- Are there any legal protections for people who suffer from discrimination due to their weight?
- Which communities have a higher percentage of obesity in the United States?
- Discuss the side effects of the fast-food industry and their advertisements on children.
- Describe how the increasing obesity rate has affected the economic condition of the United States.
- What is the current percentage of obesity all over the world? Is the obesity rate increasing with every passing day?
- Why is the obesity rate higher in the United States as compared to other countries?
- Do Asians have a greater percentage of obese people as compared to Europe?
- Does the cultural difference affect the eating habits of an individual?
- Obesity and body shaming.
- Why is a skinny body considered to be ideal? Is it an effective way to reduce the obesity rate?
Obesity Solution Essay Topics
With all the developments in medicine and technology, we still don’t have exact measures to treat obesity.
Here are some insights you can discuss in your essay:
- How do obese people suffer from metabolic complications?
- Describe the fat distribution in obese people.
- Is type 2 diabetes related to obesity?
- Are obese people more prone to suffer from diabetes in the future?
- How are cardiac diseases related to obesity?
- Can obesity affect a woman’s childbearing time phase?
- Describe the digestive diseases related to obesity.
- Obesity may be genetic.
- Obesity can cause a higher risk of suffering a heart attack.
- What are the causes of obesity? What health problems can be caused if an individual suffers from obesity?
- What are the side effects of surgery to overcome obesity?
- Which drugs are effective when it comes to the treatment of obesity?
- Is there a difference between being obese and overweight?
- Can obesity affect the sociological perspective of an individual?
- Explain how an obesity treatment works.
- How can the government help people to lose weight and improve public health?
Writing an essay is a challenging yet rewarding task. All you need is to be organized and clear when it comes to academic writing.
- Choose a topic you would like to write on.
- Organize your thoughts.
- Pen down your ideas.
- Compose a perfect essay that will help you ace your subject.
- Proofread and revise your paper.
Were the topics useful for you? We hope so!
However, if you are still struggling to write your paper, you can pick any of the topics from this list, and our essay writer will help you craft a perfect essay.
Are you struggling to write an effective essay?
If writing an essay is the actual problem and not just the topic, you can always hire an essay writing service for your help. Essay experts at 5StarEssays can help compose an impressive essay within your deadline.
All you have to do is contact us. We will get started on your paper while you can sit back and relax.
Place your order now to get an A-worthy essay.

Marketing, Thesis
As a Digital Content Strategist, Nova Allison has eight years of experience in writing both technical and scientific content. With a focus on developing online content plans that engage audiences, Nova strives to write pieces that are not only informative but captivating as well.
Was This Blog Helpful?
Keep reading.
- How to Write A Bio – Professional Tips and Examples

- Learn How to Write an Article Review with Examples

- How to Write a Poem Step-by-Step Like a Pro

- How To Write Poetry - 7 Fundamentals and Tips

- Know About Appendix Writing With the Help of Examples

- List of Social Issues Faced By the World

- How To Write A Case Study - Easy Guide

- Learn How to Avoid Plagiarism in 7 Simple Steps

- Writing Guide of Visual Analysis Essay for Beginners

- Learn How to Write a Personal Essay by Experts

- Character Analysis - A Step By Step Guide

- Thematic Statement: Writing Tips and Examples

- Expert Guide on How to Write a Summary

- How to Write an Opinion Essay - Structure, Topics & Examples

- How to Write a Synopsis - Easy Steps and Format Guide

- Learn How To Write An Editorial By Experts

- How to Get Better at Math - Easy Tips and Tricks

- How to Write a Movie Review - Steps and Examples

- Creative Writing - Easy Tips For Beginners

- Types of Plagiarism Every Student Should Know

People Also Read
- reflective essay topics
- visual analysis essay
- persuasive essay topics
- scholarship essay format
- apa vs mla format
Burdened With Assignments?
Advertisement
- Homework Services: Essay Topics Generator
© 2024 - All rights reserved
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Wiley Open Access Collection

Obesity: Risk factors, complications, and strategies for sustainable long‐term weight management
Sharon m. fruh.
1 College of Nursing, University of South Alabama, Mobile, Alabama
Background and Purpose
The aims of this article are to review the effects of obesity on health and well‐being and the evidence indicating they can be ameliorated by weight loss, and consider weight‐management strategies that may help patients achieve and maintain weight loss.
Narrative review based on literature searches of PubMed up to May 2016 with no date limits imposed. Search included terms such as “obesity,” “overweight,” “weight loss,” “comorbidity,” “diabetes,” cardiovascular,” “cancer,” “depression,” “management,” and “intervention.”
Conclusions
Over one third of U.S. adults have obesity. Obesity is associated with a range of comorbidities, including diabetes, cardiovascular disease, obstructive sleep apnea, and cancer; however, modest weight loss in the 5%–10% range, and above, can significantly improve health‐related outcomes. Many individuals struggle to maintain weight loss, although strategies such as realistic goal‐setting and increased consultation frequency can greatly improve the success of weight‐management programs. Nurse practitioners have key roles in establishing weight‐loss targets, providing motivation and support, and implementing weight‐loss programs.
Implications for Practice
With their in‐depth understanding of the research in the field of obesity and weight management, nurse practitioners are well placed to effect meaningful changes in weight‐management strategies deployed in clinical practice.
Introduction
Obesity is an increasing, global public health issue. Patients with obesity are at major risk for developing a range of comorbid conditions, including cardiovascular disease (CVD), gastrointestinal disorders, type 2 diabetes (T2D), joint and muscular disorders, respiratory problems, and psychological issues, which may significantly affect their daily lives as well as increasing mortality risks. Obesity‐associated conditions are manifold; however, even modest weight reduction may enable patients to reduce their risk for CVD, diabetes, obstructive sleep apnea (OSA), and hypertension among many other comorbidities (Cefalu et al., 2015 ). A relatively small and simple reduction in weight, for example, of around 5%, can improve patient outcomes and may act as a catalyst for further change, with sustainable weight loss achieved through a series of incremental weight loss steps. In facilitating the process of losing weight for patients, nurse practitioners play an essential role. Through assessing the patient's risk, establishing realistic weight‐loss targets, providing motivation and support, and supplying patients with the necessary knowledge and treatment tools to help achieve weight loss, followed by tools for structured lifestyle support to maintain weight lost, the nurse practitioner is ideally positioned to help patient's achieve their weight‐loss—and overall health—targets.
The obesity epidemic
The World Health Organization (WHO) defines overweight and obesity as abnormal or excessive fat accumulation that presents a risk to health (WHO, 2016a ). A body mass index (BMI) ≥25 kg/m 2 is generally considered overweight, while obesity is considered to be a BMI ≥ 30 kg/m 2 . It is well known that obesity and overweight are a growing problem globally with high rates in both developed and developing countries (Capodaglio & Liuzzi, 2013 ; WHO, 2016a , 2016b ).
In the United States in 2015, all states had an obesity prevalence more than 20%, 25 states and Guam had obesity rates >30% and four of those 25 states (Alabama, Louisiana, Mississippi, and West Virginia) had rates >35% (Centres for Disease Control and Prevention, 2016 ; Figure Figure1). 1 ). Approximately 35% and 37% of adult men and women, respectively, in the United States have obesity (Yang & Colditz, 2015 ). Adult obesity is most common in non‐Hispanic black Americans, followed by Mexican Americans, and non‐Hispanic white Americans (Yang & Colditz, 2015 ). Individuals are also getting heavier at a younger age; birth cohorts from 1966 to 1975 and 1976 to 1985 reached an obesity prevalence of ≥20% by 20–29 years of age, while the 1956–1965 cohort only reached this prevalence by age 30–39 years (Lee et al., 2010 ). Additionally, the prevalence of childhood obesity in 2‐ to 17‐year‐olds in the United States has increased from 14.6% in 1999–2000 to 17.4% in 2013–2014 (Skinner & Skelton, 2014 ). Childhood obesity is an increasing health issue because of the early onset of comorbidities that have major adverse health impacts, and the increased likelihood of children with obesity going on to become adults with obesity (50% risk vs. 10% for children without obesity; Whitaker, Wright, Pepe, Seidel, & Dietz, 1997 ).

U.S. obesity epidemic 2015.
Source . Figure adapted from Centers for Disease Control and Prevention (CDC). Retrieved from https://www.cdc.gov/obesity/data/prevalence-maps.html .
Association of obesity with mortality and comorbid disease
Obesity is associated with a significant increase in mortality, with a life expectancy decrease of 5–10 years (Berrington de Gonzalez et al., 2010 ; Kuk et al., 2011 ; Prospective Studies Collaboration et al., 2009 ). There is evidence to indicate that all‐cause, CVD‐associated, and cancer‐associated mortalities are significantly increased in individuals with obesity, specifically those at Stages 2 or 3 of the Edmonton Obesity Staging System (EOSS; Kuk et al., 2011 ; Figure Figure2). 2 ). Mortality related to cancer is, however, also increased at Stage 1, when the physical symptoms of obesity are marginal (Figure (Figure2). 2 ). Recently, a large‐scale meta‐analysis that included studies that had enrolled over 10 million individuals, indicated that, relative to the reference category of 22.5 to <25 kg/m 2 , the hazard ratio (HR) for all‐cause mortality rose sharply with increasing BMI (The Global BMI Mortality Collaboration, 2016 ). For a BMI of 25.0 to <30.0 kg/m 2 , the HR was 1.11 (95% confidence interval [CI] 1.10, 1.11), and this increased to 1.44 (1.41, 1.47), 1.92 (1.86, 1.98), and 2.71 (2.55, 2.86) for a BMI of 30.0 to <35.0, 35.0 to <40.0, and 40.0 to <60.0 kg/m 2 , respectively.

Association between EOSS stage and risk of all‐cause (A), CVD (B), cancer (C), and non‐CVD or noncancer mortality (D) in men and women. © 2011.
Source . Reproduced with permission from NRC Research Press, from Kuk et al. ( 2011 ). CVD, cardiovascular disease; NW, normal weight.
Comorbidities
Obesity is a chronic disease that is associated with a wide range of complications affecting many different aspects of physiology (Dobbins, Decorby, & Choi, 2013 ; Guh et al., 2009 ; Martin‐Rodriguez, Guillen‐Grima, Marti, & Brugos‐Larumbe, 2015 ; summarized in Table Table1). 1 ). To examine these obesity‐related morbidities in detail is beyond the scope of this review and therefore only a brief overview of some of the key pathophysiological processes is included next.
Morbidities associated with obesity (Hamdy, 2016 ; Petry, Barry, Pietrzak, & Wagner, 2008 ; Pi‐Sunyer, 2009 ; Sakai et al., 2005 ; Smith, Hulsey, & Goodnight, 2008 ; Yosipovitch, DeVore, & Dawn, 2007 )
| Class of event | Comorbidities associated with obesity |
|---|---|
| Cancer/malignancy | Postmenopausal breast, endometrial, colon and rectal, gallbladder, prostate, ovarian, endometrial renal cell, esophageal adenocarcinoma, pancreatic, and kidney cancer |
| Cardiovascular | Coronary artery disease, obesity‐associated cardiomyopathy, essential hypertension, left ventricular hypertrophy, cor pulmonale, accelerated atherosclerosis, pulmonary hypertension of obesity, dyslipidemia, chronic heart failure (CHD), left ventricular hypertrophy (LVH), cardiomyopathy, pulmonary hypertension, lymphedema (legs) |
| Gastrointestinal (GI) | Gall bladder disease (cholecystitis, cholelithiasis), gastroesophageal reflux disease (GERD), reflux esophagitis, nonalcoholic steatohepatitis (NASH), nonalcoholic fatty liver disease (NAFLD), fatty liver infiltration, acute pancreatitis |
| Genitourinary | Stress incontinence |
| Metabolic/endocrine | Type 2 diabetes mellitus, prediabetes, metabolic syndrome, insulin resistance, and dyslipidemia |
| Musculoskeletal/orthopedic | Pain in back, hips, ankles, feet and knees; osteoarthritis (especially in the knees and hips), plantar fasciitis, back pain, coxavera, slipped capital femoral epiphyses, Blount disease and Legg‐Calvé‐Perthes disease, and chronic lumbago |
| Neurological and central nervous system (CNS) | Stroke, dementia idiopathic intracranial hypertension, and meralgia paresthesia |
| Obstetric and perinatal | Pregnancy‐related hypertension, fetal macrosomia, very low birthweight, neural tube defects, preterm birth, increased cesarean delivery, increased postpartum infection and pelvic dystocia, preeclampsia, hyperglycemia, gestational diabetes (GDM) |
| Skin | Keratosis pilaris, hirsutism, acanthosis nigricans, and acrochondons, psoriasis, intertrigo (bacterial and/or fungal), and increased risk for cellulitis, venous stasis ulcers, necrotizing fasciitis, and carbuncles |
| Psychological | Depression, anxiety, personality disorder, and obesity stigmatization |
| Respiratory/pulmonary | Obstructive sleep apnea (OSA), Pickwickian syndrome (obesity hypoventilation syndrome), higher rates of respiratory infections, asthma, hypoventilation, pulmonary emboli risk |
| Surgical | Increased surgical risk and postoperative complications, deep venous thrombosis, including wound infection, pulmonary embolism, and postoperative pneumonia |
| Reproductive (Women) | Anovulation, early puberty, polycystic ovaries, infertility, hyperandrogenism, and sexual dysfunction |
| Reproductive (Men) | Hypogonadotropic hypogonadism, polycystic ovary syndrome (PCOS), decreased libido, and sexual dysfunction |
| Extremities | Venous varicosities, lower extremity venous and/or lymphatic edema |
The progression from lean state to obesity brings with it a phenotypic change in adipose tissue and the development of chronic low‐grade inflammation (Wensveen, Valentic, Sestan, Turk Wensveen, & Polic, 2015 ). This is characterized by increased levels of circulating free‐fatty acids, soluble pro‐inflammatory factors (such as interleukin [IL] 1β, IL‐6, tumor necrosis factor [TNF] α, and monocyte chemoattractant protein [MCP] 1) and the activation and infiltration of immune cells into sites of inflammation (Hursting & Dunlap, 2012 ). Obesity is also usually allied to a specific dyslipidemia profile (atherogenic dyslipidemia) that includes small, dense low‐density lipoprotein (LDL) particles, decreased levels of high‐density lipoprotein (HDL) particles, and raised triglyceride levels (Musunuru, 2010 ). This chronic, low‐grade inflammation and dyslipidemia profile leads to vascular dysfunction, including atherosclerosis formation, and impaired fibrinolysis. These, in turn, increase the risk for CVD, including stroke and venous thromboembolism (Blokhin & Lentz, 2013 ).
The metabolic and cardiovascular aspects of obesity are closely linked. The chronic inflammatory state associated with obesity is established as a major contributing factor for insulin resistance, which itself is one of the key pathophysiologies of T2D (Johnson, Milner, & Makowski, 2012 ). Furthermore, central obesity defined by waist circumference is the essential component of the International Diabetes Federation (IDF) definition of the metabolic syndrome (raised triglycerides, reduced HDL cholesterol, raised blood pressure, and raised fasting plasma glucose; International Diabetes Federation, 2006 ).
Obesity is also closely associated with OSA. To start, a number of the conditions associated with obesity such as insulin resistance (Ip et al., 2002 ), systemic inflammation, and dyslipidemia are themselves closely associated with OSA, and concurrently, the obesity‐associated deposition of fat around the upper airway and thorax may affect lumen size and reduce chest compliance that contributes to OSA (Romero‐Corral, Caples, Lopez‐Jimenez, & Somers, 2010 ).
The development of certain cancers, including colorectal, pancreatic, kidney, endometrial, postmenopausal breast, and adenocarcinoma of the esophagus to name a few, have also been shown to be related to excess levels of fat and the metabolically active nature of this excess adipose tissue (Booth, Magnuson, Fouts, & Foster, 2015 ; Eheman et al., 2012 ). Cancers have shown to be impacted by the complex interactions between obesity‐related insulin resistance, hyperinsulinemia, sustained hyperglycemia, oxidative stress, inflammation, and the production of adipokines (Booth et al., 2015 ). The wide range of morbidities associated with obesity represents a significant clinical issue for individuals with obesity. However, as significant as this array of risk factors is for patient health, the risk factors can be positively modified with weight loss.
Obesity‐related morbidities in children and adolescents
As was referred to earlier, children and adolescents are becoming increasingly affected by obesity. This is particularly concerning because of the long‐term adverse consequences of early obesity. Obesity adversely affects the metabolic health of young people and can result in impaired glucose tolerance, T2D, and early‐onset metabolic syndrome (Pulgaron, 2013 ).There is also strong support in the literature for relationships between childhood obesity and asthma, poor dental health (caries), nonalcoholic fatty liver disease (NAFLD), and gastroesophageal reflux disease (GERD; Pulgaron, 2013 ). Obesity can also affect growth and sexual development and may delay puberty in boys and advance puberty in some girls (Burt Solorzano & McCartney, 2010 ). Childhood obesity is also associated with hyperandrogenism and polycystic ovary syndrome (PCOS) in girls (Burt Solorzano & McCartney, 2010 ). Additionally, obesity is associated with psychological problems in young people including attention deficit hyperactivity disorder (ADHD), anxiety, depression, poor self‐esteem, and problems with sleeping (Pulgaron, 2013 ).
Modest weight loss and its long‐term maintenance: Benefits and risks
Guidelines endorse weight‐loss targets of 5%–10% in individuals with obesity or overweight with associated comorbidities, as this has been shown to significantly improve health‐related outcomes for many obesity‐related comorbidities (Cefalu et al., 2015 ; Figure Figure3), 3 ), including T2D prevention, and improvements in dyslipidemia, hyperglycemia, osteoarthritis, stress incontinence, GERD, hypertension, and PCOS. Further benefits may be evident with greater weight loss, particularly for dyslipidemia, hyperglycemia, and hypertension. For NAFLD and OSA, at least 10% weight loss is required to observe clinical improvements (Cefalu et al., 2015 ).

Benefits of modest weight loss. Lines demonstrate the ranges in which weight loss has been investigated and shown to have clinical benefits. Arrows indicate that additional benefits may be seen with further weight loss.
Source . Figure adapted from Cefalu et al. ( 2015 ).
Importantly, the weight‐loss benefits in terms of comorbidities are also reflected in improved all‐cause mortality. A recent meta‐analysis of 15 studies demonstrated that relatively small amounts of weight loss, on average 5.5 kg in the treatment arm versus 0.2 kg with placebo from an average baseline BMI of 35 kg/m 2 , resulted in a substantial 15% reduction in all‐cause mortality (Kritchevsky et al., 2015 ).
Cardiovascular health
Weight loss is associated with beneficial changes in several cardiovascular risk markers, including dyslipidemia, pro‐inflammatory/pro‐thrombotic mediators, arterial stiffness, and hypertension (Dattilo & Kris‐Etherton, 1992 ; Dengo et al., 2010 ; Goldberg et al., 2014 ; Haffner et al., 2005 ; Ratner et al., 2005 ). Importantly, weight loss was found to reduce the risk for CVD mortality by 41% up to 23 years after the original weight‐loss intervention (Li et al., 2014 ; Figure Figure4). 4 ). Evidence including the biological effects of obesity and weight loss, and the increased risk for stroke with obesity indicates that weight loss may be effective for primary‐ and secondary‐stroke prevention (Kernan, Inzucchi, Sawan, Macko, & Furie, 2013 ).

Reduction in cardiovascular mortality with modest weight reduction. Cumulative incidence of CVD mortality during 23 years of follow‐up in the Da Qing study (Li et al., 2014 ). Figure © 2014 Elsevier.
Source . Reproduced with permission from Li et al. ( 2014 ).
Type 2 diabetes
Three major long‐term studies, the Diabetes Prevention Program (DPP), the Diabetes Prevention Study (DPS), and the Da Qing IGT and Diabetes (Da Qing) study, have demonstrated that modest weight loss through short‐term lifestyle or pharmacologic interventions can reduce the risk for developing T2D by 58%, 58%, and 31%, respectively, in individuals with obesity and prediabetes (DPP Research Group et al., 2009 ; Pan et al., 1997 ; Tuomilehto et al., 2001 ). Long‐term benefits were maintained following the interventions; for example, in the DPP, the risk reduction of developing T2D versus placebo was 34% at 10 years and 27% at 15 years following the initial weight‐loss intervention (DPP Research Group, 2015 ; DPP Research Group et al., 2009 ). Weight loss increased the likelihood of individuals reverting from prediabetes to normoglycemia (DPP Research Group et al., 2009 ; Li et al., 2008 ; Lindstrom et al., 2003 , 2006 ; Tuomilehto et al., 2001 ), and also improved other aspects of glycemic control including fasting and postprandial glucose, and insulin sensitivity (Haufe et al., 2013 ; Li et al., 2008 ).
Sleep apnea
Data indicate that weight loss is beneficial, although not curative, in patients with obesity who experience OSA. Meta‐analyses of patients who underwent treatment with either intensive lifestyle intervention (Araghi et al., 2013 ) or bariatric surgery (Greenburg, Lettieri, & Eliasson, 2009 ) demonstrated improvements in apnea‐hypopnea index (AHI) following treatment. In the first of these meta‐analyses, in randomized controlled trials, lifestyle intervention lead to a mean reduction in BMI of 2.3 kg/m 2 , which was associated with a decrease in mean AHI of 6.0 events/h. As expected, weight loss was much higher in the second meta‐analysis that investigated the effect of bariatric surgery on measures of OSA, and this was associated with greater reductions in AHI; the mean BMI reduction of 17.9 kg/m 2 resulted in AHI events being reduced by a mean of 38.2 events/h. Once these improvements in AHI have occurred, they seem to persist for some time, irrespective of a certain degree of weight regain. In one study, an initial mean weight loss of 10.7 kg resulted in a persistent improvement in AHI over a 4‐year period despite weight regain of approximately 50% by Year 4 (Kuna et al., 2013 ).
Intentional weight loss of >9 kg reduced the risk for a range of cancers including breast, endometrium, and colon in the large‐scale Iowa Women's Health Study (Parker & Folsom, 2003 ). The overall reduction in the incidence rate of any cancer was 11% (relative risk, 0.89; 95% CI 0.79, 1.00) for participants who lost more than 9 kg compared with those who did not achieve a more than 9 kg weight loss episode. Additionally, weight loss in participants with obesity has been established to be associated with reductions in cancer biomarkers including soluble E‐selectin and IL‐6 (Linkov et al., 2012 ).
Additional health benefits
The substantial weight loss associated with bariatric surgery has been shown to improve asthma with a 48%–100% improvement in symptoms and reduction in medication use (Juel, Ali, Nilas, & Ulrik, 2012 ); however, there is a potential threshold effect so that modest weight loss of 5%–10% may lead to clinical improvement (Lv, Xiao, & Ma, 2015 ). Similarly, modest weight loss of 5%–10% improves GERD (Singh et al., 2013 ) and liver function (Haufe et al., 2013 ). A study utilizing MRI scanning to examine the effects of weight loss on NAFLD has reported a reduction in liver fat from 18.3% to 13.6% ( p = .03), a relative reduction of 25% (Patel et al., 2015 ). Taking an active role in addressing obesity through behavioral modifications or exercise can also reduce the symptoms of depression (Fabricatore et al., 2011 ), improve urinary incontinence in men and women (Breyer et al., 2014 ; Brown et al., 2006 ), and improve fertility outcomes in women (Kort, Winget, Kim, & Lathi, 2014 ). Additionally, weight loss can reduce the joint‐pain symptoms and disability caused by weight‐related osteoarthritis (Felson, Zhang, Anthony, Naimark, & Anderson, 1992 ; Foy et al., 2011 ).
Mitigating risks
Despite the array of benefits, weight loss can also be linked with certain risks that may need to be managed. One such example is the risk for gallstones with rapid weight loss, which is associated with gallstone formation in 30%–71% of individuals. Gallstone formation is particularly associated with bariatric surgery when weight loss exceeds 1.5 kg/week and occurs particularly within the first 6 weeks following surgery when weight loss is greatest. Slower rates of weight loss appear to mitigate the risk for gallstone formation compared to the general population but may not eliminate it entirely; as was noted in the year‐long, weight‐loss, SCALE trial that compared liraglutide 3.0 mg daily use to placebo and resulted in gallstone formation in 2.5% of treated subjects compared to 1% of subjects taking placebo. For this reason, the risk for cholethiasis should be considered when formulating weight‐loss programs (Weinsier & Ullmann, 1993 ).
Strategies to help individuals achieve and maintain weight loss
Rogge and Gautam have covered the biology of obesity and weight regain within another section of this supplement (Rogge & Gautam, 2017 ), so here we focus on some of the clinical strategies for delivering weight loss and weight loss maintenance lifestyle programs. Structured lifestyle support plays an important role in successful weight management. A total of 34% of participants receiving structured lifestyle support from trained‐nursing staff achieved weight loss of ≥5% over 12 weeks compared with approximately 19% with usual care (Nanchahal et al., 2009 ). This particular structured program, delivered in a primary healthcare setting, included initial assessment and goal setting, an eating plan and specific lifestyle goals, personalized activity program, and advice about managing obstacles to weight loss. Additionally, data from the National Weight Control Registry (NWCR), which is the longest prospective compilation of data from individuals who have successfully lost weight and maintained their weight loss, confirm expectations that sustained changes to both diet and activity levels are central to successful weight management (Table (Table2). 2 ). Therefore, an understanding of different clinical strategies for delivery‐structured support is essential for the nurse practitioner.
Lifestyle factors associated with achieving and maintaining weight loss
| Action | Percentage |
|---|---|
| Modified food intake | 98 |
| Increased physical activity | 94 |
| Exercised on average for 1 h each day | 90 |
| Ate breakfast every day | 78 |
| Weighed themselves weekly | 75 |
| Watched less than 10 h of television weekly | 62 |
| Lost weight with the help of a weight‐loss program | 55 |
Note . Data from (NWCR, 2016 ).
a Walking was the most common activity undertaken.
Realistic weight‐loss targets
From the outset, a patient's estimate of their achievable weight loss may be unrealistic. Setting realistic weight‐loss goals is often difficult because of misinformation from a variety of sources, including friends, media, and other healthcare professionals (Osunlana et al., 2015 ). Many individuals with obesity or overweight have unrealistic goals of 20%–30% weight loss, whereas a more realistic goal would be the loss of 5%–15% of the initial body weight (Fabricatore et al., 2007 ). Promoting realistic weight‐loss expectations for patients was identified as a key difficulty for nurse practitioners, primary care nurses, dieticians, and mental health workers (Osunlana et al., 2015 ). Visual resources showing the health and wellness benefit of modest weight loss may thus be helpful (Osunlana et al., 2015 ). Healthcare practitioners should focus on open discussion about, and re‐enforcement of, realistic weight‐loss goals and assess outcomes consistently according to those goals (Bray, Look, & Ryan, 2013 ).
Maintaining a food diary
The 2013 White Paper from the American Nurse Practitioners Foundation on the Prevention and Treatment of Obesity considers a food diary as an important evidence‐based nutritional intervention in aiding weight loss (ANPF). Consistent and regular recording in a food diary was significantly associated with long‐term weight‐loss success in a group of 220 women (Peterson et al., 2014 ). This group lost a mean of 10.4% of their initial body weight through a 6‐month group‐based weight‐management program and then regained a mean of 2.3% over a 12‐month follow‐up period, during which participants received bimonthly support in person, by telephone, or by e‐mail (Peterson et al., 2014 ). Over the 12‐month follow‐up, women who self‐monitored consistently (≥50% of the extended‐care year) had a mean weight loss of 0.98%, while those who were less consistent (<50%) gained weight (5.1%; p < .01). Therefore, frequent and consistent food monitoring should be encouraged, particularly in the weight‐maintenance phase of any program.
Motivating and supporting patients
Motivational interviewing is a technique that focuses on enhancing intrinsic motivation and behavioral changes by addressing ambivalence (Barnes & Ivezaj, 2015 ). Interviews focus on “change talk,” including the reasons for change and optimism about the intent for change in a supportive and nonconfrontational setting, and may help individuals maintain behavioral changes.
For patients that have achieved weight loss, the behavioral factors associated with maintaining weight loss include strong social support networks, limiting/avoiding disinhibited eating, avoiding binge eating, avoiding eating in response to stress or emotional issues, being accountable for one's decisions, having a strong sense of autonomy, internal motivation, and self‐efficacy (Grief & Miranda, 2010 ). Therefore, encouraging feelings of “self‐worth” or “self‐efficacy” can help individuals to view weight loss as being within their own control and achievable (Cochrane, 2008 ).
Strengthening relationships with patients with overweight or obesity to enhance trust may also improve adherence with weight‐loss programs. Patients with hypertension who reported having “complete trust” in their healthcare practitioner were more than twice as likely to engage in lifestyle changes to lose weight than those who lacked “complete trust” (Jones, Carson, Bleich, & Cooper, 2012 ). It may be prudent to ensure the healthcare staff implementing weight‐loss programs have sufficient time to foster trust with their patients.
Continued support from healthcare staff may help patients sustain the necessary motivation for lifestyle changes. A retrospective analysis of 14,256 patients in primary care identified consultation frequency as a factor that can predict the success of weight‐management programs (Lenoir, Maillot, Guilbot, & Ritz, 2015 ). Individuals who successfully maintained ≥10% weight loss over 12 months visited the healthcare provider on average 0.65 times monthly compared with an average of 0.48 visits/month in those who did not maintain ≥10% weight loss, and 0.39 visits/month in those who failed to achieve the initial ≥10% weight loss ( p < .001; Lenoir et al., 2015 ).
Educational and environmental factors
It is important to consider a patient's education and environment when formulating a weight loss strategy as environmental factors may need to be challenged to help facilitate weight loss. A family history of obesity and childhood obesity are strongly linked to adult obesity, which is likely to be because of both genetic and behavioral factors (Kral & Rauh, 2010 ). Parents create their child's early food experiences and influence their child's attitudes to eating through learned eating habits and food choices (Kral & Rauh, 2010 ). Families can also impart cultural preferences for less healthy food choices and family food choices may be affected by community factors, such as the local availability and cost of healthy food options (Castro, Shaibi, & Boehm‐Smith, 2009 ). Alongside this, genetic variation in taste sensation may influence the dietary palate and influence food choices (Loper, La Sala, Dotson, & Steinle, 2015 ). For example, sensitivity to 6‐n‐propylthiouracil (PROP) is genetically determined, and PROP‐tasting ability ranges from super taster to nontaster. When offered buffet‐style meals over 3 days, PROP nontasters consumed more energy, and a greater proportion of energy from fat compared with super tasters. So it is possible that a family's genetic profile could contribute to eating choices. To address behavioral factors, it is important to ensure that families have appropriate support and information and that any early signs of weight gain are dealt with promptly.
A healthy home food environment can help individuals improve their diet. In children, key factors are availability of fresh fruit and vegetables at home and parental influence through their own fresh fruit and vegetable intake (Wyse, Wolfenden, & Bisquera, 2015 ). In adults, unhealthy home food environment factors include less healthy food in the home and reliance on fast food ( p = .01) are all predictors of obesity (Emery et al., 2015 ).
Family mealtimes are strongly associated with better dietary intake and a randomized controlled trial to encourage healthy family meals showed a promising reduction in excess weight gain in prepubescent children (Fulkerson et al., 2015 ). Another study showed that adolescents with any level of baseline family meal frequency, 1–2, 3–4, and ≥5 family meals/week, had reduced odds of being affected by overweight or obesity 10 years later than adolescents who never ate family meals (Berge et al., 2015 ). Community health advocates have identified the failure of many families to plan meals or prepare food as a barrier to healthy family eating patterns (Fruh, Mulekar, Hall, Fulkerson et al., 2013 ). Meal planning allows healthy meals to be prepared in advance and frozen for later consumption (Fruh, Mulekar, Hall, Adams et al., 2013 ) and is associated with increased consumption of vegetables and healthier meals compared with meals prepared on impulse (Crawford, Ball, Mishra, Salmon, & Timperio, 2007 ; Hersey et al., 2001 ).
The role of the nurse practitioner
The initial and ongoing interactions between patient and nurse practitioner are keys for the determination of an effective approach and implementation of a weight loss program and subsequent weight maintenance. The initial interaction can be instigated by either the nurse practitioner or the patient and once the decision has been made to manage the patient's weight, the evaluation includes a risk assessment, a discussion about the patient's weight, and treatment goal recommendations (American Nurse Practitioner Foundation, 2013 ). Across this process, it may be advantageous to approach this using objective data and language that is motivational and/or nonjudgmental. Patients may struggle with motivation, and therefore, ongoing discussions around the health benefits and improvements to quality of life as a result of weight loss may be required (American Nurse Practitioner Foundation, 2013 ). It may be valuable to allocate personalized benefits to the weight loss such as playing with children/grandchildren (American Nurse Practitioner Foundation, 2013 ). Treatment approaches encompass nonpharmacological and pharmacological strategies; however, it is important to remember that any pharmacological agent used should be used as an adjunct to nutritional and physical activity strategies (American Nurse Practitioner Foundation, 2013 ). Pharmacotherapy options for weight management are discussed further in the article by Golden in this supplement.
Conclusions/summary
The importance of obesity management is underscored both by the serious health consequences for individuals, but also by its increasing prevalence globally, and across age groups in particular. Obesity promotes a chronic, low‐grade, inflammatory state, which is associated with vascular dysfunction, thrombotic disorders, multiple organ damage, and metabolic dysfunction. These physiological effects ultimately lead to the development of a range of morbidities, including CVD, T2D, OSA, and certain cancers along with many others, as well as causing a significant impact on mortality.
However, even modest weight loss of 5%–10% of total body weight can significantly improve health and well‐being, and further benefits are possible with greater weight loss. Weight loss can help to prevent development of T2D in individuals with obesity and prediabetes and has a positive long‐term impact on cardiovascular mortality. Beneficial, although not curative, effects have also been noted on OSA following >10% weight loss. In addition, weight loss reduces the risk for certain cancer types and has positive effects on most comorbidities including asthma, GERD, liver function, urinary incontinence, fertility, joint pain, and depression.
Weight‐loss programs that include realistic weight loss goals, frequent check‐in, and meal/activity diaries may help individuals to lose weight. Setting realistic weight‐loss goals can be difficult; however, visual resources showing the health and wellness benefit of weight loss may be helpful in discussing realistic goals, and help motivate the patient in maintaining the weight loss. Techniques such as motivational interviewing that focus on addressing resistance to behavioral change in a supportive and optimistic manner may help individuals in integrating these changes to allow them to become part of normal everyday life and thus help with maintaining the weight loss. Positive reinforcement in terms of marked early‐weight loss may also assist in improving adherence, so this should be a key goal for weight‐loss programs. Encouraging feelings of “self‐worth” or “self‐efficacy” can help individuals to view weight loss as being within their own control.
Nurse practitioners play a major role in helping patients achieve weight loss through all aspects of the process including assessment, support, motivation, goal‐setting, management, and treatment. With their in‐depth understanding of the research in the field of obesity and weight management, nurse practitioners are well placed to effect meaningful changes in the weight‐management strategies deployed in clinical practice.
List of helpful resources
| The Obesity Action Coalition (OAC): | This site has educational resources for providers and patients. It also has information on advocacy for patients. |
| Stop Obesity Alliance: | This site has many helpful resources to help prevent obesity bias and helpful educational materials for patients. It also has an excellent tool to help providers discuss the topic of obesity with patients. |
| UConn Rudd Center: | This site is an excellent resource for providers in clinical practice. This site has modules to help providers improve obesity management. |
Acknowledgments
The authors are grateful to Watermeadow Medical for writing assistance in the development of this manuscript. This assistance was funded by Novo Nordisk, who also had a role in the review of the manuscript for scientific accuracy. The author discussed the concept, drafted the outline, commented in detail on the first iteration, made critical revision of later drafts, and has revised and approved the final version for submission.
Dr. Sharon Fruh serves on the Novo Nordisk Obesity Speakers Bureau. In compliance with national ethical guidelines, the author reports no relationship with business or industry that would post a conflict of interest.
Writing and editorial support was provided by Watermeadow Medical, and funded by Novo Nordisk.
The copyright line in this article was changed on 9 August 2018 after online publication.
- American Nurse Practitioner Foundation . (2013). Nurse practitioners and the prevention and treatment of adult obesity—A White Paper of the American Nurse Practitioner Foundation (electronic version) . Summer. Retrieved from https://international.aanp.org/Content/docs/ObesityWhitePaper.pdf
- Araghi, M. H. , Chen, Y. F. , Jagielski, A. , Choudhury, S. , Banerjee, D. , Hussain, S. , … Taheri, S. , et al. (2013). Effectiveness of lifestyle interventions on obstructive sleep apnea (OSA): Systematic review and meta‐analysis . Sleep , 36 ( 10 ), 1553–1562, 1562a–1562e. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Barnes, R. D. , & Ivezaj, V. (2015). A systematic review of motivational interviewing for weight loss among adults in primary care . Obesity Reviews , 16 ( 4 ), 304–318. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Berge, J. M. , Wall, M. , Hsueh, T. F. , Fulkerson, J. A. , Larson, N. , & Neumark‐Sztainer, D. (2015). The protective role of family meals for youth obesity: 10‐year longitudinal associations . Journal of Pediatrics , 166 ( 2 ), 296–301. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Berrington de Gonzalez, A. , Hartge, P. , Cerhan, J. R. , Flint, A. J. , Hannan, L. , MacInnis, R. J. , … Thun, M. J. , et al. (2010). Body‐mass index and mortality among 1.46 million white adults . New England Journal of Medicine , 363 ( 23 ), 2211–2219. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Blokhin, I. O. , & Lentz, S. R. (2013). Mechanisms of thrombosis in obesity . Current Opinion in Hematology , 20 ( 5 ), 437–444 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Booth, A. , Magnuson, A. , Fouts, J. , & Foster, M. (2015). Adipose tissue, obesity and adipokines: Role in cancer promotion . Hormone Molecular Biology and Clinical Investigation , 21 ( 1 ), 57–74. [ PubMed ] [ Google Scholar ]
- Bray, G. , Look, M. , & Ryan, D. (2013). Treatment of the obese patient in primary care: Targeting and meeting goals and expectations . Postgraduate Medical Journal , 125 ( 5 ), 67–77. [ PubMed ] [ Google Scholar ]
- Breyer, B. N. , Phelan, S. , Hogan, P. E. , Rosen, R. C. , Kitabchi, A. E. , Wing, R. R. , … the Look AHEAD Research Group , et al. (2014). Intensive lifestyle intervention reduces urinary incontinence in overweight/obese men with type 2 diabetes: Results from the Look AHEAD trial . Journal of Urology , 192 ( 1 ), 144–149. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Brown, J. S. , Wing, R. , Barrett‐Connor, E. , Nyberg, L. M. , Kusek, J. W. , Orchard, T. J. , … Diabetes Prevention Program Research Group , et al. (2006). Lifestyle intervention is associated with lower prevalence of urinary incontinence: The Diabetes Prevention Program . Diabetes Care , 29 ( 2 ), 385–390. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Burt Solorzano, C. M. , & McCartney, C. R. (2010). Obesity and the pubertal transition in girls and boys . Reproduction , 140 ( 3 ), 399–410. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Capodaglio, P. , & Liuzzi, A. (2013). Obesity: A disabling disease or a condition favoring disability ? European Journal of Physical and Rehabilitation Medicine , 49 ( 3 ), 395–398. [ PubMed ] [ Google Scholar ]
- Castro, F. G. , Shaibi, G. Q. , & Boehm‐Smith, E. (2009). Ecodevelopmental contexts for preventing type 2 diabetes in Latino and other racial/ethnic minority populations . Journal of Behavioral Medicine , 32 ( 1 ), 89–105. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Cefalu, W. T. , Bray, G. A. , Home, P. D. , Garvey, W. T. , Klein, S. , Pi‐Sunyer, F. X. , … Ryan, D. H. , et al. (2015). Advances in the science, treatment, and prevention of the disease of obesity: Reflections from a diabetes care editors' expert forum . Diabetes Care , 38 ( 8 ), 1567–1582. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Centres for Disease Control and Prevention . (2016). Overweight and obesity . Retrieved from https://www.cdc.gov/obesity/
- Cochrane, G. (2008). Role for a sense of self‐worth in weight‐loss treatments: Helping patients develop self‐efficacy . Canadian Family Physician , 54 ( 4 ), 543–547. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Crawford, D. , Ball, K. , Mishra, G. , Salmon, J. , & Timperio, A. (2007). Which food‐related behaviours are associated with healthier intakes of fruits and vegetables among women ? Public Health Nutrition , 10 ( 3 ), 256–265. [ PubMed ] [ Google Scholar ]
- Dattilo, A. M. , & Kris‐Etherton, P. M. (1992). Effects of weight reduction on blood lipids and lipoproteins: A meta‐analysis . American Journal of Clinical Nutrition , 56 ( 2 ), 320–328. [ PubMed ] [ Google Scholar ]
- Dengo, A. L. , Dennis, E. A. , Orr, J. S. , Marinik, E. L. , Ehrlich, E. , Davy, B. M. , & Davy, K. P. (2010). Arterial destiffening with weight loss in overweight and obese middle‐aged and older adults . Hypertension , 55 ( 4 ), 855–861. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Diabetes Prevention Program ( DPP) Research Group . (2015). Long‐term effects of lifestyle intervention or metformin on diabetes development and microvascular complications over 15‐year follow‐up: The Diabetes Prevention Program Outcomes Study . Lancet Diabetes & Endocrinology , 3 ( 11 ), 866–875. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Diabetes Prevention Program ( DPP) Research Group , Knowler, W. C. , Fowler, S. E. , Hamman, R. F. , Christophi, C. A. , Hoffman, H. J. , … Nathan, D. M. , et al. (2009). 10‐year follow‐up of diabetes incidence and weight loss in the Diabetes Prevention Program Outcomes Study . Lancet , 374 ( 9702 ), 1677–1686. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Dobbins, M. , Decorby, K. , & Choi, B. C. (2013). The association between obesity and cancer risk: A meta‐analysis of observational studies from 1985 to 2011 . ISRN Preventive Medicine , 2013 , 680536 10.5402/2013/680536. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Eheman, C. , Henley, S. J. , Ballard‐Barbash, R. , Jacobs, E. J. , Schymura, M. J. , Noone, A. M. , … Edwards, B. K. , et al. (2012). Annual Report to the Nation on the status of cancer, 1975–2008, featuring cancers associated with excess weight and lack of sufficient physical activity . Cancer , 118 ( 9 ), 2338–2366. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Emery, C. F. , Olson, K. L. , Lee, V. S. , Habash, D. L. , Nasar, J. L. , & Bodine, A. (2015). Home environment and psychosocial predictors of obesity status among community‐residing men and women . International Journal of Obesity , 39 ( 9 ), 1401–1407. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Fabricatore, A. N. , Wadden, T. A. , Higginbotham, A. J. , Faulconbridge, L. F. , Nguyen, A. M. , Heymsfield, S. B. , & Faith, M. S. (2011). Intentional weight loss and changes in symptoms of depression: A systematic review and meta‐analysis . International Journal of Obesity , 35 ( 11 ), 1363–1376. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Fabricatore, A. N. , Wadden, T. A. , Womble, L. G. , Sarwer, D. B. , Berkowitz, R. I. , Foster, G. D. , & Brock, J. R. (2007). The role of patients' expectations and goals in the behavioral and pharmacological treatment of obesity . International Journal of Obesity , 31 ( 11 ), 1739–1745. [ PubMed ] [ Google Scholar ]
- Felson, D. T. , Zhang, Y. , Anthony, J. M. , Naimark, A. , & Anderson, J. J. (1992). Weight loss reduces the risk for symptomatic knee osteoarthritis in women. The Framingham Study . Annals of Internal Medicine , 116 ( 7 ), 535–539. [ PubMed ] [ Google Scholar ]
- Foy, C. G. , Lewis, C. E. , Hairston, K. G. , Miller, G. D. , Lang, W. , Jakicic, J. M. , … the Look AHEAD Research Group , et al. (2011). Intensive lifestyle intervention improves physical function among obese adults with knee pain: Findings from the Look AHEAD trial . Obesity (Silver Spring) , 19 ( 1 ), 83–93. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Fruh, S. M. , Mulekar, M. S. , Hall, H. R. , Adams, J. R. , Lemley, T. , Evans, B. , & Dierking, J. (2013). Meal‐planning practices with individuals in health disparity zip codes . Journal for Nurse Practitioners , 9 ( 6 ), 344–349. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Fruh, S. M. , Mulekar, M. S. , Hall, H. R. , Fulkerson, J. A. , Hanks, R. S. , Lemley, T. , … Dierking, J. , et al. (2013). Perspectives of community health advocates: Barriers to healthy family eating patterns . Journal for Nurse Practitioners , 9 ( 7 ), 416–421. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Fulkerson, J. A. , Friend, S. , Flattum, C. , Horning, M. , Draxten, M. , Neumark‐Sztainer, D. , … Kubik, M. , et al. (2015). Promoting healthful family meals to prevent obesity: HOME Plus, a randomized controlled trial . International Journal of Behavioral Nutrition and Physical Activity , 12 , 154. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Goldberg, R. B. , Temprosa, M. G. , Mather, K. J. , Orchard, T. J. , Kitabchi, A. E. , & Watson, K. E. , for the Diabetes Prevention Program Research Group . (2014). Lifestyle and metformin interventions have a durable effect to lower CRP and tPA levels in the diabetes prevention program except in those who develop diabetes . Diabetes Care , 37 ( 8 ), 2253–2260. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Greenburg, D. L. , Lettieri, C. J. , & Eliasson, A. H. (2009). Effects of surgical weight loss on measures of obstructive sleep apnea: A meta‐analysis . American Journal of Medicine , 122 ( 6 ), 535–542. [ PubMed ] [ Google Scholar ]
- Grief, S. N. , & Miranda, R. L. (2010). Weight loss maintenance . American Family Physician , 82 ( 6 ), 630–634. [ PubMed ] [ Google Scholar ]
- Guh, D. P. , Zhang, W. , Bansback, N. , Amarsi, Z. , Birmingham, C. L. , & Anis, A. H. (2009). The incidence of co‐morbidities related to obesity and overweight: A systematic review and meta‐analysis . BMC Public Health , 9 , 88. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Haffner, S. , Temprosa, M. , Crandall, J. , Fowler, S. , Goldberg, R. , Horton, E. , … Diabetes Prevention Program Research Group , et al. (2005). Intensive lifestyle intervention or metformin on inflammation and coagulation in participants with impaired glucose tolerance . Diabetes , 54 ( 5 ), 1566–1572. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Hamdy, O. (2016). Obesity . Retrieved from https://emedicine.medscape.com/article/123702-overview
- Haufe, S. , Haas, V. , Utz, W. , Birkenfeld, A. L. , Jeran, S. , Bohnke, J. , … Engeli, S. , et al. (2013). Long‐lasting improvements in liver fat and metabolism despite body weight regain after dietary weight loss . Diabetes Care , 36 ( 11 ), 3786–3792. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Hersey, J. , Anliker, J. , Miller, C. , Mullis, R. M. , Daugherty, S. , Das, S. , … Olivia, A. H. , et al. (2001). Food shopping practices are associated with dietary quality in low‐income households . Journal of Nutrition Education , 33 ( Suppl 1 ), S16–S26. [ PubMed ] [ Google Scholar ]
- Hursting, S. D. , & Dunlap, S. M. (2012). Obesity, metabolic dysregulation, and cancer: A growing concern and an inflammatory (and microenvironmental) issue . Annals of the New York Academy of Sciences , 1271 , 82–87. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- International Diabetes Federation . (2006). The IDF consensus worldwide definition of the metabolic syndrome (electronic version). Retrieved from https://www.idf.org/webdata/docs/IDF_Meta_def_final.pdf
- Ip, M. S. , Lam, B. , Ng, M. M. , Lam, W. K. , Tsang, K. W. , & Lam, K. S. (2002). Obstructive sleep apnea is independently associated with insulin resistance . American Journal of Respiratory and Critical Care Medicine , 165 ( 5 ), 670–676. [ PubMed ] [ Google Scholar ]
- Johnson, A. R. , Milner, J. J. , & Makowski, L. (2012). The inflammation highway: Metabolism accelerates inflammatory traffic in obesity . Immunological Reviews , 249 ( 1 ), 218–238. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Jones, D. E. , Carson, K. A. , Bleich, S. N. , & Cooper, L. A. (2012). Patient trust in physicians and adoption of lifestyle behaviors to control high blood pressure . Patient Education and Counseling , 89 ( 1 ), 57–62. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Juel, C. T. , Ali, Z. , Nilas, L. , & Ulrik, C. S. (2012). Asthma and obesity: Does weight loss improve asthma control? A systematic review . Journal of Asthma and Allergy , 5 , 21–26. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Kernan, W. N. , Inzucchi, S. E. , Sawan, C. , Macko, R. F. , & Furie, K. L. (2013). Obesity: A stubbornly obvious target for stroke prevention . Stroke , 44 ( 1 ), 278–286. [ PubMed ] [ Google Scholar ]
- Kort, J. D. , Winget, C. , Kim, S. H. , & Lathi, R. B. (2014). A retrospective cohort study to evaluate the impact of meaningful weight loss on fertility outcomes in an overweight population with infertility . Fertility and Sterility , 101 ( 5 ), 1400–1403. [ PubMed ] [ Google Scholar ]
- Kral, T. V. , & Rauh, E. M. (2010). Eating behaviors of children in the context of their family environment . Physiology & Behavior , 100 ( 5 ), 567–573. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Kritchevsky, S. B. , Beavers, K. M. , Miller, M. E. , Shea, M. K. , Houston, D. K. , Kitzman, D. W. , & Nicklas, B. J. (2015). Intentional weight loss and all‐cause mortality: A meta‐analysis of randomized clinical trials . PLoS One , 10 ( 3 ), e0121993. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Kuk, J. L. , Ardern, C. I. , Church, T. S. , Sharma, A. M. , Padwal, R. , Sui, X. , … Blair, S. N. , et al. (2011). Edmonton obesity staging system: Association with weight history and mortality risk . Applied Physiology, Nutrition, and Metabolism , 36 ( 4 ), 570–576. [ PubMed ] [ Google Scholar ]
- Kuna, S. T. , Reboussin, D. M. , Borradaile, K. E. , Sanders, M. H. , Millman, R. P. , Zammit, G. , … Sleep AHEAD Research Group of the Look AHEAD Research Group , et al. (2013). Long‐term effect of weight loss on obstructive sleep apnea severity in obese patients with type 2 diabetes . Sleep , 36 ( 5 ), 641–649A. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Lee, J. M. , Pilli, S. , Gebremariam, A. , Keirns, C. C. , Davis, M. M. , Vijan, S. , … Gurney, J. G. , et al. (2010). Getting heavier, younger: Trajectories of obesity over the life course . International Journal of Obesity , 34 ( 4 ), 614–623. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Lenoir, L. , Maillot, M. , Guilbot, A. , & Ritz, P. (2015). Primary care weight loss maintenance with behavioral nutrition: An observational study . Obesity (Silver Spring) , 23 ( 9 ), 1771–777. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Li, G. , Zhang, P. , Wang, J. , An, Y. , Gong, Q. , Gregg, E. W. , … Bennett, P. H. , et al. (2014). Cardiovascular mortality, all‐cause mortality, and diabetes incidence after lifestyle intervention for people with impaired glucose tolerance in the Da Qing Diabetes Prevention Study: A 23‐year follow‐up study . Lancet Diabetes & Endocrinology , 2 ( 6 ), 474–480. [ PubMed ] [ Google Scholar ]
- Li, G. , Zhang, P. , Wang, J. , Gregg, E. W. , Yang, W. , Gong, Q. , … Bennett, P. H. , et al. (2008). The long‐term effect of lifestyle interventions to prevent diabetes in the China Da Qing Diabetes Prevention Study: A 20‐year follow‐up study . Lancet , 371 ( 9626 ), 1783–1789. [ PubMed ] [ Google Scholar ]
- Lindstrom, J. , Eriksson, J. G. , Valle, T. T. , Aunola, S. , Cepaitis, Z. , Hakumaki, M. , … Tuomilehto, J. , et al. (2003). Prevention of diabetes mellitus in subjects with impaired glucose tolerance in the Finnish Diabetes Prevention Study: Results from a randomized clinical trial . Journal of the American Society of Nephrology , 14 ( 7 Suppl 2 ), S108–S113. [ PubMed ] [ Google Scholar ]
- Lindstrom, J. , Ilanne‐Parikka, P. , Peltonen, M. , Aunola, S. , Eriksson, J. G. , Hemio, K. , … Finnish Diabetes Prevention Study Group , et al. (2006). Sustained reduction in the incidence of type 2 diabetes by lifestyle intervention: Follow‐up of the Finnish Diabetes Prevention Study . Lancet , 368 ( 9548 ), 1673–1679. [ PubMed ] [ Google Scholar ]
- Linkov, F. , Maxwell, G. L. , Felix, A. S. , Lin, Y. , Lenzner, D. , Bovbjerg, D. H. , … DeLany, J. P. , et al. (2012). Longitudinal evaluation of cancer‐associated biomarkers before and after weight loss in RENEW study participants: Implications for cancer risk reduction . Gynecologic Oncology , 125 ( 1 ), 114–119. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Loper, H. B. , La Sala, M. , Dotson, C. , & Steinle, N. (2015). Taste perception, associated hormonal modulation, and nutrient intake . Nutrition Reviews , 73 ( 2 ), 83–91. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Lv, N. , Xiao, L. , & Ma, J. (2015). Weight management interventions in adult and pediatric asthma populations: A systematic review . J Pulm Respir Med , 5 ( 232 ), pii: 1000232. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Martin‐Rodriguez, E. , Guillen‐Grima, F. , Marti, A. , & Brugos‐Larumbe, A. (2015). Comorbidity associated with obesity in a large population: The APNA study . Obesity Research & Clinical Practice , 9 ( 5 ), 435–447. [ PubMed ] [ Google Scholar ]
- Musunuru, K. (2010). Atherogenic dyslipidemia: Cardiovascular risk and dietary intervention . Lipids , 45 ( 10 ), 907–914. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Nanchahal, K. , Townsend, J. , Letley, L. , Haslam, D. , Wellings, K. , & Haines, A. (2009). Weight‐management interventions in primary care: A pilot randomised controlled trial . British Journal of General Practice , 59 ( 562 ), e157–e166. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Osunlana, A. M. , Asselin, J. , Anderson, R. , Ogunleye, A. A. , Cave, A. , Sharma, A. M. , & Campbell‐Scherer, D. L.. (2015). 5As team obesity intervention in primary care: Development and evaluation of shared decision‐making weight management tools . Clinical Obesity , 5 ( 4 ), 219–225. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Pan, X. R. , Li, G. W. , Hu, Y. H. , Wang, J. X. , Yang, W. Y. , An, Z. X. , … Howard, B. V. , et al. (1997). Effects of diet and exercise in preventing NIDDM in people with impaired glucose tolerance. The Da Qing IGT and diabetes study . Diabetes Care , 20 ( 4 ), 537–544. [ PubMed ] [ Google Scholar ]
- Parker, E. D. , & Folsom, A. R. (2003). Intentional weight loss and incidence of obesity‐related cancers: The Iowa Women's Health Study . International Journal of Obesity and Related Metabolic Disorders: Journal of the International Association for the Study of Obesity , 27 ( 12 ), 1447–1452. [ PubMed ] [ Google Scholar ]
- Patel, N. S. , Doycheva, I. , Peterson, M. R. , Hooker, J. , Kisselva, T. , Schnabl, B. , … Loomba, R. , et al. (2015). Effect of weight loss on magnetic resonance imaging estimation of liver fat and volume in patients with nonalcoholic steatohepatitis . Clinical Gastroenterology and Hepatology , 13 ( 3 ), 561–568 e561. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Peterson, N. D. , Middleton, K. R. , Nackers, L. M. , Medina, K. E. , Milsom, V. A. , & Perri, M. G. (2014). Dietary self‐monitoring and long‐term success with weight management . Obesity (Silver Spring) , 22 ( 9 ), 1962–1967. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Petry, N. M. , Barry, D. , Pietrzak, R. H. , & Wagner, J. A. (2008). Overweight and obesity are associated with psychiatric disorders: Results from the National Epidemiologic Survey on Alcohol and Related Conditions . 70 ( 3 ), 288–297. [ PubMed ] [ Google Scholar ]
- Pi‐Sunyer, X. (2009). The medical risks of obesity . Postgraduate Medicine , 121 ( 6 ), 21–33. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Prospective Studies Collaboration , Whitlock, G. , Lewington, S. , Sherliker, P. , Clarke, R. , Emberson, J. , … Peto, R. , et al. (2009). Body‐mass index and cause‐specific mortality in 900 000 adults: Collaborative analyses of 57 prospective studies . Lancet , 373 ( 9669 ), 1083–1096. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Pulgaron, E. R. (2013). Childhood obesity: A review of increased risk for physical and psychological comorbidities . Clin Ther 35 ( 1 ), A18–A32. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Ratner, R. , Goldberg, R. , Haffner, S. , Marcovina, S. , Orchard, T. , Fowler, S. , … Diabetes Prevention Program Research Group , et al. (2005). Impact of intensive lifestyle and metformin therapy on cardiovascular disease risk factors in the diabetes prevention program . Diabetes Care , 28 ( 4 ), 888–894. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Rogge, M. M. , & Gautam, B. (2017). Biology of obesity and weight regain: Implications for clinical practice . Journal of the American Association of Nurse Practitioners , 29 (Supplement 1), S15–S29. [ PubMed ] [ Google Scholar ]
- Romero‐Corral, A. , Caples, S. M. , Lopez‐Jimenez, F. , & Somers, V. K. (2010). Interactions between obesity and obstructive sleep apnea: Implications for treatment . Chest , 137 ( 3 ), 711–719. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Sakai, R. , Matsui, S. , Fukushima, M. , Yasuda, H. , Miyauchi, H. , & Miyachi, Y. (2005). Prognostic factor analysis for plaque psoriasis . Dermatology , 211 ( 2 ), 103–106. [ PubMed ] [ Google Scholar ]
- Singh, M. , Lee, J. , Gupta, N. , Gaddam, S. , Smith, B. K. , Wani, S. B. , … Sharma, P. , et al. (2013). Weight loss can lead to resolution of gastroesophageal reflux disease symptoms: A prospective intervention trial . Obesity (Silver Spring) , 21 ( 2 ), 284–290. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Skinner, A. C. , & Skelton, J. A. (2014). Prevalence and trends in obesity and severe obesity among children in the United States, 1999–2012 . JAMA Pediatrics , 168 ( 6 ), 561–566. [ PubMed ] [ Google Scholar ]
- Smith, S. A. , Hulsey, T. , & Goodnight, W. (2008). Effects of obesity on pregnancy . J Obstet Gynecol Neonatal Nurs , 37 ( 2 ), 176–184. [ PubMed ] [ Google Scholar ]
- The Global BMI Mortality Collaboration . (2016). Body‐mass index and all‐cause mortality: Individual participant‐data meta‐analysis of 239 prospective studies in four continents . Lancet , 388 , 734–736. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- The National Weight Control Registry ( NWCR) . (2016). NCWR facts . Retrieved from https://www.nwcr.ws/
- Tuomilehto, J. , Lindstrom, J. , Eriksson, J. G. , Valle, T. T. , Hamalainen, H. , Ilanne‐Parikka, P. , … Finnish Diabetes Prevention Study Group , et al. (2001). Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance . New England Journal of Medicine , 344 ( 18 ), 1343–1350. [ PubMed ] [ Google Scholar ]
- Weinsier, R. L. , & Ullmann, D. O. (1993). Gallstone formation and weight loss . Obesity Research , 1 ( 1 ), 51–56. [ PubMed ] [ Google Scholar ]
- Wensveen, F. M. , Valentic, S. , Sestan, M. , Turk Wensveen, T. , & Polic, B. (2015). The "Big Bang" in obese fat: Events initiating obesity‐induced adipose tissue inflammation . European Journal of Immunology , 45 ( 9 ), 2446–2456. [ PubMed ] [ Google Scholar ]
- Whitaker, R. C. , Wright, J. A. , Pepe, M. S. , Seidel, K. D. , & Dietz, W. H. (1997). Predicting obesity in young adulthood from childhood and parental obesity . New England Journal of Medicine , 337 ( 13 ), 869–873. [ PubMed ] [ Google Scholar ]
- World Health Organization (WHO) . (2016a). 10 Facts on obesity . Retrieved from https://www.who.int/features/factfiles/obesity/facts/en/
- World Health Organization (WHO) . (2016b). Obesity . Retrieved from https://www.who.int/topics/obesity/en/
- Wyse, R. , Wolfenden, L. , & Bisquera, A. (2015). Characteristics of the home food environment that mediate immediate and sustained increases in child fruit and vegetable consumption: Mediation analysis from the Healthy Habits cluster randomised controlled trial . International Journal of Behavioral Nutrition and Physical Activity , 12 , 118. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Yang, L. , & Colditz, G. A. (2015). Prevalence of overweight and obesity in the United States, 2007–2012 . JAMA Internal Medicine , 175 ( 8 ), 1412–1413. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Yosipovitch, G. , DeVore, A. , & Dawn, A. (2007). Obesity and the skin: Skin physiology and skin manifestations of obesity . J Am Acad Dermatol , 56 ( 6 ), 901–916; quiz 917–920. [ PubMed ] [ Google Scholar ]
Obesity in America: Cause and Effect Essay Sample
It is clear that the American lifestyle has contributed to the increasing prevalence of obesity. With estimates from the Washington-based Centers for Disease Prevention in the Department of Health and Human Services indicating that one in three American adults is overweight, it is evident that the country is facing an obesity epidemic. To better understand the causes and effects of obesity, research is needed to further explore the issue. For those struggling with obesity, coursework assistance may be available to help them make the necessary lifestyle changes in order to live a healthier life.
Writing a thesis paper on the topic of obesity can be extremely challenging. It requires extensive research and time to adequately cover the subject. However, there are services available that can provide assistance with the writing process. Pay for a thesis allows for the benefit of having an experienced professional provide guidance and support throughout the entire process.
Causes of Obesity
Every phenomenon must have a reason. In order to write a cause and effect essay , you need to analyze the topic carefully to cover all aspects. Obesity is considered to be a complex illness, with a number of factors contributing to its development. These can be:
- hereditary;
As you may have guessed, it is the latter category of causes and effects that we are interested in. At this point, we care about the five ones that have made the biggest contribution.
Product Range
The main cause of obesity is junk food and an unbalanced diet rich in simple carbohydrates, fats, and sugars, plus a bunch of additives. Manufactured, processed, refined, and packaged meals are the most popular. Thanks to advances in technology, Americans have come to mass-produce meals that keep fresh longer and taste better. It takes less time to prepare unhealthy, processed foods in the microwave than it does to cook them yourself.
Lack of a work-life balance, high-stress levels, insufficient sleeping hours contribute to body weight gain. Not only do these factors contribute to this, but failing to take the time to do your homework can also have a negative impact on your physical health. Without a healthy, balanced approach to work, rest, and play, you may find yourself increasingly dependent on a sedentary lifestyle that can lead to overweight consequences. Many Americans work 50, 60, or more hours a week and suffer from a deficit of leisure hours. Cooking processed foods saves them hours and money, even though they end up costing them a lot more – by causing cardiovascular disease. In addition, obese people feel stressed on a regular basis in the United States metropolitan areas. Many of them are simply binge eating under the influence of negative emotions. Chronic overeating leads to a disturbance in the appetite center in the brain, and the normal amount of food eaten can no longer suppress hunger as much as necessary, affecting the body mass.
Food Deserts
The term ‘ food desert ‘ refers to poor areas (urban, suburban and rural) with limited access to fresh fruit, grains, and vegetables – places where it is much easier to access junk food. A grocery shop in a food desert that sells healthy foods may be 10-15 miles away, while a mini-market or cheap shop that sells harmful snacks is close to the house. In such a world, it takes much more effort to eat healthier, form eating habits, and stay slim.
Everyone’s Passion for Sweets
Consuming sweets in large quantities is addictive: the more and easier we give the body energy, the more the brain uses serotonin and dopamine to encourage it – it will make obese people want sweets again and again during the day. Cakes and pastries are fast carbohydrates that easily satisfy hunger and increase body mass. Despite the harm of sweets, obese people experience the need for them to satiate. Sweetened carbonated drinks are one of the main sources of sugar in the American diet. Moreover, some individuals may be more adversely affected by such diets than others: patients with a genetic predisposition to obesity gain body mass faster from sugary drinks than those without it. This leads to childhood obesity.
The Harm of Tolerance
Every year, the body positive movement is becoming more and more popular all over the world. It would seem that this major trend should have freed us from the problems associated with the cult of thinness and society’s notorious standards. In many ways, a positive attitude towards the body has proved fruitful. For example, the notion of beauty has clearly broadened. Now on fashion shows and magazine covers, you can see not only a girl with perfectly retouched skin and without a single hint of body fat but also an ordinary person with its inherent features: overweight, wrinkles, hair, and individual skin features. In general, all the things that we are all so familiar with in real life.
Does it really make that much sense? Is this a positive thing in terms of the cause and effect topic regarding obesity? In short, opinions are divided. Extremes aren’t easy to overcome. Not everyone manages to do it. Researchers have concluded that due to plus size having become positioned as a variant of the norm, more persons have become obese. Many obese Americans have formed the opinion that it is really quite normal, and they have become oblivious to the damage it does to their health. This is what we are going to focus on next.
Effects of Obesity
We all know that obesity is dangerous to health. However, medical studies show that most adults are unaware of the number of complications and diseases that obesity in America entails. So they are fairly comfortable with becoming gradually fatter. But indifference is replaced by concern when obesity related diseases begin to occur.
For interesting examples of students writing that also reveal the causes and effects of other phenomena, consult the custom essay service offering essays by professionals. In this way, you will realize the importance of highlighting the effects right after the causes.
Is obesity an aesthetic disadvantage, an inconvenience, a limitation in physical activity or is it an illness after all? How does it affect health, and what are the consequences? The visible signs of obesity are by no means the only complication associated with this condition. Obesity creates a high risk of life-threatening diseases such as atherosclerosis, hypertension, heart attack, myocardial infarction, and kidney and liver problems. Moreover, it can also lead to disability.
Cardiovascular Disease
This is the most serious and damaging impact on the body and blood vessels in particular. Every extra kilo is a huge additional load on the heart. Obesity increases the risk of heart attacks. Experts from the American Heart Association have developed a paper on the relationship between obesity and cardiovascular disease, which discusses the impact of obesity on the diagnosis and outcomes of patients with atherosclerotic cardiovascular disease, heart failure, and arrhythmias. Childhood obesity aggravates the course of cardiovascular disease from a very early age. The fact that even kids and adolescents are obese is associated with high blood pressure, dyslipidemia, and hyperglycemia.
The result is excessive insulin production in the body. This, in turn, leads to an overabundance of insulin in the blood, which makes the peripheral tissues more resistant to it. As a consequence of the above, sodium metabolism is disturbed, and blood pressure rises. It is important to remember that excessive carbohydrate food intake leads to increased production of insulin by the pancreas. Excess insulin in the human body easily converts glucose into fat. And obesity reduces tissue sensitivity to insulin itself. This kind of vicious circle leads to type 2 diabetes.
Effects on Joints
Obesity increases the load on joints to a great extent, especially if one undergoes little or no physical activity. For instance, if one lives in a megalopolis, where all physical activity consists of getting off the sofa, walking to the car, and plumping up in an office chair at work. All this leads to a reduction in muscle mass, which is already weak, and all the load falls on the joints and ligaments.
The result is arthritis, arthrosis, and osteochondrosis. Consequently, a seemingly illogical situation is formed – there is practically no exercise, but joints are worn out harder than in the case of powerlifters. In turn, according to a study by the University of California, reducing body weight reduces the risk of osteoarthritis.
Infertility
In most cases, being obese leads to endocrine infertility, as it causes an irregular menstrual cycle. Women experience thyroid disease, polycystic ovarian syndrome, problems with conception, and decreased progesterone hormone. Obese men are faced with erectile dysfunction, reduced testosterone levels, and infertility. It should be noted that the mother’s obesity affects not only her health but also the one of her unborn child. These children are at higher risk of congenital malformations.
Corresponding Inconveniences
Public consciousness is still far from the notion that obese people are sick individuals. The social significance of the issue is that people who are severely obese find it difficult to get a job. They experience discriminatory restrictions on promotion, daily living disadvantages, restrictions on mobility, clothing choices, discomfort with adequate hygiene, and sexual dysfunction. Some of these individuals not only suffer from illness and limited mobility but also have low self-esteem, depression, and other psychological problems due to involuntary isolation by watching television or playing video games. Therefore, the public has to recognize the need to establish and implement national and childhood obesity epidemic prevention programs.
Society today provokes unintentional adult and childhood obesity among its members by encouraging the consumption of high-fat, high-calorie foods and, at the same time, by technological advances, promoting sedentary lifestyles like spending time watching television or playing video games. These social and technological factors have contributed to the rise in obesity in recent decades. Developing a responsible attitude towards health will only have a full impact if people are given the opportunity to enjoy a healthy lifestyle. At the level of the community as a whole, it is therefore important to support people in adhering to dieting recommendations through the continued implementation of evidence-based and demographic-based policies to make regular physical activity and good nutrition both affordable and feasible for all. It is recommended to cut down on the food consumed.

Related posts:
- The Great Gatsby (Analyze this Essay Online)
- Pollution Cause and Effect Essay Sample
- Essay Sample on How Can I Be a Good American
- The Power of Imaging: Why I am Passionate about Becoming a Sonographer
Improve your writing with our guides

Youth Culture Essay Prompt and Discussion

Why Should College Athletes Be Paid, Essay Sample

Reasons Why Minimum Wage Should Be Raised Essay: Benefits for Workers, Society, and The Economy
Get 15% off your first order with edusson.
Connect with a professional writer within minutes by placing your first order. No matter the subject, difficulty, academic level or document type, our writers have the skills to complete it.
100% privacy. No spam ever.

Home — Essay Samples — Nursing & Health — Obesity — The Most Common Causes of Obesity
The Most Common Causes of Obesity
- Categories: Food Safety Medicare Obesity
About this sample

Words: 505 |
Published: Jan 8, 2020
Words: 505 | Page: 1 | 3 min read

Cite this Essay
Let us write you an essay from scratch
- 450+ experts on 30 subjects ready to help
- Custom essay delivered in as few as 3 hours
Get high-quality help

Dr Jacklynne
Verified writer
- Expert in: Science Nursing & Health

+ 120 experts online
By clicking “Check Writers’ Offers”, you agree to our terms of service and privacy policy . We’ll occasionally send you promo and account related email
No need to pay just yet!
Related Essays
1 pages / 552 words
3 pages / 1169 words
1 pages / 529 words
1 pages / 358 words
Remember! This is just a sample.
You can get your custom paper by one of our expert writers.
121 writers online
Still can’t find what you need?
Browse our vast selection of original essay samples, each expertly formatted and styled
Related Essays on Obesity
Oliver, J. (2010, February). Teach every child about food. TED. Retrieved from Publishers.
Government of Canada. (2006). The Health Risks of Obesity. Health Canada.Government of Canada. (2018). Obesity in Canada: A Whole-of-Society Approach for a Healthier Canada. Public Health Agency of Canada.Government of Canada. [...]
In conclusion, obesity is a growing epidemic in America that has severe health, economic, and social consequences. Addressing obesity as a societal issue requires a multi-faceted approach that addresses the root causes of the [...]
Obesity has become a significant public health concern globally, with a high prevalence rate in both developed and developing countries. According to the World Health Organization (WHO), obesity has more than doubled since 1980, [...]
It is well known today that the obesity epidemic is claiming more and more victims each day. The Centers for Disease Control and Prevention writes “that nearly 1 in 5 school age children and young people (6 to 19 years) in the [...]
The overweight or obese among the U.S. citizens is inclining at a shocking rate. Currently, it stands at 74.1% which is almost ¾ of our country’s population. It is a frightening truth that needs to be acknowledged by the entire [...]
Related Topics
By clicking “Send”, you agree to our Terms of service and Privacy statement . We will occasionally send you account related emails.
Where do you want us to send this sample?
By clicking “Continue”, you agree to our terms of service and privacy policy.
Be careful. This essay is not unique
This essay was donated by a student and is likely to have been used and submitted before
Download this Sample
Free samples may contain mistakes and not unique parts
Sorry, we could not paraphrase this essay. Our professional writers can rewrite it and get you a unique paper.
Please check your inbox.
We can write you a custom essay that will follow your exact instructions and meet the deadlines. Let's fix your grades together!
Get Your Personalized Essay in 3 Hours or Less!
We use cookies to personalyze your web-site experience. By continuing we’ll assume you board with our cookie policy .
- Instructions Followed To The Letter
- Deadlines Met At Every Stage
- Unique And Plagiarism Free

- History & Society
- Science & Tech
- Biographies
- Animals & Nature
- Geography & Travel
- Arts & Culture
- Games & Quizzes
- On This Day
- One Good Fact
- New Articles
- Lifestyles & Social Issues
- Philosophy & Religion
- Politics, Law & Government
- World History
- Health & Medicine
- Browse Biographies
- Birds, Reptiles & Other Vertebrates
- Bugs, Mollusks & Other Invertebrates
- Environment
- Fossils & Geologic Time
- Entertainment & Pop Culture
- Sports & Recreation
- Visual Arts
- Demystified
- Image Galleries
- Infographics
- Top Questions
- Britannica Kids
- Saving Earth
- Space Next 50
- Student Center
- Introduction
Defining obesity
The obesity epidemic, childhood obesity.
- Causes of obesity
- Health effects of obesity
- Treatment of obesity

Our editors will review what you’ve submitted and determine whether to revise the article.
- Live Science - Obesity: Causes, Complications & Treatments
- Mayo Clinic - Obesity
- National Library of Medicine - Obesity
- The Nemours Foundation - For Parents - Overweight and Obesity
- Cleveland Clinic - Obesity
- Verywell Health - Obesity
- Medicine LibreTexts - Obesity
- obesity - Children's Encyclopedia (Ages 8-11)
- obesity - Student Encyclopedia (Ages 11 and up)
- Table Of Contents

Recent News
obesity , excessive accumulation of body fat, usually caused by the consumption of more calories than the body can use. The excess calories are then stored as fat, or adipose tissue . Overweight, if moderate, is not necessarily obesity, particularly in muscular or large-boned individuals.

Obesity was traditionally defined as an increase in body weight that was greater than 20 percent of an individual’s ideal body weight—the weight associated with the lowest risk of death, as determined by certain factors, such as age, height, and gender. Based on these factors, overweight could then be defined as a 15–20 percent increase over ideal body weight. However, today the definitions of overweight and obesity are based primarily on measures of height and weight—not morbidity . These measures are used to calculate a number known as body mass index (BMI). This number, which is central to determining whether an individual is clinically defined as obese, parallels fatness but is not a direct measure of body fat. Interpretation of BMI numbers is based on weight status groupings, such as underweight, healthy weight, overweight, and obese, that are adjusted for age and sex. For all adults over age 20, BMI numbers correlate to the same weight status designations; for example, a BMI between 25.0 and 29.9 equates with overweight and 30.0 and above with obesity. Morbid obesity (also known as extreme, or severe, obesity) is defined as a BMI of 40.0 or higher. ( See nutritional disease: Diet and chronic disease .)
Body weight is influenced by the interaction of multiple factors. There is strong evidence of genetic predisposition to fat accumulation, and obesity tends to run in families. However, the rise in obesity in populations worldwide since the 1980s has outpaced the rate at which genetic mutations are normally incorporated into populations on a large scale. In addition, growing numbers of persons in parts of the world where obesity was once rare have also gained excessive weight. According to the World Health Organization (WHO), which considered global obesity an epidemic , in 2016 more than 1.9 billion adults (age 18 or older) worldwide were overweight and 650 million, representing 13 percent of the world’s adult population, were obese.
The prevalence of overweight and obesity varied across countries, across towns and cities within countries, and across populations of men and women. In China and Japan, for instance, the obesity rate for men and women was about 5 percent, but in some cities in China it had climbed to nearly 20 percent. In 2005 it was found that more than 70 percent of Mexican women were obese. WHO survey data released in 2010 revealed that more than half of the people living in countries in the Pacific Islands region were overweight, with some 80 percent of women in American Samoa found to be obese.

Childhood obesity has become a significant problem in many countries. Overweight children often face stigma and suffer from emotional, psychological, and social problems. Obesity can adversely affect a child’s education and future socioeconomic status. In 2004 an estimated nine million American children over age 6, including teenagers, were overweight, or obese (the terms were typically used interchangeably in describing excess fatness in children). Moreover, in the 1980s and 1990s the prevalence of obesity had more than doubled among children age 2 to 5 (from 5 percent to 10 percent) and age 6 to 11 (from 6 percent to 15 percent). By 2015, 20 percent of children age 6 to 19 were obese in the United States . Further estimates in some rural areas of the country indicated that more than 30 percent of school-age children suffered from obesity. Similar increases were seen in other parts of the world. In the United Kingdom, for example, the prevalence of obesity among children age 2 to 10 had increased from 10 percent in 1995 to 14 percent in 2003, and data from a study conducted there in 2007 indicated that 23 percent of children age 4 to 5 and 32 percent of children age 10 to 11 were overweight or obese. By 2016, WHO data indicated, worldwide some 41 million children age 5 or under were overweight or obese.
In 2005 the American Academy of Pediatrics called obesity “the pediatric epidemic of the new millennium.” Overweight and obese children were increasingly diagnosed with high blood pressure , elevated cholesterol , and type II diabetes mellitus —conditions once seen almost exclusively in adults. In addition, overweight children experience broken bones and problems with joints more often than normal-weight children. The long-term consequences of obesity in young people are of great concern to pediatricians and public health experts, because obese children are at high risk of becoming obese adults. Experts on longevity have concluded that today’s American youth might “live less healthy and possibly even shorter lives than their parents” if the rising prevalence of obesity is left unchecked.
Curbing the rise in childhood obesity was the aim of the Alliance for a Healthier Generation, a partnership formed in 2005 by the American Heart Association, former U.S. president Bill Clinton , and the children’s television network Nickelodeon. The alliance intended to reach children through a vigorous public awareness campaign. Similar projects followed, including American first lady Michelle Obama ’s Let’s Move! program, launched in 2010, and campaigns against overweight and obesity were made in other countries as well.
Efforts were also under way to develop more-effective childhood obesity-prevention strategies, including the development of methods capable of predicting infants’ risk of later becoming overweight or obese. One such tool reported in 2012 was found to successfully predict newborn obesity risk by taking into account newborn weight, maternal and paternal BMI, the number of members in the newborn’s household, maternal occupational status, and maternal smoking during pregnancy .
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Review Article
- Published: 23 September 2021
The genetics of obesity: from discovery to biology
- Ruth J. F. Loos ORCID: orcid.org/0000-0002-8532-5087 1 , 2 , 3 , 4 &
- Giles S. H. Yeo ORCID: orcid.org/0000-0001-8823-3615 5
Nature Reviews Genetics volume 23 , pages 120–133 ( 2022 ) Cite this article
155k Accesses
438 Citations
481 Altmetric
Metrics details
- Disease genetics
- Endocrine system and metabolic diseases
- Genetic association study
- Genetic variation
The prevalence of obesity has tripled over the past four decades, imposing an enormous burden on people’s health. Polygenic (or common) obesity and rare, severe, early-onset monogenic obesity are often polarized as distinct diseases. However, gene discovery studies for both forms of obesity show that they have shared genetic and biological underpinnings, pointing to a key role for the brain in the control of body weight. Genome-wide association studies (GWAS) with increasing sample sizes and advances in sequencing technology are the main drivers behind a recent flurry of new discoveries. However, it is the post-GWAS, cross-disciplinary collaborations, which combine new omics technologies and analytical approaches, that have started to facilitate translation of genetic loci into meaningful biology and new avenues for treatment.
Similar content being viewed by others
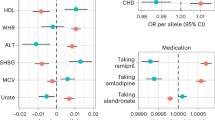
A phenome-wide comparative analysis of genetic discordance between obesity and type 2 diabetes
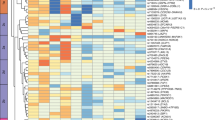
Genome-wide discovery of genetic loci that uncouple excess adiposity from its comorbidities

Independent phenotypic plasticity axes define distinct obesity sub-types
Introduction.
Obesity is associated with premature mortality and is a serious public health threat that accounts for a large proportion of the worldwide non-communicable disease burden, including type 2 diabetes, cardiovascular disease, hypertension and certain cancers 1 , 2 . Mechanical issues resulting from substantially increased weight, such as osteoarthritis and sleep apnoea, also affect people’s quality of life 3 . The impact of obesity on communicable disease, in particular viral infection 4 , has recently been highlighted by the discovery that individuals with obesity are at increased risk of hospitalization and severe illness from COVID-19 (refs 5 , 6 , 7 ).
On the basis of the latest data from the NCD Risk Factor Collaboration, in 2016 almost 2 billion adults (39% of the world’s adult population) were estimated to be overweight (defined by a body mass index (BMI) of ≥25 kg m − 2 ), 671 million (12% of the world’s adult population) of whom had obesity (BMI ≥30 kg m − 2 ) — a tripling in the prevalence of obesity since 1975 (ref. 8 ) (Fig. 1 ). Although the rate of increase in obesity seems to be declining in most high-income countries, it continues to rise in many low-income and middle-income countries and prevalence remains high globally 8 . If current trends continue, it is expected that 1 billion adults (nearly 20% of the world population) will have obesity by 2025. Particularly alarming is the global rise in obesity among children and adolescents; more than 7% had obesity in 2016 compared with less than 1% in 1975 (ref. 8 ).
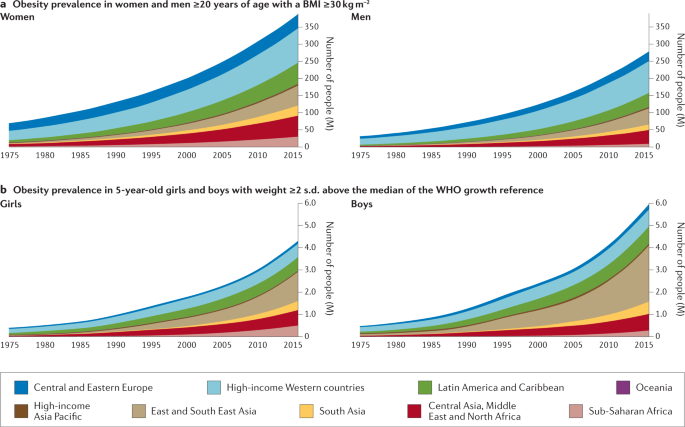
The prevalence of obesity has risen steadily over the past four decades in children, adolescents (not shown) and adults worldwide. a | Prevalence of obesity (body mass index (BMI) ≥30 kg m −2 ) in women and men ≥20 years of age, from 1975 to 2016. b | Prevalence of obesity (weight ≥2 s.d. above the median of the WHO growth reference) in 5-year-old girls and boys from 1975 to 2016. Geographical regions are represented by different colours. Graphs are reproduced from the NCD Risk Factor Collaboration (NCD RisC) website and are generated from data published in ref. 8 .
Although changes in the environment have undoubtedly driven the rapid increase in prevalence, obesity results from an interaction between environmental and innate biological factors. Crucially, there is a strong genetic component underlying the large interindividual variation in body weight that determines people’s response to this ‘obesogenic’ environment . Twin, family and adoption studies have estimated the heritability of obesity to be between 40% and 70% 9 , 10 . As a consequence, genetic approaches can be leveraged to characterize the underlying physiological and molecular mechanisms that control body weight.
Classically, we have considered obesity in two broad categories (Fig. 2 ): so-called monogenic obesity , which is inherited in a Mendelian pattern, is typically rare, early-onset and severe and involves either small or large chromosomal deletions or single-gene defects; and polygenic obesity (also known as common obesity), which is the result of hundreds of polymorphisms that each have a small effect. Polygenic obesity follows a pattern of heritability that is similar to other complex traits and diseases. Although often considered to be two distinct forms, gene discovery studies of monogenic and polygenic obesity have converged on what seems to be broadly similar underlying biology. Specifically, the central nervous system (CNS) and neuronal pathways that control the hedonic aspects of food intake have emerged as the major drivers of body weight for both monogenic and polygenic obesity. Furthermore, early evidence shows that the expression of mutations causing monogenic obesity may — at least in part — be influenced by the individual’s polygenic susceptibility to obesity 11 .
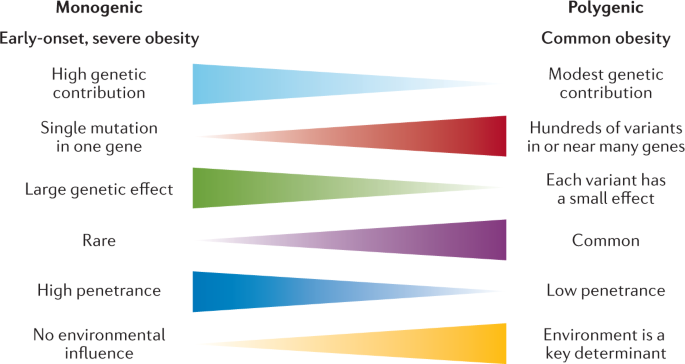
Key features of monogenic and polygenic forms of obesity .
In this Review, we summarize more than 20 years of genetic studies that have characterized the molecules and mechanisms that control body weight, specifically focusing on overall obesity and adiposity, rather than fat distribution or central adiposity. Although most of the current insights into the underlying biology have been derived from monogenic forms of obesity, recent years have witnessed several successful variant-to-function translations for polygenic forms of obesity. We also explore how the ubiquity of whole-exome sequencing (WES) and genome sequencing has begun to blur the line that used to demarcate the monogenic causes of obesity from common polygenic obesity. Syndromic forms of obesity, such as Bardet–Biedl, Prader–Willi, among many others 12 , are not reviewed here. Although obesity is often a dominant feature of these syndromes, the underlying genetic defects are often chromosomal abnormalities and typically encompass multiple genes, making it difficult to decipher the precise mechanisms directly related to body-weight regulation. Finally, as we enter the post-genomic era, we consider the prospects of genotype-informed treatments and the possibility of leveraging genetics to predict and hence prevent obesity.
Gene discovery approaches
The approaches used to identify genes linked to obesity depend on the form of obesity and genotyping technology available at the time. Early gene discovery studies for monogenic forms of obesity had a case-focused design: patients with severe obesity, together with their affected and unaffected family members, were examined for potential gene-disrupting causal mutations via Sanger sequencing. By contrast, genetic variation associated with common forms of obesity have been identified in large-scale population studies, either using a case–control design or continuous traits such as BMI. Gene discovery for both forms of obesity was initially hypothesis driven; that is, restricted to a set of candidate genes that evidence suggests have a role in body-weight regulation. Over the past two decades, however, advances in high-throughput genome-wide genotyping and sequencing technologies, combined with a detailed knowledge of the human genetic architecture, have enabled the interrogation of genetic variants across the whole genome for their role in body-weight regulation using a hypothesis-generating approach.
Gene discovery for monogenic obesity
Many of the candidate genes and pathways linked to body-weight regulation were initially identified in mice, such as the obese ( ob ) 13 and diabetes ( db ) 14 mouse lines, in which severe hyperphagia and obesity spontaneously emerged. Using reverse genetics , the ob gene was shown to encode leptin, a hormone produced from fat, and it was demonstrated that leptin deficiency resulting from a mutation in the ob gene caused the severe obesity seen in the ob/ob mouse 15 (Fig. 3 ). Shortly after the cloning of ob , the db gene was cloned and identified as encoding the leptin receptor (LEPR) 16 . Reverse genetics was also used to reveal that the complex obesity phenotype of Agouti ‘lethal yellow’ mice is caused by a rearrangement in the promoter sequence of the agouti gene that results in ectopic and constitutive expression of the agouti peptide 17 , 18 , which antagonizes the melanocortin 1 and 4 receptors (MC1R and MC4R) 19 , 20 . This finding linked the melanocortin pathway to body-weight regulation, thereby unveiling a whole raft of new candidate genes for obesity.
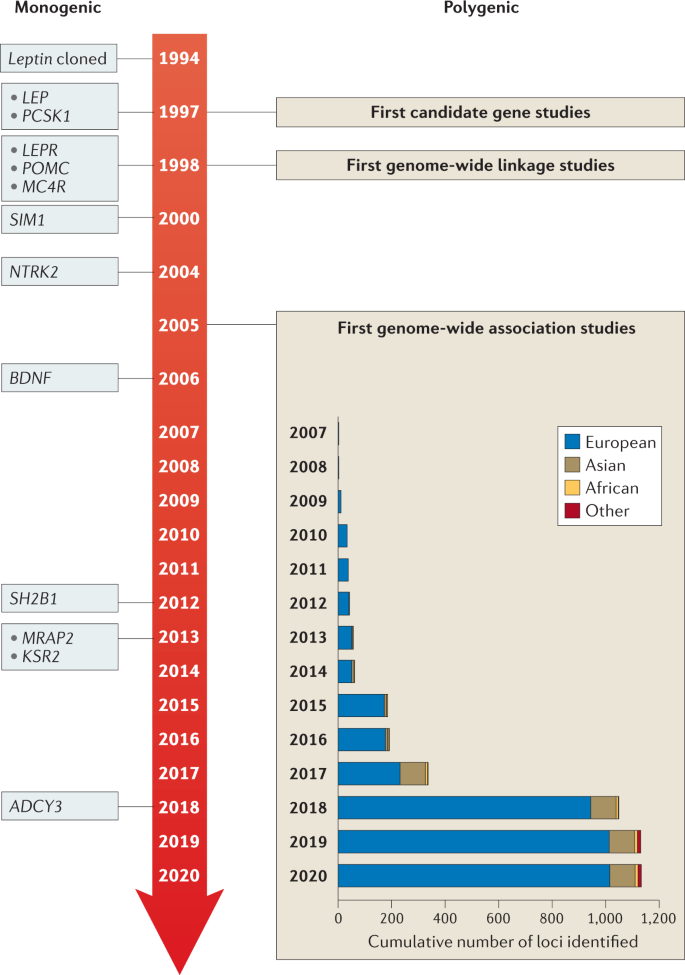
Genes identified for monogenic obesity in a given year are shown on the left. Discoveries made for polygenic obesity are shown on the right, including a cumulative count of newly discovered loci per year and by ancestry. Although candidate gene and genome-wide linkage studies became available in the late 1990s, findings were limited, and these study designs are not as frequently used as genome-wide association studies.
Once the genes for leptin and its receptor were identified, they became candidate genes for human obesity, and in 1997 the first humans with congenital leptin deficiency were identified 21 . This discovery was rapidly followed by the report of humans with mutations in the gene encoding the leptin receptor ( LEPR ) 22 , as well as in genes encoding multiple components of the melanocortin pathway, including PCSK1 (ref. 23 ), MC4R 24 , 25 , 26 and POMC 27 , 28 , 29 , all of which were found to result in severe early-onset obesity (Table 1 ).
Advances in high-throughput DNA sequencing led to candidate gene screening being replaced by WES, an unbiased approach that allows all coding sequences to be screened for mutations. However, it rapidly became clear that, whereas candidate gene studies yielded few mutations, WES identified too many potential obesity-associated variants such that the noise often masked the true causative mutations. However, with improved algorithms to predict the pathogenicity of mutations, as well as a rapidly expanding toolkit of functional assays, it has become easier to filter the likely pathogenic mutations. Several success stories have been reported in which WES has identified novel pathways and genes linked to obesity, such as the class 3 semaphorins (SEMA3A–G), which have been shown to direct the development of certain hypothalamic neurons, including those expressing pro-opiomelanocortin (POMC) 30 (see ‘Other neuronal circuits and molecules linked to severe obesity’).
Most monogenic obesity mutations have been identified in cohorts of patients with severe and early-onset (<10 years old) obesity. Additionally, as monogenic obesity often demonstrates a recessive inheritance pattern 31 , consanguinity in populations has further increased the chance of identifying mutations, owing to greater chances of homozygosity of deleterious mutations 32 . For example, studies have reported that mutations in the genes encoding leptin, LEPR and MC4R explain 30% of cases of severe obesity in children from a consanguineous Pakistani population 33 , and single-gene defects more broadly account for nearly 50% 34 .
Gene discovery for polygenic obesity
The discovery of genes that influence polygenic obesity, which is common in the general population, started off slowly with candidate gene studies and genome-wide linkage studies . The candidate gene approach was first applied in the mid-1990s and aimed to validate genes identified through human and animal models of extreme obesity for a role in common obesity (Fig. 3 ). Common variants in such candidate genes were tested for association with obesity risk, BMI or other body composition traits. Over the subsequent 15 years, hundreds of genes were studied as candidates, but variants in only six ( ADRB3 (ref. 35 ), BDNF 36 , CNR1 (ref. 37 ), MC4R 38 , PCSK1 (ref. 39 ) and PPARG 40 ) showed reproducible association with obesity outcomes. The genome-wide linkage approach made its entrance into the field towards the end of the 1990s (Fig. 3 ). Genome-wide linkage studies rely on the relatedness of individuals and test whether certain chromosomal regions co-segregate with a disease or trait across generations. Even though more than 80 genome-wide linkage studies identified >300 chromosomal loci with suggestive evidence of linkage with obesity traits, few loci were replicated and none was successfully fine-mapped to pinpoint the causal gene or genes 41 . Ultimately, candidate gene and genome-wide linkage studies, constrained by small sample sizes, sparse coverage of genetic variation across the genome and lack of replication, only had a marginal impact on the progression of gene discovery for common obesity outcomes.
However, the pace of gene discovery for common diseases accelerated with the advent of genome-wide association studies (GWAS) (Fig. 3 ). The first GWAS for obesity traits were published in 2007 and identified a cluster of common variants in the first intron of the FTO locus that was convincingly associated with BMI 42 , 43 . Many more GWAS followed and, to date, nearly 60 GWAS have identified more than 1,100 independent loci associated with a range of obesity traits 44 (Supplementary Tables 1 , 2 ).
As sample sizes increase with each consecutive GWAS, the statistical power to identify more loci also increases, in particular for loci that are less common and/or have smaller effects. For example, the first GWAS were relatively small ( n = ~5,000) and identified only the FTO locus 42 , 43 . The BMI-increasing allele of FTO is common, particularly in populations of European ancestry (minor allele frequency (MAF) 40–45%), and has a relatively large effect on BMI (0.35 kg m −2 per allele; equivalent to 1 kg for a person who is 1.7 m tall). Ten years and numerous GWAS later, the most recent GWAS for BMI included nearly 800,000 individuals, identified more than 750 loci, with MAFs as small as 1.6% and per-allele effects as low as 0.04 kg m −2 per allele (equivalent to 120 g for a person who is 1.7 m tall) 45 . Combined, these genome-wide significant loci explained 6% of variation in BMI 45 . Large-scale international collaborations have been formed, such as the Genetic Investigation for Anthropometric Traits (GIANT) consortium , that combine summary statistics of individual GWAS to generate data sets comprising hundreds of thousands of individuals. Furthermore, many GWAS efforts have maximized sample size by focusing on BMI as the primary obesity outcome, an inexpensive and easy-to-obtain measurement that is readily available in most studies. As such, the vast majority of loci have been identified first in GWAS of BMI, but their effects typically transfer to other overall adiposity outcomes.
Even though BMI is widely used, it is considered a crude proxy of overall adiposity because it does not distinguish between lean and fat mass 46 . Therefore, GWAS have been performed for more refined obesity traits, such as body fat percentage 47 , 48 , fat-free mass 49 , imaging-derived adipose tissue 50 , circulating leptin levels 51 and LEPR levels 52 . In addition, two GWAS have focused on persistent healthy thinness, assuming that genes that determine resistance to weight gain may also inform obesity prevention and weight loss maintenance 53 , 54 . Although GWAS of more refined and alternative obesity outcomes are generally much smaller than those for BMI, the phenotypes are often a more accurate representation of body-weight regulation and, as such, the loci identified tend to more often point to relevant biological pathways that underlie obesity.
Almost all GWAS loci for obesity outcomes were first identified in adults. Most of these loci also associate with obesity and/or BMI in children and adolescents, highlighting the fact that the genetic underpinning of obesity is relatively constant across the course of life 55 , 56 , 57 . Similarly to gene discovery for other common diseases, the obesity genetics field has suffered from a strong bias in population representation, with the vast majority of GWAS being performed in populations that are exclusively or predominantly of European ancestry. Nevertheless, some loci have first been discovered in populations of Asian 58 , African 59 , 60 , Hispanic or other ancestry 61 , despite their much smaller sample sizes. Broadly, loci identified in one ancestry demonstrate good transferability (that is, directionally consistent associations) across other ancestries, even though effect sizes and allele frequencies may differ. The modest-to-high genetic correlations across ancestries observed for BMI ( r = 0.78) are consistent with good transferability 62 , but also suggest that ancestry-specific loci remain to be discovered. Besides increasing the sample sizes of GWAS in populations of non-European ancestry, demographic, evolutionary and/or genomic features of specific populations (such as founder, consanguineous or isolated populations) have been leveraged for gene discovery, identifying genetic variants with large effects that are common in the discovery population, such as CREBRF , first identified in Samoan populations, and ADCY3 , first identified in the Greenlandic population, but rare or nonexistent in most others 63 , 64 , 65 , 66 . CREBRF has been shown to play a role in cellular energy storage and use, and may be implicated in cellular and organismal adaptation to nutritional stress 65 . ADCY3 colocalizes with MC4R at the primary cilia of a subset of hypothalamic neurons that have been implicated in body-weight regulation 67 .
GWAS have typically focused on biallelic, common genetic variation (MAF >5%), but have also been used to screen for the role of copy number variants (CNVs) in obesity. So far, only a few CNVs have been identified that have a convincing association with BMI, such as the 1p31.1 45-kb deletion near NEGR1 (ref. 68 ), which encodes a cell-adhesion molecule expressed in the brain 69 ; the 16p12.3 21-kb deletion upstream of GPRC5B 70 , which may modulate insulin secretion 71 ; the 10q11.22 CNV in PPYR1 (also known as NPY4R ) 72 , which encodes a potent anti-obesity agent known to inhibit food intake 73 ; and the 1p21.1 multi-allele CNV encompassing AMY1A 74 , which produces salivary α-amylase, a key enzyme in starch digestion 75 .
To determine the role of other types of variation in obesity, alternative genome-wide screens have been performed. For example, the impact of low-frequency and rare protein-coding variants has been tested using exome sequencing and exome array data 76 , 77 , 78 , 79 . It was speculated that low-frequency (MAF 1–5%) and rare (MAF <1%) variants would have larger effects than common variants, and thus be easier to detect. Nevertheless, even large-scale studies identified only a few robust associations for rare coding variants. For example, exome-wide screening based on array data from more than 400,000 individuals identified p.Tyr35Ter (rs13447324) in MC4R ; p.Arg190Gln (rs139215588) and p.Glu288Gly (rs143430880) in GIPR , which stimulates insulin secretion and mediates fat deposition 80 ; p.Arg95Ter (rs114285050) in GRP151 , which modulates habenular function that controls addiction vulnerability 81 ; and p.Arg769Ter (rs533623778) in PKHD1L1 , which has been involved in cancer development 77 , 78 . A recent study that leveraged WES data for more than 600,000 individuals identified 16 genes for which the burden of rare nonsynonymous variants was associated with BMI, including five brain-expressed G protein-coupled receptors ( CALCR , MC4R , GIPR , GPR151 and GPR75 ) 79 .
As obesity is a complex, multifactorial condition, some GWAS have integrated demographic factors (such as sex and age 82 ) and environmental factors (such as physical activity 83 , diet 84 or smoking 85 ) into their analyses. Despite sample sizes of more than 200,000 individuals, these genome-wide gene-by-environment (G×E) interaction analyses remain challenging and so far only 12 loci have been identified, the effects of which on obesity are attenuated or exacerbated by non-genetic factors. Nevertheless, the G×E interaction between the FTO locus and a healthy lifestyle has been robustly replicated. Specifically, increased physical activity or a healthy diet can attenuate the effect of the FTO locus on obesity risk by 30–40% 86 , 87 .
The increasing availability of large-scale cohorts and biobanks, such as the UK Biobank , the Million Veterans Project , All of Us , Biobank Japan and 23andMe , combined with ongoing work by the GIANT consortium, will boost sample sizes further to easily exceed 4 million participants in meta-analyses, expediting the discovery of many more obesity-associated loci. However, translation of GWAS-identified loci into new biological insights remains a major challenge.
From genes to biology
Despite the difficulties in validating causative mutations and variants, genetic studies into both rare and common obesity over the past two decades have revealed two surprisingly cogent, overarching biological messages: first, the leptin–melanocortin pathway is a key appetitive control circuit 31 , 88 (Fig. 4 ); and second, genes that are either enriched or exclusively expressed within the brain and CNS have a central role in obesity 89 .
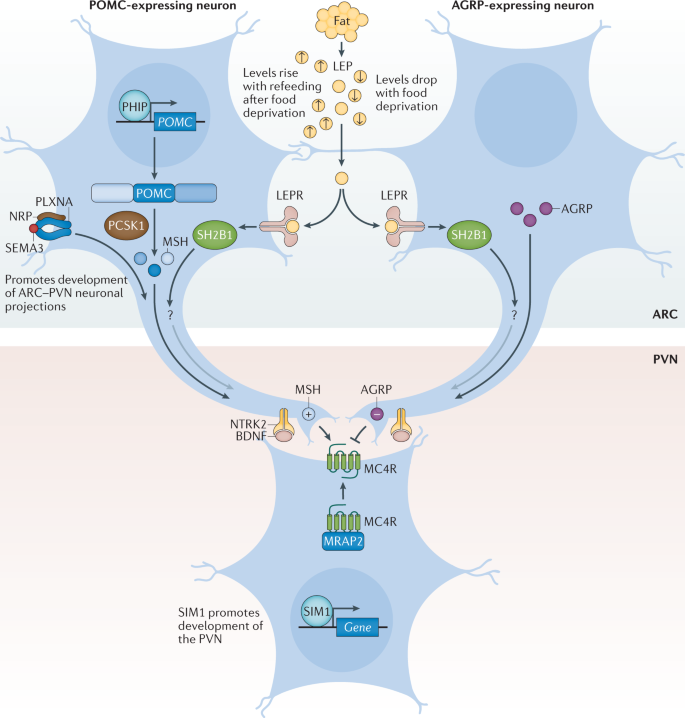
Pro-opiomelanocortin (POMC)-expressing neurons and agouti-related protein (AGRP)-expressing neurons within the arcuate nucleus of the hypothalamus (ARC) act to sense circulating leptin (LEP) levels, which reflect fat mass. These neurons signal to melanocortin 4 receptor (MC4R)-expressing neurons in the paraventricular nucleus of the hypothalamus (PVN), which controls appetite, thus linking long-term energy stores to feeding behaviour. Binding of class 3 semaphorins (SEMA3) to their receptors NRP and PLXNA influences the projection of POMC neurons to the PVN. Binding of brain-derived neurotrophic factor (BDNF) to its receptor neurotrophic receptor tyrosine kinase 2 (NTRK2) is thought to be an effector of leptin-mediated synaptic plasticity of neurons, including those in the ARC and PVN. The transcription factor SIM1 is crucial for the proper development of the PVN. +, agonist; −, antagonist; LEPR, leptin receptor; MRAP2, melanocortin receptor accessory protein 2; MSH, melanocyte-stimulating hormone; SH2B1, SH2B adaptor protein 1.
The leptin–melanocortin pathway and MC4R
Leptin is a key hormone secreted by adipocytes, which circulates at levels in proportion to fat mass 90 . Leptin also responds to acute changes in energy state, as its levels decrease with food deprivation and are restored during re-feeding. Administration of leptin to fasted mice abrogates many of the neuroendocrine consequences of starvation, suggesting that the normal biological role of leptin is to initiate the starvation response 91 . Leptin signals through the LEPR, which exists in several different isoforms. However, obesity-related effects of leptin are predominantly mediated by a long isoform that contains an intracellular domain (LEPRb), which is expressed in various regions of the CNS 90 .
Within the arcuate nucleus (ARC) of the hypothalamus, LEPRb is found on two populations of neurons at the heart of the melanocortin pathway, one of which expresses POMC and the other agouti-related protein (AGRP) 92 (Fig. 4 ). POMC is post-translationally processed by prohormone convertases to produce several biologically active moieties, including β-lipotrophin and β-endorphin, and, crucially, the melanocortin peptides adrenocorticotrophin (ACTH) and α-, β- and γ-melanocyte-stimulating hormone (MSH) 93 . The ARC POMC neurons project to MC4R neurons within the paraventricular nucleus (PVN) where melanocortin peptides signal to decrease food intake 92 . By contrast, AGRP acts as an endogenous antagonist of MC4R to increase food intake 92 , 94 . MC3R is another centrally expressed receptor that binds to both melanocortin peptides and AGRP; however, as mice with targeted deletions in the gene are not obese but instead have altered fat to lean mass ratio, MC3R is less likely to be related to food intake and more likely to be involved in nutrient partitioning 95 , 96 .
We can state with confidence that the fine balance of melanocortinergic agonism and AGRP antagonism of MC4R, in response to peripheral nutritional cues such as leptin, plays a central part in influencing appetitive drive 92 . The genetic evidence clearly supports this contention, with mutations in most genes of the melanocortin pathway resulting in hyperphagia and severe obesity in both humans and mice 31 , 88 . In fact, the vast majority of single-gene disruptions causing severe early-onset obesity in humans fall within this pathway, including LEPR , POMC , AGRP , MCR4R , PCSK1 (ref. 23 ), SH2B1 (ref. 97 ), PHIP 98 , MRAP2 (ref. 99 ) and SIM1 (ref. 100 ) (Fig. 4 ; Table 1 ). Mutations in MC4R in particular, are the most common single-gene defect leading to hyperphagia and obesity. Pathogenic mutations in MC4R are found in up to 5% of cases of severe childhood obesity 101 and up to 0.3% of the general population 101 , 102 . Of note, the degree of receptor dysfunction, as measured by in vitro assays, can predict the amount of food eaten at a test meal by an individual harbouring that particular mutation 101 . Thus MC4R does not act in a binary on/off manner, but as a rheostat; put simply, the melanocortin pathway is a ‘tunable’ system. In addition to regulating food intake, it also regulates food preference, with individuals who carry mutations in MC4R showing a preference for food with higher fat content 103 .
The importance of the melanocortin pathway in regulating feeding behaviour is highlighted by the identification of naturally occurring mutations in pathway genes in a wide range of different species where the appropriate selection pressure has been present (Table 1 ). For example, studies have found that 20–25% of Labrador retrievers, which are known to be more food-motivated than other dog breeds, carry a 14-bp deletion in POMC that disrupts the β-MSH and β-endorphin coding sequences and is associated with greater food motivation and increased body weight 104 . Also, certain breeds of pig have been shown to carry MC4R missense mutations that are associated with fatness, growth and food intake traits 105 . MC4R mutations even contribute to the adaptation and survival of blind Mexican cavefish to the nutrient-poor conditions of their ecosystem 106 .
Other neuronal circuits and molecules linked to severe obesity
It is now clear that in addition to engaging classical neuropeptide–receptor systems within the brain, leptin also rapidly modifies synaptic connections between neurons 107 , and that this structural plasticity is crucial to its downstream functions. One of the ways in which this plasticity is thought to be achieved is via brain-derived neurotrophic factor (BDNF) signalling to its receptor TrkB. BDNF is widely expressed in the CNS where it plays an important part in neuronal development 108 , 109 . In the hippocampus, BDNF contributes to synaptic plasticity and long-term potentiation associated with memory and learning 110 . However, evidence has emerged that implicates BDNF and TrkB in the regulation of mammalian eating behaviour and energy balance 111 . BDNF is downregulated by nutritional deprivation and upregulated by leptin within the ventromedial nucleus (VMN) of the hypothalamus 112 , although this regulation is probably indirect, as very few VMN BDNF neurons express the LEPR 113 (Fig. 4 ) and some evidence indicates that it acts at least in part downstream of melanocortin signalling 112 . Crucially, genetic disruption of BDNF 114 , 115 and TrkB 112 , 116 in both humans and mice results in hyperphagia and severe obesity.
Another group of neuronal proteins important in the development of neuronal circuitry and linked to energy balance are the class 3 semaphorins (SEMA3A–G). A study in humans found that 40 rare loss-of-function variants in SEMA3A–G and their receptors (PLXNA1–4, NRP1 and NRP2) were significantly enriched in 982 individuals with severe obesity compared with 4,449 controls 30 . Disruption of several of these genes in zebrafish caused increased somatic growth and/or adiposity, and experiments with mouse hypothalamic explants suggest that SEMA3 signalling via NRP2 receptors drives the development of POMC projections from the ARC to the PVN 30 . However, given that these results are from a single study, more data are required to confirm the exact role of class 3 semaphorins in energy homeostasis.
Insights from genetic loci linked to common obesity
Unlike candidate gene studies, GWAS make no a priori assumptions about the underlying biology that links genetic variants to a disease of interest. While this agnostic approach allows for new biological insights, the vast majority of GWAS-identified variants map to the non-coding parts of genes or to regions between genes. As such, they do not directly disrupt the protein-coding regions, but instead overlap with regulatory elements that influence expression of genes in close proximity or even over long distances.
However, even if the causative genes are unknown, pathway, tissue and functional enrichment analyses based on the genes located in the GWAS loci can provide insights into potential mechanisms. Since the very first GWAS for BMI 68 , 117 , such analyses have pointed to the CNS being a key player in body-weight regulation, consistent with insights from human and animal models of extreme obesity. Recent analyses that include the latest BMI-associated loci, combined with updated multi-omics databases and advanced computational tools, have further refined these observations. In addition to the hypothalamus and pituitary gland (which are both known appetite regulation sites), other brain areas have been highlighted, including the hippocampus and the limbic system (which are involved in learning, cognition and emotion) and the insula and the substantia nigra (which are related to addiction and reward) 58 , 89 , 118 , 119 . The enrichment of immune-related cells (such as lymphocytes and B cells) and adipose tissue was found to be weaker 58 .
Although enrichment analyses provide preliminary insights into the broad biology represented by genes in the GWAS loci, determining which genes, variants and/or underlying mechanisms are causal has proved an arduous task. For example, the FTO locus, which was identified more than a decade ago and harbours six genes, is the most extensively studied GWAS-identified obesity locus (Fig. 5 ). Despite its highly significant and widely replicated association with obesity 120 , the causal variants and/or genes in the FTO locus have not yet been pinpointed with convincing evidence, and the mechanisms by which the locus affects body weight have not been fully elucidated. Early functional follow-up analyses suggested that FTO itself might be responsible, as Fto deficiency in mice results in a lean phenotype, whereas Fto overexpression is associated with increased body weight 121 , 122 . Studies in mice have suggested that FTO plays a role in cellular nutrient sensing 123 , 124 . Other studies found evidence that FTO influences brain regions that affect appetite, reward processing and incentive motivation by regulating ghrelin levels in humans 125 or by controlling dopaminergic signalling in mice 126 , 127 . In addition, variants in the FTO locus were shown to alter a regulatory element that controls the transcription of Rpgrip1l in mice, a ciliary gene located immediately upstream of Fto 128 , 129 , 130 . Mice with reduced Rpgrip1l activity exhibit hyperphagic obesity, possibly mediated through diminished leptin signalling 128 , 129 , 130 . In recent years, studies in human and animal models have shown that variants in the FTO locus directly interact with the promoter of Irx3 , a gene located 0.5 Mb downstream of FTO . Irx3 -deficient mice were found to exhibit weight loss and increased metabolic rate with browning of white adipose tissue, without changes in physical activity or appetite 131 , 132 . Further in-depth functional characterization showed that rs1421085 in the FTO locus disrupts a conserved binding motif for the transcriptional repressor ARID5B, which leads to a doubling of IRX3 and IRX5 expression during early adipocyte differentiation 132 . The authors argue that increased expression of these genes results in a developmental shift from energy-dissipating beige adipocytes to energy-storing white adipocytes, a fivefold reduction in mitochondrial thermogenesis and increased lipid storage 132 . However, given that multiple studies have shown that the FTO locus is robustly associated with food intake, with no evidence to date linking it to changes in energy expenditure, the relevance of this observation to the actual observed human phenotype still needs to be explored 133 . A recent study reports that the FTO locus affects gene expression in multiple tissues, including adipose tissue and brain, and, more broadly, that the genetic architecture of disease-associated loci may involve extensive pleiotropy and allelic heterogeneity across tissues 134 .
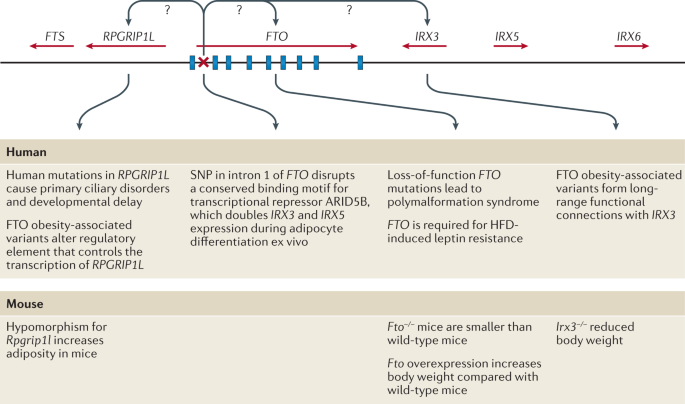
FTO contains nine exons (depicted by blue rectangles) and the body mass index (BMI)-associated SNP identified in genome-wide association studies (depicted by a red ×) maps to intron 1. IRX3 and RPGRIP1L have both been proposed to be the causal genes for obesity within the locus and to act on body weight through distinct mechanisms. HFD, high-fat diet.
Besides the FTO locus, functional follow-up analyses have been performed for only a few obesity-associated GWAS loci. For example, early studies identified a cluster of variants just downstream of TMEM18 (refs 68 , 117 ). TMEM18 encodes a poorly characterized transmembrane protein that is highly conserved across species and widely expressed across tissues, including in several regions of the brain 135 , 136 . Tmem18 deficiency in mice results in a higher body weight owing to increased food intake, whereas Tmem18 overexpression reduces food intake and limits weight gain 136 . A knockdown experiment in Drosophila melanogaster suggests that TMEM18 affects carbohydrate and lipid levels by disrupting insulin and glucagon signalling 137 .
Two other GWAS loci for which functional analyses have been performed are located just upstream of CADM1 (ref. 82 ) and in CADM2 (ref. 70 ), genes that encode cell-adhesion proteins of the immunoglobulin superfamily and mediate synaptic assembly in the CNS 138 . The BMI-increasing alleles at each locus are associated with increased expression of CADM1 and CADM2 in the hypothalamus 139 , 140 . Deficiency of either Cadm1 or Cadm2 in mice results in a lower body weight and increased insulin sensitivity, glucose tolerance and energy expenditure without any change in food intake 139 , 140 . Conversely, increased neuronal expression of either Cadm1 or Cadm2 is associated with elevated body weight 139 , 140 . Furthermore, CADM1 is expressed in POMC neurons and Cadm1 deficiency leads to an increase in the number of excitatory synapses, suggestive of an increased synaptic plasticity 140 . Cadm2 -deficient mice exhibit increased locomotor activity and higher core body temperature 139 .
Another GWAS locus, just upstream of NEGR1 , harbours two deletions associated with increased obesity risk 68 , 117 , 141 . These deletions do not overlap with the coding sequence of NEGR1 , but encompass a conserved transcription factor-binding site for NKX6.1 , a potent transcriptional repressor 68 , 141 . Loss of binding of NKX6.1 leads to higher NEGR1 expression 141 , which is consistent with the observation that BMI-increasing alleles (that is, deletions) at this locus are associated with higher NEGR1 expression in the brain. Similar to CADM1 and CADM2, NEGR1 is a cell-adhesion molecule of the immunoglobulin superfamily that is expressed in several regions of the brain and has been shown to have a role in brain connectivity 69 , 142 , a process believed to be important in obesity 143 . NEGR1 deficiency in mice was shown to result in lower body weight, mainly due to reduced lean mass, mediated by lower food intake 144 . However, two other functional studies, one in mice and one in rats, found that knockdown of Negr1 expression resulted in the opposite phenotype — increased body weight and food intake 145 , 146 . While NEGR1 deficiency in mice was found to impair core behaviours, so far, findings and proposed mechanisms are not fully aligned 69 , 147 , 148 , 149 .
Taken together, functional follow-up analyses for these loci are slowly expanding our understanding of the pathophysiology that drives weight gain. However, many more obesity-associated loci are waiting to be translated into new biological insights. A major hurdle in translating GWAS loci into plausible candidate genes and appropriate paradigms for functional research is the annotation of the associated variants in a locus. Defining the regulatory function of the non-coding variants, identifying their putative effector transcripts and determining their tissues of action remains an ongoing challenge. The advent of high-throughput genome-scale technologies for mapping regulatory elements, combined with comprehensive multi-omics databases, advanced computational tools and the latest genetic engineering and molecular phenotyping approaches, is poised to speed up the translation of GWAS loci into meaningful biology 150 .
Converging results from monogenic and polygenic forms of obesity
Gene discovery is often dichotomized by allele frequency and disease prevalence; that is, mutations are sought for monogenic forms of obesity and common variants for polygenic obesity (Fig. 2 ). However, it is increasingly recognized that monogenic and polygenic forms of obesity are not discrete entities. Instead, they lie on a spectrum and share — at least in part — the same biology. As GWAS have continued to discover more obesity-associated loci, an increasing number of these loci harbour genes that were first identified for extreme and early-onset obesity in humans or animal models, including MC4R 151 , 152 , BDNF 117 , SH2B1 (refs 68 , 117 ), POMC 70 , LEP 51 , 153 , LEPR 52 , 154 , NPY 155 , SIM1 (ref. 155 ), NTRK2 (ref. 58 ), PCSK1 (ref. 154 ) and KSR2 (ref. 77 ). In fact, most of these genes encode components of the leptin–melanocortin and BDNF–TrkB signalling pathways (Table 1 ). Thus, whereas genetic disruption of components of these pathways results in severe obesity, genetic variants in or near these same genes that have more subtle effects on their expression will influence where an individual might sit in the normal distribution of BMI.
Although most genes have been first identified for extreme forms of obesity, a locus harbouring ADCY3 was first identified in GWAS for common obesity 77 , and ADCY3 was subsequently confirmed as having a role in extreme obesity 63 , 64 . ADCY3 encodes an adenylate cyclase that catalyses the synthesis of cAMP, an important second messenger in signalling pathways. There is some evidence that ADCY3 (adenylate cyclase) colocalizes with MC4R at the primary cilia of PVN neurons 67 and that cilia are required specifically on MC4R-expressing neurons for the control of energy homeostasis 156 . In mice, disruption of Adcy3 or Mc4r in the cilia of these neurons impairs melanocortin signalling, resulting in hyperphagia and obesity 67 .
As more GWAS loci are reported, we expect that findings across different lines of obesity research will continue to converge, providing accumulating evidence for new biology.
From genes to clinical care
Genetic insights from gene discovery efforts are increasingly being used in the context of precision medicine in ways that directly affect health. Knowing a patient’s genotype may enable a more precise diagnosis of the type of obesity, which in turn allows the prescription of personalized treatment or prevention strategies. Furthermore, knowing an individual’s genetic susceptibility to obesity early in life may help to more accurately predict those most at risk of gaining weight in the future.
Use of genotype information in treatment of obesity
When a disease is caused by a single mutation and the environmental contribution is limited, as is the case for some forms of extreme and early-onset obesity, a genetic test can be instrumental in correctly diagnosing patients. Although no standard genetic testing panel is currently available for extreme and early-onset obesity, some clinics, research centres and pharmaceutical companies sequence well-known candidate genes to identify the functional mutation that may be the cause of a patient’s excess body weight. Such a genetic diagnosis can lessen the feelings of guilt and blame for the patient, and alleviate social stigma and discrimination. Importantly, a genetic diagnosis can inform disease prognosis and, in some cases, it will determine treatment. To date, there are two treatments for obesity that are tailored to patient genotype.
The prototype of genotype-informed treatment for obesity is the administration of recombinant human leptin in patients who are leptin-deficient owing to mutations in the LEP gene 157 , 158 . Although congenital leptin deficiency is exceptionally rare (only 63 cases have been reported to date 28 ), leptin replacement therapy has been remarkably beneficial for these patients by substantially reducing food intake, body weight and fat mass, and normalizing endocrine function 157 , 158 . It has literally transformed their lives.
The second genotype-informed treatment for obesity is setmelanotide, a selective MC4R agonist that was recently approved by the FDA for rare monogenic obesity conditions including LEPR, PCSK1 and POMC deficiency 159 . Setmelanotide acts as a substitute for the absent MSH in patients with POMC deficiency owing to mutations in POMC or PCSK1 , and in patients with LEPR deficiency owing to mutations in LEPR , which is essential for POMC function 160 , 161 , 162 . Daily subcutaneous injection of setmelanotide results in substantial weight loss and in reduction of hunger 160 , 161 , 162 . After a 1-year treatment with setmelanotide in phase III trials, patients with POMC deficiency lost on average 25.6% of their initial weight, with 80% of patients achieving at least a 10% weight loss 162 . The adverse effects of setmelanotide treatment are minor, and include hyperpigmentation, nausea and/or vomiting, penile erection and injection site reactions. Weight loss in patients with LEPR deficiency was less pronounced; on average, they lost 12.5% of their initial weight, with only 45% of patients achieving at least a 10% weight loss 162 . The difference in weight loss between the two patient groups may be because POMC deficiency directly affects the production of MC4R ligands (α-MSH and β-MSH), whereas LEPR deficiency affects signalling upstream of POMC 162 . As such, setmelanotide may be able to completely restore MC4R signalling in POMC deficiency, but only partially in LEPR deficiency. Even though the average weight loss in POMC-deficient patients was twice that in LEPR-deficient patients, the reduction in hunger was substantially larger in LEPR-deficient patients (−43.7%) than in POMC-deficient patients (−27.1%) 162 . The reasons for the discrepancy between weight loss and reduction in hunger remain to be studied in greater depth. It has been estimated that in the USA, >12,800 individuals carry mutations in the melanocortin pathway for whom setmelanotide may be more effective for weight loss than any other treatment 163 . Although 12,800 carriers represent only a fraction (0.004%) of the adult population in the USA, and not all of these mutation carriers are overweight or obese, for the patients for whom setmelanotide is effective, it may end a lifelong battle to lose weight 163 . In patients without genetic defects, neither setmelanotide nor leptin administration have, to date, demonstrated a substantial effect on weight loss 164 , 165 .
These two genotype-informed treatments show how insight into the underlying biological mechanisms can guide the development of molecules and medications that restore impaired pathways, at least in monogenic forms of obesity caused by deficiency of one protein. Nevertheless, there remain substantial obstacles in the transition from conventional to precision medicine for monogenic obesity, which would require the adoption of systematic WES for individuals suspected to be carriers of deleterious mutations, and eventually even standardized screening at birth. We are clearly a long way from such a scenario at present.
Use of genotype information in prediction of obesity
As more variants are being discovered for common obesity, there is a growing expectation that genetic information will soon be used to identify individuals at risk of obesity. Knowing a person’s genetic susceptibility would allow for a more accurate prediction of who is at risk of gaining weight and give an opportunity to intervene earlier to prevent obesity more effectively. Genetic susceptibility to complex disease, including obesity, is assessed using a polygenic score (PGS). PGSs to assess obesity susceptibility are based on GWAS for BMI (PGS BMI ), the latest of which includes data on more than 2 million variants and explains 8.4% of the variation in BMI 166 . The average BMI of individuals with a high PGS BMI (top decile) is 2.9 kg m −2 (equivalent to 8 kg in body weight) higher and their odds of severe obesity (BMI ≥40 kg m −2 ) is 4.2-fold higher than those with a lower PGS BMI (lowest nine deciles) 166 .
Despite these strong associations with BMI and obesity, the predictive performance of the PGS BMI is weak, which is unsurprising given its limited explained variance. For example, using the same PGS BMI and data from the UK Biobank, we estimate that the area under the receiver operating characteristic curve (AUC ROC ) is only 0.64 to predict obesity. This means that the probability that an individual with obesity has a higher PGS BMI than an individual without obesity is 0.64. However, for a PGS to have clinical utility, the AUC ROC needs to be much higher (>0.80). In addition, we calculated the extent to which a PGS BMI ≥90th percentile correctly classifies individuals with obesity (Fig. 6 ). We found that such a predictive test (PGS BMI ≥90th percentile) has a positive predictive value of 0.43, meaning that of those who were predicted to develop obesity, only 43% actually developed obesity. Its sensitivity is 0.19, which means that of the individuals who developed obesity, only 19% had been correctly classified by the PGS BMI . Given that the current treatment options for obesity are low risk, or even generally beneficial, the high false-positive rate is less concerning than the low sensitivity, as some at-risk individuals may miss the opportunity for early prevention.
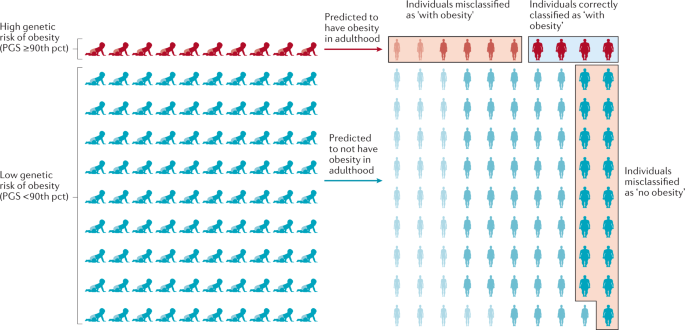
The outcome is illustrated for a polygenic score (PGS) that assumes that individuals with a score in the highest decile (≥90th percentile (pct)) will develop obesity, has a positive predictive value of 0.4 and a sensitivity of 0.19. Of ten individuals with a high score classified by the PGS as ‘with obesity’, four will be classified correctly but the other six will be misclassified and will not develop obesity — a positive predictive value of 0.4. Likewise, 17 of the 90 individuals with a score <90th pct who are predicted to not develop obesity, will develop obesity. Thus, only four of the 21 individuals who developed obesity were correctly classified by the PGS — a sensitivity of 0.19. Misclassified individuals are indicated by the red boxes, individuals correctly classified as ‘with obesity’ are indicated by a blue box. Adapted with permission from ref. 170 , Elsevier.
Thus, the current PGS BMI has a high rate of misclassification and does not reliably predict who is at risk of developing obesity and who is not. The predictive ability of PGSs are expected to improve as GWAS increase in sample size and algorithms to calculate the scores become more refined. Nevertheless, given the importance of socio-demographic, lifestyle and clinical risk factors in the aetiology of obesity, it is unlikely that a PGS BMI will ever be able to accurately predict obesity on its own. Instead, effective prediction models will have to include genetic and non-genetic factors, including a broad spectrum of demographic, environmental, clinical and possibly molecular markers, as well.
Conclusions and future perspectives
What initially began as two apparently distinct approaches, one studying rare Mendelian causes of extreme obesity, and the other exploring complex polygenic influences of population body-weight distribution, have eventually converged on the central role of the brain in regulating body weight. In particular, both approaches have highlighted the roles of the leptin–melanocortin pathway and TrkB–BDNF signalling. Perhaps it seems obvious now, but it was by no means certain that, just because genetic disruption of a pathway resulted in a severe phenotype, polymorphisms within that same pathway would produce a more subtle and nuanced result.
The GWAS approach is hypothesis-free, with the promise to reveal new genes that point to new biology and pathways. However, for the vast majority of the >1,000 GWAS-identified loci, we do not know which genes are causal, what cells, tissues and organs they act in to affect body weight, and we do not understand the underlying mechanisms. The translation from variant to function is a well-known challenge 167 , but with increasing availability of new omics data, high-throughput technologies and advanced analytical approaches, there is an unprecedented opportunity to speed up the translation of hundreds of GWAS loci.
Sample size remains a major driver for gene discovery. In an ongoing collaboration that combines data from more than 3 million individuals of diverse ancestry from the GIANT consortium, the UK Biobank and 23andMe, the number of BMI-associated GWAS loci is set to double. Also, a recent WES effort of more than 640,000 individuals has demonstrated that rare mutations are discoverable when sample sizes are sufficiently large 79 . However, alternative study designs, a focus on more refined phenotypes or a focus on population subgroups (that is, more homogeneous groups of individuals with similar outcomes) could further add to gene discovery.
Translation of only a few dozen of the GWAS-identified loci could tremendously improve our insights into the biology of obesity and possibly reveal new therapeutic targets. It would also take us a little closer to the ‘holy grail’ — the ability to move away from a failed ‘one-size-fits-all’ strategy, and towards true precision medicine for obesity, metabolic disease and other diet-related illnesses.
GBD 2015 Obesity Collaborators. Health effects of overweight and obesity in 195 countries over 25 years. N. Engl. J. Med. 377 , 13–27 (2017).
Article Google Scholar
Must, A. et al. The disease burden associated with overweight and obesity. JAMA 282 , 1523–1529 (1999).
Article CAS PubMed Google Scholar
Fontaine, K. R. & Barofsky, I. Obesity and health-related quality of life. Obes. Rev. 2 , 173–182 (2001).
Bhattacharya, I., Ghayor, C., Perez Dominguez, A. & Weber, F. E. From influenza virus to novel corona virus (SARS-CoV-2)—the contribution of obesity. Front. Endocrinol. 11 , 556962 (2020).
Petrilli, C. M. et al. Factors associated with hospital admission and critical illness among 5279 people with coronavirus disease 2019 in New York City: prospective cohort study. BMJ 369 , m1966 (2020).
Article PubMed PubMed Central Google Scholar
Cummings, M. J. et al. Epidemiology, clinical course, and outcomes of critically ill adults with COVID-19 in New York City: a prospective cohort study. Lancet 395 , 1763–1770 (2020).
Article CAS PubMed PubMed Central Google Scholar
Zhao, X. et al. Obesity increases the severity and mortality of influenza and COVID-19: a systematic review and meta-analysis. Front. Endocrinol. 11 , 595109 (2020).
Abarca-Gómez, L. et al. Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128.9 million children, adolescents, and adults. Lancet 390 , 2627–2642 (2017).
Maes, H. H., Neale, M. C. & Eaves, L. J. Genetic and environmental factors in relative body weight and human obesity. Behav. Genet. 27 , 325–351 (1997).
Elks, C. E. et al. Variability in the heritability of body mass index: a systematic review and meta-regression. Front. Endocrinol. 3 , 29 (2012). This paper reports a large-scale meta-analysis of heritability data of twin and family studies .
Chami, N., Preuss, M., Walker, R. W., Moscati, A. & Loos, R. J. F. The role of polygenic susceptibility to obesity among carriers of pathogenic mutations in MC4R in the UK Biobank population. PLoS Med. 17 , e1003196 (2020). This study shows that the effect of MC4R mutations on BMI and obesity risk is attenuated by the polygenic background .
Kaur, Y., de Souza, R. J., Gibson, W. T. & Meyre, D. A systematic review of genetic syndromes with obesity. Obes. Rev. 18 , 603–634 (2017).
Ingalls, A. M., Dickie, M. M. & Snell, G. D. Obese, a new mutation in the house mouse. J. Hered. 41 , 317–318 (1950).
Hummel, K. P., Dickie, M. M. & Coleman, D. L. Diabetes, a new mutation in the mouse. Science 153 , 1127–1128 (1966).
Zhang, Y. et al. Positional cloning of the mouse obese gene and its human homologue. Nature 372 , 425–432 (1994). This paper reports the cloning of leptin, which provided the first molecular evidence that feeding and regulation of body weight had a hormonal basis .
Article CAS Google Scholar
Chen, H. et al. Evidence that the diabetes gene encodes the leptin receptor: identification of a mutation in the leptin receptor gene in db / db mice. Cell 84 , 491–495 (1996). This paper reports the cloning of the LEPR and the localization of its signalling version, which highlights the role of the brain in the control of appetitive behaviour .
Bultman, S. J., Michaud, E. J. & Woychik, R. P. Molecular characterization of the mouse agouti locus. Cell 71 , 1195–1204 (1992).
Miller, M. W. et al. Cloning of the mouse agouti gene predicts a secreted protein ubiquitously expressed in mice carrying the lethal yellow mutation. Genes Dev. 7 , 454–467 (1993).
Lu, D. et al. Agouti protein is an antagonist of the melanocyte-stimulating-hormone receptor. Nature 371 , 799–802 (1994).
Fan, W., Boston, B. A., Kesterson, R. A., Hruby, V. J. & Cone, R. D. Role of melanocortinergic neurons in feeding and the agouti obesity syndrome. Nature 385 , 165–168 (1997).
Montague, C. T. et al. Congenital leptin deficiency is associated with severe early-onset obesity in humans. Nature 387 , 903–908 (1997). This work demonstrates that leptin signalling is also relevant in the human context, and provides early evidence, together with mutations in PCSK1 , of a monogenic cause of severe human obesity .
Clement, K. et al. A mutation in the human leptin receptor gene causes obesity and pituitary dysfunction. Nature 392 , 398–401 (1998). This work confirms the observations from mice about leptin signalling to the brain .
Jackson, R. S. et al. Obesity and impaired prohormone processing associated with mutations in the human prohormone convertase 1 gene. Nat. Genet. 16 , 303–306 (1997). This study, together with mutations in the leptin gene, provides early evidence of a monogenic cause of severe human obesity, and also highlights the role of the nascent melanocortin pathway in body-weight regulation .
Huszar, D. et al. Targeted disruption of the melanocortin-4 receptor results in obesity in mice. Cell 88 , 131–141 (1997).
Yeo, G. S. et al. A frameshift mutation in MC4R associated with dominantly inherited human obesity. Nat. Genet. 20 , 111–112 (1998).
Vaisse, C., Clement, K., Guy-Grand, B. & Froguel, P. A frameshift mutation in MC4R is associated with a dominant form of obesity. Nat. Genet. 20 , 113–114 (1998). This paper, together with Yeo et al. (1998), shows that heterozygous mutations in MC4R result in severe human obesity, establishing the role of the central melanocortin pathway in regulating human appetitive behaviour .
Krude, H. et al. Severe early-onset obesity, adrenal insufficiency and red hair pigmentation caused by POMC mutations in humans. Nat. Genet. 19 , 155–157 (1998). This paper provides direct evidence that melanocortin peptides play a key role in the regulation of energy homeostasis .
Yaswen, L., Diehl, N., Brennan, M. B. & Hochgeschwender, U. Obesity in the mouse model of pro-opiomelanocortin deficiency responds to peripheral melanocortin. Nat. Med. 5 , 1066–1070 (1999).
Challis, B. G. et al. Mice lacking pro-opiomelanocortin are sensitive to high-fat feeding but respond normally to the acute anorectic effects of peptide-YY(3-36). Proc. Natl Acad. Sci. USA 101 , 4695–4700 (2004).
van der Klaauw, A. A. et al. Human semaphorin 3 variants link melanocortin circuit development and energy balance. Cell 176 , 729–742.e18 (2019).
Farooqi, S. & O’Rahilly, S. Genetics of obesity in humans. Endocr. Rev. 27 , 710–718 (2006).
Saeed, S., Arslan, M. & Froguel, P. Genetics of obesity in consanguineous populations: toward precision medicine and the discovery of novel obesity genes. Obesity 26 , 474–484 (2018).
Article PubMed Google Scholar
Saeed, S. et al. Genetic variants in LEP, LEPR, and MC4R explain 30% of severe obesity in children from a consanguineous population. Obesity 23 , 1687–1695 (2015).
Saeed, S. et al. Genetic causes of severe childhood obesity: a remarkably high prevalence in an inbred population of Pakistan. Diabetes 69 , 1424–1438 (2020).
Kurokawa, N. et al. The ADRB3 Trp64Arg variant and BMI: a meta-analysis of 44 833 individuals. Int. J. Obes. 32 , 1240–1249 (2008).
Shugart, Y. Y. et al. Two British women studies replicated the association between the Val66Met polymorphism in the brain-derived neurotrophic factor (BDNF) and BMI. Eur. J. Hum. Genet. 17 , 1050–1055 (2009).
Benzinou, M. et al. Endocannabinoid receptor 1 gene variations increase risk for obesity and modulate body mass index in European populations. Hum. Mol. Genet. 17 , 1916–1921 (2008).
Wang, D. et al. Association of the MC4R V103I polymorphism with obesity: a Chinese case–control study and meta-analysis in 55,195 individuals. Obesity 18 , 573–579 (2010).
Nead, K. T. et al. Contribution of common non-synonymous variants in PCSK1 to body mass index variation and risk of obesity: a systematic review and meta-analysis with evidence from up to 331 175 individuals. Hum. Mol. Genet. 24 , 3582–3594 (2015).
Tonjes, A., Scholz, M., Loeffler, M. & Stumvoll, M. Association of Pro12Ala polymorphism in peroxisome proliferator-activated receptor gamma with pre-diabetic phenotypes: meta-analysis of 57 studies on nondiabetic individuals. Diabetes Care 29 , 2489–2497 (2006).
Rankinen, T. et al. The human obesity gene map: the 2005 update. Obesity 14 , 529–644 (2006).
Frayling, T. M. et al. A common variant in the FTO gene is associated with body mass index and predisposes to childhood and adult obesity. Science 316 , 889–894 (2007). This paper describes the first GWAS (for type 2 diabetes) to identify a locus ( FTO ) robustly associated with BMI .
Scuteri, A. et al. Genome-wide association scan shows genetic variants in the FTO gene are associated with obesity-related traits. PLoS Genet. 3 , e115 (2007).
Buniello, A. et al. The NHGRI-EBI GWAS Catalog of published genome-wide association studies, targeted arrays and summary statistics 2019. Nucleic Acids Res. 47 , D1005–D1012 (2019).
Yengo, L. et al. Meta-analysis of genome-wide association studies for height and body mass index in approximately 700 000 individuals of European ancestry. Hum. Mol. Genet. 27 , 3641–3649 (2018).
Javed, A. et al. Diagnostic performance of body mass index to identify obesity as defined by body adiposity in children and adolescents: a systematic review and meta-analysis. Pediatr. Obes. 10 , 234–244 (2015).
Kilpelainen, T. O. et al. Genetic variation near IRS1 associates with reduced adiposity and an impaired metabolic profile. Nat. Genet. 43 , 753–760 (2011).
Lu, Y. et al. New loci for body fat percentage reveal link between adiposity and cardiometabolic disease risk. Nat. Commun. 7 , 10495 (2016).
Zillikens, M. C. et al. Large meta-analysis of genome-wide association studies identifies five loci for lean body mass. Nat. Commun. 8 , 80 (2017).
Chu, A. Y. et al. Multiethnic genome-wide meta-analysis of ectopic fat depots identifies loci associated with adipocyte development and differentiation. Nat. Genet. 49 , 125–130 (2017).
Kilpelainen, T. O. et al. Genome-wide meta-analysis uncovers novel loci influencing circulating leptin levels. Nat. Commun. 7 , 10494 (2016).
Sun, Q. et al. Genome-wide association study identifies polymorphisms in LEPR as determinants of plasma soluble leptin receptor levels. Hum. Mol. Genet. 19 , 1846–1855 (2010).
Riveros-McKay, F. et al. Genetic architecture of human thinness compared to severe obesity. PLoS Genet. 15 , e1007603 (2019).
Orthofer, M. et al. Identification of ALK in thinness. Cell 181 , 1246–1262.e22 (2020).
Bradfield, J. P. et al. A trans-ancestral meta-analysis of genome-wide association studies reveals loci associated with childhood obesity. Hum. Mol. Genet. 28 , 3327–3338 (2019).
Felix, J. F. et al. Genome-wide association analysis identifies three new susceptibility loci for childhood body mass index. Hum. Mol. Genet. 25 , 389–403 (2016).
Vogelezang, S. et al. Novel loci for childhood body mass index and shared heritability with adult cardiometabolic traits. PLoS Genet. 16 , e1008718 (2020).
Akiyama, M. et al. Genome-wide association study identifies 112 new loci for body mass index in the Japanese population. Nat. Genet. 49 , 1458–1467 (2017).
Ng, M. C. Y. et al. Discovery and fine-mapping of adiposity loci using high density imputation of genome-wide association studies in individuals of African ancestry: African Ancestry Anthropometry Genetics Consortium. PLoS Genet. 13 , e1006719 (2017).
Gurdasani, D. et al. Uganda genome resource enables insights into population history and genomic discovery in Africa. Cell 179 , 984–1002.e36 (2019).
Wojcik, G. L. et al. Genetic analyses of diverse populations improves discovery for complex traits. Nature 570 , 514–518 (2019).
Martin, A. R. et al. Clinical use of current polygenic risk scores may exacerbate health disparities. Nat. Genet. 51 , 584–591 (2019).
Grarup, N. et al. Loss-of-function variants in ADCY3 increase risk of obesity and type 2 diabetes. Nat. Genet. 50 , 172–174 (2018).
Saeed, S. et al. Loss-of-function mutations in ADCY3 cause monogenic severe obesity. Nat. Genet. 50 , 175–179 (2018).
Minster, R. L. et al. A thrifty variant in CREBRF strongly influences body mass index in Samoans. Nat. Genet. 48 , 1049–1054 (2016).
Andersen, M. K. et al. The derived allele of a novel intergenic variant at chromosome 11 associates with lower body mass index and a favorable metabolic phenotype in Greenlanders. PLoS Genet. 16 , e1008544 (2020).
Siljee, J. E. et al. Subcellular localization of MC4R with ADCY3 at neuronal primary cilia underlies a common pathway for genetic predisposition to obesity. Nat. Genet. 50 , 180–185 (2018).
Willer, C. J. et al. Six new loci associated with body mass index highlight a neuronal influence on body weight regulation. Nat. Genet. 41 , 25–34 (2009).
Singh, K. et al. Neural cell adhesion molecule Negr1 deficiency in mouse results in structural brain endophenotypes and behavioral deviations related to psychiatric disorders. Sci. Rep. 9 , 5457 (2019).
Speliotes, E. K. et al. Association analyses of 249,796 individuals reveal 18 new loci associated with body mass index. Nat. Genet. 42 , 937–948 (2010).
Soni, A., Amisten, S., Rorsman, P. & Salehi, A. GPRC5B a putative glutamate-receptor candidate is negative modulator of insulin secretion. Biochem. Biophys. Res. Commun. 441 , 643–648 (2013).
Jarick, I. et al. Novel common copy number variation for early onset extreme obesity on chromosome 11q11 identified by a genome-wide analysis. Hum. Mol. Genet. 20 , 840–852 (2011).
Sainsbury, A. et al. Synergistic effects of Y2 and Y4 receptors on adiposity and bone mass revealed in double knockout mice. Mol. Cell Biol. 23 , 5225–5233 (2003).
Falchi, M. et al. Low copy number of the salivary amylase gene predisposes to obesity. Nat. Genet. 46 , 492–497 (2014).
Meisler, M. H. & Ting, C. N. The remarkable evolutionary history of the human amylase genes. Crit. Rev. Oral Biol. Med. 4 , 503–509 (1993).
Hendricks, A. E. et al. Rare variant analysis of human and rodent obesity genes in individuals with severe childhood obesity. Sci. Rep. 7 , 4394 (2017).
Turcot, V. et al. Protein-altering variants associated with body mass index implicate pathways that control energy intake and expenditure in obesity. Nat. Genet. 50 , 26–41 (2018). This large-scale exome-wide discovery study reports the use of array data to identify rare coding variations associated with BMI .
Emdin, C. A. et al. Analysis of predicted loss-of-function variants in UK Biobank identifies variants protective for disease. Nat. Commun. 9 , 1613 (2018).
Akbari, P. et al. Sequencing of 640,000 exomes identifies GPR75 variants associated with protection from obesity. Science 373 , eabf8683 (2021). This large-scale exome-wide discovery study reports the use of WES data to identify mutations associated with BMI .
Baggio, L. L. & Drucker, D. J. Biology of incretins: GLP-1 and GIP. Gastroenterology 132 , 2131–2157 (2007).
Antolin-Fontes, B. et al. The habenular G-protein-coupled receptor 151 regulates synaptic plasticity and nicotine intake. Proc. Natl Acad. Sci. USA 117 , 5502–5509 (2020).
Winkler, T. W. et al. The influence of age and sex on genetic associations with adult body size and shape: a large-scale genome-wide interaction study. PLoS Genet. 11 , e1005378 (2015).
Graff, M. et al. Genome-wide physical activity interactions in adiposity — a meta-analysis of 200,452 adults. PLoS Genet. 13 , e1006528 (2017).
Smith, C. E. et al. Genome-wide interactions with dairy intake for body mass index in adults of European descent. Mol. Nutr. Food Res. 62 , 1700347 (2018).
Justice, A. E. et al. Genome-wide meta-analysis of 241,258 adults accounting for smoking behaviour identifies novel loci for obesity traits. Nat. Commun. 8 , 14977 (2017).
Qi, Q. et al. Fried food consumption, genetic risk, and body mass index: gene–diet interaction analysis in three US cohort studies. BMJ 348 , g1610 (2014).
Kilpelainen, T. O. et al. Physical activity attenuates the influence of FTO variants on obesity risk: a meta-analysis of 218,166 adults and 19,268 children. PLoS Med. 8 , e1001116 (2011).
Yeo, G. S. H. Genetics of obesity: can an old dog teach us new tricks? Diabetologia 60 , 778–783 (2017).
Locke, A. E. et al. Genetic studies of body mass index yield new insights for obesity biology. Nature 518 , 197–206 (2015). This large-scale GWAS for BMI shows that BMI-associated loci frequently localize in or near genes that act in the brain .
Friedman, J. M. & Halaas, J. L. Leptin and the regulation of body weight in mammals. Nature 395 , 763–770 (1998).
Ahima, R. S. et al. Role of leptin in the neuroendocrine response to fasting. Nature 382 , 250–252 (1996).
Cowley, M. A. et al. Integration of NPY, AGRP, and melanocortin signals in the hypothalamic paraventricular nucleus: evidence of a cellular basis for the adipostat. Neuron 24 , 155–163 (1999).
Bertagna, X. Proopiomelanocortin-derived peptides. Endocrinol. Metab. Clin. North Am. 23 , 467–485 (1994).
Ollmann, M. M. et al. Antagonism of central melanocortin receptors in vitro and in vivo by agouti-related protein. Science 278 , 135–138 (1997).
Butler, A. A. et al. A unique metabolic syndrome causes obesity in the melanocortin-3 receptor-deficient mouse. Endocrinology 141 , 3518–3521 (2000).
Chen, A. S. et al. Inactivation of the mouse melanocortin-3 receptor results in increased fat mass and reduced lean body mass. Nat. Genet. 26 , 97–102 (2000).
Doche, M. E. et al. Human SH2B1 mutations are associated with maladaptive behaviors and obesity. J. Clin. Invest. 122 , 4732–4736 (2012).
Marenne, G. et al. Exome sequencing identifies genes and gene sets contributing to severe childhood obesity, linking PHIP variants to repressed POMC transcription. Cell Metab. 31 , 1107–1119.e12 (2020).
Asai, M. et al. Loss of function of the melanocortin 2 receptor accessory protein 2 is associated with mammalian obesity. Science 341 , 275–278 (2013).
Michaud, J. L. et al. Sim1 haploinsufficiency causes hyperphagia, obesity and reduction of the paraventricular nucleus of the hypothalamus. Hum. Mol. Genet. 10 , 1465–1473 (2001).
Farooqi, I. S. et al. Clinical spectrum of obesity and mutations in the melanocortin 4 receptor gene. N. Engl. J. Med. 348 , 1085–1095 (2003).
Wade, K. H. et al. Loss-of-function mutations in the melanocortin 4 receptor in a UK birth cohort. Nat. Med. 27 , 1088–1096 (2021). This paper establishes the frequency of loss-of-function mutations in MC4R to be 0.3%, much more common than previously appreciated .
van der Klaauw, A. et al. Role of melanocortin signalling in the preference for dietary macronutrients in human beings. Lancet 385 , S12 (2015).
Raffan, E. et al. A deletion in the canine POMC gene is associated with weight and appetite in obesity-prone Labrador retriever dogs. Cell Metab. 23 , 893–900 (2016).
Kim, K. S., Larsen, N., Short, T., Plastow, G. & Rothschild, M. F. A missense variant of the porcine melanocortin-4 receptor (MC4R) gene is associated with fatness, growth, and feed intake traits. Mamm. Genome 11 , 131–135 (2000).
Aspiras, A. C., Rohner, N., Martineau, B., Borowsky, R. L. & Tabin, C. J. Melanocortin 4 receptor mutations contribute to the adaptation of cavefish to nutrient-poor conditions. Proc. Natl Acad. Sci. USA 112 , 9668–9673 (2015).
Pinto, S. et al. Rapid rewiring of arcuate nucleus feeding circuits by leptin. Science 304 , 110–115 (2004).
Davies, A. M. The role of neurotrophins in the developing nervous system. J. Neurobiol. 25 , 1334–1348 (1994).
McAllister, A. K., Katz, L. C. & Lo, D. C. Opposing roles for endogenous BDNF and NT-3 in regulating cortical dendritic growth. Neuron 18 , 767–778 (1997).
Korte, M. et al. Hippocampal long-term potentiation is impaired in mice lacking brain-derived neurotrophic factor. Proc. Natl Acad. Sci. USA 92 , 8856–8860 (1995).
Kernie, S. G., Liebl, D. J. & Parada, L. F. BDNF regulates eating behavior and locomotor activity in mice. EMBO J. 19 , 1290–1300 (2000).
Xu, B. et al. Brain-derived neurotrophic factor regulates energy balance downstream of melanocortin-4 receptor. Nat. Neurosci. 6 , 736–742 (2003).
Xu, B. & Xie, X. Neurotrophic factor control of satiety and body weight. Nat. Rev. Neurosci. 17 , 282–292 (2016).
Rios, M. et al. Conditional deletion of brain-derived neurotrophic factor in the postnatal brain leads to obesity and hyperactivity. Mol. Endocrinol. 15 , 1748–1757 (2001).
Gray, J. et al. Hyperphagia, severe obesity, impaired cognitive function, and hyperactivity associated with functional loss of one copy of the brain-derived neurotrophic factor (BDNF) gene. Diabetes 55 , 3366–3371 (2006).
Yeo, G. S. et al. A de novo mutation affecting human TrkB associated with severe obesity and developmental delay. Nat. Neurosci. 7 , 1187–1189 (2004).
Thorleifsson, G. et al. Genome-wide association yields new sequence variants at seven loci that associate with measures of obesity. Nat. Genet. 41 , 18–24 (2009).
Finucane, H. K. et al. Heritability enrichment of specifically expressed genes identifies disease-relevant tissues and cell types. Nat. Genet. 50 , 621–629 (2018).
Ndiaye, F. K. et al. The expression of genes in top obesity-associated loci is enriched in insula and substantia nigra brain regions involved in addiction and reward. Int. J. Obes. 44 , 539–543 (2020).
Loos, R. J. & Yeo, G. S. The bigger picture of FTO: the first GWAS-identified obesity gene. Nat. Rev. Endocrinol. 10 , 51–61 (2014).
Church, C. et al. Overexpression of Fto leads to increased food intake and results in obesity. Nat. Genet. 42 , 1086–1092 (2010).
Fischer, J. et al. Inactivation of the Fto gene protects from obesity. Nature 458 , 894–898 (2009).
Cheung, M. K., Gulati, P., O’Rahilly, S. & Yeo, G. S. FTO expression is regulated by availability of essential amino acids. Int. J. Obes. 37 , 744–747 (2013).
Gulati, P. et al. Role for the obesity-related FTO gene in the cellular sensing of amino acids. Proc. Natl Acad. Sci. USA 110 , 2557–2562 (2013).
Karra, E. et al. A link between FTO, ghrelin, and impaired brain food-cue responsivity. J. Clin. Invest. 123 , 3539–3551 (2013).
Hess, M. E. et al. The fat mass and obesity associated gene (Fto) regulates activity of the dopaminergic midbrain circuitry. Nat. Neurosci. 16 , 1042–1048 (2013).
Ruud, J. et al. The fat mass and obesity-associated protein (FTO) regulates locomotor responses to novelty via D2R medium spiny neurons. Cell Rep. 27 , 3182–3198.e9 (2019).
Stratigopoulos, G., LeDuc, C. A., Cremona, M. L., Chung, W. K. & Leibel, R. L. Cut-like homeobox 1 (CUX1) regulates expression of the fat mass and obesity-associated and retinitis pigmentosa GTPase regulator-interacting protein-1-like (RPGRIP1L) genes and coordinates leptin receptor signaling. J. Biol. Chem. 286 , 2155–2170 (2011).
Stratigopoulos, G. et al. Hypomorphism for RPGRIP1L, a ciliary gene vicinal to the FTO locus, causes increased adiposity in mice. Cell Metab. 19 , 767–779 (2014).
Stratigopoulos, G. et al. Hypomorphism of Fto and Rpgrip1l causes obesity in mice. J. Clin. Invest. 126 , 1897–1910 (2016).
Smemo, S. et al. Obesity-associated variants within FTO form long-range functional connections with IRX3. Nature 507 , 371–375 (2014).
Claussnitzer, M. et al. FTO obesity variant circuitry and adipocyte browning in humans. N. Engl. J. Med. 373 , 895–907 (2015).
O’Rahilly, S., Coll, A. P. & Yeo, G. S. FTO obesity variant and adipocyte browning in humans. N. Engl. J. Med. 374 , 191 (2016).
PubMed Google Scholar
Sobreira, D. R. et al. Extensive pleiotropism and allelic heterogeneity mediate metabolic effects of IRX3 and IRX5. Science 372 , 1085–1091 (2021).
Almen, M. S. et al. The obesity gene, TMEM18, is of ancient origin, found in majority of neuronal cells in all major brain regions and associated with obesity in severely obese children. BMC Med. Genet. 11 , 58 (2010).
Larder, R. et al. Obesity-associated gene TMEM18 has a role in the central control of appetite and body weight regulation. Proc. Natl Acad. Sci. USA 114 , 9421–9426 (2017). Aside from the efforts at characterizing the FTO locus, this paper establishes a plausible role for yet another GWAS-identified candidate gene, TMEM18 , in energy homeostasis .
Wiemerslage, L. et al. The Drosophila ortholog of TMEM18 regulates insulin and glucagon-like signaling. J. Endocrinol. 229 , 233–243 (2016).
Biederer, T. et al. SynCAM, a synaptic adhesion molecule that drives synapse assembly. Science 297 , 1525–1531 (2002).
Yan, X. et al. Cadm2 regulates body weight and energy homeostasis in mice. Mol. Metab. 8 , 180–188 (2018).
Rathjen, T. et al. Regulation of body weight and energy homeostasis by neuronal cell adhesion molecule 1. Nat. Neurosci. 20 , 1096–1103 (2017).
Wheeler, E. et al. Genome-wide SNP and CNV analysis identifies common and low-frequency variants associated with severe early-onset obesity. Nat. Genet. 45 , 513–517 (2013).
Schafer, M., Brauer, A. U., Savaskan, N. E., Rathjen, F. G. & Brummendorf, T. Neurotractin/kilon promotes neurite outgrowth and is expressed on reactive astrocytes after entorhinal cortex lesion. Mol. Cell. Neurosci. 29 , 580–590 (2005).
Matikainen-Ankney, B. A. & Kravitz, A. V. Persistent effects of obesity: a neuroplasticity hypothesis. Ann. N. Y. Acad. Sci. 1428 , 221–239 (2018).
Lee, A. W. et al. Functional inactivation of the genome-wide association study obesity gene neuronal growth regulator 1 in mice causes a body mass phenotype. PLoS ONE 7 , e41537 (2012).
Joo, Y., Kim, H., Lee, S. & Lee, S. Neuronal growth regulator 1-deficient mice show increased adiposity and decreased muscle mass. Int. J. Obes. 43 , 1769–1782 (2019).
Boender, A. J., van Gestel, M. A., Garner, K. M., Luijendijk, M. C. & Adan, R. A. The obesity-associated gene Negr1 regulates aspects of energy balance in rat hypothalamic areas. Physiol. Rep. 2 , e12083 (2014).
Singh, K. et al. Neuronal growth and behavioral alterations in mice deficient for the psychiatric disease-associated negr1 gene. Front. Mol. Neurosci. 11 , 30 (2018).
Szczurkowska, J. et al. NEGR1 and FGFR2 cooperatively regulate cortical development and core behaviours related to autism disorders in mice. Brain 141 , 2772–2794 (2018).
PubMed PubMed Central Google Scholar
Noh, K. et al. Negr1 controls adult hippocampal neurogenesis and affective behaviors. Mol. Psychiatry 24 , 1189–1205 (2019).
Cano-Gamez, E. & Trynka, G. From GWAS to function: using functional genomics to identify the mechanisms underlying complex diseases. Front. Genet. 11 , 424 (2020).
Loos, R. J. et al. Common variants near MC4R are associated with fat mass, weight and risk of obesity. Nat. Genet. 40 , 768–775 (2008).
Chambers, J. C. et al. Common genetic variation near MC4R is associated with waist circumference and insulin resistance. Nat. Genet. 40 , 716–718 (2008).
Yaghootkar, H. et al. Genetic studies of leptin concentrations implicate leptin in the regulation of early adiposity. Diabetes 69 , 2806–2818 (2020).
Kichaev, G. et al. Leveraging polygenic functional enrichment to improve GWAS power. Am. J. Hum. Genet. 104 , 65–75 (2019).
Pulit, S. L. et al. Meta-analysis of genome-wide association studies for body fat distribution in 694 649 individuals of European ancestry. Hum. Mol. Genet. 28 , 166–174 (2019).
Wang, Y. et al. Melanocortin 4 receptor signals at the neuronal primary cilium to control food intake and body weight. J. Clin. Invest. 131 , e142064 (2021).
Article CAS PubMed Central Google Scholar
Farooqi, I. S. et al. Effects of recombinant leptin therapy in a child with congenital leptin deficiency. N. Engl. J. Med. 341 , 879–884 (1999). This paper is the first description of the treatment of leptin deficiency using leptin replacement therapy .
Farooqi, I. S. & O’Rahilly, S. 20 years of leptin: human disorders of leptin action. J. Endocrinol. 223 , T63–T70 (2014).
Yeo, G. S. H. et al. The melanocortin pathway and energy homeostasis: from discovery to obesity therapy. Mol. Metab. 48 , 101206 (2021).
Kuhnen, P. et al. Proopiomelanocortin deficiency treated with a melanocortin-4 receptor agonist. N. Engl. J. Med. 375 , 240–246 (2016). This paper is the first to demonstrate that the melanocortin pathway is a relevant and, so far, safe therapeutic target for the treatment of at least rare genetic causes of obesity .
Clement, K. et al. MC4R agonism promotes durable weight loss in patients with leptin receptor deficiency. Nat. Med. 24 , 551–555 (2018).
Clement, K. et al. Efficacy and safety of setmelanotide, an MC4R agonist, in individuals with severe obesity due to LEPR or POMC deficiency: single-arm, open-label, multicentre, phase 3 trials. Lancet Diabetes Endocrinol. 8 , 960–970 (2020).
Ayers, K. L. et al. Melanocortin 4 receptor pathway dysfunction in obesity: patient stratification aimed at MC4R agonist treatment. J. Clin. Endocrinol. Metab. 103 , 2601–2612 (2018).
Heymsfield, S. B. et al. Recombinant leptin for weight loss in obese and lean adults: a randomized, controlled, dose-escalation trial. JAMA 282 , 1568–1575 (1999).
Collet, T. H. et al. Evaluation of a melanocortin-4 receptor (MC4R) agonist (setmelanotide) in MC4R deficiency. Mol. Metab. 6 , 1321–1329 (2017).
Khera, A. V. et al. Polygenic prediction of weight and obesity trajectories from birth to adulthood. Cell 177 , 587–596.e9 (2019). This study describes a comprehensive PGS and its association with BMI throughout the life course .
Loos, R. J. F. 15 years of genome-wide association studies and no signs of slowing down. Nat. Commun. 11 , 5900 (2020).
Pearce, L. R. et al. KSR2 mutations are associated with obesity, insulin resistance, and impaired cellular fuel oxidation. Cell 155 , 765–777 (2013).
Greenfield, J. R. et al. Modulation of blood pressure by central melanocortinergic pathways. N. Engl. J. Med. 360 , 44–52 (2009).
Torkamani, A. & Topol, E. Polygenic risk scores expand to obesity. Cell 177 , 518–520 (2019).
Download references
Acknowledgements
R.J.F.L. is supported by funding from Novo Nordisk Foundation (NNF Laureate Award) and the US National Institutes of Health (R01DK110113; R01DK107786; R01HL142302; R01 DK124097). G.S.H.Y. is supported by the Medical Research Council (MRC Metabolic Diseases Unit (MC_UU_00014/1)). The authors thank M. Guindo Martinez for her help with creating data for Fig. 3 and Supplementary Tables 1 and 2.
Author information
Authors and affiliations.
Novo Nordisk Foundation Center for Basic Metabolic Research, University of Copenhagen, Copenhagen, Denmark
Ruth J. F. Loos
Charles Bronfman Institute for Personalized Medicine, Icahn School of Medicine at Mount Sinai, New York, NY, USA
Mindich Child Health and Development Institute, Icahn School of Medicine at Mount Sinai, New York, NY, USA
Department of Environmental Medicine and Public Health, Icahn School of Medicine at Mount Sinai, New York, NY, USA
MRC Metabolic Diseases Unit, University of Cambridge Metabolic Research Laboratories, Wellcome-MRC Institute of Metabolic Science, Addenbrooke’s Hospital, Cambridge, UK
Giles S. H. Yeo
You can also search for this author in PubMed Google Scholar
Contributions
The authors contributed equally to all aspects of the article.
Corresponding authors
Correspondence to Ruth J. F. Loos or Giles S. H. Yeo .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Additional information
Peer review information.
Nature Reviews Genetics thanks D. Meyre, T. Fall and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Related links
23andMe: https://research.23andme.com/collaborate/
All of Us: https://allofus.nih.gov/
Biobank Japan: http://jenger.riken.jp/en/
Genetic Investigation for ANthropometric Traits (GIANT) consortium: https://portals.broadinstitute.org/collaboration/giant/index.php/Main_Page
Million Veterans Project: https://www.research.va.gov/mvp/
NCD Risk Factor Collaboration (NCD RisC): https://www.ncdrisc.org/data-visualisations.html
UK Biobank: https://www.ukbiobank.ac.uk/
Supplementary information
Supplementary information.
An environment that promotes weight gain.
A severe, early-onset form of obesity, caused by a single-gene mutation, with little or no influence of the environment.
A common multifactorial form of obesity, resulting from an interaction between the obesogenic environment and hundreds of genetic variants.
An approach used to understand the function of a gene by analysing the consequences of genetically manipulating specific sequences within the gene.
A hypothesis-driven approach to study the effect of a given gene (chosen based on the current understanding of its biology and pathophysiology) on susceptibility to the phenotype under study.
A method that relies on the relatedness of study participants to test whether certain chromosomal regions co-segregate with a disease or trait across generations.
(GWAS). A hypothesis-generating approach that screens whole genomes for associations between genetic variants and a phenotype of interest at much higher resolution than is possible for genome-wide linkage studies, and is thus better able to narrow down the associated locus.
(PGS). A measure used to assess an individual’s genetic susceptibility to disease, calculated by summing the number of disease-increasing alleles, weighted by each variant’s effect size observed in a genome-wide association study.
(AUC ROC ). A metric used to assess the ability of a predictor to discriminate between individuals with and without a disease. The AUC ranges from 0.50 (equal to tossing a coin) to 1.0 (perfect prediction).

Rights and permissions
Reprints and permissions
About this article
Cite this article.
Loos, R.J.F., Yeo, G.S.H. The genetics of obesity: from discovery to biology. Nat Rev Genet 23 , 120–133 (2022). https://doi.org/10.1038/s41576-021-00414-z
Download citation
Accepted : 17 August 2021
Published : 23 September 2021
Issue Date : February 2022
DOI : https://doi.org/10.1038/s41576-021-00414-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
A low-calorie meal replacement improves body composition and metabolic parameters in shift workers with overweight and obesity: a randomized, controlled, parallel group trial.
- Piumika Sooriyaarachchi
- Ranil Jayawardena
- Neil A. King
Nutrition & Metabolism (2024)
Hyperphagia and impulsivity: use of self-administered Dykens’ and in-house impulsivity questionnaires to characterize eating behaviors in children with severe and early-onset obesity
- Lara Arnouk
- Hélène Chantereau
- Béatrice Dubern
Orphanet Journal of Rare Diseases (2024)
Associations between maternal pre-pregnancy BMI and infant striatal mean diffusivity
- Aylin Rosberg
- Harri Merisaari
- Jetro J. Tuulari
BMC Medicine (2024)
Identifying latent genetic interactions in genome-wide association studies using multiple traits
- Andrew J. Bass
- Shijia Bian
- Michael P. Epstein
Genome Medicine (2024)
A genomics perspective of personalized prevention and management of obesity
- Kalliopi K. Gkouskou
- Maria G. Grammatikopoulou
- Aristides G. Eliopoulos
Human Genomics (2024)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing: Translational Research newsletter — top stories in biotechnology, drug discovery and pharma.
- Patient Care & Health Information
- Diseases & Conditions
Obesity is a complex disease involving having too much body fat. Obesity isn't just a cosmetic concern. It's a medical problem that increases the risk of many other diseases and health problems. These can include heart disease, diabetes, high blood pressure, high cholesterol, liver disease, sleep apnea and certain cancers.
There are many reasons why some people have trouble losing weight. Often, obesity results from inherited, physiological and environmental factors, combined with diet, physical activity and exercise choices.
The good news is that even modest weight loss can improve or prevent the health problems associated with obesity. A healthier diet, increased physical activity and behavior changes can help you lose weight. Prescription medicines and weight-loss procedures are other options for treating obesity.
Products & Services
- A Book: The Mayo Clinic Diet Bundle
Body mass index, known as BMI, is often used to diagnose obesity. To calculate BMI , multiply weight in pounds by 703, divide by height in inches and then divide again by height in inches. Or divide weight in kilograms by height in meters squared. There are several online calculators available that help calculate BMI .
See BMI calculator
| Weight status | |
|---|---|
| Below 18.5 | Underweight |
| 18.5-24.9 | Healthy |
| 25.0-29.9 | Overweight |
| 30.0 and higher | Obesity |
Asians with a BMI of 23 or higher may have an increased risk of health problems.
For most people, BMI provides a reasonable estimate of body fat. However, BMI doesn't directly measure body fat. Some people, such as muscular athletes, may have a BMI in the obesity category even though they don't have excess body fat.
Many health care professionals also measure around a person's waist to help guide treatment decisions. This measurement is called a waist circumference. Weight-related health problems are more common in men with a waist circumference over 40 inches (102 centimeters). They're more common in women with a waist measurement over 35 inches (89 centimeters). Body fat percentage is another measurement that may be used during a weight loss program to track progress.
When to see a doctor
If you're concerned about your weight or weight-related health problems, ask your health care professional about obesity management. You and your health care team can evaluate your health risks and discuss your weight-loss options.
More Information
Obesity care at Mayo Clinic
- What is insulin resistance? A Mayo Clinic expert explains
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
Although there are genetic, behavioral, metabolic and hormonal influences on body weight, obesity occurs when you take in more calories than you burn through typical daily activities and exercise. Your body stores these excess calories as fat.
In the United States, most people's diets are too high in calories — often from fast food and high-calorie beverages. People with obesity might eat more calories before feeling full, feel hungry sooner, or eat more due to stress or anxiety.
Many people who live in Western countries now have jobs that are much less physically demanding, so they don't tend to burn as many calories at work. Even daily activities use fewer calories, courtesy of conveniences such as remote controls, escalators, online shopping, and drive-through restaurants and banks.
Risk factors
Obesity often results from a combination of causes and contributing factors:
Family inheritance and influences
The genes you inherit from your parents may affect the amount of body fat you store, and where that fat is distributed. Genetics also may play a role in how efficiently your body converts food into energy, how your body regulates your appetite and how your body burns calories during exercise.
Obesity tends to run in families. That's not just because of the genes they share. Family members also tend to share similar eating and activity habits.
Lifestyle choices
- Unhealthy diet. A diet that's high in calories, lacking in fruits and vegetables, full of fast food, and laden with high-calorie beverages and oversized portions contributes to weight gain.
- Liquid calories. People can drink many calories without feeling full, especially calories from alcohol. Other high-calorie beverages, such as sugared soft drinks, can contribute to weight gain.
- Inactivity. If you have an inactive lifestyle, you can easily take in more calories every day than you burn through exercise and routine daily activities. Looking at computer, tablet and phone screens is inactivity. The number of hours spent in front of a screen is highly associated with weight gain.
Certain diseases and medications
In some people, obesity can be traced to a medical cause, such as hypothyroidism, Cushing syndrome, Prader-Willi syndrome and other conditions. Medical problems, such as arthritis, also can lead to decreased activity, which may result in weight gain.
Some medicines can lead to weight gain if you don't compensate through diet or activity. These medicines include steroids, some antidepressants, anti-seizure medicines, diabetes medicines, antipsychotic medicines and certain beta blockers.
Social and economic issues
Social and economic factors are linked to obesity. It's hard to avoid obesity if you don't have safe areas to walk or exercise. You may not have learned healthy ways of cooking. Or you may not have access to healthier foods. Also, the people you spend time with may influence your weight. You're more likely to develop obesity if you have friends or relatives with obesity.
Obesity can occur at any age, even in young children. But as you age, hormonal changes and a less active lifestyle increase your risk of obesity. The amount of muscle in your body also tends to decrease with age. Lower muscle mass often leads to a decrease in metabolism. These changes also reduce calorie needs and can make it harder to keep off excess weight. If you don't consciously control what you eat and become more physically active as you age, you'll likely gain weight.
Other factors
- Pregnancy. Weight gain is common during pregnancy. Some women find this weight difficult to lose after the baby is born. This weight gain may contribute to the development of obesity in women.
- Quitting smoking. Quitting smoking is often associated with weight gain. And for some, it can lead to enough weight gain to qualify as obesity. Often, this happens as people use food to cope with smoking withdrawal. But overall, quitting smoking is still a greater benefit to your health than is continuing to smoke. Your health care team can help you prevent weight gain after quitting smoking.
- Lack of sleep. Not getting enough sleep can cause changes in hormones that increase appetite. So can getting too much sleep. You also may crave foods high in calories and carbohydrates, which can contribute to weight gain.
- Stress. Many external factors that affect mood and well-being may contribute to obesity. People often seek more high-calorie food during stressful situations.
- Microbiome. The make-up of your gut bacteria is affected by what you eat and may contribute to weight gain or trouble losing weight.
Even if you have one or more of these risk factors, it doesn't mean that you're destined to develop obesity. You can counteract most risk factors through diet, physical activity and exercise. Behavior changes, medicines and procedures for obesity also can help.
Complications
People with obesity are more likely to develop a number of potentially serious health problems, including:
- Heart disease and strokes. Obesity makes you more likely to have high blood pressure and unhealthy cholesterol levels, which are risk factors for heart disease and strokes.
- Type 2 diabetes. Obesity can affect the way the body uses insulin to control blood sugar levels. This raises the risk of insulin resistance and diabetes.
- Certain cancers. Obesity may increase the risk of cancer of the uterus, cervix, endometrium, ovary, breast, colon, rectum, esophagus, liver, gallbladder, pancreas, kidney and prostate.
- Digestive problems. Obesity increases the likelihood of developing heartburn, gallbladder disease and liver problems.
- Sleep apnea. People with obesity are more likely to have sleep apnea, a potentially serious disorder in which breathing repeatedly stops and starts during sleep.
- Osteoarthritis. Obesity increases the stress placed on weight-bearing joints. It also promotes inflammation, which includes swelling, pain and a feeling of heat within the body. These factors may lead to complications such as osteoarthritis.
- Fatty liver disease. Obesity increases the risk of fatty liver disease, a condition that happens due to excessive fat deposit in the liver. In some cases, this can lead to serious liver damage, known as liver cirrhosis.
- Severe COVID-19 symptoms. Obesity increases the risk of developing severe symptoms if you become infected with the virus that causes coronavirus disease 2019, known as COVID-19. People who have severe cases of COVID-19 may need treatment in intensive care units or even mechanical assistance to breathe.
Related information
- Link between extra pounds, severe COVID-19 illness grows stronger - Related information Link between extra pounds, severe COVID-19 illness grows stronger
Quality of life
Obesity can diminish the overall quality of life. You may not be able to do physical activities that you used to enjoy. You may avoid public places. People with obesity may even encounter discrimination.
Other weight-related issues that may affect your quality of life include:
- Depression.
- Disability.
- Shame and guilt.
- Social isolation.
- Lower work achievement.
- Overweight and obesity. National Heart, Lung, and Blood Institute. https://www.nhlbi.nih.gov/health-topics/overweight-and-obesity. Accessed Dec. 21, 2022.
- Goldman L, et al., eds. Obesity. In: Goldman-Cecil Medicine. 26th ed. Elsevier; 2020. https://www.clinicalkey.com. Accessed Dec. 21. 2022.
- Kellerman RD, et al. Obesity in adults. In: Conn's Current Therapy 2023. Elsevier; 2023. https://www.clinicalkey.com. Accessed Dec. 21, 2022.
- Feldman M, et al., eds. Obesity. In: Sleisenger and Fordtran's Gastrointestinal and Liver Disease: Pathophysiology, Diagnosis, Management. 11th ed. Elsevier; 2021. https://www.clinicalkey.com. Accessed Dec. 21, 2022.
- Perrault L. Obesity in adults: Prevalence, screening and evaluation. https://www.uptodate.com/contents/search. Accessed Dec. 21, 2022.
- Melmed S, et al. Obesity. In: Williams Textbook of Endocrinology. 14th ed. Elsevier; 2020. https://www.clinicalkey.com. Accessed Dec. 21, 2022.
- COVID-19: People with certain medical conditions. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html. Accessed Dec. 21, 2022.
- Perrault L. Obesity in adults: Overview of management. https://www.uptodate.com/contents/search. Accessed Dec. 21, 2022.
- Healthy weight, nutrition and physical activity. Centers for Disease Control and Prevention. https://www.cdc.gov/healthyweight/index.html. Accessed Dec. 21, 2022.
- Ferri FF. Obesity. In: Ferri's Clinical Advisor 2023. Elsevier; 2023. https://www.clinicalkey.com. Accessed Jan. 20, 2023.
- Feldman M, et al., eds. Surgical and Endoscopic Treatment of Obesity. In: Sleisenger and Fordtran's Gastrointestinal and Liver Disease: Pathophysiology, Diagnosis, Management. 11th ed. Elsevier; 2021. https://www.clinicalkey.com. Accessed Dec. 21, 2022.
- BMI and waist circumference calculator
Associated Procedures
- Bariatric surgery
- Biliopancreatic diversion with duodenal switch (BPD/DS)
- Cholesterol test
- Gastric bypass (Roux-en-Y)
- Intragastric balloon
- Liver function tests
- Sleeve gastrectomy
News from Mayo Clinic
- Mayo Clinic Minute: Health consequences of obesity Aug. 12, 2024, 04:15 p.m. CDT
- Mayo Clinic Q & A: Supporting weight-loss medications with adequate, tailored nutrition May 02, 2024, 11:00 a.m. CDT
- Mayo Clinic researchers pave the way for individualized obesity therapy, tailoring interventions to a person's needs July 12, 2023, 03:00 p.m. CDT
- People with severe obesity and a genetic pathway variant have increased risk of hypertension, Mayo Clinic research finds April 18, 2023, 08:00 p.m. CDT
- Obesity makes it harder to diagnose and treat heart disease Feb. 28, 2023, 04:15 p.m. CDT
- Mayo Clinic Minute: Obesity and heart disease Feb. 23, 2023, 05:30 p.m. CDT
- Healthy Weight Awareness Month. Mayo Clinic innovations can help you lose weight, keep it off Jan. 05, 2023, 04:15 p.m. CDT
- Mayo Clinic Q and A: Probiotics, gut bacteria and weight -- what's the connection? Sept. 25, 2022, 11:00 a.m. CDT
- Addressing health care barriers during Hispanic Heritage Month Sept. 15, 2022, 04:30 p.m. CDT
- Symptoms & causes
- Diagnosis & treatment
- Doctors & departments
- Care at Mayo Clinic
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Help transform healthcare
Your donation can make a difference in the future of healthcare. Give now to support Mayo Clinic's research.
Definition and Overview
The World Health Organization (WHO) defines overweight and obesity as having “excessive fat accumulation that presents a risk to health.” There are various methods to calculate body fat , as each range in accuracy and can have limitations. Body mass index (BMI) is one tool used to screen for excessive body fat. A BMI value of more than 25 is categorized as overweight, and a BMI value of more than 30 is categorized as obese.
Why use BMI?
Health impacts.
There are negative health impacts associated with excess body fat. The WHO estimates that in 2019, 5 million deaths from noncommunicable diseases such as cardiovascular disease and diabetes were caused by a high BMI, and rates of obesity continue to grow globally in children and adults. [1] According to the Centers for Disease Control and Prevention in the U.S., 1 in 5 children and 1 in 3 adults has obesity. [2] Children with obesity are more likely to have obesity as adults and the associated risks of heart disease, high blood pressure, type 2 diabetes, and certain types of cancer.
A healthy amount of body fat in children and teens varies based on age as well as sex. The Centers for Disease Control and Prevention (CDC) developed growth charts for boys and girls ages 2-19 that show the distribution of BMI values at each age. [3] By the CDC’s definition, a child whose BMI falls between the 85th and 94th percentile for age and sex is considered overweight; a BMI at the 95th percentile or higher for age is considered obese. As the rates of obesity rise in children, there is also a category for severe obesity in which the BMI is 120% of the 95th percentile. The American Academy of Pediatrics provides more specific classifications of severe obesity:
- Class 2 Obesity: BMI ≥120% to <140% of the 95th percentile or BMI ≥35 to <40 kg/m 2
- Class 3 Obesity: BMI ≥140% of the 95th percentile or BMI ≥40 kg/m 2
Obesity can negatively affect nearly every system in a child’s body – the heart, lungs, muscles, bones, kidneys, digestive tract, and hormones that control blood sugar and puberty – and can also take a heavy social and emotional toll. Children with obesity may be burdened by stigma and discrimination from bullying, teasing and victimization. Youth with obesity have substantially higher odds of remaining overweight or obese into adulthood increasing their risk of disease and disability later in life. [4]
The risk of developing diabetes, heart disease, and other weight-related health risks increases with an increasing body mass index (BMI). But evidence shows that in some ethnic and racial groups, weight gain and higher fat mass even if BMI remains in the normal range can still increase health risks.
The Nurses’ Health Study tracked patterns of weight gain and type 2 diabetes (T2D) development in 78,000 U.S. women to see differences by ethnic group. [5] All women were healthy at the start of the study. After 20 years, researchers found that at the same BMI, Asians had more than twice the risk of developing T2D than Whites; Hispanics and Blacks also had higher risks of diabetes than Whites, but to a lesser degree. Increases in weight over time were more harmful in Asians than in other ethnic groups – for every 11 pounds Asians gained during adulthood, they had an 84% increased risk of T2D; Hispanics, Blacks, and Whites who gained weight also had higher risk, but to a much lesser degree than Asians. Other studies have found that even with a lower BMI than Whites, increasing weight in Asians with a BMI of 25 or higher increased risk of high blood pressure, T2D, and early death from all causes. [6-8]
One reason for this difference could be amount and location of body fat. Even with a lower BMI than other populations, Chinese and South Asians tend to carry higher abdominal fat than Whites, which increases the risk for T2D, cardiovascular disease, and other metabolic disorders. [9-11] In contrast, some studies have found that blacks have lower body fat and higher lean muscle mass than whites at the same BMI, and therefore at the same BMI, may be at lower risk of obesity-related diseases. [12,13]
For this reason, the World Health Organization and other organizations have recommended a lower BMI cutoff to classify obesity in Asian people (BMI of 25-27 or greater) as well as a smaller waist circumference to measure visceral fat. [9,14]
Weight gain of greater than 10 pounds in adulthood also increases disease risk (i.e., heart disease, high blood pressure, type 2 diabetes, gallstones) even in those whose BMI remains in the normal range, according to research from the Nurses’ Health Study and Health Professionals Follow-up Study. [15-19]
With the five leading causes of death – heart disease, cancer , chronic lower respiratory disease, cerebrovascular diseases such as stroke, and unintentional injuries – obesity is a major risk factor for the first four. [20] Obesity is also associated with other health conditions such as sleep apnea, fatty liver disease, gallstones, infertility, respiratory diseases, gastroesophageal reflux disease, and musculoskeletal disorders such as arthritis. No less real are the social and emotional effects of obesity which may include discrimination, lower quality of life, and susceptibility to depression.
Economic Impacts
Obesity costs the U.S. health care system almost $173 billion annually. [2] This includes money spent directly on medical care and prescription drugs related to obesity. In the workplace, research has shown that the number of sick days, short-term disability, and workers’ compensation days increase with increasing BMI. [21] Compared with an employee with a BMI of 25, an employee with a BMI of 35 has nearly double the risk of a disability or workers’ compensation claim. Perhaps one of the most surprising consequences of the current obesity epidemic in the U.S. is its impact on recruitment for the armed services, with data showing that 3 in 5 young adults carry too much weight to qualify for military service. [2]
According to the WHO, worldwide obesity rates are rising with 1 in 8 people, or more than 1 billion people, around the world living with obesity. [14] A Lancet review showed that global adult obesity doubled from 1990 to 2022, and adolescent obesity quadrupled. [22] As low to middle-income countries adopt unhealthy eating patterns and behaviors of industrialized nations such as less physical activity, so do their obesity rates. Specific regions including Polynesia, Micronesia, the Caribbean, the Middle East, and north Africa showed the greatest increases in obesity, as well as higher-income countries such as Chile. [22] Increased eating out of home, access to ultra-processed low-nutrient-dense foods, and sedentariness (e.g., sitting at work, driving instead of walking or bicycling) have contributed. Higher cost and limited access to healthy foods and decreased opportunities for play and sports may cause inequalities in obesity and could limit the impact of policies that target unhealthy foods. [22]
The NCD Risk Factor Collaboration visualizes the prevalence of obesity globally as well as changing obesity rates in various countries since 1990. Below are data summaries of obesity rates for both adults and children around the world:
In 2018, the United States had the highest prevalence of adult obesity among high-income Western countries worldwide. [23] From 1999 through 2018, the age-adjusted prevalence of adults with obesity increased significantly from 31% to 42%. [24]. If trends continue, projections estimate that by 2030 nearly 50% of adults will have obesity, and nearly 1 in 4 adults will have severe obesity (BMI ≥35). [25]
Obesity disproportionately affects U.S. racial/ethnic minority populations. Compared to 42% of non-Hispanic whites, 50% of non-Hispanic Black and 45% of Hispanic adults have obesity. [24] There are considerable differences in obesity among non-Hispanic Black adults by sex, with 57% of non-Hispanic Black women having obesity compared to 41% of men. [24] Trends estimate that severe obesity may become the most common BMI category among non-Hispanic Black and low-income adults by 2030. [25]
Obesity rates in Canada are not as high as they are in the U.S., but Canada has seen dramatic increases over the past three decades. Obesity prevalence among Canadian adults increased from 9% in 1975 to 31% by 2016. [23] Indigenous populations in Canada are also disproportionately affected by the burden of obesity. [26]
The U.S. has among the highest childhood obesity rates in the world, with nearly 1 in 3 children with overweight or obesity. In 2015-2016, nearly 19% of children 2-19 years old had obesity, affecting an estimated 14 million children nationwide. Obesity prevalence was highest among adolescents 12-19 years old (21%) and lowest among preschool-aged children 2-5 years old (14%). [27] Recently, the prevalence of obesity declined among children ages 2-5 years old, held steady for children 6-11 years, and continued to rise among adolescents 12-19 years. [28,29] Current trends suggest that an alarming 57% of children currently between 2 and 19 years old will have obesity at age 35. [30]
Overweight and obesity disproportionally affects racial/ethnic minority populations, and such disparities exist as early as age 2 and persist into adulthood. [27,30] The highest obesity prevalence are among Hispanic (26%) and non-Hispanic Black children (22%), compared with the lowest prevalence among non-Hispanic White (14%) and non-Hispanic Asian (11%) children. [27]
Canada has also seen a rise in childhood obesity since the late 1970s. Obesity rates have more than doubled, and in some age groups, tripled. [31] But childhood obesity rates are lower there than they are in the U.S; in 2013, 10% of children ages 6-11 years old and 17% of children ages 12-17 had obesity. [32] Childhood obesity is significant among Canada’s Aboriginal groups. In a 2006 survey of Aboriginal Peoples in Canada, nearly 33% of children ages 6-8 had obesity, and 13% among children ages 9-14. [33]
Over the past several decades, obesity has become a significant health challenge in Latin America. While undernourishment persists among vulnerable groups, so do overweight and obesity. Each year, obesity among the population grows by 3.6 million individuals, and now exceeds undernourishment as the greatest nutritional threat. [34] Between 1975 and 2014, among the largest increases in BMI in regions worldwide occurred for men in central Latin America, and for women in Andean Latin America and the Caribbean. [35] In 2016, approximately 104 million adults in Latin America had obesity; 15% of men and 16% of women. [23] Countries with the highest prevalence of obesity included Bermuda (women 43%, men 30%) and Puerto Rico (women 42%, men 29%). [23]
While Latin America has shown significant progress in reducing child stunting due to undernourishment, prevalence of overweight and obesity due to malnutrition has grown to be among the highest in the world. [34] As a result, Latin American children have the dual burden of undernutrition coexisting with overweight and obesity. [36] In 2016, 15% of children ages 5-9 years and 10% of adolescents ages 10-19 years had obesity in Latin America and the Caribbean. [34] Among girls ages 5-19 years old, central Latin America demonstrated the highest increase of BMI per decade worldwide over the past 40 years. [37] Inequality further exacerbates overweight and obesity in populations with lower income, and among women, indigenous peoples, Afro-descendants, and rural families. [34]
Since 1975, obesity rates have been rising across Europe, though not as rapidly or as high as they are in the U.S. [35] Countries with the highest prevalence include Malta and the United Kingdom, hovering around 30% for both men and women. Countries with the lowest obesity prevalence include Austria, Sweden, Denmark, and Switzerland for women and Moldova and Russia for men (<20% for all). [23] The rise in women’s BMI in central and southwestern Europe has been among the lowest over the past 40 years, one of the few places worldwide that can report such a trend. [23,35]
Over the past several decades, many European countries had among the largest increases in the number of children and adolescents with obesity. [37] More recently, obesity has plateaued in many regions, particularly in eastern, northwestern, and southwestern Europe, but prevalence rates remain high in Mediterranean countries. [37,38] In Greece, Malta, and Cyprus, 16% of boys ages 5-19 have obesity, and 11% of girls in Greece and Malta. [37]
Regional surveys and analyses demonstrate similar childhood obesity trends in Europe. A 2019 systematic review of 130 studies across 28 European countries assessed prevalence trends in overweight and obesity among 2-13-year-old children between 1999-2016. [39] The prevalence of overweight and obesity tended to decrease in the Iberian region and increase in the Mediterranean regions, with no significant changes in Atlantic or Central Europe. Although the overall prevalence of childhood overweight and obesity remains high, trends have stabilized in most European countries, but continues to rise in some Mediterranean countries. [39]
Undernutrition has historically received more public health attention in Africa than overnutrition. Yet today, obesity and associated chronic diseases have become a growing problem across the continent. Some have called it a “silent epidemic,” striking countries that are still struggling with the health and economic burdens of malnutrition, stunting, infectious disease, and high childhood mortality rates. [40]
Obesity prevalence is higher among African women compared with men, and can vary widely from country to country. For example in 2016, 41% of women in South Africa had obesity (higher than in U.S. women) compared with 16% of men. In stark contrast, the lowest prevalence of obesity was in Ethiopia for women (7.3%) and in Uganda for men (2%); prevalence of undernutrition exceeds that of overnutrition in these African countries among many others. [35] Between 1975 and 2016, Botswana experienced the largest increases in obesity prevalence in these African regions, jumping from 5% to 31%. [35]
Hunger, underweight, and stunting have long been the more pressing child nutrition concerns across Africa. Even today, more children and adolescents are moderately or severely underweight than obese, particularly in central, east, and west Africa. [35] Yet here too, child obesity rates are on the rise, particularly in southern Africa. In 1975, less than 0.5% of girls and boys in South Africa had obesity, but by 2016 the prevalence jumped to 13% for girls and 10% for boys. [37]
Researchers have taken a closer look at obesity trends in the six Persian Gulf states (Oman, Bahrain, United Arab Emirates, Saudi Arabia, Qatar, and Kuwait), since these countries have seen tremendous increases in wealth since the discovery of oil reserves in the 1960s. [41] Even in 1975, obesity prevalence in Kuwait, Qatar, and the United Arab Emirates exceeded 20% among women, raking among the top 20 countries worldwide with the highest prevalence. Among men, Kuwait and Qatar also ranked among the top 20 countries with the highest prevalence in 1975, but only at 12%. [23] In 2016, the prevalence of obesity increased to 47% in Kuwait and 45% in Qatar for women, and to approximately 30% for men in both countries. The most significant increases have been observed in Saudi Arabia and Jordan, from 6% in 1975 to around 30% in 2016. [23]
The Middle East and north Africa have seen sharp increases in obesity since 1975, and this region now has among the highest prevalence of child and adolescent obesity worldwide. [38] Girls in Kuwait and Egypt and boys in Kuwait, Qatar, and Saudi Arabia have the highest obesity prevalence in the region, all hovering around 20% of the child and adolescent population. [37] In 1975, girls in the Middle East and north Africa had higher age-standardized BMI than boys, but by 2016 this gap shrank or reversed as boys gained more weight than girls. [37]
Some countries in Asia have the lowest obesity prevalence worldwide, yet here too it has become a serious problem across the region over the past four decades, even while underweight concerns persist. Japan and South Korea have among the lowest obesity prevalence in the world (<9%) for both men and women. However, recent trends in China are of special concern. Although obesity rates are still low overall, there has been a substantial increase from <1% in 1978, to 6% for women and 7% for men in 2016. [23] China is one of the most populous nations on the planet with more than 1.4 billion people, so even small percentage increases in obesity prevalence translate into millions more cases of chronic disease. Furthermore, Asians have a higher risk of weight-related diseases like type 2 diabetes at lower BMI levels , further exacerbating the health issues related to overweight and obesity.
South Asian countries like Bangladesh, India, and Pakistan have among the highest prevalence of moderate and severe underweight worldwide; 20% in girls and 29% in boys. Nevertheless, trends in mean BMI have significantly accelerated in east, south, and southeast Asia between 1975 and 2016. Although obesity prevalence remains relatively low in south Asia, their large populations add up to large numbers of children who have obesity.
Compared to south Asia, the prevalence of child and adolescent obesity is greater in high income Asia Pacific and east/southeast Asia, particularly among boys. [37,38] Obesity prevalence in Malaysia, Taiwan, and China for boys was less than 0.5% in 1975 and jumped to 15% in 2016. Girls in Asia have lower obesity prevalence compared to boys, but has still been increasing over time, most notably in Malaysia where obesity increased from 0.2% to 10% during this time period. [37]
It’s important to note that in Asian adults, the health complications associated with overweight and obesity start at a lower BMI than seen in the U.S. and Europe; therefore these estimates of child obesity prevalence in Asia likely underestimate the true public health burden of obesity in Asia.
The top 13 countries with the highest obesity prevalence worldwide are located within Oceania. Eight of the countries exceed 45% obesity prevalence among men, and 13 countries exceed 50% among women. American Samoa and Nauru have the highest obesity prevalence among women (68%) worldwide; for men it is Nauru at 60%. Australia and New Zealand have lower prevalence in the region but still hover around 30% for both men and women. [23]
Of the top 13 countries with the highest child and adolescent obesity prevalence in 2016, 11 were located in Oceania. There was more than 30% obesity prevalence for both girls and boys in the Cook Islands, Nauru, Palau, and additionally for boys in Niue and American Samoa. [37]
High-income countries in Oceania, Australia and New Zealand have childhood obesity rates in the double digits, but there’s some evidence that rates have hit a plateau. In Australia, 13% of boys and 11% of girls have obesity; in New Zealand the prevalence is higher at 18% and 15% respectively. [37] Overweight and obesity prevalence is even higher in some of New Zealand’s ethnic groups (Maori, 37%; Pacific Islanders, 57%) but have largely unchanged since early 2000. [42]
Risk Factors
Various factors can influence body weight or greater weight gain in specific areas of the body. Some of these cannot be changed, but others may be modified:
- Non-modifiable risk factors (risk factors you can’t change): age, gender, genes, ethnic origin, and sometimes medications that change how energy is processed in the body leading to weight gain. There’s also strong evidence that having obesity in infancy or childhood increases the chances of remaining obese in adulthood.
- Risk factors that can be modified: food and beverages consumed, level of physical activity, daily screen time (increased screen time is associated with reduced physical activity time and also increases exposure to marketing of unhealthy foods/beverages), poor sleep hygiene, uncontrolled negative stress. While easier said than done, evidence has shown that addressing these factors as early as possible, even in childhood, may reduce the risk of developing obesity.
Obesity is complex and not just about being born with a certain body size, taking in more calories than the body needs, or burning extra calories through exercise to lose weight. It is often the result of a combination of several non-modifiable and modifiable risk factors. When looking at diet and food, which is often the focus with obesity, there are various factors to consider than just calories in/calories out:
- Living in a food environment that lacks access to healthy food choices or income-related barriers to regularly consuming a variety of healthy foods.
- Amount of low-nutrient ultra-processed foods and sugary beverages consumed, especially when displacing high-fiber whole foods, which can increase cravings .
- Eating behaviors such as skipping meals and eating heavy meals or snacks at night before bed.
- Overeating portions not from hunger but from stress or boredom.
The environments that surround us also play an important role, as they can make a modifiable risk factor a non-modifiable one. Examples are when someone does not have the ability to secure healthy food choices due to living in a food desert or a safe place to perform regular physical activity .
There are various risk factors for obesity, but not everyone with these risk factors develops obesity. And not everyone who has obesity develops health problems. In these cases, genes may play a role. Studies of siblings or twins show genetic factors that can determine weight and body size throughout life. [43] Some research suggests differences in genes in people who are of normal weight versus those carrying extra weight that may influence appetite control, metabolic rate, or even ability to change behavior. Gene-nutrient interactions can also promote obesity. For example, genes that increase risk of developing obesity have been reported to be stimulated by saturated fatty acids but not by unsaturated fatty acids . [43] The gut microbiome may also play a role in a person’s risk of developing obesity and chronic health conditions. [44]
However, obesity caused by mutations in a single gene, or monogenic obesity, is rare and is more likely influenced by changes in many different genes, called “common” obesity. Still, the modern obesity epidemic is largely fueled by environmental factors, with excess energy intake and low physical activity pinned as the main culprits. [45] First-degree family members (parents, siblings) who live together typically share similar environments that increase the risk of obesity, and health-related habits of parents are often passed onto their children. Examples include food choices, meal preparation methods (cooking at home vs. reliance on fast food), exercise, screen time, and sleep habits, as well as lack of access to outdoor green space.
These findings suggest that genetic factors make a small contribution to obesity risk, and that our genes are not our destiny. Many people who carry potential “obesity genes” do not become overweight, and healthy lifestyles can counteract these genetic effects.
Is Prevention Possible?
Many factors contribute to rising rates of obesity in children and adults. Among them, the abundance of low-priced, high-calorie ultra processed foods and sugary drinks; incessant marketing driving people to eat more; and an environment that reduces the need for regular physical activity.
Although preventing weight gain over the years of life may not be possible for everyone due to a variety of circumstances, there are strategies to reduce the amount of weight change by increasing awareness of modifiable risk factors and working toward healthy lifestyle behaviors.
However, focusing only on the individual (e.g., nutrition and lifestyle education, weight loss medications) has little impact on global obesity prevalence. Prevention requires a broader scope that addresses food systems and an obesogenic environment , including policy changes such as regulating the marketing of ultra-processed low-nutrient-dense foods and taxing items such as sugar-sweetened beverages.
Indeed, what sometimes gets lost in the discussion is that obesity is preventable . We can turn around the obesity epidemic by collaboratively creating an environment where the default option is the healthy choice.
Obesity prevention at the individual level and beyond
- World Health Organization. Obesity. https://www.who.int/health-topics/obesity . Accessed 3/2/2024.
- Centers for Disease Control and Prevention. Overweight & Obesity. https://www.cdc.gov/obesity/php/about/index.html . Accessed 3/2/2024.
- Centers for Disease Control and Prevention. Overweight & Obesity. Defining Child BMI Categories. https://www.cdc.gov/healthyweight/assessing/bmi/childrens_bmi/about_childrens_bmi.html . Accessed 3/2/2024.
- Singh AS, Mulder C, Twisk JW, Van Mechelen W, Chinapaw MJ. Tracking of childhood overweight into adulthood: a systematic review of the literature. Obesity reviews . 2008 Sep;9(5):474-88.
- Shai I, Jiang R, Manson JE, Stampfer MJ, Willett WC, Colditz GA, Hu FB. Ethnicity, obesity, and risk of type 2 diabetes in women: a 20-year follow-up study. Diabetes care . 2006 Jul 1;29(7):1585-90.
- Deurenberg-Yap M, Schmidt G, van Staveren WA, Deurenberg P. The paradox of low body mass index and high body fat percentage among Chinese, Malays and Indians in Singapore. International journal of obesity . 2000 Aug;24(8):1011-7.
- Wen CP, Cheng TY, Tsai SP, Chan HT, Hsu HL, Hsu CC, Eriksen MP. Are Asians at greater mortality risks for being overweight than Caucasians? Redefining obesity for Asians. Public health nutrition . 2009 Apr;12(4):497-506.
- Pan WH, Flegal KM, Chang HY, Yeh WT, Yeh CJ, Lee WC. Body mass index and obesity-related metabolic disorders in Taiwanese and US whites and blacks: implications for definitions of overweight and obesity for Asians. The American journal of clinical nutrition . 2004 Jan 1;79(1):31-9.
- Li Z, Daniel S, Fujioka K, Umashanker D. Obesity among Asian American people in the United States: a review. Obesity . 2023 Feb;31(2):316-28. Author disclosure: Ken Fujioka reports consultancy fees from Amgen Inc.; Boehringer Ingelheim; Gelesis; Janssen Global Services, LLC; Nalpropion Pharmaceuticals, Inc.; Novo Nordisk; and Rhythm Pharmaceuticals, Inc. Devika Umashanker reports consultancy fees from Novo Nordisk.
- Misra A, Khurana L. The metabolic syndrome in South Asians: epidemiology, determinants, and prevention. Metabolic syndrome and related disorders . 2009 Dec 1;7(6):497-514.
- Misra A, Vikram NK. Insulin resistance syndrome (metabolic syndrome) and obesity in Asian Indians: evidence and implications. Nutrition . 2004 May 1;20(5):482-91.
- Rush EC, Goedecke JH, Jennings C, Micklesfield L, Dugas L, Lambert EV, Plank LD. BMI, fat and muscle differences in urban women of five ethnicities from two countries. International journal of obesity . 2007 Aug;31(8):1232-9.
- Aloia JF, Vaswani A, Mikhail M, Flaster ER. Body composition by dual-energy X-ray absorptiometry in black compared with white women. Osteoporosis International . 1999 Aug;10:114-9.
- WHO Expert Consultation. Appropriate body‐mass index for Asian populations and its implications for policy and intervention strategies. Lancet . 2004;363:157‐163.
- Rimm EB, Stampfer MJ, Giovannucci E, Ascherio A, Spiegelman D, Colditz GA, Willett WC. Body size and fat distribution as predictors of coronary heart disease among middle-aged and older US men. American journal of epidemiology . 1995 Jun 15;141(12):1117-27.
- Willett WC, Manson JE, Stampfer MJ, Colditz GA, Rosner B, Speizer FE, Hennekens CH. Weight, weight change, and coronary heart disease in women: risk within the ‘normal’ weight range. JAMA . 1995 Feb 8;273(6):461-5.
- Colditz GA, Willett WC, Rotnitzky A, Manson JE. Weight gain as a risk factor for clinical diabetes mellitus in women. Annals of internal medicine . 1995 Apr 1;122(7):481-6.
- Maclure KM, Hayes KC, Colditz GA, Stampfer MJ, Speizer FE, Willett WC. Weight, diet, and the risk of symptomatic gallstones in middle-aged women. New England journal of medicine . 1989 Aug 31;321(9):563-9.
- Huang Z, Willett WC, Manson JE, Rosner B, Stampfer MJ, Speizer FE, Colditz GA. Body weight, weight change, and risk for hypertension in women. Annals of internal medicine . 1998 Jan 15;128(2):81-8.
- García MC. Potentially preventable deaths among the five leading causes of death—United States, 2010 and 2014. MMWR. Morbidity and Mortality Weekly Report . 2016;65.
- Van Nuys K, Globe D, Ng-Mak D, Cheung H, Sullivan J, Goldman D. The association between employee obesity and employer costs: evidence from a panel of US employers. American journal of health promotion . 2014 May;28(5):277-85.
- NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in underweight and obesity from 1990 to 2022: a pooled analysis of 3663 population-representative studies with 222 million children, adolescents, and adults. Lancet . 2024 Feb 29:S0140-6736(23)02750-2. Author disclosure: JLB reports personal fees from Novo Nordisk Denmark and voluntary work at the European Association for the Study of Obesity, outside the submitted work.
- NCD RisC Obesity Prevalence Rankings http://ncdrisc.org/obesity-prevalence-ranking.html
- Hales, Carroll, Fryar, Ogden. Prevalence of obesity and severe obesity among adults: United States, 2017-2018. N CHS Data Brief No. 360 . February 2020
- Ward ZJ, Bleich SN, Cradock AL, Barrett JL, Giles CM, Flax C, Long MW, Gortmaker SL. Projected US state-level prevalence of adult obesity and severe obesity. New England Journal of Medicine . 2019 Dec 19;381(25):2440-50.
- Public Health Agency of Canada. Obesity in Canada: A Joint Report from the Public Health Agency of Canada and the Canadian Institute for Health Information ; 2011.
- Hales CM, Carroll MD, Fryar CD, Ogden CL. Prevalence of obesity among adults and youth: United States, 2015-2016. NCHS Data Brief No. 288 . Oct 2017.
- Ogden CL, Carroll MD, Lawman HG, Fryar CD, Kruszon-Moran D, Kit BK, Flegal KM. Trends in obesity prevalence among children and adolescents in the United States, 1988-1994 through 2013-2014. JAMA . 2016 Jun 7;315(21):2292-9.
- Hales CM, Fryar CD, Carroll MD, Freedman DS, Ogden CL. Trends in obesity and severe obesity prevalence in US youth and adults by sex and age, 2007-2008 to 2015-2016. JAMA . 2018 Apr 24;319(16):1723-5.
- Ward ZJ, Long MW, Resch SC, Giles CM, Cradock AL, Gortmaker SL. Simulation of growth trajectories of childhood obesity into adulthood. New England Journal of Medicine. 2017 Nov 30;377(22):2145-53.
- Rao DP, Kropac E, Do MT, Roberts KC, Jayaraman GC. Childhood overweight and obesity trends in Canada. Health promotion and chronic disease prevention in Canada: research, policy and practice . 2016 Sep;36(9):194.
- Statistics Canada. Obesity in Canada. Prevalence in Aboriginal Populations. https://www.canada.ca/en/public-health/services/health-promotion/healthy-living/obesity-canada/prevalence-among-aboriginal-populations.html . Accessed on 9/17/2020.
- FAO, PAHO, WFP, UNICEF and IFAD. 2021. Regional Overview of Food Security and Nutrition in Latin America and the Caribbean 2020 – Food security and nutrition for lagged territories – In brief . Santiago.
- NCD Risk Factor Collaboration. Trends in adult body-mass index in 200 countries from 1975 to 2014: a pooled analysis of 1698 population-based measurement studies with 19.2 million participants. Lancet . 2016 Apr 4;387(10026):1377.
- Corvalán C, Garmendia ML, Jones‐Smith J, Lutter CK, Miranda JJ, Pedraza LS, Popkin BM, Ramirez‐Zea M, Salvo D, Stein AD. Nutrition status of children in Latin America. Obesity reviews . 2017 Jul;18:7-18.
- NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128.9 million children, adolescents, and adults. Lancet . 2017; 390: 2627-42.
- Ng M, Fleming T, Robinson M, Thomson B, Graetz N, Margono C, Mullany EC, Biryukov S, Abbafati C, Abera SF, Abraham JP. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet . 2014 Aug 30;384(9945):766-81.
- Garrido-Miguel M, Cavero-Redondo I, Álvarez-Bueno C, Rodríguez-Artalejo F, Moreno LA, Ruiz JR, Ahrens W, Martínez-Vizcaíno V. Prevalence and trends of overweight and obesity in European children from 1999 to 2016: a systematic review and meta-analysis. JAMA pediatrics . 2019 Oct 1;173(10):e192430-.
- Ziraba AK, Fotso JC, Ochako R. Overweight and obesity in urban Africa: a problem of the rich or the poor?. BMC public health . 2009 Dec;9:1-9.
- Ng SW, Zaghloul S, Ali HI, Harrison G, Popkin BM. The prevalence and trends of overweight, obesity and nutrition‐related non‐communicable diseases in the Arabian Gulf States. Obesity reviews . 2011 Jan;12(1):1-3.
- Olds TS, Tomkinson GR, Ferrar KE, Maher CA. Trends in the prevalence of childhood overweight and obesity in Australia between 1985 and 2008. International journal of obesity . 2010 Jan;34(1):57-66.
- Castillo JJ, Orlando RA, Garver WS. Gene-nutrient interactions and susceptibility to human obesity. Genes & nutrition . 2017 Dec;12:1-9.
- Mathur R, Barlow GM. Obesity and the microbiome. Expert Review of Gastroenterology & Hepatology . 2015 Aug 3;9(8):1087-99.
- Qasim A, Turcotte M, De Souza RJ, Samaan MC, Champredon D, Dushoff J, Speakman JR, Meyre D. On the origin of obesity: identifying the biological, environmental and cultural drivers of genetic risk among human populations. Obesity reviews . 2018 Feb;19(2):121-49.
Looking for The Obesity Prevention Source?
Terms of use.
The contents of this website are for educational purposes and are not intended to offer personal medical advice. You should seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website. The Nutrition Source does not recommend or endorse any products.
- Skip to main content
- Skip to secondary menu
- Skip to primary sidebar
- Skip to footer
A Plus Topper
Improve your Grades
Obesity Essay | Essay on Obesity for Students and Children in English
February 12, 2024 by Prasanna
Obesity Essay: Obesity is a condition that occurs when a person puts on excess body fat. It is a sudden and unusual increase in body fat. It can lead to heart-related diseases, blood pressure, hypertension, cholesterol, and various other health issues. The main cause of obesity is over-eating. Consuming junk food and staying away for physical activities can lead to an increase in the cases of obesity. Every 1 out of 5 children is facing obesity around the globe.
You can read more Essay Writing about articles, events, people, sports, technology many more.
Long and Short Essays on Obesity for Students and Kids in English
In this article, we have provided a long essay and a short essay, along with ten lines on the topic, to help students write this essay in examinations. Given below is a long essay composed of about 500 words and a short essay comprising 100-150 words on Obesity in English.
Long Essay on Obesity 500 words in English
Obesity essay is usually given to classes 7, 8, 9, and 10.
The world today is facing various complex diseases. Out of them, obesity is one. Obesity is a condition wherein a person starts to gain unnecessary body fat. This is an excessive and abnormal increase in body fat which can lead to various other related health issues like heart problems, blood pressure, hypertension, cholesterol, and many more. Some people think of obesity as only a cosmetic and physical concern but that’s not true.
The lifestyle of people has changed a lot. Instead of focusing more on physical activities, there has been a paradigm shift to adapting non-physical activities. Children used to play in parks and playgrounds with friends whereas now the preference has been shifted to mobile and computer games. Not only children but also elders have changed their lifestyle a lot. Previously, people preferred to do everything by themselves. Right from doing household chores to getting things from the market, everything was done manually. But time has changed a lot. Now, everything gets delivered at the doorstep. This type of lifestyle has lead to various diseases including obesity.
Additionally, obesity is even caused due to genetics as well. Some people have heredity or have genes that force them to gain weight faster as compared to others. Also, there are some medications like those consumed by bodybuilders (steroids), antidepressants, and medicines for diabetes that make changes in the body metabolism in such a way that the appetite increases resulting in gaining weight. Some people are couch potatoes and foodaholic which means they can’t stay away from food. Under such a situation the appetite increase and the chances to fill oneself with junk food enhances. This kind of habit positively increases the chances of becoming obese.
Ever-increasing cases of obesity are surely a cause of concern, but there are various cures available to treat it. Also, not every treatment is related to medication or surgery. Some of the treatments are such that are related to changes in diet and adapting to physical activities. Eating a healthy, fibrous, and nutritious diet can help reduce that excess weight. Also not munching in between and following a diet routine can help to cure obesity.
Secondly, by doing some physical activities like walking, jogging, running, or exercising one can also burn unwanted fat and calories, thereby reducing obesity. There are various drug therapies as well as surgeries like bariatric surgery that can help reduce the weight. The drug therapies can be long term as well as short term depending on the weight to be reduced. But usually, these are clubbed with natural therapies like exercising and yoga.
Obesity is now concerning more and more people. It is thus necessary to make people aware of the symptoms, causes, and cures of the disease as well. This will help to take the necessary steps and combat obesity. Everybody should adapt to the health-enhancing lifestyle and should try to reduce unhealthy habits as much as possible. It is quite true that junk food is attractive and a healthy plate looks dull but to stay healthy and fit, one needs to choose the healthy plate over junk. This is the best way to keep the self and family away from obesity.
Short Essay on Obesity 150 words in English
Obesity essay is usually provided to classes 1, 2, 3, 4, 5, and 6.
Obesity is a cause of serious concern today. Although, many may not think of obesity as the disease still the effects of obesity can lead to various health issues. Obesity is a situation where a person faces a continuous increase in body mass. This increase is usually not normal and hence is a cause of concern. The diseases linked to obesity range from blood pressure, heart issues, hypertension, and diabetes as well. There are many causes of obesity. The most common cause of obesity is unhealthy food habits. An increase in the consumption of junk foods and munching in between leads to obesity.
The second cause of obesity is a decrease in physical activities. People have turned to couch potatoes. They prefer to sit and watch television rather than going out and doing physical exercises like running, walking, jogging, or yoga. The third reason is related to heredity or genetics. Apart there are other reasons related to medication that result in weight gain. There are various natural as well as medical treatments available for obesity. Adapting to healthy food habits and daily exercising can reduce weight. It can lead to a reduction in obesity. Apart there are drug-related therapies as well as surgeries like bariatric surgery available to reduce that excess weight.
It is important to adapt to a healthy lifestyle which includes intake of nutritious food and exercise to reduce obesity. Also making people aware of cause and cures of obesity can be of great use. The best way to keep the self and family away from obesity is to have a healthy lifestyle.
10 Lines on Obesity Essay in English
- Obesity is very common today. It is a situation where a person gains excessive and abnormal weight.
- It has affected 1 out of every 5 individuals in the world.
- It can lead to various diseases such as heart-related, hypertension, blood pressure, and many more.
- There are various causes of obesity right from genetic to habit related.
- Increased intake of junk food, decreased physical activities, increased medication, and unhealthy lifestyle is some major causes of obesity.
- The cases of obesity are more prevalent in children as they tend to be couch potatoes.
- Obesity can be cured by natural as well as medical ways.
- Natural ways to cure obesity include healthy food habits, a healthy lifestyle, and exercising.
- Medical treatments for obesity include drug treatment and surgeries like bariatric surgery.
- Making people aware of how to adapt to a better lifestyle can reduce the chances of obesity.
FAQ’s on Obesity Essay
Question 1. What is Obesity?
Answer: Obesity refers to a situation where the person gains abnormal and excessive weight. Such an increase in weight can lead to health issues.
Question 2. What are the causes of Obesity?
Answer: There are various causes of obesity. The main causes of obesity are unhealthy food habits, reduced physical exercises, increased medication, couch potato nature, and heredity.
Question 3. How can we cure obesity?
Answer: There are various natural and medical cures available for obesity. These include healthy food habits, exercising, drug treatment, and surgeries like bariatric surgery.
Question 4. What steps can be taken to reduce cases of obesity?
Answer: The steps that can be taken to reduce the chances of obesity are as follow:
- Intake of healthy food
- Adapting to a better lifestyle
- Say no to munching and junk food.
- Picture Dictionary
- English Speech
- English Slogans
- English Letter Writing
- English Essay Writing
- English Textbook Answers
- Types of Certificates
- ICSE Solutions
- Selina ICSE Solutions
- ML Aggarwal Solutions
- HSSLive Plus One
- HSSLive Plus Two
- Kerala SSLC
- Distance Education
- Search Menu
Sign in through your institution
- Browse content in Arts and Humanities
- Browse content in Archaeology
- Anglo-Saxon and Medieval Archaeology
- Archaeological Methodology and Techniques
- Archaeology by Region
- Archaeology of Religion
- Archaeology of Trade and Exchange
- Biblical Archaeology
- Contemporary and Public Archaeology
- Environmental Archaeology
- Historical Archaeology
- History and Theory of Archaeology
- Industrial Archaeology
- Landscape Archaeology
- Mortuary Archaeology
- Prehistoric Archaeology
- Underwater Archaeology
- Zooarchaeology
- Browse content in Architecture
- Architectural Structure and Design
- History of Architecture
- Residential and Domestic Buildings
- Theory of Architecture
- Browse content in Art
- Art Subjects and Themes
- History of Art
- Industrial and Commercial Art
- Theory of Art
- Biographical Studies
- Byzantine Studies
- Browse content in Classical Studies
- Classical History
- Classical Philosophy
- Classical Mythology
- Classical Numismatics
- Classical Literature
- Classical Reception
- Classical Art and Architecture
- Classical Oratory and Rhetoric
- Greek and Roman Epigraphy
- Greek and Roman Law
- Greek and Roman Archaeology
- Greek and Roman Papyrology
- Late Antiquity
- Religion in the Ancient World
- Social History
- Digital Humanities
- Browse content in History
- Colonialism and Imperialism
- Diplomatic History
- Environmental History
- Genealogy, Heraldry, Names, and Honours
- Genocide and Ethnic Cleansing
- Historical Geography
- History by Period
- History of Agriculture
- History of Education
- History of Emotions
- History of Gender and Sexuality
- Industrial History
- Intellectual History
- International History
- Labour History
- Legal and Constitutional History
- Local and Family History
- Maritime History
- Military History
- National Liberation and Post-Colonialism
- Oral History
- Political History
- Public History
- Regional and National History
- Revolutions and Rebellions
- Slavery and Abolition of Slavery
- Social and Cultural History
- Theory, Methods, and Historiography
- Urban History
- World History
- Browse content in Language Teaching and Learning
- Language Learning (Specific Skills)
- Language Teaching Theory and Methods
- Browse content in Linguistics
- Applied Linguistics
- Cognitive Linguistics
- Computational Linguistics
- Forensic Linguistics
- Grammar, Syntax and Morphology
- Historical and Diachronic Linguistics
- History of English
- Language Acquisition
- Language Variation
- Language Families
- Language Evolution
- Language Reference
- Lexicography
- Linguistic Theories
- Linguistic Typology
- Linguistic Anthropology
- Phonetics and Phonology
- Psycholinguistics
- Sociolinguistics
- Translation and Interpretation
- Writing Systems
- Browse content in Literature
- Bibliography
- Children's Literature Studies
- Literary Studies (Asian)
- Literary Studies (European)
- Literary Studies (Eco-criticism)
- Literary Studies (Modernism)
- Literary Studies (Romanticism)
- Literary Studies (American)
- Literary Studies - World
- Literary Studies (1500 to 1800)
- Literary Studies (19th Century)
- Literary Studies (20th Century onwards)
- Literary Studies (African American Literature)
- Literary Studies (British and Irish)
- Literary Studies (Early and Medieval)
- Literary Studies (Fiction, Novelists, and Prose Writers)
- Literary Studies (Gender Studies)
- Literary Studies (Graphic Novels)
- Literary Studies (History of the Book)
- Literary Studies (Plays and Playwrights)
- Literary Studies (Poetry and Poets)
- Literary Studies (Postcolonial Literature)
- Literary Studies (Queer Studies)
- Literary Studies (Science Fiction)
- Literary Studies (Travel Literature)
- Literary Studies (War Literature)
- Literary Studies (Women's Writing)
- Literary Theory and Cultural Studies
- Mythology and Folklore
- Shakespeare Studies and Criticism
- Browse content in Media Studies
- Browse content in Music
- Applied Music
- Dance and Music
- Ethics in Music
- Ethnomusicology
- Gender and Sexuality in Music
- Medicine and Music
- Music Cultures
- Music and Religion
- Music and Culture
- Music and Media
- Music Education and Pedagogy
- Music Theory and Analysis
- Musical Scores, Lyrics, and Libretti
- Musical Structures, Styles, and Techniques
- Musicology and Music History
- Performance Practice and Studies
- Race and Ethnicity in Music
- Sound Studies
- Browse content in Performing Arts
- Browse content in Philosophy
- Aesthetics and Philosophy of Art
- Epistemology
- Feminist Philosophy
- History of Western Philosophy
- Metaphysics
- Moral Philosophy
- Non-Western Philosophy
- Philosophy of Science
- Philosophy of Action
- Philosophy of Law
- Philosophy of Religion
- Philosophy of Language
- Philosophy of Mind
- Philosophy of Perception
- Philosophy of Mathematics and Logic
- Practical Ethics
- Social and Political Philosophy
- Browse content in Religion
- Biblical Studies
- Christianity
- East Asian Religions
- History of Religion
- Judaism and Jewish Studies
- Qumran Studies
- Religion and Education
- Religion and Health
- Religion and Politics
- Religion and Science
- Religion and Law
- Religion and Art, Literature, and Music
- Religious Studies
- Browse content in Society and Culture
- Cookery, Food, and Drink
- Cultural Studies
- Customs and Traditions
- Ethical Issues and Debates
- Hobbies, Games, Arts and Crafts
- Natural world, Country Life, and Pets
- Popular Beliefs and Controversial Knowledge
- Sports and Outdoor Recreation
- Technology and Society
- Travel and Holiday
- Visual Culture
- Browse content in Law
- Arbitration
- Browse content in Company and Commercial Law
- Commercial Law
- Company Law
- Browse content in Comparative Law
- Systems of Law
- Competition Law
- Browse content in Constitutional and Administrative Law
- Government Powers
- Judicial Review
- Local Government Law
- Military and Defence Law
- Parliamentary and Legislative Practice
- Construction Law
- Contract Law
- Browse content in Criminal Law
- Criminal Procedure
- Criminal Evidence Law
- Sentencing and Punishment
- Employment and Labour Law
- Environment and Energy Law
- Browse content in Financial Law
- Banking Law
- Insolvency Law
- History of Law
- Human Rights and Immigration
- Intellectual Property Law
- Browse content in International Law
- Private International Law and Conflict of Laws
- Public International Law
- IT and Communications Law
- Jurisprudence and Philosophy of Law
- Law and Politics
- Law and Society
- Browse content in Legal System and Practice
- Courts and Procedure
- Legal Skills and Practice
- Legal System - Costs and Funding
- Primary Sources of Law
- Regulation of Legal Profession
- Medical and Healthcare Law
- Browse content in Policing
- Criminal Investigation and Detection
- Police and Security Services
- Police Procedure and Law
- Police Regional Planning
- Browse content in Property Law
- Personal Property Law
- Restitution
- Study and Revision
- Terrorism and National Security Law
- Browse content in Trusts Law
- Wills and Probate or Succession
- Browse content in Medicine and Health
- Browse content in Allied Health Professions
- Arts Therapies
- Clinical Science
- Dietetics and Nutrition
- Occupational Therapy
- Operating Department Practice
- Physiotherapy
- Radiography
- Speech and Language Therapy
- Browse content in Anaesthetics
- General Anaesthesia
- Browse content in Clinical Medicine
- Acute Medicine
- Cardiovascular Medicine
- Clinical Genetics
- Clinical Pharmacology and Therapeutics
- Dermatology
- Endocrinology and Diabetes
- Gastroenterology
- Genito-urinary Medicine
- Geriatric Medicine
- Infectious Diseases
- Medical Oncology
- Medical Toxicology
- Pain Medicine
- Palliative Medicine
- Rehabilitation Medicine
- Respiratory Medicine and Pulmonology
- Rheumatology
- Sleep Medicine
- Sports and Exercise Medicine
- Clinical Neuroscience
- Community Medical Services
- Critical Care
- Emergency Medicine
- Forensic Medicine
- Haematology
- History of Medicine
- Browse content in Medical Dentistry
- Oral and Maxillofacial Surgery
- Paediatric Dentistry
- Restorative Dentistry and Orthodontics
- Surgical Dentistry
- Medical Ethics
- Browse content in Medical Skills
- Clinical Skills
- Communication Skills
- Nursing Skills
- Surgical Skills
- Medical Statistics and Methodology
- Browse content in Neurology
- Clinical Neurophysiology
- Neuropathology
- Nursing Studies
- Browse content in Obstetrics and Gynaecology
- Gynaecology
- Occupational Medicine
- Ophthalmology
- Otolaryngology (ENT)
- Browse content in Paediatrics
- Neonatology
- Browse content in Pathology
- Chemical Pathology
- Clinical Cytogenetics and Molecular Genetics
- Histopathology
- Medical Microbiology and Virology
- Patient Education and Information
- Browse content in Pharmacology
- Psychopharmacology
- Browse content in Popular Health
- Caring for Others
- Complementary and Alternative Medicine
- Self-help and Personal Development
- Browse content in Preclinical Medicine
- Cell Biology
- Molecular Biology and Genetics
- Reproduction, Growth and Development
- Primary Care
- Professional Development in Medicine
- Browse content in Psychiatry
- Addiction Medicine
- Child and Adolescent Psychiatry
- Forensic Psychiatry
- Learning Disabilities
- Old Age Psychiatry
- Psychotherapy
- Browse content in Public Health and Epidemiology
- Epidemiology
- Public Health
- Browse content in Radiology
- Clinical Radiology
- Interventional Radiology
- Nuclear Medicine
- Radiation Oncology
- Reproductive Medicine
- Browse content in Surgery
- Cardiothoracic Surgery
- Gastro-intestinal and Colorectal Surgery
- General Surgery
- Neurosurgery
- Paediatric Surgery
- Peri-operative Care
- Plastic and Reconstructive Surgery
- Surgical Oncology
- Transplant Surgery
- Trauma and Orthopaedic Surgery
- Vascular Surgery
- Browse content in Science and Mathematics
- Browse content in Biological Sciences
- Aquatic Biology
- Biochemistry
- Bioinformatics and Computational Biology
- Developmental Biology
- Ecology and Conservation
- Evolutionary Biology
- Genetics and Genomics
- Microbiology
- Molecular and Cell Biology
- Natural History
- Plant Sciences and Forestry
- Research Methods in Life Sciences
- Structural Biology
- Systems Biology
- Zoology and Animal Sciences
- Browse content in Chemistry
- Analytical Chemistry
- Computational Chemistry
- Crystallography
- Environmental Chemistry
- Industrial Chemistry
- Inorganic Chemistry
- Materials Chemistry
- Medicinal Chemistry
- Mineralogy and Gems
- Organic Chemistry
- Physical Chemistry
- Polymer Chemistry
- Study and Communication Skills in Chemistry
- Theoretical Chemistry
- Browse content in Computer Science
- Artificial Intelligence
- Computer Architecture and Logic Design
- Game Studies
- Human-Computer Interaction
- Mathematical Theory of Computation
- Programming Languages
- Software Engineering
- Systems Analysis and Design
- Virtual Reality
- Browse content in Computing
- Business Applications
- Computer Security
- Computer Games
- Computer Networking and Communications
- Digital Lifestyle
- Graphical and Digital Media Applications
- Operating Systems
- Browse content in Earth Sciences and Geography
- Atmospheric Sciences
- Environmental Geography
- Geology and the Lithosphere
- Maps and Map-making
- Meteorology and Climatology
- Oceanography and Hydrology
- Palaeontology
- Physical Geography and Topography
- Regional Geography
- Soil Science
- Urban Geography
- Browse content in Engineering and Technology
- Agriculture and Farming
- Biological Engineering
- Civil Engineering, Surveying, and Building
- Electronics and Communications Engineering
- Energy Technology
- Engineering (General)
- Environmental Science, Engineering, and Technology
- History of Engineering and Technology
- Mechanical Engineering and Materials
- Technology of Industrial Chemistry
- Transport Technology and Trades
- Browse content in Environmental Science
- Applied Ecology (Environmental Science)
- Conservation of the Environment (Environmental Science)
- Environmental Sustainability
- Environmentalist Thought and Ideology (Environmental Science)
- Management of Land and Natural Resources (Environmental Science)
- Natural Disasters (Environmental Science)
- Nuclear Issues (Environmental Science)
- Pollution and Threats to the Environment (Environmental Science)
- Social Impact of Environmental Issues (Environmental Science)
- History of Science and Technology
- Browse content in Materials Science
- Ceramics and Glasses
- Composite Materials
- Metals, Alloying, and Corrosion
- Nanotechnology
- Browse content in Mathematics
- Applied Mathematics
- Biomathematics and Statistics
- History of Mathematics
- Mathematical Education
- Mathematical Finance
- Mathematical Analysis
- Numerical and Computational Mathematics
- Probability and Statistics
- Pure Mathematics
- Browse content in Neuroscience
- Cognition and Behavioural Neuroscience
- Development of the Nervous System
- Disorders of the Nervous System
- History of Neuroscience
- Invertebrate Neurobiology
- Molecular and Cellular Systems
- Neuroendocrinology and Autonomic Nervous System
- Neuroscientific Techniques
- Sensory and Motor Systems
- Browse content in Physics
- Astronomy and Astrophysics
- Atomic, Molecular, and Optical Physics
- Biological and Medical Physics
- Classical Mechanics
- Computational Physics
- Condensed Matter Physics
- Electromagnetism, Optics, and Acoustics
- History of Physics
- Mathematical and Statistical Physics
- Measurement Science
- Nuclear Physics
- Particles and Fields
- Plasma Physics
- Quantum Physics
- Relativity and Gravitation
- Semiconductor and Mesoscopic Physics
- Browse content in Psychology
- Affective Sciences
- Clinical Psychology
- Cognitive Neuroscience
- Cognitive Psychology
- Criminal and Forensic Psychology
- Developmental Psychology
- Educational Psychology
- Evolutionary Psychology
- Health Psychology
- History and Systems in Psychology
- Music Psychology
- Neuropsychology
- Organizational Psychology
- Psychological Assessment and Testing
- Psychology of Human-Technology Interaction
- Psychology Professional Development and Training
- Research Methods in Psychology
- Social Psychology
- Browse content in Social Sciences
- Browse content in Anthropology
- Anthropology of Religion
- Human Evolution
- Medical Anthropology
- Physical Anthropology
- Regional Anthropology
- Social and Cultural Anthropology
- Theory and Practice of Anthropology
- Browse content in Business and Management
- Business Strategy
- Business History
- Business Ethics
- Business and Government
- Business and Technology
- Business and the Environment
- Comparative Management
- Corporate Governance
- Corporate Social Responsibility
- Entrepreneurship
- Health Management
- Human Resource Management
- Industrial and Employment Relations
- Industry Studies
- Information and Communication Technologies
- International Business
- Knowledge Management
- Management and Management Techniques
- Operations Management
- Organizational Theory and Behaviour
- Pensions and Pension Management
- Public and Nonprofit Management
- Social Issues in Business and Management
- Strategic Management
- Supply Chain Management
- Browse content in Criminology and Criminal Justice
- Criminal Justice
- Criminology
- Forms of Crime
- International and Comparative Criminology
- Youth Violence and Juvenile Justice
- Development Studies
- Browse content in Economics
- Agricultural, Environmental, and Natural Resource Economics
- Asian Economics
- Behavioural Finance
- Behavioural Economics and Neuroeconomics
- Econometrics and Mathematical Economics
- Economic Systems
- Economic Methodology
- Economic History
- Economic Development and Growth
- Financial Markets
- Financial Institutions and Services
- General Economics and Teaching
- Health, Education, and Welfare
- History of Economic Thought
- International Economics
- Labour and Demographic Economics
- Law and Economics
- Macroeconomics and Monetary Economics
- Microeconomics
- Public Economics
- Urban, Rural, and Regional Economics
- Welfare Economics
- Browse content in Education
- Adult Education and Continuous Learning
- Care and Counselling of Students
- Early Childhood and Elementary Education
- Educational Equipment and Technology
- Educational Strategies and Policy
- Higher and Further Education
- Organization and Management of Education
- Philosophy and Theory of Education
- Schools Studies
- Secondary Education
- Teaching of a Specific Subject
- Teaching of Specific Groups and Special Educational Needs
- Teaching Skills and Techniques
- Browse content in Environment
- Applied Ecology (Social Science)
- Climate Change
- Conservation of the Environment (Social Science)
- Environmentalist Thought and Ideology (Social Science)
- Management of Land and Natural Resources (Social Science)
- Natural Disasters (Environment)
- Pollution and Threats to the Environment (Social Science)
- Social Impact of Environmental Issues (Social Science)
- Sustainability
- Browse content in Human Geography
- Cultural Geography
- Economic Geography
- Political Geography
- Browse content in Interdisciplinary Studies
- Communication Studies
- Museums, Libraries, and Information Sciences
- Browse content in Politics
- African Politics
- Asian Politics
- Chinese Politics
- Comparative Politics
- Conflict Politics
- Elections and Electoral Studies
- Environmental Politics
- Ethnic Politics
- European Union
- Foreign Policy
- Gender and Politics
- Human Rights and Politics
- Indian Politics
- International Relations
- International Organization (Politics)
- Irish Politics
- Latin American Politics
- Middle Eastern Politics
- Political Methodology
- Political Communication
- Political Philosophy
- Political Sociology
- Political Theory
- Political Behaviour
- Political Economy
- Political Institutions
- Politics and Law
- Politics of Development
- Public Administration
- Public Policy
- Qualitative Political Methodology
- Quantitative Political Methodology
- Regional Political Studies
- Russian Politics
- Security Studies
- State and Local Government
- UK Politics
- US Politics
- Browse content in Regional and Area Studies
- African Studies
- Asian Studies
- East Asian Studies
- Japanese Studies
- Latin American Studies
- Middle Eastern Studies
- Native American Studies
- Scottish Studies
- Browse content in Research and Information
- Research Methods
- Browse content in Social Work
- Addictions and Substance Misuse
- Adoption and Fostering
- Care of the Elderly
- Child and Adolescent Social Work
- Couple and Family Social Work
- Direct Practice and Clinical Social Work
- Emergency Services
- Human Behaviour and the Social Environment
- International and Global Issues in Social Work
- Mental and Behavioural Health
- Social Justice and Human Rights
- Social Policy and Advocacy
- Social Work and Crime and Justice
- Social Work Macro Practice
- Social Work Practice Settings
- Social Work Research and Evidence-based Practice
- Welfare and Benefit Systems
- Browse content in Sociology
- Childhood Studies
- Community Development
- Comparative and Historical Sociology
- Disability Studies
- Economic Sociology
- Gender and Sexuality
- Gerontology and Ageing
- Health, Illness, and Medicine
- Marriage and the Family
- Migration Studies
- Occupations, Professions, and Work
- Organizations
- Population and Demography
- Race and Ethnicity
- Social Theory
- Social Movements and Social Change
- Social Research and Statistics
- Social Stratification, Inequality, and Mobility
- Sociology of Religion
- Sociology of Education
- Sport and Leisure
- Urban and Rural Studies
- Browse content in Warfare and Defence
- Defence Strategy, Planning, and Research
- Land Forces and Warfare
- Military Administration
- Military Life and Institutions
- Naval Forces and Warfare
- Other Warfare and Defence Issues
- Peace Studies and Conflict Resolution
- Weapons and Equipment

- < Previous chapter

26 Conclusion: Obesity and its prevention in the 21st century
- Published: September 2010
- Cite Icon Cite
- Permissions Icon Permissions
The case for a preventative approach to the obesity epidemic is compelling. Obesity poses what is arguably one of the most significant threats to population health that is currently faced. The data presented in this book highlight just how common obesity has become in children and in adults across the globe, and how it impacts disproportionately on the poor. This chapter presents a summary of the discussions in the preceding chapters.
Personal account
- Sign in with email/username & password
- Get email alerts
- Save searches
- Purchase content
- Activate your purchase/trial code
- Add your ORCID iD
Institutional access
Sign in with a library card.
- Sign in with username/password
- Recommend to your librarian
- Institutional account management
- Get help with access
Access to content on Oxford Academic is often provided through institutional subscriptions and purchases. If you are a member of an institution with an active account, you may be able to access content in one of the following ways:
IP based access
Typically, access is provided across an institutional network to a range of IP addresses. This authentication occurs automatically, and it is not possible to sign out of an IP authenticated account.
Choose this option to get remote access when outside your institution. Shibboleth/Open Athens technology is used to provide single sign-on between your institution’s website and Oxford Academic.
- Click Sign in through your institution.
- Select your institution from the list provided, which will take you to your institution's website to sign in.
- When on the institution site, please use the credentials provided by your institution. Do not use an Oxford Academic personal account.
- Following successful sign in, you will be returned to Oxford Academic.
If your institution is not listed or you cannot sign in to your institution’s website, please contact your librarian or administrator.
Enter your library card number to sign in. If you cannot sign in, please contact your librarian.
Society Members
Society member access to a journal is achieved in one of the following ways:
Sign in through society site
Many societies offer single sign-on between the society website and Oxford Academic. If you see ‘Sign in through society site’ in the sign in pane within a journal:
- Click Sign in through society site.
- When on the society site, please use the credentials provided by that society. Do not use an Oxford Academic personal account.
If you do not have a society account or have forgotten your username or password, please contact your society.
Sign in using a personal account
Some societies use Oxford Academic personal accounts to provide access to their members. See below.
A personal account can be used to get email alerts, save searches, purchase content, and activate subscriptions.
Some societies use Oxford Academic personal accounts to provide access to their members.
Viewing your signed in accounts
Click the account icon in the top right to:
- View your signed in personal account and access account management features.
- View the institutional accounts that are providing access.
Signed in but can't access content
Oxford Academic is home to a wide variety of products. The institutional subscription may not cover the content that you are trying to access. If you believe you should have access to that content, please contact your librarian.
For librarians and administrators, your personal account also provides access to institutional account management. Here you will find options to view and activate subscriptions, manage institutional settings and access options, access usage statistics, and more.
Our books are available by subscription or purchase to libraries and institutions.
| Month: | Total Views: |
|---|---|
| October 2022 | 3 |
| November 2022 | 5 |
| December 2022 | 1 |
| January 2023 | 8 |
| February 2023 | 7 |
| March 2023 | 2 |
| April 2023 | 3 |
| May 2023 | 1 |
| July 2023 | 1 |
| October 2023 | 4 |
| December 2023 | 1 |
| February 2024 | 3 |
| March 2024 | 2 |
| June 2024 | 2 |
| July 2024 | 3 |
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Rights and permissions
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
- Causes of Obesity
About About Obesity Causes of Obesity
- Prevalence of Obesity
- Obesity Classification
- Prevention of Obesity
What causes obesity? In its simplest sense, the body gains fat when it stores excess energy, and this excess energy arises from consuming more food energy than is burnt in physiological metabolism.
This imbalance in energy consumption and expenditure has several causes: in some cases it may be a genetic disorder but in most cases it arises from living in an environment that allows and encourages low levels of physical activity, extended sedentary behaviour and plentiful consumption of food, especially food rich in energy (e.g. in the form of fats, oils, sugars and starches).
In such ‘obesogenic’ environments it is hard to resist weight gain as we are naturally programmed to minimise effort and store excess food as body-fat. Once we have gained weight, however, it can be difficult to lose it.

Causes of obesity
The ROOTS of obesity
To have a real impact on obesity, we need to work together to address its many root causes throughout society.

- Commercial determinants of obesity
Obesity is a complex disease triggered by interlinking causes, from genetics to dysfunctional food systems, to social deprivation.

Weight stigma
The drivers of stigma are primarily based around a misunderstanding of the complex causes of obesity.

Consequences of obesity
People who live with obesity find it stressful and demoralising. Efforts to lose weight are frequently unsuccessful, and there is a continual feeling of hunger. While it is possible to experience apparent good health, excess bodyweight is well-known for increasing the risk of having a stroke or getting heart disease, of developing diabetes, of liver disorders and certain cancers. It also leads to orthopaedic problems with joints and back pain.
In both children and adults, obesity can lead to social stigma and isolation, reducing attendance at school and making it harder to find work and keep a job. In some countries a person with severe obesity may be registered as disabled, and be protected by anti-discrimination legislation.

"Across the world, obesity rates have increased in the last two decades in nearly all age groups. By 2025 it is estimated that 2.7 billion adults and 268 million school-age children will be overweight or obese."
What needs to change?
We need to educate, challenge and raise awareness in order to halt the growth in global obesity.
Read on to learn more about obesity classification.
Share this page
Training & Events
SCOPE E-Learning
We offer the only internationally recognised course on obesity management. Read more here.
Global Obesity Observatory
We offer various statistics, maps and key data around the topic of obesity. You can find all that and more here.
Policy & Advocacy
Our Policy Priorities
We have developed five key areas of policy that are a priority to us. Want to know more? Check them out here!
- Our Members
- Member Benefits
- Membership Application Form
- Partnerships
- Global Obesity Forum
- Patient Portal
- Finance Committee
- Annual Report and Financials
- Obesity as a disease
- Childhood Obesity
- Obesity in Universal Health Coverage
- Weight Stigma
- The ROOTS of Obesity
- World Obesity Day
- Healthy Venues
- Reinventing the Food System: A Report
- The Spotlight Project
- SCOPE Examination
- Guide to SCOPE Certification
- SCOPE Fellows
- Leadership Programme
- Accreditation
- SCOPE Schools
- SCOPE Pricing
- SCOPE Sessions
- SCOPE Accredited Events
- Event Archive
- International Congress on Obesity
Sign up for notifications
- Find Your Calm: Managing Stress & Anxiety
Stress Symptoms

What Is Stress?
Stress is your body's response to a challenging or demanding situation. When you feel stressed, your body releases certain hormones. Your hormones are chemical signals your body uses to tell your body systems what to do. The hormones your body releases when you're stressed get you ready to meet the challenge or demand in your environment. During the stress response, your body gets ready to flee or fight by increasing your heart rate, breathing rate, and blood pressure.
Not all stress is bad. In small doses, stress can help you accomplish tasks or prevent you from getting hurt. For example, stress is what makes you slam on the brakes to avoid hitting a suddenly stopped car in front of you. That's a good thing.
But people handle stressful situations differently. What stresses you out may be of little concern to someone else.
Stress can be a short-term response to something that happens once or only a few times or a long-term response to something that keeps happening. Our bodies can usually handle short-term stress without long-term effects. But long-term or chronic stress can make you sick, both mentally and physically.
The first step to managing your stress is to know the symptoms. But recognizing stress symptoms may be harder than you think. Many of us are so used to feeling stressed that we may not know it until we get sick. Read on to learn more about the various symptoms you may have when you're stressed.
Difference between stress and distress
Stress is a normal reaction to challenges in your physical environment or in your perceptions of what's happening around you. Experts consider distress to be stress that is severe, prolonged, or both. Distress is when you feel you’re under more stress than you can handle.
Emotional Stress Symptoms
Mental symptoms of emotional stress include:
- Feeling more emotional than usual, especially feeling grumpy, teary, or angry
- Feeling anxious, overwhelmed, nervous, or on edge
- Feeling sad or depressed
- Feeling restless
- Trouble keeping track of or remembering things
- Trouble getting your work done, solving problems, making decisions, or concentrating
Physical Stress Symptoms
Symptoms of stress that you might feel in your body include:
- Clenching your jaw and grinding your teeth
- Shoulder, neck, or back pain; general body aches, pains, and tense muscles
- Chest pain, increased heart rate, heaviness in your chest
- Shortness of breath
- Feeling more tired than usual (fatigue)
- Sleeping more or less than usual
- Upset stomach , including diarrhea , constipation , and nausea
- Loss of sexual desire and/or ability
- Getting sick more easily, such as getting colds and infections often
Respiratory distress
This is when you aren't getting enough oxygen or are having to work really hard to breathe. If you or a loved one has symptoms of respiratory distress, you need to call 911 and get to the ER as soon as possible. Signs include:
- Breathing faster than usual
- Color changes of your skin, mouth, lips, or fingernails. A blue color around your mouth, lips, or fingernails usually shows you aren't getting enough oxygen. Your skin may also look pale or gray.
- Grunting when you breath out
- A whistling with each breath (wheezing)
- Nose flaring
- Chest sinking below your neck or under your breastbone with each breath (retractions)
- Increased sweating, especially cold, clammy skin on your forehead
- Leaning forward while sitting to help take deeper breaths
Cognitive Stress Symptoms
Symptoms of stress that affect your mental performance include:
- Trouble getting your work done, solving problems, making decisions, or concentrating
- Feeling less commitment to your work
- Lack of motivation
- Negative thinking
Behavioral Stress Symptoms
Symptoms of behavioral stress include:
- Changes in your eating habits; losing or gaining weight
- Procrastinating and avoiding responsibilities
- Using alcohol, tobacco, or drugs to feel better
- Avoiding your friends and family; isolating yourself from others
- Failing to meet your deadlines
- Increased absences at school or work
- Doing your work more slowly
- Exercising less often
Symptoms of Chronic Stress
Chronic stress is when you experience stress over an extended time. This can have negative effects on your body and your mental state, and it can increase your risk of cardiovascular disease, anxiety, and depression.
In general, the symptoms of chronic stress are the same as those for shorter-term stress. You may not have all these symptoms, but if you have more than three symptoms and they last for a few weeks, you may have chronic stress. Potential symptoms to look for include:
- Aches and pains
- Changes in your sleeping patterns, such as insomnia or sleepiness
- Changes in your social behavior, such as avoiding other people
- Changes in your emotional response to others
- Emotional withdrawal
- Low energy, fatigue
- Unfocused or cloudy thinking
- Changes in your appetite
- Increased alcohol or drug use
- Getting sick more often than usual
Is It Stress or Something Else?
You may be dealing with something more serious than day-to-day stress if you have symptoms over a period of time even though you've tried to cope using healthy mechanisms. Long-term stress is linked to number of mental health disorders, such as:
- Chronic stress
- Substance use disorder
- Disordered eating
It may be time to visit your doctor if you're struggling to cope with the stress in your life or you have mental health problems from long-term stress. They can help you figure out ways of coping in a healthy way or refer you to a mental health professional who can help you.
Posttraumatic Stress Disorder
Posttraumatic stress disorder (PTSD) is mental health condition that you may have after you have or witness a traumatic event, such as a natural disaster, accident, or violence. PTSD overwhelms your ability to cope with new stress. PTSD can lead to symptoms such as intrusive memories, avoidance behaviors, and hyperarousal.
These symptoms can cause significant problems in your work or relationships. T alk to your doctor or a mental health professional if you've had or witnessed a traumatic event and have disturbing thoughts and feelings about it for more than a month, if your thoughts and feelings are severe, or if you feel like you're having trouble getting your life back on track.
What Are the Consequences of Long-Term Stress?
Ongoing, chronic stress can trigger or worsen many serious health problems, including:
- Mental health problems, such as depression, anxiety, and personality disorders
- Cardiovascular disease, including heart disease , high blood pressure, abnormal heart rhythms, heart attacks, and strokes
- Obesity and other eating disorders
- Menstrual problems
- Sexual dysfunction, such as impotence and premature ejaculation in men and loss of sexual desire in men and women
- Skin and hair problems , such as acne, psoriasis, and eczema, and permanent hair loss
- Gastrointestinal problems, such as GERD, gastritis , ulcerative colitis, and irritable bowel syndrome
Help Is Available for Stress
Stress is a part of life. What matters most is how you handle it. The best thing you can do to prevent stress overload and the health consequences that come with it is to know your stress symptoms.
If you or a loved one is feeling overwhelmed by stress, talk to your doctor. Many symptoms of stress can also be signs of other health problems. Your doctor can evaluate your symptoms and rule out other conditions. If stress is to blame, your doctor can recommend a therapist or counselor to help you better handle your stress.
Stress Takeaways
Stress is your body's response to a challenging or demanding situation. It can affect you physically, mentally, and behaviorally, especially when you have chronic stress. Chronic stress is when you are stressed for an extended time. Chronic stress can make it more likely for you to develop other mental health disorders, such as anxiety or depression. It can also affect your heart health and digestive health. If you're stressed and having trouble coping, it may be time for you to see your doctor or a mental health professional.
Stress FAQs
What can extreme stress cause?
Extreme stress, especially if it's prolonged, can cause emotional distress. And stress from a traumatic event, which is usually extreme, can cause posttraumatic stress disorder (PTSD). These are more serious cases of stress that overwhelm your ability to manage on your own. You may need to get a professional's help to get back on track. If you feel like you're having trouble managing your emotions, talk to your doctor. They can help you or direct you to someone who can help you.
Can stress make you throw up?
Yes, stress can make you throw up. Your digestive system is one of the many systems that stress can affect. In fact, you may have a whole range of other digestive symptoms, such as nausea, pain, and constipation or diarrhea. Not everyone has stress nausea or vomiting, but you may be more prone to it if you have a gastrointestinal condition, such as irritable bowel syndrome (IBS), or you have anxiety or depression.
You may be able to tell if you're stress vomiting if your episode passes when the stress goes away. If it doesn't, then your episode may be caused by something else. It's time to get checked out by your doctor if you have more than a couple of episodes or you can't figure out what's causing them.
Show Sources
Chu, B. Physiology, Stress Reaction , StatPearls Publishing, 2024.
American Psychological Association: "Stress effects on the body."
MedlinePlus: "Stress."
Mayo Clinic: "Stress management," "Emotional exhaustion: When your feelings feel overwhelming," "Post-traumatic stress disorder (PTSD)."
Cleveland Clinic: "Emotional Stress: Warning Signs, Management, When to Get Help," "Stress Nausea: Why It Happens and How To Deal. "
Johns Hopkins Medicine: "Signs of Respiratory Distress."
Helpguide.org: "Stress Symptoms, Signs, and Causes," "Understanding Stress."
Yale Medicine: "Chronic Stress."
Department of Health and Human Services: "Stress and Your Health."
American Institute of Stress: "Effects of Stress."

How to Feel Better in Less Than 15 Minutes
Need a quick pick-me-up? These simple steps can get you moving and boost your mood - fast!

Heart-Pounding, Stomach-Knotting: Stress and You
From knots in your stomach to headaches, heartburn and chronic health conditions, stress can lead to a variety of health issues.

Ways to Practice Self-Care
Self-care doesn't have to cost a lot. These simple steps can boost your mood and get you moving.

Natural Remedies to Alleviate Anxiety
These natural remedies can help ease your anxiety. Learn how they work - and when to see a doctor.

Is My Stress Level Too High?
From pain to digestive problems and more, the signs and symptoms of too much stress are easy to spot - once you know what to look for.
Wait, what does 'price gouging' mean? How Harris plans to control it in the grocery aisle

Democratic presidential nominee Kamala Harris is expected to announce plans to fight food inflation with a federal ban on price gouging on groceries , but how much this would help Americans is debatable, economists say.
Over the past few years, President Joe Biden’s administration has blamed corporate greed for the surge in inflation, and Harris is expected to take up that torch in a speech Friday in North Carolina's capital city of Raleigh. Corporations raised prices when snarled supply chains during the pandemic created shortages of nearly everything, and just never stopped or lowered prices again after supply chains stabilized, they argue.
“Some companies are keeping prices high even though input costs are falling, and supply chains are back to normal,” the White House said in a news release in March.
If higher grocery prices are the result of potential mergers between larger supermarkets and food producers and corporate greed, Americans may benefit from Harris' approach. However, many economists have doubts such a policy would be effective for various reasons, including whether price gouging is the root of inflation at all.
Michael Ashton, managing principal at Enduring Investments LLC, who specializes in inflation analysis, questioned the existence of price gouging "in an industry as competitive as grocery."
“Why did the price gouging just start in 2021-22?" he asked. "Did grocers just not realize they had this power before then or did they not get greedy until 2021?”
Profit margins in the food industry already tend to be among the lowest. Net profit margin in 2023 in the grocery industry hit 1.6%, the lowest level since 2019, according to FMI, The Food Industry Association.
What caused food prices to spike?
During the pandemic, economists generally agreed supply chain shortages initially caused price increases.
After supply chains were ironed out, the dispute began. Researchers from the Federal Reserve Bank of Kansas City and former Federal Reserve Chairman Ben Bernanke separately said last year that fast-rising wages when the economy reopened was a major contributor to rising grocery prices.
However, left-leaning government watchdog Accountable.US and former Labor Secretary Robert Reich say companies have been raising prices on Americans to reward stockholders with dividends and stock buybacks.
“Consumers are getting shafted, as corporations tell Wall Street they expect to be able to keep their prices and profits in the stratosphere,” Reich wrote in June .
The Groundwork Collaborative, a nonprofit that earlier this year said "climate change, corporate consolidation, and profiteering" are reasons grocery prices remain high, even quantified in January how much corporate greed contributed to inflation. In the middle of 2023, corporate profit margins accounted for roughly half of inflation and more than a third since the pandemic began, it estimated.
“The industry keeps pushing the envelope to pad profits and bring in enough money for shareholder giveaways, but Americans are fed up,” said Liz Zelnick, director of the economic security & corporate power program at Accountable.US, in a news release.
Inflation's down but prices are high?: Prices don't drop when inflation eases. Why your wallet will be hurting for a while.
Could Harris’ plan work to lower food prices?
Opinions are mixed.
Reich, who sees corporate greed as the root of soaring inflation, advocated for a policy like what Harris is expected to announce.
“Put blame for high prices squarely where it belongs: on big corporations with monopoly power to keep prices high,” he wrote. “And take those corporations on: Condemn them for price gouging. Threaten them with antitrust lawsuits, price-gouging lawsuits, even price controls. Criticize them for making huge profits and giving their top executives record pay while shafting consumers.”
Others, like Sen. Rick Scott , R-Fla . , call the plan “federal price controls,” which he says don’t work.
Harris’ solution to fighting inflation “is big government on steroids – where Washington bureaucrats stick their hands into American businesses and say what they can and can’t sell a product for,” he said in a news release on Thursday. “It never works because it causes companies to make much less of something – destroying supply and causing a mass shortage of goods.”
Such a policy could also be difficult to implement because calculating an appropriate profit margin might be tricky, said James Knightley, Dutch bank ING’s chief international economist.
“It’s critical that we get the economic facts right and avoid political rhetoric," said Sarah Gallo, senior vice president of product policy and federal affairs at the Consumer Brands Association trade group. "The reality is that there are complex economic factors at play."
Is food inflation still even a thing?
Three in 5 Americans said corporate greed was a “major cause” of inflation, according to a poll by left-leaning polling and research group Navigator Research of 1,000 registered voters. However, that was in January when annual inflation was running at a 3.1% pace . Since then, inflation has eased further.
"When looking at the inflation story, it's good now but the perception among consumers is different because prices are still elevated," Knightley said. "We're not returning to 2019 prices," which is what consumers are comparing to.
Since inflation only measures the pace at which prices are changing, actual sticker prices remain high from climbing over the past couple of years. Inflation in the 12 months through July was 2.9%, sharply down from its 40-year high of 9.1% in June 2022 and the lowest since March 2021. Overall, annual food inflation rose a smaller 2.2%, with grocery prices rising at an even slower 1.1% pace.
“Why intervene?” Knightley said. “From an economics perspective, it’s looking like a pretty good place right now. This may be good messaging for the election, but it (inflation) may be falling by the wayside.”
Medora Lee is a money, markets, and personal finance reporter at USA TODAY. You can reach her at [email protected] and subscribe to our free Daily Money newsletter for personal finance tips and business news every Monday through Friday morning.
- Search the site GO Please fill out this field.
- Newsletters
- Health Conditions A-Z
- Endocrine Diseases
What Is a Buffalo Hump (Dorsocervical Fat Pad)—and Why Does It Happen?
:max_bytes(150000):strip_icc():format(webp)/JoyEmehsheadshot1-JoyEmeh-ef67f56eb29e4a81a9f66d80745aea82.jpg)
- Complications
A buffalo hump (medically known as a dorsocervical fat pad) occurs when you develop a buildup of fat in between the shoulder blades at the back of the neck. The excess fat can form a fatty tissue protrusion that mimics the appearance of a hump.
A buffalo hump on its own is not harmful, and having it does not ultimately mean you have a medical condition. Sometimes, even having poor posture can cause it. However, certain conditions like Cushing's syndrome, adrenal cancer, osteoporosis, and obesity can raise your risk of developing one.
Motortion / Getty Images
Buffalo Hump Symptoms
The hallmark characteristic of a buffalo hump is a fatty lump behind the neck, in between the back of the shoulders. In most cases, this is actually the only symptom. However, conditions like Cushing's syndrome , adrenal cancer, obesity, or osteoporosis is causing the hump, can cause additional symptoms such as:
- A round or moon face
- Unintentional weight gain
- Thin arms and legs
- Muscle weakness
- Easy bruising
- Purple stretch marks , particularly on the breasts, abdomen, and hips
Several underlying conditions can cause a buffalo hump. The following are the most common reasons:
- Poor posture: Leaning forward, keeping your head down (such as while looking at your phone), and not walking with your shoulders pushed back can weaken the muscles in your neck and upper back and cause a hump to develop.
- Cushing's syndrome: This condition causes the overproduction of cortisol , a hormone that plays an important role in how the body responds to stress. The overproduction of this hormone sometimes triggers fat accumulation in the back of the neck.
- Adrenal cancer : The adrenal gland is the gland responsible for secreting cortisol. A cancerous tumor growing in this gland can cause it to overproduce cortisol, leading to the development of a buffalo hump.
- Antiretroviral medications: Certain HIV medications , such as protease inhibitors, can cause side effects like a buffalo hump.
- Glucocorticoids: Long-term use of glucocorticoid medications like Rayos (prednisone) and Hydrocort (hydrocortisone) can cause a buffalo hump, as these medications act like cortisol and therefore induce similar effects as high cortisol levels .
- Obesity : People who live with obesity have a higher risk of developing a buffalo hump due to excess fat deposits in the neck region.
- Lipodystrophy : This refers to a group of medical conditions characterized by abnormal fat distribution in the body. People with this condition often lack fat tissue in all or some parts of the body but have excess fat accumulation in other body parts.
- Madelung disease (multiple symmetrical lipomatosis): This condition is a rare metabolic disorder that causes an unusual build-up of fat deposits in body parts like the trunk, neck, shoulders, thighs, and upper arms. It is often associated with excessive alcohol use.
Healthcare providers can diagnose a buffalo hump by physically or visually examining you. However, they may need to run further tests to determine the underlying cause of the hump. This may include taking your medical and family history and ordering exams that check cortisol level, bone density, and strength, such as:
- Imaging tests like magnetic resonance imaging (MRI) scans, computed tomography (C)T scans , and X-rays
- Blood tests
- Urine tests
- Bone density tests
Because certain medications can also raise the risk of developing a buffalo hump, you can expect your healthcare provider to ask you about your medication use and other lifestyle habits.
How To Get Rid of a Buffalo Hump
There’s no one-size-fits-all treatment for a buffalo hump. Your healthcare team's approach to resolving a hump will often depend on the cause of your symptoms. Your exact treatment plan may also combine multiple treatment options together to see results. Treatment approaches to help reduce the appearance of a buffalo hump include the following:
- Use a posture corrector and sitting or walking straight to fix posture
- Focus on nutritious foods to help your body lose weight if needed
- Start an exercise regimen to manage obesity
- Stop or adjust the dosage of any medications that may be causing your hump
- Get cosmetic surgery to remove the excess fat deposit on the neck
- Remove tumors from the back of the neck or the adrenal gland, which may cause high cortisol levels
- Manage stress to reduce high cortisol levels, which can influence a buffalo hump to develop
There is no surefire way to prevent a buffalo hump, but incorporating the following strategies may reduce your risk of developing one:
- Exercise regularly to maintain strong bones
- Eat a nutritious diet, focusing on plant foods like fruits and vegetables, lean proteins, and whole grains
- Limit the use of glucocorticoid medications
Complications
A buffalo hump itself doesn't typically pose a danger to your health. However, in some people, the fat accumulation can be so excessive that it restricts neck or upper back movement. This can affect your ability to move, complete daily tasks, and feel more self-conscious about your body image.
However, if the underlying medical causes of a buffalo hump, like Madelung disease and Cushing's syndrome, are not treated in a timely manner, they may lead to complications like hypertension (high blood pressure), depression, sleep apnea (a chronic breathing disorder that causes your breathing to stop and restart repeatedly while you sleep), and difficulty swallowing or speaking.
That said, if you develop a buffalo hump, seeing a healthcare provider about the hump is important, as they can offer treatment options to help reduce the appearance and treat underlying conditions.
Living With a Buffalo Hump
The development of buffalo hump is often not within your control, and it can be challenging to live with this fat accumulation behind your neck, as it can limit mobility. It is best to speak to a healthcare provider as soon as you notice the hump, especially to learn if an underlying health condition is causing your symptoms. They can provide an accurate diagnosis and offer timely treatment options.
Some people who develop a buffalo hump can also sometimes experience changes in their self-perception, body image, and emotional well-being. However you feel is normal and valid—and it's also okay to reach out to a mental healthcare provider if you need support. Online support groups for conditions like Cushing's syndrome can also help you feel cared for and understood by other people living with the condition.
Frequently Asked Questions
The difference between buffalo hump and dowager’s hump lies in their causes. A buffalo hump is caused by excess fat deposition at the back of the neck, while a dowager’s hump (also called hunchback) is caused by excessive forward curvature of the thoracic spine, often due to poor posture or osteoporosis.
Since a buffalo hump can be caused by obesity, reaching a weight that is right for you and your body can reduce the accumulation of fat behind your neck and help the appearance of the hump go away.
Massage alone may not be enough to get rid of a buffalo hump, but it may be helpful if factors like poor body posture and curvature of the spine in the neck area are contributing to the protrusion of your buffalo hump. One study found that direct massage or stretching of fatty regions may decrease the volume of fat tissue, thereby reducing the appearance of fat deposits.
:max_bytes(150000):strip_icc():format(webp)/sr-a21a100afbf343f481150ff49b3a733e.jpeg)
Yuan Y, Gao J, Ogawa R. Mechanobiology and Mechanotherapy of Adipose Tissue-Effect of Mechanical Force on Fat Tissue Engineering . Plast Reconstr Surg Glob Open . 2016;3(12):e578. doi:10.1097/GOX.0000000000000564
Hoenig LJ. The Buffalo Hump of Cushing Syndrome . Clin Dermatol . 2022;40(5):617-618. doi:10.1016/j.clindermatol.2021.08.018
MedlinePlus. Hump on upper back (dorsocervical fat pad) .
National Institute of Diabetes and Digestive and Kidney Diseases. Cushing’s Syndrome .
Elsevier. Buffalo hump .
American Cancer Society. Signs and Symptoms of Adrenal Cancers .
MedlinePlus. Exogenous Cushing syndrome .
Centers for Disease Control and Prevention. Defining Adult Overweight & Obesity .
Quinn K, Chauhan S, Purcell SM. Lipodystrophies . In: StatPearls. StatPearls Publishing; 2024.
Rauso R, Rusciani A, Curinga G. An adipocitolitic aqueous micro-gelatinous solution for buffalo hump deformity reduction . J Drugs Dermatol . 2014;13(10):1282-1284.
National Organization for Rare Diseases. Madelung’s disease .
Chen S, Gui X en, Cao Q, Routy JP. Clinical outcome after lipectomy in the management of patients with human immunodeficiency virus-associated dorsocervical fat accumulation: An observational cohort study. Medicine . 2019;98(25):e16112. doi:10.1097/MD.0000000000016112
Chau C, Chu EC, Huang KH, Tam D, Cheung G. Remission of Dowager's hump by manipulative correction of spinal alignment: a case report . J Med Life . 2023;16(6):957-962. doi:10.25122/jml-2023-0026
Related Articles
Supermarkets are being infiltrated with ‘designer honey’ that can cause diabetes, obesity and liver damage

Lynne Ingram cuts a peaceful figure as she tends to a row of humming beehives in a leafy corner of Somerset, southwest England.
But the master beekeeper, who has been keeping hives for more than 40 years, has found herself in a fight against a tricky and evolving foe — honey fraudsters.
The practice of adulterating honey is well known, and historically adulterants such as ash and potato flour have been used.
Now, advancements in technology and science have made it much easier, with “bespoke, designer or bioengineered” syrups used as diluting agents capable of fooling authenticity tests, Ingram said.
She founded the UK Honey Authenticity Network (HAN UK) in 2021 to raise awareness about natural honey and warn of the threat posed by fraud.
“One of the impacts we’re seeing all over the world is beekeepers going out of business,” she said.
Adulterated honey can be sold to retailers for a price several times lower than genuine producers can afford.
As well as producing their own honey, many larger-scale beekeepers have crop pollination contracts with farmers, delivering thousands of colonies to growers across the country.
If they go out of business due to unfair competition, this vital natural method of pollinating crops is reduced and food production suffers.
The British Beekeepers Association, which represents more than 25,000 producers and where Ingram is a honey ambassador, wants the risk of fraud to be recognised to protect the industry and consumers.
“I’d like to see an acknowledgement that there is actually an issue here,” she said.
Better labelling
In May, the European Union updated its honey regulations to ensure clearer product labelling and a “honey traceability system” to increase transparency.
On the labelling for blended honeys, for example, all countries of origin are now required to appear near a product’s name, where previously it was only mandatory to state whether blending had occurred.
Labelling in the UK, which has now left the EU, is not as stringent and Ingram believes consumers are “being misled” by vague packaging.
Behind the EU action is an apparent increase in adulterated honey arriving in the 27-nation bloc.
The substandard adulterates can have adverse effects on consumers’ health, such as raising the risk of diabetes, obesity, and liver or kidney damage.
Between 2021 and 2022, 46 percent of the honey tested as it entered the EU was flagged as potentially fraudulent, up from 14 percent in the 2015-17 period.
Of the suspicious consignments, 74 percent were of Chinese origin.
Honey imported from the UK had a 100-percent suspicion rate.
The EU said this honey was probably produced in third countries and blended again in the UK before being sent to the bloc.
The UK is the second largest importer of honey in terms of volume in the whole of Europe. China is its top supplier.
Not all of the UK’s imported honey leaves the country, however. Considerable quantities stay on the domestic market.
“We think there’s an awful lot of it on the shelves,” said Ingram, adding that adulterated honey was “widely available” in big supermarkets.
Behind the closed blinds of a research laboratory at Aston University in Birmingham, central England, researchers fighting honey fraud are harnessing cutting-edge technology.
Aston scientists and beekeepers, including Ingram, are using light to reveal the contents of honey samples at the molecular level.
The technique — known as Fluorescence Excitation-Emission Spectroscopy (FLE) — involves firing lasers into samples.
The light frequencies re-emitted are then collated into a three-dimensional image — or “molecular fingerprint” — of the honey tested.
Alex Rozhin, the project lead and a reader in nanotechnology, said the test “can trace different molecules through the spectrum and confirm which type of biochemicals are present”.
In the darkened lab, the light from different honeys is clearly visible.
The first gives off a vivid green and the second a cooler blue, indicating distinct chemical compositions.
Using FLE, Rozhin says his team “can immediately trace a concentration of fraud inside samples” with “different spectral bands corresponding to syrup (or) to natural honey”.
Rozhin said FLE is more accurate than existing tests and can provide results far quicker, at a greatly reduced cost and without the need for highly trained personnel.
One of the Aston team’s aims is to create a version of FLE that can be used by honey producers or even consumers with scaled-down equipment or eventually just a smartphone.
Rolling the test out like this would also accelerate the creation of a honey database which, through machine learning, could be used as a catalogue of biometric signatures.
“If we get a new sample and it’s been tampered with and it’s different from how the database is built up, we’ll know there’s something obscure,” said Steven Daniels, an Aston research associate specialising in machine learning.
Ingram said the test could close international gaps in testing methods by establishing a unified standard, but the government needed to monitor the sector too.
“We really need to get to grips with this,” she said.
Latest in Health

Eating dinner at 5 p.m. can improve your life and boost your health. How to make it work for you

Got late-summer travel plans? Here’s where COVID cases are spiking in the U.S.

Are you ‘addicted’ to your phone? How to spot the signs—and what to do about it

High cortisol is wreaking havoc on your health. 4 simple steps can lower your levels

Mpox: Here’s what we know about the virus, and what might be done to contain it

Sweden reports 1st case of more infectious form of mpox first identified in Congo
Most popular.

Gen Z are ‘raw dogging’ flights for TikTok—but experts say it can cause thrombosis

Bill Gates ‘terrified’ employees at his foundation, book claims, where meetings felt like a king holding court

More young men are becoming NEETs than women—not in employment, education, or training

Elon Musk’s financial woes at X have Tesla bulls fearing he will liquidate more stock

Jerome Powell met Jamie Dimon and other bank CEOs behind closed doors to avoid legal fight

‘Black Swan’ hedge funder warns a recession is coming this year—and the biggest market bubble in history will soon pop
Advertisement
Supported by
Many People Are Eligible for Paxlovid. Who Should Take It?
The treatment can help prevent mild or moderate cases of Covid-19 from becoming more severe. Here’s what to know.
- Share full article

By Dani Blum
Most adults in the United States have one condition or another that makes them a candidate for Paxlovid, which can cut the risk of a severe case of Covid. Obesity, diabetes, depression, heart conditions and dozens of other issues all put people at high risk, according to the Centers for Disease Control and Prevention.
And yet Dr. Davey Smith, an infectious disease specialist at the University of California, San Diego, regularly gets calls from patients who were not able to get prescriptions, often because urgent care or primary care doctors denied their requests. More than two years after Paxlovid became widely available in the United States, and in the middle of yet another summer surge , patients and doctors are still frequently confused about who qualifies for the medication and exactly how beneficial it might be.
It’s well-established that Paxlovid saves lives. But it can be costly, and it can interact with a lengthy list of medications. Some people avoid the drug, in part because they worry about experiencing a rebound case. One study found that only about 15 percent of people who were eligible for the medication took it when they had Covid.
“In my experience, it’s usually that the provider doesn’t have enough experience with it or enough time to want to go through somebody’s medication list,” Dr. Smith said. “So they just get told, ‘Oh, you’re going to be fine.’ And most of the time, they are fine. It’s just when they’re not, it can be really bad.”
Who should take Paxlovid?
Paxlovid is designed to prevent Covid from progressing into more severe disease. It is for people who have mild or moderate symptoms but are at risk of getting very sick. (Doctors can prescribe the drug to adults and children 12 and older who weigh over 88 pounds.)
The greater your risk for hospitalization or death from Covid, the stronger your case for taking Paxlovid.
We are having trouble retrieving the article content.
Please enable JavaScript in your browser settings.
Thank you for your patience while we verify access. If you are in Reader mode please exit and log into your Times account, or subscribe for all of The Times.
Thank you for your patience while we verify access.
Already a subscriber? Log in .
Want all of The Times? Subscribe .

IMAGES
COMMENTS
Essay on obesity! Find high quality essays on 'Obesity' especially written for school, college, science and medical students. These essays will also guide you to learn about the causes, factors, treatment, management and complications related to obesity. Obesity is a chronic health condition in which the body fat reaches abnormal level.
Moreover, obesity causes diabetes, especially among adults as the body may become resistant to insulin. This resistance may lead to a high level of blood sugar, which is fatal. Besides health complications, obesity causes an array of psychological effects, including inferiority complex among victims. Obese people suffer from depression ...
In summary, papers in this issue review our current knowledge on the causes, consequences, and interventions of obesity and its associated diseases such as type 2 diabetes, NAFLD, and cardiovascular disease (Cheong and Xu, 2021; Gao et al., 2021; Love et al., 2021).
In the United States, overweight and obesity are chronic diseases that contribute to excess morbidity and mortality. Despite public health efforts, these disorders are on the rise, and their consequences are burgeoning. 1 The Centers for Disease Control and Prevention report that during 2017 to 2018, the prevalence of obesity in the United States was 42.4%, which was increased from the ...
Obesity is a growing concern in many parts of the world, with rates on the rise. According to the World Health Organization (WHO), obesity has more than doubled globally since 1980. This essay will examine the causes of obesity, including dietary habits, sedentary lifestyles, and genetic factors, and explore the significant effects it has on individuals and society as a whole.
This essay will explore the various causes of obesity and their effects on individuals and society as a whole. One of the primary causes of obesity is dietary habits and nutritional intake. The consumption of high-calorie, low-nutrient foods, such as fast food, sugary beverages, and processed snacks, has become increasingly prevalent in modern ...
carbohydrate is a crucial factor in the obesity epidemic. 18 Soft drinks, alcoholic beverages and fast food tend to be calorie rich. In Britain, there has been a signi cant rise in the amount of ...
However, there are other broader social and economic causes of obesity, such as marketing, climate, taxes, and the ability to purchase healthy food. It is important to consider the state as a whole, to investigate how much means of physical activity are available to different social groups and ages.
In your obesity essay, you might want to discuss its causes and effects or explore the issue of childhood obesity. If you're planning to work on a quantitative nursing project, a good option is to make a case study. Here we've gathered top obesity topics for presentations & research papers. Obesity essay examples as an inspiring bonus!
If you are writing a cause-and-effect obesity essay, you can mention different causes of obesity and how it can affect a person's overall health. The number of body paragraphs can increase depending on the parameters of the assignment as set forth by your instructor. Start each body paragraph with a topic sentence that is the crux of its content.
Obesity prevalence has increased in pandemic dimensions over the past 50 years. Obesity is a disease that can cause premature disability and death by increasing the risk of cardiometabolic ...
Introduction. Obesity is an increasing, global public health issue. Patients with obesity are at major risk for developing a range of comorbid conditions, including cardiovascular disease (CVD), gastrointestinal disorders, type 2 diabetes (T2D), joint and muscular disorders, respiratory problems, and psychological issues, which may significantly affect their daily lives as well as increasing ...
The main cause of obesity is junk food and an unbalanced diet rich in simple carbohydrates, fats, and sugars, plus a bunch of additives. Manufactured, processed, refined, and packaged meals are the most popular. Thanks to advances in technology, Americans have come to mass-produce meals that keep fresh longer and taste better.
The Most Common Causes of Obesity. Obesity is when our bodies store more than the acceptable amounts of fats that might have a powerful effect on our health. Therefore, People become obese for many reasons. moreover, the most trending habits that cause obesity are indiscretion nutrition, and sedentary lifestyle, stop exercising.
Defining obesity. Obesity was traditionally defined as an increase in body weight that was greater than 20 percent of an individual's ideal body weight—the weight associated with the lowest risk of death, as determined by certain factors, such as age, height, and gender. Based on these factors, overweight could then be defined as a 15-20 ...
Some genetic and lifestyle factors affect an individual's likelihood of adult obesity; thus, the significant clusters of obesity observed in specific geographical regions and contexts also signal the impact of socioeconomic and environmental factors in "obesogenic" environments [13].Understanding the causes and determinants of obesity is a critical step toward creating effective policy and ...
The prevalence of obesity has tripled over the past four decades, imposing an enormous burden on people's health. Polygenic (or common) obesity and rare, severe, early-onset monogenic obesity ...
These can include heart disease, diabetes, high blood pressure, high cholesterol, liver disease, sleep apnea and certain cancers. There are many reasons why some people have trouble losing weight. Often, obesity results from inherited, physiological and environmental factors, combined with diet, physical activity and exercise choices.
With the five leading causes of death - heart disease, cancer, chronic lower respiratory disease, cerebrovascular diseases such as stroke, and unintentional injuries - obesity is a major risk factor for the first four. [20] Obesity is also associated with other health conditions such as sleep apnea, fatty liver disease, gallstones ...
Obesity Essay: Obesity is a condition that occurs when a person puts on excess body fat. It is a sudden and unusual increase in body fat. It can lead to heart-related diseases, blood pressure, hypertension, cholesterol, and various other health issues. The main cause of obesity is over-eating. Consuming junk food and staying away for physical ...
16 Drawing possible lessons for obesity prevention and control from the tobacco-control experience Notes. Notes. 17 The ... Debates about whether it is our eating or activity that is more important as a cause of obesity, or whether preventing obesity is a personal or societal responsibility are unhelpful, and can only serve to distract us from ...
Obesity is a complex disease triggered by interlinking causes, from genetics to dysfunctional food systems, to social deprivation. The drivers of stigma are primarily based around a misunderstanding of the complex causes of obesity. People who live with obesity find it stressful and demoralising. Efforts to lose weight are frequently ...
The #1 cause of obesity is eating too much and moving too little, say experts about the epidemic plaguing America. Newsful. The Major Causes of Obesity, According to Science. Story by Leah Groth ...
Obesity and other eating disorders Menstrual problems Sexual dysfunction, such as impotence and premature ejaculation in men and loss of sexual desire in men and women
Three in 5 Americans said corporate greed was a "major cause" of inflation, according to a poll by left-leaning polling and research group Navigator Research of 1,000 registered voters.
However, conditions like Cushing's syndrome, adrenal cancer, obesity, or osteoporosis is causing the hump, can cause additional symptoms such as: A round or moon face
Supermarkets are being infiltrated with 'designer honey' that can cause diabetes, obesity and liver damage BY Daniel Matthews and AFP Some 46% of honey tested as it enters the EU is flagged as ...
People who are 65 or older, are immunocompromised or have chronic conditions like cancer, diabetes and obesity are considered among those at highest risk, and should consider the medication even ...