- Study Protocol
- Open access
- Published: 26 August 2024

Learning effect of online versus onsite education in health and medical scholarship – protocol for a cluster randomized trial
- Rie Raffing 1 ,
- Lars Konge 2 &
- Hanne Tønnesen 1
BMC Medical Education volume 24 , Article number: 927 ( 2024 ) Cite this article
123 Accesses
Metrics details
The disruption of health and medical education by the COVID-19 pandemic made educators question the effect of online setting on students’ learning, motivation, self-efficacy and preference. In light of the health care staff shortage online scalable education seemed relevant. Reviews on the effect of online medical education called for high quality RCTs, which are increasingly relevant with rapid technological development and widespread adaption of online learning in universities. The objective of this trial is to compare standardized and feasible outcomes of an online and an onsite setting of a research course regarding the efficacy for PhD students within health and medical sciences: Primarily on learning of research methodology and secondly on preference, motivation, self-efficacy on short term and academic achievements on long term. Based on the authors experience with conducting courses during the pandemic, the hypothesis is that student preferred onsite setting is different to online setting.
Cluster randomized trial with two parallel groups. Two PhD research training courses at the University of Copenhagen are randomized to online (Zoom) or onsite (The Parker Institute, Denmark) setting. Enrolled students are invited to participate in the study. Primary outcome is short term learning. Secondary outcomes are short term preference, motivation, self-efficacy, and long-term academic achievements. Standardized, reproducible and feasible outcomes will be measured by tailor made multiple choice questionnaires, evaluation survey, frequently used Intrinsic Motivation Inventory, Single Item Self-Efficacy Question, and Google Scholar publication data. Sample size is calculated to 20 clusters and courses are randomized by a computer random number generator. Statistical analyses will be performed blinded by an external statistical expert.
Primary outcome and secondary significant outcomes will be compared and contrasted with relevant literature. Limitations include geographical setting; bias include lack of blinding and strengths are robust assessment methods in a well-established conceptual framework. Generalizability to PhD education in other disciplines is high. Results of this study will both have implications for students and educators involved in research training courses in health and medical education and for the patients who ultimately benefits from this training.
Trial registration
Retrospectively registered at ClinicalTrials.gov: NCT05736627. SPIRIT guidelines are followed.
Peer Review reports
Medical education was utterly disrupted for two years by the COVID-19 pandemic. In the midst of rearranging courses and adapting to online platforms we, with lecturers and course managers around the globe, wondered what the conversion to online setting did to students’ learning, motivation and self-efficacy [ 1 , 2 , 3 ]. What the long-term consequences would be [ 4 ] and if scalable online medical education should play a greater role in the future [ 5 ] seemed relevant and appealing questions in a time when health care professionals are in demand. Our experience of performing research training during the pandemic was that although PhD students were grateful for courses being available, they found it difficult to concentrate related to the long screen hours. We sensed that most students preferred an onsite setting and perceived online courses a temporary and inferior necessity. The question is if this impacted their learning?
Since the common use of the internet in medical education, systematic reviews have sought to answer if there is a difference in learning effect when taught online compared to onsite. Although authors conclude that online learning may be equivalent to onsite in effect, they agree that studies are heterogeneous and small [ 6 , 7 ], with low quality of the evidence [ 8 , 9 ]. They therefore call for more robust and adequately powered high-quality RCTs to confirm their findings and suggest that students’ preferences in online learning should be investigated [ 7 , 8 , 9 ].
This uncovers two knowledge gaps: I) High-quality RCTs on online versus onsite learning in health and medical education and II) Studies on students’ preferences in online learning.
Recently solid RCTs have been performed on the topic of web-based theoretical learning of research methods among health professionals [ 10 , 11 ]. However, these studies are on asynchronous courses among medical or master students with short term outcomes.
This uncovers three additional knowledge gaps: III) Studies on synchronous online learning IV) among PhD students of health and medical education V) with long term measurement of outcomes.
The rapid technological development including artificial intelligence (AI) and widespread adaption as well as application of online learning forced by the pandemic, has made online learning well-established. It represents high resolution live synchronic settings which is available on a variety of platforms with integrated AI and options for interaction with and among students, chat and break out rooms, and exterior digital tools for teachers [ 12 , 13 , 14 ]. Thus, investigating online learning today may be quite different than before the pandemic. On one hand, it could seem plausible that this technological development would make a difference in favour of online learning which could not be found in previous reviews of the evidence. On the other hand, the personal face-to-face interaction during onsite learning may still be more beneficial for the learning process and combined with our experience of students finding it difficult to concentrate when online during the pandemic we hypothesize that outcomes of the onsite setting are different from the online setting.
To support a robust study, we design it as a cluster randomized trial. Moreover, we use the well-established and widely used Kirkpatrick’s conceptual framework for evaluating learning as a lens to assess our outcomes [ 15 ]. Thus, to fill the above-mentioned knowledge gaps, the objective of this trial is to compare a synchronous online and an in-person onsite setting of a research course regarding the efficacy for PhD students within the health and medical sciences:
Primarily on theoretical learning of research methodology and
Secondly on
◦ Preference, motivation, self-efficacy on short term
◦ Academic achievements on long term
Trial design
This study protocol covers synchronous online and in-person onsite setting of research courses testing the efficacy for PhD students. It is a two parallel arms cluster randomized trial (Fig. 1 ).
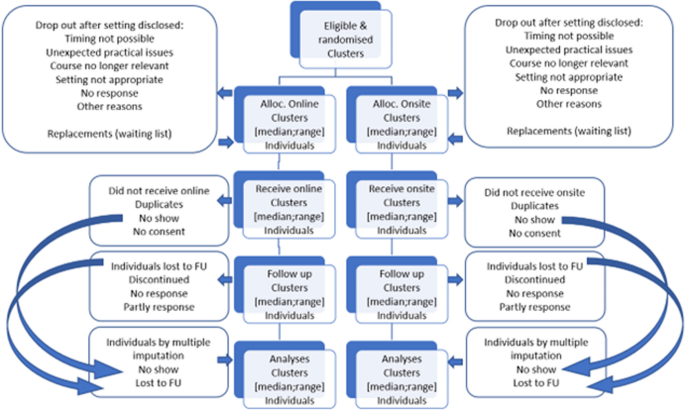
Consort flow diagram
The study measures baseline and post intervention. Baseline variables and knowledge scores are obtained at the first day of the course, post intervention measurement is obtained the last day of the course (short term) and monthly for 24 months (long term).
Randomization is stratified giving 1:1 allocation ratio of the courses. As the number of participants within each course might differ, the allocation ratio of participants in the study will not fully be equal and 1:1 balanced.
Study setting
The study site is The Parker Institute at Bispebjerg and Frederiksberg Hospital, University of Copenhagen, Denmark. From here the courses are organized and run online and onsite. The course programs and time schedules, the learning objective, the course management, the lecturers, and the delivery are identical in the two settings. The teachers use the same introductory presentations followed by training in break out groups, feed-back and discussions. For the online group, the setting is organized as meetings in the online collaboration tool Zoom® [ 16 ] using the basic available technicalities such as screen sharing, chat function for comments, and breakout rooms and other basics digital tools if preferred. The online version of the course is synchronous with live education and interaction. For the onsite group, the setting is the physical classroom at the learning facilities at the Parker Institute. Coffee and tea as well as simple sandwiches and bottles of water, which facilitate sociality, are available at the onsite setting. The participants in the online setting must get their food and drink by themselves, but online sociality is made possible by not closing down the online room during the breaks. The research methodology courses included in the study are “Practical Course in Systematic Review Technique in Clinical Research”, (see course programme in appendix 1) and “Getting started: Writing your first manuscript for publication” [ 17 ] (see course programme in appendix 2). The two courses both have 12 seats and last either three or three and a half days resulting in 2.2 and 2.6 ECTS credits, respectively. They are offered by the PhD School of the Faculty of Health and Medical Sciences, University of Copenhagen. Both courses are available and covered by the annual tuition fee for all PhD students enrolled at a Danish university.
Eligibility criteria
Inclusion criteria for participants: All PhD students enrolled on the PhD courses participate after informed consent: “Practical Course in Systematic Review Technique in Clinical Research” and “Getting started: Writing your first manuscript for publication” at the PhD School of the Faculty of Health and Medical Sciences, University of Copenhagen, Denmark.
Exclusion criteria for participants: Declining to participate and withdrawal of informed consent.
Informed consent
The PhD students at the PhD School at the Faculty of Health Sciences, University of Copenhagen participate after informed consent, taken by the daily project leader, allowing evaluation data from the course to be used after pseudo-anonymization in the project. They are informed in a welcome letter approximately three weeks prior to the course and again in the introduction the first course day. They register their consent on the first course day (Appendix 3). Declining to participate in the project does not influence their participation in the course.
Interventions
Online course settings will be compared to onsite course settings. We test if the onsite setting is different to online. Online learning is increasing but onsite learning is still the preferred educational setting in a medical context. In this case onsite learning represents “usual care”. The online course setting is meetings in Zoom using the technicalities available such as chat and breakout rooms. The onsite setting is the learning facilities, at the Parker Institute, Bispebjerg and Frederiksberg Hospital, The Capital Region, University of Copenhagen, Denmark.
The course settings are not expected to harm the participants, but should a request be made to discontinue the course or change setting this will be met, and the participant taken out of the study. Course participants are allowed to take part in relevant concomitant courses or other interventions during the trial.
Strategies to improve adherence to interventions
Course participants are motivated to complete the course irrespectively of the setting because it bears ECTS-points for their PhD education and adds to the mandatory number of ECTS-points. Thus, we expect adherence to be the same in both groups. However, we monitor their presence in the course and allocate time during class for testing the short-term outcomes ( motivation, self-efficacy, preference and learning). We encourage and, if necessary, repeatedly remind them to register with Google Scholar for our testing of the long-term outcome (academic achievement).
Outcomes are related to the Kirkpatrick model for evaluating learning (Fig. 2 ) which divides outcomes into four different levels; Reaction which includes for example motivation, self-efficacy and preferences, Learning which includes knowledge acquisition, Behaviour for practical application of skills when back at the job (not included in our outcomes), and Results for impact for end-users which includes for example academic achievements in the form of scientific articles [ 18 , 19 , 20 ].
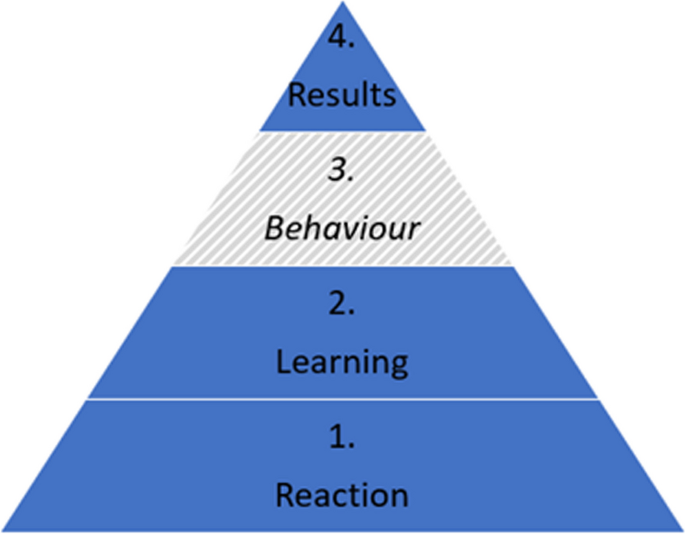
The Kirkpatrick model
Primary outcome
The primary outcome is short term learning (Kirkpatrick level 2).
Learning is assessed by a Multiple-Choice Questionnaire (MCQ) developed prior to the RCT specifically for this setting (Appendix 4). First the lecturers of the two courses were contacted and asked to provide five multiple choice questions presented as a stem with three answer options; one correct answer and two distractors. The questions should be related to core elements of their teaching under the heading of research training. The questions were set up to test the cognition of the students at the levels of "Knows" or "Knows how" according to Miller's Pyramid of Competence and not their behaviour [ 21 ]. Six of the course lecturers responded and out of this material all the questions which covered curriculum of both courses were selected. It was tested on 10 PhD students and within the lecturer group, revised after an item analysis and English language revised. The MCQ ended up containing 25 questions. The MCQ is filled in at baseline and repeated at the end of the course. The primary outcomes based on the MCQ is estimated as the score of learning calculated as number of correct answers out of 25 after the course. A decrease of points of the MCQ in the intervention groups denotes a deterioration of learning. In the MCQ the minimum score is 0 and 25 is maximum, where 19 indicates passing the course.
Furthermore, as secondary outcome, this outcome measurement will be categorized as binary outcome to determine passed/failed of the course defined by 75% (19/25) correct answers.
The learning score will be computed on group and individual level and compared regarding continued outcomes by the Mann–Whitney test comparing the learning score of the online and onsite groups. Regarding the binomial outcome of learning (passed/failed) data will be analysed by the Fisher’s exact test on an intention-to-treat basis between the online and onsite. The results will be presented as median and range and as mean and standard deviations, for possible future use in meta-analyses.
Secondary outcomes
Motivation assessment post course: Motivation level is measured by the Intrinsic Motivation Inventory (IMI) Scale [ 22 ] (Appendix 5). The IMI items were randomized by random.org on the 4th of August 2022. It contains 12 items to be assessed by the students on a 7-point Likert scale where 1 is “Not at all true”, 4 is “Somewhat true” and 7 is “Very true”. The motivation score will be computed on group and individual level and will then be tested by the Mann–Whitney of the online and onsite group.
Self-efficacy assessment post course: Self-efficacy level is measured by a single-item measure developed and validated by Williams and Smith [ 23 ] (Appendix 6). It is assessed by the students on a scale from 1–10 where 1 is “Strongly disagree” and 10 is “Strongly agree”. The self-efficacy score will be computed on group and individual level and tested by a Mann–Whitney test to compare the self-efficacy score of the online and onsite group.
Preference assessment post course: Preference is measured as part of the general course satisfaction evaluation with the question “If you had the option to choose, which form would you prefer this course to have?” with the options “onsite form” and “online form”.
Academic achievement assessment is based on 24 monthly measurements post course of number of publications, number of citations, h-index, i10-index. This data is collected through the Google Scholar Profiles [ 24 ] of the students as this database covers most scientific journals. Associations between onsite/online and long-term academic will be examined with Kaplan Meyer and log rank test with a significance level of 0.05.
Participant timeline
Enrolment for the course at the Faculty of Health Sciences, University of Copenhagen, Denmark, becomes available when it is published in the course catalogue. In the course description the course location is “To be announced”. Approximately 3–4 weeks before the course begins, the participant list is finalized, and students receive a welcome letter containing course details, including their allocation to either the online or onsite setting. On the first day of the course, oral information is provided, and participants provide informed consent, baseline variables, and base line knowledge scores.
The last day of scheduled activities the following scores are collected, knowledge, motivation, self-efficacy, setting preference, and academic achievement. To track students' long term academic achievements, follow-ups are conducted monthly for a period of 24 months, with assessments occurring within one week of the last course day (Table 1 ).
Sample size
The power calculation is based on the main outcome, theoretical learning on short term. For the sample size determination, we considered 12 available seats for participants in each course. To achieve statistical power, we aimed for 8 clusters in both online and onsite arms (in total 16 clusters) to detect an increase in learning outcome of 20% (learning outcome increase of 5 points). We considered an intraclass correlation coefficient of 0.02, a standard deviation of 10, a power of 80%, and a two-sided alpha level of 5%. The Allocation Ratio was set at 1, implying an equal number of subjects in both online and onsite group.
Considering a dropout up to 2 students per course, equivalent to 17%, we determined that a total of 112 participants would be needed. This calculation factored in 10 clusters of 12 participants per study arm, which we deemed sufficient to assess any changes in learning outcome.
The sample size was estimated using the function n4means from the R package CRTSize [ 25 ].
Recruitment
Participants are PhD students enrolled in 10 courses of “Practical Course in Systematic Review Technique in Clinical Research” and 10 courses of “Getting started: Writing your first manuscript for publication” at the PhD School of the Faculty of Health Sciences, University of Copenhagen, Denmark.
Assignment of interventions: allocation
Randomization will be performed on course-level. The courses are randomized by a computer random number generator [ 26 ]. To get a balanced randomization per year, 2 sets with 2 unique random integers in each, taken from the 1–4 range is requested.
The setting is not included in the course catalogue of the PhD School and thus allocation to online or onsite is concealed until 3–4 weeks before course commencement when a welcome letter with course information including allocation to online or onsite setting is distributed to the students. The lecturers are also informed of the course setting at this time point. If students withdraw from the course after being informed of the setting, a letter is sent to them enquiring of the reason for withdrawal and reason is recorded (Appendix 7).
The allocation sequence is generated by a computer random number generator (random.org). The participants and the lecturers sign up for the course without knowing the course setting (online or onsite) until 3–4 weeks before the course.
Assignment of interventions: blinding
Due to the nature of the study, it is not possible to blind trial participants or lecturers. The outcomes are reported by the participants directly in an online form, thus being blinded for the outcome assessor, but not for the individual participant. The data collection for the long-term follow-up regarding academic achievements is conducted without blinding. However, the external researcher analysing the data will be blinded.
Data collection and management
Data will be collected by the project leader (Table 1 ). Baseline variables and post course knowledge, motivation, and self-efficacy are self-reported through questionnaires in SurveyXact® [ 27 ]. Academic achievements are collected through Google Scholar profiles of the participants.
Given that we are using participant assessments and evaluations for research purposes, all data collection – except for monthly follow-up of academic achievements after the course – takes place either in the immediate beginning or ending of the course and therefore we expect participant retention to be high.
Data will be downloaded from SurveyXact and stored in a locked and logged drive on a computer belonging to the Capital Region of Denmark. Only the project leader has access to the data.
This project conduct is following the Danish Data Protection Agency guidelines of the European GDPR throughout the trial. Following the end of the trial, data will be stored at the Danish National Data Archive which fulfil Danish and European guidelines for data protection and management.
Statistical methods
Data is anonymized and blinded before the analyses. Analyses are performed by a researcher not otherwise involved in the inclusion or randomization, data collection or handling. All statistical tests will be testing the null hypotheses assuming the two arms of the trial being equal based on corresponding estimates. Analysis of primary outcome on short-term learning will be started once all data has been collected for all individuals in the last included course. Analyses of long-term academic achievement will be started at end of follow-up.
Baseline characteristics including both course- and individual level information will be presented. Table 2 presents the available data on baseline.
We will use multivariate analysis for identification of the most important predictors (motivation, self-efficacy, sex, educational background, and knowledge) for best effect on short and long term. The results will be presented as risk ratio (RR) with 95% confidence interval (CI). The results will be considered significant if CI does not include the value one.
All data processing and analyses were conducted using R statistical software version 4.1.0, 2021–05-18 (R Foundation for Statistical Computing, Vienna, Austria).
If possible, all analysis will be performed for “Practical Course in Systematic Review Technique in Clinical Research” and for “Getting started: Writing your first manuscript for publication” separately.
Primary analyses will be handled with the intention-to-treat approach. The analyses will include all individuals with valid data regardless of they did attend the complete course. Missing data will be handled with multiple imputation [ 28 ] .
Upon reasonable request, public assess will be granted to protocol, datasets analysed during the current study, and statistical code Table 3 .
Oversight, monitoring, and adverse events
This project is coordinated in collaboration between the WHO CC (DEN-62) at the Parker Institute, CAMES, and the PhD School at the Faculty of Health and Medical Sciences, University of Copenhagen. The project leader runs the day-to-day support of the trial. The steering committee of the trial includes principal investigators from WHO CC (DEN-62) and CAMES and the project leader and meets approximately three times a year.
Data monitoring is done on a daily basis by the project leader and controlled by an external independent researcher.
An adverse event is “a harmful and negative outcome that happens when a patient has been provided with medical care” [ 29 ]. Since this trial does not involve patients in medical care, we do not expect adverse events. If participants decline taking part in the course after receiving the information of the course setting, information on reason for declining is sought obtained. If the reason is the setting this can be considered an unintended effect. Information of unintended effects of the online setting (the intervention) will be recorded. Participants are encouraged to contact the project leader with any response to the course in general both during and after the course.
The trial description has been sent to the Scientific Ethical Committee of the Capital Region of Denmark (VEK) (21041907), which assessed it as not necessary to notify and that it could proceed without permission from VEK according to the Danish law and regulation of scientific research. The trial is registered with the Danish Data Protection Agency (Privacy) (P-2022–158). Important protocol modification will be communicated to relevant parties as well as VEK, the Joint Regional Information Security and Clinicaltrials.gov within an as short timeframe as possible.
Dissemination plans
The results (positive, negative, or inconclusive) will be disseminated in educational, scientific, and clinical fora, in international scientific peer-reviewed journals, and clinicaltrials.gov will be updated upon completion of the trial. After scientific publication, the results will be disseminated to the public by the press, social media including the website of the hospital and other organizations – as well as internationally via WHO CC (DEN-62) at the Parker Institute and WHO Europe.
All authors will fulfil the ICMJE recommendations for authorship, and RR will be first author of the articles as a part of her PhD dissertation. Contributors who do not fulfil these recommendations will be offered acknowledgement in the article.
This cluster randomized trial investigates if an onsite setting of a research course for PhD students within the health and medical sciences is different from an online setting. The outcomes measured are learning of research methodology (primary), preference, motivation, and self-efficacy (secondary) on short term and academic achievements (secondary) on long term.
The results of this study will be discussed as follows:
Discussion of primary outcome
Primary outcome will be compared and contrasted with similar studies including recent RCTs and mixed-method studies on online and onsite research methodology courses within health and medical education [ 10 , 11 , 30 ] and for inspiration outside the field [ 31 , 32 ]: Tokalic finds similar outcomes for online and onsite, Martinic finds that the web-based educational intervention improves knowledge, Cheung concludes that the evidence is insufficient to say that the two modes have different learning outcomes, Kofoed finds online setting to have negative impact on learning and Rahimi-Ardabili presents positive self-reported student knowledge. These conflicting results will be discussed in the context of the result on the learning outcome of this study. The literature may change if more relevant studies are published.
Discussion of secondary outcomes
Secondary significant outcomes are compared and contrasted with similar studies.
Limitations, generalizability, bias and strengths
It is a limitation to this study, that an onsite curriculum for a full day is delivered identically online, as this may favour the onsite course due to screen fatigue [ 33 ]. At the same time, it is also a strength that the time schedules are similar in both settings. The offer of coffee, tea, water, and a plain sandwich in the onsite course may better facilitate the possibility for socializing. Another limitation is that the study is performed in Denmark within a specific educational culture, with institutional policies and resources which might affect the outcome and limit generalization to other geographical settings. However, international students are welcome in the class.
In educational interventions it is generally difficult to blind participants and this inherent limitation also applies to this trial [ 11 ]. Thus, the participants are not blinded to their assigned intervention, and neither are the lecturers in the courses. However, the external statistical expert will be blinded when doing the analyses.
We chose to compare in-person onsite setting with a synchronous online setting. Therefore, the online setting cannot be expected to generalize to asynchronous online setting. Asynchronous delivery has in some cases showed positive results and it might be because students could go back and forth through the modules in the interface without time limit [ 11 ].
We will report on all the outcomes defined prior to conducting the study to avoid selective reporting bias.
It is a strength of the study that it seeks to report outcomes within the 1, 2 and 4 levels of the Kirkpatrick conceptual framework, and not solely on level 1. It is also a strength that the study is cluster randomized which will reduce “infections” between the two settings and has an adequate power calculated sample size and looks for a relevant educational difference of 20% between the online and onsite setting.
Perspectives with implications for practice
The results of this study may have implications for the students for which educational setting they choose. Learning and preference results has implications for lecturers, course managers and curriculum developers which setting they should plan for the health and medical education. It may also be of inspiration for teaching and training in other disciplines. From a societal perspective it also has implications because we will know the effect and preferences of online learning in case of a future lock down.
Future research could investigate academic achievements in online and onsite research training on the long run (Kirkpatrick 4); the effect of blended learning versus online or onsite (Kirkpatrick 2); lecturers’ preferences for online and onsite setting within health and medical education (Kirkpatrick 1) and resource use in synchronous and asynchronous online learning (Kirkpatrick 5).
Trial status
This trial collected pilot data from August to September 2021 and opened for inclusion in January 2022. Completion of recruitment is expected in April 2024 and long-term follow-up in April 2026. Protocol version number 1 03.06.2022 with amendments 30.11.2023.
Availability of data and materials
The project leader will have access to the final trial dataset which will be available upon reasonable request. Exception to this is the qualitative raw data that might contain information leading to personal identification.
Abbreviations
Artificial Intelligence
Copenhagen academy for medical education and simulation
Confidence interval
Coronavirus disease
European credit transfer and accumulation system
International committee of medical journal editors
Intrinsic motivation inventory
Multiple choice questionnaire
Doctor of medicine
Masters of sciences
Randomized controlled trial
Scientific ethical committee of the Capital Region of Denmark
WHO Collaborating centre for evidence-based clinical health promotion
Samara M, Algdah A, Nassar Y, Zahra SA, Halim M, Barsom RMM. How did online learning impact the academic. J Technol Sci Educ. 2023;13(3):869–85.
Article Google Scholar
Nejadghaderi SA, Khoshgoftar Z, Fazlollahi A, Nasiri MJ. Medical education during the coronavirus disease 2019 pandemic: an umbrella review. Front Med (Lausanne). 2024;11:1358084. https://doi.org/10.3389/fmed.2024.1358084 .
Madi M, Hamzeh H, Abujaber S, Nawasreh ZH. Have we failed them? Online learning self-efficacy of physiotherapy students during COVID-19 pandemic. Physiother Res Int. 2023;5:e1992. https://doi.org/10.1002/pri.1992 .
Torda A. How COVID-19 has pushed us into a medical education revolution. Intern Med J. 2020;50(9):1150–3.
Alhat S. Virtual Classroom: A Future of Education Post-COVID-19. Shanlax Int J Educ. 2020;8(4):101–4.
Cook DA, Levinson AJ, Garside S, Dupras DM, Erwin PJ, Montori VM. Internet-based learning in the health professions: A meta-analysis. JAMA. 2008;300(10):1181–96. https://doi.org/10.1001/jama.300.10.1181 .
Pei L, Wu H. Does online learning work better than offline learning in undergraduate medical education? A systematic review and meta-analysis. Med Educ Online. 2019;24(1):1666538. https://doi.org/10.1080/10872981.2019.1666538 .
Richmond H, Copsey B, Hall AM, Davies D, Lamb SE. A systematic review and meta-analysis of online versus alternative methods for training licensed health care professionals to deliver clinical interventions. BMC Med Educ. 2017;17(1):227. https://doi.org/10.1186/s12909-017-1047-4 .
George PP, Zhabenko O, Kyaw BM, Antoniou P, Posadzki P, Saxena N, Semwal M, Tudor Car L, Zary N, Lockwood C, Car J. Online Digital Education for Postregistration Training of Medical Doctors: Systematic Review by the Digital Health Education Collaboration. J Med Internet Res. 2019;21(2):e13269. https://doi.org/10.2196/13269 .
Tokalić R, Poklepović Peričić T, Marušić A. Similar Outcomes of Web-Based and Face-to-Face Training of the GRADE Approach for the Certainty of Evidence: Randomized Controlled Trial. J Med Internet Res. 2023;25:e43928. https://doi.org/10.2196/43928 .
Krnic Martinic M, Čivljak M, Marušić A, Sapunar D, Poklepović Peričić T, Buljan I, et al. Web-Based Educational Intervention to Improve Knowledge of Systematic Reviews Among Health Science Professionals: Randomized Controlled Trial. J Med Internet Res. 2022;24(8): e37000.
https://www.mentimeter.com/ . Accessed 4 Dec 2023.
https://www.sendsteps.com/en/ . Accessed 4 Dec 2023.
https://da.padlet.com/ . Accessed 4 Dec 2023.
Zackoff MW, Real FJ, Abramson EL, Li STT, Klein MD, Gusic ME. Enhancing Educational Scholarship Through Conceptual Frameworks: A Challenge and Roadmap for Medical Educators. Acad Pediatr. 2019;19(2):135–41. https://doi.org/10.1016/j.acap.2018.08.003 .
https://zoom.us/ . Accessed 20 Aug 2024.
Raffing R, Larsen S, Konge L, Tønnesen H. From Targeted Needs Assessment to Course Ready for Implementation-A Model for Curriculum Development and the Course Results. Int J Environ Res Public Health. 2023;20(3):2529. https://doi.org/10.3390/ijerph20032529 .
https://www.kirkpatrickpartners.com/the-kirkpatrick-model/ . Accessed 12 Dec 2023.
Smidt A, Balandin S, Sigafoos J, Reed VA. The Kirkpatrick model: A useful tool for evaluating training outcomes. J Intellect Dev Disabil. 2009;34(3):266–74.
Campbell K, Taylor V, Douglas S. Effectiveness of online cancer education for nurses and allied health professionals; a systematic review using kirkpatrick evaluation framework. J Cancer Educ. 2019;34(2):339–56.
Miller GE. The assessment of clinical skills/competence/performance. Acad Med. 1990;65(9 Suppl):S63–7.
Ryan RM, Deci EL. Self-Determination Theory and the Facilitation of Intrinsic Motivation, Social Development, and Well-Being. Am Psychol. 2000;55(1):68–78. https://doi.org/10.1037//0003-066X.55.1.68 .
Williams GM, Smith AP. Using single-item measures to examine the relationships between work, personality, and well-being in the workplace. Psychology. 2016;07(06):753–67.
https://scholar.google.com/intl/en/scholar/citations.html . Accessed 4 Dec 2023.
Rotondi MA. CRTSize: sample size estimation functions for cluster randomized trials. R package version 1.0. 2015. Available from: https://cran.r-project.org/package=CRTSize .
Random.org. Available from: https://www.random.org/
https://rambollxact.dk/surveyxact . Accessed 4 Dec 2023.
Sterne JAC, White IR, Carlin JB, Spratt M, Royston P, Kenward MG, et al. Multiple imputation for missing data in epidemiological and clinical research: Potential and pitfalls. BMJ (Online). 2009;339:157–60.
Google Scholar
Skelly C, Cassagnol M, Munakomi S. Adverse Events. StatPearls Treasure Island: StatPearls Publishing. 2023. Available from: https://www.ncbi.nlm.nih.gov/books/NBK558963/ .
Rahimi-Ardabili H, Spooner C, Harris MF, Magin P, Tam CWM, Liaw ST, et al. Online training in evidence-based medicine and research methods for GP registrars: a mixed-methods evaluation of engagement and impact. BMC Med Educ. 2021;21(1):1–14. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8439372/pdf/12909_2021_Article_2916.pdf .
Cheung YYH, Lam KF, Zhang H, Kwan CW, Wat KP, Zhang Z, et al. A randomized controlled experiment for comparing face-to-face and online teaching during COVID-19 pandemic. Front Educ. 2023;8. https://doi.org/10.3389/feduc.2023.1160430 .
Kofoed M, Gebhart L, Gilmore D, Moschitto R. Zooming to Class?: Experimental Evidence on College Students' Online Learning During Covid-19. SSRN Electron J. 2021;IZA Discussion Paper No. 14356.
Mutlu Aİ, Yüksel M. Listening effort, fatigue, and streamed voice quality during online university courses. Logop Phoniatr Vocol :1–8. Available from: https://doi.org/10.1080/14015439.2024.2317789
Download references
Acknowledgements
We thank the students who make their evaluations available for this trial and MSc (Public Health) Mie Sylow Liljendahl for statistical support.
Open access funding provided by Copenhagen University The Parker Institute, which hosts the WHO CC (DEN-62), receives a core grant from the Oak Foundation (OCAY-18–774-OFIL). The Oak Foundation had no role in the design of the study or in the collection, analysis, and interpretation of the data or in writing the manuscript.
Author information
Authors and affiliations.
WHO Collaborating Centre (DEN-62), Clinical Health Promotion Centre, The Parker Institute, Bispebjerg & Frederiksberg Hospital, University of Copenhagen, Copenhagen, 2400, Denmark
Rie Raffing & Hanne Tønnesen
Copenhagen Academy for Medical Education and Simulation (CAMES), Centre for HR and Education, The Capital Region of Denmark, Copenhagen, 2100, Denmark
You can also search for this author in PubMed Google Scholar
Contributions
RR, LK and HT have made substantial contributions to the conception and design of the work; RR to the acquisition of data, and RR, LK and HT to the interpretation of data; RR has drafted the work and RR, LK, and HT have substantively revised it AND approved the submitted version AND agreed to be personally accountable for their own contributions as well as ensuring that any questions which relates to the accuracy or integrity of the work are adequately investigated, resolved and documented.
Corresponding author
Correspondence to Rie Raffing .
Ethics declarations
Ethics approval and consent to participate.
The Danish National Committee on Health Research Ethics has assessed the study Journal-nr.:21041907 (Date: 21–09-2021) without objections or comments. The study has been approved by The Danish Data Protection Agency Journal-nr.: P-2022–158 (Date: 04.05.2022).
All PhD students participate after informed consent. They can withdraw from the study at any time without explanations or consequences for their education. They will be offered information of the results at study completion. There are no risks for the course participants as the measurements in the course follow routine procedure and they are not affected by the follow up in Google Scholar. However, the 15 min of filling in the forms may be considered inconvenient.
The project will follow the GDPR and the Joint Regional Information Security Policy. Names and ID numbers are stored on a secure and logged server at the Capital Region Denmark to avoid risk of data leak. All outcomes are part of the routine evaluation at the courses, except the follow up for academic achievement by publications and related indexes. However, the publications are publicly available per se.
Competing interests
The authors declare no competing interests
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary material 1., supplementary material 2., supplementary material 3., supplementary material 4., supplementary material 5., supplementary material 6., supplementary material 7., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Raffing, R., Konge, L. & Tønnesen, H. Learning effect of online versus onsite education in health and medical scholarship – protocol for a cluster randomized trial. BMC Med Educ 24 , 927 (2024). https://doi.org/10.1186/s12909-024-05915-z
Download citation
Received : 25 March 2024
Accepted : 14 August 2024
Published : 26 August 2024
DOI : https://doi.org/10.1186/s12909-024-05915-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Self-efficacy
- Achievements
- Health and Medical education
BMC Medical Education
ISSN: 1472-6920
- General enquiries: [email protected]
- Alzheimer's disease & dementia
- Arthritis & Rheumatism
- Attention deficit disorders
- Autism spectrum disorders
- Biomedical technology
- Diseases, Conditions, Syndromes
- Endocrinology & Metabolism
- Gastroenterology
- Gerontology & Geriatrics
- Health informatics
- Inflammatory disorders
- Medical economics
- Medical research
- Medications
- Neuroscience
- Obstetrics & gynaecology
- Oncology & Cancer
- Ophthalmology
- Overweight & Obesity
- Parkinson's & Movement disorders
- Psychology & Psychiatry
- Radiology & Imaging
- Sleep disorders
- Sports medicine & Kinesiology
- Vaccination
- Breast cancer
- Cardiovascular disease
- Chronic obstructive pulmonary disease
- Colon cancer
- Coronary artery disease
- Heart attack
- Heart disease
- High blood pressure
- Kidney disease
- Lung cancer
- Multiple sclerosis
- Myocardial infarction
- Ovarian cancer
- Post traumatic stress disorder
- Rheumatoid arthritis
- Schizophrenia
- Skin cancer
- Type 2 diabetes
- Full List »
share this!
August 29, 2024
This article has been reviewed according to Science X's editorial process and policies . Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
trusted source
Interprofessional training in health sciences education has a lasting impact on practice, study shows
by University of Southern California

Geriatrics experts have long known that collaboration is key to delivering quality, patient-centered care to older adults.
That's why USC's Interprofessional Education and Collaboration for Geriatrics (IECG) trains up to 150 students annually from seven health professions to teach the importance of teamwork in meeting the complex needs of the elderly.
Now, a study published in the Journal of Interprofessional Care highlights the long-term impact of IECG on USC health sciences graduates.
Researchers surveyed graduates one to three years after completing IECG to assess how the program influenced their practice. The findings were significant: 81% of the graduates worked on interprofessional teams, 80% reported that IECG had a major impact on their practice, and all confirmed they regularly used the assessment tools learned in the program.
"We've really seen over the last decade that this program consistently improves health profession graduate students' interprofessional knowledge and attitudes and also helps them prepare them for collaborative practice ," said Dawn Joosten-Hagye, first author on the study and professor of social work at the USC Suzanne Dworak-Peck School of Social Work.
"This is one of the first studies to actually look at how students sustain their interprofessional education training."
The program was initiated 14 years ago by study co-author Jo Marie Reilly, a professor of clinical family medicine at the Keck School of Medicine of USC, who saw the need for an innovative training model focused on the complex health care needs of older adults.
The collaborative effort has since included students from dentistry, medicine, occupational therapy , pharmacy, physical therapy , gerontology, psychology, and social work.
Looking forward, the study's authors believe the IECG model could be adapted to address the needs of other populations with complex health care needs, such as people with disabilities, cancer patients, and children.
Explore further
Feedback to editors

Machine learning predicts which patients will continue taking opioids after hand surgery
16 minutes ago

Study describes a new molecular pathway involved in the control of reproduction
37 minutes ago

Machine learning helps identify rheumatoid arthritis subtypes

Immune protection against tuberculosis reinfection driven by cells that dampen lung inflammation, shows study

Girls with mental health conditions have lower HPV vaccination coverage

Mankai plant found to reduce post-meal sugar levels in diabetics
2 hours ago

Unique chicken line advances research on autoimmune disease that affects humans

Navigating the digestive tract: Study offers first detailed map of the small intestine

Dental researchers develop innovative sleep apnea model to find answers to chronic pain

Smart mask monitors breath for signs of health
Related stories.

Brief teacher training found to better prepare medical students for patient education and communication
Dec 15, 2023

Pipeline program at medical school boosts primary care residency matches and representation
Aug 8, 2023

Study: Emergency department visits more likely for dementia patients with interprofessional primary care team
Nov 29, 2022

Students in health enrichment programs benefit from early team-based exposure
Oct 25, 2018

Health professionals work in teams: their training should prepare them
Jul 6, 2021

Study suggests interprofessional team training could prove effective in alcohol use disorder prevention and treatment
Mar 21, 2023
Recommended for you

Clinical trial assesses the efficacy of suvorexant in reducing delirium in older adults
6 hours ago

In-person contact linked with lower levels of loneliness in older adults
Aug 28, 2024

Low-dose THC reverses brain aging and enhances cognition in mice, research suggests
Aug 21, 2024

Marriage strongly associated with optimal health and well-being in men as they age

Study finds potential link between DNA markers and aging process
Aug 19, 2024

Cleaning up the aging brain: Scientists restore brain's waste removal system
Aug 15, 2024
Let us know if there is a problem with our content
Use this form if you have come across a typo, inaccuracy or would like to send an edit request for the content on this page. For general inquiries, please use our contact form . For general feedback, use the public comments section below (please adhere to guidelines ).
Please select the most appropriate category to facilitate processing of your request
Thank you for taking time to provide your feedback to the editors.
Your feedback is important to us. However, we do not guarantee individual replies due to the high volume of messages.
E-mail the story
Your email address is used only to let the recipient know who sent the email. Neither your address nor the recipient's address will be used for any other purpose. The information you enter will appear in your e-mail message and is not retained by Medical Xpress in any form.
Newsletter sign up
Get weekly and/or daily updates delivered to your inbox. You can unsubscribe at any time and we'll never share your details to third parties.
More information Privacy policy
Donate and enjoy an ad-free experience
We keep our content available to everyone. Consider supporting Science X's mission by getting a premium account.
E-mail newsletter
- Open access
- Published: 28 August 2024
A qualitative study identifying implementation strategies using the i-PARIHS framework to increase access to pre-exposure prophylaxis at federally qualified health centers in Mississippi
- Trisha Arnold ORCID: orcid.org/0000-0003-3556-5717 1 , 2 ,
- Laura Whiteley 2 ,
- Kayla K. Giorlando 1 ,
- Andrew P. Barnett 1 , 2 ,
- Ariana M. Albanese 2 ,
- Avery Leigland 1 ,
- Courtney Sims-Gomillia 3 ,
- A. Rani Elwy 2 , 5 ,
- Precious Patrick Edet 3 ,
- Demetra M. Lewis 4 ,
- James B. Brock 4 &
- Larry K. Brown 1 , 2
Implementation Science Communications volume 5 , Article number: 92 ( 2024 ) Cite this article
3 Altmetric
Metrics details
Mississippi (MS) experiences disproportionally high rates of new HIV infections and limited availability of pre-exposure prophylaxis (PrEP). Federally Qualified Health Centers (FQHCs) are poised to increase access to PrEP. However, little is known about the implementation strategies needed to successfully integrate PrEP services into FQHCs in MS.
The study had two objectives: identify barriers and facilitators to PrEP use and to develop tailored implementation strategies for FQHCs.
Semi-structured interviews were conducted with 19 staff and 17 PrEP-eligible patients in MS FQHCs between April 2021 and March 2022. The interview was guided by the integrated-Promoting Action on Research Implementation in Health Services (i-PARIHS) framework which covered PrEP facilitators and barriers. Interviews were coded according to the i-PARIHS domains of context, innovation, and recipients, followed by thematic analysis of these codes. Identified implementation strategies were presented to 9 FQHC staff for feedback.
Data suggested that PrEP use at FQHCs is influenced by patient and clinic staff knowledge with higher levels of knowledge reflecting more PrEP use. Perceived side effects are the most significant barrier to PrEP use for patients, but participants also identified several other barriers including low HIV risk perception and untrained providers. Despite these barriers, patients also expressed a strong motivation to protect themselves, their partners, and their communities from HIV. Implementation strategies included education and provider training which were perceived as acceptable and appropriate.
Conclusions
Though patients are motivated to increase protection against HIV, multiple barriers threaten uptake of PrEP within FQHCs in MS. Educating patients and providers, as well as training providers, are promising implementation strategies to overcome these barriers.
Peer Review reports
Contributions to the literature
We propose utilizing Federally Qualified Health Centers (FQHCs) to increase pre-exposure prophylaxis (PrEP) use among people living in Mississippi.
Little is currently known about how to distribute PrEP at FQHCs.
We comprehensively describe the barriers and facilitators to implementing PrEP at FQHCs.
Utilizing effective implementation strategies of PrEP, such as education and provider training at FQHCs, may increase PrEP use and decrease new HIV infections.
Introduction
The HIV outbreak in Mississippi (MS) is among the most critical in the United States (U.S.). It is distinguished by significant inequalities, a considerable prevalence of HIV in remote areas, and low levels of HIV medical care participation and virologic suppression [ 1 ]. MS has consistently ranked among the states with the highest HIV rates in the U.S. This includes being the 6th highest in new HIV diagnoses [ 2 ] and 2nd highest in HIV diagnoses among men who have sex with men (MSM) compared to other states [ 2 , 3 , 4 ]. Throughout MS, the HIV epidemic disproportionately affects racial and ethnic minority groups, particularly among Black individuals. A spatial epidemiology and statistical modeling study completed in MS identified HIV hot spots in the MS Delta region, Southern MS, and in greater Jackson, including surrounding rural counties [ 5 ]. Black race and urban location were positively associated with HIV clusters. This disparity is often driven by the complex interplay of social, economic, and structural factors, including poverty, limited access to healthcare, and stigma [ 5 ].
Pre-exposure prophylaxis (PrEP) has gained significant recognition due to its safety and effectiveness in preventing HIV transmission when taken as prescribed [ 6 , 7 , 8 , 9 ]. However, despite the progression in PrEP and its accessibility, its uptake has been slow among individuals at high risk of contracting HIV, particularly in Southern states such as MS [ 10 , 11 , 12 , 13 , 14 ]. According to the CDC [ 5 ], “4,530 Mississippians at high risk for HIV could potentially benefit from PrEP, but only 927 were prescribed PrEP.” Several barriers hinder PrEP use in MS including limited access to healthcare, cost, stigma, and medical mistrust [ 15 , 16 , 17 ].
Federally qualified health centers (FQHCs) are primary healthcare organizations that are community-based and patient-directed, serve geographically and demographically diverse patients with limited access to medical care, and provide care regardless of a patient’s ability to pay [ 18 ]. FQHCs in these areas exhibit reluctance in prescribing or counseling patients regarding PrEP, primarily because they lack the required training and expertise [ 19 , 20 , 21 ]. Physicians in academic medical centers are more likely to prescribe PrEP compared to those in community settings [ 22 ]. Furthermore, providers at FQHCs may exhibit less familiarity with conducting HIV risk assessments, express concerns regarding potential side effects of PrEP, and have mixed feelings about prescribing it [ 23 , 24 ]. Task shifting might also be needed as some FQHCs may lack sufficient physician support to manage all aspects of PrEP care. Tailored strategies and approaches are necessary for FQHCs to effectively navigate the many challenges that threaten their patients’ access to and utilization of PrEP.
The main objectives of this study were to identify the barriers and facilitators to PrEP use and to develop tailored implementation strategies for FQHCs providing PrEP. To service these objectives, this study had three specific aims. Aim 1 involved conducting a qualitative formative evaluation guided by the integrated-Promoting Action on Research Implementation in Health Services (i-PARIHS) framework- with FQHC staff and PrEP-eligible patients across three FQHCs in MS [ 25 ]. Interviews covered each of the three i-PARIHS domains: context, innovation, and recipients. These interviews sought to identify barriers and facilitators to implementing PrEP. Aim 2 involved using interview data to select and tailor implementation strategies from the Expert Recommendations for Implementing Change (ERIC) project [ 26 ] (e.g., provider training) and methods (e.g., telemedicine, PrEP navigators) for the FQHCs. Aim 3 was to member-check the selected implementation strategies and further refine these if necessary. Data from all three aims are presented below. The standards for reporting qualitative research (SRQR) checklist was used to improve the transparency of reporting this qualitative study [ 27 ].
Formative evaluation interviews
Interviews were conducted with 19 staff and 17 PrEP-eligible patients from three FQHCs in Jackson, Canton, and Clarksdale, Mississippi. Staff were eligible to participate if they were English-speaking and employed by their organization for at least a year. Eligibility criteria for patients included: 1) English speaking, 2) aged 18 years or older, 3) a present or prior patient at the FQHC, 4) HIV negative, and 5) currently taking PrEP or reported any one of the following factors that may indicate an increased risk for HIV: in the past year, having unprotected sex with more than one person with unknown (or positive) HIV status, testing positive for a sexually transmitted infection (STI) (syphilis, gonorrhea, or chlamydia), or using injection drugs.
Data collection
The institutional review boards of the affiliated hospitals approved this study prior to data collection. An employee at each FQHC acted as a study contact and assisted with recruitment. The contacts advertised the study through word-of-mouth to coworkers and relayed the contact information of those interested to research staff. Patients were informed about the study from FQHC employees and flyers while visiting the FQHC for HIV testing. Those interested filled out consent-to-contact forms, which were securely and electronically sent to research staff. Potential participants were then contacted by a research assistant, screened for eligibility, electronically consented via DocuSign (a HIPAA-compliant signature capturing program), then scheduled for an interview. Interviews occurred remotely over Zoom, a HIPAA-compliant, video conferencing platform. Interviews were conducted until data saturation was reached. In addition to the interview, all participants were asked to complete a short demographics survey via REDCap, a HIPAA-compliant, online, data collection tool. Each participant received a $100 gift card for their time.
The i-PARIHS framework guided interview content and was used to create a semi-structured interview guide [ 28 ]. Within the i-PARIHS framework’s elements, the interview guide content included facilitators and barriers to PrEP use at the FQHC: 1) the innovation, (PrEP), such as its degree of fit with existing practices and values at FQHCs; 2) the recipients (individuals presenting to FQHCs), such as their PrEP awareness, barriers to receiving PrEP such as motivation, resources, support, and personal PrEP experiences; and 3) the context of the setting (FQHCs), such as clinic staff PrEP awareness, barriers providing PrEP services, and recommendations regarding PrEP care. Interviews specifically asked about the use of telemedicine, various methods for expanding PrEP knowledge for both patients and providers (e.g., social media, advertisements, community events/seminars), and location of services (e.g., mobile clinics, gyms, annual health checkups, health fairs). Staff and patients were asked the same interview questions. Data were reviewed and analyzed iteratively throughout data collection, and interview guides were adapted as needed.
Data analysis
Interviews were all audio-recorded, then transcribed by an outside, HIPAA-certified transcription company. Transcriptions were reviewed for accuracy by the research staff who conducted the interviews.
Seven members of the research team (TA, LW, KKG, AB, CSG, AL, LKB) independently coded the transcripts using an a priori coding schedule that was developed using the i-PARIHS and previous studies [ 15 , 16 , 17 ]. All research team members were trained in qualitative methods prior to beginning the coding process. The coding scheme covered: patient PrEP awareness, clinic staff PrEP awareness, barriers to receiving PrEP services, barriers to providing PrEP services, and motivation to take PrEP. Each coder read each line of text and identified if any of the codes from the a priori coding framework were potentially at play in each piece of text. Double coding was permitted when applicable. New codes were created and defined when a piece of text from transcripts represented a new important idea. Codes were categorized according to alignment with i-PARIHS constructs. To ensure intercoder reliability, the first 50% of the interviews were coded by two researchers. Team meetings were regularly held to discuss coding discrepancies (to reach a consensus). Coded data were organized using NVivo software (Version 12). Data were deductively analyzed using reflexive thematic analysis, a six-step process for analyzing and reporting qualitative data, to determine themes relevant to selecting appropriate implementation strategies to increase PrEP use at FQHCs in MS [ 29 ]. The resulting thematic categories were used to select ERIC implementation strategies [ 26 ]. Elements for each strategy were then operationalized and the mechanism of change for each strategy was hypothesized [ 30 , 31 ]. Mechanisms define how an implementation strategy will have an effect [ 30 , 31 ]. We used the identified determinants to hypothesize the mechanism of change for each strategy.
Member checking focus groups
Member checking is when the data or results are presented back to the participants, who provide feedback [ 32 ] to check for accuracy [ 33 ] and improve the validity of the data [ 34 ]. This process helps reduce the possibility of misrepresentation of the data [ 35 ]. Member checking was completed with clinic staff rather than patients because the focus was on identifying strategies to implement PrEP in the FQHCs.
Two focus groups were conducted with nine staff from the three FQHCs in MS. Eligibility criteria were the same as above. A combination of previously interviewed staff and non-interviewed staff were recruited. Staff members were a mix of medical (e.g., nurses, patient navigators, social workers) and non-medical (e.g., administrative assistant, branding officer) personnel. Focus group one had six participants and focus group two had three participants. The goal was for focus group participants to comprise half of staff members who had previously been interviewed and half of non-interviewed staff.
Participants were recruited and compensated via the same methods as above. All participants electronically consented via DocuSign, and then were scheduled for a focus group. Focus groups occurred remotely over Zoom. Focus groups were conducted until data saturation was reached and no new information surfaced. The goal of the focus groups was to member-check results from the interviews and assess the feasibility and acceptability of selected implementation strategies. PowerPoint slides with the results and implementation strategies written in lay terms were shared with the participants, which is a suggested technique to use in member checking [ 33 ]. Participants were asked to provide feedback on each slide.
Focus groups were all audio-recorded, then transcribed. Transcriptions were reviewed for accuracy by the research staff who completed focus groups. Findings from the focus groups were synthesized using rapid qualitative analyses [ 36 , 37 ]. Facilitators (TA, PPE) both took notes during the focus groups of the primary findings. Notes were then compared during team meetings and results were finalized. Results obtained from previous findings of the interviews and i-PARIHS framework were presented. To ensure the reliability of results, an additional team member (KKG) read the transcripts to verify the primary findings and selected supportive quotes for each theme. Team meetings were regularly held to discuss the results.
Thirty-six semi-structured interviews in HIV hot spots were completed between April 2021 and March 2022. Among the 19 FQHC staff, most staff members had several years of experience working with those at risk for HIV. Staff members were a mix of medical (e.g., doctors, nurses, CNAs, social workers) and non-medical (e.g., receptionists, case managers) personnel. Table 1 provides the demographic characteristics for the 19 FQHC clinic staff and 17 FQHC patients.
Table 2 provides a detailed description of the findings within each category: PrEP knowledge, PrEP barriers, and PrEP motivation. Themes are described in detail, with representative quotes, below. Implementation determinants are specific factors that influence implementation outcomes and can be barriers or facilitators. Table 3 highlights which implementation determinants can increase ( +) or decrease (-) the implementation of PrEP at FQHCs in MS. Each determinant, mapped to its corresponding i-PARIHS construct, is discussed in more detail below. There were no significant differences in responses across the three FQHCs.
PrEP knowledge
Patient prep awareness (i-parihs: recipients).
Most patients had heard of PrEP and were somewhat familiar with the medication. One patient described her knowledge of PrEP as follows, “I know that PrEP is I guess a program that helps people who are high-risk with sexual behaviors and that doesn't have HIV, but they're at high-risk.”- Patient, Age 32, Female, Not on PrEP. However, many lacked knowledge of who may benefit from PrEP, where to receive a prescription, the different medications used for PrEP, and the efficacy of PrEP. Below is a comment made by a patient listing what she would need to know to consider taking PrEP. “I would need to know the price. I would need to know the side effects. I need to know the percentage, like, is it 100 or 90 percent effective.”— Patient, Age Unknown, Female, Not on PrEP. Patients reported learning about PrEP via television and social media commercials, medical providers, and their social networks. One patient reported learning about PrEP from her cousin. “The only person I heard it [PrEP] from was my cousin, and she talks about it all the time, givin’ us advice and lettin’ us know that it’s a good thing.”— Patient, Age Unknown, Female, Not on PrEP.
Clinic Staff PrEP Awareness (i-PARIHS: Context)
Training in who may benefit from PrEP and how to prescribe PrEP varied among clinic staff at different FQHCs. Not all clinics offered formal PrEP education for employees; however, most knew that PrEP is a tool used for HIV prevention. Staff reported learning about PrEP via different speakers and meetings. A clinic staff member reported learning about PrEP during quarterly meetings. “Well, sometimes when we have different staff meetings, we have them quarterly, and we discuss PrEP. Throughout those meetings, they tell us a little bit of information about it, so that's how I know about PrEP.” – Staff, Dental Assistant, Female. Some FQHC staff members reported having very little knowledge of PrEP. One staff member shared that she knew only the “bare minimum” about PrEP, stating,
“I probably know the bare minimum about PrEP. I know a little about it [PrEP] as far as if taken the correct way, it can prevent you from gettin’ HIV. I know it [PrEP] doesn’t prevent against STDs but I know it’s a prevention method for HIV and just a healthier lifestyle.” –Staff, Accountant, Female
A few of the organizations had PrEP navigators to which providers refer patients. These providers were well informed on who to screen for PrEP eligibility and the process for helping the patient obtain a PrEP prescription. One clinic staff member highlighted how providers must be willing to be trained in the process of prescribing PrEP and make time for patients who may benefit. Specifically, she said,
“I have been trained [for PrEP/HIV care]. It just depends on if that’s something that you’re willing to do, they can train on what labs and stuff to order ’cause it’s a whole lot of labs. But usually, I try to do it. At least for everybody that’s high-risk.” – Staff, OB/GYN Nurse Practitioner, Female
Another clinic staff member reported learning about PrEP while observing another staff member being training in PrEP procedures.
“Well, they kinda explained to me what it [PrEP] is, but I was in training with the actual PrEP person, so it was kinda more so for his training. I know what PrEP is. I know the medications and I know he does a patient assistance program. If my patients have partners who are not HIV positive and wanna continue to be HIV negative, I can refer 'em.” – Staff, Administrative Assistant, Female
PrEP barriers
Barriers receiving prep services (i-parihs: recipients, innovation).
Several barriers to receiving PrEP services were identified in both patient and clinic staff interviews. There was a strong concern for the side effects of PrEP. One patient heard that PrEP could cause weight gain and nightmares, “I’m afraid of gaining weight. I’ve heard that actual HIV medication, a lotta people have nightmares or bad dreams.” - Patient, Age 30, Female, Not on PrEP. Another patient was concerned about perceived general side effects that many medications have. “Probably just the [potential] side effects. You know, most of the pills have allergic reactions and side effects, dizziness, seizures, you know.” - Patient, Age 30, Female, Not on PrEP.
The burden of remembering to take a daily pill was also mentioned as a barrier to PrEP use. One female patient explained how PrEP is something she is interested in taking; however, she would be unable to take a daily medication.
“I’m in school now and not used to takin’ a medication every day. I was takin’ a birth control pill, but now take a shot. That was one of the main reasons that I didn’t start PrEP cause they did tell me I could get it that day. So like I wanna be in the mind state to where I’m able to mentally, in my head, take a pill every day. PrEP is somethin’ that I wanna do.” - Patient, Age Unknown, Female, Not on PrEP
Stigma and confidentiality were also barriers to PrEP use at FQHCs. One staff member highlighted how in small communities it is difficult to go to a clinic where employees know you personally. Saying,
“If somebody knows you’re going to talk to this specific person, they know what you’re goin’ back there for, and that could cause you to be a little hesitant in coming. So there’s always gonna be a little hesitancy or mistrust, especially in a small community. Everybody knows everybody. The people that you’re gonna see goes to church with you.” – Staff, Accountant, Female
Some patients had a low perceived risk of HIV and felt PrEP may be an unnecessary addition to their routine. One patient shared that if she perceived she was at risk for HIV, then she would be more interested in taking PrEP, “If it ever came up to the point where I would need it [PrEP], then yes, I would want to know more about it [PrEP].”— Patient, Age Unknown, Female, Not on PrEP.
Some participants expressed difficulty initiating or staying on PrEP because of associated costs, transportation and/or scheduling barriers. A staff member explained how transportation may be available in the city but not available in more rural areas,
“I guess it all depends on the person and where they are. In a city it might take a while, but at least they have the transportation compared to someone that lives in a rural area where transportation might be an issue.” - Staff, Director of Nurses, Female
Childcare during appointments was also mentioned as a barrier, “It looks like here a lot of people don't have transportation or reliable transportation and another thing I don't have anybody to watch my kids right now. —Staff, Patient Navigator, Female.
Barriers Providing PrEP Services (i-PARIHS: Context)
Barriers to providing PrEP services were also identified. Many providers are still not trained in PrEP procedures nor feel comfortable discussing or prescribing PrEP to their patients. One patient shared an experience of going to a provider who was PrEP-uninformed and assumed his medication was to treat HIV,
“Once I told her about it [PrEP], she [clinic provider] literally right in front of me, Googled it [PrEP], and then she was Googlin’ the medication, Descovy. I went to get a lab work, and she came back and was like, “Is this for treatment?” I was like, “Why would you automatically think it’s for treatment?” I literally told her and the nurse, “I would never come here if I lived here.” - Patient, Age 50, Male, Taking PrEP
Also, it was reported that there is not enough variety in the kind of providers who offer PrEP (e.g., OB/GYN, primary care). Many providers such as OB/GYNs could serve as a great way to reach individuals who may benefit from PrEP; however, patients reported a lack of PrEP being discussed in annual visits. “My previous ones (OB/GYN), they’ve talked about birth control and every other method and they asked me if I wanted to get tested for HIV and any STIs, but the conversation never came up about PrEP.” -Patient, Age Unknown, Female, Not on PrEP.
PrEP motivation
Motivation to take prep (i-parihs: recipients).
Participants mentioned several motivators that enhanced patient willingness to use PrEP. Many patients reported being motivated to use PrEP to protect themselves and their partners from HIV. Additionally, participants reported wanting to take PrEP to help their community. One patient reported being motivated by both his sexuality and the rates of HIV in his area, saying, “I mean, I'm bisexual. So, you know, anyway I can protect myself. You know, it's just bein' that the HIV number has risen. You know, that's scary. So just being, in, an area with higher incidents of cases.”— Patient, Age Unknown, Male, Not on PrEP . Some participants reported that experiencing an HIV scare also motivated them to consider using PrEP. One patient acknowledged his behaviors that put him at risk and indicated that this increased his willingness to take PrEP, “I was havin' a problem with, you know, uh, bein' promiscuous. You know? So it [PrEP] was, uh, something that I would think, would help me, if I wasn't gonna change the way I was, uh, actin' sexually.”— Patient, Age Unknown, Male, Taking PrEP .
Table 3 outlines the implementation strategies identified from themes from the interview and focus group data. Below we recognize the barriers and determinants to PrEP uptake for patients attending FQHCs in MS by each i-PARIHS construct (innovation, recipient, context) [ 28 ]. Based on the data, we mapped the determinants to specific strategies from the ERIC project [ 26 ] and hypothesized the mechanism of change for each strategy [ 30 , 31 ].
Two focus groups were conducted with nine staff from threeFQHCs in MS. There were six participants in the 1st focus group and three in the 2nd. Staff members were a mix of medical (e.g., nurses, patient navigators, social workers) and non-medical (e.g., administrative assistant, branding officer) personnel. Table 4 provides the demographic characteristics for the FQHC focus group participants.
Staff participating in the focus groups generally agreed that the strategies identified via the interviews were appropriate and acceptable. Focus group content helped to further clarify some of the selected strategies. Below we highlight findings by each strategy domain.
PrEP information dissemination
Participants specified that awareness of HIV is lower, and stigma related to PrEP is higher in rural areas. One participant specifically said,
“There is some awareness but needs to be more awareness, especially to rural areas here in Mississippi. If you live in the major metropolitan areas there is a lot of information but when we start looking at the rural communities, there is not a lot.” – Staff, Branding Officer, Male
Participants strongly agreed that many patients don’t realize they may benefit from PrEP and that more inclusive advertisements are needed. A nurse specifically stated,
“ When we have new clients that come in that we are trying to inform them about PrEP and I have asked them if they may have seen the commercial, especially the younger population. They will say exactly what you said, that “Oh, I thought that was for homosexuals or whatever,” and I am saying “No, it is for anyone that is at risk.” – Staff, Nurse, Female
Further, staff agreed that younger populations should be included in PrEP efforts to alleviate stigma. Participants added that including PrEP information with other prevention methods (i.e., birth control, vaccines) is a good place to include parents and adolescents:
“Just trying to educate them about Hepatitis and things of that nature, Herpes. I think we should also, as they are approaching 15, the same way we educate them about their cycle coming on and what to expect, it’s almost like we need to start incorporating this (PrEP education), even with different forms of birth control methods with our young ladies.” – Staff, Nurse, Female
Participants agreed that PrEP testimonials would be helpful, specifically from people who started PrEP, stopped, and then were diagnosed with HIV. Participants indicated that this may improve PrEP uptake and persistence. One nurse stated:
“I have seen where a patient has been on PrEP a time or two and at some point, early in the year or later part of the year, and we have seen where they’ve missed those appointments and were not consistent with their medication regimen. And we have seen those who’ve tested positive for HIV. So, if there is a way we could get one of those patients who will be willing to share their testimony, I think they can really be impactful because it’s showing that taking up preventive measures was good and then kind of being inconsistent, this is what the outcome is, unfortunately.” – Staff, Nurse, Female
Increase variety and number of PrEP providers
Participants agreed that a “PrEP champion” (someone to promote PrEP and answer PrEP related questions) would be helpful, especially for providers who need more education about PrEP to feel comfortable prescribing. A patient navigator said,
“I definitely think that a provider PrEP champion is needed in every clinic or organization that is offering PrEP. And it goes back to what we were saying about the providers not being knowledgeable on it [PrEP]. If you have a PrEP champion that already knows this information, it is gonna benefit everybody, patients, patient advocates, the provider, everyone all around. Everyone needs a champion." – Staff, Patient Navigator, Female
Staff noted that they have walk-in appointments for PrEP available; however, they often have too many walk-in appointments to see everyone. They noted that having more resources and providers may alleviate this barrier for some patients:
“We still have challenges with people walking in versus scheduling an appointment, but we do have same day appointments. It is just hard sometimes because the volume that we have at our clinic and the number of patients that we have that walk in on a daily basis.” – Staff, Social Worker, Female
Enhance PrEP provider alliance and trust
Participants agreed that educational meetings would be beneficial and highlighted that meetings should happen regularly and emphasized a preference for in-person meetings. This is emphasized by the statement below,
“They should be in-person with handouts. You have to kind of meet people where they are as far as learning. Giving the knowledge, obtaining the knowledge, and using it, and so you have to find a place. I definitely think that yearly in-person training to update guidelines, medication doses, different things like that." – Staff, Patient Navigator, Female
Staff also suggested hosting one very large collaborative event to bring together all organizations that offer PrEP and HIV testing to meet and discuss additional efforts:
“What I would like to see happen here in the state of Mississippi, because we are so high on the list for new HIV infections, I would like to see a big collaborative event. As far as PrEP goes, those that are not on PrEP, one big collaborative event with different community health centers. You do testing, we do PrEP, and the referral get split. Everyone coming together for one main purpose.” – Staff, Patient Navigator, Female
Increase access to PrEP
Participants highlighted that most of the clinics they worked for already offer a variety of service sites (pharmacy, mobile clinic) but that more clinics should offer these alternative options for patients to receive PrEP. One patient navigator outlined the services they offer,
“We have a mobile unit. We do not have a home health travel nurse. We do telephone visits. We offer primary care, OB/GYN. We have our own pharmacy. We also have samples in our pharmacy available to patients that can’t get their medicine on the same day cos we like to implement same day PrEP. It has worked for us. More people should utilize those services.” – Staff, Patient Navigator, Female
Other staff suggested utilizing minute clinics and pharmacies at grocery stores. Highlighting, that offering PrEP at these locations may increase PrEP uptake.
There has been great scientific expansion of HIV prevention research and priorities must now pivot to addressing how to best implement effective interventions like PrEP [ 38 ]. PrEP remains underutilized among individuals who may benefit, particularly in Southern states such as MS [ 10 , 11 , 12 , 13 , 14 ]. Implementation science could help ameliorate this by identifying barriers and facilitators to PrEP rollout and uptake. We selected and defined several strategies from the ERIC project [ 26 ] to increase PrEP use utilizing FQHCs. Our results, as shown in Table 3 , highlight the four domains of strategies selected: 1) PrEP Information Dissemination, 2) Increase Variety and Number of PrEP Providers, 3) Enhance PrEP Provider Alliance and Trust, and 4) Increase Access to PrEP.
Firstly, individuals cannot utilize PrEP if they are not aware of its presence and utility. In Mississippi, advertising PrEP services is integral to implementation efforts given the existing stigma and lack of health literacy in this region [ 39 ]. Potential avenues for expanding PrEP awareness are integrating it into educational curriculums, adolescents’ routine preventative healthcare, and health fairs. This study compliments prior research that people should be offered sexual health and PrEP education at a younger age to increase awareness of risk, foster change in social norms and enhance willingness to seek out prevention services [ 40 , 41 ]. To meet the resulting growing need for PrEP educators, healthcare professionals should receive up-to-date PrEP information and training, so that they can confidently relay information to their patients. Similar to existing research, increasing provider education could accelerate PrEP expansion [ 42 , 43 , 44 ]. Training programs aimed at increasing provider PrEP knowledge may increase PrEP prescriptions provided [ 43 ] by addressing one of the most frequently listed barriers to PrEP prescription among providers [ 45 , 46 ].
Many patients prefer to receive PrEP at the healthcare locations they already attend and report a barrier to PrEP being limited healthcare settings that offer PrEP [ 39 , 47 , 48 , 49 ]. The aforementioned PrEP training could increase the number of healthcare workers willing to provide PrEP services. It is also imperative that providers in a diverse range of healthcare settings (e.g., primary care, OB/GYN, pediatricians and adolescent medicine providers) join the list of those offering PrEP to reduce stigma and enhance patient comfort.
These results mirrored other studies in the South that have shown that using relatable healthcare providers and trusted members of the community may serve to facilitate PrEP uptake [ 41 , 50 , 51 ]. If patients have a larger number of PrEP providers to choose from, they can select one that best fits their needs (e.g., location, in-network) and preferences (e.g., familiarity, cultural similarities). Enhanced comfort facilitates a strong patient-provider alliance and can lead to more open/honest communication regarding HIV risk behavior.
The lack of conveniently located PrEP providers is consistently reported as a structural barrier in the South [ 44 , 52 ]. This creates an increase in the demand on patients to attend regular follow-up appointments. The three strategies above all play a vital role in increasing access to PrEP. If more individuals are trained to provide PrEP care, there will be more PrEP providers, and patients can choose the best option for them. A sizeable influx of new PrEP providers could help staff new care facilities and service options in the community (e.g., mobile health units, home care, community-based clinics, telemedicine). Offering PrEP via telemedicine and mobile clinics to patients has been largely supported in the literature [ 44 , 53 , 54 ]. Intra- and inter-organizational collaborations could similarly increase PrEP access by sharing information and resources to ensure patients get timely, reliable care.
Our results largely supported previous findings by two systematic reviews on the barriers to PrEP uptake and implementation strategies to overcome it [ 39 , 47 ]. Sullivan et.al.’s review focused on the Southern U.S. [ 38 ], while Bonacci et. al. explored steps to improve PrEP equity for Black and Hispanic/Latino communities [ 47 ]. Both agreed that barriers to PrEP access are complex. Thus, cooperation from policymakers and the expansion of state Medicaid or targeted Medicaid waivers is vital to make PrEP attainable for those living in the coverage gap. Further, many FQHCs receive Ryan White funding for HIV care and treatment, contracting flexibility in the utility of these other sources of support may aid in eliminating the cost of PrEP as a barrier. They also stressed the need for educating community members and healthcare personnel about PrEP, increasing and diversifying PrEP service sites, normalizing PrEP campaigns and screening to alleviate stigma, and streamlining clinical procedures to facilitate the option for same-day PrEP. However, they also noted that these strategies are easier said than done. This further highlights the need for prioritizing research efforts towards implementation studies for effectiveness and practicality of overcoming the complex and systemic needs around HIV prevention/treatment.
The present study was able to build on past findings by providing a more holistic view of the barriers to PrEP use and possible strategies to address them through querying PrEP-eligible patients, medical providers, and non-medical staff. By interviewing a diverse range of stakeholders, it was possible to identify unmet patient needs, current PrEP care procedures and infrastructure, and attitudes and needed resources among those who could potentially be trained to provide PrEP in the future.
Limitations
Our results are limited to participants and clinic staff who were willing to engage in a research interview to discuss PrEP and FQHCs. Results are only generalizable to Mississippi and may be less relevant for other geographic areas. However, this is a strength given these strategies are meant to be tailored specifically to FQHCs in MS. Due to COVID-19 restrictions, interviews were conducted via Zoom. This allowed us to reach participants unable to come in physically for an interview and may have increased their comfort responding to questions [ 55 ]. However, some participants may have been less comfortable discussing via Zoom, which may have limited their willingness to respond.
This study highlighted the need for implementing PrEP strategies to combat HIV in Mississippi. PrEP knowledge, barriers, and motivation were identified as key factors influencing PrEP utilization, and four domains of strategies were identified for improving PrEP accessibility and uptake. Future research should further refine and assess the feasibility and acceptability of selected and defined implementation strategies and test strategies.

Availability of data and materials
De-identified data from this study are not available in a public archive due to sensitive nature of the data. De-identified data from this study will be made available (as allowable according to institutional IRB standards) by emailing the corresponding author.
Abbreviations
Mississippi
Pre-Exposure Prophylaxis
Federally Qualified Health Centers
Integrated-Promoting Action on Research Implementation in Health Services
Expert Recommendations for Implementing Change
Men Who Have Sex With Men
Health MSDo. Mississippi’s Ending the HIV Epidemic Plan: MSDH; 2021. Available from: http://healthyms.com/msdhsite/_static/resources/5116.pdf .
Digre P, Avoundjian T, Johnson K, Peyton D, Lewis C, Barnabas RV, et al. Barriers, facilitators, and cost of integrating HIV-related activities into sexually transmitted disease partner services in Jackson, Mississippi. Sexually Transmit Dis. 2021;48(3):145–51.
Article Google Scholar
Rosenberg ES, Grey JA, Sanchez TH, Sullivan PS. Rates of prevalent HIV infection, prevalent diagnoses, and new diagnoses among men who have sex with men in US states, metropolitan statistical areas, and counties, 2012–2013. JMIR Public Health Surveill. 2016;2(1):e5684.
Khosropour CM, Backus KV, Means AR, Beauchamps L, Johnson K, Golden MR, et al. A pharmacist-led, same-day, HIV pre-exposure prophylaxis initiation program to increase PrEP uptake and decrease time to PrEP initiation. AIDS Patient Care STDS. 2020;34(1):1–6.
Article PubMed PubMed Central Google Scholar
Stopka TJ, Brinkley-Rubinstein L, Johnson K, Chan PA, Hutcheson M, Crosby R, et al. HIV Clustering in Mississippi: spatial epidemiological study to inform implementation science in the deep south. JMIR Publ Health Surveil. 2018;4(2):e35-e.
Choopanya K, Martin M, Suntharasamai P, Sangkum U, Mock PA, Leethochawalit M, et al. Antiretroviral prophylaxis for HIV infection in injecting drug users in Bangkok, Thailand (the Bangkok Tenofovir Study): a randomised, double-blind, placebo-controlled phase 3 trial. The Lancet. 2013;381(9883):2083–90.
Molina J-M, Capitant C, Spire B, Pialoux G, Cotte L, Charreau I, et al. On-demand preexposure prophylaxis in men at high risk for HIV-1 infection. N Engl J Med. 2015;373:2237–46.
Article CAS PubMed Google Scholar
Molina J, Charreau I, Spire B, Cotte L, Chas J, Capitant C, et al. ANRS IPERGAY Study Group Efficacy, safety, and effect on sexual behaviour of on-demand pre-exposure prophylaxis for HIV in men who have sex with men: an observational cohort study. Lancet HIV. 2017;4(9):e402–10.
Article PubMed Google Scholar
Centers for Disease Control and Prevention. How effective is PrEP? : CDC; 2022. Available from: https://www.cdc.gov/hiv/basics/prep/prep-effectiveness.html .
Kirby T, Thornber-Dunwell M. Uptake of PrEP for HIV slow among MSM. Lancet. 2014;383(9915):399–400.
Elopre L, Kudroff K, Westfall AO, Overton ET, Mugavero MJ. The right people, right places, and right practices: disparities in PrEP access among African American men, women and MSM in the Deep South. J Acquired Immune Deficiency Syndr (1999). 2017;74(1):56.
Article PubMed Central Google Scholar
Brantley ML, Rebeiro PF, Pettit AC, Sanders A, Cooper L, McGoy S, et al. Temporal trends and sociodemographic correlates of PrEP uptake in Tennessee, 2017. AIDS Behav. 2019;23:304–12.
Hollcroft MR, Gipson J, Barnes A, Mena L, Dombrowski JC, Ward LM, et al. PrEP acceptance among eligible patients attending the largest PrEP Clinic in Jackson, Mississippi. J Int Assoc Providers AIDS Care (JIAPAC). 2023;22:23259582231167960.
PubMed Google Scholar
Chase E, Mena L, Johnson KL, Prather M, Khosropour CM. Patterns of Pre-exposure Prophylaxis (PrEP) Use in a Population Accessing PrEP in Jackson, Mississippi. AIDS Behav. 2023;27(4):1082–90. https://doi.org/10.1007/s10461-022-03845-9 .
Arnold T, Brinkley-Rubinstein L, Chan PA, Perez-Brumer A, Bologna ES, Beauchamps L, et al. Social, structural, behavioral and clinical factors influencing retention in Pre-Exposure Prophylaxis (PrEP) care in Mississippi. PLoS ONE. 2017;12(2):e0172354.
Cahill S, Taylor SW, Elsesser SA, Mena L, Hickson D, Mayer KH. Stigma, medical mistrust, and perceived racism may affect PrEP awareness and uptake in black compared to white gay and bisexual men in Jackson, Mississippi and Boston, Massachusetts. AIDS care. 2017;29(11):1351–8.
Arnold T, Gaudiano BA, Barnett AP, Elwy AR, Whiteley L, Giorlando KK, et al. Development of an acceptance based PrEP intervention (ACTPrEP) to engage young black MSM in the South utilizing the Adaptome Model of intervention adaptation. J Contextual Behav Sci. 2023;28:60–70.
Administration HRS. What is a Health Center? 2023. Available from: https://bphc.hrsa.gov/about-health-centers/what-health-center .
Oster AM, Dorell CG, Mena LA, Thomas PE, Toledo CA, Heffelfinger JD. HIV risk among young African American men who have sex with men: A case–control study in Mississippi. Am J Public Health. 2011;101(1):137–43.
Hall HI, Li J, McKenna MT. HIV in predominantly rural areas of the United States. J Rural Health. 2005;21(3):245–53.
Williams PB, Sallar AM. HIV/AIDS and African American men: Urban-rural differentials in sexual behavior, HIV knowledge, and attitude towards condoms use. J Natl Med Assoc. 2010;102(12):1139–49.
Krakower D, Mayer KH. Engaging healthcare providers to implement HIV pre-exposure prophylaxis. Curr Opin HIV AIDS. 2012;7(6):593.
Krakower D, Ware N, Mitty JA, Maloney K, Mayer KH. HIV providers’ perceived barriers and facilitators to implementing pre-exposure prophylaxis in care settings: a qualitative study. AIDS Behav. 2014;18:1712–21.
Hakre S, Blaylock JM, Dawson P, Beckett C, Garges EC, Michael NL, Danaher PJ, Scott PT, Okulicz JF. Knowledge, attitudes, and beliefs about HIV pre-exposure prophylaxis among US Air Force Health Care Providers. Medicine (Baltimore). 2016;95(32):e4511. https://doi.org/10.1097/MD.0000000000004511 .
Yakovchenko V, Bolton RE, Drainoni ML, Gifford AL. Primary care provider perceptions and experiences of implementing hepatitis C virus birth cohort testing: a qualitative formative evaluation. BMC Health Serv Res. 2019;19(1):236.
Powell BJ, Waltz TJ, Chinman MJ, Damschroder LJ, Smith JL, Matthieu MM, et al. A refined compilation of implementation strategies: results from the Expert Recommendations for Implementing Change (ERIC) project. Implement Sci. 2015;10(1):21.
O'Brien BC, Harris IB, Beckman TJ, Reed DA, Cook DA. Standards for reporting qualitative research: a synthesis of recommendations. Acad Med. 2014;89(9):1245–51. https://doi.org/10.1097/ACM.0000000000000388 .
Harvey G, Kitson A. PARIHS revisited: from heuristic to integrated framework for the successful implementation of knowledge into practice. Implement Sci. 2016;11(1):33.
Braun V, Clarke V, Hayfield N, Terry G. Thematic Analysis. In: Liamputtong P, editor. Handbook of research methods in health social sciences. Singapore: Springer Singapore; 2019. p. 843–60.
Chapter Google Scholar
Lewis CC, Klasnja P, Powell BJ, Lyon AR, Tuzzio L, Jones S, Walsh-Bailey C, Weiner B. From Classification to Causality: Advancing Understanding of Mechanisms of Change in Implementation Science. Front Public Health. 2018;6:136. https://doi.org/10.3389/fpubh.2018.00136 .
Lewis CC, Powell BJ, Brewer SK, Nguyen AM, Schriger SH, Vejnoska SF, et al. Advancing mechanisms of implementation to accelerate sustainable evidence-based practice integration: protocol for generating a research agenda. BMJ Open. 2021;11(10):e053474.
Varpio L, Ajjawi R, Monrouxe LV, O’Brien BC, Rees CE. Shedding the cobra effect: problematising thematic emergence, triangulation, saturation and member checking. Med Educ. 2017;51(1):40–50.
McKim C. Meaningful member-checking: a structured approach to member-checking. Am J Qual Res. 2023;7(2):41–52.
Google Scholar
Elo S, Kääriäinen M, Kanste O, Pölkki T, Utriainen K, Kyngäs H. Qualitative content analysis: A focus on trustworthiness. SAGE Open. 2014;4(1):2158244014522633.
Candela AG. Exploring the function of member checking. The qualitative report. 2019;24(3):619–28.
Vindrola-Padros C, Johnson GA. Rapid techniques in qualitative research: a critical review of the literature. Qual Health Res. 2020;30(10):1596–604.
Neal JW, Neal ZP, VanDyke E, Kornbluh M. Expediting the analysis of qualitative data in evaluation: a procedure for the Rapid Identification of Themes from Audio recordings (RITA). Am J Eval. 2015;36(1):118–32.
Theobald S, Brandes N, Gyapong M, El-Saharty S, Proctor E, Diaz T, et al. Implementation research: new imperatives and opportunities in global health. The Lancet. 2018;392(10160):2214–28.
Sullivan PS, Mena L, Elopre L, Siegler AJ. Implementation strategies to increase PrEP Uptake in the South. Curr HIV/AIDS Rep. 2019;16(4):259–69.
Elopre L, Ott C, Lambert CC, Amico KR, Sullivan PS, Marrazzo J, et al. Missed prevention opportunities: why young, black MSM with recent HIV diagnosis did not access HIV pre-exposure prophylaxis services. AIDS Behav. 2021;25(5):1464–73.
Arnold T, Giorlando KK, Barnett AP, Gaudiano BA, Rogers BG, Whiteley L, et al. Social, structural, behavioral, and clinical barriers influencing Pre-exposure Prophylaxis (PrEP) use among young black men who have sex with men in the south: a qualitative update to a 2016 study. Arch Sex Behav. 2024;53(2):785–97.
Edelman EJ, Moore BA, Calabrese SK, Berkenblit G, Cunningham CO, Ogbuagu O, et al. Preferences for implementation of HIV pre-exposure prophylaxis (PrEP): Results from a survey of primary care providers. Prev Med Rep. 2020;17: 101012.
Petroll AE, Walsh JL, Owczarzak JL, McAuliffe TL, Bogart LM, Kelly JA. PrEP awareness, familiarity, comfort, and prescribing experience among US primary care providers and HIV specialists. AIDS Behav. 2017;21(5):1256–67.
Barnett AP, Arnold T, Elwy AR, Brock JB, Giorlando KK, Sims-Gomillia C, et al. Considerations for PrEP implementation at federally qualified health centers in Mississippi: perspectives from staff and patients. AIDS Educ Prev. 2023;35(4):309–19.
Seidman D, Carlson K, Weber S, Witt J, Kelly PJ. United States family planning providers’ knowledge of and attitudes towards preexposure prophylaxis for HIV prevention: a national survey. Contraception. 2016;93(5):463–9.
Clement ME, Seidelman J, Wu J, Alexis K, McGee K, Okeke NL, et al. An educational initiative in response to identified PrEP prescribing needs among PCPs in the Southern U.S. AIDS Care. 2018;30(5):650–5.
Bonacci RA, Smith DK, Ojikutu BO. Toward greater pre-exposure prophylaxis equity: increasing provision and uptake for black and Hispanic/Latino individuals in the US. Am J Prev Med. 2021;61(5 Suppl 1):S60-s72.
Arnold T, Whiteley L, Elwy RA, Ward LM, Konkle-Parker DJ, Brock JB, et al. Mapping Implementation Science with Expert Recommendations for Implementing Change (MIS-ERIC): strategies to improve PrEP use among black cisgender women living in Mississippi. J Racial Ethn Health Disparities. 2023;10(6):2744–61.
Hirschhorn LR, Brown RN, Friedman EE, Greene GJ, Bender A, Christeller C, Bouris A, Johnson AK, Pickett J, Modali L, Ridgway JP. Black Cisgender Women's PrEP Knowledge, Attitudes, Preferences, and Experience in Chicago. J Acquir Immune Defic Syndr. 2020;84(5):497–507. https://doi.org/10.1097/QAI.0000000000002377 .
Pichon LC, Teti M, McGoy S, Murry VM, Juarez PD. Engaging black men who have sex with men (MSM) in the South in identifying strategies to increase PrEP uptake. BMC Health Serv Res. 2022;22(1):1491.
Auerbach JD, Kinsky S, Brown G, Charles V. Knowledge, attitudes, and likelihood of pre-exposure prophylaxis (PrEP) use among US women at risk of acquiring HIV. AIDS Patient Care STDS. 2015;29(2):102–10.
Siegler AJ, Bratcher A, Weiss KM. Geographic access to preexposure prophylaxis clinics among men who have sex with men in the United States. Am J Public Health. 2019;109(9):1216–23.
Rousseau E, Julies RF, Madubela N, Kassim S. Novel platforms for biomedical HIV prevention delivery to key populations — community mobile clinics, peer-supported, pharmacy-Led PrEP delivery, and the use of telemedicine. Curr HIV/AIDS Rep. 2021;18(6):500–7.
Article CAS PubMed PubMed Central Google Scholar
Player MS, Cooper NA, Perkins S, Diaz VA. Evaluation of a telemedicine pilot program for the provision of HIV pre-exposure prophylaxis in the Southeastern United States. AIDS Care. 2022;34(12):1499–505.
Gray LM, Wong-Wylie G, Rempel GR, Cook K. Expanding qualitative research interviewing strategies: Zoom video communications. Qual Rep. 2020;25(5):1292–301.
Download references
Acknowledgements
Authors would like to acknowledge and thank Sarah Bailey for reviewing the manuscript and assisting for formatting.
This study was funded by the National Institute of Health (R34MH115744) and was facilitated by the Providence/Boston Center for AIDS Research (P30AI042853). Additionally, work by Dr. Trisha Arnold was supported by the National Institute of Mental Health Grant (K23MH124539-01A1) and work by Dr. Andrew Barnett was supported by the National Institute of Mental Health Grant (T32MH078788). Dr. Elwy is supported by a Department of Veterans Affairs Research Career Scientist Award (RCS 23–018).
Author information
Authors and affiliations.
Department of Psychiatry, Rhode Island Hospital, One Hoppin Street, Coro West, 204, Providence, RI, 02903, USA
Trisha Arnold, Kayla K. Giorlando, Andrew P. Barnett, Avery Leigland & Larry K. Brown
Department of Psychiatry and Human Behavior, Warren Alpert Medical School of Brown University, Providence, RI, USA
Trisha Arnold, Laura Whiteley, Andrew P. Barnett, Ariana M. Albanese, A. Rani Elwy & Larry K. Brown
Department of Population Health Science, University of Mississippi Medical Center, Jackson, MS, USA
Courtney Sims-Gomillia & Precious Patrick Edet
Department of Medicine, University of Mississippi Medical Center, Jackson, MS, USA
Demetra M. Lewis & James B. Brock
Center for Healthcare Organization and Implementation Research, VA Bedford Healthcare System, Bedford, MA, USA
A. Rani Elwy
You can also search for this author in PubMed Google Scholar
Contributions
TA and ARE led the conceptualization of this paper. TA, LW, LKB, DML, and JBB completed the literature search and study design. TA, LW, LKB, KKG, PPE, AB, AL, and CSG assisted with analyzing and interpreting the data. TA, ARE, and AMA finalized the results and implementation concepts of the study. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Trisha Arnold .
Ethics declarations
Ethics approval and consent to participate.
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The study was approved by both the Rhode Island Hospital Institutional Review Board and the University of Mississippi Medical Center Institutional Review Board. Informed consent was obtained from all individual participants included in the study.
Consent for publication
Not applicable.
Competing interests
All authors declare that they have no conflicts of interest or competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Arnold, T., Whiteley, L., Giorlando, K.K. et al. A qualitative study identifying implementation strategies using the i-PARIHS framework to increase access to pre-exposure prophylaxis at federally qualified health centers in Mississippi. Implement Sci Commun 5 , 92 (2024). https://doi.org/10.1186/s43058-024-00632-6
Download citation
Received : 22 May 2024
Accepted : 21 August 2024
Published : 28 August 2024
DOI : https://doi.org/10.1186/s43058-024-00632-6
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- HIV Prevention
- Implementation Science
- Pre-exposure prophylaxis (PrEP)
- Telemedicine
Implementation Science Communications
ISSN: 2662-2211
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]

Reducing H. pylori in Navajo Nation tribal members through testing and education

How can you eliminate a pervasive, yet undiscussed, bacterial infection from the Navajo Nation? For a collaborative group of researchers, it requires dedication, hours of travel, and unfailing commitment to present information in a respectful, culturally relevant way.
Helicobacter pylori , known as H. pylori , is one of the most common bacterial stomach infections worldwide and accounts for nearly three-quarters of all gastric cancer.
While gastric cancer has decreased in the United States, the incidence in the Navajo Nation is nearly four times higher than non-Hispanic white populations in the area.
In a recent publication, “ Helicobacter pylori Prevalence and Risk Factors in Three Rural Indigenous Communities of Northern Arizona ,” researchers from the University of Arizona, Northern Arizona University and San Diego State University explored the results of a study on H. pylori they conducted from June to August 2018.
The team recruited 106 self-identified Navajo adults 18 years and older from 73 households living in three Navajo chapter communities in the southwestern part of the Navajo Nation in Arizona. Their results found that 56.4% of study participants had H. pylori and 72% of households had at least one infected person.
Robin B. Harris, professor of epidemiology in the UA Mel & Enid Zuckerman College of Public Health, was the principal investigator. Other researchers included Heidi E. Brown , infectious disease epidemiologist in the UA Department of Epidemiology and Biostatistics; Rachelle L. Begay, a doctoral student in epidemiology and senior program coordinator in the Center for Indigenous Environmental Health Research in the UA Mel & Enid Zuckerman College of Public Health; Priscilla R. Sanderson (Diné), professor in the NAU Department of Health Sciences; Carmenlita Chief (Diné), senior research coordinator in the NAU Center for Health Equity Research; Fernando P. Monroy , professor in the NAU Department of Biological Sciences; and Eyal Oren , associate professor of Division of Epidemiology and Biostatistics, San Diego State University.
“The devastation of stomach cancer is a primary reason for the NACP-funded team to know the causes of Helicobacter pylori infection,” Sanderson said. “In addition, the NAU team conducted semi-structured interviews to explore the knowledge, attitudes, and behaviors of Navajo adults on Navajo Nation and in urban areas surrounding the Navajo Nation (AZ, NM, UT, CO). The NAU team are members of Navajo Nation so our work is personal as we want to save lives for our Diné extended family.”
Exploring H. pylori through the Navajo Healthy Stomach Project
In 2017, researchers from UA and NAU formed the Navajo Healthy Stomach Project, through the Partnership for Native American Cancer Prevention (NACP), to determine the prevalence of H. pylori infection among Navajo adults and to identify the local social, behavioral, and environmental factors associated with infection.
According to the National Institutes of Health, H. pylori infection usually occurs in childhood. The infection can increase the chance that a person may develop gastric cancer.
H. pylori bacteria are usually passed from person to person through direct contact with saliva, vomit or stool and may also be spread through contaminated food or water, crowded living conditions or living with someone who has H. pylori.
H. pylori study

Data gathering teams included undergraduate Diné students from NAU; medical, doctoral, a master’s degree and undergraduate Diné students from UA; an undergraduate from Diné College; and Navajo community health representatives. At least one member of each team was fluent in Navajo. The teams used GPS to locate and personally visit 143 households on the Navajo Nation. They were able to recruit participants from just over half of the households they encountered.
“It was essential [to include someone on the team who was fluent in Navajo] because these three communities we had worked with on this on this study are located in a part of the Navajo Nation that is pretty rural, where more households speak Navajo as their primary language and live several miles away from a paved road,” Chief said. “So, if you are investing 30 to 45 minutes traveling on a dirt road to get to a home, you want to make sure someone on the team can communicate effectively with household members once you get there. In many cases, those are our elders.”
The teams explained the study to participants, administered the surveys and collected specimens. In the survey, participants described their water sources, food preparation procedures, refrigeration practices, bathroom configuration, lifestyle behaviors, dietary habits, and health history.
Each participant also took a non-invasive C-Urea Breath Test, which detects the presence of H. pylori in expelled breath; specimens were analyzed by machine at the Winslow Indian Health Care Center in Winslow, AZ.
After the researchers mailed the results to participants, a Navajo CHR visited every person to make sure they received their test results and provided additional education to them.
They found H. pylori in 66 participants of the 101 viable UBT tests; —78% were male and 57% were female. The odds of having H.pylori increased for households with unregulated water, and the Navajo Healthy Stomach Project identified water sources as a primary environmental or household risk factor for infection.

Future for the Navajo Health Stomach Project
The Navajo Healthy Stomach Project also found that there was generally a low level of awareness of H. pylori , with only 24% of the participants reporting they had ever heard of the infection.
Their future work will address barriers that prevent people who test positive for H. pylori from getting treatment and expand education through medical centers for earlier diagnosis.
Since the H. pylori infection typically begins in childhood or early adulthood, the researchers said they hope to develop a follow-up study to target participants under the age of 18 and to expand the number of participants in the 18–29 age range.
The team plans to continue to explore the causes of H. pylori , with a goal of eradicating the disease and to address unregulated water for drinking and cooking.
“We are hopeful our Navajo Nation leaders will assist in our effort as this is a public health concern that needs to be addressed and prioritized as we want our Navajo extended family to see stomach cancer rate reduced to zero—just like the rest of America,” Sanderson said.
The Partnership for Native American Cancer Prevention (NACP) is the collaboration between The University of Arizona Cancer Center (UACC), Northern Arizona University (NAU), The National Institutes of Health (NIH), and The National Cancer Institute (NCI). The Partnership is funded under parallel grants, U54CA143924 (UACC) and U54CA143925 (NAU).
- Carmenlita Chief
- Navajo Healthy Stomach Project
- Priscilla Sanderson H. pylori
- Open access
- Published: 06 April 2020
The influence of education on health: an empirical assessment of OECD countries for the period 1995–2015
- Viju Raghupathi 1 &
- Wullianallur Raghupathi 2
Archives of Public Health volume 78 , Article number: 20 ( 2020 ) Cite this article
227k Accesses
311 Citations
173 Altmetric
Metrics details
A clear understanding of the macro-level contexts in which education impacts health is integral to improving national health administration and policy. In this research, we use a visual analytic approach to explore the association between education and health over a 20-year period for countries around the world.
Using empirical data from the OECD and the World Bank for 26 OECD countries for the years 1995–2015, we identify patterns/associations between education and health indicators. By incorporating pre- and post-educational attainment indicators, we highlight the dual role of education as both a driver of opportunity as well as of inequality.
Adults with higher educational attainment have better health and lifespans compared to their less-educated peers. We highlight that tertiary education, particularly, is critical in influencing infant mortality, life expectancy, child vaccination, and enrollment rates. In addition, an economy needs to consider potential years of life lost (premature mortality) as a measure of health quality.
Conclusions
We bring to light the health disparities across countries and suggest implications for governments to target educational interventions that can reduce inequalities and improve health. Our country-level findings on NEET (Not in Employment, Education or Training) rates offer implications for economies to address a broad array of vulnerabilities ranging from unemployment, school life expectancy, and labor market discouragement. The health effects of education are at the grass roots-creating better overall self-awareness on personal health and making healthcare more accessible.
Peer Review reports
Introduction
Is education generally associated with good health? There is a growing body of research that has been exploring the influence of education on health. Even in highly developed countries like the United States, it has been observed that adults with lower educational attainment suffer from poor health when compared to other populations [ 36 ]. This pattern is attributed to the large health inequalities brought about by education. A clear understanding of the health benefits of education can therefore serve as the key to reducing health disparities and improving the well-being of future populations. Despite the growing attention, research in the education–health area does not offer definitive answers to some critical questions. Part of the reason is the fact that the two phenomena are interlinked through life spans within and across generations of populations [ 36 ], thereby involving a larger social context within which the association is embedded. To some extent, research has also not considered the variances in the education–health relationship through the course of life or across birth cohorts [ 20 ], or if there is causality in the same. There is therefore a growing need for new directions in education–health research.
The avenues through which education affects health are complex and interwoven. For one, at the very outset, the distribution and content of education changes over time [ 20 ]. Second, the relationship between the mediators and health may change over time, as healthcare becomes more expensive and/or industries become either more, or less hazardous. Third, some research has documented that even relative changes in socioeconomic status (SES) can affect health, and thus changes in the distribution of education implies potential changes in the relationship between education and health. The relative index of inequality summarizes the magnitude of SES as a source of inequalities in health [ 11 , 21 , 27 , 29 ]. Fourth, changes in the distribution of health and mortality imply that the paths to poor health may have changed, thereby affecting the association with education.
Research has proposed that the relationship between education and health is attributable to three general classes of mediators: economic; social, psychological, and interpersonal; and behavioral health [ 31 ]. Economic variables such as income and occupation mediate the relationship between education and health by controlling and determining access to acute and preventive medical care [ 1 , 2 , 19 ]. Social, psychological, and interpersonal resources allow people with different levels of education to access coping resources and strategies [ 10 , 34 ], social support [ 5 , 22 ], and problem-solving and cognitive abilities to handle ill-health consequences such as stress [ 16 ]. Healthy behaviors enable educated individuals to recognize symptoms of ill health in a timely manner and seek appropriate medical help [ 14 , 35 ].
While the positive association between education and health has been established, the explanations for this association are not [ 31 ]. People who are well educated experience better health as reflected in the high levels of self-reported health and low levels of morbidity, mortality, and disability. By extension, low educational attainment is associated with self-reported poor health, shorter life expectancy, and shorter survival when sick. Prior research has suggested that the association between education and health is a complicated one, with a range of potential indicators that include (but are not limited to) interrelationships between demographic and family background indicators [ 8 ] - effects of poor health in childhood, greater resources associated with higher levels of education, appreciation of good health behaviors, and access to social networks. Some evidence suggests that education is strongly linked to health determinants such as preventative care [ 9 ]. Education helps promote and sustain healthy lifestyles and positive choices, nurture relationships, and enhance personal, family, and community well-being. However, there are some adverse effects of education too [ 9 ]. Education may result in increased attention to preventive care, which, though beneficial in the long term, raises healthcare costs in the short term. Some studies have found a positive association between education and some forms of illicit drug and alcohol use. Finally, although education is said to be effective for depression, it has been found to have much less substantial impact in general happiness or well-being [ 9 ].
On a universal scale, it has been accepted that several social factors outside the realm of healthcare influence the health outcomes [ 37 ]. The differences in morbidity, mortality and risk factors in research, conducted within and between countries, are impacted by the characteristics of the physical and social environment, and the structural policies that shape them [ 37 ]. Among the developed countries, the United States reflects huge disparities in educational status over the last few decades [ 15 , 24 ]. Life expectancy, while increasing for all others, has decreased among white Americans without a high school diploma - particularly women [ 25 , 26 , 32 ]. The sources of inequality in educational opportunities for American youth include the neighborhood they live in, the color of their skin, the schools they attend, and the financial resources of their families. In addition, the adverse trends in mortality and morbidity brought on by opioids resulting in suicides and overdoses (referred to as deaths of despair) exacerbated the disparities [ 21 ]. Collectively, these trends have brought about large economic and social inequalities in society such that the people with more education are likely to have more health literacy, live longer, experience better health outcomes, practice health promoting behaviors, and obtain timely health checkups [ 21 , 17 ].
Education enables people to develop a broad range of skills and traits (including cognitive and problem-solving abilities, learned effectiveness, and personal control) that predispose them towards improved health outcomes [ 23 ], ultimately contributing to human capital. Over the years, education has paved the way for a country’s financial security, stable employment, and social success [ 3 ]. Countries that adopt policies for the improvement of education also reap the benefits of healthy behavior such as reducing the population rates of smoking and obesity. Reducing health disparities and improving citizen health can be accomplished only through a thorough understanding of the health benefits conferred by education.
There is an iterative relationship between education and health. While poor education is associated with poor health due to income, resources, healthy behaviors, healthy neighborhood, and other socioeconomic factors, poor health, in turn, is associated with educational setbacks and interference with schooling through difficulties with learning disabilities, absenteeism, or cognitive disorders [ 30 ]. Education is therefore considered an important social determinant of health. The influence of national education on health works through a variety of mechanisms. Generally, education shows a relationship with self-rated health, and thus those with the highest education may have the best health [ 30 ]. Also, health-risk behaviors seem to be reduced by higher expenditure into the publicly funded education system [ 18 ], and those with good education are likely to have better knowledge of diseases [ 33 ]. In general, the education–health gradients for individuals have been growing over time [ 38 ].
To inform future education and health policies effectively, one needs to observe and analyze the opportunities that education generates during the early life span of individuals. This necessitates the adoption of some fundamental premises in research. Research must go beyond pure educational attainment and consider the associated effects preceding and succeeding such attainment. Research should consider the variations brought about by the education–health association across place and time, including the drivers that influence such variations [ 36 ].
In the current research, we analyze the association between education and health indicators for various countries using empirical data from reliable sources such as the Organization for Economic Cooperation and Development (OECD) and World Bank. While many studies explore the relationship between education and health at a conceptual level, we deploy an empirical approach in investigating the patterns and relationships between the two sets of indicators. In addition, for the educational indicators, we not only incorporate the level of educational attainment, but also look at the potential socioeconomic benefits, such as enrollment rates (in each sector of educational level) and school life expectancy (at each educational level). We investigate the influences of educational indicators on national health indicators of infant mortality, child vaccinations, life expectancy at birth, premature mortality arising from lack of educational attainment, employment and training, and the level of national health expenditure. Our research question is:
What are some key influencers/drivers in the education-health relationship at a country level?
The current study is important because policy makers have an increasing concern on national health issues and on policies that support it. The effect of education is at the root level—creating better overall self-awareness on personal health and making healthcare more accessible. The paper is organized as follows: Section 2 discusses the background for the research. Section 3 discusses the research method; Section 4 offers the analysis and results; Section 5 provides a synthesis of the results and offers an integrated discussion; Section 6 contains the scope and limitations of the research; Section 7 offers conclusions with implications and directions for future research.
Research has traditionally drawn from three broad theoretical perspectives in conceptualizing the relationship between education and health. The majority of research over the past two decades has been grounded in the Fundamental Cause Theory (FCT) [ 28 ], which posits that factors such as education are fundamental social causes of health inequalities because they determine access to resources (such as income, safe neighborhoods, or healthier lifestyles) that can assist in protecting or enhancing health [ 36 ]. Some of the key social resources that contribute to socioeconomic status include education (knowledge), money, power, prestige, and social connections. As some of these undergo change, they will be associated with differentials in the health status of the population [ 12 ].
Education has also been conceptualized using the Human Capital Theory (HCT) that views it as a return on investment in the form of increased productivity [ 4 ]. Education improves knowledge, skills, reasoning, effectiveness, and a broad range of other abilities that can be applied to improving health. The third approach - the signaling or credentialing perspective [ 6 ] - is adopted to address the large discontinuities in health at 12 and 16 years of schooling, which are typically associated with the receipt of a high school diploma and a college degree, respectively. This perspective considers the earned credentials of a person as a potential source that warrants social and economic returns. All these theoretical perspectives postulate a strong association between education and health and identify mechanisms through which education influences health. While the HCT proposes the mechanisms as embodied skills and abilities, FCT emphasizes the dynamism and flexibility of mechanisms, and the credentialing perspective proposes educational attainment through social responses. It needs to be stated, however, that all these approaches focus on education solely in terms of attainment, without emphasizing other institutional factors such as quality or type of education that may independently influence health. Additionally, while these approaches highlight the individual factors (individual attainment, attainment effects, and mechanisms), they do not give much emphasis to the social context in which education and health processes are embedded.
In the current research while we acknowledge the tenets of these theoretical perspectives, we incorporate the social mechanisms in education such as level of education, skills and abilities brought about by enrollment, school life expectancy, and the potential loss brought about by premature mortality. In this manner, we highlight the relevance of the social context in which the education and health domains are situated. We also study the dynamism of the mechanisms over countries and over time and incorporate the influences that precede and succeed educational attainment.
We analyze country level education and health data from the OECD and World Bank for a period of 21 years (1995–2015). Our variables include the education indicators of adult education level; enrollment rates at various educational levels; NEET (Not in Employment, Education or Training) rates; school life expectancy; and the health indicators of infant mortality, child vaccination rates, deaths from cancer, life expectancy at birth, potential years of life lost and smoking rates (Table 1 ). The data was processed using the tools of Tableau for visualization, and SAS for correlation and descriptive statistics. Approaches for analysis include ranking, association, and data visualization of the health and education data.
Analyses and results
In this section we identify and analyze patterns and associations between education and health indicators and discuss the results. Since countries vary in population sizes and other criteria, we use the estimated averages in all our analyses.
Comparison of health outcomes for countries by GDP per capita
We first analyzed to see if our data reflected the expectation that countries with higher GDP per capita have better health status (Fig. 1 ). We compared the average life expectancy at birth, average infant mortality, average deaths from cancer and average potential year of life lost, for different levels of GDP per capita (Fig. 1 ).
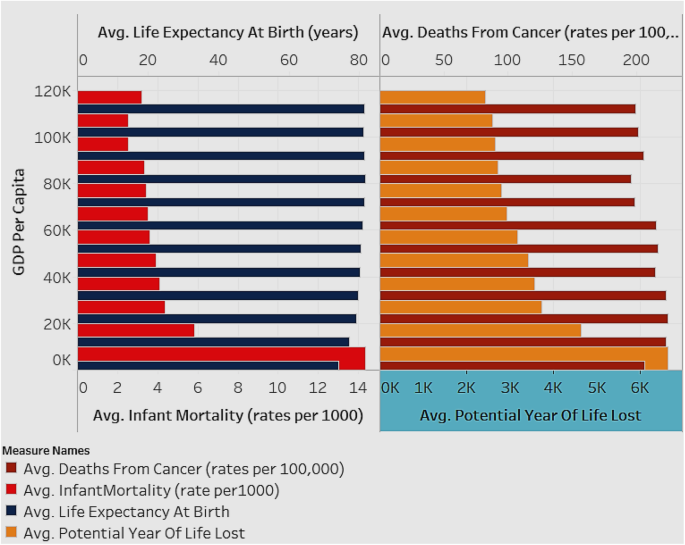
Associations between Average Life Expectancy (years) and Average Infant Mortality rate (per 1000), and between Deaths from Cancer (rates per 100,000) and Average Potential Years of Life Lost (years), by GDP per capita (for all countries for years 1995–2015)
Figure 1 depicts two charts with the estimated averages of variables for all countries in the sample. The X-axis of the first chart depicts average infant mortality rate (per 1000), while that of the second chart depicts average potential years of life lost (years). The Y-axis for both charts depicts the GDP per capita shown in intervals of 10 K ranging from 0 K–110 K (US Dollars). The analysis is shown as an average for all the countries in the sample and for all the years (1995–2015). As seen in Fig. 1 , countries with lower GDP per capita have higher infant mortality rate and increased potential year of life lost (which represents the average years a person would have lived if he or she had not died prematurely - a measure of premature mortality). Life expectancy and deaths from cancer are not affected by GDP level. When studying infant mortality and potential year lost, in order to avoid the influence of a control variable, it was necessary to group the samples by their GDP per capita level.
Association of Infant Mortality Rates with enrollment rates and education levels
We explored the association of infant mortality rates with the enrollment rates and adult educational levels for all countries (Fig. 2 ). The expectation is that with higher education and employment the infant mortality rate decreases.
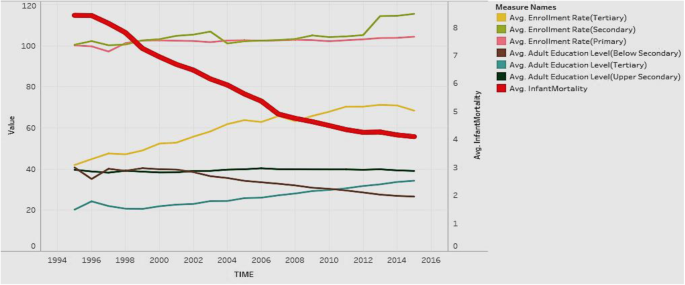
Association of Adult Education Levels (ratio) and Enrollment Rates (ratio) with Infant Mortality Rate (per 1000)
Figure 2 depicts the analysis for all countries in the sample. The figure shows the years from 1995 to 2015 on the X axis. It shows two Y-axes with one axis denoting average infant mortality rate (per 1000 live births), and the other showing the rates from 0 to 120 to depict enrollment rates (primary/secondary/tertiary) and education levels (below secondary/upper secondary/tertiary). Regarding the Y axis showing rates over 100, it is worth noting that the enrollment rates denote a ratio of the total enrollment (regardless of age) at a level of education to the official population of the age group in that education level. Therefore, it is possible for the number of children enrolled at a level to exceed the official population of students in the age group for that level (due to repetition or late entry). This can lead to ratios over 100%. The figure shows that in general, all education indicators tend to rise over time, except for adult education level below secondary, which decreases over time. Infant mortality shows a steep decreasing trend over time, which is favorable. In general, countries have increasing health status and education over time, along with decreasing infant mortality rates. This suggests a negative association of education and enrollment rates with mortality rates.
Association of Education Outcomes with life expectancy at birth
We explored if the education outcomes of adult education level (tertiary), school life expectancy (tertiary), and NEET (not in employment, education, or training) rates, affected life expectancy at birth (Fig. 3 ). Our expectation is that adult education and school life expectancy, particularly tertiary, have a positive influence, while NEET has an adverse influence, on life expectancy at birth.
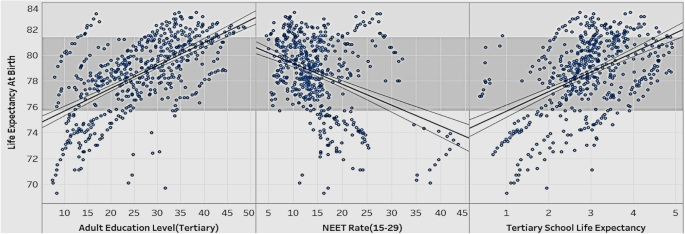
Association of Adult Education Level (Tertiary), NEET rate, School Life Expectancy (Tertiary), with Life Expectancy at Birth
Figure 3 show the relationships between various education indicators (adult education level-tertiary, NEET rate, school life expectancy-tertiary) and life expectancy at birth for all countries in the sample. The figure suggests that life expectancy at birth rises as adult education level (tertiary) and tertiary school life expectancy go up. Life expectancy at birth drops as the NEET rate goes up. In order to extend people’s life expectancy, governments should try to improve tertiary education, and control the number of youths dropping out of school and ending up unemployed (the NEET rate).
Association of Tertiary Enrollment and Education with potential years of life lost
We wanted to explore if the potential years of life lost rates are affected by tertiary enrollment rates and tertiary adult education levels (Fig. 4 ).
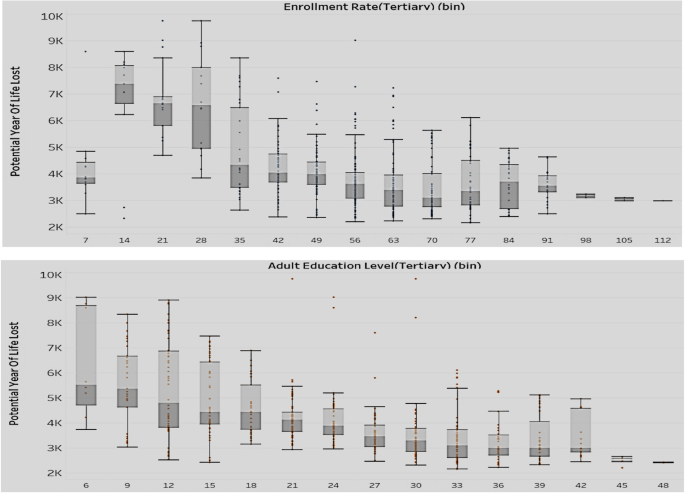
Association of Enrollment rate-tertiary (top) and Adult Education Level-Tertiary (bottom) with Potential Years of Life Lost (Y axis)
The two sets of box plots in Fig. 4 compare the enrollment rates with potential years of life lost (above set) and the education level with potential years of life lost (below set). The analysis is for all countries in the sample. As mentioned earlier, the enrollment rates are expressed as ratios and can exceed 100% if the number of children enrolled at a level (regardless of age) exceed the official population of students in the age group for that level. Potential years of life lost represents the average years a person would have lived, had he/she not died prematurely. The results show that with the rise of tertiary adult education level and tertiary enrollment rate, there is a decrease in both value and variation of the potential years of life lost. We can conclude that lower levels in tertiary education adversely affect a country’s health situation in terms of premature mortality.
Association of Tertiary Enrollment and Education with child vaccination rates
We compared the performance of tertiary education level and enrollment rates with the child vaccination rates (Fig. 5 ) to assess if there was a positive impact of education on preventive healthcare.
Association of Adult Education Level-Tertiary and Enrollment Rate-Tertiary with Child Vaccination Rates
In this analysis (Fig. 5 ), we looked for associations of child vaccination rates with tertiary enrollment and tertiary education. The analysis is for all countries in the sample. The color of the bubble represents the tertiary enrollment rate such that the darker the color, the higher the enrollment rate, and the size of the bubble represents the level of tertiary education. The labels inside the bubbles denote the child vaccination rates. The figure shows a general positive association of high child vaccination rate with tertiary enrollment and tertiary education levels. This indicates that countries that have high child vaccination rates tend to be better at tertiary enrollment and have more adults educated in tertiary institutions. Therefore, countries that focus more on tertiary education and enrollment may confer more health awareness in the population, which can be reflected in improved child vaccination rates.
Association of NEET rates (15–19; 20–24) with infant mortality rates and deaths from Cancer
In the realm of child health, we also looked at the infant mortality rates. We explored if infant mortality rates are associated with the NEET rates in different age groups (Fig. 6 ).
Association of Infant Mortality rates with NEET Rates (15–19) and NEET Rates (20–24)
Figure 6 is a scatterplot that explores the correlation between infant mortality and NEET rates in the age groups 15–19 and 20–24. The data is for all countries in the sample. Most data points are clustered in the lower infant mortality and lower NEET rate range. Infant mortality and NEET rates move in the same direction—as infant mortality increases/decrease, the NEET rate goes up/down. The NEET rate for the age group 20–24 has a slightly higher infant mortality rate than the NEET rate for the age group 15–19. This implies that when people in the age group 20–24 are uneducated or unemployed, the implications on infant mortality are higher than in other age groups. This is a reasonable association, since there is the potential to have more people with children in this age group than in the teenage group. To reduce the risk of infant mortality, governments should decrease NEET rates through promotional programs that disseminate the benefits of being educated, employed, and trained [ 7 ]. Additionally, they can offer financial aid to public schools and companies to offer more resources to raise general health awareness in people.
We looked to see if the distribution of population without employment, education, or training (NEET) in various categories of high, medium, and low impacted the rate of deaths from cancer (Fig. 7 ). Our expectation is that high rates of NEET will positively influence deaths from cancer.
Association of Deaths from Cancer and different NEET Rates
The three pie charts in Fig. 7 show the distribution of deaths from cancer in groups of countries with different NEET rates (high, medium, and low). The analysis includes all countries in the sample. The expectation was that high rates of NEET would be associated with high rates of cancer deaths. Our results, however, show that countries with medium NEET rates tend to have the highest deaths from cancer. Countries with high NEET rates have the lowest deaths from cancer among the three groups. Contrary to expectations, countries with low NEET rates do not show the lowest death rates from cancer. A possible explanation for this can be attributed to the fact that in this group, the people in the labor force may be suffering from work-related hazards including stress, that endanger their health.
Association between adult education levels and health expenditure
It is interesting to note the relationship between health expenditure and adult education levels (Fig. 8 ). We expect them to be positively associated.
Association of Health Expenditure and Adult Education Level-Tertiary & Upper Secondary
Figure 8 shows a heat map with the number of countries in different combinations of groups between tertiary and upper-secondary adult education level. We emphasize the higher levels of adult education. The color of the square shows the average of health expenditure. The plot shows that most of the countries are divided into two clusters. One cluster has a high tertiary education level as well as a high upper-secondary education level and it has high average health expenditure. The other cluster has relatively low tertiary and upper secondary education level with low average health expenditure. Overall, the figure shows a positive correlation between adult education level and compulsory health expenditure. Governments of countries with low levels of education should allocate more health expenditure, which will have an influence on the educational levels. Alternatively, to improve public health, governments can frame educational policies to improve the overall national education level, which then produces more health awareness, contributing to national healthcare.
Association of Compulsory Health Expenditure with NEET rates by country and region
Having explored the relationship between health expenditure and adult education, we then explored the relationship between health expenditure and NEET rates of different countries (Fig. 9 ). We expect compulsory health expenditure to be negatively associated with NEET rates.
Association between Compulsory Health Expenditure and NEET Rate by Country and Region
In Fig. 9 , each box represents a country or region; the size of the box indicates the extent of compulsory health expenditure such that a larger box implies that the country has greater compulsory health expenditure. The intensity of the color of the box represents the NEET rate such that the darker color implies a higher NEET rate. Turkey has the highest NEET rate with low health expenditure. Most European countries such as France, Belgium, Sweden, and Norway have low NEET rates and high health expenditure. The chart shows a general association between low compulsory health expenditure and high NEET rates. The relationship, however, is not consistent, as there are countries with high NEET and high health expenditures. Our suggestion is for most countries to improve the social education for the youth through free training programs and other means to effectively improve the public health while they attempt to raise the compulsory expenditure.
Distribution of life expectancy at birth and tertiary enrollment rate
The distribution of enrollment rate (tertiary) and life expectancy of all the countries in the sample can give an idea of the current status of both education and health (Fig. 10 ). We expect these to be positively associated.
Distribution of Life Expectancy at Birth (years) and Tertiary Enrollment Rate
Figure 10 shows two histograms with the lines representing the distribution of life expectancy at birth and the tertiary enrollment rate of all the countries. The distribution of life expectancy at birth is skewed right, which means most of the countries have quite a high life expectancy and there are few countries with a very low life expectancy. The tertiary enrollment rate has a good distribution, which is closer to a normal distribution. Governments of countries with an extremely low life expectancy should try to identify the cause of this problem and take actions in time to improve the overall national health.
Comparison of adult education levels and deaths from Cancer at various levels of GDP per capita
We wanted to see if various levels of GDP per capita influence the levels of adult education and deaths from cancer in countries (Fig. 11 ).
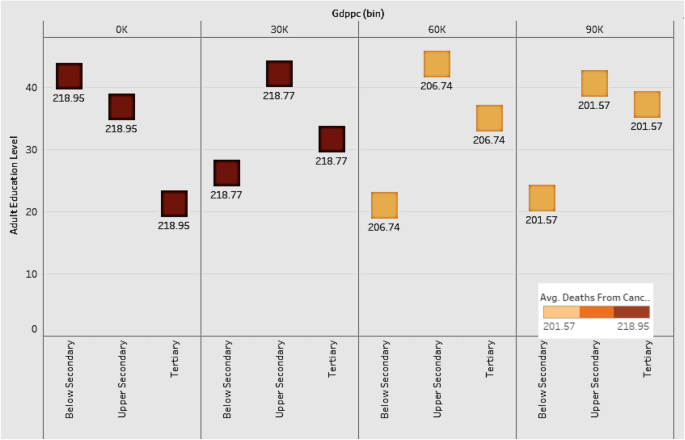
Comparison of Adult Education Levels and Deaths from Cancer at various levels of GDP per capita
Figure 11 shows the distribution of various adult education levels for countries by groups of GDP per capita. The plot shows that as GDP grows, the level of below-secondary adult education becomes lower, and the level of tertiary education gets higher. The upper-secondary education level is constant among all the groups. The implication is that tertiary education is the most important factor among all the education levels for a country to improve its economic power and health level. Countries should therefore focus on tertiary education as a driver of economic development. As for deaths from cancer, countries with lower GDP have higher death rates, indicating the negative association between economic development and deaths from cancer.
Distribution of infant mortality rates by continent
Infant mortality is an important indicator of a country’s health status. Figure 12 shows the distribution of infant mortality for the continents of Asia, Europe, Oceania, North and South America. We grouped the countries in each continent into high, medium, and low, based on infant mortality rates.
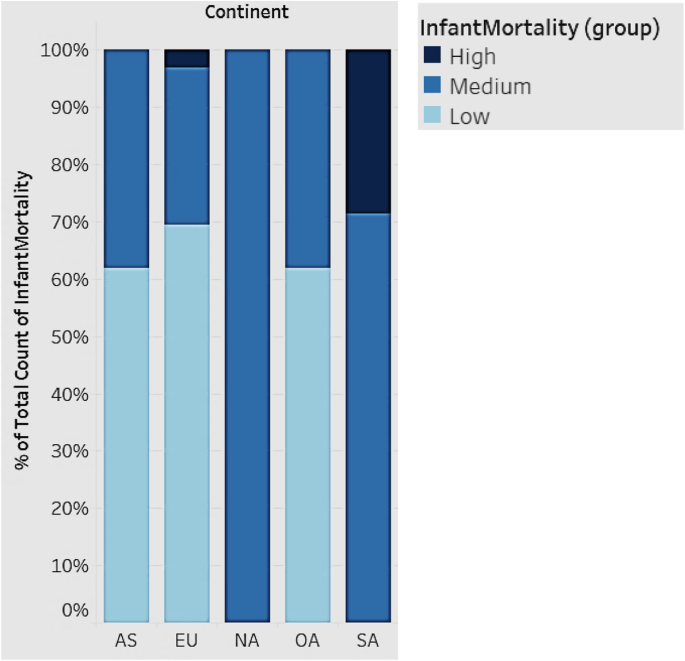
Distribution of Infant Mortality rates by Continent
In Fig. 12 , each bar represents a continent. All countries fall into three groups (high, medium, and low) based on infant mortality rates. South America has the highest infant mortality, followed by Asia, Europe, and Oceania. North America falls in the medium range of infant mortality. South American countries, in general, should strive to improve infant mortality. While Europe, in general, has the lowest infant mortality rates, there are some countries that have high rates as depicted.
Association between child vaccination rates and NEET rates
We looked at the association between child vaccination rates and NEET rates in various countries (Fig. 13 ). We expect countries that have high NEET rates to have low child vaccination rates.
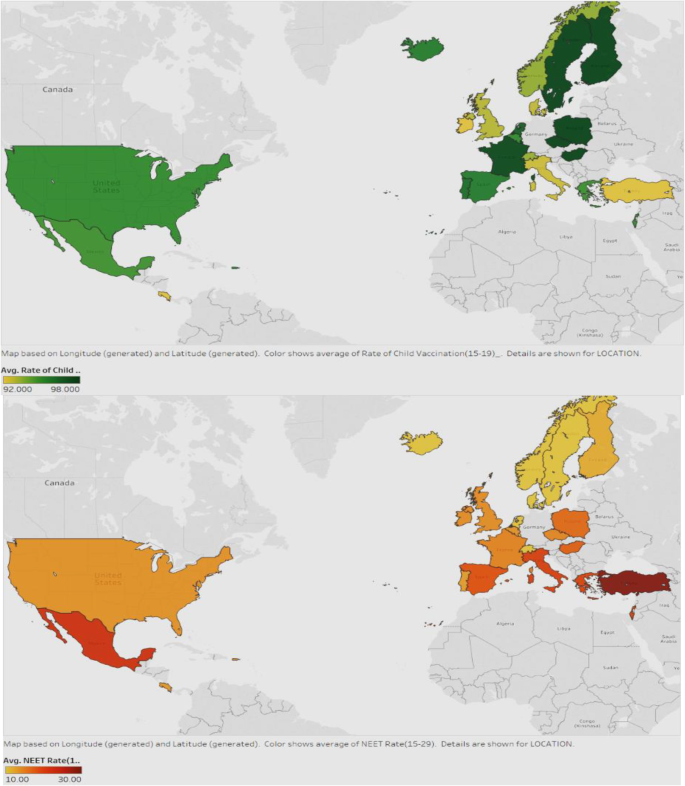
Association between Child Vaccination Rates and NEET rates
Figure 13 displays the child vaccination rates in the first map and the NEET rates in the second map, for all countries. The darker green color shows countries with higher rates of vaccination and the darker red represents those with higher NEET rates. It can be seen that in general, the countries with lower NEET also have better vaccination rates. Examples are USA, UK, Iceland, France, and North European countries. Countries should therefore strive to reduce NEET rates by enrolling a good proportion of the youth into initiatives or programs that will help them be more productive in the future, and be able to afford preventive healthcare for the families, particularly, the children.
Average smoking rate in different continents over time
We compared the trend of average smoking rate for the years 1995–201 for the continents in the sample (Fig. 14 ).
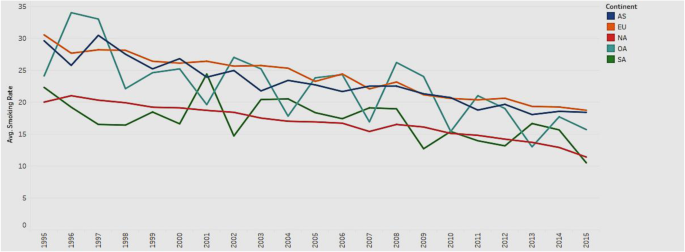
Trend of average smoking rate in different continents from 1995 to 2015
Figure 14 depicts the line charts of average smoking rates for the continents of Asia, Europe, Oceania, North and South America. All the lines show an overall downward trend, which indicates that the average smoking rate decreases with time. The trend illustrates that people have become more health conscious and realize the harmful effects of smoking over time. However, the smoking rate in Europe (EU) is consistently higher than that in other continents, while the smoking rate in North America (NA) is consistently lower over the years. Governments in Europe should pay attention to the usage of tobacco and increase health consciousness among the public.
Association between adult education levels and deaths from Cancer
We explored if adult education levels (below-secondary, upper-secondary, and tertiary) are associated with deaths from cancer (Fig. 15 ) such that higher levels of education will mitigate the rates of deaths from cancer, due to increased awareness and proactive health behavior.
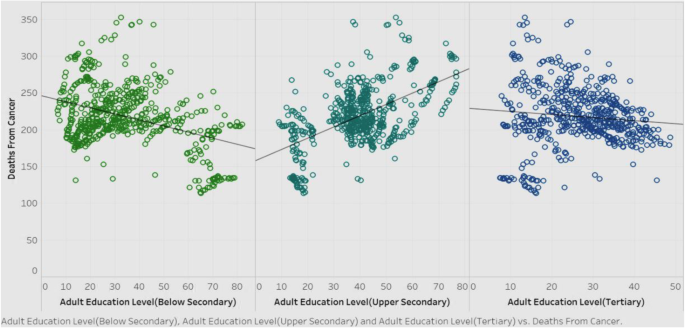
Association of deaths from cancer with adult education levels
Figure 15 shows the correlations of deaths from cancer among the three adult education levels, for all countries in the sample. It is obvious that below-secondary and tertiary adult education levels have a negative correlation with deaths from cancer, while the upper-secondary adult education level shows a positive correlation. Barring upper-secondary results, we can surmise that in general, as education level goes higher, the deaths from cancer will decrease. The rationale for this could be that education fosters more health awareness and encourages people to adopt healthy behavioral practices. Governments should therefore pay attention to frame policies that promote education. However, the counterintuitive result of the positive correlation between upper-secondary levels of adult education with the deaths from cancer warrants more investigation.
We drilled down further into the correlation between the upper-secondary education level and deaths from cancer. Figure 16 shows this correlation, along with a breakdown of the total number of records for each continent, to see if there is an explanation for the unique result.
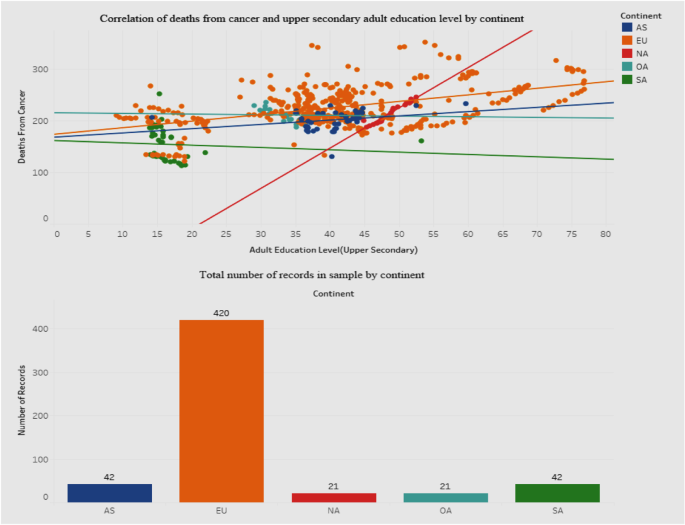
Association between deaths from cancer and adult education level-upper secondary
Figure 16 shows a dashboard containing two graphs - a scatterplot of the correlation between deaths from cancer and education level, and a bar graph showing the breakdown of the total sample by continent. We included a breakdown by continent in order to explore variances that may clarify or explain the positive association for deaths from cancer with the upper-secondary education level. The scatterplot shows that for the European Union (EU) the points are much more scattered than for the other continents. Also, the correlation between deaths and education level for the EU is positive. The bottom bar graph depicts how the sample contains a disproportionately high number of records for the EU than for other continents. It is possible that this may have influenced the results of the correlation. The governments in the EU should investigate the reasons behind this phenomenon. Also, we defer to future research to explore this in greater detail by incorporating other socioeconomic parameters that may have to be factored into the relationship.
Association between average tertiary school life expectancy and health expenditure
We moved our focus to the trends of tertiary school life expectancy and health expenditure from 1995 to 2015 (Fig. 17 ) to check for positive associations.
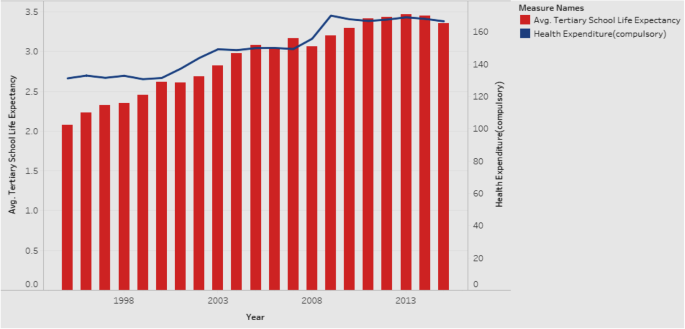
Association between Average Tertiary School Life Expectancy and Health Expenditure
Figure 17 is a combination chart explaining the trends of tertiary school life expectancy and health expenditure, for all countries in the sample. The rationale is that if there is a positive association between the two, it would be worthwhile for the government to allocate more resources towards health expenditure. Both tertiary school life expectancy and health expenditure show an increase over the years from 1995 to 2015. Our additional analysis shows that they continue to increase even after 2015. Hence, governments are encouraged to increase the health expenditure in order to see gains in tertiary school life expectancy, which will have positive implications for national health. Given that the measured effects of education are large, investments in education might prove to be a cost-effective means of achieving better health.
Our results reveal how interlinked education and health can be. We show how a country can improve its health scenario by focusing on appropriate indicators of education. Countries with higher education levels are more likely to have better national health conditions. Among the adult education levels, tertiary education is the most critical indicator influencing healthcare in terms of infant mortality, life expectancy, child vaccination rates, and enrollment rates. Our results emphasize the role that education plays in the potential years of life lost, which is a measure that represents the average years a person would have lived had he/she not died prematurely. In addition to mortality rate, an economy needs to consider this indicator as a measure of health quality.
Other educational indicators that are major drivers of health include school life expectancy, particularly at the tertiary level. In order to improve the school life expectancy of the population, governments should control the number of youths ending up unemployed, dropping out of school, and without skills or training (the NEET rate). Education allows people to gain skills/abilities and knowledge on general health, enhancing their awareness of healthy behaviors and preventive care. By targeting promotions and campaigns that emphasize the importance of skills and employment, governments can reduce the NEET rates. And, by reducing the NEET rates, governments have the potential to address a broad array of vulnerabilities among youth, ranging from unemployment, early school dropouts, and labor market discouragement, which are all social issues that warrant attention in a growing economy.
We also bring to light the health disparities across countries and suggest implications for governments to target educational interventions that can reduce inequalities and improve health, at a macro level. The health effects of education are at the grass roots level - creating better overall self-awareness on personal health and making healthcare more accessible.
Scope and limitations
Our research suffers from a few limitations. For one, the number of countries is limited, and being that the data are primarily drawn from OECD, they pertain to the continent of Europe. We also considered a limited set of variables. A more extensive study can encompass a larger range of variables drawn from heterogeneous sources. With the objective of acquiring a macro perspective on the education–health association, we incorporated some dependent variables that may not traditionally be viewed as pure health parameters. For example, the variable potential years of life lost is affected by premature deaths that may be caused by non-health related factors too. Also there may be some intervening variables in the education–health relationship that need to be considered. Lastly, while our study explores associations and relationships between variables, it does not investigate causality.
Conclusions and future research
Both education and health are at the center of individual and population health and well-being. Conceptualizations of both phenomena should go beyond the individual focus to incorporate and consider the social context and structure within which the education–health relationship is embedded. Such an approach calls for a combination of interdisciplinary research, novel conceptual models, and rich data sources. As health differences are widening across the world, there is need for new directions in research and policy on health returns on education and vice versa. In developing interventions and policies, governments would do well to keep in mind the dual role played by education—as a driver of opportunity as well as a reproducer of inequality [ 36 ]. Reducing these macro-level inequalities requires interventions directed at a macro level. Researchers and policy makers have mutual responsibilities in this endeavor, with researchers investigating and communicating the insights and recommendations to policy makers, and policy makers conveying the challenges and needs of health and educational practices to researchers. Researchers can leverage national differences in the political system to study the impact of various welfare systems on the education–health association. In terms of investment in education, we make a call for governments to focus on education in the early stages of life course so as to prevent the reproduction of social inequalities and change upcoming educational trajectories; we also urge governments to make efforts to mitigate the rising dropout rate in postsecondary enrollment that often leads to detrimental health (e.g., due to stress or rising student debt). There is a need to look into the circumstances that can modify the postsecondary experience of youth so as to improve their health.
Our study offers several prospects for future research. Future research can incorporate geographic and environmental variables—such as the quality of air level or latitude—for additional analysis. Also, we can incorporate data from other sources to include more countries and more variables, especially non-European ones, so as to increase the breadth of analysis. In terms of methodology, future studies can deploy meta-regression analysis to compare the relationships between health and some macro-level socioeconomic indicators [ 13 ]. Future research should also expand beyond the individual to the social context in which education and health are situated. Such an approach will help generate findings that will inform effective educational and health policies and interventions to reduce disparities.
Availability of data and materials
The dataset analyzed during the current study is available from the corresponding author on reasonable request.
Abbreviations
Fundamental Cause Theory
Human Capital Theory
Not in Employment, Education, or Training
Organization for Economic Cooperation and Development
Socio-economic status
Andersen RM, Newman JF. Societal and individual determinants of medical care utilization in the United States. Milbank Mem Fund Q Health Soc. 1973;51(1):95–124.
Article CAS Google Scholar
Andersen RM. Revisiting the behavioral model and access to medical care: does it matter? J Health Social Behav. 1995;36(1):1–10.
Baker DP. The Schooled Society: The Educational Transformation of Global Culture. Stanford, CA: Stanford Univ. Press: 2014; 360.
Becker GS. Human capital: a theoretical and empirical analysis, with special reference to education. Chicago: Univ. Chicago Press; 1964.
Google Scholar
Berkman LF, Syme SL. Social networks, host resistance, and mortality: a nine-year follow-up study of Alameda County residents. Oxford Acad J. 1979;109(2):186–204.
CAS Google Scholar
Crimmins EM, Kim JK, Vasunilashorn S. Biodemography: new approaches to understanding trends and differences in population health and mortality. Demography. 2010;47:S41–64.
Article Google Scholar
Spence M. Job market signalling. The Quarterly J Econ. 1973;87:355–79.
Cutler DM, Lleras-Muney A. Education and Health: Evaluating Theories and Evidence: NBER Working Papers; 2006. p. 12352.
Feinstein L. What are the effects of education on health? OECD Proceedings of the Copenhagen Symposium; 2006 . .
Folkman S, Lazarus RS. An analysis of coping in a middle-aged community sample. J Health Soc Behav. 1980;21(3):219–39.
Freedman VA, Martin LG. The role of education in explaining and forecasting trends in functional limitations among older Americans. Demography. 1999;36(4):461–73.
Freese J, Lutfey K. Fundamental causality: challenges of an animating concept for medical sociology. In: Pescosolido BA, Martin JK, McLeod JD, Rogers A, editors. Handbook of the Sociology of Health, Illness, and Healing: a blueprint for the 21st century. New York: Springer; 2011. p. 67–81.
Chapter Google Scholar
Fouweather T, Gillies C, Wohland P, Van Oyen H, Nusselde W, Robine J, Cambois E, Jagger C. Comparison of socio-economic indicators explaining inequalities in healthy life years at age 50 in Europe: 2005 and 2010. Eur J Pub Health. 2015;25:978–83.
George LK, Gwyther LP. Caregiver Weil-being: a multidimensional examination of family caregivers of demented adults. Gerontologist. 1986;26(3):253–9.
Goldman D, Smith JP. The increasing value of education to health. Soc Sc Med. 2011;72(10):1728–37.
Harper AC, Lambert LJ. The health of populations: an introduction. New York: Springer Publishing Company; 1994.
Health 2020: Education and health through the life-course. WHO Europe Sector Brief on Education Health; 2015. http://www.euro.who.int/__data/assets/pdf_file/0007/324619/Health-2020-Education-and-health-through-the-life-course-en.pdf?ua=1 .
Kino S, Bernabé E, Sabbah W. The role of healthcare and education systems in co-occurrence of health risk behaviours in 27 European countries. Eur J Public Health. 2018;28(1):186–92.
Landerman LR, Burns BJ, Swartz MS, Wagner HR, George LK. The relationship between insurance coverage and psychiatric disorder in predicting use of mental health services. Am J Psychol. 1994;151(12):1785.
Lynch SM. Cohort and life-course patterns in the relationship between education and health: a hierarchical approach. Demography. 2003;40(2):309–31.
Mackenbach J, Kunst A. Measuring the magnitude of socio-economic inequalities in health: an overview of available measures illustrated with two examples from Europe. Soc Sci Med. 1997;44(6):757–71. https://doi.org/10.1016/S0277-9536(96)00073-1 .
Article CAS PubMed Google Scholar
Manton KG, Corder L, Stallard E. Chronic disability trends in elderly United States populations: 1982-1994. Natl Acad Sci. 1997;94(6):2593–8.
Mirowski J, Ross CE. Education, learned effectiveness and health. London Rev Edu. 2005;3(3):205–20.
Montez JK, Berkman LF. Trends in the educational gradient of mortality among US adults aged 45 to 84 years: bringing regional context into the explanation. Am J Pub Health. 2014;104(1):e82–90.
Montez JK, Zajacova A. Trends in mortality risk by education level and cause of death among US white women from 1986 to 2006. Am J Pub Health. 2013;103:473–9.
Olshansky SJ, Antonucci T, Berkman L, Binstock RH, Boersch-Supan A, Cacioppo JT, Carnes BA, Carstensen LL, Fried LP, Goldman DP, Jackson J, Kohli M, Rother J, Zheng Y, Rowe J. Differences in life expectancy due to race and educational differences are widening, and many may not catch up. Health Aff. 2012;31(8):1803–13.
Pamuk ER. Social-class inequality in infant mortality in England and Wales from 1921 to 1980. Eur J Popul 1988; 4 , 1–21, https://doi.org/10.1007/BF01797104.
Phelan JC , Link BG , Tehranifar P . Social conditions as fundamental causes of health inequalities: Theory, evidence, and policy implications . J Health Soc Behav 2010 ; 51 : S28 S40 . doi : 10.1177/0022146510383498.
Renard F, Devleesschauwer B, Speybroeck N, Deboosere P. Monitoring health inequalities when the socio-economic composition changes: are the slope and relative indices of inequality appropriate? Results of a simulation study. BMC Public Health 2019; 19: 662. https://doi.org/10.1186/s12889-019-6980-1.
Ro A, Geronimus A, Bound J, Griffith D, Gee G. Educational gradients in five Asian immigrant populations: do country of origin, duration and generational status moderate the education-health relationship? Prev Med Rep. 2016;4:338–43.
Ross CE, Wu CL. The links between education and health. Am Soc Rev. 1995;60(5):719–45.
Shiels MS, Chernyavskiy P, Anderson WF, Best AF, Haozous EA. Diverging trends in premature mortality in the U.S. by sex, race, and ethnicity in the 21st century. Lancet. 2017;389:1043–54.
Tsou MT. Association of Education, health behaviors, concerns, and knowledge with metabolic syndrome among urban elderly in one medical Center in Taiwan. Int J Gerontology. 2017;11(3:138–43.
Wheaton B. Stress, personal coping resources, and psychiatric symptoms: an investigation of interactive models. J Health Soc Behav. 1983;24(3):208–29.
Williams DR, Collins C. US socioeconomic and racial differences in health: patterns and explanations. Ann Rev Soc. 1995;21:349–86.
Zajacova A, Lawrence EM. The relationship between education and health: reducing disparities through a contextual approach. Ann Rev Pub Health. 2018;39:273–89.
Zimmerman EB, Woolf SH. Understanding the relationship between education and health. Discussion Paper, Inst Med. Washington DC; 2014. https://nam.edu/wp-content/uploads/2015/06/BPH-UnderstandingTheRelationship1.pdf .
Zhong H. An over time analysis on the mechanisms behind the education–health gradients in China. China Econ Rev. 2015;34(C):135–49.
Download references
Acknowledgements
Not applicable.
Author information
Authors and affiliations.
Koppelman School of Business, Brooklyn College of the City University of New York, 2900 Bedford Ave, Brooklyn, NY, 11210, USA
Viju Raghupathi
Gabelli School of Business, Fordham University, 140 W. 62nd Street, New York, NY, 10023, USA
Wullianallur Raghupathi
You can also search for this author in PubMed Google Scholar
Contributions
Both authors contributed equally to all parts of the manuscript.
Corresponding author
Correspondence to Viju Raghupathi .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Raghupathi, V., Raghupathi, W. The influence of education on health: an empirical assessment of OECD countries for the period 1995–2015. Arch Public Health 78 , 20 (2020). https://doi.org/10.1186/s13690-020-00402-5
Download citation
Received : 16 October 2019
Accepted : 26 February 2020
Published : 06 April 2020
DOI : https://doi.org/10.1186/s13690-020-00402-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Education level
- Enrollment rate
- Life expectancy
- Potential years of life lost
- Infant mortality
- Deaths from cancer
Archives of Public Health
ISSN: 2049-3258
- General enquiries: [email protected]
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- HHS Author Manuscripts

The relationship between education and health: reducing disparities through a contextual approach
Anna zajacova.
Western University
Elizabeth M. Lawrence
University of North Carolina
Adults with higher educational attainment live healthier and longer lives compared to their less educated peers. The disparities are large and widening. We posit that understanding the educational and macro-level contexts in which this association occurs is key to reducing health disparities and improving population health. In this paper, we briefly review and critically assess the current state of research on the relationship between education and health in the United States. We then outline three directions for further research: We extend the conceptualization of education beyond attainment and demonstrate the centrality of the schooling process to health; We highlight the dual role of education a driver of opportunity but also a reproducer of inequality; We explain the central role of specific historical socio-political contexts in which the education-health association is embedded. This research agenda can inform policies and effective interventions to reduce health disparities and improve health of all Americans.
URGENT NEED FOR NEW DIRECTIONS IN EDUCATION-HEALTH RESEARCH
Americans have worse health than people in other high-income countries, and have been falling further behind in recent decades ( 137 ). This is partially due to the large health inequalities and poor health of adults with low education ( 84 ). Understanding the health benefits of education is thus integral to reducing health disparities and improving the well-being of 21 st century populations. Despite tremendous prior research, critical questions about the education-health relationship remain unanswered, in part because education and health are intertwined over the lifespans within and across generations and are inextricably embedded in the broader social context.
We posit that to effectively inform future educational and heath policy, we need to capture education ‘in action’ as it generates and constrains opportunity during the early lifespans of today’s cohorts. First, we need to expand our operationalization of education beyond attainment to consider the long-term educational process that precedes the attainment and its effect on health. Second, we need to re-conceptualize education as not only a vehicle for social success, valuable resources, and good health, but also as an institution that reproduces inequality across generations. And third, we argue that investigators need to bring historical, social and policy contexts into the heart of analyses: how does the education-health association vary across place and time, and how do political forces influence that variation?
During the past several generations, education has become the principal pathway to financial security, stable employment, and social success ( 8 ). At the same time, American youth have experienced increasingly unequal educational opportunities that depend on the schools they attend, the neighborhoods they live in, the color of their skin, and the financial resources of their family. The decline in manufacturing and rise of globalization have eroded the middle class, while the increasing returns to higher education magnified the economic gaps among working adults and families ( 107 ). In addition to these dramatic structural changes, policies that protected the welfare of vulnerable groups have been gradually eroded or dismantled ( 129 ). Together, these changes triggered a precipitous growth of economic and social inequalities in the American society ( 17 ; 106 ).
Unsurprisingly, health disparities grew hand in hand with the socio-economic inequalities. Although the average health of the US population improved over the past decades ( 67 ; 85 ), the gains largely went to the most educated groups. Inequalities in health ( 53 ; 77 ; 99 ) and mortality ( 86 ; 115 ) increased steadily, to a point where we now see an unprecedented pattern: health and longevity are deteriorating among those with less education ( 92 ; 99 ; 121 ; 143 ). With the current focus of the media, policymakers, and the public on the worrisome health patterns among less-educated Americans ( 28 ; 29 ), as well as the growing recognition of the importance of education for health ( 84 ), research on the health returns to education is at a critical juncture. A comprehensive research program is needed to understand how education and health are related, in order to identify effective points of intervention to improve population health and reduce disparities.
The article is organized in two parts. First, we review the current state of research on the relationship between education and health. In broad strokes, we summarize the theoretical and empirical foundations of the education-health relationship and critically assess the literature on the mechanisms and causal influence of education on health. In the second part, we highlight gaps in extant research and propose new directions for innovative research that will fill these gaps. The enormous breadth of the literature on education and health necessarily limits the scope of the review in terms of place and time; we focus on the United States and on findings generated during the rapid expansion of the education-health research in the past 10–15 years. The terms “education” and “schooling” are used interchangeably. Unless we state otherwise, both refer to attained education, whether measured in completed years or credentials. For references, we include prior review articles where available, seminal papers, and recent studies as the best starting points for further reading.
THE ASSOCIATION BETWEEN EDUCATION AND HEALTH
Conceptual toolbox for examining the association.
Researchers have generally drawn from three broad theoretical perspectives to hypothesize the relationship between education and health. Much of the education-health research over the past two decades has been grounded in the Fundamental Cause Theory ( 75 ). The FCT posits that social factors such as education are ‘fundamental’ causes of health and disease because they determine access to a multitude of material and non-material resources such as income, safe neighborhoods, or healthier lifestyles, all of which protect or enhance health. The multiplicity of pathways means that even as some mechanisms change or become less important, other mechanisms will continue to channel the fundamental dis/advantages into differential health ( 48 ). The Human Capital Theory (HCT), borrowed from econometrics, conceptualizes education as an investment that yields returns via increased productivity ( 12 ). Education improves individuals’ knowledge, skills, reasoning, effectiveness, and a broad range of other abilities, which can be utilized to produce health ( 93 ). The third approach, the Signaling or Credentialing perspective ( 34 ; 125 ) has been used to explain the observed large discontinuities in health at 12 or 16 years of schooling, typically associated with the receipt of a high school and college degrees, respectively. This perspective views earned credentials as a potent signal about one’s skills and abilities, and emphasizes the economic and social returns to such signals. Thus all three perspectives postulate a causal relationship between education and health and identify numerous mechanisms through which education influences health. The HCT specifies the mechanisms as embodied skills and abilities, FCT emphasizes the dynamism and flexibility of mechanisms, and credentialism identifies social responses to educational attainment. All three theoretical approaches, however, operationalize the complex process of schooling solely in terms of attainment and thus do not focus on differences in educational quality, type, or other institutional factors that might independently influence health. They also focus on individual-level factors: individual attainment, attainment effects, and mechanisms, and leave out the social context in which the education and health processes are embedded.
Observed associations between education and health
Empirically, hundreds of studies have documented “the gradient” whereby more schooling is linked with better health and longer life. A seminal 1973 book by Kitagawa and Hauser powerfully described large differences in mortality by education in the United States ( 71 ), a finding that has since been corroborated in numerous studies ( 31 ; 42 ; 46 ; 109 ; 124 ). In the following decades, nearly all health outcomes were also found strongly patterned by education. Less educated adults report worse general health ( 94 ; 141 ), more chronic conditions ( 68 ; 108 ), and more functional limitations and disability ( 118 ; 119 ; 130 ; 143 ). Objective measures of health, such as biological risk levels, are similarly correlated with educational attainment ( 35 ; 90 ; 140 ), showing that the gradient is not a function of differential reporting or knowledge.
The gradient is evident in men and women ( 139 ) and among all race/ethnic groups ( 36 ). However, meaningful group differences exist ( 60 ; 62 ; 91 ). In particular, education appears to have stronger health effects for women than men ( 111 ) and stronger effects for non-Hispanic whites than minority adults ( 134 ; 135 ) even if the differences are modest for some health outcomes ( 36 ). The observed variations may reflect systematic social differences in the educational process such as quality of schooling, content, or institutional type, as well as different returns to educational attainment in the labor market across population groups ( 26 ). At the same time, the groups share a common macro-level social context, which may underlie the gradient observed for all.
To illustrate the gradient, we analyzed 2002–2016 waves of the National Health Interview Survey (NHIS) data from adults aged 25–64. Figure 1 shows the levels of three health outcomes across educational attainment levels in six major demographic groups predicted at age 45. Three observations are noteworthy. First, the gradient is evident for all outcomes and in all race/ethnic/gender groups. Self-rated health exemplifies the staggering magnitude of the inequalities: White men and women without a high school diploma have about 57% chance of reporting fair or poor health, compared to just 9% for college graduates. Second, there are major group differences as well, both in the predicted levels of health problems, as well as in the education effects. The latter are not necessarily visible in the figures but the education effects are stronger for women and weaker for non-white adults as prior studies showed (table with regression model results underlying the prior statement is available from the authors). Third, an intriguing exception pertains to adults with “some college,” whose health is similar to high school graduates’ in health outcomes other than general health, despite their investment in and exposure to postsecondary education. We discuss this anomaly below.

Predicted Probability of Health Problems
Source: 2002–2016 NHIS Survey, Adults Age 25–64
Pathways through which education impacts health
What explains the improved health and longevity of more educated adults? The most prominent mediating mechanisms can be grouped into four categories: economic, health-behavioral, social-psychological, and access to health care. Education leads to better, more stable jobs that pay higher income and allow families to accumulate wealth that can be used to improve health ( 93 ). The economic factors are an important link between schooling and health, estimated to account for about 30% of the correlation ( 36 ). Health behaviors are undoubtedly an important proximal determinant of health but they only explain a part of the effect of schooling on health: adults with less education are more likely to smoke, have an unhealthy diet, and lack exercise ( 37 ; 73 ; 105 ; 117 ). Social-psychological pathways include successful long-term marriages and other sources of social support to help cope with stressors and daily hassles ( 128 ; 131 ). Interestingly, access to health care, while important to individual and population health overall, has a modest role in explaining health inequalities by education ( 61 ; 112 ; 133 ), highlighting the need to look upstream beyond the health care system toward social factors that underlie social disparities in health. Beyond these four groups of mechanisms that have received the most attention by investigators, many others have been examined, such as stress, cognitive and noncognitive skills, or environmental exposures ( 11 ; 43 ). Several excellent reviews further discuss mechanisms ( 2 ; 36 ; 66 ; 70 ; 93 ).
Causal interpretation of the education-health association
A burgeoning number of studies used innovative approaches such as natural experiments and twin design to test whether and how education causally affects health. These analyses are essential because recommendations for educational policies, programs, and interventions seeking to improve population health hinge on the causal impact of schooling on health outcomes. Overall, this literature shows that attainment, measured mostly in completed years of schooling, has a causal impact on health across numerous (though not all) contexts and outcomes.
Natural experiments take advantage of external changes that affect attainment but are unrelated to health, such as compulsory education reforms that raise the minimum years of schooling within a given population. A seminal 2005 study focused on increases in compulsory education between 1915 and 1939 across US states and found that a year of schooling reduced mortality by 3.6% ( 78 ). A re-analysis of the data indicated that taking into account state-level mortality trends rendered the mortality effects null but it also identified a significant and large causal effect on general health ( 88 ). A recent study of a large sample of older Americans reported a similar pattern: a substantial causal effect of education for self-rated health but not for mortality ( 47 ). School reform studies outside the US have reported compelling ( 122 ) or modest but significant ( 32 ) effects of schooling on health, although some studies have found nonsignificant ( 4 ), or even negative effects ( 7 ) for a range of health outcomes.
Twin design studies compare the health of twins with different levels of education. This design minimizes the influence of family resources and genetic differences in skills and health, especially for monozygotic twins, and thus serves to isolate the effect of schooling. In the US, studies using this design generated robust evidence of a causal effect of education on self-rated health ( 79 ), although some research has identified only modest ( 49 ) or not significant ( 3 ; 55 ) effects for other physical and mental health outcomes. Studies drawing on the large twin samples outside of the US have similarly found strong causal effects for mortality ( 80 ) and health ( 14 ; 16 ; 51 ) but again some analyses yielded no causal effects on health ( 13 ; 83 ) or health behaviors ( 14 ). Beyond our brief overview, readers may wish consult additional comprehensive reviews of the causal studies ( 40 ; 45 ; 89 ).
The causal studies add valuable evidence that educational attainment impacts adult health and mortality, even considering some limitations to their internal validity ( 15 ; 88 ). To improve population health and reduce health disparities, however, they should be viewed as a starting point to further research. First, the findings do not show how to improve the quality of schooling or its quantity for in the aggregate population, or how to overcome systematic intergenerational and social differences in educational opportunities. Second, their findings do take into account contexts and conditions in which educational attainment might be particularly important for health. In fact, the variability in the findings may be attributable to the stark differences in contexts across the studies, which include countries characterized by different political systems, different population groups, and birth cohorts ranging from the late 19 th to late 20 th centuries that were exposed to education at very different stages of the educational expansion process ( 9 ).
TOWARD A SOCIALLY-EMBEDDED UNDERSTANDING OF THE EDUCATION-HEALTH RELATIONSHIP
To date, the extensive research we briefly reviewed above has identified substantial health benefits of educational attainment in most contexts in today’s high-income countries. Still, many important questions remain unanswered. We outline three critical directions to gain a deeper understanding of the education-health relationship with particular relevance for policy development. All three directions shift the education-health paradigm to consider how education and health are embedded in life course and social contexts.
First, nearly universally, the education-health literature conceptualizes and operationalizes education in terms of attainment, as years of schooling or completed credentials. However, attainment is only the endpoint, although undoubtedly important, of an extended and extensive process of formal schooling, where institutional quality, type, content, peers, teachers, and many other individual, institutional, and interpersonal factors shape lifecourse trajectories of schooling and health. Understanding the role of the schooling process in health outcome is relevant for policy because it can show whether interventions should be aimed at increasing attainment, or whether it is more important to increase quality, change content, or otherwise improve the educational process at earlier stages for maximum health returns. Second, most studies have implicitly or explicitly treated educational attainment as an exogenous starting point, a driver of opportunities in adulthood. However, education also functions to reproduce inequality across generations. The explicit recognition of the dual function of education is critical to developing education policies that would avoid unintended consequence of increasing inequalities. And third, the review above indicates substantial variation in the education-health association across different historical and social contexts. Education and health are inextricably embedded in these contexts and analyses should therefore include them as fundamental influences on the education-health association. Research on contextual variation has the potential to identify contextual characteristics and even specific policies that exacerbate or reduce educational disparities in health.
We illustrate the key conceptual components of future research into the education-health relationship in Figure 2 . Important intergenerational and individual socio-demographic factors shape educational opportunities and educational trajectories, which are directly related to and captured in measures of educational attainment. This longitudinal and life course process culminates in educational disparities in adult health and mortality. Importantly, the macro-level context underlies every step of this process, shaping each of the concepts and their relationships.

Enriching the conceptualization of educational attainment
In most studies of the education-health associations, educational attainment is modeled using years of schooling, typically specified as a continuous covariate, effectively constraining each additional year to have the same impact. A growing body of research has substituted earned credentials for years. Few studies, however, have considered how the impact of additional schooling is likely to differ across the educational attainment spectrum. For example, one additional year of education compared to zero years may be life-changing by imparting basic literacy and numeracy skills. The completion of 14 rather than 13 years (without the completion of associated degree) could be associated with better health through the accumulation of additional knowledge and skills as well, or perhaps could be without health returns, if it is associated with poor grades, stigma linked to dropping out of college, or accumulated debt ( 63 ; 76 ). Examining the functional form of the education-health association can shed light on how and why education is beneficial for health ( 70 ). For instance, studies found that mortality gradually declines with years of schooling at low levels of educational attainment, with large discontinuities at high school and college degree attainment ( 56 ; 98 ). Such findings can point to the importance of completing a degree, not just increasing the quantity (years) of education. Examining mortality, however, implicitly focused on cohorts who went to school 50–60 years ago, within very different educational and social contexts. For findings relevant to current education policies, we need to focus on examining more recent birth cohorts.
A particularly provocative and noteworthy aspect of the functional form is the attainment group often identified as “some college:” adults who attended college but did not graduate with a four-year degree. Postsecondary educational experiences are increasingly central to the lives of American adults ( 27 ) and college completion has become the minimum requirement for entry into middle class ( 65 ; 87 ). Among high school graduates, over 70% enroll in college ( 22 ) but the majority never earn a four-year degree ( 113 ). In fact,, the largest education-attainment group among non-elderly US adults comprises the 54 million adults (29% of total) with some college or associate’s degree ( 113 ). However, as in Figure 1 , this group often defies the standard gradient in health. Several recent studies have found that the health returns to their postsecondary investments are marginal at best ( 110 ; 123 ; 142 ; 144 ). This finding should spur new research to understand the outcomes of this large population group, and to glean insights into the health returns to the postsecondary schooling process. For instance, in the absence of earning a degree, is greater exposure to college education in terms of semesters or earned credits associated with better health or not? How do the returns to postsecondary schooling differ across the heterogeneous institutions ranging from selective 4-year to for-profit community colleges? How does accumulated college debt influence both dropout and later health? Can we identify circumstances under which some college education is beneficial for health? Understanding the health outcomes for this attainment group can shed light on the aspects of education that are most important for improving health.
A related point pertains to the reliability and validity of self-reported educational attainment. If a respondent reports 16 completed years of education, for example, are they carefully counting the number of years of enrollment, or is 16 shorthand for “completed college”? And, is 16 years the best indicator of college completion in the current context when the median time to earn a four-year degree exceeds 5 years ( 30 )? And, is longer time in college given a degree beneficial for health or does it signify delayed or disrupted educational pathways linked to weaker health benefits ( 132 )? How should we measure part-time enrollment? As studies begin to adjudicate between the health effects of years versus credentials ( 74 ) in the changing landscape of increasingly ‘nontraditional’ pathways through college ( 132 ), this measurement work will be necessary for unbiased and meaningful analyses. An in-depth understanding may necessitate primary data collection and qualitative studies. A feasible direction available with existing data such as the National Longitudinal Survey of Youth 1997 (NLSY97) is to assess earned college credits and grades rather than years of education beyond high school.
As indicated in Figure 2 , beyond a more in-depth usage of the attainment information, we argue that more effective conceptualization of the education-health relationship as a developmental life course process will lead to important findings. For instance, two studies published in 2016 used the NLSY97 data to model how gradual increases in education predict within-individual changes in health ( 39 ; 81 ). Both research teams found that gradual accumulation of schooling quantity over time was not associated with gradual improvements in health. The investigators interpreted the null findings as an absence of causal effects of education on health, especially once they included important confounders (defined as cognitive and noncognitive skills and social background). Alternatively, perhaps the within-individual models did not register health because education is a long-term, developing trajectory that cannot be reduced to point-in-time changes in exposure. Criticisms about the technical aspects of theses studies notwithstanding ( 59 ), we believe that these studies and others like them, which wrestle with the question of how to capture education as a long-term process grounded in the broader social context, and how this process is linked to adult health, are desirable and necessary.
Education as (re)producer of inequality
The predominant theoretical framework for studying education and health focuses on how education increases skills, improves problem-solving, enhances employment prospects, and thus opens access to other resources. In sociology, however, education is viewed not (only) as increasing human capital but as a “sieve more than a ladder” ( 126 ), an institution that reproduces inequality across generations ( 54 ; 65 ; 103 ; 114 ). The mechanisms of the reproduction of inequality are multifarious, encompassing systematic differences in school resources, quality of instruction, academic opportunities, peer influences, or teacher expectations ( 54 ; 114 ; 132 ). The dual role of education, both engendering and constraining social opportunities, has been recognized from the discipline’s inception ( 52 ) and has remained the dominant perspective in sociology of education ( 18 ; 126 ). Health disparities research, which has largely dismissed the this perspective as “specious” ( 93 ), could benefit from pivoting toward this complex sociological paradigm.
As demonstrated in Figure 2 , parental SES and other background characteristics are key social determinants that set the stage for one’s educational experiences ( 20 ; 120 ). These characteristics, however, shape not just attainment, but the entire educational and social trajectories that drive and result in particular attainment ( 21 ; 69 ). Their effects range from the differential quality and experiences in daycare or preschool settings ( 6 ), K-12 education ( 24 ; 136 ), as well as postsecondary schooling ( 5 ; 127 ). As a result of systematically different experiences of schooling over the early life course stratified by parental SES, children of low educated parents are unlikely to complete higher education: over half of individuals with college degrees by age 24 came from families in the top quartile of family income compared to just 10% in the bottom quartile ( 23 ).
Unfortunately, prior research has generally operationalized the differences in educational opportunities as confounders of the education-health association or as “selection bias” to be statistically controlled, or best as a moderating influence ( 10 ; 19 ). Rather than remove the important life course effects from the equation, studies that seek to understand how educational and health differences unfold over the life course, and even across generations could yield greater insight ( 50 ; 70 ). A life course, multigenerational approach can provide important recommendations for interventions seeking to avoid the unintended consequence of increasing disparities. Insofar as socially advantaged individuals are generally better positioned to take advantage of interventions, research findings can be used to ensure that policies and programs result in decreasing, rather than unintentionally widening, educational and health disparities.
Education and health in social context
Finally, perhaps the most important and policy-relevant emerging direction to improving our understanding of the education-health relationship is to view both as inextricably embedded within the broad social context. As we highlight in Figure 2 , this context underlies every feature of the development of educational disparities in health. In contrast to the voluminous literature focusing on individual-level schooling and health, there has been a “startling lack of attention to the social/political/economic context” in which the relationships are grounded ( 33 ). By context, we mean the structure of a society that varies across time and place, encompassing all major institutions, policy environments, as well as gender, race/ethnicity, age, and socioeconomic stratification. Under what circumstances, conditions, and policies are the associations between education and health stronger or weaker?
Within the United States, the most relevant units of geo-political boundaries generating distinct policy contexts are states, although smaller geographic units are also pertinent ( 44 ; 100 ). Since the 1980s, the federal government has devolved an increasing range of key socioeconomic, political, and health-care decisions to states. This decentralization has resulted in increasing diversity across states in conditions for a healthy life ( 96 ; 101 ). A recent study demonstrates how different environments across US states yield vastly different health returns to education ( 100 ). State-level characteristics had little impact on adults with high education, whose disability levels were similarly low regardless of their state of residence. In contrast, disability levels of low-educated adults were not only high but also varied substantially across states: disability was particularly high in states that have invested less in the social welfare of its residents, such as Mississippi, Kentucky, and West Virginia. Highly-educated adults, particularly white adults and men who can convert education into other resources most readily, use personal resources to protect their health like a ‘personal firewall’ ( 97 ). Their less-educated peers, meanwhile, are vulnerable without social safety nets. Demonstrating the potential for informing policy in this area, the findings directly identify state policies that influence the extent to which educational attainment matters for health and longevity. These include economic policies including state income tax structures and education expenditures per capita, as well as policies influencing social cohesion in a state, such as income inequality and unemployment rates. Beyond the US, investigators can leverage differences in political systems across countries to assess the impact of different welfare regimes on the education-health associations, as some European researchers began generating ( 41 ; 82 ).
Similar to variation across geo-political boundaries, research on variation across time can highlight policies and conditions that mitigate or inflate health disparities. How has the education-health association changed over time? In recent decades, the association has become increasingly strong, with widening disparities in health outcomes across education ( 53 ; 77 ; 86 ; 116 ; 143 ). These increases started in the 1980s ( 17 ) at the same time that social inequality began rising with the political embrace of pro-market neoliberal policies ( 33 ). Since then, the United States has been increasingly marked by plummeting economic wellbeing (except for the wealthiest Americans), growing economic segregation, emerging mass incarceration, downward social mobility, and despair in many working-class communities ( 17 ; 95 ; 129 ). Conversely, in the two decades prior (1960s and 70s), social disparities in health were decreasing ( 1 ; 72 ). During those decades, many pro-social policies such as Civil rights legislation, War on Poverty programs, and racial desegregation were improving social inequalities. Macro-level political forces, clearly, can influence not only social but also health inequalities ( 104 ). Two facts follow: growing disparities are not inevitable and changes in the education-health relationship may be strongly linked to social policies. While some of the growth in educational inequalities may be attributable to changes in educational composition of the population with increasingly negatively select groups of adults at the lowest levels of schooling, these compositional changes likely play only a minor role in the overall trends ( 38 ; 58 ). Linking education and health to the broader social context brings to the forefront the ways in which we, as individuals and a collective society, produce and maintain health disparities.
Implications for Policy and Practice
Reducing macro-level inequalities in health will require macro-level interventions. Technological progress and educational expansion over the past several decades have not decreased disparities; on the contrary, educational disparities in health and mortality have grown in the US. Moreover, the consistent, durable relationship between education and health and the multitude of mechanisms linking them suggests that programs targeting individual behaviors will have limited impact to counteract disparities. Thus, we argue that future findings from the new research directions proposed here can be used to intervene at the level of social contexts to alter educational trajectories from an early age, with the ultimate goal of reducing health disparities. We note two promising avenues for policy development.
One potential solution may focus on universal federal and state-level investment in the education and well-being of children early in the life course to disrupt the reproduction of social inequalities and change subsequent educational trajectories. Several experimental early-education programs such as the Perry Preschool Project and Carolina Abecedarian Project have demonstrated substantial, lasting, and wide-ranging benefits, including improved adult health ( 25 ; 57 ; 102 ). These programs provided intensive, exceptionally high-quality, and diverse services to children, and it is these characteristics that appear central to their success ( 138 ). Further research on the qualitative and social dimensions of education and their effects on health can inform future model educational programs and interventions across all ages.
Another important issue for both researchers and policymakers pertains to postsecondary enrollment and attrition, and their effects on health. Educational expansion in the college-for-all era has yielded high post-secondary enrollment, but also unacceptable dropout rates with multiple detrimental consequences, including high rates of student debt ( 64 ) and stigma ( 76 ), which may negatively affect health. Emerging studies found that college dropouts fail to benefit from their postsecondary investments. Next we need to understand under what circumstances college goers do reap health benefits, or how their postsecondary experience can be modified to improve their health.
For both of these avenues, effective implementation will need further research on the specific institutional characteristics and social contexts that shape the schooling effects. However, in designing interventions and policies, we need to be aware of the dual role of education as a drive and reproducer of inequality. Individuals from advantaged backgrounds may be better positioned to take advantage of new educational opportunities, and thus any interventions and programs need to ensure that marginalized populations have equal or greater access in order to avoid the unintended consequence of further intensifying disparities. Finally, researchers and policymakers should engage in a dialogue such that researchers effectively communicate their insights and recommendations to policymakers, and policymakers convey the needs and challenges of their practices to researchers.
Education and health are central to individual and population well-being. They are also inextricably embedded in the social context and structure. Future research needs to expand beyond the individual-focused analyses and hypothesize upstream ( 96 ), taking a contextual approach to understanding education and health. Such an approach will require interdisciplinary collaborations, innovations in conceptual models, and rich data sources. The three directions for further research on health returns to education we outlined above can help generate findings that will inform effective educational and health policies and interventions to reduce disparities. During this critical time when health differences are widening and less educated Americans are experiencing social and health declines, research and policy has the opportunity to make a difference and improve the health and well-being of our population.
Contributor Information
Anna Zajacova, Western University.
Elizabeth M. Lawrence, University of North Carolina.
Health Education and Health Promotion: Key Concepts and Exemplary Evidence to Support Them
- First Online: 09 October 2018
Cite this chapter

- Hein de Vries 8 ,
- Stef P. J. Kremers 8 &
- Sonia Lippke 9
3321 Accesses
12 Citations
Health is regarded as the result of an interaction between individual and environmental factors. While health education is the process of educating people about health and how they can influence their health, health promotion targets not only people but also their environments. Promoting health behavior can take place at the micro level (the personal level), the meso level (the organizational level, including e.g. families, schools and worksites) and at the macro level (the (inter)national level, including e.g. governments). Health education is one of the methods used in health promotion, with health promotion extending beyond just health education.
Models and theories that focus on understanding health and health behavior are of key importance for health education and health promotion. Different classes of models and theories can be distinguished, such as planning models, behavioral change models, and diffusion models. Within these models different topics and factors are relevant, ranging from health literacy, attitudes, social influences, self-efficacy, planning, and stages of change to evaluation, implementation, stakeholder involvement, and policy changes. Exemplary health promotion settings are schools, worksites, and healthcare, but also the domains that are involved with policy development. Main health promotion methods can involve a variety of different methods and approaches, such as counseling, brochures, eHealth, stakeholder involvement, consensus meetings, community ownership, panel discussions, and policy development. Because health education and health promotion should be theory- and evidence-based, personalized interventions are recommended to take empirical findings and proven theoretical assumptions into account.
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
Institutional subscriptions
Similar content being viewed by others

Health Promotion Practice

Principled Health Promotion Research: A Comprehensive and Action-Oriented Approach
Aarts, H., Paulussen, T., & Schaalma, H. (1997). Physical exercise habit: On the conceptualization and formation of habitual health behaviours. Health Education Research, 12 (3), 363.
Article PubMed Google Scholar
Abraham, C., & Michie, S. (2008). A taxonomy of behavior change techniques used in interventions. Health Psychology, 27 (3), 379–387.
Abraham, C., & Sheeran, P. (2003). Acting on intentions: The role of anticipated regret. The British Journal of Social Psychology, 42 (Pt 4), 495–511.
Abraham, C., & Sheeran, P. (2005). The Health Belief Model. In M. Conner & P. Norman (Eds.), Predicting health behaviour (pp. 28–80). Berkshire: Open University Press.
Google Scholar
Abroms, L. C., & Maibach, E. W. (2008). The effectiveness of mass communication to change public behavior. Annual Review of Public Health, 29 , 219–234.
Adams, J., & White, M. (2003). Are activity promotion interventions based on the transtheoretical model effective? A critical review. British Journal of Sports Medicine, 37 (2), 106–114.
Article PubMed PubMed Central Google Scholar
Ajzen, I. (1988). Attitudes, personality, and behavior . Chicago: Dorsey Press.
Ajzen, I. (1991). The theory of planned behavior. Organizational Behavior and Human Decision Processes, 50 (2), 179–211.
Article Google Scholar
Ajzen, I., & Fishbein, M. (1980). Understanding attitudes and predicting social behavior . Englewood Cliffs: Prentice-Hall.
Aldana, S. G., Merrill, R. M., Price, K., Hardy, A., & Hager, R. (2005). Financial impact of a comprehensive multisite workplace health promotion program. Preventive Medicine, 40 (2), 131–137.
Alderman, M. H., & Schoenbaum, E. E. (1975). Detection and treatment of hypertension at the work site. The New England Journal of Medicine, 293 (2), 65–68.
Armitage, C. J. (2009). Is there utility in the transtheoretical model? British Journal of Health Psychology, 14 (2), 195–210.
Armitage, C. J. (2004). Evidence that implementation intentions reduce dietary fat intake: A randomized trial. Health Psychology, 23 (3), 319.
Armitage, C. J., & Conner, M. (2001). Efficacy of the theory of planned behaviour: A meta-analytic review. The British Journal of Social Psychology, 40 (Pt 4), 471–499.
Armstrong, N., & Powell, J. (2008). Preliminary test of an Internet-based diabetes self-management tool. Journal of Telemedicine and Telecare, 14 (3), 114–116.
Asch, S. E. (1956). Studies of independence and conformity: I. A minority of one against a unanimous majority. Psychological Monographs, 70 (9), 1.
Ashford, S., Edmunds, J., & French, D. P. (2010). What is the best way to change self-efficacy to promote lifestyle and recreational physical activity? A systematic review with meta-analysis. British Journal of Health Psychology, 15 (Pt 2), 265–288.
Ausems, M., Mesters, I., van Breukelen, G., & De Vries, H. (2004). Effects of in-school and tailored out-of-school smoking prevention among Dutch vocational school students. Health Education Research, 19 (1), 51–63.
Austin, J. T., & Vancouver, J. B. (1996). Goal constructs in psychology: Structure, process, and content. Psychological Bulletin, 120 (3), 338.
Aveyard, P., Massey, L., Parsons, A., Manaseki, S., & Griffin, C. (2009). The effect of Transtheoretical Model based interventions on smoking cessation. Social science and medicine, 68 (3), 397–403.
Babbin, S. F., Harrington, M., Burditt, C., Redding, C., Paiva, A., Meier, K., Oatley, K., McGee, H., & Velicer, W. F. (2011). Prevention of alcohol use in middle school students: Psychometric assessment of the decisional balance inventory. Addictive Behaviors, 36 (5), 543–546.
Bagozzi, R. P. (1992). The self-regulation of attitudes, intentions, and behavior. Social Psychology Quarterly, 55 (2), 178.
Bagozzi, R. P., & Dholakia, U. (1999). Goal setting and goal striving in consumer behavior. Journal of Marketing, 63 , 19–32.
Baker, D. W., Parker, R. M., Williams, M. V., & Clark, W. S. (1998). Health literacy and the risk of hospital admission. Journal of General Internal Medicine, 13 (12), 791–798.
Bandura, A. (1977). Social learning theory . New York: General Learning Press.
Bandura, A. (1986). Social foundations of thought and action: A social cognitive theory . Englewood Cliffs: Prentice-Hall.
Bandura, A. (1989). Human agency in social cognitive theory. American Psychologist, 44 (9), 1175–1184.
Bandura, A. (1993). Perceived self-efficacy in cognitive development and functioning. Educational Psychologist, 28 (2), 117–148.
Bandura, A. (1997). Editorial. American Journal of Health Promotion, 12 (1), 8–10.
Bargh, J. A. (2005). Bypassing the will: Toward demystifying the nonconscious control of social behavior. In R. R. Hassin, J. S. Uleman, & J. A. Bargh (Eds.), The new unconscious (pp. 37–58). New York: Oxford University Press.
Bartholomew, L. K., Parcel, G. S., Kok, G., & Gottlieb, N. H. (2001). Intervention-mapping: Designing theory and evidence-based health promotion programs . Mountain View: Mayfield.
Bartholomew, L. K., Parcel, G. S., Kok, G., Gottlieb, N. H., & Fernández, M. E. (2011). Planning health promotion: An intervention mapping approach (3rd ed.). San Francisco: Jossey Bass.
Bentz, C. J., Bruce Bayley, K., Bonin, K. E., Fleming, L., Hollis, J. F., Hunt, J. S., LeBlanc, B., McAfee, T., Payne, N., & Siemienczuk, J. (2007). Provider feedback to improve 5A’s tobacco cessation in primary care: A cluster randomized clinical trial. Nicotine & Tobacco Research, 9 (3), 341–349.
Berkman, L. F., & Syme, S. L. (1979). Social networks, host resistance, and mortality: A nine-year follow-up study of Alameda County residents. American Journal of Epidemiology, 109 (2), 186–204.
Beyer, J. M., & Trice, H. M. (1978). Implementing change: Alcoholism policies in work organization . New York: Free Press.
Blissmer, B., & McAuley, E. (2002). Testing the requirements of stages of physical activity among adults: The comparative effectiveness of stage-matched, mismatched, standard care, and control interventions. Annals of Behavioral Medicine, 24 (3), 181–189.
Bodenheimer, T., Lorig, K., Holman, H., & Grumbach, K. (2002). Patient self-management of chronic disease in primary care. JAMA, 288 (19), 2469–2475.
Boer, H., & Seydel, E. R. (1996). Protection motivation theory. In M. Conner & P. Norman (Eds.), Predicting health behavior (pp. 95–120). Buckingham: Open University Press.
Bolman, C., Arwert, T. G., & Vollink, T. (2011). Adherence to prophylactic asthma medication: Habit strength and cognitions. Heart & Lung, 40 (1), 63–75.
Bonfadelli, H. (2002). Medieninhaltsforschung: Grundlagen, Methoden, Anwendungen . Konstanz: UVK.
Borland, R., Balmford, J., Segan, C., Livingston, P., & Owen, N. (2003). The effectiveness of personalized smoking cessation strategies for callers to a Quitline service. Addiction, 98 (6), 837–846.
Botvin, G. J., Eng, A., & Williams, C. L. (1980). Preventing the onset of cigarette smoking through life skills training. Preventive Medicine, 9 (1), 135–143.
Botvin, G. J., & Griffin, K. W. (2004). Life skills training: Empirical findings and future directions. The Journal of Primary Prevention, 25 (2), 211.
Bracht, N. (1990). Community organization principles in health promotion: A five-stage model. In N. Bracht & L. Kingsbury (Eds.), Health promotion at the community level . Thousand Oaks: Sage.
Bracht, N. (1999). Health promotion at the community level: New advances . Thousand Oaks: Sage.
Brewer, N. T., Weinstein, N. D., Cuite, C. L., & Herrington, J. E. (2004). Risk perceptions and their relation to risk behavior. Annals of Behavioral Medicine, 27 (2), 125.
Brewer, N. T., Brewer, N. T., & Fazekas, K. I. (2007). Predictors of HPV vaccine acceptability: A theory-informed, systematic review. Preventive Medicine: An International Journal Devoted to Practice and Theory, 45 (2–3), 107.
Brinn, M. P., Carson, K. V., Esterman, A. J., Chang, A. B., & Smith, B. J. (2010). Mass media interventions for preventing smoking in young people. Cochrane Database of Systematic Reviews, 11 , CD001006.
Britt, E., Hudson, S. M., & Blampied, N. M. (2004). Motivational interviewing in health settings: A review. Patient Education and Counseling, 53 (2), 147–155.
Brodie, M., Flournoy, R. E., Altman, D. E., Blendon, R. J., Benson, J. M., & Rosenbaum, M. D. (2000). Health information, the Internet, and the digital divide. Health Affairs (Millwood), 19 (6), 255–265.
Brouwer, W., Oenema, A., Raat, H., Crutzen, R., de Nooijer, J., de Vries, N. K., & Brug, J. (2010). Characteristics of visitors and revisitors to an Internet-delivered computer-tailored lifestyle intervention implemented for use by the general public. Health Education Research, 25 (4), 585–595.
Brown, T., & Summerbell, C. (2009). Systematic review of school-based interventions that focus on changing dietary intake and physical activity levels to prevent childhood obesity: An update to the obesity guidance produced by the National Institute for Health and Clinical Excellence. Obesity Reviews, 10 (1), 110–141.
Brug, J., Lechner, L., & De Vries, H. (1995). Psychosocial determinants of fruit and vegetable consumption. Appetite, 25 (3), 285.
Brug, J., Steenhuis, I., van Assema, P., & de Vries, H. (1996). The impact of a computer-tailored nutrition intervention. Preventive Medicine, 25 (3), 236–242.
Brug, J., Steenhuis, I. H. M., Van Assema, P., Glanz, K., & De Vries, H. (1999). The impact of two computer tailored nutrition education interventions. Health Education Research, 14 , 249–256.
Brug, J., Conner, M., Harré, N., Kremers, S., McKellar, S., & Whitelaw, S. (2005). The transtheoretical model and stages of change: A critique. Observations by five commentators on the paper by Adams, J., & White, M. (2004). Why don’t stage-based activity promotion interventions work? Health Education Research, 20 (2), 244.
Bruvold, W. H. (1993). A meta-analysis of adolescent smoking prevention programs. American Journal of Public Health, 83 (6), 872.
Bryan, A., Fisher, J. D., & Fisher, W. A. (2002). Tests of the mediational role of preparatory safer sexual behavior in the context of the theory of planned behavior. Health Psychology, 21 (1), 71–80.
Campbell, M. K., Demark-Wahnefried, W., Symons, M., Kalsbeek, W. D., Dodds, J., Cowan, A., Jackson, B., Motsinger, B., Hoben, K., Lashley, J., Demissie, S., & McClelland, J. W. (1999). Fruit and vegetable consumption and prevention of cancer: The Black Churches United for Better Health project. American Journal of Public Health, 89 (9), 1390–1396.
Chaiken, S., Liberman, A., & Eagly, A. H. (1989). Heuristic and systematic information processing within and beyond the persuasion context. In J. S. Uleman & J. A. Bargh (Eds.), Unintended thought . New York: The Guilford Press.
Charles, C., Whelan, T., & Gafni, A. (1999). What do we mean by partnership in making decisions about treatment? BMJ, 319 (7212), 780–782.
Chinn, M. D., & Fairlie, R. W. (2007). The determinants of the global digital divide: A cross-country analysis of computer and internet penetration. Oxford Economic Papers, 16 , f-44.
Cohen, S., & Wills, T. A. (1985). Stress, social support, and the buffering hypothesis. Psychological Bulletin, 98 (2), 310.
Collins, J. L. (1982, March). Self-efficacy and ability in achievement behavior. Paper presented at the annual meeting of the American Educational Research Association, New York.
Conner, M., & Norman, P. (2005). Predicting health behaviour: Research and practice with social cognition models . Maidenhead: Open University Press.
Conner, M., & Armitage, C. J. (1998). Extending the theory of planned behavior: A review and avenues for further research. Journal of Applied Social Psychology, 28 (15), 1429.
Conner, M., Godin, G., Sheeran, P., & Germain, M. (2013). Some feelings are more important: Cognitive attitudes, affective attitudes, anticipated affect, and blood donation. Health Psychology, 32 (3), 264.
Coster, S., & Norman, I. (2009). Cochrane reviews of educational and self-management interventions to guide nursing practice: A review. International Journal of Nursing Studies, 46 (4), 508–528.
Cramer, J. A. (2004). A systematic review of adherence with medications for diabetes. Diabetes Care, 27 (5), 1218–1224.
Cranney, M., Warren, E., Barton, S., Gardner, K., & Walley, T. (2001). Why do GPs not implement evidence-based guidelines? A descriptive study. Family Practice, 18 (4), 359–363.
Cutrona, S. L., Choudhry, N. K., Stedman, M., Servi, A., Liberman, J. N., Brennan, T., Fischer, M. A., Alan Brookhart, M., & Shrank, W. H. (2010). Physician effectiveness in interventions to improve cardiovascular medication adherence: A systematic review. Journal of General Internal Medicine, 25 (10), 1090–1096.
de Bruijn, G. J., Kremers, S. P., De Vries, H., Van Mechelen, W., & Brug, J. (2007). Associations of social-environmental and individual-level factors with adolescent soft drink consumption: Results from the SMILE study. Health Education Research, 22 (2), 227–237.
de Meij, J. S., Chinapaw, M. J., Kremers, S. P., Jurg, M. E., & Van Mechelen, W. (2010). Promoting physical activity in children: The stepwise development of the primary school-based JUMP-in intervention applying the RE-AIM evaluation framework. British Journal of Sports Medicine, 44 (12), 879–887.
de Nooijer, J., Lechner, L., & de Vries, H. (2002). Early detection of cancer: Knowledge and behavior among Dutch adults. Cancer Detection and Prevention, 26 (5), 362–369.
de Vet, E., de Nooijer, J., de Vries, N. K., & Brug, J. (2008a). Testing the transtheoretical model for fruit intake: Comparing web-based tailored stage-matched and stage-mismatched feedback. Health Education Research, 23 (2), 218–227.
de Vet, E., De Nooijer, J., De Vries, N. K., & Brug, J. (2008b). Do the transtheoretical processes of change predict transitions in stages of change for fruit intake? Health Education & Behavior, 35 (5), 603–618.
de Vet, E., Gebhardt, W. A., Sinnige, J., Van Puffelen, A., Van Lettow, B., & de Wit, J. B. (2011). Implementation intentions for buying, carrying, discussing and using condoms: The role of the quality of plans. Health Education Research, 26 (3), 443–455.
de Vries, H., & Backbier, E. (1994). Self-efficacy as an important determinant of quitting among pregnant women who smoke: The phi-pattern. Preventive Medicine, 23 (2), 167–174.
de Vries, H., & Brug, J. (1999). Computer-tailored interventions motivating people to adopt health promoting behaviours: Introduction to a new approach. Patient Education and Counseling, 36 (2), 99–105.
de Vries, H., & van Dillen, S. (2002). Prevention of Lyme disease in Dutch children: Analysis of determinants of tick inspection by parents. Preventive Medicine, 35 (2), 160–165.
de Vries, H., & van Dillen, S. (2007). I PLAN: Planning the prevention of Lyme disease, a health promotion approach. In P. van Nitch (Ed.), Research on Lyme disease . New York: Nova Science.
de Vries, H., Dijkstra, M., & Kuhlman, P. (1988). Self-efficacy: The third factor besides attitude and subjective norm as a predictor of behavioural intentions. Health Education Research, 3 (3), 273.
de Vries, H., Backbier, E., Kok, G., & Dijkstra, M. (1995). The impact of social influences in the context of attitude, self-efficacy, intention and previous behavior as predictors of smoking onset. Journal of Applied Social Psychology, 25 , 237–257.
de Vries, H., Mudde, A. N., Dijkstra, A., & Willemsen, M. C. (1998). Differential beliefs, perceived social influences, and self-efficacy expectations among smokers in various motivational phases. Preventive Medicine, 27 (5 Pt 1), 681–689.
de Vries, H., Mudde, A., Leijs, I., Charlton, A., Vartiainen, E., Buijs, G., Clemente, M. P., Storm, H., González Navarro, A., Nebot, M., Prins, T., & Kremers, S. (2003). The European Smoking Prevention Framework Approach (EFSA): An example of integral prevention. Health Education Research, 18 (5), 611–626.
de Vries, H., Lezwijn, J., Hol, M., & Honing, C. (2005). Skin cancer prevention: Behaviour and motives of Dutch adolescents. European Journal of Cancer Prevention, 14 (1), 39–50.
de Vries, H., Candel, M., Engels, R., & Mercken, L. (2006). Challenges to the peer influence paradigm: Results for 12–13 year olds from six European countries from the European Smoking Prevention Framework Approach study. Tobacco Control, 15 (2), 83–89.
de Vries, H., van’t Riet, J., Panday, S., & Reubsaet, A. (2007). Access point analysis in smoking and nonsmoking adolescents: Findings from the European Smoking Prevention Framework Approach study. European Journal of Cancer Prevention, 16 (3), 257–265.
de Vries, H., Kremers, S., Smeets, T., & Reubsaet, A. (2008a). Clustering of diet, physical activity and smoking and a general willingness to change. Psychology & Health, 23 (3), 265.
de Vries, H., van’t Riet, J., Spigt, M., Metsemakers, J., van den Akker, M., Vermunt, J. K., & Kremers, S. (2008b). Clusters of lifestyle behaviors: Results from the Dutch SMILE study. Preventive Medicine, 46 (3), 203–208.
de Vries, H., Kremers, S. P. J., Smeets, T., Brug, J., & Eijmael, K. (2008c). The effectiveness of tailored feedback and action plans in an intervention addressing multiple health behaviors. American Journal of Health Promotion, 22 (6), 417–425.
Dean, A. J., Walters, J., & Hall, A. (2010). A systematic review of interventions to enhance medication adherence in children and adolescents with chronic illness. Archives of Disease in Childhood, 95 (9), 717–723.
Della Mea, V. (2001). What is e-Health (2): The death of telemedicine? Journal of Medical Internet Research, 3 (2), e22.
Dempsey, A. R., Johnson, S. S., & Westhoff, C. L. (2011). Predicting oral contraceptive continuation using the transtheoretical model of health behavior change. Perspectives on Sexual and Reproductive Health, 43 (1), 23–29.
Dictionary, O. E. (2010). “Mass media, n.”, Oxford University Press.
Dijk, F., & de Vries, H. (2009). Smoke alert: A computer-tailored smoking-cessation intervention for Dutch adolescents. Documentation of a FCHE workshop held in Berlin, 18–19 September 2008. Research and Practice of Health Promotion, 14 , 34–46.
Dijkstra, A. (2005). Working mechanisms of computer-tailored health education: Evidence from smoking cessation. Health Education Research, 20 (5), 527–539.
Dijkstra, A., & De Vries, H. (1999). The development of computer-generated tailored interventions. Patient Education and Counseling, 36 (2), 193–203.
Dijkstra, A., & De Vries, H. (2000). Subtypes of precontemplating smokers defined by different long-term plans to change their smoking behavior. Health Education Research, 15 (4), 423–434.
Dijkstra, A., Bakker, M., & De Vries, H. (1997). Subtypes within a sample of precontemplating smokers: A preliminary extension of the stages of change. Addictive Behaviors, 22 (3), 327–337.
Dijkstra, A., De Vries, H., Roijackers, J., & van Breukelen, G. (1998). Tailored interventions to communicate stage-matched information to smokers in different motivational stages. Journal of Consulting and Clinical Psychology, 66 (3), 549–557.
Dijkstra, A., Conijn, B., & De Vries, H. (2006). A match–mismatch test of a stage model of behaviour change in tobacco smoking. Addiction, 101 (7), 1035–1043.
DiMatteo, M. R. (2004). Social support and patient adherence to medical treatment: A meta-analysis. Health Psychology, 23 (2), 207–218.
Dlamini, S., Taylor, M., Mkhize, N., Huver, R., Sathiparsad, R., de Vries, H., Naidoo, K., & Jinabhai, C. (2009). Gender factors associated with sexual abstinent behaviour of rural South African high school going youth in KwaZulu-Natal, South Africa. Health Education Research, 24 (3), 450–460.
Dunton, G. F., Lagloire, R., & Robertson, T. (2009). Using the RE-AIM framework to evaluate the statewide dissemination of a school-based physical activity and nutrition curriculum: “Exercise Your Options”. American Journal of Health Promotion, 23 (4), 229–232.
Dusenbury, L., Brannigan, R., Falco, M., & Hansen, W. B. (2003). A review of research on fidelity of implementation: Implications for drug abuse prevention in school settings. Health Education Research, 18 (2), 237–256.
Epstein, S. (1994). Integration of the cognitive and the psychodynamic unconscious. The American Psychologist, 49 (8), 709–724.
Etter, J. F. (2009). Comparing computer-tailored, internet-based smoking cessation counseling reports with generic, untailored reports: A randomized trial. Journal of Health Communication, 14 (7), 646–657.
Evans, R. I. (1976). Smoking in children: Developing a social psychological strategy of deterrence. Preventive Medicine, 5 (1), 122–127.
Evans-Whipp, T., Beyers, J. M., Lloyd, S., Lafazia, A. N., Toumbourou, J. W., Arthur, M. W., & Catalano, R. F. (2004). A review of school drug policies and their impact on youth substance use. Health Promotion International, 19 (2), 227.
Eysenbach, G. (2005). The law of attrition. Journal of Medical Internet Research, 7 (1), e11.
Faggiano, F., Vigna-Taglianti, F. D., Versino, E., Zambon, A., Borraccino, A., & Lemma, P. (2008). School-based prevention for illicit drugs use: A systematic review. Preventive Medicine, 46 (5), 385–396.
Farquhar, J. W., Fortmann, S. P., Flora, J. A., Taylor, C. B., Haskell, W. L., Williams, P. T., Maccoby, N., & Wood, P. D. (1990). Effects of communitywide education on cardiovascular disease risk factors. The Stanford Five-City Project. JAMA, 264 (3), 359–365.
Fazio, R. H. (1990). Multiple processes by which attitudes guide behaviour: The MODE model as an integrative framework. In M. P. Zanna (Ed.), Advances in experimental social psychology (pp. 75–109). San Diego: Academic Press.
Feifer, C., Ornstein, S. M., Jenkins, R. G., Wessell, A., Corley, S. T., Nemeth, L. S., Roylance, L., Nietert, P. J., & Liszka, H. (2006). The logic behind a multimethod intervention to improve adherence to clinical practice guidelines in a nationwide network of primary care practices. Evaluation & the Health Professions, 29 (1), 65–88.
Festinger, L. (1954). A theory of social comparison processes. Human Relations, 7 , 117.
Fishbein, M., & Ajzen, I. (1975). Belief, attitude, intention, and behavior: An introduction to theory and research . Reading: Addison-Wesley.
Fishbein, M., & Ajzen, I. (2010). Predicting and changing behavior: The reasoned action approach . New York: Taylor & Francis Group.
Fletcher, A., Bonell, C., & Hargreaves, J. (2008). School effects on young people’s drug use: A systematic review of intervention and observational studies. The Journal of Adolescent Health, 42 (3), 209–220.
Fleuren, M., Wiefferink, K., & Paulussen, T. (2004). Determinants of innovation within health care organizations: Literature review and Delphi study. International Journal for Quality in Health Care, 16 (2), 107–123.
Floyd, D. L., Prentice-Dunn, S., & Rogers, R. W. (2000). A meta-analysis of research on protection motivation theory. Journal of Applied Social Psychology, 30 (2), 407–429.
Fox, M. P. (2009). A systematic review of the literature reporting on studies that examined the impact of interactive, computer-based patient education programs. Patient Education and Counseling, 77 (1), 6–13.
Fransen, G. A. J., Mesters, I., Janssen, M. J. R., Knottnerus, J. A., & Muris, J. W. M. (2009). Which patient-related factors determine self-perceived patient adherence to prescribed dyspepsia medication? Health Education Research, 24 (5), 788–798.
Gaglio, B., Shoup, J. A., & Glasgow, R. E. (2013). The RE-AIM framework: A systematic review of use over time. American Journal of Public Health, 103 (6), e38–e46.
Gagne, C., & Godin, G. (2000). The theory of planned behavior: Some measurement issues concerning belief-based variables. Journal of Applied Social Psychology, 30 (10), 2173–2193.
Glanz, K., Rimer, B. K., & Viswanath, K. (2008). Health behavior and health education: Theory, research, and practice . San Francisco: Jossey-Bass.
Glasgow, R. E., Vogt, T. M., & Boles, S. M. (1999). Evaluating the public health impact of health promotion interventions: The RE-AIM framework. American Journal of Public Health, 89 (9), 1322–1327.
Glasgow, R. E., Lichtenstein, E., & Marcus, A. C. (2003). Why don’t we see more translation of health promotion research to practice? Rethinking the efficacy-to-effectiveness transition. American Journal of Public Health, 93 (8), 1261–1267.
Glynn, T. J. (1989). Essential elements of school-based smoking prevention programs. The Journal of School Health, 59 (5), 181–188.
Godin, G., & Conner, M. (2008). Intention-behavior relationship based on epidemiologic indices: An application to physical activity. American Journal of Health Promotion, 22 (3), 180–182.
Godin, G., & Kok, G. (1996). The theory of planned behavior: A review of its applications to health-related behaviors. American Journal of Health Promotion, 11 (2), 87–98.
Goebbels, A. F., Goebbels, A. F. G., Nicholson, J. M., Walsh, K., & De Vries, H. (2008). Teachers’ reporting of suspected child abuse and neglect: Behaviour and determinants. Health Education Research, 23 (6), 941–951.
Goetzel, R. Z., & Ozminkowski, R. J. (2008). The health and cost benefits of work site health-promotion programs. Annual Review of Public Health, 29 , 303–323.
Gollwitzer, P. M. (1990). Action phases and mind-sets. In E. T. Higgins & R. M. Sorrentino (Eds.), Handbook of motivation and cognition: Foundations of social behavior (Vol. 2, pp. 53–92). New York: Guilford Press.
Gollwitzer, P. M. (1999). Implementation intentions: Strong effects of simple plans. American Psychologist, 54 (7), 493.
Gollwitzer, P. M., & Sheeran, P. (2006). Implementation intentions and goal achievement: A Meta-analysis of effects and processes. Advances in Experimental Social Psychology, 38 , 69–119.
Grant, R. W., Wald, J. S., Poon, E. G., Schnipper, J. L., Gandhi, T. K., Volk, L. A., & Middleton, B. (2006). Design and implementation of a web-based patient portal linked to an ambulatory care electronic health record: Patient gateway for diabetes collaborative care. Diabetes Technology & Therapeutics, 8 (5), 576–586.
Green, L. W. (1980). Health education planning: A diagnostic approach . Palo Alto: Mayfield.
Green, L. W., & Kreuter, M. W. (1991). Health promotion planning: An educational and environmental approach . Mountain View: Mayfield.
Green, L. W., & Kreuter, M. (1999). Health promotion planning: An educational and ecological approach . Mountain View: Mayfield.
Green, L. W., & Kreuter, M. W. (2005). Health program planning: An educational and ecological approach . New York: McGraw-Hill.
Grilli, R., Ramsay, C., & Minozzi, S. (2002). Mass media interventions: Effects on health services utilisation. Cochrane Database of Systematic Reviews, 1 , CD000389.
Groeneveld, I. F., Proper, K. I., Van der Beek, A. J., & Van Mechelen, W. (2010). Sustained body weight reduction by an individual-based lifestyle intervention for workers in the construction industry at risk for cardiovascular disease: Results of a randomized controlled trial. Preventive Medicine, 51 (3-4), 240–246.
Grol, R., & Jones, R. (2000). Twenty years of implementation research. Family Practice, 17 (Suppl 1), S32–S35.
Grube, J. W., Morgan, M., & McGree, S. T. (1986). Attitudes and normative beliefs as predictors of smoking intentions and behaviours: A test of three models. The British Journal of Social Psychology, 25 (Pt 2), 81–93.
Hagger, M. S., Lonsdale, A. J., Hein, V., Koka, A., Lintunen, T., Pasi, H., Lindwall, M., Rudolfsson, L., & Chatzisarantis, N. L. D. (2011). Predicting alcohol consumption and binge drinking in company employees: An application of planned behaviour and self-determination theories. British Journal of Health Psychology, 17 (2), 379–407.
Hall, K. L., & Rossi, J. S. (2008). Meta-analytic examination of the strong and weak principles across 48 health behaviors. Preventive Medicine, 46 (3), 266–274.
Hallfors, D., & Godette, D. (2002). Will the ‘principles of effectiveness’ improve prevention practice? Early findings from a diffusion study. Health Education Research, 17 (4), 461–470.
Handley, M., MacGregor, K., Schillinger, D., Sharifi, C., Wong, S., & Bodenheimer, T. (2006). Using action plans to help primary care patients adopt healthy behaviors: A descriptive study. Journal of American Board of Family Medicine, 19 (3), 224–231.
Hansen, W. B. (1992). School-based substance abuse prevention: A review of the state of the art in curriculum, 1980–1990. Health Education Research, 7 (3), 403–430.
Harakeh, Z., Scholte, R. H., Vermulst, A. A., de Vries, H., & Engels, R. C. (2004). Parental factors and adolescents’ smoking behavior: An extension of the theory of planned behavior. Preventive Medicine, 39 (5), 951–961.
Harden, A., Peersman, G., Oliver, S., Mauthner, M., & Oakley, A. (1999). A systematic review of the effectiveness of health promotion interventions in the workplace. Occupational Medicine (London), 49 (8), 540–548.
Harting, J., Rutten, G. M., Rutten, S. T., & Kremers, S. P. (2009). A qualitative application of the diffusion of innovations theory to examine determinants of guideline adherence among physical therapists. Physical Therapy, 89 (3), 221–232.
Hawkins, R. P., Kreuter, M., Resnicow, K., Fishbein, M., & Dijkstra, A. (2008). Understanding tailoring in communicating about health. Health Education Research, 23 (3), 454–466.
US Department of Health and Human Services. (1991). Healthy people 2000: National health promotion and disease prevention objectives and healthy schools. Journal of School Health, 61 (7), 298–328.
Heckhausen, H. (1991). Motivation and action . New York: Springer.
Book Google Scholar
Helmink, J. H., Meis, J. J., de Weerdt, I., Visser, F. N., de Vries, N. K., & Kremers, S. P. (2010). Development and implementation of a lifestyle intervention to promote physical activity and healthy diet in the Dutch general practice setting: The BeweegKuur programme. International Journal of Behavioral Nutrition and Physical Activity, 7 , 49.
Henderson, V. (1966). The nature of nursing . New York: Macmillan.
Hendriksen, E. S., Pettifor, A., Lee, S. J., Coates, T. J., & Rees, H. V. (2007). Predictors of condom use among young adults in South Africa: The Reproductive Health and HIV Research Unit National Youth Survey. American Journal of Public Health, 97 (7), 1241–1248.
Herzog, T. A., & Blagg, C. O. (2007). Are most precontemplators contemplating smoking cessation? Assessing the validity of the stages of change. Health Psychology, 26 (2), 222.
Hettema, J., Steele, J., & Miller, W. R. (2005). Motivational interviewing. Annual Review of Clinical Psychology, 1 , 91–111.
Hochbaum, G. M. (1971). Measurement of effectiveness of health education activites. International Journal of Health Education, 2 , 54–59.
Hoffman, D. L., & Novak, T. P. (1998). Bridging the racial divide on the Internet. Science, 280 , 390–391.
Hofmann, W., Friese, M., & Wiers, R. W. (2008). Impulsive versus reflective influences on health behavior: A theoretical framework and empirical review. Health Psychology Review, 2 , 111–137.
Holm, K., Kremers, S. P., & de Vries, H. (2003). Why do Danish adolescents take up smoking? European Journal of Public Health, 13 (1), 67–74.
Horowitz, S. M. (2003). Applying the transtheoretical model to pregnancy and STD prevention: A review of the literature. American Journal of Health Promotion, 17 (5), 304–328.
Hoving, E. F., Mudde, A. N., & de Vries, H. (2006). Smoking and the O pattern; predictors of transitions through the stages of change. Health Education Research, 21 (3), 305–314.
Hovland, C. I., Janis, I. L., & Kelley, H. H. (1953). Communication and persuasion: Psychological studies of opinion change . New Haven: Yale UP.
Huver, R. M. E., Engels, R. C. M. E., & de Vries, H. (2006). Are anti-smoking parenting practices related to adolescent smoking cognitions and behavior? Health Education Research, 21 (1), 66–77.
Huver, R. M., Engels, R. C. M. E., Vermulst, A. A., & de Vries, H. (2007). Is parenting style a context for smoking-specific parenting practices? Drug and Alcohol Dependence, 89 (2-3), 116–125.
Hyman, H. H., & Sheatsley, P. B. (1947). Some reasons why information campaigns fail. Public Opinion Quarterly, 11 , 412–423.
Ito, K. E., & Brown, J. D. (2010). To friend or not to friend: Using new media for adolescent health promotion. North Carolina Medical Journal, 71 (4), 367–372.
PubMed Google Scholar
Jackson, C., Lawton, R., Knapp, P., Raynor, D. K., Conner, M., Lowe, C., & Closs, S. J. (2005). Beyond intention: Do specific plans increase health behaviours in patients in primary care? A study of fruit and vegetable consumption. Social Science & Medicine, 60 (10), 2383.
James, S., Reddy, P., Ruiter, R. A., McCauley, A., & Borne, B. V. D. (2006). The impact of an HIV and AIDS life skills program on secondary school students in KwaZulu-Natal, South Africa. AIDS Educ Prev, 18 (4), 281–294.
Janis, I. L., & Mann, L. (1977). Decision making: A psychological analysis of conflict, choice, and commitment . New York: Free Press.
Janssen, E., van Osch, L., de Vries, H., & Lechner, L. (2011). Measuring risk perceptions of skin cancer: Reliability and validity of different operationalizations. British Journal of Health Psychology, 16 (Pt 1), 92–112.
Janssen, E., van Osch, L., Lechner, L., Candel, M., & de Vries, H. (2012). Thinking versus feeling: Differentiating between cognitive and affective components of perceived cancer risk. Psychology & Health, 27 (7), 767–783.
Janssen, E., van Osch, L., de Vries, H., & Lechner, L. (2013). Examining direct and indirect pathways to health behaviour: The influence of cognitive and affective probability beliefs. Psychology & Health, 28 (5), 546–560.
Janz, N. K., & Becker, M. H. (1984). The Health Belief Model: A decade later. Health Education Quarterly, 11 (1), 1–47.
Johnson, C. E., Mues, K. E., Mayne, S. L., & Kiblawi, A. N. (2008). Cervical cancer screening among immigrants and ethnic minorities: A systematic review using the Health Belief Model. Journal of Lower Genital Tract Disease, 12 (3), 232–241.
Joosten, E. A., DeFuentes-Merillas, L., De Weert, G. H., Sensky, T., Van Der Staak, C. P. F., & de Jong, C. A. (2008). Systematic review of the effects of shared decision-making on patient satisfaction, treatment adherence and health status. Psychotherapy and Psychosomatics, 77 (4), 219–226.
Jurg, M. E., Kremers, S. P., Candel, M. J., Van der Wal, M. F., & Meij, J. S. D. (2006). A controlled trial of a school-based environmental intervention to improve physical activity in Dutch children: JUMP-in, kids in motion. Health Promotion International, 21 (4), 320.
Kamarck, T. W., Manuck, S. B., & Jennings, J. R. (1990). Social support reduces cardiovascular reactivity to psychological challenge: A laboratory model. Psychosomatic Medicine, 52 (1), 42.
Kemp, R., Kirov, G., Everitt, B., Hayward, P., & David, A. (1998). Randomised controlled trial of compliance therapy. 18-month follow-up. The British Journal of Psychiatry, 172 , 413–419.
King, E. S., Rimer, B. K., Seay, J., Balshem, A., & Engstrom, P. F. (1994). Promoting mammography use through progressive interventions: Is it effective? American Journal of Public Health, 84 (1), 104–106.
Kirby, D. B., Laris, B. A., & Rolleri, L. A. (2007). Sex and HIV education programs: Their impact on sexual behaviors of young people throughout the world. The Journal of Adolescent Health, 40 (3), 206–217.
Knai, C., Pomerleau, J., Lock, K., & McKee, M. (2006). Getting children to eat more fruit and vegetables: A systematic review. Preventive Medicine: An International Journal Devoted to Practice and Theory, 42 (2), 85.
Kok, G., Lo, S. H., Peters, G. J. Y., & Ruiter, R. A. (2011). Changing energy-related behavior: An intervention mapping approach. Energy Policy, 39 , 5280–5286.
Kolbe, L. J. (1985). Why school health education? An empirical point of view. Health Education, 16 (2), 116–120.
Kremers, S. P. (2010). Theory and practice in the study of influences on energy balance-related behaviors. Patient Education and Counseling, 79 (3), 291–298.
Kremers, S. P., & Brug, J. (2008). Habit strength of physical activity and sedentary behavior among children and adolescents. Pediatric Exercise Science, 20 (1), 5–14. Discussion 14-7.
Kremers, S. P. J., Mudde, A. N., & de Vries, H. (2001). Subtypes within the precontemplation stage of adolescent smoking acquisition. Addictive Behaviors, 26 (2), 237.
Kremers, S. P., De Bruijn, G. J., Visscher, T. L., Van Mechelen, W., De Vries, N. K., & Brug, J. (2006). Environmental influences on energy balance-related behaviors: A dual-process view. International Journal of Behavioral Nutrition and Physical Activity, 3 , 9.
Kreuter, M. W., & Strecher, V. J. (1996). Do tailored behavior change messages enhance the effectiveness of health risk appraisal? Results from a randomized trial. Health Education Research, 11 (1), 97–105.
Kreuter, M. W., Farrell, D. W., Olevitch, L. R., & Brennan, L. K. (2000). Tailoring health messages: Customizing communication with computer technology . Mahwah: Lawrence Erlbaum Associates.
Kroeze, W., Werkman, A., & Brug, J. (2006). A systematic review of randomized trials on the effectiveness of computer-tailored education on physical activity and dietary behaviors. Annals of Behavioral Medicine, 31 (3), 205–223.
Kruger, S. (1991). The patient educator role in nursing. Applied Nursing Research, 4 (1), 19–24.
Kwak, L., Kremers, S. P., van Baak, M. A., & Brug, J. (2007). Formation of implementation intentions promotes stair use. American Journal of Preventive Medicine, 32 (3), 254.
Latham, G. P., & Locke, E. A. (2006). Enhancing the benefits and overcoming the pitfalls of goal setting. Organizational Dynamics, 35 (4), 332–340.
Lazarus, R. S. (1966). Psychological stress and the coping process . New York: McGraw-Hill.
Leung, L. (2008). Internet embeddedness: Links with online health information seeking, expectancy value/quality of health information websites, and Internet usage patterns. Cyberpsychology & Behavior, 11 (5), 565–569.
Leventhal, H. (1970). Findings and theory in the study of fear communications. In L. Berkowitz (Ed.), Advances in experimental social psychology . New York: Academic Press.
Leventhal, H., & Cameron, L. (1987). Behavioral theories and the problem of compliance. Patient Education and Counseling, 10 (2), 117.
Leventhal, H., Nerenz, D. R., & Steele, D. J. (1984). Illness representation and coping with health threats . In A. Baum, S. E. Taylor, & J. E. Singer (Eds.), Handbook of psychology and health (pp. 219–252). Hillsdale: Lawrence Erlbaum Associates.
Lewis, B. A., Williams, D. M., Neighbors, C. J., Jakicic, J. M., & Marcus, B. H. (2010). Cost analysis of Internet vs. print interventions for physical activity promotion. Psychology of Sport and Exercise, 11 (3), 246–249.
Lippke, S., & Plotnikoff, R. C. (2012). Testing two principles of the health action process approach in individuals with type 2 diabetes. Health Psychology .
Lippke, S., & Ziegelmann, J. P. (2008). Theory-based health behavior change: Developing, testing, and applying theories for evidence-based interventions. Applied Psychology, 57 (4), 698–716.
Lippke, S., Ziegelmann, J. P., & Schwarzer, R. (2004). Initiation and maintenance of physical exercise: Stage-specific effects of a planning intervention. Research in Sports Medicine, 12 (3), 221.
Lippke, S., Ziegelmann, J. P., & Schwarzer, R. (2005). Stage-specific adoption and maintenance of physical activity: Testing a three-stage model. Psychology of Sport and Exercise, 6 , 585–603.
Lippke, S., Schwarzer, R., Ziegelmann, J. P., Scholz, U., & Schüz, B. (2010). Testing stage-specific effects of a stage-matched intervention: A randomized controlled trial targeting physical exercise and its predictors. Health Education & Behavior, 37 (4), 533–546.
Liu, L. L., & Park, D. C. (2004). Aging and medical adherence: The use of automatic processes to achieve effortful things. Psychology and Aging, 19 (2), 318–325.
Locke, E. A., & Latham, G. P. (2002). Building a practically useful theory of goal setting and task motivation. A 35-year odyssey. The American Psychologist, 57 (9), 705–717.
Lotrean, L. M., Dijk, F., Mesters, I., Ionut, C., & De Vries, H. (2010). Evaluation of a peer-led smoking prevention programme for Romanian adolescents. Health Education Research, 25 (5), 803.
Luszczynska, A., & Schwarzer, R. (2003). Planning and self-efficacy in the adoption and maintenance of breast self-examination: A longitudinal study on self-regulatory cognitions. Psychology & Health, 18 (1), 93–108.
MacGregor, K., Handley, M., Wong, S., Sharifi, C., Gjeltema, K., Schillinger, D., & Bodenheimer, T. (2006). Behavior-change action plans in primary care: A feasibility study of clinicians. The Journal of the American Board of Family Medicine, 19 , 215–223.
Marks, R., Allegrante, J. P., & Lorig, K. (2005). A review and synthesis of research evidence for self-efficacy-enhancing interventions for reducing chronic disability: Implications for health education practice (part II). Health Promotion Practice, 6 (2), 148–156.
Marlatt, G. A., & George, W. H. (1984). Relapse prevention: Introduction and overview of the model. British Journal of Addiction, 79 (3), 261–273.
Marshall, S. J., & Biddle, S. J. (2001). The transtheoretical model of behavior change: A meta-analysis of applications to physical activity and exercise. Annals of Behavioral Medicine, 23 (4), 229–246.
Martinez, M. (2008). High attrition rates in e-learning: Challenges, predictors, and solutions (p. 15). Santa Rosa: The E-Learning Developers’ Journal.
Mays, D., Streisand, R., Walker, L. R., Prokhorov, A. V., & Tercyak, K. P. (2012). Cigarette smoking among adolescents with type 1 diabetes: Strategies for behavioral prevention and intervention. Journal of Diabetes and its Complications, 26 (2), 148–153.
McGuire, W. J. (1985). Attitudes and attitude change. In G. Lindzey & E. Aronson (Eds.), Handbook of social psychology (Vol. II). New York: Lawrence Erlbaum Associates.
McKenzie, J. F., & Smeltzer, J. L. (2001). Planning, implementing and evaluating health promotion programs . Boston: Allyn and Bacon.
McLean, S. M., Burton, M., Bradley, L., & Littlewood, C. (2010). Interventions for enhancing adherence with physiotherapy: A systematic review. Manual Therapy, 15 (6), 514–521.
McLeroy, K. R., Bibeau, D., Steckler, A., & Glanz, K. (1988). An ecological perspective on health promotion programs. Health Education Quarterly, 15 (4), 351–377.
Mercken, L., Snijders, T. A., Steglich, C., & de Vries, H. (2009). Dynamics of adolescent friendship networks and smoking behavior: Social network analyses in six European countries. Social Science & Medicine, 69 (10), 1506.
Mercken, L., Candel, M., Van Osch, L., & De Vries, H. (2010). No smoke without fire: The impact of future friends on adolescent smoking behaviour. British Journal of Health Psychology, 16 (Pt 1), 170–188.
Milgram, S. (1963). Behavioral study of obedience. Journal of Abnormal Psychology, 67 , 371–378.
Miller, W. R., & Rollnick, S. (2002). Motivational interviewing: Preparing people to change (2nd ed.). New York: Guilford Press.
Milne, S., Sheeran, P., & Orbell, S. (2000). Prediction and intervention in health-related behavior: A meta-analytic review of protection motivation theory. Journal of Applied Social Psychology, 30 (1), 106.
Milne, S., Orbell, S., & Sheeran, P. (2002). Combining motivational and volitional interventions to promote exercise participation: Protection motivation theory and implementation intentions. British Journal of Health Psychology, 7 (Pt 2), 163–184.
Montaño, D. E., & Kasprzyk, D. (2008). Theory of reasoned action, theory of planned behavior and the integrated behavioral model. In K. Glanz, B. K. Rimer, & K. Viswanath (Eds.), Health behavior and health education (4th ed.). San Francisco: Jossey-Bass.
Moritz, S. E., Feltz, D. L., Fahrbach, K. R., & Mack, D. E. (2000). The relation of self-efficacy measures to sport performance: A meta-analytic review. Research Quarterly for Exercise and Sport, 71 (3), 280–294.
Morrison, V., & Bennett, P. (2008). An introduction to health psychology (2nd ed.). London: Pearson Publishing.
Mulvaney, S. A., Rothman, R. L., Wallston, K. A., Lybarger, C., & Dietrich, M. S. (2010). An internet-based program to improve self-management in adolescents with type 1 diabetes. Diabetes Care, 33 (3), 602–604.
Newman, I. M., Martin, G. L., & Ang, J. (1982). The role of attitudes and social norms in adolescent cigarette smoking. The New Zealand Medical Journal, 95 (715), 618–621.
Ni Mhurchu, C., Aston, L. M., & Jebb, S. A. (2010). Effects of worksite health promotion interventions on employee diets: A systematic review. BMC Public Health, 10 (62), 1.
Nichols, J., Schutte, N. S., Brown, R. F., Dennis, C. L., & Price, I. (2009). The impact of a self-efficacy intervention on short-term breast-feeding outcomes. Health Education & Behavior, 36 (2), 250–258.
Nigg, C. R., Albright, C., Williams, R., Nichols, C., Renda, G., Stevens, V. J., & Vogt, T. M. (2010). Are physical activity and nutrition indicators of the checklist of health promotion environments at worksites (CHEW) associated with employee obesity among hotel workers? Journal of Occupational and Environmental Medicine, 52 (Suppl. 1), S4–S7.
Noar, S. M., & Harrington, N. G. (2012). eHealth applications . New York: Routledge.
Noar, S. M., Benac, C. N., & Harris, M. S. (2007). Does tailoring matter? Meta-analytic review of tailored print health behavior change interventions. Psychological Bulletin, 133 (4), 673–693.
Noar, S. M., Black, H. G., & Pierce, L. B. (2009). Efficacy of computer technology-based HIV prevention interventions: A meta-analysis. AIDS, 23 (1), 107.
Noar, S. M., Webb, E. M., Van Stee, S. K., Redding, C. A., Feist-Price, S., Crosby, R., & Troutman, A. (2011). Using computer technology for HIV prevention among African-Americans: Development of a tailored information program for safer sex (TIPSS). Health Education Research, 26 (3), 393–406.
Norman, G. J., Velicer, W. F., Fava, J. L., & Prochaska, J. O. (2000). Cluster subtypes within stage of change in a representative sample of smokers. Addictive Behaviors, 25 (2), 183.
Norman, P., Boer, H., & Seydel, E. R. (2005). Protection motivation theory. In M. Conner & P. Norman (Eds.), Predicting health behavior (pp. 81–126). London: Open University Press.
Norris, S. L., Engelgau, M. M., & Narayan, K. V. (2001). Effectiveness of self-management training in type 2 diabetes a systematic review of randomized controlled trials. Diabetes Care, 24 (3), 561–587.
Norris, S. L., Lau, J., Smith, S. J., Schmid, C. H., & Engelgau, M. M. (2002). Self-management education for adults with type 2 diabetes a meta-analysis of the effect on glycemic control. Diabetes Care, 25 (7), 1159–1171.
O’Leary, A. (1985). Self-efficacy and health. Behaviour Research and Therapy, 23 (4), 437.
Oei, T. P., & Burrow, T. (2000). Alcohol expectancy and drinking refusal self-efficacy: A test of specificity theory. Addictive Behaviors, 25 (4), 499–507.
Oenema, A., Brug, J., & Lechner, L. (2001). Web-based tailored nutrition education: Results of a randomized controlled trial. Health Education Research, 16 (6), 647–660.
Oostveen, T., Knibbe, R., & de Vries, H. (1996). Social influences on young adults’ alcohol consumption: Norms, modeling, pressure, socializing, and conformity. Addictive Behaviors, 21 (2), 187–197.
Orbell, S., & Sheeran, P. (1998). ‘Inclined abstainers’: A problem for predicting health-related behaviour. The British Journal of Social Psychology, 37 (Pt 2), 151–165.
Panday, S., Reddy, S. P., Ruiter, R. A., Bergström, E., & de Vries, H. (2005). Determinants of smoking cessation among adolescents in South Africa. Health Education Research, 20 (5), 586–599.
Parcel, G. S., Eriksen, M. P., Lovato, C. Y., Gottlieb, N. H., Brink, S. G., & Green, L. W. (1989). The diffusion of school-based tobacco-use prevention programs: Project description and baseline data. Health Education Research, 4 (1), 111.
Parker, R. M., & Jacobson, T. A. (2000). The role of health literacy in narrowing the treatment gap for hypercholesterolemia. The American Journal of Managed Care, 6 (12), 1340–1342.
Pelletier, K. R. (2009). A review and analysis of the clinical and cost-effectiveness studies of comprehensive health promotion and disease management programs at the worksite: Update VII 2004–2008. Journal of Occupational and Environmental Medicine, 51 (7), 822–837.
Perry, C. L., Kelder, S. H., & Klepp, K. I. (1994). Community-wide cardiovascular disease prevention in young people: Long-term outcomes of the class of 1989 study. European Journal of Public Health, 4 (3), 188–194.
Perry, C. L., Williams, C. L., Veblen-Mortenson, S., Toomey, T. L., Komro, K. A., Anstine, P. S., McGovern, P. G., Finnegan, J. R., Forster, J. L., Wagenaar, A. C., & Wolfson, M. (1996). Project Northland: Outcomes of a communitywide alcohol use prevention program during early adolescence. American Journal of Public Health, 86 (7), 956–965.
Peters, L. W., Wiefferink, C. H., Hoekstra, F., Buijs, G. J., ten Dam, G. T., & Paulussen, T. G. (2009). A review of similarities between domain-specific determinants of four health behaviors among adolescents. Health Education Research, 24 (2), 198–223.
Peterson, A. V., Jr., Kealey, K. A., Mann, S. L., Marek, P. M., & Sarason, I. G. (2000). Hutchinson Smoking Prevention Project: Long-term randomized trial in school-based tobacco use prevention – Results on smoking. Journal of the National Cancer Institute, 92 (24), 1979–1991.
Petty, R. E., & Cacioppo, J. T. (1986). Communication and persuasion, central and peripheral routes to attitude change . New York: Springer.
Pinto, A. M., Heinberg, L. J., Coughlin, J. W., Fava, J. L., & Guarda, A. S. (2008). The Eating Disorder Recovery Self-Efficacy Questionnaire (EDRSQ): Change with treatment and prediction of outcome. Eating Behaviors, 9 (2), 143.
Plotnikoff, R. C., Lippke, S., Courneya, K. S., Birkett, N., & Sigal, R. J. (2008). Physical activity and social cognitive theory: A test in a population sample of adults with type 1 or type 2 diabetes. Applied Psychology, 57 (4), 628–643.
Plotnikoff, R. C., Lippke, S., Johnson, S. T., & Courneya, K. S. (2010a). Physical activity and stages of change: A longitudinal test in types 1 and 2 diabetes samples. Annals of Behavioral Medicine, 40 (2), 138–149.
Plotnikoff, R. C., Lippke, S., Trinh, L., Courneya, K. S., Birkett, N., & Sigal, R. J. (2010b). Protection motivation theory and the prediction of physical activity among adults with type 1 or type 2 diabetes in a large population sample. British Journal of Health Psychology, 15 (Pt 3), 643–661.
Pomp, S., Lippke, S., Fleig, L., & Schwarzer, R. (2010). Synergistic effects of intention and depression on action control: Longitudinal predictors of exercise after rehabilitation. Mental Health and Physical Activity, 2 , 78–84.
Presson, C. C., Chassin, L., Sherman, S. J., Olshavsky, R., Bensenberg, M., & Corty, E. (1984). Predictors of adolescents’ intentions to smoke: Age, sex, race, and regional differences. The International Journal of the Addictions, 19 (5), 503–519.
Elders, M. J. (1994). Preventing tobacco use among young people. A report of the Surgeon General. Executive summary. MMWR – Recommendations and Reports, 43 (RR-4), 1–10.
Price, V., & Zaller, J. (1993). Who gets the news? Alternative measures of news reception and their implications for research. Public Opinion Quarterly, 57 (2), 133.
Prochaska, J. O., & DiClemente, C. C. (1983). Stages and processes of self-change of smoking: Toward an integrative model of change. Journal of Consulting and Clinical Psychology, 51 (3), 390–395.
Prochaska, J. O., & Velicer, W. F. (1997). The transtheoretical model of health behavior change. American Journal of Health Promotion, 12 (1), 38–48.
Prochaska, J. O., Velicer, W. F., Rossi, J. S., Goldstein, M. G., Marcus, B. H., Rakowski, W., Fiore, C., Harlow, L. L., Redding, C. A., Rosenbloom, D., & Rossi, S. R. (1994). Stages of change and decisional balance for 12 problem behaviors. Health Psychology, 13 (1), 39–46.
Prochaska, J. O., Velicer, W. F., Redding, C., Rossi, J. S., Goldstein, M., DePue, J., Greene, G. W., Rossi, S. R., Sun, X., & Fava, J. L. (2005). Stage-based expert systems to guide a population of primary care patients to quit smoking, eat healthier, prevent skin cancer, and receive regular mammograms. Preventive Medicine, 41 (2), 406–416.
Prochaska, J. J., Spring, B., & Nigg, C. R. (2008). Multiple health behavior change research: An introduction and overview. Preventive Medicine, 46 (3), 181–188.
Puska, P. M., Puska, P. M. J., Barrueco, M., Roussos, C., Hider, A., & Hogue, S. (2005). The participation of health professionals in a smoking-cessation programme positively influences the smoking cessation advice given to patients. International Journal of Clinical Practice, 59 (4), 447–452.
Quinlan, K. B., & McCaul, K. D. (2000). Matched and mismatched interventions with young adult smokers: Testing a stage theory. Health Psychology, 19 (2), 165.
Rahimi, B., Timpka, T., Vimarlund, V., Uppugunduri, S., & Svensson, M. (2009). Organization-wide adoption of computerized provider order entry systems: A study based on diffusion of innovations theory. BMC Medical Informatics and Decision Making, 9 (1), 52.
Rakowski, W., Ehrich, B., Goldstein, M. G., Rimer, B. K., Pearlman, D. N., Clark, M. A., Velicer, W. F., & Woolverton III, H. (1998). Increasing mammography among women aged 40–74 by use of a stage-matched, tailored intervention. Preventive Medicine, 27 (5 Pt 1), 748–756.
Renner, B., Kwon, S., Yang, B.-H., Paik, K.-C., Kim, S. H., Roh, S., Song, J., & Schwarzer, R. (2008). Social-cognitive predictors of dietary behaviors in South Korean men and women. International Journal of Behavioral Medicine, 15 (1), 4–13.
Resnicow, K., & Vaughan, R. (2006). A chaotic view of behavior change: A quantum leap for health promotion. International Journal of Behavioral Nutrition and Physical Activity, 3 , 25.
Resnicow, K., DiIorio, C., Soet, J. E., Borrelli, B., Hecht, J., & Ernst, D. (2002). Motivational interviewing in health promotion: It sounds like something is changing. Health Psychology, 21 (5), 444.
Rigotti, N. A., Munafo, M. R., & Stead, L. F. (2008). Smoking cessation interventions for hospitalized smokers: A systematic review. Archives of Internal Medicine, 168 (18), 1950–1960.
Riper, H., Kramer, J., Smit, F., Conijn, B., Schippers, G., & Cuijpers, P. (2008). Web-based self-help for problem drinkers: A pragmatic randomized trial. Addiction, 103 (2), 218.
Rivis, A., & Sheeran, P. (2003). Descriptive norms as an additional predictor in the theory of planned behaviour: A meta-analysis. Current Psychology: Developmental, Learning, Personality, Social, 22 , 218–233.
Rogers, R. W. (1975). A protection motivation theory of fear appeals and attitude change. Journal of Psychology: Interdisciplinary and Applied, 91 (1), 93.
Rogers, R. W. (1983). Cognitive and physiological processes in fear appeals and attitude change: A revised theory of protection motivation. In J. T. Cacioppo & R. E. Petty (Eds.), Social psychophysiology . New York: Guilford Press.
Rogers, R. W. (2003). Diffusion of innovations (5th ed.). New York: Free Press.
Rohrbach, L. A., Grana, R., Sussman, S., & Valente, T. W. (2006). Type II translation: Transporting prevention interventions from research to real-world settings. Evaluation & the Health Professions, 29 (3), 302–333.
Rosenstock, I. (1974). Historical origins of the Health Belief Model. Health Education Monographs, 2 (4), 336.
Rosseel, J. P., Hilberink, S. R., Jacobs, J. E., Maassen, I. M., Plasschaert, A. J. M., & Grol, R. P. T. M. (2010). Are oral health complaints related to smoking cessation intentions? Community Dentistry and Oral Epidemiology, 38 (5), 470–478.
Ruiter, R. A., Kessels, L. T., Jansma, B. M., & Brug, J. (2006). Increased attention for computer-tailored health communications: An event-related potential study. Health Psychology, 25 (3), 300–306.
Rutter, D. R., Steadman, L., & Quine, L. (2006). An implementation intentions intervention to increase uptake of mammography. Annals of Behavioral Medicine, 32 (2), 127–134.
Salpeter, S. R., Buckley, N. S., Ormiston, T. M., & Salpeter, E. E. (2006). Meta-analysis: Effect of long-acting beta-agonists on severe asthma exacerbations and asthma-related deaths. Annals of Internal Medicine, 144 (12), 904–912.
Sarafino, E. P. (1994). Health psychology: Biopsychosocial interactions (2nd ed.). New York: Wiley.
Sarkar, U., Karter, A. J., Liu, J. Y., Adler, N. E., Nguyen, R., López, A., & Schillinger, D. (2011). Social disparities in internet patient portal use in diabetes: Evidence that the digital divide extends beyond access. Journal of the American Medical Informatics Association, 18 (3), 318–321.
Say, R. E., & Thomson, R. (2003). The importance of patient preferences in treatment decisions – Challenges for doctors. BMJ, 327 (7414), 542–545.
Schaalma, H., Kok, G., & Peters, L. (1993). Determinants of consistent condom use by adolescents: The impact of experience of sexual intercourse. Health Education Research, 8 (2), 255.
Schoenmakers, T., Wiers, R. W., & Field, M. (2008). Effects of a low dose of alcohol on cognitive biases and craving in heavy drinkers. Psychopharmacology, 197 (1), 169–178.
Schwarzer, R. (Ed.). (1992). Self-efficacy: Thought control of action . Washington, DC: Hemisphere.
Schwarzer, R. (2008a). Modeling health behavior change: The Health Action Process Approach (HAPA) . Available from: http://www.hapa-model.de/
Schwarzer, R. (2008b). Modeling health behavior change: How to predict and modify the adoption and maintenance of health behaviors. Applied Psychology. An International Review, 57 (1), 1.
Schwarzer, R., Schüz, B., Ziegelmann, J. P., Lippke, S., Luszczynska, A., & Scholz, U. (2007). Adoption and maintenance of four health behaviors: Theory-guided longitudinal studies on dental flossing, seat belt use, dietary behavior, and physical activity. Annals of Behavioral Medicine, 33 (2), 156.
Schwarzer, R., Luszczynska, A., Ziegelmann, J. P., Scholz, U., & Lippke, S. (2008). Social-cognitive predictors of physical exercise adherence: Three longitudinal studies in rehabilitation. Health Psychology, 27 (Suppl. 1), S54.
Schwarzer, R., Lippke, S., & Luszczynska, A. (2011). Mechanisms of health behavior change in persons with chronic illness or disability: The Health Action Process Approach (HAPA). Rehabilitation Psychology, 56 (3), 161.
Segaar, D., Willemsen, M. C., Bolman, C., & De Vries, H. (2007a). Nurse adherence to a minimal-contact smoking cessation intervention on cardiac wards. Research in Nursing & Health, 30 (4), 429–444.
Segaar, D., Bolman, C., Willemsen, M. C., & De Vries, H. (2007b). Identifying determinants of protocol adoption by midwives: A comprehensive approach. Health Education Research, 22 (1), 14–26.
Senge, P. (1990). The fifth discipline: The art and practice of the learning organization . New York: Currency Doubleday.
Sheeran, P., & Orbell, S. (2000). Using implementation intentions to increase attendance for cervical cancer screening. Health Psychology, 19 (3), 283–289.
Sheeran, P., Webb, T. L., & Gollwitzer, P. M. (2005). The interplay between goal intentions and implementation intentions. Personality and Social Psychology Bulletin, 31 (1), 87–98.
Sherif, M. (1935). A study of some social factors in perception. Archives of Psychology, 187 .
Simonds, S. K. (1978). Health education: Facing issues of policy, ethics, and social justice. Health Education Monographs, 6 (Suppl. 1), 18–27.
Skår, S., Sniehotta, F. F., Molloy, G. J., Prestwich, A., & Araujo-Soares, V. (2011). Do brief online planning interventions increase physical activity amongst university students? A randomised controlled trial. Psychology & Health, 26 (4), 399–417.
Skinner, C. S., Sykes, R. K., Monsees, B. S., Andriole, D. A., Arfken, C. L., & Fisher, E. B. (1998). Learn, share, and live: Breast cancer education for older, urban minority women. Health Education & Behavior, 25 (1), 60–78.
Slovic, P. (1987). Perception of risk. Science, 236 (4799), 280–285.
Slovic, P., & Peters, E. (2006). Risk perception and affect. Current Directions in Psychological Science, 15 (6), 322–325.
Smeets, T., Brug, J., & de Vries, H. (2008). Effects of tailoring health messages on physical activity. Health Education Research, 23 (3), 402–413.
Smerecnik, C., Quaak, M., van Schayck, C. P., van Schooten, F. J., & de Vries, H. (2011). Are smokers interested in genetic testing for smoking addiction? A socio-cognitive approach. Psychology & Health, 26 (8), 1099–1112.
Sniehotta, F. F. (2009). Towards a theory of intentional behaviour change: Plans, planning, and self-regulation. British Journal of Health Psychology, 14 (2), 261.
Sniehotta, F. F., Scholz, U., Schwarzer, R., Fuhrmann, B., Kiwus, U., & Völler, H. (2005). Long-term effects of two psychological interventions on physical exercise and self-regulation following coronary rehabilitation. International Journal of Behavioral Medicine, 12 (4), 244–255.
Sniehotta, F. F., Scholz, U., & Schwarzer, R. (2006). Action plans and coping plans for physical exercise: A longitudinal intervention study in cardiac rehabilitation. British Journal of Health Psychology, 11 (Pt 1), 23–37.
Snyder, L. B., Hamilton, M. A., Mitchell, E. W., Kiwanuka-Tondo, J., Fleming-Milici, F., & Proctor, D. (2004). A meta-analysis of the effect of mediated health communication campaigns on behavior change in the United States. Journal of Health Communication, 9 (Suppl. 1), 71–96.
Soler, R. E., Leeks, K. D., Razi, S., Hopkins, D. P., Griffith, M., Aten, A., Chattopadhyay, S. K., Smith, S. C., Habarta, N., & Goetzel, R. Z. (2010). A systematic review of selected interventions for worksite health promotion. The assessment of health risks with feedback. American Journal of Preventive Medicine, 38 (2 Suppl), S237–S262.
Stock, J., & Cervone, D. (1990). Proximal goal-setting and self-regulatory processes. Cognitive Therapy and Research, 14 (5), 483–498.
Strack, F., & Deutsch, R. (2004). Reflective and impulsive determinants of social behavior. Personality and Social Psychology Review, 8 (3), 220.
Strecher, V. J. (1999). Computer-tailored smoking cessation materials: A review and discussion. Patient Education and Counseling, 36 (2), 107–117.
Strecher, V. J., & Rosenstock, I. M. (1997). The Health Belief Model. In A. Baum et al. (Eds.), Cambridge handbook of psychology, health and medicine . Cambridge: Cambridge University Press.
Strecher, V. J., McEvoy DeVellis, B., Becker, M. H., & Rosenstock, I. M. (1986). The role of self-efficacy in achieving health behavior change. Health Education Quarterly, 13 (1), 73–92.
Strecher, V. J., Kreuter, M., Den Boer, D. J., Kobrin, S., Hospers, H. J., & Skinner, C. S. (1994). The effects of computer-tailored smoking cessation messages in family practice settings. The Journal of Family Practice, 39 (3), 262–270.
Strecher, V. J., Shiffman, S., & West, R. (2005). Randomized controlled trial of a web-based computer-tailored smoking cessation program as a supplement to nicotine patch therapy. Addiction, 100 (5), 682–688.
Strecher, V. J., McClure, J. B., Alexander, G. L., Chakraborty, B., Nair, V. N., Konkel, J. M., Greene, S. M., Collins, L. M., Carlier, C. C., & Wiese, C. J. (2008). Web-based smoking-cessation programs: Results of a randomized trial. American Journal of Preventive Medicine, 34 (5), 373–381.
Suissa, S., & Ernst, P. (2001). Inhaled corticosteroids: Impact on asthma morbidity and mortality. The Journal of Allergy and Clinical Immunology, 107 (6), 937–944.
Sutton, S. (2000). Interpreting cross-sectional data on stages of change. Psychology and Health, 15 (2), 163–171.
Swinburn, B., Egger, G., & Raza, F. (1999). Dissecting obesogenic environments: The development and application of a framework for identifying and prioritizing environmental interventions for obesity. Preventive Medicine, 29 (6 Pt 1), 563–570.
Taylor, S. E., Falke, R. L., Shoptaw, S. J., & Lichtman, R. R. (1986). Social support, support groups, and the cancer patient. Journal of Consulting and Clinical Psychology, 54 (5), 608–615.
Te Poel, F., Bolman, C., Reubsaet, A., & de Vries, H. (2009). Efficacy of a single computer-tailored e-mail for smoking cessation: Results after 6 months. Health Education Research, 24 (6), 930–940.
Thomas, R. (2002). School-based programmes for preventing smoking. Cochrane Database of Systematic Reviews, 4 , CD001293.
Thomas, R., & Perera, R. (2013). School-based programmes for preventing smoking. Cochrane Database of Systematic Reviews, 4 , CD001293.
Thurstone, L. L. (1931). Measurement of social attitudes. Journal of Abnormal and Social Psychology, 26 , 249–269.
Tichenor, P. J., Donohue, G. A., & Olien, C. N. (1970). Mass media flow and differential growth in knowledge. Public Opinion Quarterly, 34 .
Tu, H. T., & Cohen, G. R. (2008). Striking jump in consumers seeking health care information. Tracking Report, 20 , 1–8.
Turner, J. C. (1991). Social influence . Belmont: Wadsworth Publishing.
Tyler-Smith, K. (2006). Early attrition among first time eLearners: A review of factors that contribute to drop-out, withdrawal and non-completion rates of adult learners undertaking eLearning programmes. Journal of Online Learning and Teaching, 2 , 73–85.
Uchino, B. N. (2006). Social support and health: A review of physiological processes potentially underlying links to disease outcomes. Journal of Behavioral Medicine, 29 (4), 377.
USDHHS. (1980). Promoting health/preventing disease: Objectives for the nation . Washington, DC: US Government Printing Office.
USDHHS. (1990). The health benefits of smoking cessation. A report of the Surgeon General’s Office on Smoking and Health . Rockville: U.S. Govt. Printing Office.
Valente, T. W. (2002). Evaluating health promotion programs . New York: Oxford University Press.
van der Velde, F. W., Hooykaas, C., & van der Pligt, J. (1996). Conditional versus unconditional risk estimates in models of AIDS-related risk behaviour. Psychology & Health, 12 (1), 87.
van Keulen, H. M., Mesters, I., Ausems, M., Van Breukelen, G., Campbell, M., Resnicow, K., Brug, J., & De Vries, H. (2011). Tailored print communication and telephone motivational interviewing are equally successful in improving multiple lifestyle behaviors in a randomized controlled trial. Annals of Behavioral Medicine, 41 (1), 104–118.
van Osch, L., Reubsaet, A., Lechner, L., & de Vries, H. (2008a). The formation of specific action plans can enhance sun protection behavior in motivated parents. Preventive Medicine, 47 (1), 127–132.
van Osch, L., Reubsaet, A., Lechner, L., Candel, M., Mercken, L., & De Vries, H. (2008b). Predicting parental sunscreen use: Disentangling the role of action planning in the intention-behavior relationship. Psychology and Health, 23 (7), 829–846.
van Osch, L., Lechner, L., Reubsaet, A., & De Vries, H. (2010). From theory to practice: An explorative study into the instrumentality and specificity of implementation intentions. Psychology & Health, 25 (3), 351–364.
van Stralen, M. M., Kok, G., de Vries, H., Mudde, A. N., Bolman, C., & Lechner, L. (2008). The Active plus protocol: Systematic development of two theory-and evidence-based tailored physical activity interventions for the over-fifties. BMC Public Health, 8 (1), 399.
Vartiainen, E., Puska, P., Koskela, K., Nissinen, A., & Toumilehto, J. (1986). Ten-year results of a community-based anti-smoking program (as part of the North Karelia Project in Finland). Health Education Research, 1 (3), 175–184.
Vassallo, M., Saba, A., Arvola, A., Dean, M., Messina, F., Winkelmann, M., Claupein, E., Lähteenmäki, L., & Shepherd, R. (2009). Willingness to use functional breads. Applying the Health Belief Model across four European countries. Appetite, 52 (2), 452.
Velicer, W. F., Diclemente, C. C., Rossi, J. S., & Prochaska, J. O. (1990). Relapse situations and self-efficacy: An integrative model. Addictive Behaviors, 15 (3), 271–283.
Velicer, W. F., Prochaska, J. O., Bellis, J. M., DiClemente, C. C., Rossi, J. S., Fava, J. L., & Steiger, J. H. (1993). An expert system intervention for smoking cessation. Addictive Behaviors, 18 (3), 269–290.
Velicer, W. F., Prochaska, J. O., & Redding, C. A. (2006). Tailored communications for smoking cessation: Past successes and future directions. Drug and Alcohol Review, 25 (1), 49–57.
Vernon, S. W. (1999). Risk perception and risk communication for cancer screening behaviors: A review. Journal of the National Cancer Institute. Monographs, 25 , 101–119.
Verplanken, B., & Faes, S. (1999). Good intentions, bad habits, and effects of forming implementation intentions on healthy eating. European Journal of Social Psychology, 29 (5-6), 591.
Vries, H. D., & Mudde, A. N. (1998). Predicting stage transitions for smoking cessation applying the attitude-social influence-efficacy model. Psychology and Health, 13 (2), 369–385.
Wagner, T. H., Bundorf, M. K., Singer, S. J., & Baker, L. C. (2005). Free internet access, the digital divide, and health information. Medical Care, 43 (4), 415–420.
Webb, T. L., & Sheeran, P. (2006). Does changing behavioral intentions engender behavior change? A meta-analysis of the experimental evidence. Psychological Bulletin, 132 (2), 249–268.
Webb, T. L., Joseph, J., Yardley, L., & Michie, S. (2010). Using the internet to promote health behavior change: A systematic review and meta-analysis of the impact of theoretical basis, use of behavior change techniques, and mode of delivery on efficacy. Journal of Medical Internet Research, 12 (1), e4.
Weinstein, N. D. (1988). The precaution adoption process. Health Psychology, 7 (4), 355–386.
Weinstein, N. D., & Sandman, P. M. (1992). A model of the precaution adoption process: Evidence from home radon testing. Health Psychology, 11 (3), 170–180.
Weinstein, N. D., Lyon, J. E., Sandman, P. M., & Cuite, C. L. (1998). Experimental evidence for stages of health behavior change: The precaution adoption process model applied to home radon testing. Health Psychology, 17 (5), 445.
WHO. (1978). Declaration of Alma-Ata . International conference on Primary Health Care, Alma-Ata, USSR, 6–12 September. Geneva: WHO.
WHO. (1985). Prerequisites for health. In WHO Regional Office of Europe (Ed.), Targets for all: Targets in support of the European regional strategy for health for all . Copenhagen: WHO Regional Office of Europe.
WHO. (1986). Ottawa charter of health promotion . In Health promotion I , Ottawa.
U.S. Department of Health and Human Services. (2000). Healthy people 2010: Understanding and improving health (2nd ed.). Washington, DC: U.S. Government Printing Office.
WHO. (2013). In J. M. Pelikan, I. Kickbusch, F. Apfel, & A. D. Tsouros (Eds.), Health literacy; solid facts .
WHO, [WHO definition of Health]. (1946). Preamble to the Constitution of the World Health Organization as adopted by the International Health Conference , New York, 19–22 June 1946; signed on 22 July 1946 by the representatives of 61 States (Official Records of the World Health Organization, no. 2, p. 100) and entered into force on 7 April 1948.
Wielm, A. G. (2004). Digital Nation: Towards an inclusive information society (pp. 133–134). Cambridge, MA: MIT Press.
Wiers, R. W., Bartholow, B. D., van den Wildenberg, E., Thush, C., Engels, R. C. M. E., Sher, K. J., Grenard, J., Ames, S. L., & Stacy, A. W. (2007). Automatic and controlled processes and the development of addictive behaviors in adolescents: A review and a model. Pharmacology, Biochemistry, and Behavior, 86 (2), 263–283.
Wiers, R. W., Rinck, M., Kordts, R., Houben, K., & Strack, F. (2009). Retraining automatic action-tendencies to approach alcohol in hazardous drinkers. Addiction, 105 (2), 279–287.
Wilde, M. H., & Garvin, S. (2007). A concept analysis of self-monitoring. Journal of Advanced Nursing, 57 (3), 339–350.
Wilson, M. G., Holman, P. B., & Hammock, A. (1996). A comprehensive review of the effects of worksite health promotion on health-related outcomes. American Journal of Health Promotion, 10 (6), 429–435.
Winett, L. B., & Wallack, L. (1996). Advancing public health goals through the mass media. Journal of Health Communication, 1 (2), 173–196.
Ziegelmann, J. P., Lippke, S., & Schwarzer, R. (2006). Adoption and maintenance of physical activity: Planning interventions in young, middle-aged, and older adults. Psychology & Health, 21 (2), 145–163.
Ziegelmann, J. P., Luszczynska, A., Lippke, S., & Schwarzer, R. (2007). Are goal intentions or implementation intentions better predictors of health behavior? A longitudinal study in orthopedic rehabilitation. Rehabilitation Psychology, 52 (1), 97.
Download references
Author information
Authors and affiliations.
Department of Health Promotion, Maastricht University, Maastricht, The Netherlands
Hein de Vries & Stef P. J. Kremers
Department of Psychology and Methods, Bremen International Graduate School of Social Sciences, Jacobs University Bremen, Bremen, Germany
Sonia Lippke
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Hein de Vries .
Editor information
Editors and affiliations.
Department of Health Behavior, Gillings School of Global Public Health, University of North Carolina at Chapel Hill, Chapel Hill, NC, USA
Edwin B. Fisher
Psychological Sciences, University of California, Merced, Merced, CA, USA
Linda D. Cameron
Department of Psychological and Brain Sciences and Department of Internal Medicine, The University of Iowa, Iowa City, IA, USA
Alan J. Christensen
Department of Clinical Psychology and Psychotherapy, University of Zurich, Zürich, Switzerland
Ulrike Ehlert
School of Public Health, Peking University Health Science Center, Beijing, China
Melbourne School of Population and Global Health, University of Melbourne, Melbourne, Australia
Brian Oldenburg
Departments of Medical Psychology, Academic Medical Center (AMC) and VU University Medical Center (VUMC), Amsterdam, The Netherlands
Frank J. Snoek
Rights and permissions
Reprints and permissions
Copyright information
© 2018 Springer Science+Business Media LLC
About this chapter
de Vries, H., Kremers, S.P.J., Lippke, S. (2018). Health Education and Health Promotion: Key Concepts and Exemplary Evidence to Support Them. In: Fisher, E., et al. Principles and Concepts of Behavioral Medicine. Springer, New York, NY. https://doi.org/10.1007/978-0-387-93826-4_17
Download citation
DOI : https://doi.org/10.1007/978-0-387-93826-4_17
Published : 09 October 2018
Publisher Name : Springer, New York, NY
Print ISBN : 978-0-387-93825-7
Online ISBN : 978-0-387-93826-4
eBook Packages : Behavioral Science and Psychology Behavioral Science and Psychology (R0)
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research
- Search Menu
- Sign in through your institution
- Advance Articles
- Editor's Choice
- Author Guidelines
- Submission Site
- Open Access
- Reasons to publish with us
- About Health Education Research
- Editorial Board
- Advertising and Corporate Services
- Journals Career Network
- Self-Archiving Policy
- Dispatch Dates
- Journals on Oxford Academic
- Books on Oxford Academic
About the Journal
Publishing original, refereed papers, Health Education Research deals with all the vital issues involved in health education and promotion worldwide - providing a valuable link between the health education research and practice communities. Health Education Research gives highest priority to original research focused on health education and promotion research, particularly intervention studies with solid research designs. The journal welcomes rigorous qualitative studies or those that concentrate on hard-to-reach populations. Because of the high number of submissions, cross sectional studies, instrument development, psychometric studies, and pilot data are assigned lower priority. Manuscripts evaluating health professional training programs or clinical research studies are not within the scope of the journal’s themes unless they are directly related to the broad area of changing health behaviors and the conditions that influence health.
Abstracting and Indexing Services
Health Education Research is covered by the following major indexing services: Abstracts in Anthropology Abstracts on Hygiene and Communicable Diseases Addiction Abstracts Applied Social Sciences Index & Abstracts (ASSIA) British Education Index British Nursing Index CAB Abstracts CINAHL Contents Page in Education Current Contents® /Social and Behavioral Sciences Dairy Science Abstracts Education Research Abstracts Educational Management Abstracts Educational Technology Abstracts EMBASE Environmental Science and Pollution Management E-psyche Excerpta Medica Abstract Journals Global Health Health & Safety Science Abstracts Helminthology Abstracts Index Veterinarius Journal Citation Reports /Social Sciences Edition Leisure, Recreation and Tourism Abstracts Multicultural Education Abstracts Nutrition Abstracts and Reviews Periodicals Index Online (PIO) Physical Education Index PROQUEST DATABASE : MEDLINE with Full Text PROQUEST DATABASE : ProQuest 5000 International PROQUEST DATABASE : ProQuest Central PROQUEST DATABASE : ProQuest Health & Medical Complete PROQUEST DATABASE : ProQuest Health Management PROQUEST DATABASE : ProQuest Medical Library PROQUEST DATABASE : ProQuest Nursing & Allied Health Source PROQUEST DATABASE : ProQuest Pharma Collection PROQUEST DATABASE : ProQuest Psychology Journals PROQUEST DATABASE : ProQuest Wilson Databases PROQUEST DATABASE : PsycINFO Database with Full Text PubMed Psychlit Research into Higher Education Abstracts Review of Medical and Veterinary Mycology Rural Development Abstracts Social Sciences Citation Index® Social Scisearch® Sociology of Education Special Education Needs Abstracts Studies on Women and Gender Abstracts (SWA) The Standard Periodical Directory Tropical Diseases Bulletin Vocational Education & Training Abstracts Wilson OmniFile Full Text Mega Edition World Agricultural Economics and Rural Sociology Abstracts
Impact Factor and Indexing
| Year | Impact Factor | Ssi: Education & Educational Research | Ssi: Public, Environmental & Occupational Health |
|---|---|---|---|
| 2023 | 2.100 | 179 out of 756 | 202 out of 403 |
| 2022 | 2.400 | 131 out of 269 | 106 out of 180 |
| 2021 | 2.221 | 153 out of 267 | 128 out of 182 |
| 2020 | 1.538 | 205 out of 265 | 136 out of 176 |
| 2019 | 1.108 | 193 out of 263 | 138 out of 171 |
| 2018 | 1.307 | 145 out of 243 | 116 out of 162 |
| 2017 | 1.479 | 103 out of 238 | 87 out of 156 |
| 2016 | 1.816 | 43 out of 235 | 59 out of 157 |
| 2015 | 1.667 | 36 out of 231 | 58 out of 153 |
| 2014 | 1.574 | 31 out of 224 | 58 out of 145 |
| 2013 | 1.944 | 22 out of 219 | 37 out of 136 |
| 2012 | 1.615 | 22 out of 216 | 50 out of 136 |
| 2011 | 1.656 | 20 out of 203 | 44 out of 131 |
| 2010 | 1.889 | 19 out of 177 | 28 out of 114 |
| 2009 | 2.146 | 8 out of 139 | 20 out of 95 |
| 2008 | 2.310 | 5 out of 112 | 14 out of 76 |
| 2007 | 1.786 | 7 out of 105 | 18 out of 70 |
| 2006 | 1.623 | 6 out of 100 | 24 out of 66 |
Latest information is taken from the Journal Citation Reports (Source Clarivate, 2023)
- Recommend to your Library
Affiliations
- Online ISSN 1465-3648
- Print ISSN 0268-1153
- Copyright © 2024 Oxford University Press
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.

IMAGES
VIDEO
COMMENTS
Extensive scientific research substantiates the crucial role of physical education (PE) in promoting lifelong health and well-being in school-aged youth. PE not only encourages youth to be physically active during classes but also motivates them to adopt healthier lifestyles and engage in regular physical activity (PA) outside of school ...
"As a kidney donor and research scientist in the field, it is reassuring to see the progress we have made," said study co-author Macey L. Levan, JD, PhD, an associate professor in the Departments of Surgery and Population Health at NYU Grossman School of Medicine, and director of the C-STAR Qualitative Core. Dr. Levan, who is also the vice ...
The disruption of health and medical education by the COVID-19 pandemic made educators question the effect of online setting on students' learning, motivation, self-efficacy and preference. In light of the health care staff shortage online scalable education seemed relevant. Reviews on the effect of online medical education called for high quality RCTs, which are increasingly relevant with ...
Interprofessional training in health sciences education has a lasting impact on practice, study shows. ... Apart from any fair dealing for the purpose of private study or research, no part may be ...
This study compliments prior research that people should be offered sexual health and PrEP education at a younger age to increase awareness of risk, foster change in social norms and enhance willingness to seek out prevention services [40, 41]. To meet the resulting growing need for PrEP educators, healthcare professionals should receive up-to ...
Future for the Navajo Health Stomach Project. The Navajo Healthy Stomach Project also found that there was generally a low level of awareness of H. pylori, with only 24% of the participants reporting they had ever heard of the infection.. Their future work will address barriers that prevent people who test positive for H. pylori from getting treatment and expand education through medical ...
The longitudinal study considered documentation practices and weekly visit volume of more than 18,000 outpatient doctors -- mostly primary care physicians and some medical and surgical specialists ...
Professor of Religious Studies Amy Allocco spent the 2023-24 academic year in South India on a Fulbright-Nehru Academic and Professional Excellence Fellowship engaged in research for a project titled "The Drummer-Priests of South India: Intergenerational Learning in a Tamil Performance Tradition.". Allocco's nine-month ethnographic study focused on one hereditary family of Tamil Hindu ...
Health Education Research publishes original, peer-reviewed studies that deal with all the vital issues involved in health education and promotion worldwide—providing a valuable link between the health education research and practice communities. Explore the reasons why HER is the perfect home for your research.
The study found that health education program participants had significantly improved their cognitive examination and memory domain scores when compared with control group participants. These results suggest that health education can expand beyond its traditional uses. ... Research on widespread health education campaigns has occurred; however ...
Health Education Journal is a peer reviewed journal publishing high quality papers on health education as it relates to individuals, populations, groups and communities vulnerable to and/or at risk of health issues and problems. A strongly educational perspective is adopted with a focus on activities, interventions and programmes that work well in the contexts in which they are applied.
Health Education Research gives highest priority to original research focused on health education and promotion research, particularly intervention studies with solid research designs. The journal welcomes rigorous qualitative studies or those that concentrate on hard-to-reach populations. Because of the high number of submissions, cross ...
U.S. studies describing how the education-health association (often referred to as "the gradient") varies across contexts have focused on states (Montez, Hayward, and Zajacova 2019; Montez, Zajacova, et al. 2019). These studies have also offered hypotheses about why the gradient is stronger in some areas than others.
rch within the health education setting has seen a considerable increase in recent years. The limited published literature reviews within the school health e. litera. ureCorresponding author Shona Lee Thorp: [email protected]. 55-67review. One recent leading literature review within the field of research, Dixon and Robertson's ...
The seven articles selected for the review were research studies published in English and between the years 2016 and 2021, thus ensuring an analysis of the results on the application of programs for health promotion was updated. ... The planning and inclusion of health education in the school curriculum give it the continuous and integrated ...
Introduction. This NAM Perspectives paper provides an overview of health education in schools and challenges encountered in enacting evidence-based health education; timely policy-related opportunities for strengthening school health education curricula, including incorporation of essential health literacy concepts and skills; and case studies demonstrating the successful integration of school ...
Health Education & Behavior (HEB) is a peer-reviewed bi-monthly journal that provides empirical research, case studies, program evaluations, literature reviews, and discussions of theories of health behavior and health status, as well as strategies to improve social and behavioral health.HEB also examines the processes of planning, implementing, managing, and assessing health education and ...
A clear understanding of the macro-level contexts in which education impacts health is integral to improving national health administration and policy. In this research, we use a visual analytic approach to explore the association between education and health over a 20-year period for countries around the world. Using empirical data from the OECD and the World Bank for 26 OECD countries for ...
reviews health education theories and definitions, identifies the components of evidence-based health education and outlines the abilities necessary to engage in effective practice. Much has been written over the years about the relationship and overlap between health education, health promotion and other concepts, such as health literacy.
2.1. Educational Goals. The adaptive goal mainly focuses on the students' present, so that students can understand the changing trends and characteristics of the future society, help them establish a long-term and stable outlook on life, values, and world outlook in line with the direction of social progress, and pursue high-level life meaning and guide them through various abilities.
Self-assessed health is a well-established index of morbidity and predictor of mortality. 32,33 A recent study compares the association of educational attainment with self-assessed health in US and Canadian populations. 34,35 Controlling for basic demographics and income, those with less than a high school education in the United States are 2.4 ...
Abstract. Health education is the main, and at the same time, integral part of complementary health promotion. The main assumption. underlying the essence of health education is an assertion that ...
URGENT NEED FOR NEW DIRECTIONS IN EDUCATION-HEALTH RESEARCH. Americans have worse health than people in other high-income countries, and have been falling further behind in recent decades ().This is partially due to the large health inequalities and poor health of adults with low education ().Understanding the health benefits of education is thus integral to reducing health disparities and ...
Multiple studies have investigated the role of attitudes for several health behaviors. Studies have also examined which variables or beliefs distinguish a healthy group from an unhealthy group (Godin & Kok, 1996). For instance, ... Health Education Research, 20(5), 527-539.
Certified Health Education Specialist (CHES) creden tial to its first group of individuals in 1990. A bach elor's degree with at least 25 semester hours of concentrated study in health education is now required to sit for the CHES examination. However, it is in the Authors' Note: Please address correspondence to Elizabeth K.
Abstract. To focus on the benefits and importance of research to the practice of health education. The paper discussed the potential of quality research as well as the barriers that keep health ...
Health Education Research gives highest priority to original research focused on health education and promotion research, particularly intervention studies with solid research designs. The journal welcomes rigorous qualitative studies or those that concentrate on hard-to-reach populations. Because of the high number of submissions, cross ...
Key messages. The goal of Health 2020 is to significantly improve the health and well-being of populations, reduce health inequalities, strengthen public health and ensure people-centred health systems that are universal, equitable, sustainable and of high quality. 1. Health and wellbeing are public goods and assets for human development that ...
Leading educators and health professionals have long documented the interdependent relationship between health and education (Basch, 2011; Institute of Medicine, 1997; Kolbe, 2019).School-age children and adolescents experiencing health issues such as stress, physical and emotional abuse, hunger, safety concerns, vision, hearing or dental problems, asthma, or other chronic illnesses have ...
While numerous studies assess the relationship between education and health, no consensus has been reached on whether education really improves health. We perform a meta-analysis of 4866 estimates gleaned from 99 published studies that examine the health effects of education.