Narrative: Review of Anterior Knee Pain Differential Diagnosis (Other than Patellofemoral Pain)
- Current Reviews in Musculoskeletal Medicine 14(2)
- This person is not on ResearchGate, or hasn't claimed this research yet.

- Stanford University
Discover the world's research
- 25+ million members
- 160+ million publication pages
- 2.3+ billion citations
- Kassem Ghayyad

- Maham Abbas
- Faiza Asghar

- BMC MUSCULOSKEL DIS
- Liangjing Lyu
- Yongliang Li

- Arias Claudia
- Lustig Sebastien

- Sarah Darweesh
- Vladimir Stoychev

- Alfred Phillips

- Dominic King

- Morad Chughtai
- Jason Genin
- ARTHROSCOPY

- Wen-Yi Chou

- J SCI MED SPORT
- Trevor Vander Doelen
- Wilma Jelley

- Curr Sports Med Rep
- Lauren E Splittgerber
- Joseph M Ihm
- AM J SPORT MED

- Robert F. LaPrade

- Timothy C. Meade
- Marcus S. Briones
- Adam W. Fosnaugh
- Jeffrey M. Daily
- Recruit researchers
- Join for free
- Login Email Tip: Most researchers use their institutional email address as their ResearchGate login Password Forgot password? Keep me logged in Log in or Continue with Google Welcome back! Please log in. Email · Hint Tip: Most researchers use their institutional email address as their ResearchGate login Password Forgot password? Keep me logged in Log in or Continue with Google No account? Sign up

BRANDON Q. JONES, MD, CARLTON J. COVEY, MD, AND MARVIN H. SINEATH, JR., MD
Am Fam Physician. 2015;92(10):875-883
Patient information : See related handout on knee pain , written by the authors of this article.
Author disclosure: No relevant financial affiliations.
The role of the family physician in managing knee pain is expanding as recent literature supports nonsurgical management for many patients. Effective treatment depends on the etiology of knee pain. Oral analgesics—most commonly nonsteroidal anti-inflammatory drugs and acetaminophen—are used initially in combination with physical therapy to manage the most typical causes of chronic knee pain. The American Academy of Orthopaedic Surgeons recommends against glucosamine/chondroitin supplementation for osteoarthritis. In patients who are not candidates for surgery, opioid analgesics should be used only if conservative pharmacotherapy is ineffective. Exercise-based therapy is the foundation for treating knee osteoarthritis and patellofemoral pain syndrome. Weight loss should be encouraged for all patients with osteoarthritis and a body mass index greater than 25 kg per m 2 . Aside from stabilizing traumatic knee ligament and tendon tears, the effectiveness of knee braces for chronic knee pain is uncertain, and the use of braces should not replace physical therapy. Foot orthoses can be helpful for anterior knee pain. Corticosteroid injections are effective for short-term pain relief in patients with osteoarthritis. The benefit of hyaluronic acid injections is controversial, and recommendations vary; recent systematic reviews do not support a clinically significant benefit. Small studies suggest that regenerative injections can improve pain and function in patients with chronic knee tendinopathies and osteoarthritis.
Knee pain affects approximately 25% of adults, limiting function, mobility, and quality of life. 1 The prevalence of knee pain has increased 65% over the past 20 years, 1 with an estimated 4 million primary care visits per year attributed to knee pain. 2 Knee symptoms are the 10th most common reason for outpatient visits. 3 Recent studies support nonsurgical management for common knee diseases, such as osteoarthritis and meniscal disease. 4 – 6 Although there are many causes of and treatments for knee pain, this article focuses on the evidence supporting nonsurgical interventions for typical causes of knee pain in adults: osteoarthritis ( Table 1 7 – 22 ) ; patellofemoral pain syndrome ( Table 2 12 , 23 – 27 ) ; and meniscal, tendon, and ligament injuries ( Table 3 28 – 35 ) .
| Exercise-based therapy is the first-line treatment for knee osteoarthritis and patellofemoral pain syndrome, in addition to weight loss, if necessary, for those with osteoarthritis. | C | , |
| Nonsteroidal anti-inflammatory drugs are effective for short-term treatment of knee osteoarthritis and patellofemoral pain syndrome. | B | , , |
| Glucosamine/chondroitin supplementation has limited effectiveness in the treatment of osteoarthritis. | B | , , , , |
| Active rehabilitation is as effective as arthroscopy at reducing pain and improving function in patients with nontraumatic degenerative medial meniscal tears without mechanical symptoms. | A | , |
| Braces are a reasonable option for treatment of common knee overuse conditions, but should not replace treatments such as active rehabilitation. | C | , , , , |
| Do not use glucosamine and chondroitin to treat patients with symptomatic osteoarthritis of the knee. | American Academy of Orthopaedic Surgeons |
| Do not use lateral wedge insoles to treat patients with symptomatic medial compartment osteoarthritis of the knee. | American Academy of Orthopaedic Surgeons |
| Physical therapy and weight loss | Combination of aerobic and strength training is recommended, and weight loss if body mass index is greater than 25 kg per m , ; home programs are as effective as supervised programs |
| Ice improves range of motion and strength, but not pain | |
| There is some evidence for patellar taping or therapeutic ultrasonography to improve physical function and decrease pain , | |
| Pharmacotherapy | Extended-release acetaminophen, 1,300 mg three times daily, is effective and well tolerated; however, other studies show inconclusive evidence of effectiveness , |
| Glucosamine/chondroitin supplements show mixed benefit and are not recommended by the American Academy of Orthopaedic Surgeons , – | |
| Opioid analgesics should be used only if conservative pharmacotherapy is ineffective in patients who are not candidates for surgery | |
| Selective and nonselective nonsteroidal anti-inflammatory drugs are effective | |
| Injections | Corticosteroid injections provide short-term improvements in pain and function |
| Hyaluronic injections have questionable benefit for pain and function, and are best reserved for patients in whom first-line conservative treatments have been ineffective and who are not candidates for surgery , , | |
| Braces, orthoses, and other therapies | Limited evidence for medial unloader valgus brace , |
| Physical therapy | Quadriceps and hip strengthening combined with stretching of quadriceps, hamstrings, hip flexors, and iliotibial band three times weekly for six to eight weeks is effective in reducing pain and improving functionality |
| Ultrasonography and patellar taping have conflicting results but may be helpful adjuncts , | |
| Pharmacotherapy | Nonsteroidal anti-inflammatory drugs are effective for short-term treatment |
| Braces and orthoses | There is limited evidence for lateral patellar buttress brace , |
| Physical therapy | Active rehabilitation is as effective as arthroscopy for improving pain and function in patients with nontraumatic medial meniscal tears, and is as good as meniscectomy for improving physical function in patients with meniscal tears and osteoarthritis |
| Eccentric training is beneficial, but specific protocols are lacking | |
| Pharmacotherapy | Nonsteroidal anti-inflammatory drugs decrease ligamentous pain, but may have adverse effects on tendon healing |
| Injections | Corticosteroid injections provide short-term benefit for iliotibial band syndrome |
| Braces, orthoses, and other therapies | There is limited evidence for infrapatellar strap |
| Immobilizer braces for acute major ligamentous tears for support and stabilization may decrease pain in the acute phase , |

Osteoarthritis
Physical therapy and weight loss.
Physical therapy and exercise are the foundation of nonsurgical management of osteoarthritis-associated knee pain ( Figure 1 ) . Evidence has shown that active management (e.g., stretching, strengthening, exercise programs) is more effective in decreasing knee pain and improving function than passive modalities (e.g., therapeutic ultrasonography, electrical stimulation, taping, cryotherapy, heat). 36 Patellar taping is a popular adjunct treatment that has been shown to reduce pain in patients with knee osteoarthritis. 11 Ice massage and application of cold packs decrease swelling and improve range of motion and strength, but do not affect pain. 10 The American Academy of Orthopaedic Surgeons (AAOS) recently updated its guideline on the treatment of knee osteoarthritis to focus on exercise-based therapies and targeted weight loss. 7
Patients with a body mass index greater than 25 kg per m 2 should be encouraged to lose weight. 7 The addition of a calorie-restricted diet (25% to 30% decrease) to a combined aerobic/strength-training program improves pain, function, and body composition scores vs. exercise alone. 10 All types of exercise have been shown to improve osteoarthritis pain and physical function scores. 37 Home exercise programs are as effective as a supervised clinical exercise program in improving function and six-minute walk distance in persons with knee osteoarthritis. 9 Twisting and high-impact activities (e.g., running) should be avoided.
PHARMACOTHERAPY
Acetaminophen and nonsteroidal anti-inflammatory drugs (NSAIDs) improve pain in patients with osteoarthritis and are considered first-line treatments. Randomized controlled trials (RCTs) have shown that acetaminophen is as effective as ibuprofen, regardless of the dosage. 38 , 39 A recent double-blind RCT found that extended-release acetaminophen (1,300 mg three times daily) is effective for knee and hip osteoarthritis pain and is well tolerated. 13 Furthermore, a 2004 systematic review of five RCTs suggested that acetaminophen should be considered initial therapy because it is effective and has fewer adverse effects than NSAIDs. 40 Acetaminophen is especially appropriate as first-line therapy in patients who cannot tolerate NSAIDs. 14 A systematic review of 13 high-quality RCTs concluded that acetaminophen provides modest short-term relief for knee and hip osteoarthritis. 41 It is important to confirm that patients who report lack of benefit have taken acetaminophen continuously and at an adequate dosage.
Selective and nonselective NSAIDs are equally effective in the treatment of osteoarthritis. 7 , 8 A meta-analysis showed that NSAIDs should not be used for long-term treatment, but that limited use is superior to placebo. 42 Because of the gastrointestinal and renal adverse effects associated with nonselective NSAIDs, the lowest effective dosage should be used.
Topical NSAIDs and topical capsaicin are effective in patients with knee osteoarthritis who cannot tolerate oral NSAIDs. Local skin reactions are the most common adverse effects, and systemic adverse effects for both agents were similar to those for placebo. 42 – 44 A 2012 RCT showed that in patients with knee osteoarthritis that was not adequately controlled with NSAIDs, adding a combination of tramadol/acetaminophen significantly improved pain, although neither agent was superior when added alone. 45
Opioid analgesics are an option for patients with symptomatic knee osteoarthritis in whom previous medical management has been ineffective and who are not candidates for total joint arthroplasty. 8 A Cochrane review found low-quality evidence to support the effectiveness of opioids in carefully selected patients. These agents should not be used in patients with a history of substance abuse. 46 Vitamin D supplementation has not been proven beneficial in reducing pain from knee osteoarthritis. 47 The AAOS does not recommend the use of glucosamine/chondroitin supplementation in persons with knee osteoarthritis, 10 and studies have shown mixed benefit. 15 – 17 One recent RCT showed that glucosamine/chondroitin supplementation provided clinically significant pain relief, 18 but Cochrane reviews suggest that glucosamine is no better than placebo. 48 In addition, a Cochrane review of low-quality studies found that chondroitin supplementation only marginally improved pain in patients with osteoarthritis. 49
Intra-articular corticosteroid injections are commonly used in the management of knee osteoarthritis. A Cochrane review showed that although this therapy is effective, pain relief lasts for only one to two weeks. 50 The AAOS does not make a strong recommendation on the use of corticosteroid injections for the treatment of knee osteoarthritis. If used, they should not be given more often than once every three months. 19
Hyaluronic acid injections (viscosupplementation) for the treatment of knee osteoarthritis are controversial. Initial studies and meta-analyses were promising, specifically in patients with severe disease. 51 However, more recent data cite a lack of high-quality studies showing a beneficial effect. A high-quality 2012 systematic review concluded that viscosupplementation provided no clinically significant improvement in pain or function compared with saline or placebo injection. 52 The most recent recommendations from the American College of Rheumatology and Osteoarthritis Research Society International include hyaluronic acid injections in the treatment regimen for osteoarthritis if initial conservative interventions are ineffective. 8 , 20 However, the AAOS does not recommend them for patients with chronic osteoarthritis. 7 Because higher-quality evidence shows a lack of benefit from viscosupplementation, it is best reserved for patients in whom other pharmacologic and nonpharmacologic treatment options are ineffective and who have less advanced osteoarthritis, are poor surgical candidates, or are younger than 65 years. Older patients and those with more severe disease are not likely to respond to viscosupplementation. 51
BRACES, ORTHOSES, AND OTHER THERAPIES
There is little evidence that the use of knee braces causes harm; therefore, it is a reasonable option to consider as part of a multidisciplinary approach to the management of chronic overuse injuries, including knee osteoarthritis. However, the use of a brace should not replace a comprehensive physical therapy or home exercise program that addresses functional deficits in strength and flexibility. Small studies have shown medial unloader valgus braces to be beneficial in patients with predominant medial compartment osteoarthritis. 21 , 22
There is no evidence that orthoses decrease pain or improve function in patients with knee osteoarthritis. 22 A recent study recommended against the use of lateral wedge inserts, which agrees with the recent AAOS guideline. 53 A 2010 Cochrane review on the use of therapeutic ultrasonography for knee osteoarthritis concluded that studies were small and of poor quality, and did not show evidence of clinically or statistically significant benefit. 12
Patellofemoral Pain Syndrome
Physical therapy.
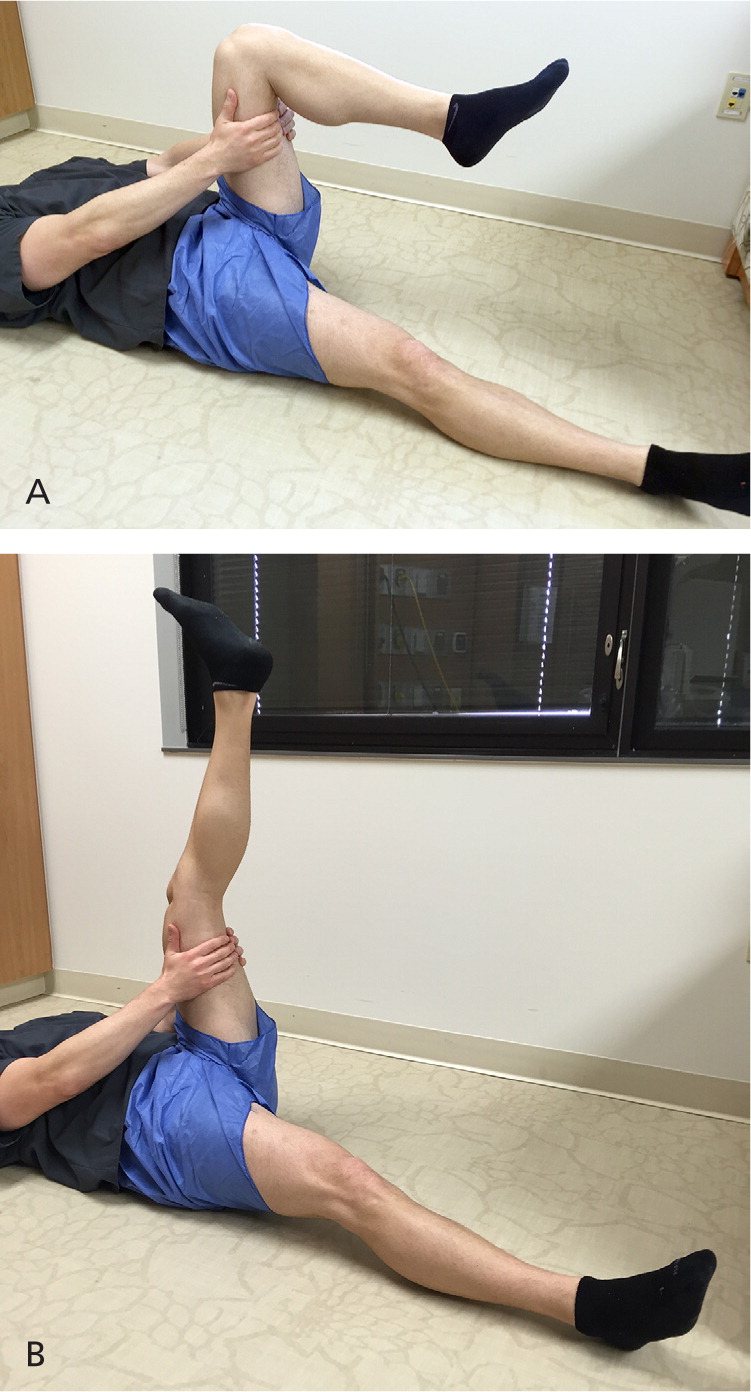
Active treatments, such as strength training and stretching, are the first-line therapies for patellofemoral pain syndrome (PFPS). Strengthening exercises targeting the quadriceps and hip musculature, combined with stretching of the quadriceps, hamstrings, hip abductors, and iliotibial band complex, are often recommended. 23 A Cochrane review concluded that based on low-quality studies, there is likely some benefit for exercise in patients with PFPS, but researchers could not draw conclusions about the most effective modality. 54 Figures 2 through 5 demonstrate stretching and strengthening exercises that are often used in the treatment of PFPS.
Patellar taping has mixed results in the treatment of PFPS. A Cochrane review showed no significant effect on pain, 55 whereas a recent meta-analysis showed that early taping helped improve pain scores. 24 Evidence to support transcutaneous electrical stimulation, biofeedback, or chiropractic manipulation is limited.
Limited data show that NSAIDs are effective in relieving short-term pain from PFPS. 25 Evidence supporting the use of other oral analgesics is lacking.
BRACES AND ORTHOSES
Foot orthoses—with or without physical therapy—are effective for the treatment of anterior knee pain. 56 Lateral tracking of the patella may contribute to the pathology associated with the pain and limited function of PFPS. Although it is common practice to suggest a trial of a lateral buttress patellar brace in patients with PFPS, strong evidence to support this practice is lacking. However, no data suggest that using a brace to determine whether the patient could benefit will result in harm. 26 , 27
Meniscal, Tendon, and Ligament Injuries
Degenerative meniscal tears are common in patients with osteoarthritis. Patients should be referred to an orthopedic surgeon only if mechanical symptoms are present (locking or catching). Physical therapy and a structured exercise program are first-line treatments. 7 Active rehabilitation is as effective as arthroscopy in decreasing pain and improving function in patients with nontraumatic, degenerative medial meniscal tears. 28 A recent study involving patients with concomitant osteoarthritis and meniscal tears showed that physical function scores at six and 12 months were similar in patients who underwent a partial meniscectomy vs. those who completed physical therapy alone. 29 Eccentric exercise has been proven beneficial for treating patellar tendinosis. 30
NSAIDs may provide short-term relief of pain associated with ligamentous tears, including cruciate and collateral ligament tears. Although NSAIDs are effective in decreasing pain and helping patients with ankle sprains return to physical activity, studies have not been performed in patients with ligamentous knee pain, and the effect of NSAID therapy on tendinopathy is uncertain. 31 Although there are no high-quality studies examining the effectiveness of oral analgesics for meniscal tears, it is common practice to use NSAIDs or acetaminophen.
Although physicians should avoid injecting corticosteroids into weight-bearing tendons such as the quadriceps and patellar tendon at the knee, it is accepted practice to provide a local corticosteroid injection over the femoral epicondyle in patients with iliotibial band friction syndrome if conservative measures are ineffective. 32 Regenerative injections, using dextrose-based or platelet-rich plasma, are an emerging option for the care of chronic musculoskeletal conditions if conservative care is ineffective. Regenerative injections have shown modest improvements in pain and function in the treatment of chronic patellar tendinopathy 57 – 59 and osteoarthritis. 60 – 62 Although the results of small studies are promising, further research with large RCTs is needed before definitive recommendations can be made.
Short-term use of a knee immobilizer brace can protect the knee immediately after an acute injury, such as complete major ligament or tendon tears and patellar fracture or dislocation. In patients with grade 1 or 2 medial collateral ligament injuries, minimally restrictive bracing can be helpful when combined with oral analgesics and early physical therapy. 34 Braces commonly used for overuse knee conditions include an iliotibial band strap for patients with iliotibial band friction syndrome or an infrapatellar strap for those with patellar tendinopathy 33 ; however, these braces have not been studied in robust clinical trials. A Cochrane review found insufficient evidence regarding deep friction tissue massage for the treatment of lateral knee tendinitis. 63 Patients with partial anterior cruciate ligament tears may benefit from bracing during the acute injury phase, such as a hinged knee brace coupled with range-of-motion exercises. 35 Patients with full-thickness tears should be referred to an orthopedic surgeon.
Data Sources : We conducted literature searches using Ovid, PubMed, the Cochrane database, Essential Evidence Plus, and guidelines from major orthopedic and rheumatologic organizations, focusing on the keywords knee osteoarthritis, meniscal tears, ligament and tendon tears, patellofemoral syndrome, pharmacotherapy, physical therapy, bracing, orthotics, proinflammatory injections, corticosteroid injections, and hyaluronic acid injections. Search dates: May 30, 2014, to February 4, 2015.
The opinions and assertions contained herein are the private views of the authors and are not to be construed as official or as reflecting the views of the U.S. Air Force Medical Department or the U.S. Air Force at large.
Nguyen US, Zhang Y, Zhu Y, Niu J, Zhang B, Felson DT. Increasing prevalence of knee pain and symptomatic knee osteoarthritis: survey and cohort data. Ann Intern Med. 2011;155(11):725-732.
Baker P, Reading I, Cooper C, Coggon D. Knee disorders in the general population and their relation to occupation. Occup Environ Med. 2003;60(10):794-797.
Cherry DK, Woodwell DA, Rechtsteiner EA; Centers for Disease Control and Prevention. National Ambulatory Medical Care Survey: 2005 summary. http://www.cdc.gov/nchs/data/ad/ad387.pdf . Accessed September 1, 2014.
Buchbinder R, Richards B, Harris I. Knee osteoarthritis and role for surgical intervention: lessons learned from randomized clinical trials and population-based cohorts. Curr Opin Rheumatol. 2014;26(2):138-144.
Mezhov V, Teichtahl AJ, Strasser R, Wluka AE, Cicuttini FM. Meniscal pathology—the evidence for treatment. Arthritis Res Ther. 2014;16(2):206.
Mordecai SC, Al-Hadithy N, Ware HE, Gupte CM. Treatment of meniscal tears: an evidence based approach. World J Orthop. 2014;5(3):233-241.
Brown GA. AAOS clinical practice guideline: treatment of osteoarthritis of the knee: evidence-based guideline, 2nd edition. J Am Acad Orthop Surg. 2013;21(9):577-579.
Hochberg MC, Altman RD, April KT, et al. American College of Rheumatology 2012 recommendations for the use of nonpharmacologic and pharmacologic therapies in osteoarthritis of the hand, hip, and knee. Arthritis Care Res (Hoboken). 2012;64(4):465-474.
Deyle GD, Allison SC, Matekel RL, et al. Physical therapy treatment effectiveness for osteoarthritis of the knee: a randomized comparison of supervised clinical exercise and manual therapy procedures versus a home exercise program. Phys Ther. 2005;85(12):1301-1317.
Brosseau L, Wells GA, Tugwell P, et al. Ottawa Panel evidence-based clinical practice guidelines for the management of osteoarthritis in adults who are obese or overweight. Phys Ther. 2011;91(6):843-861.
Hinman RS, Crossley KM, McConnell J, Bennell KL. Efficacy of knee tape in the management of osteoarthritis of the knee: blinded randomised controlled trial. BMJ. 2003;327(7407):135-138.
Rutjes AW, Nüesch E, Sterchi R, Jüni P. Therapeutic ultrasound for osteoarthritis of the knee or hip. Cochrane Database Syst Rev. 2010;1:CD003132.
Prior MJ, Harrison DD, Frustaci ME. A randomized, double-blind, placebo-controlled 12 week trial of acetaminophen extended release for the treatment of signs and symptoms of osteoarthritis. Curr Med Res Opin. 2014;30(11):2377-2387.
Jawad AS. Analgesics and osteoarthritis: are treatment guidelines reflected in clinical practice?. Am J Ther. 2005;12(1):98-103.
Reichenbach S, Sterchi R, Scherer M, et al. Meta-analysis: chondroitin for osteoarthritis of the knee or hip. Ann Intern Med. 2007;146(8):580-590.
Vlad SC, LaValley MP, McAlindon TE, Felson DT. Glucosamine for pain in osteoarthritis: why do trial results differ?. Arthritis Rheum. 2007;56(7):2267-2277.
Michel BA, Stucki G, Frey D, et al. Chondroitins 4 and 6 sulfate in osteoarthritis of the knee: a randomized, controlled trial. Arthritis Rheum. 2005;52(3):779-786.
Provenza JR, Shinjo SK, Silva JM, Peron CR, Rocha FA. Combined glucosamine and chondroitin sulfate, once or three times daily, provides clinically relevant analgesia in knee osteoarthritis [published ahead of print August 3, 2014]. July 8, 2015.
Jones T, Kelsberg G, Safranek S. FPIN's clinical inquiries: Intra-articular corticosteroid injections for osteoarthritis of the knee. Am Fam Physician. 2014;90(2):115-116.
Zhang W, Nuki G, Moskowitz RW, et al. OARSI recommendations for the management of hip and knee osteoarthritis: part III: Changes in evidence following systematic cumulative update of research published through January 2009. Osteoarthritis Cartilage. 2010;18(4):476-499.
Kirkley A, Webster-Bogaert S, Litchfield R, et al. The effect of bracing on varus gonarthrosis. J Bone Joint Surg Am. 1999;81(4):539-548.
Brouwer RW, Jakma TS, Verhagen AP, Verhaar JA, Bierma-Zeinstra SM. Braces and orthoses for treating osteoarthritis of the knee. Cochrane Database Syst Rev. 2005;1:CD004020.
Rixe JA, Glick JE, Brady J, Olympia RP. A review of the management of patellofemoral pain syndrome. Phys Sportsmed. 2013;41(3):19-28.
Barton C, Balachandar V, Lack S, Morrissey D. Patellar taping for patellofemoral pain: a systematic review and meta-analysis to evaluate clinical outcomes and biomechanical mechanisms. Br J Sports Med. 2014;48(6):417-424.
Heintjes E, Berger MY, Bierma-Zeinstra SM, Bernsen RM, Verhaar JA, Koes BW. Pharmacotherapy for patellofemoral pain syndrome. Cochrane Database Syst Rev. 2004;3:CD003470.
D'hondt NE, Struijs PA, Kerkhoffs GM, et al. Orthotic devices for treating patellofemoral pain syndrome. Cochrane Database Syst Rev. 2002;2:CD002267.
Bizzini M, Childs JD, Piva SR, Delitto A. Systematic review of the quality of randomized controlled trials for patellofemoral pain syndrome. J Orthop Sports Phys Ther. 2003;33(1):4-20.
Herrlin S, Hållander M, Wange P, Weidenhielm L, Werner S. Arthroscopic or conservative treatment of degenerative medial meniscal tears: a prospective randomised trial. Knee Surg Sports Traumatol Arthrosc. 2007;15(4):393-401.
Katz JN, Brophy RH, Chaisson CE, et al. Surgery versus physical therapy for a meniscal tear and osteoarthritis. N Engl J Med. 2013;368(18):1675-1684.
Visnes H, Bahr R. The evolution of eccentric training as treatment for patellar tendinopathy (jumper's knee): a critical review of exercise programmes. Br J Sports Med. 2007;41(4):217-223.
Mehallo CJ, Drezner JA, Bytomski JR. Practical management: nonsteroidal antiinflammatory drug (NSAID) use in athletic injuries. Clin J Sport Med. 2006;16(2):170-174.
Gunter P, Schwellnus MP. Local corticosteroid injection in iliotibial band friction syndrome in runners: a randomised controlled trial. Br J Sports Med. 2004;38(3):269-272.
Lavagnino M, Arnoczky SP, Dodds J, Elvin N. Infrapatellar straps decrease patellar tendon strain at the site of the jumper's knee lesion: a computational analysis based on radiographic measurements. Sports Health. 2011;3(3):296-302.
Azar FM. Evaluation and treatment of chronic medial collateral ligament injuries of the knee. Sports Med Arthrosc. 2006;14(2):84-90.
DeFranco MJ, Bach BR. A comprehensive review of partial anterior cruciate ligament tears. J Bone Joint Surg Am. 2009;91(1):198-208.
Bennell KL, Hunter DJ, Hinman RS. Management of osteoarthritis of the knee. BMJ. 2012;345:e4934.
Martin SN, McGowan HJ, Smith RF. Exercise for the treatment of knee osteoarthritis. Am Fam Physician. 2011;84(5):1. Accessed May 6, 2015. https://www.aafp.org/afp/2011/0901/od1.html
Bradley JD, Brandt KD, Katz BP, Kalasinski LA, Ryan SI. Comparison of an antiinflammatory dose of ibuprofen, an analgesic dose of ibuprofen, and acetaminophen in the treatment of patients with osteoarthritis of the knee. N Engl J Med. 1991;325(2):87-91.
Verkleij SP, Luijsterburg PA, Bohnen AM, Koes BW, Bierma-Zeinstra SM. NSAIDs vs acetaminophen in knee and hip osteoarthritis: a systematic review regarding heterogeneity influencing the outcomes. Osteoarthritis Cartilage. 2011;19(8):921-929.
Wegman A, van der Windt D, van Tulder M, Stalman W, de Vries T. Nonsteroidal antiinflammatory drugs or acetaminophen for osteoarthritis of the hip or knee? A systematic review of evidence and guidelines. J Rheumatol. 2004;31(2):344-354.
Machado GC, Maher CG, Ferreira PH, et al. Efficacy and safety of paracetamol for spinal pain and osteoarthritis: systematic review and meta-analysis of randomised placebo controlled trials. BMJ. 2015;350:h1225.
Derry S, Moore RA, Rabbie R. Topical NSAIDs for chronic musculoskeletal pain in adults. Cochrane Database Syst Rev. 2012;9:CD007400.
Massey T, Derry S, Moore RA, McQuay HJ. Topical NSAIDs for acute pain in adults. Cochrane Database Syst Rev. 2010;6:CD007402.
Mason L, Moore RA, Derry S, Edwards JE, McQuay HJ. Systematic review of topical capsaicin for the treatment of chronic pain. BMJ. 2004;328(7446):991.
Park KS, Choi JJ, Kim WU, Min JK, Park SH, Cho CS. The efficacy of tramadol/acetaminophen combination tablets (Ultracet ® ) as add-on and maintenance therapy in knee osteoarthritis pain inadequately controlled by nonsteroidal anti-inflammatory drug (NSAID). Clin Rheumatol. 2012;31(2):317-323.
Noble M, Treadwell JR, Tregear SJ, et al. Long-term opioid management for chronic noncancer pain. Cochrane Database Syst Rev. 2010(1):CD006605.
McAlindon T, LaValley M, Schneider E, et al. Effect of vitamin D supplementation on progression of knee pain and cartilage volume loss in patients with symptomatic osteoarthritis: a randomized controlled trial. JAMA. 2013;309(2):155-162.
Towheed TE, Maxwell L, Anastassiades TP, et al. Glucosamine therapy for treating osteoarthritis. Cochrane Database Syst Rev. 2005;2:CD002946.
Singh JA, Noorbaloochi S, MacDonald R, Maxwell LJ. Chondroitin for osteoarthritis. Cochrane Database Syst Rev. 2015;1:CD005614.
Bellamy N, Campbell J, Robinson V, Gee T, Bourne R, Wells G. Intraarticular corticosteroid for treatment of osteoarthritis of the knee. Cochrane Database Syst Rev. 2006;2:CD005328.
Divine JG, Shaffer MD. Use of viscosupplementation for knee osteoarthritis: an update. Curr Sports Med Rep. 2011;10(5):279-284.
Rutjes AW, Jüni P, da Costa BR, Trelle S, Nüesch E, Reichenbach S. Viscosupplementation for osteoarthritis of the knee: a systematic review and meta-analysis. Ann Intern Med. 2012;157(3):180-191.
Parkes MJ, Maricar N, Lunt M, et al. Lateral wedge insoles as a conservative treatment for pain in patients with medial knee osteoarthritis: a meta-analysis. JAMA. 2013;310(7):722-730.
van der Heijden RA, Lankhorst NE, van Linschoten R, Bierma-Zeinstra SM, van Middelkoop M. Exercise for treating patellofemoral pain syndrome. Cochrane Database Syst Rev. 2015;1:CD010387.
Callaghan MJ, Selfe J. Patellar taping for patellofemoral pain syndrome in adults. Cochrane Database Syst Rev. 2012;4:CD006717.
Collins NJ, Bisset LM, Crossley KM, Vicenzino B. Efficacy of nonsurgical interventions for anterior knee pain: systematic review and meta-analysis of randomized trials. Sports Med. 2012;42(1):31-49.
Ryan M, Wong A, Rabago D, Lee K, Taunton J. Ultrasound-guided injections of hyperosmolar dextrose for overuse patellar tendinopathy: a pilot study. Br J Sports Med. 2011;45(12):972-977.
Mautner K, Colberg RE, Malanga G, et al. Outcomes after ultrasound-guided platelet-rich plasma injections for chronic tendinopathy: a multicenter, retrospective review. PM R. 2013;5(3):169-175.
Filardo G, Kon E, Della Villa S, Vincentelli F, Fornasari PM, Marcacci M. Use of platelet-rich plasma for the treatment of refractory jumper's knee. Int Orthop. 2010;34(6):909-915.
Rabago D, Patterson JJ, Mundt M, et al. Dextrose prolotherapy for knee osteoarthritis: a randomized controlled trial [published correction appears in Ann Fam Med . 2013;11(5):480]. Ann Fam Med. 2013;11(3):229-237.
Kon E, Mandelbaum B, Buda R, et al. Platelet-rich plasma intra-articular injection versus hyaluronic acid viscosupplementation as treatments for cartilage pathology: from early degeneration to osteoarthritis. Arthroscopy. 2011;27(11):1490-1501.
Patel S, Dhillon MS, Aggarwal S, Marwaha N, Jain A. Treatment with platelet-rich plasma is more effective than placebo for knee osteoarthritis: a prospective, double-blind, randomized trial. Am J Sports Med. 2013;41(2):356-364.
Loew LM, Brosseau L, Tugwell P, et al. Deep transverse friction massage for treating lateral elbow or lateral knee tendinitis. Cochrane Database Syst Rev. 2014;11:CD003528.
Continue Reading

More in AFP
More in pubmed.
Copyright © 2015 by the American Academy of Family Physicians.
This content is owned by the AAFP. A person viewing it online may make one printout of the material and may use that printout only for his or her personal, non-commercial reference. This material may not otherwise be downloaded, copied, printed, stored, transmitted or reproduced in any medium, whether now known or later invented, except as authorized in writing by the AAFP. See permissions for copyright questions and/or permission requests.
Copyright © 2024 American Academy of Family Physicians. All Rights Reserved.
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Current issue
- BMJ Journals
You are here
- Volume 60, Issue 2
- Knee pain and osteoarthritis in older adults: a review of community burden and current use of primary health care
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- R McCarney ,
- Primary Care Sciences Research Centre, Keele University, UK
- Dr G Peat, Primary Care Sciences Research Centre, School of Postgraduate Medicine, Keele University, The Medical Institute, Hartshill Road, Stoke-on-Trent ST7 4NY, UK g.m.peat{at}hfac.keele.ac.uk
BACKGROUND Osteoarthritis is the single most common cause of disability in older adults, and most patients with the condition will be managed in the community and primary care.
AIM To discuss case definition of knee osteoarthritis for primary care and to summarise the burden of the condition in the community and related use of primary health care in the United Kingdom.
DESIGN Narrative review.
METHOD A literature search identified studies of incidence and prevalence of knee pain, disability, and radiographic osteoarthritis in the general population, and data related to primary care consultations. Findings from UK studies were summarised with reference to European and international studies.
RESULTS During a one year period 25% of people over 55 years have a persistent episode of knee pain, of whom about one in six in the UK and the Netherlands consult their general practitioner about it in the same time period. The prevalence of painful disabling knee osteoarthritis in people over 55 years is 10%, of whom one quarter are severely disabled.
CONCLUSION Knee osteoarthritis sufficiently severe to consider joint replacement represents a minority of all knee pain and disability suffered by older people. Healthcare provision in primary care needs to focus on this broader group to impact on community levels of pain and disability.
- knee osteoarthritis
- epidemiology
- primary care
https://doi.org/10.1136/ard.60.2.91
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
Read the full text or download the PDF:
Bicompartmental Knee Arthroplasty: a systematic review and Delphi consensus from the European Knee Society
- Knee Arthroplasty
- Published: 09 August 2024
Cite this article

- Stefano Campi ORCID: orcid.org/0000-0002-7544-7427 1 , 2 ,
- Gareth Jones 3 ,
- Fabian von Knoch 4 ,
- Alexandre Lunebourg 5 ,
- David Barrett 6 , 7 ,
- Nick London 8 , 9 &
- Jean-Noel Argenson 10 , 11
26 Accesses
Explore all metrics
This is a preview of subscription content, log in via an institution to check access.
Access this article
Subscribe and save.
- Get 10 units per month
- Download Article/Chapter or eBook
- 1 Unit = 1 Article or 1 Chapter
- Cancel anytime
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions

Willis-Owen CA, Brust K, Alsop H, Miraldo M, Cobb JP (2009) Unicondylar knee arthroplasty in the UK National Health Service: an analysis of candidacy, outcome and cost efficacy. Knee 16:473–478
Article PubMed Google Scholar
National Institute for Health and Care Exellence (NICE) (2020) Joint replacement (primary): hip, knee and shoulder [NICE Guideline NG157], pp 1–75
Garner A, Van Arkel RJ, Cobb J (2019) Classification of combined partial knee arthroplasty. Bone Jt J 101 B:922–928
Article Google Scholar
Yamabe E et al (2013) Study of surgical indication for knee arthroplasty by cartilage analysis in three compartments using data from Osteoarthritis Initiative (OAI). BMC Musculoskelet Disord 14:1
Berger RA et al (2005) Results of unicompartmental knee arthroplasty at a minimum of ten years of follow-up. J Bone Jt Surg 87:999–1006
Reed M et al (2022) 19th annual report 2022: National Joint Registry for England, Wales, Northern Ireland and the Isle of Man
Elbardesy H et al (2021) Does bicompartmental knee arthroplasty hold an advantage over total knee arthroplasty? Systematic review and meta-analysis. Sicot J 7:38
Article PubMed PubMed Central Google Scholar
Kooner S, Johal H, Clark M (2017) Bicompartmental knee arthroplasty vs total knee arthroplasty for the treatment of medial compartment and patellofemoral osteoarthritis. Arthroplasty Today 3:309–314
Palumbo BT et al (2011) Initial experience of the journey-deuce bicompartmental knee prosthesis: a review of 36 cases. J Arthroplasty 26:40–45
Brown D (2020) A review of the PubMed PICO tool: using evidence-based practice in health education. Health Promot Pract 21:496–498
Slim K et al (2003) Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg 73:712–716
Cats-Baril W et al (2013) International consensus on periprosthetic joint infection: description of the consensus process. Clin Orthop Relat Res 471:4065–4075
Bori G et al (2019) Hip and knee section, treatment, prosthesis factors: proceedings of international consensus on orthopedic infections. J Arthroplasty 34:S453–S457
Linstone HA, Turoff M (1975) The Delphi method: techniques and applications. The Delphi method: techniques and applications. Addison-Wesley, Boston
Google Scholar
Schrednitzki D, Beier A, Marx A, Halder AM (2020) No major functional benefit after bicompartmental knee arthroplasty compared to total knee arthroplasty at 5-year follow-up. J Arthroplasty 35:3587–3593
Goh JKM et al (2020) Ten year outcomes for the prospective randomised trial comparing unlinked, modular bicompartmental knee arthroplasty and total knee arthroplasty. Knee 27:1914–1922
Parratte S et al (2015) Is knee function better with contemporary modular bicompartmental arthroplasty compared to total knee arthroplasty? Short-term outcomes of a prospective matched study including 68cases. Orthop Traumatol Surg Res 101:547–552
Article PubMed CAS Google Scholar
Shah S, Dutton A, Liang S, Dasde S (2013) Bicompartmental versus total knee arthroplasty for medio-patellofemoral osteoarthritis: a comparison of early clinical and functional outcomes. J Orthop Surg (Hong Kong) 21:281–284
Tan SM, Dutton AQ, Bea KC, Kumar VP (2013) Bicompartmental versus total knee arthroplasty for medial and patellofemoral osteoarthritis. J Orthop Surg (Hong Kong) 21:281–284
Morrison TA, Nyce JD, Macaulay WB, Geller JA (2011) Early adverse results with bicompartmental knee arthroplasty: a prospective cohort comparison to total knee arthroplasty. J Arthroplasty 26:35–39
Benazzo F, Rossi SMP, Ghiara M (2014) Partial knee arthroplasty: patellofemoral arthroplasty and combined unicompartmental and patellofemoral arthroplasty implants—general considerations and indications, technique and clinical experience. Knee 21:S43–S46
Rossi SMP, Perticarini L, Clocchiatti S, Ghiara M, Benazzo F (2021) Mid-to long-term follow-up of combined small implants: a third-generation patellofemoral arthroplasty associated with a medial or lateral unicompartmental knee arthroplasty. Bone Jt J 103:840–845
Kamath AF, Levack A, John T, Thomas BS, Lonner JH (2014) Minimum two-year outcomes of modular bicompartmental knee arthroplasty. J Arthroplasty 29:75–79
Tamam C, Plate JF, Augart M, Poehling GG, Jinnah RH (2015) Retrospective clinical and radiological outcomes after robotic assisted bicompartmental knee arthroplasty. Adv Orthop 2015
Yeo NEM et al (2015) Prospective randomised trial comparing unlinked, modular bicompartmental knee arthroplasty and total knee arthroplasty: a five years follow-up. Knee 22:321–327
Biazzo A, Silvestrini F, Manzotti A, Confalonieri N (2019) Bicompartmental (uni plus patellofemoral) versus total knee arthroplasty: a match-paired study. Musculoskelet Surg 103:63–68
Al-Dadah O, Hawes G, Chapman-Sheath PJ, Tice JW, Barrett DS (2020) Unicompartmental vs. segmental bicompartmental vs. total knee replacement: comparison of clinical outcomes. Knee Surg Relat Res 32:1–11
Wang B, Sun H, Fu Z, Kang J, Yu X (2021) Application of unicompartmental knee arthroplasty in the treatment of knee osteoarthritis. Arthroplasty 3:1–7
Waldstein W, Kasparek MF, Faschingbauer M, Windhager R, Boettner F (2017) Lateral-compartment osteophytes are not associated with lateral-compartment cartilage degeneration in arthritic varus knees. Clin Orthop Relat Res 475:1386–1392
Faschingbauer M, Renner L, Waldstein W, Boettner F (2015) Are lateral compartment osteophytes a predictor for lateral cartilage damage in varus osteoarthritic knees? Data from the osteoarthritis initiative. Bone Jt J 97B:1634–1639
Kozinn SC, Marx C, Scott RD (1989) Unicompartmental knee arthroplasty: a 4.5–6-year follow-up study with a metal-backed tibial component. J Arthroplasty 4:S1–S9
Berend KR et al (2015) Consensus statement on indications and contraindications for medial unicompartmental knee arthroplasty. J Surg Orthop Adv 24:252
PubMed Google Scholar
Bull D et al (2022) Medial/central PF arthritis and functionally stable ACL deficiency do not compromise outcomes of fixed-bearing medial UKA. Knee 35:8–15
Beard DJ et al (2007) The influence of the presence and severity of pre-existing patellofemoral degenerative changes on the outcome of the Oxford medial unicompartmental knee replacement. J Bone Jt Surg Ser B 89:1597–1601
Article CAS Google Scholar
Crawford DA, Berend KR, Lombardi AV (2018) Management of the failed medial unicompartmental knee arthoplasty. J Am Acad Orthop Surg 26(20):e426-e433
Mancuso F, Dodd CA, Murray DW, Pandit H (2016) Medial unicompartmental knee arthroplasty in the ACL-deficient knee. J Orthop Traumatol 17:267–275
Calixto NE et al (2015) Examining the relationship between degenerative anterior cruciate ligament lesions and patellofemoral cartilage integrity with quantitative magnetic resonance imaging parameters. Osteoarthr Cartil 23:A214–A216
Marx R, Jones E (2005) Measuring improvement following total hip and knee arthroplasty using patient-based measures of outcome. J Bone Jt Surg Am 87-A:1999–2005
Amstutz HC, Le Duff MJ (2019) Infographic: effects of physical activity on long-term survivorship after metal-on-metal hip resurfacing arthroplasty: is it safe to return to sports? Bone Jt J 101-B:1184–1185
Larsson A, Rolfson O, Kärrholm J (2019) Evaluation of Forgotten Joint Score in total hip arthroplasty with Oxford Hip Score as reference standard. Acta Orthop 90:253–257
Steinhoff AK, Bugbee WD (2016) Knee Injury and Osteoarthritis Outcome Score has higher responsiveness and lower ceiling effect than Knee Society Function Score after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 24:2627–2633
Chung JY, Min BH (2013) Is bicompartmental knee arthroplasty more favourable to knee muscle strength and physical performance compared to total knee arthroplasty? Knee Surg Sports Traumatol Arthrosc 21:2532–2541
Mittal A, Meshram P, Kim WH, Kim TK (2020) Unicompartmental knee arthroplasty, an enigma, and the ten enigmas of medial UKA. J Orthop Traumatol 21
Download references
The authors did not receive support from any organization for the submitted work.
Author information
Authors and affiliations.
Department of Medicine and Surgery, Università Campus Bio-Medico di Roma, Via Alvaro del Portillo, 21, 00128, Rome, Italy
Stefano Campi
Fondazione Policlinico Universitario Campus Bio-Medico, Via Alvaro del Portillo, 200, 00128, Rome, Italy
MSk Lab, Imperial College London, White City Campus, London, W12 0BZ, UK
Gareth Jones
Zurich Bone and Joint Center, Zurich, Switzerland
Fabian von Knoch
CCAL, Yverdon Hospital, 1400, Yverdon-les-Bains, Switzerland
Alexandre Lunebourg
School of Engineering Science, University of Southampton, Southampton, UK
David Barrett
King Edward VII Hospital, London, UK
Yorkshire Knee Clinic, Leeds, UK
Nick London
Leeds Beckett University (Carnegie School of Sport), Leeds, UK
Department of Orthopedics and Traumatology, Institute for Locomotion, Aix-Marseille University, 270 Boulevard Sainte Marguerite, BP 29, 13274, Marseille, France
Jean-Noel Argenson
Institute for Locomotion, CNRS 5, St. Marguerite Hospital, 270 Boulevard Sainte Marguerite, BP 29, 13274, Marseille, France
You can also search for this author in PubMed Google Scholar
Contributions
SC has received consultant honoraria from Smith and Nephew, Medacta and Stryker. FvK has received consultant honoraria from Zimmer Biomet and Depuy Synthes. AL has received consultant honoraria from Zimmer Biomet and Lima. DB has received royalties from Depuy Synthes. NL has received consultant honoraria/royalties from Zimmer-Biomet and Eventum and own shares in Eventum. JNA has received consultant honoraria/royalties from Zimmer-Biomet. JNA is in the Board of Journal of Arthroplasty, APCORT (Chair, Board of Trustees).
Corresponding author
Correspondence to Stefano Campi .
Ethics declarations
Conflict of interest.
The conflict of interest of the authors are reported in the conflict of interest statement.
Ethical approval
No ethical approval was required for this type of study.
Informed consent
No informed consent was required for this study, as it does not involve human subjects.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Campi, S., Jones, G., von Knoch, F. et al. Bicompartmental Knee Arthroplasty: a systematic review and Delphi consensus from the European Knee Society. Arch Orthop Trauma Surg (2024). https://doi.org/10.1007/s00402-024-05434-y
Download citation
Received : 07 January 2024
Accepted : 27 June 2024
Published : 09 August 2024
DOI : https://doi.org/10.1007/s00402-024-05434-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Bicompartmental knee arthroplasty
- Partial knee arthroplasty
- Patellofemoral joint replacement
- Find a journal
- Publish with us
- Track your research

Literature review of the causes of pain following total knee replacement surgery: prosthesis, inflammation and arthrofibrosis
- Download PDF
Adverse knee pain occurs in 10–34% of all total knee replacements (TKR), and 20% of TKR patients experience more pain post-operatively than pre-operatively. Knee pain is amongst the top five reasons for knee replacement revision in the United Kingdom. The number of TKRs is predicted to continue increasing due to the ageing population.
A narrative literature review was performed on the different causes of pain following TKR. A database search on Scopus, PubMed, and Google Scholar was conducted to look for articles related to TKR, pain, and cause. Articles were selected based on relevance, publication date, quality of research and validation. Relevant sections were added to the review.
One hundred and fourteen articles were identified and potential causes of TKR pain included: arthrofibrosis, aseptic loosening, avascular necrosis, central sensitization, component malpositioning, infection, instability, nerve damage, overstuffing, patellar maltracking, polyethylene wear, psychological factors and unresurfaced patella.
It is important to tailor our approach to address the individual causes of pain. Certain controllable risk factors can be managed pre-operatively to minimize post-operative pain. Risk factors help to predict adverse pain outcomes and identify specific causes.
There are multiple causes of pain following TKR. Some factors will require further extensive studies, and as pain is a commonly attributed reason for TKR revision, its underlying aetiologies should be explored. Understanding these factors helps to develop effective methods for diagnosis, prevention and management of TKR pain, which help to improve patient outcomes.
Cite this article: EFORT Open Rev 2020;5:534-543. DOI: 10.1302/2058-5241.5.200031
- Introduction
Total knee replacement (TKR) is a cost-effective surgical procedure. 1 According to the national joint registry, 2 274,495 total knee replacements were performed in England, Wales, Northern Ireland and the Isle of Man in 2016–2018. The majority of TKR in 2018 were cemented, unconstrained fixed TKR (60.8%); followed by cemented, posterior-stabilized fixed TKR (19.8%). By 2030, TKR demand is predicted to increase six-fold from its demand in 2005 in line with the increasingly ageing population. 3
The most common indication for TKR is osteoarthritis (OA). 1 In 2018, 96.2% of primary knee replacements were conducted solely due to osteoarthritis. 2 TKR helps to improve quality of life and function in end-stage, symptomatic osteoarthritis patients. 4 – 7 However, 10–34% of TKR patients receive adverse pain outcomes between three months and five years following surgery and around 20% of TKR patients experience more knee pain and swelling than before surgery. 8 – 10 Despite advancements in surgical techniques, prostheses, pain control, and medical care, there is evidence to suggest worsening pain and functional scores of some patients over time following TKR surgery. 11
In 2018, 6,357 revision knee joint operations were conducted compared to 4,417 revisions in 2008 in England, Wales, Northern Ireland and the Isle of Man. The most common causes for knee replacement revision in 2018 in descending order are aseptic loosening/lysis, infection, pain, progressive arthritis, and instability; knee pain continues to be one of the top five reasons for revision surgery. 2 A retrospective study by Erivan R et al 12 showed that in patients with unexplained chronic knee pain following TKR, 4.5% of cases were caused by infection, 2.7% were due to instability without real dislocation, 1.8% were due to placement error from rotational problems, 22.3% were due to loosening in tibia and femoral components, 8.0% were due to polyethylene wear, 33.9% were due to periarticular involvement with quadricep deficiency, iliotibial tendinitis, pes bursitis, stiffness or prepatellar bursitis, 18.8% were due to projected pain, 2.7% were due to complex regional pain syndrome and 6.3% had no explaining diagnosis. Following the report by Preston et al 13 on the aetiologies of pain following TKR, newer evidence has surfaced to explain the process of pain development following TKR. This review aims to examine the causes of pain following TKR, assessing previous research in light of new evidence.
- Materials and methods
A literature review on the causes of pain following total knee replacements was performed based on research papers published up to 1 April 2020. A database search on Scopus, PubMed and Google Scholar was conducted to look for articles in English with the search terms “total knee replacement”, “pain”, and “cause”. The initial search yielded over 1,000 articles. One hundred and fourteen relevant articles were ultimately selected based on relevance, recentness, quality of research and citations. Fig. 1 summarizes the methods of research.

Flowchart showing how articles were selected and reviewed.
Citation: EFORT Open Reviews 5, 9; 10.1302/2058-5241.5.200031
- Download Figure
- Download figure as PowerPoint slide
- Arthrofibrosis
Arthrofibrosis is the excessive production of collagen and adhesions which contributes to pain and restrictive joint motion. 14 Of TKR patients, 3–10% develop arthrofibrosis after TKR and report pain with activities from < 30% for light manual work to 78% for jumping and pivoting. 15 – 18 Pathological development of fibrosis can also be seen in multiple organs following wound healing by fibroblasts. 19 – 21 TGF-β1 is an important mediator causing fibrosis in multiple organs, and this has also been increased in arthrofibrosis. 22 TGF-β1 has been known to increase expression of α-smooth muscle actin (α-SMA) which causes the activation of fibroblasts as well as other fibrotic associated proteins, e.g. collagen I/III, fibronectin. 23 With increased fibrotic gene expression in fibroblasts caused by TGF-β1, they can also modulate their behaviours to changes in the microenvironment. 23
Following TKR, receptors TLR3, TLR4, IL1-R1 are expressed in the infrapatellar fat and synovial membrane, where the strongest expression is by IL-1R1 and this is induced to produce an inflammatory process in response to IL-1α and IL-1β. 23 Pain in a knee with arthrofibrosis can also be caused by femoropatellar joint impairment from increased pressure from peripatellar scar tissues. This in turn leads to joint overload and structural changes, e.g. cartilage destruction. 24 Of patients with arthrofibrosis, 79% also develop osteoarthritis 5.7 years following surgery, which can lead to a painful joint. 25 Pain in arthrofibrosis can also be attributed to reflex sympathetic dystrophy which is a spontaneous regional pain that happens in 15.2% of patients. 24
Fibrous adhesions (abnormal tissue connections) are also correlated to intermittent pain, inflammation, loss of function and progressive joint degeneration. 26 , 27 There has been evidence to show fibroblasts under inflammation cause monocyte recruitment through the production of the C-C motif chemokine ligand 2 (CCL2) and that levels of CCL2 are associated with reported pain. CCL2 expression (dependant on NFkB) is also stimulated by IL-1α which might explain persistent fibrosis that causes inflammation in response to IL-1α immune triggers. Sensory neurones contain C-C chemokine receptor type 2 (CCR2) and this engages with CCL2 to cause excitation of the nociceptive neurones that can lead to pain sensation. 28 – 31 Following TKR, three anatomical parts of the knee have been found to express increased proinflammatory states. These are the infrapatellar fat pad, synovial membrane, and synovial fluid. Other inflammatory markers are increased in all these sites where IL-8 is the most induced. 32
- Instability
Thirty-two per cent of patients reported knee instability with activity limitation and pain six months following TKR. 33 A study by Leichtenberg et al 34 showed that 76% and 21% of patients reported instability before and at one year following TKR, respectively. Patients who retained instability also reported significantly more pain, poorer quality of life and increased activity limitation. Results show that 25% of patients with pre-operative instability retain the instability one year after TKR. This correlation between instability and knee pain has also been supported by other previous studies. 33 , 35 – 37
Flexion instability occurs when there is an imbalance of flexion and extension, leading to hemarthrosis, swelling, knee pain and giving way. 38 Flexion instability can be caused by tissue insufficiencies such as ligament injury or implant failure. 39 Excessive release of the medial ligament, inadequate distal femoral resection, excessive tibial slope, internal rotation of components and an undersized femoral component can also lead to flexion instability. 38 – 41 A study by Lewallen et al 42 showed increased extracellular matrix (ECM) remodelling gene expression in TKR patients with flexion instability and also suggested a correlation between ECM degradation and exposure of oxidative stress during tissue remodelling and inflammation.
A retrospective study by Sharma 43 defined mid-flexion instability as the restraint of the posterior knee capsule. The main contributors include the excessive release of the medial collateral ligament (a stabilizer between 30–60 degrees of motion) anteriorly, and malpositioning of the implant to epicondyles that causes malfunctioning of the tibial post-femoral geometry.
In a systematic review by Rouquette et al 44 exploring the causes of tibiofemoral dislocation (a rare but serious form of instability) after TKR, key factors for tibiofemoral dislocation included comorbidities such as obesity and pre-operative deformity, and intra-operative iatrogenic destabilization. Higher rates of dislocation recurrence were associated with non-operative management such as splints.
A study by Slane et al 45 demonstrated an increase in patellar tendon buckling in post-TKR patients compared to the control. These patients also exhibited larger buckling angle, magnitude, and amplitude. Lower distal buckling angles are also correlated with better Knee Society Scores. Buckling happens when the tendon ruffles back on itself when extended or moved passively, and many factors can contribute to this including patella positioning, infrapatellar fat pad resection (increasing joint space for buckling), alteration in patellar tracking following TKR and trauma from surgery. Greater increase in tendon buckling is known to increase knee instability and reduce the ability to reach full extension. 46 – 48 Factors to consider are that patients with OA might already have differences in patellar tendon buckling as OA leads to weakness in the quadriceps due to the anatomical function of the patellar tendon as part of a muscle unit. 45 , 49
- Component malpositioning
TKR consists of the femoral and tibial components within the knee (a hinge joint). These articulate with each other and between the patellar and femoral surfaces within the patellofemoral joint. The femoral component articulates with the total polyethylene tibial component, tibial base plate and the polyethylene surface which allows flexion and extension with a slight lateral/medial motion. 50
The causes of post-TKR pain can be attributed to modified kinematics, alteration of ligament tensions and increased retro patellar pressure which commonly leads to anterior knee pain. 51 – 54 Poor component positioning affects the kinematic part of the knee, which also increases the risk of instability and the chance of polyethylene wear. 55 – 57 Component positions also influence ligament tension in in vitro studies. 58 , 59
Some clinical observation studies have shown that the internal rotation of the femoral implant component may contribute to patellofemoral pain syndrome. 60 – 62 While internal rotation increases the stress that contributes to anterior knee pain, external rotation of the trochlear groove and femoral component reduces the retro patellar tension and therefore decreases pain. 63
A study by Fottner et al 64 has found that, using computer simulation, malpositioning of the tibial baseplate component mostly affects ligament tension (posterior cruciate and collateral ligaments) which influences the tibia and femur kinematics and their contact forces. This has its effect on poorer clinical outcomes following surgery, including pain, higher rate of early loosening, instability and reduced range of motion. Regarding kinematics, the greatest changes were observed in tibiofemoral rotation. Tibiofemoral rollback was also influenced by translation medially and laterally, with medialization having the greatest effect. A study by Nicoll et al 65 showed that internal rotation errors of the tibial implant are associated with medial and anterior knee pain and suggested that the location happens either at the central part of the tibial tubercle or talus.
- Aseptic loosening
According to studies by Dalury et al and Schroer et al, 66 , 67 aseptic loosening is one of the leading causes for revision after TKR. It affects patients up to 20 years after surgery. It is, however, one of the least understood TKR failure mechanisms. Various factors can lead to aseptic loosening. These include instability, component malpositioning, and osteolysis secondary to polyethylene wear. Osteolysis involves the generation of debris from polyethylene wear and metal and cement particles which generate an immunological response upon access to the bone–implant interface. Loose locking mechanisms, backside wear and micromotion increase modularity and therefore increase wear particle generation.
Other studies from Crotti et al and Gehrke et al 68 , 69 explained the immunological response is commenced by macrophages that phagocytose any small wear particles < 5 μm in diameter, and this induces the release of interleukin-1ß (IL-1ß) and tumour necrosis factor-α. These stimulate the recruitment and activation of osteoclasts via the RANK-L pathway and thus osteolysis occurs adjacent to the bone–implant interfaces. This may be followed by prosthesis micromotion and further debris particle dissemination. It is unclear whether these biological processes are solely responsible for the loosening of the joint.
Osteolysis is more common in the tibial compartment due to its relation to the polyethylene insert, gravity and the use of screws for fixation which facilitate wear particle migration into the bone. 70 The access of the bone particles to the bone–implant surface is more frequent on, but not restricted to, cementless components. According to a study by Goodman, 71 the wear rate of polyethylene is affected by multiple factors including manufacturing and sterilization methods, backside wear, alignment and stability of the TKR and patient activity level. Malalignment results in asymmetric loading and early loosening and is more common with varus formations.
A study by Math et al 72 suggested aseptic loosening is usually painless in the early stages of the disease, but activity-related pain localized to the tissues surrounding the loose components may develop, particularly on weight-bearing. Tibial osteolysis is readily visible on anteroposterior (AP) radiographs with a radiolucent area around the implant or cement, varus or valgus subsidence of the tibial component, cement fragmentation and progressive widening of the cement–bone or bone–prosthesis interface.
- Patellar maltracking
Patellar maltracking is the disproportional relationship in the trochlea and the patella which is associated with an abnormal anatomical change. 73 The patellofemoral joint is high in complexity and involves the multidirectional (mostly cranial and caudal) articulations between the patellar and the femoral groove. It also consists of the muscles and ligaments which act on the patella for stability and tracking. 50 The patella does not remain in the femoral groove during knee movement, which results in pain. Chronic maltracking causes pain by contributing to patellofemoral cartilage damage and OA. 74 A study by Manghwani et al 75 showed that anterior knee pain was significantly lower when there is a 100% contact between the femoral trochlea of the implant and the patella, suggesting that contact is an important factor in determining pain levels post-TKR.
Patellar maltracking can be caused by different risk factors: the surgical approach, implant or the patient. Factors related to patients are pre-operative patellar subluxation and valgus deformity which can cause the release of the lateral retinacula in the implant. 76
Patellar maltracking can also be due to the lack of soft tissue balancing or malpositioning of different components. A dynamic valgus deformity from tibial and femoral internal rotation can be exacerbated by weak hip abductors causing more internal rotation of the femur. 77 A cross-sectional study by Laubach et al 78 demonstrated an association between anterior knee pain and the strength of the quadriceps muscles, as well as a lower patellar position and a thinner inlay. There was also a significantly lower tissue elasticity in the patellar and quadriceps tendons in subjects with anterior knee pain than those without.
In addition, pain normally depends on the size of the Q-angle, which is the angle formed by a line drawn from the anterior superior iliac spine to central patella, and a line drawn from tibial tubercle to central patella. This is normally 10–15 degrees. 79 A large Q-angle due to excessive internal rotation of the implantation of a tibial tray can displace the tibial tuberosity laterally and pull on the patellar tendon. 80 This in turn causes pain in the knee in addition to the tightness of the lateral retinaculum. 81 Sanchis-Alfonso et al 82 discovered that there is an increased density of nociceptors in patients with anterior knee pain at the lateral retinaculum. This could explain why patients with lateral patellar maltracking suffer more pain after TKR.
- Overstuffing
Overstuffing occurs when there is an imbalance of the implant thickness compared to the femoral and patellar bone cuts following TKR, which involves a measured resection technique. It occurs in 80% of patients after TKR. 83 The relationship between overstuffing and pain is unclear. A study by Marmor et al 84 showed that overstuffing TKRs is associated with extensive osteophytes and intra-articular femoral valgus which may suggest an association with excessive joint tension due to implant protrusion contributing to knee pain and stiffness. A study by Kemp et al 85 showed that there is no association between Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) and combined patellofemoral overstuffing involving the patella and trochlea. The authors suggest that there is a significant association between knee pain/functional score and increasing anterior trochlear offset. However, a study by Beldman et al 86 found no correlation between overstuffing and anterior knee pain after TKR and does not suggest any unexplained overstuffed knee joint revision surgery. An overstuffed patellofemoral compartment results in higher pressure and reaction forces in the joint which can contribute to periprosthetic fractures. Patellar maltracking has also been linked to post-operative patellar fractures. 87
- Polyethylene wear
Polyethylene wear of the arthroplasty articulating surfaces is a common mechanism of TKR failure. Gradual surface wear results in delamination and pitting of the polyethylene insert. Along with adhesive and abrasive wear, this results in the release of multiple debris particles. This is associated with osteolysis and painful synovitis. It most commonly affects the medial compartment and is demonstrated on radiographs as asymmetric joint space narrowing. Imaging may also aid bone loss monitoring, identification and pre-operative quantification of osteolysis. 88 Wear-related failure is a complex phenomenon, arising from the inherent tribology of imperfectly congruent surfaces. Factors include the manufacturing and properties of polyethylene, implant design, surgical technique, and patient factors. 89 Polyethylene properties, such as density and the degree of cross-linking, have been investigated in their contribution to wear, and in the generation wear-resistant highly cross-linked polyethylene. 90 Whilst its introduction in hip arthroplasties has been successful, long-term clinical data on its efficacy in TKR are lacking. Implant factors include component design and polyethylene insert characteristics, e.g. thickness and structure. The surgical technique determines the implant alignment and joint axis which affects polyethylene wear. Patient factors include age, weight and activity level. 91
- Unresurfaced patella
Looking at patellar resurfacing rates from a global perspective, it appears that the practice varies with geographic location. Rates of resurfacing are highest in the United States at 82% and are far lower internationally, with Norway displaying the lowest rates at 4%. Fraser and Spangehl 92 speculate that the reason for this variation hinges not solely on surgeons’ consideration for post-TKR anterior knee pain limitation, but rather on a multitude of factors such as past training methods, individual hospital protocols and personal preferences.
Currently, the literature is split when comparing which practice, patellar resurfacing or unresurfacing, limits post-TKR anterior knee pain the most. Several studies show evidence for and against the practice of patellar resurfacing by comparing rates of post-TKR anterior knee pain: some report that the resurfaced patella confers lower post-operative anterior knee pain rates, 93 – 96 yet others find no difference. 93 , 97 , 98 Two meta-analyses of 749 and 3,034 TKRs, the latter of which compiled the quantitative findings of 16 randomized controlled trials, found no evidence of a difference between post-operative anterior knee pain rates when comparing resurfaced and unresurfaced patellae. 97 In contrast, another meta-analysis of 1,223 cases found that resurfaced patellae conferred a 13.8% absolute risk reduction in post-operative anterior knee pain. 96 Overall, no one practice appears immediately favourable over the other.
Several authors have identified reasons patellar resurfacing may pose a risk to the structural integrity of the knee joint and therefore contribute to pain post-operatively. The practice, they argue, carries the underlying risks of patella fracture, patellar tendon injury, joint infection and instability, avascular necrosis, polyethylene wear of the patellar component, aseptic loosening and overstuffing. 92 – 94 These factors can be considered throughout the TKR management pathway.
Pain is often associated with infections. The pain is thought to be secondary to inflammation and infection. The release of inflammatory cytokines during an infection contributes to the initiation and persistence of pain. 99 Cytokines that cause pain primarily include IL-1β. 100 In addition, there is also evidence to suggest direct activation of nociceptor neurons by pathogens themselves. 101
A major cause for prosthetic joint infection is gram-positive cocci such as Staphylococcus aureus , coagulase-negative staphylococci species, and, increasingly, Corynebacterium species. 102 – 104 Staphylococcus aureus produces pain through the release of α-hemolysin, which activates nociceptor neurones, while formyl peptide nociceptors are also stimulated by n-formyl peptides, which are by-products of all bacterial pathogens. 103
Risk factors for infective prosthetic joint infection requiring revision include constrained condylar prostheses, use of posterior-stabilized fixed-bearing prostheses, the requirement of a tibial patellofemoral graft, inflammatory arthropathy, previous septic arthritis, surgery for trauma, peripheral vascular disease, connective tissue and rheumatic diseases, diabetes, chronic pulmonary disease, high body mass index (BMI), higher American Society of Anaesthesiologist (ASA) grade, young age and male gender. 105
- Other possible factors
A study by Bierke et al 106 demonstrated that psychological factors such as somatization dysfunction and depressive symptoms can impact on post-TKR pain score, even with uncomplicated TKR, for up to five years post-operatively. This is consistent with the results from a review by Bonnin et al 107 for patients with higher depressive and anxiety states in uncomplicated TKRs. This suggests that psychological variables may influence post-TKR pain. Damage to the saphenous infrapatellar nerve branch following a standard midline skin incision is common in TKRs and this causes painful neuroma that reduces the range of motion of the knee. 108 – 110 In a study by Koh et al, 111 central sensitization index (a measure of central sensitization for persistent pain and dissatisfaction following total knee arthroplasty due to the augmentation of the central nervous system signalling for pain) persists in individuals with high pre-operative central sensitization index following TKR compared to those with a lower level. Although with clinical improvement these patients also showed significantly worse pain scores, lower quality of life, functional disability and a correlation with dissatisfaction.
In this review, we have identified supporting information for TKR pain, though conflicting results from meta-analyses on the practice of unresurfacing patellae and the findings from studies on overstuffing suggest further research is required. We gathered information on how arthrofibrosis causes pain, which can be explained by the cytokine pathways leading up to an inflammatory response or structural causes. Pain from instability can be explained by tissue insufficiency, buckling and other factors in relation to the implant and the surrounding tissues. Component malpositioning contributes to pain often due to kinematics, tensions and pressure which can be explained by the implant position involving both femoral and tibial components and their rotations. Malpositioning can also increase the risk of instability and polyethylene wear. Polyethylene wear causes pain via the release of debris particles initiating osteolysis. This release is affected by implant properties, patient factors and surgical techniques. Similar to polyethylene wear, pain from aseptic loosening can be explained by osteolysis and can initiate an immunological response. Aseptic loosening is often a result of aforementioned factors including instability, component malposition and polyethylene wear, making their relationship multifactorial and interlinked. In patellar maltracking, pain is often due to a lack of tissue balance or component malpositioning resulting in a poor relationship between the trochlea and the patella with ensuing cartilage damage and OA. In addition, this review has identified common pathogens for pain in TKR infections and discussed the biological explanation for pain. Other causes of post-TKR pain were explored involving the nervous system and psychological factors. Table 1 summarizes our findings.
A summary of the causes of pain identified in this review
The frequency of TKR surgery has increased over the past decade and its frequency is predicted to rise in the future. 2 , 3 Although TKR surgery has a high satisfaction rate of 80–100%, 112 10–34% of patients develop adverse pain as a complication. 10 This highlights the importance of addressing pain expectations and managing pain post-operatively. It also emphasizes the importance of early detection and prompt management of the intra-articular causes of pain to improve patient satisfaction.
Being able to identify risk factors for adverse outcomes such as those highlighted in this review is important, as this can be used to predict the likelihood of adverse pain outcomes and to identify specific causes. Controllable risk factors, such as BMI, 105 can be managed and considered pre- and post-operatively to minimize complications of pain.
It is likely that the causes of pain will become more evident in upcoming years with technological advancements and a greater understanding of pain aetiology. The consensus is that further studies are required to explore the different aetiologies of pain alongside the development of methods for diagnosis, prevention and management of each specific cause. Healthcare professionals should be prepared to make tailored changes to patient care as there is no ‘one size fits all’ solution.
Through developing effective prevention and management of post-TKR pain, fewer patients will suffer from pain or spend time receiving care as follow-ups, reducing both cost and time. Studies have suggested that insufficient management of acute TKR pain contributes to chronic pain, which also highlights the importance of early diagnosis and appropriate management following TKR. 113 , 114 In addition, with reduced revision frequency, the risks patients are exposed to from invasive surgical procedures are minimized, improving patient outcomes. Resources in any publicly funded health system such as those in the United Kingdom and other European countries can therefore be redistributed.
- Open access
This article is distributed under the terms of the Creative Commons Attribution-Non Commercial 4.0 International (CC BY-NC 4.0) licence ( https://creativecommons.org/licenses/by-nc/4.0/ ) which permits non-commercial use, reproduction and distribution of the work without further permission provided the original work is attributed.
The author declares no conflict of interest relevant to this work.
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Varacallo M , Luo T , Johanson N . Total knee arthroplasty (TKA) techniques . National Center for Biotechnology Information , 2020 . https://www.ncbi.nlm.nih.gov/books/NBK499896/ ( date last accessed 1 April 2020 ).
- Search Google Scholar
- Export Citation
National Joint Registry . NJR 16th Annual Report 2019 . https://reports.njrcentre.org.uk/Portals/0/PDFdownloads/NJR%2016th%20Annual%20Report%202019.pdf ( date last accessed 1 April 2020 ).
Kurtz S , Ong K , Lau E , Mowat F , Halpern M . Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030 . J Bone Joint Surg Am 2007 ; 89 : 780 – 785 .
Rissanen P , Aro S , Slätis P , Sintonen H , Paavolainen P . Health and quality of life before and after hip or knee arthroplasty . J Arthroplasty 1995 ; 10 : 169 – 175 .
Drewett RF , Minns RJ , Sibly TF . Measuring outcome of total knee replacement using quality of life indices . Ann R Coll Surg Engl 1992 ; 74 : 286 – 289 .
Fitzgerald JD , Orav EJ & Lee TH et al. Patient quality of life during the 12 months following joint replacement surgery . Arthritis Rheum 2004 ; 51 : 100 – 109 .
Bachmeier CJ , March LM , Cross MJ , et al ; Arthritis Cost and Outcome Project Group . A comparison of outcomes in osteoarthritis patients undergoing total hip and knee replacement surgery . Osteoarthritis Cartilage 2001 ; 9 : 137 – 146 .
Bade MJ , Kohrt WM , Stevens-Lapsley JE . Outcomes before and after total knee arthroplasty compared to healthy adults . J Orthop Sports Phys Ther 2010 ; 40 ( 9 ): 559 – 567 .
Hofmann S , Seitlinger G , Djahani O , Pietsch M . The painful knee after TKA: a diagnostic algorithm for failure analysis . Knee Surg Sports Traumatol Arthrosc 2011 ; 19 : 1442 – 1452 .
Beswick AD , Wylde V , Gooberman-Hill R , Blom A , Dieppe P . What proportion of patients report long-term pain after total hip or knee replacement for osteoarthritis? A systematic review of prospective studies in unselected patients . BMJ Open 2012 ; 2 : e000435 .
Singh JA , Lewallen DG . Are outcomes after total knee arthroplasty worsening over time? A time-trends study of activity limitation and pain outcomes . BMC Musculoskelet Disord 2014 ; 15 : 440 .
Erivan R , Jacquet C , Villatte G , Ollivier M , Paprosky W . Epidemiology of painful knee after total knee arthroplasty in a tertiary care center: assessment by decision tree . Knee 2020 ; 27 : 1049 – 1056 .
Preston S , Petrera M , Kim C , Zywiel MG , Gandhi R . Towards an understanding of the painful total knee: what is the role of patient biology? Curr Rev Musculoskelet Med 2016 ; 9 : 388 – 395 .
Usher KM , Zhu S , Mavropalias G , Carrino JA , Zhao J , Xu J . Pathological mechanisms and therapeutic outlooks for arthrofibrosis . Bone Res 2019 ; 7 : 9 .
Mayr H , Stöhr A . Arthroscopic treatment of arthrofibrosis after ACL reconstruction: local and generalized arthrofibrosis . Oper Orthop Traumatol 2014 ; 26 : 7 – 18 .
Schiavone Panni A , Cerciello S , Vasso M , Tartarone M . Stiffness in total knee arthroplasty . J Orthop Traumatol 2009 ; 10 : 111 – 118 .
Gandhi R , de Beer J , Leone J , Petruccelli D , Winemaker M , Adili A . Predictive risk factors for stiff knees in total knee arthroplasty . J Arthroplasty 2006 ; 21 : 46 – 52 .
Gollwitzer H , Burgkart R , Diehl P , Gradinger R , Bühren V . [Therapy of arthrofibrosis after total knee arthroplasty] . Orthopade 2006 ; 35 : 143 – 152 .
Phan SH . The myofibroblast in pulmonary fibrosis . Chest 2002 ; 122 : 286S – 289S .
Bataller R , Brenner DA . Liver fibrosis . J Clin Invest 2005 ; 115 : 209 – 218 .
Hinz B , Phan SH , Thannickal VJ , Galli A , Bochaton-Piallat ML , Gabbiani G . The myofibroblast: one function, multiple origins . Am J Pathol 2007 ; 170 : 1807 – 1816 .
Zeichen J , Haeder L , Jagodzinski M , Lobenhoffer P , Bosch U , Brand J . [Localization of TGF-beta and PDGF and their relevance for the pathogenesis of arthrofibrosis] . Unfallchirurg 2008 ; 111 : 79 – 84 .
Dixon D , Coates J & del Carpio Pons A et al. A potential mode of action for Anakinra in patients with arthrofibrosis following total knee arthroplasty . Sci Rep 2015 ; 5 : 16466 .
Mayr HO , Hochrein A . The stiff knee . Knee 2015 ; 22 : 354 – 355 .
Mayr H , Tröger M , Hein W . Retropatellararthrose bei Arthrofibrose . Arthroskopie 2005 ; 18 : 308 – 312 .
Pujol N , Boisrenoult P , Beaufils P . Post-traumatic knee stiffness: surgical techniques . Orthop Traumatol Surg Res 2015 ; 101 : S179 – S186 .
Kim YS , Youn HK , Kim BS , Choi YJ , Koh YG . Arthroscopic evaluation of persistent pain following supramalleolar osteotomy for varus ankle osteoarthritis . Knee Surg Sports Traumatol Arthrosc 2016 ; 24 : 1860 – 1807 .
Menetski J , Mistry S & Lu M et al. Mice overexpressing chemokine ligand 2 (CCL2) in astrocytes display enhanced nociceptive responses . Neuroscience 2007 ; 149 : 706 – 714 .
White FA , Sun J & Waters SM et al. Excitatory monocyte chemoattractant protein-1 signaling is up-regulated in sensory neurons after chronic compression of the dorsal root ganglion . Proc Natl Acad Sci U S A 2005 ; 102 : 14092 – 14097 .
White FA , Bhangoo SK , Miller RJ . Chemokines: integrators of pain and inflammation . Nat Rev Drug Discov 2005 ; 4 : 834 – 844 .
Ji R-R , Xu Z-Z , Gao Y-J . Emerging targets in neuroinflammation-driven chronic pain . Nat Rev Drug Discov 2014 ; 13 : 533 – 548 .
Paish HL , Kalson NS & Smith GR et al. Fibroblasts promote inflammation and pain via IL-1α induction of the monocyte chemoattractant chemokine (C-C Motif) ligand 2 . Am J Pathol 2018 ; 188 : 696 – 714 .
Fleeton G , Harmer AR & Nairn L et al. Self-reported knee instability before and after total knee replacement surgery . Arthritis Care Res (Hoboken) 2016 ; 68 : 463 – 471 .
Leichtenberg CS , Vliet Vlieland TPM , Kroon HM , et al ; LOAS Studygroup . Self-reported knee instability associated with pain, activity limitations, and poorer quality of life before and 1 year after total knee arthroplasty in patients with knee osteoarthritis . J Orthop Res 2018 ; 36 : 2671 – 2678 .
van der Esch M , Knoop J & van der Leeden M et al. Self-reported knee instability and activity limitations in patients with knee osteoarthritis: results of the Amsterdam osteoarthritis cohort . Clin Rheumatol 2012 ; 31 : 1505 – 1510 .
Felson DT , Niu J & McClennan C et al. Knee buckling: prevalence, risk factors, and associated limitations in function . Ann Intern Med 2007 ; 147 : 534 – 540 .
Fitzgerald GK , Piva SR , Irrgang JJ . Reports of joint instability in knee osteoarthritis: its prevalence and relationship to physical function . Arthritis Rheum 2004 ; 51 : 941 – 946 .
Abdel MP , Pulido L , Severson EP , Hanssen AD . Stepwise surgical correction of instability in flexion after total knee replacement . Bone Joint J 2014 ; 96-B : 1644 – 1648 .
Seil R , Pape D . Causes of failure and etiology of painful primary total knee arthroplasty . Knee Surg Sports Traumatol Arthrosc 2011 ; 19 : 1418 – 1432 .
Cottino U , Sculco PK , Sierra RJ , Abdel MP . Instability after total knee arthroplasty . Orthop Clin North Am 2016 ; 47 : 311 – 316 .
Fehring TK , Odum S , Griffin WL , Mason JB , Nadaud M . Early failures in total knee arthroplasty . Clin Orthop Relat Res 2001 ; 392 : 315 – 318 .
Lewallen EA , Salib CG & Trousdale WH et al. Molecular pathology of total knee arthroplasty instability defined by RNA-seq . Genomics 2018 ; 110 : 247 – 256 .
Sharma RK . Mid flexion instability after primary total knee arthroplasty . Orthopaedic Proceedings 2013 ; 95-B : 326 .
Rouquette L , Erivan R , Pereira B , Boisgard S , Descamps S , Villatte G . Tibiofemoral dislocation after primary total knee arthroplasty: a systematic review . Int Orthop 2019 ; 43 : 1599 – 1609 .
Slane LC , Dandois F , Bogaerts S , Scheys L , Vandenneucker H . Patellar tendon buckling in post-operative total knee arthroplasty patients is more prominent than in healthy controls . Med Eng Phys 2019 ; 69 : 28 – 32 .
Wilson CJ , Theodoulou A , Damarell RA , Krishnan J . Knee instability as the primary cause of failure following total knee arthroplasty (TKA): a systematic review on the patient, surgical and implant characteristics of revised TKA patients . Knee 2017 ; 24 : 1271 – 1281 .
Sharkey PF , Lichstein PM , Shen C , Tokarski AT , Parvizi J . Why are total knee arthroplasties failing today: has anything changed after 10 years? J Arthroplasty 2014 ; 29 : 1774 – 1778 .
Sharkey PF , Hozack WJ , Rothman RH , Shastri S , Jacoby SM . Insall Award paper. Why are total knee arthroplasties failing today? Clin Orthop Relat Res 2002 ; 404 : 7 – 13 .
Johnson GA , Tramaglini DM , Levine RE , Ohno K , Choi N-Y , Woo SL . Tensile and viscoelastic properties of human patellar tendon . J Orthop Res 1994 ; 12 : 796 – 803 .
Petersen W , Rembitzki IV & Brüggemann G-P et al. Anterior knee pain after total knee arthroplasty: a narrative review . Int Orthop 2014 ; 38 : 319 – 328 .
Lützner J , Kirschner S , Günther KP , Harman MK . Patients with no functional improvement after total knee arthroplasty show different kinematics . Int Orthop 2012 ; 36 : 1841 – 1847 .
van Kempen RW , Schimmel JJ , van Hellemondt GG , Vandenneucker H , Wymenga AB . Reason for revision TKA predicts clinical outcome: prospective evaluation of 150 consecutive patients with 2-years followup . Clin Orthop Relat Res 2013 ; 471 : 2296 – 2302 .
Zihlmann MS , Stacoff A , Romero J , Quervain IK , Stüssi E . Biomechanical background and clinical observations of rotational malalignment in TKA: literature review and consequences . Clin Biomech (Bristol, Avon) 2005 ; 20 : 661 – 668 .
Vince KG . Why knees fail . J Arthroplasty 2003 ; 18 : 39 – 44 .
Fuchs S , Skwara A , Tibesku CO , Rosenbaum D . Retropatellar contact characteristics before and after total knee arthroplasty . Knee 2005 ; 12 : 9 – 12 .
Howell SM , Hodapp EE , Vernace JV , Hull ML , Meade TD . Are undesirable contact kinematics minimized after kinematically aligned total knee arthroplasty? An intersurgeon analysis of consecutive patients . Knee Surg Sports Traumatol Arthrosc 2013 ; 21 : 2281 – 2287 .
Steinbruck A , Fottner A , Schroder C , Woiczinski M , Schmitt-Sody M & Muller T et al. Influence of mediolateral tibial baseplate position in TKA on knee kinematics and retropatellar pressure . Knee Surg Sports Traumatol Arthrosc 2017 ; 25 : 2602 – 2608 .
Kuriyama S , Ishikawa M , Furu M , Ito H , Matsuda S . Malrotated tibial component increases medial collateral ligament tension in total knee arthroplasty . J Orthop Res 2014 ; 32 : 1658 – 1666 .
Thompson JA , Hast MW , Granger JF , Piazza SJ , Siston RA . Biomechanical effects of total knee arthroplasty component malrotation: a computational simulation . J Orthop Res 2011 ; 29 : 969 – 975 .
Murakami AM , Hash TW , Hepinstall MS , Lyman S , Nestor BJ , Potter HG . MRI evaluation of rotational alignment and synovitis in patients with pain after total knee replacement . J Bone Joint Surg Br 2012 ; 94 : 1209 – 1215 .
Berger RA , Crossett LS , Jacobs JJ , Rubash HE . Malrotation causing patellofemoral complications after total knee arthroplasty . Clin Orthop Relat Res 1998 ; 356 : 144 – 153 .
Barrack RL , Schrader T , Bertot AJ , Wolfe MW , Myers L . Component rotation and anterior knee pain after total knee arthroplasty . Clin Orthop Relat Res 2001 ; 392 : 46 – 55 .
Woiczinski M , Kistler M & Schröder C et al. TKA design-integrated trochlea groove rotation reduces patellofemoral pressure . Knee Surg Sports Traumatol Arthrosc 2019 ; 27 : 1680 – 1692 .
Fottner A , Woiczinski M & Schröder C et al. Impact of tibial baseplate malposition on kinematics, contact forces and ligament tensions in TKA: a numerical analysis . J Mech Behav Biomed Mater 2020 ; 103 : 103564 .
Nicoll D , Rowley DI . Internal rotational error of the tibial component is a major cause of pain after total knee replacement . J Bone Joint Surg Br 2010 ; 92 : 1238 – 1244 .
Dalury DF , Pomeroy DL , Gorab RS , Adams MJ . Why are total knee arthroplasties being revised? J Arthroplasty 2013 ; 28 : 120 – 121 .
Schroer WC , Berend KR & Lombardi AV et al. Why are total knees failing today? Etiology of total knee revision in 2010 and 2011 . J Arthroplasty 2013 ; 28 : 116 – 119 .
Crotti TN , Smith MD & Findlay DM et al. Factors regulating osteoclast formation in human tissues adjacent to peri-implant bone loss: expression of receptor activator NFkappaB, RANK ligand and osteoprotegerin . Biomaterials 2004 ; 25 : 565 – 573 .
Gehrke T , Sers C & Morawietz L et al. Receptor activator of nuclear factor kappaB ligand is expressed in resident and inflammatory cells in aseptic and septic prosthesis loosening . Scand J Rheumatol 2003 ; 32 : 287 – 294 .
Higuera C , Parvizi J . 18 causes and diagnosis of aseptic loosening after total knee replacement . In: Hirschmann MT , Becker R , eds. The unhappy total knee replacement: a comprehensive review and management guide . Cham : Springer , 2015 : 225 - 237 .
Goodman S . Wear particulate and osteolysis . Orthop Clin North Am 2005 ; 36 : 41 – 48 , vi .
Math KR , Zaidi SF , Petchprapa C , Harwin SF . Imaging of total knee arthroplasty . Semin Musculoskelet Radiol 2006 ; 10 : 47 – 63 .
Jibri Z , Jamieson P , Rakhra KS , Sampaio ML , Dervin G . Patellar maltracking: an update on the diagnosis and treatment strategies . Insights Imaging 2019 ; 10 : 65 .
Tsavalas N , Katonis P , Karantanas AH . Knee joint anterior malalignment and patellofemoral osteoarthritis: an MRI study . Eur Radiol 2012 ; 22 : 418 – 428 .
Manghwani J , Vaidya SV , Patel H , Vaidya CS . Does total contact of the patella with the femoral trochlea during no thumb test significantly reduce anterior knee pain? Knee 2019 ; 26 : 1338 – 1347 .
Gasparini G , Familiari F , Ranuccio F . Patellar malalignment treatment in total knee arthroplasty . Joints 2013 ; 1 : 10 – 17 .
MacIntyre NJ , Hill NA , Fellows RA , Ellis RE , Wilson DR . Patellofemoral joint kinematics in individuals with and without patellofemoral pain syndrome . J Bone Joint Surg Am 2006 ; 88 : 2596 – 2605 .
Laubach M , Hellmann JT & Dirrichs T et al. Anterior knee pain after total knee arthroplasty: a multifactorial analysis . J Orthop Surg (Hong Kong) 2020 ; 28 : 2309499020918947 .
Horton MG , Hall TL . Quadriceps femoris muscle angle: normal values and relationships with gender and selected skeletal measures . Phys Ther 1989 ; 69 : 897 – 901 .
McPherson EJ . Patellar tracking in primary total knee arthroplasty . Instr Course Lect 2006 ; 55 : 439 – 448 .
Mizuno Y , Kumagai M & Mattessich SM et al. Q-angle influences tibiofemoral and patellofemoral kinematics . J Orthop Res 2001 ; 19 : 834 – 840 .
Sanchis-Alfonso V , Roselló-Sastre E , Monteagudo-Castro C , Esquerdo J . Quantitative analysis of nerve changes in the lateral retinaculum in patients with isolated symptomatic patellofemoral malalignment: a preliminary study . Am J Sports Med 1998 ; 26 : 703 – 709 .
Kandhari VK , Desai MM , Bava SS , Wade RN . Digging deeper into the patella-femoral joint: patello-femoral composite – a new dimension for overstuffing of patello-femoral joint . J Clin Diagn Res 2017 ; 11 : RC04 – RC07 .
Marmor S , Renault E , Valluy J , Saffarini M . Over-voluming predicted by pre-operative planning in 24% of total knee arthroplasty . Knee Surg Sports Traumatol Arthrosc 2019 ; 27 : 1544 – 1551 .
Kemp MA , Metcalfe AJ , Sayers A , Wylde V , Eldridge JD , Blom AW . Does overstuffing of the patellofemoral joint in total knee arthroplasty have a significant effect on postoperative outcomes? Knee 2018 ; 25 : 874 – 881 .
Beldman M , Breugem SJM , van Jonbergen HPW . Overstuffing in total knee replacement: no effect on clinical outcomes or anterior knee pain . Int Orthop 2015 ; 39 : 887 – 891 .
Assiotis A , To K , Morgan-Jones R , Pengas IP , Khan W . Patellar complications following total knee arthroplasty: a review of the current literature . Eur J Orthop Surg Traumatol 2019 ; 29 : 1605 – 1615 .
Fritz J , Lurie B , Miller TT . Imaging of hip arthroplasty . Semin Musculoskelet Radiol 2013 ; 17 : 316 – 327 .
Chakrabarty G , Vashishtha M , Leeder D . Polyethylene in knee arthroplasty: a review . J Clin Orthop Trauma 2015 ; 6 : 108 – 112 .
Lachiewicz PF , Geyer MR . The use of highly cross-linked polyethylene in total knee arthroplasty . J Am Acad Orthop Surg 2011 ; 19 : 143 – 151 .
Naudie DD , Ammeen DJ , Engh GA , Rorabeck CH . Wear and osteolysis around total knee arthroplasty . J Am Acad Orthop Surg 2007 ; 15 : 53 – 64 .
Fraser JF , Spangehl MJ . International rates of patellar resurfacing in primary total knee arthroplasty, 2004–2014 . J Arthroplasty 2017 ; 32 : 83 – 86 .
Meneghini RM . Should the patella be resurfaced in primary total knee arthroplasty? An evidence-based analysis . J Arthroplasty 2008 ; 23 : 11 – 14 .
Migliorini F , Eschweiler J , Niewiera M , El Mansy Y , Tingart M , Rath B . Better outcomes with patellar resurfacing during primary total knee arthroplasty: a meta-analysis study . Arch Orthop Trauma Surg 2019 ; 139 : 1445 – 1454 .
Nizard RS , Biau D & Porcher R et al. A meta-analysis of patellar replacement in total knee arthroplasty . Clin Orthop Relat Res 2005 ; 432 : 196 – 203 .
Pakos EE , Ntzani EE , Trikalinos TA . Patellar resurfacing in total knee arthroplasty: a meta-analysis . J Bone Joint Surg Am 2005 ; 87 : 1438 – 1445 .
Fu Y , Wang G , Fu Q . Patellar resurfacing in total knee arthroplasty for osteoarthritis: a meta-analysis . Knee Surg Sports Traumatol Arthrosc 2011 ; 19 : 1460 – 1466 .
He JY , Jiang LS , Dai LY . Is patellar resurfacing superior than nonresurfacing in total knee arthroplasty? A meta-analysis of randomized trials . Knee 2011 ; 18 : 137 – 144 .
Zhang J-M , An J . Cytokines, inflammation, and pain . Int Anesthesiol Clin 2007 ; 45 : 27 – 37 .
Copray JC , Mantingh I & Brouwer N et al. Expression of interleukin-1 beta in rat dorsal root ganglia . J Neuroimmunol 2001 ; 118 : 203 – 211 .
Chiu IM , Pinho-Ribeiro FA , Woolf CJ . Pain and infection: pathogen detection by nociceptors . Pain 2016 ; 157 : 1192 – 1193 .
Tande AJ , Patel R . Prosthetic joint infection . Clin Microbiol Rev 2014 ; 27 : 302 – 345 .
Chiu IM , Heesters BA & Ghasemlou N et al. Bacteria activate sensory neurons that modulate pain and inflammation . Nature 2013 ; 501 : 52 – 57 .
Hernandez NM , Buchanan MW & Cullen MM et al. Corynebacterium total hip and knee arthroplasty prosthetic joint infections . Arthroplast Today 2020 ; 6 : 163 – 168 .
Lenguerrand E , Whitehouse MR , Beswick AD , et al ; National Joint Registry for England, Wales, Northern Ireland and the Isle of Man . Risk factors associated with revision for prosthetic joint infection following knee replacement: an observational cohort study from England and Wales . Lancet Infect Dis 2019 ; 19 : 589 – 600 .
Bierke S , Häner M , Karpinski K , Hees T , Petersen W . Midterm effect of mental factors on pain, function, and patient satisfaction 5 years after uncomplicated total knee arthroplasty . J Arthroplasty 2020 ; 35 : 105 – 111 .
Bonnin MP , Basiglini L , Archbold HAP . What are the factors of residual pain after uncomplicated TKA? Knee Surg Sports Traumatol Arthrosc 2011 ; 19 : 1411 – 1417 .
Harris JD , Fazalare JJ , Griesser MJ , Flanigan DC . Infrapatellar branch of saphenous neurectomy for painful neuroma: a case report . Am J Orthop (Belle Mead NJ) 2012 ; 41 : 37 – 40 .
Kachar SM , Williams KM , Finn HA . Neuroma of the infrapatellar branch of the saphenous nerve a cause of reversible knee stiffness after total knee arthroplasty . J Arthroplasty 2008 ; 23 : 927 – 930 .
Sundaram RO , Ramakrishnan M , Harvey RA , Parkinson RW . Comparison of scars and resulting hypoaesthesia between the medial parapatellar and midline skin incisions in total knee arthroplasty . Knee 2007 ; 14 : 375 – 378 .
Koh IJ , Kang BM , Kim MS , Choi KY , Sohn S , In Y . How does preoperative central sensitization affect quality of life following total knee arthroplasty? J Arthroplasty 2020 . https://doi.org/10.1016/j.arth.2020.04.004 [Epub ahead of print].
Kahlenberg CA , Nwachukwu BU , McLawhorn AS , Cross MB , Cornell CN , Padgett DE . Patient satisfaction after total knee replacement: a systematic review . HSS J 2018 ; 14 : 192 – 201 .
Perkins FM , Kehlet H . Chronic pain as an outcome of surgery: a review of predictive factors . Anesthesiology 2000 ; 93 : 1123 – 1133 .
Puolakka PA , Rorarius MG , Roviola M , Puolakka TJ , Nordhausen K , Lindgren L . Persistent pain following knee arthroplasty . Eur J Anaesthesiol 2010 ; 27 : 455 – 460 .
EFORT Open Reviews is committed to supporting researchers in demonstrating the impact of their articles published in the journal.
As an open-access journal, EFORT Open Reviews articles are immediately available to read on publication, without restriction. The two types of article metrics we measure are (i) more traditional full-text views and pdf downloads, and (ii) Altmetric data, which shows the wider impact of articles in a range of non-traditional sources, such as social media.
More information is on the Reasons to publish page.
| Dec 2021 onwards | Past Year | Past 30 Days | |
|---|---|---|---|
| Full Text Views | 6987 | 3799 | 1071 |
| PDF Downloads | 4130 | 1563 | 110 |
- Share on facebook Share on linkedin Share on twitter
Related Articles
Article information.
- Get Permissions
- View raw image
- Download Powerpoint Slide
- PubMed Citation
- Article by Cheuk Yin Li
- Article by Kenneth Jordan Ng Cheong Chung
- Article by Omar M. E. Ali
- Article by Nicholas D. H. Chung
- Article by Cheuk Heng Li
- Similar articles in PubMed
Google Scholar
Online ISSN: 2058-5241 Print ISSN: 2396-7544
Author Information
Author Guidelines
Open Access Policy
Permissions
Librarian Information
General Information
Read and Publish Deal
Contact the journal
Advertising

Strengthening biomedical communities to advance science and health
Accessibility
Privacy and Cookies
Terms and Conditions
About Bioscientifica
All Bioscientifica Journals
Publishing Alliances
Bioscientifica Ltd | Starling House | 1600 Bristol Parkway North | Bristol BS34 8YU | UK
Bioscientifica Ltd | Registered in England no 3190519
© 2024 Bioscientifica Ltd
- [185.126.86.119]
- 185.126.86.119
Character limit 500 /500
Information
- Author Services
Initiatives
You are accessing a machine-readable page. In order to be human-readable, please install an RSS reader.
All articles published by MDPI are made immediately available worldwide under an open access license. No special permission is required to reuse all or part of the article published by MDPI, including figures and tables. For articles published under an open access Creative Common CC BY license, any part of the article may be reused without permission provided that the original article is clearly cited. For more information, please refer to https://www.mdpi.com/openaccess .
Feature papers represent the most advanced research with significant potential for high impact in the field. A Feature Paper should be a substantial original Article that involves several techniques or approaches, provides an outlook for future research directions and describes possible research applications.
Feature papers are submitted upon individual invitation or recommendation by the scientific editors and must receive positive feedback from the reviewers.
Editor’s Choice articles are based on recommendations by the scientific editors of MDPI journals from around the world. Editors select a small number of articles recently published in the journal that they believe will be particularly interesting to readers, or important in the respective research area. The aim is to provide a snapshot of some of the most exciting work published in the various research areas of the journal.
Original Submission Date Received: .
- Active Journals
- Find a Journal
- Proceedings Series
- For Authors
- For Reviewers
- For Editors
- For Librarians
- For Publishers
- For Societies
- For Conference Organizers
- Open Access Policy
- Institutional Open Access Program
- Special Issues Guidelines
- Editorial Process
- Research and Publication Ethics
- Article Processing Charges
- Testimonials
- Preprints.org
- SciProfiles
- Encyclopedia

Article Menu

- Subscribe SciFeed
- Recommended Articles
- Google Scholar
- on Google Scholar
- Table of Contents
Find support for a specific problem in the support section of our website.
Please let us know what you think of our products and services.
Visit our dedicated information section to learn more about MDPI.
JSmol Viewer
Assessing the value of imaging data in machine learning models to predict patient-reported outcome measures in knee osteoarthritis patients.

1. Introduction
2. materials and methods, 2.1. ethics considerations, 2.2. data source, 2.3. outcome measure, 2.4. feature selection and data pre-processing, 2.5. model development, training and validation.
Click here to enlarge figure
2.6. Statistical Analysis and Feature Importance
3.1. data distribution, 3.2. model performance, 3.3. feature importance, 4. discussion, 5. conclusions, author contributions, institutional review board statement, informed consent statement, data availability statement, conflicts of interest.
| Patient Feature | Subgroups within Each Feature |
|---|---|
| Age | Age ≤ 50; 50 < Age < 60; 60 ≤ Age < 70; Age ≥ 70 |
| Sex | Male; Female |
| Ethnicity | White/Caucasian; Black/African American/Asian & other Non-White |
| Living Status | Lives Alone; Lives with someone else |
| Education Status | Less than high school graduate; High school graduate; Some college; College graduate; Some graduate school; Graduate degree |
| Employment Status | Yes; No |
| Body Mass Index (BMI) | Underweight (BMI < 18.5); Healthy (18.5–24.9); Overweight (25.0–29.9); Obese (30.0–39.9); Morbidly obese (BMI > 40) |
| Comorbidities (Charlson Comorbidity Index) | None; Mild (CCI = 1–2), Moderate (CCI = 3–4); Severe (CCI > 5) |
| Inflammatory Arthritis | None; OA/degenerative only; gout/other only; OA/degenerative and gout/other |
| Injury to knee | Yes; No |
| Knee Surgery | No; Left or Right; Left and Right |
| Osteoarthritis medication | None; corticosteroids; supplements (methylsulfonylmethane, fluorides, glucosamine); Combination of above |
| Osteoporosis medication | None; Vitamin D/Calcium; Bisphosphonate; Oestrogen/Raloxifene; Calcitonin/Teriparatide; Combination of above |
| Analgesic medication | None; WHO Pain Ladder 1 (mild); WHO Pain Ladder 2 and above (moderate to severe) |
| Hypertension | Normal (SBP < 140 & DBP < 90); Stage 1 (SBP ≥ 140/DBP ≥ 90); Stage 2 (SBP ≥ 160/DBP ≥ 100); Severe (SBP > 180 or DBP > 110) |
| 20m walk assessment | No risk; Risk of disability (based on cut-off point of ≥10 s) |
| Short Form-12 (SF-12) Mental | normal; low mental health score |
| Physical Activity Scale for Elderly (PASE) score | Normal physical activity (≥120); Low physical activity (<120) |
| Joint Space Narrowing (JSN)—Medial | Osteoarthritis Research Society International (OARSI) Grade 0–3 |
| Joint Space Narrowing (JSN)—Lateral | Osteoarthritis Research Society International (OARSI) Grade 0–3 |
| Kellgren–Lawrence Grade | Normal (0); Doubtful (1); Mild (2); Moderate (3); Severe (4) |
| Cartilage morphology (medial femorotibial joint) | None; thickness loss in one subregion; thickness loss in more than one subregion |
| Cartilage morphology (lateral femorotibial joint) | None; thickness loss in one subregion; thickness loss in more than one subregion |
| Cartilage morphology (patellofemoral joint) | None; thickness loss in one subregion; thickness loss in more than one subregion |
| Bone marrow lesions (medial femorotibial joint) | None; in one subregion; in more than one subregion |
| Bone marrow lesions (lateral femorotibial joint) | None; in one subregion; in more than one subregion |
| Bone marrow lesions (patellofemoral joint) | None; in one subregion; in more than one subregion |
| Meniscal tear | None; in one subregion; in more than one subregion |
| WOMAC | WOMAC < 24; WOMAC ≥ 24 |
| Data Interpretation Tasks | RStudio Software Package |
|---|---|
| Data Visualisation | Amelia (version 1.8.0) |
| Collinearity Visualisation | corrplot (version 0.92) |
| Data Pre-Processing—setting seed; sample split | simEd (version 2.0.0); caTools (version 1.17.1) |
| Area Under Curve Score; Receiver Operative Characteristic Curves | ROCR (version 1.0-11); pROC (version 1.18.0) |
| F1 Score—confusionMatrix | caret (version 3.45) |
| Generalised Linear Models (Logistic Regression) | glm (version 3.6.2) |
| Regularised General Linear Models (Lasso Regression) | glmnet (version 4.1-4) |
| Regularised General Linear Models (Ridge Regression) | glmnet (version 4.1-4) |
| Recursive Partitioning and Regression Trees (Decision Tree) | rpart (version 4.1.16) |
| Breiman and Cutler’s Random Forest Models | randomForest (version 4.7-1.1) |
| Generalised Boosted Regression Models | gbm (version 2.1.8) |
| ML Algorithm | Internal Test | External Test | ||
|---|---|---|---|---|
| Change in AUC * | Change in F1 * | Change in AUC * | Change in F1 * | |
| Logistic | −0.017 | 0.024 | 0.02 | −0.035 |
| Lasso | −0.013 | 0.017 | 0.014 | −0.011 |
| Ridge | −0.008 | 0.007 | 0.02 | −0.019 |
| Decision Tree | 0.024 | −0.042 | −0.087 | 0.158 |
| Random Forest | 0.009 | 0.051 | 0.017 | 0.007 |
| GBM | −0.007 | 0.019 | 0.018 | 0.023 |
- GBD 2021 Osteoarthritis Collaborators. Global, regional, and national burden of osteoarthritis, 1990–2020 and projections to 2050: A systematic analysis for the Global Burden of Disease Study 2021. Lancet Rheumatol. 2023 , 5 , 508–522. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Duong, V.; Oo, W.M.; Ding, C.; Culvenor, A.G.; Hunter, D.J. Evaluation and Treatment of Knee Pain: A Review. JAMA 2023 , 330 , 1568–1580. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Vitaloni, M.; Botto-van Bemden, A.; Sciortino Contreras, R.M.; Scotton, D.; Bibas, M.; Quintero, M.; Monfort, M.; Carné, X.; de Abajo, F.; Oswald, E.; et al. Global management of patients with knee osteoarthritis begins with quality of life assessment: A systematic review. BMC Musculoskelet. Disord. 2019 , 20 , 493. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Davis, A.M.; King, L.K.; Stanaitis, I.; Hawker, G.A. Fundamentals of osteoarthritis: Outcome evaluation with patient-reported measures and functional tests. Osteoarthr. Cartil. 2022 , 30 , 775–785. [ Google Scholar ] [ CrossRef ]
- Woolacott, N.F.; Corbett, M.S.; Rice, S.J.C. The use and reporting of WOMAC in the assessment of the benefit of physical therapies for the pain of osteoarthritis of the knee: Findings from a systematic review of clinical trials. Rheumatology 2012 , 51 , 1440–1446. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Deng, W.; Shao, H.; Zhou, Y.; Li, H.; Wang, Z.; Huang, Y. Reliability and validity of commonly used patient-reported outcome measures (PROMs) after medial unicompartmental knee arthroplasty. Orthop. Traumatol. Surg. Res. 2022 , 108 , 103096. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Kwon, S.B.; Ku, Y.; Han, H.; Lee, M.C.; Kim, H.C.; Ro, D.H. A machine learning-based diagnostic model associated with knee osteoarthritis severity. Sci. Rep. 2020 , 10 , 15743. [ Google Scholar ] [ CrossRef ]
- Giesinger, J.M.; Hamilton, D.F.; Jost, B.; Behrend, H.; Giesinger, K. WOMAC, EQ-5D and Knee Society Score Thresholds for Treatment Success after Total Knee Arthroplasty. J. Arthroplast. 2015 , 30 , 2154–2158. [ Google Scholar ] [ CrossRef ]
- Rahman, S.A.; Narhari, P.; Sharifudin, M.A.; Shokri, A.A. Western Ontario and McMaster Universities (WOMAC) Osteoarthritis Index as an Assessment Tool to Indicate Total Knee Arthroplasty in Patients with Primary Knee Osteoarthritis. IIUM Med. J. 2020 , 19 , 47–53. [ Google Scholar ] [ CrossRef ]
- Makhni, E.C.; Hennekes, M.E. The Use of Patient-Reported Outcome Measures in Clinical Practice and Clinical Decision Making. J. Am. Acad. Orthop. Surg. 2023 , 31 , 1059–1066. [ Google Scholar ] [ CrossRef ]
- Nagai, K.; Nakamura, T.; Fu, F.H. The diagnosis of early osteoarthritis of the knee using magnetic resonance imaging. Ann. Jt. 2018 , 3 , 110. [ Google Scholar ] [ CrossRef ]
- Mortensen, J.F.; Mongelard, K.B.G.; Radev, D.I.; Kappel, A.; Rasmussen, L.E.; Østgaard, S.E.; Odgaard, A. MRi of the knee compared to specialized radiography for measurements of articular cartilage height in knees with osteoarthritis. J. Orthop. 2021 , 25 , 191–198. [ Google Scholar ] [ CrossRef ]
- Yusuf, E.; Kortekaas, M.C.; Watt, I.; Huizinga, T.W.J.; Kloppenburg, M. Do knee abnormalities visualised on MRI explain knee pain in knee osteoarthritis? A systematic review. Ann. Rheum. Dis. 2011 , 70 , 60–67. [ Google Scholar ] [ CrossRef ]
- Culvenor, A.G.; Øiestad, B.E.; Hart, H.F.; Stefanik, J.J.; Guermazi, A.; Crossley, K.M. Prevalence of knee osteoarthritis features on magnetic resonance imaging in asymptomatic uninjured adults: A systematic review and meta-analysis. Br. J. Sports Med. 2019 , 53 , 1268–1278. [ Google Scholar ] [ CrossRef ]
- Khan, M.M.; Pincher, B.; Pacheco, R. Unnecessary magnetic resonance imaging of the knee: How much is it really costing the NHS? Ann. Med. Surg. 2021 , 70 , 102736. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Hofmann, B.; Håvik, V.; Andersen, E.R.; Brandsæter, I.Ø.; Kjelle, E. Low-value MRI of the knee in Norway: A register-based study to identify the proportion of potentially low-value MRIs and estimate the related costs. BMJ Open 2024 , 14 , e081860. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Ashikyan, O.; Buller, D.C.; Pezeshk, P.; McCrum, C.; Chhabra, A. Reduction of unnecessary repeat knee radiographs during osteoarthrosis follow-up visits in a large teaching medical center. Skelet. Radiol. 2019 , 48 , 1975–1980. [ Google Scholar ] [ CrossRef ]
- Ota, S.; Sasaki, E.; Sasaki, S.; Chiba, D.; Kimura, Y.; Yamamoto, Y.; Kumagai, Y.; Ando, M.; Tsuda, E.; Ishibashi, Y. Relationship between abnormalities detected by magnetic resonance imaging and knee symptoms in early knee osteoarthritis. Sci. Rep. 2021 , 11 , 15179. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Sakellariou, G.; Conaghan, P.G.; Zhang, W.; Bijlsma, J.W.J.; Boyesen, P.; D’Agostino, M.A.; Doherty, M.; Fodor, D.; Kloppenburg, M.; Miese, F.; et al. EULAR recommendations for the use of imaging in the clinical management of peripheral joint osteoarthritis. Ann. Rheum. Dis. 2017 , 76 , 1484–1494. [ Google Scholar ] [ CrossRef ]
- Sidey-Gibbons, J.A.M.; Sidey-Gibbons, C.J. Machine learning in medicine: A practical introduction. BMC Med. Res. Methodol. 2019 , 19 , 64. [ Google Scholar ] [ CrossRef ]
- Mahmoud, K.; Alagha, M.A.; Nowinka, Z.; Jones, G. Predicting total knee replacement at 2 and 5 years in osteoarthritis patients using machine learning. BMJ Surg. Interv. Health Technol. 2023 , 5 , e000141. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Nowinka, Z.; Alagha, M.A.; Mahmoud, K.; Jones, G.G. Predicting Depression in Patients with Knee Osteoarthritis Using Machine Learning: Model Development and Validation Study. JMIR Form. Res. 2022 , 6 , e36130. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Chan, L.C.; Li, H.H.T.; Chan, P.K.; Wen, C. A machine learning-based approach to decipher multi-etiology of knee osteoarthritis onset and deterioration. Osteoarthr. Cartil. Open 2021 , 3 , 100135. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Widera, P.; Welsing, P.M.J.; Ladel, C.; Loughlin, J.; Lafeber Floris, P.F.J.; Petit Dop, F.; Larkin, J.; Weinans, H.; Mobasheri, A.; Bacardit, J. Multi-classifier prediction of knee osteoarthritis progression from incomplete imbalanced longitudinal data. Sci. Rep. 2020 , 10 , 8427. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Jafarzadeh, S.; Felson, D.T.; Nevitt, M.C.; Torner, J.C.; Lewis, C.E.; Roemer, F.W.; Guermazi, A.; Neogi, T. Use of clinical and imaging features of osteoarthritis to predict knee replacement in persons with and without radiographic osteoarthritis: The most study. Osteoarthr. Cartil. 2020 , 28 , S308–S309. [ Google Scholar ] [ CrossRef ]
- Leung, K.; Zhang, B.; Tan, J.; Shen, Y.; Geras, K.J.; Babb, J.S.; Cho, K.; Chang, G.; Deniz, C.M. Prediction of Total Knee Replacement and Diagnosis of Osteoarthritis by Using Deep Learning on Knee Radiographs: Data from the Osteoarthritis Initiative. Radiology 2020 , 296 , 584–593. [ Google Scholar ] [ CrossRef ]
- Choi, Y.; Ra, H.J. Patient Satisfaction after Total Knee Arthroplasty. Knee Surg. Relat. Res. 2016 , 28 , 1–15. [ Google Scholar ] [ CrossRef ]
- Siontis, G.C.M.; Tzoulaki, I.; Castaldi, P.J.; Ioannidis, J.P.A. External validation of new risk prediction models is infrequent and reveals worse prognostic discrimination. J. Clin. Epidemiol. 2015 , 68 , 25–34. [ Google Scholar ] [ CrossRef ]
- Tugwell, P.; Knottnerus, J.A. Clinical prediction models are not being validated. J. Clin. Epidemiol. 2015 , 68 , 1–2. [ Google Scholar ] [ CrossRef ]
- Nevitt, M.C.; Felson, D.T.; Lester, G. The Osteoarthritis Initiative. In Protocol for the Cohort Study ; National Institute of Arthritis, Musculoskeletal and Skin Diseases: Bethesda, MD, USA, 2006. Available online: https://nda.nih.gov/oai/study-details.html (accessed on 21 May 2022).
- Segal, N.A.; Nevitt, M.C.; Gross, K.D.; Gross, K.D.; Hietpas, J.; Glass, N.A.; Lewis, C.E.; Torner, J.C. The Multicenter Osteoarthritis Study: Opportunities for rehabilitation research. PM R J. Inj. Funct. Rehabil. 2013 , 5 , 647–654. [ Google Scholar ] [ CrossRef ]
- Maredupaka, S.; Meshram, P.; Chatte, M.; Kim, W.H.; Kim, T.K. Minimal clinically important difference of commonly used patient-reported outcome measures in total knee arthroplasty: Review of terminologies, methods and proposed values. Knee Surg. Relat. Res. 2020 , 32 , 19. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- MacKay, C.; Clements, N.; Wong, R.; Davis, A.M. A systematic review of estimates of the minimally clinically important difference and patient acceptable symptom state of the western ontario and mcmaster universities osteoarthritis index in patients who underwent total hip and total knee replacement. Osteoarthr. Cartil. 2019 , 27 , S238–S239. [ Google Scholar ] [ CrossRef ]
- Escobar, A.; García Pérez, L.; Herrera-Espiñeira, C.; Aizpuru, F.; Sarasqueta, C.; Gonzalez Sáenz de Tejada, M.; Quintana, J.; Bilbao, A. Total knee replacement; minimal clinically important differences and responders. Osteoarthr. Cartil. 2013 , 21 , 2006–2012. [ Google Scholar ] [ CrossRef ]
- National Institute for Health and Care Excellence. Hypertension in Adults: Diagnosis and Management. 2019. Available online: https://www.nice.org.uk/guidance/ng136 (accessed on 21 May 2022).
- Bonakdari, H.; Jamshidi, A.; Pelletier, J.; Abram, F.; Tardif, G.; Martel-Pelletier, J. A warning machine learning algorithm for early knee osteoarthritis structural progressor patient screening. Ther. Adv. Musculoskelet. Dis. 2021 , 13 , 1759720X21993254. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Anekar, A.A.; Cascella, M. WHO Analgesic Ladder ; StatPearls Publishing: Treasure Island, FL, USA, 2022. [ Google Scholar ]
- Kokkotis, C.; Moustakidis, S.; Papageorgiou, E.; Giakas, G.; Tsaopoulos, D.E. Machine learning in knee osteoarthritis: A review. Osteoarthr. Cartil. Open 2020 , 2 , 100069. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Koo, B.S.; Eun, S.; Shin, K.; Yoon, H.; Hong, C.; Kim, D.; Hong, S.; Kim, Y.-G.; Lee, C.-K.; Yoo, B.; et al. Machine learning model for identifying important clinical features for predicting remission in patients with rheumatoid arthritis treated with biologics. Arthritis Res. Ther. 2021 , 23 , 178. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Venkatasubramaniam, A.; Wolfson, J.; Mitchell, N.; Barnes, T.; JaKa, M.; French, S. Decision trees in epidemiological research. Emerg. Themes Epidemiol. 2017 , 14 , 1–12. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Natekin, A.; Knoll, A. Gradient boosting machines, a tutorial. Front. Neurorobotics 2013 , 7 , 21. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Zou, K.H.; O’Malley, A.J.; Mauri, L. Receiver-Operating Characteristic Analysis for Evaluating Diagnostic Tests and Predictive Models. Circulation 2007 , 115 , 654–657. [ Google Scholar ] [ CrossRef ]
- Hajian-Tilaki, K. Receiver Operating Characteristic (ROC) Curve Analysis for Medical Diagnostic Test Evaluation. Casp. J. Intern. Med. 2013 , 4 , 627–635. [ Google Scholar ]
- Mandrekar, J.N. Receiver operating characteristic curve in diagnostic test assessment. J. Thorac. Oncol. 2010 , 5 , 1315–1316. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Wegier, W.; Ksieniewicz, P. Application of Imbalanced Data Classification Quality Metrics as Weighting Methods of the Ensemble Data Stream Classification Algorithms. Entropy 2020 , 22 , 849. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Bastick, A.N.; Wesseling, J.; Damen, J.; Verkleij, S.P.; Emans, P.J.; Bindels, P.J.; Bierma-Zeinstra, S.M. Defining knee pain trajectories in early symptomatic knee osteoarthritis in primary care: 5-year results from a nationwide prospective cohort study (CHECK). Br. J. Gen. Pract. 2016 , 66 , e32–e39. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Devana, S.K.; Shah, A.A.; Lee, C.; Roney, A.R.; van der Schaar, M.; SooHoo, N.F. A Novel, Potentially Universal Machine Learning Algorithm to Predict Complications in Total Knee Arthroplasty. Arthroplast. Today 2021 , 10 , 135–143. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Couronné, R.; Probst, P.; Boulesteix, A. Random forest versus logistic regression: A large-scale benchmark experiment. BMC Bioinform. 2018 , 19 , 270. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Binvignat, M.; Pedoia, V.; Butte, A.J.; Louati, K.; Klatzmann, D.; Berenbaum, F.; Mariotti-Ferrandiz, E.; Sellam, J. Use of machine learning in osteoarthritis research: A systematic literature review. RMD Open 2022 , 8 , e001998. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Gorial, F.I.; Anwer Sabah, S.A.; Kadhim, M.B.; Jamal, N.B. Functional Status in Knee Osteoarthritis and its Relation to Demographic and Clinical Features. Mediterr. J. Rheumatol. 2018 , 29 , 207–210. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Lee, J.Y.; Han, K.; Park, Y.G.; Park, S. Effects of education, income, and occupation on prevalence and symptoms of knee osteoarthritis. Sci. Rep. 2021 , 11 , 13983. [ Google Scholar ] [ CrossRef ]
- Sinatti, P.; Sánchez Romero, E.A.; Martínez-Pozas, O.; Villafañe, J.H. Effects of Patient Education on Pain and Function and Its Impact on Conservative Treatment in Elderly Patients with Pain Related to Hip and Knee Osteoarthritis: A Systematic Review. Int. J. Environ. Res. Public Health 2022 , 19 , 6194. [ Google Scholar ] [ CrossRef ]
- Bzdok, D.; Altman, N.; Krzywinski, M. Statistics versus machine learning. Nat. Methods 2018 , 15 , 233–234. [ Google Scholar ] [ CrossRef ]
- Perry, T.A.; Wang, X.; Gates, L.; Parsons, C.M.; Sanchez-Santos, M.T.; Garriga, C.; Cooper, C.; Nevitt, M.C.; Hunter, D.J.; Arden, N.K. Occupation and risk of knee osteoarthritis and knee replacement: A longitudinal, multiple-cohort study. Semin. Arthritis Rheum. 2020 , 50 , 1006–1014. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Feehan, M.; Owen, L.A.; McKinnon, I.M.; DeAngelis, M.M. Artificial Intelligence, Heuristic Biases, and the Optimization of Health Outcomes: Cautionary Optimism. J. Clin. Med. 2021 , 10 , 5284. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Neogi, T.; Felson, D.; Niu, J.; Nevitt, M.; Lewis, C.E.; Aliabadi, P.; Sack, B.; Torner, J.; Bradley, L.; Zhang, Y. Association between radiographic features of knee osteoarthritis and pain: Results from two cohort studies. BMJ 2009 , 339 , b2844. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Guan, B.; Liu, F.; Mizaian, A.H.; Demehri, S.; Samsonov, A.; Guermazi, A.; Kijowski, R. Deep learning approach to predict pain progression in knee osteoarthritis. Skelet. Radiol. 2022 , 51 , 363–373. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Javaid, M.K.; Kiran, A.; Guermazi, A.; Kwoh, K.; Zaim, S.; Carbone, L.; Harris, T.; McCulloch, C.E.; Arden, N.K.; Lane, N.E.; et al. Individual MRI and radiographic features of knee OA in subjects with unilateral knee pain: Health ABC study. Arthritis Rheumatol. 2012 , 64 , 3246–3255. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Ashinsky, B.G.; Bouhrara, M.; Coletta, C.E.; Lehallier, B.; Urish, K.L.; Lin, P.; Goldberg, I.G.; Spencer, R.G. Predicting early symptomatic osteoarthritis in the human knee using machine learning classification of magnetic resonance images from the Osteoarthritis Initiative. J. Orthop. Res. 2017 , 35 , 2243–2250. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Schiratti, J.; Dubois, R.; Herent, P.; Cahané, D.; Dachary, J.; Clozel, T.; Wainrib, G.; Keime-Guibert, F.; Lalande, A.; Pueyo, M.; et al. A deep learning method for predicting knee osteoarthritis radiographic progression from MRI. Arthritis Res. Ther. 2021 , 23 , 262. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Karimi, D.; Dou, H.; Warfield, S.K.; Gholipour, A. Deep learning with noisy labels: Exploring techniques and remedies in medical image analysis. Med. Image Anal. 2020 , 65 , 101759. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Chang, G.H.; Felson, D.T.; Qiu, S.; Guermazi, A.; Capellini, T.D.; Kolachalama, V.B. Assessment of knee pain from MR imaging using a convolutional Siamese network. Eur. Radiol. 2020 , 30 , 3538–3548. [ Google Scholar ] [ CrossRef ]
- Abedin, J.; Antony, J.; McGuinness, K.; Moran, K.; O’Connor, N.E.; Rebholz-Schuhmann, D.; Newell, J. Predicting knee osteoarthritis severity: Comparative modeling based on patient’s data and plain X-ray images. Sci. Rep. 2019 , 9 , 5761. [ Google Scholar ] [ CrossRef ]
- Johnson, J.M.; Khoshgoftaar, T.M. Survey on deep learning with class imbalance. J. Big Data 2019 , 6 , 27. [ Google Scholar ] [ CrossRef ]
| Model | Category | Feature |
|---|---|---|
| Clinical and Imaging Datasets | Patient Demographics | Age |
| Sex | ||
| Ethnicity | ||
| Living Status | ||
| Education Status | ||
| Employment Status | ||
| Body Mass Index (BMI) | ||
| Past Medical/Surgical History | Comorbidities (Charlson Comorbidity Index) | |
| Inflammatory Arthritis | ||
| Injury to knee | ||
| Knee Surgery | ||
| Drug History | Osteoarthritis medication | |
| Osteoporosis medication | ||
| Analgesic medication | ||
| Baseline Examination | Hypertension | |
| 20 m walk assessment | ||
| Baseline Questionnaire | Short Form-12 (SF-12) Mental Component | |
| Physical Activity Scale for Elderly (PASE) score | ||
| Imaging Dataset | Radiograph | Joint Space Narrowing (JSN)—Medial |
| Joint Space Narrowing (JSN)—Lateral | ||
| Kellgren–Lawrence (KL) Grade | ||
| Magnetic Resonance Imaging | Cartilage morphology (medial femorotibial joint) | |
| Cartilage morphology (lateral femorotibial joint) | ||
| Cartilage morphology (patellofemoral joint) | ||
| Bone marrow lesions (medial femorotibial joint) | ||
| Bone marrow lesions (lateral femorotibial joint) | ||
| Bone marrow lesions (patellofemoral joint) | ||
| Meniscal tear | ||
| Outcome | 2-year WOMAC score | |
| Feature | Most Common Subgroup | OAI, N (%) (n = 2408) | MOST, N (%) (n = 629) |
|---|---|---|---|
| Age | 60–70 years | 827 (34.3) | 238 (37.8) |
| Sex | Female | 1531 (63.6) | 369 (58.7) |
| Ethnicity | White/Caucasian | 2031 (84.3) | 563 (89.5) |
| Living Status | Lives with someone | 1932 (80.2) | 525 (83.5) |
| Education Status | Graduate degree | 757 (31.4) | 147 (23.4) |
| Employment Status | Paid work | 1430 (59.4) | 420 (66.8) |
| Body Mass Index (BMI) | Overweight (25.0–29.9) | 982 (40.8) | 258 (41.0) |
| Comorbidities (Charlson Comorbidity Index) | None | 1846 (76.7) | 485 (77.1) |
| Inflammatory Arthritis | None | 2291 (95.1) | 621 (98.7) |
| Injury to knee | None | 1293 (53.7) | 372 (59.1) |
| Knee Surgery | None | 1807 (75.0) | 522 (83.0) |
| Osteoarthritis medication | None | 1480 (61.5) | 434 (69.0) |
| Osteoporosis medication | None | 1095 (45.5) | 316 (50.2) |
| Analgesic medication | None | 1453 (60.3) | 154 (24.5) |
| Hypertension | Normal (SBP < 140 & DBP < 90) | 1919 (79.7) | 512 (81.4) |
| 20m walk assessment | Normal pace (≥1.22 s) | 1692 (70.3) | 392 (62.3) |
| Short Form-12(SF-12) Mental Component | Normal mental health status | 1214 (50.4) | 319 (50.7) |
| Physical Activity Scale for Elderly (PASE) | Normal physical activity (≥120) | 1614 (67.0) | 482 (76.6) |
| Joint Space Narrowing (JSN)—Medial | None | 974 (40.4) | 391 (62.2) |
| Joint Space Narrowing (JSN)—Lateral | None | 1905 (79.1) | 509 (80.9) |
| Kellgren–Lawrence (KL) Grade | Moderate (KL = 3) | 739 (30.7) | 79 (12.6) |
| Cartilage morphology (medial FTJ ) | No thickness loss | 937 (38.9) | 271 (43.1) |
| Cartilage morphology (lateral FTJ ) | No thickness loss | 1144 (47.5) | 345 (54.8) |
| Cartilage morphology (PFJ ) | Thickness loss in one or more subregion | 1463 (60.8) | 145 (23.1) |
| Bone marrow lesions (medial FTJ ) | None | 1532 (63.6) | 474 (75.4) |
| Bone marrow lesions (lateral FTJ ) | None | 1899 (78.9) | 542 (86.2) |
| Bone marrow lesions (PFJ ) | None | 940 (39.0) | 283 (45.0) |
| Meniscal tear | None | 1151 (47.8) | 415 (66.0) |
| WOMAC | Normal (<24) | 1775 (73.7) | 460 (73.1) |
| ML Algorithm | Clinical Dataset | Imaging Dataset | ||
|---|---|---|---|---|
| Training AUC (95% CI) | Internal Test AUC (95% CI) | Training AUC (95% CI) | Internal Test AUC (95%CI) | |
| Logistic | 0.745 (0.721–0.770) | 0.749 (0.700–0.797) | 0.791 (0.768–0.814) | 0.732 (0.682–0.782) |
| Lasso | 0.734 (0.709–0.759) | 0.751 (0.703–0.800) | 0.779 (0.755–0.803) | 0.738 (0.688–0.787) |
| Ridge | 0.730 (0.705–0.756) | 0.753 (0.705–0.801) | 0.777 (0.753–0.801) | 0.745 (0.696–0.795) |
| Decision Tree | 0.628 (0.602–0.655) | 0.630 (0.577–0.682) | 0.667 (0.639–0.694) | 0.654 (0.600–0.707) |
| Random Forest | 0.784 (0.761–0.808) | 0.777 (0.730–0.823) | 0.820 (0.799–0.842) | 0.786 (0.739–0.832) |
| GBM | 0.736 (0.711–0.761) | 0.759 (0.712–0.806) | 0.783 (0.760–0.807) | 0.752 (0.703–0.801) |
| ML Algorithm | Clinical Dataset | Imaging Dataset | ||
|---|---|---|---|---|
| Internal Test F1 | External Test F1 | Internal Test F1 | External Test F1 | |
| Logistic | 0.526 | 0.547 | 0.550 | 0.512 |
| Lasso | 0.528 | 0.534 | 0.545 | 0.523 |
| Ridge | 0.536 | 0.541 | 0.543 | 0.522 |
| Decision Tree | 0.473 | 0.286 | 0.431 | 0.444 |
| Random Forest | 0.566 | 0.529 | 0.617 | 0.536 |
| GBM | 0.539 | 0.525 | 0.558 | 0.548 |
| Clinical Dataset | Influence Factor | Imaging Dataset | Influence Factor |
|---|---|---|---|
| Education Background | 21.99 | KL Grade | 9.60 |
| Arthritis History | 10.56 | Education Background | 7.66 |
| Comorbidities | 9.73 | 20 m walk test | 7.62 |
| Osteoporosis medication | 8.59 | JSN—Medial | 7.46 |
| Past Knee Surgery | 6.70 | Pain medication | 5.85 |
| The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
Share and Cite
Nair, A.; Alagha, M.A.; Cobb, J.; Jones, G. Assessing the Value of Imaging Data in Machine Learning Models to Predict Patient-Reported Outcome Measures in Knee Osteoarthritis Patients. Bioengineering 2024 , 11 , 824. https://doi.org/10.3390/bioengineering11080824
Nair A, Alagha MA, Cobb J, Jones G. Assessing the Value of Imaging Data in Machine Learning Models to Predict Patient-Reported Outcome Measures in Knee Osteoarthritis Patients. Bioengineering . 2024; 11(8):824. https://doi.org/10.3390/bioengineering11080824
Nair, Abhinav, M. Abdulhadi Alagha, Justin Cobb, and Gareth Jones. 2024. "Assessing the Value of Imaging Data in Machine Learning Models to Predict Patient-Reported Outcome Measures in Knee Osteoarthritis Patients" Bioengineering 11, no. 8: 824. https://doi.org/10.3390/bioengineering11080824
Article Metrics
Article access statistics, further information, mdpi initiatives, follow mdpi.

Subscribe to receive issue release notifications and newsletters from MDPI journals
The page could not be loaded. The CMS.gov Web site currently does not fully support browsers with "JavaScript" disabled. Please enable "JavaScript" and revisit this page or proceed with browsing CMS.gov with "JavaScript" disabled. Instructions for enabling "JavaScript" can be found here. Please note that if you choose to continue without enabling "JavaScript" certain functionalities on this website may not be available.

An official website of the United States government
Here's how you know
The .gov means it's official.
Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure.
The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.

Tracking Sheet
Intraarticular knee injections of hyaluronan, document note, note history, contractor information.
| Contractor Name | Contract Type | Contract Number | Jurisdiction | States |
|---|---|---|---|---|
| MAC - Part A | 05101 - MAC A | J - 05 | Iowa | |
| MAC - Part B | 05102 - MAC B | J - 05 | Iowa | |
| MAC - Part A | 05201 - MAC A | J - 05 | Kansas | |
| MAC - Part B | 05202 - MAC B | J - 05 | Kansas | |
| MAC - Part A | 05301 - MAC A | J - 05 | Missouri - Entire State | |
| MAC - Part B | 05302 - MAC B | J - 05 | Missouri - Entire State | |
| MAC - Part A | 05401 - MAC A | J - 05 | Nebraska | |
| MAC - Part B | 05402 - MAC B | J - 05 | Nebraska | |
| MAC - Part A | 05901 - MAC A | J - 05 | Alabama Alaska Arizona Arkansas California - Entire State Colorado Connecticut Delaware Florida Georgia Hawaii Idaho Illinois Indiana Iowa Kansas Kentucky Louisiana Maine Maryland Massachusetts Michigan Mississippi Missouri - Entire State Montana Nebraska Nevada New Hampshire New Jersey New Mexico North Carolina North Dakota Ohio Oklahoma Oregon Pennsylvania Rhode Island South Carolina South Dakota Tennessee Texas Utah Vermont Virginia Washington West Virginia Wisconsin Wyoming | |
| MAC - Part A | 08101 - MAC A | J - 08 | Indiana | |
| MAC - Part B | 08102 - MAC B | J - 08 | Indiana | |
| MAC - Part A | 08201 - MAC A | J - 08 | Michigan | |
| MAC - Part B | 08202 - MAC B | J - 08 | Michigan |
LCD Information
Document information.
CPT codes, descriptions, and other data only are copyright 2023 American Medical Association. All Rights Reserved. Applicable FARS/HHSARS apply.
Fee schedules, relative value units, conversion factors and/or related components are not assigned by the AMA, are not part of CPT, and the AMA is not recommending their use. The AMA does not directly or indirectly practice medicine or dispense medical services. The AMA assumes no liability for data contained or not contained herein.
Current Dental Terminology © 2023 American Dental Association. All rights reserved.
Copyright © 2024 , the American Hospital Association, Chicago, Illinois. Reproduced with permission. No portion of the AHA copyrighted materials contained within this publication may be copied without the express written consent of the AHA. AHA copyrighted materials including the UB‐04 codes and descriptions may not be removed, copied, or utilized within any software, product, service, solution, or derivative work without the written consent of the AHA. If an entity wishes to utilize any AHA materials, please contact the AHA at 312‐893‐6816.
Making copies or utilizing the content of the UB‐04 Manual, including the codes and/or descriptions, for internal purposes, resale and/or to be used in any product or publication; creating any modified or derivative work of the UB‐04 Manual and/or codes and descriptions; and/or making any commercial use of UB‐04 Manual or any portion thereof, including the codes and/or descriptions, is only authorized with an express license from the American Hospital Association. The American Hospital Association (the "AHA") has not reviewed, and is not responsible for, the completeness or accuracy of any information contained in this material, nor was the AHA or any of its affiliates, involved in the preparation of this material, or the analysis of information provided in the material. The views and/or positions presented in the material do not necessarily represent the views of the AHA. CMS and its products and services are not endorsed by the AHA or any of its affiliates.
This LCD outlines limited coverage for this service with specific details under Coverage Indications, Limitations and/or Medical Necessity .
Grammatical changes made throughout with no change in coverage.

CMS National Coverage Policy
This LCD supplements but does not replace, modify or supersede existing Medicare applicable National Coverage Determinations (NCDs) or payment policy rules and regulations for intra-articular injection of hyaluronate polymers. Federal statute and subsequent Medicare regulations regarding provision and payment for medical services are lengthy. They are not repeated in this LCD. Neither Medicare payment policy rules nor this LCD replace, modify or supersede applicable state statutes regarding medical practice or other health practice professions acts, definitions and/or scopes of practice. All providers who report services for Medicare payment must fully understand and follow all existing laws, regulations and rules for Medicare payment for intra-articular injection of hyaluronate polymers and must properly submit only valid claims for them. Please review and understand them and apply the medical necessity provisions in the policy within the context of the manual rules. Relevant CMS manual instructions and policies may be found in the following Internet-Only Manuals (IOMs) published on the CMS Web site:
IOM Citations
- CMS IOM Publication 100-02, Medicare Benefit Policy Manual, Chapter 15 Covered Medical and Other Health Services, § 50.3 Incident-to Requirements and 50.4.1 Approved Use Of Drug.
- CMS IOM Publication 100-04, Medicare Claims Processing Manual, Chapter 17 Drugs and Biologicals, § 40 Discarded Drugs and Biologicals and 90.2 Drugs, Biologicals, and Radiopharmaceuticals.
- CMS IOM Publication 100-08, Medicare Program Integrity Manual, Chapter 13 Local Coverage Determinations, § 13.5.4 Reasonable and Necessary Provision in an LCD.
Social Security Act (Title XVIII) Standard References
- Title XVIII of the Social Security Act, Section 1833(e) states that no payment shall be made to any provider for any claim that lacks the necessary information to process the claim.
- Title XVIII of the Social Security Act, Section 1862(a)(1)(A) states that no Medicare payment shall be made for items or services which are not reasonable and necessary for the diagnosis or treatment of illness or injury.
- Title XVIII of the Social Security Act, Section 1862(a)(7). This section excludes routine physical examinations.
Coverage Guidance
Compliance with the provisions in this policy may be monitored and addressed through post payment data analysis and subsequent medical review audits.
History/Background and/or General Information
Hyaluronic acid, also known as hyaluronan or hyaluronate, is a naturally occurring substance found in the synovial fluid surrounding joints. Osteoarthritic joints are found to have lower concentrations of hyaluronic acid. 1 Intra-articular injection of hyaluronic acid, also known as viscosupplementation, has been proposed as a means of restoring the normal viscoelasticity of the synovial fluid in individuals with osteoarthritis.
Viscosupplementation is most commonly used to treat symptoms of osteoarthritis of the knee. Osteoarthritis (OA) results from articular cartilage failure due to the complex interplay of genetic, metabolic, biochemical and biomechanical factors with a secondary component of inflammation. The primary symptom of osteoarthritis of the knee is pain, however, because cartilage is aneural, significant radiographic findings are often noted in asymptomatic individuals imaged for other reasons.
Typical candidates for viscosupplementation are those with knee osteoarthritis who have failed to improve with other non-surgical treatments. Several synthetic preparations of hyaluronic acid-based polymers have been approved by the U.S. Food and Drug Administration (FDA) and are indicated for the treatment of pain in OA of the knee in patients who have failed to respond adequately to conservative non-pharmacologic therapy and simple analgesics (e.g., acetaminophen) or non-steroidal anti-inflammatory drugs (NSAIDS). 2
By adding hyaluronic acid to the existing joint fluid of an osteoarthritic knee, the goal is to:
- Facilitate better knee movement
- Reduce pain
- Perhaps slow osteoarthritis progression 3
The most recent research, however, has not found viscosupplementation to be effective at significantly reducing pain or improving function. Although some patients report pain relief with the procedure, others are not helped by the injections. 1
Covered Indications
Viscosupplementation therapy for the knee via intra-articular injections of hyaluronic preparations will be considered medically reasonable and necessary when ALL of the following conditions are met:
- The patient is symptomatic. Such symptoms may include pain which interferes with the activities of daily living such as ambulation and prolonged standing, or pain interrupting sleep, crepitus, and/or knee stiffness.
- The clinical diagnosis is supported by radiologic evidence of osteoarthritis of the knee such as joint space narrowing, subchondral sclerosis, osteophytes and sub-chondral cysts.
- If appropriate, other diagnoses have been excluded by appropriate evaluation and management services, laboratory and imaging studies (i.e., the pain and functional disability is not considered likely to be due to a diagnosis other than osteoarthritis of the knee).
- Nonpharmacologic therapy (such as but not limited to home exercise program, education, weight loss, physical therapy if indicated); and
- If not contraindicated, simple analgesics and (e.g., acetaminophen) or NSAIDS per hyaluronan product prescribing information.
- The patient has failed to respond to aspiration of the knee when effusion is present and intra-articular corticosteroid injection therapy when inflammation is a significant component of the patient’s symptoms and intra-articular corticosteroids are not contraindicated.
A repeat series* of hyaluronan knee injection(s) for patients who have responded to a prior series is considered to be reasonable and necessary under the following circumstances:
- Symptoms have recurred AND ,
- At least six months have elapsed since the prior series of injections AND ,
- There was significant improvement in pain and functional capacity achieved with the prior series of injections using a standardized assessment tool OR
- There is significant reduction in the doses of NSAID medications taken or reduction in the number of intra-articular steroid injections to the knees during the six-month period following the injection(s).
*Note: A series is defined as a set of injections for each joint and each treatment (initial or repeat).
Limitations The following are considered not reasonable and necessary and therefore will be denied:
- Drugs and biologicals and other products approved for marketing by the FDA are considered safe and effective when used for indications specified on the labeling. The labeling lists the safe and effective, i.e., medically reasonable and necessary dosage and frequency. Therefore, doses and frequencies that exceed the accepted standard of recommended dosage and/or frequency, as described in the package insert, are considered not reasonable and necessary and therefore, not subject to coverage.
- Intra-articular injections of other therapeutic agents, such as corticosteroids, should not be performed in the same knee during the course of viscosupplementation therapy unless there is documented medical necessity (e.g., for documented reactions requiring the use of the additional therapeutic agent).
- Viscosupplementation of joints other than the knee(s) are considered not reasonable and necessary and are not subject to coverage.
- Imaging procedures (e.g., arthrography, CT scan, MRI) for the purpose of visualization of the knee to provide guidance for needle placement are considered not medically reasonable and necessary and will not be covered. The only imaging procedures that may be considered reasonable and necessary for the purpose of needle guidance for viscosupplementation are fluoroscopy or ultrasound. If needle guidance is utilized, the documentation must support that the presentation of the patient’s affected knee on the day of the procedure makes needle insertion problematic. Routine use of fluoroscopy or ultrasound guidance may result in a pre-payment medical review of records. No other imaging modality for the purpose of needle guidance and placement will be covered. The imaging modality used for the purpose of needle guidance must be reported appropriately and in conjunction with the appropriate intra-articular injection procedure code for the knee. For coding information on the use of imaging procedures with viscosupplementation of the knee, please refer to the companion Article A56157, Billing and Coding: Intraarticular Knee Injections of Hyaluronan.
- If the hyaluronan preparation is denied, then any associated procedure code(s) (e.g., intra-articular injection, fluoroscopy, ultrasound) would be considered not medically reasonable and necessary.
- The course of treatment must consist of the use of one agent for the entire course of treatment. Therefore, initiating a course of treatment with one agent, then switching before completion to a different agent is considered not medically reasonable and necessary. Example: Treatment is initiated with Synvisc. After the application of two doses, the provider switches to Synvisc-One. The Synvisc-One would not be considered medically reasonable and necessary.
- Coverage of viscosupplementation therapy of the knee assumes that knee arthroplasty is not being considered as a current treatment option.
- Viscosupplementation is considered not medically reasonable and necessary following total or partial knee arthroplasty.
- Viscosupplementation is considered not medically reasonable and necessary at the end of a knee surgical procedure or during the postoperative period following a knee surgical procedure (e.g., anterior cruciate ligament [ACL] reconstruction or arthroscopic meniscectomy). It would be expected that use of viscosupplementation would not be initiated until after the patient has made a full recovery from the knee surgery (individualized for each patient); and the patient is symptomatic with a diagnosis of osteoarthritis; and clinical presentation meets the covered indications as stated.
- When the diagnosis is anything other than osteoarthritis
- As the initial treatment of osteoarthritis of the knee
- When failure of/or contraindication to conservative therapy and/or corticosteroid injections are not documented in the medical record
- When a repeat series of injections is initiated prior to six months after completion of the previous course of treatment
- When a repeat series of injections is administered when there was no symptomatic/functional improvement evidenced from the previous series of injections
- Topical application of hyaluronate preparations
Provider Qualifications
Services will be considered medically reasonable and necessary only if both of the following criteria are met:
- All aspects of the procedure and its related care are within the scope of practice of the provider’s professional licensure; and
- All procedures are performed by appropriately trained providers in the appropriate setting. Patient safety and quality of care mandate that healthcare professionals who perform intra-articular injections for treatment of osteoarthritis of the knee are appropriately trained and are competent to perform all aspects of these procedures safely and effectively. The core curriculum of any training program should include the performance and management of the procedures addressed in this policy with documentation of trainee competency assessment included by formal examination and case history document review.
*At a minimum, training must cover and develop an understanding of anatomy and drug pharmacodynamics and kinetics, proficiency in evaluation, diagnosis and management of diseases necessitating the procedures, technical performance of the procedure and performing and interpreting medically reasonable imaging modalities required for procedure performance (imaging technique, contrast material use, and image interpretation) as well as the evaluation, diagnosis and management of potential complications from the intervention.
Acceptable training or certification may be evidenced by any one of the following means:
- Satisfactory completion of an Accreditation Council for Graduate Medical Education (ACGME) or American Osteopathic Association (AOA) accredited residency and/or fellowship program in a relevant specialty; or
- Board certification in a relevant specialty by an American Board of Medical Specialties (ABMS) member board or equivalent AOA board; or
- Satisfactory completion of an accredited non-physician practitioner educational program that provides substantially equal content and scope as those mentioned in bullets 1 or 2 above and includes the minimum requirements stated in the preceding paragraph (see * above), with trainee competency directly assessed by state licensure examination or certification examination by a nationally recognized accrediting agency and maintenance of a case log of procedures performed; or
- Demonstration of satisfactory performance of the specific services in this policy on a regular basis over the five years immediately preceding implementation of this policy. Medicare considers an average of ten services per month to meet this requirement, and may be substantiated by Medicare or other payer claim history supported by patient medical records of appropriate care, procedural performance and outcomes.
Reimbursement for procedures utilizing imaging may be made to providers who meet training requirements for the procedures in this policy when permitted under relevant state professional practice acts.
Documentation of training and licensures must be made available to Medicare upon request.
Please refer to the Local Coverage Article: Billing and Coding: Intraarticular Knee Injections of Hyaluronan , A56157, for coding guidelines and drug wastage information.
Notice: Services performed for any given diagnosis must meet all the indications and limitations stated in this policy, the general requirements for medical necessity as stated in CMS payment policy manuals, any and all existing CMS national coverage determinations, and all Medicare payment rules.
The redetermination process may be utilized for consideration of services performed outside of the reasonable and necessary requirements in this LCD.
Technology Assessment Systematic Review
Newberry et al 4 conducted a systematic review for effectiveness of hyaluronic acid in the treatment of severe degenerative joint disease (DJD) of the knee. The Coverage and Analysis Group at the Centers for Medicare and Medicaid Services (CMS) requested from The Technology Assessment Program (TAP) at the Agency for Healthcare Research and Quality (AHRQ), a review of the evidence that intraarticular injections of hyaluronic acid (HA) in individuals with degenerative joint disease (osteoarthritis [OA]) of the knee improve function and quality of life (QoL) and that they delay or prevent the need for total knee replacement (TKR), specifically for individuals age 65 and over. The results of the systematic review were as follows: Only one randomized controlled trial (RCT) reported on delay or avoidance of TKR as a pre-specified outcome of interest and found a non-statistically significantly longer delay of TKR compared with placebo; two RCTs reported TKR only as a secondary outcome; and 13 published observational studies reported on TKR as an outcome in HA-treated participants.
Eighteen RCTs that enrolled participants of average age 65 or older reported on functional outcomes of intra-articular HA injection: pooled analysis of ten sham-injection placebo-controlled, assessor-blinded trials showed a standardized mean difference of -0.23 (95% CI -0.34, -0.02) significantly favoring HA at 6 months’ follow-up. Durability of effect could not be assessed because of the short duration of most studies. Too few head-to-head trials were available to assess superiority of one product over another. Three RCTs that compared changes in QoL/Health-Related (HR) QoL between HA- and placebo-treated participants reported no differences between active treatment and placebo. Two recent large, good quality systematic reviews that conducted meta-analysis of the effects of HA on pain and function (pooling 71 and 52 RCTs for the outcome of pain, respectively) showed a significant and clinically important effect of HA on both outcomes among adults of all ages, but a subgroup analysis that included only the largest double-blind placebo-controlled studies reduced the average effect of HA to less than the prespecified minimum clinically important difference. Studies of intra-articular HA reported few serious adverse events, with no statistically significant difference in the rates of serious or non-serious adverse events between HA- and placebo-treated groups.
The authors concluded that trials enrolling older participants show a small, statistically significant effect of HA on function and relatively few serious adverse events; however, no studies limited participation to those 65 years or older. No conclusions can be drawn from the available literature on delay or avoidance of TKR using HA. Studies that can compare large numbers of treated and untreated individuals, preferably with a randomized design, are needed to answer this question.
Evidence-Based Guidelines
The Department of Veterans Affairs (VA) and The Department of Defense (DoD) Evidence Based Clinical Practice Guideline for Non-surgical Management of the Hip and Knee Osteoarthritis Guideline Summary 5 states there is insufficient evidence to recommend for or against the use of intra-articular hyaluronate/hylan injection in patients with osteoarthritis of the knee; however, it may be considered for patients who have not responded adequately to nonpharmacologic measures and who have an inadequate response, intolerable adverse events, or contraindications to other pharmacologic therapies.
The National Institute for Health and Care Excellence (NICE) Clinical Guideline Osteoarthritis: care and management 6 recommendations include: do not offer intra-articular hyaluronan injections for the management of osteoarthritis.
The American Academy of Orthopaedic Surgeons (AAOS) Treatment of Osteoarthritis of the Knee: Evidence-Based Guideline, 2nd Edition 7 , is based on a systematic review of the current scientific and clinical research. This guideline contains 15 recommendations, replaces the 2008 AAOS clinical practice guideline, and was reevaluated earlier than the 5-year recommendation of the National Guideline Clearinghouse because of methodologic concerns regarding the evidence used in the first guideline. The current guideline does not support the use of viscosupplementation for the treatment of osteoarthritis of the knee. In addition, the work group highlighted the need for better research in the treatment of knee osteoarthritis.
Hochberg et al 8 (American College of Rheumatology 2012 recommendations for the use of nonpharmacologic and pharmacologic therapies in osteoarthritis of the hand, hip, and knee) conditionally recommended for the initial management of patients with knee OA included acetaminophen, oral and topical NSAIDs, tramadol, and intraarticular corticosteroid injections. Intraarticular hyaluronate injections, duloxetine, and opioids were conditionally recommended in patients who had an inadequate response to initial therapy.
Published Literature
Filardo et al 9 conducted a double-blind randomized controlled trial to evaluate the effects, in terms of pain control and functional recovery, provided by a single HA injection performed at the end of arthroscopic meniscectomy. The results showed no major adverse events were reported using HA postoperatively. A statistically significant increase in all the clinical scores was reported in both treatment groups, but no significant intergroup difference was documented at any follow-up evaluation. No difference was observed also in the objective measurements. The mean time to return to full sports activity was not different between groups, and a comparable satisfaction rate was recorded in both treatment groups. The authors concluded that early postoperative viscosupplementation did not provide significant clinical benefits after arthroscopic meniscectomy. Despite the lack of major adverse events, the administration of a single HA injection at the end of the surgical procedure is not a successful strategy to provide either faster functional recovery or symptomatic improvement after meniscectomy.
DiMartino et al 10 conducted a double-blind, randomized controlled trial to evaluate pain control and functional recovery provided by a single injection of HA performed the day after anterior cruciate ligament (ACL) reconstruction. The results showed no severe adverse events were documented after early viscosupplementation. A significant improvement was documented in both treatment groups. Significant differences were documented in the transpatellar circumference at 60 days and in active range of motion (ROM) at 30 days postoperatively; patients who received HA had better values compared with the placebo group (P equal to .022 and .027, respectively). No statistically relevant intergroup differences were found in the clinical scores. The authors concluded that the study documented no adverse events and had some positive findings in terms of active ROM recovery and transpatellar circumference reduction. However, the early postoperative application of viscosupplementation did not lead to significant improvement in clinical scores after ACL reconstruction.
Berkoff et al 11 conducted a review to determine the effect of ultrasound guidance on the accuracy of needle placement, clinical outcomes, and cost-effectiveness in comparison with anatomical landmark-guided intra-articular large joint injections, with particular emphasis on the knee. A total of 13 relevant studies were identified; 5 studied the knee, 7 studied the shoulder, 1 used both the knee and shoulder, and none studied the hip. Ultrasound was used in 7 studies; the remaining studies utilized air arthrography, fluoroscopy, magnetic resonance arthrography, or magnetic resonance imaging. Across all studies (using all imaging modalities and all joints), needle placement accuracy ranged from 63% to 100% with ultrasound and from 39% to 100% with conventional anatomical guidance. Imaging guidance improved the accuracy of intra-articular injections of the knee (96.7% versus 81.0%, P less than 0.001) and shoulder (97.3% versus 65.4%, P less than 0.001). In particular, ultrasound guidance of knee injections resulted in better accuracy than anatomical guidance (95.8% versus 77.8%, P less than 0.001), yielding an odds ratio of 6.4 (95% confidence interval 2.9-14). Ultrasound guidance notably improves injection accuracy in the target intra-articular joint space of large joints including the knee. The enhanced injection accuracy achieved with ultrasound needle guidance directly improves patient-reported clinical outcomes and cost-effectiveness.
Various polymers of hyaluronic acid have been approved and marketed as implanted prosthetic devices. Clinical practice guidelines for the treatment of knee osteoarthritis have conflicting recommendations for intra-articular hyaluronic acid treatment for knee osteoarthritis. 12 The systematic review by the technology assessment program 4 reported a small, statistically significant effect of HA on function. Clinical studies of sodium hyaluronate and hylan G-F 20 have demonstrated that injection of these agents into the joint space of osteoarthritic knees is sometimes marginally more effective than placebo procedures in reduction of pain and improvement in functional capacity in some patients. These marginal beneficial results are more pronounced with the larger molecular weight compound hylan G-F 20. There is no data indicating that these agents reverse or retard the osteoarthritic process in the injected joints. The long-term effects of repeated injections are unknown.
Literature evaluating pain control and functional recovery of viscosupplementation performed at the end of arthroscopic meniscectomy or in the postoperative period after ACL reconstruction does not demonstrate significant clinical benefits. 9-10
Literature suggests that fluoroscopy or ultrasound guidance may improve injection accuracy in the target intra-articular joint space of large joints including the knee. The use of other imaging procedures for viscosupplement injections has not been established as having an improvement on health outcomes.
Proposed Process Information
| Changes | Fields Changed |
|---|---|
| N/A |
| Meeting Date | Meeting States | Meeting Information |
|---|
| Meeting Date | Meeting States | Meeting Information |
|---|
| Requestor Name | Requestor Letter |
|---|---|
Coding Information
Bill type codes.
| Code | Description |
|---|
Revenue Codes
CPT/HCPCS Codes
Icd-10-cm codes that support medical necessity, icd-10-cm codes that do not support medical necessity, additional icd-10 information, general information.
Refer to Local Coverage Article: Billing and Coding: Intraarticular Knee Injections of Hyaluronan, A56157, for all coding information.
Documentation Requirements
- All documentation must be maintained in the patient's medical record and made available to the contractor upon request.
- Every page of the record must be legible and include appropriate patient identification information (e.g., complete name, dates of service[s]). The documentation must include the legible signature of the physician or non-physician practitioner responsible for and providing the care to the patient.
- The medical record documentation must support the medical necessity of the services as stated in this policy.
- The medical records must document that the patient has symptomatic osteoarthritis of the knee, the nature of the symptoms and the functional limitations using a standardized assessment tool.
- Radiographic confirmation of osteoarthritis of the knee in the form of an x-ray report and/or notation in the record must accompany the clinical description.
- The medical record must include documentation that supports that conservative therapy was attempted prior to viscosupplementation therapy. If conservative therapy and/or corticosteroid injections were contraindicated or failed, the reason(s) must be supported in the documentation submitted for review.
- The medical record must indicate whether one or both knees are being treated and in the former instance, which knee is being treated.
- If fluoroscopy or ultrasound is used for needle guidance with the intra-articular injection, documentation must support that the presentation of the patient’s affected knee on the day of the procedure makes needle insertion problematic.
- If intra-articular injections of other therapeutic agents, such as corticosteroids, are performed in the same knee during the course of viscosupplementation therapy, the reason(s) requiring the use of the additional therapeutic agent must be documented.
- The frequency of injections and the dosage given must be clearly indicated.
- The response to treatment must be noted. Medical records should describe the assessment tool utilized. Repeat courses of viscosupplementation in the absence of documentation of response to the previous course of treatment will be considered not reasonable and necessary and not subject to coverage.
Utilization Guidelines
In accordance with CMS Ruling 95-1 (V), utilization of these services should be consistent with locally acceptable standards of practice.
Depending on the hyaluronan preparation used, a series may consist of a single intra-articular injection or 2 to 5 weekly intra-articular injections per knee.
The maximum allowable frequency of injection(s) for the initial or repeat series is as follows:
| Synvisc-One, Gel-One, Monovisc, Durolane | Single injection per knee |
| Hymovis | 2 weekly injections per knee |
| Euflexxa, Gelsyn-3, Synvisc, Visco-3, TriVisc, Synojoynt, triluron | 3 weekly injections per knee |
| Orthovisc | 3-4 weekly injections per knee |
| Hyalgan, Supartz, Genvisc 850 | 3-5 weekly injections per knee |
*Note: The duration of treatment per series is from the FDA medication package insert full prescribing information.
For additional information on drug dosing and the proper number of units to report per dose, please refer to the Local Coverage Article: Billing and Coding: Intraarticular Knee Injections of Hyaluronan, A56157.
Other Contractors Policies
Novitas Solutions, Inc. LCD L35427 Hyaluronan Acid Therapies for Osteoarthritis of the Knee.
UnitedHealthCare Medical Policy Number: CS110.N. Sodium Hyaluronate. Effective Date June 1, 2018.
- American Academy of Orthopaedic Surgeons. Viscosupplementation Treatment for Knee Arthritis. OrthoInfo . Last Reviewed February 2021. https://orthoinfo.aaos.org/en/treatment/viscosupplementation-treatment-for-knee-arthritis/. Accessed January 18, 2023.
- U.S. Food and Drug Administration (FDA) approval letters and manufacturer’s inserts. [email protected]://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfcfr/CFRSearch.cfm?CFRPart=170&showFR=1&subpartNode=21:3.0.1.1.1.5 . Accessed January 5, 2023.
- Vad VB. Hyaluronic Acid Injections for Knee Osteoarthritis. Arthritis-Health . Updated 03/28/2019. https://www.arthritis-health.com/treatment/injections/viscosupplementation-knee-osteoarthritis. Accessed March 7, 2023.
- Newberry SJ, Fitzgerald JD, Maglione MA, et al. Systematic Review for Effectiveness of Hyaluronic Acid in the Treatment of Severe Degenerative Joint Disease (DJD) of the Knee . Rockville (MD): Agency for Healthcare Research and Quality (US); July 23, 2015.
- VA/DoD Clinical Practice Guideline for Non-Surgical Management of Hip and Knee Osteoarthritis Guideline Summary. Prepared by The Osteoarthritis Working Group. V1.0; 2014. https://www.healthquality.va.gov/. Accessed January 20, 2023.
- National Institute for Health and Care Excellence (NICE) Clinical Guideline Osteoarthritis: care and management. Updated October 19, 2022. Nice.org.uk/guidance/cg177. Accessed January 17, 2023.
- American Academy of Orthopaedic Surgeons, Treatment of Osteoarthritis of the Knee Evidence-Based Guideline, 2nd Edition, Adopted by the American Academy of Orthopaedic Surgeons Board of Directors May 18, 2013.
- Hochberg MC, Altman RD, April KT, et al. American College of Rheumatology 2012 recommendations for the use of nonpharmacologic and pharmacologic therapies in osteoarthritis of the hand, hip, and knee. Arthritis Care Res . 2012 Apr;64(4):465-74.
- Filardo G, Di Matteo B, Tentoni F, et al. No Effects of Early Viscosupplementation After Arthroscopic Partial Meniscectomy: A Randomized Controlled Trial. Am J Sports Med . 2016 Dec;44(12):3119-3125.
- Di Martino A, Tentoni F, Di Matteo B, et al. Early Viscosupplementation After Anterior Cruciate Ligament Reconstruction: A Randomized Controlled Trial. Am J Sports Med . 2016 Oct;44(10):2572-2578.
- Berkoff DJ, Miller LE, Block JE. Clinical utility of ultrasound guidance for intra-articular knee injections: a review. Clin Interv Aging . 2012;7:89-95. doi: 10.2147/CIA.S29265.
- Altman RD, Schemitsch E, Bedi A. Assessment of clinical practice guideline methodology for the treatment of knee osteoarthritis with intra-articular hyaluronic acid. Semin Arthritis Rheum . 2015 Oct;45(2):132-9. doi: 10.1016/j.semarthrit.2015.04.013.
- Aetna Policy Number: 0179. Viscosupplementation. Last Reviewed 04/13/2018.
- Altman R, Hackel J, Niazi F, Shaw P, Nicholls M. Efficacy and safety of repeated courses of hyaluronic acid injections for knee osteoarthritis: A systematic review. Semin Arthritis Rheum . 2018 Oct;48(2):168-175. doi: 10.1016/j.semarthrit.2018.01.009.
- American Medical Association (AMA) CPT Assistant. Coding Clarification: Hip Arthrography. June 2012, Volume 22, Issue 6, page 14.
- Bert JM and Waddell DD. Viscosupplementation with Hylan G-F 20 in Patients with Osteoarthrosis of the Knee. Ther Adv Musculoskelet Dis . 2010 Jun; 2(3): 127–132. doi: 10.1177/1759720X10370930.
- Florida Blue Medical Coverage Guideline 09-J10000-22 Viscosupplementation, Hyaluronan Injections (e.g. Synvisc®). Revised 04/01/2021.
- Maricar N, Parkes MJ, Callaghan MJ, Felson DT, O'Neill TW. Where and how to inject the knee a systematic review. Semin Arthritis Rheum . 2013 Oct;43(2):195-203. doi: 10.1016/j.semarthrit.2013.04.010.
- Telikicherla M, Kamath SU. Accuracy of Needle Placement into the Intra-Articular Space of the Knee in Osteoarthritis Patients for Viscosupplementation. J Clin Diagn Res . 2016 Feb;10(2):RC15-7. doi: 10.7860/JCDR/2016/17127.7275.
- U.S. Food and Drug Administration (FDA) approval letters and manufacturer’s inserts. Devices@FDA. https://www.accessdata.fda.gov/cdrh_docs/pdf17/P170016D.pdf. Accessed January 17, 2023.
- U.S. Food and Drug Administration (FDA) approval letters and manufacturer’s inserts. Devices@FDA. https://www.accessdata.fda.gov/cdrh_docs/pdf18/P180040C.pdf. Accessed January 18, 2023.
Revision History Information
| Revision History Date | Revision History Number | Revision History Explanation | Reasons for Change |
|---|
Associated Documents
| Updated On | Effective Dates | Status | |
|---|---|---|---|
| 04/21/2023 | 06/11/2023 - N/A | Currently in Effect | You are here |
Read the LCD Disclaimer
Email this document to yourself or someone else
An asterisk ( * ) indicates a required field. This email will be sent from you to the recipient email address(es) you enter. Please do not use this feature to contact CMS. To submit a comment or question to CMS, please use the Feedback/Ask a Question link available at the bottom of every MCD page.
Contractor Detail
Lcd disclaimer, license agreements.
License Agreements American Medical Association Current Procedural Terminology American Dental Association Current Dental Terminology American Hospital Association NUBC UB-04
Please review the licensing information below and indicate your agreement and acceptance.
License for Use of Current Procedural Terminology (CPT)
End User Point and Click Agreement: CPT codes, descriptions and other data only are copyright 2023 American Medical Association. All Rights Reserved (or such other date of publication of CPT). CPT is a trademark of the American Medical Association (AMA).
You, your employees, and agents are authorized to use CPT only as agreed upon with the AMA internally within your organization within the United States for the sole use by yourself, employees, and agents. Use is limited to use in Medicare, Medicaid or other programs administered by the Centers for Medicare and Medicaid Services (CMS). You agree to take all necessary steps to insure that your employees and agents abide by the terms of this agreement.
Any use not authorized herein is prohibited, including by way of illustration and not by way of limitation, making copies of CPT for resale and/or license, transferring copies of CPT to any party not bound by this agreement, creating any modified or derivative work of CPT, or making any commercial use of CPT. License to use CPT for any use not authorized herein must be obtained through the AMA, CPT Intellectual Property Services, AMA Plaza, 330 Wabash Ave., Suite 39300, Chicago, IL 60611-5885. Applications are available at the AMA Web site, http://www.ama-assn.org/go/cpt http://www.ama-assn.org/go/cpt .
Applicable FARS\DFARS Restrictions Apply to Government Use.
This product includes CPT which is commercial technical data and/or computer data bases and/or commercial computer software and/or commercial computer software documentation, as applicable which were developed exclusively at private expense by the American Medical Association, AMA Plaza, 330 N. Wabash Ave., Suite 39300, Chicago, IL 60611-5885. U.S. Government rights to use, modify, reproduce, release, perform, display, or disclose these technical data and/or computer data bases and/or computer software and/or computer software documentation are subject to the limited rights restrictions of FAR 52.227-14 (December 2007) and/or subject to the restricted rights provisions of FAR 52.227-14 (December 2007) and FAR 52.227-19 (December 2007), as applicable, and any applicable agency FAR Supplements, for non-Department of Defense Federal procurements.
The scope of this license is determined by the AMA, the copyright holder. Any questions pertaining to the license or use of the CPT should be addressed to the AMA. End Users do not act for or on behalf of the CMS. CMS disclaims responsibility for any liability attributable to end user use of the CPT. CMS will not be liable for any claims attributable to any errors, omissions, or other inaccuracies in the information or material contained on this page. In no event shall CMS be liable for direct, indirect, special, incidental, or consequential damages arising out of the use of such information or material.
License For Use of Current Dental Terminology (CDT TM )
License for use of current dental terminology (cdt™).
These materials contain Current Dental Terminology (CDT TM ), copyright© 2023 American Dental Association (ADA). All rights reserved. CDT is a trademark of the ADA.
The license granted herein is expressly conditioned upon your acceptance of all terms and conditions contained in this agreement. By clicking below on the button labeled "I accept", you hereby acknowledge that you have read, understood, and agreed to all terms and conditions set forth in this agreement.
If you do not agree with all terms and conditions set forth herein, click below on the button labeled "I do not accept" and exit from this computer screen.
If you are acting on behalf of an organization, you represent that you are authorized to act on behalf of such organization and that your acceptance of the terms of this agreement creates a legally enforceable obligation of the organization. As used herein, "you" and "your" refer to you and any organization on behalf of which you are acting.
Subject to the terms and conditions contained in this Agreement, you, your employees and agents are authorized to use CDT only as contained in the following authorized materials and solely for internal use by yourself, employees and agents within your organization within the United States and its territories. Use of CDT is limited to use in programs administered by Centers for Medicare & Medicaid Services (CMS). You agree to take all necessary steps to ensure that your employees and agents abide by the terms of this agreement. You acknowledge that the ADA holds all copyright, trademark and other rights in CDT. You shall not remove, alter, or obscure any ADA copyright notices or other proprietary rights notices included in the materials.
Any use not authorized herein is prohibited, including by way of illustration and not by way of limitation, making copies of CDT for resale and/or license, transferring copies of CDT to any party not bound by this agreement, creating any modified or derivative work of CDT, or making any commercial use of CDT. License to use CDT for any use not authorized herein must be obtained through the American Dental Association, 211 East Chicago Avenue, Chicago, IL 60611. Applications are available at the American Dental Association web site, http://www.ADA.org/ http://www.ADA.org/ .
Applicable Federal Acquisition Regulation Clauses (FARS)/Department of Defense Federal Acquisition Regulation supplement (DFARS) Restrictions Apply to Government Use.
Organizations who contract with CMS acknowledge that they may have a commercial CDT license with the ADA, and that use of CDT codes as permitted herein for the administration of CMS programs does not extend to any other programs or services the organization may administer and royalties dues for the use of the CDT codes are governed by their commercial license.
ADA DISCLAIMER OF WARRANTIES AND LIABILITIES CDT is provided "as is" without warranty of any kind, either expressed or implied, including but not limited to, the implied warranties of merchantability and fitness for a particular purpose. No fee schedules, basic unit, relative values, or related listings are included in CDT. The ADA does not directly or indirectly practice medicine or dispense dental services. The sole responsibility for software, including any CDT and other content contained therein, is with (insert name of applicable entity) or the CMS; and no endorsement by the ADA is intended or implied. The ADA expressly disclaims responsibility for any consequences or liability attributable to or related to any use, non-use, or interpretation of information contained or not contained in this file/product. This Agreement will terminate upon notice to you if you violate the terms of this Agreement. The ADA is a third-party beneficiary to this Agreement.
CMS DISCLAIMER The scope of this license is determined by the ADA, the copyright holder. Any questions pertaining to the license or use of the CDT should be addressed to the ADA. End Users do not act for or on behalf of the CMS. CMS disclaims responsibility for any liability attributable to end user use of the CDT. CMS will not be liable for any claims attributable to any errors, omissions, or other inaccuracies in the information or material covered by this license. In no event shall CMS be liable for direct, indirect, special, incidental, or consequential damages arising out of the use of such information or material.
The license granted herein is expressly conditioned upon your acceptance of all terms and conditions contained in this agreement. If the foregoing terms and conditions are acceptable to you, please indicate your agreement by clicking below on the button labeled "I Accept". If you do not agree to the terms and conditions, you may not access or use software. Instead, you must click below on the button labeled "I Do Not Accept" and exit from this computer screen.
License For Use of National Uniform Billing Committee (NUBC) UB-04
These materials contain NUBC Official UB-04 Specifications (UB-04 Data), which is copyrighted by the American Hospital Association (AHA).
THE LICENSE GRANTED HEREIN IS EXPRESSLY CONDITIONED UPON YOUR ACCEPTANCE OF ALL TERMS AND CONDITIONS CONTAINED IN THIS AGREEMENT. BY CLICKING BELOW ON THE BUTTON LABELED "I ACCEPT", YOU HEREBY ACKNOWLEDGE THAT YOU HAVE READ, UNDERSTOOD AND AGREED TO ALL TERMS AND CONDITIONS SET FORTH IN THIS AGREEMENT.
IF YOU DO NOT AGREE WITH ALL TERMS AND CONDITIONS SET FORTH HEREIN, CLICK BELOW ON THE BUTTON LABELED "I DO NOT ACCEPT" AND EXIT FROM THIS COMPUTER SCREEN. IF YOU ARE ACTING ON BEHALF OF AN ORGANIZATION, YOU REPRESENT THAT YOU ARE AUTHORIZED TO ACT ON BEHALF OF SUCH ORGANIZATION AND THAT YOUR ACCEPTANCE OF THE TERMS OF THIS AGREEMENT CREATES A LEGALLY ENFORCEABLE OBLIGATION OF THE ORGANIZATION. AS USED HEREIN, "YOU" AND "YOUR" REFER TO YOU AND ANY ORGANIZATION ON BEHALF OF WHICH YOU ARE ACTING.
- Subject to the terms and conditions contained in this Agreement, you, your employees, and agents are authorized to use UB-04 Data only as contained in the following authorized materials and solely for internal use by yourself, employees and agents within your organization within the United States and its territories. Use of UB-04 Data is limited to use in programs administered by Centers for Medicare & Medicaid Services (CMS). You agree to take all necessary steps to ensure that your employees and agents abide by the terms of this Agreement. You acknowledge that the AHA holds all copyright, trademark, and other rights in UB-04 Data. You shall not remove, alter, or obscure any AHA copyright notices or other proprietary rights notices included in the materials.
- Any use not authorized herein is prohibited, including, by way of illustration and not by way of limitation, making copies of UB-04 Data for resale and/or license, transferring copies of UB-04 Data to any party not bound by this agreement, creating any modified or derivative work of UB-04 Data, or making any commercial use of UB-04 Data. License to use UB-04 Data for any use not authorized herein must be obtained through the American Hospital Association, 155 N. Wacker Drive, Suite 400, Chicago, Illinois, 60606. Applications are available at the NUBC website, http://www.nubc.org/ http://www.nubc.org/ .
- The UB-04 Data included in this product is commercial technical data and/or computer databases and/or commercial computer software and/or commercial computer software documentation, as applicable, which was developed exclusively at private expense by the American Hospital Association, 155 N. Wacker Drive, Suite 400, Chicago, Illinois 60606. U.S. Government rights to use, modify, reproduce, release, perform, display, or disclose these technical data and/or computer data bases and/or computer software and/or computer software documentation are subject to the limited rights restrictions of DFARS 252.227-7015(b)(2) (November 1995) and/or subject to the restrictions of DFARS 227.7202-1(a) (June 1995) and DFARS 227.7202-3(a) (June 1995), as applicable for U.S. Department of Defense procurements and the limited rights restrictions of FAR 52.227-14 (December 2007) and FAR 52.227-19 (December 2007), as applicable, and any applicable agency FAR Supplements, for non-Department of Defense Federal procurements.
- AHA DISCLAIMER OF WARRANTIES AND LIABILITIES. UB-04 Data is provided "as is" without warranty of any kind, either expressed or implied, including but not limited to, the implied warranties of merchantability and fitness for a particular purpose. The sole responsibility for the software, including any UB-04 Data and other content contained therein, is with the Medicare/Medicaid Contractor or the CMS; and no endorsement by the AHA is intended or implied. The AHA expressly disclaims responsibility for any consequences or liability attributable to or related to any use, non-use, or interpretation of information contained or not contained in this file/product. This Agreement will terminate upon notice to you if you violate the terms of this Agreement. The AHA is a third-party beneficiary to this Agreement.
- CMS DISCLAIMER. The scope of this license is determined by the AHA, the copyright holder. Any questions pertaining to the license or use of the UB-04 Data should be addressed to the AHA. End users do not act for or on behalf of the CMS. CMS DISCLAIMS RESPONSIBILITY FOR ANY LIABILITY ATTRIBUTABLE TO END USER USE OF THE UB-04 DATA. CMS WILL NOT BE LIABLE FOR ANY CLAIMS ATTRIBUTABLE TO ANY ERRORS, OMISSIONS, OR OTHER INACCURACIES IN THE INFORMATION OR MATERIAL COVERED BY THIS LICENSE. In no event shall CMS be liable for direct, indirect, special, incidental, or consequential damages arising out of the use of such information or material.
Page Help for LCD - Intraarticular Knee Injections of Hyaluronan (L39529)
Introduction.
This page displays your requested Local Coverage Determination (LCD). The document is broken into multiple sections. You can use the Contents side panel to help navigate the various sections. A Local Coverage Determination (LCD) is a decision made by a Medicare Administrative Contractor (MAC) on whether a particular service or item is reasonable and necessary, and therefore covered by Medicare within the specific jurisdiction that the MAC oversees. Please note that codes (CPT/HCPCS and ICD-10) have moved from LCDs to Billing & Coding Articles.
More information
MACs are Medicare contractors that develop LCDs and process Medicare claims. MACs develop an LCD when there is no national coverage determination (NCD) or when there is a need to further define an NCD for the specific jurisdiction. LCDs outline how the contractor will review claims to ensure that the services provided meet Medicare coverage requirements. Before an LCD becomes final, the MAC publishes Proposed LCDs, which include a public comment period. LCD document IDs begin with the letter "L" (e.g., L12345). Proposed LCD document IDs begin with the letters "DL" (e.g., DL12345). The guidelines for LCD development are provided in Chapter 13 of the Medicare Program Integrity Manual. The Social Security Act, Sections 1869(f)(2)(B) and 1862(l)(5)(D) define LCDs and provide information on the process
The LCD Tracking Sheet is a pop-up modal that is displayed on top of any Proposed LCD that began to appear on the MCD on or after 1/1/2022. The Tracking Sheet provides key details about the Proposed LCD, including a summary of the issue, who requested the new/updated policy, links to key documents, important process-related dates, who to contact with questions about the policy, and the history of previous policy considerations. The information displayed in the Tracking Sheet is pulled from the accompanying Proposed LCD and its correlating Final LCD and will be updated as new data becomes available. The Tracking Sheet modal can be closed and re-opened when viewing a Proposed LCD.
Printing a Document to PDF
Frequently Asked Questions (FAQs)
Are you a provider and have a question about billing or coding.
Please contact your Medicare Administrative Contractor (MAC). MACs can be found in the MAC Contacts Report .
Do you have questions related to the content of a specific Local Coverage Determination (LCD) or an Article?
Are you a beneficiary and have questions about your coverage, are you looking for codes (e.g., cpt/hcpcs, icd-10), local coverage.
For the most part, codes are no longer included in the LCD (policy). You will find them in the Billing & Coding Articles. Try using the MCD Search to find what you're looking for. Enter the code you're looking for in the "Enter keyword, code, or document ID" box. The list of results will include documents which contain the code you entered.
Please Note: For Durable Medical Equipment (DME) MACs only, CPT/HCPCS codes remain located in LCDs. All other Codes (ICD-10, Bill Type, and Revenue) have moved to Articles for DME MACs, as they have for the other Local Coverage MAC types.
National Coverage
NCDs do not contain claims processing information like diagnosis or procedure codes nor do they give instructions to the provider on how to bill Medicare for the service or item. For this supplementary claims processing information we rely on other CMS publications, namely Change Requests (CR) Transmittals and inclusions in the Medicare Fee-For-Service Claims Processing Manual (CPM).
In order for CMS to change billing and claims processing systems to accommodate the coverage conditions within the NCD, we instruct contractors and system maintainers to modify the claims processing systems at the national or local level through CR Transmittals. CRs are not policy, rather CRs are used to relay instructions regarding the edits of the various claims processing systems in very descriptive, technical language usually employing the codes or code combinations likely to be encountered with claims subject to the policy in question. As clinical or administrative codes change or system or policy requirements dictate, CR instructions are updated to ensure the systems are applying the most appropriate claims processing instructions applicable to the policy.
How do I find out if a specific CPT code is covered in my state?
Enter the CPT/HCPCS code in the MCD Search and select your state from the drop down. (You may have to accept the AMA License Agreement.) Look for a Billing and Coding Article in the results and open it. (Or, for DME MACs only, look for an LCD.) Review the article, in particular the Coding Information section.
If you need more information on coverage, contact the Medicare Administrative Contractor (MAC) who published the document. The contractor information can be found at the top of the document in the Contractor Information section (expand the section to see the details).
If you don’t find the Article you are looking for, contact your MAC .
Did you receive a Medicare coverage denial?
Was your Medicare claim denied? Here are some hints to help you find more information:
1) Check out the Beneficiary card on the MCD Search page.
2) Try using the MCD Search and enter your information in the "Enter keyword, code, or document ID" box. Your information could include a keyword or topic you're interested in; a Local Coverage Determination (LCD) policy or Article ID; or a CPT/HCPCS procedure/billing code or an ICD-10-CM diagnosis code. Try entering any of this type of information provided in your denial letter.
3) Contact your MAC .
4) Visit Medicare.gov or call 1-800-Medicare.
It is Thursday and the weekly MCD data isn’t refreshed?
Are you having technical issues with the medicare coverage database (mcd), mcd session expiration warning.
Your MCD session is currently set to expire in 5 minutes due to inactivity. If your session expires, you will lose all items in your basket and any active searches. If you would like to extend your session, you may select the Continue Button.
Reset MCD Search Data
If you are experiencing any technical issues related to the search, selecting the 'OK' button to reset the search data should resolve your issues.
- Share full article
Advertisement
Supported by
The Ezra Klein Show
Nate Silver on How Kamala Harris Changed the Odds

By Ezra Klein
Nate Silver came to fame in American politics for election forecasting. But before Silver was in politics, he was a poker player. And after getting into politics, he went back to being a poker player. He’s been running through poker championships and out there on tables — partly because he’s been writing a book about risk.
The book is called “ On the Edge: The Art of Risking Everything .” And it applies the frameworks of the gambler to politics, to A.I., to venture capital.
The way Silver thinks about politics I find very useful. So I invited him on my podcast to talk about how that thinking has guided him over the past year and how he’s thinking about the election going forward.
This is an edited transcript of part of our conversation. For the full conversation, watch the video below, or listen to “ The Ezra Klein Show .”
The election forecaster discusses 2024 and what politicians can learn from gamblers.
“Nate Silver came to fame in American politics for election forecasting. He built models that were pretty damn successful at predicting American politics.” “Nate Silver is the founder of fivethirtyeight.com, a polling website that correctly predicted the winner of 49 of the 50 states in the last presidential election.” “Election Oracle, ESPN’s Nate Silver, he predicted every state in the last presidential election.” “And once again, Nate Silver completely nailed it.” “The guy’s amazing.” “But before Silver was in politics, he was a poker player. And after getting into politics, he went back to being a poker player. He’s been running through poker championships and out there on tables —” “Savage, savage bluff by Silver. Oh, my God.” “— partially because he’s been writing a book about risks. The book is called ‘On the Edge: The Art of Risking Everything.’ And it applies the frameworks of, I would say, the gambler, maybe say the poker player, to politics, to AI, to venture capital. Nate, the way he thinks about politics I find very useful. I find that he thinks more clearly about risk and probabilities than a lot of people do and maybe more people should follow. So I wanted to have him on to talk about how that thinking has guided him over the past year and how he’s thinking about it in the election going forward. As always, my email, [email protected].” [THEME MUSIC] “Nate Silver, welcome to the show.” “Thank you, Ezra. Happy to be here.” “Last I looked, your model has Harris winning the election at around 52 percent. It might be mildly different today. But this has been an unusual election. So how much stock do you put in your model right now?” “I think the model is balancing the different factors pretty well. I mean, there are some things you could argue are favorable to Harris, one of which is that for the past few weeks we’ve been in what the model thinks is supposed to be the convention bounce period for republicans, where typically you poll pretty well after your convention. There’s the afterglow of the new nomination and things like that — the afterglow of the VP pick, often, too. And Kamala Harris kind of stomped on Donald Trump’s news cycle. So maybe it’s an overly favorable assumption for Harris. There’s also in polls what’s known as nonpartisan response bias. So when voters get more enthusiastic, you’d rather have that than not as a candidate. But it also means that they sometimes are more likely to respond to polls. At the same time, her momentum has been pretty good, which usually I dismiss. We don’t really kind of know what the baseline is here, right? You know, Hillary Clinton, who was, I think, kind of a terrible candidate, won the popular vote by two points. Is she a little bit better than Hillary Clinton? Probably, right? So can she win by three or four? Well, if you win by three or four, then you win the electoral college in most instances.” “I don’t think many people expected — if you did, I’d like to know it — the turnaround in her numbers we have seen since she’s become the presumptive nominee. She’s gone to net favorables, which I would not have bet a ton of money on at this speed at least. People were looking at a lot of data on Harris and assuming that data was solid. That data was not solid.” “When a candidate’s a hypothetical candidate, you have to treat that polling very carefully. People are — I think it’s a weird thing to ask, you know, what if Gavin Newsom ran against Trump. It’s not the same thing as when you actually have the candidate in front of you, and have the advertisements, and have the news articles, and everything else to actually evaluate. I mean, I think this is, like, on the higher side for a jump in favorables, but, you know, she was amazingly well-organized at getting the entire establishment behind her within literally minutes [LAUGHS]: of Biden announcing that he was going to step down. And so that suggested that maybe she did have more support in the party than she let on. And also, you know, I don’t — I think the Biden people may have been in somewhat bad faith. Maybe not consciously, but I’m not sure they weren’t trying to undermine her. Because the obvious thing to do would be to have this qualified, if not always that politically adept, you know, much, much younger vice president take over for you when you’re about to be 82. But they gave her the border. They gave her voting rights, which is kind of the one major domestic policy area where they got very little done. So I don’t think they gave her a very good hand to play. But meanwhile, she’s getting a lot of reps, and giving speeches, and building connections, and played the game really well. I have a lot of respect for that.” “Well, the key thing, I think, is that Biden had a huge amount of influence over how the party viewed her in both directions. There was a long period, I would say, when the quiet signals out of Biden world were this isn’t going well.” “Yeah.” “And when there was pressure to push Biden off the ticket, those signals got louder — Harris cannot do this. If you get rid of him, you’re going to get her. You’re going to lose. But then the thing you saw happen is a moment Biden actually stepped aside and fully endorsed her. That was a signal so powerful that it functionally won the potential primary for Harris instantly. Nobody was going to go against Joe Biden in that moment. And so, in both directions, Biden had, and the team around him, a lot of influence. When implicitly Biden world told the Democratic Party Harris can’t do it, the Democratic Party believed them. And then when explicitly Biden himself told the Democratic Party and the world Harris could do it, the Democratic Party believed him. And by the way, from what I could tell, it seems he was right. And I don’t blame Biden, I think, for things that happened earlier in the administration. That was a lot of staff talk. And to be fair, it was based on some things. There were problems in her office. There were reasons to be skeptical. But he and they had tremendous power. In a way, this was not, to me, like a mini primary. This was a parliamentary process, right? The party came together and chose a leader through endorsements from elected officials. That’s functionally what happened.” “Yeah, it felt very British. It felt like —” “It felt very British.” “— the Liz Truss kind of thing or something, right, where, yeah. There’s a loss of confidence. Those are fascinating dynamics to study. But yeah, it’s interesting to have the inside view versus the outside view a little bit. And, you know, again, we talk about this in the book a little bit, but I come at a position where I’m more skeptical about the competence of people who work in politics. Right? Even if I like the candidates they endorse — I mean, I plan to plan to vote for Kamala Harris. I would not have voted for Joe Biden, by the way. I think it was deeply irresponsible to nominate him, and I would have voted libertarian or something. But I have a more skeptical view, and I think even the rationales they state out loud are sometimes maybe the rationales they believe or not. But, you know, I think human behavior is pretty strategic when you understand people’s incentives, and kind of information set, and things like that. And I think it was in Biden’s narrow self-interest to make Harris look weaker. And I think that plays a role at all sorts of subconscious margins in terms of how she was treated.” “Well, let’s talk about that skepticism. You and I have known each other a long time. We’re old-school bloggers. And my read of you is that somewhat over the 2016 election, then specifically over the pandemic —” “Yeah.” “— and your experience, I think, with online liberalism in the pandemic, you became much more disillusioned with the people who once felt to you like your group, your coalition, your tribe. There’s been a kind of an alienation for you. Is that a fair read?” “Yeah, I’d say it’s three things, right. Number one, the 2016 aftermath, I thought a lot of the kind of liberal and centrist news media, kind of were in denial about their own role in the ‘But her emails’ stuff and then picked scapegoats for Trump’s victory that were not the real reasons that he won. You know, Russian bot farms have approximately nothing to do with why Donald Trump won the 2016 election. And the Russia stuff, in general, I think was treated with an order of magnitude more importance than it probably objectively had. And blaming Facebook and the tech industry for that, I thought that was irresponsible. And also kind of the obsession over the polls in 2016, where I think there was some revisionist history where the polls actually showed a pretty close race. I mean, we had Trump with a 30 percent chance. And it was kind of the conventional wisdom that assumed that he was dead in the water. So the ability to conveniently lie a little bit or manipulate facts and spin facts, I mean, that was part one. Part two was the pandemic. Absolutely. And, you know, ‘orange man bad,’ I think, was often the reason that people believed a lot of what they believed. Because in some ways, the move to shut down society in some ways kind of went against the values of traditional liberalism, right? There’s a transfer of welfare from younger people [LAUGHS]: and people who are not able to work from home to wealthy suburbanites and older people who you’re protecting their health, but you’re undermining the education of millions and millions and millions of schoolkids around the country, and essential workers are still putting themselves at risk that you deem unacceptable for people who are able to work with laptops to take. So I thought it was very self-serving, and I thought kind of expertise was co-opted and corrupted by political partisans. And then third was the Biden stuff.” “Well, it seemed to me it happened for you before the Biden stuff.” “Yeah. I mean —” “And you were crosswise with a lot of liberals on Twitter. I mean, I came back to Twitter for three weeks during the height of Bidenmania to try to be sort of in touch with that sentiment and mostly stay away from it. But Twitter is a place that groups that exist outside the online hothouse purify inside the online hothouse. So there’s the public health community outside Twitter, and then there’s how it acts inside Twitter — political scientists outside Twitter and then inside Twitter, republicans outside Twitter, then inside Twitter. And my sense was that you ended up in a lot of fights with liberals who had a much lower risk tolerance than you did. And between that and what was, I believe, unfair criticism of the 2016 model, which got the election much more right than most did, that it sort of — you began to see habits of — you call it ‘the village.’ The village is your term for —” “Yeah. And that’s been a term that’s been used by other right. But the village is basically media, politics, government, progressive —” “The establishment.” “The establishment, ‘The New York Times,’ Harvard University.” “The regime.” “The regime. Yeah. The Democratic White House. Maybe not a Republican White House, but that’s a more complicated kind of edge case.” “Or maybe a different Republican White House.” “Yeah.” “Right? George W. Bush was part of the village.” “Absolutely.” “Maybe Donald Trump wasn’t.” “Absolutely.” “I think you’ve also called it the indigo blob in different ways, that you began to see it as a kind of set of aligned cognitive tendencies that you disagreed with. What were they?” “So one of them is the failure to do what I call decoupling. It’s not my term. Decoupling is the act of separating an issue from the context. So the example I give in the book is that if you’re able to say I abhor the Chick-fil-A’s CEO’s position on gay marriage — I don’t know if it’s changed or not, but he was anti-gay marriage, at least for some period of time — but they make a really delicious chicken sandwich. Like, that’s decoupling.” “I abhor their treatment of chickens.” “Yeah.” “I have a strong direct take on Chick-fil-A. I don’t like how they treat chickens.” “O.K. Or you can say or separate out, you know, Michael Jackson, Woody Allen, separate the art from the artist kind of thing. Right? You know, that tendency goes against kind of the tendency on the progressive left to care a lot about the identity of the speaker in terms of the racial or gender identity and in terms of their credentials. And this other world that I call ‘the river,’ the kind of gambling, risk-taking world, all that matters is that you’re right.” “The river is your name for the community of people who think about risk roughly the way you do and are willing to make big bets, willing to accept loss. The river is your — it’s your world of gamblers at all levels of society.” “Capital and lowercase g gambling.” “So hedge funds —” “Expected value.” “— venture capitalists.” “Yeah. And then you get kind of the more —” “Crypto.” “— groundwater stuff where it’s like crypto, and meme stocks, and things like that. It doesn’t matter who you are, it matters that you’re right and you’re able to prove it or bet on it in some way. And that’s very against, I think, the kind of credentialism that you have within the progressive Democratic left, which I also call the indigo blob, because it’s a fusion of purple and blue. There’s not a clear separation between the nonpartisan, centrist media and the left-leaning progressive media that’s kind of rooting for Democrats. Different parts of ‘The New York Times’ have both those functions in place. And as someone who’s kind of more on the nonpartisan side, even though, again, I would prefer to see Kamala Harris than Donald Trump, I think people are exploiting the trust that institutions have earned for political gain. And particularly in the kind of pre-Elon pandemic-era Twitter days, the pile-ons were kind of insane, and 98 percent of people don’t have the tolerance for that. But I didn’t really care because these people are not my friends, and I have a good life outside of Twitter, and because, you know, to some extent, even if you run a newsletter, being a little polarizing is O.K., right? If I have 10 random people yelling at me on Twitter and 10 people sign up to be paid subscribers to ‘Silver Bulletin,’ then I come out like way ahead in that deal. And so I think I couldn’t do my job without running afoul of this group of people.” “Let me ask you about the definition of decoupling there, because I think decoupling is interesting. And I found the examples you pick also interesting but contestable.” “Yeah.” “So in the Chick-fil-A example, I’m between a vegetarian and vegan these days, so I got my own issues with Chick-fil-a, but was not a believer necessarily in boycotting it if you didn’t have my issues. But I understood it as more like a boycott, that theory, right? You don’t want to give money to something that’s going to work against your interests. The question of decoupling art and artist, which I’m more on the side of decoupling, but also has a dimension of — those both strike me as versions of activism, right? What you want to do, what people who hold those positions are trying to do, is affect change in the world by applying consequences to beliefs. And maybe you don’t want that, or you don’t agree that the beliefs they are trying to affect should have those consequences on them. But it’s kind of different than the idea of things are being pressed together that don’t go together. I think an interesting sort of decoupling issue that happened in the pandemic was the same public health voices who were at one point saying you had to be so careful, even outside oftentimes were then pro joining the George Floyd protests, which a lot of people found very upsetting. What people were looking to the public health world for right then was not their views on protests but their views on distancing. And that felt like it coupled things in a way that undermined one to achieve another.” “Well, and they framed it in, like, oh, this is good for public health reasons, right? If they had said, look, I’m a big believer in racial equity; there is a little bit of risk here; but outside, wear a mask, and probably not a huge problem — I mean, that would be honest, right?” “Which ended up being true too.” “Yeah. But instead it was in the name of public health, right? I think people don’t do enough thinking about thinking and don’t read enough of the literature on cognitive biases. Ironically, this is kind of like the expert literature on how powerful the human mind is at confirmation bias, and how powerful a drug political partisanship is, and how smart people are maybe better rationalizes in certain respects. I mean, a lot of irrational traits are like rational on some halfway approximate different version of the universe. You know what I mean?” “My first book was on polarization. And what I understand you as doing in the book in part is making an interesting cut in society between people with different forms of both risk tolerance and thinking about risk. And you write something that caught my eye where you say, quote, ‘COVID made those risk preferences public, worn on our proverbial sleeves and our literal faces.’ And you go on to say, quote, ‘People are becoming more bifurcated in their risk tolerance, and this affects everything from who we hang out with to how we vote.’” “Yeah.” “Tell me about both sides of that — the way that it made risk tolerance visible, but then your view that since then risk tolerance is becoming a deeper cleavage in society.” “I mean, on the one hand, there are lots of signs that risk tolerance is going down, right? Among young people in particular, they’re smoking less, drinking less, doing fewer drugs, having less sex. A different type of risk tolerance, they are less willing to defend free speech norms if it potentially would cause injury to someone. That’s kind of a — free speech is kind of a pro-risk kind of take in some ways because speech can cause effects, of course. On the other hand, you have this boom and bust, and various booms and busts, in crypto. You have Las Vegas bringing in record revenue. You have record revenue in sports betting and things like that. You have the CEO of OpenAI saying, yeah, this might destroy the universe, but it’s worth it. It’s a good gamble to take. You have FTX and all this stuff. And the first trip I made after COVID was to a Casino in Florida, which is every bit the shit show that you think it might be. And the tournament drew record numbers of Poker players. And so it just seems to me like we are in a world now where institutions are less trusted. And some people respond to that by saying, O.K., I make my own rules now, and this is great, and I have lots of agency. And some respond by kind of withdrawing into an online world, or maybe clinging on to beliefs and experts that have lost their credibility, or just by becoming more risk averse. I mean, I think the pandemic also revealed that there’s a lot of differences in introversion versus extroversion. I just can’t deal with being cooped up inside all day. This doesn’t work for me at all. But I think some people kind of secretly like the idea that, O.K., there’s no more FOMO. I can kind of be cozy all day. And that’s fine. There’s differences in desire for human companionship and things like that too.” “Let’s talk about a couple of those people. One of the things that’s kind of fun about the book is you spend time with people whose approach to risk you find sophisticated and interesting.” “Yeah.” “One of them is Peter Thiel. What were your impressions of Peter Thiel? What did he learn spending time with him?” “The first impression is that he’s a weird dude. I interviewed him by phone. And the first question I asked him he took half an hour to answer. So he’s very thoughtful. And the question was what I thought was kind of a softball question. It’s like, if you ran the world 1,000 times or 10,000 times, how often do you think you’d wind up in a situation like the one that you’re in? And it was kind of a nerdy way to ask, do you think you got lucky. Which in Thiel’s case is interesting. There’s an anecdote in the book about this famous or infamous car trip he took with Elon Musk. They were going to pitch Michael Moritz at Sequoia Capital, and Elon had a new McLaren F1 and was going way too fast, and spun out of control in the middle of whichever Sand Hill Road or whatever, and they totaled the car. They could easily have been killed. And instead, they actually hitchhiked to this meeting and saved what was then called Confinity — it was like the future of Paypal, right? And so this twist of fate, twist of good fortune, kind of helped [LAUGHS]: Peter Thiel out. But most people understand, like —” “Wait, how did it help him out? I mean, he didn’t die.” “Well, he didn’t die. So he avoided — yeah, he avoided dying, I guess I’d say. So probably the expectation was not that he’d die. But the point is still that you can easily have a world in which Elon Musk and Peter Thiel are not a part of it if there’s a car going the wrong way and the other side of the road. So most people, when you ask that question — I asked Mark Cuban, for example — they’ll give the politically correct response. Which is, oh, of course I’ve been very lucky, and I’m a talented person, but of course it’s a 1 in a million thing. Right? And Thiel objected to the question. He said, you know, well, if it’s predetermined, then the odds are 100 percent. And if the world’s not predetermined, then the odds are probably approximately zero. But that doesn’t really make sense. Like, how can you perturb the world by exactly this amount? But I think he kind of believes in predestiny a little bit. And —” “As a spiritual thing or as a matter of classical physics?” “There’s a good book by I think Max Chafkin was the journalist — or ‘Chaff-kin’— I don’t how you say his last name — about Peter Thiel called ‘The Contrarian,’ which is convincing that Thiel is actually quite conservative, more than libertarian, and probably quite religious. But I also think that if you ARE one of these people, just the amounts of wealth, and success, and power that Silicon Valley has, I do think some of these people kind of pinch themselves and wonder if they have been one of the chosen ones in some ways or been blessed in some ways, or, maybe the nerdy version of it, think they’re living in a simulation of some kind. Like, what odds would you give yourself that that actually makes sense that you’re the protagonist of the story? It must be kind of weird, right?” “So I used to interview Thiel. Not super regularly but every so often. My impression of him, which has been my impression of a lot of the I would call them ideologist VCs, which is not all VCs, but the ones who are heavily behind or out online and sort of pushing a kind of what I would think of as like VC ideology that leans now right, talking to him always interesting. Because over the course of a conversation, he would offer like 15 or 20 ideas. I would call them more thought experiments than analytical arguments. They were not empirically backed, typically. And you would leave and be like, 13 of those seem genuinely ridiculous to me. Two of them might be very importantly right. I’m not 100 percent sure which are the two and which are the 13. And Peter Thiel, I think, is very — he is a sort of template of the VC mind, and a lot of VCs try to be him. And he’s been very successful. I mean, he’s a guy who has backed a number of very important companies, found a number of very important founders. He is able to do something there. But it is oriented towards being right in important and counterintuitive ways, like, three out of 20 times and doesn’t care about being wrong 17 out of 20 times. Whereas if you think about media, media is oriented towards being right 17 out of 20 times, and the three that it gets wrong are going to be really big because they’re going to be correlated across the entirety of American institutions. But it’s a very different way of thinking about risk. It’s like you want big payouts, not a high betting average.” “And that’s because this is core to the VC mindset. The two things that you hear from every VC, one is the importance of the longer time horizon. So you’re making investments that might not pay off for 10 or 15 years. But number two, even more important, is the asymmetric ability to bet on upside. They are all terrified because they all had an experience early in their career where Mark Zuckerberg walked through their door, or Larry Page or Sergey Brin walked through their door, and they didn’t give them funding. And then they wound up missing on an investment that paid out at 100x or 1000x or 10,000x. And so if you can only lose 1x your money, but you can make 1000x if you have a successful company, then that changes your mindset about everything, and you want to avoid false negatives. You want to avoid missed opportunities. And I think there’s a tendency for a certain type of smart person to provoke, to troll a little bit. I think he’s like that a little bit mean. This is also partly the thing on Twitter, right? I kind of us Twitter sometimes as a sketch pad [LAUGHS]: a little bit for slightly irreverent, half-trollish ideas that might later turn into newsletter posts or something like that, or might be developed further, and probing around and seeing what things land and what don’t. Like a stand mic night at a comedy show or something. And I think that’s how Twitter is meant to be used. But other people use it for enforcing consensus. But we’ve already talked about Twitter. But yeah —” “Well, you can never talk about it enough, particularly with these people. The one thing I will say on that, and I think this is true for virtually everybody I know who has been on that platform for a long period of time, is they will tell you that I have this persona on Twitter.” “Yeah.” “Right? Twitter is not real life. I mean, I use it to provoke. I’m having fun. I’m shitposting. I’m trolling. And people, over time, if they spend a lot of time there, become more like who they are there. That is true for Marc Andreessen, another person who you profile and talk to in the book. It’s true for lots of people in politics I know. Ted Cruz has become his Twitter persona even more than he once was. It happened in Democratic politics I think in 2020. Different campaigns became more like their Twitter incarnations than that person had been in politics before. And I think it has to do with social dynamics. Because over time, the people you get praise from become more persuasive and credible to you. The people who begin to hate you, you sort of repel from. People I think always think they can be playful in their social dynamics, but actually who you end up surrounding yourself, even online, you become them. It’s very, very hard to maintain that kind of separation.” “I mean, clearly, Elon Musk maintained a stance for a while that, oh, I’m just kind of a libertarian moderate. Like, no, he’s kind of like a right-pilled conservative.” “Yeah. And I’m just having fun. I’m posting funny things. He’s his Twitter persona now. You spent some time with Sam Bankman-Fried.” “Yeah.” “Tell me what you learned from him or learned about him.” “I think Sam is kind of insane [CHUCKLES]:, and I’m not very sympathetic to him. I mean, I’m sympathetic in the sense that this is this very dramatic reversal of fortune, where he’s kind of literally emerging and on top of the whole world, and shooting commercials with Tom Brady, and it kind of all collapses, and he becomes very abandoned overnight. So he’s kind of reaching out to a couple of journalists to have conversations because he basically no friends left in the Bahamas anymore. And his parents are there and two of his employees are there, but everyone else has fled the island. Sam is somebody who has to be owned by the river. But, you know, he is unabashedly a part of that world. I mean, he had his tentacles in every part of that world. He was active in Democratic and actually, under the radar, Republican political donations. He was trying to figure out how to get into sports betting legally and things like that. And so he is kind of everywhere. And of course, most of all, with the effect of altruists — in the original plan for the book, there was this awkward transition between the chapter on crypto and the chapter on effective altruism. I’m like, how do I have a natural transition? And then SBF is very important in both worlds, and it’s a very strange connection that somehow crypto profits are funding these people who want to cure malaria or something in Africa. But, you know, I think there are a couple of things. One is that I think people were overly impressed by SBF, partly because he was able to manipulate his self image. I mean, he’s not the most conventionally normal guy, right? But he was very aware that founders — the founder algorithm, the VC algorithm is like we can’t — weirdness is good for VCs. The fact that SBF would play video games in investor pitch meetings or things like that, or dress down, or have a fidget spinner, they’re like, oh, he’s a little bit on the spectrum, and that’s actually probably good for a founder because you want the single-minded devotion. And he’s a little weird, but you want variance, variance, variance.” “Sleeps on a beanbag. Right? There was a real mythos around him.” “Which is kind of carefully constructed. He’s kind of inhabiting a character which is inspired by some inner SBF. And he’s kind of playing that character and then kind of forgets what has ever inner core values, whatever they were, might have been. But he is not a very competent manager of risk. He invested all this money in this Democratic primary for a candidate named Carrick Flynn in Oregon’s — I forget which — six or seventh district, maybe eighth district. And the candidate had been ahead in the polls by 15 points and wound up losing by 15 points. Because to spend $8 million in a congressional primary is kind of insane if you’re not in the New York media market or something. So the candidate would go to people’s houses, and they’d be like, hey, I’m Carrick Flynn. I’m a candidate for the Oregon primary. And they’re like, oh, I have your literature and bring out a stack of 20 flyers that SBF’s super PAC had sent on behalf of Carrick Flynn and made him look like a weird freak backed by this mysterious crypto billionaire. So, yeah, he had a tendency — and this is based on testimony from both the court case and an interview I did with Tara MacAulay I think his her name, his original co-founder at Alameda. He had the kind of often good initial instincts, and being a good estimator is an important skill in my world, but then would kind of double down on that a lot and rationalize things a lot. And there was also a bystander effect problem where so many people vouched for him — Sequoia Capital and all these Oxford philosophers, these effective altruists. And he’s on stage with Bill Clinton or whatever, and he’s invited to the Met Gala, and Tom Brady is shooting commercials with him. So what could possibly be wrong with this guy? I mean, maybe he seems a little bit weird to me, but all these other people are kind of in his corner. But no one was doing the due diligence. And he kind of figured out that despite — there’s a little contradiction in the river, where on the one hand we tend to think of ourselves as being contrarian. On the other hand, we’re pretty big fans of markets, because we know that it’s kind of hard to beat the Las Vegas point spread or it’s hard to beat the S&P 500 Index funds or things like that. So the market judgment is that SBF is a credible actor, and how would I trust my own judgment over the market judgment a little bit. And there was too much deference toward that and too much actually groupthink about SBF, because the problems were evident the whole way. I mean, he told Tyler Cowen that if he could flip a coin to double the amount of utility in the world plus 1 epsilon or something but there’s a 50/50 chance of blowing the world up, that he would take the coin flip and repeatedly.” “So you’re actually getting two earths, but you’re risking a 49 percent chance of it all disappearing.” “And again, I feel compelled to say caveats here of how would you really know that’s what’s happening, blah, blah, blah, whatever. Put that aside. Take the hypothetical — the pure hypothetical. Yeah. Yeah.” “And then you keep on playing the game. So what’s the chance we’re left with anything? Don’t I just Saint Petersburg paradox you into non-existence?” “Well, not necessarily. Maybe Saint Petersburg paradox into an enormously valuable existence. That’s the other option.” “I remember seeing that Tyler Cowen interview and thinking, that’s nuts. But I think it gets at a kind of nuts that there is a bias towards in the world you’re describing. There is an aesthetic around talking in probabilities. There’s an ability to think in probabilities, and there’s an aesthetic around probabilities — people attaching, I would often say, almost random probabilities to things. I see this a lot in Silicon valley, people who I would call it like faux Bayesian reasoning where they’re given some probability, but they have no reason to base the probability — 50 percent of this. And it makes you sound much more precise. It makes you sound like what you’re talking about. SBF was known for always talking in terms of expected value. Which is very appealing to the kinds of people you’re describing, maybe the kind of person even that you are. And people who know how to talk like that get through a lot of filters, because you sort of assume, if they’ve converted everything into probabilities, and they’re great at math, and he worked at Jane Street. I worried about this a lot with effective altruists for a while, which is a group I have a lot more sympathy for than most people now have. But there can be this tendency, I think, to fetishize a certain form of discourse. It’s like the first people into that form of discourse are doing something valuable, and then, after that, I think it can become a kind of costume of sloppy thinking. This worries me about models too. I’m curious how you think about it, because I often find that people talk in terms of probabilities but people hear them in terms of certainties. That somehow talking in terms of probabilities makes people more willing to believe you without actually being skeptical or attaching a failure risk to you.” “Yeah. I mean, there’s two things here. One is just there is a kind of jargon. In some ways I liken being from the river to being from the South of the United States or something, where there’s just a lot of shared cultural norms and unspoken discursive tendencies — it’s just the way we communicate, I think, in the river. But also, it’s really easy to build bad models. Even in narrow problems, like I want to forecast the NFL or something or build an election model, it’s easy to build bad models. And on these open-ended problems, it’s really easy to fall in love with the incomplete model of the world and then forget that — what’s the Kamala Harris coconut tree quote? A model does not fall from a coconut tree. It exists —” “It exists in the context of all that came before it. Sure.” “So a model is supposed to describe something in the real world. And if you lose sight of the real world and it fails to describe the real world, then it’s the model’s fault and your fault for building the model and not the real world’s fault. And that’s a lesson that people, I think, have a lot of trouble learning.” “Bankman-Fried is in prison. Thiel might in some ways be responsible for destroying the Republican ticket this year. I mean, in a close election, JD Vance now seems to have about as much negative value as we’ve seen from a recent Vice President. I’m not saying Peter Thiel’s the only reason Vance got chosen for the ticket, but he is one of the key reasons Vance is in politics. Before now, you would said JD Vance was Peter Thiel’s political bet that paid off best.” “Yeah.” “And now it might be his political bet that pays off worst. You mentioned Bankman-Fried’s political donations, which were kind of disastrous in a direct way sometimes. Also ended up taking a lot of other people down over time. If these guys are so good at making bets or seem to be so good at making bets, what are they missing in politics? As somebody who straddles those worlds, what is not in their models? So both these groups, both the river and the village, are groups of elites. And I think, ironically, both groups’ critiques of one another are kind of true, right? I mean, they kind of can be epistemic trespassers, but they are not very data driven when it comes to politics. And part of it, too, is that if you’re a VC, and you’re evaluating a lot of pitches and a lot of opportunities, you have very quick twitch reflexes for saying, O.K., something about this founder seems smart. Let’s investigate further. Let’s do an initial seed round of investing. But it’s like thin slicing and not necessarily — for this part of the river, the VC part of the river — more profound analytical takes on things. And so you’re surrounded by people that are inclined to agree with you, and you kind of see enemies on the other side. He thought maybe that people had some deeper intuitive sense in 2016 that something was wrong with Hillary Clinton, even though she was ahead in the polls. And to his credit, he did back Trump at a time when that seemed like a big risk to take. It seemed like it was probably going to be the wrong bet, and it seemed like he was losing a lot of credibility. And now, it turns out that he was kind of ahead of the curve. You know, people like Peter Thiel thought that the village had been discredited by 2016 and other things. You can’t really trust the polls, and they said Trump would never do x, y or z. But no, I mean, these guys often are pretty dumb about [LAUGHS]: politics. And it’s the same — the guys in the hedge fund poker game that I play sometimes are the guys that are like, I think Gavin Newsom is going to replace Joe Biden on the ticket. And it’s like, you actually were kind of right about part of this, but why Gavin Newsom? What is the infatuation with Gavin Newsom.” “I heard so many versions of that. I always thought it was so crazy.” “Yeah.” “But, you know, it’s funny. I would say what they’ve often missed, and Thiel’s particular on this, is how human beings react to different human beings. So JD Vance, for instance, wildly underperforms in the Ohio Senate race. And Vance’s problem right now, he’s pushed onto the ticket by, as best we can tell, people like Steve Bannon, Don Trump, Jr., Tucker Carlson, Elon Musk — so the very online, very reactionary pale, the people around Trump. And what is missed about him is he’s kind of offputting. He doesn’t talk to other people in a way they would like to be spoken to. He’s able to make even popular ideas like a child tax credit sound completely bizarre when he talks about them in terms of punishing childless adults — that there is something here, I think, when people look at the world — and I’ve seen this in a lot of different dimensions of these kinds of folks — when they look at the world too much in numbers, the intangibles begin to dissolve for them.” “Although I think some of these tangibles aren’t so intangible. Right? Where you can look at JD Vance’s margins in Ohio, you can look at historically candidates who don’t have experience getting elected to some lower office and then ascending the ranks, underperform. It’s been a factor in our congressional midterm models for years, for example. But, look, in some ways, these VCs are obviously incredibly, deeply flawed people. And so, why do they succeed despite that? I think because the idea of having a longer time horizon, number one, and being willing to make these plus expected value, positive expected value, high risk, but very, very, very high-upside bets, and gathering a portfolio of them repeatedly, and making enough of these bets that you effectively do hedge your risk, those two ideas are so good that it makes up for the fact that these guys often have terrible judgment and are kind of vainglorious assholes — half of them, right? They’re interesting people too. I mean, they’re very interesting I think. And they — I’m happy that the book is able to present, I think, a complete journalistic portrait of some of them. But they have lots and lots of flaws, and it’s made up for by the fact that this is kind of a magic formula for making money.” “Let me get us back to the election. So we mentioned before Harris’s approval ratings have gone from significantly underwater to net favorable very, very fast. She’s now leading in head-to-head polls. More than that, there’s a real deep, whatever Republicans have convinced themselves to the contrary, organic enthusiasm that has unleashed itself around her. She turns out to be very memeable in a way I’m not sure people quite predicted. I know most Democrats didn’t predict this. I don’t think you predicted it. So what was missed here? What wasn’t in the Harris model that should have been?” “Yeah, maybe you really can meme your way to victory. [CHUCKLES]: I don’t know. I wouldn’t necessarily have thought that. I mean, there’s something about how it’s off trend a little bit, and it’s kind of unexpected a little bit. And there’s something about that, that I think people were ready for a vibe shift, right? I think people in politics neglect just how annoying the pedantic, dramatic, no fun tone of politics was and the having to be like serious all the time. And if the worst Republicans can say about Kamala Harris, oh, she laughs a lot, maybe it kind of suits the mood a little bit after so many years of doom and gloom. So maybe it was just spontaneous and lucky. I mean, it’s also the case maybe when Kamala Harris was a candidate for the nomination in 2019, I had these tiers, and the top tier was Joe Biden and Kamala Harris. And the line was always, O.K., I got one of those right and one of those about as wrong as possible. But she was seen as this rising, up-and-coming political talent, and maybe the combination of misaligned strategy in 2019 and then not being marketed well by the White House, and we debated before what the reasons for that are, maybe that was the underperformance. And the rising star that people thought she was kind of the real Kamala Harris after all.” “So Harris ended up choosing Tim Walz, the governor of Minnesota, as her VP pick. You made a case that it should have been Josh Shapiro. Tell me why.” “Pennsylvania, number one. There’s about a 4 percent chance in our model that Harris will lose the election because of Pennsylvania, where she wins the other Midwestern swing states but she’s 19 votes or fewer electoral votes fewer because of Pennsylvania. And if you’re a probabilist, then a 4 percent chance — because campaigns often don’t make a difference, right? If we go into a recession in the third quarter, then Harris will probably lose through no fault of her own. But in the worlds where campaign strategy can make a difference, then the VP being from Pennsylvania is a reasonably big upgrade. And the fact that he has demonstrated his popularity with this very diverse state that’s kind of a microcosm of the US as a whole — in Pennsylvania, you have the Northeast, you have the Midwest, and even you have a little bit of the South creeping in the Appalachian part of the state. You have the suburbs, you have rural areas, and you have one of the biggest cities in the United States. You have a big African-American vote. You have lots of famous colleges and things like that. You have everything there, and he’s 15 points above water approval-wise. And that’s pretty powerful information to work with. I happen to think that Tim Walz is an above-average pick, better than most, better than JD Vance. Not a particularly high bar, but better than a lot of the recent picks. I mean, I think he’s kind of memeable as America’s goofy dad kind of way, and he had a pretty moderate track record in Congress. And again, my premise is that, generally speaking, moderation wins. A lot of people disagree with that, but I think the empirical evidence is strong there. More progressive governance, of course, in Minnesota. But I think it was a somewhat risk-averse decision. Now, if you read —” “Why do you say that? I found this argument you’ve made very weird. So I think there’s a very good chance — I always told people on the VP pick my head says Shapiro and my heart says Walz.” “Yeah.” “I think that because I am a cautious person, if I were running for president, worried about losing Pennsylvania, I would have found it very hard not to pick Shapiro. Because if you don’t pick Shapiro, and you end up in a we lost Pennsylvania scenario, everybody’s going to blame you for blowing the decision that could have won Pennsylvania. In terms of the expected value, both on the front end and the back end, I understood Walz as a choice on vibes, this sort of energy, this momentum she has created. He was sort of able to upend and remake all Democratic messaging in a single morning Joe appearance. There is some intangible charisma to Walz that has made him — developed him overnight, this huge online fan base, that the cautious candidate, the one, listening to the consultants, the one reading Nate Silver polls, that candidate goes with Shapiro. Walz is something else. Why did you say that you understood Walz as risk averse?” “Because I think they were worried about news cycles where the left got mad, and/or the Gaza issue was elevated, and/or you had protests at the convention in Chicago in a couple of weeks. I think they were worried about that, and maybe kind of undermining what is clearly good vibes right now, and maybe overrating — I mean, maybe it’s not. Maybe I just think it’s the lower expected value decision of what gives Kamala Harris a higher chance of winning the electoral college in November.” “I think one of the questions I’ve been reflecting on — because I often think about, where do I disagree with writers I otherwise agree with? And I think I’m typically pretty aligned with you on a bunch of things, or Iglesias, or [INAUDIBLE], or some others. But a lot of you have really gotten into a view that I think takes the median voter theorem almost too seriously. That it’s like as if politics is unidimensional, and how close you are to ideologically the median voter is what decides elections. Which I do think moderation has an effect in. I mean, we see this in the political science research. But that doesn’t have a lot of room in that model for energy, for enthusiasm, for the mediation of politics — the thing that happens in between the candidate and the public for what is happening on social media, for what is happening on cable news. And you can often sort of back out explanations here and there. But I, for instance, think this sort of in retrospect explanation that what led Obama to victory was careful moderation — one of the things he did was moderate on some issues like gay marriage. Another thing he did was unleash astonishing levels of enthusiasm in the electorate for reasons orthogonal in many ways to his policy positions. And so I’m curious how you think about that. Because to me, one of the questions Shapiro and Walz raised, Shapiro and Harris sort of are a lot like each other. I think they sort of come off as the two smartest members of the law review. Right?” “Yeah, that’s interesting —” “Which is like kind of —” “— for sure.” “— not necessary the visual you want — maybe it is but might not be — and that there is something here that is I guess people call it vibes now. I feel like it’s a little dismissive. But how you play out in earned media, in social media, how much people want to talk about you, that feeling of enthusiasm, how do you think about that as somebody who builds models and handicaps politics?” “I mean, look, if you’re literally building a congressional model, there’s a model that forecasts the vote based on fundamentals, which means not the polls if you don’t have polling, for example, based on whatever it is, seven or eight factors. And one of those factors, if you’re incumbent, is how often do you vote with your party. And the more often you buck your party, actually the more often — like Susan Collins or Joe Manchin — then you tend to overperform in your congressional race. Now, that’s also one of eight factors. Right? And even when you have all eight factors, there’s still quite a bit of uncertainty in the race. So to me, it’s like this is something where if you’re used to looking at larger data sets, you can come up with counterexamples of Jon Tester is pretty progressive actually and somehow manages to get reelected in Montana with this kind of maybe Tim Walz-like folksy personality or something —” “Sherrod Brown. Sort of similar to that.” “Also pretty progressive. But if you take all the data from every congressional race since 1990, then it becomes clear in the aggregate, right? And I’d also say, if we could get progressives to the point where — I don’t know who we is in this sentence, because I’m not sure I identify as progressive — liberal but not progressive, I’d say — if we could get them to the point where they said, yes, the median voter theorem is mostly true but sometimes outweighed by other factors. But yeah, to get them to that point, instead of thinking, oh, you win elections by winning the base — I mean, that might have narrowly been true in an earlier —” “Wait, you’re turning this around on progressives. Because I’m asking it of you. I agree that progressives should take the median voter theorem more seriously. But I am asking you whether energy, enthusiasm, media — I just think attention in politics is undertheorized. I think if you look at Donald Trump, and you do a thing that I’ve seen people do, and say, look, he is more like the median voter on certain things like immigration, et cetera, or at least he was perceived as more moderate than Hillary Clinton and that’s why he won, I think that is an undertold story about Donald Trump that is somewhat true. I think that missing the showmanship of Donald Trump, the entertainment value, the energy he unlocks in people. There’s a reason that Trump had Dana White from the UFC and Hulk Hogan on his night of the RNC. So in 2020, Joe Biden’s view is that the election should be about Donald Trump, and Donald Trump’s view is that the election should be about Donald Trump. And that was a theory of attention they both agreed on, and it worked out for Joe Biden. In 2024, Joe Biden’s view is the election should be about Donald Trump. Donald Trump’s view was the election should probably be about Donald Trump. And that was a bad theory of attention. Biden had no way of shifting a narrative that wasn’t any good for him.” “Yeah.” “And so I guess this is what I’m getting at, that one thing that I worry about in some of this thinking among people I like is that attention is important. Candidates have different theories of it, but I don’t know that we know how to think about it as rigorously as I wish we did.” “Look, I agree. I mean, again, with Harris, maybe you do have to revise your views a little bit. I think also maybe in a campaign that’s a sprint and not a marathon, then maybe you never reach the long run. It seems possible. Usually, I’d say don’t worry about momentum over the next two weeks, because inevitably you’re going to have a bad news cycle later on. It’s just how the media works and it’s how elections work. It is possible they can just sprint their way to a memeified victory in this shortened, modified campaign. That they have a good convention, and that she wins whenever the debate is held, and then you’re in October and everyone’s crazy and explicitly partisan, they may be able to sprint to a narrow electoral college victory without having this skeptical news cycle. So that may be an argument for Walz, I think.” “One of the reasons on my mind is not actually Walz. And as I said before, because I do want to say this, I’m not sure who she should have picked as VP. I actually have very conflicted views on this, although I really, really enjoy Tim Walz, and really enjoyed interviewing him, and think he’s a pretty unusual political talent. But I think you could say the same about Josh Shapiro in different ways, and Pennsylvania is a very big state. But I’ve been interested in the shift in — look, you have a campaign staffed by many of the same people, particularly in the first two weeks, and yet the campaign’s tenor has completely changed. The tone of press releases is now they are trying to get you to talk about them and doing that by courting controversy, by being kind of mean in a way. Democrats have not been mean in a long time. That Tim Walz actually made a JD Vance couch joke in his introducing himself as her vice presidential pick speech — let’s put it this way, that is not something that Joe Biden campaign was going to do. They want people to talk about them. They want to court kind of controversy, outrage. They want attention. But I think the reason it’s all on my mind is what I am seeing in them is a radically different relationship to attention than the campaign that the same people were running two weeks ago.” “Yeah. And this why we rely on you for how much these people overlap. Like, that’s not something I really —” “They overlap tremendously.” “Yeah.” “I mean, it’s not the exact same people. Mike Donilon isn’t running things anymore. But there’s enough of the same people here that you’re not dealing with ‘nobody knew how to write these press releases’ a month ago.” “It is interesting that Joe Biden, based on the polling, would probably have been better off in election with low turnout. The one thing that might have saved him is if you get that special election, midterm election, lower turnout where people aren’t very happy about it, but they go to the polls and vote for Biden and the Trump people don’t bother to show up. Because unlike in the past, the marginal voters have been more likely to vote for Trump than for Biden. So maybe by having a really boring campaign, it kind of suited their interests. With Harris, who is bringing back some of the younger voters and some of the voters of color that had defected to Kennedy, or defected to Trump, or defected to sitting out the election, those are also some of the more marginal voters. And so, now, all of a sudden, she probably doesn’t mind as much higher turnout which is going to get young Latino women to vote for her or young Black men to vote for her when they might not have voted for Biden. And so it kind of matches the incentives of where you want to turnout to be on November 5.” “Tim Alberta in the Atlantic had a great piece on the way the Trump campaign was thinking about the race that came out around the time of the debate or right after the debate. And they felt they had Nevada, North Carolina completely locked up — and Georgia — and that this was really a race in three, maybe four states. My understanding is Harris and her team think they have re-expanded the map. They think that Nevada, Arizona, Georgia are for sure back in play. They think that North Carolina might be back in play. Do you think that’s true? Do you think the map has gotten bigger?” “I think that’s right. Because, again, look at the voters that Biden was falling off with. Nevada, people don’t remember, they think of it as kind of libertarian old miners, right? No, Nevada is extremely diverse, and it’s working class voters of color. Big fall-off constituency for Biden. Georgia, you have tons of young professionals, and tons of great colleges and universities, and, of course, tons of Black voters — the same groups that he’s declining from a little bit. North Carolina has been, interestingly, kind of close in the polls. Arizona is the one that didn’t seem to have moved quite as much, though there was one poll yesterday with Harris ahead there. But that’s right. I mean, I think the map has expanded, and it’s obviously plausible again now that she would win Georgia, especially with the Brian Kemp stuff not helping Trump one bit. At the moment — I was playing in a poker tournament, very on-brand, right — when Trump gets shot and has the iconic photo, which I’m not a Trump fan, but you kind of have to admire that, I think a little bit, I think a lot of people assume he’s going to win the election. I mean, with Biden already, he’s not going to lose after this. They try to shoot him, and he has this great photo opportunity, right? And then it seems like he’s at a high water mark. And then he picks JD Vance, and I think got a little arrogant.” [LAUGHS] “Because his initial instinct apparently was not to pick necessarily JD Vance and kind of talked out of it by his sons. And I don’t know what influence Peter Thiel or whatever had. But the VC guys were like, oh, JD Vance is kind of one of us. And he probably is smarter than the average VP or something. But that appeal has been demonstrated not to work. I mean, you saw it with Blake Masters for example, right? It works every now and then. I guess Rick Scott had a background in I don’t know what exactly, but like —” “Medicare fraud.” “O.K., yeah. [LAUGHS]: But for the most part, these —” “The guy the guy ran a health company that was convicted of the single largest Medicare fraud at that point in history.” “What I tell my VC friends is if you have a rich guy, just have him buy a basketball team or something. He’s not going to come across very well to the average voter. And I think they don’t understand that. And then, again, in a poker tournament or a poker home cash game, when you go from having a big stack and you’re kind of like, oh, this is so nice. Man, I’m going to go home and cash out my winnings. Maybe I’ll have a nice little whiskey at the bar or something. And this is going to be — I’ll text my friends about how well my session ran. And then you lose a big pot, and then you lose another big pot, and then you go on tilt. And before long, you have no chips left.” “What is tilt?” “Tilt is playing emotionally, particularly in poker or other forms of gambling. It’s often sparked by a bad beat. Meaning that you got unlucky. Or it can be sparked by getting bluffed and getting mad at your opponent. Or bad luck. Or sometimes you can actually have what’s called winner’s tilt too, where maybe this is what Trump had in picking JD Vance. You have a bunch of things that are going really well. I mean, this election was going about as well as it could for Donald Trump. He’s not a popular guy, yet he had moved ahead in some of the National polls by four or five points. It’s pretty hard to do. I mean, he’s lost the popular vote twice.” “Trump feels very on tilt to me. When you think about him, for Donald Trump, he had been pretty on his message. He was talking a lot about immigration. He was talking a lot about inflation. He was letting it be known that he was thinking about picking Doug Burgum. He seemed to be enjoying this idea that he was — people were longing for a stability They now associated with his presidency rightly or wrongly. They wanted the lower prices back. They don’t like the war in Gaza. They don’t like the war in Ukraine. Maybe Trump is a strong man who can bring it back. And he was kind of playing into that. And since the Harris switch and him beginning to fall in the polls, you feel this old Trump returning. The Trump who goes to Georgia and begins yelling at the governor — the Republican governor — of Georgia. The Trump that goes to the National Association of Black Journalists and begins to talk about how nobody knew Kamala Harris was Black. The Trump who is just trying out attack lines, trying to find something that will work no matter what the kind of cost might be. I mean, your description of him playing emotionally — he’s not listening to anybody right now. He’s flailing.” “And the fact that, according to the reporting, that they weren’t prepared for the eventuality when Joe Biden dropped out was kind of inexcusable. I mean, if you looked at prediction markets, it was immediately a live consideration after the debate. I think they overestimated the degree to which Democrats are a personality cult. I mean, they can be. There was maybe a personality cult around Obama, or Bill Clinton, or things like that. But there wasn’t one around Joe Biden. He was kind of always the candidate of the party. And it was not in the party’s interest any longer to have him as their nominee. And so the Democratic Party is capable and powerful in a way the GOP is not. And they extrapolated from their views to how Democrats would behave and underestimated the smart decision that the party was capable of making.” “I talked to Republicans about this, about why they weren’t more prepared, and one thing I heard from them is they just didn’t think Biden was going to step aside. I mean, if you’re a party that has completely bent the knee to Donald Trump and is now years and years into not being able to convince Donald Trump of functionally anything, it might shift your sense of how people in power, particularly the apex of power, act. It’s one reason — this is a place where you and I’ve been a little bit different — I’ve been more on the side of Joe Biden did something difficult that deserves praise. Because — and I think you see this in how Republicans were thinking — leaders just often don’t do this. The kind of personality that gets you to that point is not the kind of personality that leaves power gracefully. It’s why, when people are talking about dictators, there’s endlessly this talk of how to create golden parachutes for dictators. You’re dealing with a kind of human being that has told a story about their own essentialness. Going back to your point about Elon Musk and feeling like you’re the main character of global life — particularly you’ve become the American president — you sort of were the main character of global life for a while — that does something to you. Those people don’t give it up easily.” “No. And if you look at the history of — before there was whichever Amendment it was, 20-something Amendment —” “22.” “— that prevents you from running for more than two terms, it was pretty routine for candidates to tease — Woodrow Wilson had a stroke and wanted a third term. Harry Truman had like a 32 percent approval rating and wanted a third term, second full term. Old men are often pretty stubborn. And I think the most interesting thing is that if Harris wins — or maybe comes close, but mostly if she wins — what that will say about the primary system, right? Maybe we should go back to giving a larger role to superdelegates for example.” “I want to end on a part of your book I found really interesting, which is about the physical experience of risk — in gambling, but in other things. You talk about pain tolerance. You talk about how the body feels when you’re behind on a hand and you’re losing your chips. You’ve talked about being on tilt. But I see it in politics too. I mean, there is a physical question that comes into the decisions you make. I see it on this podcast. There are times when a question is physically uncomfortable for me to ask another person. Tell me a bit about how you think about this relationship between the body and the ability to act under pressure to make intuitive decisions in moments of very high stress.” “So human beings have tens of thousands of years of evolutionary pressure which is inclined to respond in a heightened way to moments that are high stakes, that are high-stress moments. If you’ve ever been in a situation where you saw someone’s life in danger or your own life was in danger — you know, I was in LA in January, and there was an armed robbery outside the place where I was trying to get just a cup of coffee. And time kind of slows down a little bit in situations like that. And you don’t realize how stressed out you are until I texted my partner and be like, LOL, almost got shot, ha, ha. And I was kind of like, oh yeah, I was too cool for school. And then an hour later, I’m getting some tacos or something and I almost break down. It’s like, oh my god, it could have gone really, really badly. Public speaking also triggers this for people because objectively it’s a pretty high-stakes thing. If you’re playing a $1 or $2 poker game, and it’s nothing for you, your body will when you’re playing a $100-200 game where it really matters — you will just know. You’ll experience that stress. Even if you suppress it consciously, it will still affect the way that you’re literally kind of ingesting your five senses. So if your heart rate goes up, that has discernible effects. But actually, your body is providing you with more information. You’re taking in more in these kind of short bursts of time. People who can master that zone — and I use the term zone intentionally, because it’s very related to being ‘in the zone’ like Michael Jordan used to talk about, or golfers, or hockey goalies, or whatever else — learning to master that and relish that is a very powerful skill. Because you are experiencing physical stress whether you want to or not.” “How much is that, in your view, in your experience, learnable, and how much of it is a kind of natural physical intelligence some people have and some people don’t?” “I think it’s actually quite learnable. It’s a little bit like if you’ve been on mushrooms before [LAUGHS]: then you kind of learn, oh, this is the part of the brain that is — this is the things that look a little funny when you’re on mushrooms, right? You can kind of maybe tone it up or tone it down a little bit. So it’s very much like that. I mean, it’s terrifying the first time it happens. But when you start to recognize it, and you kind of make a conscious effort to slow down a little bit, and take your time, and try to execute the basics, it’s not as much about trying to be a hero. It’s about trying to execute the basics. Because when everyone’s losing their shit, if you can do your basic ABC blocking and tackling, then you’re ahead of 95 percent of people. And keeping bandwidth free for dealing with emergency situations, that will take you very far.” “It’s funny, because that feels to me like a very important question that is hard to test in politics.” “Yeah.” “People have to make profound decisions under incredibly high stress. And we have simulacrums of it. The debate, in a way, is a simulacrum of that. Very, very high stress. Speeches on teleprompters are not very good analogies for that. But this question of how good is a person at that moment —” “I mean —” “— how do you evaluate that?” “I mean, Trump, after getting shot, kind of performed very well. And I think, again, the Harris moment of leaping right into action to secure the nomination also has to be seen as very good performance under stress. And Biden’s failure under stress — I mean, he went to some kind of spiral of some kind or another, physical, or mental, or whatever else. So those kind of three pivotal moments — the assassination, the debate, and then Harris seizing the nomination in record time — speak to the difference in performance. And that’s why the two of them, Harris and Trump, are still candidates for the presidency, and Biden is not.” “I was just reading Nancy Pelosi’s new book before I was reading yours, because I just had her on the show, and she talks about how, above all, she says, that what a Speaker of the House needs is intuition. They need to be able to act. And she says that the key thing is you have to act fast. Because every moment you don’t act, your options are diminishing. And I ended up thinking, then, when reading your book, of it. Because what she was describing is quite, I think, for her, physical. Like something in her knows how to act and is unafraid to act in those moments. The thing that was crucial about her, I think, in this process, inside the Democratic Party of getting Biden out, is she was willing to act in public to take the pressure of that in ways very few people were. And somebody had to be doing that in public to create space for others to be considering it in private. But you look at her career, and she has this sort of intuitive capability to know when to move. And there’s something in it that I don’t think she can explain how she does it, but it makes her a fascinating leader. People believe that she will act. And she will act because something in her knows when to act, and she’s unafraid.” “Yeah. So is gut instinct overrated or underrated? Well, it depends on how much experience you have, right? Poker players have — because now poker is actually kind of a solved game. There are computer solvers they’re called that spit out this very complicated solution to poker. Hard to execute in practice, but it’s technically speaking a solved game. However, the best poker players can have uncannily good instincts based on reading physical tells, just the kind of vibe someone gives off. And if — you know, I played a lot of Poker and writing this book, more live poker than I have in the past, and you develop a sixth sense. Not all the time. It helps if you’re well rested. But you develop a sixth sense for whether someone has a strong hand or something. Like they’re glowing green or something almost sometimes. And you can test it, because you can say, I know that I’m supposed to fold this hand here. It’s a little bit too weak to call against a bluff. But I just have a sense that he’s bluffing. And lo and behold, you’re right more often than you’d think — more often than you need to be to make that call correct based on the odds that you’re getting from the pot. So if Nancy Pelosi has decades and decades of experience in politics and reading the moves of how the coalition is moving, I mean, that’s something where intuition probably plays a pretty good role. And also the fact that being willing to work with incomplete information — I mean, I don’t know how much longer Biden could have — maybe they could have run out the clock [LAUGHS]: potentially.” “Oh, they 100 percent could of. That day when he sent that letter to congressional Democrats and said, I’m not leaving — this conversation is over, stop trying to overturn the will of the primary voters — I was getting congressional Democrats telling me, this is done. It’s a fait accompli. He’s quelled the rebellion. It looked to me like he had. I was talking to other people. They said, 10 percent shot he’s out. Nancy Pelosi goes on ‘Morning Joe’ two days later and says, we’re really looking forward to him making a decision. And I asked her about it. And I said, what was happening? I mean, he had just sent that letter. And she said, yeah, but that was just a letter.” “Yeah.” “I didn’t accept the letter as anything but a letter. I mean, there are some people who were unhappy with the letter. Let me say it a different — some said that some people were unhappy with the letter. I’ll put it in somebody else’s mouth. Because it was a — I don’t think — it didn’t sound like Joe Biden to me.” “I’m like, oh, you read a bluff.” “So I think Nancy Pelosi might be pretty good at poker.” “Good place to end. Always our final question — what are three books you’d recommend to the audience.” “So one book is pertinent to the discussion that we had a moment ago, which is called ‘The Hour Between Dog and Wolf.’ It’s written by John Coates, who is an academic economist who then became a derivatives trader, I think, for Deutsche Bank in New York and found out that the traders that he studied were really weird. Like these traders would have strange physical and mental stress responses to the market rising or falling. And he was so fascinated by it that he went back and became a neuroscientist and basically did studies of traders. So you test the testosterone of like an options trader or a guy who works at a hedge fund and see how it varies from day to day and correlates with performance. So yeah, so he studies the physical responses of risk-takers, and the book is called ‘The Hour Between Dog and Wolf.’ So that’s one recommendation. Number two, in a totally different direction, ‘The Making of the Atomic Bomb’ by Richard Rhodes. We didn’t talk as much about some of the AI stuff today, but at the end of the book there’s a pretty long, elaborate comparison between the Manhattan Project and the building of these large language models that some people think could be potentially very dangerous. And nuclear weapons are, I think, a pivot point in human history, and this book is kind of the best history of that. The third is called ‘Addiction by Design,’ by Natasha Schüll. And Natasha is an NYU anthropologist who studied Las Vegas as her thesis basically. She did a lot of reporting just about the properties of slot machines, and how addictive they are, and about the kind of casino gambling industry in general. And of course, she draws metaphors between that and the rest of society.” “Nate Silver, thank you very much.” “Thank you, Ezra.” [THEME MUSIC]

The last I looked, your model has Kamala Harris winning the election at around 52 percent — it might be a little different today. But this has been an unusual election. How much stock do you put in your model right now?
We are having trouble retrieving the article content.
Please enable JavaScript in your browser settings.
Thank you for your patience while we verify access. If you are in Reader mode please exit and log into your Times account, or subscribe for all of The Times.
Thank you for your patience while we verify access.
Already a subscriber? Log in .
Want all of The Times? Subscribe .
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Biomechanical and functional efficacy of knee sleeves: A literature review
Affiliations.
- 1 Department of Biomedical Engineering, Faculty of Engineering, University of Malaya, 50603, Kuala Lumpur, Malaysia.
- 2 Sports Medicine Unit, Faculty of Medicine, University of Malaya, 50603, Kuala Lumpur, Malaysia.
- 3 Department of Biomedical Engineering, Faculty of Engineering, University of Malaya, 50603, Kuala Lumpur, Malaysia; Centre for Applied Biomechanics, Faculty of Engineering, University of Malaya, 50603, Kuala Lumpur, Malaysia. Electronic address: [email protected].
- PMID: 28673759
- DOI: 10.1016/j.ptsp.2017.05.001
Background: Knee sleeves are widely used for the symptomatic relief and subjective improvements of knee problems. To date, however, their biomechanical effects have not been well understood.
Objective: To determine whether knee sleeves can significantly improve the biomechanical variables for knee problems.
Method: Systematic literature search was conducted on four online databases - PubMed, Web of Science, ScienceDirect and Springer Link - to find peer-reviewed and relevant scientific papers on knee sleeves published from January 2005 to January 2015. Study quality was assessed using the Structured Effectiveness Quality Evaluation Scale (SEQES).
Results: Twenty studies on knee sleeves usage identified from the search were included in the review because of their heterogeneous scope of coverage. Twelve studies found significant improvement in gait parameters (3) and functional parameters (9), while eight studies did not find any significant effects of knee sleeves usage.
Conclusion: Most improvements were observed in: proprioception for healthy knees, gait and balance for osteoarthritic knees, and functional improvement of injured knees. This review suggests that knee sleeves can effect functional improvements to knee problems. However, further work is needed to confirm this hypothesis, due to the lack of homogeneity and rigor of existing studies.
Keywords: Biomechanics; Knee sleeve; Proprioception; Review.
Copyright © 2017 Elsevier Ltd. All rights reserved.
PubMed Disclaimer
Similar articles
- A kinetic and kinematic analysis of the effect of stochastic resonance electrical stimulation and knee sleeve during gait in osteoarthritis of the knee. Collins A, Blackburn T, Olcott C, Jordan JM, Yu B, Weinhold P. Collins A, et al. J Appl Biomech. 2014 Feb;30(1):104-12. doi: 10.1123/jab.2012-0257. Epub 2013 Jul 22. J Appl Biomech. 2014. PMID: 23878205 Clinical Trial.
- Efficacy of knee braces and foot orthoses in conservative management of knee osteoarthritis: a systematic review. Raja K, Dewan N. Raja K, et al. Am J Phys Med Rehabil. 2011 Mar;90(3):247-62. doi: 10.1097/PHM.0b013e318206386b. Am J Phys Med Rehabil. 2011. PMID: 21273902 Review.
- The effect of bracing on proprioception of knees with anterior cruciate ligament injury. Beynnon BD, Good L, Risberg MA. Beynnon BD, et al. J Orthop Sports Phys Ther. 2002 Jan;32(1):11-5. doi: 10.2519/jospt.2002.32.1.11. J Orthop Sports Phys Ther. 2002. PMID: 11787904 Review.
- Clinical practice guidelines for rest orthosis, knee sleeves, and unloading knee braces in knee osteoarthritis. Beaudreuil J, Bendaya S, Faucher M, Coudeyre E, Ribinik P, Revel M, Rannou F. Beaudreuil J, et al. Joint Bone Spine. 2009 Dec;76(6):629-36. doi: 10.1016/j.jbspin.2009.02.002. Joint Bone Spine. 2009. PMID: 19467901 Review.
- Role of bracing in the management of knee osteoarthritis. Rannou F, Poiraudeau S, Beaudreuil J. Rannou F, et al. Curr Opin Rheumatol. 2010 Mar;22(2):218-22. doi: 10.1097/BOR.0b013e32833619c4. Curr Opin Rheumatol. 2010. PMID: 20035222 Review.
- Knee sleeves improve gait symmetry during fast walking in older adults. Inai T, Kudo S, Tsuchida W, Fujimoto M. Inai T, et al. Front Bioeng Biotechnol. 2024 Jul 17;12:1394314. doi: 10.3389/fbioe.2024.1394314. eCollection 2024. Front Bioeng Biotechnol. 2024. PMID: 39086498 Free PMC article.
- Impact of a Semi-Rigid Knee Orthotic Intervention on Pain, Physical Activity, and Functional Capacity in Patients with Medial Knee Osteoarthritis. Stetter BJ, Fiedler J, Arndt M, Stein T, Sell S. Stetter BJ, et al. J Clin Med. 2024 Mar 7;13(6):1535. doi: 10.3390/jcm13061535. J Clin Med. 2024. PMID: 38541761 Free PMC article.
- Effect of Knee Orthosis and Kinesio Taping on Clinical and Neuromuscular Outcomes in Patients with Knee Osteoarthritis: A Randomized Clinical Trial. Fazli F, Farsi A, Ebrahimi Takamjani I, Mansour Sohani S, Yousefi N, Azadinia F. Fazli F, et al. Arch Bone Jt Surg. 2023;11(10):625-634. doi: 10.22038/ABJS.2023.72208.3362. Arch Bone Jt Surg. 2023. PMID: 37873530 Free PMC article.
- Cushioned Footwear Effect on Pain and Gait Characteristics of Individuals with Knee Osteoarthritis: A Double-Blinded 3 Month Intervention Study. Schwartz I, Ofran Y, Bernovsky S, Kandel L, Rivkin G, Karniel N, Seyres M, Portnoy S. Schwartz I, et al. Sensors (Basel). 2023 Jan 26;23(3):1375. doi: 10.3390/s23031375. Sensors (Basel). 2023. PMID: 36772413 Free PMC article. Clinical Trial.
- Can a knee sleeve influence ground reaction forces and knee joint power during a step-down hop in participants following anterior cruciate ligament reconstruction? A secondary analysis. Sole G, Pataky T, Hammer N, Lamb P. Sole G, et al. PLoS One. 2022 Dec 16;17(12):e0272677. doi: 10.1371/journal.pone.0272677. eCollection 2022. PLoS One. 2022. PMID: 36525413 Free PMC article. Clinical Trial.
Publication types
- Search in MeSH
Related information
- Cited in Books
LinkOut - more resources
Full text sources.
- Elsevier Science
Other Literature Sources
- scite Smart Citations
- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
Warning: The NCBI web site requires JavaScript to function. more...
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.

Extended Reality Interventions for Chronic Pain: A Systematic Review
Evidence Synthesis Program
Elizabeth Goldsmith , MD, PhD, Conceptualization, Methodology, Investigation, Formal analysis, Visualization, Writing – original draft, Writing – review & editing, Supervision, Project administration, Maylen Anthony , MPH, Conceptualization, Methodology, Investigation, Formal analysis, Visualization, Writing – original draft, Writing – review & editing, Project administration, Adrienne Landsteiner , PhD, MPH, Conceptualization, Methodology, Investigation, Formal analysis, Visualization, Writing – original draft, Writing – review & editing, Kristen Ullman , MPH, Conceptualization, Methodology, Investigation, Formal analysis, Writing – original draft, Writing – review & editing, Caleb Kalinowski , MA, Conceptualization, Methodology, Investigation, Formal analysis, Writing – original draft, Writing – review & editing, Nick Zerzan , MPH, Conceptualization, Methodology, Investigation, Formal analysis, Visualization, Writing – original draft, Writing – review & editing, David Ewart , MD, Conceptualization, Methodology, Writing – review & editing, Tonya Rich , PhD, Conceptualization, Methodology, Writing – review & editing, Wendy Miller , MD, Conceptualization, Methodology, Investigation, Formal analysis, Writing – review & editing, Collin Calvert , PhD, Conceptualization, Investigation, Formal analysis, Writing – original draft, Writing – review & editing, David Thomas , MD, MS, Conceptualization, Investigation, Formal analysis, Writing – original draft, Writing – review & editing, Timothy Wilt , MD, MPH, Conceptualization, Methodology, Writing – review & editing, Supervision, and Wei (Denise) Duan-Porter , MD, PhD, Conceptualization, Methodology, Investigation, Formal analysis, Visualization, Writing – original draft, Writing – review & editing, Supervision, Project administration.
Affiliations
- Copyright and Permissions
In this systematic review, we synthesized evidence on benefits and harms of XR interventions for treatment of chronic pain or to prevent development of chronic pain (if treating acute pain). We present findings by pain condition, beginning with chronic low back pain and chronic neck pain, followed by other conditions. Within each condition, we provide results separately for VR and AR interventions, and then types of XR interventions (and comparators) within these categories. We conducted meta-analyses where feasible and provide qualitative summaries otherwise.
- Collapse All
- ACKNOWLEDGMENTS
- Executive Summary
- ABBREVIATIONS TABLE
- TOPIC DEVELOPMENT
- REGISTRATION AND REVIEW
- KEY QUESTIONS AND ELIGIBILITY CRITERIA
- SEARCHING AND SCREENING
- DATA ABSTRACTION AND RISK OF BIAS ASSESSMENT
- LITERATURE FLOW DIAGRAM
- OVERVIEW OF INCLUDED STUDIES
- CHRONIC LOW BACK PAIN (KQ1)
- CHRONIC NECK PAIN (KQ1)
- FIBROMYALGIA (KQ1)
- CHRONIC KNEE PAIN (KQ1)
- KQ1. OTHER CONDITIONS
- POST-SURGICAL PAIN & REHABILITATION (KQ2)
- KQ2. OTHER CONDITIONS
- Summary of Key Findings
- Limitations
- EVIDENCE GAPS & FUTURE RESEARCH
- CONCLUSIONS
- APPENDIX A. SEARCH STRATEGIES
- APPENDIX B. STUDIES EXCLUDED DURING FULL-TEXT SCREENING
- APPENDIX C. ONGOING STUDIES
- APPENDIX D. RISK OF BIAS ASSESSMENTS
- APPENDIX E. CHRONIC BACK PAIN
- APPENDIX F. CHRONIC NECK PAIN
- APPENDIX G. FIBROMYALGIA
- APPENDIX H. CHRONIC KNEE PAIN
- APPENDIX I. KQ1 OTHER CONDITIONS
- APPENDIX J. POST-SURGICAL PAIN
- APPENDIX K. KQ2 OTHER CONDITIONS
- APPENDIX L. PEER REVIEW COMMENTS AND RESPONSES
Suggested citation:
Goldsmith E, Anthony M, Landsteiner A, et al. Extended Reality Interventions for Chronic Pain: A Systematic Review. Washington, DC: Evidence Synthesis Program, Health Systems Research, Office of Research and Development, Department of Veterans Affairs. VA ESP Project #09-009; 2024.
Disclosures : This report was prepared by the Evidence Synthesis Program Center located at the Minneapolis VA Health Care System, directed by Timothy J. Wilt, MD, MPH and Wei Duan-Porter, MD, PhD and funded by the Department of Veterans Affairs, Veterans Health Administration, Health Systems Research.
The findings and conclusions in this document are those of the author(s) who are responsible for its contents and do not necessarily represent the views of the Department of Veterans Affairs or the United States government. Therefore, no statement in this article should be construed as an official position of the Department of Veterans Affairs. The final research questions, methodology, and/or conclusions may not necessarily represent the views of contributing operational and content experts. No investigators have affiliations or financial involvement ( eg , employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties) that conflict with material presented in the report.
This publication is in the public domain and is therefore without copyright. All text from this work may be reprinted freely. Use of these materials should be acknowledged.
- Cite this Page Goldsmith E, Anthony M, Landsteiner A, et al. Extended Reality Interventions for Chronic Pain: A Systematic Review. Washington (DC): Department of Veterans Affairs (US); 2024 Mar.
- PDF version of this title (3.4M)
Other titles in this collection
- VA Evidence-based Synthesis Program Reports
Recent Activity
- Extended Reality Interventions for Chronic Pain: A Systematic Review Extended Reality Interventions for Chronic Pain: A Systematic Review
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers

IMAGES
COMMENTS
This literature review helps clinicians to make evidence-based decisions for reducing knee pain and treating people living with knee OA to prevent knee replacement. This narrative review presented (i) the most recent updates on the pathogenesis of knee OA with the risk factors for developing OA and (ii) the most recent evidence for reducing ...
Patellofemoral pain typically affects people younger than 40 years who are physically active and has a lifetime prevalence of approximately 25%. The presence of anterior knee pain during a squat is approximately 91% sensitive and 50% specific for patellofemoral pain. Meniscal tears affect an estimated 12% of the adult population and can occur ...
KOA primarily manifests as knee joint pain that is aggravated by fatigue or weather changes and cold and wet weather, and relieved after rest or the application of heat. ... Smith SL, Marreiros SS, Steultjens M. Identification of clinical phenotypes in knee osteoarthritis: A systematic review of the literature. BMC Musculoskelet Disord. 2016 ...
A literature review on the causes of pain following total knee replacements was performed based on research papers published up to 1 April 2020. A database search on Scopus, PubMed and Google Scholar was conducted to look for articles in English with the search terms "total knee replacement", "pain", and "cause".
Knee pain affects approximately 25% of adults, and its prevalence has increased almost 65% over the past 20 years, accounting for nearly 4 million primary care visits annually. Initial evaluation ...
Knee Osteoarthritis: A Review of Literature. Ashraf Ramadan Hafez 1 *, Aqeel Mohammed . Alenazi 2, ... prevalence of knee pain and symptomatic knee osteoarthritis: survey and . cohort data. Ann ...
Background: Knee osteoarthritis is the most common joint disease and a major cause of functional limitation and pain in adults. The aim of this literature review is to review the existing evidence regarding the impact of exercise in people with knee osteoarthritis concerning physical and functional outcomes.
Abstract. Osteoarthritis of the knee is a prevalent condition that causes pain, discomfort, and disability that can severely impact the quality of life. This literature review aims to review the various interventional pain management techniques available to treat knee osteoarthritis. It analyzes the efficacy of various interventions such as ...
This literature review helps clinicians to make evidence-based decisions for reducing knee pain and treating people living with knee OA to prevent knee replacement.
Article PDF Available Literature Review. Narrative: Review of Anterior Knee Pain Differential Diagnosis (Other than Patellofemoral Pain) June 2021; Current Reviews in Musculoskeletal Medicine 14(2)
The general evaluation of the adult presenting with undifferentiated knee pain is discussed here, including details about differentiating among the causes of knee pain based upon the history and examination findings. For cases where knee pain develops following acute, low-energy trauma or chronic overuse, often in athletes or active adults, and ...
Small studies suggest that regenerative injections can improve pain and function in patients with chronic knee tendinopathies and osteoarthritis. Knee pain affects approximately 25% of adults ...
This literature review aims to review the various interventional pain management techniques available to treat knee osteoarthritis. It analyzes the efficacy of various interventions such as intra-articular corticosteroids, prolotherapy, viscosupplementation, platelet-rich plasma, and genicular nerve blocks with radiofrequency ablation or ...
The evaluation of knee pain most likely caused by musculoskeletal injury from acute trauma, chronic overuse, or a combination of these, particularly as this may occur in athletic and active adults, is reviewed here. The topic includes details about obtaining an effective history and a general scheme for differentiating among the causes of ...
Knee osteoarthritis (KOA) is a common chronic debilitating disease with an estimated prevalence of 23.9% in the general adult population. The condition is characterised by joint pain, functional impairment and significant reduction in quality of life. Management for KOA can generally be divided into conservative (non-operative) and surgical ...
A Systematic Integrated Literature Review was conducted. Published work related to pain management in individuals with chronic pain was identified by searching databases and reviewed. ... OA pain of the knee: Quasi-experimental study: CBT based on Bandura's concept of self-efficacy and behavior change: This program trial was a 4 week arthritis ...
DESIGN Narrative review. METHOD A literature search identified studies of incidence and prevalence of knee pain, disability, and radiographic osteoarthritis in the general population, and data related to primary care consultations. Findings from UK studies were summarised with reference to European and international studies.
A number of terms have historically been used in the literature to describe the combination of a patellofemoral joint replacement with a unicondylar knee arthroplasty, but a recent publication by Garner et al. conducted a literature review to establish which term was the most intuitive and appropriate . The recommendation was that a ...
Abstract. Purpose of Review. Anterior knee pain is a common musculoskeletal complaint among people of all ages and activity levels. Non-operative approaches with an emphasis on physical therapy management are the recommended initial course of care. The purpose of this review is to describe the current evidence for physical therapist management ...
The objectives of the present study were as follows: (1) review the literature characterizing the relationship between MME and knee OA; (2) summarize the OA-related sequela of MME; and (3) report and investigate the MRI methods of measuring MME. ... However, Liu et al 24 reported that a threshold of 2.5 mm of extrusion was found to be most ...
Knee pain is amongst the top five reasons for knee replacement revision in the United Kingdom. The number of TKRs is predicted to continue increasing due to the ageing population.A narrative literature review was performed on the different causes of pain following TKR.
Adverse knee pain occurs in 10-34% of all total knee replacements (TKR), and 20% of TKR patients experience more pain post-operatively than pre-operatively. Knee pain is amongst the top five reasons for knee replacement revision in the United Kingdom. The number of TKRs is predicted to continue increasing due to the ageing population. A narrative literature review was performed on the ...
Knee osteoarthritis (OA) affects over 650 million patients worldwide. Total knee replacement is aimed at end-stage OA to relieve symptoms of pain, stiffness and reduced mobility. However, the role of imaging modalities in monitoring symptomatic disease progression remains unclear. This study aimed to compare machine learning (ML) models, with and without imaging features, in predicting the two ...
The most common symptom of runner's knee is dull, aching pain in the front of the knee behind or around the kneecap. This pain worsens with weight-bearing activities when the knee is bent, such ...
Biomechanical and clinical relationships between lower back pain and knee osteoarthritis: a systematic review. Piyumi Amarasinghe, 1, 2 Surangika Wadugodapitiya, 1 and Ishanka Weerasekara ... There is a paucity of pooled information in the literature, and inconsistent findings have been reported about the alignment of the ... Knee pain scores: ...
This review will provide an essential guide for candidate variable selection in future primary care prognostic confirmatory studies.Key messagesBilateral knee pain and lower educational level were associated with persistent knee pain.Many baseline factors were associated with outcome in individual studies but not consistently between studies ...
Literature evaluating pain control and functional recovery of viscosupplementation performed at the end of arthroscopic meniscectomy or in the postoperative period after ACL reconstruction does not ... Where and how to inject the knee a systematic review. Semin Arthritis Rheum. 2013 Oct;43(2):195-203. doi: 10.1016/j.semarthrit.2013.04.010 ...
You talk about pain tolerance, you talk about how the body feels when you're behind on a hand and you're losing your chips. You've talked about being on tilt. But I see it in politics, too.
Conclusion: Most improvements were observed in: proprioception for healthy knees, gait and balance for osteoarthritic knees, and functional improvement of injured knees. This review suggests that knee sleeves can effect functional improvements to knee problems. However, further work is needed to confirm this hypothesis, due to the lack of ...
In this systematic review, we synthesized evidence on benefits and harms of XR interventions for treatment of chronic pain or to prevent development of chronic pain (if treating acute pain). We present findings by pain condition, beginning with chronic low back pain and chronic neck pain, followed by other conditions. Within each condition, we provide results separately for VR and AR ...