An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager

Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Rectal cancer
Affiliation.
- 1 Robert H. Lurie Comprehensive Cancer Center of Northwestern University, USA.
- PMID: 23221790
- DOI: 10.6004/jnccn.2012.0158
These NCCN Clinical Practice Guidelines in Oncology provide recommendations for the management of rectal cancer, beginning with the clinical presentation of the patient to the primary care physician or gastroenterologist through diagnosis, pathologic staging, neoadjuvant treatment, surgical management, adjuvant treatment, surveillance, management of recurrent and metastatic disease, and survivorship. This discussion focuses on localized disease. The NCCN Rectal Cancer Panel believes that a multidisciplinary approach, including representation from gastroenterology, medical oncology, surgical oncology, radiation oncology, and radiology, is necessary for treating patients with rectal cancer.
PubMed Disclaimer
Similar articles
- Rectal Cancer, Version 2.2015. Benson AB 3rd, Venook AP, Bekaii-Saab T, Chan E, Chen YJ, Cooper HS, Engstrom PF, Enzinger PC, Fenton MJ, Fuchs CS, Grem JL, Grothey A, Hochster HS, Hunt S, Kamel A, Kirilcuk N, Leong LA, Lin E, Messersmith WA, Mulcahy MF, Murphy JD, Nurkin S, Rohren E, Ryan DP, Saltz L, Sharma S, Shibata D, Skibber JM, Sofocleous CT, Stoffel EM, Stotsky-Himelfarb E, Willett CG, Gregory KM, Freedman-Cass D. Benson AB 3rd, et al. J Natl Compr Canc Netw. 2015 Jun;13(6):719-28; quiz 728. doi: 10.6004/jnccn.2015.0087. J Natl Compr Canc Netw. 2015. PMID: 26085388
- Localized colon cancer, version 3.2013: featured updates to the NCCN Guidelines. Benson AB 3rd, Bekaii-Saab T, Chan E, Chen YJ, Choti MA, Cooper HS, Engstrom PF, Enzinger PC, Fakih MG, Fenton MJ, Fuchs CS, Grem JL, Hunt S, Kamel A, Leong LA, Lin E, May KS, Mulcahy MF, Murphy K, Rohren E, Ryan DP, Saltz L, Sharma S, Shibata D, Skibber JM, Small W Jr, Sofocleous CT, Venook AP, Willett CG, Gregory KM, Freedman-Cass DA; National Comprehensive Cancer Network. Benson AB 3rd, et al. J Natl Compr Canc Netw. 2013 May 1;11(5):519-28. doi: 10.6004/jnccn.2013.0069. J Natl Compr Canc Netw. 2013. PMID: 23667203
- [Multidisciplinary management of rectal cancer]. De Bari B, Bosset JF, Gérard JP, Maingon P, Valentini V. De Bari B, et al. Cancer Radiother. 2012 Dec;16(8):711-20. doi: 10.1016/j.canrad.2012.10.007. Epub 2012 Nov 20. Cancer Radiother. 2012. PMID: 23182080 French.
- [Neoadjuvant radiochemotherapy for rectal cancer]. Zehentmayr F, Wolf M, Weissenborn Y, Feldmann HJ, Belka C. Zehentmayr F, et al. MMW Fortschr Med. 2011 Sep 1;153(35):31-3. MMW Fortschr Med. 2011. PMID: 21916302 German. No abstract available.
- Progress in the multidisciplinary treatment of gastrointestinal cancer and the impact on clinical practice: perioperative management of rectal cancer. Cervantes A, Roselló S, Rodríguez-Braun E, Navarro S, Campos S, Hernández A, García-Granero E. Cervantes A, et al. Ann Oncol. 2008 Sep;19 Suppl 7:vii266-72. doi: 10.1093/annonc/mdn438. Ann Oncol. 2008. PMID: 18790964 Review. No abstract available.
- Influence of High-Risk Pathological Factors and their Interaction on the Survival Benefit of Adjuvant Chemotherapy in Stage II Rectal Cancer: A Retrospective Study. Zhao K, Li H, Pang W, Zhao X, Zhang B, Fen Z, Jin L, Xue J, Chu T, Yan S, Wang W, Han Q, Yao Y, Zhang X, Su X, Zhang C. Zhao K, et al. J Cancer. 2024 May 5;15(11):3531-3538. doi: 10.7150/jca.95769. eCollection 2024. J Cancer. 2024. PMID: 38817859 Free PMC article.
- Acetone compression improves lymph node yield and metastasis detection in colorectal cancer. Schnoz C, Schmid K, Ortega Sanchez G, Schacher-Kaufmann S, Adamina M, Peros G, Erdin D, Bode PK. Schnoz C, et al. Clin Exp Metastasis. 2024 Feb;41(1):45-53. doi: 10.1007/s10585-023-10259-x. Epub 2024 Jan 4. Clin Exp Metastasis. 2024. PMID: 38177714 Free PMC article.
- Lymph Node Metastases and Associated Recurrence-Free Survival in Microsatellite Stable and Unstable Colon Cancer. Hakki L, Khan A, Gonen M, Stadler Z, Segal NH, Shia J, Widmar M, Wei IH, Smith JJ, Pappou EP, Nash GM, Paty PB, Garcia-Aguilar J, Weiser MR. Hakki L, et al. Ann Surg Oncol. 2023 Dec;30(13):8487-8494. doi: 10.1245/s10434-023-14270-0. Epub 2023 Sep 12. Ann Surg Oncol. 2023. PMID: 37700171
- Rectal cancer-derived exosomes activate the nuclear factor kappa B pathway and lung fibroblasts by delivering integrin beta-1. Gao Q, An K, Gao Z, Wang Y, Ding C, Niu P, Lei F. Gao Q, et al. Korean J Physiol Pharmacol. 2023 Jul 1;27(4):375-381. doi: 10.4196/kjpp.2023.27.4.375. Korean J Physiol Pharmacol. 2023. PMID: 37386835 Free PMC article.
- Comparison of flexible endoscopy and magnetic resonance imaging in determining the tumor height in rectal cancer. Basendowah MH, Ezzat MA, Khayyat AH, Alamri ESA, Madani TA, Alzahrani AH, Bokhary RY, Badeeb AO, Hijazi HA. Basendowah MH, et al. Cancer Rep (Hoboken). 2023 Feb;6(2):e1705. doi: 10.1002/cnr2.1705. Epub 2022 Aug 17. Cancer Rep (Hoboken). 2023. PMID: 36806725 Free PMC article.
- Search in MeSH
Related information
Linkout - more resources, full text sources.
- Sheridan PubFactory
- Genetic Alliance

- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
Locally Advanced Rectal Cancer
Mini Review 08 October 2020 Modern MR Imaging Technology in Rectal Cancer; There Is More Than Meets the Eye Hester E. Haak , 2 more and Regina G. H. Beets-Tan 4,049 views 7 citations
Loading... Review 18 August 2020 Selection and Outcomes in Abdominoperineal Resection Norbert Garcia-Henriquez , 1 more and John R. T. Monson 8,285 views 20 citations
Review 14 August 2020 Delivery of Personalized Care for Locally Advanced Rectal Cancer: Incorporating Pathological, Molecular Genetic, and Immunological Biomarkers Into the Multimodal Paradigm Éanna J. Ryan , 1 more and Kieran Sheahan 4,234 views 16 citations
Review 31 July 2020 Laparoscopic Approach to Rectal Cancer—The New Standard? Christine Hsieh and Kyle G. Cologne 5,420 views 12 citations
Mini Review 29 April 2020 Quality Assurance, Metrics, and Improving Standards in Rectal Cancer Surgery in the United States Zhaomin Xu and Fergal J. Fleming 2,355 views 13 citations
Loading... Review 05 March 2020 Ultimate Functional Preservation With Intersphincteric Resection for Rectal Cancer Maxime Collard and Jérémie H. Lefevre 13,637 views 22 citations
Loading... Mini Review 17 January 2020 Controversies in the Management of Lateral Pelvic Lymph Nodes in Patients With Advanced Rectal Cancer: East or West? Jaime Otero de Pablos and Julio Mayol 14,755 views 31 citations
Original Research 03 December 2019 Lateral Lymph Node Metastases in Locally Advanced Low Rectal Cancers May Not Be Treated Effectively With Neoadjuvant (Chemo)Radiotherapy Only Anouck Haanappel , 11 more and Tarik Sammour 3,757 views 13 citations
Advances in Colorectal Cancer Research
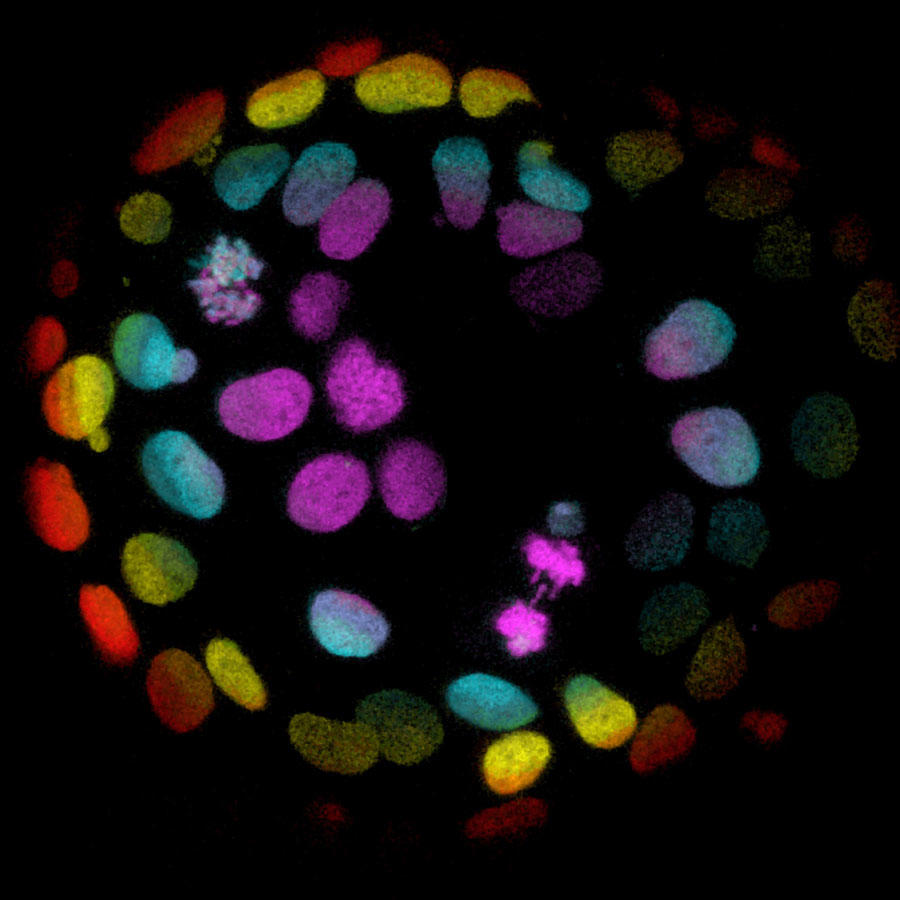
Colorectal cells grown into organoids, stem cell-derived human 'mini-organs' that are used to study human development and disease.
NCI-funded researchers are working to advance our understanding of how to prevent, detect, and treat colorectal cancer. They are also looking at what factors influence screening behaviors, how to address disparities, and the rising rates of colorectal cancer in younger people.
This page highlights some of the latest colorectal cancer research, including clinical advances that may soon translate into improved care, NCI-supported programs that are fueling progress, and findings from recent studies.
Prevention and Early Detection
Screening can prevent colorectal cancer through detection of precancerous growths, or polyps , which can be removed before they become cancerous. It can also allow colorectal cancers to be detected early, before they cause symptoms and when treatment may be more effective.
Colorectal cancer screening tests. These include colonoscopy , sigmoidoscopy , stool-based tests to detect hidden blood ( fecal immunochemical test ing (FIT) or fecal occult blood testing (FOBT)), and virtual colonoscopy . (See Screening Tests to Detect Colorectal Cancer and Polyps for more information.)
Despite the availability of effective colorectal cancer screening tests, some people choose not to get screened. Some reasons may be because of the personal nature of the procedures, a lack of recommendation by their doctor, perceived costs or lack of insurance, or the preparation involved for a colonoscopy.
Can Colorectal Cancer in Younger Adults Be Found Early?
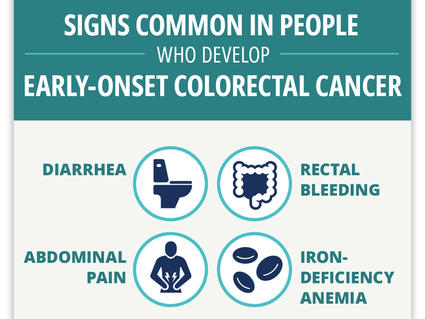
Researchers find four “red flag” signs that may identify colorectal cancer early in younger adults.
Although not currently recommended for screening, there are new techniques under development such as:
- finding technologies that improve the genetic analysis of stool samples, which may reveal the presence of tumor DNA
- looking at changes in the gut microbiome and trying to identify specific bacteria that could potentially help identify patients at risk for colorectal cancer
Repeat screening or follow-up . The guideline for getting a screening colonoscopy is every 10 years. However, people who have noncancerous polyps detected at colonoscopy are generally asked to return for a repeat colonoscopy earlier than that.
NCI’s FORTE Colorectal Cancer Prevention Trial , is now looking at whether some people with one or two small polyps can wait 10 years before returning for another colonoscopy. By comparing two study groups, one with repeat colonoscopy after 5 years, and one with repeat colonoscopy after 10 years, researchers hope to learn whether waiting 10 years is as good at preventing colorectal cancer as follow-up exams after 5 years.
For colorectal cancer screening to be effective, people need to follow up on abnormal test results. In one study, researchers found that people who had a positive at-home stool test to screen for colorectal cancer, but did not have a follow-up colonoscopy , were twice as likely to die from colorectal cancer as those who did have a follow-up colonoscopy.
NCI is funding research to better understand the many factors that can contribute to why a person may not have a follow-up test and how to increase repeat screening and follow-up colonoscopy after abnormal stool tests. Researchers are also studying how the many levels of the healthcare delivery system affect the decision to get screened.
Treatment for Colorectal Cancer
Surgically removing the cancer is the most common treatment for many stages of colorectal cancer. Chemotherapy, radiation , targeted therapy , radiofrequency ablation , and cryosurgery are other treatments that may be used to treat colorectal cancer, depending on the stage.
Because of an increased risk of recurrence, differences in anatomy, and poorer prognosis , the treatment of rectal cancer may differ from that of colon cancer. Although surgery remains a common type of treatment for local and locally advanced rectal cancer, people with some stages may be treated with radiation, chemotherapy, and/or targeted therapy with or without surgery.
In addition to these standard treatments for rectal cancer, researchers continue to study both new treatments, such as immunotherapies, and new combinations of existing treatments in clinical trials.
One trial is comparing a standard treatment (chemoradiation followed by combination chemotherapy) with chemoradiation followed by combination chemotherapy that includes an additional chemotherapy drug. The goal is to find out whether the additional chemotherapy drug may increase the likelihood of the cancer responding and possibly avoid the need for surgery.
Immunotherapy for patients with Lynch syndrome or MSI-H colorectal cancer
Approximately 5% of colorectal cancer cases are due to Lynch syndrome , an inherited DNA repair disorder . People with this disorder have an increased risk of developing colorectal cancer, typically before they reach the age of 50. Lynch syndrome colorectal cancer tumors have many mutations, which may make them more susceptible to immunotherapies.
A genetic feature known as microsatellite instability-high (MSI-H) is seen in about 15% of patients with stages II and III colorectal cancer and about 5% with stage IV. MSI-H means that there are mistakes in the way the DNA is copied in cancer cells, which can make them grow out of control.
The immune checkpoint inhibitors nivolumab (Opdivo) , ipilimumab (Yervoy) , and pembrolizumab (Keytruda) have all been approved for the treatment of metastatic colorectal cancer in patients with Lynch syndrome and in patients with MSI-H cancers.
The NCI-sponsored COMMIT study is testing the addition of atezolizumab (Tecentriq) to the combination of chemotherapy and the targeted therapy bevacizumab (Avastin) , for treating patients that have defective DNA mismatch repair. The hope is that combining drugs that work in different ways will improve treatment results in patients with colorectal cancer.
Another NCI-sponsored trial is studying whether atezolizumab will improve outcomes in people with earlier-stage disease (specifically, stage III colon cancer) that is deficient in DNA mismatch repair. This trial will compare combination chemotherapy with or without atezolizumab.
For people with locally advanced rectal cancer who have MSI-H cancer, one trial is studying the effects of nivolumab and ipilimumab when given together with short-course radiation therapy .
Combining immunotherapy with other treatments for patients without Lynch syndrome
Immune checkpoint inhibitors have been less effective in colorectal cancer patients without Lynch syndrome and whose cancers don't have mismatch repair deficiency . Scientists are currently testing various agents, such as chemotherapy drugs, targeted therapies and viruses, in combination with immune-based therapy to determine whether combining treatments would be effective in killing cancer cells.
Using targeted therapies for metastatic colorectal cancer
Using targeted therapies against genetic mutations that may drive tumor growth is another key area of research for metastatic colorectal cancer. The goal is to find agents that can block the activity of the abnormal proteins produced by these mutations. For example:
- The drug encorafenib (Braftovi ), which targets the BRAF protein, is approved for the treatment of some patients with colorectal cancer . This drug is used in combination with cetuximab (Erbitux) in adults with metastatic colorectal cancer whose tumors have a certain mutation in the BRAF gene and who have already undergone treatment.
- An NCI-supported trial showed that colorectal cancer that contains mutations in the BRAF gene responds to treatment with the drug vemurafenib (Zelboraf) in combination with cetuximab and irinotecan (Camptosar) . Vermurafentib targets mutant B-Raf proteins when combined with these two drugs.
- The NCI-sponsored SOLARIS trial is testing the addition of vitamin D3 to the combination of chemotherapy and bevacizumab for treating patients with metastatic colorectal cancer.
- In January 2023, the Food and Drug Administration (FDA) approved the combination of two targeted drugs, tucatinib (Tukysa) and trastuzumab (Herceptin) for people with advanced colorectal cancer that produces an excess amount of a protein called HER2. (3% or less of people with advanced colorectal cancer have tumors that overexpress this protein.) In the clinical trial that led to the approval, called MOUNTAINEER, more than one third of people who received the drug combination had their tumors shrink or disappear. For another third, tumors stopped growing for some time.
Testing liquid biopsies
Liquid biopsies are a promising new approach being explored to detect, analyze, and track DNA, cells, and other substances shed from tumors into bodily fluids, such as blood and urine. Scientists are testing this method to detect colorectal cancer early, measure treatment responses, identify treatment resistance, and monitor for disease recurrence.
One example is the COBRA trial, which found that testing blood for fragments of genetic material (DNA) shed by tumors , known as circulating tumor DNA (ctDNA), could identify patients with stage IIA colon cancer who might benefit from additional treatment with chemotherapy after surgery.
An ongoing trial is studying ctDNA in people with stage II or III colon cancer. The goal is to determine whether and what type of chemotherapy will benefit patients who have had surgery for their colon cancer based on the presence or absence of ctDNA.
NCI-Supported Research Programs
Many NCI-funded researchers at the NIH campus, and across the United States and world, are seeking ways to address colorectal cancer more effectively. Some research is basic, exploring questions as diverse as the biological underpinnings of cancer and the social factors that affect cancer risk. And some is more clinical, seeking to translate this basic information into improving patient outcomes. The programs listed below are a small sampling of NCI’s research efforts for colorectal cancer.
- The NCI-supported genetic study, ENLACE, aims to learn more about colorectal cancer in people of Hispanic and Latino descent , with the ultimate goal of improving treatments for this population group. To achieve this, scientists are also testing ways to engage more people from this group in cancer research.
- The Population-based Research to Optimize the Screening PRocess (PROSPR) is an NCI-supported network conducting research to better understand how to improve the entire cancer screening process (recruitment, screening, diagnosis, referral for treatment) for lung, colorectal, and cervical cancer in community healthcare settings.
- Accelerating Colorectal Cancer Screening and Follow-Up Through Implementation Science (ACCIS) is intended to promote research in colorectal cancer screening, follow-up, referral-to-care and best practices for how multilevel interventions can be scaled-up in regions of the United States where screening rates are below national standards.
- Approaches to Identify and Care for Individuals with Inherited Cancer Syndromes are studies designed to increase screening, prevention, and early treatment of people at high risk of cancer due to an inherited genetic susceptibility .
- The NCI-funded Colon Cancer Family Registry (CCFR) has established an international cohort of thousands of colorectal cancer patients, their relatives, and individuals at increased risk of colorectal and other cancers. Over 10,000 families from the United States, Canada, Australia, and New Zealand have been registered. The database includes more than 2,000 individuals with Lynch syndrome, from 781 families.
- The goal of the Screen to Save Initiative , funded by NCI’s Center for Cancer Health Equity , is to increase colorectal cancer screening in areas that need it most. Through community health educators, the program provides education and outreach to increase access to resources for those who may be affected by colorectal cancer.
- Dissemination of a Colorectal Cancer Screening Program Across American Indian Communities in the Southern Plains and Southwest United States is an effort to increase the use of colorectal cancer screening tests in American Indians. This project supports research on system-level changes and culturally appropriate media to promote screening, with the goal of closing the gap in colorectal cancer outcomes between the American Indian population and the general US population.
- NCI's Gastrointestinal (GI) SPOREs focus on translational research in the gastrointestinal system. Currently, GI SPOREs focus on cancers of the colon, rectum, esophagus, liver, gastrointestinal stromal tumors (GIST), and pancreas, which account for the majority of new diagnoses.
Clinical Trials
NCI funds and oversees both early- and late-phase clinical trials to develop new treatments and improve patient care. Trials are available for colorectal cancer screening , to prevent colon and rectal cancer , and treatment for colon cancer and rectal cancer.
Colorectal Cancer Research Results
The following are some of our latest news articles on colorectal cancer research:
- ctDNA May Guide Who Needs Chemo After Colorectal Cancer Surgery
- ENLACE Study Explores Colorectal Cancer in Hispanic and Latino People
- Is AI Ready to Play a Leading Role in Colorectal Cancer Screening?
- Some People with Rectal Cancer Can Skip Radiation Before Surgery
- How Fatty Liver Disease Helps Cancer Thrive in the Liver
- Study Identifies Potential Warning Signs of Colorectal Cancer in Younger Adults
View the full list of Colorectal Cancer Research Results and Study Updates .
DigitalCommons@UNMC
Home > Eppley Institute > Theses & Dissertations
Theses & Dissertations: Cancer Research
Theses/dissertations from 2024 2024.
Novel Spirocyclic Dimer (SpiD3) Displays Potent Preclinical Effects in Hematological Malignancies , Alexandria Eiken
Chemotherapy-Induced Modulation of Tumor Antigen Presentation , Alaina C. Larson
Understanding the role of MASTL in colon homeostasis and colitis-associated cancer development , Kristina Pravoverov
Dying Right: Supporting Anti-Cancer Therapy Through Immunogenic Cell Death , Elizabeth Schmitz
Therapeutic Effects of BET Protein Inhibition in B-cell Malignancies and Beyond , Audrey L. Smith
Targeting KSR1 to inhibit stemness and therapy resistance , Heidi M. Vieira
Identifying the Molecular Determinants of Lung Metastatic Adaptation in Prostate Cancer , Grace M. Waldron
Identification of Mitotic Phosphatases and Cyclin K as Novel Molecular Targets in Pancreatic Cancer , Yi Xiao
Theses/Dissertations from 2023 2023
Development of Combination Therapy Strategies to Treat Cancer Using Dihydroorotate Dehydrogenase Inhibitors , Nicholas Mullen
Overcoming Resistance Mechanisms to CDK4/6 Inhibitor Treatment Using CDK6-Selective PROTAC , Sarah Truong
Theses/Dissertations from 2022 2022
Omics Analysis in Cancer and Development , Emalie J. Clement
Investigating the Role of Splenic Macrophages in Pancreatic Cancer , Daisy V. Gonzalez
Polymeric Chloroquine in Metastatic Pancreatic Cancer Therapy , Rubayat Islam Khan
Evaluating Targets and Therapeutics for the Treatment of Pancreatic Cancer , Shelby M. Knoche
Characterization of 1,1-Diarylethylene FOXM1 Inhibitors Against High-Grade Serous Ovarian Carcinoma Cells , Cassie Liu
Novel Mechanisms of Protein Kinase C α Regulation and Function , Xinyue Li
SOX2 Dosage Governs Tumor Cell Identity and Proliferation , Ethan P. Metz
Post-Transcriptional Control of the Epithelial-to-Mesenchymal Transition (EMT) in Ras-Driven Colorectal Cancers , Chaitra Rao
Use of Machine Learning Algorithms and Highly Multiplexed Immunohistochemistry to Perform In-Depth Characterization of Primary Pancreatic Tumors and Metastatic Sites , Krysten Vance
Characterization of Metastatic Cutaneous Squamous Cell Carcinoma in the Immunosuppressed Patient , Megan E. Wackel
Visceral adipose tissue remodeling in pancreatic ductal adenocarcinoma cachexia: the role of activin A signaling , Pauline Xu
Phos-Tag-Based Screens Identify Novel Therapeutic Targets in Ovarian Cancer and Pancreatic Cancer , Renya Zeng
Theses/Dissertations from 2021 2021
Functional Characterization of Cancer-Associated DNA Polymerase ε Variants , Stephanie R. Barbari
Pancreatic Cancer: Novel Therapy, Research Tools, and Educational Outreach , Ayrianne J. Crawford
Apixaban to Prevent Thrombosis in Adult Patients Treated With Asparaginase , Krishna Gundabolu
Molecular Investigation into the Biologic and Prognostic Elements of Peripheral T-cell Lymphoma with Regulators of Tumor Microenvironment Signaling Explored in Model Systems , Tyler Herek
Utilizing Proteolysis-Targeting Chimeras to Target the Transcriptional Cyclin-Dependent Kinases 9 and 12 , Hannah King
Insights into Cutaneous Squamous Cell Carcinoma Pathogenesis and Metastasis Using a Bedside-to-Bench Approach , Marissa Lobl
Development of a MUC16-Targeted Near-Infrared Antibody Probe for Fluorescence-Guided Surgery of Pancreatic Cancer , Madeline T. Olson
FGFR4 glycosylation and processing in cholangiocarcinoma promote cancer signaling , Andrew J. Phillips
Theses/Dissertations from 2020 2020
Cooperativity of CCNE1 and FOXM1 in High-Grade Serous Ovarian Cancer , Lucy Elge
Characterizing the critical role of metabolic and redox homeostasis in colorectal cancer , Danielle Frodyma
Genomic and Transcriptomic Alterations in Metabolic Regulators and Implications for Anti-tumoral Immune Response , Ryan J. King
Dimers of Isatin Derived Spirocyclic NF-κB Inhibitor Exhibit Potent Anticancer Activity by Inducing UPR Mediated Apoptosis , Smit Kour
From Development to Therapy: A Panoramic Approach to Further Our Understanding of Cancer , Brittany Poelaert
The Cellular Origin and Molecular Drivers of Claudin-Low Mammary Cancer , Patrick D. Raedler
Mitochondrial Metabolism as a Therapeutic Target for Pancreatic Cancer , Simon Shin
Development of Fluorescent Hyaluronic Acid Nanoparticles for Intraoperative Tumor Detection , Nicholas E. Wojtynek
Theses/Dissertations from 2019 2019
The role of E3 ubiquitin ligase FBXO9 in normal and malignant hematopoiesis , R. Willow Hynes-Smith
BRCA1 & CTDP1 BRCT Domainomics in the DNA Damage Response , Kimiko L. Krieger
Targeted Inhibition of Histone Deacetyltransferases for Pancreatic Cancer Therapy , Richard Laschanzky
Human Leukocyte Antigen (HLA) Class I Molecule Components and Amyloid Precursor-Like Protein 2 (APLP2): Roles in Pancreatic Cancer Cell Migration , Bailee Sliker
Theses/Dissertations from 2018 2018
FOXM1 Expression and Contribution to Genomic Instability and Chemoresistance in High-Grade Serous Ovarian Cancer , Carter J. Barger
Overcoming TCF4-Driven BCR Signaling in Diffuse Large B-Cell Lymphoma , Keenan Hartert
Functional Role of Protein Kinase C Alpha in Endometrial Carcinogenesis , Alice Hsu
Functional Signature Ontology-Based Identification and Validation of Novel Therapeutic Targets and Natural Products for the Treatment of Cancer , Beth Neilsen
Elucidating the Roles of Lunatic Fringe in Pancreatic Ductal Adenocarcinoma , Prathamesh Patil
Theses/Dissertations from 2017 2017
Metabolic Reprogramming of Pancreatic Ductal Adenocarcinoma Cells in Response to Chronic Low pH Stress , Jaime Abrego
Understanding the Relationship between TGF-Beta and IGF-1R Signaling in Colorectal Cancer , Katie L. Bailey
The Role of EHD2 in Triple-Negative Breast Cancer Tumorigenesis and Progression , Timothy A. Bielecki
Perturbing anti-apoptotic proteins to develop novel cancer therapies , Jacob Contreras
Role of Ezrin in Colorectal Cancer Cell Survival Regulation , Premila Leiphrakpam
Evaluation of Aminopyrazole Analogs as Cyclin-Dependent Kinase Inhibitors for Colorectal Cancer Therapy , Caroline Robb
Identifying the Role of Janus Kinase 1 in Mammary Gland Development and Breast Cancer , Barbara Swenson
DNMT3A Haploinsufficiency Provokes Hematologic Malignancy of B-Lymphoid, T-Lymphoid, and Myeloid Lineage in Mice , Garland Michael Upchurch
Theses/Dissertations from 2016 2016
EHD1 As a Positive Regulator of Macrophage Colony-Stimulating Factor-1 Receptor , Luke R. Cypher
Inflammation- and Cancer-Associated Neurolymphatic Remodeling and Cachexia in Pancreatic Ductal Adenocarcinoma , Darci M. Fink
Role of CBL-family Ubiquitin Ligases as Critical Negative Regulators of T Cell Activation and Functions , Benjamin Goetz
Exploration into the Functional Impact of MUC1 on the Formation and Regulation of Transcriptional Complexes Containing AP-1 and p53 , Ryan L. Hanson
DNA Polymerase Zeta-Dependent Mutagenesis: Molecular Specificity, Extent of Error-Prone Synthesis, and the Role of dNTP Pools , Olga V. Kochenova
Defining the Role of Phosphorylation and Dephosphorylation in the Regulation of Gap Junction Proteins , Hanjun Li
Molecular Mechanisms Regulating MYC and PGC1β Expression in Colon Cancer , Jamie L. McCall
Pancreatic Cancer Invasion of the Lymphatic Vasculature and Contributions of the Tumor Microenvironment: Roles for E-selectin and CXCR4 , Maria M. Steele
Altered Levels of SOX2, and Its Associated Protein Musashi2, Disrupt Critical Cell Functions in Cancer and Embryonic Stem Cells , Erin L. Wuebben
Theses/Dissertations from 2015 2015
Characterization and target identification of non-toxic IKKβ inhibitors for anticancer therapy , Elizabeth Blowers
Effectors of Ras and KSR1 dependent colon tumorigenesis , Binita Das
Characterization of cancer-associated DNA polymerase delta variants , Tony M. Mertz
A Role for EHD Family Endocytic Regulators in Endothelial Biology , Alexandra E. J. Moffitt
Biochemical pathways regulating mammary epithelial cell homeostasis and differentiation , Chandrani Mukhopadhyay
EPACs: epigenetic regulators that affect cell survival in cancer. , Catherine Murari
Role of the C-terminus of the Catalytic Subunit of Translesion Synthesis Polymerase ζ (Zeta) in UV-induced Mutagensis , Hollie M. Siebler
LGR5 Activates TGFbeta Signaling and Suppresses Metastasis in Colon Cancer , Xiaolin Zhou
LGR5 Activates TGFβ Signaling and Suppresses Metastasis in Colon Cancer , Xiaolin Zhou
Theses/Dissertations from 2014 2014
Genetic dissection of the role of CBL-family ubiquitin ligases and their associated adapters in epidermal growth factor receptor endocytosis , Gulzar Ahmad
Strategies for the identification of chemical probes to study signaling pathways , Jamie Leigh Arnst
Defining the mechanism of signaling through the C-terminus of MUC1 , Roger B. Brown
Targeting telomerase in human pancreatic cancer cells , Katrina Burchett
The identification of KSR1-like molecules in ras-addicted colorectal cancer cells , Drew Gehring
Mechanisms of regulation of AID APOBEC deaminases activity and protection of the genome from promiscuous deamination , Artem Georgievich Lada
Characterization of the DNA-biding properties of human telomeric proteins , Amanda Lakamp-Hawley
Studies on MUC1, p120-catenin, Kaiso: coordinate role of mucins, cell adhesion molecules and cell cycle players in pancreatic cancer , Xiang Liu
Epac interaction with the TGFbeta PKA pathway to regulate cell survival in colon cancer , Meghan Lynn Mendick
Theses/Dissertations from 2013 2013
Deconvolution of the phosphorylation patterns of replication protein A by the DNA damage response to breaks , Kerry D. Brader
Modeling malignant breast cancer occurrence and survival in black and white women , Michael Gleason
The role of dna methyltransferases in myc-induced lymphomagenesis , Ryan A. Hlady
Design and development of inhibitors of CBL (TKB)-protein interactions , Eric A. Kumar
Pancreatic cancer-associated miRNAs : expression, regulation and function , Ashley M. Mohr
Mechanistic studies of mitochondrial outer membrane permeabilization (MOMP) , Xiaming Pang
Novel roles for JAK2/STAT5 signaling in mammary gland development, cancer, and immune dysregulation , Jeffrey Wayne Schmidt
Optimization of therapeutics against lethal pancreatic cancer , Joshua J. Souchek
Theses/Dissertations from 2012 2012
Immune-based novel diagnostic mechanisms for pancreatic cancer , Michael J. Baine
Sox2 associated proteins are essential for cell fate , Jesse Lee Cox
KSR2 regulates cellular proliferation, transformation, and metabolism , Mario R. Fernandez
Discovery of a novel signaling cross-talk between TPX2 and the aurora kinases during mitosis , Jyoti Iyer
Regulation of metabolism by KSR proteins , Paula Jean Klutho
The role of ERK 1/2 signaling in the dna damage-induced G2 , Ryan Kolb
Regulation of the Bcl-2 family network during apoptosis induced by different stimuli , Hernando Lopez
Studies on the role of cullin3 in mitosis , Saili Moghe
Characteristics of amyloid precursor-like protein 2 (APLP2) in pancreatic cancer and Ewing's sarcoma , Haley Louise Capek Peters
Structural and biophysical analysis of a human inosine triphosphate pyrophosphatase polymorphism , Peter David Simone
- Eppley Institute Website
- McGoogan Library
Advanced Search
- Notify me via email or RSS
- Collections
- Disciplines
Author Corner
Home | About | FAQ | My Account | Accessibility Statement
Privacy Copyright
Do a more advanced search »
Search for dissertations about: "thesis for colon cancer"
Showing result 1 - 5 of 270 swedish dissertations containing the words thesis for colon cancer .
1. Risk and survival for colorectal cancer in northern Sweden : sociodemographic factors and surveillance programs
Author : Olle Sjöström ; Beatrice S. Melin ; Lars H Lindholm ; Richard Palmqvist ; Johannes Blom ; Umeå universitet ; [] Keywords : MEDICIN OCH HÄLSOVETENSKAP ; MEDICAL AND HEALTH SCIENCES ; Colorectal cancer ; Risk factors ; Cancer epidemiology ; Endoscopy general ; Health economy ; Cancer prevention ; Hereditary colorectal ; Surveillance colonoscopy ; Cancer Epidemiology ; cancerepidemiologi ; Genetics ; genetik ; Surgery ; kirurgi ; Oncology ; onkologi ;
Abstract : BackgroundColorectal cancer (CRC) – i.e., cancer in the colon or rectum – is one of the most common cancers both globally and in Sweden. The risk for CRC is mainly related to age, heredity, and life-style risk factors. READ MORE
2. Hereditary Nonpolyposis Colorectal Cancer - Molecular Genetics and Biology of Associated Tumors
Author : Maria Planck ; Bröstcancer-genetik ; [] Keywords : MEDICIN OCH HÄLSOVETENSKAP ; MEDICAL AND HEALTH SCIENCES ; endometrial cancer ; rectal cancer ; colon cancer ; mismatch repair protein expression ; coding repeats ; microsatellite instability ; MSH6 ; MSH2 ; Hereditary nonpolyposis colorectal cancer ; MLH1 ; small bowel cancer ; Cytology ; oncology ; cancerology ; Cytologi ; onkologi ; cancer ;
Abstract : This thesis focuses on one of the most common types of hereditary cancer, hereditary nonpolyposis colorectal cancer (HNPCC). This syndrome is characterized by an autosomal dominant inheritance, an increased risk for several types of cancer (especially cancer of the colorectum, small bowel, endometrium, ovary and urinary tract), early age at diagnosis, and frequent development of multiple primary malignancies. READ MORE
3. Chemoradiation in Gastrointestinal Cancer
Author : Adalsteinn Gunnlaugsson ; Bröstcancer-genetik ; [] Keywords : MEDICIN OCH HÄLSOVETENSKAP ; MEDICAL AND HEALTH SCIENCES ; Biliary tract cancer ; capecitabine ; cholangiocarcinoma ; chemoradiation ; colon cancer ; enteritis 5-fluorouracil ; gallbladder cancer ; oxaliplatin ; pancreatic cancer ; rectal cancer. ;
Abstract : Locally advanced inextirpable gastrointestinal cancer has poor prognosis and is associated with high morbidity. One treatment option is to use radiotherapy, often combined with chemotherapy (chemoradiation), either as preoperative treatment to facilitate surgery or in the palliative setting to relieve symptoms. READ MORE
4. Cancer and Inflammation : Role of Macrophages and Monocytes
Author : Alexander Hedbrant ; Jonny Wijkander ; Dick Delbro ; Ann Erlandsson ; Anita Sjölander ; Karlstads universitet ; [] Keywords : NATURVETENSKAP ; NATURAL SCIENCES ; MEDICIN OCH HÄLSOVETENSKAP ; MEDICAL AND HEALTH SCIENCES ; MEDICIN OCH HÄLSOVETENSKAP ; MEDICAL AND HEALTH SCIENCES ; M1 macrophages ; M2 macrophages ; colon cancer ; lung cancer ; prostaglandin E2 ; Biomedical Sciences ; Biomedicinsk vetenskap ;
Abstract : Macrophages are cells of the innate immune system that can be found in large quantities in cancer tumors and affect cancer progression by regulating growth and invasiveness of cancer cells. There are two main phenotypes of macrophages denoted M1 and M2. READ MORE
5. Circulating markers of risk and etiology in colorectal cancer
Author : Justin Harbs ; Sophia Harlid ; Bethany van Guelpen ; Xijia Liu ; Henrik Grönberg ; Umeå universitet ; [] Keywords : MEDICIN OCH HÄLSOVETENSKAP ; MEDICAL AND HEALTH SCIENCES ; Colorectal cancer ; CRC ; sex hormones ; colon cancer ; DNA methylation ; proteomics ; risk ; etiology ; Cancer Epidemiology ; cancerepidemiologi ;
Abstract : Background: Colorectal cancer is the third most commonly diagnosed cancer in men and women. Worldwide around 2 million individuals are diagnosed each year – a number expected to increase as colorectal cancer risk factors become more prevalent. READ MORE
Searchphrases right now
- life-threatening
- short term voltage stability
- Company based acquisition
- it infrastructure management
- climate change mortality
- ultrasound.
- quality management in healthcare
- strain-rate
- pilot scale
Popular searches
- WATER QUALITY
- temporal information
- viral hepatitis
- RATIO ANALYSIS
- thesis on semiotics
- manufacturing design engineering thesis
- thesis in microbiology
- twist grain boundary phase
- Experimental methods
- intonation.
Popular dissertations yesterday (2024-08-15)
- Virtualizing Operational Technology by Distributed Digital Twins
- Cardiovascular comorbidity in rheumatoid arthritis
- Chiral Recognition by Means of Mass Spectrometry
- Svensk vattenkraft ur ett europeiskt perspektiv : några exempel
- Rummet och människans rörelser
- Calibration Adjustment for Nonresponse in Sample Surveys
- Development and application of methods for analysis of flow and heat transfer and heat exchanger networks
- The influence of codon context on translation termination and messenger RNA levels
- Bacterial vagimosis. Diagnosis, treatment and significance in gynaecological practice
- Nuclear medicine and cytotoxic studies in renal cell cancer
- Popular complementary terms: essays, phd thesis, master thesis, papers, importance, trend, impact, advantages, disadvantages, role of, example, case study.
See yesterday's most popular searches here . Dissertations.se is the english language version of Avhandlingar.se .
- Featured News
- Artificial Intelligence
- Bioprocessing
- Drug Discovery
- Genome Editing
- Infectious Diseases
- Translational Medicine
- Browse Issues
- Learning Labs
- eBooks/Perspectives
- GEN Biotechnology
- Re:Gen Open
- New Products
- Conference Calendar
- Get GEN Magazine
- Get GEN eNewsletters

Novel Mutated Driver Genes Uncovered in Colorectal Cancer
Credit: SCIENCE ARTWORK/SCIENCE PHOTO LIBRARY
The Institute of Intelligent Medical Research (IIMR) of BGI Genomics, in collaboration with Sweden’s Uppsala University, have uncovered 33 novel mutated driver genes in colorectal cancer (CRC). The researchers analyzed the whole genomes and transcriptomes of 1,063 primary colorectal cancers within a population-based cohort, with 94% of the patients completing a five-year clinical follow-up. Their analysis identified 96 mutated driver genes, nine of which were previously unknown in CRC, and 24 that were new to any form of cancer.
The findings are published in the journal Nature in an article entitled “ Prognostic genome and transcriptome signatures in colorectal cancers .”
“Colorectal cancer is caused by a sequence of somatic genomic alterations affecting driver genes in core cancer pathways,” the researchers wrote. “Here, to understand the functional and prognostic impact of cancer-causing somatic mutations, we analysed the whole genomes and transcriptomes of 1,063 primary colorectal cancers in a population-based cohort with long-term follow-up. From the 96 mutated driver genes, 9 were not previously implicated in colorectal cancer and 24 had not been linked to any cancer. Two distinct patterns of pathway co-mutations were observed, timing analyses identified nine early and three late driver gene mutations, and several signatures of colorectal-cancer-specific mutational processes were identified.”
Several specific mutation patterns that are unique to CRC were identified. Mutations in specific pathways (WNT, EGFR, TGFβ), a mitochondrial gene (CYB), three regulatory elements, 21 copy-number variations (alterations in the number of copies of a particular gene), and a specific mutation signature (COSMIC SBS44) were linked to patient survival rates.
Building on these findings, the researchers developed a new strategy to molecularly classify colorectal cancer. Through an integrated analysis that combined mutated genes with gene expression levels, they identified five distinct CRC prognostic subtypes (CRPSs), each with unique molecular characteristics. This new classification system is poised to revolutionize the way CRC is diagnosed and treated.
Through timing analysis, the study uncovered that specific genetic alterations, such as those in APC, TP53, KRAS, BRAF, ZFP36L2, TCF7L2, FBXW7, BCL9L, and SOX9, tend to occur early in the cancer’s progression. Meanwhile, other mutations, particularly in TRPS1, GNAS, and CEP170, are more likely to appear during the later stages of cancer development.
Beyond identifying critical molecular changes linked to tumor invasion and metastasis, the study uncovered disease-related mutations in the mitochondrial genome and non-coding regions, offering a comprehensive summary of mutations that play a significant role in disease progression.
The discovery of the mutations and expression subtypes can guide future efforts to individualized colorectal cancer therapy.
Related Content

The Role Receptor Protein Tyrosine Phosphatases Play in Cancer and Tissue Repair

Strokes and Heart Problems Linked by Immune Epigenetics

Idea for Curbing Colon Cancer: Get a Jump on Retroviruses

Base Editing Tweaks Mouse Gut Microbiome, in Scientific First
Proteologics reports progress in drug discovery collaboration with teva pharmaceutical, mechanism for gene silencing in skin cancer discovered.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- AME Case Rep

Radiation induced rectal cancer: a case report with review of the literature
Mustapha dahiri.
1 Department of digestive surgery, National Institute of Oncology, Rabat, Morocco;
2 Faculty of Medicine and Pharmacy, Mohammed V University, Souissi, Rabat, Morocco
Nariman Salmi
Anas ahallat, nezha el bahaoui, omar belkouchi, amine souadka, anas majbar, amine benkabbou, abdeslam bougtab, raouf mohsine.
Cervical cancer is the second most common cancer and the third cause of cancer death in women. Radiotherapy occupies a prominent place in the therapeutic arsenal of cervical cancer in localized stages. Radiation induced secondary cancer is an entity that has been well described in the literature. We report a case of a rectal adenocarcinoma occurring in a woman previously treated by radiotherapy and brachytherapy for a squamous cell carcinoma of the cervix.
Introduction
Colorectal cancer is the third diagnosed cancer in men and the second in women, with an estimated of 1.4 million cases and 693,900 deaths occurring in 2012. The risk of colorectal cancer is higher within men ( 1 ).
The main risk factors for colorectal cancer are age above 50 years, inflammatory bowel diseases, personal or family history of adenoma or colorectal cancer, genetic predisposition, excessive consumption of red meat, alcohol, smoking and obesity ( 2 - 11 ).
The role of pelvic radiotherapy in the induction of rectal cancer has been found in several cases of rectal cancers after pelvic irradiation for a primary cancer other than the rectum. In this article we describe the case of a patient who developed a rectal adenocarcinoma, 18 years after being irradiated for squamous cell carcinoma of the cervix.
Case presentation
Our patient is a 73 years old woman, not a cigarette smoker or alcoholic, followed in our hospital since 1999 for squamous cell carcinoma of the cervix and presented 18 years after rectal bleeding and a rectal syndrome that revealed a well differentiated adenocarcinoma of the rectum. She has no history of inflammatory bowel disease or polyp and no history of cancer in the family. The squamous cell carcinoma of the cervix was according to the FIGO classification classified as stage IIB. The patient received external radiotherapy at a dose of 46 Gray with brachytherapy supplement at the dose of 26 Gray followed by a radical hysterectomy extended to both parameters with pelvic lymph node dissection. Subacute inflammatory rearrangements associated with a few perennial cervical tumor residues, with an inflammatory vaginal collar with some non-perennial tumor residues, were found in the histological study.
The patient was put under surveillance. She remained in good control until August 2017 when she presented rectal bleeding with a rectal syndrome. A hemi-circumferential budding process located at 2 cm from the anal margin was found in the digital rectal examination. She weighed 60 kilograms, heighted 160 cm with a body mass index of 23.4. The rest of the physical examination was normal. The colonoscopy found an ulcerative budding process 2 cm from the anal margin without other abnormalities in the rest of the colon. A well differentiated adenocarcinoma was diagnosed in the histological study. The chest-abdomen-pelvis CT scan performed as part of the extension assessment showed a thickening of the lower rectum without secondary locations. Pelvic magnetic resonance imaging showed thickening of the lower rectum without mesorectal adenomegaly ( Figure 1 ). Tumor markers CEA and CA 19-9 were normal (CEA at 2.5 nanograms per milliliter and CA19-9 at 12 international units per milliliter).

Two MRI images showing a posterior hemi-circumferential tumor of the lower rectum in our patient.
The patient’s file was discussed at a multidisciplinary consultation meeting and a surgery was indicated at first. She had benefited from abdominoperineal resection with permanent left iliac fossa end colostomy.
The pathological analysis of the resection specimen showed a well differentiated adenocarcinoma infiltrating the rectal wall to perirectal fat with clearance of 1 millimeter, lymphovascular and perineural invasion were absent, proximal and distal margins were free, no ganglion was positive on 3 ganglions removed. The tumor was classified pT3N0M0 according to the TNM classification.
No adjuvant treatment was received and the patient is currently under control, with no evidence of local or metastatic recurrence with a follow-up of 8 months.
Cervical cancer is the second most common cancer in women after breast cancer ( 1 ). Radiotherapy occupies an angular place in the treatment of cervical cancer ( 12 , 13 ). Improvement in overall survival reveals long term complications in long term survivors. Among these complications is the possibility of a radio induced secondary cancer. Cahan et al. are among the first to introduce the notion of secondary radio induced cancer, in 1948, by describing a series of 11 cases and they proposed criteria defining the radio induced tumors which are: tumor located in the initial field of irradiation, having a different histology from the initial lesion which appears after a relatively long delay of more than 5 years after irradiation ( 14 ).
PubMed research has found reports of isolated cases of rectal cancer after cervical cancer radiotherapy ( 15 - 18 ). In these publications, the delay between secondary cancer and radiotherapy was variable but relatively long ranging from 12 to 46 years.
Rodriguez and al conducted a study based on SEER data on 64507 patients with cervical cancer, more than half of whom (52.6%) received pelvic radiotherapy ( 19 ). The authors showed in this study that there is no significant difference in the risk of occurrence of colorectal cancer in patients who received radiotherapy versus patients who did not receive it, although the risk becomes significant after 8 years for colon cancer and after 15 years for rectal cancer. Based on these results, the authors propose early detection of colorectal cancer in patients who have not reached the age of 50, 8 years after cervical cancer irradiation. These results were confirmed by a second study that showed a significant difference in the occurrence of rectal cancer in patients receiving radiation therapy on cervical cancer versus those who did not receive it (482 vs. 108) ( 20 ).
Our patient presented an adenocarcinoma of the rectum 18 years after being irradiated for her squamous cell carcinoma of the cervix. This delay is consistent with what it has been found in the literature. She presents criteria to diagnose a radio induced cancer proposed by Cahan et al. Also, she presents only one risk factor for colorectal cancer: age over 50 years. Considering all these elements, it is thought that this is a radio induced cancer more than a non-radio induced cancer.
Conclusions
We report a rare case of rectal adenocarcinoma in previously irradiated patient for cervical cancer. Available literature data currently show that rectal cancer may be a late complication of radiotherapy. We must think about considering this entity in monitoring protocols for long term survival patients who have been irradiated for cervical cancer.
Acknowledgements
Informed Consent: Written informed consent was obtained from the patient for publication of this Case Report and any accompanying images.
Conflicts of Interest: The authors have no conflicts of interest to declare.
Choose your country or region:
- United Kingdom
New Modeling Data Show the Cologuard® Test Has Detected More Than 623,000 Cancers and Precancers Over Past Decade, Saving U.S. Health Care System $22 Billion

Data demonstrate long-term impact of the Cologuard test, a powerful tool for preventing and detecting cancer
MADISON, Wis., Aug. 15, 2024 — Exact Sciences Corp. (Nasdaq: EXAS), a leading provider of cancer screening and diagnostic tests, shared new modeling data today describing the projected impact of the Cologuard test on patients, health care professionals, and the U.S. health care system since its FDA approval 10 years ago.
The data assessed the far-reaching benefits of the first and only multi-target stool DNA test for patients, their families, and the health care system. Over the past 10 years, the Cologuard test has been used to screen for colorectal cancer (CRC) more than 16 million times.
The Cologuard test is the most effective noninvasive option for CRC screening 1 and an important tool for closing the gap of 60 million Americans not up to date with screening. 2 According to data from the Centers for Disease Control and Prevention (CDC), Cologuard test use is the primary contributor to the increase in colon cancer screening rates from 63% in 2015 to 72% in 2021 among Americans ages 50-75. 3 In addition, a new study from EPIC research showed the number of people ages 45-49 completing screening with the Cologuard test tripled from 2021 to 2023. 4
“As Exact Sciences marks the 10th anniversary of Cologuard, we reflect on the vital role that it has played in the prevention and early detection of colorectal cancer, making screening more accessible and effective for patients,” said Kevin Conroy, chairman and CEO of Exact Sciences. “We reached this milestone thanks to long-standing partnerships from health care professionals and advocacy organizations, as well as the support of our dedicated team. With our next-generation Cologuard test currently under FDA review, we look forward to bringing patients a new level of accuracy and innovation in at-home testing.”
10 years of patient impact
The modeled data projects that over the past 10 years 5* :
· There have been more than 16 million completed screenings with the Cologuard test, or approximately one every 20 seconds.
· The Cologuard test detected 525,000 people with advanced precancerous lesions — growths most likely to advance to cancer. Removal of these growths can help prevent cancer.
· 80% of cancers detected by the Cologuard test were early-stage cancers.
· 42,000 people were identified to have stage I. By detecting cancer earlier, patients are less likely to need chemotherapy or radiation treatment, sparing them and their families that difficult experience.
“Colorectal cancer is the number two cancer killer 6 , but it doesn’t need to be this way. We have very effective tools to find the precursors to this cancer and also to detect these cancers at earlier, more curable stages,” said Dr. Folasade May, director of quality in digestive diseases at UCLA Health and co-founder and board member of the Association of Black Gastroenterologists and Hepatologists. “ With the convenience of a noninvasive use-at-home test and ability to find more than 90% of cancers as well as many pre-cancers 7 , Cologuard is unique among non-invasive tests. That’s why I recommend it as an option to average-risk individuals who prefer to screen with a home-based option.” †
Improvements in CRC screening participation, health care and the economy
The strong performance of the Cologuard test has also positively impacted CRC screening rates, the economy, health care access and costs. The modeled data projected that since the Cologuard test was introduced 5* :
· More than $22B has been saved in health care costs due to pre-cancer and early cancer detection as compared to no screening. 5, 8,9 *
· The Cologuard test contributed to 77% of the improvement in CRC screening rates between 2018 and 2021. 9
· Health care staff were able to reduce hours spent toward screening average risk and asymptomatic people, allowing them to focus on treating people with symptoms and those who are high risk with colonoscopies. The projections show use of the Cologuard test as an alternative to colonoscopy in eligible patients has helped save:
o 2.1 million scheduling hours 5,10*
o 3.5 million nursing hours 5,10*
o 1.1 million provider hours 5,10*
During a time when at-home health and wellness tests were relatively limited, the Cologuard test transformed CRC screening access. Within a decade, more people screened for colorectal cancer than ever before because of the Cologuard test — playing a critical role in addressing the screening gap for average-risk adults that colonoscopies and other tests cannot close alone. Data show that if colonoscopy were the only tool available, it would take more than 10 years to address the backlog. 1,5,11
"I was 48 when I screened with Cologuard," said Katie Hawbaker, a stage II CRC survivor. "Early detection is everything. Finding out I had a cancerous mass was a huge shock, but I have lots to be thankful for — I needed no chemo or radiation because my cancer was caught early."
Exact Sciences continues to invest in innovation and improvements to the Cologuard test, emphasizing the company’s commitment to revolutionizing CRC screening and closing the screening gap. The next-generation Cologuard test is under review with the U.S. Food and Drug Administration.
*Estimates are based on modeling projections using performance data from the pivotal DeeP-C study
† Dr. Folasade May has provided consulting services for Exact Sciences. She has not been compensated for any media work.
1. Fendrick AM, Fisher DA, Saoud L, Ozbay AB, Karlitz JJ, Limburg PJ. Impact of Patient Adherence to Stool-Based Colorectal Cancer Screening and Colonoscopy Following a Positive Test on Clinical Outcomes. Cancer Prev Res (Phila) . 2021;14(9):845-850. doi:10.1158/1940-6207.CAPR-21-0075
2. Ebner DW, Kisiel JB, Fendrick AM, et al. Estimated Average-Risk Colorectal Cancer Screening-Eligible Population in the US. JAMA Netw Open . 2024;7(3):e245537.
3. National Institutes of Health. The Cancer Trends Progress Report. https://progressreport.cancer.gov/detection/colorectal_cancer . Accessed July 29, 2024.
4. Epic Research. DNA Stool Tests for Colorectal Cancer Screening Growing in Popularity, Especially for Patients Under Age 50. May 14, 2024. https://www.epicresearch.org/articles/dna-stool-tests-for-colorectal-cancer-screening-growing-in-popularity-especially-for-patients-under-age-50 . Accessed July 29, 2024.
5. Estes C, Dehghani M, Ozbay A, et al. Clinical, social and economic impacts of colorectal cancer screening with the multi-target stool-DNA test: 10-year experience – a simulated study. MedRxiv.org https://doi.org/10.1101/2024.08.07.24311643
6. ACS. Cancer facts & figures 2024. Atlanta: American Cancer Society; 2024.
7. Imperiale TF, Ransohoff DF, Itzkowitz SH, et al. Multitarget stool DNA testing for colorectal-cancer screening. N Engl J Med. 2014;370(14):1287-1297.
8. Fitch K, Pyenson B, Blumen H, et al. The value of colonoscopic colorectal cancer screening of adults aged 50 to 64. National Library of Medicine . 2015; 21(7):e430-8. Accessed June 27, 2024. https://pubmed.ncbi.nlm.nih.gov/26295271/
9. Ebner DW, Finney Rutten LJ, Miller-Wilson LA, et al. Trends in Colorectal Cancer Screening from the National Health Interview Survey: Analysis of the Impact of Different Modalities on Overall Screening Rates. Cancer Prev Res (Phila) . 2024;17(6):275-280.
10. Horejsi A, Roberts, C, Walter J, et al. Augmenting Intelligence & Amplifying Health: Proactive Outreach for Enhanced Preventive Screening. Mayo Foundation for Medical Education and Research. 2024. Accessed June 27, 2024. https://www.ache.org/-/media/ache/learning-center/research/2024-poster-presentation-posters/poster-13.pdf?_sm_nck=1 11. Joseph DA, Meester RG, Zauber AG, et al. Colorectal cancer screening: Estimated future colonoscopy need and current volume and capacity [published correction appears in Cancer. 2017 Oct 1;123(19):3857]. Cancer. 2016;122(16):2479-2486.
About the Cologuard test
The Cologuard test is a first-line colorectal cancer screening test for use in adults age 45 or older who are at average risk for the disease. It is included in national colorectal cancer screening guidelines by the American Cancer Society (2018) 1 and the U.S. Preventive Services Task Force (2021) 2 .
The Cologuard test revolutionized colorectal cancer screening by providing a best-in-class, noninvasive testing option for those at average risk. The test looks for certain DNA markers and blood in the stool that are associated with colorectal cancer and precancer and was shown to effectively detect colorectal cancer and precancer in the pivotal phase 3 DeeP-C study. 3 The Cologuard test is easy to use. It can be completed at home and does not require any time off or special preparation. In the initial 10 years since launch, the Cologuard test was used more than 16 million times.
Important information about the Cologuard test
Do not use the Cologuard test if you have had precancer, have inflammatory bowel disease and certain hereditary syndromes, or have a personal or family history of colorectal cancer. The Cologuard test is not a replacement for colonoscopy in high-risk patients. The Cologuard test performance in adults ages 45-49 is estimated based on a large clinical study of patients 50 and older. The Cologuard test performance in repeat testing has not been evaluated. The Cologuard test result should be interpreted with caution. A positive test result does not confirm the presence of cancer. Patients with a positive test result should be referred for colonoscopy. A negative test result does not confirm the absence of cancer. Patients with a negative test result should discuss with their doctor when they need to be tested again. Medicare and most major insurers cover the Cologuard test. For more information about the Cologuard test, visit Cologuard.com . Rx only.
About Exact Sciences Corp. A leading provider of cancer screening and diagnostic tests, Exact Sciences gives patients and health care professionals the clarity needed to take life-changing action earlier. Building on the success of the Cologuard® and Oncotype® tests, Exact Sciences is investing in its pipeline to develop innovative solutions for use before, during, and after a cancer diagnosis. For more information, visit ExactSciences.com , follow Exact Sciences on X (formerly known as Twitter) @ExactSciences, or find Exact Sciences on LinkedIn and Facebook.
NOTE: Exact Sciences and Cologuard are trademarks or registered trademarks of Exact Sciences Corporation. Oncotype, Oncotype DX, Oncotype DX Breast Recurrence Score, RSClin, and Recurrence Score are trademarks or registered trademarks of Genomic Health, Inc. All other trademarks and service marks are the property of their respective owners. Cologuard is not available outside of the U.S. Exact Sciences’ multi-cancer early detection test is still in development.
Forward-Looking Statements
This news release contains forward-looking statements concerning our expectations, anticipations, intentions, beliefs, or strategies regarding the future. These forward-looking statements are based on assumptions that we have made as of the date hereof and are subject to known and unknown risks and uncertainties that could cause actual results, conditions and events to differ materially from those anticipated. Therefore, you should not place undue reliance on forward-looking statements. Risks and uncertainties that may affect our forward-looking statements are described in the Risk Factors sections of our most recent Annual Report on Form 10-K and any subsequent Quarterly Reports on Form 10-Q, and in our other reports filed with the Securities and Exchange Commission. We undertake no obligation to publicly update any forward-looking statement, whether written or oral, that may be made from time to time, whether as a result of new information, future developments or otherwise.
Media Contact (U.S.): Lindsey Dickinson +1 608-690-0383 [email protected] Investor Contact: Erik Holznecht +1 608-800-6605 [email protected]
Subscribe To The Blog
- Community(6)
- Infographics(3)
- Healthy Living(13)
- Hero of the Month(10)
- Colon Cancer News and Information(20)
- Press Releases(88)
- Colon Cancer Awareness(4)
- Investor Relations(41)
- Company(50)
- Exact Sciences News(108)
- Partnerships(13)
Recommended Content

Court Ruling Enables Exact Sciences to Proceed with Lawsuit against Geneoscopy


Exact Sciences Demonstrates Continued Scientific Advancement in Colorectal Cancer Screening with Multiple Data Presentations at DDW ® 2024

Exact Sciences Names Aaron Bloomer as New Chief Financial Officer
- Bibliography
- More Referencing guides Blog Automated transliteration Relevant bibliographies by topics
- Automated transliteration
- Relevant bibliographies by topics
- Referencing guides
U.S. Food and Drug Administration
- Search
- Menu
- Development & Approval Process | Drugs
- Drug Approvals and Databases
- Resources for Information | Approved Drugs
FDA D.I.S.C.O. Burst Edition: FDA approvals of Augtyro (repotrectinib) for NTRK gene fusion-positive solid tumors and Krazati (adagrasib) for KRAS G12C-mutated colorectal cancer
Welcome back to the D.I.S.C.O., FDA’s Drug Information Soundcast in Clinical Oncology, Burst Edition, brought to you by FDA’s Division of Drug Information in partnership with FDA’s Oncology Center of Excellence. Today we’ll provide a quick update on two recent FDA cancer drug approvals.
On June 13, 2024, the FDA granted accelerated approval to repotrectinib (brand name Augtyro) for adult and pediatric patients 12 years and older with solid tumors that have a neurotrophic tyrosine receptor kinase gene fusion, are locally advanced or metastatic or where surgical resection is likely to result in severe morbidity, and that have progressed following treatment or have no satisfactory alternative therapy.
Efficacy was evaluated in TRIDENT-1, a multicenter, single-arm, open-label, multi-cohort trial in 88 adult patients with locally advanced or metastatic neurotrophic tyrosine receptor kinase gene fusion-positive solid tumors who had either received a prior tyrosine receptor kinase tyrosine kinase inhibitor or were tyrosine kinase inhibitor-naïve. All patients were assessed for central nervous lesions at baseline, and patients with symptomatic brain metastases were excluded. Tumor assessments were performed every 8 weeks.
The major efficacy outcome measures were overall response rate and duration of response according to RECIST v1.1 as assessed by blinded independent central review. Confirmed overall response rate in the tyrosine kinase inhibitor-naïve group was 58% and 50% in the tyrosine kinase inhibitor-pretreated group. Median duration of response was not estimable in the tyrosine kinase inhibitor-naïve group and 9.9 months in the tyrosine kinase inhibitor-pretreated group.
The most common adverse reactions reported in more than 20% of patients were dizziness, dysgeusia, peripheral neuropathy, constipation, dyspnea, fatigue, ataxia, cognitive impairment, muscular weakness, and nausea.
This review used the Assessment Aid , a voluntary submission from the applicant to facilitate the FDA’s assessment.
On June 21, 2024, the FDA granted accelerated approval to adagrasib (brand name Krazati) plus cetuximab for adults with KRAS G12C-mutated locally advanced or metastatic colorectal cancer, as determined by an FDA-approved test, who have received prior treatment with fluoropyrimidine-, oxaliplatin-, and irinotecan-based chemotherapy.
Efficacy was evaluated in KRYSTAL-1, a multicenter, single-arm expansion cohort trial. Eligible patients were required to have locally advanced or metastatic KRAS G12C-mutated colorectal cancer previously treated with fluoropyrimidine-, oxaliplatin-, and irinotecan-based chemotherapy, and a VEGF inhibitor, if eligible. Patients were treated with adagrasib 600 mg twice daily plus cetuximab administered either biweekly or weekly. Tumor assessments were performed every 6 weeks. Adagrasib discontinuation required cetuximab discontinuation, however patients could continue adagrasib if cetuximab was discontinued.
The major efficacy outcome measures were confirmed overall response rate and duration of response according to RECIST v1.1 assessed by blinded independent central review. In the 94 enrolled patients, overall response rate was 34%, all responses were partial responses, and median duration of response was 5.8 months. Thirty-one percent of responding patients had a duration of response of at least 6 months.
The most common adverse reactions reported in more than 20% of patients were rash, nausea, diarrhea, vomiting, fatigue, musculoskeletal pain, hepatotoxicity, headache, dry skin, abdominal pain, decreased appetite, edema, anemia, cough, dizziness, constipation, and peripheral neuropathy.
Full prescribing information for these approvals can be found on the web at www.fda.gov/drugsatfda .
Health care professionals should report serious adverse events to www.fda.gov/medwatch .
Follow the Division of Drug Information on X @FDA_Drug_Info and the Oncology Center of Excellence @FDAOncology . Send your feedback via email to [email protected] . Thanks for tuning in to the D.I.S.C.O. Burst Edition.
- Aboriginal and Torres Strait Islander Health Performance Framework
- Australian Mesothelioma Registry
- GEN Aged Care Data
- Housing data
- Indigenous Mental Health and Suicide Prevention Clearinghouse
- Metadata Online Registry (METEOR)
- Regional Insights for Indigenous Communities
- Help & tools
- Increase text size
- Decrease text size

Cancer data in Australia
Australian Institute of Health and Welfare (2024) Cancer data in Australia , AIHW, Australian Government, accessed 17 August 2024.
Australian Institute of Health and Welfare. (2024). Cancer data in Australia. Retrieved from https://www.aihw.gov.au/reports/cancer/cancer-data-in-australia
Cancer data in Australia. Australian Institute of Health and Welfare, 15 August 2024, https://www.aihw.gov.au/reports/cancer/cancer-data-in-australia
Australian Institute of Health and Welfare. Cancer data in Australia [Internet]. Canberra: Australian Institute of Health and Welfare, 2024 [cited 2024 Aug. 17]. Available from: https://www.aihw.gov.au/reports/cancer/cancer-data-in-australia
Australian Institute of Health and Welfare (AIHW) 2024, Cancer data in Australia , viewed 17 August 2024, https://www.aihw.gov.au/reports/cancer/cancer-data-in-australia
Get citations as an Endnote file : Endnote
PDF | 7.2Mb
Overview of cancer in Australia, 2024
The following provides a brief summary of some notable trends in the latest cancer data. More comprehensive data is available throughout the Cancer data in Australia report for the cancers summarised as well as many other cancers.
Please note that when survival rates are discussed in the summary that these are relative survival rates. Age-standardised incidence and mortality rates are standardised to the 2024 Australian population. All rates are age-standardised unless they are for specific age groups or are otherwise specified. All cancers combined incidence data excludes basal and squamous cell carcinomas of the skin. When discussing histology types, NOS is the abbreviation for ‘not otherwise specified’. The presence of NOS after a term generally indicates that a diagnosis is not as specific as it could theoretically be. For example, there are many kinds of adenocarcinoma but often the diagnosis is simply “adenocarcinoma”. This is referred to as “adenocarcinoma NOS”.
All cancers combined
The annual number of cancer cases diagnosed may surpass 200,000 by 2034.
In 2000, there were around 88,000 cases of cancer diagnosed in Australia. By 2024, it is estimated there will be around 169,000 cases of cancer diagnosed in Australia. An increase of around 93% over 24 years with the majority of the increase due to increases in population size and increasing numbers of people reaching older ages for which cancer rates are higher.
Had the cancer incidence rates from 2000 for the various age groups remained constant between 2000 and 2024 there would be around 158,000 cases of cancer diagnosed in Australia in 2024 – an increase of around 70,000 cases. This number is reflective of increases due to population size and the ageing population alone. The additional cases to arrive at the estimated 169,000 cases is indicative of the increase due to increasing cancer rates. Overall, around 86% of the estimated increase of cancer incidence between 2000 and 2024 is attributable to population increase and the ageing population alone.
By 2034, with increasing population and estimated increasing rates of cancer, it is estimated there will be around 209,000 cases of cancer diagnosed in Australia.
The age-adjusted cancer incidence rate increased from 582 cases per 100,000 people in 2000 to an estimated 624 cases per 100,000 people in 2024. Over the corresponding period, age-adjusted cancer mortality rates decreased from 255 deaths per 100,000 people to an estimated 194 deaths per 100,000 people (Figure 1). Increasing cancer survival rates increase the gap between incidence and mortality rates.
Figure 1: Age-standardised cancer incidence and mortality rates, persons, 2000–2024

- Rates are standardised to the 2024 Australian population.
- 2023 and 2024 are projections for mortality and 2021 to 2024 are projections for incidence.
Source: AIHW Australian Cancer Database 2020 and National Mortality Database
Cancer survival rates continue to increase
The 5-year survival for cancer in 1991–1995 was 55% and by 2016–2020, the rate had increased to 71%.
Even with decreasing mortality rates and increasing survival, the number of deaths from cancer has been increasing. In 2000, there were around 36,000 deaths from cancer and by 2024 the number of deaths from cancer is estimated to have increased by 45% to 53,000 people. Had mortality rates from 2000 not improved and remained constant, there would have been around 69,000 deaths from cancer in 2024.
Males remain more likely to be diagnosed with cancer
Males continue to be more likely to be diagnosed with cancer although the difference in age-adjusted incidence rates between males and females in 2024 is less than it was in 2000. In 2024, the age-adjusted cancer incidence rate for males is estimated to be 729 cases per 100,000 males and increased from 713 cases per 100,000 males in 2000. For the same period, the equivalent rate for females increased from 487 cases per 100,000 females to 534 cases per 100,000 females.
Age-adjusted cancer mortality rates for males and females have decreased between 2000 and 2024. The age-adjusted mortality rates for males decreased from 339 deaths per 100,000 males to an estimated 240 deaths per 100,000 males. The decrease in the age-adjusted mortality rate for females over the same period was 196 deaths per 100,000 females to 157 deaths per 100,000 females. Similar to cancer incidence, the difference in cancer mortality rates between males and females remains high in 2024 but is less than it was in 2000 (Figure 2).
Figure 2: Age-standardised cancer incidence and mortality rates, by sex, 2000–2024

- Prostate cancer incidence rates increased in the early 2000s before decreasing. The rate changes strongly influenced all cancers combined rates for males. More information about prostate cancer incidence is available in Cancer data commentary 9 .
Between 1991–1995 and 2016–2020, the 5-year survival rate for females increased from 59% to 73%. The corresponding survival rates for males improved from 51% to 70%. The greater improvements in survival for males and small increases in incidence rates leads to decreases in the gap between male and female mortality rates.
COVID-19 lockdown and the reduction of cancer cases
In 2020, the number of cases of cancer diagnosed decreased for the first time since 1996 with 147,500 cases diagnosed in 2020, compared with 148,800 cases diagnosed in 2019. This is different to the pattern from 2000 and 2019 where the number of cancer cases diagnosed increased, on average, 3,200 cases per year (Figure 3). The number of cases diagnosed in 2020 was less across the most common cancers, with decreases of around 1,000 cases for both colorectal cancer and melanoma of the skin. There was also a decrease of just over 500 for breast cancer and a very small increase for prostate cancer (89 cases) compared with prostate cancer increases of around 1,000 cases in previous years.
These decreases coincide with the onset of COVID-19 and associated restrictions and lockdowns. It is known that the Breastscreen Australia was closed for around a month and people were less willing to visit medical practitioners. At this stage it is not clear what impact this will have on cancer outcomes.
Figure 3: Cancer cases diagnosed, persons, 2000–2020

Source: AIHW Australian Cancer Database 2020
Cancer is becoming more commonly diagnosed in people in their 30s and 40s
Cancer occurs across all ages but is more common in older ages. To highlight the difference by age, cancer incidence rates for people under the age of ten is estimated to be 16 cases per 100,000 people in 2024 while for people in their eighties it is estimated to be around 2,800 cases per 100,000 people.
Cancer remains most common in older ages (in 2024 an estimated 88% of cancers diagnosed will occur in people aged 50 or more. However, cancer incidence rates for the young are increasing. This section focuses on cancer incidence of the populations aged 30 to 49. These age groups account for around 84% of the 20,000 cancer cases estimated to be diagnosed in the population under 50 in 2024.
Cancer incidence rates for people in their thirties and forties have been increasing. The age-specific rates for the respective age groups increased between 2000 to 2024 from 121 cases per 100,000 people to an estimated 141 cases per 100,000 people and from 280 to 323 cases per 100,000 people.
Cancers strongly contributing to cancer incidence rate increases for people in their thirties are colorectal cancer and thyroid cancer. Cancers strongly contributing to cancer incidence increases for the population in their forties are thyroid cancer, breast cancer, prostate cancer, colorectal cancer, and kidney cancer. Table 1 provides an overview of some of the cancers contributing to the increasing rates as well as the cancers that are more common within these age groups.
| Cancer type / group | People aged 30 to 39 | People aged 40 to 49 | ||||
|---|---|---|---|---|---|---|
| Rate in 2000 | Rate in 2024 | Change in rates | Rate in 2000 | Rate in 2024 | Change in rates | |
| Breast cancer | 22.1 | 23.0 | 0.9 | 76.6 | 85.6 | 9.0 |
| Cervical cancer | 5.5 | 8.0 | 2.5 | 5.6 | 8.5 | 2.9 |
| Colorectal cancer | 6.3 | 17.2 | 10.9 | 24.9 | 29.9 | 5.0 |
| Kidney cancer | 2.0 | 3.7 | 1.7 | 7.0 | 11.6 | 4.6 |
| Liver cancer | 0.3 | 0.5 | 0.2 | 2.1 | 2.4 | 0.3 |
| Lung cancer | 2.1 | 2.1 | 0.0 | 11.4 | 9.4 | -2.0 |
| Melanoma of the skin | 31.4 | 23.6 | -7.8 | 50.5 | 52.2 | 1.7 |
| Pancreatic cancer | 0.5 | 1.5 | 1.0 | 3.2 | 5.2 | 2.0 |
| Prostate cancer | 0.1 | 0.3 | 0.2 | 4.9 | 11.6 | 6.7 |
| Testicular cancer | 7.3 | 9.9 | 2.6 | 4.1 | 5.6 | 1.5 |
| Thyroid cancer | 7.0 | 16.8 | 9.8 | 9.6 | 20.8 | 11.2 |
| Uterine cancer | 1.2 | 2.9 | 1.7 | 5.3 | 8.3 | 3.0 |
| All cancers combined | 120.5 | 141.1 | 20.6 | 280.1 | 323.2 | 43.1 |
Source AIHW Australian Cancer Database 2020
Cancer mortality rates for people aged in their 30s are decreasing
Even though cancer incidence rates have been increasing, cancer mortality rates have been decreasing for people aged in their thirties and forties. For people in their forties age-specific mortality rates have been steadily decreasing between 2000 and 2024 (60 deaths per 100,000 people to an estimated 37 deaths per 100,000 people). The cancer mortality rate also decreased for people aged in their thirties over this time (18 deaths per 100,000 people to an estimated 12 deaths per 100,000 people).
The incidence rate increases for various cancers noted in Table 1 were not generally accompanied by corresponding mortality rate increases. The most notable exception was colorectal cancer for people in their thirties where the mortality rate increased by 1 death per 100,000 people (1.8 to an estimated 2.8 deaths per 100,000 people). The Cancer mortality by age data visualisation provides more information about the changing mortality rates of cancers for people in their thirties and forties.
Cancer accounts for around 3 of every 10 deaths in Australia
In 2024, it is estimated that cancer will be responsible for around 3 of every 10 deaths in Australia. The percentage has increased gradually from 17% in 1971 but has been relatively stable between 28% and 30% from the turn of the century.
The proportion of deaths from cancer varies considerably by age (Figure 4). In 2024, cancer is estimated to be responsible for around 45% of deaths in the population aged 60 to 69. The 0 to 9 age group has the smallest percentage of deaths from cancer and is estimated to be responsible for 5.5% of all deaths for the age group in 2024. In the 1970’s the proportion of deaths from cancer for this age group did not exceed 4%.
Figure 4: Percentage of deaths from cancer, by age group, 1971–2024

- 2023 and 2024 are projections.
Source: National Mortality Database
Prostate cancer
In 2024, prostate cancer is estimated to be the most commonly diagnosed cancer for males and for Australia overall. With an estimated 26,400 cases diagnosed in 2024, prostate cancer is estimated to account for 28% of the cancers to be diagnosed in males for the year.
Since 2000, prostate cancer incidence rates have been more volatile than any other cancer ( see Cancer commentary 9 ). Prostate cancer incidence projections have more uncertainty than other cancers but, if more recent prostate cancer incidence rates were to remain the same and occur in future years, there will be around 31,800 cases of prostate cancer diagnosed in 2034.
In 2020, over 96% of prostate cancers diagnosed were adenocarcinomas. The 5-year survival rate for this type of prostate cancer in 2016–2020 was 98% and strongly influenced the overall prostate cancer 5-year survival rates of 96% for the period.
While prostate cancer survival rates are high, exceptions exist such as neuroendocrine neoplasms. Between 2016 and 2020, around 0.1% of prostate cancers diagnosed were neuroendocrine neoplasms. The 5-year survival rates for these prostate cancers in 2016–2020 was 9.9%.
Prostate cancer mortality rates have been decreasing this century. Prostate cancer mortality rate reductions began in the early to mid-1990s, several years after the introduction of prostate specific antigen testing. In 1994, prostate cancer mortality rates were 62 deaths per 100,000 males. In 2024, it is estimated that prostate cancer mortality rates will be 33 deaths per 100,000 males.
While the mortality rates have been decreasing, the number of deaths from prostate cancer continue to rise (Figure 5). In 2000, there were around 2,700 deaths from prostate cancer and in 2024 it is estimated there will be around 3,900. Population growth in combination with an ageing population exceeds reductions in age-adjusted mortality rates to result in increasing numbers of deaths from prostate cancer.
Figure 5: Prostate cancer deaths and age-standardised mortality rate, 2000–2024

Breast cancer
Breast cancer is the most commonly diagnosed cancer for females in Australia.
It is estimated there will be around 21,000 breast cancer cases diagnosed in females in 2024. This is around 28% of the estimated cancers diagnosed in females. It is the second most commonly diagnosed cancer in Australia for persons aged 20 to 39 and 60 to 79, and the most commonly diagnosed cancer for persons aged 40 to 59.
Breast cancer incidence has increased from 134 cases per 100,000 females in 2000 to an estimated 149 cases per 100,000 females in 2024. A large portion of this increase occurred around 2013 when breast screening was expanded to include women aged 70 to 74.
Breast cancer 5-year survival improved from 79% in 1991–1995 to 92% in 2016–2020.
While survival rates for breast cancer overall are high, there is substantial variation in survival for different types of breast cancer. For females, carcinomas were the most common type of breast cancer accounting for 99% of all breast cancer cases in 2020. The main types of breast carcinoma were ductal carcinomas (84% of all breast cancer cases) followed by lobular carcinomas (13%). There are different types of ductal carcinomas which have varied survival rates. The most common type of ductal carcinoma, the infiltrating duct carcinoma (NOS) (74% of all breast cancers), had a 5-year survival of 93% in 2016–2020. For the same period, other less common ductal carcinomas had much lower 5-year survival rates (for example, inflammatory carcinomas (59%) and metaplastic carcinomas (75%)).
In 2024, it is estimated that nearly 3,300 females will die from breast cancer; in 2000, around 2,500 females died from breast cancer. Like many other cancers, the increasing number of deaths is attributable to increasing population size and the ageing population. Age-adjusted breast cancer mortality rates have been decreasing for females and were around 30 deaths per 100,000 females in 2000 compared to an estimated 22 deaths per 100,000 females in 2024.
Melanoma of the skin
Melanoma of the skin incidence rates have increased from 53 cases per 100,000 people in 2000 to an estimated 70 cases per 100,000 people in 2024. In 2024, it is estimated that 35% of melanoma of the skin cancer cases are diagnosed on the trunk of the body, 26% on the upper limbs (including shoulder), 18% on the lower limbs (including hip) and 7.7% on the scalp and neck.
The proportion of melanoma of the skin diagnosed by site varies by sex. For example, in 2024 it is estimated that 25% of melanoma of the skin cases are diagnosed on the lower limbs (including hip) for females while for males it is 13%. Conversely, the trunk accounts for 41% of the cases for males and 27% for females.
Melanoma of the skin incidence rates for females are estimated to be 56 cases per 100,000 females in 2024 while male rates are 86 cases per 100,000 males.
Melanoma of the skin incidence rates have been decreasing for people under 40 since the late-1990s. Incidence rates for people aged 40 to 49 ranged between 44 and 53 cases per 100,000 people since the mid-1990s. Rates for people aged 50 and over continue to rise, although there was a decrease in 2020 which was also the year where COVID-19 restrictions were in place.
The ‘Slip Slop Slap’ campaign was a very large skin cancer awareness and prevention campaign commencing from the early 1980s. In 2024, the population aged under 40 were born after or around the ‘Slip Slop Slap’ campaign and have spent their lives in an environment where skin cancer awareness has been greater. Skin cancer awareness and prevention advice continues today. While populations over 40 have increasing incidence rates, the rate increases are greater for the oldest populations who are likely to have spent more of their lives in times when there was less skin cancer awareness.
After many years of increasing, melanoma of the skin mortality age-adjusted rates peaked at 8.0 deaths per 100,000 people in 2013. In 2024, the estimated age-adjusted mortality rate is 4.9 deaths per 100,000 people. The reduction in mortality rates is accompanied by reductions in the number of deaths (1,625 deaths in 2013 and an estimated 1,340 in 2024).
Since 1996–2000, 5-year melanoma of the skin survival rates have been a little over 90%. The melanoma of the skin 5-year survival rate for 2016–2020 was 94% and is the highest rate recorded for melanoma of the skin.
Colorectal cancer
With around 15,500 cases estimated, colorectal cancer is estimated to be the fourth most commonly diagnosed cancer in Australia in 2024. At the beginning of the century, it was the most diagnosed cancer in Australia.
Since 2000, colorectal cancer incidence rates have decreased more than any other cancer. Age-standardised incidence rates peaked in 2001 at 86 cases per 100,000 people and is estimated to have decreased to an estimated age-standardised rate of 57 cases per 100,000 people in 2024.
Five-year survival for colorectal cancer increased from 56% in 1991–1995 to 71% in 2016–2020. Decreasing incidence combined with improvements in survival have led to reducing mortality rates. The age-standardised mortality rate for colorectal cancer decreased from 35 deaths per 100,000 people in 2000 to an estimated 19 deaths per 100,000 people in 2024.
Colorectal cancer is far more common in the older population than the young. In 2024, around 6.5% of colorectal cancers are estimated to be diagnosed in people aged under 40. In 2000, only around 2.2% of colorectal cancers were diagnosed in people aged under 40. The increasing proportion occurred because, while colorectal cancer is decreasing overall and for older populations, colorectal cancer incidence is increasing for the young.
Incidence rates for younger populations remain much lower than for older populations but the trends are very different. Age groups under 40 years old have seen increases in incidence rates of colorectal cancer, particularly since around 2005. Incidence rates for 40–49 year olds increased from 22 cases per 100,000 people in 2005 to an estimated 30 cases in 2024. Over the same period, incidence rates decreased from 201 cases per 100,000 people to 142 cases per 100,000 people for the population aged 50 and over.
Some portion of the increasing rates for the younger population is attributable to neuroendocrine neoplasms but increases also occur for adenocarcinomas in the 20–39 age group. The increase for neuroendocrine neoplasms more generally may be explained by various factors such as increasing incidence of this malignancy, improvements in imaging technologies, increased use of endoscopy and colonoscopy, increased awareness in clinical practice and the introduction of the 2010 World Health Organisation classification for neuroendocrine tumours (Wyld D et al. 2019).
Cancer survival rates are higher for younger populations than older. In 2016–2020, survival was 98% for 0–19 year olds, between 70–81% for age groups 20–39, 40–59 and 60–79 years old, and 61% for 80 years and older.
Colorectal cancer sites and types diagnosed differ by age. Some of these differences are discussed below but much more comprehensive information is available in the cancer by histology and cancer by subsite data visualisations and spreadsheets.
Colorectal cancer can originate in the broad areas of the colon, rectum or the rectosigmoid junction (which is the limit separating the sigmoid colon and the rectum). In 2024, it is estimated that most cases of colorectal cancer will be in the colon (71% of all colorectal cancer cases), followed by the rectum (22%) and lastly the rectosigmoid junction (7%). The appendix, which is part of the colon, is not a common site of colorectal cancer in the overall population (estimated 5.6% of cases in 2024). However, the majority of colorectal cancer cases in the youngest age groups are located in the appendix (estimated 97% of cases in 0–14 year olds and an estimated 88% of cases in 15–24 year olds in 2024).
The majority of colorectal cancers diagnosed were carcinomas (95% of all colorectal cancers in 2020). In the general population, the most common type of colorectal carcinoma diagnosed was adenocarcinomas (87%) followed by neuroendocrine neoplasms (5.5%). However, neuroendocrine neoplasms were very common in younger age groups accounting for 100% and 81% of colorectal cancer cases in 0–14 and 15–24 year olds respectively.
Colorectal survival outcomes differ by age and type. Figure 6 provides a small selection of these for 2016–2020. Adenocarcinomas had a 5-year survival of 73% in 2016–2020 while neuroendocrine neoplasms had 89% survival. However, the difference in survival for neuroendocrine neoplasms is partly due to greater proportions of cases of this cancer being in younger age groups, who tend to have higher survival than older age groups. More extensive statistics are available in the cancer by histology data visualisation and Excel data.
Figure 6: Colorectal cancer 5-year relative survival by specified histologies, by age group, 2016–2020

Source: AIHW Australian Cancer Database 2020
Lung cancer
With around 15,100 cases estimated, lung cancer is estimated to be the fifth most commonly diagnosed cancer in Australia in 2024. Of the 5 most common cancers in Australia, its survival rates are the lowest (5-year survival of 26% in 2016–2020 for lung cancer with colorectal cancer survival the next lowest at 71%).
While lung cancer is a low survival cancer, 5-year survival rates have improved over time. Survival increased from 9.7% in 1991–1995 to 21% in 2016–2020 for males and from 12% to 31% for females. Survival differs by age with 5-year survival at 94% for 20–24 year-olds, 76% for 25–29, 61% for 30–34, between 23% and 36% for age groups between 40 and 79, and only 9.1% for those aged 85 and over in 2016–2020.
Lung cancer age-standardised incidence rates have been fairly stable at 57 cases per 100,000 people in 2000 to an estimated 56 cases in 2024. National rates are however comprised of very different trends for males and females. Males have seen strong and enduring decreases from 84 cases per 100,000 males in 2000 to an estimated 61 cases per 100,000 males in 2024. In contrast, females have seen an increase from 36 cases per 100,000 females in 2000 to an estimated 52 cases per 100,000 females in 2024.
The increasing incidence rates of this low survival cancer have seen lung cancer account for increasing proportions of cancer deaths for females. In 2000, lung cancer accounted for around 15% of cancer deaths in females and is estimated to be 17% in 2024. Conversely, lung cancer represented 22% of all cancer deaths for males in 2000 and this is estimated to reduce to 17% in 2024.
In 2024, it is estimated that around 8,900 people will die of lung cancer in Australia. This is the most common cause of cancer-related death. Age-standardised mortality rates for males have decreased substantially from 74 deaths per 100,000 males in 2000 to an estimated 39 deaths per 100,000 males in 2024. Female lung cancer mortality rates remain lower than males, but in contrast to males have increased from 29 deaths per 100,000 females in 2000 to a peak of 32 deaths per 100,000 females in 2010 before decreasing to an estimated 28 deaths per 100,000 females in 2024.
Blood cancers
All blood cancers combined is the aggregate of many different types of blood cancer. While useful for detailing the overall number of cases and general survival of these cancers in Australia, different types of blood cancer often have different incidence and mortality trends and survival rates.
In 2024, it is estimated that around 20,000 people will be diagnosed with a blood cancer (59% in males). The most common type of blood cancer in 2024 is estimated to be non-Hodgkin lymphoma followed by multiple myeloma and then chronic lymphocytic leukaemia.
Blood cancers accounted for an estimated 12% of all cancer cases in 2024. However, blood cancers are relatively more common in the 0–19 year old age group accounting for an estimated 40% of all cancer cases. While not a common cancer in the general population, acute lymphoblastic leukaemia was the most common cancer diagnosed in 0–19 year olds (estimated 17% of cancer cases in 2024).
Age-standardised incidence rates for blood cancer increased from 66 cases per 100,000 people in 2003 to an estimated 74 cases in 2024. Males have had consistently higher rates of all blood cancers combined than females (estimated 92 compared to 58 cases per 100,000 males and females respectively in 2024).
Five-year survival for blood cancers increased slightly from 67% in 2011–2015 to 70% in 2016–2020. In 2016–2020, 5-year survival was over 90% for age groups 0–19 and 20–39, and then decreased with increasing age from 85% in 40–59 year olds to 70% in 60–79 year olds to 44% for those aged 80 years older. There is substantial variation in survival between different types of blood cancer. Blood cancers with comparatively higher 5-year survival in 2016–2020 were immunoproliferative cancers (92%), Hodgkin lymphoma (89%), and chronic lymphocytic leukaemia (87%). Lower survival blood cancers included acute myeloid leukaemia (27%) and myelodysplastic syndromes (39%).
Age-standardised blood cancer mortality decreased from 30 deaths per 100,000 people in 2000 to an estimated 23 deaths in 2024. This decrease was seen in both males and females although males had consistently higher mortality rates.
The Cancer data in Australia report contains finer details of blood cancer incidence and survival rates. For example, Hodgkin lymphoma incidence and survival statistics are accompanied by statistics on types of Hodgkin lymphoma such as nodular lymphocyte predominant Hodgkin, classic Hodgkin lymphoma and the subtypes nodular sclerosis classic Hodgkin lymphoma, lymphocyte-rich classic Hodgkin lymphoma, mixed cellularity classic Hodgkin lymphoma and lymphocyte-depleted classic Hodgkin lymphoma. The Blood cancer by histology data visualisations provide more detailed blood cancer statistics.
Gynaecological cancers
Gynaecological cancers include cervical cancer, ovarian cancer, placenta cancer, uterine cancer, vaginal cancer, vulvar cancer, and cancer of other female genital organs. Gynaecological cancer is estimated to account for around 9.2% of cancers diagnosed in females in 2024 and around 9.7% of female deaths from cancer.
In the following paragraphs, ovarian cancer and serous carcinomas of the fallopian tube are discussed rather than ovarian cancer. This is because the time series for this cancer appears to better reflect ovarian cancer as it is more traditionally understood while ovarian cancer trends are complicated by the changed understanding of where many serous carcinomas originate ( see Cancer data commentary 5 for more information ).
Gynaecological cancer age adjusted incidence rates ranged between 49 and 53 cases per 100,000 females between 1982 and 1994 before decreasing to a low of 44 cases per 100,000 females in 2003. Decreases in cervical cancer incidence drove the reduction where rates decreased from 14 to 7.7 cases per 100,000 females between 1994 and 2003. The National Cervical Cancer Screening program was introduced in 1991 and led to falls in cervical cancer incidence and mortality due to the program’s ability to detect pre-cancerous abnormalities that may, if left, progress to cancer.
Since 2003, gynaecological cancer incidence has gradually increased to an estimated 49 cases per 100,000 females in 2024. Uterine cancer has largely influenced this change and increased from 20 to an estimated 24 cases per 100,000 females between 2003 and 2024. Uterine cancer incidence had been increasing before this time and has been steadily and gradually increasing since 1989 (16 cases per 100,000 females).
Five-year survival for gynaecological cancers has improved from 64% in 1991–1995 to 71% in 2016–2020. There is substantial variation in survival between different types of gynaecological cancers. The gynaecological cancers with the highest survival in 2016–2020 were placenta (90%), and uterine (82%). Lower survival gynaecological cancers include ovarian cancer and serous carcinomas of the fallopian tube (49%) and vaginal cancer (54%). Ovarian cancer and serous carcinomas of the fallopian tube 5-year survival rates have been improving over time, increasing from 40% in 1991–1995.
The mortality rate for gynaecological cancer has changed from 17 deaths per 100,000 females in 2000 to an estimated 16 deaths in 2024. Mortality rates for cervical cancer decreased from 3.1 deaths per 100,000 females in 2000 to an estimated 1.7 deaths in 2024. Mortality for uterine cancer increased from 3.3 deaths per 100,000 females in 2000 to an estimated 4.8 deaths in 2024.
In 2024, ovarian cancer and serous carcinomas of the fallopian tube are estimated to account for around 26% of the gynaecological cancers diagnosed. With survival lower than other gynaecological cancers, and an estimated 1,070 deaths in 2024, ovarian cancer and serous carcinomas of the fallopian tube are estimated to account for 48% of the 2,240 deaths from gynaecological cancer in 2024.
Brain cancer
Brain cancer age-adjusted incidence rates from 2000 to 2024 ranged between 7.4 and 8.5 cases per 100,000 people. Males had higher incidence rates than females throughout this period. In 2024, the incidence rate for males is estimated to be 9.2 cases per 100,000 males and the rate for females is estimated to be 5.7 cases per 100,000 females.
Survival vastly differs by age; in 2016–2020, 5-year survival for brain cancer was 63% for 0–19 year olds, 69% for 20–39 year olds, 28% for 40–59 year olds, 8.7% for 60–79 year olds and 1.9% for people aged 80 years and over.
Overall, brain cancer survival has improved from 20% in 1991–1995 to 23% in 2016–2020. Brain cancer survival rates over time are often impacted by changes in the age composition of those diagnosed with brain cancer. In particular, greater proportions of older people are diagnosed and older people have lower survival rates. When adjusted for age, brain cancer 5-year survival has more than doubled from 11% in 1991–1995 to 23% in 2016–2020.
The mortality rate for brain cancer ranged from 5.9 to 7.0 deaths per 100,000 people between 2000 and 2024.
The most common types of brain cancer were gliomas, glioneuronal tumours and neuronal tumours, which accounted for 94% of brain cancers diagnosed in 2020. Embryonal tumours only accounted for 2.8% of brain cancers in the general population but 37% of brain cancers in 0–19 year olds. Survival varies considerably for different types of brain cancer. Glioblastomas, IDH-wildtype accounted for 65% of all brain cancers in 2020 and had a 5-year relative survival of only 5.9% in 2016–2020. Oligodendroglioma, IDH-mutant and 1p/19q-codeleted accounted for 5.7% of brain cancer cases and had 84% 5-year survival.
Figure 7: Brain cancer incidence, selected types, persons, 2020

Thyroid cancer
Thyroid cancer is a common cancer, with much higher rates in females. In 2024, it is estimated that around 4,300 cases will be diagnosed, approximately 70% of which will be in females.
The age-adjusted incidence of thyroid cancer increased from 8.5 cases per 100,000 females in 2000 to an estimated 22 cases per 100,000 females in 2024. While lower, the incidence rates for males have also increased from 3.3 cases to an estimated 10.0 cases per 100,000 males over the same period. The increase in thyroid cancer may be due to an increase in medical surveillance and the introduction of new diagnostic techniques such as neck ultrasonography (Vaccarella et al. 2016).
While thyroid cancer is common, it is a high survival cancer resulting in relatively few deaths. Five-year survival is higher for females than males (98% and 94% in 2016–2020 respectively).
Despite an increase in the incidence rate, the age-adjusted mortality rate for thyroid cancer has been broadly stable since 2000, between 0.5 and 0.7 deaths per 100,000 people. However, males are overrepresented in deaths from thyroid cancer. While it is estimated that only around 30% of thyroid cancer cases in 2024 will be in males, around half of the deaths are estimated to be males (79 of the 155 deaths in 2024).
Rare cancers
Rare Cancers Australia and RARECARENet defines a cancer to be ‘rare’ if it has an incidence rate of less than 6 cases per 100,000 people per year. If the incidence rate is greater than or equal to 6 cases per 100,000 people per year but less than 12 cases per 100,000 people per year, the cancer is ‘less common’. ‘Common’ cancers are defined as those with an incidence rate of 12 or more cases per 100,000 people per year. Crude incidence rates are used to define cancer rarity in this report.
Cancers can change rarity over time. Cancers that changed from rare to less common between 2000 and 2024 were chronic lymphocytic leukaemia, liver cancer, multiple myeloma and oesophageal cancer. Cancers that changed from less common to common were bladder cancer, kidney cancer and pancreatic cancer. Thyroid cancer was the only cancer to go from rare to common between 2000 and 2024.
Rare cancers are individually rare, but collectively are estimated to account for 12% of cases diagnosed in 2024. Less common cancers accounted for around 12% of cancer cases in 2024 and common cancers for around 76% of cases. While rare and less common cancers are estimated to collectively account for 24% of cases, they are estimated to account for 33% of all cancer deaths in 2024 (Table 2).
| Type | Number of cases | Percent of all cancer cases | Number of deaths | Percent of all deaths |
|---|---|---|---|---|
| Rare cancers | 19,861 | 12% | 7,354 | 15% |
| Less common cancers | 20,371 | 12% | 8,701 | 18% |
| Common cancers | 126,425 | 76% | 32,269 | 67% |
- Rare cancers are those with incidence rates of less than 6 cases per 100,000 people. Less common cancers are those with incidence rates of at least 6 and less than 12 cases per 100,000 people. Common cancers are those with incidence rates of 12 or more cases per 100,000 people (with rarity based on estimated rates from 2024).
- Individual cancers were grouped based on rarity and the numbers of new cases were summed accordingly. Unknown primary site and cancer of other and ill-defined sites are excluded from cancer rarity classification.
- The sum of cancers by rarity for mortality will not equal all cancers combined estimated as stated from either the NMD or ACD as the individual cancers in the cancer rarity estimates were sourced from whichever of the NMD or ACD are recommended for use.
- Non-melanoma skin cancer rarity classification is derived from cancer incidence rates that exclude basal and squamous cell carcinomas of the skin. For consistency, non-melanoma skin cancer mortality also excludes basal and squamous cell carcinomas of the skin.
- The sum of cancers by rarity will not equal all cancers combined incidence totals from the ACD as the small number of bone cancers outside of C40-C41 ICD-10 coding are coded to bone cancer as well as the relevant ICD-10 site.
- Cancer incidence and mortality counts and proportions may change depending on the cancers included within analysis.
Cancer rarity classifications using the International Classification of Diseases – Tenth Revision (ICD-10)
Histology refers to the cells or soft tissue in which cancer originates. ICD-10 coding generally relates to the site of the body. The cancer by rarity information within this report understates the number of cancers classified as rare in Australia compared to if histology was used to classify rarity – at present ICD-10 is used. The following helps to illustrate how cancer rarity would change when using histology information.
Prostate cancer is a common cancer. Using the ICD-10 framework, all 23,350 prostate cancer cases in 2020 were counted as common cancers. However, there are different types of prostate cancer when considered by histology – these include acinar adenocarcinoma and adenocarcinoma (NOS), infiltrating duct carcinoma (NOS), small cell carcinoma and mixed acinar-ductal carcinoma and many other types. In 2020, around 22,000 of the 23,350 prostate cancers were acinar adenocarcinoma and adenocarcinomas (NOS) and these would remain as classified as common cancers in a histology framework for cancer rarity. Each of the other mentioned prostate cancers would be categorised as rare cancers.
The prostate cancers are different types and their outcomes differ but the ICD-10 considers these only as prostate cancer and a common cancer. If histology were used, there would be at least another 200 cases of prostate cancer categorised as rare cancers in 2020. Similarly, all other common and less common cancers such as breast cancer, lung cancer, liver cancer and so on, would likely see a portion of the cancer types by histology categorised as rare cancers.
Each year in the CdiA, the number of cancers sites reported by histology has been increasing. Once all sites have their histology structure mapped for reporting, it will be possible to consider cancer rarity reporting by histology within this report.
Rare Cancer Europe notes several of the specific challenges presented by rare cancers. These include:
- late or incorrect diagnosis
- lack of access to appropriate therapies and clinical expertise
- very limited number of clinical studies due to the small number of patients
- lack of interest in developing new therapies due to limitations in the market (RCE 2021).
Between 1987–1991 and 2016–2020, rare cancers in Australia have not recorded the same degree of improvement in survival outcomes as less common or common cancers. The 5-year survival for the common cancer group increased by around 22 percentage points, the less common cancer group increased by around 19 percentage points and rare cancers by around 13 percentage points (Table 3).
Cancers can change rarity classification over time. Please note that the survival by rarity for Table 3 represents the survival rates for rarity based on 1989 cancer rarity classifications.
Survival rates by rarity for 2016–2020 based on 2024 rarity would see rare cancers 5-year survival as 59%, less common cancers at 53% and common cancers as 77%. Future survival rates will be able to consider whether the rare cancers of today, overall, improve more slowly than more common cancers. Less common cancers continue to include a higher proportion of cancers with lower survival rates such as brain cancer and liver cancer.
| Type | Survival 1987–1991 | Survival 2016–2020 |
|---|---|---|
| Rare cancers | 50% | 63% |
| Less common cancers | 24% | 43% |
| Common cancers | 57% | 79% |
- Rare cancers are those with incidence rates of less than 6 cases per 100,000 people. Less common cancers are those with incidence rates of at least 6 and less than 12 cases per 100,000 people. Common cancers are those with incidence rates of 12 or more cases per 100,000 people.
- Rarity for this table used ICD-10 structure for cancers and 1987 rates to classify the rarity group for individual cancers.
- Non-melanoma skin cancer rarity classification is derived from cancer incidence rates that exclude basal and squamous cell carcinomas of the skin.
The following visualisation helps to understand cancer incidence by rarity over time. Caution is recommended interpreting the data as a time series. Changes in rates may be due to a cancer changing its rarity classification (for example, a rare cancer's rates increase and thereby becomes a less common cancer). The information does however illustrate that common cancers consistently represent the majority of cancers diagnosed in Australia. It also shows that while individually rare, rare cancers collectively consistently represent over 10% of the cancers diagnosed in Australia.























IMAGES
COMMENTS
The series of meta-analysis presented in this thesis gives an unbiased opinion on rectal cancer management from its initial presentation to subsequent investigations and eventual treatment. The results therefore, offer a sound evidence base for researchers to continue investigating the best treatment options for rectal cancer patients.
Over 1.8 million new colorectal cancer (CRC) cases and 881000 deaths were estimated to occur in 2018, accounting for approximately 1 in 10 cancer cases and deaths. ... [105-108], but these topics are beyond the scope of this dissertation.
Impact of androgens on sexual function in women with rectal cancer - a prospective cohort study Svanström Röjvall A, Buchli C, Flöter Rådestad A, Martling A, Segelman J, J Sex Med. 2021 Aug;18(8):1374-1382. doi: 10.1016/j.jsxm.2021.05.018. Epub 2021 Jul 18.PMID: 34284953 IV. Impac t of radiotherapy on bone health in women with rectal cancer
In the past 40 years, the treatment of locally advanced rectal cancer has evolved with the addition of radiotherapy or chemoradiotherapy and providing (neo)adjuvant systemic chemotherapy to major surgery. However, recent trends have focused on improving our ability to risk-stratify patients and tailoring treatment to achieve the best oncologic outcome while limiting the impact on long-term ...
Colorectal cancer is the third most popular occurring cancer in men and the second most commonly occurring cancer in women. There were over 1.9 million new cases in 2020 [3,8]. Colorectal cancer is the second most common cause of death from cancer, estimated to be responsible for almost 935,000 cancer deaths .
Purpose: Bibliometric analysis highlights the key topics and studies which have led to the current understanding and treatment of a disease of interest. In this original article we analyze the 100 most cited manuscripts in the field of colorectal cancer (CRC). Materials and methods: The Thomson Reuters Web of Science database with the search terms 'colorectal cancer,' 'colorectal cancer ...
Introduction. Colorectal cancer is the third leading cancer worldwide and the second leading cause of cancer-related deaths with an estimated 1.8 million new cases per year and 881,000 deaths worldwide (1, 2).Surgical therapy remains the gold standard for rectal growths and the outcomes of surgical treatment for rectal pathologies primarily depend on the location and stage of the tumor, the ...
2 To my parents Stephanie and Carleton Lord (for doing all the childcare in the world), my husband Phil Pucher (for setting the competitive bar high, but also helping me with stat
Advanced-stage diagnosis and mortality from colorectal cancer before 50 years of age are increasing. This is not a detection-bias effect; it is a r … Colorectal cancer screening from 45 years of age: Thesis, antithesis and synthesis World J Gastroenterol. 2019 Jun 7;25(21) :2565-2580 ... Practice Guidelines as Topic*
These NCCN Clinical Practice Guidelines in Oncology provide recommendations for the management of rectal cancer, beginning with the clinical presentation of the patient to the primary care physician or gastroenterologist through diagnosis, pathologic staging, neoadjuvant treatment, surgical management, adjuvant treatment, surveillance, management of recurrent and metastatic disease, and ...
4. For patients with cT1-2N0 rectal cancer who may need an APR, neoadjuvant chemoradiation is conditionally recommended to improve the chance of sphincter preservation. 5. For patients with rectal cancer where radiation is indicated, RT should be performed preoperatively rather than postoperatively.
The authors of the OPRA trial 1 have reported on their work in neoadjuvant therapy for rectal cancer that incorporated modern practices of watch and wait into the treatment algorithm. The present study has used organ preservation as a secondary end point and compared induction and consolidation chemotherapy against historic controls of chemoradiation alone in a pick the winner design.
The thesis is based on four original research papers and two unpublished studies (additional results 1 and 2). ... Paper II Excessive collagen turnover products are released during colorectal cancer progression and elevated in serum from metastatic colorectal cancer patients. Stephanie N. Kehlet, Rebeca Sanz-Pamplona, Susanne Brix, Diana J ...
According to the burst analysis (Figure 2C), radiotherapy for rectal cancer was a hot topic in Europe, Japan, Korea, and Australia between 2000 and 2007. Between 2009 and 2012, research on radiotherapy for rectal cancer increased in popularity in Germany. Studies related to radiotherapy for rectal cancer have been accumulating in China since ...
6,808 Topic views. Locally advanced rectal cancer (LARC), defined as stage II (T3-4, node negative) or stage III (node positive) disease has experienced a paradigm shift in management over the past few decades. Advances in surgical technique, namely total mesorectal excision (TME) and the development of combined modality therapy, have led to ...
Lynch syndrome colorectal cancer tumors have many mutations, which may make them more susceptible to immunotherapies. A genetic feature known as microsatellite instability-high (MSI-H) is seen in about 15% of patients with stages II and III colorectal cancer and about 5% with stage IV. MSI-H means that there are mistakes in the way the DNA is ...
FGFR4 glycosylation and processing in cholangiocarcinoma promote cancer signaling, Andrew J. Phillips. Theses/Dissertations from 20202020. PDF. Cooperativity of CCNE1 and FOXM1 in High-Grade Serous Ovarian Cancer, Lucy Elge. PDF. Characterizing the critical role of metabolic and redox homeostasis in colorectal cancer, Danielle Frodyma. PDF.
Showing result 1 - 5 of 270 swedish dissertations containing the words thesis for colon cancer . 1. Risk and survival for colorectal cancer in northern Sweden : sociodemographic factors and surveillance programs. Abstract : BackgroundColorectal cancer (CRC) - i.e., cancer in the colon or rectum - is one of the most common cancers both ...
Colorectal cancer screening is becoming a hot topic of discussion after the proposal of a local pilot screening program of colorectal cancer in the Policy Address 2014. Colorectal screening is traditionally performed by faecal occult blood test and optical colonoscopy.
List of dissertations / theses on the topic 'Colon and Rectal Cancer'. Scholarly publications with full text pdf download. Related research topic ideas. Bibliography; Subscribe; ... To see the other types of publications on this topic, follow the link: Colon and Rectal Cancer. Author: Grafiati. Published: 4 June 2021 Last updated: 1 February 2022
Dissertations / Theses on the topic 'Colon rectal cancer' To see the other types of publications on this topic, follow the link: Colon rectal cancer. Author: Grafiati. Published: 4 June 2021 Last updated: 6 February 2022 Create a spot-on reference in APA, MLA, Chicago, Harvard, and other styles ...
The researchers analyzed the whole genomes and transcriptomes of 1,063 primary colorectal cancers within a population-based cohort, with 94% of the patients completing a five-year clinical follow-up.
Radiation induced secondary cancer is an entity that has been well described in the literature. We report a case of a rectal adenocarcinoma occurring in a woman previously treated by radiotherapy and brachytherapy for a squamous cell carcinoma of the cervix. Keywords: Rectal cancer, cervical cancer, radiation induced cancer, secondary cancer.
It is included in national colorectal cancer screening guidelines by the American Cancer Society (2018) 1 and the U.S. Preventive Services Task Force (2021) 2. The Cologuard test revolutionized colorectal cancer screening by providing a best-in-class, noninvasive testing option for those at average risk.
(SACRAMENTO) The American College of Surgeons (ACS) and the National Accreditation Program for Rectal Cancer (NAPRC) has designated the colorectal surgery program at UC Davis Health a Surgical Quality Partner. The award is given to programs that excel in quality of care, preventing complications, saving lives and reducing costs "UC Davis Health was one of the first institutions in the country ...
Dissertations / Theses on the topic 'Long-Term Rectal Cancer Survivors' To see the other types of publications on this topic, follow the link: Long-Term Rectal Cancer Survivors. Author: Grafiati. Published: 4 June 2021 Last updated: 9 February 2022 Create a spot-on reference in APA, MLA, Chicago, Harvard, and other styles ...
Listen to a soundcast of the June 13, 2024, and June 21, 2024, Augtyro (repotrectinib) for NTRK gene fusion-positive solid tumors and Krazati (adagrasib) for KRAS G12C-mutated colorectal cancer.
Network analysis of metabolomic-microbiome correlations of eoCRC vs. aoCRC. Credit: npj Precision Oncology (2024). DOI: 10.1038/s41698-024-00647-1
Colorectal cancer. With around 15,500 cases estimated, colorectal cancer is estimated to be the fourth most commonly diagnosed cancer in Australia in 2024. At the beginning of the century, it was the most diagnosed cancer in Australia. Since 2000, colorectal cancer incidence rates have decreased more than any other cancer.
Offering self-sampling kits to women overdue for cervical cancer (CC) or colorectal cancer (CRC) screening when they attend breast cancer (BC) screening can result in increased screening ...