- skip to Cookie Notice
- skip to Main Navigation
- skip to Main Content
- skip to Footer
- Find a Doctor
- Find a Location
- Appointments & Referrals
- Patient Gateway
- Español
- Leadership Team
- Quality & Safety
- Equity & Inclusion
- Community Health
- Education & Training
- Centers & Departments
- Browse Treatments
- Browse Conditions A-Z
- View All Centers & Departments
- Clinical Trials
- Cancer Clinical Trials
- Cancer Center
- Digestive Healthcare Center
- Heart Center
- Mass General for Children
- Neuroscience
- Orthopaedic Surgery
- Information for Visitors
- Maps & Directions
- Parking & Shuttles
- Services & Amenities
- Accessibility
- Visiting Boston
- International Patients
- Medical Records
- Billing, Insurance & Financial Assistance
- Privacy & Security
- Patient Experience
- Explore Our Laboratories
- Industry Collaborations
- Research & Innovation News
- About the Research Institute
- Innovation Programs
- Education & Community Outreach
- Support Our Research
- Find a Researcher
- News & Events
- Ways to Give
- Patient Rights & Advocacy
- Website Terms of Use
- Apollo (Intranet)

Plastic & Reconstructive Surgery
- Like us on Facebook
- Follow us on Twitter
- See us on LinkedIn
- Print this page
Transgender Surgical Program
- 617-726-3525
Contact Information
Phone: 617-726-3525 Fax: 617-724-7126
Email: [email protected]
Explore This Treatment
About gender-affirming surgery at mass general.
Specialists in the Transgender Health Program and Transgender Surgical Program at Massachusetts General Hospital are dedicated to ensuring a welcoming and affirming environment for all patients. We offer patients a wide spectrum of gender-affirming services to support them throughout their entire care journey, including comprehensive primary care, surgical treatment, hormone management, case management and behavioral health support.
The Transgender Surgical Program is a collaboration with specialists from the Mass General Division of Plastic and Reconstructive Surgery , the Department of Urology and the Department of Obstetrics and Gynecology . Our multidisciplinary surgical team works closely with providers from the Transgender Health Program and every patient to develop a safe and all-inclusive surgical plan that aligns with the patient’s personal goals.
Gender-Affirming Surgical Procedures
Our expert team performs a variety of highly specialized gender-affirming surgical procedures tailored to meet the needs of transgender and gender-nonconforming patients.
- Vaginoplasty , sometimes referred to as bottom surgery, is a surgery that is used to create a vulva, labia, and vaginal canal
- Orchiectomy , also known as testicle removal surgery and/or bottom surgery, is a procedure in which the testicles are surgically removed
- Hysterectomy and/or oophorectomy is a surgery that involves the removal of the uterus and, in some case, the ovaries
- Phalloplasty , sometimes referred to as bottom surgery, is surgery to create a penis. It can include a variety of different procedures, depending on individual goals
- Mastectomy , sometimes referred to as top surgery, is a surgery to remove breast tissue from the chest
- Breast augmentation is surgery that uses implants made of silicone or saline to enhance the size of a person’s natural breasts
- Facial feminization or masculinization is surgery to alter facial features—the chin, nose, cheeks, forehead, etc.—to create a more feminine or masculine facial structure
- Voice feminization surgery is a procedure that alters the pitch and quality of an individual's voice to align it with a more feminine sound though surgery that involves lengthening the vocal cords or adjusting the tension of the vocal cords. Before undergoing surgical intervention, patients will work with a speech therapist specializing in voice feminization
- Voice masculinization surgery is a procedure that alters the pitch and quality of an individual's voice to align it with a more masculine sound though surgery to decrease the tension of the vocal cords. In addition to surgery, some individuals may benefit from speech therapy to further refine their vocal skills and communication. This procedure is not common, as only 75% of people can masculinize their voice with hormone therapy
Frequently Asked Questions About Gender-Affirming Surgery
For genital or “bottom” surgery, the first step is to schedule an initial visit with the Transgender Health Program. To schedule this appointment, call 617-726-3525 or email us . For breast or “top” surgery, you are not required to schedule an intake visit with the Transgender Health Program, unless you need a referral for support services. Instead, please contact the Transgender Surgery Program team at 617-726-3525 to learn how to proceed with a surgical consult. Providers should fax referrals to 617-724-7126.
Following confirmation from the Transgender Health Program that you are ready to move forward with bottom surgery, the Transgender Surgery Program team will contact you to set up a surgical consult.
Fertility preservation offers the opportunity to freeze eggs or sperm to be used for building a family in the future. This can be done prior to initiation of gender affirming hormone therapy or surgery. For some, it can also be used after hormonal therapy has already been started. Resources and care are also available for coordinating use of eggs or sperm from another person (donor) or for another individual to carry a pregnancy (gestational carrier).
Patients who desire fertility preservation or family building through Mass General must:
- Complete a consultation with the Mass General Fertility Center
- Be of reproductive age (requirements vary by family building plan)
- Follow center-specific guidance and protocols for selected treatment
During your surgical consultation, your physician will ask you about your fertility preservation goals and will assist you with setting up a consultation with a fertility specialist. We are committed to supporting you and guiding you through this process.
Required documents prior to gender-affirming surgery vary depending on the type of procedure. Our surgical program coordinator will assist you with questions and provide you with more information during your surgical consult.
Once we’ve scheduled a date for your surgery, we will submit a prior authorization for surgery to your insurance company for approval. Some out-of-network insurances may require you to obtain prior authorization for surgical consultations. Please reach out to your insurance company to determine what is required. Our dedicated surgical coordinator is happy to assist you with this process.
There are medical rates at many of the surrounding local hospitals. Depending on the procedure, you may need to remain local for a few weeks. If you are interested in medical rates, our dedicated surgical coordinator will be happy to provide you with more information.
Patient Stories
Patients who underwent gender-affirming surgery at Mass General share their experiences.
Finally, Herself: Elise’s Journey to Gender-Affirming Surgery
When Elise first heard of gender-affirming surgery, it seemed next to impossible in her situation. After a few years filled with research and conversations about her gender identity, what seemed impossible became achievable. She sought care with the Mass General Transgender Health Program team.

Tanner Chose Mass General for Gender-Affirming Care
"I wouldn’t have been able to do it if I didn’t have my team by my side every step of the way. I went from worrying, to feeling grateful," Tanner Bonanza, gender-affirming surgical patient.

Meet Our Team
The Mass General Transgender Surgical Program and the Transgender Health Program form a multidisciplinary and collaborative team of providers and staff who work together to provide gender-affirming care for all patients.

Jay Austen, MD
- Chief, Plastic and Reconstructive Surgery
- Chief, Division of Burn Surgery
- Interim Chief of the Department of Oral & Maxillofacial Surgery

Branko Bojovic, MD
- Plastic and Reconstructive Surgery
- Department of Surgery

Katherine Carruthers, MD, MS
- Attending Surgeon, Massachusetts General Hospital

Beth Drzewiecki, MD
- Pediatric Urology, MassGeneral Hospital for Children

Rich Ehrlichman, MD
- Assistant Professor of Surgery, Harvard Medical School
- Assistant Surgeon, Massachusetts General Hospital

Ariel Frey-Vogel, MD, MAT
- Primary Care
- Department of Medicine
- Department of Pediatrics

Youngwu Kim, MD
- Urogynecologist
- Urogynecology and Reconstructive Pelvic Surgeon

Jenny Siegel, MD

Eleanor Tomczyk, MD

Milena Weinstein, MD
- Chief of Urogynecology and Reconstructive Pelvic Surgery (URPS)
- Co-chair, Center for Pelvic Floor Disorders
- Director of Research, Urogynecology and Reconstructive Pelvic Surgery Fellowship

Jonathan Winograd, MD
- Associate Visiting Surgeon, Massachusetts General Hospital
- Associate Professor, Harvard Medical School
Telehealth at Mass General
Virtual visits allow you to conveniently meet with your provider from home—either online (over your computer or device) or by phone.
A Top Hospital in America
Mass General is recognized as a top hospital on the U.S. News Best Hospitals Honor Roll for 2024-2025.
If you would like to request an appointment with or refer a patient to the Division of Plastic and Reconstructive Surgery, please use the following contact information.
Transgender Mastectomy (Top Surgery)

What Do our Patients Say ?
Dr.transman, let’s start your journey from here.
Our experience, our technologically-advanced facilities and our compassionate staff are the best in the business for transgender confirmation procedures, holistic therapy and the overall patient experience.

Gender-Affirming Surgery (Top Surgery)
Gender-affirming surgery is a collection of surgical procedures for adults ages 18 and older diagnosed with gender dysphoria. The operations are often referred to as “top surgery" and "bottom surgery.” Duke Health offers several top surgery options to transgender, gender-diverse, nonbinary, and gender-nonconforming adults who want their appearance to align with their internal identity. If, after a consultation with our doctors, you decide to pursue top surgery, we work toward a positive outcome that improves your physical, emotional, and psychological well-being.
What You Should Know About Gender-Affirming Surgery
Choosing to pursue gender-affirming surgery is an individual, personal decision. You’ll want to consider how it will change your quality of life and how it will help you achieve your goals.
Gender Dysphoria One important step is understanding how much you are affected by gender dysphoria, a diagnosis that the American Psychiatric Association defines as a conflict between your physical or assigned gender and the gender with which you identify.
Candidates for Top Surgery To be a candidate for top surgery, you must:
- Be 18 or older
- Be in good health without illness or a condition that can increase your risk of surgical complications
- Have a BMI under 35
- Provide a clearance letter from your mental health or primary care provider stating you have gender dysphoria and you have been living in your assigned gender for at least 12 months
Top Surgery Costs Some private insurance plans will cover transgender surgery when it is used to address a diagnosis of gender dysphoria. Check with your insurance plan to determine your coverage.
Understanding Which Top Surgery Is Right for You There are several approaches to transgender surgery. We will review these with you during your initial consultation and make a recommendation based on your physical exam and medical history.
You May Have Scars Your surgeon will use the natural contours of your breasts to minimize scarring as much as possible. In some cases, depending on your breast size and weight, a small bunching of tissue may result in scars known as “dog ears” following mastectomy. These can be corrected later with revision surgery.
Understand the Risks Top surgery carries the same risks as other standard surgeries. These include the risk of bleeding and infection and risks associated with general anesthesia. Your doctor will discuss these risks with you if surgery is recommended.
Initial Consultation and Tests
Consultation and Exam Your first step will be an in-person consultation. Our providers spend time meeting with you, evaluating your anatomy, answering your questions, and determining if this surgery will help you achieve your goals.
Your surgeon will review your family history, general health status, lifestyle habits such as smoking, previous operations, any medications you may be taking, and conditions that can put you at risk for surgery.
Measurements, Photographs, Tests Your breasts will be measured and assessed for size and shape, and photographs may be taken for your medical record. Before treatment is recommended, you will also undergo one or more of the following tests.
- Blood tests may be necessary to evaluate your hormone levels. Pre-surgical testing also requires several blood tests to assess your liver and kidney function and to determine if you have a previously undetected infection, blood disorder, or anemia.
- A mammogram may be performed to look for any underlying breast abnormalities. Additional imaging, including ultrasound and MRI, may also be requested.
Recommending Treatment Based on these findings, your surgeon will recommend an approach to surgery. She will discuss the expected outcome, potential risks and complications, and your post-operation recovery. Alternatively, your surgeon may recommend that you lose weight, quit smoking, or discontinue medication before surgery to ensure you experience the best possible outcome.
If You Take Hormone Therapy Some gender-affirming hormone therapy , such as testosterone, can be continued if you pursue transgender surgery. Others, such as anti-estrogen therapy, may be stopped. Your surgeon will explain what you need to do to prepare for surgery.
Top Surgeries
Chest reconstruction - mastectomy, breast reduction.
We use different approaches to remove breast tissue and contour breasts to appear more masculine. The right approach depends on your anatomy and the size of your breasts. Techniques for medium to large breasts include nipple-sparing, double incision, buttonhole, and inverted-T incision. Keyhole and peri-areolar techniques may be used for smaller breasts or for those with good skin elasticity. Your surgeon will discuss your options with you after your physical exam and consultation.
Breast Augmentation
There are also many different approaches to breast augmentation, including the use of implants and fat grafting. We can also combine breast augmentation with body contouring, liposuction, and neurotoxin injections such as Botox injections and dermal fillers.
The Procedure Length
On average, top surgery takes about two to three hours and is performed under general anesthesia in an outpatient ambulatory surgery center. In some case, an overnight stay may be required. Sometimes a second procedure is needed to further tighten skin and achieve optimal cosmetic results.
Your chest will be wrapped in bandages, and a compression chest vest or surgical bra will be worn after the procedure. Drains will be required after mastectomy but not after breast augmentation. Initial recovery takes about one week. It may take three to six months for all swelling to subside and scars to fade.
Duke University Hospital is proud of our team and the exceptional care they provide. They are why we are once again recognized as the best hospital in North Carolina, and nationally ranked in 11 adult and 10 pediatric specialties by U.S. News & World Report for 2024–2025.
Why Choose Duke
You'll Work With a Plastic Surgeon Experienced in Gender Affirmation Surgery Our plastic surgeon has worked with many individuals seeking gender confirmation surgery. She is fellowship trained in body contouring, which means she has completed additional training in procedures that improve the body shape. Our surgeon is also a member of the World Professional Association for Transgender Health (WPATH), a nonprofit organization working to standardize and improve transgender care.
Duke Health Is Committed to the LGBTQ+ Community Duke Health values diversity and has taken many steps to show its commitment to eliminating discrimination, promoting equality, and standing beside our lesbian, gay, bisexual, transgender, and queer (LGBTQ+) community. Duke University Hospital, Duke Regional Hospital, and Duke Raleigh Hospital are recognized as LGBTQ+ Healthcare Equality Leaders by the Human Rights Campaign Foundation for perfect scores across areas of patient-centered care, support services, and inclusive health insurance policies for LGBTQ+ patients.
Related Care
- Gender-Affirming Hormone Therapy
- Patient Care & Health Information
- Tests & Procedures
- Feminizing surgery
Feminizing surgery, also called gender-affirming surgery or gender-confirmation surgery, involves procedures that help better align the body with a person's gender identity. Feminizing surgery includes several options, such as top surgery to increase the size of the breasts. That procedure also is called breast augmentation. Bottom surgery can involve removal of the testicles, or removal of the testicles and penis and the creation of a vagina, labia and clitoris. Facial procedures or body-contouring procedures can be used as well.
Not everybody chooses to have feminizing surgery. These surgeries can be expensive, carry risks and complications, and involve follow-up medical care and procedures. Certain surgeries change fertility and sexual sensations. They also may change how you feel about your body.
Your health care team can talk with you about your options and help you weigh the risks and benefits.
Products & Services
- A Book: Mayo Clinic Family Health Book
- Available Sexual Health Solutions at Mayo Clinic Store
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Why it's done
Many people seek feminizing surgery as a step in the process of treating discomfort or distress because their gender identity differs from their sex assigned at birth. The medical term for this is gender dysphoria.
For some people, having feminizing surgery feels like a natural step. It's important to their sense of self. Others choose not to have surgery. All people relate to their bodies differently and should make individual choices that best suit their needs.
Feminizing surgery may include:
- Removal of the testicles alone. This is called orchiectomy.
- Removal of the penis, called penectomy.
- Removal of the testicles.
- Creation of a vagina, called vaginoplasty.
- Creation of a clitoris, called clitoroplasty.
- Creation of labia, called labioplasty.
- Breast surgery. Surgery to increase breast size is called top surgery or breast augmentation. It can be done through implants, the placement of tissue expanders under breast tissue, or the transplantation of fat from other parts of the body into the breast.
- Plastic surgery on the face. This is called facial feminization surgery. It involves plastic surgery techniques in which the jaw, chin, cheeks, forehead, nose, and areas surrounding the eyes, ears or lips are changed to create a more feminine appearance.
- Tummy tuck, called abdominoplasty.
- Buttock lift, called gluteal augmentation.
- Liposuction, a surgical procedure that uses a suction technique to remove fat from specific areas of the body.
- Voice feminizing therapy and surgery. These are techniques used to raise voice pitch.
- Tracheal shave. This surgery reduces the thyroid cartilage, also called the Adam's apple.
- Scalp hair transplant. This procedure removes hair follicles from the back and side of the head and transplants them to balding areas.
- Hair removal. A laser can be used to remove unwanted hair. Another option is electrolysis, a procedure that involves inserting a tiny needle into each hair follicle. The needle emits a pulse of electric current that damages and eventually destroys the follicle.
Your health care provider might advise against these surgeries if you have:
- Significant medical conditions that haven't been addressed.
- Behavioral health conditions that haven't been addressed.
- Any condition that limits your ability to give your informed consent.
Like any other type of major surgery, many types of feminizing surgery pose a risk of bleeding, infection and a reaction to anesthesia. Other complications might include:
- Delayed wound healing
- Fluid buildup beneath the skin, called seroma
- Bruising, also called hematoma
- Changes in skin sensation such as pain that doesn't go away, tingling, reduced sensation or numbness
- Damaged or dead body tissue — a condition known as tissue necrosis — such as in the vagina or labia
- A blood clot in a deep vein, called deep vein thrombosis, or a blood clot in the lung, called pulmonary embolism
- Development of an irregular connection between two body parts, called a fistula, such as between the bladder or bowel into the vagina
- Urinary problems, such as incontinence
- Pelvic floor problems
- Permanent scarring
- Loss of sexual pleasure or function
- Worsening of a behavioral health problem
Certain types of feminizing surgery may limit or end fertility. If you want to have biological children and you're having surgery that involves your reproductive organs, talk to your health care provider before surgery. You may be able to freeze sperm with a technique called sperm cryopreservation.
How you prepare
Before surgery, you meet with your surgeon. Work with a surgeon who is board certified and experienced in the procedures you want. Your surgeon talks with you about your options and the potential results. The surgeon also may provide information on details such as the type of anesthesia that will be used during surgery and the kind of follow-up care that you may need.
Follow your health care team's directions on preparing for your procedures. This may include guidelines on eating and drinking. You may need to make changes in the medicine you take and stop using nicotine, including vaping, smoking and chewing tobacco.
Because feminizing surgery might cause physical changes that cannot be reversed, you must give informed consent after thoroughly discussing:
- Risks and benefits
- Alternatives to surgery
- Expectations and goals
- Social and legal implications
- Potential complications
- Impact on sexual function and fertility
Evaluation for surgery
Before surgery, a health care provider evaluates your health to address any medical conditions that might prevent you from having surgery or that could affect the procedure. This evaluation may be done by a provider with expertise in transgender medicine. The evaluation might include:
- A review of your personal and family medical history
- A physical exam
- A review of your vaccinations
- Screening tests for some conditions and diseases
- Identification and management, if needed, of tobacco use, drug use, alcohol use disorder, HIV or other sexually transmitted infections
- Discussion about birth control, fertility and sexual function
You also may have a behavioral health evaluation by a health care provider with expertise in transgender health. That evaluation might assess:
- Gender identity
- Gender dysphoria
- Mental health concerns
- Sexual health concerns
- The impact of gender identity at work, at school, at home and in social settings
- The role of social transitioning and hormone therapy before surgery
- Risky behaviors, such as substance use or use of unapproved hormone therapy or supplements
- Support from family, friends and caregivers
- Your goals and expectations of treatment
- Care planning and follow-up after surgery
Other considerations
Health insurance coverage for feminizing surgery varies widely. Before you have surgery, check with your insurance provider to see what will be covered.
Before surgery, you might consider talking to others who have had feminizing surgery. If you don't know someone, ask your health care provider about support groups in your area or online resources you can trust. People who have gone through the process may be able to help you set your expectations and offer a point of comparison for your own goals of the surgery.
What you can expect
Facial feminization surgery.
Facial feminization surgery may involve a range of procedures to change facial features, including:
- Moving the hairline to create a smaller forehead
- Enlarging the lips and cheekbones with implants
- Reshaping the jaw and chin
- Undergoing skin-tightening surgery after bone reduction
These surgeries are typically done on an outpatient basis, requiring no hospital stay. Recovery time for most of them is several weeks. Recovering from jaw procedures takes longer.
Tracheal shave
A tracheal shave minimizes the thyroid cartilage, also called the Adam's apple. During this procedure, a small cut is made under the chin, in the shadow of the neck or in a skin fold to conceal the scar. The surgeon then reduces and reshapes the cartilage. This is typically an outpatient procedure, requiring no hospital stay.
Top surgery
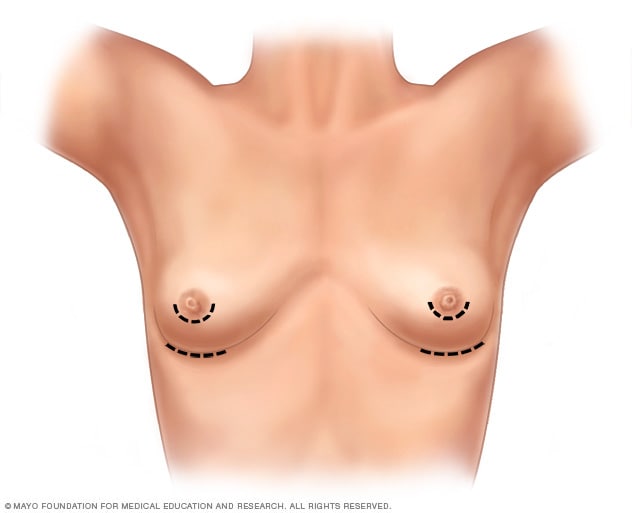
- Breast augmentation incisions
As part of top surgery, the surgeon makes cuts around the areola, near the armpit or in the crease under the breast.
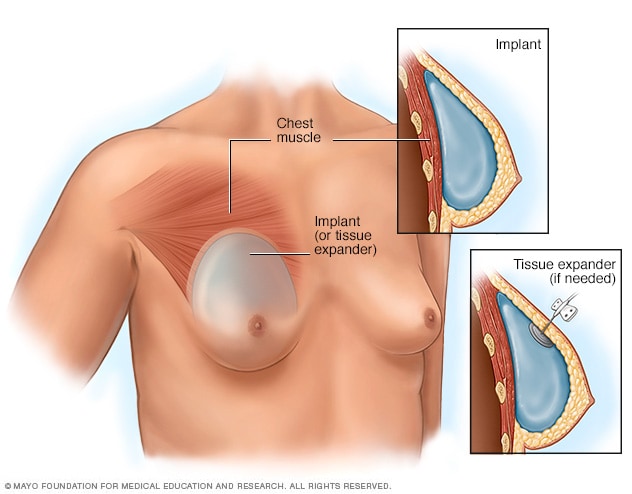
- Placement of breast implants or tissue expanders
During top surgery, the surgeon places the implants under the breast tissue. If feminizing hormones haven't made the breasts large enough, an initial surgery might be needed to have devices called tissue expanders placed in front of the chest muscles.
Hormone therapy with estrogen stimulates breast growth, but many people aren't satisfied with that growth alone. Top surgery is a surgical procedure to increase breast size that may involve implants, fat grafting or both.
During this surgery, a surgeon makes cuts around the areola, near the armpit or in the crease under the breast. Next, silicone or saline implants are placed under the breast tissue. Another option is to transplant fat, muscles or tissue from other parts of the body into the breasts.
If feminizing hormones haven't made the breasts large enough for top surgery, an initial surgery may be needed to place devices called tissue expanders in front of the chest muscles. After that surgery, visits to a health care provider are needed every few weeks to have a small amount of saline injected into the tissue expanders. This slowly stretches the chest skin and other tissues to make room for the implants. When the skin has been stretched enough, another surgery is done to remove the expanders and place the implants.
Genital surgery
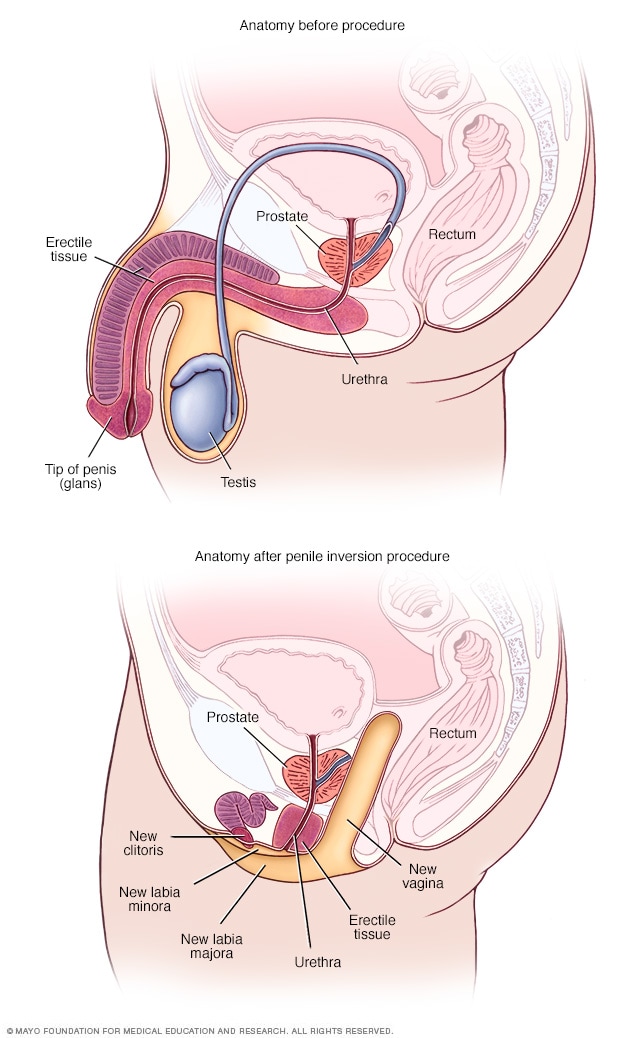
- Anatomy before and after penile inversion
During penile inversion, the surgeon makes a cut in the area between the rectum and the urethra and prostate. This forms a tunnel that becomes the new vagina. The surgeon lines the inside of the tunnel with skin from the scrotum, the penis or both. If there's not enough penile or scrotal skin, the surgeon might take skin from another area of the body and use it for the new vagina as well.
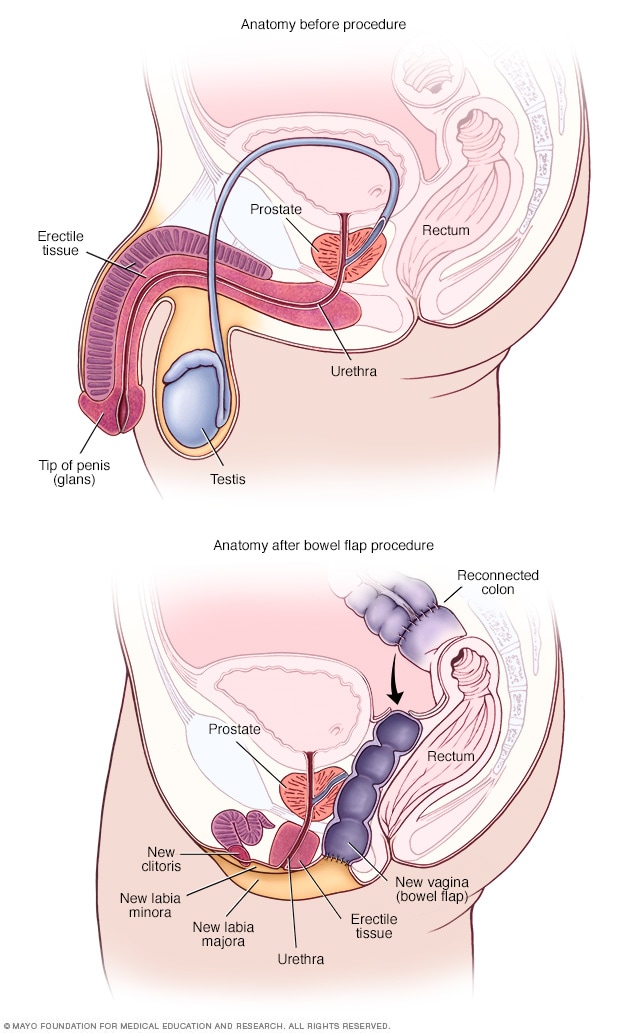
- Anatomy before and after bowel flap procedure
A bowel flap procedure might be done if there's not enough tissue or skin in the penis or scrotum. The surgeon moves a segment of the colon or small bowel to form a new vagina. That segment is called a bowel flap or conduit. The surgeon reconnects the remaining parts of the colon.
Orchiectomy
Orchiectomy is a surgery to remove the testicles. Because testicles produce sperm and the hormone testosterone, an orchiectomy might eliminate the need to use testosterone blockers. It also may lower the amount of estrogen needed to achieve and maintain the appearance you want.
This type of surgery is typically done on an outpatient basis. A local anesthetic may be used, so only the testicular area is numbed. Or the surgery may be done using general anesthesia. This means you are in a sleep-like state during the procedure.
To remove the testicles, a surgeon makes a cut in the scrotum and removes the testicles through the opening. Orchiectomy is typically done as part of the surgery for vaginoplasty. But some people prefer to have it done alone without other genital surgery.
Vaginoplasty
Vaginoplasty is the surgical creation of a vagina. During vaginoplasty, skin from the shaft of the penis and the scrotum is used to create a vaginal canal. This surgical approach is called penile inversion. In some techniques, the skin also is used to create the labia. That procedure is called labiaplasty. To surgically create a clitoris, the tip of the penis and the nerves that supply it are used. This procedure is called a clitoroplasty. In some cases, skin can be taken from another area of the body or tissue from the colon may be used to create the vagina. This approach is called a bowel flap procedure. During vaginoplasty, the testicles are removed if that has not been done previously.
Some surgeons use a technique that requires laser hair removal in the area of the penis and scrotum to provide hair-free tissue for the procedure. That process can take several months. Other techniques don't require hair removal prior to surgery because the hair follicles are destroyed during the procedure.
After vaginoplasty, a tube called a catheter is placed in the urethra to collect urine for several days. You need to be closely watched for about a week after surgery. Recovery can take up to two months. Your health care provider gives you instructions about when you may begin sexual activity with your new vagina.
After surgery, you're given a set of vaginal dilators of increasing sizes. You insert the dilators in your vagina to maintain, lengthen and stretch it. Follow your health care provider's directions on how often to use the dilators. To keep the vagina open, dilation needs to continue long term.
Because the prostate gland isn't removed during surgery, you need to follow age-appropriate recommendations for prostate cancer screening. Following surgery, it is possible to develop urinary symptoms from enlargement of the prostate.
Dilation after gender-affirming surgery
This material is for your education and information only. This content does not replace medical advice, diagnosis and treatment. If you have questions about a medical condition, always talk with your health care provider.
Narrator: Vaginal dilation is important to your recovery and ongoing care. You have to dilate to maintain the size and shape of your vaginal canal and to keep it open.
Jessi: I think for many trans women, including myself, but especially myself, I looked forward to one day having surgery for a long time. So that meant looking up on the internet what the routines would be, what the surgery entailed. So I knew going into it that dilation was going to be a very big part of my routine post-op, but just going forward, permanently.
Narrator: Vaginal dilation is part of your self-care. You will need to do vaginal dilation for the rest of your life.
Alissa (nurse): If you do not do dilation, your vagina may shrink or close. If that happens, these changes might not be able to be reversed.
Narrator: For the first year after surgery, you will dilate many times a day. After the first year, you may only need to dilate once a week. Most people dilate for the rest of their life.
Jessi: The dilation became easier mostly because I healed the scars, the stitches held up a little bit better, and I knew how to do it better. Each transgender woman's vagina is going to be a little bit different based on anatomy, and I grew to learn mine. I understand, you know, what position I needed to put the dilator in, how much force I needed to use, and once I learned how far I needed to put it in and I didn't force it and I didn't worry so much on oh, did I put it in too far, am I not putting it in far enough, and I have all these worries and then I stress out and then my body tenses up. Once I stopped having those thoughts, I relaxed more and it was a lot easier.
Narrator: You will have dilators of different sizes. Your health care provider will determine which sizes are best for you. Dilation will most likely be painful at first. It's important to dilate even if you have pain.
Alissa (nurse): Learning how to relax the muscles and breathe as you dilate will help. If you wish, you can take the pain medication recommended by your health care team before you dilate.
Narrator: Dilation requires time and privacy. Plan ahead so you have a private area at home or at work. Be sure to have your dilators, a mirror, water-based lubricant and towels available. Wash your hands and the dilators with warm soapy water, rinse well and dry on a clean towel. Use a water-based lubricant to moisten the rounded end of the dilators. Water-based lubricants are available over-the-counter. Do not use oil-based lubricants, such as petroleum jelly or baby oil. These can irritate the vagina. Find a comfortable position in bed or elsewhere. Use pillows to support your back and thighs as you lean back to a 45-degree angle. Start your dilation session with the smallest dilator. Hold a mirror in one hand. Use the other hand to find the opening of your vagina. Separate the skin. Relax through your hips, abdomen and pelvic floor. Take slow, deep breaths. Position the rounded end of the dilator with the lubricant at the opening to your vaginal canal. The rounded end should point toward your back. Insert the dilator. Go slowly and gently. Think of its path as a gentle curving swoop. The dilator doesn't go straight in. It follows the natural curve of the vaginal canal. Keep gentle down and inward pressure on the dilator as you insert it. Stop when the dilator's rounded end reaches the end of your vaginal canal. The dilators have dots or markers that measure depth. Hold the dilator in place in your vaginal canal. Use gentle but constant inward pressure for the correct amount of time at the right depth for you. If you're feeling pain, breathe and relax the muscles. When time is up, slowly remove the dilator, then repeat with the other dilators you need to use. Wash the dilators and your hands. If you have increased discharge following dilation, you may want to wear a pad to protect your clothing.
Jessi: I mean, it's such a strange, unfamiliar feeling to dilate and to have a dilator, you know to insert a dilator into your own vagina. Because it's not a pleasurable experience, and it's quite painful at first when you start to dilate. It feels much like a foreign body entering and it doesn't feel familiar and your body kind of wants to get it out of there. It's really tough at the beginning, but if you can get through the first month, couple months, it's going to be a lot easier and it's not going to be so much of an emotional and uncomfortable experience.
Narrator: You need to stay on schedule even when traveling. Bring your dilators with you. If your schedule at work creates challenges, ask your health care team if some of your dilation sessions can be done overnight.
Alissa (nurse): You can't skip days now and do more dilation later. You must do dilation on schedule to keep vaginal depth and width. It is important to dilate even if you have pain. Dilation should cause less pain over time.
Jessi: I hear that from a lot of other women that it's an overwhelming experience. There's lots of emotions that are coming through all at once. But at the end of the day for me, it was a very happy experience. I was glad to have the opportunity because that meant that while I have a vagina now, at the end of the day I had a vagina. Yes, it hurts, and it's not pleasant to dilate, but I have the vagina and it's worth it. It's a long process and it's not going to be easy. But you can do it.
Narrator: If you feel dilation may not be working or you have any questions about dilation, please talk with a member of your health care team.
Research has found that gender-affirming surgery can have a positive impact on well-being and sexual function. It's important to follow your health care provider's advice for long-term care and follow-up after surgery. Continued care after surgery is associated with good outcomes for long-term health.
Before you have surgery, talk to members of your health care team about what to expect after surgery and the ongoing care you may need.
Clinical trials
Explore Mayo Clinic studies of tests and procedures to help prevent, detect, treat or manage conditions.
Feminizing surgery care at Mayo Clinic
- Tangpricha V, et al. Transgender women: Evaluation and management. https://www.uptodate.com/ contents/search. Accessed Aug. 16, 2022.
- Erickson-Schroth L, ed. Surgical transition. In: Trans Bodies, Trans Selves: A Resource by and for Transgender Communities. 2nd ed. Kindle edition. Oxford University Press; 2022. Accessed Aug. 17, 2022.
- Coleman E, et al. Standards of care for the health of transgender and gender diverse people, version 8. International Journal of Transgender Health. 2022; doi:10.1080/26895269.2022.2100644.
- AskMayoExpert. Gender-affirming procedures (adult). Mayo Clinic; 2022.
- Nahabedian, M. Implant-based breast reconstruction and augmentation. https://www.uptodate.com/contents/search. Accessed Aug. 17, 2022.
- Erickson-Schroth L, ed. Medical transition. In: Trans Bodies, Trans Selves: A Resource by and for Transgender Communities. 2nd ed. Kindle edition. Oxford University Press; 2022. Accessed Aug. 17, 2022.
- Ferrando C, et al. Gender-affirming surgery: Male to female. https://www.uptodate.com/contents/search. Accessed Aug. 17, 2022.
- Doctors & Departments
- Care at Mayo Clinic
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
5X Challenge
Thanks to generous benefactors, your gift today can have 5X the impact to advance AI innovation at Mayo Clinic.
- Election 2024
- Entertainment
- Newsletters
- Photography
- AP Buyline Personal Finance
- AP Buyline Shopping
- Press Releases
- Israel-Hamas War
- Russia-Ukraine War
- Global elections
- Asia Pacific
- Latin America
- Middle East
- Election results
- Google trends
- AP & Elections
- U.S. Open Tennis
- Paralympic Games
- College football
- Auto Racing
- Movie reviews
- Book reviews
- Financial Markets
- Business Highlights
- Financial wellness
- Artificial Intelligence
- Social Media
Trans kids’ treatment can start younger, new guidelines say

This photo provided by Laura Short shows Eli Bundy on April 15, 2022 at Deception Pass in Washington. In South Carolina, where a proposed law would ban transgender treatments for kids under age 18, Eli Bundy hopes to get breast removal surgery next year before college. Bundy, 18, who identifies as nonbinary, supports updated guidance from an international transgender health group that recommends lower ages for some treatments. (Laura Short via AP)
FILE - Dr. David Klein, right, an Air Force Major and chief of adolescent medicine at Fort Belvoir Community Hospital, listens as Amanda Brewer, left, speaks with her daughter, Jenn Brewer, 13, as the teenager has blood drawn during a monthly appointment for monitoring her treatment at the hospital in Fort Belvoir, Va., on Sept. 7, 2016. Brewer is transitioning from male to female. (AP Photo/Jacquelyn Martin, File)
- Copy Link copied

A leading transgender health association has lowered its recommended minimum age for starting gender transition treatment, including sex hormones and surgeries.
The World Professional Association for Transgender Health said hormones could be started at age 14, two years earlier than the group’s previous advice, and some surgeries done at age 15 or 17, a year or so earlier than previous guidance. The group acknowledged potential risks but said it is unethical and harmful to withhold early treatment.
The association provided The Associated Press with an advance copy of its update ahead of publication in a medical journal, expected later this year. The international group promotes evidence-based standards of care and includes more than 3,000 doctors, social scientists and others involved in transgender health issues.
The update is based on expert opinion and a review of scientific evidence on the benefits and harms of transgender medical treatment in teens whose gender identity doesn’t match the sex they were assigned at birth, the group said. Such evidence is limited but has grown in the last decade, the group said, with studies suggesting the treatments can improve psychological well-being and reduce suicidal behavior.
Starting treatment earlier allows transgender teens to experience physical puberty changes around the same time as other teens, said Dr. Eli Coleman, chair of the group’s standards of care and director of the University of Minnesota Medical School’s human sexuality program.
But he stressed that age is just one factor to be weighed. Emotional maturity, parents’ consent, longstanding gender discomfort and a careful psychological evaluation are among the others.
“Certainly there are adolescents that do not have the emotional or cognitive maturity to make an informed decision,” he said. “That is why we recommend a careful multidisciplinary assessment.”
The updated guidelines include recommendations for treatment in adults, but the teen guidance is bound to get more attention. It comes amid a surge in kids referred to clinics offering transgender medical treatment , along with new efforts to prevent or restrict the treatment.
Many experts say more kids are seeking such treatment because gender-questioning children are more aware of their medical options and facing less stigma.
Critics, including some from within the transgender treatment community, say some clinics are too quick to offer irreversible treatment to kids who would otherwise outgrow their gender-questioning.
Psychologist Erica Anderson resigned her post as a board member of the World Professional Association for Transgender Health last year after voicing concerns about “sloppy” treatment given to kids without adequate counseling.
She is still a group member and supports the updated guidelines, which emphasize comprehensive assessments before treatment. But she says dozens of families have told her that doesn’t always happen.
“They tell me horror stories. They tell me, ‘Our child had 20 minutes with the doctor’” before being offered hormones, she said. “The parents leave with their hair on fire.’’
Estimates on the number of transgender youth and adults worldwide vary, partly because of different definitions. The association’s new guidelines say data from mostly Western countries suggest a range of between a fraction of a percent in adults to up to 8% in kids.
Anderson said she’s heard recent estimates suggesting the rate in kids is as high as 1 in 5 — which she strongly disputes. That number likely reflects gender-questioning kids who aren’t good candidates for lifelong medical treatment or permanent physical changes, she said.
Still, Anderson said she condemns politicians who want to punish parents for allowing their kids to receive transgender treatment and those who say treatment should be banned for those under age 18.
“That’s just absolutely cruel,’’ she said.
Dr. Marci Bowers, the transgender health group’s president-elect, also has raised concerns about hasty treatment, but she acknowledged the frustration of people who have been “forced to jump through arbitrary hoops and barriers to treatment by gatekeepers ... and subjected to scrutiny that is not applied to another medical diagnosis.’’
Gabe Poulos, 22, had breast removal surgery at age 16 and has been on sex hormones for seven years. The Asheville, North Carolina, resident struggled miserably with gender discomfort before his treatment.
Poulos said he’s glad he was able to get treatment at a young age.
“Transitioning under the roof with your parents so they can go through it with you, that’s really beneficial,’’ he said. “I’m so much happier now.’’
In South Carolina, where a proposed law would ban transgender treatments for kids under age 18, Eli Bundy has been waiting to get breast removal surgery since age 15. Now 18, Bundy just graduated from high school and is planning to have surgery before college.
Bundy, who identifies as nonbinary, supports easing limits on transgender medical care for kids.
“Those decisions are best made by patients and patient families and medical professionals,’’ they said. “It definitely makes sense for there to be fewer restrictions, because then kids and physicians can figure it out together.’’
Dr. Julia Mason, an Oregon pediatrician who has raised concerns about the increasing numbers of youngsters who are getting transgender treatment, said too many in the field are jumping the gun. She argues there isn’t strong evidence in favor of transgender medical treatment for kids.
“In medicine ... the treatment has to be proven safe and effective before we can start recommending it,’’ Mason said.
Experts say the most rigorous research — studies comparing treated kids with outcomes in untreated kids — would be unethical and psychologically harmful to the untreated group.
The new guidelines include starting medication called puberty blockers in the early stages of puberty, which for girls is around ages 8 to 13 and typically two years later for boys. That’s no change from the group’s previous guidance. The drugs delay puberty and give kids time to decide about additional treatment; their effects end when the medication is stopped.
The blockers can weaken bones, and starting them too young in children assigned males at birth might impair sexual function in adulthood, although long-term evidence is lacking.
The update also recommends:
—Sex hormones — estrogen or testosterone — starting at age 14. This is often lifelong treatment. Long-term risks may include infertility and weight gain, along with strokes in trans women and high blood pressure in trans men, the guidelines say.
—Breast removal for trans boys at age 15. Previous guidance suggested this could be done at least a year after hormones, around age 17, although a specific minimum ag wasn’t listed.
—Most genital surgeries starting at age 17, including womb and testicle removal, a year earlier than previous guidance.
The Endocrine Society, another group that offers guidance on transgender treatment, generally recommends starting a year or two later, although it recently moved to start updating its own guidelines. The American Academy of Pediatrics and the American Medical Association support allowing kids to seek transgender medical treatment, but they don’t offer age-specific guidance.
Dr. Joel Frader, a Northwestern University a pediatrician and medical ethicist who advises a gender treatment program at Chicago’s Lurie Children’s Hospital, said guidelines should rely on psychological readiness, not age.
Frader said brain science shows that kids are able to make logical decisions by around age 14, but they’re prone to risk-taking and they take into account long-term consequences of their actions only when they’re much older.
Coleen Williams, a psychologist at Boston Children’s Hospital’s Gender Multispecialty Service, said treatment decisions there are collaborative and individualized.
“Medical intervention in any realm is not a one-size-fits-all option,” Williams said.
Follow AP Medical Writer Lindsey Tanner at @LindseyTanner.
The Associated Press Health and Science Department receives support from the Howard Hughes Medical Institute’s Department of Science Education. The AP is solely responsible for all content.

- Share full article
Advertisement
Supported by
More Trans Teens Are Choosing ‘Top Surgery’
Small studies suggest that breast removal surgery improves transgender teenagers’ well-being, but data is sparse. Some state leaders oppose such procedures for minors.

By Azeen Ghorayshi
Listen to This Article
Michael, 17, arrived in the sleek white waiting room of his plastic surgeon’s office in Miami for a moment he had long anticipated: removing the bandages to see his newly flat chest.
After years of squeezing into compression undershirts to conceal his breasts, the teenager was overcome with relief that morning last December. Wearing an unbuttoned shirt, he posed for photos with his mother and the surgeon, Dr. Sidhbh Gallagher, happy to share his bare chest with the doctor’s large following on social media.
“It just felt right — like I’d never had breasts in the first place,” Michael said. “It was a ‘Yes, finally’ kind of moment.”
Michael is part of a very small but growing group of transgender adolescents who have had top surgery, or breast removal, to better align their bodies with their experience of gender. Most of these teenagers have also taken testosterone and changed their name, pronouns or clothing style.
Few groups of young people have received as much attention. Republican elected officials across the United States are seeking to ban all so-called gender-affirming care for minors, turning an intensely personal medical decision into a political maelstrom with significant consequences for transgender adolescents and their families.
Gender-related surgeries, in particular, have been thrust into the spotlight. Arizona and Alabama passed laws this year making it illegal for doctors to perform gender-related surgeries on transgender patients under 18. Conservative commentators with large followings on social media have recently targeted children’s hospitals that offer gender surgeries, leading to online harassment and bomb threats .
We are having trouble retrieving the article content.
Please enable JavaScript in your browser settings.
Thank you for your patience while we verify access. If you are in Reader mode please exit and log into your Times account, or subscribe for all of The Times.
Thank you for your patience while we verify access.
Already a subscriber? Log in .
Want all of The Times? Subscribe .
Call us today to discuss cosmetic surgery options to enhance your enjoyment of life
Alameda: 510-864-1800
Brentwood: 925-240-8775
Text Us: 510.650.0383
Gender Reassignment Surgery
Gender reassignment Female-to-Male Breast Surgery
Gender dysphoria occurs in 0.3% of the population. The female-to-male (FTM) gender reassignment surgery in our Alameda and Brentwood practice involves removing both breasts: termed mastectomy, with preservation of the nipple areola complex and with the creation of a contoured, male-looking chest.

- First Name *
- Last Name *
- Procedure of Interest * Procedure of Interest Breast Surgery Gender Reassignment Surgery Male Breast Reduction Arm Lift Surgery Chin Augmentation Slit & Torn Earlobe Repair Eyelid & Eyebrow Lift Facelift Fat Grafting Lip Augmentation Liposuction Otoplasty Post-Bariatric Surgery Rhinoplasty Thigh Lift Tummy Tuck Pediatric Plastic Surgery Reconstruction Skin Treatments Injectables
BRENTWOOD OFFICE
Quick Links
Breast Surgery
Cosmetic Surgery
Pediatric Plastic Surgery
Reconstruction
Skin Treatments
Meet the Team
Surgical Care
Accessibility Statement
Read Patient Reviews »
Alameda Location:
2070 Clinton Ave, Alameda, CA 94501
510-864-1800.
Brentwood Location
1280 Central Blvd, Suite J-5, Brentwood, CA 94513
925-240-8775.
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- Diet & Nutrition
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board

Gender Confirmation Surgery (GCS)
What is Gender Confirmation Surgery?
- Transfeminine Tr
Transmasculine Transition
- Traveling Abroad
Choosing a Surgeon
Gender confirmation surgery (GCS), known clinically as genitoplasty, are procedures that surgically confirm a person's gender by altering the genitalia and other physical features to align with their desired physical characteristics. Gender confirmation surgeries are also called gender affirmation procedures. These are both respectful terms.
Gender dysphoria , an experience of misalignment between gender and sex, is becoming more widely diagnosed. People diagnosed with gender dysphoria are often referred to as "transgender," though one does not necessarily need to experience gender dysphoria to be a member of the transgender community. It is important to note there is controversy around the gender dysphoria diagnosis. Many disapprove of it, noting that the diagnosis suggests that being transgender is an illness.
Ellen Lindner / Verywell
Transfeminine Transition
Transfeminine is a term inclusive of trans women and non-binary trans people assigned male at birth.
Gender confirmation procedures that a transfeminine person may undergo include:
- Penectomy is the surgical removal of external male genitalia.
- Orchiectomy is the surgical removal of the testes.
- Vaginoplasty is the surgical creation of a vagina.
- Feminizing genitoplasty creates internal female genitalia.
- Breast implants create breasts.
- Gluteoplasty increases buttock volume.
- Chondrolaryngoplasty is a procedure on the throat that can minimize the appearance of Adam's apple .
Feminizing hormones are commonly used for at least 12 months prior to breast augmentation to maximize breast growth and achieve a better surgical outcome. They are also often used for approximately 12 months prior to feminizing genital surgeries.
Facial feminization surgery (FFS) is often done to soften the lines of the face. FFS can include softening the brow line, rhinoplasty (nose job), smoothing the jaw and forehead, and altering the cheekbones. Each person is unique and the procedures that are done are based on the individual's need and budget,
Transmasculine is a term inclusive of trans men and non-binary trans people assigned female at birth.
Gender confirmation procedures that a transmasculine person may undergo include:
- Masculinizing genitoplasty is the surgical creation of external genitalia. This procedure uses the tissue of the labia to create a penis.
- Phalloplasty is the surgical construction of a penis using a skin graft from the forearm, thigh, or upper back.
- Metoidioplasty is the creation of a penis from the hormonally enlarged clitoris.
- Scrotoplasty is the creation of a scrotum.
Procedures that change the genitalia are performed with other procedures, which may be extensive.
The change to a masculine appearance may also include hormone therapy with testosterone, a mastectomy (surgical removal of the breasts), hysterectomy (surgical removal of the uterus), and perhaps additional cosmetic procedures intended to masculinize the appearance.
Paying For Gender Confirmation Surgery
Medicare and some health insurance providers in the United States may cover a portion of the cost of gender confirmation surgery.
It is unlawful to discriminate or withhold healthcare based on sex or gender. However, many plans do have exclusions.
For most transgender individuals, the burden of financing the procedure(s) is the main difficulty in obtaining treatment. The cost of transitioning can often exceed $100,000 in the United States, depending upon the procedures needed.
A typical genitoplasty alone averages about $18,000. Rhinoplasty, or a nose job, averaged $5,409 in 2019.
Traveling Abroad for GCS
Some patients seek gender confirmation surgery overseas, as the procedures can be less expensive in some other countries. It is important to remember that traveling to a foreign country for surgery, also known as surgery tourism, can be very risky.
Regardless of where the surgery will be performed, it is essential that your surgeon is skilled in the procedure being performed and that your surgery will be performed in a reputable facility that offers high-quality care.
When choosing a surgeon , it is important to do your research, whether the surgery is performed in the U.S. or elsewhere. Talk to people who have already had the procedure and ask about their experience and their surgeon.
Before and after photos don't tell the whole story, and can easily be altered, so consider asking for a patient reference with whom you can speak.
It is important to remember that surgeons have specialties and to stick with your surgeon's specialty. For example, you may choose to have one surgeon perform a genitoplasty, but another to perform facial surgeries. This may result in more expenses, but it can result in a better outcome.
A Word From Verywell
Gender confirmation surgery is very complex, and the procedures that one person needs to achieve their desired result can be very different from what another person wants.
Each individual's goals for their appearance will be different. For example, one individual may feel strongly that breast implants are essential to having a desirable and feminine appearance, while a different person may not feel that breast size is a concern. A personalized approach is essential to satisfaction because personal appearance is so highly individualized.
Davy Z, Toze M. What is gender dysphoria? A critical systematic narrative review . Transgend Health . 2018;3(1):159-169. doi:10.1089/trgh.2018.0014
Morrison SD, Vyas KS, Motakef S, et al. Facial Feminization: Systematic Review of the Literature . Plast Reconstr Surg. 2016;137(6):1759-70. doi:10.1097/PRS.0000000000002171
Hadj-moussa M, Agarwal S, Ohl DA, Kuzon WM. Masculinizing Genital Gender Confirmation Surgery . Sex Med Rev . 2019;7(1):141-155. doi:10.1016/j.sxmr.2018.06.004
Dowshen NL, Christensen J, Gruschow SM. Health Insurance Coverage of Recommended Gender-Affirming Health Care Services for Transgender Youth: Shopping Online for Coverage Information . Transgend Health . 2019;4(1):131-135. doi:10.1089/trgh.2018.0055
American Society of Plastic Surgeons. Rhinoplasty nose surgery .
Rights Group: More U.S. Companies Covering Cost of Gender Reassignment Surgery. CNS News. http://cnsnews.com/news/article/rights-group-more-us-companies-covering-cost-gender-reassignment-surgery
The Sex Change Capital of the US. CBS News. http://www.cbsnews.com/2100-3445_162-4423154.html
By Jennifer Whitlock, RN, MSN, FN Jennifer Whitlock, RN, MSN, FNP-C, is a board-certified family nurse practitioner. She has experience in primary care and hospital medicine.

Female-to-Male Top Surgery Cost & Procedure Information
The female-to-male transsexual in Atlanta often desires an aesthetically pleasing male chest as his first and arguably most important surgical procedure to continue the gender transition. This Female-to-Male (FTM) or gender reassignment surgery (GRS) allows the patient to live more easily in the male gender role and facilitates a real-life experience. Top Surgery includes bilateral mastectomy (removal of the breasts) and male chest contouring and is one of the most frequent female to male surgeries performed. Top Surgery is also sometimes referred to as male chest reconstruction or simply, chest surgery. The female to male breast removal surgery removes almost all of the breast tissue and greatly reduces, almost eliminating, the possibility of developing breast cancer. Mammograms are no longer recommended after he transitions FTM. We perform gender transition surgery for patients in Atlanta and surrounding suburbs near Marietta, Cumming, Kennesaw, and Alpharetta.
Request A Consultation
Click Here to Visit our Trans Top Surgery Center's Website to Learn More!
Female-to-Male Transition Top Surgery
The female-to-male breast surgery is known as a subcutaneous mastectomy and there are several techniques that are used. The patient's breast size and body build determine which technique is ideal for him. On occasion, when breasts are so large as to cause severe and incapacitating back, neck, and shoulder pain, the breast reduction procedure may be a covered service by your insurance policy. We can help you determine if you have these benefits in your plan.
For some doctors performing the female to male transition surgery, the mastectomy is done in two steps, first, the contents of the breast are removed. The surgeon removes the contents through either a cut inside the areola or around it, and then let the skin retract for about a year. After a year the second surgery removes the excess skin. This technique results in far less scarring, and the nipple-areola doesn't need to be removed and grafted. I have developed my own unique female to male breast augmentation procedure because the existing procedures didn't fully address the needs of my patient. It is called the "Comma Procedure" because of the shape of the surgical scar resembles a comma. I take each and every individual's needs and unique attributes into consideration when planning out their procedure to make sure their gender transition surgery goes beyond their expectations.
Male-to-Female Transition Top Surgery
The male-to-female transsexual in Atlanta generally has worn external breast prostheses for several years prior to making a decision to have breast augmentation surgery. She has developed a very accurate image of the size breast that looks best on her body which makes the decision of choosing the proper implant size much easier than for the usual small-breasted woman requesting breast augmentation.
We provide breast augmentation surgery as well for the MTF transition. During your initial consultation, Dr. Lincenberg will review your medical history and answer any questions you may have. You will need to make decisions on breast size (cup size), on the type and shape of implants you will receive, and on the location of your incisions. Dr. Lincenberg will ask you for your personal preferences so he can recommend the right implant size and shape for you. You will also be able to try on breast implant sizers to help you with your decision on breast augmentation surgery.
You may choose either silicone or saline implants. Silicone implants are made from a gel that holds together uniformly while retaining the natural give that resembles breast tissue. Saline implants are filled with a saltwater solution similar to the fluid that makes up most of the human body and has a slightly firmer feel.
Male-to-Neutrois Top Surgery
MTN or Male to Neutrois transition refers to individuals who have been identified at birth to have male genitalia, but whose personal identity falls outside of the binary male gender they've been assigned to. Neutrois is best understood as a non-binary gender that doesn't identify as singularly male or female. Dr. Lincenberg has experience working with individuals to shape their chest to be more gender neutral.
Female-to-Neutrois Top Surgery
FTN or Femail to Neutrois transition refers to individuals who have been identified at birth to have female genitalia. These individual's personal identity falls outside of the binary female gender they've been assigned to. To transition to a non-binary gender, our FTN clients normally want to remove their breasts and shape their chest to be more gender neutral.
How Much Does A Transgender Mastectomy Cost?
The Mastectomy procedure can cost anywhere from $8400 - $8600. The actual costs will be determined after we understand your individual needs and wants for the procedure. We understand plastic surgery is an investment and want all of our clients to pursue it with as much knowledge as possible. Schedule a consultation to meet with Dr. Lincenberg to learn more about the Atlanta plastic surgery procedures you’re interested in and get a specific quote.
Dr. Lincenberg Reviews
"Dr. Lincenberg and his staff are amazing! He is definitely worth every penny. They were all so accepting, they treated us like family. Dr. Lincenberg makes you feel so comfortable and he shares in on the excitement that you feel! He is amazing at what he does!!! I love Dr. Sheldon and his staff." - Kaylyn
"Staff was so friendly and accommodating! Dr. Lincenberg made me feel so at ease about my procedure and I am very happy with the results!!" - Drewlonda
"This the absolute best surgeon in Atlanta! He did an amazing job on my chest! The staff is wonderful and so very personable and helpful. You cannot ask for better service and experience with the staff and doctor! Thanks so much for a new outlook on life! Y’all are awesome!!!" - Lee
"Wonderful experience with both the doctor and staff. It was prompt and every question was answered with professional ease. I would recommend Georgia Plastic Surgery to anyone that was looking for advice." - Caiden
Before and After Gallery
Gender confirmation surgery.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Review Article
- Published: 12 April 2011
Gender reassignment surgery: an overview
- Gennaro Selvaggi 1 &
- James Bellringer 1
Nature Reviews Urology volume 8 , pages 274–282 ( 2011 ) Cite this article
4001 Accesses
153 Citations
41 Altmetric
Metrics details
- Pathogenesis
- Reconstruction
- Urogenital diseases
This article has been updated
Gender reassignment (which includes psychotherapy, hormonal therapy and surgery) has been demonstrated as the most effective treatment for patients affected by gender dysphoria (or gender identity disorder), in which patients do not recognize their gender (sexual identity) as matching their genetic and sexual characteristics. Gender reassignment surgery is a series of complex surgical procedures (genital and nongenital) performed for the treatment of gender dysphoria. Genital procedures performed for gender dysphoria, such as vaginoplasty, clitorolabioplasty, penectomy and orchidectomy in male-to-female transsexuals, and penile and scrotal reconstruction in female-to-male transsexuals, are the core procedures in gender reassignment surgery. Nongenital procedures, such as breast enlargement, mastectomy, facial feminization surgery, voice surgery, and other masculinization and feminization procedures complete the surgical treatment available. The World Professional Association for Transgender Health currently publishes and reviews guidelines and standards of care for patients affected by gender dysphoria, such as eligibility criteria for surgery. This article presents an overview of the genital and nongenital procedures available for both male-to-female and female-to-male gender reassignment.
The management of gender dysphoria consists of a combination of psychotherapy, hormonal therapy, and surgery
Psychiatric evaluation is essential before gender reassignment surgical procedures are undertaken
Gender reassignment surgery refers to the whole genital, facial and body procedures required to create a feminine or a masculine appearance
Sex reassignment surgery refers to genital procedures, namely vaginoplasty, clitoroplasty, labioplasty, and penile–scrotal reconstruction
In male-to-female gender dysphoria, skin tubes formed from penile or scrotal skin are the standard technique for vaginal construction
In female-to-male gender dysphoria, no technique is recognized as the standard for penile reconstruction; different techniques fulfill patients' requests at different levels, with a variable number of surgical technique-related drawbacks
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
195,33 € per year
only 16,28 € per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others

Principles and outcomes of gender-affirming vaginoplasty

Sexual function of transgender assigned female at birth seeking gender affirming care: a narrative review

The effect of early puberty suppression on treatment options and outcomes in transgender patients
Change history, 26 april 2011.
In the version of this article initially published online, the statement regarding the frequency of male-to-female transsexuals was incorrect. The error has been corrected for the print, HTML and PDF versions of the article.
Meyer, W. 3rd. et al . The Harry Benjamin International Gender Dysphoria Association's standards of care for gender identity disorders, sixth version. World Professional Association for Transgender Health [online] , (2001).
Google Scholar
Bakker, A., Van Kesteren, P., Gooren, L. & Bezemer, P. The prevalence of transsexualism in The Netherlands. Acta Psychiatr. Scand. 87 , 237–238 (1993).
Article CAS Google Scholar
Selvaggi, G. et al . Gender identity disorder: general overview and surgical treatment for vaginoplasty in male-to-female transsexuals. Plast. Reconstr. Surg. 116 , 135e–145e (2005).
Article Google Scholar
Benjamin, H. (ed.) The Transsexual Phenomenon (Julian Press Inc., New York, 1966).
World Professional Association for Transgender Health [online] , (2010).
Zhou, J. N., Hofman, M. A., Gooren, L. J. & Swaab, D. F. A sex difference in the human brain and its relation to transsexuality. Nature 378 , 68–70 (1995).
Kruijver, F. P. et al . Male-to-female transsexuals have female neuron numbers in a limbic nucleus. J. Clin. Endocrinol. Metab. 85 , 2034–2041 (2000).
Swaab, D. F., Chun, W. C., Kruijver, F. P., Hofman, M. A. & Ishuina, T. A. Sexual differentiation of the human hypothalamus. Adv. Exp. Med. Biol. 511 , 75–105 (2002).
Garcia-Falgueras, A. & Swaab, D. F. A sex difference in the hypothalamic uncinate nucleus: relationship to gender identity. Brain 131 , 3115–3117 (2008).
Cohen-Kettenis, P. & Kuiper, B. Transseksualiteit en psychotherapie [Dutch]. Tijdschr. Psychoth. 3 , 153–166 (1984).
Kuiper, B. & Cohen-Kettenis, P. Sex reassignment surgery: a study of 141 Dutch transsexuals. Arch. Sex. Behav. 17 , 439–457 (1988).
Kanhai, R. C., Hage, J. J., Karim, R. B. & Mulder, J. W. Exceptional presenting conditions and outcome of augmentation mammoplasty in male-to female transsexuals. Ann. Plast. Surg. 43 , 476–483 (1999).
Kanagalingm, J. et al . Cricothyroid approximation and subluxation in 21 male-to-female transsexuals. Laryngoscope 115 , 611–618 (2005).
Bouman, M. Laparoscopic assisted colovaginoplasty. Presented at the 2009 biennial World Professional Association for Transgender Health meeting, Oslo.
Rubin, S. O. Sex-reassignment surgery male-to-female. Review, own results and report of a new technique using the glans penis as a pseudoclitoris. Scand. J. Urol. Nephrol. Suppl. 154 , 1–28 (1993).
CAS PubMed Google Scholar
Fang, R. H., Chen, C. F. & Ma, S. A new method for clitoroplasty in male-to-female sex reassignment surgery. Plast. Reconstr. Surg. 89 , 679–682 (1992).
Selvaggi, G. et al . Genital sensitivity in sex reassignment surgery. Ann. Plast. Surg. 58 , 427–433 (2007).
Watanayusakul, S. SRS procedures. The Suporn Clinic [online] , (2010).
Melzer, T. Managing complications of male to female surgery. Presented at the 2007 World Professional Association for Transgender Health biennial meeting, Chicago.
Gilleard, O., Qureshi, M., Thomas, P. & Bellringer, J. Urethral bleeding following male to female gender reassignmetn surgery. Presented at the 2009 World Professional Association for Transgender Health biennial meeting, Oslo.
Beckley, I., Thomas, P. & Bellringer, J. Aetiology and management of recto-vaginal fistulas following male to female gender reassignment. Presented at 2008 EAU section of genitourinary surgeons and the EAU section of andrological urology meeting, Madrid.
Monstrey, S. et al . Chest wall contouring surgery in female-to-male (FTM) transsexuals: a new algorithm. Plast. Reconstr. Surg. 121 , 849–859 (2008).
Mueller, A. & Gooren, L. Hormone-related tumors in transsexuals receiving treatment with cross-sex hormones. Eur. J. Endocrinol. 159 , 197–202 (2008).
Selvaggi, G., Elander, A. & Branemark, R. Penile epithesis: preliminary study. Plast. Reconstr. Surg. 126 , 265e–266e (2010).
Selvaggi, G. & Elander, A. Penile reconstruction/formation. Curr. Opin. Urol. 18 , 589–597 (2008).
Gilbert, D. A., Jordan, G. H., Devine, C. J. Jr & Winslow, B. H. Microsurgical forearm “cricket bat-transformer” phalloplasty. Plast. Reconstr. Surg. 90 , 711–716 (1992).
Bettocchi, C., Ralph, D. J. & Pryor, J. P. Pedicled pubic phalloplasty in females with gender dysphoria. BJU Int. 95 , 120–124 (2005).
Monstrey, S. et al . Penile reconstruction: is the radial forearm flap really the standard technique? Plast. Reconstr. Surg. 124 , 510–518 (2009).
Selvaggi, G. et al . Donor-site morbidity of the radial forearm free flap after 125 phalloplasties in gender identity disorder. Plast. Reconstr. Surg. 118 , 1171–1177 (2006).
Hoebeke, P. et al . Impact of sex reassignment surgery on lower urinary tract function. Eur. Urol. 47 , 398–402 (2005).
Agrawal, V. & Ralph, D. An audit of implanted penile prosteses in the UK. BJU Int. 98 , 393–395 (2006).
Hoebeke, P. B. et al . Erectile implants in female-to-male transsexuals: our experience in 129 patients. Eur. Urol. 57 , 334–340 (2010).
Vesely, J. et al . New technique of total phalloplasty with reinnervated latissimus dorsi myocutaneous free flap in female-to-male transsexuals. Ann. Plast. Surg. 58 , 544–550 (2007).
Selvaggi, G. et al . Scrotal reconstruction in female-to-male transsexuals: a novel scrotoplasty. Plast. Reconstr. Surg. 123 , 1710–1718 (2009).
Download references
Author information
Authors and affiliations.
Gender Surgery Unit, Charing Cross Hospital, Imperial College NHS Trust, 179–183 Fulham Palace Road, London, W6 8QZ, UK
Gennaro Selvaggi & James Bellringer
You can also search for this author in PubMed Google Scholar
Contributions
G. Selvaggi and J. Bellringer contributed equally to the research, discussions, writing, reviewing, and editing of this article.
Corresponding author
Correspondence to James Bellringer .
Ethics declarations
Competing interests.
The authors declare no competing financial interests.
Rights and permissions
Reprints and permissions
About this article
Cite this article.
Selvaggi, G., Bellringer, J. Gender reassignment surgery: an overview. Nat Rev Urol 8 , 274–282 (2011). https://doi.org/10.1038/nrurol.2011.46
Download citation
Published : 12 April 2011
Issue Date : May 2011
DOI : https://doi.org/10.1038/nrurol.2011.46
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
A bibliometric and visualisation analysis on the research of female genital plastic surgery based on the web of science core collection database.
- Xianling Zhang
Aesthetic Plastic Surgery (2024)
Chest Feminization in Transwomen with Subfascial Breast Augmentation—Our Technique and Results
- James Roy Kanjoor
- Temoor Mohammad Khan
Aesthetic Plastic Surgery (2023)
Vaginoplasty in Male to Female transgenders: single center experience and a narrative review
- Luca Ongaro
- Giulio Garaffa
- Giovanni Liguori
International Journal of Impotence Research (2021)
Urethral complications after gender reassignment surgery: a systematic review
- L. R. Doumanian
Overview on metoidioplasty: variants of the technique
- Marta Bizic
- Borko Stojanovic
- Miroslav Djordjevic
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.

Gender Affirming Surgery
- Clinical Policy Bulletins
- Medical Clinical Policy Bulletins
Number: 0615


IMAGES
VIDEO
COMMENTS
Chest Feminization. A breast augmentation procedure may be part of a gender-affirming surgical plan, and can create a more feminine chest appearance. Breast augmentation involves a surgeon inserting a gel or liquid-filled implant into a pocket formed behind the breast tissue or under the pectoral muscle and centering each implant beneath the two nipples.
For zero-depth procedures patients should expect to be in Cleveland for 3-4 days after the surgery and for a full-depth procedure, 7-10 days after surgery. Appointments 216.445.6308. Request an Appointment. See before and after photos of patients who have undergone gender-affirming surgeries at Cleveland Clinic, including breast augmentations ...
For breast or "top" surgery, you are not required to schedule an intake visit with the Transgender Health Program, unless you need a referral for support services. Instead, please contact the Transgender Surgery Program team at 617-726-3525 to learn how to proceed with a surgical consult. Providers should fax referrals to 617-724-7126.
Transgender Mastectomy (Top Surgery) Elective cosmetic mastectomy, or "top surgery", is a procedure designed to remove unwanted breast tissue in order to create a more masculine chest appearance. Alongside hormone therapy, top surgery is typically one of the first steps for patients who are transitioning from female to male; this may also ...
Overview. Masculinizing surgery, also called gender-affirming surgery or gender-confirmation surgery, involves procedures that help better align the body with a person's gender identity. Masculinizing surgery includes several options, such as top surgery to create a more male-contoured chest and bottom surgery that changes the genitals.
This procedure includes removal of breast tissue with masculinizing chest contouring and nipple grafting in some cases. Chest surgery is sometimes performed as an outpatient procedure but some patients may require one night stay in the hospital. ... For more information about the program or to make an appointment, please contact the Transgender ...
Gender-affirming surgery is a collection of surgical procedures for adults ages 18 and older diagnosed with gender dysphoria. The operations are often referred to as "top surgery" and "bottom surgery.". Duke Health offers several top surgery options to transgender, gender-diverse, nonbinary, and gender-nonconforming adults who want their ...
The average range for cost of FTM and FTN top surgery is currently between $3,000 and $10,000. The average cost range for MTF and MTN top surgery varies greatly depending on factors such as body ...
Breast removal: People assigned female at birth would follow the steps of top surgery that transmasculine people would follow. Depending on your chest size, your own preferences, and your surgeon ...
There are multiple forms of gender-affirming surgery, including the removal of breasts — a mastectomy — and the altering of the genital region, known as "bottom" surgery. Examples of ...
Overview. Feminizing surgery, also called gender-affirming surgery or gender-confirmation surgery, involves procedures that help better align the body with a person's gender identity. Feminizing surgery includes several options, such as top surgery to increase the size of the breasts. That procedure also is called breast augmentation.
A leading transgender health association has lowered its recommended minimum age for gender transition treatment in teens, including starting sex hormones at age 14 and some surgeries at 15. ... Gabe Poulos, 22, had breast removal surgery at age 16 and has been on sex hormones for seven years. The Asheville, North Carolina, resident struggled ...
There is no coinsurance if a person is discharged within 60 days. The standard premium for Medicare Part B in 2024 is $174.70 each month, plus a $240 annual deductible cost. After a person pays ...
Request an Appointment. Call 215-662-7300 or request an appointment online. Penn Medicine proudly offers gender confirmation surgery, also known as gender affirmation surgery, to help align your identity.
Double incision. With this procedure, incisions are typically made at the top and bottom of the pectoral muscle and the chest tissue is removed. The skin is pulled down and reconnected at the ...
Small studies suggest that breast removal surgery improves transgender teenagers' well-being, but data is sparse. Some state leaders oppose such procedures for minors.
Gender dysphoria occurs in 0.3% of the population. The female-to-male (FTM) gender reassignment surgery in our Alameda and Brentwood practice involves removing both breasts: termed mastectomy, with preservation of the nipple areola complex and with the creation of a contoured, male-looking chest. People undergoing gender reassignment surgery ...
Research consistently shows that people who choose gender affirmation surgery experience reduced gender incongruence and improved quality of life. Depending on the procedure, 94% to 100% of people report satisfaction with their surgery results. Gender-affirming surgery provides long-term mental health benefits, too.
Mastectomy (breast removal) Gonadectomy (removing testes or ovaries) Hysterectomy (uterus removal) ... For surgery, have completed at least 12 months of hormone therapy (or longer if needed for the surgery). To Get Gender-Affirming Care: Start with your primary care provider (PCP). Your physician and mental health provider can refer you for ...
Gender Confirmation (GCS), formerly known as sex reassignment surgery, can be very complex. Find out more about these procedures. Gender Confirmation (GCS), formerly known as sex reassignment surgery, can be very complex. ... Penectomy is the surgical removal of external male genitalia. ... one individual may feel strongly that breast implants ...
This Female-to-Male (FTM) or gender reassignment surgery (GRS) allows the patient to live more easily in the male gender role and facilitates a real-life experience. Top Surgery includes bilateral mastectomy (removal of the breasts) and male chest contouring and is one of the most frequent female to male surgeries performed.
Top surgery is surgery that removes or augments breast tissue and reshapes the chest to create a more masculine or feminine appearance for transgender and nonbinary people. Facial gender surgery: While hormone replacement therapy can help achieve gender affirming changes to the face, surgery may help. Facial gender surgery can include a variety ...
Gender reassignment surgery is a series of complex surgical procedures (genital and nongenital) performed for the treatment of gender dysphoria. ... such as breast enlargement, mastectomy, facial ...
Medical Necessity. Aetna considers gender affirming surgery medically necessary when criteria for each of the following procedures is met: Requirements for Breast Removal. Signed letter from a qualified mental health professional (see Appendix) assessing the transgender/gender diverse individual's readiness for physical treatment; and.
The department in 2017 issued a $200,000 fine against the insurer Health Net for gaps in coverage related to gender reassignment surgery and other procedures. Most recently, in December, the Department of Managed Health Care announced a $200,000 fine against California Physicians' Service , the doctor reimbursement side of BlueCross, also ...